Abstract
Background:
Despite the health benefits of physical activity, many women remain inactive and the needs of rural women are understudied.
Purpose:
To understand access to physical activity barriers, opportunities, and intervention preferences in rural women and determine how these differ by self-reported activity level.
Methods:
A mailed questionnaire was distributed to 900 rural women and included measures of physical activity, health status, barriers, opportunities for exercise, and preferences for intervention type, components, and delivery.
Results:
Questionnaires were completed by 507 women; 72.0% reported meeting the physical activity guideline. Inactive women reported greater barriers to activity (higher scores on 18 of 22 barriers; p<.05), less access to or usage of 8 of 9 places to exercise (p<.05), and less belief in the relevance of physical activity to personal health (p<.001). Both inactive and active women were most interested in programs that use walking, yoga, or strength training.
Conclusions:
Physical activity interventions for rural women need to address their specific needs, including barriers to physical activity and lower access to places in which to be physically active.
Keywords: Exercise, Barriers, Epidemiology, Health promotion, Health behavior
Introduction
Despite the benefits of a physically active lifestyle, most US women remain insufficiently active. Estimates from self-reported data show that only 46% of women report meeting the aerobic physical activity guideline of 150 minutes per week of moderate-to-vigorous intensity physical activity (Centers for Disease Control and Prevention, 2014). When direct measurement via accelerometers is used, less than 10% of women are estimated to meet the guideline (Troiano et al., 2008). Furthermore, data from the National Health and Examination Survey (NHANES) show that physical activity patterns differ for rural vs. urban adults (Fan, Wen, & Kowaleski-Jones, 2014). For example, rural individuals report more household physical activity but less vigorous-intensity activity than do those in urban areas (Fan et al., 2014). Additionally, rural adults have higher prevalence of obesity relative to urban adults (Befort, Nazir, & Perri, 2012), meaning that physical activity is of particular importance in rural populations given its role in helping maintain energy balance and reducing risk of chronic diseases such as diabetes, cardiovascular disease, and cancer (Colberg et al., 2016; Lobelo et al., 2018; Moore et al., 2016).
The rural United States includes 60 million individuals--nearly 1 in 5 US residents. In our efforts to promote physical activity and reverse the obesity epidemic, it is critical that we increase our attention to rural communities with a focus on understanding and addressing their specific needs. In particular, given that women are less active than men at all ages (Keadle et al., 2016; Troiano et al., 2008), it is important to understand how the specific characteristics of rural life may influence women’s access to physical activity opportunities as well as their preferences and needs for physical activity programming. There is growing recognition for the importance of understanding physical activity determinants and barriers in rural populations (Lo et al., 2017; Marshall et al., 2013; Park et al., 2017; Peterson et al., 2013; Zimmermann et al., 2016). However, specific research is needed to understand the perceptions and barriers for rural women, and what they want and need from an intervention.
This purpose of this cross-sectional study was to understand inactive and active rural women’s access to physical activity opportunities, their preferences for specific intervention components/characteristics, and barriers to physical activity.
Methods
Participants and recruitment
Participants were recruited from women who had previously participated in the Survey of the Health of Wisconsin (SHOW), an annual population-based cross-sectional survey of multiple determinants of the health. The methods of SHOW have been described previously (Nieto et al., 2010). Briefly, SHOW gathers health-related data on representative samples of state residents and communities. Two-stage cluster sampling is used to select households and recruit approximately 800-1,000 participants per year. Recruitment and initial interviews are done at the household; additional interviews and physical exams are conducted at permanent or mobile examination centers. For this ancillary study, SHOW provided a sampling frame of 900 rural women aged 18-74 who, during their previous participation in SHOW, agreed to be contacted for future studies. To select the sampling frame, rural residence was established based on the US Census urban and rural designations. Specifically, urban areas are those that meet minimum requirements regarding population density plus adjacent areas with lower population density. These are further subdivided into “urbanized areas” (population ≥50,000) and “urban clusters” (population 2,500-49,999). Rural areas are the remaining, low-density blocks with populations <2,500 (U.S. Census Bureau, 2015). Potential participants were mailed a postcard notifying them of the project and alerting them to expect the questionnaire to arrive in the mail. Two weeks later, the questionnaire was mailed along with a personalized cover letter, $2 cash incentive and a pre-stamped return envelope. From the initial postcard mailing, 77 participants were no longer at eligible for the study (deceased, moved, no forwarding address) to give a sampling frame of 823 for the questionnaire. If no response was received within two weeks, the questionnaire and return envelope were sent a second time. No incentive was included in the second mailing.
Measures
Participant characteristics.
Participants reported their age, work status (full-time, part-time, not employed outside home), and occupational activity level (high, moderate, low, not applicable). Physical activity levels and sitting time were estimated using the International Physical Activity Questionnaire (IPAQ) – Short Form (Craig et al., 2003). Physical activity volume (MET-hrs/week) was calculated with assigned MET levels of 8.0 METs for vigorous-intensity activity, 4.0 METs for moderate-level activity, and 3.3 METs for walking. Activity volume at or greater than 10.0 MET-hrs/week was considered to meet the physical activity guideline of 150 minutes per week (US Department of Health and Human Services, 2018). The two-part EuroQOL instrument was used to measure health status. The first component (EQ-5D-3L) was a 5-item scale that asked participants to rate their health with respect to the domains of mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. The second component was a visual analog scale (EQ-VAS), in which participants rate their current health state on a scale from 0 (worst imaginable health state) to 100 (best imaginable health state) (van Reenan, 2005; Whynes & Group, 2008). Technology use was assessed because it is critical for understanding the degree to which a population is equipped to take part in technology-based components that may be part of a future intervention. Items included (a) availability and type of home internet access, (b) type of cell phone (none, traditional flip phone, smartphone), (c) for those with a smartphone, what activities it was used for (texting, email, calendar, browsing the internet, photos/videos, social media) and use of physical activity tracking devices (Fitbit tracker, other brand of web-connected tracker, basic step-counting pedometer). These items were adapted from those used in our previous research (Cadmus-Bertram et al., 2015a; Cadmus-Bertram et al., 2015b).
Access to places to be physically active.
Self-reported access to nine well-established features of the built environment known to promote physical activity was also assessed via questionnaire (Sallis, 2009). These were: sidewalks/paths near home, sidewalks/paths near work, trails or other nature areas, gyms, schools (including gym at a school), community centers, parks, swimming pools, and areas to exercise within the home. Response categories were “Yes, and I use it,” “Yes, but I don’t use it,” “No,” and “I don’t know.”
Interest in and preferences for physical activity intervention programming.
Participants used 5-point Likert scales to rate the perceived importance of physical activity to their own health, as well as their interest level in joining a hypothetical physical activity program “assuming that it fit with your schedule, location, and preferences.” A checklist was used to indicate reasons why they would join a physical activity program: health improvement, weight loss, increase energy levels, support and motivation for physical activity, the desire to meet new people, or some other reason. Participants then indicated up to three preferred delivery modes for physical activity intervention programming from the following list: smartphone app, mail-based, email, text messages, social media, telephone coaching, in-person group-based program. They also indicated preferred type(s) of activity: walking, jogging/running, bicycling, weights/strength training, stretching/yoga, group aerobics classes, other). Finally, they used a 5-point Likert scales to rate the importance of individual support provided by a coach and preference for 16 potential program characteristics/features.
Barriers to physical activity.
Participants rated 23 potential barriers to physical activity on a 5-point scale ranging from (“not at all a barrier” to “very much so a barrier”). After rating each potential barrier, participants were asked to circle the three factors that were the biggest barriers for them. Potential barriers were selected based on previous literature (Marcus & Forsyth, 2008); additional items specific to the rural context (e.g., fear of safety due to wild animals) were added based on data from unpublished focus groups.
Statistical analyses
Analyses were conducted in SAS 9.4 (Cary, NC). Data were summarized as means with standard deviations, frequencies, and percentages. The prevalence of meeting physical activity guideline was calculated using the IPAQ-SF standardized scoring method with participants reporting equal to or greater than 600 MET-minutes/week of physical activity. Chi-square tests were used to investigate differences by category of meeting or not meeting federal activity guidelines. T-tests were used to test group mean differences across discrete categorical variables. Analyses of variance (ANOVA) was used for multi-level categorical variables to test if categorical means were different across levels of the variables. Significance was set at p< 0.5, two-sided.
Results
Questionnaires were completed by 507 women for a completion rate of 61.6%. Characteristics of the sample are provided in Table 1. On average, participants were 54.6 years of age (SD=12.9) with a body mass index of 29.2 (SD=7.2). The majority were of white race (95.3%), married or living with a partner (78.9%), and employed outside the home (61.2%). Over a third (38.1%) had a college degree or higher. Seventy-two percent reported physical activity levels that met or exceeded the guideline of 150 min/week (≥10.0 MET hours/week). Inactive women (those not meeting the guideline) were less likely to report higher levels of occupational physical activity (p=.01) and had lower self-rated health on both the 5-item scale (p<.0001) and the visual analog scale component (p<.0001) of the EuroQOL assessment. Small but significant differences were observed in cell phone use, with inactive women less likely to be using a smartphone vs. a flip-phone (p<.05). Likewise, inactive women were less likely to report use of a consumer-grade accelerometer-based tracker (such as a Fitbit) (p<.03), although they did not differ from their more active counterparts with respect to use of basic pedometers.
Table 1.
Characteristics of questionnaire respondents, overall and stratified by meeting vs. not meeting aerobic PA guideline.
| Total sample |
Meeting PA guideline | p- value |
||
|---|---|---|---|---|
| Yes | No | |||
| Mean (SD) or % |
Mean (SD) or % |
Mean (SD) or % |
||
| N | 507 | 370 | 137 | |
| Age in years | 54.6 (12.9) | 54.0 (12.9) | 56.2 (12.9) | .10 |
| Body mass index (kg/m2) | 29.2 (7.0) | 28.5 (6.5) | 31.2 (8.0) | .0002 |
| Race (white alone) | 483 (95.3%) | 350 (94.6%) | 133 (97.0%) | .781 |
| College degree | 193 (38.1%) | 156 (42.2%) | 37 (27.0%) | .002 |
| Married or cohabitating w/ partner | 400 (78.9%) | 287 (77.6%) | 113 (82.5%) | .68 |
| Work status | .19 | |||
| Full-time | 236 | 173 (46.8%) | 63 (46.0%) | |
| Part-time | 94 | 75 (20.3%) | 19 (13.8%) | |
| Not employed outside home | 173 | 120 (32.4%) | 53 (38.7%) | |
| Self-rated occupational activity | .01 | |||
| High | 65 (12.8%) | 54 (14.6%) | 11 (8.0%) | |
| Moderate | 121 (23.8%) | 96 (26.0%) | 25 (18.3%) | |
| Low | 125 (24.6%) | 81 (21.9%) | 44 (32.1%) | |
| N/A (not employed outside home) | 196 (38.7%) | 129 (37.6%) | 57 (41.6%) | |
| MVPA (MET-hrs/week) | 72.1 (105.9) | 85.1 (111.2) | 5.5 (2.9) | <.0001 |
| Sitting time (hrs/week) | 5.8 (5.1) | 5.7 (5.7) | 6.2 (3.1) | .26 |
| Health status (EuroQOL EQ-5D_3L) a | 6.3 (1.5) | 6.1 (1.4) | 6.8 (1.8) | <.0001 |
| Self-rated health (EuroQOL EQ-VAS) | 72.3 (16.6) | 74.3 (16.1) | 66.9 (16.8) | <.0001 |
| Internet access | .47 | |||
| Broadband | 294 (58.0%) | 222 (60.0%) | 72 (52.5%) | |
| Cell company data plan | 159 (32.8%) | 117 (32.8%) | 42 (32.6%) | |
| Dial-up | 6 (1.2%) | 4 (1.1%) | 2 (1.5%) | |
| Unsure of type | 72 (14.8%) | 51 (14.3%) | 21 (16.3%) | |
| None | 30 (6.2%) | 18 (5.1%) | 12 (9.3%) | |
| Cell phone | .048 | |||
| Smartphone | 402 (79.3%) | 297 (80.3%) | 105 (76.6%) | |
| Traditional cell (e.g., flip phone) | 78 (15.4%) | 50 (13.5%) | 28 (20.4%) | |
| None | 14 (2.8%) | 13 (3.5%) | 1 (0.7%) | |
| Use of devices to track activity/weight | ||||
| Accelerometer-based tracker | 173 (34.1%) | 136 (36.8%) | 37 (27.0%) | .03 |
| Basic step-counting pedometer | 270 (53.3%) | 199 (53.8%) | 71 (51.8%) | .70 |
Index measure of 5 domains; scores range from 5-15. Higher scores reflect worse QOL.
Note: Proportion of missing values ranges from 1.8 – 15.8%
Access to places to be physically active
Broad differences were observed between inactive vs. active women with respect to access to and usage of, various opportunities for exercise (Table 2). Inactive women were significantly less likely to report access/usage of sidewalks/paths both near home (p=.03) and work (p=.02), trails and other nature areas (p<.0001), gyms (p<.001), schools (p<.04), parks (p=.02), swimming pools (p=.01), and within the home (p=.02). The only facility rated similarly between the groups was community centers, with most women either lacking access or being unsure of their access. A substantial proportion of participants (65.1% of inactive and 54.1% of active women) lacked sidewalks or paths near their home.
Table 2.
Access to, and usage of, places to exercise among inactive and active rural women.
| Meeting PA guideline |
p-value | ||
|---|---|---|---|
| No | Yes | ||
| Sidewalks/paths near home | .03 | ||
| Yes, and I use it | 30 (23.3%) | 134 (37.5%) | |
| Yes, but I don’t use it | 14 (10.9%) | 29 (8.1%) | |
| No | 84 (65.1%) | 193 (54.1%) | |
| Unsure | 1 (0.8%) | 1 (0.3%) | |
| Sidewalks/paths near work | .02 | ||
| Yes, and I use it | 16 (13.7%) | 83 (25.7%) | |
| Yes, but I don’t use it | 35 (13.7%) | 84 (26.0%) | |
| No | 60 (51.2%) | 150 (46.4%) | |
| Unsure | 6 (5.1%) | 6 (1.9%) | |
| Trails or other nature areas | <.0001 | ||
| Yes, and I use it | 25 (19.4%) | 162 (46.0%) | |
| Yes, but I don’t use it | 55 (42.6%) | 98 (27.8%) | |
| No | 45 (34.9%) | 90 (25.6%) | |
| Unsure | 4 (3.1%)) | 2 (0.6%) | |
| Gym | <.0001 | ||
| Yes, and I use it | 10 (7.6%) | 88 (24.7%) | |
| Yes, but I don’t use it | 68 (51.9%) | 174 (48.7%) | |
| No | 50 (38.2%) | 93 (26.1%) | |
| Unsure | 3 (2.3%) | 2 (0.6%) | |
| School | .004 | ||
| Yes, and I use it | 4 (3.2%) | 23 (6.6%) | |
| Yes, but I don’t use it | 52 (40.9%) | 185 (53.2%) | |
| No | 52 (40.9%) | 117 (33.6%) | |
| Unsure | 19 (15.0) | 23 (6.6%) | |
| Community center | .19 | ||
| Yes, and I use it | 3 (2.3%) | 9 (2.6%) | |
| Yes, but I don’t use it | 24 (18.8%) | 98 (28.1%) | |
| No | 84 (65.6%) | 207 (59.3%) | |
| Unsure | 17 (13.3%) | 35 (10.0%) | |
| Local park | .02 | ||
| Yes, and I use it | 14 (10.8%) | 84 (23.8%) | |
| Yes, but I don’t use it | 74 (56.9%) | 169 (47.9%) | |
| No | 39 (30.0%) | 93 (26.4%) | |
| Unsure | 3 (2.3%) | 7 (2.0%) | |
| Swimming pool | .01 | ||
| Yes, and I use it | 8 (6.2%) | 48 (13.6%) | |
| Yes, but I don’t use it | 39 (30.0%) | 137 (38.9%) | |
| No | 77 (59.2%) | 159 (45.2%) | |
| Unsure | 6 (4.6%) | 8 (2.3%) | |
| Within my home | .02 | ||
| Yes, and I use it | 48 (37.5%) | 183 (52.3%) | |
| Yes, but I don’t use it | 43 (33.6%) | 78 (22.3%) | |
| No | 35 (27.3%) | 87 (24.9%) | |
| Unsure | 2 (1.6%) | 2 (0.6%) | |
Note: Missing values: 4.1%-6.3%,” except sidewalks/paths near work (13.2% missing.
Preferences for physical activity programs
Although inactive women rated physical activity as less important to their own health (p<.0001), both inactive and active women had similar levels of interest in a physical activity intervention (Table 3). Across both groups, 75.8% expressed that they were at least “somewhat interested” in partaking in a program. No significant differences by activity level were observed in reasons for interest in joining a physical activity program – the majority of women cited a desire to improve their health, lose weight, and increase energy. Likewise, inactive and active women did not differ in preferences for physical activity type or delivery mode (Figure 1). Overall, the most preferred activities were walking (chosen by 79.1% of all participants), yoga (63.3%), and strength training (47.8%). Preferred delivery modes were an in-person group program (chosen by 59.7% of all participants), a smartphone app (33.7%), and printed materials in the mail (28.9%). Both inactive and active women rated individualized coaching as moderately important. With respect to preference for specific intervention components, both inactive and active women were highly interested in home-based programs and those tailored to women at their own stage of life.
Table 3.
Preferences for physical activity programming.
| Meeting PA Guidelines |
p-value | ||
|---|---|---|---|
| No | Yes | ||
| Importance of physical activity to personal healtha | <.0001 | ||
| Not at all important | 1 (0.7%) | 0 (0%) | |
| Not very important | 1 (0.7%) | 4 (1.1%) | |
| Somewhat important | 42 (30.7%) | 52 (14.1%) | |
| Important | 59 (43.1%) | 146 (39.7%) | |
| Very important | 34 (24.8%) | 166 (45.1%) | |
| Interest in joining a physical activity intervention assuming fit with schedule/location/preferencesb | |||
| .80 | |||
| Not at all interested | 14 (10.7%) | 38 (10.4%) | |
| Not very interested | 18 (13.7%) | 50 (13.7%) | |
| Somewhat interested | 42 (32.1%) | 104 (28.5%) | |
| Interested | 25 (19.1%) | 89 (24.4%) | |
| Very interested | 32 (24.4%) | 84 (23.0%) | |
| Reasons for joining a physical activity programc | |||
| Improve health | 98 (82.7%) | 267 (80.9%) | .99 |
| Lose weight | 94 (77.7%) | 235 (71.2%) | .15 |
| Increase energy | 89 (73.6%) | 232 (70.3%) | .48 |
| Support and motivation for PA | 45 (37.1%) | 146 (44.1%) | .16 |
| Meet new people | 28 (23.1%) | 74 (22.4%) | .80 |
| Other | 6 (5.0%) | 19 (5.8%) | .99 |
| Preferred delivery mode (Check up to 3)d | |||
| A group program that meets in person | 72 (63.7%) | 190 (58.4%) | .32 |
| A smartphone-based app | 31 (27.4%) | 117 (35.9%) | .11 |
| Printed materials in the mail | 33 (29.2%) | 94 (28.8%) | .99 |
| 25 (22.1%) | 75 (23.0%) | .89 | |
| Text messages | 17 (15.0%) | 65 (19.9%) | .27 |
| Phone calls with an individual coach | 14 (12.4%) | 43 (13.2%) | 1.00 |
| Social media | 11 (9.7%) | 39 (12.0%) | .61 |
| Preferred activities (Multi-check)e | |||
| Walking | 109 (83.2%) | 282 (77.7%) | .21 |
| Yoga | 82 (62.6%) | 231 (63.6%) | .83 |
| Strength training | 54 (41.2%) | 182 (50.1%) | .08 |
| Biking | 42 (32.1%) | 143 (39.4%) | .14 |
| Group aerobics class | 37 (28.2%) | 123 (33.9%) | .28 |
| Running | 15 (11.5%) | 63 (17.4%) | .13 |
| Importance of individual support from a coach? | |||
| Mean score (1-5 scale) | 2.9 (1.2) | 2.9 (1.1) | .77 |
Proportion of missing values: 0.4%
Proportion of missing values: 2.2%
Proportion of missing values ranges from 10.8-11.2%
N’s are the number of participants who indicated at least one preference. Percentages are calculated using these Ns as a denominator. Percentages sum to >1 within each column because participants could choose more than one option.
Proportion of missing values: 2.6%
Figure 1.
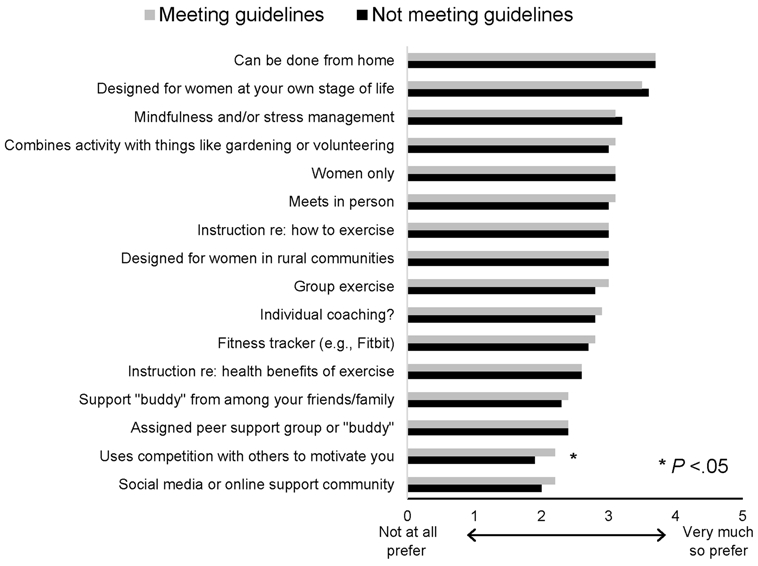
Preferences for specific components of a physical activity intervention among active and inactive women.
Barriers to physical activity
Inactive and active women largely agreed about which barriers were most problematic (Figure 2). The top three barriers in each group were the same: lack of motivation, tiredness, and problems posed by winter weather. However, 18 of the 22 potential barriers were rated as more problematic by inactive vs. active women (p<.05 for all). No significant differences were reported for fear of safety due to crime (p=.06), lack of time due to caregiving for children (p=.19), and lack of time due to chores and/or housework (p=.06). Cost was the only barrier that was rated as less problematic by inactive vs. active women (p=.0002).
Figure 2.
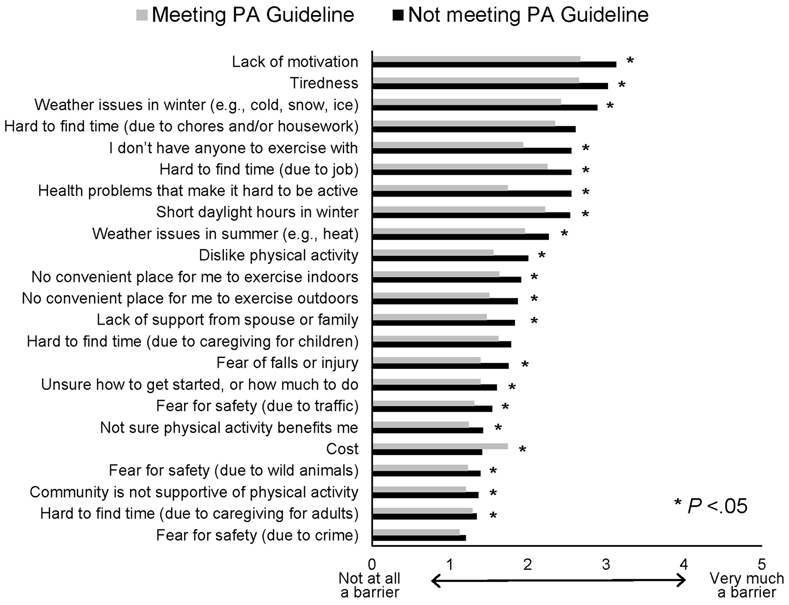
Barriers to physical activity among active and inactive women.
Discussion
The results of this study are relevant to researchers and public health officials interested in understanding and promoting physical activity among women living in rural communities. The first important finding pertains to the ability to access opportunities for physical activity. With the exception of community centers, to which a majority of all women reported no access, those who were inactive reported less access to or usage of eight common places to exercise. These support the findings of Kegler et al., who found that in a sample of African-American and Caucasian women in the rural US south, many lacked access to what in urban settings are traditionally considered places or features that promote exercise (Kegler et al., 2012). The relevance of specific components of the environment is not always clear in different contexts, particularly for rural women. For example, lack of access to sidewalks or paths near the home may pose a large obstacle for a woman who lives on a busy county highway, but not be as problematic for one who lives on a low-traffic street within a small town. In the former case, walking on the shoulder of the road is likely dangerous, particularly in the winter when daylight hours are short and conditions are slippery. In the latter case, walking on the side of the road may be safe and pleasant. The majority of women did have access to a private gym, although most did not use it. Similarly, most women indicated that they could exercise within their home, although most currently did not do so. These settings, along with schools and parks, are potential opportunities for implementation of physical activity interventions.
Perhaps surprisingly, while inactive women placed less belief than active women in the relevance of physical activity to personal health, both inactive and active women had similar preferences for the components of physical activity interventions. Both strongly endorsed interventions that are designed for women only and/or women at their own stage of life. For example, program content could be tailored to address the specific needs and concerns of women with young children, those experiencing the menopausal transition, or older women who are concerned with maintaining physical function and reducing risk of falls. Age-specific approaches were also identified as important in a qualitative study of rural Montana residents, although in that sample the concerns were largely specific to in-person interventions (i.e., greater comfort level exercising with one’s peer age group vs. those much younger) (Lo et al., 2017). Women strongly endorsed the incorporation of home-based programs and in-person approaches, suggesting that interventions may be most successful when women have flexibility to choose to exercise either alone or with others.
We were also interested in learning about women’s level of interest in using technology as part of a physical activity intervention. Reaching rural populations can be difficult, particularly for those who are in highly rural or geographically isolated areas. Technology can help solve this problem by remotely delivering intervention content and assisting with self-monitoring and assessment; it can also make it easier to scale up the intervention. Technologies such as fitness trackers and apps offer numerous opportunities for physical activity promotion (Phillips et al., 2018). While a smartphone app was among the most popular options for intervention delivery method, there was only moderate support for use of fitness trackers, and low-to-moderate support for social media approaches. Similarly, women – and particularly those who were inactive -- expressed only low-to-moderate enthusiasm for interventions that use competition with others as a form of motivation. Overall, the findings do not necessary discourage technology-based approaches but highlight the importance of taking time to ensure maximum comfort with the technology, educating participants about the benefits of the approach, and, when possible, providing opportunities for face-to-face interaction for those individuals who want it.
Our data show that while walking and yoga remain popular forms of physical activity among women, there is also quite strong interest in strength training. This is important given the cardiovascular and musculoskeletal benefits of strength training for women (Bocalini et al., 2009; Kamada et al., 2017). Although strength training still understudied in rural women specifically, there is initial evidence to suggest that it is well-accepted and is associated with benefits for self-image and health-related quality of life (Seguin et al., 2008; Seguin et al., 2013).
Both inactive and active women identified similar barriers to physical activity. At the same time, the perceived difficulty of these barriers was higher among inactive women compared to active women. The relative ranking of barriers was similar – both groups were most concerned about motivation, fatigue, and winter weather – but inactive women considered each barrier to be more problematic than did active women. The tendency for less active individuals to report greater barriers was also reported by Kurti et al. is a sample of men and women living in rural Florida (Kurti et al., 2015). One explanation is that inactive women are inactive in part, because they face objectively higher barriers. It is also possible that barriers are objectively similar (e.g., similar time constraints, fatigue, and weather barriers) between inactive vs. active women but inactive women perceive the barriers as more problematic. They may have attempted to overcome the barrier without success, or perhaps have not attempted to become more physically active yet. In contrast, by virtue of their experience being physically active, active women may have more confidence in their ability to overcome barriers. This would also explain why cost was a significantly higher barrier for active women – they may simply be more aware of the cumulative costs of exercise clothing, equipment, and/or gym memberships.
Major strengths of this study include the large sample size from a wide range of rural areas across Wisconsin and an excellent response rate to the questionnaire. In order to assess the generalizability of our data, we used data from the US Census Bureau’s American Community Survey to compared our sample characteristics to those of the general population of Wisconsin women aged 18-74. Relative to the general population, our sample was generally comparable with respect to race (95.3% white alone vs. 92.0% in the general population), employment status (65.6% working vs. 65.9% in general population), educational attainment (38.1% with a college degree vs. 29.0% in the general population), and marital status (78.9% married or living with a partner vs. 61.7% married in the general population). Although our sample was somewhat older than the general population (54.6 years vs. 47.5), this magnitude of difference is unlikely to be associated with major difference in the prevalence of physical activity (Tucker et al., 2011). Other strengths include (a) the timing of the questionnaire during the fall, which avoided the issues associated with assessing physical activity during the peak of either summer or winter weather, and (b) a detailed set of questions allowing us to gain specific information about what types of interventions are of interest. Limitations include (a) lack of device-based measurement (e.g., accelerometers), which likely resulted in over-estimation physical activity and (b) and constrained generalizability given that the characteristics of rural populations differ between geographic regions of the United States. However, Wisconsin tends to be generally representative of the US a whole with respect to physical activity and obesity (Centers for Disease Control and Prevention, 2014; Matthews et al., 2017).
In conclusion, this study provides detailed information for researchers or public health officials interested in promoting physical activity in rural women. Given the aging of the rural US population and the increasing prevalence of obesity, the role of physical activity and other modifiable risk factors will continue to be important for chronic disease risk and management. Specifically, it is essential to understand how to leverage the physical environment and community resources of rural areas. Rural communities vary widely – some have high social cohesion and attractive opportunities for outdoor exercise, whereas others have fewer opportunities. However, because rural communities all feature low population size and density, they typically cannot support the wide variety of physical activity programming that may be feasible in urban or suburban areas. Thus, interventions should be designed to be flexible so as to suit the needs of individuals at a range of ages and fitness levels, including those with chronic diseases and functional limitations.
Acknowledgments
Funding sources: This study was supported by the Virginia Horne Henry Committee. Dr. Cadmus-Bertram is supported by 1K07CA178870. The Survey of the Health of Wisconsin is supported by the Wisconsin Partnership Program grant #2791.
Footnotes
Conflicts of interest: The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
References
- Befort CA, Nazir N, & Perri MG (2012). Prevalence of obesity among adults from rural and urban areas of the United States: Findings from NHANES (2005-2008). Journal of Rural Health, 28(4), 392–397. doi: 10.1111/j.1748-0361.2012.00411.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bocalini DS, Serra AJ, dos Santos L, Murad N, & Levy RF (2009). Strength training preserves the bone mineral density of postmenopausal women without hormone replacement therapy. Journal of Aging and Health, 21(3), 519–527. doi: 10.1177/0898264309332839 [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau (2015). 2010 Census Urban and Rural Classification and Urban Area Criteria [WWW Document]. Last Revis. Febr. 09, 2015 Retrieved from https://www.census.gov/geo/reference/ua/urban-rural-2010.html [Google Scholar]
- Cadmus-Bertram LA, Marcus BH, Patterson RE, Parker BA, & Morey BL (2015). Randomized trial of a Fitbit-based physical activity intervention for women. American Journal of Preventive Medicine, 49(3), 414–418. doi: 10.1016/j.amepre.2015.01.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cadmus-Bertram L, Marcus BH, Patterson RE, Parker BA, & Morey BL (2015). Use of the Fitbit to measure adherence to a physical activity intervention among overweight or obese, postmenopausal women: Self-monitoring trajectory during 16 weeks. JMIR Mhealth Uhealth, 3(4), e96. doi: 10.2196/mhealth.4229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention (2014). Health Behaviors of Adults: United States, 2011-2014. Retrieved from https://ftp.cdc.gov/pub/Health_Statistics/NCHS/NHIS/SHS/2011-2014_AHB_Table_PA-1.pdf [Google Scholar]
- Centers for Disease Control and Prevention (2014). State Indicator Report on Physical Activity, 2014. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, … Tate DF (2016). Physical activity/exercise and diabetes: A position statement of the American Diabetes Association. Diabetes Care, 39(11), 2065–2079. doi: 10.2337/dc16-1728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Craig CL, Marshall AL, Sjostrom M, Bauman AE, Booth ML, Ainsworth BE, … Oja P (2003). International Physical Activity Questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise, 35(8), 1381–1395. doi: 10.1249/01.MSS.0000078924.61453.FB [DOI] [PubMed] [Google Scholar]
- Fan JX, Wen M, & Kowaleski-Jones L (2014). Rural-urban differences in objective and subjective measures of physical activity: Findings from the National Health and Nutrition Examination Survey (NHANES) 2003-2006. Preventing Chronic Disease, 11, E141. doi: 10.5888/pcd11.140189 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kamada M, Shiroma EJ, Buring JE, Miyachi M, & Lee IM (2017). Strength training and all-cause, cardiovascular disease, and cancer mortality in older women: A cohort study. J Am Heart Assoc, 6(11). doi: 10.1161/JAHA.117.007677 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keadle SK, McKinnon R, Graubard BI, & Troiano RP (2016). Prevalence and trends in physical activity among older adults in the United States: A comparison across three national surveys. Preventive Medicine, 89, 37–43. doi: 10.1016/j.ypmed.2016.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kegler MC, Swan DW, Alcantara I, Wrensford L, & Glanz K (2012). Environmental influences on physical activity in rural adults: The relative contributions of home, church and work settings. Journal of Physical Activity and Health, 9(7), 996–1003. [DOI] [PubMed] [Google Scholar]
- Kurti AN, Logan H, Manini T, & Dallery J (2015). Physical activity behavior, barriers to activity, and opinions about a smartphone-based physical activity intervention among rural residents. Telemedicine Journal and e-Health, 21(1), 16–23. doi: 10.1089/tmj.2014.0034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lo BK, Morgan EH, Folta SC, Graham ML, Paul LC, Nelson ME, … Seguin RA (2017). Environmental influences on physical activity among rural adults in Montana, United States: Views from built environment audits, resident focus groups, and key informant interviews. International Journal of Environmental Research and Public Health, 14(10). doi: 10.3390/ijerph14101173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lobelo F, Rohm Young D, Sallis R, Garber MD, Billinger SA, Duperly J, … Stroke, Council. (2018). Routine assessment and promotion of physical activity in healthcare settings: A scientific statement from the American Heart Association. Circulation, 137(18), e495–e522. doi: 10.1161/CIR.0000000000000559 [DOI] [PubMed] [Google Scholar]
- Marcus BH, & Forsyth LH (2008). Motivating People to Be Physically Active (2nd Edition ed.): Human Kinetics. [Google Scholar]
- Marshall ES, Bland H, & Melton B (2013). Perceived barriers to physical activity among pregnant women living in a rural community. Public Health Nursing, 30(4), 361–369. doi: 10.1111/phn.12006 [DOI] [PubMed] [Google Scholar]
- Matthews KA, Croft JB, Liu Y, Lu H, Kanny D, Wheaton AG, … Giles WH (2017). Health-related behaviors by urban-rural county classification - United States, 2013. MMWR: Surveillance Summaries, 66(5), 1–8. doi: 10.15585/mmwr.ss6605a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SC, Lee IM, Weiderpass E, Campbell PT, Sampson JN, Kitahara CM, … Patel AV (2016). Association of leisure-time physical activity with risk of 26 types of cancer in 1.44 Million Adults. JAMA Intern Med, 176(6), 816–825. doi: 10.1001/jamainternmed.2016.1548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nieto FJ, Peppard PE, Engelman CD, McElroy JA, Galvao LW, Friedman EM, … Malecki KC (2010). The Survey of the Health of Wisconsin (SHOW), a novel infrastructure for population health research: Tationale and methods. BMC Public Health, 10, 785. doi: 10.1186/1471-2458-10-785 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Park T, Eyler AA, Tabak RG, Valko C, & Brownson RC (2017). Opportunities for promoting physical activity in rural communities by understanding the interests and values of community members. Journal of Environmental and Public Health, 2017, 8608432. doi: 10.1155/2017/8608432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson J, Schmer C, & Ward-Smith P (2013). Perceptions of Midwest rural women related to their physical activity and eating behaviors. Journal of Community Health Nursing, 30(2), 72–82. doi: 10.1080/07370016.2013.778722 [DOI] [PubMed] [Google Scholar]
- Phillips SM, Cadmus Bertram L, Rosenberg D, Buman M, & Lynch B (2018). Wearable technology and physical activity in chronic disease: Opportunities and challenges. American Journal of Preventive Medicine, 54(1):144–150. doi: 10.1016/j.amepre.2017.08.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sallis JF (2009). Measuring physical activity environments: A brief history. American Journal of Preventive Medicine, 36(4 Suppl), S86–92. doi: 10.1016/j.amepre.2009.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seguin RA, Economos CD, Hyatt R, Palombo R, Reed PN, & Nelson ME (2008). Design and national dissemination of the StrongWomen Community Strength Training Program. Preventing Chronic Disease, 5(1), A25. [PMC free article] [PubMed] [Google Scholar]
- Seguin RA, Eldridge G, Lynch W, & Paul LC (2013). Strength Training Improves Body Image and Physical Activity Behaviors Among Midlife and Older Rural Women. J Ext, 51(4). [PMC free article] [PubMed] [Google Scholar]
- Troiano RP, Berrigan D, Dodd KW, Masse LC, Tilert T, & McDowell M (2008). Physical activity in the United States measured by accelerometer. Medicine and Science in Sports and Exercise, 40(1), 181–188. doi: 10.1249/mss.0b013e31815a51b3 [DOI] [PubMed] [Google Scholar]
- Tucker JM, Welk GJ, & Beyler NK (2011). Physical activity in U.S.: adults compliance with the Physical Activity Guidelines for Americans. American Journal of Preventive Medicine, 40(4), 454–461. doi: 10.1016/j.amepre.2010.12.016 [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services (2018). Physical Activity Guidelines for Americans: 2nd Edition. Retrieved from https://health.gov/paguidelines/second-edition/pdf/Physical_Activity_Guidelines_2nd_edition.pdf [Google Scholar]
- van Reenan Mandy. (2005). EQ-5D-3L User Guide. EuroQol Research Foundation; Retrieved from https://euroqol.org/wp-content/uploads/2016/09/EQ-5D-3L_UserGuide_2015.pdf [Google Scholar]
- Whynes DK, & Group, Tombola. (2008). Correspondence between EQ-5D health state classifications and EQ VAS scores. Health Qual Life Outcomes, 6, 94. doi: 10.1186/1477-7525-6-94 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann K, Carnahan LR, & Peacock NR (2016). Age-associated perceptions of physical activity facilitators and barriers among women in rural southernmost Illinois. Preventing Chronic Disease, 13, E138. doi: 10.5888/pcd13.160247 [DOI] [PMC free article] [PubMed] [Google Scholar]


