Abstract
Background
Timely identification of patients at a high risk of clinical deterioration is key to prioritizing care, allocating resources effectively, and preventing adverse outcomes. Vital signs–based, aggregate-weighted early warning systems are commonly used to predict the risk of outcomes related to cardiorespiratory instability and sepsis, which are strong predictors of poor outcomes and mortality. Machine learning models, which can incorporate trends and capture relationships among parameters that aggregate-weighted models cannot, have recently been showing promising results.
Objective
This study aimed to identify, summarize, and evaluate the available research, current state of utility, and challenges with machine learning–based early warning systems using vital signs to predict the risk of physiological deterioration in acutely ill patients, across acute and ambulatory care settings.
Methods
PubMed, CINAHL, Cochrane Library, Web of Science, Embase, and Google Scholar were searched for peer-reviewed, original studies with keywords related to “vital signs,” “clinical deterioration,” and “machine learning.” Included studies used patient vital signs along with demographics and described a machine learning model for predicting an outcome in acute and ambulatory care settings. Data were extracted following PRISMA, TRIPOD, and Cochrane Collaboration guidelines.
Results
We identified 24 peer-reviewed studies from 417 articles for inclusion; 23 studies were retrospective, while 1 was prospective in nature. Care settings included general wards, intensive care units, emergency departments, step-down units, medical assessment units, postanesthetic wards, and home care. Machine learning models including logistic regression, tree-based methods, kernel-based methods, and neural networks were most commonly used to predict the risk of deterioration. The area under the curve for models ranged from 0.57 to 0.97.
Conclusions
In studies that compared performance, reported results suggest that machine learning–based early warning systems can achieve greater accuracy than aggregate-weighted early warning systems but several areas for further research were identified. While these models have the potential to provide clinical decision support, there is a need for standardized outcome measures to allow for rigorous evaluation of performance across models. Further research needs to address the interpretability of model outputs by clinicians, clinical efficacy of these systems through prospective study design, and their potential impact in different clinical settings.
Keywords: machine learning, early warning systems, clinical deterioration, ambulatory care, acute care, remote patient monitoring, vital signs, sepsis, cardiorespiratory instability, risk prediction
Introduction
Patient deterioration and adverse outcomes are often preceded by abnormal vital signs [1-3]. These warning signs frequently appear a few hours to a few days before the event, which can provide sufficient time for intervention. In response, clinical decision support early warning systems (EWS) have been developed that employ periodic observations of vital signs along with a predetermined criteria or cut-off range for alerting clinicians of patient deterioration [4].
EWS typically employ heart rate (HR), respiratory rate (RR), blood pressure (BP), peripheral oxygen saturation (SpO2), temperature, and sometimes the level of consciousness [5]. Aggregate-weighted EWS incorporate several vital signs and other patient characteristics with clearly defined thresholds. Weights are assigned to each of these vital signs and characteristics based on a threshold, and an overall risk score is calculated by adding each of the weighted scores [6].
Some of the commonly used aggregate-weighted EWS for predicting cardiorespiratory insufficiency and mortality are the Modified Early Warning Score (MEWS) [7], National Early Warning Score (NEWS) [8], and Hamilton Early Warning Score [9], which all incorporate vital signs and the level of consciousness (Alert, Verbal, Pain, Unresponsive [AVPU]) but have varying thresholds for assigning scores.
The predictive ability of aggregate-weighted EWS has limitations. First, the scores indicate the present risk of the patient but do not incorporate trends nor provide information about the possible risk trajectory [6]; thus, the scores do not communicate whether the patient is improving or deteriorating and the rate of this change [10]. Second, these scores do not capture any correlations between the parameters, as the score for each parameter is calculated independently through simple addition [6] (eg, HR or RR can be interpreted differently when body temperature is taken into consideration).
A newer approach to EWS relies on machine learning (ML). ML models learn patterns and relationships directly from data rather than relying on a rule-based system [11]. Unlike aggregate-weighted EWS, ML models are computationally intensive, but can incorporate trends in risk scores, adjust for varying numbers of clinical covariates, and be optimized for different care settings and populations [12]. Like other EWS, ML models can be integrated into electronic health records to analyze vital sign measurements continuously and provide predictions of patient outcomes as part of a clinical decision support system [13].
Two systematic reviews in 2019 [14,15] evaluated the ability of ML models to predict clinical deterioration in adult patients using vital signs. The review by Brekke et al [15] examined the utility of trends within intermittent vital sign measurements from adult patients admitted to all hospital wards and emergency departments (ED) but identified only 2 retrospective studies that met their inclusion criteria. The review identified that vital sign trends were of value in detecting clinical deterioration but concluded that there is a lack of research in intermittently monitored vital sign trends and highlighted the need for controlled trials.
The review conducted by Linnen et al [14] compared the accuracy and workload of ML-based EWS with that of aggregate-weighted EWS. This review focused on studies that reported adult patient transfers to intensive care units (ICUs) or mortality as the outcome(s) and excluded all other clinical settings; 6 studies were identified that reported the performance metrics for both the ML-based EWS and aggregate-weighted EWS. The review identified that ML modelling consistently performed better than aggregate-weighted models while generating clinical workload. They also highlighted the need for standardized performance metrics and deterioration outcome definitions.
These are important findings, but to date no review has systematically reviewed the evidence from studies using ML-based EWS using vital sign measurements of varying frequencies, across different care settings and clinical outcomes in order to identify common methodological trends and limitations with current approaches to generate recommendations for future research in this area.
The objective of this study was to scope the state of research in ML-based EWS using vital signs data for predicting the risk of physiological deterioration in patients across acute and ambulatory care settings and to identify directions for future research in this area.
Methods
A systematic scoping review was conducted by following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) extension for scoping reviews (PRISMA-ScR) framework [16]. This process provides an analysis of the available research, current state of utility of ML-based EWS, challenges facing their clinical implementation, and how they compare to aggregate-weighted EWS by identifying, synthesizing, and appraising the relevant evidence in the area. The literature search, assessment of eligibility of full-text articles, inclusion in the review, and extraction of study data were carried out by a single author.
Search Strategy
We searched PubMed, CINAHL, Cochrane Library, Web of Science, Embase, and Google Scholar for peer-reviewed studies without using any filters for study design and language. Searches were also conducted without any date restrictions. The reference lists of all studies that met the inclusion criteria were screened for additional articles. The search strategy involved a series of searches using a combination of relevant keywords and synonyms, including “vital signs,” “clinical deterioration,” and “machine learning.” See Multimedia Appendix 1 for search terms.
Eligibility Criteria
The inclusion criteria covered the following:
Peer-reviewed studies evaluating continuous or intermittent vital sign monitoring in adult patients so that all data collection or sampling frequencies (eg, 1 measurement per minute vs 1 measurement every 2 hours) wedre taken into consideration;
Studies conducted using data gathered from all acute and ambulatory care settings including medical or surgical hospital wards, ICUs, step-down units, ED, and in-home care;
Quantitative, observational, retrospective, and prospective cohort studies and randomized controlled trials;
Studies that involved ML or multivariable statistical or ML models and reported some model performance measure (eg, area under the curve) [17];
Studies that reported mortality or any outcomes related to clinical deterioration so that EWS models and performance can be examined for all explored outcomes.
The exclusion criteria included the following:
Studies that used any laboratory values as predictors for the ML-based EWS, as this review focuses on examining time-sensitive predictions of clinical deterioration using patient parameters that are readily available across all care settings;
Studies involving pediatric or obstetric populations due to these patients having different or altered physiologies that cannot be compared to standard adult patients;
Qualitative studies, reviews, preprints, case reports, commentaries, or conference proceedings.
Study Selection
References from the preliminary searches were handled using Mendeley reference management software. After duplicates were removed, titles and abstracts were screened to assess preliminary eligibility. Eligible studies were then read in full length to be assessed against the inclusion and exclusion criteria.
Data Extraction
Data were extracted from eligible studies using an extraction sheet that followed the PRISMA [18] and Cochrane Collaboration guidelines for systematic reviews [19] and the Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis (TRIPOD) guidelines [20] for the reporting of predictive models. Study characteristics, setting, demographics, patient outcomes, ML model characteristics, and model performance data were extracted. The model performance results were extracted from the validation data set rather than from the model derivation or training data set to decrease the potential for model overfitting. When studies explored multiple ML models, the model with the best performance was selected for reporting and comparison. If studies compared the performance of ML models to aggregate-weighted EWS, then the performance data of these warning systems were also extracted.
Results
Search Results and Study Selection
The search for “vital signs” AND “clinical deterioration” AND “machine learning” using the same query terms and filters identified 417 studies after duplicate removal. During the title and abstract screening process, 386 studies were excluded. Of the 31 full-text articles that were assessed, 7 studies were excluded for not meeting the eligibility criteria: 2 studies did not use ML models to predict deterioration, 3 studies included vital sign measurements in addition to laboratory values as predictors, 1 study focused on a cohort of pregnant women, and 1 study did not meet the criteria for model performance measures. A review of the reference lists of the 24 selected studies did not yield any additional studies fulfilling the eligibility criteria (refer to Figure 1).
Figure 1.
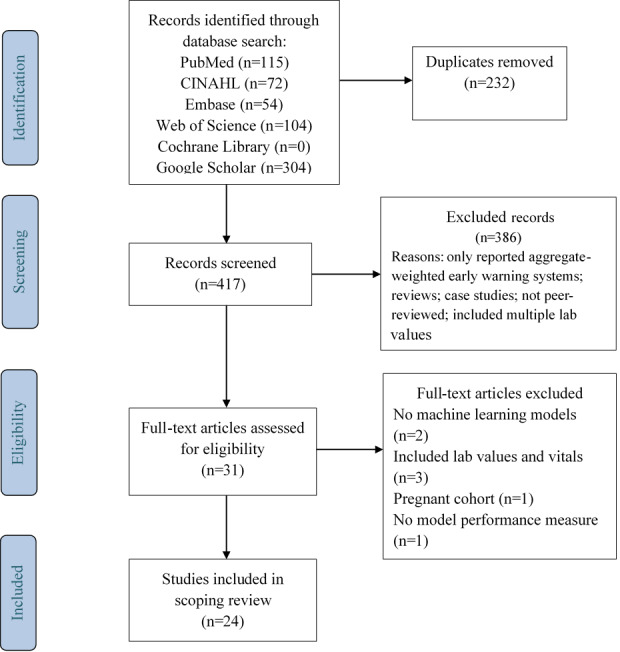
PRISMA flowchart of the search strategy and study selection.
Study Characteristics
Of the selected studies, 23 conducted a retrospective analysis of the vital signs data, while 1 study [21] used a prospective cohort study design. Seventeen studies only analyzed continuous vital signs measurements collected through wearable devices and bedside monitors, whereas 3 [22-24] studies analyzed vital signs that were collected both manually and intermittently by clinical staff. Two studies [25,26] analyzed vital signs that were collected both continuously and intermittently, while the remaining 2 studies did not report how the vital sign data were collected.
Studies were conducted in a variety of settings within hospitals while the study by Larburu et al [22] was conducted in an ambulatory setting. While 3 studies [27-29] aimed to develop a remote home-based monitoring tool, the vital sign data used were obtained from the Medical Information Mart for Intensive Care (MIMIC and MIMIC-II) databases [30,31] consisting of data captured from patient monitors in different ICUs. Regarding location, 5 studies [24,26,32-34] were conducted on general wards, 4 studies [11,23,35,36] were conducted in EDs, 7 studies [26,34,37-41] were conducted in ICUs, 2 studies [25,42] were conducted in postoperative wards, and 4 studies [21,43-45] in acute stay wards (medical admission unit, step-down units). Cohort sizes for the studies ranged from 12 patients [39] to 10,967,518 patient visits [11] (refer to Table 1).
Table 1.
Study characteristics.
| Authors, year | Setting(s) | Data collection | Cohort description | Event rate | Study purpose | Predictors | Measurement frequency | Outcome |
| Badriyah et al, 2014 [45] | Medical assessment unit for 24 hours | Personal digital assistants running VitalPAC software | 35,585 admissions | 199 (0.56%), cardiac arrest; 1161 (3.26%) unanticipated ICUa admissions; 1789 (5.02%) deaths; 3149 (8.85%) any outcome |
Compare the performance of a decision tree analysis with NEWSb | HRc, RRd, SBPe, temperature, SpO2, AVPUf level, % breathing air at the time of SpO2 measurement | Not specified | Cardiac arrest, unanticipated ICU admission, or death, each within 24 hours of a given vital sign observation |
| Chen at al, 2017 [44] | Step-down unit | Bedside monitors | 1880 patients (1971 admissions) | 997 patients (53%) or 1056 admissions (53.6%) who experienced CRIg events | Describe the dynamic and personal character of CRI risk evolution observed through continuous vital sign monitoring of individual patients | HR, RR, SPO2 (at 1/20 Hz), SBP, DBPh | Every 2 hours | CRI |
| Churpek et al, 2016 [24] | All wards at the University of Chicago and 4 North Shore University Health System hospitals | Data collected manually, documented electronically | 269,999 admissions | 16,452 outcomes (6.09%) | Whether adding trends improves accuracy of early detection of clinical deterioration and which methods are optimal for modelling trends | Temperature, HR, RR, SpO2, DBP, SBP | Every 4 hours | Development of critical illness on the wards: deaths, cardiac arrest, ICU transfers |
| Chiew et al, 2019 [23] | EDi at Singapore general hospital | Measurements at triage; hospital EHRj | 214 patients | 40 patients (18.7%) met outcome | Compare the performance of HR variability–based machine learning models vs conventional risk stratification tools to predict 30-day mortality | Age, gender, ethnicity, temperature, HR, RR, SBP, DBP, GCSk, HR variability | At triage | 30-day mortality due to sepsis |
| Chiu et al, 2019 [42] | Postoperative surgical wards at 4 UK adult cardiac surgical centers | VitalPac to electronically capture patients’ vital signs | Adults undergoing risk-stratified major cardiac surgery, n=13,631 | 578 patients (4.2%) with an outcome; 499 patients (3.66%) with unplanned ICU readmissions | Using logistic regression to model the association of NEWS variables with a serious patient event in the subsequent 24 hours; secondary objectives: comparing the discriminatory power of each model for events in the next 6 hours or 12 hours | RR, SpO2, SBP, HR, temperature, consciousness level | Not specified | Death, cardiac arrest, unplanned ICU readmissions |
| Clifton et al, 2014 [25] | Postoperative ward of the cancer center, Oxford University Hospitals NHSl Trust, United Kingdom | Continuous vitals monitored by wearable devices; intermittent vitals monitored manually by ward staff | 200 patients in the postoperative ward following upper gastrointestinal cancer surgery | Not specified | Using continuous vitals monitoring to provide early warning of physiological deterioration, such that preventative clinical action may be taken | SpO2, HR (256 Hz), BP, RR | Continuously (SpO2, HR), intermittently (BP, RR) | Physiological deterioration |
| Desautels et al, 2016 [37] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMICm-III) | 22,853 ICU stays | 2577 (11.28%) stays with confirmed sepsis | Validate a sepsis prediction method, InSight, for the new Sepsis-3 definitions and make predictions using a minimal set of variables | GCS, HR, RR, SpO2, temperature, invasive and noninvasive SBP and DBP | At least 1 measurement per hour | Onset of sepsis |
| Forkan et al, 2017 [28] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMIC-II) | 1023 patients | Not specified | Develop a probabilistic model for predicting the future clinical episodes of a patient using observed vital sign values prior to the clinical event | HR, SBP, DBP, mean BP, RR, SpO2 | All samples converted to per-minute sampling | Abnormal clinical events |
| Forkan et al, 2017 [27] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMIC & MIMIC-II) | 85 patients | Not specified | Develop an intelligent method for personalized monitoring and clinical decision support through early estimation of patient-specific vital sign values | HR, SBP, DBP, mean BP, RR, SpO2 | Per-minute sampling | Patient-specific anomalies, disease symptoms, and emergencies |
| Forkan et al, 2017 [29] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMIC-II) | 4893 patients | Not specified | Build a prognostic model, ViSiBiD, that can accurately identify dangerous clinical events of a home-monitored patient in advance | HR, SBP, DBP, mean BP, RR, SpO2 | Per-minute sampling | Dangerous clinical events |
| Guillame-Bert et al, 2017 [43] | Step-down unit | Bedside monitor measurements over 8 weeks | 297 admissions | 127 patients (43%) exhibited at least 1 real event during their stay | Forecast CRI utilizing data from continuous monitoring of physiologic vital sign measurements | HR, RR, SPO2, SBP, DBP, mean BP | Every 20 seconds (HR, RR, SPO2), every 2 hours (SBP, DBP, and mean BP) | At least 1 event threshold limit criteria exceeded for >80% of last 3 minutes |
| Ho et al, 2017 [38] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMIC-II) | 763 patients | 197 patients (25.8%) experienced a cardiac arrest event | Build a cardiac arrest risk prediction model capable of early notification at time z (z ≥5 hours prior to the event) | Temperature, SpO2, HR, RR, DBP, SBP, pulse pressure index | 1 reading per hour | Cardiac arrest |
| Jang et al, 2019 [35] | ED visits to a tertiary academic hospital | EHR data from ED visits | Nontraumatic ED visits | 374,605 eligible ED visits of 233,763 patients; 1097 (0.3%) patients with cardiac arrest | Develop and test artificial neural network classifiers for early detection of patients at risk of cardiac arrest in EDs | Age, sex, chief complaint, SBP, DBP, HR, RR, temperature, AVPU | Not specified | Development of cardiac arrest within 24 hours after prediction |
| Kwon et al, 2018 [26] | Cardiovascular teaching hospital and community general hospital | Data collected manually by staff on general wards, by bedside monitors in ICUs | 52,131 patients | 419 patients (0.8%) with cardiac arrest; 814 (1.56%) deaths without attempted resuscitation | Predict whether an input vector belonged within the prediction time window (0.5-24 hours before the outcome) | SBP, HR, RR, temperature | 3 times a day on general wards, every 10 minutes in ICUs | Primary outcome: first cardiac arrest; secondary outcome: death without attempted resuscitation |
| Kwon et al, 2018 [11] | 151 EDs in Korea | Korean National Emergency Department Information System (NEDIS) | 10,967,518 ED visits | 153,217 (1.4%) in-hospital deaths; 625,117 (5.7%) critical care admissions; 2,964,367 (27.0%) hospitalizations | Validate that a DTASn identifies high-risk patients more accurately than existing triage and acuity scores | Age, sex, chief complaint, time from symptom onset to ED visit, arrival mode, trauma, initial vital signs (SBP, DBP, HR, RR, temperature), mental status | At ED admission | Primary outcome: in-hospital mortality; secondary outcome: critical care; tertiary outcome: hospitalization |
| Larburu et al, 2018 [22] | OSI Bilbao-Basurto (Osakidetza) Hospital and ED admissions, ambulatory | Collected manually by clinicians and patients | 242 patients | 202 predictable decompensations | Prevent mobile heart failure patients’ decompensation using predictive models | SBP, DBP, HR, SaO2, weight | At diagnosis and 3-7 times per week in ambulatory patients | Heart failure decompensation |
| Li et al, 2016 [39] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMIC-II) | 12 patients | Not specified | Adaptive online monitoring of patients in ICUs | HR, SBP, DBP, MAPo, RR | At least 1 measurement per hour | Signs of deterioration |
| Liu et al, 2014 [36] | ED of a tertiary hospital in Singapore | Manual vital measurements by nurses or physicians | 702 patients with undifferentiated, nontraumatic chest pain | 29 (4.13%) patients met primary outcome | Discover the most relevant variables for risk prediction of major adverse cardiac events using clinical signs and HR variability | SBP, RR, HR | Not specified | Composite of events such as death and cardiac arrest within 72 hours of arrival at the ED |
| Mao et al, 2018 [34] | ICU, inpatient wards, outpatient visits | UCSFp dataset:inpatient and outpatient visits; MIMIC-III: ICU bedside monitors | UCSF: 90,353 patients; MIMIC-III: 21,604 patients |
UCSF: 1179 (1.3%) sepsis, 349 (0.39%) severe sepsis, 614 (0.68%) septic shock; MIMIC-III: sepsis (1.91%), severe sepsis (2.82%), septic shock (4.36%) | Sepsis prediction | SBP, DBP, HR, RR, SpO2, temperature | Hourly | Sepsis, severe sepsis, septic shock |
| Olsen et al, 2018 [46] | PACUq, Rigshospitalet, University of Copenhagen, Denmark | IntelliVue MP5, BMEYE Nexfin bedside monitors during admission to post anesthetic care unit | 178 patients | 160 (89.9%) had ≥1 microevent occurring during admission; 116 patients (65.2%) had ≥1 microevent with a duration >15 minutes | Develop a predictive algorithm detecting early signs of deterioration in the PACU using continuously collected cardiopulmonary vital signs | SpO2, SBP, HR, MAP | Every minute (SpO2, SBP, HR), every 15 minutes (MAP) | Signs of deterioration |
| Shashikumar et al, 2017 [40] | Adult ICU units | ICU bedside monitors, Bedmaster system; up to 24 hours of monitoring | Patients with unselected mixed surgical procedures | 242 sepsis cases | Predict onset of sepsis 4 hours ahead of time, using commonly measured vital signs | MAP, HR, SpO2, SBP, DBP, RR, GCS, temperature, comorbidity, clinical context, admission unit, surgical specialty, wound type, age, gender, weight, race | ≥1 measurement per hour | Onset of sepsis |
| Tarassenko et al, 2006 [32] | General wards at John Radcliffe Hospital in Oxford, United Kingdom | Bedside monitors for at least 24 hours per patient | 150 general-ward patients | Not specified | A real-time automated system, BioSign, which tracks patient status by combining information from vital signs | HR, RR, SpO2, skin temperature, average SBP -average DBP | Every 30 minutes (BP), every 5 seconds (other vitals) | Signs of deterioration |
| Van Wyk et al, 2017 [33] | Methodist LeBonheur Hospital, Memphis, TN | Bedside monitors: Cerner CareAware iBus system | 2995 patients | 343 patients (11.5%) diagnosed with sepsis | Classify patients into sepsis and nonsepsis groups using data collected at various frequencies from the first 12 hours after admission | HR, MAP, DBP, SBP, SpO2, age, race, gender, fraction of inspired oxygen | Every minute | Sepsis detection |
| Yoon et al, 2019 [41] | Beth Israel Deaconess Medical Center ICU | ICU bedside monitors and medical records (MIMIC-II) | 2809 subjects | 787 tachycardia episodes | Predicting tachycardia as a surrogate for instability | Arterial DBP, arterial SBP, HR, RR, SpO2, MAP | 1/60 Hz or 1 Hz | Tachycardia episode |
aICU: intensive care unit.
bNEWS: National Early Warning Score.
cHR: heart rate.
dRR: respiratory rate.
eSBP: systolic blood pressure.
fAVPU: alert, verbal, pain, unresponsive.
gCRI: cardiorespiratory instability.
hDBP: diastolic blood pressure.
iED: emergency department.
jEHR: electronic health record.
kGCS: Glasgow Coma Score.
lNHS: National Health Service.
mMIMIC: Medical Information Mart for Intensive Care.
nDTAS: Deep learning–based Triage and Acuity Score.
oMAP: mean arterial pressure.
pUCSF: University of California, San Francisco.
qPACU: postanesthesia care unit.
Predictor Variables
The most commonly used vital sign predictors were HR, RR, systolic BP, diastolic BP, SpO2, body temperature, level of consciousness through either the Glasgow Coma Score or the AVPU scale, and mean arterial pressure. Measurement frequencies for these variables ranged from once every 5 seconds [32] in hospital wards to 3-7 times per week [22] in an ambulatory setting. Other commonly used predictors included age, gender, weight, ethnicity, chief complaint, and comorbidities.
Outcomes
The outcomes being predicted in most studies focused on cardiorespiratory insufficiency–related events. Cardiac arrest was the primary outcome in 7 [24,26,35,36,38,42,45] studies, while general cardiorespiratory deterioration or decompensation was the primary outcome in 5 studies [25,39,41,43,44]. Another commonly predicted outcome was sepsis, which included the time of onset of sepsis [34,37,40], severe sepsis [33,34], septic shock [34], and sepsis-related mortality [23]. Other outcomes explored within the studies include unanticipated ICU admissions [24,42,45], development of critical illness [24], general physiological deterioration [25,32,39,46], abnormal or dangerous clinical events [27-29], and mortality [11,24,42].
Outcomes were first identified, and baseline models were created using predefined parameter thresholds (ground truth) consistent with the MEWS [23,26,35] or NEWS [23,42,46] criteria for cardiorespiratory instability and general physiological deterioration, while the sepsis-related outcomes were identified based on the thresholds set within the systemic inflammatory response syndrome [34], quick Sequential Organ Failure Assessment (qSOFA) [23], and SOFA [37] criteria. Some studies [22,27-29,43,44] also used thresholds and criteria based on the population served by their individual care setting.
ML Models and Performance
All included studies consider the prediction of deterioration risk to be a classification task and therefore use different types of classification models in the process, including tree-based models, linear models, kernel-based methods, and neural networks (refer to Table 2 for a full inventory of methods used, model performance achieved, and prediction windows, and see Multimedia Appendix 2 for a description of ML methods).
Table 2.
Machine learning (ML) models and comparisons used for outcome prediction.
| Study | Cohort | Event rate | ML model(s) | Missing data handling | Best ML model performance | ML model comparisons | Prediction window | Aggregate weighted EWSa comparisons |
| Badriyah et al, 2014 [45] | 35,585 admissions | 199 (0.56%), cardiac arrest; 1161 (3.26%) unanticipated ICUb admissions; 1789 (5.02%) deaths; 3149 (8.85%) any outcome |
Decision tree analysis | Not specified | Decision tree predicted cardiac arrest: AUROCc=0.708; unanticipated ICU admission: AUROC=0.862; death: AUROC=0.899; any outcomes: AUROC=0.877 |
Not specified | Within 24 hours preceding events | NEWSd AUROC: cardiac arrest, 0.722; unanticipated ICU admission, 0.857; death, 0.894; any outcomes, 0.873 |
| Chen at al, 2017 [44] | 1880 patients (1971 admissions) | 997 patients (53%) or 1056 admissions (53.6%) who experienced CRIe events | Variant of the random forest classification model using nonrandom splits | Not specified | Random forest AUCf initially remained constant (0.58-0.60), followed by an increasing trend, with AUCs rising from 0.57 to 0.89 during the 4 hours immediately preceding events | Logistic regression: AUC=0.7; lasso logistic regression: AUC=0.82 | Within 4 hours preceding events | No comparison |
| Churpek et al, 2016 [24] | 269,999 admissions | 16,452 outcomes (6.09%) | Univariate analysis, bivariate analysis |
Forward imputation, median value imputation | Trends increased model accuracy compared to a model containing only current vital signs (AUC 0.78 vs 0.74); vital sign slope improved AUC by 0.013 | Not specified | Within 4 hours preceding events | No comparison |
| Chiew et al, 2019 [23] | 214 patients | 40 patients (18.7%) met outcome | K-nearest neighbor, random forest, adaptive boosting, gradient boosting, support vector machine | Not specified | Gradient boosting predicted 30-day sepsis-related mortality: F1 score=0.50, AUPRC=0.35, precision (PPVg)=0.62, recall=0.5 | K-nearest neighbor: F1 score=0.10, AUPRC=0.10, precision (PPV)=0.33, recall=0.6; random forest: F1 score=0.35, AUPRC=0.27, precision (PPV)=0.26, recall=0.56; adaptive boosting: F1 score=0.40, AUPRC=0.31, precision (PPV)=0.43, recall=0.38; SVMh: F1 score=0.43, AUPRC=0.29, precision (PPV)=0.33, recall=0.63 | Within 30 days preceding event | SEDSi: F1=0.40, AUPRC=0.22; qSOFAj: F1=0.32, AUPRC=0.21; NEWS; F1=0.38, AUPRC=0.28; MEWSk: F1=0.30, AUPRC=0.25 |
| Chiu et al, 2019 [42] | Adults undergoing risk-stratified major cardiac surgery (n=13,631) | 578 patients (4.2%) with an outcome; 499 patients (3.66%) with unplanned ICU readmissions | Logistic regression | Observations with missing values were excluded | Logistic regression predicted the event 24 hours in advance: AUROC=0.779; 12 hours in advance: AUROC=0.815; 6 hours in advance: AUROC=0.841 | Not specified | Within 24, 12, and 6 hours preceding event | NEWS: 24 hours before event, AUROC=0.754; 12 hours before event, AUROC=0.789; 6 hours before event, AUROC=0.813 |
| Clifton et al, 2014 [25] | 200 patients in the postoperative ward following upper gastrointestinal cancer surgery | Not specified | Classifiers, Gaussian process, one-class support vector machine, kernel estimate | Missing channels replaced by mean of that channel | SVM predicted deterioration: accuracy=0.94, partial AUC=0.28, sensitivity=0.96, specificity=0.93 | Conventional SVM: accuracy=0.90, partial AUC=0.26, sensitivity=0.92, specificity=0.87; Gaussian mixture models: accuracy=0.9, partial AUC=0.24, sensitivity=0.97, specificity=0.84; Gaussian processes: accuracy=0.90, partial AUC=0.26, sensitivity=0.91, specificity=0.89; kernel density estimate: accuracy=0.91, partial AUC=0.26, sensitivity=0.94, specificity=0.87 | Not specified | No comparison |
| Desautels et al, 2016 [37] | 22,853 ICU stays | 2577 (11.28%) stays with confirmed sepsis | Insight classifier | Carry forward imputation | Classifier predicts sepsis at onset: AUROC=0.880, APRl=0.6, accuracy=0.8; classifier predicts sepsis 4 hours before onset: AUROC=0.74, APR=0.28, accuracy=0.57 | Not specified | Within 4 hours preceding event and at time of event onset | SIRSm: AUROC= 0.609, APR= 0.160; qSOFA: AUROC= 0.772, APR=0.277; MEWS: AUROC=0.803, APR=0.327; SAPSn II: AUROC=0.700, APR=0.225; SOFA: AUROC=0.725, APR=0.284 |
| Forkan et al, 2017 [28] | 1023 patients | Not specified | PCAo used to separate patients into multiple categories; hidden Markov Model adopted for probabilistic classification and future prediction | Data with consecutive missing values over a long period are eliminated | Hidden Markov Model event prediction: accuracy=97.8%, precision=92.3, sensitivity=97.7, specificity=98, F-score=95% | Neural network: accuracy=93% | Within 30 minutes preceding event | No comparison |
| Forkan et al, 2017 [27] | 85 patients | Not specified | Multilabel classification algorithms are applied in classifier design; result analysis with J48 decision tree, random tree and sequential minimal optimization (SMO, a simplified version of SVM) | Where ≥1 vital signs data are missing while clean values of others are available, considered as recoverable and imputed using median-pass and k-nearest neighbor filter | Predictions across 24 classifier combinations yielded a Hamming score of 90%-95%; F1-micro average of 70.1%-84%; accuracy of 60.5%-77.7% | Not specified | Within 1 hour preceding event | No comparison |
| Forkan et al, 2017 [29] | 4893 patients | Not specified | J48 decision tree, random forest, sequential minimal optimization, MapReduce random forest | Data with consecutive missing values over a long period are eliminated | Event prediction by random forest: within a 60-minute forecast horizon, F score=0.96, accuracy=95.86; within a 90-minute forecast horizon, F-score=0.95, accuracy=95.35; within a 120-minute forecast horizon, F-score=0.95, accuracy=95.18 | J48 decision tree: within a 60-minute forecast horizon, F score=0.93, accuracy=92.46; within a 90-minute forecast horizon, F score=0.92, accuracy=91.59; within a 120-minute forecast horizon, F score=0.91, accuracy=91.30; Event prediction with sequential minimal optimization: within a 60-minute forecast horizon, F score=0.91, accuracy=90.72; within a 90-minute forecast horizon, F score=0.90, accuracy=90.08; within a 120-minute forecast horizon, F score=0.89, accuracy=89.23 |
1 hour preceding event | No comparison |
| Guillame-Bert et al, 2017 [43] | 297 admissions | 127 patients (43%) exhibited at least 1 real CRI event during their stay in the step-down unit | TITAp rules, rule fusion algorithm; mapping function from rule-based features to forecast model learned using random forest classifier | Not specified | Event forecast alert within 17 minutes, 51 seconds before onset of CRI (false alert every 12 hours); event forecast alert within 10 minutes, 58 seconds before onset of CRI (false alert every 24 hours) | Random forest: event forecast alert within 11 minutes, 25 seconds before onset of CRI (false alert every 12 hours); event forecast alert within 5 minutes, 52 seconds before onset of CRI (false alert every 24 hours) | Within 17 minutes, 51 seconds preceding CRI onset | No comparison |
| Ho et al, 2017 [38] | 763 patients | 197 patients (25.8%) experienced a cardiac arrest event | Temporal transfer learning-based model (TTL-Reg) | Imputed values based on the median from patients of the same gender and similar ages | TTL-Reg predicts events with an AUC of 0.63 | Not specified | Within 6 hours preceding event | No comparison |
| Jang et al, 2019 [35] | Non-traumatic ED visits | 374,605 eligible ED visits of 233,763 patients; 1097 (0.3%) patients with cardiac arrest | ANNq with multilayer perceptron, ANN with LSTMr, hybrid ANN; comparison with random forest and logistic regression | Not specified | Event prediction: ANN with multilayer perceptron, AUROC=0.929; ANN with LSTM, AUROC=0.933; hybrid ANN, AUROC=0.936 | Random forest, AUROC=0.923; logistic regression, AUROC=0.914 | Within 24 hours preceding event | MEWS: AUROC=0.886 |
| Kwon et al, 2018 [26] | 52,131 patients | 419 patients (0.8%) with cardiac arrest; 814 (1.56%) deaths without attempted resuscitation | 3 RNNs layers with LSTM to deal with time series data; compared to random forest and logistic regression | Most recent value was used; if no value available, then median value used | Event prediction: RNNs, AUROC=0.85, AUPRCt=0.044 | Random forest, AUROC=0.78, AUPRC=0.014; logistic regression, AUROC=0.613, AUPRC=0.007 |
30 minutes to 24 hours preceding event | MEWS: AUROC=0.603, AUPRC=0.003 |
| Kwon et al, 2018 [11] | 10,967,518 ED visits | 153,217 (1.4%) in-hospital deaths; 625,117 (5.7%) critical care admissions; 2,964,367 (27.0%) hospitalizations | DTASu using multilayer perceptron with 5 hidden layers |
Excluded | Event prediction: DTAS using multilayer perceptron, AUROC=0.935, AUPRC=0.264 | Random forest: AUROC= 0.89, AUPRC= 0.14; logistic regression: AUROC= 0.89, AUPRC=0.16 | Not specified | Korean triage and acuity score: AUROC =0.785, AUPRC=0.192; MEWS: AUROC=0.810, AUPRC=0.116; |
| Larburu et al, 2018 [22] | 242 patients | 202 predictable decompensations | Naïve Bayes, decision tree, random forest, SVM | Not specified | Decompensation event prediction: naïve Bayes, AUC=67% | Decision tree, neural network, random forest, support vector machine, stochastic gradient descent | Not specified | No comparison |
| Li et al, 2016 [39] | 12 patients | Not specified | L-PCA (combination of just-in-time learning and PCA) | Not specified | Fault detection rate with L-PCA: 20% higher than with PCA; 47% higher than with fast moving-window PCA; best detection rate achieved was 99.8% | Not specified | Not specified | No comparison |
| Liu et al, 2014 [36] | 702 patients with undifferentiated, non-traumatic chest pain | 29 (4.13%) patients met primary outcome | Novel variable selection framework based on ensemble learning; random forest was the independent variable selector for creating the decision ensemble | Not specified | Event prediction with ensemble learning model: AUC=0.812, cut-off score=43, sensitivity=82.8%, specificity=63.4% | Not specified | Within 72 hours of arrival at ED | TIMIv: AUC=0.637; MEWS: AUC=0.622 |
| Mao et al, 2018 [34] | UCSFw: 90,353 patients; MIMICx-III: 21,604 patients | UCSF: 1179 (1.3%) sepsis, 349 (0.39%) severe sepsis, 614 (0.68%) septic shock; MIMIC-III: sepsis (1.91%), severe sepsis (2.82%), septic shock (4.36%) | Gradient tree boosting + transfer learning using MIMIC-III as source and UCSF as target | Carry forward imputation | Detection with gradient tree boosting: AUROC=0.92 for sepsis; AUROC=0.87 for severe sepsis at onset; AUROC=0.96 for septic shock 4 hours before; AUROC=0.85 for severe sepsis prediction 4 hours before | Not specified | At onset of sepsis and severe sepsis; within 4 hours preceding septic shock and severe sepsis | MEWS: AUROC=0.76; SOFA: AUROC=0.65; SIRS: AUROC=0.72 |
| Olsen et al, 2018 [46] | 178 patients | 160 (89.9%) had ≥1 microevent occurring during admission; 116 patients (65.2%) had ≥1 microevent with a duration >15 minutes | Random forest classifier | Not specified | Detection of early signs of deterioration with random forest: accuracy=92.2%, sensitivity=90.6%, specificity=93.0%, AUROC=96.9% | Not specified | Not specified | Compared with hospital's current alarm system: number of false alarms decreased by 85%, number of missed early signs of deterioration decreased by 73% |
| Shashikumar et al, 2017 [40] | Patients with unselected mixed surgical procedures | 242 sepsis cases | Elastic net logistic classifier | Median values (if multiple measurement were available); otherwise, the old values were kept (sample-and-hold interpolation); mean imputation for replacing all remaining missing values | Event prediction: elastic net logistic classifier using entropy features alone, AUROC=0.67, accuracy=47%; elastic net logistic classifier using social demographics + EMRy features, AUROC=0.7, accuracy=50%; elastic net logistic classifier using all features, AUROC=0.78, accuracy=61% | Not specified | 4 hours prior to onset | No comparison |
| Tarassenko et al, 2006 [32] | 150 general-ward patients | Not specified | Biosign; data fusion method: probabilistic model of normality in five dimensions | Historic, median filtering | 95% of Biosign alerts were classified as “True” by clinical experts | Not specified | Within 120 minutes of event | No comparison |
| Van Wyk et al, 2017 [33] | 2995 patients | 343 patients (11.5%) diagnosed with sepsis | CNNz (constructed images using raw patient data) with random dropout to reduce overfitting; multilayer perceptron with random dropout between layers to avoid overfitting | Not specified | Event classification with a 1-minute observation frequency: CNN, accuracy=86.1%; event classification with a 10-minute observation frequency: CNN, accuracy=78.2% | Event classification with a 1-minute observation frequency: multilayer perceptron, accuracy=76.5%; event classification with a 10-minute observation frequency: multilayer perceptron, accuracy=71% |
Not specified | No comparison |
| Yoon et al, 2019 [41] | 2809 subjects | 787 tachycardia episodes | Regularized logistic regression and random forest classifiers | Discrete Fourier transform, cubic-spline interpolation of heart rate and respiratory rate data for missing data as long as ≥20% of the data were available | Event prediction: random forest, AUC=0.869, accuracy=0.806 | Logistic regression with L1 regularization, AUC=0.8284, accuracy=0.7668 | Within 3 hours preceding onset | No comparison |
aEWS: early warning system.
bICU: intensive care unit.
cAUROC: area under the receiver operator characteristic.
dNEWS: National Early Warning Score.
eCRI: cardiorespiratory instability.
fAUC: area under the curve.
gPPV: positive predictive value.
hSVM: support vector machine.
iSEDS: Singapore Emergency Department Sepsis.
jqSOFA: quick Sequential Organ Failure Assessment.
kMEWS: Modified Early Warning Score.
lAPR: area under the precision-recall curve.
mSIRS: systemic inflammatory response syndrome.
nSAPS II: simplified acute physiology score.
oPCA: principal component analysis.
pTITA: temporal interval tree association.
qANN: artificial neural network.
rLSTM: long short-term memory.
sRNN: recurrent neural network.
tAUPRC: area under the precision-recall curve.
uDTAS: Deep learning–based Triage and Acuity Score.
vTIMI: Thrombolysis in Myocardial Infarction.
wUCSF: University of California, San Francisco.
xMIMIC: Medical Information Mart for Intensive Care.
yEMR: electronic medical record.
zCNN: convolutional neural network.
Measures used to assess model performance varied across the studies. The most common measure was the area under the receiver operator characteristic (AUROC) along with model accuracy, sensitivity, and specificity. Area under the precision-recall, F-score, Hamming’s score, and precision (positive predictive value) were reported less commonly.
Prediction windows ranged from 30 minutes to 30 days before an event.
Model performance varied substantially based on outcome measure being predicted (eg, cardiorespiratory insufficiency vs sepsis), ML method used (eg, linear vs tree-based), and prediction window (eg, 30 minutes before an event vs 4 hours before).
Comparison With Aggregate-Weighted EWS
Nine studies compared the performance of ML-based EWS with aggregate-weighted EWS. Studies exploring cardiorespiratory outcomes, general physiological deterioration, or mortality carried out comparisons with NEWS [42,45], MEWS [11,26,35,36], and the Thrombolysis in Myocardial Infarction score [36]. The 3 studies exploring sepsis-related outcomes additionally included the SOFA, qSOFA, and SIRS criteria and the simplified acute physiology (II) score [23,34,37]. A few studies also drew comparisons with other customized scoring systems individual to their care setting or region such as the Korean Triage and Acuity Score [11], Singapore Emergency Department Sepsis model [23], and postanesthesia care unit alarm system [46].
In all 9 studies, the ML models performed better than the aggregate-weighted EWS systems for all clinical outcomes except for cardiac arrest in the study by Badriyah et al [45]. For example, in the study by Jang et al [35], a long short-term memory neural network achieved an AUROC of 0.933, an improvement over MEWS, which achieved an AUROC of 0.886 using the same data. Similarly, in the study by Kwon et al [26], recurrent neural networks achieved an AUROC of 0.85 compared to 0.603 for MEWS and 0.785 for the Korean Triage and Acuity Score. Some studies reported much more modest improvements, such as the study by Chiu et al [42] that achieved an AUROC of 0.779 using logistic regression, compared to 0.754 using MEWS for the same 24-hour prediction window. A full side-by-side comparison of ML vs aggregate-weighted EWS is presented in Multimedia Appendix 3.
Discussion
Based on this scoping review, ML-based EWS models show considerable promise, but there exist several important avenues for future research if these models are to be effectively implemented in clinical practice.
Prediction Window
A model’s prediction window refers to how far in advance a model is predicting an adverse event. Most studies included in our review used a prediction window between 30 minutes [26] and 72 hours [36] before the clinical deterioration took place. The length of a model’s prediction window is important because a prediction window that is too short will not yield any real clinical benefit (it would not give a clinical team sufficient time to intervene), but a number of studies [29,34,37,42] showed a decrease in model performance when the prediction window was longer (eg, AUROC drops from 0.88 at the time of onset to 0.74 at 4 hours before the event). Future research seeking to maximize the clinical benefit of ML EWS should strive to achieve an optimum balance between a clinically relevant prediction window and clinically acceptable model performance, rather than simply maximizing a model performance metric, such as AUROC.
Clinically Actionable Explanations
The studies included in this review focused on ML model development and did not explore how the output of these models would be communicated to clinicians. Since many ML models are “black boxes” [46,47], it may not be immediately clear to clinicians what the likely reason for an alert might be until the patient is assessed, which can cause further delays in time-sensitive scenarios. However, in the broader ML field, there has been significant recent progress in explainable ML techniques, and it has been pointed out that these approaches may be preferred by the medical community and regulators [48,49]. Several explanation methods take specific, previously black-box methods, such as convolutional neural networks [50], and allow for post-hoc explanation of their decision-making process. Other explainability algorithms are model-agnostic, meaning they can be applied to any type of model, regardless of its mathematical basis [51]. In the study by Lauritsen et al [52], an explainable EWS was developed based on a temporal convolutional network, using a separate module for explanations. These methodologies are promising, but their application to health care, including to EWS, has been limited. Objective evaluation of the utility of explanation methods is a difficult, ongoing problem, but is an important direction for future research in the area of ML-based EWS if they are to be effectively deployed in clinical practice [53].
Expanded Study Settings
Nearly all the studies included in this review were conducted in inpatient settings. While EWS are highly valuable in an inpatient context, there is also considerable need in the ambulatory setting, particularly postdischarge. For example, the VISION study [54] found that 1.8% of all patients die within 30 days postsurgery and 29.4% of all deaths occurred after patients were discharged from hospital. Patients often receive postoperative monitoring only 3-4 weeks [54] after discharge during a follow-up visit with their surgeon. During this period, it has been shown that many patients suffer from prolonged unidentified hypoxemia [55] and hypotension [56], which are precursors to serious postoperative complications. While EWS research has historically focused on inpatient settings due to the availability of continuous vital signs data, the increasing availability of remote patient monitoring and wearable technologies offer the opportunity to direct future EWS research to the ambulatory setting to address a significant clinical need.
Retrospective Versus Prospective Evaluation
All but one study [21] included in this review were retrospective in nature, leaving open the possibility that algorithm performance in a clinical environment may be lower than the performance achieved in a controlled retrospective setting [34]. It is also unclear how often these EWS were able to identify clinical deterioration that had not already been detected by a care team. Further, alerts for clinical deterioration may be easily disregarded by clinicians due to alert fatigue, even when the risk of deterioration has been correctly identified [43]. In the single case where an ML-based EWS was studied prospectively, Olsen et al [21] found that the random forest classifier decreased false alarm rates by 85% and the rate of missed alerts by 73% when compared to the existing aggregate-weighted alarm system. While the predictions were independently scored for severity by 2 clinician experts, the interpretation of the clinical impact of these alerts was not explored any further, leaving the question of clinical benefit unanswered. Future research into ML-based EWS should begin to include prospective evaluation, both of model accuracy (to understand how model performance is affected when faced with real-world data) and of clinical outcomes (to understand whether alerts in fact produce clinical benefits).
Standardizations of Performance Metrics
A key observation from this review is the lack of an agreed-upon standard among the research community for reporting performance measures across studies. This makes meaningful comparison between the outcomes of these studies difficult, and where there is overlap, it is not clear that the most clinically relevant metrics have been chosen. The majority of the studies in this review report the AUROC as the main performance metric, reflecting a common practice in the ML literature. However, AUROC may not be adequate for evaluating the performance of the EWS in a clinical setting [57].
As Romero-Brufau et al [58] discussed in their article, AUROC does not incorporate information about the prevalence of physiological deterioration, which can be lower than 0.02 daily in a general inpatient setting. This can make AUROC a misleading metric, leading to overestimation of clinical benefit and underestimation of clinical workload and resources. [58] When the prevalence is low (<0.1), even a model with high sensitivity and specificity may not yield a high posttest probability for a positive prediction [15]. Therefore, reporting metrics that incorporate the prevalence would be more appropriate.
The performance of an EWS depends on the tradeoff between 2 goals: early detection of outcomes versus issuance of fewer false-positive alerts to prevent alarm fatigue [43]. Sensitivity can be a good metric to evaluate the first goal as it would provide the percentage of true-positive predictions within a certain time period. To evaluate the clinical burden of false-positive alerts, the positive predictive value, which incorporates prevalence, can be used as it gives a percentage of useful alerts that lead to a clinical outcome. The number needed to evaluate can be a useful measure of clinical utility and cost-efficiency of each alert as it provides the number of patients that need to be evaluated further to detect one outcome. Using these metrics to evaluate tradeoffs between outcome detection and workload would be essential for determining the clinical utility of the EWS [58]. Additionally, the F1 score can also be a useful metric as it provides a measure of the model’s overall accuracy through the calculation of the harmonic mean of the precision and recall (sensitivity). Balancing the use of these 2 metrics could yield a more realistic measure of the model’s performance [58].
Comparison to “Gold Standard” EWS
On a related note, only 9 of the studies included in our review made comparisons between their ML-based models and a “gold standard” aggregate-weighted EWS, such as MEWS or NEWS. Future research in the area should report a commonly used aggregate-weighted EWS as a baseline model, which would aid in making effective comparisons between them. NEWS may be particularly well suited to this area of research as its input variables can all be measured automatically and continuously via devices.
Strengths of the Review
The search strategy was comprehensive while not being too focused on specific clinical outcomes, sampling frequencies, or filtering for time. This allowed for the identification of as many studies as possible that examined the use of ML models and vital signs to predict the risk of patient deterioration. No additional studies were identified through citation tracking after the original search, indicating our search strategy was comprehensive. Unlike previous reviews, inclusion criteria for the review supported the examination of findings from studies conducted across a variety of clinical settings including specialty units or wards and ambulatory care. This helped in characterizing the use of ML-based prediction models in different patient-care environments with varying clinical endpoints. Wherever the original studies provided the data, comparisons were drawn between the performance of the ML models and that of aggregate-weighted EWS. This gives an indication of the differences in accuracy of the models in predicting clinical deterioration.
Limitations
The findings within this review are subject to some limitations. First, the literature search, assessment of eligibility of full-text articles, inclusion in the review, and extraction of study data were carried out by only 1 author. Second, only the findings from published studies were included in this scoping review, which may affect the results due to publication bias. While studies from a variety of settings were included, the generalizability of our findings may be limited due to the heterogeneity of patient populations, clinical practices, and study methodologies. Sampling procedures and frequencies varied across studies from single to multiple observations of patient vital signs, and clinical outcome definitions were based on different criteria or aggregate-weighted EWS. Finally, due to this variation in ML methods, prediction windows, and outcome reporting, a meta-analysis was not feasible.
Conclusion
Our findings suggest that ML-based EWS models incorporating easily accessible vital sign measurements are effective in predicting physiological deterioration in patients. Improved prediction performance was also observed with these models when compared to traditional aggregate-based risk stratification tools. The clinical impact of these ML-based EWS could be significant for clinical staff and patients due to decreased false alerts and increased early detection of warning signs for timely intervention, though further development of these models is needed and the necessary prospective research to establish actual clinical utility does not yet exist.
Abbreviations
- AUROC
area under the receiver operating characteristic
- AVPU
alert, verbal, pain, unresponsive
- BP
blood pressure
- ED
emergency department
- EWS
early warning system
- HR
heart rate
- ICU
intensive care unit
- MEWS
Modified Early Warning Score
- MIMIC
Medical Information Mart for Intensive Care
- ML
machine learning
- NEWS
National Early Warning Score
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- qSOFA
quick Sequential Organ Failure Assessment
- RR
respiratory rate
- TRIPOD
Transparent Reporting of a Multivariable Prediction Model for Individual Prognosis or Diagnosis
Appendix
Search terms.
Description of ML methods and relevant terms.
Comparison between performance of ML based EWS and aggregate EWS.
Footnotes
Authors' Contributions: SM contributed to conceptualization, data collection, data analysis, and manuscript writing. JP contributed to conceptualization, manuscript writing, and manuscript review. WN and SD contributed equally to manuscript writing and review. PD contributed to manuscript writing and review. MM and NB contributed to manuscript review.
Conflicts of Interest: PJD is a member of a research group with a policy of not accepting honorariums or other payments from industry for their own personal financial gain. They do accept honorariums/payments from industry to support research endeavours and costs to participate in meetings.
Based on study questions PJD has originated and grants he has written, he has received grants from Abbott Diagnostics, AstraZeneca, Bayer, Boehringer Ingelheim, Bristol-Myers-Squibb, Coviden, Octapharma, Philips Healthcare, Roche Diagnostics, Siemens, and Stryker.
PJD has participated in advisory board meetings for GlaxoSmithKline, Boehringer Ingelheim, Bayer, and Quidel Canada. He also attended an expert panel meeting with AstraZeneca and Boehringer Ingelheim.
The other authors declare no conflicts of interest.
References
- 1.Barfod C, Lauritzen MMP, Danker JK, Sölétormos G, Forberg JL, Berlac PA, Lippert F, Lundstrøm LH, Antonsen K, Lange KHW. Abnormal vital signs are strong predictors for intensive care unit admission and in-hospital mortality in adults triaged in the emergency department - a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2012 Apr 10;20:28. doi: 10.1186/1757-7241-20-28. https://sjtrem.biomedcentral.com/articles/10.1186/1757-7241-20-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hillman KM, Bristow PJ, Chey T, Daffurn K, Jacques T, Norman SL, Bishop GF, Simmons G. Antecedents to hospital deaths. Intern Med J. 2001 Aug;31(6):343–8. doi: 10.1046/j.1445-5994.2001.00077.x. [DOI] [PubMed] [Google Scholar]
- 3.McGaughey J, Alderdice F, Fowler R, Kapila A, Mayhew A, Moutray M. Outreach and Early Warning Systems (EWS) for the prevention of intensive care admission and death of critically ill adult patients on general hospital wards. Cochrane Database Syst Rev. 2007 Jul 18;(3):CD005529. doi: 10.1002/14651858.CD005529.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Smith GB, Prytherch DR, Schmidt PE, Featherstone PI, Higgins B. A review, and performance evaluation, of single-parameter "track and trigger" systems. Resuscitation. 2008 Oct;79(1):11–21. doi: 10.1016/j.resuscitation.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 5.Gardner-Thorpe J, Love N, Wrightson J, Walsh S, Keeling N. The value of Modified Early Warning Score (MEWS) in surgical in-patients: a prospective observational study. Ann R Coll Surg Engl. 2006 Oct;88(6):571–5. doi: 10.1308/003588406X130615. http://europepmc.org/abstract/MED/17059720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao H, McDonnell A, Harrison DA, Moore T, Adam S, Daly K, Esmonde L, Goldhill DR, Parry GJ, Rashidian A, Subbe CP, Harvey S. Systematic review and evaluation of physiological track and trigger warning systems for identifying at-risk patients on the ward. Intensive Care Med. 2007 Apr;33(4):667–79. doi: 10.1007/s00134-007-0532-3. [DOI] [PubMed] [Google Scholar]
- 7.Subbe CP, Slater A, Menon D, Gemmell L. Validation of physiological scoring systems in the accident and emergency department. Emerg Med J. 2006 Nov;23(11):841–5. doi: 10.1136/emj.2006.035816. http://europepmc.org/abstract/MED/17057134. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith GB, Prytherch DR, Meredith P, Schmidt PE, Featherstone PI. The ability of the National Early Warning Score (NEWS) to discriminate patients at risk of early cardiac arrest, unanticipated intensive care unit admission, and death. Resuscitation. 2013 Apr;84(4):465–70. doi: 10.1016/j.resuscitation.2012.12.016. [DOI] [PubMed] [Google Scholar]
- 9.Tam B, Xu M, Kwong M, Wardell C, Kwong A, Fox-Robichaud A. The Admission Hamilton Early Warning Score (HEWS) Predicts the Risk of Critical Event during Hospitalization. Can Journ Gen Int Med. 2017 Feb 24;11(4):1. doi: 10.22374/cjgim.v11i4.190. [DOI] [Google Scholar]
- 10.Prytherch DR, Smith GB, Schmidt PE, Featherstone PI. ViEWS--Towards a national early warning score for detecting adult inpatient deterioration. Resuscitation. 2010 Aug;81(8):932–7. doi: 10.1016/j.resuscitation.2010.04.014. [DOI] [PubMed] [Google Scholar]
- 11.Kwon J, Lee Y, Lee Y, Lee S, Park H, Park J. Validation of deep-learning-based triage and acuity score using a large national dataset. PLoS One. 2018;13(10):e0205836. doi: 10.1371/journal.pone.0205836. https://dx.plos.org/10.1371/journal.pone.0205836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bates DW, Saria S, Ohno-Machado L, Shah A, Escobar G. Big data in health care: using analytics to identify and manage high-risk and high-cost patients. Health Aff (Millwood) 2014 Jul;33(7):1123–31. doi: 10.1377/hlthaff.2014.0041. [DOI] [PubMed] [Google Scholar]
- 13.Churpek MM, Yuen TC, Park SY, Gibbons R, Edelson DP. Using electronic health record data to develop and validate a prediction model for adverse outcomes in the wards*. Crit Care Med. 2014 Apr;42(4):841–8. doi: 10.1097/CCM.0000000000000038. http://europepmc.org/abstract/MED/24247472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Linnen DT, Escobar GJ, Hu X, Scruth E, Liu V, Stephens C. Statistical Modeling and Aggregate-Weighted Scoring Systems in Prediction of Mortality and ICU Transfer: A Systematic Review. J Hosp Med. 2019 Mar;14(3):161–169. doi: 10.12788/jhm.3151. http://europepmc.org/abstract/MED/30811322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Brekke IJ, Puntervoll LH, Pedersen PB, Kellett J, Brabrand M. The value of vital sign trends in predicting and monitoring clinical deterioration: A systematic review. PLoS One. 2019;14(1):e0210875. doi: 10.1371/journal.pone.0210875. https://dx.plos.org/10.1371/journal.pone.0210875. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018 Oct 02;169(7):467–473. doi: 10.7326/M18-0850. https://www.acpjournals.org/doi/10.7326/M18-0850?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. [DOI] [PubMed] [Google Scholar]
- 17.Zweig MH, Campbell G. Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem. 1993 Apr;39(4):561–77. [PubMed] [Google Scholar]
- 18.Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009 Jul 21;6(7):e1000097. doi: 10.1371/journal.pmed.1000097. https://dx.plos.org/10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Higgins JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. 2011. [2021-01-09]. www.handbook.cochrane.org.
- 20.Collins GS, Reitsma JB, Altman DG, Moons KGM. Transparent Reporting of a multivariable prediction model for Individual Prognosis Or Diagnosis (TRIPOD): the TRIPOD Statement. Br J Surg. 2015 Feb;102(3):148–58. doi: 10.1002/bjs.9736. [DOI] [PubMed] [Google Scholar]
- 21.Olsen RM, Aasvang EK, Meyhoff CS, Dissing Sorensen HB. Towards an automated multimodal clinical decision support system at the post anesthesia care unit. Comput Biol Med. 2018 Oct 01;101:15–21. doi: 10.1016/j.compbiomed.2018.07.018. [DOI] [PubMed] [Google Scholar]
- 22.Larburu N, Artetxe A, Escolar V, Lozano A, Kerexeta J. Artificial Intelligence to Prevent Mobile Heart Failure Patients Decompensation in Real Time: Monitoring-Based Predictive Model. Mobile Information Systems. 2018 Nov 05;2018:1–11. doi: 10.1155/2018/1546210. [DOI] [Google Scholar]
- 23.Chiew CJ, Liu N, Tagami T, Wong TH, Koh ZX, Ong MEH. Heart rate variability based machine learning models for risk prediction of suspected sepsis patients in the emergency department. Medicine (Baltimore) 2019 Feb;98(6):e14197. doi: 10.1097/MD.0000000000014197. doi: 10.1097/MD.0000000000014197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Churpek MM, Adhikari R, Edelson DP. The value of vital sign trends for detecting clinical deterioration on the wards. Resuscitation. 2016 May;102:1–5. doi: 10.1016/j.resuscitation.2016.02.005. http://europepmc.org/abstract/MED/26898412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Clifton L, Clifton DA, Pimentel MAF, Watkinson PJ, Tarassenko L. Predictive monitoring of mobile patients by combining clinical observations with data from wearable sensors. IEEE J Biomed Health Inform. 2014 May;18(3):722–30. doi: 10.1109/JBHI.2013.2293059. [DOI] [PubMed] [Google Scholar]
- 26.Kwon J, Lee Y, Lee Y, Lee S, Park J. An Algorithm Based on Deep Learning for Predicting In-Hospital Cardiac Arrest. J Am Heart Assoc. 2018 Jun 26;7(13):1. doi: 10.1161/JAHA.118.008678. https://www.ahajournals.org/doi/10.1161/JAHA.118.008678?url_ver=Z39.88-2003&rfr_id=ori:rid:crossref.org&rfr_dat=cr_pub%3dpubmed. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Forkan ARM, Khalil I. PEACE-Home: Probabilistic estimation of abnormal clinical events using vital sign correlations for reliable home-based monitoring. Pervasive and Mobile Computing. 2017 Jul;38:296–311. doi: 10.1016/j.pmcj.2016.12.009. [DOI] [Google Scholar]
- 28.Forkan ARM, Khalil I. A clinical decision-making mechanism for context-aware and patient-specific remote monitoring systems using the correlations of multiple vital signs. Comput Methods Programs Biomed. 2017 Feb;139:1–16. doi: 10.1016/j.cmpb.2016.10.018. [DOI] [PubMed] [Google Scholar]
- 29.Forkan ARM, Khalil I, Atiquzzaman M. ViSiBiD: A learning model for early discovery and real-time prediction of severe clinical events using vital signs as big data. Computer Networks. 2017 Feb;113:244–257. doi: 10.1016/j.comnet.2016.12.019. [DOI] [Google Scholar]
- 30.Lee J, Scott D, Villarroel M, Clifford G, Saeed M, Mark R. Open-access MIMIC-II database for intensive care research. Conf Proc IEEE Eng Med Biol Soc. 2011;2011:8315–8. doi: 10.1109/iembs.2011.6092050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Johnson AEW, Pollard TJ, Shen L, Lehman LH, Feng M, Ghassemi M, Moody B, Szolovits P, Celi LA, Mark RG. MIMIC-III, a freely accessible critical care database. Sci Data. 2016 May 24;3:160035. doi: 10.1038/sdata.2016.35. doi: 10.1038/sdata.2016.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tarassenko L, Hann A, Young D. Integrated monitoring and analysis for early warning of patient deterioration. Br J Anaesth. 2006 Jul;97(1):64–8. doi: 10.1093/bja/ael113. https://linkinghub.elsevier.com/retrieve/pii/S0007-0912(17)35184-X. [DOI] [PubMed] [Google Scholar]
- 33.van Wyk F, Khojandi A, Kamaleswaran R, Akbilgic O, Nemati S, Davis RL. How much data should we collect? A case study in sepsis detection using deep learning. IEEE Healthcare Innovations and Point of Care Technologies (HI-POCT); November 6-8, 2017; Bethesda, MD. 2017. [DOI] [Google Scholar]
- 34.Mao Q, Jay M, Hoffman JL, Calvert J, Barton C, Shimabukuro D, Shieh L, Chettipally U, Fletcher G, Kerem Y, Zhou Y, Das R. Multicentre validation of a sepsis prediction algorithm using only vital sign data in the emergency department, general ward and ICU. BMJ Open. 2018 Jan 26;8(1):e017833. doi: 10.1136/bmjopen-2017-017833. https://bmjopen.bmj.com/lookup/pmidlookup?view=long&pmid=29374661. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Jang D, Kim J, Jo YH, Lee JH, Hwang JE, Park SM, Lee DK, Park I, Kim D, Chang H. Developing neural network models for early detection of cardiac arrest in emergency department. Am J Emerg Med. 2020 Jan;38(1):43–49. doi: 10.1016/j.ajem.2019.04.006. [DOI] [PubMed] [Google Scholar]
- 36.Liu N, Koh ZX, Goh J, Lin Z, Haaland B, Ting BP, Ong MEH. Prediction of adverse cardiac events in emergency department patients with chest pain using machine learning for variable selection. BMC Med Inform Decis Mak. 2014 Aug 23;14:75. doi: 10.1186/1472-6947-14-75. https://bmcmedinformdecismak.biomedcentral.com/articles/10.1186/1472-6947-14-75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desautels T, Calvert J, Hoffman J, Jay M, Kerem Y, Shieh L, Shimabukuro D, Chettipally U, Feldman MD, Barton C, Wales DJ, Das R. Prediction of Sepsis in the Intensive Care Unit With Minimal Electronic Health Record Data: A Machine Learning Approach. JMIR Med Inform. 2016 Sep 30;4(3):e28. doi: 10.2196/medinform.5909. https://medinform.jmir.org/2016/3/e28/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ho J, Park Y. Learning from different perspectives: Robust cardiac arrest prediction via temporal transfer learning. Annu Int Conf IEEE Eng Med Biol Soc. 2017 Jul;2017:1672–1675. doi: 10.1109/EMBC.2017.8037162. [DOI] [PubMed] [Google Scholar]
- 39.Li X, Wang Y. Adaptive online monitoring for ICU patients by combining just-in-time learning and principal component analysis. J Clin Monit Comput. 2016 Dec;30(6):807–820. doi: 10.1007/s10877-015-9778-4. [DOI] [PubMed] [Google Scholar]
- 40.Shashikumar SP, Stanley MD, Sadiq I, Li Q, Holder A, Clifford GD, Nemati S. Early sepsis detection in critical care patients using multiscale blood pressure and heart rate dynamics. J Electrocardiol. 2017;50(6):739–743. doi: 10.1016/j.jelectrocard.2017.08.013. http://europepmc.org/abstract/MED/28916175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Yoon JH, Mu L, Chen L, Dubrawski A, Hravnak M, Pinsky MR, Clermont G. Predicting tachycardia as a surrogate for instability in the intensive care unit. J Clin Monit Comput. 2019 Dec;33(6):973–985. doi: 10.1007/s10877-019-00277-0. http://europepmc.org/abstract/MED/30767136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chiu Y, Villar SS, Brand JW, Patteril MV, Morrice DJ, Clayton J, Mackay JH. Logistic early warning scores to predict death, cardiac arrest or unplanned intensive care unit re-admission after cardiac surgery. Anaesthesia. 2020 Feb;75(2):162–170. doi: 10.1111/anae.14755. http://europepmc.org/abstract/MED/31270799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Guillame-Bert M, Dubrawski A, Wang D, Hravnak M, Clermont G, Pinsky MR. Learning temporal rules to forecast instability in continuously monitored patients. J Am Med Inform Assoc. 2017 Jan;24(1):47–53. doi: 10.1093/jamia/ocw048. http://europepmc.org/abstract/MED/27274020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen L, Ogundele O, Clermont G, Hravnak M, Pinsky MR, Dubrawski AW. Dynamic and Personalized Risk Forecast in Step-Down Units. Implications for Monitoring Paradigms. Ann Am Thorac Soc. 2017 Mar;14(3):384–391. doi: 10.1513/AnnalsATS.201611-905OC. http://europepmc.org/abstract/MED/28033032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Badriyah T, Briggs JS, Meredith P, Jarvis SW, Schmidt PE, Featherstone PI, Prytherch DR, Smith GB. Decision-tree early warning score (DTEWS) validates the design of the National Early Warning Score (NEWS) Resuscitation. 2014 Mar;85(3):418–23. doi: 10.1016/j.resuscitation.2013.12.011. [DOI] [PubMed] [Google Scholar]
- 46.Cabitza F, Rasoini R, Gensini GF. Unintended Consequences of Machine Learning in Medicine. JAMA. 2017 Aug 08;318(6):517–518. doi: 10.1001/jama.2017.7797. [DOI] [PubMed] [Google Scholar]
- 47.Stead WW. Clinical Implications and Challenges of Artificial Intelligence and Deep Learning. JAMA. 2018 Sep 18;320(11):1107–1108. doi: 10.1001/jama.2018.11029. [DOI] [PubMed] [Google Scholar]
- 48.Tonekaboni S, Joshi S, McCradden MD, Goldenberg A. What Clinicians Want: Contextualizing Explainable Machine Learning for Clinical End Use. Proceedings of the 4th Machine Learning for Healthcare Conference. 2019;106:359–380. [Google Scholar]
- 49.Wiens J, Saria S, Sendak M, Ghassemi M, Liu VX, Doshi-Velez F, Jung K, Heller K, Kale D, Saeed M, Ossorio PN, Thadaney-Israni S, Goldenberg A. Do no harm: a roadmap for responsible machine learning for health care. Nat Med. 2019 Sep;25(9):1337–1340. doi: 10.1038/s41591-019-0548-6. [DOI] [PubMed] [Google Scholar]
- 50.Wang ZJ, Turko R, Shaikh O, Park H, Das N, Hohman F, Kahng M, Chau DH. CNN EXPLAINER: Learning Convolutional Neural Networks with Interactive Visualization. IEEE Trans. Visual. Comput. Graphics. 2020:1. doi: 10.1109/tvcg.2020.3030418. [DOI] [PubMed] [Google Scholar]
- 51.Ribeiro MT, Singh S, Guestrin C. "Why Should I Trust You?": Explaining the Predictions of Any Classifier. Cornell University. 2016. [2021-01-09]. https://arxiv.org/abs/1602.04938.
- 52.Lauritsen SM, Kristensen M, Olsen MV, Larsen MS, Lauritsen KM, Jørgensen MJ, Lange J, Thiesson B. Explainable artificial intelligence model to predict acute critical illness from electronic health records. Nat Commun. 2020 Jul 31;11(1):3852. doi: 10.1038/s41467-020-17431-x. doi: 10.1038/s41467-020-17431-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Sokol K, Flach P. Explainability Fact Sheets: A Framework for Systematic Assessment of Explainable Approaches. Cornell University. 2019. [2021-01-09]. https://arxiv.org/abs/1912.05100.
- 54.Vascular Events in Noncardiac Surgery Patients Cohort Evaluation (VISION) Study Investigators. Spence J, LeManach Y, Chan MT, Wang CY, Sigamani A, Xavier D, Pearse R, Alonso-Coello P, Garutti I, Srinathan SK, Duceppe E, Walsh M, Borges FK, Malaga G, Abraham V, Faruqui A, Berwanger O, Biccard BM, Villar JC, Sessler DI, Kurz A, Chow CK, Polanczyk CA, Szczeklik W, Ackland G, Jacka M, Guyatt GH, Sapsford RJ, Williams C, Cortes OL, Coriat P, Patel A, Tiboni M, Belley-Côté EP, Yang S, Heels-Ansdell D, McGillion M, Parlow S, Patel M, Pettit S, Yusuf S, Devereaux PJ. Association between complications and death within 30 days after noncardiac surgery. CMAJ. 2019 Jul 29;191(30):E830–E837. doi: 10.1503/cmaj.190221. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=31358597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sun Z, Sessler DI, Dalton JE, Devereaux PJ, Shahinyan A, Naylor AJ, Hutcherson MT, Finnegan PS, Tandon V, Darvish-Kazem S, Chugh S, Alzayer H, Kurz A. Postoperative Hypoxemia Is Common and Persistent: A Prospective Blinded Observational Study. Anesth Analg. 2015 Sep;121(3):709–15. doi: 10.1213/ANE.0000000000000836. http://europepmc.org/abstract/MED/26287299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Turan A, Chang C, Cohen B, Saasouh W, Essber H, Yang D, Ma C, Hovsepyan K, Khanna AK, Vitale J, Shah A, Ruetzler K, Maheshwari K, Sessler DI. Incidence, Severity, and Detection of Blood Pressure Perturbations after Abdominal Surgery: A Prospective Blinded Observational Study. Anesthesiology. 2019 Apr;130(4):550–559. doi: 10.1097/ALN.0000000000002626. https://pubs.asahq.org/anesthesiology/article-lookup/doi/10.1097/ALN.0000000000002626. [DOI] [PubMed] [Google Scholar]
- 57.Cook NR. Use and misuse of the receiver operating characteristic curve in risk prediction. Circulation. 2007 Feb 20;115(7):928–35. doi: 10.1161/CIRCULATIONAHA.106.672402. http://circ.ahajournals.org/cgi/pmidlookup?view=long&pmid=17309939. [DOI] [PubMed] [Google Scholar]
- 58.Romero-Brufau S, Huddleston JM, Escobar GJ, Liebow M. Why the C-statistic is not informative to evaluate early warning scores and what metrics to use. Crit Care. 2015 Aug 13;19:285. doi: 10.1186/s13054-015-0999-1. https://ccforum.biomedcentral.com/articles/10.1186/s13054-015-0999-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Search terms.
Description of ML methods and relevant terms.
Comparison between performance of ML based EWS and aggregate EWS.


