Abstract
Background
COVID-19 has brought unprecedented demands to general practitioners (GPs) worldwide. We examined their knowledge, preparedness, and experiences managing COVID-19 in Australia.
Methods
A cross-sectional online survey of GPs members of the Royal Australian College of General Practitioners (RACGP) was conducted between June and September 2020.
Results
Out of 244 survey responses, a majority of GPs (76.6%) indicated having good knowledge of COVID-19, relying mostly on state/territory department of health (84.4%) and the RACGP (76.2%) websites to source up-to-date information. Most felt prepared to manage patients with COVID-19 (75.7%), yet over half reported not receiving training in the use of PPE. The majority were concerned about contracting SARS-CoV-2, more stressed than usual, and have heavier workloads. Their greatest challenges included scarcity of PPE, personal distress, and information overload.
Conclusion
Access to PPE, training, accurate information, and preparedness are fundamental for the successful role of general practices during outbreaks.
Keywords: COVID-19, General practitioners, Personal protective equipment, Primary health care, Outbreaks
Introduction
The Coronavirus disease 2019 (COVID-19) has introduced countless challenges to global health systems forcing institutions and stakeholders to rapidly adapt in order to control the spread [1]. Australia responded to the early outbreak [2,3], implementing an array of measures across federal, state and territory governments [[4], [5], [6]].
General practitioners (GPs) are usually the first point of contact the Australian community has with the health system, and they are critical to any public health crisis response. In most countries, key components of effectively providing primary care healthcare have been challenged while managing the COVID-19 pandemic [7]. Experiences of GPs as reported in the literature have included rapid restructuring of practice systems and processes including telehealth consultations, clinical pathway redesign and resources prioritisation [[8], [9], [10]]. Several Australian studies have attempted to profile GPs response to COVID-19 focusing on the pandemic's impact on daily practice nation-wide [11]. Yet, there are still gaps in information to further describe the experiences of GPs working during COVID-19. This study examines the knowledge, preparedness and experiences of GPs managing COVID-19 in the Australian healthcare settings.
Methods
Study design
A cross-sectional study using an online survey was conducted supported by The Royal Australian College of General Practitioners (RACGP) using their channels of communication.
Setting and population
Individuals holding current membership with RACGP were invited to participate. Members of the RACGP include Australian registered GPs (including retried or GPs not currently in active clinical general practice), overseas registered medical practitioners, and students/trainees working towards general practice. No other inclusion or exclusion criteria were considered. Participation consent was based explicitly on submission of the survey.
Instrument development
A voluntary, anonymous online survey was developed using the Research Electronic Data Capture (REDcap™) software by a panel of experts from general practice, primary healthcare, infectious diseases, and infection prevention and disease control. The Capability, Opportunity, Motivation, Behaviour (COM-B) model of behaviour [12] was used in constructing the survey questions. Survey questions were adapted from questionnaires used to study healthcare workers' perspectives amid previous outbreaks, and included several COVID-19 specific questions [[13], [14], [15], [16], [17], [18], [19], [20]]. The instrument comprised 36 close and open questions related to: i) respondents’ demographics; ii) knowledge about COVID-19; iii) preparedness for COVID-19; and iv) experiences of working in a pandemic. The survey was reviewed, pilot tested and validated by the expert panel prior to distribution.
Data collection and analysis
The survey was sent out to 36,515 RACGP members via e-newsletters and emails by the college secretariat and was active between June and September 2020. Once closed, raw data were downloaded from REDcap™, cleaned in Microsoft Excel, and analysed in IBM SPSS 26®. Questions with no response were treated as missing values, with the respective denominator adjusted accordingly. Descriptive statistics were used to analyse the data. Responses to open questions were analysed using content analysis. Coding categories derived from participants answers to open questions. The emergent codes were then organised and grouped into meaningful clusters which provided further information about the concept being explored [21]. Human research ethics approval was sought and granted for this study from the University of Sydney (HREC number 2020/200).
Results
There were 278 survey responses collected. Of these, 33 were excluded due to incompletion beyond the demography section. Consequently, 244 survey responses were included in the analysis.
GPs from all Australian states and territories participated in the survey, with the largest proportion confirming NSW as their current location for work (36.9%, n = 90). Respondents reported an average of 21.04 (SD 11.76) years of professional experience (Table 1 ).
Table 1.
General practitioners’ demographics and other characteristics.
| Characteristics | N = 244 (%) |
|---|---|
| Current state or territory of work: | |
| Australian Capital Territory | 7 (2.9) |
| New South Wales | 90 (36.9) |
| Northern Territory | 7 (2.9) |
| Queensland | 41 (16.8) |
| South Australia | 21 (8.6) |
| Tasmania | 9 (3.7) |
| Victoria | 53 (21.7) |
| Western Australia | 16 (6.6) |
| Country of residency: | |
| Australia | 241 (98.8) |
| Other countries | 3 (1.2) |
| Member of COVID-19 planning and response committee: | |
| Not a member | 166 (68) |
| At local practice level | 54 (22.1) |
| At hospital level | 14 (5.7) |
| At health district level | 20 (8.2) |
| At corporate practice level | 1 (0.4) |
| At state level | 15 (6.1) |
| At national level | 4 (1.6) |
| At international level | 3 (1.2) |
Knowledge about COVID-19
A majority of GPs (76.6%, n = 187) rated their level of knowledge about COVID-19 at the time of the survey as ‘good’ (41.8%, n = 102) or ‘very good’ (34.8%, n = 85).
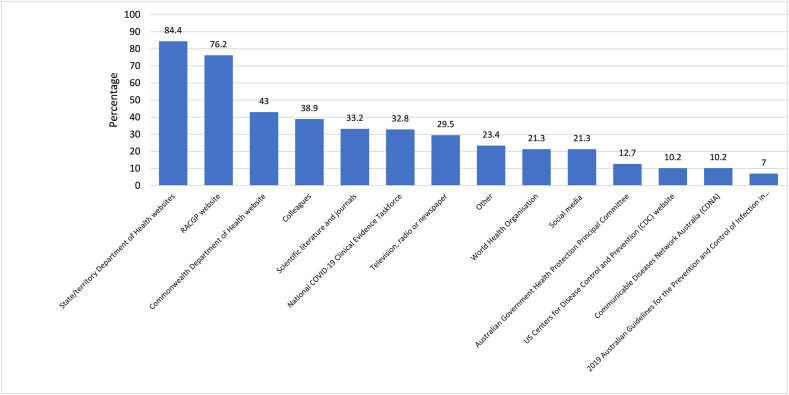
Respondents were asked where they went for up-to-date information about COVID-19 (Fig. 1 ). A majority routinely used their respective state/territory department of health websites (84.4%, n = 206), resources available within the RACGP website (76.2%, n = 186), and the Commonwealth Department of Health website (43%, n = 105).
Figure 1.
Sources of up-to-date COVID-19 information used by respondents.
Throughout the pandemic, the RACGP has provided its membership with a variety of COVID-19 resources (Supplementary Fig. 1). The top three RACGP resources used by GPs were specific information about the new Medicare benefits Schedule (MBS) items for phone and video consultation (65.6%, n = 160), protocols on assessing and testing patients with suspected mild COVID-19 (52%, n = 127), and guidelines on managing suspected cases in general practice (50.4%, n = 123).
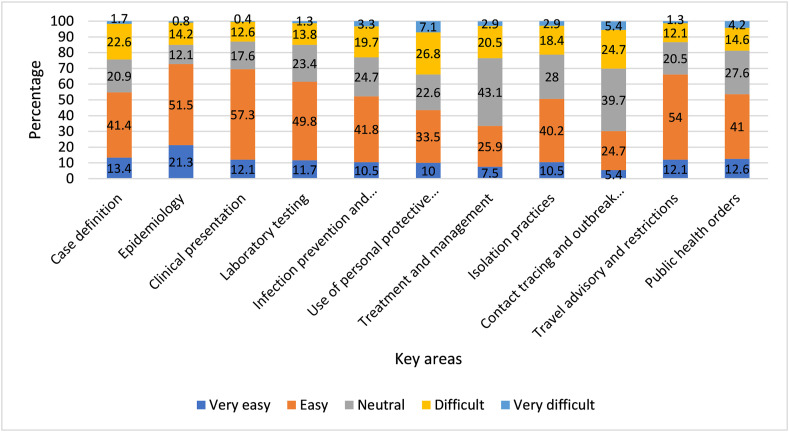
We asked GPs how easy it was to keep up-to-date with 11 areas of COVID-19 information. They found ‘contact tracing and outbreak management’ (30.1%, n = 72), ‘treatment and management’ (33.4%, n = 80), and ‘use of personal protective equipment (PPE)’ (43.5%, n = 104) difficult areas to keep up with. The majority indicated it was ‘easy’ or ‘very easy’ to follow COVID-19 information across all other fields (Fig. 2 ).
Figure 2.
GPs' opinion about how easy or difficult it is to keep up-to-date with 11 key areas of information about COVID-19.
Preparedness for COVID-19
On an individual level, most GPs (73.9%, n = 173) reported they were not at all prepared for COVID-19 on 31 December 2019. However, by the time of survey completion, most of them (75.7%, n = 177) felt ‘moderately’ or ‘extremely’ prepared for managing the pandemic. A smaller proportion (61.5%, n = 144) agreed their respective general practice/healthcare facility was ‘moderately’ or ‘extremely’ prepared to manage COVID-19 into the future. In contrast, 18% of GPs (n = 42) felt that Australia was ‘moderately’ or ‘extremely’ prepared against the pandemic.
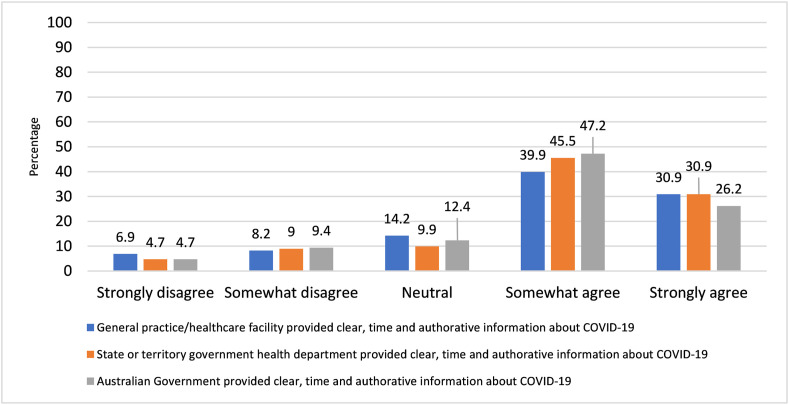
Most GPs stated that clear, timely and authoritative information about COVID-19 had been efficiently provided by their workplace (70.8%, n = 165/233), state or territory health department (76.4%, n = 178), and by the Australian Department of Health (73.4%, n = 171) (Fig. 3 ).
Figure 3.
GPs opinion about the provision of clear, timely and authoritative information about COVID-19.
More than half of GPs (56.7%, n = 132/233) reported that their workplace had COVID-19 guidelines and an outbreak response plan in place. Of these, most (75%, n = 99) stated they were ‘moderately’ or ‘extremely familiar’ with guidelines and plans and that these were ‘easy’ or ‘very easy’ to adhere to (60.6%, n = 80). Some participants (28.8%, n = 67) did not know if they existed, while others (14.6%, n = 34) reported neither existed in their workplace.
Over half of GPs (59.2%, n = 138) reported having specific education, training, or instruction about COVID-19 within their workplace. The nature of this instruction varied, with 45.1% reporting it as in-house education (n = 110), RACGP webinars (21.7%, n = 53), training by PHN (20.9%, n = 51), and provided by external parties (17.2%, n = 42). The vast majority rated these instructions as ‘mostly’ or ‘entirely’ adequate (81.1%, n = 112/138).
The majority of the GPs (63.1%, n = 147) reported not receiving training or certification in the use of PPE for managing COVID-19. For those who did, 69.8% rated it as ‘mostly’ or ‘entirely’ adequate (n = 60). In terms of their level of confidence in using PPE for managing COVID-19 patients, more than half (52.4%, n = 122/233) reported they were not confident to some extent (Table S1).
Experiences with COVID-19
Most GPs indicated their workplace was involved in assessing (63.2%, n = 146/231) and treating suspected or confirmed cases of COVID-19 (73.6%, n = 170/231). Just over half (51.2%, n = 125) of the respondents reviewed and updated policies or procedures as well as supporting healthcare staff (48%, n = 117). While some participated in establishing fever clinics (13.5%, n = 33) and planning for surge capacity (22.1% n = 54), as per Table S2.
Most GPs (77.1%, n = 178/231) were ‘slightly to moderately’ concerned about contracting SARS-CoV-2. However, a small proportion of the respondents took annual leave (7.8%, n = 18/231) or sick leave (9.1%, n = 21) due to their concern about contracting SARS-CoV-2. Almost three-quarters (74.9%, n = 173/231) of GPs avoided telling others about their involvement caring for COVID-19 patients out of fear of negative reactions. While almost a third (29.9%, n = 69/231) said they felt their family or friends had avoided contact with them due to the nature of their work, and 17.3% (n = 40/231) had experienced or witnessed racial or other forms of discrimination at work associated with the outbreak.
While most GPs (86.1%, n = 199/231) felt more stressed at work than usual due to COVID-19, some (13.9%, n = 32/231) were not stressed at all. Over half (62.4%, n = 144/231) reported that COVID-19 had somewhat increased their workload, whereas 13% (n = 30/231) indicated their workload had remained the same and 24.6% (n = 57/231) that it had lessened.
Less than half of the GPs (42.8%, n = 99/231) indicated their workplace provided staff debriefings and psychological support services regarding COVID-19. The majority reported never having attended debriefings (62.3%, n = 144/231). Likewise, almost all never had accessed psychological support services (95.7%, n = 221/231). For those who did attend debriefings or psychological support, 35.2% (n = 81) and 3.5% (n = 8) rated them ‘useful’ to some extent, respectively. Further details are listed in Table S3.
We asked respondents to identify significant challenges experienced during COVID-19. We received 115 open text responses, which were organised in 10 categories (Table S4). The top three challenges were: i) PPE supply and availability at their general practice (23 comments, 20%); ii) increasing level of stress triggered by factors including feeling unprepared at early stages of the pandemic, managing, and assessing suspected cases face-to-face, adapting to teleconsulting, and income loss (18 comments, 15.7%); and iii) keeping up with up-to-date information (16 comments, 13.9%).
Discussion
GPs are frontline healthcare workers (HCWs) in primary healthcare setting, and responsible for the initial provision of essential outpatient services to the community [22,23]. Previous outbreak responses have shown that frontline HCWs often face challenges including having to work under an emerging threatening environment [13,20], information overload [19], changes in their daily work [17], and stress [24]. Our study showed that GPs working during COVID-19 experienced similar challenges. The information provided, particularly at early stages of COVID-19 pandemic, was constantly changing, making it difficult for GPs to keep up-to-date. Previous reports have highlighted that multiple sources of information at a rapid changing pace will likely impact the professional learning process [25]. Yet, respondents' agreed that the provision of information about COVID-19 had been efficient and consistent through their workplace, state/territory health departments, Federal Government Department of Health and the RACGP. Clear messages have been reported to be crucial to help reassure HCWs’ preparedness and ultimately optimise work performance by reducing associated difficulties [26].
Although the majority of our respondents felt they kept up-to-date with key information relating to COVID-19, some reported difficulties with contact tracing and outbreak management, treatment and management, and the use of PPE. Previous studies also highlight these as the significant challenges in general practices worldwide [25,27,28]. COVID-19 requires multi-disciplinary and collaborative management. Coordination of the many disciplines in preparedness and response is critical to managing large outbreaks [25,27,28] Our respondents’ knowledge and level of preparedness to manage the pandemic was supported by the ease of access to official sources of information provided by state/territory departments of health and the RACGP. Nevertheless, they were not entirely prepared for the implementation of telehealth, ever-changing protocols for patient assessment, testing and managing COVID-19. Interestingly, these have been recurrent topics voiced by other GPs worldwide [11,27,29,30].
The availability and access to PPE, as well as its adequate use, have been critical to providing general practice services throughout the pandemic. Recent data suggest that the largest proportion of physician deaths have been GPs (42%) and emergency physicians, potentially due to the number of patients with COVID-19 seen by these specialties, as well as limited PPE [31]. Using PPE appropriately is critical to preventing transmission of COVID-19 in HCWs [32]. PPE shortages in general practice have been documented globally [8,33]. Studies from the UK found that 16.2% of GPs and 11% of emergency physicians had poor availability and accessibility to PPE [34,35]. The majority of our respondents expressed concerns about contracting SARS-CoV-2 and not feeling confident in using PPE. As first-contact practitioners for the community, GPs are at higher risk of exposure to COVID-19 [28]. It was noteworthy that most GPs avoided, or were reluctant, to disclose their involvement in caring for COVID-19 patients to minimise the risk of being subject to negative reactions. More proactive support focused on the needs of GPs, particularly in terms of risk of acquisition, should be considered and implemented.
It was noted that only about half of respondents confirmed their practice had COVID-19 guidelines and outbreak plans in place at the start of the pandemic. Although general practice specific pandemic plans were available, there was limited preparedness at an individual practice level. GP specific plans had been developed following the previous H1N1 pandemic through the RACGP Pandemic FluKit (aligned with the National AHMPPI) and the ERPT (emergency response planning tool) developed for GP business continuity in disasters and pandemics. These resources are readily available and should be referred to in future outbreaks to ensure GPs and medical practices are sufficiently prepared to manage patients during an outbreak or a pandemic of a similar scale. Our findings support recommendations from previous studies [25,36] which have emphasised that the primary healthcare services preparedness require active and effective ongoing support during interpandemic phases such that general practitioners can be assured that the rising demands over primary care are safely and adequately fulfilled in future pandemic emergencies.
Previous studies have reported high levels of stress and anxiety among front-line HCWs during large-scale outbreaks [37]. Our results demonstrate a similar effect on GPs, with a large majority feeling more stressed at work than usual due to COVID-19. This could be due to various factors including the levels of concern about contracting the virus and the reported unpredictable fluctuations in workload. It is interesting to note that despite confirming feeling stressed, only few respondents accessed psychological support services and debriefings provided by their practice. Previous studies have suggested that GPs are reluctant to seek psychological help [38]. The availability of mental health services for GPs and other healthcare providers during public health emergencies is critical to reduce stress and anxiety [39].
This study presents some limitations. Due to the voluntary nature of the survey, the response rate is rather low when compared to the RACGP membership, with no significant representation across all states or territories. An inherent limitation associated with the cross-sectional design of this study was that the variations in participants’ knowledge, preparedness and behaviours throughout the COVID-19 pandemic could not be explored. Future studies can employ longitudinal design to provide the necessary evidence for potential changes that could be of practical importance in pandemic planning and management.
Our results provide a broad insight into Australian GPs’ involvement managing COVID-19, highlighting the need for integration of planning and preparedness across general practice to ensure a strong primary healthcare system response to future pandemics.
Ethics
Human research ethics approval for this study was granted by The University of Sydney Human Research Ethics Committee (Approval 2020/200).
Authorship statement
CSC: Conceptualization, Methodology, Validation, Formal Analysis, Investigation, Data Curation, Writing Original Draft, Writing Review and Editing, Project Administration, Manuscript submission. SN: Conceptualization, Methodology, Validation, Formal Analysis, Investigation, Data Curation, Writing Review and Editing. CL: Conceptualization, Methodology, Validation, Formal Analysis, Data Curation, Writing Review and Editing. CH: Methodology, Formal Analysis, Data Curation, Writing Review and Editing. PB: Methodology, Formal Analysis, Data Curation, Writing Review and Editing. RZS: Conceptualization, Methodology, Validation, Formal Analysis, Investigation, Data Curation, Writing Original Draft, Writing Review and Editing. All authors contributed to the final analysis and interpretation of the results. All authors contributed to the drafting of this manuscript and approved it for submission.
Conflict of interest
Professor Ramon Z. Shaban is a senior editor of Infection, Disease and Health but was blinded to this submission in the journal’s editorial management system and had no role in the peer review or editorial decision-making whatsoever. There were no other conflicts of interest declared.
Funding
This study was an investigator-initiated research and did not receive financial support from funding agencies in the public, commercial or not-for-profit sectors.
Provenance and peer review
Not commissioned; externally peer reviewed.
Acknowledgements
Authors would like to thank the Royal Australian College of General Practitioners for their support and assistance in distributing the survey to their members.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.idh.2021.01.004.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kaba M., Kitaw Y. Novel Coronavirus (2019-nCoV) - reminiscent of Spanish flu: a challenge to global public health systems. Ethiop J Health Dev. 2020;34(1):1–4. [Google Scholar]
- 2.Duckett S., Stobart Anika. 2020. 4 ways Australia's coronavirus response was a triumph, and 4 ways it fell short the Conversation.https://theconversation.com/4-ways-australias-coronavirus-response-was-a-triumph-and-4-ways-it-fell-short-139845 Available from: [Google Scholar]
- 3.Bremmer I. 2020. The best global responses to COVID-19 pandemic. Time. [Google Scholar]
- 4.Australian Government Department of Health . 2020. Australian health sector emergency response plan for novel coronavirus (COVID-19) [Google Scholar]
- 5.Australian Government Department of Health . National Health Plan resources; 2020. Coronavirus (COVID-19) [Google Scholar]
- 6.Australian Comission on Safety and Quality in Health Care . 2020. COVID-19 infection prevention and control risk management - Guidance. [Google Scholar]
- 7.Chang A.Y., Cullen M.R., Harrington R.A., Barry M. The impact of novel coronavirus COVID-19 on noncommunicable disease patients and health systems: a review. J Intern Med. 2020 doi: 10.1111/joim.13184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma S.C., Sharma S., Thakker A., Sharma G., Roshan M., Varakantam V. Revolution in UK general practice due to COVID-19 pandemic: a cross-sectional survey. Cureus. 2020;12(8) doi: 10.7759/cureus.9573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Huston P., Campbell J., Russell G., Goodyear-Smith F., Phillips R.L., Jr., van Weel C. COVID-19 and primary care in six countries. BJGP Open. 2020;4(4) doi: 10.3399/bjgpopen20X101128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Marshall M., Howe A., Howsam G., Mulholland M., Leach J. COVID-19: a danger and an opportunity for the future of general practice. Br J Gen Pract. 2020;70(695):270–271. doi: 10.3399/bjgp20X709937. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kippen R., O'Sullivan B., Hickson H., Leach M., Wallace G. A national survey of COVID-19 challenges, responses and effects in Australian general practice. Aust J Gen Pract. 2020;49(11):745–751. doi: 10.31128/AJGP-06-20-5465. [DOI] [PubMed] [Google Scholar]
- 12.Michie S., van Stralen M.M., West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. doi: 10.1186/1748-5908-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Deng J.F., Olowokure B., Kaydos-Daniels S.C., Chang H.J., Barwick R.S., Lee M.L. Severe acute respiratory syndrome (SARS): knowledge, attitudes, practices and sources of information among physicians answering a SARS fever hotline service. Publ Health. 2006;120(1):15–19. doi: 10.1016/j.puhe.2005.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Piţigoi D., Săndulescu O., Ionescu T., Niţescu B., Niţescu M., Streinu-Cercel A. Assessment of knowledge, attitudes and perceptions regarding Ebola disease in healthcare workers from a tertiary care hospital in Romania. Publ Health. 2018;164:7–15. doi: 10.1016/j.puhe.2018.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lam S.K.K., Kwong E.W.Y., Hung M.S.Y., Pang S.M., Chiang V.C. Nurses' preparedness for infectious disease outbreaks: a literature review and narrative synthesis of qualitative evidence. J Clin Nurs. 2018;27(7–8):e1244–e1255. doi: 10.1111/jocn.14210. [DOI] [PubMed] [Google Scholar]
- 16.Kelly B., Squiers L., Bann C., Stine A., Hansen H., Lynch M. Perceptions and plans for prevention of Ebola: results from a national survey. BMC Publ Health. 2015;15:1136. doi: 10.1186/s12889-015-2441-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Alsahafi A.J., Cheng A.C. Knowledge, attitudes and behaviours of healthcare workers in the kingdom of Saudi Arabia to MERS coronavirus and other emerging infectious diseases. Int J Environ Res Publ Health. 2016;13(12) doi: 10.3390/ijerph13121214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Al-Amri S., Bharti R., Alsaleem S.A., Al-Musa H.M., Chaudhary S., Al-Shaikh A. Knowledge and practices of primary health care physicians regarding updated guidelines of MERS-CoV infection in Abha city. J Fam Med Prim Care. 2019;8(2):455–461. doi: 10.4103/jfmpc.jfmpc_336_18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Abbag H.F., El-Mekki A.A., Al Bshabshe A.A.A., Mahfouz A.A., Al-Dosry A.A., Mirdad R.T. Knowledge and attitude towards the Middle East respiratory syndrome coronavirus among healthcare personnel in the southern region of Saudi Arabia. J Infect Public Health. 2018;11(5):720–722. doi: 10.1016/j.jiph.2018.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Khan M.U., Shah S., Ahmad A., Fatokun O. Knowledge and attitude of healthcare workers about Middle East Respiratory Syndrome in multispecialty hospitals of Qassim, Saudi Arabia. BMC Publ Health. 2014;14:1281. doi: 10.1186/1471-2458-14-1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsieh H.F., Shannon S.E. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- 22.Cohidon C., Imhof F., Bovy L., Birrer P., Cornuz J., Senn N. Patients' and general practitioners' views about preventive care in family medicine in Switzerland: a cross-sectional study. J Prev Med Public Health. 2019;52(5):323–332. doi: 10.3961/jpmph.19.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Skarshaug L.J., Svedahl E.R., Bjørngaard J.H., Steinsbekk A., Pape K. Contact with primary health care physicians before an acute hospitalisation. Scand J Prim Health Care. 2019;37(3):283–293. doi: 10.1080/02813432.2019.1639900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Verma S., Mythily S., Chan Y.H., Deslypere J.P., Teo E.K., Chong S.A. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann Acad Med Singapore. 2004;33(6):743–748. [PubMed] [Google Scholar]
- 25.Gray R., Sanders C. A reflection on the impact of COVID-19 on primary care in the United Kingdom. J Interprof Care. 2020;34(5):672–678. doi: 10.1080/13561820.2020.1823948. [DOI] [PubMed] [Google Scholar]
- 26.Prescott K., Baxter E., Lynch C., Jassal S., Bashir A., Gray J. COVID-19: how prepared are front-line healthcare workers in England? J Hosp Infect. 2020;105(2):142–145. doi: 10.1016/j.jhin.2020.04.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wright M., Versteeg R., Hall J. General practice's early response to the COVID-19 pandemic. Aust Health Rev. 2020;44(5):733–736. doi: 10.1071/AH20157. [DOI] [PubMed] [Google Scholar]
- 28.Campbell R.G. SARS-CoV-2 and the nose: risks and implications for primary care. Aust J Gen Pract. 2020;49(11):728–732. doi: 10.31128/AJGP-05-20-5452. [DOI] [PubMed] [Google Scholar]
- 29.The Royal Australian College of General Practitioners . RACGP; Vic: 2020. Coronavirus (COVID-19) information for GPs east Melbourne.www.racgp.org.au/coronavirus Available from: [Google Scholar]
- 30.Lee A. General practitioners as frontiers in COVID-19: the Hong Kong experience. Aust J Gen Pract. 2020;49 doi: 10.31128/AJGP-COVID-15. [DOI] [PubMed] [Google Scholar]
- 31.Ing E.B., Xu Q.A., Salimi A., Torun N. Physician deaths from corona virus (COVID-19) disease. Occup Med (Lond) 2020;70(5):370–374. doi: 10.1093/occmed/kqaa088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ambigapathy S., Rajahram G.S., Shamsudin U.K., Khoo E.M., Cheah W.K., Peariasamy K.M. How should front-line general practitioners use personal protective equipment (PPE)? Malays Fam Physician. 2020;15(1):2–5. [PMC free article] [PubMed] [Google Scholar]
- 33.Fiorino G., Colombo M., Natale C., Azzolini E., Lagioia M., Danese S. Clinician education and Adoption of preventive measures for COVID-19: a survey of a convenience sample of general practitioners in Lombardy, Italy. Ann Intern Med. 2020;173(5):405–407. doi: 10.7326/M20-1447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Trivedi N., Trivedi V., Moorthy A., Trivedi H. Recovery, restoration and risk: a cross sectional survey of the impact of COVID-19 on general practitioners in the first UK city to lockdown. BJGP Open. 2020 doi: 10.3399/bjgpo.2020.0151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Mantelakis A., Spiers H.V.M., Lee C.W., Chambers A., Joshi A. Availability of personal protective equipment in NHS hospitals during COVID-19: a national survey. Ann Work Expo Health. 2020 doi: 10.1093/annweh/wxaa087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li X., Krumholz H.M., Yip W., Cheng K.K., De Maeseneer J., Meng Q. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–1812. doi: 10.1016/S0140-6736(20)30122-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Maunder R. The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philos Trans R Soc Lond B Biol Sci. 2004;359(1447):1117–1125. doi: 10.1098/rstb.2004.1483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Davidson S.K., Schattner P.L. Doctors' health-seeking behaviour: a questionnaire survey. Med J Aust. 2003;179(6):302–305. doi: 10.5694/j.1326-5377.2003.tb05552.x. [DOI] [PubMed] [Google Scholar]
- 39.Monterrosa-Castro A., Redondo-Mendoza V., Mercado-Lara M. Psychosocial factors associated with symptoms of generalized anxiety disorder in general practitioners during the COVID-19 pandemic. J Invest Med. 2020;68(7):1228–1234. doi: 10.1136/jim-2020-001456. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.