Abstract
Background
It has been previously shown that a high percentage of medical students have sleep problems that interfere with academic performance and mental health.
Methods
To study the impact of sleep quality, daytime somnolence, and sleep deprivation on medical students, we analyzed data from a multicenter study with medical students in Brazil (22 medical schools, 1350 randomized medical students). We applied questionnaires of daytime sleepiness, quality of sleep, quality of life, anxiety and depression symptoms and perception of educational environment.
Results
37.8% of medical students presented mild values of daytime sleepiness (Epworth Sleepiness Scale - ESS) and 8.7% presented moderate/severe values. The percentage of female medical students that presented ESS values high or very high was significantly greater than male medical students (p < 0.05). Students with lower ESS scores presented significantly greater scores of quality of life and perception of educational environment and lower scores of depression and anxiety symptoms, and these relationships showed a dose-effect pattern. Medical students reporting more sleep deprivation showed significantly greater odds ratios of presenting anxiety and depression symptoms and lower odds of good quality of life or perception of educational environment.
Conclusions
There is a significant association between sleep deprivation and daytime sleepiness with the perception of quality of life and educational environment in medical students.
Keywords: Medical education, Quality of life, Sleep disorders, Academic environment, Anxiety, Depression, Medical students, Sleep quality, Daytime sleepiness
Background
Sleep problems are very frequent in the general population and medical students are one group that is vulnerable to poor sleep [1, 2]. The prevalence of sleep disturbances in medical students is higher than in non-medical students [1, 3]. There are many reasons to the high prevalence of sleep problems in medical students, including many hours of classes and study, clinical clerkships that include overnight work, emotional stress, choices concerning lifestyle and many hours using virtual social media [4, 5].
There is evidence that enough good quality sleep is important for long term learning, for neurocognitive and psychomotor performance and for physical and mental health [6]. In addition, sleep deprivation in medical students can make them more vulnerable to depressive and anxiety disorders [1]. Moreover, there are concerns related to patient safety when health professionals are sleep deprived. A review by Curcio et al. suggested that student learning and academic performance are closely related to sleep quantity and quality [7].
To our knowledge there was no previous work that evaluated the relationship between sleep quality and sleep deprivation with quality of life and perception of academic environment in medical students. To better understand the impact of sleep quality and quantity on medical students we analyzed data from a multicenter study with medical students in Brazil [8–11]. The purpose of this study was to evaluate the relationship between sleep deprivation, sleep quality and daytime sleepiness, and quality of life, perception of academic environment and symptoms of depression and anxiety.
Methods
Study design and sample
We performed this protocol as part of a multicentric study with 22 Brazilian medical schools (VERAS study, translated to English as “Students’ and Residents’ life in health professions”). Detailed description of this study was previously published [8–11]. Schools participating in the study were from all regions of Brazil, and with a diverse legal status and location (13 public and 9 private, 13 in state capital cities and 9 in other cities). The research protocol was approved by the Ethics Committee of the School of Medicine of the University of Sao Paulo. All medical schools included approved the study.
When our study was performed, Brazil had 153 medical schools with at least one graduating class, with approximately 86,000 medical students. The sample size of the study was defined to enable an effect size of 0.165, with 80% power at a 0.05 significance level, when comparing two samples of equal size. We then increased the sample to 1650 students to account for 30% loss of participants [8–11].
Sixty students were randomly selected from each of 22 medical schools. Five male and five female medical students were selected from each year of the undergraduate program. The selection was performed using a computer-generated list of random numbers [10]. Students were invited to participate by e-mail and social media. Participation was voluntary, without any compensation or incentive. We guaranteed both confidentiality and anonymity, and participating students completed an informed consent form [8–11].
Data collection
Students accessed an electronic survey platform, that was designed specifically for the study and had 10 days to complete the survey (thirteen questionnaires). After finishing the survey, voluntary received feedback on their scores. Medical students received their score for each domain of each questionnaire and information about the meaning of each result. We offered to the students the opportunity to contact the research group for guidance and/or emotional support. Confidentiality and anonymity were guaranteed in the consent form [8–11].
Instruments
To assess daytime sleepiness, we used the Epworth Sleepiness Scale (ESS) [12]. This questionnaire consists of 8 self-rated items, each scored from 0 to 3, that measure a subject’s habitual “likelihood of dozing or falling asleep” in common situations of daily living. The final score is the sum of individual items (scores 0–24). Values > 10 are considered excessive daytime sleepiness and values > 15 are considered severe sleepiness. ESS was translated and validated to Brazilian Portuguese [13].
To assess sleep quality, we used Pittsburgh Sleep Quality Index (PSQI) [14]. This questionnaire has 19 items to evaluate subjective sleep quality. We used only the global score of PSQI (range 0 to 21). Higher scores indicate worse sleep quality. Values > 5 are considered poor quality of sleep [14]. PSQI had been previously translated and validated to Brazilian Portuguese [13].
To assess sleep deprivation, we calculated the difference between mean hours of sleep during weekends and mean hours of sleep during weekdays, that was called Sleep Deprivation Index (SDI). SDI was derived from the questions: a) How many hours, on average, did you sleep on weekdays during the last 2 weeks? b) On weekends, if nobody wakes you up, how many hours, on average, do you sleep?
To assess quality of life (QoL) we used three questionnaires:
WHOQOL-BREF, that has 26 items with four domains: environment, psychological, social relationships, and physical health [15]. Answers are given on a 5-point Likert scale and points within each domain are transformed to a score from 0 to 100. Higher scores represent better QoL (WHOQOL GROUP 1995). This questionnaire was translated and validated to Brazilian Portuguese [16].
QoL self-assessment, that consisted of two questions to evaluate students’ perception regarding their overall QoL and QoL related to medical school (MSQoL) on a scale from 0 to 10. The items were [1] rate your overall quality of life [2]; rate your quality of life in medical school [8, 10].
VERAS-Q that is a questionnaire created to evaluate quality of life from students in the health professions. This questionnaire has 45 statements on a 5-points Likert scale divided in four domains (time management, psychological, physical health and learning environment) and a global score [17, 18].
To assess the perception of the educational environment in medical school we used DREEM (Dundee Ready Education Environment Measure), a 50-item questionnaire which evaluates educational environment perceptions. This questionnaire has 5 domains: perceptions of learning, perceptions of teachers, academic self-perceptions, perceptions of atmosphere, and social self-perceptions [19, 20]. Answers are given on a 5-point Likert scale. This questionnaire was translated and validated to Brazilian Portuguese [21].
To assess emotional symptoms, we used Beck Depression Inventory (BDI) and State Trait Anxiety Inventory (STAI). BDI is a 21-item questionnaire to measure depression symptoms [22]. Scores of each item vary from 0 to 3 according to increasing symptom intensity. This questionnaire was translated and validated to Brazilian Portuguese [23]. STAI has a scale with 20 items each evaluating the intensity of state-anxiety and of trait-anxiety symptoms [24]. This questionnaire was also previously translated and validated to Brazilian Portuguese [23].
The results of the reliability analyses performed using the Cronbach’s α coefficient demonstrated that the data had and α value between 0.65 and 0.94 for all domains of the questionnaires (data not shown).
Statistical analysis
Students were divided according the results of ESS in three groups, respectively ESS ≤ 10, 10 < ESS < 16 and ESS > 16. Comparisons among these three groups were performed using one-way ANOVA followed by Dunn test.
We divided medical students in three groups according to quartiles of sleep deprivation. We present categorical variables as counts and proportions and their distributions across sleep deprivation groups are analyzed using chi-squared trend tests for proportions. Quality of life (Overall, medical school-related, WHOQOL and VERAS-Q), mental symptoms (BDI, STAI-state and STAI-trait), and DREEM scores are presented as medians and interquartile ranges and their distributions across sleep deprivation groups are analyzed using the Jonckheere-Terpstra trend test. We built binary logistic regression models to study the association between sleep deprivation and daytime sleepiness, and the association between sleep deprivation and high scores in each of these scales. High scores were defined as a score equal or above the median for the whole sample. Binary logistic models are presented adjusted for age, sex, and year of medical school. Significance level was set at 0.05. Analyses were performed using R software, version 3.2.0.
Results
As previously shown, of 1650 randomly selected students, 1350 (81.8%) accepted to participate and completed the study [8–11]. The main reason to refuse to participate in the study (16.6%) was lack of time. Their ages ranged between 17 and 40 (22.8 ± 1.3) years old.
From the 1350 participants, 714 (52.9%) were women, 459 (34.0%) were in the 1st or 2nd year of medical school (basic sciences), 491 (36.4%) were in the 3rd or 4th year of medical school (clinical sciences) and 400 (29.6%) in the last 2 years of medical course (clerkships).
Table 1 shows the results of Epworth Daytime Sleepiness Scale (ESS): 37;8% medical students presented high values of ESS and 8.7% presented very high values. The percentages of female medical students that presented ESS values high or very high were significantly greater than male medical students.
Table 1.
Results of the Epworth Daytime Sleepiness Scale (ESS) in all medical students evaluated
| ESS results | Males | Females | Total |
|---|---|---|---|
| 0–10 | 388 (61.0%) | 334 (46.8%)* | 722 (53.5%) |
| 11–15 | 211 (33.2%) | 299 (41.9%)* | 510 (37.8%) |
| 16–24 | 37 (5.8%) | 81 (11.3%)* | 118 (8.7%) |
* P < 0.05 compared to males
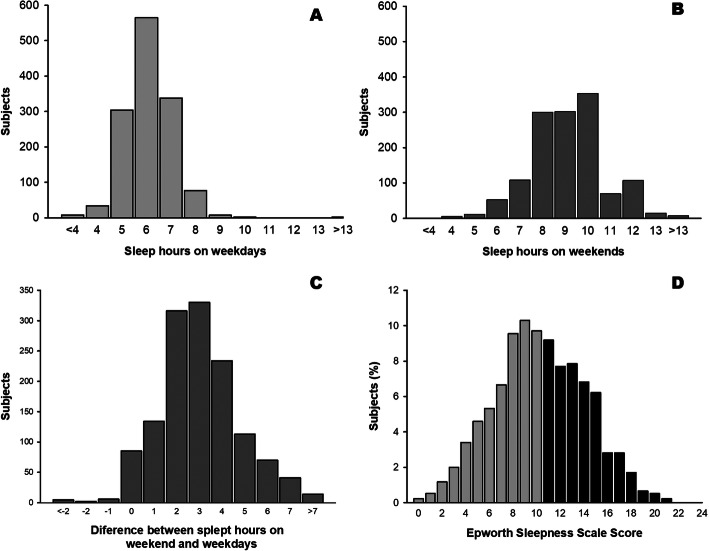
Figure 1 shows the distribution of self-related sleep hours during weekdays (A), weekends (B), difference between mean weekend and weekday sleep hours (C) and ESS scores of medical students (D).
Fig. 1.
Sleep pattern and daily sleepiness among medical students. Histograms represent the distribution of self-related sleep hours during weekdays (a), weekends (b), difference between mean weekend and weekday sleep hours (c) and Epworth Sleepiness Scale (ESS) scores of medical students (d). Gray bars represent normal values of ESS and black bars represent increased daytime somnolence
We evaluated the differences in the results of questionnaires of quality of life, education environment, and depression and anxiety symptoms among medical students with normal values of ESS (< 10), students with values between 11 and 15 and students with values > 15.
The association between excessive daytime sleepiness and quality of life is shown in Fig. 2. We observed a dose-effect pattern, with lower values of ESS corresponding to higher values of quality of life scores. We observed statistically significant differences among the three groups in all domains of WHOQOL-BREF and VERAS-Q questionnaires and in the scores of quality of life in general and medical school-related quality of life.
Fig. 2.
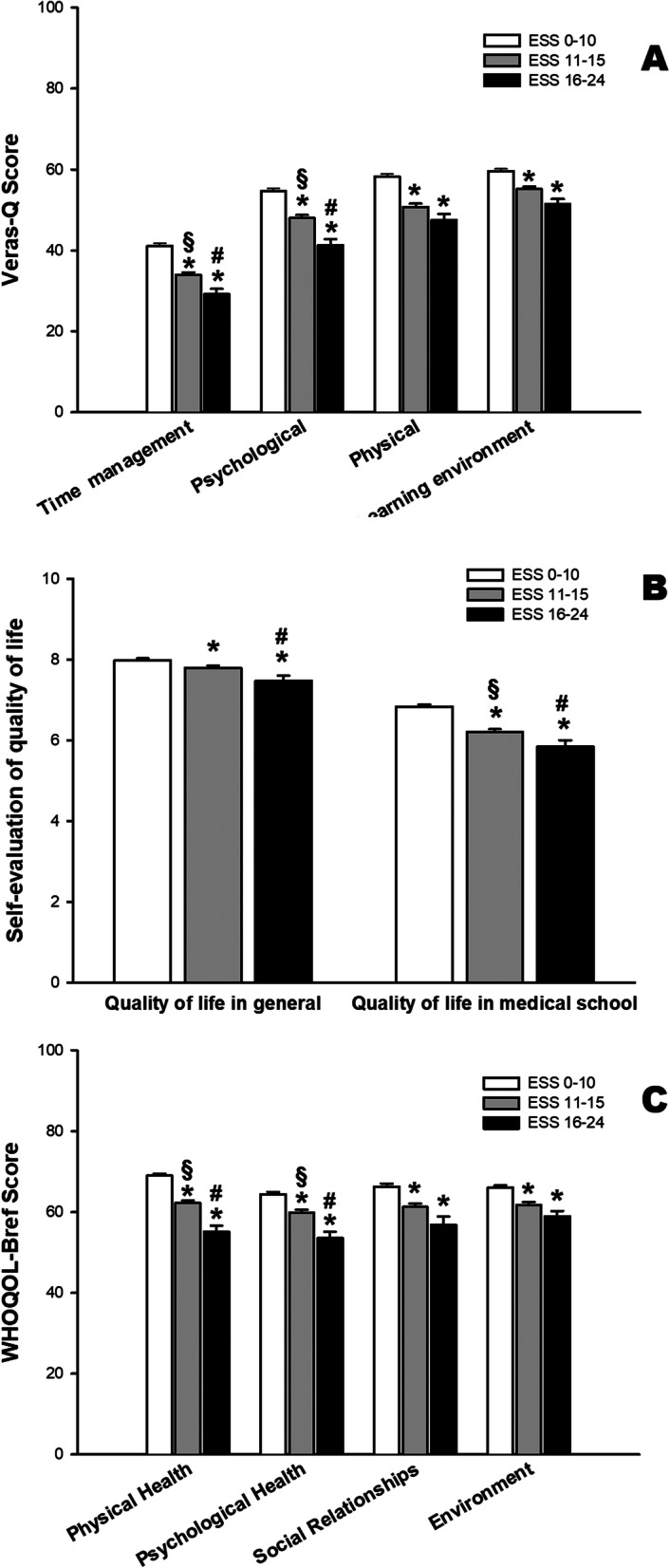
Quality of life of medical students decreases with higher daily sleepiness scores. Mean and standard error values of VERAS-Q (a), self-evaluation of QoL (b) and WHOQOL-BREF questionnaires (c) in the three groups of medical students based on ESS scores. * p < 0.05 compared to ESS 0–10; § p < 0.05 compared to ESS 16–24; # p < 0.05 compared to ESS 11–15
We also observed that students with higher values of ESS presented a worse perception of education environment. Both in global DREEM score and in the five domains of DREEM there were statistically significant differences among the three groups of medical students concerning the results of ESS (Fig. 3).
Fig. 3.
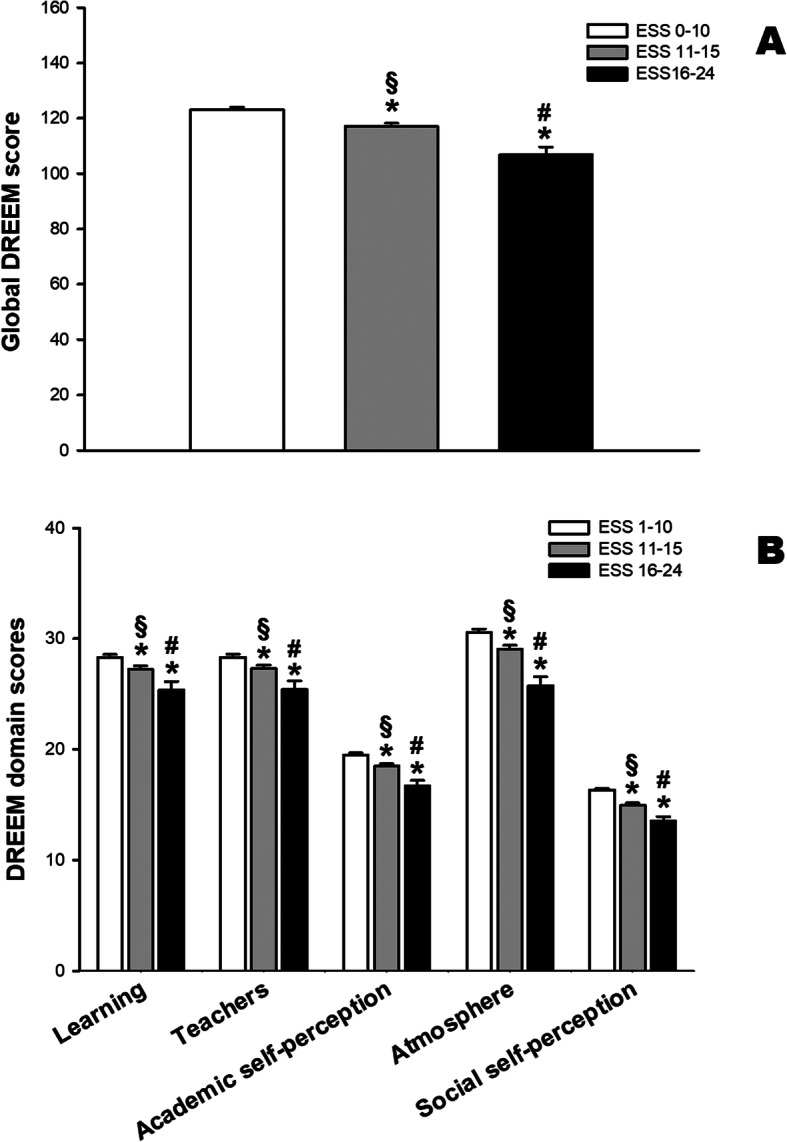
Medical students that presents higher daily sleepiness scores (ESS) showed lower perception of educational environment. Bars indicate mean (and standard error) values of DREEM global (a) and domain scores (b) * p < 0.05 compared to ESS 0–10; § p < 0.05 compared to ESS 16–24; # p < 0.05 compared to ESS 11–15
Higher scores of daytime sleepiness were also associated with higher scores of depression symptoms and with state and trait anxiety scores. We also observed a dose-response relationship and the differences were statistically significant among the three groups of ESS values (Fig. 4).
Fig. 4.
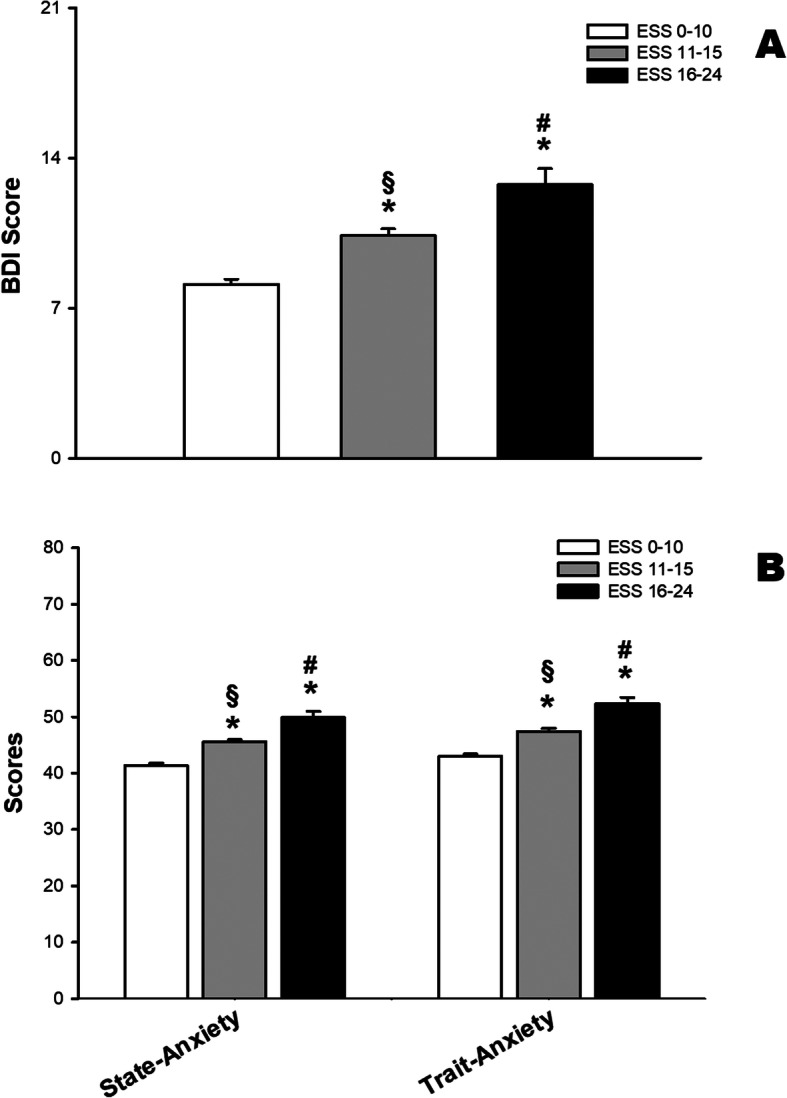
Higher scores of sleepiness are associated with higher scores of depression and anxiety. Beck Depression Inventory (BDI (a) and State and Trait Anxiety scores (b) (Means and standard errors). BDI scores range from 0 to 21 and STAI scores range from 20 to 80. * p < 0.05 compared to ESS 0–10; § p < 0.05 compared to ESS 16–24; # p < 0.05 compared to ESS 11–15
Medical students that presented higher ESS scores showed lower quality of sleep measured by PSQI. PSQI global score range from 0 to 21, lower scores represent better quality of sleep (Fig. 5a). Figure 5b shows the distribution of PSQI scores in all medical students.
Fig. 5.
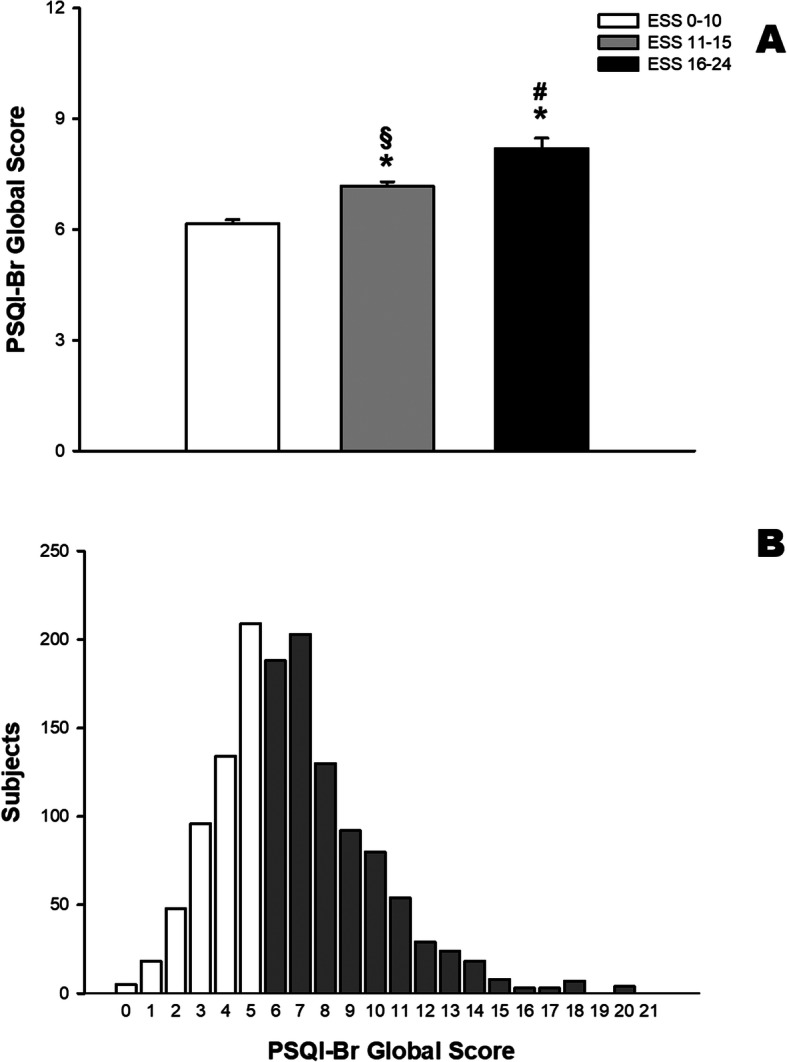
Medical students that presents higher daily sleepiness score showed lower quality of sleep measured by PSQI-Br. PSQI-Br global score ranges from 0 to 21, and lower scores represent better quality of sleep. a Mean (and standard error) values of PSQI-Br global scores. b Distribution of number of medical students with each value of PSQI-Br. Values higher than 5 indicate poor quality of sleep (gray bars). * p < 0.05 compared to ESS 0–10; § p < 0.05 compared to ESS 16–24; # p < 0.05 compared to ESS 11–15
We divided medical students in four quartiles concerning the values of this sleep deprivation index (SDI), with SDI respectively ≤2 (Q1), =3 (Q2), =4 (Q3) and > 4 (Q4) hours. Table 2 shows the distribution of medical students and values of the studied questionnaires according to deprivation groups (Q1, Q2 + Q3 and Q4).
Table 2.
Description of the study sample, according to sleep deprivation groups, from Sleep Deprivation Index
| Q1 (N = 536) ≤ 2 h |
Q2-Q3 (N = 564) 3 and 4 h |
Q4 (N = 238) > 4 h |
Total (N = 1338) | |
|---|---|---|---|---|
| Age (mean ± SD) | 23.0 ± 3.0 | 22.5 ± 2.9 | 22.6 ± 3.0 | 22.7 ± 3.0 |
| Year of medical school (N (%)) | ||||
| 1st/2nd (Basic) | 175 (32.6%) | 196 (34.8%) | 83 (34.9%) | 454 (33.9%) |
| 3rd/4th (Clinical) | 195 (36.4%) | 209 (37.1%) | 81 (34.0%) | 485 (36.2%) |
| 5th/6th (Clerkship) | 166 (31.0%) | 159 (28.2%) | 74 (31.1%) | 399 (29.8%) |
| Female sex - N (%) | 276 (51.5%) | 304 (53.9%) | 131 (55.0%) | 711 (53.1%) |
| WHOQOL (median [P25 - P75]) | ||||
| Physical | 71.4 [60.7–78.6] | 64.3 [57.1–75.0] | 60.7 [46.4–71.4] | 67.9 [53.6–75.0] |
| Psychological | 66.7 [54.2–75.0] | 62.5 [54.2–70.8] | 58.3 [45.8–66.7] | 62.5 [54.2–75.0] |
| Social Relationships | 66.7 [58.3–75.0] | 66.7 [50.0–75.0] | 58.3 [50.0–75.0] | 66.7 [50.0–75.0] |
| Environment | 65.6 [56.3–75.0] | 65.6 [53.1–75.0] | 59.4 [50.0–68.8] | 65.6 [53.1–75.0] |
| VERAS-Q (median [P25 - P75]) | ||||
| Time use | 39.8 [29.6–52.3] | 36.4 [25.0–45.5] | 29.6 [20.4–40.9] | 36.4 [25.0–47.7] |
| Psychological | 54.2 [43.8–66.7] | 50.0 [39.6–60.4] | 43.8 [33.3–54.2] | 50.0 [39.6–62.5] |
|
Physical Environment |
59.4 [43.8–71.9] 58.9 [50.0–67.9] |
53.1 [40.6–65.6] 57.1 [49.5–66.1] |
46.9 [34.4–59.4] 55.4 [46.4–62.5] |
53.1 [40.6–68.8] 57.1 [48.2–66.1] |
| Quality of life (median [P25 - P75]) | ||||
| Overall | 8.0 [7.0–9.0] | 8.0 [7.0–9.0] | 8.0 [7.0–9.0] | 8.0 [7.0–9.0] |
| Medical school-related | 7.0 [6.0–8.0] | 7.0 [6.0–7.0] | 6.0 [5.0–7.0] | 7.0 [6.0–8.0] |
| Mental symptoms (median [P25 - P75]) | ||||
| Depression (BDI) | 7.0 [3.0–11.0] | 8.0 [5.0–13.0] | 11.0 [7.0–17.0] | 8.0 [4.0–13.0] |
| Anxiety-state | 41.0 [34.0–50.0] | 42.0 [35.0–51.0] | 47.0 [40.0–57.0] | 43.0 [35.0–52.0] |
| Anxiety-trait | 43.0 [34.0–50.0] | 46.0 [37.8–53.0] | 50.0 [41.2–59.0] | 45.0 [37.0–53.0] |
| DREEM (median [P25 - P75]) | ||||
| Perceptions of learning | 28.5 [23.0–33.0] | 28.0 [23.0–33.0] | 26.0 [22.0–32.0] | 28.0 [23.0–33.0] |
| Perception of teachers | 28.0 [23.0–32.0] | 28.0 [24.0–33.0] | 27.0 [23.0–31.0] | 28.0 [23.0–32.0] |
| Perceptions of the atmosphere | 20.0 [16.0–23.0] | 19.0 [16.0–23.0] | 17.5 [14.2–21.0] | 19.0 [15.2–22.0] |
| Academic self-perceptions | 31.0 [25.0–36.0] | 30.5 [25.0–35.0] | 28.0 [23.0–33.0] | 30.0 [25.0–35.0] |
| Social self-perceptions | 16.0 [13.0–20.0] | 16.0 [13.0–18.2] | 14.0 [11.0–17.0] | 16.0 [13.0–19.0] |
| Global | 123.5 [102.8–142.0] | 121.0 [101.8–139.0] | 113.0 [98.0–128.8] | 120.0 [101.0–139.0] |
Groups that showed statistically significant differences (P < 0.05) are in bold
Table 3 shows the results of binary logistic regression models. We show the odds ratios (and 95% confidence intervals) for the association between sleep deprivation groups and high quality of life, depression and anxiety symptoms and perception of academic environment. The results are presented crude and adjusted for age, sex and year of medical school. Group Q1 was used as reference and the odds ratio that were statistically significant are presented in bold.
Table 3.
Odds ratios (and 95% confidence intervals) for the association between sleep deprivation groups and high quality of life, mental symptoms, and DREEM scores
| Crude | Adjusted | |||||
|---|---|---|---|---|---|---|
|
Q1 ≤ 2 h |
Q2-Q3 3 and 4 h |
Q4 > 4 h |
Q1 ≤ 2 h |
Q2-Q3 3 and 4 h |
Q4 > 4 h |
|
| WHOQOL | ||||||
| Physical | Ref (1.0) | 0.61 (0.48–0.77) | 0.36 (0.26–0.49) | Ref (1.0) | 0.61 (0.48–0.78) | 0.36 (0.26–0.49) |
| Psychological | Ref (1.0) | 0.63 (0.49–0.80) | 0.41 (0.30–0.55) | Ref (1.0) | 0.62 (0.49–0.80) |
0.41 (0.30–0.55) 0.56 (0.41–0.77) |
| Social Relationships | Ref (1.0) | 0.70 (0.55–0.89) | 0.58 (0.42–0.78) | Ref (1.0) | 0.68 (0.54–0.87) | |
| Environment | Ref (1.0) | 0.88 (0.69–1.11) | 0.45 (0.33–0.62) | Ref (1.0) | 0.84 (0.66–1.07) | 0.44 (0.32–0.60) |
| VERAS-Q | ||||||
| Time use | Ref (1.0) | 0.69 (0.54–0.87) | 0.37 (0.27–0.50) | Ref (1.0) | 0.68 (0.54–0.87) | 0.36 (0.27–0.50) |
| Psychological | Ref (1.0) | 0.58 (0.46–0.74) | 0.44 (0.32–0.60) | Ref (1.0) | 0.58 (0.45–0.74) | 0.44 (0.32–0.60) |
| Physical | Ref (1.0) | 0.71 (0.56–0.90) | 0.38 (0.28–0.52) | Ref (1.0) | 0.69 (0.54–0.88) | 0.37 (0.27–0.51) |
| Environment | Ref (1.0) | 0.85 (0.67–1.07) | 0.65 (0.48–0.88) | Ref (1.0) | 0.81 (0.63–1.03) | 0.62 (0.46–0.85) |
| Quality of life | ||||||
| Overall | Ref (1.0) | 0.97 (0.75–1.25) | 0.76 (0.55–1.04) | Ref (1.0) | 0.94 (0.73–1.21) | 0.74 (0.54–1.01) |
| Medical school-related | Ref (1.0) | 0.73 (0.58–0.93) | 0.45 (0.33–0.62) | Ref (1.0) | 0.71 (0.56–0.91) | 0.44 (0.32–0.60) |
| Mental symptoms | ||||||
| BDI | Ref (1.0) | 1.47 (1.16–1.86) | 2.99 (2.16–4.14) | Ref (1.0) | 1.46 (1.15–1.86) | 3.01 (2.16–4.19) |
| Anxiety-state | Ref (1.0) | 1.07 (0.85–1.36) | 1.95 (1.42–2.67) | Ref (1.0) | 1.07 (0.84–1.36) | 1.94 (1.42–2.67) |
| Anxiety-trait | Ref (1.0) | 1.56 (1.23–1.98) | 2.62 (1.90–3.60) | Ref (1.0) | 1.55 (1.22–1.98) | 2.63 (1.90–3.64) |
| DREEM | ||||||
| Perceptions of learning | Ref (1.0) | 0.81 (0.64–1.02) | 0.63 (0.46–0.86) | Ref (1.0) | 0.79 (0.62–0.9998) | 0.62 (0.45–0.84) |
| Perception of teachers | Ref (1.0) | 1.07 (0.84–1.36) | 0.71 (0.53–0.97) | Ref (1.0) | 1.04 (0.81–1.32) | 0.70 (0.51–0.96) |
| Perceptions of atmosphere | Ref (1.0) | 0.80 (0.63–1.02) | 0.46 (0.34–0.63) | Ref (1.0) | 0.80 (0.63–1.02) | 0.46 (0.34–0.63) |
| Academic self-perceptions | Ref (1.0) | 0.92 (0.73–1.17) | 0.53 (0.39–0.73) | Ref (1.0) | 0.91 (0.72–1.16) | 0.53 (0.39–0.72) |
| Social self-perceptions | Ref (1.0) | 0.72 (0.57–0.91) | 0.46 (0.33–0.62) | Ref (1.0) | 0.71 (0.56–0.90) | 0.45 (0.33–0.62) |
| Global | Ref (1.0) | 0.90 (0.71–1.14) | 0.44 (0.32–0.61) | Ref (1.0) | 0.89 (0.70–1.13) | 0.44 (0.32–0.60) |
High scores are defined as those equal of above the median for the whole sample. P-values below 0.05 are in bold. Adjusted models are adjusted for age, sex and year of medical school
Groups with higher sleep deprivation (Q2 + Q3 and Q4) had lower odds for higher scores of quality of life in all domains of VERAS-Q and WHOQOL-BREF questionnaires with the exception of environment domains of group Q2 + Q3. Interestingly, lower odds for quality of life were observed in the groups with sleep deprivation only for medical school-related quality of live but not for overall QoL.
We observed higher odds for depression symptoms in medical students with higher differences between weekends and weekdays sleep hours (SDI). Medical student that reported more than 4 h of SDI had an odds ratio of 3.01 (2.16 to 4.19) of higher depression symptoms compared to students with a SDI less than 3. We also observed higher odds rations of higher anxiety symptoms for state anxiety in Group Q4 and for trait anxiety in groups Q2 + Q3 and Q4.
When we studied the odds ratios of higher DREEM scores, we observed statistically significant lower odds ratios in Group Q4 compared to Q1 in global DREEM scores and in all DREEM domains (learning, teachers, educational atmosphere, academic and social self-perception). Group Q2 + Q3 presented lower odds only in two domains (perception of learning and social self-perception).
Table 4 shows the results of a binary logistic regression model for the association between sleep deprivation index (SDI) and daytime sleepiness (ESS). We show the odds ratios (and 95% confidence intervals) for the association between sleep deprivation groups and daytime sleepiness. The results were adjusted for age, sex and year of medical school. Group Q1 was used as reference. Students in the quartile 2 and quartile 3 of the SDI had an increase of 59,9% the odds of having pathologic values of daytime sleepiness, in comparison with Q1. In addition, students in the quartile 4 of SDI had an increase of 122,8% in the odds of having pathologic values of daytime sleepiness, in comparison with Q1 group.
Table 4.
Results of binary logistic regression models for the association between sleep deprivation index (SDI) and Epworth scale (daytime sleepiness)
| SDI | Adjusted data OR (95% CI) |
P | |
|---|---|---|---|
| Epworth > 10 | Q1 (≤ 2 h) | Ref (1.0) | |
| Q2 + Q3 (3 and 4 h) | 1.56 (1.25 to 2.04) | < 0.001 | |
| Q4 (≥ 4 h) | 2.23 (1.62 to 3.05) | < 0.001 |
Discussion
Our data reveal consistent associations between daytime sleepiness and sleep deprivation and worse perception of quality of life and academic environment, and anxiety and depression symptoms in medical students. A dose-response relationship was observed for these associations.
In our study, there was a high frequency of students who had high scores on the Epworth scale (46.5%). This number, if compared with most studies involving medical students, was impressive. A study from Malaysia showed a percentage of 35.0% [25] of high scores on the Epworth scale. In India, this value was 30.6% [26]. Our data also showed that females had greater daytime sleepiness in relation to the males.
Our results showed that there was also a high percentage of students who had poor sleep quality by PSQI (62.2%). This number was higher than other studies in medical students, with scores ranging from 19.0% in China [27], 38.9% in Brazil [28] and 40.0% in Lithuania [29]. A national study, which evaluated the general adult population, showed a mean of 4.9 of the overall PSQI score and worse scores in females [30]. Our data did not show differences between males and females, and we observed a worse mean of the overall PSQI score.
Some studies have evaluated sleep in healthy young general population, identifying habitual sleep ranges from 7.0 to 8.5 h, and their determinants are social factors and lifestyle [31–34]. However, when offered the opportunity of extended sleep time in experiments with protected hours, the amount of nocturnal sleep can increase more than 1 h, ranging from 8.4 to 8.9 h [31–36]. The recommendation of the National Sleep Foundation is that individuals from 18 to 25 years of age sleep between 7 and 9 h [37]. The extended period of sleep brings potential benefits to the individual because this implies that all phases of sleep are respected, allowing physical and mental restoration [32]. One practical way in which people compensate for the lack of sleep that may incorporate into their routine is a short nap throughout the day.
The difference between the hours of sleep in the week and at the weekend associated with not meeting the actual need for sleep suggests that many students in our study had chronic sleep deprivation. The smaller mean hours of sleep during the week in the group with worse daytime sleepiness scores (Epworth> 10) also reinforce this data. Other studies have shown that young adults have sleep deprivation from one to three hours at night during the week, with a much longer sleep duration and wake-up time later at weekends [38]. Coupled with this behavior, many medical students view sleep deprivation as a symbol of dedication to the profession [39]. This aspect has a strong influence of the hidden curriculum, which concerns the student’s socialization in the process of becoming a doctor, or the construction of their professional identity, acquiring habits and behaviors patterns of their peers and models [40]. The common sense is that the successful doctor is the one who is too busy to abstain from hours of leisure, socializing and self-care, in favor of the health care of others [41]. This model that underestimates self-care can be assimilated and reproduced by students, sacrificing their hours of sleep for other interests.
Specialists in time management suggest that the agenda begins by delimiting the necessary hours of sleep and from there the other daily tasks are distributed. The question that arises is that there is a desire among the students to include all complementary training opportunities to the formal curriculum, often causing harm to their health. This overload can be motivated both by the competitiveness among the students and by the generational multitasking characteristic [42].
Few data exist on the medical student’s routine in the past. A 1968 study in England found that on average the medical student slept eight hours a day and that the amount of sleep did not change between the week and the weekend [43]. An Australian study reported the worst academic performance when waking later in the morning, especially at weekends [44]. The same author, years later, after developing the Epworth scale, found an average of this score of 7.6 [45], whereas in our data the average daytime sleepiness score was 10.3. The analysis of these studies shows that in addition to the cultural differences, it is necessary to highlight the historicity of the samples.
Some authors compared the sleep of medical students with that of other courses. There is a large percentage of college students in general who sleep less than 7 h per night, ranging from 24 to 49% [46]. Medical students had worse PSQI scores in relation to Law and Economics courses in Lithuania [29].
Several studies have reported the relationship between daytime sleepiness and academic performance. There were better performances in students who slept earlier and who had greater hours of sleep during the week. Sleep deprivation has negative effects on emotional intelligence, including the ability to demonstrate empathy [47–49]. Of course, these studies report only associations, and cause-effect of sleepiness versus academic performance or emotional abilities cannot be precisely established.
In the same context, it is unclear whether sleepiness leads to deterioration of the student’s mental health, or whether drowsiness can be one of the consequences of anxiety or depression. A national study revealed an increased risk of minor psychiatric disorders among students with sleepiness, sleep interruption, insomnia, and sleep hours of less than 7 h [50]. Loayza et al. [50] suggest that the evaluation of sleepiness in medical students can be a good tool for psychiatric screening and preventive measures.
The overall PSQI scores were related to the range of ESS scores, that is, there was a positive association of the instruments, indicating that the higher the PSQI Global score (meaning poorer sleep quality), the greater the tendency of the individual have an ESS altered score (indicating greater daytime sleepiness).
Few studies compared WHOQOL-BREF with Epworth scale, and these studies were from specific populations, such as elderly patients with chronic pain or sleep apnea [51–53]. All studies revealed a relationship between sleepiness and decreased the quality of life.
Our DREEM results show that students had a more positive than negative perception of educational environment (total score between 101 and 150), according to the syntax of DREEM [19]. The mean of the global score was similar to the results of other studies conducted in developing countries such as Iran, India, Kuwait and Sri Lanka [54–57].
Odds Ratio (OR) values were significant for most associations between sleep and quality of life and educational environment. These logistic regression results are robust because they carefully exclude confounding factors such as age, sex, and course year. With this analysis, the impact of sleep deprivation on the medical student’s quality of life confirms the practical relevance of this issue. However, data on quality of life are multifactorial and sleepiness is not an isolated factor in the worsening of the quality of life and in the perception of the educational environment. It is worth mentioning that only the group with the highest drowsiness (Epworth quartile 4) presented a significant association of ORs for the domains of DREEM and Global score, except for perception of learning and social relation’s domains, which also showed significance in the intermediate drowsiness group (quartiles 2 + 3).
The present study has some strengths: the original format, the national multicenter design, with an expressive number of randomized respondents, a low number of losses, a high response rate and a variety of instruments that analyze the quality of life, sleep, emotional symptoms, and medical student educational environment. Another positive aspect of the study was the possibility for respondents to receive feedback on their results and the opportunity for support and guidance.
Our study has as limitations the transversal design that does not allow us to analyze causality and the fact that the results are generalizable only to the universe of Brazilian students, although we can infer that they are similar to those found in other cultures. There are some limitations of studies that use self-reports. Specifically, in relation to studies of sleep, the results can be compared with more objective measures, such as polysomnography or actigraphy. More stressed individuals tend to report more sleepiness and fatigue in relation to people who are less stressed [58]. Concerning quality of life, individuals with more critical views may negatively direct their responses to some items.
Conclusions
Sleep deprivation and daytime sleepiness are associated to a worse the perception of quality of life and educational environment and depression and anxiety symptoms in medical students.
Curricular changes that include redistribution of academic activities, individual orientation for mentoring activity, health promotion programs and protected hours for study and leisure are valid strategies to assist the student in the management of his/her time, which indirectly can improve his / her learning, sleep and decrease their daytime sleepiness, ultimately improving the medical student’s quality of life.
Acknowledgements
The authors acknowledge the students and the medical schools that participated in the study: Universidade Federal do Rio de Janeiro, Universidade Federal de Ciências da Saúde de Porto Alegre, Universidade Estadual do Piauí, Faculdade de Medicina de Petrópolis, Faculdade de Ciências Médicas da Paraíba, Pontifícia Universidade Católica de São Paulo, Universidade Federal do Ceará, Universidade Federal de Goias, Universidade Federal de Mato Grosso do Sul, Escola Baiana de Medicina e Saúde Pública, Faculdade de Medicina de Marília, Faculdade de Medicina de São José do Rio Preto, Faculdade de Ciências Médicas da Paraíba, Faculdade Evangélica do Paraná, Faculdade de Medicina do ABC, Fundação Universidade Federal de Rondônia, Pontifícia Universidade Católica do Rio Grande do Sul, Universidade Federal do Tocantins, Universidade Federal de Uberlândia, Universidade Estadual Paulista Júlio de Mesquita Filho, Centro Universitário Serra dos Orgaos, Universidade de Fortaleza and Universidade de Passo Fundo.
Abbreviations
- ESS
Epworth Sleepiness Scale
- PSQI
Pittsburgh Sleep Quality Index
- SDI
Sleep Deprivation Index
- QoL
Overall quality of life
- MSQoL
Medical School related quality of life
- BDI
Beck Depression Inventory
- STAI
State Trait Anxiety Inventory
- DREEM
Dundee Ready Education Environment Measure
- VERAS-Q
Questionnaire to evaluate quality of life in students of health professions
Authors’ contributions
Study design: BP, HP, GL, MAM, PZT. Data collection: BP, EAF, HP, MAM, PZT. Data analysis: BP, FMA, SCE, ISS, GL. Writing of manuscript: BP, FMA, SCE, ISS, MAM, PZT. Review and approval of manuscript: BP, FMA, SCE, EAF, HP, ISS, GL, MAM, PZT.
Funding
This study was supported by the following Brazilian Scientific Agencies: FAPESP (Sao Paulo), CNPq (Brazil) and CAPES (Brazil).
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Ethics approval and consent to participate
The research protocol was approved by the Ethics Committee of the School of Medicine of the University of Sao Paulo (protocol number 181/11). All medical schools included approved the study.
Our study was performed according to STROBE (Strengthening the Reporting of Observational Studies in Epidemiology) guidelines for reporting observational studies.
Participation was voluntary, and we did not offer any compensation or incentive. We guaranteed both confidentiality and anonymity, and participating students completed an informed consent form.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests concerning this manuscript.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Azad MC, Fraser K, Rumana N, Abdullah AF, Shahana N, Hanly PJ, et al. Sleep disturbances among medical students: a global perspective. J Clin Sleep Med. 2015;15:69–74. doi: 10.5664/jcsm.4370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates Arch Gen Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 3.Palatty PL, Fernandes E, Suresh S, Baliga MS. Comparison of sleep pattern between medical and law students. Sleep Hypn. 2011;13:1–2. [Google Scholar]
- 4.Wong JGWS, Patil NG, Beh SL, Cheung EPT, Wong V, Chan LC, et al. Cultivating psychological well-being in Hong Kong's future doctors. Med Teach. 2005;27:715–719. doi: 10.1080/01421590500237945. [DOI] [PubMed] [Google Scholar]
- 5.Abdulghani HM, Alrowais NA, Bin-Saad NS, Al-Subaie NM, Haji AMA, Alhaqwi AI. Sleep disorder among medical students: relationship to their academic performance. Med Teach. 2012;34(Suppl 1):37–41. doi: 10.3109/0142159X.2012.656749. [DOI] [PubMed] [Google Scholar]
- 6.Gomes AA, Tavares J, de Azevedo MH. Sleep and academic performance in undergraduates: a multi-measure, multi-predictor approach. Chronobiol Int. 2011;28:786–801. doi: 10.3109/07420528.2011.606518. [DOI] [PubMed] [Google Scholar]
- 7.Curcio G, Ferrara M, De Gennaro L. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10:323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 8.Enns SC, Perotta B, Paro HB, Gannam S, Peleias M, Mayer FB, et al. Medical students' perception of their educational environment and quality of life: is there a positive association? Acad Med. 2016;91:409–417. doi: 10.1097/ACM.0000000000000952. [DOI] [PubMed] [Google Scholar]
- 9.Mayer FB, Santos IS, Silveira PSP, Lopes MHI, Souza ARND, Campos EP, et al. Factors associated to depression and anxiety in medical students: a multicenter study. BMC Med Educ. 2016;16:282. doi: 10.1186/s12909-016-0791-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Paro HBMS, Silveira PSP, Perotta B, Gannam S, Enns SC, Giaxa RRB, et al. Empathy among medical students: is there a relation with quality of life and burnout? PLoS One. 2014;9:e94133. doi: 10.1371/journal.pone.0094133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tempski P, Santos IS, Mayer FB, Enns SC, Perotta B, Paro HBMS, et al. Relationship among medical student resilience, educational environment and quality of life. PLoS One. 2015;29:e0131535. doi: 10.1371/journal.pone.0131535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14:540–545. doi: 10.1093/sleep/14.6.540. [DOI] [PubMed] [Google Scholar]
- 13.Bertolazi AN, Fagondes SC, Hoff LS, DartoraI EG, Miozzo ICS, Barba MEF, et al. Validation of the Brazilian Portuguese version of the Pittsburgh sleep quality index. Sleep Med. 2011;12:70–75. doi: 10.1016/j.sleep.2010.04.020. [DOI] [PubMed] [Google Scholar]
- 14.Buysse DJ, Berman SR, Kupfer DJ, Monk TH, Reynolds CF. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28:193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 15.WHOQOL Group The World Health Organization quality of life assessment (WHOQOL): position paper from the World Health Organization. Soc Sci Med. 1995;10:1403–1409. doi: 10.1016/0277-9536(95)00112-k. [DOI] [PubMed] [Google Scholar]
- 16.Fleck MPA, Leal OF, Louzada S, Xavier M, Chachamovich E, Vieira G, et al. Desenvolvimento da versão em português do instrumento de avaliação de qualidade de vida da OMS. Rev Bras Psiquiatr. 1999;21:19–28. doi: 10.1590/S1516-44461999000100006. [DOI] [Google Scholar]
- 17.Tempski P, Perotta B, Pose RA, Vieira JE. A questionnaire on the quality of life of medical students. Med Educ. 2009;43:1107–1108. doi: 10.1111/j.1365-2923.2009.03476.x. [DOI] [PubMed] [Google Scholar]
- 18.Peleias M, Tempski P, Paro HBMS, Perotta B, Mayer FB, Enns SC, et al. Leisure time physical activity and quality of life in medical students: results from a multicentre study. BMJ Open Sport Exerc Med. 2017;3:e000213. doi: 10.1136/bmjsem-2016-000213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Roff S, McAleer S, Harden RM, Al-Qahtani M, Ahmed AU, Deza H, et al. Development and validation of the Dundee ready education environment measure (DREEM) Med Teach. 1997;19:295–299. doi: 10.3109/01421599709034208. [DOI] [Google Scholar]
- 20.McAleer S, Roff S. A practical guide to using the Dundee ready education environment measure (DREEM) AMEE Education Guide No. 2001;23:29–33. [Google Scholar]
- 21.de Oliveira Filho GR, Vieira JE, Schonhorst L. Psychometric properties of the Dundee ready educational environment measure (DREEM) applied to medical residents. Med Teach. 2005;27:343–347. doi: 10.1080/01421590500046387. [DOI] [PubMed] [Google Scholar]
- 22.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 23.Gorenstein C, Andrade L. Validation of a Portuguese version of the Beck depression inventory and the state-trait anxiety inventory in Brazilian subjects. Braz J Med Biol Res. 1996;29:453–457. [PubMed] [Google Scholar]
- 24.Spielberger GL. Manual for the state-trait anxiety inventory. Palo Alto: Consulting psychologists Press; 1983. [Google Scholar]
- 25.Zailinawati AH, Teng CL, Chung YC, Teow TL, Lee PN, Jagmohni KS. Daytime sleepiness and sleep quality among Malaysian medical students. Med J Malaysia. 2009;64:108–110. [PubMed] [Google Scholar]
- 26.Giri P, Baviskar M, Phalke D. Study ofsleep habits and sleep problems among medical students of Pravara Institute of Medical Sciences Ioni, Western Maharashtra, India. Ann Med Health Sci Res. 2013;3:51–54. doi: 10.4103/2141-9248.109488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Feng G, Chen J, Yang X. Study on the status and quality of sleep-related influencing factors in medical college students. Zhonghua Liu Xing Bing Xue Za Zhi. 2005;26:328–331. [PubMed] [Google Scholar]
- 28.Medeiros ALD, Mendes DBF, Lima PF, Araujo JF. The relationships between sleep-wake cycle and academic performance in medical students. Biol Rhythm Res. 2001;32:263–270. doi: 10.1076/brhm.32.2.263.1359. [DOI] [Google Scholar]
- 29.Preišegolavičiūtė E, Leskauskas D, Adomaitienė V. Associations of quality of sleep with lifestyle factors and profile of studies among Lithuanian students. Medicina (Kaunas) 2010;46:482–489. doi: 10.3390/medicina46070070. [DOI] [PubMed] [Google Scholar]
- 30.Beijamini F, Knutson KL, Lorenzi-Filho G, Egan KJ, Taporoski TP, De Paula LKG, et al. Timing and quality of sleep in a rural Brazilian family-based cohort, the Baependi heart study. Sci Rep. 2016;6:39283. doi: 10.1038/srep39283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Arnal PJ, Sauvet F, Leger D, van Beers P, Bayon V, Bougard C, et al. Benefits of sleep extension on sustained attention and sleep pressure before and during total sleep deprivation and recovery. Sleep. 2015;38:1935–1943. doi: 10.5665/sleep.5244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Harrison Y, Horne JA. Long-term extension to sleep--are we chronically sleep deprived. Psychophysiology. 1996;33:22–30. doi: 10.1111/j.1469-8986.1996.tb02105.x. [DOI] [PubMed] [Google Scholar]
- 33.Kitamura S, Katayose Y, Nakazaki K, Motomura Y, Oba K, Katsunuma R, et al. Estimating individual optimal sleep duration and potential sleep debt. Sci Rep. 2016;24:35812. doi: 10.1038/srep35812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Klerman EB, Dijk D-J. Age-related reduction in the maximal capacity for sleep - implications for insomnia. Curr Biol. 2008;18:1118–1123. doi: 10.1016/j.cub.2008.06.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Rajaratnam SMW, Middleton B, Stone BM, Arendt J, Dijk D-J. Melatonin advances the circadian timing of EEG sleep and directly facilitates sleep without altering its duration in extended sleep opportunities in humans. J Physiol. 2004;15:339–351. doi: 10.1113/jphysiol.2004.073742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wehr TA, Moul DE, Barbato G, Giesen HA, Seidel JA, Barker C, et al. Conservation of photoperiod-responsive mechanisms in humans. Am J Physiol Integr Comp Physiol. 1993;265:R846–R857. doi: 10.1152/ajpregu.1993.265.4.R846. [DOI] [PubMed] [Google Scholar]
- 37.Hirshkowitz M, Whiton K, Albert SM, Alessi C, Bruni O, DonCarlos L, et al. National Sleep Foundation’s sleep time duration recommendations: methodology and results summary. Sleep Health. 2015;1:40–43. doi: 10.1016/j.sleh.2014.12.010. [DOI] [PubMed] [Google Scholar]
- 38.Hansen M, Janssen I, Schiff A, Zee PC, Dubocovich ML. The impact of school daily schedule on adolescent sleep. Pediatrics. 2005;115:1555–1561. doi: 10.1542/peds.2004-1649. [DOI] [PubMed] [Google Scholar]
- 39.Daugherty SR, Baldwin DC. Sleep deprivation in senior medical students and first-year residents. Acad Med. 1996;71:S93–S95. doi: 10.1097/00001888-199601000-00054. [DOI] [PubMed] [Google Scholar]
- 40.Cruess RL, Cruess SR, Boudreau JD, Snell L, Steinert Y. A schematic representation of the professional identity formation and socialization of medical students and residents. Acad Med. 2015;90:718–725. doi: 10.1097/ACM.0000000000000700. [DOI] [PubMed] [Google Scholar]
- 41.Tempski P, Bellodi PL, Paro HBMS, Enns SC, Martins MA, Schraiber LB. What do medical students think about their quality of life? A qualitative study. BMC Med Educ. 2012;12:106. doi: 10.1186/1472-6920-12-106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Prenskly M. Digital natives, digital immigrants. MCB University Press. 2001;9:1–6. [Google Scholar]
- 43.Anderson J, Beckitt D, Geal MA, Cocker P. How clinical students spend their time. Br J Med Educ. 1968;2:4–10. doi: 10.1111/j.1365-2923.1968.tb01995.x. [DOI] [PubMed] [Google Scholar]
- 44.Johns MW, Hocking B. Daytime sleepiness and sleep habits of Australian workers. Sleep. 1997;20:844–849. doi: 10.1093/sleep/20.10.844. [DOI] [PubMed] [Google Scholar]
- 45.Johns MW. Reliability and factor analysis of the Epworth sleepiness scale. Sleep. 1992;15:376–381. doi: 10.1093/sleep/15.4.376. [DOI] [PubMed] [Google Scholar]
- 46.Webb E, Ashton CH, Kelly P, Kamali F. Alcohol and drug use in UK university students. Lancet. 1996;348:922–925. doi: 10.1016/S0140-6736(96)03410-1. [DOI] [PubMed] [Google Scholar]
- 47.Chen D, Lew R, Hershman W, Orlander J. A cross-sectional measurement of medical student empathy. J Gen Intern Med. 2007;22:1434–1439. doi: 10.1007/s11606-007-0298-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Killgore WDS, Kahn-Greene ET, Lipizzi EL, Newman RA, Kamimori GH, Balkin TJ. Sleep deprivation reduces perceived emotional intelligence and constructive thinking skills. Sleep Med. 2008;9:517–526. doi: 10.1016/j.sleep.2007.07.003. [DOI] [PubMed] [Google Scholar]
- 49.Kloster MC, Perotta B, Hauer JA, Paro HB, Tempski P. Sonolência diurna e habilidades sociais em estudantes de medicina. Rev Bras Educ Med. 2013;37:103–109. doi: 10.1590/S0100-55022013000100015. [DOI] [Google Scholar]
- 50.Loayza HMP, Ponte TS, Carvalho CG, Pedrotti MR, Nunes PV, Souza CM, et al. Association between mental health screening by self-report questionnaire and insomnia in medical students. Arq Neuropsiquiatr. 2001;59:180–185. doi: 10.1590/S0004-282X2001000200005. [DOI] [PubMed] [Google Scholar]
- 51.Asghari A, Mohammadi F, Kamrava SK, Jalessi M, Farhadi M. Evaluation of quality of life in patients with obstructive sleep apnea. Eur Arch Otorhinolaryngol. 2013;270:1131–1136. doi: 10.1007/s00405-012-2157-6. [DOI] [PubMed] [Google Scholar]
- 52.Uchmanowicz I, Koltuniuk A, Stepién A, Uchmanowicz B, Rosińczuk J. The influence of sleep disorders on the quality of life in patients with chronic low back pain. Scand J Caring Sci. 2019;33:119–127. doi: 10.1111/scs.12610. [DOI] [PubMed] [Google Scholar]
- 53.Yosunkaya S, Kutlu R, Cihan FG. Evaluation of depression and quality of life in patients with obstructive sleep apnea syndrome. Niger J Clin Pract. 2016;19:573–579. doi: 10.4103/1119-3077.188703. [DOI] [PubMed] [Google Scholar]
- 54.Abraham R, Ramnarayan K, Vinod P, Torke S. Students’ perceptions of learning environment in an Indian medical school. BMC Med Educ. 2008;11:1–5. doi: 10.1186/1472-6920-8-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Aghamolaei T, Fazel I. Medical students’ perceptions of the educational environment at an Iranian Medical Sciences University. BMC Med Educ. 2010;29:87. doi: 10.1186/1472-6920-10-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Bouhaimed M, Thalib L, Doi SAR. Perception of the educational environment by medical students undergoing a curricular transition in Kuwait. Med Princ Pract. 2009;18:204–208. doi: 10.1159/000204351. [DOI] [PubMed] [Google Scholar]
- 57.Jiffry MTM, McAleer S, Fernando S, Marasinghe RB. Using the DREEM questionnaire to gather baseline information on an evolving medical school in Sri Lanka. Med Teach. 2005;27:348–352. doi: 10.1080/01421590500151005. [DOI] [PubMed] [Google Scholar]
- 58.Alapin I, Fichten CS, Libman E, Creti L, Bailes S, Wright J. How is good and poor sleep in older adults and college students related to daytime sleepiness, fatigue, and ability to concentrate? J Psychosom Res. 2000;49:381–390. doi: 10.1016/S0022-3999(00)00194-X. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.