Abstract
Background
Unroofed coronary sinus (UCS) is a rare congenital cardiac anomaly in which there is complete or partial absence of the roof of the coronary sinus (CS) resulting in a communication between the right and left atria. There are four types of UCS described in the literature. While usually asymptomatic and discovered incidentally on imaging, UCS can be the source of a brain abscess or paradoxical embolism.
Case summary
A 62-year-old gentleman presented to the emergency department with sudden onset of right-sided weakness and subsequent unresponsiveness. His brain computed tomography (CT) was consistent with left-sided stroke. Transthoracic echocardiography was remarkable for a dilated CS and an agitated saline study was suggestive of an UCS. A gated cardiac CT with coronary angiography confirmed a wide communication between the CS and left atrium. Right heart catheterization did not show evidence of left to right shunt. He had no abnormal rhythm on telemetry monitoring throughout his hospital stay.
Discussion
Unroofed coronary sinus is the least prevalent form of an atrial septal defect. Unroofed coronary sinus is usually asymptomatic and is diagnosed incidentally in imaging studies, however, it should be suspected in patients with cerebral emboli or evidence of left to right shunt with unexplained arterial desaturation. Transthoracic echocardiography is the most widely used imaging modality for the diagnosis of UCS but is limited in its ability to visualize the posterior cardiac structures such as the CS and pulmonary veins. Gated cardiac CT is a great diagnostic tool for UCS.
Keywords: Unroofed coronary sinus, Coronary sinus defect, Paradoxical emboli, Atrial septal defect, Case report
Learning points
Unroofed coronary sinus (UCS), also known as coronary sinus defect, is a rare congenital cardiac anomaly that is usually asymptomatic and diagnosed incidentally on imaging.
Four types of UCS have been described—Type I is completely unroofed with persistent left superior vena cava (PLSVC). Type II is completely unroofed without PLSVC, Type III is partially unroofed in the mid-portion of the vein, and Type IV is partially unroofed in the terminal portion of the vein.
Unroofed coronary sinus can be a source for paradoxical embolism and brain abscess formation.
Introduction
A normal coronary sinus (CS) drains the cardiac veins into the right atrium. Unroofed coronary sinus (UCS), also known as CS defect, is a rare congenital cardiac anomaly in which there is complete or partial absence of the roof of the CS that communicates with the left atrium (LA). This anomalous connection is thought to be either due to dysfunctional development of the common wall between the LA and CS or subsequent dissolution of this wall. Unroofed coronary sinus was first described by Raghib et al. in 1965. The prevalence of UCS remains low accounting for <1% of atrial septal defects.1,2 Persistent left superior vena cava (PLSVC) is a commonly associated condition.3 There are four types of UCS. Type I, which is associated with PLSVC, is completely unroofed. Type II UCS is also completely unroofed, but without PLSVC. In Type III, the CS is partially unroofed in the mid-portion of the vein. Finally, in Type IV, the CS is partially unroofed in the terminal portion.4,5
Unroofed coronary sinus is usually asymptomatic and is incidentally discovered on imaging. Unroofed coronary sinus can be the source of a brain abscess or paradoxical embolism due to right-to-left shunting.5 In this article, we report a case of a massive embolic middle cerebral artery stroke who was found to have a large UCS.
Timeline
| Timeline | Events |
|---|---|
| Initial presentation |
|
| Day 1 |
|
| Day 2 |
|
| Day 3 |
|
| Day 4 |
|
| Day 4 |
|
| Day 5 |
|
Case presentation
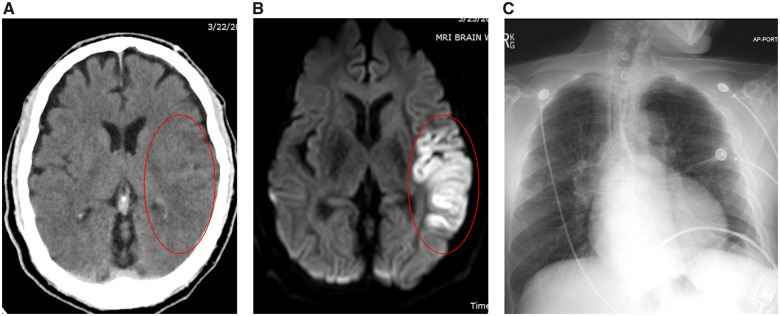
A 62-year-old gentleman with a past medical history of hypertension, hyperlipidaemia, and hepatitis C was brought into the emergency department with sudden onset right-sided weakness and subsequent unresponsiveness. An immediate brain computed tomography (CT) showed a hypodensity in the left sylvian branch of the middle cerebral artery (M2) region (Figure 1A). The patient was administered tPA and underwent urgent thrombectomy. Vital signs were notable for hypertension with a blood pressure of 188/159 mmHg and heart rate of 93 b.p.m.; respiratory rate and oxygen saturation were within normal limits. Significant findings on the physical exam included confusion, right-sided weakness, and expressive aphasia. The cardiovascular exam, specifically, revealed a regular rate and rhythm with normal heart sounds. Initial Troponin I was 0.03 ng/mL (nL <0.03 ng/mL) and later peaked at 0.04 ng/mL. His laboratory tests including complete blood count, basic metabolic panel, and liver function tests were within normal limits. Magnetic resonance imaging (MRI) of the brain confirmed the stroke (Figure 1B). The chest X-ray was unremarkable (Figure 1C). The electrocardiogram showed sinus rhythm with septal Q waves and inferolateral T-wave inversions (Figure 2).
Figure 1.
Representative brain computed tomography and magnetic resonance imaging and chest X-ray of the patient. (A) Brain computed tomography demonstrating subtle changes in the left middle cranial artery territory. (B) Brain magnetic resonance imaging demonstrating left middle cranial artery infarct. (C) Chest X-ray demonstrating clear lung fields with normal cardiac silhouette.
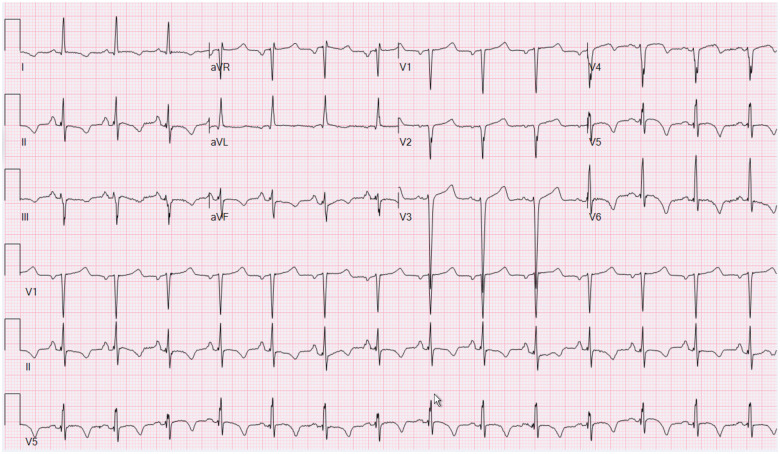
Figure 2.
Electrocardiogram demonstrating sinus rhythm with septal Q waves and inferolateral T-wave inversions.
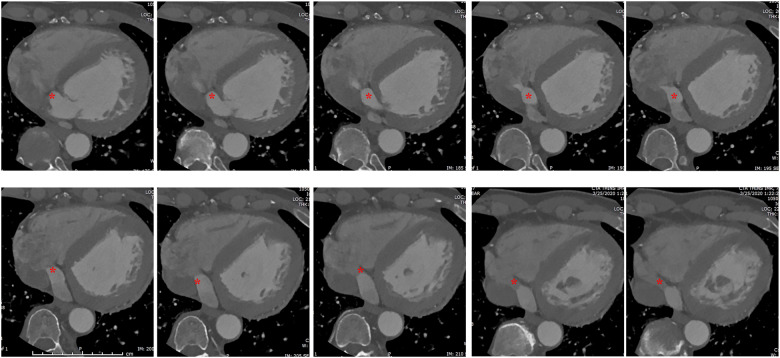
The patient was started on nicardipine drip and transferred to the neuro-intensive care unit. Head and neck CT angiogram revealed mild atherosclerosis of bilateral carotid arteries with no evidence of stenosis or dissection. Assessment of the aortic arch revealed a bovine configuration aortic arch. No arrhythmias were observed on telemetry monitoring throughout the hospitalization (total 5 days). Transthoracic echocardiography was remarkable for a dilated CS and an agitated saline study, administered via left upper extremity (to evaluate the presence of concomitant PLSVC), showed evidence of microbubbles appearing late in the LA and left ventricle (LV) suggestive of an UCS (Figure 3, Video 1). Additionally, the LV was normal in size but moderately reduced in systolic function with a left ventricular ejection fraction of 35%. There was akinesis of the distal septum and dyskinesis of the apex with moderate hypokinesis of the remaining walls. No LV or left atrial thrombus seen. Gated cardiac CT confirmed a wide communication between the CS and LA consistent with UCS (Figure 4).
Figure 3.
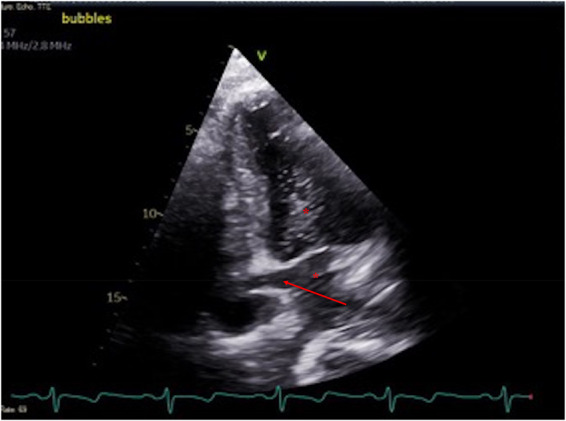
Echocardiographic image of the heart demonstrating unroofed coronary sinus (arrow) and appearance of the microbubbles in the coronary sinus, left atrium, and left ventricle (asterisk) in modified apical four-chamber view (posterior angulation).
Figure 4.
Contrast-enhanced gated cardiac computed tomography. Asterisks indicating unroofed coronary sinus.
The ostium of the defect measured by CT was >15 mm in diameter (Figure 4). In addition to its normal connection to the right atrium, the CS had a direct connection with the LA as noted by the contrast shunting from the LA into the CS and subsequently into the right atrium (Figure 4). No other congenital anomalies, including PLSVC, were identified on the CT. The LA was normal in size measuring 3.7 cm in the AP dimension. The LV was dilated with an end-diastolic dimension of 5.9 cm. Apical wall akinesis and hypokinesis of the rest of the walls were found, however, no mural thrombus was identified.
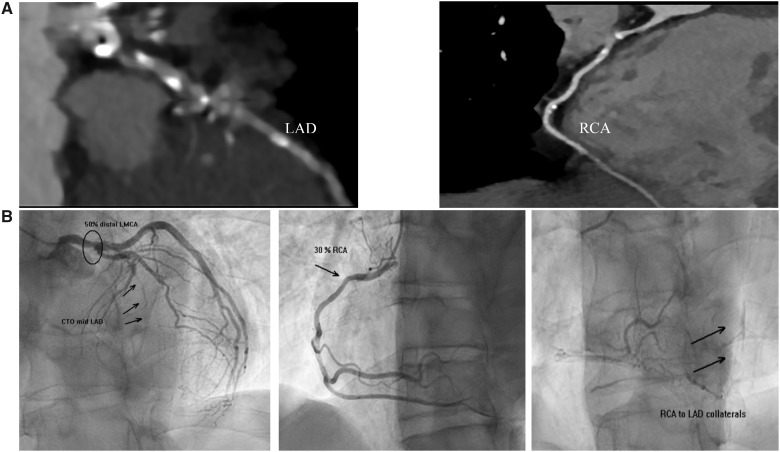
Computed tomography coronary angiography demonstrated extensive coronary plaque in the left main (LM) and in the proximal to mid left anterior descending (LAD) >70% stenosis (Figure 5A). Additionally, the proximal to mid right coronary artery (RCA) had a 50–69% stenosis. There was no evidence of pulmonary emboli. He subsequently underwent invasive coronary angiography which similarly showed a 50% distal LM lesion and a chronic total occlusion of the mid-LAD (Figure 5B). Right heart catheterization with stepwise assessment of oxygen saturation was not consistent with a significant left to right shunt. Cardiac surgery was consulted for possible closure of the UCS and coronary artery bypass. Further evaluation of surgical candidacy was deferred to allow for 6 weeks of rehabilitation. The patient was thus discharged to an acute rehabilitation facility. He had a tele visit with neurologist following discharge from rehabilitation facility and reported ambulating without difficulties but noted some trouble with his speech and confusion from time to time.
Figure 5.
Representative computed tomography coronary angiography and coronary angiogram of the patient. (A) Computed tomography coronary angiography demonstrating calcification and plaque in the left anterior descending and right coronary arteries. (B) Coronary angiography demonstrating 50% distal left main lesion, chronic total occlusion of the mid left anterior descending, and 30% right coronary artery lesion with collaterals from right coronary artery to left anterior descending. CTO, chronic total occlusion.
Discussion
Unroofed coronary sinus is usually asymptomatic and is diagnosed incidentally in imaging studies. It should be suspected in patients with cerebral emboli or evidence of left to right shunt with unexplained arterial desaturation especially when it is accompanied by PLSVC. Isolated UCS is associated with a low rate of morbidity and mortality. However, UCS and/or PLSVC may cause right ventricular failure.6
Chest X-ray findings in UCS might show increased cardiac silhouette and pulmonary vascular markings. Electrocardiogram might show evidence of sinus node dysfunction, right axis deviation, evidence of right ventricular hypertrophy, and right atrial enlargement.
Transthoracic echocardiography is the most widely used imaging modality for the diagnosis of UCS but is limited in its ability to visualize the posterior cardiac structures such as the CS and pulmonary veins. When the CS is draining into the posterior wall of the LA, this is not well delineated by transthoracic echocardiogram. In the parasternal long-axis view, it is easy to visualize the CS when it is dilated. A dilated CS should raise the suspicion of an UCS. In addition, an agitated saline study, administered via left upper extremity, showing evidence of microbubbles appearing in the LA and LV is suggestive of an UCS. If PLSVC is present, it is important to administer agitated saline via left arm as it enters directly the LA. If PLSVC is not present, administration of agitated saline via the left vs. right side does not matter and the saline can be administered via any arm as it enters first the right atrium and via the coronary ostium the LA.
Computed tomography and/or MRI is a great diagnostic tool for UCS due to its high spatial and temporal resolution. Cardiac catheterization is only needed to evaluate haemodynamics in complicated cases and is generally not necessary for the diagnosis.
Surgical closure in childhood is the recommended therapy for UCS with clinically significant left-to-right shunts associated with cardiomegaly. Medical treatment includes diuretic therapy and digoxin if there are signs and symptoms of heart failure.7
In this case, we demonstrate a rare case of wide UCS presenting with an acute embolic stroke. Given the negative workup for usual causes of stroke, it is highly suspected that this could be cardioembolic in origin due to the presence of a wide UCS.
Conclusion
Patients with UCS can present with paradoxical/cryptogenic strokes. Transthoracic echocardiogram with an agitated saline study is the most widely used study for the diagnosis of UCS. Cardiac CT is a great diagnostic tool for UCS.
Lead author biography

Dr Savalan Babapoor is currently a cardiovascular disease fellow at Einstein Medical Center. He completed internal medicine residency at Thomas Jefferson University Hospital. Prior to his residency, he completed a post-doctoral research fellowship at Johns Hopkins Hospital. His research interest is mainly focused on cardiac electrophysiology.
Supplementary material
Supplementary material is available at European Heart Journal - Case Reports online.
Supplementary Material
Acknowledgements
The authors are grateful to our colleagues, who contributed invaluable clinical information.
Slide sets: A fully edited slide set detailing this case and suitable for local presentation is available online as Supplementary data.
Consent: The authors confirm that written consent for submission and publication of this case report including image(s) and associated text has been obtained from the patient in line with COPE guidance.
Conflict of interest: none declared.
Funding: None declared.
References
- 1. Knauth A, McCarthy KP, Webb S, Ho SY, Allwork SP, Cook AC. et al. Interatrial communication through the mouth of the coronary sinus. Cardiol Young 2002;12:364–372. [DOI] [PubMed] [Google Scholar]
- 2. Raghib G, Ruttenberg HD, Anderson RC, Amplatz K, Adams JP, Edwards JE.. Termination of left superior vena cava in left atrium, atrial septal defect, and absence of coronary sinus: a developmental complex. Circulation 1965;31:906–918. [DOI] [PubMed] [Google Scholar]
- 3. Chen MC, Hung JS, Chang KC, Lo PH, Chen YC, Fu M.. Partially unroofed coronary sinus and persistent left superior vena cava: intracardiac echocardiographic observation. J Ultrasound Med 1996;15:875–879. [DOI] [PubMed] [Google Scholar]
- 4. Thangaroopan M, Truong QA, Kalra MK, Yared K, Abbara S.. Rare case of an unroofed coronary sinus: diagnosis by multidetector computed tomography. Circulation 2009;119:e518–e520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ootaki Y, Yamaguchi M, Yoshimura N, Oka S, Yoshida M, Hasegawa T.. Unroofed coronary sinus syndrome: diagnosis, classification, and surgical treatment. J Thorac Cardiovasc Surg 2003;126:1655–1656. [DOI] [PubMed] [Google Scholar]
- 6. Kühn A, Hauser M, Eicken A, Vogt M.. Right heart failure due to an unroofed coronary sinus in an adult. Int J Cardiol 2006;113:248–249. [DOI] [PubMed] [Google Scholar]
- 7. Rao PS, Harris AD.. Recent advances in managing septal defects: atrial septal defects. F1000Res 2017;6:2042. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.