Abstract
Issue addressed
Noncommunicable chronic disease underlies much of the life expectancy gap experienced by Aboriginal and Torres Strait Islander people. Modifying contributing risk factors; tobacco smoking, nutrition, alcohol consumption, physical activity, social and emotional wellbeing (SNAPS) could help close this disease gap. This scoping review identified and describes SNAPS health promotion programs implemented for Aboriginal and Torres Strait Islander people in Australia.
Methods
Databases PubMed, CINAHL, Informit (Health Collection and Indigenous Peoples Collection), Scopus, Trove and relevant websites and clearing houses were searched for eligible studies until June 2015. To meet the inclusion criteria the program had to focus on modifying one of the SNAPS risk factors and the majority of participants had to identify as being of Aboriginal and/or Torres Strait Islander heritage.
Results
The review identified 71 health promotion programs, described in 83 publications. Programs were implemented across a range of health and community settings and included all Australian states and territories, from major cities to remote communities. The SNAPS factor addressed most commonly was nutrition. Some programs included the whole community, or had multiple key audiences, whilst others focused solely on one subgroup of the population such as chronic disease patients, pregnant women or youth. Fourteen of the programs reported no outcome assessments.
Conclusions
Health promotion programs for Aboriginal and Torres Strait Islander people have not been adequately evaluated. The majority of programs focused on the development of individual skills and changing personal behaviours without addressing the other health promotion action areas, such as creating supportive environments or reorienting health care services.
So What?
This scoping review provides a summary of the health promotion programs that have been delivered in Australia for Aboriginal and Torres Strait Islander people to prevent or manage chronic disease. These programs, although many are limited in quality, should be used to inform future programs. To improve evidence‐based health promotion practice, health promotion initiatives need to be evaluated and the findings published publicly.
1. BACKGROUND
The life expectancy gap between Aboriginal and Torres Strait Islander and non‐Indigenous Australians is approximately a decade. 1 A significant contributor to the gap is the higher burden of chronic disease in Aboriginal and Torres Strait Islander communities; much of which is deemed preventable. 1 The five leading risk factors associated with noncommunicable chronic diseases are tobacco smoking, poor nutrition, alcohol consumption, physical inactivity and social and emotional wellbeing, 2 (collectively simplified by the acronym SNAPS). While there is a recognised need for urgent action to address these risk factors for Aboriginal and Torres Strait Islander peoples, 3 the financial and human resource supports required are currently inadequate. 4
Behavioural risk factors (also referred to as lifestyle risk factors) that contribute to preventable chronic disease have proven to be difficult to modify. 5 There are a variety of health promotion/ behaviour change theories such as the health belief, stages of change and trans‐theoretical models that consider the complexities of behaviour change and that offer “intervention” strategies. 6 Behaviour change theories highlight the role of social influences as well as the importance of the perceived outcomes and the influence of perceptions of control over said behaviours. 7 The ability to change is further complicated by the environment within which individuals live. Changing complex behaviours such as tobacco smoking, dietary intake, physical activity and alcohol consumption require a coordinated and concerted health promotion effort. 8 Acknowledging this complexity, the Ottawa Charter identifies five action areas for comprehensive health promotion: building healthy public policy, creating supportive environments, strengthening community action, developing personal skills and reorienting health care services towards prevention of illness and promotion of health. 9
Historical, cultural, socio‐economic and political dimensions play an important role in determining the health status of Aboriginal and Torres Strait Islander individuals, their families and the communities in which they live. The difficulty of affecting behavioural risk factors for Aboriginal and Torres Strait Islander peoples is further challenged by factors directly and indirectly linked to colonisation and past and ongoing policies of assimilation such as intergenerational stress, social disadvantage, racism, low self‐efficacy and low income. 10 Health promotion programs that are developed specifically or primarily for Aboriginal and Torres Strait Islander peoples and consider historical, cultural, socio‐economic and political dimensions could contribute to a much greater reduction in the burden of disease and thus life expectancy gap. 11
Whilst health promotion activity is a core activity of comprehensive primary health care (PHC), it often extends beyond the reach and capacity of PHC services as it by necessity includes public policy, food pricing and marketing/advertising programs. However, the role of PHC services is vital as they are best placed to influence individuals and families through knowledge exchange and motivation to change behaviours within an individual's control. They can also advocate on behalf of their communities to effect change more broadly 12 and work collaboratively with other key stakeholders. Thus, PHC services are essential contributors for the delivery of health promotion programs, particularly in Aboriginal and Torres Strait Islander communities, because of their in‐depth knowledge of their local community and the cultural and socio‐economic aspects impacting on health behaviours. 13 The National Aboriginal and Torres Strait Islander Health Plan 2013‐2023 focuses on building the health promotion capacity of Aboriginal and Torres Strait Islander health professionals in the PHC workforce as this is vital to help to ensure improved health and wellbeing in Aboriginal people. 13
Through wide consultation with the Aboriginal health sector the National Health and Medical Research Council funded Centre for Research Excellence in Aboriginal Chronic Disease Knowledge Translation and Exchange (CREATE) identified research priorities to inform practice and policy in the Aboriginal and Torres Strait Islander health sector to ultimately improve health and wellbeing. Health promotion was identified as a key topic for evidence synthesis to inform the Aboriginal Health sector. 14 The CREATE leadership group, which consisted of the chief investigators and representative from the Aboriginal and Torres Strait Islander Health sector, the majority of whom identified as Aboriginal and/or Torres Strait Islander, were actively engaged in determining the scope of this review and provided input into the interpretation of the findings and the manuscript. This scoping review aimed to identify and describe health promotion programs implemented primarily for Aboriginal and Torres Strait Islander peoples that focused on modifying the SNAPS risk factors (specifically to reduce smoking and alcohol consumption, increase physical activity and improve nutrition and social and emotional wellbeing) across a diverse range of health and community settings. The review also included programs designed to prevent or improve the management of noncommunicable disease through nonpharmaceutical means (specifically obesity, type 2 diabetes, chronic kidney disease and cardiovascular disease) among Aboriginal and Torres Strait Islander peoples. It adhered to recognised methodology for the conduct of a scoping review. 15
2. METHODS
2.1. Inclusion criteria
2.1.1. Participants
Studies were included if the participants were Aboriginal and/or Torres Strait Islander peoples living in Australia. Studies that included participants of other ethnicities living in Australia were considered if more than 50% of participants were Aboriginal and/or Torres Strait Islander peoples. Eligible studies included participants of any age or morbidity status.
2.1.2. Concept
To be included, health promotion activities and programs must have aimed to prevent or manage chronic disease by modifying one or more of the following SNAPS behavioural risk factors; tobacco smoking, nutrition, alcohol consumption or physical activity and social and emotional wellbeing. Programs also had to be delivered to individuals and/or groups by appropriately trained staff. Unlike smoking, nutrition and alcohol, a decision was made that physical activity brief intervention, or discussion about physical activity would not be included; a program had to include an actual movement activity.
Health promotion policies, such as healthy catering policies, no smoking policies, environmental policies or urban design modification were not included, nor were activities that were limited to the provision of information in the form of posters, brochures, online websites or smartphone applications if they did not include personal contact (including telehealth or video link) with appropriately trained staff supporting the health promotion activities/advice. Health promotion activities that utilised only pharmaceutical interventions, such as nicotine replacement therapy, in isolation from other interventions, such as counselling, were also excluded as were programs for the management of asthma and mental illnesses other than depression.
2.1.3. Context
Health promotion activities and programs delivered in all regions (urban, rural and remote) and any setting (PHC centres, schools, workplaces or community centres) were included with the exception of programs implemented in a live‐in facility, such as alcohol or drug rehabilitation or a facility for diagnosed mental illness, which were not included.
2.1.4. Types of studies
All qualitative, quantitative, economic and mixed methods studies were considered for inclusion. Policy papers and expert opinion were not included. Systematic reviews or literature reviews were also excluded.
3. SEARCH STRATEGY
The search strategy aimed to identify published studies indexed in commercial databases and studies only available in the grey literature. An initial search of PubMed was completed to establish and finalise search terms. A second, database‐specific search using all identified keywords and index terms modified to fit each database was then undertaken in PubMed, CINAHL, Informit (Health Collection and Indigenous Peoples Collection), Scopus and Trove databases. The search in Trove was limited to theses only as other publication types were captured in the remaining databases. The search strategies for each database can be obtained from the corresponding author. To provide a complete scope and capture all available studies no date limitation was applied. The search was completed in June 2015.
To ensure comprehensiveness of the search strategy, the following websites and clearing houses that provide information, links and resources related to Aboriginal and Torres Strait Islander health were also searched.
Australian Institute of Aboriginal and Torres Strait Islander Studies
The Lowitja Institute
Australian Government Office of Aboriginal and Torres Strait Islander Health
National Aboriginal Community Controlled Health Organisation
Australian Health and Medical Research Council of New South Wales
Victorian Aboriginal Community Controlled Health Organisation
Queensland Aboriginal and Islander Health Council
Aboriginal Health Council of South Australia
Aboriginal Health Council of Western Australia
Aboriginal Medical Services Alliance Northern Territory; and
Central Australian Aboriginal Congress.
The reference list of included manuscripts was also checked for additional eligible papers.
3.1. Study selection
Citations retrieved from database searching were downloaded into Endnote X7 software (Clarivate Analytics, USA) and titles and abstracts were screened and assessed for eligibility against the inclusion criteria (KC, EA, CT and CL). If deemed potentially eligible, full text of the articles were retrieved for detailed assessment. Determination of final eligibility was undertaken by KJC, CD and EA; any disagreements were resolved through discussion until a consensus was reached.
4. DATA EXTRACTION
Data from each study were extracted with the assistance of a data extraction tool. 15 Data extracted included; author(s), year of publication, aims/objectives, program setting, participants' inclusion criteria (age, gender, ethnicity), SNAPS risk factors addressed, a brief description of the program and the key outcomes reported. The geographical classification of the program setting was determined using the Australian Standard Geographical Classification System (ASGC), 16 which since 2011 has been the geographical framework used by the Australia Bureau of Statistics (Box 1). 17 The health promotion action areas in the publication were also captured. Where multiple publications were located for one study or program, all available data were used to complete the extracted details.
BOX 1. ASGC system remoteness area (RA) classifications.
| RA1 | Major Cities |
| RA2 | Inner Regional Australia |
| RA3 | Outer Regional Australia |
| RA4 | Remote Australia |
| RA5 | Very Remote Australia |
| RA6 | Migratory |
5. RESULTS
This scoping review located 83 published articles 18 , 19 , 20 , 21 , 22 , 23 , 24 , 25 , 26 , 27 , 28 , 29 , 30 , 31 , 32 , 33 , 34 , 35 , 36 , 37 , 38 , 39 , 40 , 41 , 42 , 43 , 44 , 45 , 46 , 47 , 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 , 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 , 89 , 90 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 98 , 99 , 100 that met our inclusion criteria from which we identified 71 unique health promotion programs (Figure 1). The extensive search of websites yielded no additional papers that met our inclusion criteria. The earliest paper that met the inclusion criteria was published in 1987, 47 with only 12 articles published before 2000. 22 , 32 , 43 , 44 , 45 , 47 , 50 , 52 , 56 , 57 , 73 , 86
Figure 1.
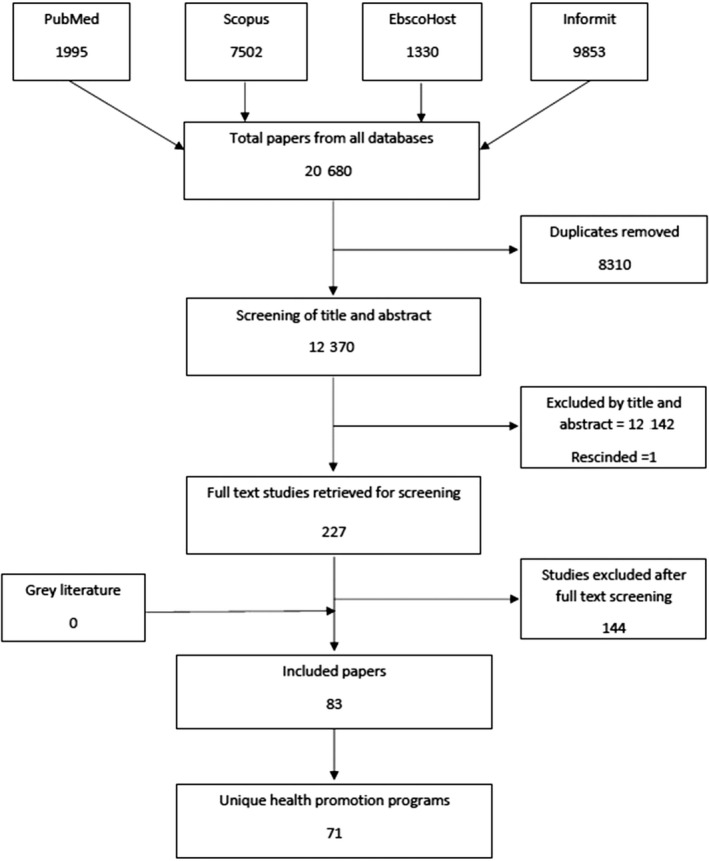
Flow diagram detailing results of literature search and study inclusion
The programs that met the inclusion criteria have been displayed across five tables (Tables 1, 2, 3, 4, 5), one for each of the SNAPS risk factors. Programs that focused on more than one of the SNAPS risk factors are displayed in all relevant tables. The tables offer some basic information about the programs including the name of the program (if applicable), the reference(s) associated with the program, the setting in which the program was run, including, where possible, the geographical classification of the location, a description of the participants included in the program, the SNAPS risk factor(s) that were of focus, an indication if an outcome was assessed and reported and a brief description of the program.
Table 1.
Smoking – Programs that included a tobacco smoking prevention and/or cessation component
|
Program name or publication title References |
Setting | Participants | S | N | A | P | So | Outcomes assessed? | Program brief |
|---|---|---|---|---|---|---|---|---|---|
|
“Smokin' No Way”, “SmokeCheck”, “Smoke Rings” Programs 26 (Campbell, Bohanna et al 2014) |
RA 4 and 5 – QLD Community, PHC and School Settings |
Aboriginal and Torres Strait Islander Community members, school children and smokers trying to quit. | ✓ | ✓ | A multilayered intervention: event support program, training for health workers, group support program for individuals trying to quit, lesson plans for teachers and school staff, policy guide for organisations to address smoking and monitoring of compliance with legislation on tobacco sales. | ||||
|
An intensive smoking cessation intervention for pregnant Aboriginal and Torres Strait Islander females on smoking rates at 36 wks' gestation 40 (Eades, Sanson‐Fisher et al 2012) |
RA 1– QLD and WA PHC Setting |
Pregnant females, aged 16 y and older, who were current smokers or recent quitters. | ✓ | ✓ | Pregnant females were assisted by their GP's to quit through a number of techniques including engaging their partner. Nicotine replacement therapy was offered after two failed quit attempts. | ||||
|
“Be Smoke Free” 50 (Gamarania, Malpraburr et al 1998) |
RA 5 – NT Community and School Settings |
Primary and high School children in remote NT communities (non‐Indigenous students were excluded from the analysis). | ✓ | ✓ | A 2‐wk educational smoking intervention involving pre‐ and postintervention questionnaires about current practices and knowledge and attitudes to smoking. | ||||
|
Multicomponent, community‐based tobacco interventions in remote Aboriginal communities 55 (Ivers, Castro et al 2006) |
RA 5 – NT Community and School Settings |
Community members and school children | ✓ | ✓ | There were a number of components to this program including health promotion activities, community and school tobacco education session and community events. | ||||
|
The Koori Tobacco Cessation Project 63 (Mark, McLeod et al 2004) |
RA 1 and 2 – NSW Community Setting |
Aboriginal and Torres Strait Islanders who smoke | ✓ | ✓ | A combination of smoking cessation group sessions and a subsidised course of nicotine replacement therapy. | ||||
|
Be Our Ally Beat Smoking Program 64 , 65 , 66 (Marley, Atkinson et al 2012, Marley, Atkinson et al 2014, Marley, Kitaura et al 2014) |
RA 4 and 5 – WA Community and PHC Settings |
Aboriginal or Torres Strait Islander current smokers 16 y+ who wish to quit or cut down or who have quit within 2 wks of enrolling | ✓ | ✓ | Tailored smoking cessation counselling during face‐to‐face visits which were held weekly for the first four weeks, monthly to 6 mo and two monthly to 12 mo. | ||||
|
Adult health checks for Indigenous Australians: the first years' experience from the Inala Indigenous Health Service 89 (Spurling, Hayman et al 2009) |
RA 1 – QLD PHC Setting |
Aboriginal and Torres Strait Islander Adults | ✓ | ✓ | Health checks undertaken in conjunction with lifestyle and health advice. About 95% of current smokers received brief smoking cessation advice and 67% received “lifestyle” advice. | ||||
|
Healthy Food Awareness Program 107 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW PHC Setting |
Individuals with Chronic Disease | ✓ | ✓ | ✓ | A one day a week session focused on diet and exercise and other health‐related issues, including smoking at the AMS and at the AMS's outreach clinics. | |||
|
Healthy Lifestyles Project 30 (Cargo, Marks et al 2011) |
RA 5 – NT Community and PHC Settings |
Aboriginal Community in North East Arnhem Land | ✓ | ✓ | ✓ | ✓ | Community health screening, feedback and discussion. Coordinated community‐directed approach to increase the allocation of community resources to prevention activities. Multiple intervention strategies implemented; family food garden, community market, new school canteen and a 4‐day healthy lifestyle festival. | ||
|
“Step up to health” –Tasmanian Aboriginal Centre (TAC) Rehabilitation Program 35 (Davey, Moore et al 2014) |
RA 2 – TAS PHC Setting, Private Physiotherapy Practice and outdoors |
Adult Aboriginal people diagnosed with COPD, IHD, or CHF and people with at least two risk factors for developing CVD | ✓ | ✓ | ✓ | ✓ | ✓ | Two 1‐h supervised exercise sessions and one, 1‐h educational session per week for 8 wks. Sessions promoted self‐management approaches, cardiovascular and respiratory health, benefits of exercise, shopping, cooking and eating healthy food, medication, stress and psychological wellbeing, and smoking cessation. | |
|
Heart Health – For Our People By Our People 37 , 38 (Dimer, Jones et al 2010, Dimer, Dowling et al 2013) |
RA 1 – WA PHC Setting |
Patients with CVD or at high risk of CVD | ✓ | ✓ | ✓ | ✓ | A cardiovascular disease (CVD) management program involving assessment and reassessment, provision of health information and an individualised program including motivational and education sessions; diet and nutrition; risk factor modification (including smoking cessation); managing stress and emotion (with referral for counselling when indicated); benefits of physical activity; diabetes management and medication usage. | ||
|
Strong Women, Strong Babies, Strong Culture Program 36 , 44 , 45 , 60 (d'Espaignet, Measey et al 2003, Fejo 1994, Fejo and Rae 1996, Mackerras 2001) |
Multiple communities – NT Community and PHC Settings |
Pregnant Women | ✓ | ✓ | ✓ | ✓ | ✓ | Women within Aboriginal communities help other Aboriginal women prepare for pregnancy by working together with nutritionists, community‐based health workers, local schools and other women in the community. | |
|
Waminda's Wellbeing Program 46 (Firth, Crook et al 2012) |
RA 2 – NSW Community Setting |
Predominately Aboriginal and Torres Strait Islander women, including non‐Indigenous women | ✓ | ✓ | ✓ | ✓ | ✓ | Pilot program that evolved into intensive programs. Multiple components: exercise sessions; community gardens; cooking healthy meals; smoking cessation; health and wellbeing camps. | |
|
Karalundi Peer Support and Skills Training Program 52 (Gray, Sputore et al 1998) |
RA 5 – WA School Setting |
Primary, high school and TAFE students aged 10‐20 y. | ✓ | ✓ | ✓ | ✓ | Ten programs aimed at: developing students' interpersonal, problem solving and decision‐making skills; quit smoking; drug; alcohol and petrol sniffing education; sex education, arts and crafts, general health promotion; eye, ear and nose care and the use of natural medicines. | ||
|
National Fetal Alcohol Spectrum Disorder Prevention Strategy –‐ Reducing Alcohol and Tobacco Consumption in Pregnancy 53 (Hayward, Scrine et al 2008) |
RA 1 – QLD Community and PHC Settings |
Pregnant women | ✓ | ✓ | ✓ | Community to inform about the dangers of Foetal Alcohol Syndrome. The program also included a resource kit for health to integrate brief interventions for smoking and alcohol use into their clinical practice. | |||
|
Malabar Community Midwifery Link Service 54 (Homer, Foureur et al 2012) |
RA 1 – NSW PHC Setting |
Pregnant Aboriginal and/or Torres Strait Islander women and non‐Indigenous women having an Aboriginal and/or Torres Strait Islander baby | ✓ | ✓ | ✓ | ✓ | A unique model of antenatal care that addresses stress, smoking and alcohol consumption in pregnancy along with other care. | ||
|
Deadly Choices Program 61 , 62 (Malseed, Nelson et al 2014, Malseed, Nelson et al 2014) |
RA 1 – QLD School Setting |
High school students Grade 7‐12 | ✓ | ✓ | ✓ | ✓ | ✓ | Seven‐week physical activity and education program. Education components included leadership, chronic disease, physical activity, nutrition, smoking, harmful substances and health services. Health checks were also facilitated. | |
|
Getting Better at Chronic Care 70 (McDermott, Schmidt et al 2015) |
RA 5–‐ QLD PHC Setting |
Clients with diabetes and one major comorbidity, aged 18 y or more, poor glycaemic control and receiving regular care from the identified health service | ✓ | ✓ | ✓ | A self‐management program supporting patients in making and keeping appointments, understanding medications and nutrition and the effects of smoking. | |||
|
The Chronic Disease Self‐Management Project 75 (Mobbs, Nguyen et al 2003) |
RA5 –‐ NT Community and PHC Settings |
Patients previously diagnosed with diabetes and/or hypertension with or without renal involvement | ✓ | ✓ | ✓ | ✓ | ✓ | Self‐care program to develop skills including changing behaviour; smoking, nutrition, physical activity and weight loss. Building family and community healthy lifestyle infrastructure using community empowerment framework. Production of local resources (booklets and videos) including HP messages. Establishment of women's healthy weight groups, walking groups and tobacco action initiative. | |
|
The Looma Diabetes Program and Looma Healthy Lifestyle Project 33 , 84 (Clapham, O’Dea et al 2007, Rowley, Daniel et al 2000) |
RA5–‐ WA Community Setting |
Initially Aboriginal people with diabetes or at high risk, progressing to the whole community | ✓ | ✓ | ✓ | ✓ | Following community wide diabetes screening, multiple strategies were implemented progressively over several years starting with a nutrition and exercise program for diabetes and high‐risk patients progressing to range of community wide initiatives. | ||
|
Wadja Warriors Healthy Weight Program and the Injury Protection Project 88 (Smith 2002) |
RA 4 – QLD Community Setting |
Men from the local football team and other interested men in community | ✓ | ✓ | ✓ | ✓ | ✓ | Injury Prevention Project to reduce on and off field violence including family violence and alcohol and drug use to reduce a major cause of injury: broken glass. Program developed to include a lifestyle program promoting good nutrition and physical activity and teaching skills that are required for making healthy changes. | |
|
WuChopperen Drug Alcohol and Other Substances program 0101 (Strempel and Drugs 2004) |
RA 1‐3 – QLD Community and PHC Settings |
Aboriginal and Torres Strait Islander youth | ✓ | ✓ | ✓ | ✓ | Provides counselling and support for young people in areas of physical, social and emotional health, and coordinates and delivers alcohol and other drug education to staff and health facilitators. | ||
|
The COACH (Coaching patients On Achieving Cardiovascular Health) program (TCP) 87 , 98 , 99 (Ski, Vale et al 2015, Vale, Jelinek et al 2003, Vale, Jelinek et al 2002.) |
Multiple RA zones QLD Telephone and postal |
Patients with Chronic Disease (CD) or at high risk of CD | ✓ | ✓ | ✓ | ✓ | A standardised coaching program delivered by registered nurses targeting CD patients and those at risk of CD, delivered by telephone and mail‐out. Coaches educate, advise and encourage patients to close the “treatment gaps” and achieve guideline‐recommended risk factor targets whilst working with their usual doctor(s). |
Abbreviations: A, alcohol; AMS, Aboriginal Medical Service; CD, chronic disease; CHF, chronic heart failure; COPD, chronic obstructive heart failure; CVD, cardiovascular disease; GP, General Practitioner; HP, health promotion; IHD ischaemic heart disease; N, nutrition; NSW, New South Wales; NT, Northern Territory; P, physical activity; PHC, Primary Health Care; QLD, Queensland; RA, remote area; S, smoking; So, social and emotional wellbeing; TAFE, Technical and Further Education; TAS, Tasmania; WA, Western Australia.
Table 2.
Nutrition – Programs that included a nutrition component
|
Program name or publication title References |
Setting | Participants | S | N | A | P | So | Outcomes assessed? | Program brief |
|---|---|---|---|---|---|---|---|---|---|
|
Diabetes Cooking Course 18 (Abbott, Davison et al 2012) |
RA 1–‐ NSW PHC Setting |
Adult Aboriginal Australians | ✓ | ✓ | Eighteen weekly cooking classes of 4 h duration to promote healthy eating on a budget. | ||||
|
Healthy Lifestyle and Weight Management Program 0105 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 1–‐ NSW PHC Setting |
Aboriginal clients of Awabakal AMS, with a focus on overweight clients or those suffering hypertension | ✓ | ✓ | Nutrition education activities and health screenings over a 6‐wk period to improve nutrition knowledge and food choice. | ||||
|
Fruit and Vegetable Program and Market Garden 0108 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW School Setting |
School students and health centre clients on Centrelink benefits who agree to regular health checks |
✓ | Market garden built in the school which provided fresh fruit and vegetables to students. Students also learnt about gardening and preparing healthy meals. Garden also provided subsidised fruit and vegetable boxes for eligible clients of the health service. | |||||
|
Community Kitchens 110 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 3 – NSW Setting not identified |
Aboriginal women | ✓ | Nutrition education program. One 3‐h sessions held every week for 3 mo. | |||||
|
Community Kitchen 0106 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 1 – NSW PHC Settings |
Community members | ✓ | Weekly 3‐h sessions held at AMS including nutrition education and food preparation skills. Participants plan meals, cook and share the food they have prepared. Facilitated by a Community Nutritionist and Health Promotion Officer. | |||||
|
Need for Feed Program 21 (Aliakbari, Latimore et al 2013) |
RA 4 and 5 – Qld PHC and School Settings |
Aboriginal and Torres Strait Islander adolescents | ✓ | ✓ | Hands on, innovative cooking and nutrition program for adolescents. Including 20 h of tuition focusing on knife skills, nutrition, label reading, food budgeting and meal planning | ||||
|
Flinders Model of Self‐Management Support 23 (Battersby, Ah Kit et al 2008) |
RA 4 and 5 ‐ SA Community and PHC Settings |
Aboriginal people with type 2 diabetes aged 40 y+ | ✓ | ✓ | Aboriginal patients with diabetes interviewed by Aboriginal Health Workers to develop care plans. General practitioner and other current care providers are also involved in providing self‐management education and identifying goals in relation to weight, nutrition and exercise. | ||||
|
The Fruit and Vegetable Subsidy Program 24 , 25 (Black, Vally et al 2013, Black, Vally et al 2014) |
RA 2 and 3 ‐ NSW Community Setting |
Aboriginal children and their families | ✓ | ✓ | The provision of heavily subsidised fruit and vegetable boxes to children and their families. These boxes were accompanied by nutrition and dietary education sessions provided by dietitians or trained nutrition health workers. | ||||
|
The Healthy Lifestyle Programme (HELP) 31 (Chan, Ware et al 2007) |
RA 1 and 4 – QLD Community Setting |
Adult Aboriginal and/or Torres Strait Islander people over 20 y of age with either type 2 diabetes and/or overweight | ✓ | ✓ | Series of educational workshops on nutrition and exercise. Participants were encouraged to self‐monitor their physical activity through the use of pedometers. Participants with type 2 diabetes were also encouraged to monitor fasting plasma glucose. | ||||
|
Nutrition: at the heart of good health 0102 (Fitzpatrick and Australians for Native Title Reconciliation 2007) |
RA 5 – WA Community Setting |
Aboriginal children and their mothers | ✓ | Drop‐in centre providing healthy meals and nutrition education. Cooking classes and nutrition education for women. | |||||
|
Good food, great kids: An Indigenous Community Nutrition Project 0103 (Fitzpatrick and Australians for Native Title Reconciliation 2007) |
RA 2 –‐ VIC Community and School Setting |
Aboriginal community members, in particular school children and women | ✓ | Multiple components including school gardens, healthy food policies in school and school cooking program. Nutrition and cooking program for women and a community garden. | |||||
|
Pathways to Prevention Project – Practical Cooking Workshops 49 (Foley 2010) |
RA 1 – QLD Community Setting |
Aboriginal and Torres Strait Islander adults | ✓ | ✓ | A series of practical cooking workshops. | ||||
|
Walk‐about Together Program 59 (Longstreet, Heath et al 2008) |
RA 3 –‐ QLD Community and PHC Setting |
Overweight Aboriginal and Torres Strait Islander adults | ✓ | ✓ | Participants received nutrition and physical activity advice and were provided a pedometer and log book. | ||||
|
Cooking Classes for Diabetes 76 , 104 (Moore, Webb et al 2006, Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 1 – NSW Community and PHC Settings |
Clients with diabetes and their families | ✓ | ✓ | Cooking classes for people with diabetes and their families including health education. | ||||
|
The Bindjareb Yorgas Health Programme 78 (Nilson, Kearing‐Salmon et al 2015) |
RA 2 – WA Community Setting |
Aboriginal Women | ✓ | ✓ | The program consisting of four health promotion components, this paper is only reporting on the cooking and nutrition classes which were run weekly during school term over a 12‐mo period. | ||||
|
Minjilang Good Food and Health Project 56 , 57 (Lee, Bailey et al 1994, Lee, Bonson et al 1995) |
RA 5 – NT Community and PHC Settings |
Aboriginal community members | ✓ | ✓ | Community health screening, regular dietary intake monitoring and nutrition education including promotion of healthy foods in stores. | ||||
|
Outreach School Garden Project 100 (Viola 2006) |
RA 5 – QLD School Setting |
Aboriginal and Torres Strait Islander Students | ✓ | ✓ | This program incorporated formal nutrition and gardening education lessons into the core school curriculum through key learning areas. Healthy changes to the tuckshop menu were also made. | ||||
|
Spring into Shape Program 0109 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW PHC Setting |
Not specified | ✓ | ✓ | ✓ | Exercise and nutrition program to promote healthy lifestyle change and manage stress in a better way. Wide range of physical activities occur with nutrition education sessions. Fruit and vegetable box provided for the cost of $5 including recipes. | |||
|
Healthy Lifestyle Program 111 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 3 – NSW Community and PHC Settings |
Aboriginal adults | ✓ | ✓ | Weekly meeting with a weigh‐in and talks on topics such as healthy eating, physical activity and meal preparation. Program also includes exercise sessions and a 30‐min group walk. Sessions supported by Weight Watchers. | ||||
|
Building Healthy Communities Project 112 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 4 – NSW PHC Setting |
Aboriginal community members including children | ✓ | ✓ | ✓ |
Multiple components. Nutrition and cooking classes through “Quick Meals for Kooris” program. Community vegetable garden was established, the walking track was upgraded and a range of physical activity sessions. Women's self‐ esteem classes, craft and jewellery making classes were also part of the project. |
|||
|
Healthy Food Awareness Program 107 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW PHC Setting |
Individuals with Chronic Disease | ✓ | ✓ | ✓ | A one day a week session focused on diet and exercise and other health‐related issues, including smoking at the AMS and at the AMS's outreach clinics. | |||
|
The Chronic Disease Self‐Management pilot study 20 (Ah Kit, Prideaux et al 2003) |
RA 4 and 5 – SA Community and PHC Settings |
Aboriginal people with type 2 diabetes. | ✓ | ✓ | ✓ | A chronic disease self‐management model for Aboriginal people consisting of local support coordination, extension of preventive health programs, self‐management processes and tools to suit goal setting and behaviour change including group exercise and diet education sessions and appropriate staff training. | |||
|
Aboriginal and Torres Strait Islander Women's Fitness Program 27 , 28 , 29 (Canuto, McDermott et al 2011, Canuto, Cargo et al 2012, Canuto, Spagnoletti et al 2013) |
RA 1 – SA Community Setting |
Aboriginal and Torres Strait Islander Women 18‐64 y with waist circumference greater than 80cm | ✓ | ✓ | ✓ | Twelve‐week program including two 60‐min group exercise classes per week, and four nutrition education workshops. RCT vs waitlisted controls. | |||
|
Healthy Lifestyles Project 30 (Cargo, Marks et al 2011) |
RA 5 – NT Community and PHC Settings |
Community members | ✓ | ✓ | ✓ | ✓ | Community health screening, feedback and discussion. Coordinated community‐directed approach to increase the allocation of community resources to prevention activities. Multiple intervention strategies implemented; family food garden, community market, new school canteen and a 4‐day healthy lifestyle festival. | ||
|
Aunty Jean's Good Health Program 34 (Curtis, Service et al 2004) |
RA 3 – NSW Community and PHC Settings |
Aboriginal Elders | ✓ | ✓ | ✓ | Twelve‐week program involving weekly group sessions that included a medical check, group exercise and information sharing from health professionals across multiple topics (nutrition and cooking, exercise, diabetes and stress management). This was combined with a self‐managed, self‐directed home program. | |||
|
“Step up to health” ‐Tasmanian Aboriginal Centre (TAC) Rehabilitation Program 35 (Davey, Moore et al 2014) |
RA 2 –TAS PHC Setting, Private Physiotherapy Practice and outdoors |
Adult Aboriginal people diagnosed with COPD, IHD or CHF and people with at least two risk factors for developing CVD | ✓ | ✓ | ✓ | ✓ | ✓ | Two 1‐h supervised exercise sessions and one, 1‐h educational session per week for 8 wks. Sessions promoted self‐management approaches, cardiovascular and respiratory health, benefits of exercise, shopping, cooking and eating healthy food, medication, stress and psychological wellbeing and smoking cessation. | |
|
Heart Health – For Our People By Our People 37 , 38 (Dimer, Jones et al 2010, Dimer, Dowling et al 2013) |
RA 1 – WA PHC Setting |
Patients with CVD or at high risk of CVD | ✓ | ✓ | ✓ | ✓ | A cardiovascular disease (CVD) management program involving assessment and reassessment, provision of health information and an individualised program including motivational and education sessions; diet and nutrition; risk factor modification (including smoking cessation); managing stress and emotion (with referral for counselling when indicated); benefits of physical activity; diabetes management and medication usage. | ||
|
Birth to Elders Nutrition Program 41 , 42 (Edwards 2004, Edwards 2005) |
RA 3 and 5 – SA Community, Child Care Centres, PHC and School Settings |
Aboriginal community members | ✓ | ✓ | ✓ | ✓ | Multiple community‐based social and emotional wellbeing activities, providing health paraphernalia to communities, including nutritional education and physical health interventions such as indoor little athletics and sports events. | ||
|
Gut Busters 43 (Egger, Fisher et al 1999) |
RA 5 –‐ QLD Community Setting |
Aboriginal and Torres Strait Islander men | ✓ | ✓ | ✓ | ✓ | Program run on four remote islands targeting four major lifestyle risk factors; reducing fat intake; increasing dietary fibre; increasing daily movement and changing “obesogenic” habits. The program encourages long‐term lifestyle changes including moderate use of alcohol and moderate‐intensity accumulated activity. Regular planned walking groups occurred on two islands. | ||
|
Strong Women, Strong Babies, Strong Culture Program 36 , 44 , 45 , 60 (d'Espaignet, Measey et al 2003, Fejo 1994, Fejo and Rae 1996, Mackerras 2001) |
Multiple communities – NT Community and PHC Settings |
Pregnant Women | ✓ | ✓ | ✓ | ✓ | ✓ | Women within Aboriginal communities help other Aboriginal women prepare for pregnancy by working together with nutritionists, community‐based health workers, local schools and other women in the community. | |
|
Waminda's Wellbeing Program 46 (Firth, Crook et al 2012) |
RA 2 – NSW Community Setting |
Predominately Aboriginal and Torres Strait Islander women, including non‐Indigenous women | ✓ | ✓ | ✓ | ✓ | ✓ | Pilot program that evolved into intensive programs. Multiple components: exercise sessions; community gardens; cooking healthy meals; smoking cessation; health and wellbeing camps. | |
|
Diabetes Management and Care Program 51 (Gracey, Bridge et al 2006) |
RA 5 – WA Community and PHC Settings |
Aboriginal community members | ✓ | ✓ | ✓ | Multiple strategies including lifestyle disease education, promotion of healthy eating, exercise and active recreation program, health screening and medication compliance. | |||
|
Deadly Choices Program 61 , 62 (Malseed, Nelson et al 2014, Malseed, Nelson et al 2014) |
RA 1 – QLD School Setting |
High school students Grade 7‐12 | ✓ | ✓ | ✓ | ✓ | ✓ | Seven‐week physical activity and education program. Education components included leadership, chronic disease, physical activity, nutrition, smoking, harmful substances and health services. Health checks were also facilitated. | |
|
Getting Better at Chronic Care 70 (McDermott, Schmidt et al 2015) |
RA 5 – QLD PHC Setting |
Clients with diabetes and one major comorbidity, aged 18 y or more, poor glyacemic control and receiving regular care from the identified health service | ✓ | ✓ | ✓ | A self‐management program supporting patients in making and keeping appointments, understanding medications and nutrition and the effects of smoking. | |||
|
The Chronic Disease Self‐Management Project 75 (Mobbs, Nguyen and Bell 2003) |
RA5 – NT Community and PHC Settings |
Patients previously diagnosed with diabetes and/or hypertension with or without renal involvement | ✓ | ✓ | ✓ | ✓ | ✓ | Self‐care program to develop skills including changing behaviour; smoking, nutrition, physical activity and weight loss. Building family and community healthy lifestyle infrastructure using community empowerment framework. Production of local resources (booklets and videos) including HP messages. Establishment of women's healthy weight groups, walking groups and tobacco action initiative. | |
|
Awareness and Self‐Management Programme 81 (Payne 2013) |
RA 3 – QLD Community Setting |
Women with type 2 diabetes or identified has having an elevated risk of developing disease. | ✓ | ✓ | ✓ | Support groups involving information sessions on self‐management strategies; grief and loss; health ownership and concepts of shared knowledge; and diet and exercise. | |||
|
A pilot study of Aboriginal health promotion from an ecological perspective 82 , 83 (Reilly, Doyle et al 2007, Reilly, Cincotta et al 2011) |
RA 2 – VIC Community Setting |
Multiple subgroups; Elders, women, junior footballers, employees, sporting club members | ✓ | ✓ | ✓ | Multiple programs including; a health “summer school” for health promotion practitioners; a nutrition program for under 17‐year‐old footballers; initiatives to improve the dietary quality of food supplied at the football and netball club; a series of focus groups to adapt mainstream nutrition guidelines for the Indigenous community; a weekly self‐directed health‐focused meeting for women; and a workplace exercise program. | |||
|
The Looma Diabetes Program and Looma Healthy Lifestyle Project 33 , 84 (Clapham, O'Dea et al 2007, Rowley, Daniel et al 2000) |
RA5 – WA Community Setting |
Initially Aboriginal people with diabetes or at high risk, progressing to the whole community | ✓ | ✓ | ✓ | ✓ | Following community wide diabetes screening, multiple strategies were implemented progressively over several years starting with a nutrition and exercise program for diabetes and high‐risk patients progressing to range of community wide initiatives. | ||
|
Wadja Warriors Healthy Weight Program and the Injury Protection Project 88 (Smith 2002) |
RA 4 – QLD Community Setting |
Men from the local football team and other interested men in community | ✓ | ✓ | ✓ | ✓ | ✓ | Injury Prevention Project to reduce on‐ and off‐field violence including family violence and alcohol and drug use to reduce a major cause of injury: broken glass. Program developed to include a lifestyle program promoting good nutrition and physical activity and teaching skills that are required for making healthy changes. | |
|
The COACH (Coaching patients On Achieving Cardiovascular Health) program (TCP) 87 , 98 , 99 (Ski, Vale et al 2015, Vale, Jelinek et al 2003, Vale, Jelinek et al 2002.) |
Multiple RA zones QLD Telephone and postal |
Patients with Chronic Disease (CD) or at high risk of CD | ✓ | ✓ | ✓ | ✓ | A standardised coaching program delivered by registered nurses targeting CD patients and those at risk of CD, delivered by telephone and mail‐out. Coaches educate, advise and encourage patients to close the “treatment gaps” and achieve guideline‐recommended risk factor targets whilst working with their usual doctor(s). |
Abbreviations: A, alcohol; AMS, Aboriginal Medical Service; CD, chronic disease; CVD, cardiovascular disease; N, nutrition; NSW, New South Wales; NT, Northern Territory; P, physical activity; PHC, Primary Health Care; QLD, Queensland; RA, remote area; RCT, Randomised Controlled Trial; S, smoking; SA, South Australia; So, social and emotional wellbeing; VIC, Victoria; WA, Western Australia.
Table 3.
Alcohol – Programs that included an alcohol prevention and/or management component
|
Program name or publication title References |
Setting | Participants | S | N | A | P | So | Outcomes assessed? | Program brief |
|---|---|---|---|---|---|---|---|---|---|
|
An Alcohol Prevention Program for Aboriginal Children 22 (Barber, Walsh et al 1988) |
RA4 – Qld School Setting |
Year 7 school children | ✓ | ✓ | Community developed lesson plans which were delivered by school teachers. The program was divided in to eight lessons that focused on the misuse of alcohol and promoting healthy choices and behaviours. | ||||
|
Community Approach to Drug Abuse Prevention 47 (Fisher and van der Heide 1987) |
Community Setting | Young Aboriginal people at risk of alcohol abuse | ✓ | Aboriginal workers are assisted to develop programs specifically tailored to their communities. Activities include teaching community members about teamwork, health promotion, community development and planning for action. | |||||
|
Aboriginal Women's Group 58 (Lee, Dawson and Conigrave 2013) |
RA1 – NSW PHC and Outpatient Hospital Settings |
Aboriginal female clients of an outpatient alcohol and drug treatment service | ✓ | ✓ | A group of women who attended a drug and alcohol clinic met up to discuss support and develop personal skills. | ||||
|
Central Australian Aboriginal Alcohol Programs Unit – Grog Action Plan 73 (Miller 1995) |
Multiple RA Zones – NT Community and School Settings |
Aboriginal and Torres Strait Islander people | ✓ | ✓ | Primary, secondary and tertiary prevention and treatment programs including school‐based education programs, Men's and Women's day care program, outreach awareness programs, men's, women's and children's evening program. Local communities are also encouraged to develop their own Grog Action Plans. | ||||
|
When You Think About It 86 (Sheehan, Schonfeld et al 1995) |
RA3 – Qld School Setting |
Aboriginal High School Students | ✓ | ✓ | Educating students on what constituted responsible drinking in order to reduce drinking driving by Queensland high school students. The program consisted of six lessons accompanied by handbook guided classes with teachers. | ||||
|
The Waringarri Project 32 (Chisholm 1989) |
RA4 – WA Community and School setting |
Aboriginal community members | ✓ | ✓ | Trained staff implemented psycho‐social method of targeting individuals in crisis and using community development strategies to overcome the crisis, also established self‐help groups and introducing alcohol concepts into schools | ||||
|
Gut Busters 43 (Egger, Fisher et al 1999) |
RA5 – QLD Community Setting |
Aboriginal and Torres Strait Islander men | ✓ | ✓ | ✓ | ✓ | Program run on four remote islands targeting four major lifestyle risk factors; reducing fat intake; increasing dietary fibre; increasing daily movement and changing “obesogenic” habits. The program encourages long‐term lifestyle changes including moderate use of alcohol and moderate‐intensity accumulated activity. Regular planned walking groups occurred on two islands. | ||
|
Strong Women, Strong Babies, Strong Culture Program 36 , 44 , 45 , 60 (d'Espaignet, Measey et al 2003, Fejo 1994, Fejo and Rae 1996, Mackerras 2001) |
Multiple communities ‐–NT Community and PHC Settings |
Pregnant Women | ✓ | ✓ | ✓ | ✓ | ✓ | Women within Aboriginal communities help other Aboriginal women prepare for pregnancy by working together with nutritionists, community‐based health workers, local schools and other women in the community. | |
|
Karalundi Peer Support and Skills Training Program 52 (Gray, Sputore et al 1998) |
RA5 – WA School Setting |
Primary, high school and TAFE students aged 10‐20 y | ✓ | ✓ | ✓ | ✓ | Ten programs aimed at: developing students' interpersonal, problem‐solving and decision‐making skills; quit smoking; drug; alcohol and petrol sniffing education; sex education, arts and crafts, general health promotion; eye, ear and nose care and the use of natural medicines. | ||
|
National Fetal Alcohol Spectrum Disorder Prevention Strategy ‐ Reducing Alcohol and Tobacco Consumption in Pregnancy 53 (Hayward, Scrine et al 2008) |
RA1 – QLD Community and PHC Settings |
Pregnant women | ✓ | ✓ | ✓ | Community to inform about the dangers of Foetal Alcohol Syndrome. The program also included a resource kit for health to integrate brief interventions for smoking and alcohol use into their clinical practice. | |||
|
Malabar Community Midwifery Link Service 54 (Homer, Foureur et al 2012) |
RA 1 – NSW PHC Setting |
Pregnant Aboriginal and/or Torres Strait Islander women and non‐Indigenous women having an Aboriginal and/or Torres Strait Islander baby | ✓ | ✓ | ✓ | ✓ | A unique model of antenatal care that addresses stress, smoking and alcohol consumption in pregnancy along with other care. | ||
|
Deadly Choices Program 61 , 62 (Malseed, Nelson et al 2014, Malseed, Nelson et al 2014) |
RA 1 – QLD School Setting |
High school students Grade 7‐12 | ✓ | ✓ | ✓ | ✓ | ✓ | Seven‐week physical activity and education program. Education components included leadership, chronic disease, physical activity, nutrition, smoking, harmful substances and health services. Health checks were also facilitated. | |
|
Watharoung Koori Youth Prevention Programs 74 (Milward 2009) |
RA1 – Vic Community Setting |
Aboriginal Youth | ✓ | ✓ | ✓ | A variety of programs in partnership with other organisations to prevention the use of alcohol and other drugs. The programs are designed to empower youth, strengthen individual Koori identity and learn more about their culture through camps, surfing competitions and an AFL football program. | |||
|
Wadja Warriors Healthy Weight Program and the Injury Protection Project 88 (Smith 2002) |
RA 4 – QLD Community Setting |
Men from the local football team and other interested men in community | ✓ | ✓ | ✓ | ✓ | ✓ | Injury Prevention Project to reduce on‐ and off‐field violence including family violence and alcohol and drug use to reduce a major cause of injury: broken glass. Program developed to include a lifestyle program promoting good nutrition and physical activity and teaching skills that are required for making healthy changes. | |
|
WuChopperen Drug Alcohol and Other Substances program 90 (Strempel and Australian National Council on Drugs 2004) |
RA 1‐3 – QLD Community and PHC Settings |
Aboriginal and Torres Strait Islander youth | ✓ | ✓ | ✓ | ✓ | Provides counselling and support for young people in areas of physical, social and emotional health, and coordinates and delivers alcohol and other drug education to staff and health facilitators. | ||
|
The COACH (Coaching patients On Achieving Cardiovascular Health) program (TCP) 87 , 98 , 99 (Ski, Vale et al 2015, Vale, Jelinek et al 2003, Vale, Jelinek et al 2002.) |
Multiple RA zones QLD Telephone and postal |
Patients with Chronic Disease (CD) or at high risk of CD | ✓ | ✓ | ✓ | ✓ | A standardised coaching program delivered by registered nurses targeting CD patients and those at risk of CD, delivered by telephone and mail‐out. Coaches educate, advise and encourage patients to close the “treatment gaps” and achieve guideline‐recommended risk factor targets whilst working with their usual doctor(s). |
Abbreviations: A, alcohol; AFL, Australian Football League; CD, chronic disease; N, nutrition; NSW, New South Wales; NT, Northern Territory; P, physical activity; PHC, Primary Health Care; QLD, Queensland; RA, remote area; S, smoking; So, social and emotional wellbeing; VIC, Victoria; WA, Western Australia.
Table 4.
Physical activity – Programs that included a physical activity component
|
Program name or publication title References |
Setting | Participants | S | N | A | P | So | Outcomes assessed? | Program brief |
|---|---|---|---|---|---|---|---|---|---|
|
Water Aerobics Program 110 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 3 – NSW Community Setting |
Individuals with chronic disease | ✓ | ✓ | Two 1‐h water‐aerobic sessions per week for 6 wks. Includes regular monitoring of participant's measurements. | ||||
|
Koori Walkabout 106 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 1 – NSW Community and PHC Settings |
Aboriginal adults | ✓ | Koori Walkabout is a group walking program registered with the National Heart Foundation. Participants receive Heart Foundation information packs and a pedometer. T‐shirt incentive after seven sessions. The group walks once a week for 30‐45 min. The walk is followed by a healthy lunch at the AMS. | |||||
|
A 12‐wk sports‐based exercise program for inactive Indigenous Australian men 72 (Mendham, Duffield et al 2014) |
Regional NSW Community Setting |
Inactive Aboriginal and/or Torres Strait Islander men with not diagnosed with no pre‐existing CVD or metabolic disorders | ✓ | ✓ | Two to three strength and cardio exercise sessions per week. | ||||
|
Our Games Our Health 80 (Parker, Meiklejohn et al 2006) |
RA 2 and 4 – QLD Community and School Settings |
The Aboriginal Community groups and school students | ✓ | ✓ | The program consisted of three interlocking stages, community engagement, community mobilisation, and community capacity building. The project aimed to focus on men and older people, however, was redirected to focus on school children. Physical activity was Indigenous games form the book Choopadoo Games from the Dreamtime. | ||||
|
Healthy Food Awareness Program 107 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW PHC Setting |
Individuals with Chronic Disease | ✓ | ✓ | ✓ | A one day a week session focused on diet and exercise and other health‐related issues, including smoking at the AMS and at the AMS's outreach clinics. | |||
|
Spring into Shape Program 109 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW PHC Setting |
Not specified | ✓ | ✓ | ✓ | Exercise and nutrition program to promote healthy lifestyle change and manage stress in a better way. Wide range of physical activities occur with nutrition education sessions. Fruit and vegetable box provided for the cost of $5 including recipes. | |||
|
Healthy Lifestyle Program 111 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 3 – NSW Community and PHC Settings |
Aboriginal adults | ✓ | ✓ | Weekly meeting with a weigh in and talks on topics such as healthy eating, physical activity and meal preparation. Program also includes exercise sessions and a 30‐min group walk. Sessions supported by Weight Watchers. | ||||
|
Building Healthy Communities Project 112 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 4 – NSW PHC Setting |
Aboriginal community members including children | ✓ | ✓ | ✓ | Multiple components. Nutrition and cooking classes through “Quick Meals for Kooris” program. Community vegetable garden was established, the walking track was upgraded and a range of physical activity sessions. Women's self‐ esteem classes, craft and jewellery making classes were also part of the project. | |||
|
The Chronic Disease Self‐Management pilot study 20 (Ah Kit, Prideaux et al 2003) |
RA 4 and 5 – SA Community and PHC Settings |
Aboriginal people with type 2 diabetes. | ✓ | ✓ | ✓ | A chronic disease self‐management model for Aboriginal people consisting of local support coordination, extension of preventive health programs, self‐management processes and tools to suit goal setting and behaviour change including group exercise and diet education sessions and appropriate staff training. | |||
|
Aboriginal and Torres Strait Islander Women's Fitness Program 27 , 28 , 29 (Canuto, McDermott et al 2011, Canuto, Cargo et al 2012, Canuto, Spagnoletti et al 2013) |
RA 1 – SA Community Setting |
Aboriginal and Torres Strait Islander Women 18‐64 y with waist circumference greater than 80cm | ✓ | ✓ | ✓ | Twelve‐week program including two 60‐min group exercise classes per week, and four nutrition education workshops. RCT vs waitlisted controls. | |||
|
Healthy Lifestyles Project 30 (Cargo, Marks et al 2011) |
RA 5 – NT Community and PHC Settings |
Aboriginal Community in North East Arnhem Land | ✓ | ✓ | ✓ | ✓ | Community health screening, feedback and discussion. Coordinated community‐directed approach to increase the allocation of community resources to prevention activities. Multiple intervention strategies implemented; family food garden, community market, new school canteen, weekly walking program and a 4‐day healthy lifestyle festival. | ||
|
Aunty Jean's Good Health Program 34 (Curtis, Service et al 2004) |
RA 3 – NSW Community and PHC Settings |
Aboriginal Elders | ✓ | ✓ | ✓ | Twelve‐week program involving weekly group sessions that included a medical check, group exercise and information sharing from health professionals across multiple topics; nutrition and cooking, exercise, diabetes and stress management. This was combined with a self‐managed, self‐directed home program. | |||
|
“Step up to health” ‐Tasmanian Aboriginal Centre (TAC) Rehabilitation Program 35 (Davey, Moore et al 2014) |
RA 2 – TAS PHC Setting, Private Physiotherapy Practice and outdoors |
Adult Aboriginal people diagnosed with COPD, IHD, or CHF and people with at least 2 risk factors for developing CVD | ✓ | ✓ | ✓ | ✓ | ✓ | Two 1‐h supervised exercise sessions and one, 1‐h educational session per week for 8 wks. Sessions promoted self‐management approaches, cardiovascular and respiratory health, benefits of exercise, shopping, cooking and eating healthy food, medication, stress and psychological wellbeing, and smoking cessation. | |
|
Birth to Elders Nutrition Program 41 , 42 (Edwards 2004, Edwards 2005) |
RA 3 and 5 ‐ SA Community, Child Care Centres, PHC and School Settings |
Aboriginal community members | ✓ | ✓ | ✓ | ✓ | Multiple community‐based social and emotional wellbeing activities, providing health paraphernalia to communities, including nutritional education, and physical health interventions such as indoor little athletics and sports events. | ||
|
Gut Busters 43 (Egger, Fisher et al 1999) |
RA5 – QLD Community Setting |
Aboriginal and Torres Strait Islander men | ✓ | ✓ | ✓ | ✓ | Program run on four remote islands targeting four major lifestyle risk factors; reducing fat intake; increasing dietary fibre; increasing daily movement and changing “obesogenic” habits. The program encourages long‐term lifestyle changes including moderate use of alcohol and moderate‐intensity accumulated activity. Regular planned walking groups occurred on two islands. | ||
|
Waminda's Wellbeing Program 46 (Firth, Crook et al 2012) |
RA2 – NSW Community Setting |
Predominately Aboriginal and Torres Strait Islander women, including non‐Indigenous women | ✓ | ✓ | ✓ | ✓ | ✓ | Pilot program that evolved into intensive programs. Multiple components: exercise sessions; community gardens; cooking healthy meals; smoking cessation; health and wellbeing camps. | |
|
Diabetes Management and Care Program 51 (Gracey, Bridge et al 2006) |
RA5 – WA Community and PHC Settings |
Aboriginal community members | ✓ | ✓ | ✓ | Multiple strategies including lifestyle disease education, promotion of healthy eating, exercise and active recreation program, health screening and medication compliance. | |||
|
Deadly Choices Program 61 , 62 (Malseed, Nelson et al 2014, Malseed, Nelson et al 2014) |
RA1 – QLD School Setting |
High school students Grade 7‐12 | ✓ | ✓ | ✓ | ✓ | ✓ | Seven‐week physical activity and education program. Education components included leadership, chronic disease, physical activity, nutrition, smoking, harmful substances and health services. Health checks were also facilitated. | |
|
Watharoung Koori Youth Prevention Programs 74 (Milward 2009) |
RA1 – Vic Community Setting |
Aboriginal Youth | ✓ | ✓ | ✓ | A variety of programs in partnership with other organisations to prevention the use of alcohol and other drugs. The programs are designed to empower youth, strengthen individual Koori identity and learn more about their culture through camps, surfing competitions and an AFL football program. | |||
|
The Chronic Disease Self‐Management Project 75 (Mobbs, Nguyen et al 2003) |
RA5 – NT Community and PHC Settings |
Patients previously diagnosed with diabetes and/or hypertension with or without renal involvement | ✓ | ✓ | ✓ | ✓ | ✓ | Self‐care program to develop skills including changing behaviour; smoking, nutrition, physical activity and weight loss. Building family and community healthy lifestyle infrastructure using community empowerment framework. Production of local resources (booklets and videos) including HP messages. Establishment of women's healthy weight groups, walking groups and tobacco action initiative. | |
|
A pilot study of Aboriginal health promotion from an ecological perspective 82 , 83 (Reilly, Doyle et al 2007, Reilly, Cincotta et al 2011) |
RA2 – VIC Community Setting |
Multiple subgroups; Elders, women, junior footballers, employees, sporting club members | ✓ | ✓ | ✓ | Multiple programs including; a health “summer school” for health promotion practitioners; a nutrition program for under 17‐year‐old footballers; initiatives to improve the dietary quality of food supplied at the football and netball club; a series of focus groups to adapt mainstream nutrition guidelines for the Indigenous community; a weekly self‐directed health‐focused meeting for women; and a workplace exercise program. | |||
|
The Looma Diabetes Program and Looma Healthy Lifestyle Project 33 , 84 (Clapham, O'Dea et al 2007, Rowley, Daniel et al 2000) |
RA5 – WA Community Setting |
Initially Aboriginal people with diabetes or at high risk, progressing to the whole community | ✓ | ✓ | ✓ | ✓ | Following community wide diabetes screening, multiple strategies were implemented progressively over several years starting with a nutrition and exercise program for diabetes and high‐risk patients progressing to range of community wide initiatives. | ||
|
Indigenous Surf Programs 85 (Rynne, Rossi et al 2012) |
Multiple RAs – NSW, QLD, Vic and SA Community and School Settings |
Aboriginal and Torres Strait Islander peoples (three sites focused on youth) | ✓ | ✓ | ✓ | Five surfing programs across four states. Aim to foster connection to culture, identity, promote physical activity and social connection. | |||
|
Wadja Warriors Healthy Weight Program and the Injury Protection Project 88 (Smith 2002) |
RA 4 – QLD Community Setting |
Men from the local football team and other interested men in community | ✓ | ✓ | ✓ | ✓ | ✓ | Injury Prevention Project to reduce on‐ and off‐field violence including family violence and alcohol and drug use to reduce a major cause of injury: broken glass. Program developed to include a lifestyle program promoting good nutrition and physical activity and teaching skills that are required for making healthy changes. |
Abbreviations: A, alcohol; AFL, Australian Football League; AMS, Aboriginal Medical Service; CHF, chronic heart failure; COPD, chronic obstructive heart failure; CVD, cardiovascular disease; IHD ischaemic heart disease; N, nutrition; NSW, New South Wales; NT, Northern Territory; P, physical activity; PHC, Primary Health Care; QLD, Queensland; RA, remote area; RCT, Randomised Controlled Trial; S, smoking; SA, South Australia; So, social and emotional wellbeing; TAS, Tasmania; VIC, Victoria; WA, Western Australia.
Table 5.
Social and emotional wellbeing – Programs that included a social and emotional wellbeing component
|
Program name or publication title References |
Setting | Participants | S | N | A | P | So | Outcomes assessed? | Program brief |
|---|---|---|---|---|---|---|---|---|---|
|
Aboriginal Girls Circle 39 (Dobia, Bodkin‐Andrews et al 2014) |
RA 2 – NSW School Setting |
Aboriginal girls attending secondary schools. | ✓ | ✓ | An intervention targeting social connection, participation, resilience, cultural identity and self confidence amongst Aboriginal girls attending secondary schools. | ||||
|
Yarrabah's Yaba Bimbie Men's Group and Ma'Ddaimba Balas men's group 67 , 69 (McCalman, Baird et al 2007, McCalman, Tsey et al 2010) |
RA 3 – QLD Community Setting |
Aboriginal and Torres Strait Islander men | ✓ | ✓ | Men's groups that has a multilevel empowerment framework addressing social and emotional wellbeing, linked with the Family Empowerment Program | ||||
|
The Family Wellbeing Program 68 , 71 (McEwan, Tsey et al 2009, McCalman, McEwan et al 2010) |
RA 3 – Qld and RA 4 – NT Community Setting |
Aboriginal adults from two regions | ✓ | ✓ | An educational program that builds communication, problem‐solving, conflict resolution and other necessary skills to enable individuals to take greater control and responsibility for family, work and community life. | ||||
|
Yanan Ngurra‐ngu Walalja – The Halls Creek Community Family Programme 77 (Munns 2010) |
RA 5 – WA Community Setting |
Antenatal clients and all parents with children aged 0‐3 y | ✓ | ✓ | A comprehensive home visiting strategy with a holistic focus on the family's child rearing environment, recognising psychosocial influences. This program also assisted parents to develop strategies to address their children's physical, cognitive, emotional, behavioural, educational and language development, along with general health and nutritional needs for the children and the whole family. | ||||
|
Kulintja Nganampa Maa‐kunpuntjaku (Strengthening Our Thinking) 79 (Osborne 2013) |
RA 5 – SA Community and School Settings |
School aged children | ✓ | ✓ | Mind matters social and emotional wellbeing program adapted for use in Anangu schools. | ||||
|
Voices United for Harmony 91 , 92 , 93 (Sun and Buys 2012, Sun and Buys 2013, Sun and Buys 2013) |
Unidentified communities – QLD Community and PHC Settings |
Aboriginal and Torres Strait Islander adults | ✓ | ✓ | Twelve‐month‐old singing program with weekly 2‐h sessions and monthly performances led by skilled experienced singing group leaders. | ||||
|
Family Wellbeing Personal Development and Empowerment Program 97 (Tsey, Whiteside et al 2005) |
RA 5 – Qld School Settings |
Indigenous school children | ✓ | ✓ | A group program that helps children develop analytical and problem‐solving skills, thereby enhancing their psychosocial development. Program delivered by three out‐reach staff (two of whom were Indigenous) over 12 1‐h sessions, every 2‐3 wks over two school terms. | ||||
|
Family Wellbeing Course 94 , 95 , 96 (Tsey 2000, Tsey and Every 2000, Tsey and Every 2001) |
RA 4 – NT Community and School Settings |
Aboriginal and Torres Strait Islander families | ✓ | ✓ | Family Wellbeing course aims to empower participants and their families to assume a greater control over the conditions influencing their lives. It places particular emphasis on parenting and relationship skills. Four stages of the course, each runs for 10 wks with one 4‐h session per week by trained counsellors. | ||||
|
Spring into Shape Program 109 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 2 – NSW PHC Setting |
Not specified | ✓ | ✓ | ✓ | Exercise and nutrition program to promote healthy lifestyle change and manage stress in a better way. Wide range of physical activities occur with nutrition education sessions. Fruit and vegetable boxes provided for the cost of $5 including recipes. | |||
|
Building Healthy Communities Project 112 (Aboriginal Health Medical Research Council of New South Wales 2009) |
RA 4 – NSW PHC Setting |
Aboriginal community members including children | ✓ | ✓ | ✓ | Multiple components. Nutrition and cooking classes through “Quick Meals for Kooris” program. Community vegetable garden was established, the walking track was upgraded and a range of physical activity sessions. Women's self‐ esteem classes, craft and jewellery making classes were also part of the project. | |||
|
The Waringarri Project 32 (Chisholm 1989) |
RA 4 – WA Community and School setting |
Aboriginal community members | ✓ | ✓ | Trained staff implemented psycho‐social method of targeting individuals in crisis and using community development strategies to overcome the crisis, also established self‐help groups and introducing alcohol concepts into schools | ||||
|
“Step up to health” –Tasmanian Aboriginal Centre (TAC) Rehabilitation Program 35 (Davey, Moore et al 2014) |
RA 2 –TAS PHC Setting, Private Physiotherapy Practice and outdoors |
Adult Aboriginal people diagnosed with COPD, IHD, or CHF and people with at least two risk factors for developing CVD | ✓ | ✓ | ✓ | ✓ | ✓ | Two 1‐h supervised exercise sessions and one, 1‐h educational session per week for 8 wks. Sessions promoted self‐management approaches, cardiovascular and respiratory health, benefits of exercise, shopping, cooking and eating healthy food, medication, stress and psychological wel‐lbeing, and smoking cessation. | |
|
Heart Health – For Our People By Our People 37 , 38 (Dimer, Jones et al 2010, Dimer, Dowling et al 2013) |
RA 1 – WA PHC Setting |
Patients with CVD or at high risk of CVD | ✓ | ✓ | ✓ | ✓ | A cardiovascular disease (CVD) management program involving assessment and reassessment, provision of health information and an individualised program including motivational and education sessions; diet and nutrition; risk factor modification (including smoking cessation); managing stress and emotion (with referral for counselling when indicated); benefits of physical activity; diabetes management and medication usage. | ||
|
Birth to Elders Nutrition Program 41 , 42 (Edwards 2004, Edwards 2005) |
RA 3 and 5 – SA Community, Child Care Centres, PHC and School Settings |
Aboriginal community members | ✓ | ✓ | ✓ | ✓ | Multiple community‐based social and emotional wellbeing activities, providing health paraphernalia to communities, including nutritional education, and physical health interventions such as indoor little athletics and sports events. | ||
|
Strong Women, Strong Babies, Strong Culture Program 36 , 44 , 45 , 60 (d'Espaignet, Measey et al 2003, Fejo 1994, Fejo and Rae 1996, Mackerras 2001) |
Multiple communities – NT Community and PHC Settings |
Pregnant Women | ✓ | ✓ | ✓ | ✓ | ✓ | Women within Aboriginal communities help other Aboriginal women prepare for pregnancy by working together with nutritionists, community‐based health workers, local schools and other women in the community. | |
|
Waminda's Wellbeing Program 46 (Firth, Crook et al 2012) |
RA2 – NSW Community Setting |
Predominately Aboriginal and Torres Strait Islander women, including non‐Indigenous women | ✓ | ✓ | ✓ | ✓ | ✓ | Pilot program that evolved into intensive programs. Multiple components: exercise sessions; community gardens; cooking healthy meals; smoking cessation; health and wellbeing camps. | |
|
Karalundi Peer Support and Skills Training Program 52 (Gray, Sputore et al 1998) |
RA5 – WA School Setting |
Primary, high school and TAFE students aged 10‐20 y. | ✓ | ✓ | ✓ | ✓ | Ten programs aimed at: developing students' interpersonal, problem‐solving and decision‐making skills; quit smoking; drug; alcohol and petrol sniffing education; sex education, arts and crafts, general health promotion; eye, ear and nose care and the use of natural medicines. | ||
|
Malabar Community Midwifery Link Service 54 (Homer, Foureur et al 2012) |
RA1 – NSW PHC Setting |
Pregnant Aboriginal and/or Torres Strait Islander women and non‐Indigenous women having an Aboriginal and/or Torres Strait Islander baby | ✓ | ✓ | ✓ | ✓ | A unique model of antenatal care that addresses stress, smoking and alcohol consumption in pregnancy along with other care. | ||
|
Watharoung Koori Youth Prevention Programs 74 (Milward 2009) |
RA1 – Vic Community Setting |
Aboriginal Youth | ✓ | ✓ | ✓ | A variety of programs in partnership with other organisations to prevention the use of alcohol and other drugs. The programs are designed to empower youth, strengthen individual Koori identity and learn more about their culture through camps, surfing competitions and an AFL football program. | |||
|
The Chronic Disease Self‐Management Project 75 (Mobbs, Nguyen et al 2003) |
RA5 – NT Community and PHC Settings |
Patients previously diagnosed with diabetes and/or hypertension with or without renal involvement | ✓ | ✓ | ✓ | ✓ | ✓ | Self‐care program to develop skills including changing behaviour; smoking, nutrition, physical activity and weight loss. Building family and community healthy lifestyle infrastructure using community empowerment framework. Production of local resources (booklets and videos) including HP messages. Establishment of women's healthy weight groups, walking groups and tobacco action initiative. | |
|
Awareness and Self‐Management Programme 81 (Payne 2013) |
RA3 – QLD Community Setting |
Women with type 2 diabetes or identified has having an elevated risk of developing disease. | ✓ | ✓ | ✓ | Support groups involving information sessions on self‐management strategies; grief and loss; health ownership and concepts of shared knowledge; and diet and exercise. | |||
|
Indigenous Surf Programs 85 (Rynne, Rossi et al 2012) |
Multiple RAs – NSW, QLD, Vic and SA Community and School Settings |
Aboriginal and Torres Strait Islander peoples (three sites focused on youth) | ✓ | ✓ | ✓ | Five surfing programs across four states. Aim to foster connection to culture, identity, promote physical activity and social connection. | |||
|
WuChopperen Drug Alcohol and Other Substances program 90 (Strempel and Australian National Council on Drugs 2004) |
RA 1‐3 – QLD Community and PHC Settings |
Aboriginal and Torres Strait Islander youth | ✓ | ✓ | ✓ | ✓ | Provides counselling and support for young people in areas of physical, social and emotional health, and coordinates and delivers alcohol and other drug education to staff and health facilitators. |
Abbreviations: A, alcohol; AFL, Australian Football League; CHF, chronic heart failure; COPD, chronic obstructive heart failure; CVD, cardiovascular disease; IHD ischaemic heart disease; N, nutrition; NSW, New South Wales; NT, Northern Territory; P, physical activity; PHC, Primary Health Care; QLD, Queensland; RA, remote area; S, smoking; SA, South Australia; So, social and emotional wellbeing; TAFE Technical and Further Education; TAS, Tasmania; VIC, Victoria; WA, Western Australia.
Of the programs identified by this review, most were based in Queensland (n = 24) 21 , 22 , 26 , 31 , 40 , 43 , 49 , 53 , 59 , 61 , 62 , 67 , 68 , 69 , 70 , 71 , 80 , 81 , 85 , 86 , 87 , 88 , 89 , 91 , 92 , 93 , 97 , 98 , 99 , 100 , 101 or New South Wales (n = 21). 18 , 19 , 24 , 25 , 34 , 39 , 46 , 54 , 58 , 63 , 72 , 76 , 85 Ten of the programs were based in Western Australia, 32 , 33 , 38 , 40 , 51 , 52 , 64 , 65 , 66 , 77 , 78 , 84 , 102 nine in the Northern Territory, 30 , 36 , 44 , 45 , 50 , 55 , 56 , 57 , 60 , 68 , 71 , 73 , 75 , 94 , 95 , 96 six in South Australia, 20 , 23 , 27 , 28 , 29 , 41 , 42 , 79 , 85 five in Victoria 74 , 82 , 83 , 85 , 87 , 98 , 99 , 103 and one in Tasmania. 35 One program did not identify the community in which it was run. 47 Four programs were implemented in more than one state or territory. 40 , 68 , 71 , 85 , 87 , 98 , 99 About 18 of the identified programs were based in a major city (RA 1), 18 , 27 , 28 , 29 , 31 , 38 , 40 , 49 , 53 , 54 , 58 , 61 , 62 , 63 , 74 , 76 , 85 , 89 , 101 , 104 , 105 , 106 14 in an inner regional centre (RA 2), 24 , 25 , 35 , 39 , 46 , 63 , 78 , 80 , 82 , 83 , 85 , 90 , 103 , 107 , 108 , 109 12 in an outer regional centre (RA 3), 24 , 25 , 34 , 41 , 42 , 59 , 67 , 69 , 81 , 85 , 86 , 90 , 107 , 110 , 111 13 in a remote area (RA 4) 20 , 21 , 22 , 23 , 24 , 31 , 32 , 64 , 65 , 66 , 80 , 85 , 88 , 94 , 95 , 96 , 112 and 21 in a very remote area (RA 5). 20 , 21 , 23 , 26 , 30 , 31 , 41 , 42 , 43 , 50 , 51 , 52 , 55 , 56 , 57 , 64 , 65 , 66 , 70 , 75 , 77 , 79 , 84 , 97 , 100 , 102 The communities for six programs could not be identified therefore no remote area classification was allocated. 22 , 36 , 44 , 45 , 47 , 60 , 72 , 73 , 87 , 91 , 92 , 93 , 98 , 99
Programs were delivered in a variety of settings. Of those delivered in just one setting, the community setting was most common (n = 20), 24 , 25 , 27 , 28 , 29 , 31 , 33 , 43 , 46 , 47 , 49 , 63 , 67 , 68 , 69 , 71 , 72 , 74 , 77 , 78 , 81 , 82 , 83 , 84 , 88 , 102 , 110 then the PHC setting (n = 11) 18 , 37 , 38 , 40 , 54 , 70 , 89 , 105 , 106 , 107 , 109 , 112 or a school (n = 8). 22 , 39 , 52 , 61 , 62 , 86 , 97 , 100 , 108 Programs were also delivered across multiple settings such as the community and PHC settings (n = 16), 20 , 23 , 30 , 34 , 36 , 44 , 45 , 51 , 53 , 56 , 57 , 59 , 60 , 64 , 65 , 66 , 75 , 76 , 91 , 92 , 93 , 101 , 104 , 106 , 111 community and school (n = 9), 32 , 50 , 55 , 73 , 79 , 80 , 85 , 94 , 95 , 96 , 103 community, PHC and school (n = 2), 26 , 41 , 42 PHC and school (n = 1),21 PHC and outpatients (n = 1) 58 community, PHC and physiotherapist practice (n = 1) 35 and one was delivered via telephone and postal service. 87 , 98 , 99
Thirty of the programs focused on more than one of the SNAPS risk factors. 20 , 27 , 28 , 29 , 30 , 32 , 33 , 34 , 35 , 36 , 37 , 41 , 42 , 43 , 44 , 45 , 46 , 51 , 52 , 53 , 54 , 60 , 61 , 62 , 70 , 74 , 75 , 81 , 82 , 83 , 84 , 85 , 87 , 88 , 98 , 99 , 101 , 107 , 109 , 111 , 112 Forty‐one of the programs focused on modifying only one behavioural risk factor; of these, seven focused on smoking (see Table 1), 26 , 40 , 50 , 55 , 63 , 64 , 65 , 66 , 89 seventeen on nutrition (see Table 2), 18,21, 23‐25,31,49,56,57,59,76,78,100,102‐106,108,110 five focused solely on alcohol prevention and/or management (see Table 3), 22 , 47 , 58 , 73 , 86 four on physical activity (see Table 4) 72 , 80 , 106 , 110 and eight on social and emotional wellbeing (see Table 5). 39 , 67 , 68 , 69 , 71 , 77 , 79 , 91 , 92 , 93 , 94 , 95 , 96 , 97 None of the programs identified focused on modifying all five of SNAPS risk factors. The number of SNAPS factors that the programs addressed are indicated in Figure 2.
Figure 2.
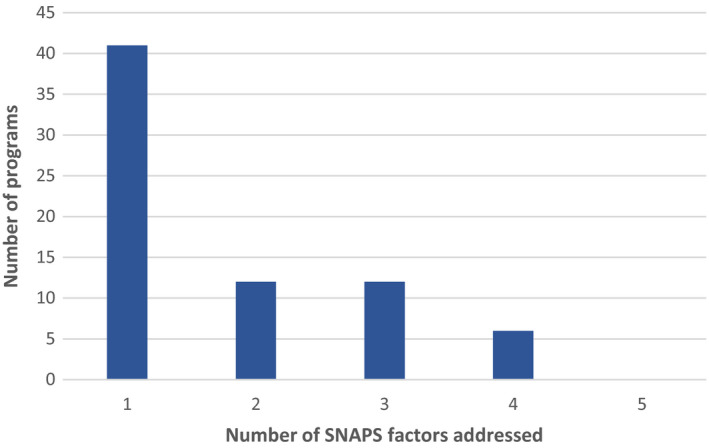
Number of SNAPS risk factors addressed in the identified programs
5.1. Programs that focused on smoking prevention and/or cessation
Twenty‐three of the identified programs aimed to prevent or reduce smoking rates in Aboriginal and Torres Strait Islander communities (Table 1). 26 , 30 , 31 , 35 , 36 , 37 , 38 , 40 , 44 , 45 , 46 , 50 , 52 , 53 , 54 , 55 , 61 , 62 , 63 , 64 , 65 , 66 , 70 , 75 , 84 , 87 , 88 , 89 , 90 , 107 Seven of the programs focused solely on smoking, 26 , 40 , 50 , 55 , 62 , 63 , 64 , 65 , 66 , 89 while most included a focus on additional SNAPS risk factors (Figure 2). All but one program reported outcomes of some description.0107 Seven programs focused on participants with a chronic disease such as type 2 diabetes or cardiovascular disease. 33 , 35 , 37 , 38 , 70 , 75 , 84 , 87 , 98 , 99 , 107 Six programs included a focus on children/youth (as defined by the program description), 26 , 50 , 52 , 55 , 61 , 62 , 101 and four focused on pregnant women. 36 , 40 , 44 , 45 , 53 , 54 , 60 One program also offered nicotine replacement therapy (NRT) to participants who had two failed quit attempts during the intervention,40 while another offered subsidised NRT combined with support groups.63 All but one of the programs reported outcomes that were assessed. 107
5.2. Programs that focused on healthy nutrition
The most commonly addressed behaviour risk factor was nutrition, with 40 programs identified (Table 2). 18 , 21 , 23 , 24 , 25 , 27 , 28 , 29 , 30 , 31 , 33 , 34 , 35 , 36 , 37 , 38 , 41 , 42 , 43 , 44 , 45 , 46 , 49 , 51 , 56 , 57 , 59 , 61 , 62 , 75 , 76 , 78 , 81 , 82 , 83 , 84 , 87 , 88 , 98 , 99 , 100 , 102 , 103 , 104 , 105 , 106 , 107 , 108 , 109 , 110 , 111 , 112 , 113 Seventeen of the programs focused on nutrition only, 18 , 19 , 20 , 21 , 23 , 24 , 25 , 31 , 48 , 49 , 56 , 57 , 59 , 76 , 78 , 100 however, some of these also included education about physical activity and/or other interventions such as an education session for chronic disease management. 23 , 31 , 59 , 76 , 104 An additional 22 programs included initiatives to address other SNAPS risk factors together with nutrition. Sixteen programs included hands‐on cooking classes or demonstrations, 18 , 21 , 27 , 28 , 29 , 34 , 35 , 46 , 49 , 76 , 78 , 102 , 103 , 104 , 105 , 106 , 108 , 110 , 112 six included a community or school garden 46 , 100 , 103 , 108 , 111 , 112 and three programs included subsidised fruit and vegetable boxes, 24 , 25 , 108 , 109 while 18 were education or brief intervention only. It was not possible to differentiate between intensive nutrition education sessions delivered by a nutritionist or dietician as opposed to brief intervention. Nine of these programs did not report any outcomes. 102 , 103 , 106 , 107 , 108 , 109 , 110 , 111 , 112
5.3. Programs that focused on reducing/ eliminating alcohol consumption
Sixteen of the identified programs aimed to reduce alcohol consumption (Table 3). 22 , 32 , 36 , 43 , 44 , 45 , 47 , 52 , 53 , 54 , 58 , 60 , 61 , 62 , 73 , 74 , 86 , 87 , 88 , 98 , 99 , 101 Of those, only five programs focused on alcohol consumption and no other included SNAPS factors. 22 , 47 , 58 , 73 , 86 In addition to the programs included in this review there were additional programs identified that address alcohol consumption but were ineligible as they required participants to be outside of their normal living environment, either at a camp or residential facility, for example Oolong Houses 114 or included multiple steams of intervention including pharmaceutical and results were not reported separately.115 Of the programs that included a focus on alcohol together with other SNAPS risk factors it was difficult to determine the level or intensity of the alcohol education or brief intervention. Three of these programs did not report any assessed outcomes. 32 , 47 , 74
5.4. Programs that focused on the promotion of physical activity
Twenty‐four of the identified programs included a physical activity component (Table 4). 20,23,27‐31,33‐35,41‐43,46,51,59,61,62,72,75,80,82‐85,88,10 6,107,109‐112 Of those, only four programs focused on physical activity in the absence of other SNAPS risk factors included in this review. 72 , 80 , 106 , 110 None of the programs that described education or brief intervention in physical activity indicated that the advice was given by a qualified exercise physiologist, unlike nutrition education, which was commonly delivered by a nutritionist or dietician. All but five of the programs had reported an outcome that had been assessed. 106 , 107 , 109 , 111 , 112
5.5. Programs that focused on improving social and emotional wellbeing
Twenty‐three of the identified programs aimed to improve social and emotional wellbeing (Table 5), 32 , 35 , 36 , 37 , 38 , 39 , 41 , 42 , 44 , 45 , 46 , 52 , 54 , 67 , 68 , 69 , 71 , 74 , 75 , 77 , 79 , 81 , 85 , 91 , 92 , 93 , 94 , 95 , 96 , 97 , 101 , 109 , 112 of those eight focused on social and emotional wellbeing without addressing other SNAP factors. 39 , 67 , 68 , 69 , 71 , 77 , 79 , 91 , 92 , 93 , 94 , 95 , 96 , 97 Six of the programs were specifically for children or youth, 39 , 52 , 74 , 79 , 97 , 101 five were specifically for Aboriginal and Torres Strait Islander women or girls 36 , 39 , 44 , 45 , 46 , 54 , 81 and two of which were for pregnant women. 36 , 44 , 45 , 54 Four programs focused on people diagnosed with a chronic condition such as type 2 diabetes, 35 , 37 , 38 , 75 , 81 two programs focused on families, 77 , 94 , 95 , 96 while only one of social and emotional wellbeing programs were specifically for Aboriginal and Torres Strait Islander men. 67 , 69 Four of these programs did not provide any assessed outcomes. 32 , 74 , 109 , 112
6. DISCUSSION
Health promotion programs and activities play a key role in supporting the health of Aboriginal and Torres Strait Islander communities. 116 This review has focused on programs addressing those key risk factors for noncommunicable chronic diseases which impact most strongly on Aboriginal and Torres Strait Islander Health, using the SNAPS framework. A number of these health promotion programs were similar to, or based on, programs originally delivered in non‐Indigenous communities, that were modified for Aboriginal and Torres Strait Islander participants, for example, school‐based nutrition programs, 100 the Coaching patients On Achieving Cardiovascular Health (COACH) study 87 , 98 , 99 and the Gut Busters program. 43 However, some were specifically designed for and by Aboriginal and Torres Strait Islander people with a strong consideration of local culture and context such as the “Smokin' No way, SmokeCheck and Smoke Rings” programs 26 and the health promotion program conducted within the Koori community of the Goulburn‐Murray region of northern Victoria, Australia. 82 , 83
The National Aboriginal and Torres Strait Islander Health Plan 2013‐2023 identifies the importance of Aboriginal and Torres Strait Islander health professionals being involved in the development and delivery of culturally safe health promotion and health education programs and the engagement of Aboriginal and Torres Strait Islander people in their own health, and emphasises the importance of PHC settings for the delivery of health promotion programs. 13 In this review we attempted to identify programs which were specifically designed for or modified for Aboriginal and/or Torres Strait Islander participants to ensure cultural appropriateness and acceptability, however this information was seldom reported.
A 2011 review of health promotion interventions for Aboriginal and Torres Strait Islanders (up to August 2007) focused on smoking, nutrition, alcohol and physical activity but excluded papers that were not defined as an “intervention”; which was defined as a program that assessed the effectiveness of a clinical or public health intervention, or an intervention to improve health care delivery to Indigenous Australians. 117 The current scoping review utilised broad inclusion criteria and included many programs that may not be not considered “research” or “interventions” including 12 programs that did not have any reported outcomes. 32 , 47 , 74 , 102 , 103 , 106 , 107 , 108 , 109 , 110 , 111 , 112 Nine of the programs without reported outcomes were published in the grey literature; seven of these were from the “10 out of 10 deadly health stories”, a document of health promotion programs implemented by NSW Aboriginal community controlled health services 19 and two were from a book showcasing Indigenous health success stories. 48 These inclusions are important to provide a comprehensive scoping review that can identify all studies and programs that can inform the Aboriginal health sector.
The most commonly addressed individual risk factor identified through this review was nutrition (40 programs), with 24 programs identified in addressing physical activity, 23 for smoking and social and emotional wellbeing and 16 programs focussing on alcohol. It should be noted that 41% of the programs identified in this review addressed more than one SNAPS risk factor but the extent of the focus on each risk factor in these programs was often unclear. For example, only four programs focussed solely on physical activity, whilst the other 19 had varying elements of physical activity included. Of the 23 programs identified that had some elements addressing social and emotional wellbeing, only nine had a key focus on this risk factor. Given that social and emotional wellbeing is consistently identified as a major determinant of health for Aboriginal and Torres Strait Islander people and the National Aboriginal and Torres Strait Islander Health Plan 2013‐2023 notes a number of priorities for Aboriginal Health programs including the importance of including social and emotional wellbeing as a central platform for prevention and clinical care, we found this disappointing and feel it should be a core consideration when developing all health promotion programs. 13 It was encouraging to see that 32% of programs focused on or included children or youth (32%), given the importance of early intervention in health promotion and prevention, 118 which is also highlighted in the National Aboriginal and Torres Strait Islander Health Plan 2013‐2023. 12
The health action areas identified in the Ottawa Charter provide a comprehensive framework for planning and evaluating health promotion programs.9 There is growing evidence that identifies the importance of using multiple Ottawa Charter action areas to achieve sustainable health outcomes.118 The majority of the programs in this review used the development of personal skills as their key strategy – mainly through education. Creating supportive environments was particularly evident in those programs that specifically considered cultural appropriateness and acceptability. 43 , 68 , 71 , 82 , 83 , 100 , 108 Very few programs reported strategies to empower the community or develop healthy public policy or reorient health services, which was surprising considering how many programs actively involved a PHC centre. In Aboriginal and Torres Strait Islander communities in particular, the importance of creating supportive environments and strengthening community action are vital and developing personal skills will not be sustainable in most instances without these added elements. 119
Another key component of health promotion programs in Aboriginal and Torres Strait Islander contexts identified by this review was the use of a multidisciplinary approach. The importance of such an approach is similarly emphasised in the Closing the Gap National Aboriginal and Torres Strait Islander Health Plan 2013‐2023. 13 One benefit of delivering health promotion programs through Aboriginal Community Controlled Health Organisations (ACCHOs) which are community owned and controlled PHC services and understand and foster community involvement and empowerment, is that they are multidisciplinary and provide an environment that understands and supports the local community in which programs can be developed by and with the local community. 120
The systematic search identified reviews and systematic reviews published on health promotion strategies for Aboriginal and Torres Strait Islander (some that included other international indigenous populations) that were focused on one or more of the risk factors. The majority were again focused on tobacco and nutrition. The evidence appears to be still insufficient to draw evidence‐based conclusions on the effectiveness of health promotion activities with the reviews finding few studies, many of which had small sample sizes and lacked rigorous research design.
Aligned with the scoping review method followed, 15 this review did not attempt to assess the quality of any evaluation that was undertaken, and therefore the validity of any program outcomes. The Closing the Gap. National Aboriginal and Torres Strait Islander Health Plan 2013‐2023 emphasises the importance of monitoring and surveillance, however, it appears that resourcing for evaluation is often not available when planning health promotion programs. Baum et al 121 note that health promotion itself often competes for resources with more pressing clinical needs, so evaluation is often not able to be funded or undertaken. A review in 2007 of the evaluated Australian Indigenous health promotion initiatives highlighted the issue of poor evaluation design and the lack of rigour that resulted in insufficient evidence to demonstrate positive outcomes. 116 There is also an issue with the capacity and skilled sets of people working in PHC to undertake evaluation activities. External evaluations are generally preferable in terms of independent reporting, however, these can be very expensive and funding for evaluation should be an independent and essential part of the overall project funding so that it does not get absorbed by or prioritised to service delivery. 122 Another aspect which makes critiquing many of the articles identified was a lack of information about the design and methods of data collection. Without this information, it is difficult to provide definitive information on what may be effective and to justify ongoing financial commitment to programs that cannot demonstrate positive outcomes.
6.1. Strengths and limitations
One of the key strengths of this scoping review was the comprehensive search undertaken, which used broad inclusion criteria and so identified a wide range of health promotion programs undertaken in both PHC and non‐PHC settings. Despite this, it should also be noted that there are many PHC services are delivering health promotion programs and activities that will not be captured in this scoping study as many of the programs undertaken are not published in the research literature and can only be found in their annual reports or on their webpages. Evaluating health promotion programs and then publishing the findings require the availability of time, resources including costs for publications and research skills, which are not often a PHC service's strength or priority.
The broad scope of the review was also the limitation for the search. As the search located so many publications that did not meet the inclusion criteria, reviewing over 10 000 publications by title and abstract was an enormous task and was divided and allocated to four reviewers KJC, EA, CL and CT. The inclusion criteria applied to this review was broad. To be inclusive, the inclusion criteria lacked specifics which led to problems and was interpreted differently by reviewers. Consequently, the review of titles and abstracts was redone to capture any paper missed by this misinterpretation. Likewise, data extraction completed by multiple reviewers, regardless of the data extraction tool and guidelines, were inconsistent and considerable reediting by KJC and KC was required. We hope that the double‐checking and handling of the data, although time consuming, has resulted in a thorough review.
7. CONCLUSION AND IMPLICATIONS
This scoping study identified a wide variety of health promotion programs focussing on the SNAPS risk factors. Approximately half of the programs focused on more than one of the SNAPS factors. Given the burden of chronic disease in Aboriginal and Torres Strait Islander populations and the interplay of the factors and their collective risk, such a focus across factors seems appropriate. The programs being implemented across settings other than PHC centres often included multiple settings which were encouraging to note, however, the focus on individual skills and personal behaviour change without addressing the other health action areas was disappointing.
Given the importance of social and emotional wellbeing as a central platform for prevention and clinical care, any future health promotion programs should also prioritise integration of culture, social and emotional wellbeing and specific strategies developed by or with Aboriginal and Torres Strait Islander people.
Furthermore, the importance of monitoring and evaluation must be considered. 13 If evaluation was to be included in all health promotion program funding, it would be possible to determine the effectiveness of health promotion programs in Aboriginal and Torres Strait Islander communities much more accurately. This could also act as an enabler for the publication of the results of health promotion programs so lessons learned (including strategies that may not be successful) can be more broadly disseminated.
It is positive to see an emerging emphasis on the importance of evaluation through documents such as the “Implementation Plan for the National Aboriginal and Torres Strait islander Health Plan 2013‐2023” 123 and the more recent Productivity Commission project entitled “Indigenous Evaluation Strategy”. 124 The Indigenous Evaluation Strategy released an Issues paper in June 2019 inviting submissions from individual and organisations. 124 The Commission has been asked to; establish a principles‐based framework for the evaluation of policies and programs affecting Indigenous Australians; identify priorities for evaluation; set out its approach for reviewing agencies' conduct of evaluations against the strategy. 124 Hopefully this will ultimately improve the quality of the evidence to inform future health promotion initiatives for Aboriginal and Torres Strait Islander people.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
ACKNOWLEDGEMENTS
This scoping review is supported by a Centre of Research Excellence in Aboriginal Chronic Disease Knowledge Translation and Exchange (CREATE) funded by the National Health and Medical Research Council (#1061242). The scope of this review was developed in consultation with the CREATE leadership group comprised of representatives from the Aboriginal and Torres Strait Islander Health Sector and was led by an Indigenous researcher with health promotion training and experience. We thank Maureen Bell, Research Librarian from the University of Adelaide for her guidance in the development of the search strategy and Arwen Nikolof and Seth Westhead who assisted in the data extraction of the case studies. AB is supported by a Senior Research Fellowship from NHMRC (#1137563).
Canuto KJ, Aromataris E, Burgess T, et al. A scoping review of Aboriginal and Torres Strait Islander health promotion programs focused on modifying chronic disease risk factors. Health Promot J Austral. 2021;32:46–74. 10.1002/hpja.307
REFERENCES
- 1. Australian Institute of Health and Welfare . The health and welfare of Australia's Aboriginal and Torres Strait Islander peoples: 2015. Canberra: AIHW; 2015. [Google Scholar]
- 2. World Health Organization . Global Health Observatory (GHO) data. Risk Factors [cited 2016]. Available from: http://www.who.int/gho/ncd/risk_factors/en/
- 3. McDermott RA, McCulloch BG, Campbell SK, Young DM. Diabetes in the Torres Strait Islands of Australia: better clinical systems but significant increase in weight and other risk conditions among adults, 1999–2005. MJA. 2007;186(10):505–8. [DOI] [PubMed] [Google Scholar]
- 4. Treatment costs, health promotion saves [press release]. Australia Health Promotion Association; 2016. [cited 2019]. Available from: https://www.healthpromotion.org.au/images/MediaStatementElectionAHPAJune2016_NATIONAL.pdf [Google Scholar]
- 5. Institute of Medicine (US) Committee on Health and Behavior: Research Practice, and Policy . Health and behavior: the interplay of biological, behavioral, and societal influences. Washington, DC: National Academies Press (US); 2001. [PubMed] [Google Scholar]
- 6. Glanz K. Behavioural and Social Science Research. 2011. In: Social and Behavioural Theories [Internet]. Bethesda: Available from: http://www.esourceresearch.org/eSourceBook/SocialandBehavioralTheories/4ImportantTheoriesandTheirKeyConstructs/tabid/730/Default.aspx [Google Scholar]
- 7. Green J. The role of theory in evidence‐based health promotion practice. Health Educ Res. 2000;15(2):125–9. [DOI] [PubMed] [Google Scholar]
- 8. Boyce T, Robertson R, Disxon A. Commissioning and behaviour change: kicking bad habits final report. London: Kings Fund; 2008. [Google Scholar]
- 9. World Health Organization . The Ottawa Charter for Health Promotion: World Health Organization; 1986. [cited 2016]. Available from: http://www.who.int/healthpromotion/conferences/previous/ottawa/en/index1.html
- 10. Calma T. Social determinants and the health of Indigenous peoples in Australia ‐ a human rights based approach. International Symposium on the Social Determinants of Indigenous Health. Adelaide: Australian Human Rights Commission; 2007. [Google Scholar]
- 11. Arabena K, Rowley K, McLean S. Building evidence about effective health promotion in Aboriginal and Torres Strait Islander communities. Aust J Prim Health. 2014;20:317–8. [DOI] [PubMed] [Google Scholar]
- 12. World Health Organization . Primary health care: World Health Organization; 2016. [cited 2016]. Available from: http://www.who.int/topics/primary_health_care/en/
- 13. Department of Health (Australia) . National Aboriginal and Torres Strait Islander Health Plan 2013–2023. 2013. [cited 2019]. Available from: https://www1.health.gov.au/internet/main/publishing.nsf/content/B92E980680486C3BCA257BF0001BAF01/$File/health-plan.pdf
- 14. Canuto K, Aromataris E, Lockwood C, Tufanaru C, Brown A. Aboriginal and Torres Strait Islander health promotion programs for the prevention and management of chronic diseases: a scoping review protocol. JBI Database System Rev Implement Rep. 2017;15(1):10–4. [DOI] [PubMed] [Google Scholar]
- 15. Peters MD, Godfrey CM, Khalil H, McInerney P, Parker D, Soares CB. Guidance for conducting systematic scoping reviews. Int J Evid Based Healthc. 2015;13(3):141–6. [DOI] [PubMed] [Google Scholar]
- 16. Department of Health (Australia) . Australian Standard Geographical Classification System ‐ Remoteness Area (ASGC‐RA 2006) [cited 2016]. Available from: http://www.doctorconnect.gov.au/internet/otd/publishing.nsf/Content/locator
- 17. Australian Bureau of Statistics . Australian Statistical Geography Standard (ASGS): Australian Bureau of Statistics; 2014. [cited 2016]. Available from: http://www.abs.gov.au/websitedbs/D3310114.nsf/home/Australian+Statistical+Geography+Standard+(ASGS)
- 18. Abbott PA, Davison JE, Moore LF, Rubinstein R. Effective nutrition education for Aboriginal Australians: lessons from a diabetes cooking course. J Nutr Educ Behav. 2012;44(1):55–9. [DOI] [PubMed] [Google Scholar]
- 19. Aboriginal Health Medical Research Council of New South Wales . 10 out of 10 deadly health stories: nutrition and physical activity: successful program from NSW Aboriginal community controlled health services. Surry Hills, NSW: Aboriginal Health and Medical Research Council of New South Wales, 2009; 2009. Report No.: 9780980515916. [Google Scholar]
- 20. Ah Kit J, Prideaux C, Harvey P, Collins J, Battersby M, Mills P, et al. Chronic disease self‐management in Aboriginal communities: towards a sustainable program of care in rural communities. Aust J Prim Health. 2003;9(2–3):168–76. [Google Scholar]
- 21. Aliakbari J, Latimore R, Polson C, Ross‐Kelly M, Hannan‐Jones M. A partnership approach to delivering health education in remote Indigenous communities. 12th National Rural Health Conference: strong commitment, bright future: 7–10 April 2013, Adelaide Convention Centre; 2013; Deakin, ACT. In: 12th National Rural Health Conference: strong commitment, bright future: 7–10 April 2013, Adelaide Convention Centre. Deakin, ACT: National Rural Health Alliance, 2013: 6p: National Rural Health Alliance; 2013. p. 6p.
- 22. Barber JG, Walsh C, Bradshaw R. An alcohol prevention program for Aboriginal children. Drug Educ J Aust. 1988;2(2):91–103. [Google Scholar]
- 23. Battersby MW, Ah Kit J, Prideaux C, Harvey PW, Collins JP, Mills PD. Implementing the Flinders model of self‐management support with Aboriginal people who have diabetes: findings from a pilot study. Aust J Prim Health. 2008;14(1):66–74. [Google Scholar]
- 24. Black AP, Vally H, Morris P, Daniel M, Esterman A, Karschimkus CS, et al. Nutritional impacts of a fruit and vegetable subsidy programme for disadvantaged Australian Aboriginal children. Br J Nutr. 2013;110(12):2309–17. [DOI] [PubMed] [Google Scholar]
- 25. Black AP, Vally H, Morris P, Daniel M, Esterman A, Smith F, et al. High folate levels in Aboriginal children after subsidised fruit and vegetables and mandatory folic acid fortification. Aust N Z J Public Health. 2014;38(3):241–6. [DOI] [PubMed] [Google Scholar]
- 26. Campbell S, Bohanna I, McKeown‐Young D, Esterman A, Cadet‐James Y, McDermott R. Evaluation of a community‐based tobacco control intervention in five remote north Queensland Indigenous communities. Int J Health Promot Educ. 2014;52(2):78–89. [Google Scholar]
- 27. Canuto K, Cargo M, Li M, D'Onise K, Esterman A, McDermott R. Pragmatic randomised trial of a 12‐week exercise and nutrition program for Aboriginal and Torres Strait Islander women: clinical results immediate post and 3 months follow‐up. BMC Public Health. 2012;12:933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Canuto KJ, McDermott RA, Cargo M, Esterman AJ. Study protocol: A pragmatic randomised controlled trial of a 12‐week physical activity and nutritional education program for overweight Aboriginal and Torres Strait Islander women. BMC Public Health. 2011;11:655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Canuto KJ, Spagnoletti B, McDermott RA, Cargo M. Factors influencing attendance in a structured physical activity program for Aboriginal and Torres Strait Islander women in an urban setting: a mixed methods process evaluation. Int J Equity Health. 2013;12:11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Cargo M, Marks E, Brimblecombe J, Scarlett M, Maypilama E, Dhurrkay JG, et al. Integrating an ecological approach into an Aboriginal community‐based chronic disease prevention program: a longitudinal process evaluation. BMC Public Health. 2011;11:299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Chan LCK, Ware R, Kesting J, Marczak M, Good D, Shaw JTE. Short term efficacy of a lifestyle intervention programme on cardiovascular health outcome in overweight Indigenous Australians with and without type 2 diabetes mellitus: the healthy lifestyle programme (HELP). Diabetes Res Clin Pract. 2007;75(1):65–71. [DOI] [PubMed] [Google Scholar]
- 32. Chisholm D. The Waringarri Project: how we did it. Yarranma. 1989;2(3):1–3. [Google Scholar]
- 33. Clapham K, O'Dea K, Chenhall RD. Interventions and sustainable programs In: Carson B, Dunbar T, Chenhall R, Bailie R, editors. Social determinants of Indigenous health. Crows Nest, NSW: Allen and Unwin, 2007; p. 271–95. [Google Scholar]
- 34. Curtis S; Illawarra Health Service, NSW Health Aboriginal Vascular Program . Aunty Jean's Good Health Team: listening to the voices of the elders to create an Aboriginal chronic and complex care program: participatory evaluation of the Illawarra Health, Aboriginal Chronic and Complex Care, Pilot Program. Wollongong, NSW: Illawarra Health, 2004, . Report No.: 0646436619. [Google Scholar]
- 35. Davey M, Moore W, Walters J. Tasmanian Aborigines step up to health: evaluation of a cardiopulmonary rehabilitation and secondary prevention program. BMC Health Serv Res. 2014;14(1):349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. d'Espaignet ET, Measey ML, Carnegie MA, Mackerras D. Monitoring the 'Strong Women, Strong Babies, Strong Culture Program': the first eight years. J Paediatr Child Health. 2003;39(9):668–72. [DOI] [PubMed] [Google Scholar]
- 37. Dimer L, Dowling T, Jones J, Cheetham C, Thomas T, Smith J, et al. Build it and they will come: outcomes from a successful cardiac rehabilitation program at an Aboriginal Medical Service. Aust Health Rev. 2013;37(1):79–82. [DOI] [PubMed] [Google Scholar]
- 38. Dimer L, Jones J, Dowling T, Cheetham C, Maiorana A, Smith J. Heart health: new ways to deliver cardiac rehabilitation. Aust Nurs J. 2010;18(6):41. [PubMed] [Google Scholar]
- 39. Dobia B, Bodkin‐Andrews G, Parada R, O'Rourke V, Gilbert S, Daley A, et al. Aboriginal girls circle: enhancing connectedness and promoting resilience for Aboriginal girls. New South Wales: University of Western Sydney, 2014; 2014. Report No.: 9781741083033 9781741083040. [Google Scholar]
- 40. Eades SJ, Sanson‐Fisher RW, Wenitong M, Panaretto K, D'Este C, Gilligan C, et al. An intensive smoking intervention for pregnant Aboriginal and Torres Strait Islander women: a randomised controlled trial. MJA. 2012;197(1):42–6. [DOI] [PubMed] [Google Scholar]
- 41. Edwards C. Birth to elders: nutrition for life ‐ Pika Wiya health service. Aborig Isl Health Work J. 2004;28(6):22–3, 27. [Google Scholar]
- 42. Edwards C. Marree Aboriginal school…taking health promotion on the road. Aborig Isl Health Work J. 2005;29(1):17, 20–1. [Google Scholar]
- 43. Egger G, Fisher G, Piers S, Bedford K, Morseau G, Sabasio S, et al. Abdominal obesity reduction in indigenous men. Int J Obes. 1999;23(6):564–9. [DOI] [PubMed] [Google Scholar]
- 44. Fejo L. The strong women, strong babies, strong culture program. Aborig Isl Health Work J. 1994;18(6):16. [Google Scholar]
- 45. Fejo L, Rae C; Strong Women, Strong Babies, Strong Culture project . 1996; Australia. Aboriginal health, social and cultural transitions: proceedings of a conference at the Northern Territory University, Darwin, 29‐30 September, 1995/edited by Gary Robinson. Darwin: NTU Press, 1996: 77‐821996. p. 77–82. [Google Scholar]
- 46. Firth W, Crook L, Thompson M, Worner F, Board W. Waminda's Wellbeing program. Aborig Isl Health Work J. 2012;36(2):20–3. [Google Scholar]
- 47. Fisher D, van der Heide G. CADAP ‐ community approach to drug abuse prevention. Aborig Isl Health Work J. 1987;11(1):41–4. [Google Scholar]
- 48. Fitzpatrick S; Australians for Native Title Reconciliation . Success stories in indigenous health: a showcase of successful Aboriginal and Torres Strait Islander health projects. Rozelle, NSW: Australians for Native Title Reconciliation, 2007; 2007. 35 pp. [Google Scholar]
- 49. Foley W. Family food work: lessons learned from urban Aboriginal women about nutrition promotion. Aust J Prim Health. 2010;16(3):268–74. [DOI] [PubMed] [Google Scholar]
- 50. Gamarania G, Malpraburr T, Johnston F, Beecham R, Dalgleish P. The Maningrida: 'Be Smoke Free' project. Health Promot J Austr. 1998;8(1):12–7. [Google Scholar]
- 51. Gracey M, Bridge E, Martin D, Jones T, Spargo RM, Shephard M, et al. An Aboriginal‐driven program to prevent, control and manage nutrition‐related "lifestyle" diseases including diabetes. Asia Pac J Clin Nutr. 2006;15(2):178–88. [PubMed] [Google Scholar]
- 52. Gray D, Sputore B, Walker J. Evaluation of an Aborignal health promotion program: a case study from Karalundi. Health Promot J Austr. 1998;8(1):24–8. [Google Scholar]
- 53. Hayward C, Scrine C, Venz T, Smith M. Rio Tinto Child Health Partnership: delivering improvements in Aboriginal and Torres Strait Islander child and maternal health. Perth, WA: Kulunga Research Network and Telethon Institute for Child Health Research, 2008. [Google Scholar]
- 54. Homer CS, Foureur MJ, Allende T, Pekin F, Caplice S, Catling‐Paull C. 'It's more than just having a baby' women's experiences of a maternity service for Australian Aboriginal and Torres Strait Islander families. Midwifery. 2012;28(4):E449–E455. [DOI] [PubMed] [Google Scholar]
- 55. Ivers R, Castro A, Parfitt D, Bailie RS, D'Abbs PH, Richmond RL. Evaluation of a multi‐component community tobacco intervention in three remote Australian aboriginal communities. Aust N Z J Public Health. 2006;30(2):132–6. [DOI] [PubMed] [Google Scholar]
- 56. Lee AJ, Bailey APV, Yarmirr D, O'Dea K, Mathews JD. Survival tucker: improved diet and health indicators in an Aboriginal community. Aust J Public Health. 1994;18(3):277–85. [DOI] [PubMed] [Google Scholar]
- 57. Lee AJ, Bonson APV, Yarmirr D, O'Dea K, Mathews JD. Sustainability of a successful health and nutrition program in a remote Aboriginal community. Med J Aust. 1995;162(12):632–5. [DOI] [PubMed] [Google Scholar]
- 58. Lee KSK, Dawson A, Conigrave KM. The role of an Aboriginal women's group in meeting the high needs of clients attending outpatient alcohol and other drug treatment. Drug Alcohol Rev. 2013;32(6):618–26. [DOI] [PubMed] [Google Scholar]
- 59. Longstreet D, Heath D, Savage I, Vink R, Panaretto K. Estimated nutrient intake of urban indigenous participants enrolled in a lifestyle intervention program. Nutr Diet. 2008;65(2):128–33. [Google Scholar]
- 60. Mackerras D. Birthweight changes in the pilot phase of the strong women strong babies strong culture program in the Northern Territory. Aust N Z J Public Health. 2001;25(1):34–40. [DOI] [PubMed] [Google Scholar]
- 61. Malseed C, Nelson A, Ware R. Evaluation of a school‐based health education program for urban Indigenous young people in Australia. Health. 2014;6(7):587–97. [Google Scholar]
- 62. Malseed C, Nelson A, Ware R, Lacey I, Lander K. Deadly choicestrade; community health events: a health promotion initiative for urban Aboriginal and Torres Strait Islander people. Aust J Prim Health. 2014;20(4):379–83. [DOI] [PubMed] [Google Scholar]
- 63. Mark A, McLeod I, Booker J, Ardler C. The Koori Tobacco Cessation Project. Health Promot J Austr. 2004;15(3):200–4. [Google Scholar]
- 64. Marley JV, Atkinson D, Kitaura T, Nelson C, Gray D, Metcalf S, et al. The Be Our Ally Beat Smoking (BOABS) study, a randomised controlled trial of an intensive smoking cessation intervention in a remote aboriginal Australian health care setting. BMC Public Health. 2014;14(1):32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65. Marley JV, Atkinson D, Nelson C, Kitaura T, Gray D, Metcalf S, et al. The protocol for the Be Our Ally Beat Smoking (BOABS) study, a randomised controlled trial of an intensive smoking cessation intervention in a remote Aboriginal Australian health care setting. BMC Public Health. 2012;12:232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Marley JV, Kitaura T, Atkinson D, Metcalf S, Maguire GP, Gray D. Clinical trials in a remote Aboriginal setting: lessons from the BOABS smoking cessation study. BMC Public Health. 2014;14:579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. McCalman J, Baird B, Tsey K. Indigenous men taking their rightful place ‐ how one Aboriginal community is achieving results. Aborig Isl Health Work J. 2007;31(4):8–11. [Google Scholar]
- 68. McCalman J, McEwan A, Tsey K, Blackmore E, Bainbridge R. Towards social sustainability: the case of the family wellbeing community empowerment education program. J Econ Soc Pol. 2010;13(2):211–47. [Google Scholar]
- 69. McCalman J, Tsey K, Wenitong M, Wilson A, McEwan A, James YC, et al. Indigenous mens support groups and social and emotional wellbeing: a meta‐synthesis of the evidence. Aust J Prim Health. 2010;16(2):159–66. [DOI] [PubMed] [Google Scholar]
- 70. McDermott RA, Schmidt B, Preece C, Owens V, Taylor S, Li M, et al. Community health workers improve diabetes care in remote Australian indigenous communities: results of a pragmatic cluster randomized controlled trial. BMC Health Serv Res. 2015;15(1):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. McEwan A, Tsey K; Health CRCfA . The role of spirituality in social and emotional wellbeing initiatives: the Family Wellbeing Program at Yarrabah. Casuarina, NT: Cooperative Research Centre for Aboriginal Health, 2009; 2009. Report No.: 97807340399271834–156X. [Google Scholar]
- 72. Mendham AE, Duffield R, Marino F, Coutts AJ. A 12‐week sports‐based exercise programme for inactive Indigenous Australian men improved clinical risk factors associated with type 2 diabetes mellitus. J Sci Med Sport. 2015;18:438–43. [DOI] [PubMed] [Google Scholar]
- 73. Miller K, Rowse T. CAAAPU: an evaluation. Darwin, NT: Menzies School of Health Research, 1995. [Google Scholar]
- 74. Milward K. Prevention of alcohol‐related harms in Victoria's Koori communities. Prev Res Q. 2009;2:1–26. [Google Scholar]
- 75. Mobbs R, Nguyen HT, Bell A. The chronic disease self‐management project at Katherine West Health Board Aboriginal Corporation in the Northern Territory: a report of the first year. Aust J Prim Health. 2003;9(2–3):160–7. [Google Scholar]
- 76. Moore L, Webb R, Abbott P, Zonka B. Cooking classes for diabetes: a partnership between Daruk Aboriginal Medical Service and the Western Sydney Institute of TAFE. Aborig Isl Health Work J. 2006;30(6):11–3. [Google Scholar]
- 77. Munns A. Yanan Ngurra‐ngu Walalja Halls Creek Community Families Programme. Neonatal Pediatr Child Health Nurs. 2010;13(1):18–21. [Google Scholar]
- 78. Nilson C, Kearing‐Salmon KA, Morrison P, Fetherston C. An ethnographic action research study to investigate the experiences of Bindjareb women participating in the cooking and nutrition component of an Aboriginal health promotion programme in regional Western Australia. Public Health Nutr. 2015;18:3394–405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79. Osborne S. Kulintja nganampa maa‐kunpuntjaku (strengthening our thinking): place‐based approaches to mental health and wellbeing in anangu schools. Aust J Indigenous Educ. 2013;42(2):182–93. [Google Scholar]
- 80. Parker E, Meiklejohn B, Patterson C, Edwards K, Preece C, Shuter P, et al. Our games our health: a cultural asset for promoting health in Indigenous communities. Health Promot J Austr. 2006;17(2):103–8. [DOI] [PubMed] [Google Scholar]
- 81. Payne C. A diabetes support group for Nywaigi women to enhance their capacity for maintaining physical and mental wellbeing. Contemp Nurse. 2013;46(1):41–5. [DOI] [PubMed] [Google Scholar]
- 82. Reilly R, Doyle J, Rowley K. Koori community‐directed health promotion in the Goulburn Valley. Aust Community Psychol. 2007;19(1):39–46. [Google Scholar]
- 83. Reilly RE, Cincotta M, Doyle J, Firebrace BR, Cargo M, van den Tol G, et al. A pilot study of Aboriginal health promotion from an ecological perspective. BMC Public Health. 2011;11:749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84. Rowley KG, Daniel M, Skinner K, Skinner M, White GA, O'Dea K. Effectiveness of a community‐directed 'healthy lifestyle' program in a remote Australian Aboriginal community. Aust N Z J Public Health. 2000;24(2):136–44. [DOI] [PubMed] [Google Scholar]
- 85. Rynne S, Rossi T; Australian Sports Commission, University of Queensland . The impact of Indigenous community sports programs: the case of surfing: report on findings. Canberra, ACT: Australian Sports Commission, 2012; 2012. Report No.: 9781740131223. [Google Scholar]
- 86. Sheehan M, Schonfeld C, Hindson E, Ballard R. Alcohol education in an Indigenous community school in Queensland, Australia. Drugs Educ Prev Polic. 1995;2(3):259–73. [Google Scholar]
- 87. Ski CF, Vale MJ, Bennett GR, Chalmers VL, McFarlane K, Jelinek VM, et al. Improving access and equity in reducing cardiovascular risk: The Queensland health model. Med J Aust. 2015;202(3):148–53. [DOI] [PubMed] [Google Scholar]
- 88. Smith J. Wadja Warriors football team's healthy weight program. Aborig Isl Health Work J. 2002;26(4):13–5. [Google Scholar]
- 89. Spurling G, Hayman N, Cooney A. Adult health checks for Indigenous Australians: the first year's experience from the Inala Indigenous Health Service. Med J Aust. 2009;190(10):562–4. [DOI] [PubMed] [Google Scholar]
- 90. Strempel P; Australian National Council on Drugs . Indigenous drug and alcohol projects: elements of best practice. Canberra: Australian National Council on Drugs, 2004; 2004. 92 p. [Google Scholar]
- 91. Sun J, Buys N. Effectiveness of participative community singing intervention program on promoting resilience and mental health of Aboriginal and Torres Strait Islander People in Australia In: Olisah V, editor. Essential Notes in Psychiatry. Croatia: InTech, 2002; p. 245–52. [Google Scholar]
- 92. Sun J, Buys N. Effectiveness of a participative community singing program to improve health behaviors and increase physical activity in Australian Aboriginal and Torres Strait Islander people. Int J Disabil Hum Dev. 2013;12(3):297–304. [Google Scholar]
- 93. Sun J, Buys N. Participatory community singing program to enhance quality of life and social and emotional well‐being in aboriginal and torres strait islander australians with chronic diseases. Int J Disabil Hum Dev. 2013;12(3):317–23. [Google Scholar]
- 94. Tsey K. An innovative family support program by and for Indigenous Australians: reflections in evaluation practice. J Fam Stud. 2000;6(2):302–8. [Google Scholar]
- 95. Tsey K, Every A. Evaluating Aboriginal empowerment programs: the case of Family WellBeing. Aust N Z J Public Health. 2000;24(5):509–14. [DOI] [PubMed] [Google Scholar]
- 96. Tsey K, Every A. Evaluation of an Aboriginal empowerment program. Casuarina, NT: Cooperative Research Centre for Aboriginal and Tropical Health, 2001; 2000. Report No.: 1876831065. [Google Scholar]
- 97. Tsey K, Whiteside M, Daly S, Deemal A, Gibson T, Cadet‐James Y, et al. Adapting the 'Family Wellbeing' empowerment program to the needs of remote Indigenous school children. Aust N Z J Public Health. 2005;29(2):112–6. [DOI] [PubMed] [Google Scholar]
- 98. Vale MJ, Jelinek MV, Best JD, Dart AM, Grigg LE, Hare DL, et al. Coaching patients on achieving cardiovascular health (coach): A multicenter randomized trial in patients with coronary heart disease. Arch Intern Med. 2003;163(22):2775–83. [DOI] [PubMed] [Google Scholar]
- 99. Vale MJ, Jelinek MV, Best JD, Santamaria JD. Coaching patients with coronary heart disease to achieve the target cholesterol. J Clin Epidemiol. 2002;55(3):245–52. [DOI] [PubMed] [Google Scholar]
- 100. Viola A. Evaluation of the Outreach School Garden Project: building the capacity of two Indigenous remote school communities to integrate nutrition into the core school curriculum. Health Promot J Austr. 2006;17(3):233–9. [DOI] [PubMed] [Google Scholar]
- 101. Strempel P, Saggers S, Gray D, Stearne A. WuChopperen Health Service Ltd: drugs, alcohol and other substances program In: Strempel P, Saggers S, Gray D, Stearne A, editors. Indigenous drug and alcohol projects: elements of best practice. Canberra, ACT: Australian National Council on Drugs, 2004; p. 35–42. [Google Scholar]
- 102. Fitzpatrick S; Australians for Native Title Reconciliation . Nutrition: at the heart of good health: Jalaris Aboriginal Corporation. Success stories in Indigenous health: a showcase of successful Aboriginal and Torres Strait Islander health projects. Rozelle, NSW: Australians for Native Title Reconciliation; 2007. p. 10–1. [Google Scholar]
- 103. Fitzpatrick S; Australians for Native Title Reconciliation . Good Food, Great Kids: Yarra Valley Community Health Service. Success stories in Indigenous health: a showcase of successful Aboriginal and Torres Strait Islander health projects. Rozelle, NSW: Australians for Native Title Reconciliation; 2007. p. 12–3. [Google Scholar]
- 104. Aboriginal Health Medical Research Council of New South Wales . Cooking Classes for Diabetes Program. 10 out of 10 Deadly Health Stories: Nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales; 2009. p. 7–10. [Google Scholar]
- 105. Aboriginal Health Medical Research Council of New South Wales . Healthy Lifestyle and Weight Management Program: Awabakal Aboriginal Medical Service, Newcastle. 10 out of 10 Deadly Health Stories: Nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales, 2009. p. 10–3. [Google Scholar]
- 106. Aboriginal Health Medical Research Council of New South Wales . Community Kitchen Program and ‘Koori Walkabout’: Tharawal Aboriginal Medical Service, Campbelltown. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales; 2009. p. 36–41. [Google Scholar]
- 107. Aboriginal Health Medical Research Council of New South Wales . Healthy Food Awareness Program: Dharah Gibinj Aboriginal Medical Service, Casino. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales, 2009. p. 22–5. [Google Scholar]
- 108. Aboriginal health Medical Research Council of New South Wales . Fruit and Vegetable Program and Market Garden: Bulgarr Ngaru Aboriginal Medical Service, Grafton. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal health Medical Research Council of New South Wales, 2009. p. 14–7. [Google Scholar]
- 109. Aboriginal Health Medical Research Council of New South Wales . Spring into Shape Program: Galambila Aboriginal Health Service, Coffs Harbour. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales, 2009. p. 26–7. [Google Scholar]
- 110. Aboriginal Health Medical Research Council of New South Wales . Community Kitchens Program and Water Aerobics Program: Pius X Aboriginal Medical Service, Moree. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal health Medical Research Council of New South Wales, 2009. p. 34–5. [Google Scholar]
- 111. Aboriginal Health Medical Research Council of New South Wales . Healthy Lifestyle Program: Griffith Aboriginal Medical Service. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales, 2009. p. 28–9. [Google Scholar]
- 112. Aboriginal Health Medical Research Council of New South Wales . Building Healthy Communities Project: Murrin Bridge Aboriginal Health Service. 10 out of 10 Deadly Health Stories: nutrition and physical activity: successful programs from NSW Aboriginal Community Controlled Health Services. Surry Hills, NSW: Aboriginal Health Medical Research Council of New South Wales, 2009. p. 30–3. [Google Scholar]
- 113. McDermott R, Tulip F, Schmidt B, Sinha A. Sustaining better diabetes care in remote Indigenous Australian communities. BMJ. 2003;32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114. Oolong Houses . Sharing and caring. Nowra, NSW: Oolong Houses; 1981. [Google Scholar]
- 115. d'Abbs P, Togni S, Rosewarne C, Boffa J. The Grog Mob: lessons from an evaluation of a multi‐disciplinary alcohol intervention for Aboriginal clients. Aust N Z J Public Health. 2013;37(5):450–6. [DOI] [PubMed] [Google Scholar]
- 116. Mikhailovich K, Morrison PA, Arabena K. Evaluating Australian Indigenous community health promotion initiatives: a selective review. Rural Remote Health. 2007;7:746. [PubMed] [Google Scholar]
- 117. Clifford A, Pulver LJ, Richmond R, Shakeshaft A, Ivers R. Smoking, nutrition, alcohol and physical activity interventions targeting Indigenous Australians: rigorous evaluations and new directions needed. Aust N Z J Public Health. 2011;35(1):38–46. [DOI] [PubMed] [Google Scholar]
- 118. Australian Institute of Health and Welfare . Primary Health Care in Australia. Australia's Health 2014. Cat. no. AUS 178. Canberra, Australia: AIHW, 2014. [Google Scholar]
- 119. World Health Organization . The Ottawa Charter for Health Promotion: World Health Organization; 1986. [cited 2016]. Available from: http://www.who.int/healthpromotion/conferences/previous/ottawa/en/index1.html
- 120. National Aboriginal Community Controlled Health Organisation . About NACCHO 2016 [cited 2017]. Available from: http://www.naccho.org.au/about/
- 121. HealthInfoNet AI . Summary of developments in Indigenous health promotion 2005 [cited 2017]. Available from: http://www.healthinfonet.ecu.edu.au/health-systems/health-promotion/reviews/our-review
- 122. McCalman J, Tsey K, Bainbridge R, Rowley K, Percival N, O'Donoghue L, et al. The characteristics, implementation and effects of Aboriginal and Torres Strait Islander health promotion tools: a systematic literature search. BMC Public Health. 2014;14(1):712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123. Department of Health . Implementation Plan for the National Aboriginal and Torres Strait islander Health Plan 2013–2023 [cited 2019]. Available from: https://www1.health.gov.au/internet/main/publishing.nsf/Content/AC51639D3C8CD4ECCA257E8B00007AC5/$File/DOH_ImplementationPlan_v3.pdf
- 124. Productivity Commission . Indigenous Evaluation Strategy: Productivity Commission Issues Paper June 2019. [cited 2019] Available from: https://www.pc.gov.au/inquiries/current/indigenous-evaluation/issues/indigenous-evaluation-issues.pdf


