Abstract
Objectives
We aimed to estimate the pooled prevalence of erectile dysfunction (ED) among patients with diabetes mellitus (DM) in Ethiopia and to identify its associated factors.
Methods
We performed a systematic search of scientific databases (PubMed, ScienceDirect); the grey literature was also searched (Google, Google Scholar). Data were extracted from primary studies using a data extraction format and exported for statistical analysis. I2 tests were used to assess the heterogeneity of studies. Owing to heterogeneity among the included studies, we used a random-effects model to determine pooled estimates of ED. Publication bias was assessed using Egger’s and Begg’s tests.
Results
The pooled prevalence of ED among patients with DM in Ethiopia was 54.3% (95% confidence interval [CI]: 28.2–80.5). Older age (OR: 4.42, 95% CI: 2.83–6.00) and duration of DM (OR: 3.2, 95% CI: 1.74–4.66) had statistically significant associations with ED.
Conclusion
One in two individuals with DM in Ethiopia also had ED. This finding highlights the need to integrate assessment and management of ED into routine medical care in diabetes follow-up visits. Special attention is recommended for patients with older age and a longer duration of DM.
Keywords: Erectile dysfunction, diabetes mellitus, risk factor, Ethiopia, older patient, diabetes management
Introduction
Diabetes mellitus (DM) is a chronic disease that affects nearly every organ in the human body. DM is a major public health problem in both developed and developing countries. Globally, the prevalence of diabetes is increasing at an alarming rate, affecting 463 million people. The World Health Organization has projected that 300 and 700 million people will develop DM by 2025 and 2045, respectively.1,2 Erectile dysfunction (ED) is one of the most common but underdiagnosed complications of DM.3
ED, also called impotence, is a condition characterized by the inability to initiate and maintain an erection firm enough to have satisfying sexual intercourse. ED is common in men who have diabetes, particularly those with type 2 diabetes. The onset of ED also occurs 10 to 15 years earlier in men with diabetes than it does in sex-matched counterparts without diabetes. Studies indicate that the ED prevalence in men with diabetes ranges from 35% to 75% versus 26% in the general population.3,4
At least some degree of ED is experienced by 35% to 75% of men with diabetes globally. The prevalence of ED among men with diabetes is over 50% in the United States, 35% to 78% in Mexico, 41% in The Netherlands, and 80% to 90% in Saudi Arabia.5,6 In Africa, evidence from a systematic review and meta-analysis showed that the ED prevalence ranges from 36% to 95%, with pooled prevalence of 71.45%.7 In Ethiopia, the prevalence of ED among patients with diabetes ranges from 6.8% to 85.5%.8,9
ED can stem from organic causes including hormone-induced, drug-induced, vascular, traumatic or post-surgical, and psychogenic causes including depression, relationship problems, and performance anxiety. ED is also linked to other conditions common in men with diabetes, such as high blood pressure and heart disease. ED has a substantial negative physical, psychological, and social impact on patients with diabetes and can affect their quality of life.10,11
Owing to an inability to recognize ED as a common consequence of DM that should be addressed and treated, providers are missing an important opportunity to improve their patients' quality of life.3 Despite the negative impact of ED on quality of life in patients with diabetes, talking openly about sexually related issues is taboo in Ethiopia. Because of this, most patients fear discussing sexual problems with their doctor or partner. Health care providers often do not ask male patients with diabetes about their sexual function owing to societal norms. This leads to sexual disorders being under-recognized and under-treated in this country.
Although some studies have reported the prevalence and predictors of ED among people with diabetes in Ethiopia, the magnitude of these studies is inconsistent and great variability has been observed.8,9 Moreover, nonexistence of country-wide data that represent the national ED prevalence and its determinant factors is a considerable research gap. Therefore, in this systematic review and meta-analysis, we aimed to estimate the pooled prevalence of ED among people with diabetes in Ethiopia. This finding will be helpful for policymakers, health personnel, and other stakeholders, to help reduce the negative consequences of ED by designing appropriate preventive and interventional programs for people with DM.
Methods
Protocol and registration
The results of this systematic review and meta-analysis were reported based on the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) statement.12We used the PRISMA flowchart to depict the selection process, from the initially identified articles to the finally included studies. The protocol for this review is registered on the International Prospective Register of Systematic Reviews (PROSPERO) with reference number CRD42020201825.
Because this review was concerned with published research articles, there was no need to obtain ethical approval or informed consent from participants.
Search strategy
A preliminary search was conducted using scientific databases, including PubMed and ScienceDirect. To identify additional articles, we performed a search of the grey literature using Google and Google Scholar. Endnote X 8.1 reference manager software was used to collect and organize the search results and to remove duplicate articles. The searches were restricted to free full-text articles reporting human studies in English language. All relevant articles available online through 1 August 2020 were considered.
Articles related to the prevalence and/or associated factors of ED among patients with diabetes were retrieved. We used combinations of the following key terms in the search: “erectile dysfunction”, “sexual function”, “sexual dysfunction”, “impotence”, “diabetes mellitus”, “risk factors”, “determinants”, “predictors” and “Ethiopia”.
Eligibility criteria
Inclusion criteria
All observational studies conducted on the prevalence of ED among patients with DM in Ethiopia, published prior to 1 August 2020 that were accessible and written in English were eligible for inclusion in the current systematic review and meta-analysis.
Exclusion criteria
We excluded articles that were not fully accessible, duplicate reports possessing a low quality score per the stated criteria, and case series.
Data extraction process
A data extraction template was used to extract the data including author names, year of publication, study design, sample size, sampling technique, prevalence of ED, number of events, and diagnostic criteria used for ED. Data from selected articles were extracted and presented in Microsoft Excel.
Outcome measures
The prevalence of ED and determinant factors were the outcome variables in this systematic review and meta-analysis. Predictors of ED among patients with diabetes were assessed using odds ratios (ORs).
Quality assessment
The quality of primary studies included in this systematic review and meta-analysis were assessed using the Newcastle–Ottawa Scale, adapted for cross-sectional study quality assessment.13 This scale is used to assess the methodological quality of each study, the comparability of primary studies, and the quality of original articles with respect to statistical analysis. Two group of authors (BST, SAK) and ABW evaluated the quality of each original article independently using this assessment tool. Inconsistencies between assessors were resolved through discussion, and the average score of different assessment results were used. Articles fulfilling at least 50% of the quality assessment criteria were included in this review.
Statistical analysis
Data analysis was carried out using Stata/SE version 16 (StataCorp LLC, College Station, TX, USA). Heterogeneity among reported prevalence results was assessed by computing p-values for the I2 statistic.14 The pooled prevalence of ED was carried out using a random-effects meta-analysis model. To deal with heterogeneity among primary studies, we used a random-effects model. Publication bias was assessed using a funnel plot and the Egger’s test with a 5% significance level. Point prevalence with 95% confidence interval (CI) was presented in forest plot format.
Results
Search results
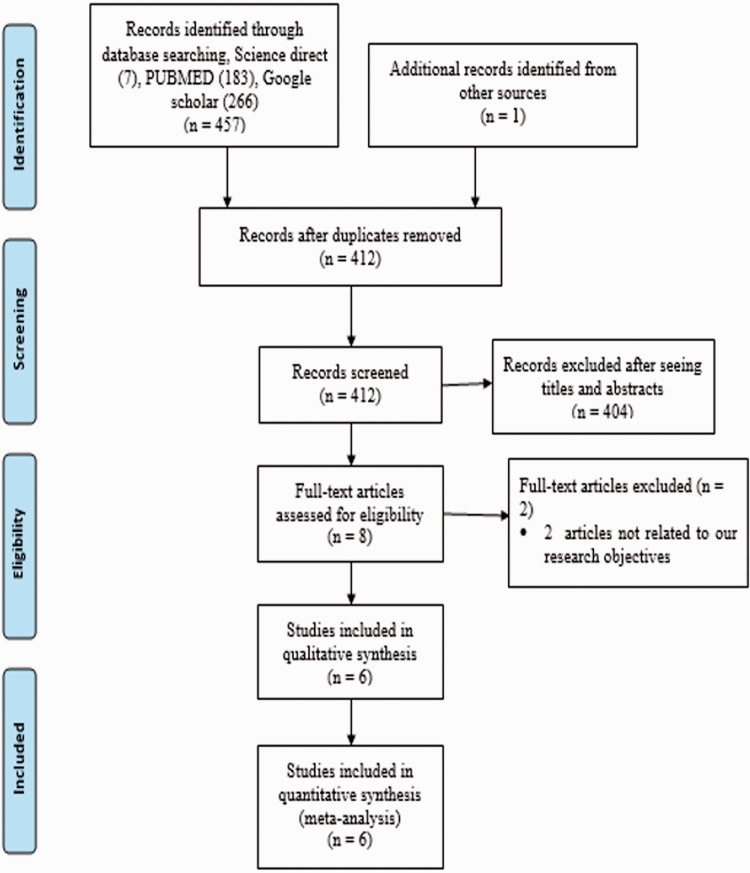
In the first step, 457 articles were retrieved from scientific databases (PubMed = 183, ScienceDirect = 7). An additional 267 articles were also identified from other sources (Google Scholar and Google). After removing duplicates, 412 articles were considered eligible for title and abstract evaluation. Of these, 398 articles were excluded and the remaining 14 articles were considered for further full-text evaluation. A full-text article review resulted in further exclusion of two articles owing to differences in the outcomes of interest. Finally, 6 papers met the eligibility criteria and were included in the systematic review and meta-analysis (Figure 1).
Figure 1.
PRISMA flowchart showing the selection of primary studies.
Characteristics of included studies
All studies included in this systematic review and meta-analysis had a cross-sectional study design.8,9,15–18 The minimum sample size among the included studies was 192 patients from a study in Jimma8 and the maximum sample size was 423 patients from a study in Mizan–Tepi.15 Six studies were included, with a total sample size of 2003 participants, to estimate the pooled prevalence of ED among patients with diabetes in Ethiopia. These studies were published between 20108 and 2020.16 Of the included studies, three were conducted in Oromia,8,15,16 two in the Amhara region9,18 (one from the grey literature), and one in the Tigray region.17
Except for the study from Mizan–Tepi15 with a response rate of 94%, the response rate of the remaining five studies was 100%.8,9,16–18 The mean age of patients in the six studies included in this systematic review and meta-analysis ranged from 41.76 (±9.00) years15 to 54.12 (±16.51) years. Regarding assessment tools of ED, four studies9,16–18 (the Gondar study was from the grey literature) used the International Index of Erectile Function (IIEF-5), and one study used the 14-item Sexual Functioning Questionnaire (CSFQ-14).15 The instrument used was not reported in one study8 (Table 1).
Table 1.
Baseline characteristics of studies included in the systematic review and meta-analysis of erectile dysfunction prevalence among patients with diabetes in Ethiopia, 2020.
| Authors (Reference) | Publication year | Study area/region | Study design | Sample size | Instrument | Response rate | Age, y (mean ± SD) | Prevalence |
|---|---|---|---|---|---|---|---|---|
| Seid A et al.17 | 2017 | Tigray | Cross-sectional | 249 | IIEF-5 | 100% | 43.39 ± 14.7 | 69.90% |
| Hurisa AD & Negera GZ16 | 2020 | Oromia | Cross-sectional | 350 | IIEF-5 | 100% | 47.90 ± 12.2 | 60.40% |
| Asefa A et al.15 | 2019 | Oromia | Cross-sectional | 423 | CSFQ-14 | 94% | 41.76 ± 9.00 | 53.30% |
| Tesfaye T et al.18 | 2020 | Amhara | Cross-sectional | 367 | IIEF-5 | 100% | 54.12 ± 16.51 | 53.10% |
| Walle B et al.9 | 2018 | Amhara | Cross-sectional | 422 | IIEF-5 | 100% | 45.70 ± NR | 86% |
| Worku D et al.8 | 2010 | Oromia | Cross-sectional | 192 | NR | 100% | 44.40 ± 15.6 | 6.8% |
IIEF-5: International Index of Erectile Function; NR: not reported; CSFQ-14: 14-item Changes in Sexual Functioning Questionnaire; SD: standard deviation.
Meta-analysis of erectile dysfunction (ED) in Ethiopia
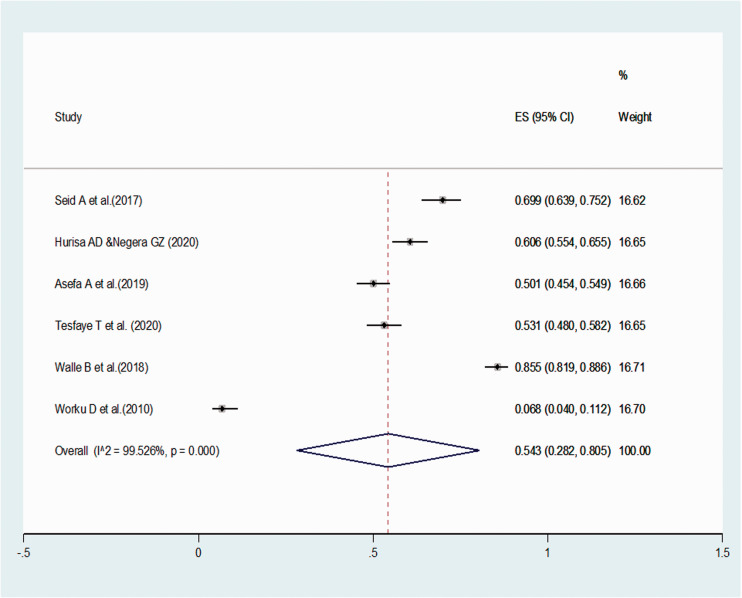
The pooled prevalence of ED among patients with diabetes in Ethiopia was 54.3% (95% CI: 28.2, 80.5). Because of significant heterogeneity across the included studies (I2 = 100%, p < 0.001), a random-effects meta-analysis model was used to estimate the pooled prevalence of ED in Ethiopia. In this meta-analysis, the highest prevalence was 85.5% (95% CI: 81.9, 88.6), reported in the study by Walle et al.9 The lowest prevalence of 6.8% (95% CI: 4.0, 11.2) was reported by Worku et al.8 (Figure 2).
Figure 2.
Pooled estimated prevalence of erectile dysfunction among patients with diabetes in Ethiopia, 2020.
Factors associated with ED
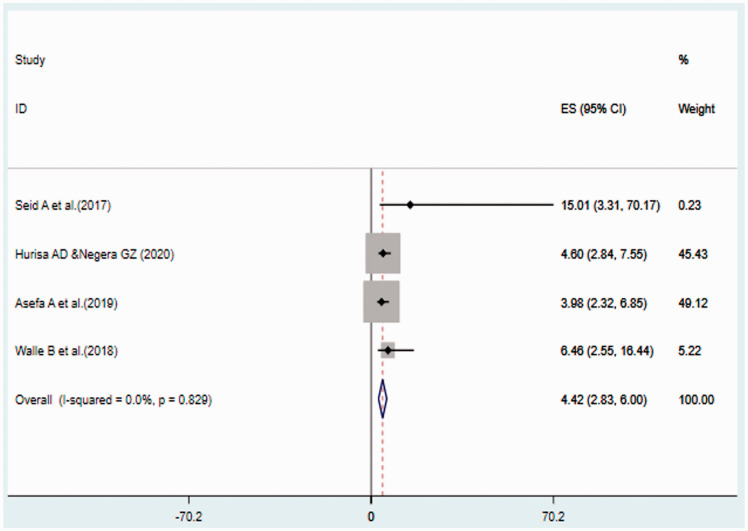
Five of the six studies included in this systematic review and meta-analysis reported factors associated with ED among patients with diabetes. In more than one study, these factors were duration of diabetes, type of DM, and age of study participants. The pooled meta-analysis using four studies revealed that being over the age of 40 years was significantly associated with ED among patients with diabetes. Patients aged over 40 years were 4.42 times more likely to develop ED than those aged less than 40 years (pooled OR: 4.42, 95% CI: 2.83, 6.00) (Figure 3).
Figure 3.
Forest plot of pooled odds ratios between age and erectile dysfunction among patients with diabetes in Ethiopia.
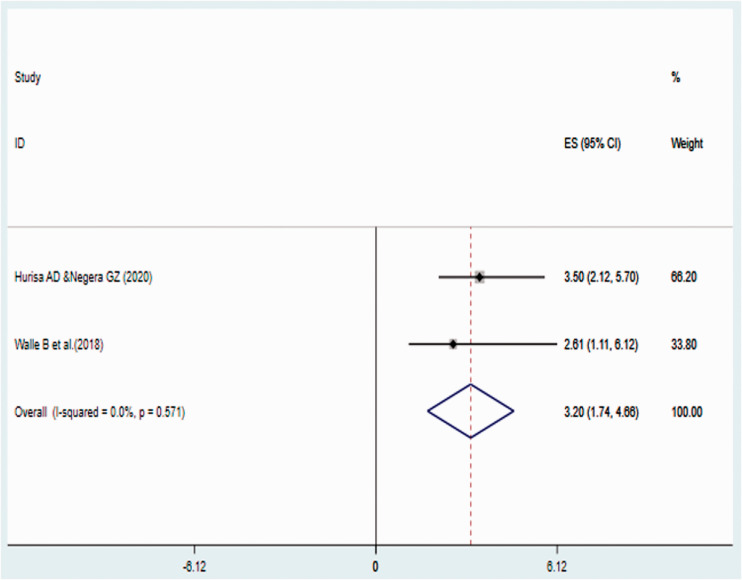
In the study, the duration of DM was significantly associated with ED. An aggregated meta-analysis using two studies indicated that patients with a longer duration of DM (more than 5 years) had a 3.2-times higher odds of developing ED than those with DM for less than 5 years (pooled OR: 3.2, 95% CI: 1.74, 4.66) (Figure 4).
Figure 4.
Forest plot of pooled odds ratios between duration of diabetes mellitus and erectile dysfunction among patients with diabetes in Ethiopia.
Publication bias
Small-study effects were assessed using Egger’s and Begg’s tests and the results showed no evidence of publication bias among the included studies (p = 0.612 and 0.848, respectively). However, it should be noted that the funnel plot and Egger's test are less reliable when the number of studies is less than 10.
Discussion
There are several studies regarding the magnitude and associated factors of ED among patients with diabetes in Ethiopia. This is the first systematic review and meta-analysis to assess the prevalence and associated factors of ED among patients with diabetes in the country. However, we observed large variation and inconsistencies in the reported results across these primary studies. For example, the highest (85.5%) and the lowest (6.80%) prevalence were reported in the Amhara9 and Oromia region,8 respectively.
This systematic review and meta-analysis showed that the pooled prevalence of ED among patients with DM in Ethiopia was 54.3% (95% CI: 28.2, 80.5). The magnitude of ED in this systematic review and meta-analysis was lower than the findings from a systematic review and meta-analysis done globally (59.1%)19 and in Africa (71.45%).7 This disparity might be owing to differences in the number of study participants. The number of patients in the current systematic review and meta-analysis was low compared with those previous two reviews, which might contribute to the lower prevalence of ED in the current study. Cultural norms in Ethiopia might also be a contributing factor; ED is under-recognized because of societal norms.
Subgroup analysis was also performed based on the geographical area in which each study was conducted. Accordingly, a higher pooled prevalence of ED (69.50%) was observed among studies in the northern part of the country and lower ED prevalence (40.17%) was found among studies in the southern part of Ethiopia. This could be explained by most included patients with DM from the north of the country being older, which makes the occurrence of ED more likely.
In this study, factors associated with ED were also identified among people with DM. The meta-analysis results showed that the type of DM, patient age, and duration of DM had statistically significant associations with ED among participants with DM. Patients with diabetes aged more than 40 years were 4.42 times more likely to develop ED than those aged less than 40 years. This finding is in line with a previous meta-analysis.20 This significant association can possibly be explained by age-related physiological changes in the testicles and declining sex hormones in older men.21
The duration of DM was also significantly associated with ED among patients with diabetes, which is in agreement with previous studies.20,22,23 Patients with a long duration of DM (more than 5 years) had a 3.2-times greater odds of developing ED than those patients who had DM for less than 5 years. A possible explanation for this is that patients living with DM for a longer time have an increased risk of DM-related complications and other comorbidities, as well as poor glycemic control, which can affect sexual function. Moreover, the risk of micro- and macrovascular complications increases over time, giving rise to diabetes-related ED that is mostly neurogenic and vasculogenic in etiology.20
Strengths and limitations of the study
This review was conducted with rigorous adherence to the PRISMA statement. The main limitation of this meta-analysis is the difficulty in determining whether the results are nationally representative of Ethiopia as the included primary studies were only from three administrative regions of the country. The other limitation is that this was a hospital-based study and patients presenting for medical care may differ from the general population in unpredictable ways.
Conclusions
In this study, we found that one in every two individuals with diabetes in Ethiopia also had ED. This finding highlights the need to integrate assessment and management of ED into routine medical care provided in follow-up clinics for patients with DM. Special attention by health care providers is recommended for older patients and those with a longer duration of DM.
Footnotes
Authors’ contributions: ABW had a primary role in conceptualization, data review, data extraction, data analysis, and writing and editing of this manuscript. BST and SAK had a role in data review, data extraction, and writing and editing of this manuscript. All the authors approved the final version of the manuscript.
Declaration of conflicting interest: The authors declare that there is no conflict of interest.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
ORCID iD: Adisu Birhanu Weldesenbet https://orcid.org/0000-0003-3964-4252
References
- 1.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025: prevalence, numerical estimates, and projections. Diabetes Care 1998; 21: 1414–1431. [DOI] [PubMed] [Google Scholar]
- 2.Saeedi P, Petersohn I, Salpea P, et al. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: Results from the International Diabetes Federation Diabetes Atlas. Diabetes Res Clin Pract 2019; 157: 107843. [DOI] [PubMed] [Google Scholar]
- 3.David FP, Hunter W. Erectile Dysfunction in Diabetic Patients. Diabetes Spectr 2004; 17: 225–230. [Google Scholar]
- 4.Chu NV, Edelman SV. Diabetes and erectile dysfunction. Clin Diabetes 2001; 19: 45–47. [Google Scholar]
- 5.Sharifi F, Asghari M, Jaberi Y, et al. Independent predictors of erectile dysfunction in type 2 diabetes mellitus: Is it true what they say about risk factors? ISRN Endocrinol 2012; 2012: 502353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Díaz-Díaz E, Salinas CA, Timossi CM, et al. Erectile dysfunction: a chronic complication of the diabetes mellitus. INTECH Open Access Publisher, 2012. [Google Scholar]
- 7.Shiferaw WS, Akalu TY, Aynalem YA. Prevalence of erectile dysfunction in patients with diabetes mellitus and its association with body mass index and glycated hemoglobin in Africa: a systematic review and meta-analysis. Int J Endocrinol 2020; 2020: 5148370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Worku D, Hamza L, Woldemichael K. Patterns of diabetic complications at jimma university specialized hospital, southwest ethiopia. Ethiop J Health Sci 2010; 20: 33–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Walle B, Lebeta KR, Fita YD, et al. Prevalence of erectile dysfunction and associated factors among diabetic men attending the diabetic clinic at Felege Hiwot Referral Hospital, Bahir Dar, North West Ethiopia, 2016. BMC Res Notes 2018; 11: 130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Chu NV, Edelman SV. Diabetes and erectile dysfunction. Curr Diab Rep 2001; 19: 45–47. [DOI] [PubMed] [Google Scholar]
- 11.Nelson CJ. The impact of male sexual dysfunction on the female partner. Curr Sex Health Rep 2006; 3: 37–41. [Google Scholar]
- 12.Liberati A, Altman DG, Tetzlaff J, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 2009; 6: e1000100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25: 603–605. [DOI] [PubMed] [Google Scholar]
- 14.Rücker G, Schwarzer G, Carpenter JR, et al. Undue reliance on I 2 in assessing heterogeneity may mislead. BMC Med Res Methodol 2008; 8: 79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Asefa A, Nigussie T, Henok A, et al. Prevalence of sexual dysfunction and related factors among diabetes mellitus patients in Southwest Ethiopia. BMC Endocr Disord 2019; 19: 141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hurisa AD, Negera GZ. Erectile Dysfunction among Diabetic Patients in a Tertiary Hospital of Southwest Ethiopia. Open Publ Health J 2020; 13. [Google Scholar]
- 17.Seid A, Gerensea H, Tarko S, et al. Prevalence and determinants of erectile dysfunction among diabetic patients attending in hospitals of central and northwestern zone of Tigray, northern Ethiopia: a cross-sectional study. BMC Endocr Disord 2017; 17: 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tesfaye T, Bayisa M, Mesfin N. Prevalence and associated factors of erectile dysfunction among men DM patients in Gondar University Hospital, Gondar Ethiopia. Research Square 2020.
- 19.Kouidrat Y, Pizzol D, Cosco T, et al. High prevalence of erectile dysfunction in diabetes: a systematic review and meta‐analysis of 145 studies. Diabet Med 2017; 34: 1185–1192. [DOI] [PubMed] [Google Scholar]
- 20.Mulligan T, Frick M, Zuraw Q, et al. Prevalence of hypogonadism in males aged at least 45 years: the HIM study. Int J Clin Pract 2006; 60: 762–769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mutagaywa RK, Lutale J, Aboud M, et al. Prevalence of erectile dysfunction and associated factors among diabetic men attending diabetic clinic at Muhimbili National Hospital in Dar-es-Salaam, Tanzania. Pan Afr Med J 2014; 17: 227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Cho N, Ahn C, Park J, et al. Prevalence of erectile dysfunction in Korean men with type 2 diabetes mellitus. Diabet Med 2006; 23: 198–203. [DOI] [PubMed] [Google Scholar]
- 23.Kalter-Leibovici O, Wainstein J, Ziv A, et al. Clinical, socioeconomic, and lifestyle parameters associated with erectile dysfunction among diabetic men. Diabetes Care 2005; 28: 1739–1744. [DOI] [PubMed] [Google Scholar]