Summary
Several studies have reported on the negative impact of interruptions and distractions on anaesthetic, surgical and team performance in the operating theatre. This study aimed to gain a deeper understanding of these events and why they remain part of everyday clinical practice. We used a mixed methods observational study design. We scored each distractor and interruption according to an established scheme during induction of anaesthesia and the surgical procedure for 58 general surgical cases requiring general anaesthesia. We made field notes of observations, small conversations and meetings. We observed 64 members of staff for 148 hours and recorded 4594 events, giving a mean (SD) event rate of 32.8 (16.3) h‐1. The most frequent events observed during induction of anaesthesia were door movements, which accounted for 869 (63%) events, giving a mean (SD) event rate of 28.1 (14.5) h‐1. These, however, had little impact. The most common events observed during surgery were case‐irrelevant verbal communication and smartphone usage, which accounted for 1020 (32%) events, giving a mean (SD) event rate of 9.0 (4.2) h‐1. These occurred mostly in periods of low work‐load in a sub‐team. Participants ranged from experiencing these events as severe disruption through to a welcome distraction that served to keep healthcare professionals active during low work‐load, as well as reinforcing the social connections between colleagues. Mostly, team members showed no awareness of the need for silence among other sub‐teams and did not vocalise the need for silence to others. Case‐irrelevant verbal communication and smartphone usage may serve a physical and psychological need. The extent to which healthcare professionals may feel disrupted depends on the situation and context. When a team member was disrupted, a resilient team response often lacked. Reducing disruptive social activity might be a powerful strategy to develop a habit of cross‐monitoring and mutual help across surgical and anaesthetic sub‐teams. Further research is needed on how to bridge cultural borders and develop resilient interprofessional behaviours.
Keywords: communication, distractions, performance monitoring, resilience
Introduction
It is recognised widely that human factors and non‐technical skills play a key role for critical incident prevention in the peri‐operative period [1]. More specifically, the frequency of interruption and distraction has been associated with the incidence of human error [2]. Previous research has associated distraction with: the performance of the surgeon [3, 4], the anaesthetist [5, 6, 7] or the team as a whole [3, 4]; surgical delay and inefficiency [8]; cognitive overload and stress [9, 10, 11]; and miscommunication [4]. Case‐irrelevant communication constitutes a significant proportion of the distractions observed in the operating theatre [3, 12]. Outside of the operating theatre, distractions are sometimes seen as beneficial, for example, in the context of medical device alarms and patient call alerts on wards [13]. There have been calls for the use of more precise language around interruption and distraction in healthcare settings in the clinical environments and contexts within which they occur [14, 15].
Our aim was to understand when and why distractions happen, how they are experienced and how members of the peri‐operative team handle them. For this, we conducted observations in the context of general surgical operating theatres at a large Dutch teaching hospital.
Methods
According to local and national policy, formal ethical approval was not required for this non‐interventional observational study of healthcare professionals. We obtained consent from included healthcare professionals and did not observe potential participants who did not wish to be observed. All participants were aware they would be observed during their normal duties, but they were not aware of the aim of the study or the nature of the observations.
The study was conducted at a large Dutch teaching hospital in three general surgical operating theatres. A variety of long and short procedures were undertaken including vascular, trauma and general surgery. We undertook observations on every weekday during day‐time hours. We aimed to match the total number of observation hours with previous comparable studies [3, 12], but data collection nevertheless continued until ‘saturation’ was achieved, where no new themes emerged. The observer was granted permission to remain in the operating theatre unless the environment became crowded (more than 10 essential individuals). The observer was granted priority over non‐essential team members, such as medical or nursing students. The approach to data collection was through ascertaining the frequency of certain types of behaviours, unstructured qualitative field note observations and informal participant interviews. Two authors recorded observations independently, which were cross‐checked against each other at the end of every observation period.
The first phase of observations replicated the methods of previous research to determine the frequency and nature of distractions [3, 12]. We also recorded free‐text field notes of distractions in the operating theatre to develop themes around their persistence. During observations, the observer was there solely to observe and not to undertake a clinical or administrative role [16]. Although they were visible and sometimes had to move around to be able to observe, the observers tried to minimise interaction to prevent distraction or a change in the behaviour of the observers. The categories of distractors were predefined and the observer recorded the frequencies with which these events occurred. Every distractor was weighted with an impact score (Table 1). The forms used to record these frequencies and the free‐text field notes are provided in online Appendix S1. Following the completion of the first phase of observations, we debriefed participants by explaining our aims and member checking our initial findings [17].
Table 1.
The 9‐point ordinal scale used to judge the impact of observed events as adapted from [12].
|
For the second phase of data collection, we focused observations on case‐irrelevant verbal communication and smartphone usage, which we categorised as social activity. The role of the observer changed from passive observation to participant observer. Observers were asked to ensure that after the sign‐out, the team made a judgment on whether they had kept quiet when needed. Their presence facilitated disclosure in small, informal conversations and enabled the observer to ask clarifying questions.
Analyses were performed in an inductive iterative process concurrently with data collection by the observer and a second investigator. We continually looked for differences and similarities within and between themes and this informed subsequent data collection. After the first member check, all authors independently read the expanded field notes to combine interpretations as much as possible, resulting in a list of codes and their subsequent themes. The observer and second observer expanded this list during the next procedures. After 28 procedures in phase 2, all authors read the field notes independently again, but no more themes emerged. By consensus, they combined the list into four overarching concepts that served as a framework to present the results.
The qualitative data are presented in summarised observations, short extracts or quotes, and vignettes. These vignettes serve to evoke a vicarious experience, facilitating translation of findings to other settings [18]. The selection of these vignettes has been guided by their potential to learn about the role of social activity in the operating theatre. Using a previously published observation scheme as a reference, we chose to present means instead of medians for reasons of comparability with earlier studies [12]. Furthermore, to correct the frequency of a distractor for the impact of that distractor, we chose the interference criterion to determine the most prominent distractions (Table 2). For the analysis and discussion, we used previously published definitions of interruption, distraction and disruptiveness [11]. All quantitative analyses were carried out using IBM SPSS Statistics v24 (IBM, Armonk, NY, USA).
Table 2.
| Term | Definition |
|---|---|
| Distractor | The trigger that can cause one to become distracted. |
| Distraction |
A momentary lapse of attention on the primary task without suspending it. Examples:
|
| Interruption |
The suspension of the stream of work before completion, with the intent of returning to and completing the original stream of work. Interruptions always create a distraction. Consequently, distractions include interruptions. Examples:
|
| Disruptiveness | The degree to which interruptions have negative effects on the control of the process and are unsettling for a person and/or a team. |
| Impact |
The extent to which a distractor leads to a pause and to which it involves more individuals. Example:
|
| Frequency | The number of distractors per hour. |
| Interference | A rated frequency enabling the comparison of frequent distractors with little impact and rare distractors with high impact. As such, it is a measure for the disturbance of the operative process. |
| Induction | The time frame that starts when the patient receives an oxygen mask or is positioned for a spinal or epidural to the time of the first incision. During this time frame, the surgical team enters the room (if not already inside) and gathers around the table. |
| Incision‐to‐closure | The time frame that starts at incision and ends when the sign‐out starts (when instruments and gauzes are finally checked and postoperative plan is set). |
| Sub‐team |
A part of the complete operating team. The team in the operating room can be divided in to the following sub‐teams:
Depending on the topic, division can also form along the lines of sterile team vs. non‐sterile teams. Sub‐teams are not fixed but consist of shifting configurations. |
Results
Participants included 27 surgeons, 17 operating theatre nurses and 16 surgical trainees. From the large anaesthesia team (approximately 60 consultants, 37 trainees and 62 nurses), only two nurses and two consultants were dedicated to general surgery. Operating theatre nurses, consultant surgeons and senior anaesthetists had often worked together for several years. Performing a briefing at the start of the day, a time‐out before incision, and a sign‐out before leaving the operating theatre was standard practice. In this hospital, smartphones were allowed in the operating theatre for professional purposes.
The total observation time during induction of anaesthesia and for the surgical procedure was 148 h, which included 80 (54%) h for phase 1 observations and 68 (46%) h for phase 2 observations. Of these, 32 (22%) h were during induction of anaesthesia and 116 (78%) h during the surgical procedure. In total, 4594 distraction events were observed with a mean (SD) event rate of 32.8 (16.3) h‐1. Door movements were observed most frequently, with 11.7 (9.2) h‐1 and were common during induction of anaesthesia, where there were 28.1 (14.5) h‐1, but these had little mean (SD) impact [1.9 (0.4)] on participants. Equipment failures or missing materials caused the most impact [4.3 (1.5)] but were not frequent, with 1.1 (0.8) h‐1. Door movements were of the highest mean (SD) interference during induction of anaesthesia [52.2 (29.3)], and case‐irrelevant verbal communication plus smartphone usage were of the highest mean (SD) interference during surgery [23.1 (12.9)]. The results of phase 1 that were used for member checking in phase 2 are in line with the overall results (Table 3).
Table 3.
Impact, frequency and interference of distractors. Interference rating is impact multiplied by frequency from each source in cases where those events were recorded. When case‐irrelevant verbal communication involved members of different sub‐teams, the initiating sub‐team was marked as the source. Values are mean (SD). Impact is measured on a 9‐point ordinal scale [12]. Impact and interference are dimensionless and allow comparisons to be made between categories of distractions.
| Impact | Events per hour | Interference | |
|---|---|---|---|
| Induction of anaesthesia | |||
| Smartphone | 2.9 (0.9) | 3.8 (3.0) | 11.5 (12.3) |
| Door movements | 1.9 (0.4) | 28.1 (14.5) | 52.2 (29.3) |
| Phone | 2.5 (0.6) | 4.5 (4.5) | 11.2 (12.4) |
| Pager | 2.7 (0.6) | 5.7 (4.9) | 15.4 (11.9) |
| Radio | 2.3 (1.1) | 2.7 (3.1) | 5.8 (6.1) |
| Case‐irrelevant verbal communication: surgical team | 2.9 (0.6) | 2.5 (2.24) | 7.1 (6.6) |
| Case‐irrelevant verbal communication: anaesthesia team | 2.8 (1.0) | 2.9 (2.3) | 8.0 (5.9) |
| Case‐irrelevant verbal communication: nursing team | 2.6 (0.8) | 4.0 (5.5) | 11.4 (19.3) |
| Case‐irrelevant verbal communication: external personnel | 3.1 (0.2) | 1.9 (0.9) | 5.9 (3.1) |
| Case‐irrelevant verbal communication: overall | 2.6 (0.7) | 5.8 (5.3) | 16.2 (17.6) |
| Equipment failure | 3.6 (1.6) | 2.4 (1.1) | 8.2 (4.9) |
| Work environment | 3.4 (1.1) | 2.4 (1.1) | 7.6 (5.4) |
| Procedural | 2.5 (0.7) | 2.2 (1.0) | 8.9 (5.4) |
| Shutter | 2.5 (1.1) | 2.3 (1.2) | 6.1 (4.4) |
| Overall | 2.1 (0.3) | 42.0 (22.5) | 90.6 (56.8) |
| Incision to closure | |||
| Smartphone | 2.7 (0.7) | 2.9 (2.2) | 7.8 (6.6) |
| Door movements | 2.1 (0.4) | 6.2 (2.9) | 12.7 (6.7) |
| Phone | 2.4 (0.6) | 6.0 (2.4) | 14.7 (7.2) |
| Pager | 2.9 (0.6) | 1.2 (0.8) | 3.4 (2.9) |
| Radio | 2.7 (1.3) | 1.1 (0.7) | 3.4 (3.1) |
| Case‐irrelevant verbal communication: surgical team | 2.7 (0.9) | 1.7 (1.1) | 4.3 (2.8) |
| Case‐irrelevant verbal communication: anaesthesia team | 3.0 (1.1) | 2.3 (2.2) | 7.1 (7.5) |
| Case‐irrelevant verbal communication: nursing team | 2.5 (0.6) | 2.6 (1.9) | 6.1 (3.9) |
| Case‐irrelevant verbal communication: external personnel | 3.0 (0.8) | 1.7 (1.6) | 5.1 (5.8) |
| Case‐irrelevant verbal communication: overall | 2.7 (0.6) | 6.7 (3.6) | 17.9 (9.8) |
| Equipment failure | 4.4 (1.6) | 1.2 (1.0) | 5.2 (4.8) |
| Work environment | 3.1 (1.0) | 1.0 (0.7) | 3.2 (3.0) |
| Procedural | 2.2 (0.6) | 3.7 (3.0) | 8.9 (8.7) |
| Shutter | 2.9 (0.4) | 2.8 (1.8) | 8.1 (5.2) |
| Overall | 2.5 (0.3) | 28.3 (8.9) | 72.4 (28.7) |
Most case‐irrelevant verbal communication concerned ‘small talk’, defined as polite uncontroversial conversation. Work‐related case‐irrelevant verbal communication typically concerned the planning of the next case or focused on the education and learning of junior team members. In this study, smartphones were used frequently, and most of the time this was for private purposes. Typically, smartphones were used in silence and distracted the smartphone user rather than other team members. We observed incoming messages distracting the user and the user seeking distraction by sending messages or scrolling for information. Information retrieved from the smartphone sometimes triggered case‐irrelevant verbal communication. We categorised all this as smartphone usage and case‐irrelevant verbal communication.
Key themes with their accompanying extracts have been selected to illustrate both the typical observations and responses collated and the diversity and breadth of the data set. Four key themes emerged: low work‐load; disruptiveness; division of professions; and individual competence.
Low work‐load
Low work‐load means being without active tasks. Passive tasks include monitoring, being available for requests, and watching the work undertaken. Low work‐load may occur when staff have few tasks at hand. These low work‐load episodes are not easy to avoid, as Extract 1 illustrates.
Extract 1 – Anaesthetist S
The anaesthesia nurse is attending a stable patient and Anaesthetist S is talking to another participant for some time when she says “I really don’t know what I have to do here, I feel pretty useless”. Not long after, she leaves. Later that day, the observer meets her by chance when she is going home. The next conversation evolves.
Observer: “Did you have a good day?”
Anaesthetist S: “No, I have the feeling that I really didn't do much today, that doesn't feel good.”
Observer: “How come?”
Anaesthetist S: “All rooms I had to supervise went very well, but I have to stay around because if anything goes wrong, I have to be there in seconds.”
Observer: “And it is not possible to work on one of the computers in the operating theatre complex?”
Anaesthetist S: “No, I really cannot concentrate there because I have to check my patients regularly, […] there are a lot of people walking around there asking questions.”
Vignettes 1, 2 and 4 (Table 4) provide further examples of participants in periods of low work‐load. Observed behaviours in these examples are talking, walking around, engaging with a smartphone and educating students. On other occasions, we saw participants yawning, rubbing their eyes, looking around, gazing, preparing for the next procedure, refilling stocks or dancing to music.
Table 4.
Four major themes emerged from the qualitative analysis. Four vignettes are given in which case‐irrelevant verbal communication and smartphone usage occurred. Vignettes 1–3 are examples of disruptive social activity for one of the sub‐teams. Vignette 4 exemplifies a situation in which case‐irrelevant communication and smartphone usage are handled such that they do not become disruptive and are supportive for the team.
|
Vignette 1 – The distracted surgeon The surgeon, the trainee and the scrub nurse are operating on a patient. The anaesthesia team is talking about an upcoming professional examination and rehearsing their knowledge in a low voice. The circulating nurse and a student nurse are sitting on a stool watching their smartphones when suddenly, they start laughing at a video they are watching. The nurses find humour in this and the anaesthesia team becomes interested and joins the conversation. At the end of the procedure, when the silence‐to‐concentrate is evaluated, everyone expresses their satisfaction with the conduct of the day. The surgeon and the observer leave together for lunch. When asked about distractions, the surgeon admits, “I was distracted by the gossip about the video. It made me curious and I wanted to see the video as well. I had real difficulty concentrating on the procedure.” Observer: “So why did you not mention this in the evaluation of silence‐to‐concentrate?” Surgeon: “Well, I didn’t want to be a bore. The next day we have to work together again, you know.” |
|
Vignette 2 – The interrupted anaesthetist In the briefing at 0805, the team decides that one anaesthesia assistant will guard the silence‐to‐concentrate. After the briefing, everybody but the anaesthesia team leaves the room. At 0830, the patient lies on the table and the anaesthesia team is administering induction agents. A trainee surgeon enters the operating theatre: “Good morning everybody!” He turns to the observer and asks loudly, “You are watching for distractions?” The observer whispers “Yes”. The trainee surgeon, turning his eyes to the table, “Oh I thought the patient was already asleep”. A few minutes later, the trainee, who is circling around the patient and touching the patient, is asked whether he is willing to insert the urinary catheter. He answers ironically, “Sure, that is my hobby”. When finished, the anaesthetist asks, “Would you mind putting on a mask, we opened a sterile set.” Her voice has a slightly higher pitch when she says, “We have to take care that we are not going to be in each other’s way.” Up to this point, seven persons enter the operating room and leave again, without an obvious reason. They are all talking, greeting and asking questions. Additionally, the ultrasound machine is not working and the anaesthetist has to fetch another one before they can proceed. |
|
Vignette 3 – The multi‐tasking circulating nurse A patient with an acute traumatic injury is on the operating table. The team agreed to focus on no entrances during induction of anaesthesia. Nevertheless, there were 13 entrances. By now, the first senior circulating nurse is walking up and down to fetch materials and meanwhile, answers questions from the surgeons and the operating room phone, which is ringing all the time. Five times she answers requests with “wait a minute” and once with “just start with one thing at the time.” She mumbles to herself things like “where did I leave my form?” There is a lot of movement, material failure, noise, music, loud talking about all kinds of subjects and a lot of apparatus that is to be put in place. There are 11 people in the operating theatre, but the second circulating nurse has her coffee break. The anaesthetist, looking at the situation, remarks to the observer: “I go nuts, what an exhibition, I really need a pill.” |
|
Vignette 4 – The resilient team Today, there is a long 8‐h procedure and it will be performed by an experienced team. Main surgeon, nurse and anaesthetist are all aged > 50 y. The team agrees in the briefing that today they will be alert regarding minimising door movements and silence‐to‐concentrate. A few minutes later, only the anaesthesia team is in the operating theatre. The anaesthetist is talking to the patient to provide comfort whilst administering induction agents, when a nurse silently brings in a trolley. She accidently knocks over a metal stool that bangs on the floor. Startled and apologetic, she looks up to the anaesthetist. The anaesthetist just pauses to observe the reaction of the patient – no reaction – and then calmly continues his comfort talk. The nurse mumbles softly to herself “who put the stool over here” and places the stool aside. After induction and before the incision time‐out, there is some chatting and joking. Therefore, the nurse calls a team member by name to get his attention and asks to put on the mask before bringing in the sterile material. The surgeon puts his smartphone near the computer station in quiet mode. Halfway through the morning, the anaesthetist shows a picture of his son on his smartphone to the circulating nurse. They talk about it with a whispering voice at some distance from the sterile team. Thirty minutes later, the circulating nurse assists the intern by explaining the views on the monitor and by offering relevant information on her smartphone. Around noon, a large part of the sterile team and one of the anaesthesia team members leaves for a 15 min lunch break. On several occasions, team members disclosed to the observer that they really appreciated this team because they could work together so well. During the debriefing, team members complimented each other with the good results including few door movements (22 in total) and silence‐to‐concentrate. |
We inferred that talking during periods of low work‐load, like the nurses in Vignette 1, serves the need to stay active and alert, and sometimes even to fight the risks of fatigue. The behaviour of the surgeon in Vignette 2 and Anaesthetist S in Extract 1, illustrates the inclination or urge to be active. The rise in talking after induction of anaesthesia and before the first surgical incision, as in Vignettes 1 and 4, again might illustrate this need for activity. Low work‐load evokes strategies to stay active and feel socially comfortable. Case‐irrelevant verbal communication and smartphone usage are among those strategies. Making a distinction between work‐related and private case‐irrelevant verbal communication or smartphone usage may be useful, but should not be the basis for valuing their putative disruptiveness. Depending on the context, private small talk can contribute to better performance, and work‐related education can be disruptive.
We observed that different team members had low work‐load during different phases. Low work‐load for the anaesthesia team was typical when the patient was anaesthetised and haemodynamically stable. They were observed to monitor the vital signs and refill medication. For long procedures, without many requests for materials, this was also the low work‐load phase for the circulating nurse. For the surgeons, the low work‐load phase was the period in which they waited for the team to prepare for surgery, and also the phase of closing the wound which was often left to the trainee. Cycles of action and low work‐load were asynchronous for the sub‐teams. Therefore, the evoked strategies to stay active and connect socially were often helpful for one sub‐team but disruptive for the other. To establish the level of disruptiveness, the whole must be considered.
Disruptiveness
Disruptiveness is the degree to which interruptions have negative effects on the process and are unsettling for a person and/or a team, whereas interference is the impact multiplied by frequency (Table 2). On member checking the findings of the first phase with the operating theatre nurses, there was surprise that case‐irrelevant verbal communication was the highest interference. Their main concerns were with the phones and pagers of the surgeons, and a change of surgeons during the procedure. In their view, these distractors often lead to a risky situation of multitasking and cognitive overload.
There were 365 phone calls observed. The nurses answered phones or pagers for the surgeon eight times, and twice they left the phone of the surgeon ringing out. These moments stood out in the memory of the nurses as disruptive, and they connect these events to situations of multitasking and cognitive overload. From our observations, we cannot confirm this connection, but we can understand that in a situation where there is multitasking and cognitive overload (Table 4; Vignette 3), any distraction can be seriously disruptive. Situations with many distractions at the same time may stand out in the memory as disruptive much more than numerous non‐disruptive instants of case‐irrelevant verbal communication, which generated a score as highly interfering.
During member checking among participants, the surgeons remarked that ‘small talk’ in the operating theatre was not harmful. However, on several occasions individual surgeons voiced their displeasure with the case‐irrelevant verbal communication of the nurses or the anaesthetic team, which was felt to be disruptively distracting (Extracts 2 and 3, Table 4; Vignette 1). Thus, the surgeons expressed that they can experience small talk as relaxing and as disruptive as well, depending on the situation and on individual preferences. In this study, the preference for silence was not associated with the age or experience of the surgeon (Vignette 4).
Extract 2 – Surgeon H
A nurse was looking at her personal messages and shared the content of the messages with the team. Shortly thereafter, the following conversation took place:
Surgeon H: “Are you enjoying the chatting?”
Nurse K: “Is it bothering you?”
Surgeon H: “No not at all, feel free to go on.”
Observer: “When do you experience disturbance during a procedure?”
Surgeon H: “The chattering away during the operation this morning was really too much. I made a sarcastic remark about it, but the nurses didn’t seem to understand.”
Extract 3 – Surgeons B and D
During a small pause, the following conversation took place:
Observer: “What do you consider disturbing during a procedure?”
Surgeon B: “I really hate all that prattling.”
Surgeon D: “Yeah, that they are going to talk about movies or spouses or that sort of thing.”
For anaesthetists, door movement was rated as the most interfering factor during induction of anaesthesia. However, it was the talking and greeting accompanying the door movements that disrupted them the most. We observed this on several occasions. Anaesthetists sometimes asked for silence during induction of anaesthesia, but more often they did not.
All professions agreed that a serious safety threat arises when there is a change of surgeon (Extracts 4, 5 and 6). We did not observe a change of surgeon, but several times we observed that the trainee, who had been there all the time, finished the procedure alone. Although the research team was in doubt whether to categorise the situation as a handover and/or as a distraction, the professionals all considered it a distraction. The situation as described in Extract 4 was scored in the observation instrument as category 1 (person leaving) and impact 2 (the leaving was noticed by circulating participants). Category 1 did not generate high interference. There was no category for ‘change of surgical team’ in the observation instrument.
Extract 4
‘A nurse came to me to tell me that there had been a complication that I had missed because, from my position at the moment, I was not able to hear the conversation at the table. When Surgeon T assigned Trainee A to close the wound, he did not specify that the drain had to be unfastened. The wound was already closed partially and had to be re‐opened. The scrub nurse noticed. If she had not, it might have caused a complication later on.’
Extract 5 – Surgeon K
Surgeon K: “Most complications arise as a consequence of forgetting to perform the sign‐out, a change of surgeon and leaving the closing of the wound to less experienced surgeons.”
Extract 6
“We presented the finding that a change of surgeon, a preoccupation especially of the nurses, was seldom observed. The participants responded to that by stating that this finding does not prove the nurses wrong because incidents from the past tell us that a change in surgeon, or leaving the trainee to finish, poses a risk.”
In all of these findings, the interference rating did not match the experienced disruptiveness. All professions agreed that a change of surgeon or leaving the trainee to finish the procedure was an important distractive event. This was, however, not a category in the observation instrument.
Division of professions
The division of professions refers to the distance between professions, especially anaesthetists and surgeons, which becomes visible in interaction patterns, humour and the awareness of sub‐teams. We observed that the operating theatre team is a collection of sub‐teams and each has limited awareness of the others. This lack of awareness, in combination with asynchronous work‐loads, influences the way distractions are handled in the team. In Vignette 1, neither the circulating nurse nor the anaesthesia team were aware how distracting their conversation was for the surgeon. In Vignette 2, the surgeon lacked awareness of the needs of the anaesthesia team. The anaesthetist tried to raise awareness, and to redirect behaviour by giving a task to the waiting surgeon, but he did not respond in an understanding way to this. In Vignette 3, the anaesthetist was aware of the needs of the nurse, but did not step forward to intervene. The rest of the team lacked awareness and therefore the team could not adjust to the situation effectively, for example, by stopping the radio, asking for help, or co‐ordinating communication.
On several occasions, we observed that the surgical team left the room during induction of anaesthesia to create silence, showing they were aware of the necessity for it. However, it was often not clear what instigated their return to the room. Sometimes, they came back when the anaesthesia team was not yet ready and was administering drugs or intubating the patient's trachea
In Vignette 4, the whole team was aware of each other’s needs. However, this was more an exception than a rule. The nurse as well as the anaesthesia team responded effectively to the distraction by the noise of the falling stool, and they were alert enough not to distract others by their small talk, by choosing the right time, the right place and by speaking quietly. Remarkably, this specific team had lunch together whereas usually every profession turns to its own corner of the canteen. Furthermore, in this team the green sheet, dividing the space between surgery and anaesthesia, was put up at a height that the anaesthesia team could easily watch the procedure and communicate with the surgeon. On many occasions it was much higher, giving the impression to the observer that it served to shield the personal space for the anaesthesia team. Extract 7 shows a small conversation on this subject.
Extract 7
“The surgical team is positioning the monitors and the anaesthesia team has positioned the green sheet at quite a high level, such that it might obstruct the view of the monitor for the anaesthesia team. The observer asks: “Why has the sheet to be that high?” The surgeon reacts by lowering the sheet and saying: “There is no need to do so at all”.
The team in Vignette 4 was crossing cultural borders by ignoring the usual divisions in the operating theatre and by lowering the green sheet. They had more awareness of the team and this helped them to act appropriately and thus resiliently in the situation.
Individual competence
Resilience requires awareness of the situation and acting accordingly. In most cases, lack of awareness seemed to be the bottle neck. The team tried to improve its awareness and handling of case‐irrelevant verbal communication by making ‘silence when needed’ a common goal in the briefing and by evaluating it during sign‐out. Surprisingly, this hardly contributed to awareness of the needs of other team members. The team members rarely shared their need for silence (Table 4; Vignette 1).
Reminding each other of the need for silence to concentrate during the team briefing was done consistently. However, the evaluation during the sign‐out was performed less consistently. Sometimes, when the sign‐out was not performed with the whole team, the observer evaluated with individual team members or in small groups. It appeared that when asked individually, participants were more negative than when they had to give their evaluation in front of the team. Participants tended to trivialise the experience of disruptiveness of case‐irrelevant verbal communication in front of the team. This may have been the case when the surgeons stated during member checking that ‘small talk’ in the operating theatre was not harmful.
Several times, the anaesthetists asked explicitly for silence, yet conversations revealed that on several other occasions, they felt the need for it but did not ask for it. Vignette 2 shows how the distracted anaesthesia team was speaking up. First, by requesting help, later by saying “we have to take care that we are not going to be in each other’s way.” In Vignettes 1 and 3, the surgeon and nurse kept quiet about their need for silence, as did Surgeon H in Extract 2. If a team member does not share his or her need for silence, it becomes more difficult for the rest of the team to become aware of it and act accordingly.
When asked why they kept quiet about their need for silence, participants’ answers were in line with those from Vignette 1. They said they did not want to damage relations or their image. Apparently, one feels the expectation of being able to perform in a context with case‐irrelevant verbal communication. Hence, it is framed as a matter of individual competence.
Discussion
In all comparable studies [3, 12], case‐irrelevant verbal communication formed a substantial proportion of distractors. Phones, pagers and door movements came next. Other studies confined themselves to the surgical phase: incision‐to‐closure. In this study, impact scored systematically lower than in other studies without affecting the relative importance of the categories of interruption and distraction (Fig. 1).
Figure 1.
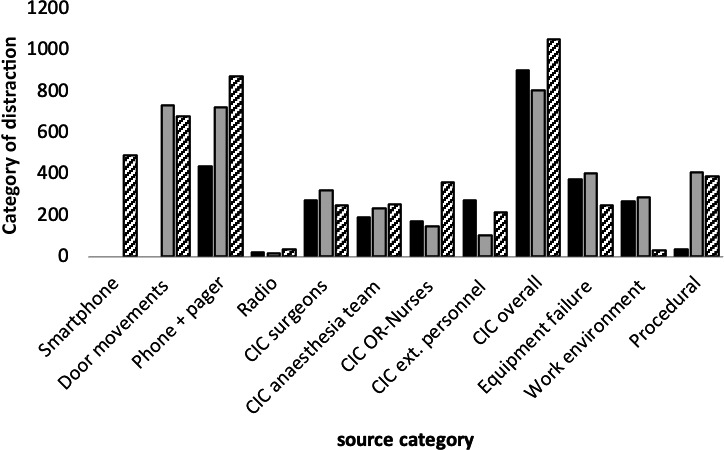
Relative importance of the distractors during incision to closure in three studies. Interference (frequency x impact) during surgery caused by different sources as measured in the studies by Healey et al. [12] ( ), Antoniadis et al. [3] (
), Antoniadis et al. [3] ( ), Van Harten et al. [this paper] (
), Van Harten et al. [this paper] ( ). Healey et al. did not count door movements. Smartphones were not counted in earlier studies. The pattern in all studies is similar. CIC, case‐irrelevant communication.
). Healey et al. did not count door movements. Smartphones were not counted in earlier studies. The pattern in all studies is similar. CIC, case‐irrelevant communication.
We found that case‐irrelevant verbal communication and smartphone usage persist in the operating theatre because they fulfil a physical need to stay active and a psychological need to feel comfortable in the team in phases with low work‐loads. This is in keeping with previous suggestions that sitting next to others, doing nothing and saying nothing may precipitate tension [20]. It is also in keeping with earlier findings that conversations and jokes maintain relationships and minimise tension whilst still achieving goals [19], for example, when a waiting consultant makes a joke to relax a nurse. In turn, the nurse will be more inclined to return a favour later on, for example, by staying longer or speeding up.
Contrasting the quantitative with the qualitative observations revealed that case‐irrelevant verbal communication and smartphone usage have high mean interference scores, but that this does not necessarily reflect their experienced disruptiveness in a given situation. Case‐irrelevant verbal communication is not always disruptive, and some teams handled it well, but most did not, mainly due to a lack of awareness of the needs of other sub‐teams. This lack of awareness is fed by cultural divisions between sub‐teams and maintained by keeping quiet about participants’ own need for silence due to the prevailing culture of individual competence. The example of the resilient team shows that it is possible to bridge these divisions and profit from the positive functions of case‐irrelevant verbal communication, whilst avoiding the disruptive consequences.
There are several topics where our findings differ from earlier research on distractions, where almost all were quantitative and most of the time restricted to one sub‐team. We argue that our methods and scope of the team enabled us to generate some understandings that quantitative research focused on a single sub‐team could not. First, earlier research focused mainly on the relationship between distractions and performance or outcome. Most studies, but not all, favour silence. Our ethnographic method enabled us to understand why case‐irrelevant verbal communication and smartphone usage occur, or what function they fulfil. The understanding that one needs something to stay active and to feel socially comfortable during periods of low work‐load, leads us to conclude that it is not practical to prevent case‐irrelevant verbal communication, unless one has an alternative that would fill the void.
Second, team members can effectively adjust to the need for concentration, and case‐irrelevant communication is not always disruptive [21]. However, in this study only case‐irrelevant communication was observed within the scrub team from incision to closure. We rarely observed that sub‐teams adjusted to other sub‐teams, and consequently, case‐irrelevant verbal communication was often disruptive. More importantly, our study implies that an observation instrument measuring the interference of distractors generates an illusion of precision. We found that the interference criterion did not match the experienced disruptiveness. Disruptiveness of case‐irrelevant verbal communication depended on: timing; volume; distance; content; simultaneity of other distractors; availability of help; and the scope of the team. This complexity cannot be built into an observation tool. However, the researchers found the use of ethnography useful, in that the reflections of the team showed what distractors really mattered. For example, a new type of distractor came to the front: a change of surgeon or when a surgeon leaves during the operation.
Third, the concept of a ‘sterile cockpit’ has been advocated as a potential remedy against noise during critical phases of a procedure, such as induction of anaesthesia [5]. We argue that initiatives such as this apply very well to predictable phases. However, there are other critical phases that are less predictable and these events are different for different procedures and individuals [22]. In informal interviews, we observed that team members did not always ask for a ‘silent cockpit’ in unpredictable events, although as a team they agreed to do so.
Finally, our ethnographic approach gave us a holistic lens on the team and its cultural context, in which participants keep quiet about their need for silence. The arguments participants gave for not asking for silence came up in a study on barriers for speaking up [23]. The question of why team members, especially surgeons, feel it would hurt their relations or image has been addressed at length by others [24, 25, 26]. They describe the surgical culture as one of individual competence, the ability to operate effectively and efficiently. In a culture that unconsciously favours individual competence to perform optimally under any circumstances, it may not be possible to ask for silence from the whole team. Campbell et al. state “distractions are common in anaesthetic practice and managing them is a key professional skill which appears to be part of the tacit knowledge of anaesthesia” [7]. We advocate adding a team perspective and organisational culture perspective to the professional skills perspective. If teams bridge their professional and cultural boundaries and develop mutual performance monitoring and mutual help, as in Vignette 4, they develop resilient behaviour in predictable and unpredictable situations.
Our study has important implications for clinical practice. Efforts to reduce disruptive distractions should not focus on new rules or training, but should instead stimulate situational awareness and mutual performance monitoring [27]. This perspective is in line with the Safety‐II approach [28, 29]. This advocates learning from daily practice, as that provides daily feedback and offers the opportunity to develop new habits and routines. Therefore, learning to handle case‐irrelevant verbal communication and smartphone usage might be a valuable exercise in developing resilience or, more specifically, a habit of cross‐monitoring and mutual help. That habit will help in handling rare life‐threatening situations as well.
Regarding future research, quantitative observation might be useful to facilitate local reflections. But to further our understanding more broadly, there should be more participative action research methodology, to understand how we can bridge cultural borders and develop resilience. We might even need to rethink the concept of quality of care [30]. We note that different research methodologies in the field of quality and safety are now available and hope to have made a valuable contribution to that line of research.
Supporting information
Appendix S1. Tool to identify intra‐operative workflow interruptions.
Acknowledgements
The authors thank D. van den Hurk for helping with data collection and participating in the interpretation, and L. Fluit for helping with the qualitative analysis. No external funding or competing interests declared.
This article is accompanied by an Editorial by Shelton and Smith, Anaesthesia 2021; 76: 305–8.
Contributor Information
A. van Harten, Email: annetvanharten@me.com, @annetvanh.
H. G. Gooszen, @HeinGooszen.
J. J. Koksma, @JurKoksma.
T. J. H. Niessen, @Theoniessen.
References
- 1. Jones CPL, Fawker‐Corbett J, Groom P, et al. Human factors in preventing complications in anaesthesia: a systematic review. Anaesthesia 2018; 73(S1): 12–24. [DOI] [PubMed] [Google Scholar]
- 2. Wiegmann DA, ElBardissi AW, Dearani JA, et al. Disruptions in surgical flow and their relationship to surgical errors: an exploratory investigation. Surgery 2007; 142: 658–65. [DOI] [PubMed] [Google Scholar]
- 3. Antoniadis S, Passauer‐Baierl S, Baschnegger H, et al. Identification and interference of intraoperative distractions and interruptions in operating rooms. Journal of Surgical Research 2014; 188: 21–9. [DOI] [PubMed] [Google Scholar]
- 4. Wheelock A, Suliman A, Wharton R, et al. The impact of operating room distractions on stress, workload, and teamwork. Annals of Surgery 2015; 261: 1079–84. [DOI] [PubMed] [Google Scholar]
- 5. Broom MA, Capek AL, Carachi P, et al. Critical phase distractions in anaesthesia and the sterile cockpit concept. Anaesthesia 2011; 66: 175–9. [DOI] [PubMed] [Google Scholar]
- 6. Savoldelli GL, Thieblemont J, Clergue F, et al. Incidence and impact of distracting events during induction of general anaesthesia for urgent surgical cases. European Journal of Anaesthesiology 2010; 27: 683–9. [DOI] [PubMed] [Google Scholar]
- 7. Campbell G, Arfanis K, Smith AF. Distraction and interruption in anaesthetic practice. British Journal of Anaesthesia 2012; 109: 707–15. [DOI] [PubMed] [Google Scholar]
- 8. Zheng B, Martinec DV, Cassera MA, et al. A quantitative study of disruption in the operating room during laparoscopic antireflux surgery. Surgical Endoscopy 2008; 22: 2171–7. [DOI] [PubMed] [Google Scholar]
- 9. Westbrook JI, Coiera E, Dunsmuir WTM, et al. The impact of interruptions on clinical task completion. British Medical Journal Quality and Safety 2010; 19: 284–9. [DOI] [PubMed] [Google Scholar]
- 10. Li SY, Magrabi F, Coiera E. A systematic review of the psychological literature on interruption and its patient safety implications. Journal of the American Medical informatics Association 2012; 19: 6–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Boehm‐Davis DA, Remington R. Reducing the disruptive effects of interruption: a cognitive framework for analysing the costs and benefits of intervention strategies. Accident Analysis and Prevention 2009; 41: 1124–9. [DOI] [PubMed] [Google Scholar]
- 12. Healey AN, Sevdalis N, Vincent CA. Measuring intra‐operative interference from distraction and interruption observed in the operating theatre. Ergonomics 2006; 49: 589–604. [DOI] [PubMed] [Google Scholar]
- 13. Myers RA, McCarthy MC, Whitlatch A, et al. Differentiating between detrimental and beneficial interruptions: a mixed‐methods study. British Medical Journal Quality and Safety 2016; 25: 881. [DOI] [PubMed] [Google Scholar]
- 14. Coiera E. The science of interruption. BMJ Quality and Safety 2012; 21: 357–60. [DOI] [PubMed] [Google Scholar]
- 15. Grundgeiger T, Dekker S, Sanderson P, et al. Obstacles to research on the effects of interruptions in healthcare. BMJ Quality and Safety 2016; 25: 392–5. [DOI] [PubMed] [Google Scholar]
- 16. Gold RL. Roles in sociological field observations. Social Forces 1958; 36: 217–23. [Google Scholar]
- 17. Lincoln YS, Guba EG. Naturalistic inquiry. Beverly Hills: CA: Sage Publications, 1985. [Google Scholar]
- 18. Abma TA, Stake RE. Stake's responsive evaluation: core ideas and evolution. New Directions for Evaluation 2001; 2001: 7–22. [Google Scholar]
- 19. Lingard L, Reznick R, Espin S, et al. Team communications in the operating room: talk patterns, sites of tension, and implications for novices. Academic Medicine 2002; 77: 232–7. [DOI] [PubMed] [Google Scholar]
- 20. Goffman E. The presentation of self in everyday life. Harmondsworth: Penguin, 1971. [Google Scholar]
- 21. Widmer LW, Keller S, Tschan F, et al. More than talking about the weekend: content of case‐irrelevant communication within the or team. World Journal of Surgery 2018; 42: 2011–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Wadhera RK, Parker SH, Burkhart HM, et al. Is the "sterile cockpit" concept applicable to cardiovascular surgery critical intervals or critical events? The impact of protocol‐driven communication during cardiopulmonary bypass. Journal of Thoracic and Cardiovascular Surgery 2010; 139: 312–9. [DOI] [PubMed] [Google Scholar]
- 23. Beament T, Mercer SJ. Speak up! Barriers to challenging erroneous decisions of seniors in anaesthesia. Anaesthesia 2016; 71: 1332–40. [DOI] [PubMed] [Google Scholar]
- 24. Jin CJ, Martimianakis MA, Kitto S, et al. Pressures to “measure up” in surgery: managing your image and managing your patient. Annals of Surgery 2012; 256: 989–93. [DOI] [PubMed] [Google Scholar]
- 25. Orri M, Farges O, Clavien P‐A, et al. Being a surgeon—the myth and the reality: a meta‐synthesis of surgeons' perspectives about factors affecting their practice and well‐being. Annals of Surgery 2014; 260: 721–8. [DOI] [PubMed] [Google Scholar]
- 26. Bosk CL. Forgive and remember: managing medical failure, 2nd edn Chicago: The University of Chicago Press, 2003. [Google Scholar]
- 27. Rutherford JS. Monitoring teamwork: a narrative review. Anaesthesia 2017; 72(S1): 4–94. [DOI] [PubMed] [Google Scholar]
- 28. Smith AF, Plunkett E. People, systems and safety: resilience and excellence in healthcare practice. Anaesthesia 2019; 74: 508–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Hollnagel E. Safety‐I and safety‐II: the past and future of safety management. Boca Raton, FL: Taylor and Francis, 2014. [Google Scholar]
- 30. Koksma JJ, Kremer JAM. Beyond the quality illusion: the learning era. Academic Medicine 2019; 94: 166–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Tool to identify intra‐operative workflow interruptions.


