Abstract
Context: Medical cannabis use has increased in recent years despite being a federally illegal drug in the United States. States with medical cannabis use laws require patients to be certified by physicians. However, little is known about the education, knowledge, and practice characteristics of physicians who recommend and supervise patients' use of medical cannabis.
Objective: This study assessed how U.S. physicians who practice cannabis medicine are educated, self-assess their knowledge, and describe their practice.
Methods: In fall 2017, a 57-item, electronic survey was sent to all members of the Society of Cannabis Clinicians. Because California has had legalized medical cannabis for longer than any other state, we analyzed responses for 14 items between California and non-California physicians.
Results: Of 282 surveyed, 133 were eligible and 45 completed the survey. Of those, multiple medical specialties were represented. Only one physician received education during medical school about cannabis medicine, but physicians gained knowledge through conferences (71%, 32/45), the medical literature (64%, 29/45), and websites (62%, 28/45). Just over half (56%, 20/45) felt that there was sufficient information available to practice cannabis medicine. Of the 37 who answered the knowledge question, most felt knowledgable about cannabinoids (78%, 29/37) and the endocannabinoid system (76%, 28/37). There was a wide variation in the number of cannabis recommendations provided by physicians over the course of their practice career (median 1200; interquartile range, 100–5000), and most provided condition-specific treatment (69%, 31/45) and dosing recommendations (62%, 28/45). The majority (81%, 30/37) of physicians received referrals from mainstream medical providers. No differences were found between California and non-California physicians, except more women were from California (p=0.02).
Conclusions: The use of medical cannabis continues to increase in the United States and globally. All states that allow medical cannabis require a physician's recommendation, yet few states require specific clinical training. Findings of this study suggest the need for more formal education and training of physicians in medical school and residency, more opportunities for cannabis-related continuing medical education for practicing physicians, and clinical and basic science research that will inform best practices in cannabis medicine.
Keywords: medical cannabis, marijuana, cannabinoid, education, self-assessment
Introduction
In 1996, California became the first U.S. state to legalize medical cannabis, ushering in a new era of states asserting the right to use medical cannabis. Today, medical cannabis is legal in 33 states as well as the District of Columbia, Guam, and Puerto Rico,1 despite continuing to be a Schedule I federally illegal drug. Eleven of the 33 states additionally allow adult-use cannabis. However, all state laws require the patient to obtain a recommendation from a physician to use medical cannabis. Many states also allow a recommendation from an advanced practice nurse practitioner (e.g., District of Columbia, Hawaii, Maine, Minnesota, New Hampshire, New Mexico, New York, North Dakota, Utah, Vermont, and Washington) or physician assistant (e.g., District of Columbia, Maine, Minnesota, New Mexico, New York, Utah, Vermont, and Washington). A few states have specified cannabis-related training requirements for physicians (e.g., Florida, Ohio, New York, Pennsylvania, Washington, and West Virginia).
In 1999, just 3 years after state legalization of medical cannabis, the California Cannabis Research Medical Group was formed, so physicians could share information and collaborate with other physicians recommending cannabis to patients. In 2004, the Society of Cannabis Clinicians (SCC) was formed by members of this group. The SCC is the oldest U.S. scientific organization of clinicians supporting the use of medical cannabis, and is comprised of physicians and allied professionals from around the world. One of its stated goals is to facilitate the “best practice standards for cannabis consultations.”2
Currently, there are a number of physicians across the country who practice cannabis medicine primarily by assessing patients and making recommendations of its use for approved state medical conditions to meet the state requirement for a physician recommendation. However, it is unknown how these cannabis physicians become educated and knowledgable about a therapy that is federally illegal, rarely included in medical school curricula, and has limited clinical evidence to guide them.3,4 Therefore, the purpose of this study was to assess how U.S. physicians who practice cannabis medicine are educated, self-assess their knowledge, and describe their practice. Since California physicians have engaged in the field of cannabis medicine longer than physicians in other states, we hypothesized that their knowledge would be greater than physicians in other states.
Materials and Methods
Study design and participants
This study used an electronic survey. In September 2017, 282 SCC members listed in the SCC e-mail database were e-mailed an invitation to participate in the study. Members of the SCC include physicians, clinical and research associates, health care associates, graduate students, veterans, and affiliates. The invitation described the study and included a link to the electronic survey. Survey respondents were told that by clicking on the survey link they were providing informed consent. Reminder e-mails, which included the survey link, were sent at least once a week for 4 weeks after the initial e-mail. After 4 weeks, a final e-mail, and six e-mail invitations to participate, the study was closed. No incentives were used to encourage participation. We included only licensed U.S. physicians in the results. International members and nonphysician members were excluded from participation. The A.T. Still University-Mesa Institutional Review Board reviewed the study and considered it to be exempt.
Survey instrument
The electronic survey used in this study was designed specifically for the study by members of the SCC board of directors and research committee and by researchers from A.T. Still University. The survey was created and managed utilizing Research Electronic Data Capture (REDCap), a secure web-based data collection tool.5 The survey consisted of 57 items that were organized into three sections: demographics, physician assessment, and research.
Because of the extensive number of questions on the survey, for reporting of this study we focused our analysis on the portions of the survey that were most generalizable to the practice of cannabis medicine. Specifically, we chose four demographic characteristics, five education questions, one knowledge question, and four practice characteristic questions. Demographic information analyzed included gender, type of physician (e.g., allopathic [MD] or osteopathic [DO]), state licensed to practice cannabis medicine, and types of board certifications.
Education questions asked about any education received in clinical cannabis medicine in either medical school or residency (yes or no), where they obtained information and education about cannabinoid medicine (seven different choices including “other” with an option to write in a response), whether they completed online medical cannabis continuing medical education (CME, yes or no), whether they felt there was sufficient information available to perform their job as a cannabis specialist (yes or no), and ranking 7 different educational modalities on preference for receiving medical cannabis education (from 1 [least preferred] to 7 [most preferred]).
The knowledge question asked how well informed they felt on the properties of cannabinoids, the properties of terpenes, and other phytoconstituents of cannabis, and the endocannabinoid system (5-point Likert-like scale from 1 [uninformed] to 5 [expert]). The practice characteristic questions asked what percentage of their practice involved cannabis recommendations (visual analog scale), how many patients they provided cannabis recommendations to (fill in the blank), what components of cannabinoid medicine they provided in their practice (six multiple choices including “other” with an option to write in a response), and whether they received referrals from mainstream medical providers (yes or no).
Data analysis
Frequency and percentage, median and interquartile range (IQR), or mean and standard error (SE) were reported for survey responses. Doctors were categorized into California and non-California based on where they self-reported their state of practice. Fisher's exact tests were used to assess the association between California practice with demographic information, education at medical school and residency, where information and education were obtained, feeling knowledgable about cannabinoids, terpenes, and the endocannabinoid system (defined as at least 4 on the 5-point Likert-like scale), components of cannabis medicine, and referrals. A mixed-effects model was used to test whether preference rankings for any of the seven education modalities depended on California practice. A random participant effect was used to allow for correlation of responses from the same participant. Wilcoxon rank-sum tests were used to test for a difference between doctor categories in both the number of patients provided cannabis recommendations and the percentage of practices that involved cannabis recommendations. SAS version 9.4 software (SAS Institute, Inc.) was used to conduct the analyses. A p<0.05 was considered statistically significant.
Results
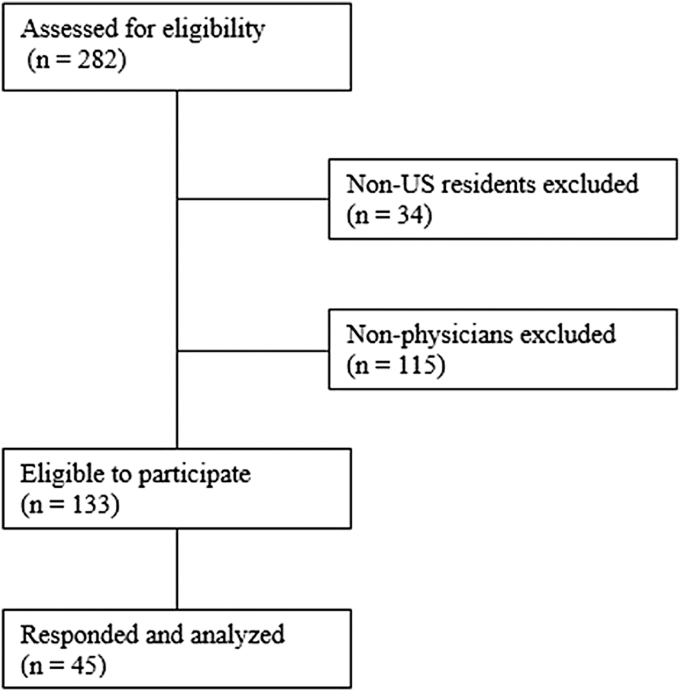
Forty-five physicians completed the study survey (33.8% response rate) (Fig. 1). Demographic characteristics of respondents are shown in Table 1. When comparing demographic characteristics of California (n=20) and non-California (n=25) respondents, only gender was significantly different: more women were from California (45%, 9/20) than non-California states (17%, 4/24, p=0.02).
FIG. 1.
Flow chart of survey responders.
Table 1.
Demographic Characteristics of Study Respondents
| Demographic characteristic | No. (%) |
p-Value | ||
|---|---|---|---|---|
| Total (N=45) | California (n=20) | Non-California (n=25) | ||
| Gendera | 0.02 | |||
| Male | 29 (66) | 9 (45) | 20 (83) | |
| Female | 13 (30) | 9 (45) | 4 (17) | |
| Neither/both | 2 (5) | 2 (10) | 0 (0) | |
| Professional qualifications | >0.99 | |||
| Allopathic physician | 43 (96) | 19 (95) | 24 (96) | |
| Osteopathic physician | 2 (4) | 1 (5) | 1 (4) | |
| State licensed to practice cannabinoid medicine | ||||
| California | 20 (44) | NA | NA | |
| Not California | 25 (56) | NA | NA | |
| Board-certified specialtyb,c | ||||
| Family medicine | 10 (29) | 6 (30) | 4 (16) | 0.30 |
| Emergency medicine | 6 (17) | 3 (15) | 3 (12) | >0.99 |
| Internal medicine | 5 (14) | 3 (15) | 2 (8) | 0.64 |
| Pediatrics | 2 (6) | 1 (5) | 1 (4) | >0.99 |
| Oncology | 2 (6) | 1 (5) | 1 (4) | >0.99 |
| Pain medicine | 2 (6) | 1 (5) | 1 (4) | >0.99 |
| Psychiatry | 1 (3) | 0 (0) | 1 (4) | >0.99 |
| Obstetrics/gynecology | 1 (3) | 0 (0) | 1 (4) | >0.99 |
| Other | 14 (40) | 5 (25) | 9 (36) | 0.76 |
N=44 because 1 respondent from outside California did not indicate gender.
N=35 because 10 participants did not indicate a specialty.
Individual physicians could be board certified in more than one specialty.
NA, not applicable.
Education
Of the 34 who indicated formal education in clinical cannabis medicine, only 1 respondent (3%) had some medical school education in cannabis medicine (Table 2). Four (12%) had some residency education. No differences were found between California and non-California respondents (both p>0.61).
Table 2.
Participant Responses to Survey Questions About Education
| Education | No. (%) |
p-Value | ||
|---|---|---|---|---|
| Total (N=45) | California (n=20) | Non-California (n=25) | ||
| Clinical cannabis medicine educationa | ||||
| Medical school | 1 (3) | 0 (0) | 1 (6) | >0.99 |
| Residency | 4 (12) | 1 (7) | 3 (16) | 0.61 |
| How cannabis information obtained | ||||
| Conferences | 32 (71) | 15 (75) | 17 (68) | 0.74 |
| Websites | 26 (58) | 12 (60) | 14 (56) | >0.99 |
| Peer-reviewed publications | 29 (64) | 13 (65) | 16 (64) | >0.99 |
| Communication with colleagues | 22 (49) | 10 (50) | 12 (48) | >0.99 |
| SCC website | 28 (62) | 14 (70) | 14 (56) | 0.37 |
| SCC quarterly meetings | 17 (38) | 11 (55) | 6 (24) | 0.06 |
| Other | 7 (16) | 4 (20) | 3 (12) | 0.68 |
| Completed online CME in cannabinoid medicineb | 29 (76) | 13 (72) | 16 (80) | 0.71 |
| Sufficient information to work as cannabis specialistc | 20 (56) | 8 (50) | 12 (60) | 0.74 |
N=34, n=15 for California, and n=19 for non-California.
N=38, n=18 for California, and n=20 for non-California.
N=36, n=16 for California, and n=20 for non-California.
CME, continuing medical education; SCC, Society of Cannabis Clinicians.
Most respondents obtained information and education about cannabis medicine through conferences (71%, 32/45), peer-reviewed medical literature (64%, 29/45), or the SCC website (62%, 28/45) (Table 2). Of the 38 who answered the question on their clinical education, the majority (76%, 29/38) completed online CME in cannabis medicine, and of the 36 who indicated their clinical needs, more than half (56%, 20/36) felt that there was sufficient information available to work as a cannabis specialist. No differences were found between California and non-California respondents (all p>0.06).
For obtaining sources of information related to the practice of cannabis medicine, most respondents preferred online CME and conferences (Table 3). The mean (SE) rank was 5.8 (0.3) for online CME and 5.6 (0.3) for conferences. No difference was found between California and non-California respondents (p=0.32).
Table 3.
Participant Preferences for Sources for Obtaining Information About Cannabinoid Medicine
| Preferred source | Mean (SE) [No.a] |
||
|---|---|---|---|
| Total (N=45) | California (n=20) | Non-California (n=25) | |
| Online CME | 5.8 (0.3) [27] | 5.3 (0.5) [11] | 6.2 (0.4) [16] |
| Conferences | 5.6 (0.3) [25] | 6.2 (0.4) [11] | 5.2 (0.4) [14] |
| Webcast | 4.3 (0.3) [24] | 4.6 (0.4) [10] | 4.1 (0.3) [14] |
| SCC quarterly meetings | 4.4 (0.3) [24] | 5.2 (0.5) [10] | 3.9 (0.4) [14] |
| Peer mentoring | 3.3 (0.3) [23] | 3.2 (0.4) [10] | 3.3 (0.4) [14] |
| Shadowing a cannabis clinician | 2.9 (0.5) [24] | 3 (0.7) [10] | 2.9 (0.6) [14] |
| Case discussions/informal consultations | 3.5 (0.4) [31] | 3.6 (0.5) [14] | 3.5 (0.5) [17] |
Responses ranked the seven educational modalities on preference for receiving medical cannabis education from least preferred (1) to most preferred (7).
Not all respondents ranked all educational modalities.
SE, standard error.
Knowledge
For the item assessing knowledge, 29 (78%) felt knowledgable on the properties of cannabinoids, 15 (41%) felt knowledgable on the properties of terpenes and other phytoconstituents of cannabis, and 28 (76%) felt knowledgable on the endocannabinoid system (Table 4). No differences were found between California and non-California respondents (all p>0.25).
Table 4.
Participant Responses on Feeling Knowledgable About Cannabinoids
| Knowledge | No. (%) |
p-Value | ||
|---|---|---|---|---|
| Total (N=37) | California (n=17) | Non-California (n=20) | ||
| Properties of cannabinoids | 29 (78) | 14 (82) | 15 (75) | 0.70 |
| Properties of terpenes and other phytoconstituents of cannabis | 15 (41) | 5 (29) | 10 (50) | 0.32 |
| Knowing endocannabinoid system | 28 (76) | 11 (64) | 17 (85) | 0.25 |
Responses were assessed on a 5-point Likert-like scale from uninformed (1 point) to expert (5 points). Classification of knowledgable was based on a response of at least 4.
Practice characteristics
Of the 37 who indicated their practice information, the median (IQR) percentage of practices that involved cannabis recommendations was 76 (24–99%) (Table 5). Of the 35 who responded about how many patient cannabis recommendations they have provided, the median number of patients provided cannabis recommendations over the course of their practice career was 1200 (100–5000), totaling over 160,000 patients treated. No differences were found between California and non-California respondents (both p>0.36).
Table 5.
Participant Responses to Survey Questions About Practice Characteristics
| Practice characteristic | Median (IQR) or No. (%) |
p-Value | ||
|---|---|---|---|---|
| Total (N=45) | California (n=20) | Non-California (n=25) | ||
| Percentage of practice involving cannabis recommendationsa | 76 (24–99) | 93 (20–100) | 57 (25–97) | 0.72 |
| No. of patients provided cannabis recommendationsb | 1200 (100–5000) | 2500 (150–8000) | 700 (100–3000) | 0.36 |
| Current practices | ||||
| Specific dosing recommendations | 28 (62) | 12 (60) | 16 (64) | >0.99 |
| Specific chemotype recommendations | 14 (31) | 9 (45) | 5 (20) | 0.11 |
| Specific phytoconstituent profile or ratio recommendations | 19 (42) | 7 (35) | 12 (48) | 0.54 |
| Specific delivery method recommendations | 26 (58) | 10 (50) | 16 (64) | 0.38 |
| Condition-specific treatment | 31 (69) | 13 (65) | 18 (72) | 0.75 |
| Other | 4 (9) | 2 (10) | 2 (8) | >0.99 |
| Received referrals from mainstream medical providersc | 30 (81) | 12 (71) | 18 (90) | 0.21 |
N=37, n=17 for California, and n=20 for non-California.
N=35, n=16 for California, and n=19 for non-California.
N=37, n=17 for California, and n=20 for non-California.
IQR, interquartile range.
More than half (62%, 28/45) of respondents provided specific dosing recommendations (Table 5). About a third (31%, 14/45) provided specific chemotype recommendations, and more than a third (42%, 19/45) provided specific phytoconstituent profile or ratio recommendations. More than half (58%, 26/45) provided specific delivery method recommendations, and most (69%, 31/45) provided condition-specific treatment recommendations. Of the 37 who responded about referrals, the majority (81%, 30/37) received referrals from mainstream medical providers. No differences were found between California and non-California respondents (all p>0.11).
Discussion
To our knowledge, this study is the first to describe the types of physicians who practice cannabis medicine, how they become educated, and how they self-assess their knowledge and describe their practice characteristics. We were somewhat surprised that there were no statistically significant differences between California and non-California physicians, except for gender (more women practiced in California). We would guess that not enough time had transpired between the legalization of medical cannabis in California and other states to see differences in education, knowledge, or practice characteristics. Two years after California legalized medical cannabis, Alaska, Oregon, and Washington legalized it. The next year, Maine legalized it, and the year after Colorado, Hawaii, and Nevada did.1 Thus, within 5 years, medical cannabis was legal in seven other states.
While the characteristics of study participants were similar (within 5% points) to the gender breakdown of U.S. physicians and the ratio of MD to DO for actively licensed physicians,6 almost half of respondents were from California. This over-representation of California physicians may be the result of SCC being founded in California or permissive attitudes from practicing in a state with a long movement to legalize cannabis that started in 1972 with Proposition 19, the California Marijuana Initiative.7,8 Board certification of respondents was spread across a variety of primary care specialties as we had expected since medical cannabis use reportedly affects a number of conditions that span many medical specialties.
Few respondents had any cannabis education in medical school or residency, which is consistent with another study.9 The lack of formal education makes intuitive sense given that the understanding of the endocannabinoid system is relatively recent,10 medical cannabis does not fall neatly into any specific curriculum, medical cannabis is not legal in all states, and synthesized or components of cannabis are an accepted U.S. Food and Drug Administration treatment in limited populations with just four medications (Cesamet,11 Epidiolex,12 Marinol,13 and Syndros14). The lack of medical cannabis education in medical school and residency curricula is incongruent with the progressive legalization of medical cannabis in additional states and the increasing prevalence of patients using or wanting to use cannabis for therapeutic purposes.
Physicians used a variety of resources to become educated about cannabis medicine. The majority used conferences, the medical literature, and websites, including the SCC website. The least used resources were SCC quarterly meetings, particularly for non-California physicians, and communication with colleagues. We were surprised that few used the SCC quarterly meetings, which are web-based meetings featuring an expert speaker, and that only half used collegial communication given the cannabis practice environment lacks established norms for treatment regimens. Over three-quarters completed online medical cannabis CME, which was the most common way of obtaining education. Despite a variety of available cannabis resources, just over half felt that there was sufficient information to work as a cannabis physician, which may represent a lack of scientific information necessary to practice or an educational gap in knowledge. Future studies should investigate the specific challenges of preparing physicians to practice cannabis medicine.
Understanding the methods preferred by physicians for obtaining information about cannabis medicine may help organizations like the SCC provide effective education to physicians in the field. Respondents of this study preferred obtaining information from online CME and conferences the most, followed by webcasts and SCC quarterly meetings. California physicians trended toward preferring SCC quarterly meetings more than non-California physicians. Perhaps there are more long-standing, collegial relationships among California physicians practicing cannabis medicine, or the proximity to meetings, which are often held in California but are web based to encourage remote participation, may be responsible for this result. Study respondents preferred case discussions/informal consultations, peer mentoring, and shadowing a cannabis clinician the least. Since this study was performed, the number of cannabis-related medical conferences and online CME courses available to all U.S. physicians has increased, which suggests a growing need to meet the demand for educational resources.
Respondents of this study felt knowledgable about the properties of cannabinoids and the endocannabinoid system but less so about the properties of terpenes. This result was expected because the intricacies of the endocannabinoid system have been known since the 1970s,10 but the interaction of cannabinoids and terpenoids has only recently been studied.15 This finding may indicate additional research, and education is needed to train physicians about cannabinoids and terpenoids.
In this study, the median percentage of practice involving cannabis recommendations was nearly double for California physicians when compared with non-California physicians. Although this difference was not statistically significant, it suggests that there may be a higher demand for recommendations in California than in other states, or that non-California respondents cared for relatively few patients requiring recommendations. The physicians who completed the survey provided care to >180,000 patients, and the majority of services provided were for condition-specific treatment recommendations, specific dosing recommendations, and delivery method recommendations. Less than half provided chemotype, phytoconstituent profile, or ratio recommendations. Given that condition-specific treatment recommendations and dosing and delivery methods are not clearly elucidated in the medical literature or necessarily even understood16,17 (though dosing recommendations have been proposed18), this result is not surprising. Similarly, information about chemotype and phytoconstituent profile recommendations is likely limited by the availability and consistency of products in each state, and again our results indicate a need for more research and education in chemotypes and phytoconstituent profile recommendations.
Surprisingly, over three-quarters of cannabis physicians received referrals from mainstream medical providers. This result may arise from limitations placed on physicians employed by hospitals and health care organizations that fear losing their federal license or the Centers for Medicare and Medicaid Services certification. Therefore, those physicians refer their patients to cannabis physicians. Another explanation for these results may be related to the increasing view among physicians that cannabis has therapeutic properties and treatment value (K.M. Takakuwa, F.S. Shofer, and R.M. Shears, unpublished data, 2019).
Our study is different from a Canadian national needs survey in which physicians were asked about their educational needs to provide cannabis for therapeutic purposes.19 Unlike our study that surveyed cannabis clinicians, they surveyed all doctors, of which 51% and 44% were reported to be specialists and general practitioners, respectively. Their biggest gap between their current and desired knowledge was for dosing and treatment plans using medical cannabis and their preferred educational format of online CME, our highest preferred method, placed second behind reading peer-reviewed literature.
Our study had several limitations. Only survey responses from U.S. physicians were analyzed since they are the only health care professionals who can recommend cannabis in all cannabis legal states. Although a third of eligible physicians completed the survey, which is a respectable response rate, SCC members who resided in states without legal cannabis laws or in nonoperational states may have been dissuaded from completing the survey because they thought it was irrelevant to them. While our sample size appears low and is arguably a small subset of the overall population of U.S. physicians, we believe that it is robust as a sample of cannabis physicians since it was drawn from the SCC, which is the oldest U.S. clinical organization of physicians supporting the use of medical cannabis. We unfortunately do not have an estimate of the number of U.S. physicians who consider themselves cannabis physicians because there is no official American Board of Medical Specialties subspecialty that includes cannabis medicine.20
Because we used an online survey, results are subject to participation bias. Further, our lower response rate may have arisen from possible measurement issues and technical challenges of an online survey.21 For example, some may have been dissuaded from completing the survey because of its length or because it was online, required technical and computer skills, or required users to use e-mail accounts. Alternatively, some may have feared being identified as a cannabis physician even though it was an anonymous survey. Because we only surveyed physician members of the SCC, our findings are not necessarily generalizable to all practicing cannabis physicians in the United States or other clinicians, such as advanced practice nurse practitioners or physician assistants, who can legally recommend cannabis in certain states. To address this limitation, a larger survey study could be conducted, which includes the entire cannabis clinician population; however, a way to identify and study this population must first be found.
Conclusion
Physicians surveyed in this study represented a wide array of physician specialties from multiple states that practice cannabis medicine. The respondents mostly received their cannabis medicine training from self-initiated sources because of limitations in formal medical education. While physicians felt knowledgable about some areas of cannabis medicine, there were other areas in which they had limited knowledge. Overall, our results suggest the need for more formal education and training of physicians during medical school and residency, more opportunities for cannabis-related CME, and clinical and basic science research that will elucidate best practices in cannabis medicine.
Acknowledgments
The authors are indebted to the Society of Cannabis Clinicians for their administrative support and to the members of the research committee who contributed to this project: Kirk Anderson, MD; Darlene Brice; Kenton Crowley, PharmD; Diane Dickenson, MD; Eric Gordon, MD; Mara Gordon; David Hepburn, MD; Albert Lai, MD; Anne Lee, MD; Taylor Lougheed, MD; Kenneth Malamud, MD; Urmila Sandhu, PA; Michelle Sexton, ND; Justin Sterett, MD; Stephen Robinson, MD; and Genester Wilson-King, MD. They also acknowledge Deborah Goggin, MA, ELS, for her editorial assistance in preparing the article.
Abbreviations Used
- CME
continuing medical education
- IQR
interquartile range
- REDCap
Research Electronic Data Capture
- SCC
Society of Cannabis Clinicians
Author Disclosure Statement
K.M.T. has a financial interest in the medical cannabis company MGC LLC that did not exist when this study was performed. D.S. is owner of Integr8 Health, equity owner of Healer.com, and medical advisor for Zelda Therapeutics.
Funding Information
No funding was received for this article.
Cite this article as: Takakuwa KM, Mistretta A, Pazdernik VK, Sulak D (2021) Education, knowledge, and practice characteristics of cannabis physicians: a survey of the Society of Cannabis Clinicians, Cannabis and Cannabinoid Research 6:1, 58–65, DOI: 10.1089/can.2019.0025.
References
- 1. National Conference of State Legislatures. State medical marijuana laws. . http://www.ncsl.org/research/health/state-medical-marijuana-laws.aspx. Accessed June25, 2019
- 2. Society of Cannabis Clinicians. Our Mission. http://www.cannabisclinicians.org/about-scc-2/. Accessed November15, 2018
- 3. Rubin R. Medical marijuana is legal in most states, but physicians have little evidence to guide them. JAMA. 2017;317:1611–1613 [DOI] [PubMed] [Google Scholar]
- 4. Häuser W, Petzke F, Fitzcharles MA. Efficacy, tolerability and safety of cannabis-based medicines for chronic pain management—an overview of systematic reviews. Eur J Pain. 2018;22:455–470 [DOI] [PubMed] [Google Scholar]
- 5. REDCap. About. https://projectredcap.org/about/. Accessed February3, 2019
- 6. Young A, Chaudhry HJ, Pei X, et al. A census of actively licensed physicians in the United States, 2016. J Med Regul. 2017;103:7–21 [Google Scholar]
- 7. Ballotpedia. California 1972 ballot propositions. https://ballotpedia.org/California_1972_ballot_propositions#November_7.2C_1972. Accessed February10, 2019
- 8. Lacey M. California rejects marijuana legalization. New York Times. November 3, 2010:P8. https://archive.nytimes.com/www.nytimes.com/2010/11/03/us/politics/03ballot.html. Accessed February2, 2019
- 9. Evanoff AB, Quan T, Dufault C, et al. Physicians-in-training are not prepared to prescribe medical marijuana. Drug Alcohol Depend. 2017;180:151–155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Di Marzo V. A brief history of cannabinoid and endocannabinoid pharmacology as inspired by the work of British scientists. Trends Pharmacol Sci. 2006;27:134–140 [DOI] [PubMed] [Google Scholar]
- 11. Cesamet (nabilone) [package insert]. Valeant Pharmaceuticals International; May 2006. https://www.accessdata.fda.gov/drugsatfda_docs/label/2006/018677s011lbl.pdf. Accessed January292019
- 12. U.S. Food and Drug Administration. FDA approves first drug comprised of an active ingredient derived from marijuana to treat rare, severe forms of epilepsy. Published June 25, 2018. https://www.fda.gov/newsevents/newsroom/pressannouncements/ucm611046.htm. Accessed September12, 2018
- 13. Marinol (dronabinol) [package insert]. AbbVie, Inc.; August 2017. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/018651s029lbl.pdf. Accessed January29, 2019
- 14. Syndros (dronabinol) [package insert]. Insys Therapeutics, Inc.; September 2018. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/205525s007lbl.pdf. Accessed January29, 2019
- 15. Russo EB. Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br J Pharmacol. 2011;163:1344–1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. National Academies of Sciences, Engineering, and Medicine. The Health Effects of Cannabis and Cannabinoids: the current state of evidence and recommendations for research. National Academies Press: Washington, DC, 2017 [PubMed] [Google Scholar]
- 17. Hanuš LO, Meyer SM, Muñoz E, et al. Phytocannabinoids: a unified critical inventory. Nat Prod Rep. 2016;33:1357–1392 [DOI] [PubMed] [Google Scholar]
- 18. MacCallum CA, Russo EB. Practical considerations in medical cannabis administration and dosing. Eur J Intern Med. 2018;49:12–19 [DOI] [PubMed] [Google Scholar]
- 19. Ziemianski D, Capler R, Tekanoff R, et al. Cannabis in medicine: a national educational needs assessment among Canadian physicians. BMC Med Educ. 2015;15:52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. American Board of Medical Specialties. Specialty and subspecialty certificates. https://www.abms.org/member-boards/specialty-subspecialty-certificates/. Accessed February13, 2019
- 21. Granello DH, Wheaton JE. Online data collection: strategies for research. J Couns Dev. 2004;82:387–393 [Google Scholar]