Abstract
Background
Individualizing goals for people with type 2 diabetes may result in deintensification of medication, but a comprehensive picture of deprescribing practices is lacking.
Aims
To conduct a scoping review in order to assess the rates, determinants and success of implementing deprescribing of glucose‐, blood pressure‐ or lipid‐lowering medications in people with diabetes.
Methods
A systematic search on MEDLINE and Embase between January 2007 and January 2019 was carried out for deprescribing studies among people with diabetes. Outcomes were rates of deprescribing related to participant characteristics, the determinants and success of deprescribing, and its implementation. Critical appraisal was conducted using predefined tools.
Results
Fourteen studies were included; eight reported on rates, nine on determinants and six on success and implementation. Bias was high for studies on success of deprescribing. Deprescribing rates ranged from 14% to 27% in older people with low HbA1c levels, and from 16% to 19% in older people with low systolic blood pressure. Rates were not much affected by age, gender, frailty or life expectancy. Rates were higher when a reminder system was used to identify people with hypoglycaemia, which led to less overtreatment and fewer hypoglycaemic events. Most healthcare professionals accepted the concept of deprescribing but differed on when to conduct it. Deprescribing glucose‐lowering medications could be successfully conducted in 62% to 75% of participants with small rises in HbA1c.
Conclusions
Deprescribing of glucose‐lowering medications seems feasible and acceptable, but was not widely implemented in the covered period. Support systems may enhance deprescribing. More studies on deprescribing blood pressure‐ and lipid‐lowering medications in people with diabetes are needed.
What's new?
Potential overtreatment is common among older people with diabetes.
Deprescribing has gained attention in the past decade but may be difficult to implement.
Deprescribing was uncommon in potentially overtreated people with diabetes up to 2017.
Deprescribing rates were marginally influenced by comorbidity or frailty.
Healthcare professionals accepted the concept of deprescribing in diabetes.
Decision‐support tools can increase deprescribing and decrease hypoglycaemia.
Little is known about deprescribing of blood pressure‐ or lipid‐lowering medications in people with diabetes.
Healthcare professionals need additional support and guidance to enhance deprescribing in people with diabetes.
1. INTRODUCTION
Deprescribing is the planned process of reducing or stopping medication, supervised by a healthcare professional (HCP), in order to improve patient outcomes. 1 This approach has emerged in the past decade from evidence of the adverse effects of polypharmacy and inappropriate drug use. 2 Polypharmacy and potential overtreatment are major problems in people with type 2 diabetes. 3 Such individuals often receive intensive treatment of glucose‐, blood pressure‐, and lipid‐lowering medications to prevent complications. However, in older people, the benefits of intensive glucose and cardiovascular risk factor control are uncertain because of increased risks of hypoglycaemia, hypotension and mortality. 4 , 5 Treatment guidelines have therefore shifted to a more personalized approach, where treatment goals may depend on an individual's characteristics and preferences. 6 This may result in less intensive treatment in older and frail people with any type of diabetes. 7 , 8 , 9 , 10 To date, there is limited evidence regarding the benefits and risks of deprescribing in people with diabetes. 11 , 12 , 13
Potential overtreatment appears to be common among older people with diabetes, and deprescribing may be difficult to implement in practice. 12 , 14 , 15 , 16 Clinical guidelines for the treatment of diabetes and cardiovascular risk factors focus more on intensification than on deintensification of medications. 17 Guidelines often do not provide clear recommendations on when or how to deintensify medication. 18 In 2017, a guideline on deprescribing anti‐hyperglycaemic agents in older individuals was published, including an algorithm with recommendations on when and how to deprescribe. 19 In 2018, a UK stakeholder initiative also presented more specific guidance on deintensification thresholds for glucose‐lowering medication. 20 In the same year, the American College of Physicians issued a guidance statement that clinicians should consider deprescribing in all people with type 2 diabetes who achieve HbA1c levels below 48 mmol/mol (6.5%). 7 Recently, several deprescribing networks and organizations around the world have started to support deprescribing in clinical practice. 21
To develop programmes for enhancing deprescribing in people with type 2 diabetes, we need to know more about the process and implementation of deprescribing. The main aim of the present scoping review was to generate an overview of what is known about the deprescribing rates in relation to participant characteristics, and the determinants and success of deprescribing and of interventions to implement deprescribing of glucose‐, blood pressure‐ and/or lipid‐lowering medications in people with diabetes.
2. METHODS
2.1. Design and reporting
We conducted a scoping review to obtain a broad view on the available information and evidence by including a wide range of study designs, outcomes and populations. 22 The Preferred Reporting Items for Systematic Reviews and Meta‐Analyses extension for Scoping Reviews (PRISMA‐ScR) guideline and checklist was used for the search process and to guide reporting (Appendix S1). 23
2.2. Information search and data sources
A search for relevant articles in the past decade was conducted in Embase and MEDLINE for the period from 1 January 2007 to 1 January 2019. A combination of search terms for deprescribing (e.g. ‘deprescribe’, ‘deintensify’, ‘discontinue’, ‘withdrawal’) and diabetes mellitus (e.g. ‘diabetes mellitus’, ‘impaired glucose tolerance’) were used (Appendix S2). There was no restriction in our initial search on type of medication. Reference lists from included articles were screened to identify additional articles. This ‘snowballing’ approach was used because previous work showed that it is difficult to develop a sensitive search strategy for this topic. 24
2.3. Eligibility criteria
2.3.1. Definition of deprescribing
There is no internationally accepted definition of deprescribing. Based on the review by Reeve et al., 1 deprescribing was defined as the planned process of (1) dosage decrease, (2) stepping down, or (3) withdrawal of medication without dosage increase, switching to an equivalent agent, or stepping up or addition of another agent, where the goal is to reduce the risk of harm and improve outcomes within the context of an individual's goals and preferences. Deprescribing is thus a proactive process of medication deintensification.
2.3.2. Included studies
The present scoping review considered studies that evaluated some aspect of the process of deprescribing of glucose‐, blood pressure‐ and/or lipid‐lowering medications in people with type 2 diabetes. Studies related to people with type 2 diabetes as well as people with any type of diabetes were included as the majority will concern type 2 diabetes. Given the aim of the present study, studies in people with diabetes focusing on (1) inappropriate medication in general, (2) improving adherence or (3) reacting to acute drug‐related problems were excluded. Additionally, studies on medication changes related to end‐of‐life in people with diabetes were excluded. Experimental studies, observational studies, surveys, as well as qualitative and mixed‐method studies, were eligible for inclusion. Reviews, comments, study protocols, opinions and editorials were excluded. In the process of title and abstract screening, articles in languages other than English, Dutch, German and French were not reviewed.
2.3.3. Main outcomes
Outcomes included: (1) rates of deprescribing in relation to participants’ characteristics (e.g. HbA1c or systolic blood presure, age, comorbidity); (2) determinants associated with the process of deprescribing (e.g. barriers and enablers from the perspectives of individuals with diabetes and healthcare professionals); (3) success of deprescribing; and (4) success of interventions to implement deprescribing in people with diabetes. Notably, the outcomes retrieved for this review are not necessarily the primary outcomes as defined by the authors of the included studies.
2.4. Selection of sources of evidence and data extraction
Two authors (M.P.O., K.P.K.) developed the search strategy, and independently screened titles and abstracts. A third author (P.D.) checked all potentially relevant records. Additionally, P.D. checked a quarter of the excluded records, confirming that no potentially relevant records had been missed. Potentially eligible articles were retrieved as full texts and examined for final inclusion by two authors (M.P.O., P.D.). Cohen's kappa statistic was calculated to assess inter‐rater agreement between authors for the title‐abstract screening and for the full‐text screening. Disagreements were resolved by discussion between the authors (M.P.O., P.D., K.P.K.) to reach consensus. Two authors (M.P.O., P.D.) independently extracted the following information on a data extraction form: research questions according to the defined outcomes; study design; study period; country in which the study was conducted; participants; setting; methods and instruments used; determinants or interventions; definition of outcomes; statistical analysis; and results (Appendix S3).
2.5. Synthesis of results and critical appraisal
A narrative and descriptive synthesis of the results was conducted as the included studies were heterogeneous with regard to research questions, study design, analysis and outcomes. Critical appraisal of the included studies was conducted by assessing the risk of bias. This was done by two authors (M.P.O., P.D.) using the National Heart, Lung and Blood Institute [National Insitute of Health (NIH)] tool for observational cohort and cross‐sectional studies, the NIH tool for before‐and‐after studies with no control group, 25 and the domain‐based risk‐of‐bias tool for cross‐sectional survey studies. 26 These tools were slightly modified to cover the following domains for all study designs where possible: selection of participants; exposure measurement; outcome measurement; incomplete data; analysis; and sample size. All assessments were categorized as low, uncertain or high risk of bias (Appendix S4).
3. RESULTS
Fourteen articles were included in this scoping review (Figure 1). Agreement between reviewers (M.P.O. and K.K.) for title/abstract screening was 98.7%, with a kappa value of 0.44, mainly driven by larger inclusion of potential papers by one of the reviewers. All potentially relevant papers indicated by either one of the reviewers were screened by a third reviewer (P.D.). The agreement for the full‐text screening was 97.7%, with a kappa value of 0.90.
FIGURE 1.
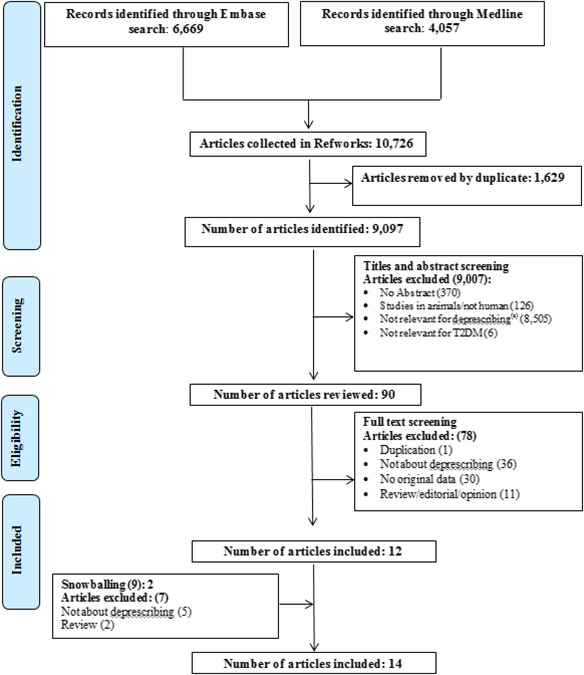
PRISMA flow diagram of identified studies. (a) For example, studies focusing on efficacy/safety of medication, inappropriate medication in general, improving adherence, or reducing drug‐related problems
3.1. Study characteristics and bias
The majority of the studies were conducted in the USA (Table 1). 15 , 38 The study periods covered ranged from 2001 to 2017. Study methodologies comprised retrospective cohort studies, 15 , 16 , 27 , 28 , 29 , 30 , 31 prospective cohort or before‐and‐after studies, 32 , 33 , 34 , 35 , 36 and surveys. 37 , 38
TABLE 1.
Characteristics of included studies (structured by main outcome)
| No | Author (year) | Main outcome for review | Country/setting | Study period | Study design | Methods used (database, instrument, intervention) | Diabetes population | Sample size | Risk of bias | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | McCoy et al. (2016) 16 | Rates | USA | 2001–2013 | Retrospective cohort study | Claims database including private and Medicare plans (OptumLabs Data Warehouse) | People with type 2 diabetes aged >18 years | 6653 participants | Uncertain | ||
| 2 | Yotsapon et al. (2016) 31 | Rates | Thailand, 1 hospital | 2014–2015 | Retrospective cohort study | Medical records | People with type 2 diabetes aged >85 years | 125 participants | High | ||
| 3 | Maciejewski et al. (2018) 27 | Rates and determinants | USA, 10 Eastern states | 2010–2011 | Retrospective cohort study | Claims database (Medicare patients) | People with diabetes aged ≥65 years (no clear exclusion type 1) | 8560 participants | Low | ||
| 4 | McAlister et al. (2018) 29 | Rates and determinants | United Kingdom, primary care | 2003–2015 | Retrospective cohort study | Electronic medical records database [The Health Improvement Network (THIN)] |
People with diabetes aged ≥20 years (no clear exclusion type 1). |
154 691 participants (HbA1c cohort), 187 852 (blood pressure cohort) |
Low | ||
| 5 | McAlister et al. (2017) 28 | Rates and determinants | USA | 2004–2010 | Retrospective cohort study | Clinical database with inpatient and outpatient data for commercially insured patients outside Veteran Affairs System (Clinformatics Data Mart Database) | People with diabetes aged ≥20 years (no clear exclusion type 1) | 99 694 participants | Low | ||
| 6 | Sussman et al. (2015) 15 | Rates and determinants | USA, primary care veterans | 2012 | Retrospective cohort study | Veteran Affairs database (Corporate Data Warehouse) | People with type 1 or type 2 diabetes aged >70 years |
179 991 participants (HbA1c cohort), 211 667 (blood pressure cohort) |
Low | ||
| 7 | Vimalananda et al. (2017) 32 | Rates and success of implementation | USA, 8 veteran affairs systems | 2013–2014 | Prospective cohort study, before‐and‐after comparison | Intervention using a clinical alerting system developed by VANEHS Clinical Informatics; the system includes a tool for collecting data from patients and process outcomes with prespecified questions | People with diabetes aged >74 years | 2830 screened participants; potential overtreatment: 2465 people | Uncertain | ||
| 8 | Wright et al. (2018) 30 | Rates and success of implementation | USA, 7 veterans medical centers and outpatient clinics | 2012–2017 | Retrospective dynamic cohort study, before‐and‐after comparison | Intervention using a clinical alerting system linked to the electronic medical records of the Veterans Health Administration (VHA); the system includes a tool for collecting data from patients and process outcomes with prespecified questions | People with diabetes aged ≥75 years | 8495 participants; deprescribing cohort: 395 participants | Uncertain | ||
| 9 | Sjoblom et al. (2008) 34 | Success of deprescribing | Sweden, 17 nursing homes in 2 counties | 2006 | Prospective cohort study, before‐and‐after comparison | Intervention (withdrawal study) | Type 2 diabetes people, mean age 84 years (range 58–100) | 32 participants | High | ||
| 10 | Masumoto et al. (2017) 36 | Determinants, and success of deprescribing | Japan, hospital | ‐ | Prospective cohort study, before‐and‐after comparison | Intervention (withdrawal study) in clinical practice | Adults with type 2 diabetes (no age limit in the inclusion criteria) | 16 participants | High | ||
| 11 | Abdelhafiz et al. (2014) 33 | Determinants and success of deprescribing | United Kingdom, 1 outpatient clinic | ‐ | Before‐and‐after comparison, retrospective study | Not specified | People with diabetes ≥75 (no clear exclusion type 1) | 8 participants | High | ||
| 12 | Vischer et al. (2010) 35 | Determinants and success of implementation | Switzerland, 1 geriatric hospital | ‐ | Prospective cohort study | Review of diabetes medication during consultation, where oral glucose‐lowering medication was withdrawn in patients with fasting blood glucose <7.5 mmol ⁄ l and an HbA1c <58 mmol ⁄mol (7.5%) | People with diabetes aged >65 years (no clear exclusion type 1) | 89 participants | High | ||
| 13 | Genere et al. (2016) 38 | Determinants | USA, 1 academic medical center and 1 suburban healthcare system | 2015 | Cross‐sectional survey study | Survey questionnaire about self‐reported practice of initiating conversations about deprescribing of glucose‐lowering medication | Adults with type 2 diabetes (no age limit) | 156 physicians | Uncertain | ||
| 14 | Caverly et al. (2015) 37 | Determinants | USA, Veterans Affairs | 2014 | Cross‐sectional survey study | Survey questionnaire including hypothetical patients at high risk of hypoglycaemia | People with type 2 diabetes aged 77 years (as hypothetical cases) | 594 physicians | Uncertain | ||
The studies looking at participant characteristics associated with deprescribing rates had a low risk of bias (Figure 2). 15 , 27 , 28 , 29 The studies looking at participant characteristics associated with successful deprescribing and those reporting on the success of deprescribing had a high risk of bias. 33 , 34 , 36 Those studies also included very small sample sizes. Finally, the studies reporting on the success of interventions to enhance deprescribing had an uncertain to high risk of bias. 30 , 32 , 35
FIGURE 2.
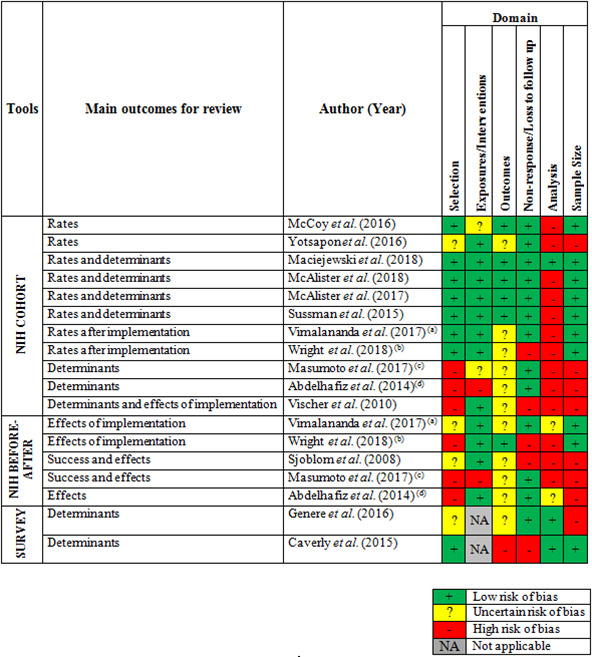
Risk‐of‐bias summary. (a) Vimalananda et al. and (b) Wright et al. had two outcomes related with the study objectives: (1) the rates after implementation of the deprescribing programme in the cohort and (2) the success of the implementation programme. (c) Masumoto et al. and (d) Abdelhafiz et al. had two outcomes related with the study objectives: (1) the determinants related to successful deprescribing in the cohort and (2) the success of deprescribing
3.2. Deprescribing rates
Six studies reported on rates of deprescribing glucose‐lowering medications, 15 , 16 , 27 , 28 , 29 , 31 including two studies that also provided deprescribing rates of blood pressure‐lowering medications. 15 , 29 No study reported deprescribing rates of lipid‐lowering medication in people with diabetes. Three studies included only adults with diabetes 16 , 28 , 29 , whereas the other studies included only older people, aged ≥65 years, 27 >70 years, 15 and >85 years. 31 Studies looked at different time windows for assessing deprescribing rates, ranging from 120 to 180 days after the index HbA1c or systolic blood pressure measurement.
3.2.1. Deprescribing glucose‐lowering medications and participant characteristics
Deprescribing rates among eligible adults ranged from 21% to 45% for very low HbA1c levels <42 mmol/mol (<6.0%), and similar rates were seen for higher HbA1c levels (Figure 3a). 16 , 28 , 29 Among older people, the rates ranged from 20% to 27% for HbA1c levels <42 mmol/mol (<6.0%), and from 14% to 21% for HbA1c levels between 42 and 48 mmol/mol (6.0–6.5%; Figure 3b), 15 , 27 , 31 whereas this was 6% for HbA1c levels >64 mmol/mol (>8.0%). 31 There were some indications that deprescribing occurred more often in people with more comorbidities or lower life expectancy. 27 , 33 The rates, however, differed by less than five percentage points for people with different levels of clinical complexity, 16 age, gender or race, 27 frailty, 28 , 29 or life expectancy 15 (Appendix S3: Table A). The association between the HbA1c levels and deprescribing was not significantly modified by health status or lower life expectancy. 15 , 28 , 29 The three low‐quality studies looking at participants’ characteristics associated with successful deprescribing showed no consistent results (Appendix S3: Table B). 33 , 35 , 36
FIGURE 3.
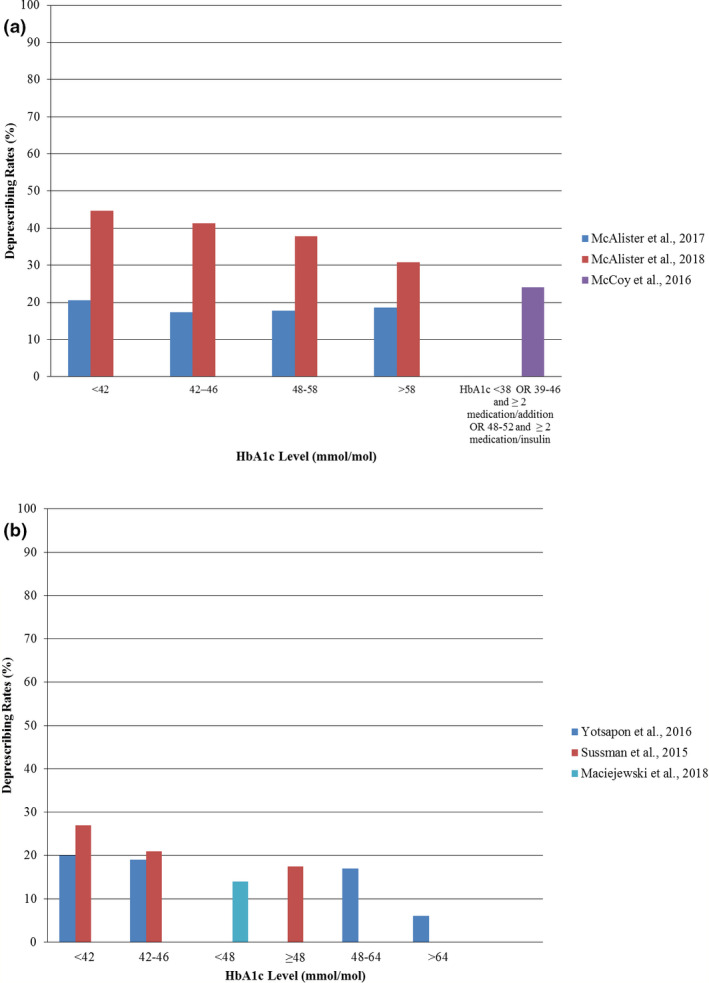
(a) Deprescribing rates among adults according to their index HbA1c level. (b) Deprescribing rates among older people according to their index HbA1c level. HbA1c values are given in International Federation of Clinical Chemistry and Laboratory Medicine (IFCC) units (mmol/mol); conversion to Diabetes Control and Complications Trial (DCCT) units (%) is as follows: 38 mmol/mol = 5.6%, 39 mmol/mol = 5.7%, 42 mmol/mol = 6%, 46 mmol/mol = 6.4%, 48 mmol/mol = 6.5%, 52 mmol/mol = 6.9%, 58 mmol/mol = 7.5%, 64 mmol/mol = 8%
3.2.2. Deprescribing blood pressure‐lowering medications and participant characteristics
The deprescribing rate among eligible adults ranged from 40% for systolic blood pressure levels <120 mmHg to 34% for levels >140 mmHg (Appendix S3: Table A). 29 Among older people with very low (<120 mmHg) to low (120–129 mmHg) blood pressure levels, the rates were 19% and 16%, whereas this rate was 15% for higher blood pressure levels. 15 There was a weak association between life expectancy and deprescribing. 15 Rates differed by three to eight percentage points for people with different levels of frailty, 29 or life expectancy. 15 The association between systolic blood pressure levels and deprescribing was not significantly modified by health status 15 , 29 (Appendix S3: Table B).
3.3. Barriers and enablers for deprescribing
No studies exploring barriers and enablers for deprescribing cardiometabolic medication from the perspectives of the individuals with diabetes were found. Two survey studies looked into the beliefs and perspectives of HCPs regarding deprescribing of glucose‐lowering medications. 37 , 38 The concept of deprescribing for people with diabetes was well accepted, although HCPs had different opinions on the HbA1c threshold at which they would initiate conversations about deprescribing. Other patient‐related factors that could lead to deprescribing according to most HCPs were medication side effects, limited life expectancy, or polypharmacy. 38 Beliefs about treatment benefits and concerns about vulnerability for malpractice claims were barriers for deprescribing 37 . The majority of HCPs believed that clinical decision‐support tools and patient education materials would be helpful to support the process of deprescribing. 37
3.4. Success of deprescribing
In a small study in 32 nursing home residents with an HbA1c level of 42 mmol/mol (6.0%) or lower, deprescribing was successful in 24 of them. 34 After successful withdrawal of oral glucose‐lowering medications or reduced insulin, a slight increase in HbA1c level from 33 to 40 mmol/mol (5.2 to 5.8%) was seen. In another study, withdrawal of all glucose‐lowering medications was conducted in eight older participants with no significant change between baseline HbA1c of 44 mmol/mol (6.2%) and 1‐year follow‐up HbA1c of 48 mmol/mol (6.5%). 33 In a third study, including 16 eligible adults with stable HbA1c levels below 53 mmol/mol (7.0%), successful discontinuation was possible in 10 participants (62%), showing no significant changes between baseline HbA1c of 44 mmol/mol and 12‐week HbA1c of 44 mmol/mol (6.2%). 36
Hypoglycaemia occurrence reduced significantly in a group of older people who had a self‐reported risk of hypoglycaemia after deprescribing of glucose‐lowering medications (n = 395) compared to those with no change in treatment (n = 387). 30
3.5. Success of interventions to enhance deprescribing
Three studies evaluated the success of deprescribing implementation programmes (Appendix S3: Table C). 30 , 32 , 35 A reminder system, linked to the electronic medical records, to stimulate deprescribing glucose‐lowering medication in older people with HbA1c levels <53 mmol/mol (<7.0%) resulted in a deprescribing rate of 26%. 30 A similar reminder system that was combined with a shared decision‐making programme resulted in a deprescribing rate of 37%. 32 Those rates were higher among people with fear or symptoms of hypoglycaemia (51–57%), or with severe or frequent hypoglycaemia (62–95%). 30 , 32 There was a significant absolute reduction in the percentage of potentially overtreated people by 22% after 18 months. 32 There was a reduction in percentages of people at high risk of hypoglycaemia with an HbA1c <53 mmol/mol (<7.0%) from 35.7% to 28.4%, and similar relative reductions for people with an HbA1c <48 mmol/mol (<6.5%). 30 Finally, a complete withdrawal of glucose‐lowering medications was attempted as part of a medication review during hospitalization among 70 older people with diabetes, resulting in 58 people (65%) with good glycaemic control who received no medication at discharge. 35
4. DISCUSSION
Deprescribing rates for glucose‐ and blood pressure‐lowering medications in older people of at least 65 years of age with diabetes were rather low, ranging from 14% to 27% for deprescribing of glucose‐lowering medication in older people with HbA1c levels <48 mmol/mol (<6.5%), and from 16% to 19% for deprescribing of blood pressure‐lowering medication in older people with systolic blood pressure levels <130 mmHg. Deprescribing was somewhat more likely in people with high comorbidity or lower life expectancy, even though the rates remained quite low in such individuals. HCPs accepted the concept of deprescribing in people with diabetes, but differed in opinion regarding when to conduct deprescribing. Deprescribing of glucose‐lowering medications occurred more often when a clinical reminder system was applied to identify potentially overtreated older people. Such a reminder programme appeared to reduce overtreatment and hypoglycaemic events. Deprescribing of glucose‐lowering medications seemed possible in people with stable or tight glycaemic control without large increases in HbA1c, but better‐quality studies are needed to draw firm conclusions. Little is known about deprescribing of blood pressure‐ and lipid‐lowering medications in people with diabetes.
Proactive medication deintensification in older people with diabetes and low risk factor levels needs more attention, given the low deprescribing rates observed. In older people with high HbA1c levels of more than 64 mmol/mol (8.0%), the rate of deprescribing was 6%, indicating that minimal deintensification will occur also in people with poorly controlled diabetes. To our surprise, there was little variation in deprescribing rates according to participant characteristics, such as age or comorbidity. There may be several explanations for the observed low rates of deprescribing in people with diabetes. During the studied period, HCPs may have received little guidance on when and how to conduct deprescribing. Moreover, few of the recommendations to deintensify treatment are based on strong evidence. 4 , 17 Strong evidence usually relies on randomized clinical trials (RCTs), but this scoping review confirms findings from previous reviews that RCTs evaluating the benefits and harms of deprescribing are still lacking. 11 , 12 , 13 Based on limited evidence, the conclusion remains that deprescribing of glucose‐lowering medications without substantial deterioration of glycaemic control seems feasible. Notably, marginal increases in HbA1c, such as from 33 to 40 mmol/mol (5.2% to 5.8%), 34 could be considered a failure of sufficient deprescribing if an individual was still on glucose‐lowering medication. No evidence was found regarding the benefits or harms of deprescribing blood pressure‐ or lipid‐lowering medication in people with diabetes. Recently, it was concluded that, for older people with diabetes in general, there is insufficient evidence to make firm conclusions about any positive or negative effects of discontinuing blood pressure‐lowering drugs. 39
Eligibility criteria for deprescribing varied among the studies but usually included HbA1c or systolic blood pressure levels below a certain level and/or being at high risk of adverse events. There is still debate about the eligibility criteria for deprescribing. 40 Successful deprescribing in terms of benefits and harms is likely to depend on these criteria. Several low‐quality studies showed that successful deprescribing of glucose‐lowering medications was possible in 62% to 75% of older people with low and/or stable HbA1c levels 33 , 34 , 36 ; however, those studies involved people in nursing home or clinical settings. There is a great need for large high‐quality studies in primary care settings assessing the success in terms of benefits and harms. People with a high risk of hypoglycaemia are more likely to benefit from deprescribing glucose‐lowering drugs. The present review showed that supportive strategies for deprescribing in such people may reduce overtreatment and hypoglycaemic events. 30 , 32
In general, the concept of deprescribing glucose‐lowering medications was well accepted among HCPs, although they had different opinions on when and how to deprescribe. 37 , 38 Many would initiate deprescribing in people experiencing adverse effects, but there was less agreement on other criteria, including the HbA1c level below which they would consider deprescribing. 37 , 38 Both intrinsic factors, such as knowledge and attitudes, and extrinsic factors, such as the individual's condition and aspects of the healthcare system, may influence the HCPs’ decisions to deprescribe. This is in line with barriers and enablers that have been identified for deprescribing in general. 41
No studies assessing the perspectives of people with diabetes on deprescribing were identified. This is surprising because it has been acknowledged that individuals’ beliefs and preferences are important when considering deprescribing 41 , 42 . In general, people with diabetes seem to be willing to reduce their medication if their physician says it is possible and appropriate. 42 It is not clear whether this also holds for specific medication used by people with diabetes. HCPs may experience uncertainty about the outcomes when deprescribing such medication, and worries about negative consequences appear to inhibit deprescribing. 37 , 43 Furthermore, no studies looking at impact of deprescribing on quality of life or patient‐reported treatment satisfaction or in terms of cost reduction were found.
Additional efforts are needed to enhance deprescribing in people with type 2 diabetes. Clinical decision‐support tools, as well as patient education materials, may be of help to support the implementation of deprescribing. 30 , 32 , 37 A recent study showed that the use of evidence‐based guidelines supported with algorithms for deprescribing proton pump inhibitors, benzodiazepine receptor agonists and antipsychotic drug classes increased HCPs’ self‐efficacy in implementing a plan to reduce or discontinue such medication. 44 So far, most initiatives for people with diabetes have focused on deprescribing of glucose‐lowering medication. More attention is needed for deprescribing of blood pressure‐ and lipid‐lowering medication. Importantly, the focus should shift from conducting deprescribing mainly in people who experience side effects to a more proactive approach of reducing overtreatment, particularly in comorbid or frail people with diabetes. For this, alerting systems identifying such individuals can be of help. 32 This requires further implementation of detecting frailty in primary care. Recently, a frailty assessment pathway was proposed which could be incorporated in the diabetes care systems. 45 Furthermore, setting individualized treatment targets resulting in shared decisions about deprescribing requires education and involvement. 30 Informed people with diabetes and HCPs with sufficient communication skills are the basis of successful shared decision‐making.
In addition, more evidence about the benefits and harms of deprescribing is needed. To measure the impact of deprescribing glucose‐, blood pressure‐ or lipid‐lowering medications, one should not only focus on control of the specific risk factor, such as HbA1c. One of the aims of deprescribing may be less stringent risk factor control, and thus an increase in the risk factor level. Core outcome sets have been developed for trials of medication reviews and improving appropriateness of polypharmacy in older people, 46 , 47 which are also relevant for deprescribing. Meaningful patient outcomes for studying the success of deprescribing include sufficient disease control without adverse effects, better quality of life, and reduction of medication burden and regimen complexity. Finally, studies are needed to assess the cost‐effectiveness of deprescribing interventions.
This scoping review used a broad search strategy, focusing on deprescribing of glucose‐, blood pressure‐ or lipid‐lowering medications in people with diabetes, including studies on interventions to enhance deprescribing and studies on determinants associated with deprescribing and its implementation. Thus, studies that were not identified in previous reviews were included. 11 , 12 , 13 All review steps were conducted by two people, and risk of bias was assessed.
Some limitations should be mentioned. First, our search ended in 2019 and included studies with data up to 2017. It is possible that rates of deprescribing have increased in more recent years, although we observed no trends towards more deprescribing in older people with diabetes over time. A recent study in 23 participants aged ≥75 years, who had an HbA1c ≤53 mmol/mol (≤7%) with documented hypoglycaemia and were treated with a sulfonylurea or with insulin showed that deintensification of treatment still did not occur in more than half the cases. 48 Second, the retrieved outcomes were not necessarily the primary outcomes as defined by the authors of the included studies. In some cases, it was difficult to extract the numbers needed for the outcomes, because they were not clearly reported. Third, given the definition of deprescribing, studies where medication was just simplified or switched or discontinued because of contraindications were excluded. For this reason, the study by Aspinall et al., 49 which was included in previous reviews, was excluded because it evaluated discontinuation of glyburide in participants with renal impairment, advising that an alternative agent, such as glipizide, be considered. Inclusion of this study would not have changed the conclusions. Also, we did not focus on stopping medication at the end of life, because other considerations, such as a general wish to continue only palliative medication, become relevant at that stage. None of the articles included for full‐text screening, however, were excluded for this reason. A recent study observed that end‐of‐life status may increase the likelihood of deprescribing glucose‐lowering medications in nursing homes. 50 Finally, the quality of many of the included studies was poor. When interpreting the results, this was taken into account.
In conclusion, deprescribing rates in people with diabetes were low to moderate and only marginally influenced by participants’ comorbidity or frailty. The concept of deprescribing glucose‐lowering medication in people with diabetes is supported, although its implementation in practice appears to be challenging and primarily focused on people experiencing drug‐related problems. Deprescribing to reduce drug burden or to prevent future adverse events in vulnerable people is not yet common practice. To develop and implement plans for deprescribing in a broader range of people with diabetes, clinical decision‐support tools and education materials could be useful. Evidence on the benefits and risks of deprescribing is poor and further attention should be paid to the effects on patient‐relevant outcomes and costs. More research is also needed about deprescribing of blood pressure‐ and lipid‐lowering medications in people with diabetes.
COMPETING INTERESTS
K.P.K., E.H. and P.D. have nothing to disclose. M.P.O. reports a scholarship from the Indonesia Endowment Fund for Education (LPDP) during the conduct of the study. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Supporting information
ACKNOWLEDGEMENTS
M.P.O. would like to thank the LPDP for their support of her PhD programme. Financial support from the LPDP has helped many Indonesian students to obtain higher education in order to promote Indonesia development. The authors also acknowledge Mrs D. G. van Ittersum from the Central Library of the University Medical Centre Groningen, the Netherlands, for help during developing the search strategy in the scoping review.
Funding information
The authors did not receive any specific grant for this research from funding agencies in the public, commercial or not‐for‐profit sectors.
REFERENCES
- 1. Reeve E, Gnjidic D, Long J, Hilmer S. A systematic review of the emerging definition of ‘deprescribing’ with network analysis: implications for future research and clinical practice. Br J Clin Pharmacol. 2015;80:1254‐1268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Scott IA, Hilmer SN, Reeve E, et al. Reducing inappropriate polypharmacy: the process of deprescribing. JAMA Intern Med. 2015;175:827‐834. [DOI] [PubMed] [Google Scholar]
- 3. Formiga F, Vidal X, Agusti A, et al. Inappropriate prescribing in elderly people with diabetes admitted to hospital. Diabet Med. 2016;33:655‐662. [DOI] [PubMed] [Google Scholar]
- 4. Scott IA, Hilmer SN, Le Couteur DG. Going Beyond the Guidelines in Individualising the Use of Antihypertensive Drugs in Older Patients. Drugs Aging. 2019;36:675‐685. [DOI] [PubMed] [Google Scholar]
- 5. Rodriguez‐Gutierrez R, Montori VM. Glycemic Control for Patients With Type 2 Diabetes Mellitus: Our Evolving Faith in the Face of Evidence. Circ Cardiovasc Qual Outcomes. 2016;9:504‐512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Davies MJ, D'Alessio DA, Fradkin J, et al. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 2018;61:2461‐2498. [DOI] [PubMed] [Google Scholar]
- 7. Qaseem A, Wilt TJ, Kansagara D, Horwitch C, Barry MJ, Forciea MA. Hemoglobin A1c targets for glycemic control with pharmacologic therapy for nonpregnant adults with type 2 diabetes mellitus: A guidance statement update from the American college of physicians. Ann Intern Med. 2018;168:569‐576. [DOI] [PubMed] [Google Scholar]
- 8. Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts)Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Eur Heart J. 2016;37:2315‐2381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Stone NJ, Robinson JG, Lichtenstein AH, et al. 2013 ACC/AHA guideline on the treatment of blood cholesterol to reduce atherosclerotic cardiovascular risk in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol. 2014;63(25 Pt B):2889‐2934. [DOI] [PubMed] [Google Scholar]
- 10. U.S. Department of Veterans Affairs . Hypoglycemia Safety Initiative (HSI) ‐ Quality, Safety & Value. November 6, 2018; Available at: https://www.qualityandsafety.va.gov/ChoosingWiselyHealthSafetyInitiative/HypoglycemiaSite/Hypoglycemia.asp. Last accessed 27 August 2019.
- 11. Black CD, Thompson W, Welch V, et al. Lack of Evidence to Guide Deprescribing of Antihyperglycemics: A Systematic Review. Diabetes Ther. 2017;8:23‐31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Abdelhafiz AH, Sinclair AJ. Deintensification of hypoglycaemic medications‐use of a systematic review approach to highlight safety concerns in older people with type 2 diabetes. J Diabetes Complications. 2018;32:444‐450. [DOI] [PubMed] [Google Scholar]
- 13. Seidu S, Kunutsor SK, Topsever P, Hambling CE, Cos FX, Khunti K. Deintensification in older patients with type 2 diabetes: a systematic review of approaches, rates and outcomes. Diabetes Obes Metab. 2019;21:1668‐1679. [DOI] [PubMed] [Google Scholar]
- 14. Lipska KJ, Ross JS, Miao Y, Shah ND, Lee SJ, Steinman MA. Potential overtreatment of diabetes mellitus in older adults with tight glycemic control. JAMA Intern Med. 2015. Mar;175(3):356‐362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Sussman JB, Kerr EA, Saini SD, et al. Rates of Deintensification of Blood Pressure and Glycemic Medication Treatment Based on Levels of Control and Life Expectancy in Older Patients With Diabetes Mellitus. JAMA Intern Med. 2015;175:1942‐1949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. McCoy RG, Lipska KJ, Yao X, Ross JS, Montori VM, Shah ND. Intensive Treatment and Severe Hypoglycemia Among Adults With Type 2 Diabetes. JAMA Intern Med. 2016;176:969‐978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Markovitz AA, Hofer TP, Froehlich W, et al. An Examination of Deintensification Recommendations in Clinical Practice Guidelines: Stepping Up or Scaling Back? JAMA Intern Med. 2018;178:414‐416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Mallery LH, Ransom T, Steeves B, Cook B, Dunbar P, Moorhouse P. Evidence‐informed guidelines for treating frail older adults with type 2 diabetes: from the Diabetes Care Program of Nova Scotia (DCPNS) and the Palliative and Therapeutic Harmonization (PATH) program. J Am Med Dir Assoc. 2013;14:801‐808. [DOI] [PubMed] [Google Scholar]
- 19. Farrell B, Black C, Thompson W, et al. Deprescribing antihyperglycemic agents in older persons: Evidence‐based clinical practice guideline. Can Fam Physician. 2017;63:832‐843. [PMC free article] [PubMed] [Google Scholar]
- 20. Strain WD, Hope SV, Green A, Kar P, Valabhji J, Sinclair AJ. Type 2 diabetes mellitus in older people: a brief statement of key principles of modern day management including the assessment of frailty. A national collaborative stakeholder initiative. Diabet Med. 2018;35:838‐845. [DOI] [PubMed] [Google Scholar]
- 21. Deprescribing Resources. 2019; Available at: https://www.primaryhealthtas.com.au/resources/deprescribing‐resources/. Last accessed 18 July 2019.
- 22. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tricco AC, Lillie E, Zarin W, et al. PRISMA Extension for Scoping Reviews (PRISMA‐ScR): Checklist and Explanation. Ann Intern Med. 2018;169:467‐473. [DOI] [PubMed] [Google Scholar]
- 24. Reeve E, Shakib S, Hendrix I, Roberts MS, Wiese MD. Review of deprescribing processes and development of an evidence‐based, patient‐centred deprescribing process. Br J Clin Pharmacol. 2014;78:738‐747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. National Heart, Lung, and Blood Institute (NHLBI) . Study Quality Assessment Tools. Available at https://www.nhlbi.nih.gov/health‐topics/study‐quality‐assessment‐tools. Last accessed 23 May 2019.
- 26. Gardiner KM, Singleton JA, Sheridan J, Kyle GJ, Nissen LM. Health professional beliefs, knowledge, and concerns surrounding medicinal cannabis ‐ A systematic review. PLoS One. 2019;14:e0216556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Maciejewski ML, Mi X, Sussman J, et al. Overtreatment and Deintensification of Diabetic Therapy among Medicare Beneficiaries. J Gen Intern Med. 2018;33:34‐41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. McAlister FA, Youngson E, Eurich DT. Treatment Deintensification Is Uncommon in Adults With Type 2 Diabetes Mellitus: A Retrospective Cohort Study. Circ Cardiovasc Qual Outcomes. 2017;10:e003514. [DOI] [PubMed] [Google Scholar]
- 29. McAlister FA, Lethebe BC, Lambe C, Williamson T, Lowerison M. Control of glycemia and blood pressure in British adults with diabetes mellitus and subsequent therapy choices: a comparison across health states. Cardiovasc Diabetol. 2018;17:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Wright SM, Hedin SC, McConnell M, et al. Using Shared Decision‐Making to Address Possible Overtreatment in Patients at High Risk for Hypoglycemia: The Veterans Health Administration's Choosing Wisely Hypoglycemia Safety Initiative. Clin Diabetes. 2018;36:120‐127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Yotsapon T, Sirinate K, Ekgaluck W, et al. Clinical characteristics and outcomes of the oldest old people with type 2 diabetes ‐ perspective from a tertiary diabetes center in Thailand. BMC Endocr Disord. 2016;16:30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Vimalananda VG, DeSotto K, Chen T, et al. A Quality Improvement Program to Reduce Potential Overtreatment of Diabetes Among Veterans at High Risk of Hypoglycemia. Diabetes Spectr. 2017;30:211‐216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Abdelhafiz AH, Chakravorty P, Gupta S, Haque A, Sinclair AJ. Can hypoglycaemic medications be withdrawn in older people with type 2 diabetes? Int J Clin Pract. 2014;68:790‐792. [DOI] [PubMed] [Google Scholar]
- 34. Sjoblom P, AndersTengblad LUB, Lannering C, et al. Can diabetes medication be reduced in elderly patients? An observational study of diabetes drug withdrawal in nursing home patients with tight glycaemic control. Diabetes Res Clin Pract. 2008;82:197‐202. [DOI] [PubMed] [Google Scholar]
- 35. Vischer UM, Perrenoud L, Genet C, Ardigo S, Registe‐Rameau Y, Herrmann FR. The high prevalence of malnutrition in elderly diabetic patients: implications for anti‐diabetic drug treatments. Diabet Med. 2010;27:918‐924. [DOI] [PubMed] [Google Scholar]
- 36. Masumoto N, Otsuki H, Iwakawa S, Inada S, Koga M. Usefulness of glycated albumin in decisions regarding the discontinuation of a diabetes drug and factors associated with poor glycemic control following discontinuation in patients with type 2 diabetes mellitus. Diabetol Int. 2016;8:39‐44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Caverly TJ, Fagerlin A, Zikmund‐Fisher BJ, et al. Appropriate Prescribing for Patients With Diabetes at High Risk for Hypoglycemia: National Survey of Veterans Affairs Health Care Professionals. JAMA Intern Med. 2015;175:1994‐1996. [DOI] [PubMed] [Google Scholar]
- 38. Genere N, Sargis RM, Masi CM, et al. Physician perspectives on de‐intensifying diabetes medications. Medicine (Baltimore). 2016;95:e5388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Reeve E, Jordan V, Thompson W, et al. Withdrawal of antihypertensive drugs in older people. Cochrane Database Syst Rev. 2020;6:CD012572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. American College of Physicians (ACP) Internist . Reconciling conflicting diabetes guidance. ACP and other professional medical societies disagree on a proper target for the long‐term benefits of glucose control. June 2018; Available at https://acpinternist.org/archives/2018/06/reconciling‐conflicting‐diabetes‐guidance.htm. Last accessed 29 August 2019.
- 41. Anderson K, Stowasser D, Freeman C, Scott I. Prescriber barriers and enablers to minimising potentially inappropriate medications in adults: a systematic review and thematic synthesis. BMJ Open. 2014;4:e006544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Reeve E, To J, Hendrix I, Shakib S, Roberts MS, Wiese MD. Patient barriers to and enablers of deprescribing: a systematic review. Drugs Aging. 2013;30:793‐807. [DOI] [PubMed] [Google Scholar]
- 43. van Middelaar T, Ivens SD, van Peet PG, et al. Prescribing and deprescribing antihypertensive medication in older people by Dutch general practitioners: a qualitative study. BMJ Open. 2018;8:e020871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Farrell B, Richardson L, Raman‐Wilms L, de Launay D, Alsabbagh MW, Conklin J. Self‐efficacy for deprescribing: A survey for health care professionals using evidence‐based deprescribing guidelines. Res Social Adm Pharm. 2018;14:18‐25. [DOI] [PubMed] [Google Scholar]
- 45. Sinclair AJ, Abdelhafiz A, Dunning T, et al. An International Position Statement on the Management of Frailty in Diabetes Mellitus: Summary of Recommendations 2017. J Frailty Aging. 2018;7:10‐20. [DOI] [PubMed] [Google Scholar]
- 46. Beuscart JB, Knol W, Cullinan S, et al. International core outcome set for clinical trials of medication review in multi‐morbid older patients with polypharmacy. BMC Med. 2018;16:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Rankin A, Cadogan CA, In Ryan C, Clyne B, Smith SM, Hughes CM. Core Outcome Set for Trials Aimed at Improving the Appropriateness of Polypharmacy in Older People in Primary Care. J Am Geriatr Soc. 2018;66:1206‐1212. [DOI] [PubMed] [Google Scholar]
- 48. Pirela DV, Garg R. De‐Intensification of Diabetes Treatment in Elderly Patients with Type 2 Diabetes Mellitus. Endocr Pract. 2019;25:1317‐1322. [DOI] [PubMed] [Google Scholar]
- 49. Aspinall SL, Zhao X, Good CB, et al. Intervention to decrease glyburide use in elderly patients with renal insufficiency. Am J Geriatr Pharmacother. 2011;9:58‐68. [DOI] [PubMed] [Google Scholar]
- 50. Niznik JD, Hunnicutt JN, Zhao X, et al. Deintensification of Diabetes Medications among Veterans at the End of Life in VA Nursing Homes. J Am Geriatr Soc. 2020;68:736‐745. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials


