Abstract
Critical care scientists are a little known but increasingly prominent group of professionals, included in both the government-run Modernising Scientific Careers initiative and 2019 Guidelines for the Provision of Intensive Care Services. This article outlines the role of critical care scientists, their training programme and potential future directions for the role. A wider appreciation and acknowledgement of the critical care scientist’s role within the multi-disciplinary team will allow critical care units to fully understand the potential benefits that may be brought to patient care and service delivery.
Keywords: Healthcare science, critical care scientist, technologist, clinical scientist, intensive therapy unit, ITU, allied health professions
Introduction
As the NHS moves towards the digital age, and medical advances incorporate more technology in healthcare, there has become a pressing need for an innovative workforce to bridge the technical, scientific and clinical aspects of care delivery. The exploration of innovative roles within the multi-disciplinary team (MDT) has been further encouraged by nursing and medical staff shortages. To this effect, the government has launched the Modernising Scientific Careers initiative, which covers the training and recognition of critical care scientists (CCS). The current healthcare scientist workforce now makes up over 50,000 personnel in the NHS and public health services, contributing to approximately 80% of all clinical diagnoses and conducting over 1 billion diagnostic tests each year, and is one of the fastest growing staff groupings.1–3 Historically, the performance of tasks undertaken by a CCS belonged to the nurses and doctors, who were expected to trial and use any medical equipment needed to provide patient care. The expansion of medical technology over the last few decades has made this more challenging and complex for the already busy units to keep abreast of. The need for a group of equipment ‘super users’ has appeared, to provide around-the-clock assistance, as well as have the scientific understanding of key principles behind novel interventions required to direct innovation and research. The CCS role, which has emerged to address these needs, crucially involves understanding the science underpinning advanced therapies, combining it with in-depth technical understanding of medical equipment and applying this to a broad range of clinical situations. Hence, the title ‘Scientist’ superseded ‘Technologist’ (as exemplified by the name change of the CCS professional society’s journal),4 as the role of the CCS is not restricted to the provision of technical support, but encompasses expert clinical knowledge in the application of technology to physiological problems. The profession has now gained its own chapter in the 2019 Guidelines for the Provision of Intensive Care Services.5 There have also been recent role promotional materials that have gained attention through Twitter and the Academy for Healthcare Science media.6 This article explores the role and future of CCS.
CCS have advanced scientific and clinical knowledge of specialist equipment that provides specialist therapies, advanced monitoring and diagnostics. CCS provide front-line equipment troubleshooting, assistance with intra-hospital transfers, as well as patient stabilisation, and provide an on-call or 24-h service. The CCS team is responsible for diagnostics such as clotting profiles and arterial blood gas analysis; maintaining equipment, conducting local and national quality assurance as well as performing and interpreting these specialist tests. CCS are heavily involved with the equipment lifecycle across all critical care areas; including procurement, maintenance, new technology trials, and incident investigation. As such, CCS provide a crucial link between medical engineering and clinical staff on the unit, ensuring safe and effective functionality of all critical care equipment. CCS are often called upon to facilitate complex clinical solutions that have not been explored before, and are uniquely placed to derive safe and effective solutions to the patient’s holistic needs. CCS often adopts specialist roles to match the patient needs across the varied units in which they work, including specialist Intensive Care Units, Operating Theatres and Emergency Departments. Such roles may include paediatric retrievals, transcranial Doppler services, supporting long-term ventilation in the community, as well as bronchoscopies, and response to major trauma and hospital cardiac arrest calls (Table 1). The exact tasks performed will vary between centres, as will the extent of CCS involvement in specific activities (ranging from equipment set-up, to managing aspects of therapies). The Society of Critical Care Technologies (formerly Society of Critical Care Technologists) is the professional body that represents the profession.7
Table 1.
A non-exhaustive list of the various duties provided as part of critical care science service delivery across different locations in the UK.
| Monitoring and diagnostics (including troubleshooting) | Therapeutic and supportive interventions | Equipment management | Other |
|---|---|---|---|
| Pulse oximetry, electrocardiography, end-tidal and transcutaneous CO2 monitoring, invasive and non-invasive blood pressure monitoring | Ventilation modes and settings | Data download | Transfers/scans |
| Electroencephalography including derivative technologies like Cerebral Function Monitoring and depth of anaesthesia monitoring | Nebulisers | Major incident planning and support | Retrieval services |
| Cardiac output (calibrated and non-calibrated) | High frequency oscillation | Clinical incident investigation | Participation in crash teams |
| Rotational viscoelastic haemostatic assays | Nitric oxide therapy | Standard operating procedures and protocol development | Clinical research |
| Transcranial Dopplers | Extracorporeal CO2 removal | National equipment safety alert assessment | Healthcare scientist role promotion |
| Focused intensive care echocardiography | Nasal high flow | New technology specification writing | Multidisciplinary education |
| Bronchoscopy | Non-invasive ventilation | Service improvements – new technology | External quality assurance and monitoring |
| Intra-abdominal pressure monitoring | Renal replacement therapy | Cardiopulmonary exercise testing | |
| Intra-cranial pressure monitoring | Targeted temperature management systems | Vascular access Support | |
| Arterial blood gases |
Note: This list has been compiled on the basis of the authors’ work across different locations and their interaction with CCS from other centres.
In locations without a dedicated CCS presence, the tasks of a CCS are split between the MDT with a large contribution from dedicated intensive care nurses who have additional technological training, known as “nurse techs.” As such, there is considerable variation in the service provided, depending on the hospital structure and the specific services it is commissioned to provide. The CCS team in Manchester has become successfully embedded within the MDT across all adult and paediatric critical care areas. Below, a Consultant and Research Nurse provide overviews of their interaction with CCS.
Within the Paediatric Critical Care Unit, CCS are becoming an increasingly indispensable part of the MDT; the CCS team provides a reliable service facilitating the safe application of technologically advanced diagnostic, monitoring and therapeutic equipment. With the high turnover rates of junior medical and nursing staff in critical care areas, the CCS team represent a consistent resource with a level of experience and expertise in maintaining, deploying, optimally using and trouble-shooting equipment that cannot be matched by other professional groups. As such the CCS team are uniquely positioned to improve direct patient care, educate their partners within the MDT, conduct original research, and work with partners in industry to evaluate innovative products. In the past, the ability of clinicians to optimally deploy complex technological equipment was often limited by their personal knowledge and the availability of specific members of staff; this led to unacceptable variations in clinical care. With the evolution of consistent, 24-h a day CCS team support across critical care areas, patients will benefit from the timely application of advanced equipment and will receive high quality, safer medical care – Paediatric Critical Care Consultant.
Achieving best clinical practice requires new knowledge, and we view the role of the CCS to be an essential element in our team to improve patient outcomes and accelerate the adoption of research and innovation into practice. By analysing and reviewing scientific literature, and clinically evaluating new critical care technologies, we work as a team to manage service development in clinical practice, and determine the impact for future development in paediatric critical care. The role of the healthcare scientist role is critical and invaluable in developing innovative treatments and care for the future, and the evolving health care needs of our patients and their families, and their contribution to research and innovation should be widely supported to foster their growth – Paediatric Critical Care Research Nurse.
Training structure
The Scientist Training Programme (STP) is a graduate-entry scheme involving a part-time MSc in Clinical Science. Currently, the academic component for the CCS STP is only delivered by Manchester Metropolitan University, though the practical component has so far been delivered across four sites (four trained at Manchester, two trained at Southampton, one at Papworth and one at Portsmouth). STP CCS trainees complete a portfolio of competences accompanied by professional examinations, alongside full-time supernumerary NHS employment, traditionally at Band 6.8 Once qualified, a registered Clinical Scientist is expected to progress to/ or becomes eligible to apply for band 7 posts.9
The CCS STP course is delivered alongside other Clinical Science specialisms, especially others also belonging to the physiology grouping of Healthcare Science specialisms, in particular Cardiac Science, and Respiratory and Sleep Science.9,10 Throughout the course trainees complete a professionalism module, an elective where trainees can spend up to six weeks exploring a clinical area of their interest, e.g. work in a different country, a hospital with a different structure, or within a different service that links with critical care. Trainees also complete a research project spanning two academic years, life support training,11 and specialist modules involving both work-based and university assessments (Figure 1).10 The training structure ensures that STP graduate CCS do not only have the technical skills to work within the critical care environment, but also have the necessary clinical physiology knowledge to provide advice to the medical and nursing teams, as well as the necessary soft skills to navigate the healthcare environment.
Figure 1.
Flow diagram detailing the STP structure. STP: Scientist Training Programme.
There are currently no opportunities open to non-graduates to enter the clinical scientist pathway in critical care due to a lack of a Practitioner Training Programme (PTP). The PTP is an undergraduate science degree that produces students ready to undertake roles such as cardiac and respiratory physiologists. Apprenticeship opportunities are currently being explored and would provide a long-term flow of ‘trained on the job’ personnel to enhance CCS departments.
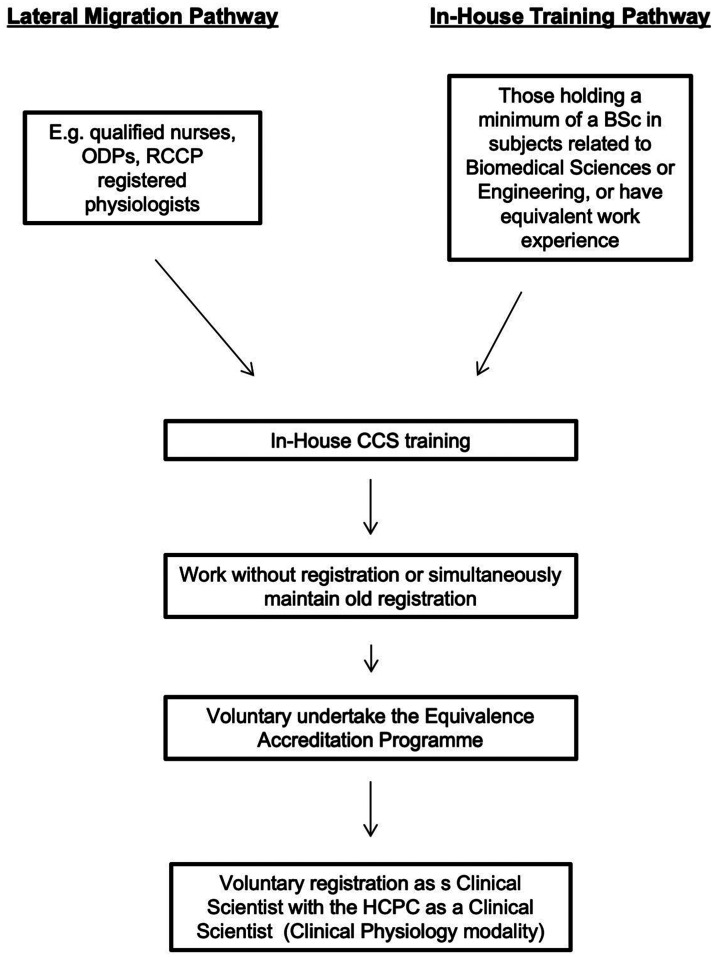
The CCS STP has only been introduced in the last 10 years, and most CCS working in the UK have not completed the programme. Traditionally, staff would come from a medical physics and physiological measurement background (the forerunner to many modern healthcare specialisms), and nowadays there is still a lot of lateral migration into the role, with people coming in from both clinical and scientific/engineering backgrounds (Figure 2). Those who have entered the profession via the in-service route can choose to complete an equivalence programme, which will allow them to register with the Health and Care Professionals Council (HCPC) through completion of a portfolio proving that they possess the skills and knowledge equivalent to STP graduates, and without the need to complete the MSc. While currently registration with the HCPC is not compulsory, this might change in the future with the constant emphasis on central reassurances for patient safety and fitness to practice accreditations. It is hoped that more established staff will take the equivalence route to help to raise the profile of the profession.
Figure 2.
Flow diagram detailing the lateral migration and in-house training structures.
Comparison with other professions and countries
To show the extent of the clinical training as well as to give a better picture of the role to those not based in the UK, it is worth comparing the STP CCS programme with other professions.
The STP is a MSc level graduate entry programme with concurrent employment and on-the-job clinical training; as such it is largely similar to the Advanced Critical Care Practitioner (ACCP) training structure or Perfusionist training.12,13 As opposed to ACCP and Physician Associate training, the emphasis is primarily on physiological investigations, application of technology to therapy, and clinical research. Currently, the training and funding structure is similar to graduate medical training. STP applicants in England and Wales apply via a national portal (Oriel)14 where, based on a point scoring system, they get accepted into their chosen specialisms, with the highest scoring individuals being allocated their preferred learning centres. STP trainee salaries, university fees, and a small training grant to the hosting Trust are provided by Health Education England.
The role of the CCS, while not ubiquitously, is present in other countries, such as New Zealand15 and Australia. Moreover, with the CCS STP emphasis on mechanical ventilation, there is a large overlap with the North American Respiratory Therapists.16 Currently, CCS do not tend to perform comprehensive patient assessments like Respiratory Therapists do, though this is an area that Clinical Scientists do engage in (e.g. in consultant scientists posts, or specialist physiology clinics).
Future directions
The future of CCS and the developing role will be largely determined by technological advances. Dr Eric Topol’s review of preparing the healthcare workforce to deliver the digital future highlights how telemedicine, remote monitoring, interventional robotics and predictive analysis using artificial intelligence (AI) are all key development areas within the NHS over the next 20 years.17 The importance of this has been highlighted by the recent announcement of the development of NHSX (the NHS digital transformation programme).18 The advances in use of apps for smart devices, virtual reality and wearable technology will have the potential to revolutionise critical care and the locations in which it is provided. CCS will not only be vital in the research and innovation required for the development of these techniques, but also in their integration and application, shaping a new standard of clinical practice, which will also be largely driven by the requirements of the specialist units, and their unique therapeutic and diagnostic requirements, across which CCS work. For example, progress in miniaturisation will extend the range of point-of-care technologies that could be used at the bedside. Developments in AI and ‘big data’ (e.g. the processing of large volumes of monitoring and outcome data) will allow the integration of patient information with algorithmic analysis, and produce guidance on further treatment, helping to make precision medicine a reality in critical care. CCS are ideally suited to research and implement such technologies, with their expert knowledge of equipment and clinical physiology. Engaging with research teams as well as industry will continue to be an important role within CCS.
Currently, CCS is one of the few Clinical Science specialisms that does not have a Higher Specialist Scientist Training (HSST) programme (a five-year doctoral level consultant training scheme).19 Such programmes do already exist for other physiological specialisms, such as Cardiac Science, and Respiratory and Sleep Science where Clinical Scientists provide advanced patient assessments to guide specialist therapies. Within the current structure of the critical care MDT, there would probably little uptake of a CCS HSST but this is a potential area for exploration.
With the development of the profession, CCS could relieve the ever-increasing burden on the medical and nursing team, especially in the light of the relative staff shortages compared to the level of care we wish to receive,3,20 while simultaneously ensuring that a specialist delivers the appropriate care by taking greater ownership of their areas of expertise, such as mechanical ventilation, management of renal replacement therapies, and non-routine interventions to which CCS might have had more exposure to than the rest of the MDT. These are areas in which CCS already provide extensive support to the rest of the MDT, e.g. by advising staff how to optimise prescriptions for hemofiltration or the use of anaesthetic conservation devices. Moreover, NHS England is currently in the process of starting a consultation on whether Clinical Scientists should be allowed to work under patient group directives. If CCS were granted this privilege, it would open new avenues in how they are utilised. As the profession gains prominence, and the healthcare system continues to adapt to the ever-changing clinical landscape, it is hoped that CCS become more established members of the MDT in critical care areas across the country, delivering innovative solutions to the physiological and technological needs of patients.
Conclusion
CCS are highly trained in clinical physiology and in the use of medical technologies. As such, they are uniquely positioned to manage the medical technologies emerging in the ever more complex critical care environment. CCS can provide advice to the whole MDT on the safe and effective use of these technologies. Within busy, and pathologically varied, critical care units CCS can support the medical and nursing team in interpreting the results of complex diagnostic and monitoring technologies, and in the application of those results to therapeutic interventions, especially non-routine and technologically advanced options. CCS are not only a valuable member of the MDT, but with the increasing importance of research and the advent of precision medicine, they are ideally suited to facilitate the transition of the latest technologies from the bench to the bedside.
Supplemental Material
Supplemental material, INC903232 Supplemental Material for Critical care scientists: Role, training and future directions by Natalie Fowler, Raashid Ali, Jonathan Bannard-Smith, Claire Jennings, Stephen Playfor and Michal Pruski in Journal of the Intensive Care Society
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Natalie Fowler https://orcid.org/0000-0003-2310-7938
Michal Pruski https://orcid.org/0000-0001-7582-1418
References
- 1.NHS England. What is healthcare science? www.england.nhs.uk/healthcare-science/what/ (accessed 30 July 2019).
- 2.Academy For Healthcare Science. The Healthcare Science Industry. The Academy For Healthcare Science, www.ahcs.ac.uk/about/the-healthcare-science-industry/ (accessed 30 July 2019).
- 3.Buchan J, Charlesworth A, Gershlick B, et al. A critical moment: NHS staffing trends, retention and attrition 2019. The Health Foundation. [Google Scholar]
- 4.Society of Critical Care Technologies. Journal, www.criticalcaretech.org.uk/index.php/journal (accessed 2 November 2019).
- 5.Curry S, Pruski M, Rubino A, et al. Healthcare scientists specialising in critical care. In: FICM, ICS (eds) Guidelines for the provision of intensive care services. UK: FICM & ICS, 2019, pp. 66–68.
- 6.Academy For Healthcare Science. Raashid Ali Health Care Science Week, www.youtube.com/watch?v=sIl8psxs3DA&feature=youtu.be (2019, accessed 30 July 2019).
- 7.Society of Critical Care Technologies. Home, www.criticalcaretech.org.uk/ (accessed 21 September 2017).
- 8.National School of Healthcare Science. Routes into the programme — scientist training programme. NSHCS, https://nshcs.hee.nhs.uk/programmes/stp/applicants/routes-into-programme/ (accessed 11 October 2019).
- 9.NHS Health Careers. Critical Care Science, www.healthcareers.nhs.uk/explore-roles/physiological-sciences/critical-care-science (2015, accessed 21 September 2017).
- 10.National School of Healthcare Science. Critical Care Science (2017). Curriculum Library, https://curriculum.nshcs.org.uk/programmes/stp/SPS1-5 (accessed 30 July 2019).
- 11.National School of Healthcare Science. Modernising Scientific Careers Scientist Training Programme Work-Based Training Learning Guide: Cardiac, Critical Care, Vascular, Respiratory and Sleep Sciences 2016/2017, http://www.nshcs.hee.nhs.uk/images/guidance/curricula/stp-ccvrs-lg-v1.0-2016-17.pdf (accessed 3 May 2018).
- 12.Lee G, Gilroy J-A, Ritchie A, et al. Advanced critical care practitioners – practical experience of implementing the advanced critical care practitioner faculty of intensive care medicine curriculum in a London critical care unit. J Intensive Care Soc 2018; 19: 147–154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.The Society of Clinical Perfusion Scientists of Great Britain and Ireland, The College of Clinical Perfusion Scientists of Great Britsain and Ireland. Interested in Perfusion: Education and Training, www.scps.org.uk/index.php?option=com_content&task=view&id=55&Itemid=58 (accessed 25 September 2019).
- 14.National School of Healthcare Science. Applying to the programme — scientist training programme. NSHCS, https://nshcs.hee.nhs.uk/programmes/stp/applicants/applying-to-the-programme/ (accessed 11 October 2019).
- 15.Canterbury District Health Board Careers. ICU Technician, www.cdhbcareers.co.nz/Science-Technical/ICU-Technician/ (accessed 25 September 2019).
- 16.The Michener Institute of Education at UHN. Respiratory Therapy Curriculum. The Michener Institute, https://michener.ca/academic-programs/michener/respiratory-therapy-curriculum/ (accessed 30 July 2019).
- 17.Topol E. The Topol review: preparing the healthcare workforce to deliver the digital future, https://topol.hee.nhs.uk/wp-content/uploads/HEE-Topol-Review-2019.pdf (2019, accessed 30 July 2019).
- 18.GOV.UK. NHSX: new joint organisation for digital, data and technology, www.gov.uk/government/news/nhsx-new-joint-organisation-for-digital-data-and-technology (2019, accessed 30 July 2019).
- 19.Health Education England. Facing the facts, shaping the future: a draft health and care workforce strategy for England to 2027, www.hee.nhs.uk/sites/default/files/documents/Facing%20the%20Facts%2C%20Shaping%20the%20Future%20%E2%80%93%20a%20draft%20health%20and%20care%20workforce%20strategy%20for%20England%20to%202027.pdf (2017, accessed 30 July 2019).
- 20.The Health Foundation, The King’s Fund, Nuffield Trust. The health care workforce in England: make or break? 2018.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, INC903232 Supplemental Material for Critical care scientists: Role, training and future directions by Natalie Fowler, Raashid Ali, Jonathan Bannard-Smith, Claire Jennings, Stephen Playfor and Michal Pruski in Journal of the Intensive Care Society