Abstract
Aim
To assess the feasibility, tolerance and effectiveness of enteral nutrition in critically ill patients receiving invasive mechanical ventilation in the prone position for severe Acute Respiratory Distress Syndrome (ARDS).
Methods
Prospective observational study conducted in a multidisciplinary critical care unit of a tertiary care hospital from January 2013 until July 2015. All patients with ARDS who received invasive mechanical ventilation in prone position during the study period were included. Patients’ demographics, severity of illness (Acute Physiology and Chronic Health Evaluation (APACHE II) score), baseline markers of nutritional status (subjective global assessment (SGA) and body mass index), details of nutrition delivery during prone and supine hours and outcomes (Length of stay and discharge status) were recorded.
Results
Fifty-one patients met inclusion criteria out of whom four patients were excluded from analysis since they did not receive any enteral nutrition due to severe hemodynamic instability. The mean age of patients was 46.4 ± 12.9 years, with male:female ratio of 7:3. On admission, SGA revealed moderate malnutrition in 51% of patients and the mean APACHE II score was 26.8 ± 9.2. The average duration of prone ventilation per patient was 60.2 ± 30.7 h. All patients received continuous nasogastric/orogastric feeds. The mean calories (kcal/kg/day) and protein (g/kg/day) prescribed in the supine position were 24.5 ± 3.8 and 1.1 ± 0.2 while the mean calories and protein prescribed in prone position were 23.5 ± 3.6 and 1.1 ± 0.2, respectively. Percentage of prescribed calories received by patients in supine position was similar to that in prone position (83.2% vs. 79.6%; P = 0.12). Patients received a higher percentage of prescribed protein in supine compared to prone position (80.8% vs. 75%, P = 0.02). The proportion of patients who received at least 75% of the caloric and protein goals was 37 (78.7%) and 37 (78.7%) in supine and 32 (68.1%) and 21 (44.6%) in prone position.
Conclusion
In critically ill patients receiving invasive mechanical ventilation in the prone position, enteral nutrition with nasogastric/orogastric feeding is feasible and well tolerated. Nutritional delivery of calories and proteins in prone position is comparable to that in supine position.
Keywords: ARDS, calorie goal, feed intolerance, nutrition, prone ventilation
Background and aim
Nutritional modulation of the stress response to critical illness includes early enteral nutrition (EN), appropriate macronutrient and micronutrient delivery and meticulous glycemic control. Delivering early EN is seen as a proactive therapeutic strategy that has been shown to reduce disease severity, diminish complications, decrease length of stay (LOS) in the Intensive Care Unit (ICU) and favorably impact patient outcome.1–5 Within the gut, EN has been associated with improved local perfusion, trophic effects, enhancement of gut immune function and reduction in bacterial translocation.6–8 Enteral feeds in the ICU are usually given by continuous controlled infusion through a nasogastric/orogastric tube to achieve sufficient caloric and protein intake. It is well recognized that early initiation of EN and reaching target nutrition goals has favorable impact on outcomes.9,10
Interruptions in enteral feeding, often for the fear of aspiration, are quite common in an intensive care setting and occur due to several reasons such as anticipated procedures, physiotherapy, routine nursing care, etc. and this hinders the achievement of nutritional targets.11 In recent times, with growing evidence for the beneficial effects of prone ventilation in patients with Acute Respiratory Distress Syndrome (ARDS),12 ventilating patients in the prone position is a common occurrence in the ICUs. Prone ventilation is associated with a risk of inadvertent displacement of endotracheal tubes, venous access and nasogastric tubes. Additionally, there is apprehension among care providers to continue EN for patients in the prone position in view of the relatively flat body position, increase in abdominal pressure and the use of sedative and paralytic agents in high doses. These risk factors leading to increased gastric residual volume (GRV) and emesis have also been variably reported.13
It remains largely unknown if prone position affects gastric emptying and risk of aspiration. The feasibility, effectiveness and tolerance for continued enteral feeding in prone positioning have not been adequately evaluated. Existing studies that have evaluated the feasibility of EN in prone position14–16 are limited by very small number of patients or their observations were affected by local nursing and nutritional protocols and policies. We hence sought to study the feasibility and tolerance of EN in critically ill patients receiving invasive mechanical ventilation in the prone position for severe ARDS in our center.
Methods
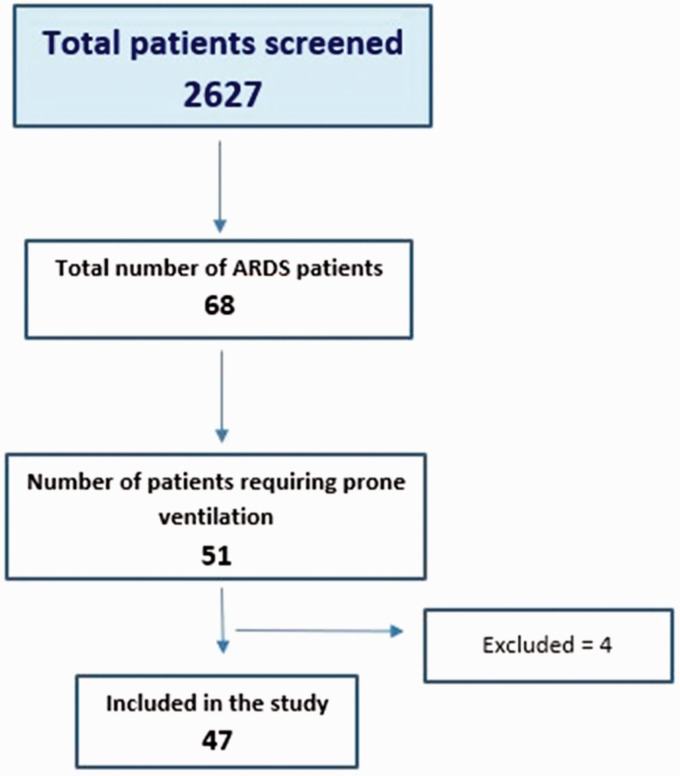
This was a prospective observational study conducted in 24-bed, multidisciplinary critical care unit of a tertiary care hospital from January 2013 until July 2015. This unit admitted mixed adult medical and surgical patients including trauma (excluding post cardio-thoracic surgery). A total of 2627 patients were screened during the study period. All adult patients with ARDS who were subjected to invasive mechanical ventilation in the prone position during the study period were eligible and included (Figure 1). Patients who were not fed enterally due to significant hemodynamic instability were excluded from analysis. Severe ARDS was identified based on Berlin criteria for diagnosis.17 The decision to prone was taken by the treating intensivist based on severity of ARDS, response to initial treatment and other standard criteria.18 Proning of the patient was performed by trained personnel following standard operating protocols of the unit. RotoProne beds were not utilized to prone patients. All patients had a nasogastric/orogastric tube inserted (in addition to a central venous access, arterial line and a urinary catheter) and position always confirmed with a chest X-ray prior to being proned. In the absence of contraindications, the choice of route between nasogastric or orogastric was based on physician preference. In addition to the initial check X-ray, our institutional policy required a sixth hourly re-assessment of naso/orogastric tube patency and position by the treating nurse, by inflating the stomach with 10–20 ml of air with a syringe via the feeding tube and simultaneously auscultating for the gush of air entry over the epigastrium. Any resistance to inflation or lack of air entry on auscultation warranted immediate cessation of feeds and a repeat chest X-ray to confirm feeding tube position. Apart from this, feeding tube position was noted and documented every time a chest X-ray was done for any other reason. Patients receiving supine ventilation were nursed in 30° recumbency while those in prone position were given a 15° reverse Trendelenburg position. Lung protective ventilation and sedation were based on standard ICU protocols.5 While data pertaining to these were documented as part of patient care, they were not captured in the study. Nutrition prescription was initiated by the treating clinician as early as possible (within 24–48 h) in the absence of contraindications based on SCCM and ASPEN guidelines for nutrition support in critically ill patients.19 Calorie (usually 25–30 kcal/kg) and protein (1–1.5 g/kg) prescriptions were made based on ideal body weight (IBW) or actual body weight depending on patient’s nutrition risk and volume status. Devine’s formula was used for calculating the IBW. Total volume of enteral feeds per day was prescribed by the bedside clinician based on patient’s physiology and volume status. The best combination of enteral scientific formula that could meet the calorie and protein goals within the volume prescribed for each patient was then used to deliver nutrition. Calorie density of feed used varied from 1 kcal/ml to 2.1 kcal/ml. Nasogastric or orogastric feeding was carried out as a continuous infusion. Feed infusion was started at a low rate and stepped up gradually based on tolerance to the desired rate. Prokinetics were not routinely employed and were used on an as needed basis at the discretion of the clinician.
Figure 1.
Flowchart – study overview.
ARDS: Acute Respiratory Distress Syndrome.
Routine nutritional assessment using SGA was performed on admission by a Clinical Dietitian. Nutrition prescription practice was the same whether the patient was in supine or prone position. Protein and energy requirements were calculated using weight-based equations, as per ASPEN guidelines. Pattern of nutrition delivery, feed interruptions and intolerance (vomiting, feed regurgitation and diarrhea) were recorded by the clinical dietitian. Although there is a debate on value of routine GRV measurements20 we elected to record these, every 6 h to assess tolerance of feeds as per our unit protocol. Feed volume was adjusted in a protocolized manner every 6 h based on GRV values. If GRV was <250 ml, feed was returned and continued at the same rate or increased as per prescription whereas for volumes between 250 ml and 300 ml. Feed was continued at a reduced rate after returning 250 ml back through the feeding tube. Prokinetic agents were prescribed at the discretion of the treating intensivist. Feed cessation for an hour followed by re-initiation at a reduced rate along with a prokinetic agent was recommended for GRV >300 ml.
Patients’ demographics, severity of illness on admission (Acute Physiology and Chronic Health Evaluation (APACHE II) score), baseline markers of nutritional status (subjective global assessment (SGA), and body mass index (BMI)), details of nutrition delivery during proning and supination until discharge and clinical outcomes were recorded.
The study was approved by the Institution’s Ethical Committee and all study procedures were done according to Declaration of Helsinki.
All continuous variables were assessed for normality using Shapiro-Wilk’s test and logarithmic transformation. Variables that did not follow normal distribution were analyzed using Mann-Whitney U test. Other variables were analyzed by independent sample t-test. Comparison of categorical variables were done using Chi square test (SPSS version 16.0). P value < 0.05 was considered significant (two-tailed).
Results
Fifty-one patients met inclusion criteria of whom four were excluded from analysis since they did not receive any EN in prone position due to severe hemodynamic instability. The mean age of the patients who were included was 46.4 ± 12.9 years, with male to female ratio of 7:3. Twenty patients (39%) were admitted with ARDS while the remaining had developed ARDS during their hospital stay. SGA on admission revealed moderate malnourishment in 51% of patients; others were well-nourished. There were no severely malnourished patients. The mean APACHE II score was 26.8 ± 9.2. The average duration of prone positioning per patient was 60.2 ± 30.7 h (Table 1). A total of 2831.6 h of prone ventilation (23.1%) and 15,506.1 h of supine ventilation (76.9%) were observed for feasibility and tolerance of enteral nasogastric feeding. The mean calories (kcals/kg/day) and protein (g/kg/day) prescribed in supine and prone position were 24.5 ± 3.8 and 1.1 ± 0.2 and 23.5 ± 3.6 and 1.1 ± 0.2, respectively. The total percentage of caloric goal achieved during the supine period (329.9 ± 304.8 h) was 83.2% whereas during prone period (60.2 ± 30.7 h) was 79.6%. The total percentage of protein goal achieved during the supine period was 80.8% while during prone period was 75% (Table 2). There was no significant difference between the calories received by patients during proning and supination (P = 0.12); however, patients received higher percentage of protein goals in supine compared to prone position (P = 0.02). During pronation, early initiation of EN within 6 h was possible in (87%) of patients. Interruption in feeding was not statistically significant between prone hours (12.3%) and supine hours (24.1%) (P = 0.344). There were no manifestations of GI intolerance like vomiting, gastroparesis and diarrhea in prone position whereas in supine position 6.6% of interruption was due to gastroparesis (increased GRV) and 1.4% had vomiting (Table 3). Though the mean GRV was different in patients between prone and supine hours (5.3 ± 3.9 vs. 15.1 ± 18.5 ml, respectively, P = 0.03), the actual volume was not clinically relevant.
Table 1.
Patient characteristics.
| N = 47 | Mean ± SD/ percentage |
|---|---|
| Age (yrs) | 46.4 ± 12.9 |
| Sex | |
| Males | 68% |
| Females | 32% |
| APACHE score | 26.8 ± 9.2 |
| SGA | |
| Well nourished | 49% |
| Moderately malnourished | 51% |
| Height (cm) | 163.5 ± 6.9 |
| Body weight (kg) | 68.9 ± 12.6 |
| BMI (kg/m2) | 26.0 ± 5.0 |
| Route of feeding | |
| Nasogastric | 74% |
| Orogastric | 26% |
| Outcome | |
| Discharged | 62% |
| Deceased | 38% |
| Median (IQR) | |
| ICU LOS (days) | 15 (8–20) |
| Hospital LOS (days) | 18 (11.5–27) |
| Average duration of proning (h) | 46.8 (35–84.8) |
APACHE: acute physiology and chronic health evaluation score; SGA: subjective global assessment; LOS: length of stay.
Table 2.
Nutrition delivery.
| Categories | N = 47 | Prone | Supine | P value |
|---|---|---|---|---|
| Total duration (h) | 2831.6 | 15,506.1 | ||
| % of Goal achieved | Calorie | 79.60% | 83.20% | 0.12 |
| Protein | 75.00% | 80.80% | 0.025 |
Table 3.
EN interruption.a
| Categories | Prone hours (%) | Supine hours (%) |
|---|---|---|
| Total duration of Interruption (h) | 260.75 | 878.75 |
| Procedures inside ICU (airway manipulations, chest physiotherapy, etc.) | 187.75 (72%) | 363.25 (41.3%) |
| Procedures outside ICU | 0 | 167.5 (19.1%) |
| GI bleed | 0 | 24 (2.7%) |
| Diarrhea (>3 times/day) | 0 | 0 |
| Gastroparesis | 0 | 58 (6.6%) |
| >250 ml GRV | 32 (12.3%) | 212 (24.1%) |
| Vomiting/nausea | 0 | 12 (1.4%) |
| Others (nursing care, bedside procedures, etc.) | 41 (15.7%) | 42 (4.8%) |
Difference between both the groups was insignificant in all the categories.
Discussion
Traditionally, prone position in the ICU has been associated with unsupported apprehension of aspiration, gastric intolerance and various other complications related to feeding.15 These have been mostly reported as case series or small observations. There are reports of withholding EN for proning being the only reason.21 Needless to say, this would impede achieving nutritional goals and adversely impact patient outcomes. In this prospective observational study conducted over 31 months, we were able to demonstrate that it is feasible to effectively provide controlled, continuous nasogastric feeding in critically ill patients ventilated in prone position.
EN was started early and was well tolerated in our study population despite a high severity of illness (APACHE II score 26.8 ± 9.2) compared to other reports.22 More than half of the patients in our study were moderately malnourished highlighting its incidence among the critically ill and the need for early aggressive nutritional therapy. One reason for such a high incidence of malnourishment on admission could be the fact that 39% of patients were admitted with ARDS, after a variable period of illness. We did not capture the number of patients referred from other hospitals and duration of illness prior to hospitalization in our unit.
The total caloric goal achieved was 83.2% during supine hours and 79.6% during prone hours (P = 0.12) demonstrating that enteral feeding was possible and successful with similar feeding practices in supine and prone positions. The total protein goal achieved during supine and prone hours were 80.80% and 75%, respectively (P = 0.02). The discrepancy between achieving calorie and protein goal is best explained by the inherent difficulty in meeting protein goals even with the best available protein dense scientific formula feeds. This is further influenced by volume restriction and use of calorie dense feeds, which tend to help achieve caloric goals without necessarily augmenting protein delivery. Prone hours are generally associated with maximum severity of respiratory failure and a corresponding limitation on fluid allowance. Once supine ventilation can be sustained, there is a scope for improving feed volume. We did not report a day-to-day analysis of goal achievement due to variability in prone and supine hours and therefore complexity of interpretation.
Earlier trials reporting difficulty in achieving nutritional goals have not clearly identified or specified the true impediment.15 It is possible that differences existed in the actual mode of prescription and/or delivery. We implemented the same nutritional delivery protocol both in supine and prone patients. One notable distinction with our protocol compared to that used in earlier trials was that the feed volume was stepped up (in accordance to GRV) once every 6 h as against once every day. This facilitates the administration of feeds earlier and stepping up aggressively to achieve goals.
We found no difference in the tolerance to early EN between the two groups in terms of GRV (more than 250 ml), vomiting or diarrhea. No additional maneuvers, special precautions or medications such as prokinetics were required in either of the groups. GI intolerance in the prone position and therefore a trend toward increased incidence of VAP has also been reported.15 Our study was however not designed to analyze association with infectious complications or patient outcomes.
There was no significant difference between the groups while analyzing the number of hours of feed interruption. The most common reason for feed interruption was a procedure inside the ICU, which required the patient to lie flat. This included the actual process of proning or supination in addition to airway and central venous interventions, physiotherapy and nursing care.
There is growing evidence to support the feasibility and effectiveness of EN for patients receiving mechanical ventilation in the prone position. This, together with increasing experience with nursing critically ill prone patients should clearly allay fears of early institution of EN in this patient subgroup. Rigorous training and strict implementation of feeding protocols will help achieve nutrition goals and impact patient outcomes favorably.
Conclusion
In critically ill patients receiving invasive mechanical ventilation in the prone position, EN is feasible and well tolerated with continuous nasogastric/orogastric feeding. Nutritional delivery in prone position is comparable with that of supine position.
Supplemental Material
Supplemental material, INC900100 Supplemental Material for Feasibility, tolerance and effectiveness of enteral feeding in critically ill patients in prone position by Raymond Dominic Savio, Rajalakshmi Parasuraman, Daphnee Lovesly, Bhuvaneshwari Shankar, Lakshmi Ranganathan, Nagarajan Ramakrishnan and Ramesh Venkataraman in Journal of the Intensive Care Society
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Ramesh Venkataraman https://orcid.org/0000-0003-1949-3979
Supplemental material: Supplemental material for this article is available online.
References
- 1.Kudsk KA, Croce MA, Fabian TC, et al. Enteral versus parenteral feeding. Ann Surg 1992; 215: 503–513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bortenschlager L, Roberts PR, Black KW, et al. Enteral feeding minimizes liver injury during hemorrhagic shock. Shock 1994; 2: 351–354. [DOI] [PubMed] [Google Scholar]
- 3.Heyland DK, Cook DJ. Enteral nutrition in the critically ill patient: a critical review of the evidence. Intensive Care Med 1993; 19: 435–442. [DOI] [PubMed] [Google Scholar]
- 4.Beier-Holgersen R, Boesby S. Influence of postoperative enteral nutrition on postsurgical infections. Gut 1996; 39: 833–835. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Braga M, Gianotti L, Vignali A, et al. Artificial nutrition after major abdominal surgery: impact of route of administration and composition of the diet. Crit Care Med 1998; 26: 24–30. [DOI] [PubMed] [Google Scholar]
- 6.Windsor AC, Kanwar S, Li AG, et al. Compared with parenteral nutrition, enteral feeding attenuates the acute phase response and improves disease severity in acute pancreatitis. Gut 1998; 42: 431–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moore FA, Feliciano DV, Andrassy RJ, et al. Early enteral feeding, compared with parenteral, reduces postoperative septic complications: the result of meta-analysis. Ann Surg 1992; 216: 172–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wicks C, Somasundaram S, Bjarnason I, et al. Comparison of enteral feeding and total parenteral nutrition after liver transplantation. Lancet 1994; 344: 837–840. [DOI] [PubMed] [Google Scholar]
- 9.Beth E Taylor, Stephen A Mc Clave, et al. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: society of critical care medicine (SCCM) and American society for parenteral and enteral nutrition (A.S.P.E.N.). J Parenter Enteral Nutr 2016; 40: 159–211. [DOI] [PubMed] [Google Scholar]
- 10.Guérin C, Reignier J, Richard JC, et al. Prone positioning in severe acute respiratory distress syndrome. N Engl J Med 2013; 368: 2159–2168. [DOI] [PubMed] [Google Scholar]
- 11.Piehl MA, Brown RS. Use of extreme position changes in acute respiratory failure. Crit Care Med 1976; 4: 13–14. [DOI] [PubMed] [Google Scholar]
- 12.Van der, Voort P, Zandstra D. Enteral feeding in the critically ill: comparison between the supine and the prone positions: a prospective crossover study in mechanically ventilated patients. Crit Care 2001; 5: 216–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reignier J, Thenoz-Jost N, Fiancette M, et al. Early enteral nutrition in mechanically ventilated patients in the prone position. Crit Care Med 2004; 32: 94–99. [DOI] [PubMed] [Google Scholar]
- 14.Reignier J, Dimet J, Martin-Lefevre L, et al. Before-after study of a standardized ICU protocol for early enteral feeding in patients turned in the prone position. Clin Nutr 2010; 29: 210–216. [DOI] [PubMed] [Google Scholar]
- 15.ARDS Definition Task Force. Ranieri VM, Rubenfeld GD, et al. Acute respiratory distress syndrome: the Berlin Definition. JAMA 2012; 307: 2526–2533. [DOI] [PubMed] [Google Scholar]
- 16.Scholten EL, Beitler JR, Kim Prisk G, et al. Treatment of ARDS with prone positioning. CHEST 2017; 151: 215–224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martindale RG, McClave SA, Vanek VW, et al. American College of Critical Care Medicine; the A.S.P.E.N. Board of Directors. Guidelines for the provision and assessment of nutrition support therapy in the adult critically ill patient: Society of Critical Care Medicine and American Society for Parenteral and Enteral Nutrition. Crit Care Med 2009; 37: 1757–1761. [DOI] [PubMed] [Google Scholar]
- 18.Hurt RT, McClave SA. Gastric residual volumes in critical illness: what do they really mean? Crit Care Clin 2010; 26: 481–490. [DOI] [PubMed] [Google Scholar]
- 19.Heyland DK, Tougas G, King D, et al. Impaired gastric emptying in mechanically ventilated, critically ill patients. Intensive Care Med 1996; 22: 1339–1344. [DOI] [PubMed] [Google Scholar]
- 20.Messerole E, Peine P, Wittkopp S, et al. The pragmatics of prone positioning. Am J Respir Crit Care Med 2002; 165: 1359–1363. [DOI] [PubMed] [Google Scholar]
- 21.Yang S, Wu X, Yu W, et al. Early enteral nutrition in critically Ill patients with hemodynamic instability: an evidence-based review and practical advice. Nutr Clin Pract 2014; 29: 90–96. [DOI] [PubMed] [Google Scholar]
- 22.Saez de la Fuente I, Saez de la Fuente J, Quintana Estelles MD, et al. Enteral nutrition in patients receiving mechanical ventilation in a prone position. J Parenter Enteral Nutr 2016; 40: 250–255. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, INC900100 Supplemental Material for Feasibility, tolerance and effectiveness of enteral feeding in critically ill patients in prone position by Raymond Dominic Savio, Rajalakshmi Parasuraman, Daphnee Lovesly, Bhuvaneshwari Shankar, Lakshmi Ranganathan, Nagarajan Ramakrishnan and Ramesh Venkataraman in Journal of the Intensive Care Society