Abstract
Tropomyosin receptor kinase A, B and C (TRKA, TRKB and TRKC), which are well-known members of the cell surface receptor tyrosine kinase (RTK) family, are encoded by the neurotrophic receptor tyrosine kinase 1, 2 and 3 (NTRK1, NTRK2 and NTRK3) genes, respectively. TRKs can regulate cell proliferation, differentiation and even apoptosis through the RAS/MAPKs, PI3K/AKT and PLCγ pathways. Gene fusions involving NTRK act as oncogenic drivers of a broad diversity of adult and pediatric tumors, and TRKs have become promising antitumor targets. Therefore, achieving a comprehensive understanding of TRKs and relevant TRK inhibitors should be urgently pursued for the further development of novel TRK inhibitors for potential clinical applications. This review focuses on summarizing the biological functions of TRKs and NTRK fusion proteins, the development of small-molecule TRK inhibitors with different chemotypes and their activity and selectivity, and the potential therapeutic applications of these inhibitors for future cancer drug discovery efforts.
KEY WORDS: Tropomyosin receptor kinase, Neurotrophic receptor tyrosine kinase fusions, Small-molecule inhibitor, NTRK fusion cancer
Abbreviations: AFAP1, actin filament-associated protein 1; AML, acute myeloid leukemia; ARHGEF2, Rho/Rac guanine nucleotide exchange factor 2; BCAN, brevican; BDNF, brain-derived neurotrophic factor; BTBD1, BTB (POZ) domain containing 1; CDK-2, cyclin-dependent kinase 2; CR, complete response; CRC, colorectal cancer; CTCs, sequencing of circulating tumor cells; DFG, Asp-Phe-Gly; DOR, durable objective responses; ETV6, ETS translocation variant 6; EWG, electron-withdrawing group; FDA, U.S. Food and Drug Administration; FISH, fluorescence in situ hybridization; GBM, glioblastoma multiforme; HNSCC, head and neck squamous cell carcinoma; HTS, high-throughput screening; ICC, intrahepatic cholangiocarcinoma; IG-C2, Ig-like C2 type I; LMNA, lamin A/C; MASC, mammary analogue secretory carcinoma; MPRIP, myosin phosphatase Rho interacting protein; NACC2, NACC family member 2; NCCN, National Comprehensive Cancer Network; NFASC, neurofascin; NGF, nerve growth factor; NGS, next-generation sequencing of tumor tissue; NSCLC, non-small cell lung cancer; NT3, neurotrophin-3; NTRK, neurotrophic receptor tyrosine kinase; OAK, osteoarthritis of the knee; ORR, overall response rate; PAN3, poly(A) nuclease 3; PPL, periplakin; PROTAC proteolysis targeting chimera, QKI; quaking I protein, RABGAP1L; RABGTPase activating protein 1-like, RFWD2; ring finger and WD repeat domain 2, E3 ubiquitin protein ligase; RTK, receptor tyrosine kinase; SAR, structure–activity relationship; SBC, secretory breast carcinoma; SCYL3, SCY1 like pseudokinase 3; SQSTM1, sequestosome 1; TFG, TRK-fused gene; TP53, tumor protein P53; TPM3, tropomyosin 3; TPR, translocated promoter region; TRIM24, tripartite motif containing 24; TRK, tropomyosin receptor kinase; VCL, vinculin; VEGFR2, vascular endothelial growth factor receptor 2
Graphical abstract
This review summarized the biological structure and function of tropomyosin receptor kinases (TRKs), as well as neurotrophic receptor tyrosine kinase (NTRK) fusion proteins. The discovery and development of typical TRK inhibitors were discussed by concentrating on their different chemotypes, activity, selectivity and cocrystal structures.
1. Introduction
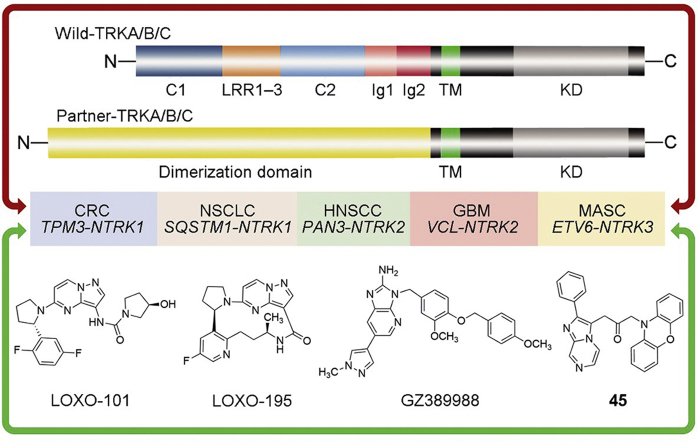
Tropomyosin receptor kinases A, B and C (TRKA, TRKB and TRKC), which belong to the cell surface receptor tyrosine kinase (RTK) family, are encoded by the neurotrophic receptor tyrosine kinase 1, 2 and 3 (NTRK1, NTRK2 and NTRK3) genes, respectively1. TRKs are transmembrane receptor proteins that contain an extracellular ligand-binding domain, a transmembrane domain, and an intracellular domain with kinase activity (Fig. 1A)2. The intracellular kinase domain of RTK is structurally conserved, and the kinase domains of TRKA, TRKB, and TRKC have a total sequence homology ranging from 71.9% to 78.3%, with TRKB and TRKC being the most similar homologs3. The main distinction between the three subtypes of the TRKs is the different ligands that activate the receptors. The nerve growth factors binding to TRKA are mainly nerve growth factor (NGF), neurotrophin-7, and neurotrophin-62,4, while TRKB binds nerve growth factors such as brain-derived neurotrophic factor (BDNF) and neurotrophin-4/55, and TRKC specifically binds to neurotrophin-3 (NT3)6. Previous studies confirmed that as nerve growth factor receptors, these TRKs can modulate cell proliferation, differentiation, metabolism, and even apoptosis through the phosphorylation of their downstream matrix targets7, 8, 9. TRKs are constitutively activated via various mechanisms in malignant human cancers. The most acknowledged mechanism of this is represented by the NTRK gene fusions, in which the 3ʹ region of the NTRK gene is rearranged intrachromosomally or interchromosomally and then connects with the 5ʹ sequence of the fusion partner gene, leading to a high risk of tumorigenesis10. Different NTRK fusion proteins, e.g., tropomyosin 3-NTRK1 (TPM3-NTRK1) in colorectal cancer (CRC)9 and ETS translocation variant 6-NTRK3 (ETV6-NTRK3) in secreted mesoblastic congenital fibrosarcoma and in infantile fibrosarcoma11,12, can mediate the same downstream pathway and increase the oncogenic risk of TRKs through the dimerization/oligomerization of the NTRK fusion proteins13. Other oncogenic forms of NTRK, e.g., activation of the NTRK1 gene, splice variants and overexpression of TRKs, have also been observed in multiple cancers, including human neuroblastoma14, acute myeloid leukemia specimens (AML)15, lung cancer, cylindrical tumor, breast cancer, and others16, 17, 18, 19. The activation of TRK receptors caused by NTRK fusions is considered as a pan-cancer carcinogenic factor. Because the transmembrane fusions of the TRKs regularly result in a lack of extracellular domains, common targeted therapies (e.g., monoclonal antibody therapy) will not be efficient. Therefore, the main method of targeting NTRK fusion genes is the employment of TRK small molecule inhibitors.
Figure 1.
(A) The structure of TRKs and (B) apo crystal structure of TRKA protein (PDB ID: 6D22, 2.5 Å).
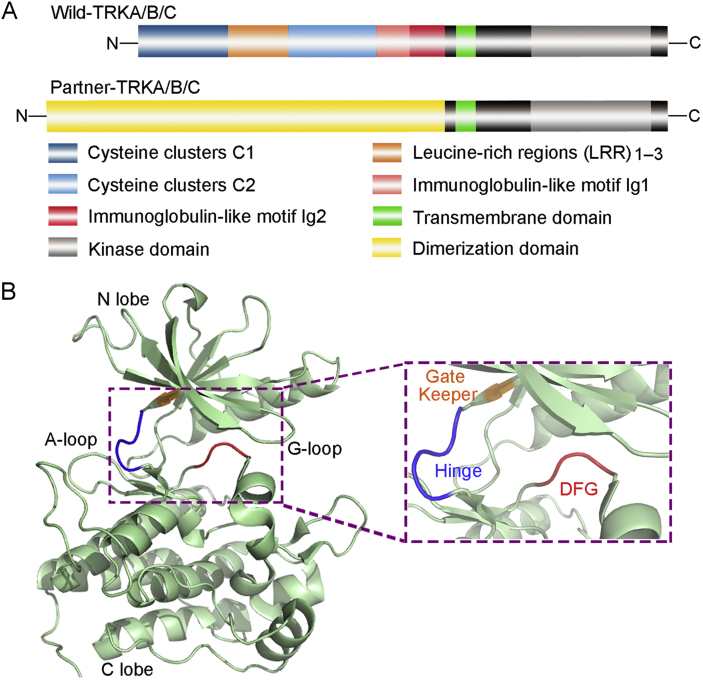
Over the past decade, NTRK fusion cancers have attracted extensive attention from pharmaceutical companies and pharmaceutical chemistry researchers, and TRKs have become important antitumor targets with promising research prospects. Consequently, substantial efforts have been made in the development of targeted therapies for this disease, primarily reflected in the emergence of a large number of TRK small-molecule inhibitors, including larotrectinib, entrectinib, belizatinib, AZ23, Cpd5n, PHA-E429, milciclib, GNF-5837, cabozantinib, sitravatinib, and altiratinib. Among these, larotrectinib (Vitrakvi®) and entrectinib (Rozlytrek®) as anticancer drugs were approved by the U.S. Food and Drug Administration (FDA) in November 2018 and August 2019, respectively (Fig. 2)20,21. Both of these drugs were approved based upon biomarkers rather than on being tumor-agnostic, which changes the traditional treatment strategy for the primary tumor site and reflects the progress in using biomarkers to guide drug development and more precise drug administration22. In addition, a number of other TRK inhibitors, such as XL18423, MGCD51624, DS-605125, TSR-01126, DCC270127, LOXO-19528,29, and TPX-000530 (Fig. 2), are currently being evaluated in various phases of clinical trials. Unfortunately, similar to other targeted therapies, acquired drug resistance toward entrectinib in an NTRK1-positive CRC patient was reported after four months of treatment, which limited the efficacy of the TRK small-molecule inhibitors28,31. Encouragingly, more effective drugs have overcome the resistance of the first-generation TRK inhibitors. In particular, LOXO-19528,29 and TPX-000530 have shown in vitro activity in the low nanomolar range against multiple TRK mutants.
Figure 2.
Representative TRK inhibitors in clinical trials and clinic.
Herein, we summarize the structural characteristics, biological functions, and aberrations of TRKs. In addition, this review aims to present an overview of NTRK fusion proteins and a summary of typical TRK inhibitors from the perspective of their activity, selectivity, cocrystal structures and the structural basis of drug resistance, as well as the potential therapeutic strategies against acquired drug resistance.
2. Structures and downstream signaling pathways of TRKs
As summarized in our previous review, a kinase is a part of a signaling cascade, and its main function is to catalyze the diversion of a terminal phosphate group from ATP to a protein substrate32. The catalytic domain of TRKs consists of a small amino terminus (N-lobe) and a large carboxyl terminus (C-lobe) connected by a hinge region; an example of this is shown in Fig. 1B in the apo crystal structure of the TRKA protein. The proximal activation loop is labeled with a conserved Asp-Phe-Gly (DFG) sequence to regulate enzyme activity. This loop is completely ordered in the inactivated state of TRKs and occupies the active site, thereby preventing the binding of ATP33. In the DFG-out conformation, the phenylalanine of the DFG motif is located in the hydrophobic pocket behind the gatekeeper phenylalanine of the active site. The DFG-in conformation is characterized by a rotation of the DFG residues out of the active site, in which ATP binds to the kinase and subsequently transfers its terminal phosphate group.
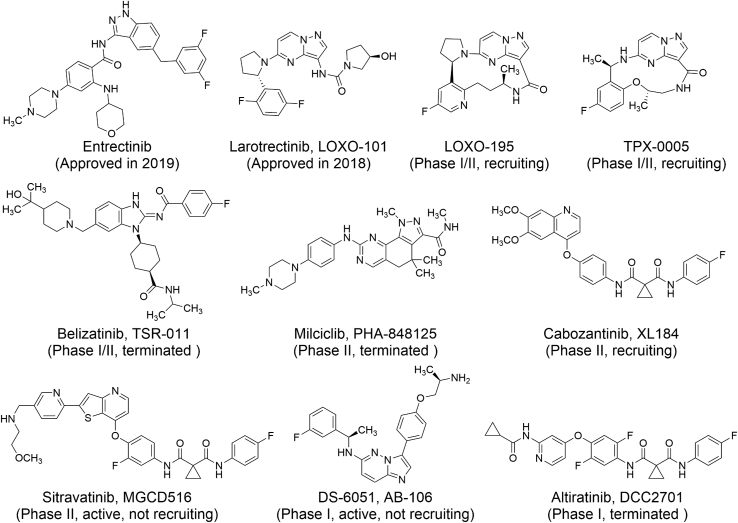
Similar to most tyrosine kinases, the receptor–ligand interaction leads to receptor dimerization, autophosphorylation, and the subsequent activation of TRK activity34,35. As shown in Fig. 3, activated kinases trigger the transduction of downstream signaling pathways, leading to cell proliferation, differentiation, and survival36. TRK proteins can activate multiple signaling pathways (Fig. 3). The combination of NGF and TRKA can inhibit apoptotic proteins, promote neuron differentiation and axon growth, and mediate allergic reactions by activating the PI3K/MAPK/PLCγ signaling pathways37. BDNF binds to the TRKB receptor and triggers a variety of downstream signaling cascades, including the RAS/MAPK pathway, the PI3K/3−PDK1/AKT pathway, and the activated PLCγ pathway, causing nerve metabolic cell proliferation and differentiation38. TRKC mediates NT3 signaling through the PI3K/AKT pathway, thereby increasing cell survival and preventing apoptosis39. However, the TRK signaling pathways have not been fully clarified. There are other ways to activate downstream signaling pathways. For instance, in colon cancer KM12 cells, the abnormal expression of the TPM3-NTRK1 chimeric protein makes the downstream PI3K/AKT, RAS/MAPK, and PLCγ pathways also abnormally active16. The TRK fusion proteins will be continuously active, triggering a permanent signaling cascade that drives the proliferation and growth of the TRK fusion tumors.
Figure 3.
Schematic representation of TRK receptors signaling pathways.
3. NTRK gene expression in related diseases
3.1. NTRK mutations, splice variants, and TRK overexpression
It is now well established that TRKs are activated through NTRK fusions, mutations, splice variants, and TRK overexpression. These activated TRKs are no longer regulated and controlled by nerve growth factor ligands and have a risk of inducing carcinogenesis. Somatic NTRK mutations have been reported in different types of cancers, such as CRC9, melanoma40, AML41, large cell neuron cancer and non-small cell lung cancer (NSCLC)42,43. However, the potential role of NTRK mutations in promoting tumorigenesis and cancer progression has not been identified. In addition, splice variants that activate NTRK1 have been detected and characterized. It is reported that the NTRK1 splice variant TRKAIII and the framework deletion mutant (ΔTRKA) have been detected to be carcinogenic in human neuroblastoma9 and AML specimens44, 45, 46, 47. Finally, the overexpression of TRKs in all kinds of adult and pediatric cancers, including breast cancer, intraepithelial carcinoma, malignant melanoma, lung cancer, and neuroblastoma16, 17, 18, 19, can affect the migration of cancer cells. In summary, TRK activated by NTRK mutations, splice variants, and TRK overexpression can disrupt the ability to regulate the kinase domains, suggesting that loss of the extracellular domain form or function is a key attribute in TRK's oncogenic potential.
3.2. NTRK fusions
Gene fusions involving NTRK represent the most common mechanism for TRK activation in malignant tumors5. These fusions stimulate the occurrence and development of tumors through the PLCγ, PI3K and RAS/RAF pathways to stimulate uncontrolled signal amplification and transmission48, 49, 50, 51. For example, the RAS/RAF pathway has been observed in both CRC (KM-12) and lung cancers (CUTO-3). NTRK fusions can be found in adult and pediatric patients with multiple tumor types, but the exact frequency in solid tumors is unknown45,52. In common cancers, including NSCLC, CRC, and others, the incidence of NTRK fusion is relatively low, approximately 1%–3%45,52, but in some rare cancers, such as infantile fibrosarcoma, similar to secretory breast cancer, congenital mesoderm nephroma (cell or mixed subtype), and others, the incidence of NTRK fusion can reach 90% or higher6,53, 54, 55, 56. In general, due to the promotion of tumor formation, NTRK fusion genes have been considered as an important mediator of early tumorigenesis and development. To date, approximately 25 NTRK fusion proteins have been reported to act as oncogenic drivers in various tumor types, among which TPM3-NTRK1 and ETV6-NTRK3 are the two most common variants45. Table 111,48,57, 58, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80 shows the NTRK fusion proteins and their associated cancer types reported to date.
Table 1.
Reported NTRK gene fusion partners and corresponding cancers.
| Cancer type | NTRK1 | NTRK2 | NTRK3 | Ref. |
|---|---|---|---|---|
| CRC | TPM3 | – | – | 11,57,58 |
| LMNA | – | – | 59 | |
| TPR | – | – | 60 | |
| SCYL3 | – | – | 61 | |
| NSCLC | CD74 | – | – | 48 |
| MPRIP | – | – | 48 | |
| SQSTM1 | – | – | 62 | |
| – | TRIM24 | – | 63 | |
| GBM | ARHGEF2 | – | – | 64 |
| BCAN | – | – | 65,66 | |
| NFASC | – | – | 66 | |
| TPM3 | – | – | 63 | |
| – | – | ETV6 | 63,64 | |
| – | VCL | – | 63 | |
| – | – | BTBD1 | 63 | |
| Pilocytic astrocytoma | – | NACC2 | – | 67 |
| – | QKI | – | 67 | |
| Spitzoid melanoma | TP53 | – | – | 68 |
| LMNA | – | – | 68 | |
| Papillary thyroid cancer | TPM3 | – | – | 69 |
| TFG | – | – | 70 | |
| TPR | – | – | 71 | |
| Thyroid carcinoma | PPL | – | – | 62 |
| Large cell neuroendocrine tumor (lung) | RFWD2 | – | – | 72 |
| ICC | RABGAP1L | – | – | 73 |
| MASC | – | – | ETV6 | 74,75 |
| SBC | – | – | ETV6 | 76 |
| Infantile fibrosarcoma | LMNA | – | – | 77 |
| – | – | ETV6 | 78 | |
| HNSCC | – | PAN3 | – | 79 |
| Mesoblastic | – | – | ETV6 | 80 |
| Low-grade glioma | – | AFAP1 | – | 79 |
−Not applicable.
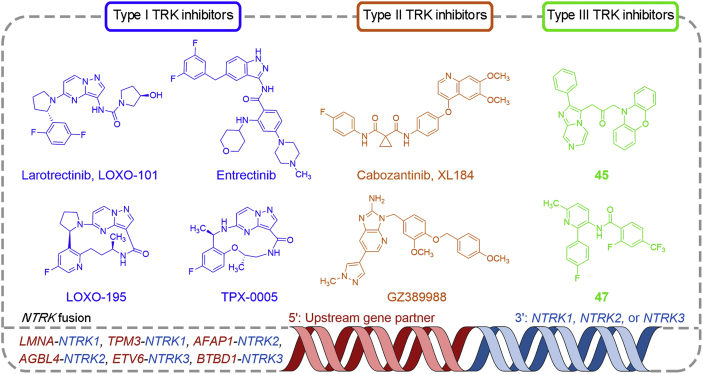
4. TRK inhibitors and their therapeutic implications
The prevalence of NTRK gene fusions is estimated to be 17%–20% in cancer24,76. Blocking abnormal TRK signaling pathways through small-molecule inhibitors has been suggested to be a useful method for inhibiting the proliferation of NTRK fusion tumor cells, which has boosted the ever-increasing interest of the scientific community in developing drugs to inhibit the TRK domains. Therefore, tremendous efforts have been made over the past decade to develop TRK inhibitors with different chemotypes. TRK small-molecule inhibitors can be classified into three different types, namely type I, II and III, based on their site of binding to the TRKs. Small-molecule inhibitors that target the ATP-binding site of an activated kinase are known as type I kinase inhibitors. Inhibitors that target the kinase ATP-binding site and interact with the adjacent hydrophobic pockets are defined as type II kinase inhibitors. Type III kinase inhibitors are also called allosteric inhibitors. They target hydrophobic pockets distant from the ATP-binding site and regulate kinase activity by causing conformational changes in the ATP-binding pocket. Next, we will introduce the discovery, structure–activity relationship (SAR) and activity of existing inhibitors from the perspective of medicinal chemistry.
4.1. Type I TRK inhibitors
Type I kinase inhibitors with ATP competition can recognize the DFG-in conformation of the kinase. Owing to the highly conservative structure of the ATP-binding sites of all kinases, most of these inhibitors have inhibitory activity against other kinases in the same family. The loss of selectivity for the TRKs directly leads to side effects and the toxicity of these drugs. However, through structural optimization, it is still possible to find potential drugs with a high selectivity for the TRKs.
4.1.1. Approved drugs targeting the TRKs
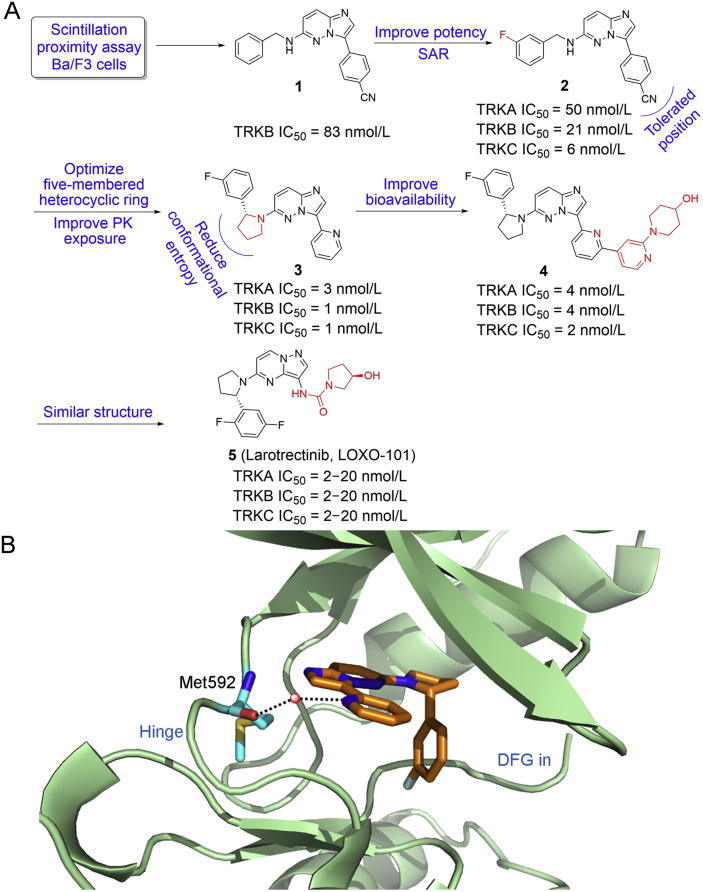
At present, two TRK inhibitors, larotrectinib and entrectinib, have been approved by the FDA for treating patients with solid tumors that have an NTRK fusion without a known acquired drug-resistant mutation. Metastatic or surgical resection may lead to serious morbidity without a satisfactory alternative treatment or progression after treatment22,79. In 2008, by screening with a TRKB scintillation proximity assay, Choi and colleagues81 identified a TRKB inhibitor (IC50 = 83 nmol/L) with a novel benzonitrile-substituted imidazopyridine core (compound 1, Fig. 4A). Due to its poor pharmacokinetic properties, it was difficult to undertake clinical trials. Therefore, it was further optimized. According to the SAR analysis, the 3-substitution of the electron-withdrawing group (EWG) on the benzylamine phenyl ring resulted in a 10-folds increase in the titer (Fig. 4A), e.g., 3-F, while the benzene ring on the other side was substituted with a greater tolerance (compound 2)81. The structurally rigid benzylamine moiety was then changed in a cyclic manner to reduce the conformational entropy, which further improved the potency. As a result, it was found that the dense five-membered ring and the R-configuration showed better efficacy (Fig. 4A, compound 3)81. Compound 3 occupied the front pocket of ATP in the DFG-in conformation and formed a key hydrogen bond with Met592 (Fig. 4B). Derivatization with a cyano group resulted in the report of compound 4 having an effective antiproliferative activity on TRK-transfected BA/F3 and KM-12 cell lines81. However, compound 4 was not entered into clinical trials due to its poor pharmacodynamics81. Compound 5 (larotrectinib) showed low nanomolar cell potency against TRKA/B/C with IC50 values of 2–20 nmol/L (Fig. 4A). Moreover, the biochemical and cell experiments illustrated that the selectivity of compound 5 for TRKA/B/C was approximately 100-folds over a panel of 100 kinases derived from various families21. Currently, the discovery of compound 5 cocrystal structures with TRKs has not been reported. However, due to the structural similarity of compounds 5 and 4, we can deduce that compound 5 has an SAR and crystal-binding mode similar to 4. Compound 5 (larotrectinib) was the first TRK inhibitor approved by the FDA. A large number of clinical tests, including phase I trials for adults (LOXO-TRK-14001, NCT02122913), phase I/II trials for pediatric patients (SCOUT, NCT02637687), and phase II trials for adults and adolescents (NAVIGATE, NCT02576431), showed that the overall response rate (ORR) based on investigator assessment was 81% (95% CI: 72–88, 95% confidence interval: 72–88), in which 63% of the patients had a partial disease response (PR), and 17% of the patients had a complete response (CR)45. Overall, regardless of age or tumor type, larotrectinib has significant and long-lasting antitumor activity in patients with NTRK fusion cancers. Larotrectinib is recommended by the National Comprehensive Cancer Network (NCCN) guidelines as a first-line therapy for those advanced NSCLC patients carrying NTRK fusions82 and as a new second-line therapy for patients with NTRK fusions in metastatic CRC83.
Figure 4.
(A) Discovery and design procedure of the TRK inhibitor, larotrectinib, by combing Scintillation Proximity Assay and medicinal chemistry and (B) X-ray cocrystal structure of TRKA with the R-enantiomer of compound 3 (PDB ID: 4YNE, 2.0 Å). The kinase is illustrated with green ribbons, and the hydrogen bonds are depicted in black dashed lines. Compound atoms are in different colors: C, orange; N, blue; F, light cyan.
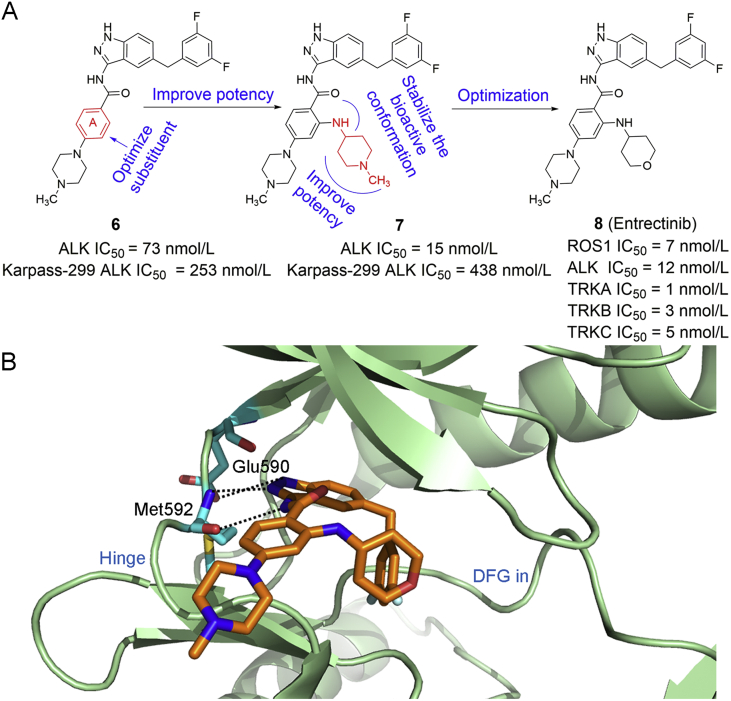
Menichincheri and coworkers84 reported a potential 3-amino-5-substituted indazole compound 6 (Fig. 5A). Compound 6 showed a good inhibitory activity against ALK (IC50 = 73 nmol/L) and a moderate antiproliferative activity in ALK-positive Karpas-299 cells (IC50 = 253 nmol/L)84. Further optimization of the ring A substituent resulted in the identification of compound 7 (ALK IC50 = 15 nmol/L) and compound 8 (entrectinib, ALK IC50 = 12 nmol/L), of which compound 8 displayed a better cell activity (Fig. 5A). Due to the similar three-dimensional structure and catalytic mechanism of the phosphorylation catalytic region of ALK and TRK, compound 8, as an ALK inhibitor, also presented a pan-TRK suppressive activity (TRKA/B/C IC50 = 1, 3, and 5 nmol/L, respectively)85. In the cocrystal complex of TRKA bound with 8 (Fig. 5B), compound 8 occupied the front pocket of ATP in the DFG-in conformation and formed two hydrogen bonds with Glu590 and Met592. Compared with compound 6, the 4-amino tetrahydrofuran moiety was grafted onto ring A in the most optimal way to fill the sugar pocket of ATP and adopt a substantially orthogonal orientation relative to the scaffold. In the phase II STARTRK-2 trial of compound 8 (NCT02568267), the ORR was 56.9% in patients with NTRK fusion solid tumors, and the intracranial ORR for patients with central nervous system metastases was 50%, with durable objective responses (DOR) of 10.4 months86. In view of its potency, high selectivity for TRKs, and favorable pharmacokinetic properties, compound 8 was accelerated for approval by the FDA on August 15, 2019 as a treatment for solid tumors carrying NTRK, ROS1 or ALK gene fusions86. The launch of larotrectinib and entrectinib is another great example of a basket trial, an innovative clinical trial involving a precision medicine design.
Figure 5.
(A) Entrectinib was generated by optimizing the substituent of benzene A in compound 6 and (B) X-ray cocrystal structure of compound 8 in TRKA (PDB ID: 5KVT, 2.5 Å). The kinase is illustrated with green ribbons, and the hydrogen bonds are depicted in black dashed lines. Compound atoms are in different colors: C, orange; N, blue; O, red; F, light cyan.
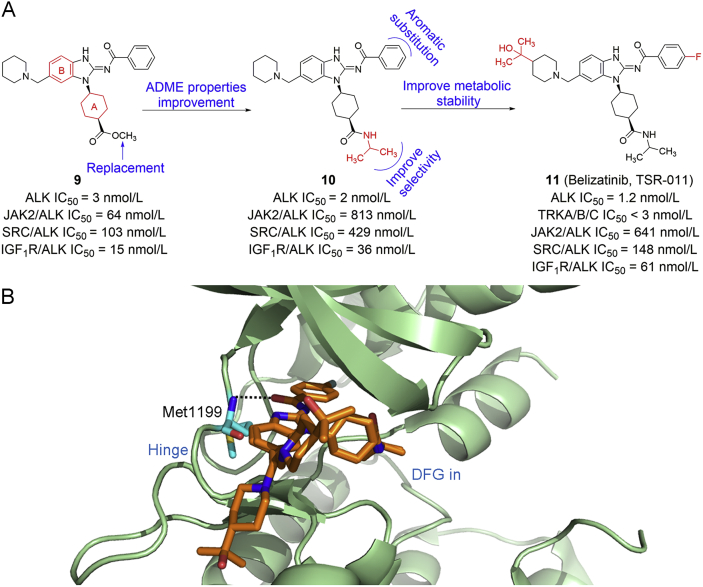
4.1.2. Other type I TRK inhibitors
In 2012, Lewis et al.87 employed high-throughput screening (HTS) to obtain a novel benzimidazole compound 9, which exhibited strong biological efficacy for ALK (IC50 = 3 nmol/L, Fig. 6A). To enhance cellular viability, selectivity for ALK, and metabolic stability, compound 10 was discovered by further optimization of loop A (Fig. 6A). Compared to compound 9, the selectivity of compound 10 for ALK was greatly improved. Fig. 6A illustrated that modification of ring B yielded a more metabolically stable compound 11 (belizatinib, TSR-011). As shown in Fig. 6B, the branch structure promoted the dual occupation of the ribocyst and the hydrophobic pocket II through the cyclohexyl and the benzamide motifs87. Subsequently, Weiss et al.88 found that compound 11 inhibited TRKA/B/C with an IC50 value below 3 nmol/L. A phase I/II clinical trial (NCT02048488) of belizatinib for the therapy of patients with advanced solid tumors and lymphomas was completed. Due to limited clinical activity, the further development of TSR-011 as an ALK inhibitor was ceased.
Figure 6.
(A) Optimization of ring A and B in compound 9 resulted in the generation of TSR-011 and (B) X-ray cocrystal structure of compound 11 in ALK (PDB ID: 4FOD; 2.0 Å). The kinase is illustrated with green ribbons, and the hydrogen bonds are depicted in black dashed lines. Compound atoms are in different colors: C, orange; N, blue; O, red; F, light cyan.
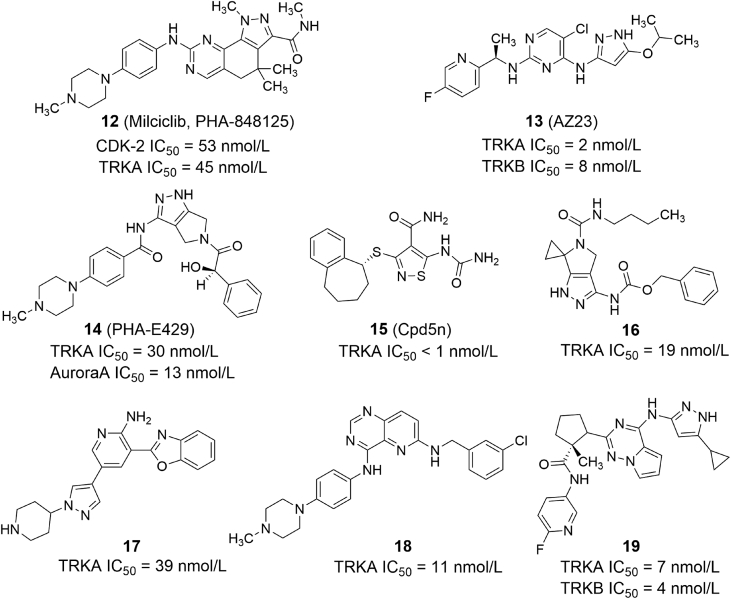
Albanese's group89, 90, 91 reported compound 12 (milciclib, PHA-848125) as a dual inhibitor of cyclin-dependent kinase (CDK-2)/TRKA (Fig. 7), which can effectively inhibit NGF-induced TRKA phosphorylation and downstream signaling in DU-145 human prostate cancer cells with IC50 values of 53 and 45 nmol/L, respectively. Phase II clinical trials (NCT01011439 and NCT01301391) of milciclib for therapy for malignant thymoma were terminated. Thress's research group92 discovered a series of 4-aminopyrimidine compounds as highly selective and potent TRKA/B inhibitors. Representative compound 13 (AZ-23, Fig. 7) effectively inhibited TRKA and TRKB with IC50 values of 2 and 8 nmol/L, respectively92. Through screening, Fancelli et al.93 identified a series of 5-phenyl acetyl 1,4,5,6-tetrahydropyrrolo [3,4-c]pyrazoles, which are dual inhibitors of the TRKA/cell cycle kinases (Aurora). The IC50 values of representative compound 14 against TRKA/Aurora were 30 and 13 nmol/L, respectively (Fig. 7). In Fig. 7, compound 15 is an isothiazole derivative screened by HTS, which has picomolar activity against kinases (TRKA IC50 < 1 nmol/L) and nanomolar activity against cell growth driven by TRKs (IC50 = 7 nmol/L)94. Compound 16 is a type I TRK inhibitor, and its IC50 value was 19 nmol/L. SAR studies have shown that benzyl cyclopropyl carbamate and benzyl carbamate are crucial for the potency of these compounds95. Han et al.96 reported benzoxazole-substituted aminopyridine nuclear compound 17 as a c-Met inhibitor. Kinase profile analysis showed that compound 17 inhibited TRKA with an IC50 of 39 nmol/L (Fig. 7). Stachel et al.97 devoted themselves to designing valid TRK inhibitors on the basis of a pyrido [3,2-d]pyrimidine core scaffold, of which compound 18 (Fig. 7) exhibited a favorable biochemical activity (TRKA IC50 = 11 nmol/L). Compound 19 (Fig. 7), developed by Carboni98, is a dual inhibitor of IGF1R/IR. It was subsequently identified as active against TRKA/B (IC50 = 7 and 4 nmol/L). All of these type I kinase inhibitors have nanomolar-level kinase inhibitory activity. Due to their low selectivity within the same family of kinases, their use for specific treatment is limited. However, their pan-inhibitory activity also promotes their treatment of broad-spectrum tumors and provides an impetus for their development.
Figure 7.
Chemical structures of reported other type I TRK inhibitors and their kinase activity.
4.1.3. Second-generation type I TRK inhibitors
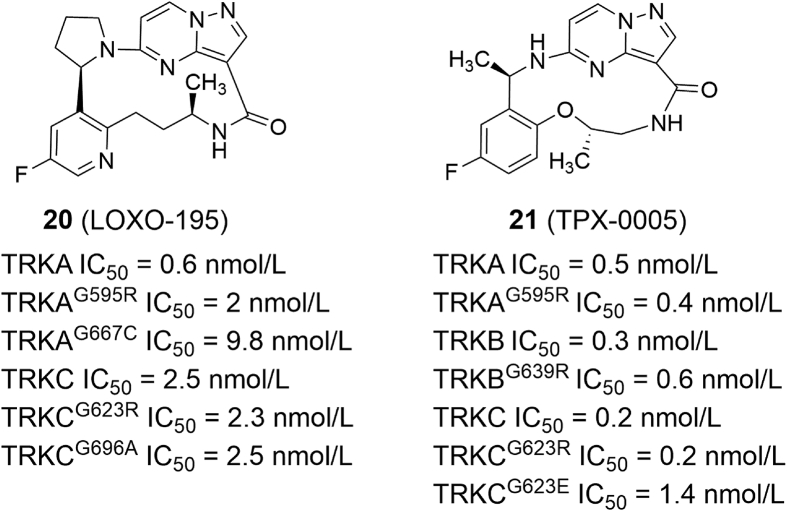
Similar to many other metastatic cancers, the cancers caused by NTRK fusions will relapse repeatedly, leading to acquired resistance, which necessitates the choice of new targeted therapies. For example, drug tolerance to larotrectinib is caused by three diverse mutations, including solvent frontal mutations (NTRK1 p. G595R, NTRK3 p. G623R), a gatekeeper mutation (NTRK1 p. F589L), and 3-xDFG (NTRK1 p. G667S, NTRK3 p. G696A) mutations17. The structural model predicted that each mutation directly interfered spatially with the binding of larotrectinib and other TRK inhibitors, thereby reducing their inhibitory abilities11,28. It is encouraging that the second-generation TRK inhibitors 20 and 21 (LOXO-195 and TPX-0005) are undergoing clinical studies to overcome these recurrent resistance mutations (Fig. 8). Both compounds were designed as fused macrocyclics to decrease the superficial area in contact with the active site, thereby reducing unnecessary interaction with the binding pocket28,29. Compound 20 achieved low nanomolar inhibitory activity against TRKAG595R, TRKAG667C, TRKCG696A and TRKCG623R (IC50 = 2, 9.8, 2.3 and 2.5 nmol/L, respectively)28. Compound 21 can effectively inhibit ROS1G2032R (IC50 = 8.4 nmol/L), TRKAG595R (IC50 = 0.4 nmol/L), TRKBG639R (IC50 = 0.6 nmol/L), TRKCG623R (IC50 = 0.2 nmol/L) and TRKCG623E (IC50 = 1.4 nmol/L)29 (Fig. 8). Undoubtedly, both drugs also had potent inhibitory activity against the wild type protein and had little selectivity between wild type and mutant TRKs.
Figure 8.
The reported chemical structures of two second-generation type I TRK inhibitors in clinical and their inhibitory activity against TRK mutations.
Blue medicines disclosed a series of pyrazolopyrimidine compounds in the patents WO201703554 and WO2017087778, wherein compounds 22 and 23 (Fig. 9) exhibited inhibitory activity on TRKA and TRKAG595R in the nanomolar range99,100. The pyrazolopyrimidine compound 24 (Fig. 9) reported by Chia Tai Tianqing Pharmaceutical101 was very similar to larotrectinib, and it demonstrated effective inhibitory activity against TRKA/B/C (TRKA/B/C IC50 < 1 nmol/L), as well as TRKAG667C mutant. Fochon Pharmaceuticals102 also covered a series of pyrazolopyrimidine compounds in patent WO2019174598. The representative compound 25 (Fig. 9) indicated nanomolar inhibition against TRKAG595R and TRKCG623R in cellular assay102. Hitgen103 disclosed imidazopyridazine compound 26 in patent WO2019120267. Compound 26 was similar to LOXO-195 and TPX-0005, all of which were macrocyclic compounds. Compound 26 showed good inhibitory activity in the assay of mutant cell activities of TRKAG595R, TRKAF589L and TRKCG623R (IC50 = 1, 2.3, and 2.4 nmol/L, Fig. 9) 103. In view of second-generation type I inhibitors reported in recent years, most of them have effective inhibitory effects on TRKA mutants. However, compared with first-generation type I inhibitors, their structures are relatively simple and lack of diversification. Therefore, the second-generation inhibitors still have a broad development prospect.
Figure 9.
Chemical structures of reported other second-generation type I TRK inhibitors and their kinase activity.
4.2. Type II TRK inhibitors
Type II inhibitors can bind to the DFG-out conformation of the kinase and thereby stabilize it. Similar to type I inhibitors, type II inhibitors not only bind to the ATP-binding site in the kinase but also extend the interaction to an allosteric site. The DFG motif can be rotated to an “outward” state to access its allosteric site, thereby opening the adjacent hydrophobic pockets. These inhibitors with heterocyclic or aromatic heterocyclic structures can form one or two hydrogen bonds with the hinge region, and its extended structures can occupy exposed allosteric sites. Type II TRK inhibitors have a higher safety and selectivity for the TRKs than the type I inhibitors, due to the non-conservative allosteric sites.
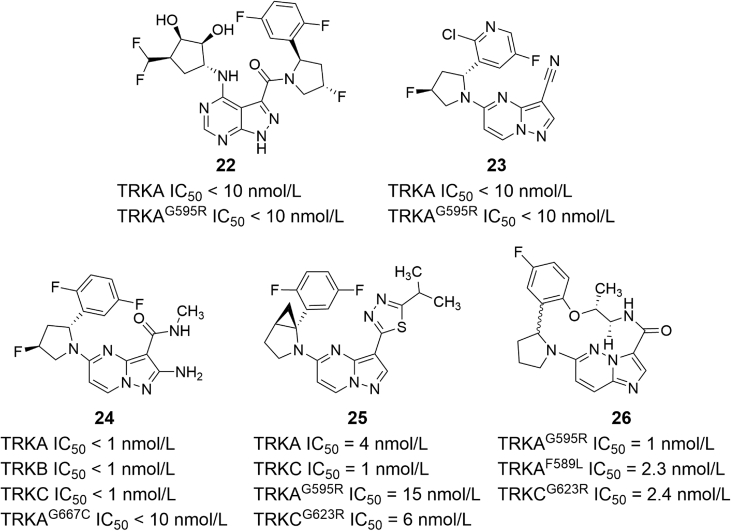
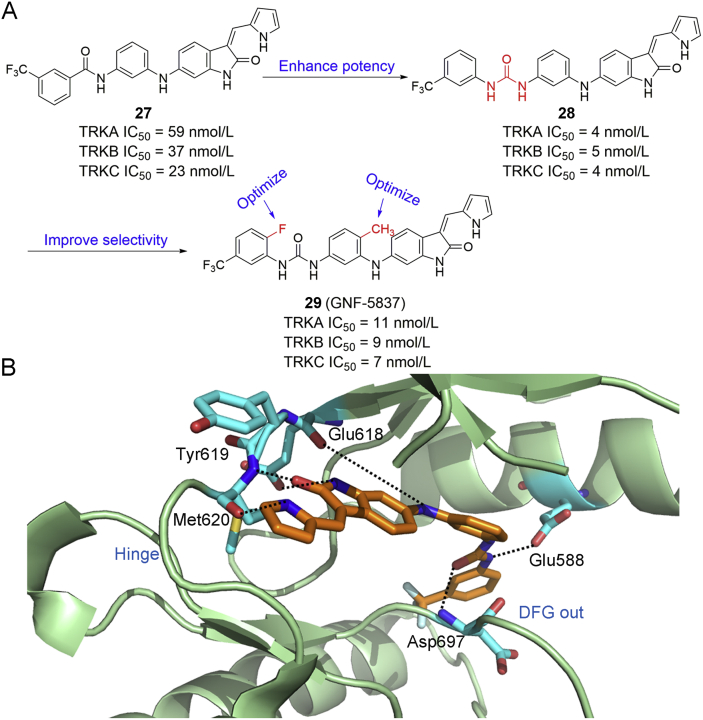
4.2.1. Type II TRK inhibitors in clinical trials
Albaugh et al.104 screened a promising oxindole compound 27 (Fig. 10A), which showed excellent inhibitory activity against B3/F3-Tel-TRKA/B/C with an IC50 value below 60 nmol/L. Compound 28, obtained by replacing the amide with urea, had a higher cell potency and selectivity for the TRKs (Fig. 10A)104. The methyl group and fluorine were introduced into the middle benzene ring and the terminal benzene of compound 28 to form compound 29 (GNF-5837). Fig. 10A illustrates that compound 29 had pan-TRK inhibitory activity (IC50 values towards TRKA/B/C were 11, 9, and 7 nmol/L, respectively), and showed good selectivity in the human kinome104. The cocrystal complex of 28 in TRKC was obtained and is shown in Fig. 10B. Compound 28 was immobilized to the hinge region via two key hydrogen bonds between the pyrrole nitrogen and the backbone of residues Tyr619 and Met620. The urea functional group engaged in a strong hydrophobic interaction through Asp697 of the DFG motif104.
Figure 10.
(A) Discovery and optimization procedure of compound 27 to 29 and (B) cocrystal structure of compound 28 in TRKC (PDB ID: 3V5Q; 2.2 Å). The kinase is illustrated with green ribbons, and the hydrogen bonds are depicted in black dashed lines. Compound atoms are in different colors: C, orange; N, blue; O, red; F, light cyan.
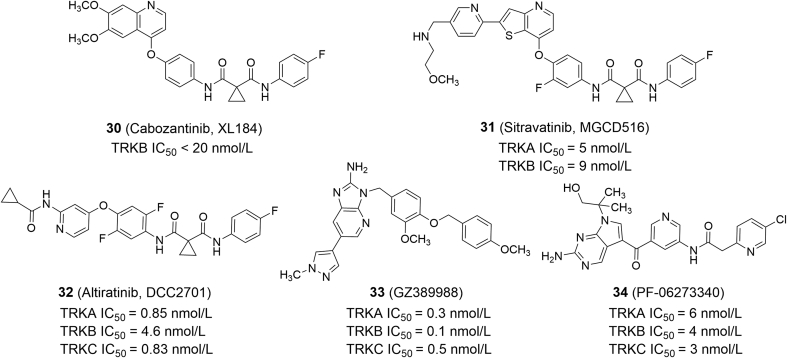
Compound 30 (cabozantinib, XL184), with preferential activity for c-Met/vascular endothelial growth factor receptor 2 (VEGFR2), was subsequently identified as an effective TRKB inhibitor (IC50 value was below 20 nmol/L)105. Currently, compound 30 is undergoing multiple phase II trials (NCT01639508), including for NSCLC with the RET fusion and for cancers with other gene fusions (including ROS1, NTRK, MET, or AXL, Fig. 11). Patwardhan et al.24 discovered a dicarboxamide derivative compound 31 (sitravatinib, MGCD516), which was initially identified as a multiple kinase inhibitor for UFO, VEGFR2, FLT3, and c-KIT. Subsequently, it was demonstrated that the IC50 values for TRKA/B were 5 and 9 nmol/L (Fig. 11). Furthermore, compound 31 is currently in a phase I clinical study for treating advanced solid tumor malignancies (NCT02219711). Compound 32 (altiratinib, DCC2701), identified by Smith and coworkers27 in 2015, showed a high potency against TRKA/B/C, with IC50 values of 0.85, 4.6, and 0.83 nmol/L, respectively (Fig. 11). Notably, compound 32 can cross the blood−brain barrier, which enables the capacity for treating brain cancer and brain metastatic cancer. A phase I study of compound 32 for the therapy of locally advanced tumors and metastatic solid tumors was terminated (Fig. 11), but the results have not been announced. Compound 33 (GZ-389988), a novel, potent, selective, and locally delivered TRKA inhibitor, effectively suppressed TRKA/B/C with IC50 values of 0.3, 0.1, and 0.5 nmol/L, respectively106 (Fig. 11). Additionally, a phase II study of GZ-389988 for treating osteoarthritis (NCT02845271) was completed. The results showed that GZ-389988 can reduce pain significantly and has an acceptable safety profile. Skerratt et al.107 reported the pan-TRK inhibitor 34 (PF-06273340) through HTS of TRKA/B cells and SAR (IC50 values towards TRKA/B/C were 6, 4, and 3 nmol/L, respectively). A phase I clinical trial was completed for assessment of the analgesic effects of PF-06273340 in healthy volunteers using evoked pain endpoints. The result demonstrated for the first time that the use of pan-TRK inhibitors translated non-clinical effects into humans in the pharmacodynamic endpoint of inflammatory analgesia.
Figure 11.
Type II TRK inhibitors in clinical trials and their kinase activity.
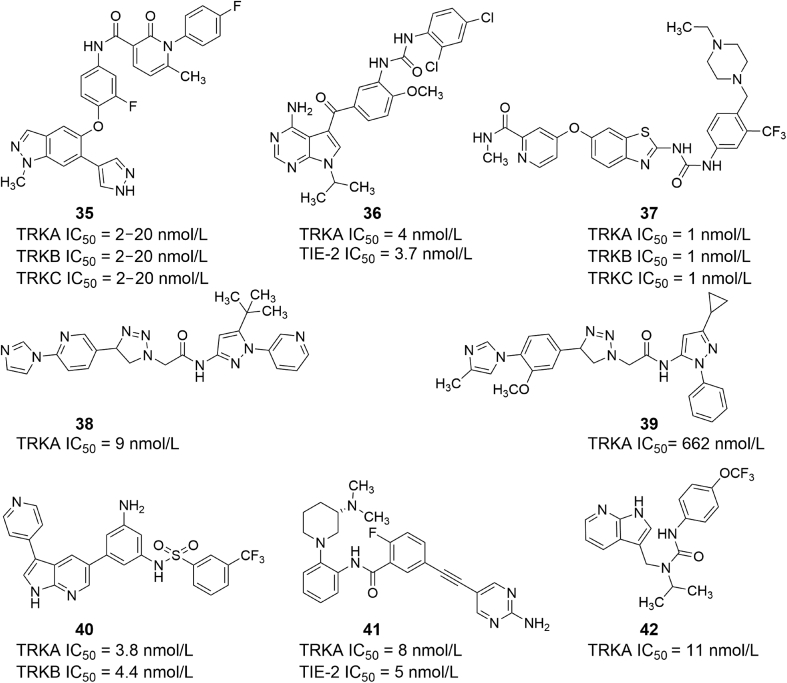
4.2.2. Other type II TRK inhibitors
Compound 35, according to the 4-aminopyrrolopyrimidine core scaffold, was initially reported as an effective oral bioavailable c-Met inhibitor by Vaishnavi et al.48 (Fig. 12). Enzyme- and cell-based assays indicated that compound 35 displayed potent inhibition of TRKA/B/C, ROS1 and AXL. Compound 36 (CE-245677) was a dual inhibitor of TIE-2 and TRKA, with IC50 values of 3.7 and 4 nmol/L, respectively (Fig. 12). Nevertheless, further research on compound 36 was unfortunately prohibited in a phase I clinical trial because of the severe central nervous system adverse events107,108. EI Zein's group109 developed a benzothiazole derivative 37 as a multiple kinase inhibitor, which displayed a good inhibitory activity against VEGFR2, ABL, and TRKA/B. The IC50 values of TRKA/B/C were 1 nmol/L (Fig. 12). Compound 38 with a novel core scaffold, shown in Fig. 12, was obtained by HTS from a compound database97. Of particular note, compound 38 (Fig. 12) showed a low nanomolar IC50 value against TRKA in both enzyme activity and cell viability assays (the TRKA enzymatic IC50 value was 9 nmol/L and the cellular IC50 value was 7 nmol/L). Compound 38 bound to multiple sites across TRKA in a unique pattern, in which the imidazole formed a key hydrogen bond with the hinge, and the pyrazole ring occupied the hydrophobic pocket. The same binding mode was observed in compound 39 reported by Wang110. It exhibited excellent efficacy in enzyme- and cellular-based assays, with a TRKA enzymatic IC50 value of 662 nmol/L and a cellular-based IC50 value of 47 nmol/L (Fig. 12)110. Hong and colleagues111 screened the promising 3,5-disubstituted-7-azaindole compound 40, which demonstrated favorable biochemical viability against TRKA/B (IC50 values of TRKA/B were 3.8 and 4.4 nmol/L, respectively, Fig. 12). Aminopyrimidine derivative 41 was obtained through medicinal chemistry efforts (Fig. 12). It is a dual inhibitor for TIE-2 and TRKA (the IC50 values of TIE-2 and TRKA were 5 and 8 nmol/L, respectively)112. Through HTS, Stachel et al.112 identified the TRKA inhibitor 42 (TRKA kinase IC50 = 11 nmol/L, cellular IC50 = 3 nmol/L, Fig. 12). Unlike typical type II inhibitors, the azaindole ring of compound 42 formed weaker hydrogen bonds with the hinge region. In addition, the most important interactions occurred in adjacent allosteric pockets.
Figure 12.
Other type II TRK inhibitors in preclinical trials and their kinase activity.
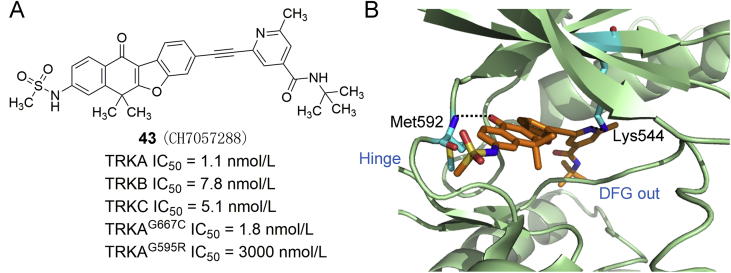
4.2.3. Second-generation type II TRK inhibitors
In the patent WO2017073706, the Chugai Pharmaceutical Co.113 disclosed a novel pan-TRK inhibitor 43 (CH7057288, Fig. 13A) derived from dihydronaphthobenzofuran. The cocrystal structure of TRKA in complex with compound 43 revealed that compound 43 bonded to the DFG-out of TRKA, where picoline entered the allosteric pocket and interacted with Lys544 (Fig. 13B)113. Compound 43 possessed an excellent inhibitory effect on TRKAG667C mutation resistant to entrectinib, while also remaining a favorable inhibitory activity against TRKA/B/C114. Furthermore, compound 43 showed strong in vivo growth inhibition in a mouse xenograft tumor model114. Taken together, compound 43 has potential for further development.
Figure 13.
(A) Chemical structure of compound 43 and (B) cocrystal structure of compound 43 in TRKA (PDB ID:5WR7; 2.8 Å). The kinase is illustrated with green ribbons, and the hydrogen bonds are depicted in black dashed lines. Compound atoms are in different colors: C, orange; N, blue; O, red.
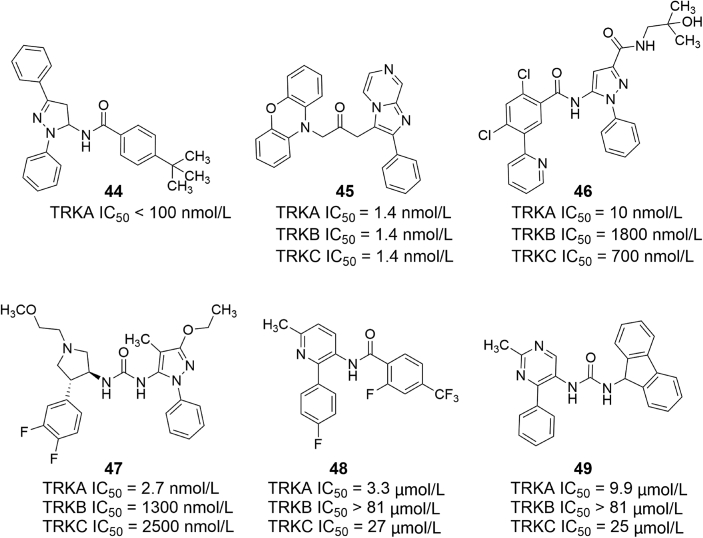
4.3. Type Ⅲ TRK inhibitors
The type III inhibitors bind to the allosteric site of the kinase and regulate the binding between the ATP and kinase, maintaining its inactive state by inducing the conformational change. This type of molecule binds to a specific site on the kinase, i.e., the near-membrane region. The near-membrane region of TRKA is shorter than in TRKB/C, and there are many different amino acid residues in the region where the ligand interacts with the protein. Therefore, this area provides new ideas for the development of selective TRKA inhibitors.
4.3.1. Type Ⅲ TRK inhibitors in clinical trials
Allosteric inhibitors may alleviate the challenge of acquired resistance on accounted that their unique binding pattern can circumvent obstructive kinase domain mutations. To date, some allosteric TRKA specific inhibitors have entered clinical trials, but their structures have not yet been disclosed. VM-902A participated in the short phase IIa clinical trial (NCT02847702) as an oral analgesic for treatment of patients with osteoarthritis of the knee (OAK), but the trial was terminated three months later115. VMD-928 was a dual allosteric and irreversible TRKA selective inhibitor. It is currently in a phase I clinical trial (NCT03556228) for the treatment of solid tumors or lymphomas and patients driven by NTRK1 and its drug-resistant mutants116. The allosteric TRKA inhibitor AK1830 (ARRY-954) developed by Array BioPharma is currently in phase I clinical trials for the inflammation therapy115.
4.3.2. Other type Ⅲ TRK inhibitors
Subramanian et al.117 screened a promising benzamide derivative 44 from the ZINC database by HTRF analysis and then further improved its poor physical properties (such as solubility, Fig. 14). Compound 45 (TRKA/B/C IC50 = 1.4 nmol/L) was obtained through scaffold hopping and further SAR analysis (Fig. 14)118. Compound 45 bound in the conformation of DFG-out at the allosteric site and away from the ATP-binding site. The cocrystal structure of compound 45 and TRKA showed that the amide NH of compound 45 generated a key hydrogen bond interaction with D668 of the activation ring. In addition, the carbonyl group also had direct hydrogen bonding with I490 near the membrane region. Currently, Skerratt et al.107 have discovered an N-phenyl-pyrazole derivative 46, a highly selective TRKA inhibitor (Fig. 14). Compound 46 exhibited excellent TRKA inhibitory activity (the TRKA IC50 value was 10 nmol/L), and TRKA had a nearly 100-folds selectivity over TRKB and TRKC (the IC50 values of TRKB and TRKC were 1800 and 700 nmol/L, respectively)107. Allen119 disclosed a novel TRKA inhibitor 47 in US2012158413A2. Compound 47 (Fig. 14) had a certain selectivity for different TRK isoforms and showed a favorable TRKA inhibitory activity (the IC50 values of TRKA/B/C were 2.7, 1300, and 2500 nmol/L, respectively)119. Su et al.120 employed an affinity ligand recognition mass spectrometry (ALIS) strategy to screen the promising benzamide derivative 48 (Fig. 14), which has a certain selectivity for TRKA (TRKA IC50 = 3.3 μmol/L, TRKB IC50 > 81.0 μmol/L, TRKC IC50 > 27.0 μmol/L). Compound 49, another highly selective TRKA inhibitor (Fig. 14), was screened by Su et al.120 via the same strategy. Compared with TRKB and TRKC, its selectivity for TRKA was more than 2500-folds (TRKA IC50 = 9.9 μmol/L; 8182-folds and 2525-folds selectivity over TRKB/C, respectively).
Figure 14.
Chemical structures of other type III TRK inhibitors and their kinase activity.
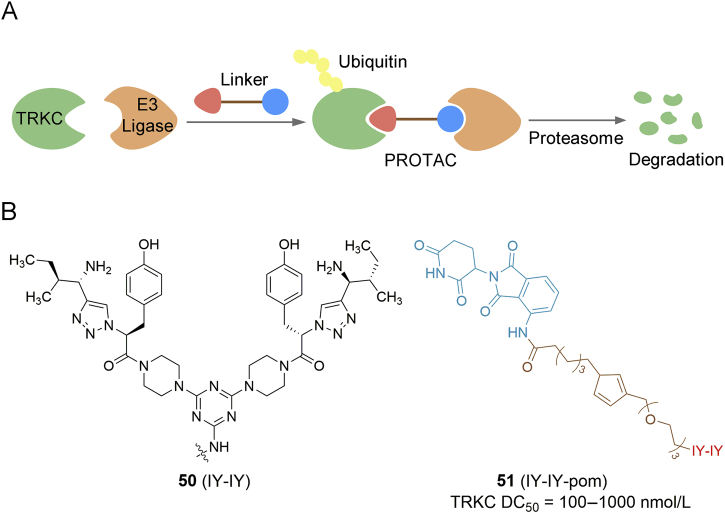
4.4. Proteolysis targeting chimeras (PROTACs) of TRKs
At present, PROTAC technology has been extensively used in drug development121, 122, 123, but TRK PROTACs have been rarely reported. The strategy of TRKC degradation is shown in Fig. 15A. In 2019, Zhao et al.124 developed a TRK PROTAC (compound 51, IY-IY-pom) by conjugating the small-molecule fragment 50 (IY-IY) to TRKC with the CRBN ligand pomalidomide (Fig. 15B). Compound 51 can induce effective TRKC degradation at 1–10 μmol/L, with a DC50 value (50% concentration of protein degradation) of approximately 100–1000 nmol/L124. Although compounds that induce the degradation of TRKs need further exploration, TRK PROTACs have apparently provided a new strategy for targeted TRK therapies.
Figure 15.
(A) The strategy of TRKC degradation and (B) chemical structures of the reported TRK PROTAC.
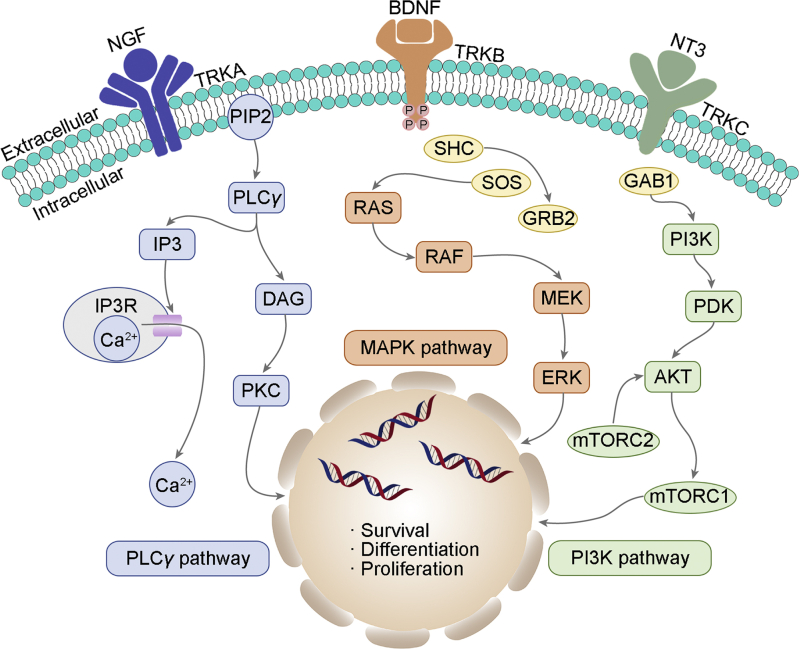
5. Concluding remarks and future perspectives
Of note, NTRK fusions may act as drivers in a variety of adult and pediatric cancers, which are inhibited by small-molecule inhibitors of TRKs (Fig. 16). Several small-molecule compounds targeting TRKs are currently used in preclinical and clinical trials (Fig. 16). Most of the kinase inhibitors developed for TRKs display their remarkable therapeutic potential in clinical trials but exhibit an inferior selectivity toward any of the three subtypes (TRKA, TRKB, and TRKC). In contrast, inhibitors with a high selectivity for a single TRK isoform can be further investigated on TRK biological functions. Moreover, it would be beneficial to utilize highly selective inhibitors with a single TRK isoform to determine the importance of subtypes and to elucidate interactions in preclinical TRK models. At present, the first-generation TRK inhibitors, larotrectinib and entrectinib, have demonstrated their remarkable antitumor activities in patients of different ages and with different cancer tissues but having NTRK fusion mutations.
Figure 16.
Representative small-molecule inhibitors targeting TRKs for the treatment of NTRK fusion cancers.
However, similar to other targeted treatments, the occurrence of acquired (secondary) resistance limits the potency of TRK inhibitors. Although targeted resistance mediated by mutations in the TRK domains can be eliminated using the second-generation TRK inhibitors, the treatment of acquired resistance with TRK inhibitors remains an ongoing challenge. Inspired by the resistance of other kinases, dual-blocking TRKs and other kinases have been demonstrated to be a new alternative for a drug-resistant treatment approach. In addition, the combination of TRK inhibitors with chemotherapy or immunotherapy is yet another promising therapeutic method to combat drug resistance, but it is worth noting that additional toxicity should be avoided. In particular, the PROTAC technology has also been applied to develop TRK drugs. Compounds promoting degradation with a similar mechanism to PROTAC are also an active and quickly advancing research direction, which opens a new window for targeted TRK therapy.
At present, more accurate and efficient detection technologies, such as fluorescence in situ hybridization (FISH), next-generation sequencing of tumor tissue (NGS), and sequencing of circulating tumor cells (CTCs), may provide more accurate methods for detecting NTRK fusions and serve as complementary strategies to optimize the current treatments. With the development of computational biology technology, computer-aided drug design has been able to participate in the identification of protein residues in drug development and to gradually clarify the binding characteristics of existing drugs125. Additionally, it is beneficial to develop novel TRK drugs and explore drug-resistance mechanisms based upon the sequence, structure and kinetic methods. In addition, a comprehensive understanding of the functions of TRKs in cancer therapies and more accurate detection means for NTRK fusions are critical for improving clinical treatments. We believe that more TRK inhibitors would enter clinical trials and become therapeutic applications, and the issue of drug resistance would be addressed soon with a further understanding of TRK intracellular signaling pathways and drug-resistance mechanisms.
Acknowledgments
This work was supported by grants from National Natural Science Foundation of China (Grants 81922064, 81874290, 81803755, and 91853109), and Sichuan Science and Technology Program (Grants 2019YFSY0038 and 2019JDRC0091, China).
Author contributions
Liang Ouyang and Yi Chen conceived the project and supervised the project. Tingting Jiang and Guan Wang summed up the literature and drafted the manuscript. Yao Liu was involved in drawing the figures. Lu Feng and Meng Wang collected and organized the inhibitors. Guan Wang and Jie Liu proofread the structures and figures. Liang Ouyang and Yi Chen revised the manuscript. All authors approved the final manuscript.
Conflicts of interest
The authors have no conflicts of interest to declare.
Footnotes
Peer review under responsibility of Institute of Materia Medica, Chinese Academy of Medical Sciences and Chinese Pharmaceutical Association.
Contributor Information
Yi Chen, Email: toddychan@163.com.
Liang Ouyang, Email: ouyangliang@scu.edu.cn.
References
- 1.Huang E.J., Reichardt L.F. Neurotrophins: roles in neuronal development and function. Annu Rev Neurosci. 2001;24:677–736. doi: 10.1146/annurev.neuro.24.1.677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kozaki R., Yoshizawa T., Tsukamoto K., Kato H., Kawabata K. Abstract 2954A: a potent and selective TRK inhibitor ONO-5390556, shows potent antitumor activity against both TRK-rearranged cancers and the resistant mutants. Canc Res. 2016;76 2954A–54A. [Google Scholar]
- 3.Huse M., Kuriyan J. The conformational plasticity of protein kinases. Cell. 2002;109:275–282. doi: 10.1016/s0092-8674(02)00741-9. [DOI] [PubMed] [Google Scholar]
- 4.Bannen L., Chan D., Forsyth T., Khoury R., Leahy J., Mac M., inventors. Exelixis Inc., assignee . 2011 Nov 29. c-Met modulators and methods of use. [Google Scholar]
- 5.Kaplan D.R., Martin-Zanca D., Parada L.F. Tyrosine phosphorylation and tyrosine kinase activity of the TRK proto-oncogene product induced by NGF. Nature. 1991;350:158–160. doi: 10.1038/350158a0. [DOI] [PubMed] [Google Scholar]
- 6.Klein R., Nanduri V., Jing S.A., Lamballe F., Tapley P., Bryant S. The TRKB tyrosine protein kinase is a receptor for brain-derived neurotrophic factor and neurotrophin-3. Cell. 1991;66:395–403. doi: 10.1016/0092-8674(91)90628-c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Frade J.M., Barde Y.A. Nerve growth factor: two receptors, multiple functions. Bioessays. 1998;20:137–145. doi: 10.1002/(SICI)1521-1878(199802)20:2<137::AID-BIES6>3.0.CO;2-Q. [DOI] [PubMed] [Google Scholar]
- 8.Patel T.D., Jackman A., Rice F.L., Kucera J., Snider W.D. Development of sensory neurons in the absence of NGF/TRKA signaling in vivo. Neuron. 2000;25:345–357. doi: 10.1016/s0896-6273(00)80899-5. [DOI] [PubMed] [Google Scholar]
- 9.Teng H.K., Teng K.K., Lee R., Wright S., Tevar S., Almeida R.D. ProBDNF induces neuronal apoptosis via activation of a receptor complex of p75NTR and sortilin. J Neurosci. 2005;25:5455–5463. doi: 10.1523/JNEUROSCI.5123-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Vaishnavi A., Le A.T., Doebele R.C. TRKing down an old oncogene in a new era of targeted therapy. Canc Discov. 2015;5:25–34. doi: 10.1158/2159-8290.CD-14-0765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Créancier L., Vandenberghe I., Gomes B., Dejean C., Blanchet J.C., Meilleroux J. Chromosomal rearrangements involving the NTRK1 gene in colorectal carcinoma. Canc Lett. 2015;365:107–111. doi: 10.1016/j.canlet.2015.05.013. [DOI] [PubMed] [Google Scholar]
- 12.Drilon A., Li G., Dogan S., Gounder M., Shen R., Arcila M. What hides behind the MASC: clinical response and acquired resistance to entrectinib after ETV6-NTRK3 identification in a mammary analogue secretory carcinoma (MASC) Ann Oncol. 2016;27:920–926. doi: 10.1093/annonc/mdw042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Skálová A., Vanecek T., Simpson R.H.W., Laco J., Majewska H., Baneckova M. Mammary analogue secretory carcinoma of salivary glands: molecular analysis of 25 ETV6 gene rearranged tumors with lack of detection of classical ETV6-NTRK3 fusion transcript by standard RT-PCR: report of 4 cases harboring ETV6-X gene fusion. Am J Surg Pathol. 2016;40:3–13. doi: 10.1097/PAS.0000000000000537. [DOI] [PubMed] [Google Scholar]
- 14.Cocco E., Scaltriti M., Drilon A. NTRK fusion-positive cancers and TRK inhibitor therapy. Nat Rev Clin Oncol. 2018;15:731–747. doi: 10.1038/s41571-018-0113-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chen S.N., Schneider B., Nagel S., Geffers R., Kaufmann M., Quentmeier H. Spliceosomal targeting in acute myeloid leukemia cells with ETV6-NTRK3 fusion. Blood. 2009;22:5042. [Google Scholar]
- 16.Strohmaier C., Carter B.D., Urfer R., Barde Y.A., Dechant G. A splice variant of the neurotrophin receptor TRKB with increased specificity for brain-derived neurotrophic factor. EMBO J. 1996;15:3332–3337. [PMC free article] [PubMed] [Google Scholar]
- 17.Eggert A., Grotzer M.A., Ikegaki N., Liu X.G., Evans A.E., Brodeur G.M. Expression of the neurotrophin receptor TRKA down-regulates expression and function of angiogenic stimulators in SH-SY5Y neuroblastoma cells. Canc Res. 2002;62:1802–1808. [PubMed] [Google Scholar]
- 18.Lagadec C., Meignan S., Adriaenssens E., Foveau B., Vanhecke E., Romon R. TRKA overexpression enhances growth and metastasis of breast cancer cells. Oncogene. 2009;28:1960–1970. doi: 10.1038/onc.2009.61. [DOI] [PubMed] [Google Scholar]
- 19.Lange A.M., Lo H.W. Inhibiting TRK proteins in clinical cancer therapy. Cancers. 2018;10:e105. doi: 10.3390/cancers10040105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Scott L.J. Larotrectinib: first global approval. Drugs. 2019;79:201–206. doi: 10.1007/s40265-018-1044-x. [DOI] [PubMed] [Google Scholar]
- 21.Al Salama Z.T., Keam S.J. Entrectinib: first global approval. Drugs. 2019;79:1477–1483. doi: 10.1007/s40265-019-01177-y. [DOI] [PubMed] [Google Scholar]
- 22.Rajan N., Elliott R., Clewes O., Mackay A., Reis-Filho J.S., Burn J. Dysregulated TRK signalling is a therapeutic target in CYLD defective tumours. Oncogene. 2011;30:4243–4260. doi: 10.1038/onc.2011.133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Phase 1 study of PLX7486 as single agent in patients with advanced solid tumors. ClinicalTrails.gov, 2018. Available from: https://clinicaltrials.gov/ct2/show/NCT01804530.
- 24.Patwardhan P.P., Ivy K.S., Musi E., de Stanchina E., Schwartz G.K. Significant blockade of multiple receptor tyrosine kinases by MGCD516 (sitravatinib), a novel small molecule inhibitor, shows potent anti-tumor activity in preclinical models of sarcoma. Oncotarget. 2016;7:4093–4109. doi: 10.18632/oncotarget.6547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.A first-in-human study to evaluate the safety, tolerability and pharmacokinetics of DS-6051b. ClinicalTrials.gov, 2019. Available from: https://clinicaltrials.gov/ct2/show/NCT02279433.
- 26.A phase I/IIa open-label, dose escalation and cohort expansion trial of oral TSR-011 in patients with advanced solid tumors and lymphomas. ClinicalTrials.gov, 2019. Available from: https://www.clinicaltrials.gov/ct2/show/NCT02048488. [DOI] [PMC free article] [PubMed]
- 27.Smith B.D., Kaufman M.D., Leary C.B., Turner B.A., Wise S.C., Ahn Y.M. Altiratinib inhibits tumor arowth, invasion, angiogenesis, and microenviroment-mediated drug resistance via balanced inhibition of MET, TIE2, and VEGFR2. Mol Canc Therapeut. 2015;14:2023–2034. doi: 10.1158/1535-7163.MCT-14-1105. [DOI] [PubMed] [Google Scholar]
- 28.Russo M., Misale S., Wei G., Siravegna G., Crisafulli G., Lazzari L. Acquired resistance to the TRK inhibitor Entrectinib in colorectal cancer. Canc Discov. 2016;6:36–44. doi: 10.1158/2159-8290.CD-15-0940. [DOI] [PubMed] [Google Scholar]
- 29.Drilon A., Nagasubramanian R., Blake J.F., Ku N., Tuch B.B., Ebata K. A next-generation TRK kinase inhibitor overcomes acquired resistance to prior TRK kinase inhibition in patients with TRK fusion-positive solid tumors. Canc Discov. 2017;7:963–972. doi: 10.1158/2159-8290.CD-17-0507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cui J.J., Zhai D., Deng W., Rogers E., Huang Z., Whitten J. TPX-0005, a novel ALK/ROS1/TRK inhibitor, effectively inhibited a broad spectrum of mutations including solvent front ALK G1202R, ROS1 G2032R and TRKA G595R mutants. Eur J Canc. 2016;69:S32. [Google Scholar]
- 31.Nishiyama A., Yamada T., Kita K., Wang R., Arai S., Fukuda K. Foretinib overcomes entrectinib resistance associated with the NTRK1G667C mutation in NTRK1 fusion-positive tumor cells in a brain metastasis model. Clin Canc Res. 2018;10:2357–2369. doi: 10.1158/1078-0432.CCR-17-1623. [DOI] [PubMed] [Google Scholar]
- 32.Xiang H.G., Zhang J.F., Lin C.C., Zhang L., Liu B., Ouyang L. Targeting autophagy-related protein kinases for potential therapeutic purpose. Acta Pharm Sin B. 2020;10:569–581. doi: 10.1016/j.apsb.2019.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Klein R., Jing S., Nanduri V., O'Rourke E., Barbacid M. The TRK protooncogene encodes a receptor for nerve growth factor. Cell. 1991;65:189–197. doi: 10.1016/0092-8674(91)90419-y. [DOI] [PubMed] [Google Scholar]
- 34.Lamballe F., Klein R., Barbacid M. TRKC, a new member of the TRK family of tyrosine protein kinases, is a receptor for neurotrophin-3. Cell. 1991;66:967–979. doi: 10.1016/0092-8674(91)90442-2. [DOI] [PubMed] [Google Scholar]
- 35.He P.X., Niu S.G., Wang S., Shi X.J., Feng S.Q., Du L.N. Discovery of WS-157 as a highly potent, selective and orally active EGFR inhibitor. Acta Pharm Sin B. 2019;9:1193–1203. doi: 10.1016/j.apsb.2019.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deinhardt K., Chao M. TRK receptors. Handb Exp Pharmacol. 2014;220:103–119. doi: 10.1007/978-3-642-45106-5_5. [DOI] [PubMed] [Google Scholar]
- 37.Nakagawara A. TRK receptor tyrosine kinases: a bridge between cancer and neural development. Canc Lett. 2001;169:107–114. doi: 10.1016/s0304-3835(01)00530-4. [DOI] [PubMed] [Google Scholar]
- 38.Julius D., Basbaum A.I. Molecular mechanisms of nociception. Nature. 2001;413:203–210. doi: 10.1038/35093019. [DOI] [PubMed] [Google Scholar]
- 39.Li M., Dai F.R., Du X.P., Yang Q.D., Zhang X., Chen Y. Infusion of BDNF into the nucleus accumbens of aged rats improves cognition and structural synaptic plasticity through PI3K-ILK-Akt signaling. Behav Brain Res. 2012;231:146–153. doi: 10.1016/j.bbr.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 40.Miranda C., Mazzoni M., Sensi M., Pierotti M.A., Greco A. Functional characterization of NTRK1 mutations identified in melanoma. Genes Chromosomes Cancer. 2014;53:875–880. doi: 10.1002/gcc.22200. [DOI] [PubMed] [Google Scholar]
- 41.Geiger T.R., Song J.Y., Rosado A., Peeper D.S. Functional characterization of human cancer-derived TRKB mutations. PLoS One. 2011;6 doi: 10.1371/journal.pone.0016871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Harada T., Yatabe Y., Takeshita M., Koga T., Yano T., Wang Y. Role and relevance of TRKB mutations and expression in non-small cell lung cancer. Clin Canc Res. 2011;17:2638–2645. doi: 10.1158/1078-0432.CCR-10-3034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Marchetti A., Felicioni L., Pelosi G., Del Grammastro M., Fumagalli C., Sciarrotta M. Frequent mutations in the neurotrophic tyrosine receptor kinase gene family in large cell neuroendocrine carcinoma of the lung. Hum Mutat. 2008;29:609–616. doi: 10.1002/humu.20707. [DOI] [PubMed] [Google Scholar]
- 44.Tomasson M.H., Xiang Z., Walgren R., Zhao Y., Kasai Y., Miner T. Somatic mutations and germline sequence variants in the expressed tyrosine kinase genes of patients with de novo acute myeloid leukemia. Blood. 2008;111:4797–4808. doi: 10.1182/blood-2007-09-113027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Reuther G.W., Lambert Q.T., Caligiuri M.A., Der C.J. Identification and characterization of an activating TRKA deletion mutation in acute myeloid leukemia. Mol Cell Biol. 2000;20:8655–8666. doi: 10.1128/mcb.20.23.8655-8666.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Tacconelli A., Farina A.R., Cappabianca L., Gulino A., Mackay A.R. Alternative TRKAIII splicing: a potential regulated tumor-promoting switch and therapeutic target in neuroblastoma. Future Oncol. 2005;1:689–698. doi: 10.2217/14796694.1.5.689. [DOI] [PubMed] [Google Scholar]
- 47.Tacconelli A., Farina A.R., Cappabianca L., Desantis G., Tessitore A., Vetuschi A. TRKA alternative splicing: a regulated tumor-promoting switch in human neuroblastoma. Canc Cell. 2004;6:347–360. doi: 10.1016/j.ccr.2004.09.011. [DOI] [PubMed] [Google Scholar]
- 48.Vaishnavi A., Capelletti M., Le A.T., Kako S., Butaney M., Ercan D. Oncogenic and drug-sensitive NTRK1 rearrangements in lung cancer. Nat Med. 2013;19:1469–1472. doi: 10.1038/nm.3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ranzi V., Meakin S., Miranda C., Mondellini P., Pierotti M., Greco A. The signaling adapters sibroblast growth factor receptor substrate 2 and 3 are activated by the thyroid TRK oncoproteins. Endocrinology. 2003;144:922–928. doi: 10.1210/en.2002-221002. [DOI] [PubMed] [Google Scholar]
- 50.Miranda C., Greco A., Miele C., Pierotti M.A., Van Obberghen E. IRS-1 and IRS-2 are recruited by TRKA receptor and oncogenic TRK-T1. J Cell Physiol. 2001;186:35–46. doi: 10.1002/1097-4652(200101)186:1<35::AID-JCP1003>3.0.CO;2-X. [DOI] [PubMed] [Google Scholar]
- 51.Roccato E., Miranda C., Ranzi V., Gishizki M., Pierotti M., Greco A. Biological activity of the thyroid TRK-T3 oncogene requires signalling through Shc. Br J Canc. 2002;87:645–653. doi: 10.1038/sj.bjc.6600544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Drilon A., Laetsch T.W., Kummar S., DuBois S.G., Lassen U.N., Demetri G.D. Efficacy of larotrectinib in TRK fusion-positive cancers in adults and children. N Engl J Med. 2018;378:731–739. doi: 10.1056/NEJMoa1714448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Amatu A., Sartore-Bianchi A., Siena S. Gene fusions as novel targets of cancer therapy across multiple tumour types. ESMO Open. 2016;1 doi: 10.1136/esmoopen-2015-000023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Halalsheh H., McCarville M.B., Neel M., Reynolds M., Cox M.C., Pappo A.S. Dramatic bone remodeling following larotrectinib administration for bone metastasis in a patient with TRK fusion congenital mesoblastic nephroma. Pediatr Blood Canc. 2018;65 doi: 10.1002/pbc.27271. [DOI] [PubMed] [Google Scholar]
- 55.Davis J.L., Lockwood C.M., Albert C.M., Tsuchiya K., Hawkins D.S., Rudzinski E.R. Infantile NTRK-associated mesenchymal tumors. Pediatr Dev Pathol. 2018;21:68–78. doi: 10.1177/1093526617712639. [DOI] [PubMed] [Google Scholar]
- 56.Laetsch T.W., DuBois S.G., Mascarenhas L., Turpin B., Federman N., Albert C.M. Larotrectinib for paediatric solid tumours harbouring NTRK gene fusions: phase 1 results from a multicentre, open-label, phase 1/2 study. Lancet Oncol. 2018;19:705–714. doi: 10.1016/S1470-2045(18)30119-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ardini E., Menichincheri M., Banfi P., Casero D., Giorgini M.L., Saccardo M. Abstract 2092: the ALK inhibitor NMOL/LS-E628 also potently inhibits ROS1 and induces tumor regression in ROS-driven models. Canc Res. 2013;73 2092–92. [Google Scholar]
- 58.Shah N., Lankerovich M., Lee H., Yoon J.G., Schroeder B., Foltz G. Exploration of the gene fusion landscape of glioblastoma using transcriptome sequencing and copy number data. BMC Genom. 2013;14:818. doi: 10.1186/1471-2164-14-818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sartore Bianchi A., Ardini E., Bosotti R., Amatu A., Valtorta E., Somaschini A. Sensitivity to Entrectinib associated with a novel LMNA-NTRK1 gene fusion in metastatic colorectal cancer. J Natl Cancer Inst. 2016;108:306. doi: 10.1093/jnci/djv306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lee S.J., Li G.G., Kim S.T., Hong M.E., Jang J., Yoon N. NTRK1 rearrangement in colorectal cancer patients: evidence for actionable target using patient-derived tumor cell line. Oncotarget. 2015;6:39028–39035. doi: 10.18632/oncotarget.5494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Milione M., Ardini E., Christiansen J., Valtorta E., Veronese S., Bosotti R. Identification and characterization of a novel rearrangement in a colorectal cancer patient. Oncotarget. 2017;8:55353–55360. doi: 10.18632/oncotarget.19512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Farago A.F., Le L.P., Zheng Z., Muzikansky A., Drilon A., Patel M. Durable clinical response to Entrectinib in NTRK1-rearranged non-small cell lung cancer. J Thorac Oncol. 2015;10:1670–1674. doi: 10.1097/01.JTO.0000473485.38553.f0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wu G., Diaz A.K., Paugh B.S., Rankin S.L., Ju B., Li Y. The genomic landscape of diffuse intrinsic pontine glioma and pediatric non-brainstem high-grade glioma. Nat Genet. 2014;46:444–450. doi: 10.1038/ng.2938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Zheng Z., Liebers M., Zhelyazkova B., Cao Y., Panditi D., Lynch K.D. Anchored multiplex PCR for targeted next-generation sequencing. Nat Med. 2014;20:1479–1484. doi: 10.1038/nm.3729. [DOI] [PubMed] [Google Scholar]
- 65.Solomon B.J., Mok T., Kim D.W., Wu Y.L., Nakagawa K., Mekhail T. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N Engl J Med. 2014;371:2167–2177. doi: 10.1056/NEJMoa1408440. [DOI] [PubMed] [Google Scholar]
- 66.Frattini V., Trifonov V., Chan J.M., Castano A., Lia M., Abate F. The integrated landscape of driver genomic alterations in glioblastoma. Nat Genet. 2013;45:1141–1149. doi: 10.1038/ng.2734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Jones D.T.W., Hutter B., Jäger N., Korshunov A., Kool M., Warnatz H.J. Recurrent somatic alterations of FGFR1 and NTRK2 in pilocytic astrocytoma. Nat Genet. 2013;45:927–932. doi: 10.1038/ng.2682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wiesner T., He J., Yelensky R., Esteve-Puig R., Botton T., Yeh I. Kinase fusions are frequent in spitz tumours and spitzoid melanomas. Nat Commun. 2014;5:3116. doi: 10.1038/ncomms4116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Bongarzone I., Pierotti M.A., Monzini N., Mondellini P., Manenti G., Donghi R. High frequency of activation of tyrosine kinase oncogenes in human papillary thyroid carcinoma. Oncogene. 1989;4:1457–1462. [PubMed] [Google Scholar]
- 70.Greco A., Mariani C., Miranda C., Lupas A., Pagliardini S., Pomati M. The DNA rearrangement that generates the TRK-T3 oncogene involves a novel gene on chromosome 3 whose product has a potential coiled-coil domain. Mol Cell Biol. 1995;15:6118–6127. doi: 10.1128/mcb.15.11.6118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Greco A., Pierotti M.A., Bongarzone I., Pagliardini S., Lanzi C., Della Porta G. TRK-T1 is a novel oncogene formed by the fusion of TPR and TRK genes in human papillary thyroid carcinomas. Oncogene. 1992;7:237–242. [PubMed] [Google Scholar]
- 72.Fernandez Cuesta L., Peifer M., Lu X., Sun R., Ozretić L., Seidal D. Frequent mutations in chromatin-remodelling genes in pulmonary carcinoids. Nat Commun. 2014;5:3518. doi: 10.1038/ncomms4518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ross J.S., Wang K., Gay L., Al Rohil R., Rand J.V., Jones D.M. New routes to targeted therapy of intrahepatic cholangiocarcinomas revealed by next-generation sequencing. Oncol. 2014;19:235–242. doi: 10.1634/theoncologist.2013-0352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Ito S., Ishida E., Skalova A., Matsuura K., Kumamoto H., Sato I. Case report of mammary analog secretory carcinoma of the parotid gland. Pathol Int. 2012;62:149–152. doi: 10.1111/j.1440-1827.2011.02759.x. [DOI] [PubMed] [Google Scholar]
- 75.Del Castillo M., Chibon F., Arnould L., Croce S., Ribeiro A., Perot G. Secretory breast carcinoma: a histopathologic and genomic spectrum characterized by a joint specific ETV6-NTRK3 gene fusion. Am J Surg Pathol. 2015;39:1458–1467. doi: 10.1097/PAS.0000000000000487. [DOI] [PubMed] [Google Scholar]
- 76.Tognon C., Knezevich S.R., Huntsman D., Roskelley C.D., Melnyk N., Mathers J.A. Expression of the ETV6-NTRK3 gene fusion as a primary event in human secretory breast carcinoma. Canc Cell. 2002;2:367–376. doi: 10.1016/s1535-6108(02)00180-0. [DOI] [PubMed] [Google Scholar]
- 77.Wong V., Pavlick D., Brennan T., Yelensky R., Crawford J., Ross J.S. Evaluation of a congenital infantile fibrosarcoma by comprehensive genomic profiling reveals an LMNA-NTRK1 gene fusion responsive to crizotinib. J Natl Cancer Inst. 2016;108:307. doi: 10.1093/jnci/djv307. [DOI] [PubMed] [Google Scholar]
- 78.Knezevich S.R., McFadden D.E., Tao W., Lim J.F., Sorensen P.H. A novel ETV6-NTRK3 gene fusion in congenital fibrosarcoma. Nat Genet. 1998;18:184–187. doi: 10.1038/ng0298-184. [DOI] [PubMed] [Google Scholar]
- 79.Stransky N., Cerami E., Schalm S., Kim J.L., Lengauer C. The landscape of kinase fusions in cancer. Nat Commun. 2014;5:4846. doi: 10.1038/ncomms5846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Anderson J., Gibson S., Sebire N.J. Expression of ETV6-NTRK in classical, cellular and mixed subtypes of congenital mesoblastic nephroma. Histopathology. 2006;48:748–753. doi: 10.1111/j.1365-2559.2006.02400.x. [DOI] [PubMed] [Google Scholar]
- 81.Choi H.S., Rucker P.V., Wang Z., Fan Y., Albaugh P., Chopiuk G. (R)-2-Phenylpyrrolidine substituted imidazopyridazines: a new class of potent and selective pan-TRK inhibitors. ACS Med Chem Lett. 2015;6:562–567. doi: 10.1021/acsmedchemlett.5b00050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.David S., Douglas E., Dara L. 2019. NCCN clinical practice guidelines in oncology: non-small cell lung cancer (2019. V3)https://www.nccn.org/professionals/physician_gls/default.aspx#site Available from: [Google Scholar]
- 83.Aib A.P., Mahmoud M. 2019. NCCN clinical practice guidelines in oncology: colon cancer (2019. V1)https://www.nccn.org/professionals/physician_gls/default.aspx#colon Available from: [Google Scholar]
- 84.Menichincheri M., Ardini E., Magnaghi P., Avanzi N., Banfi P., Bossi R. Discovery of Entrectinib: a new 3-aminoindazole as a potent anaplastic lymphoma kinase (ALK), c-ros oncogene 1 kinase (ROS1), and pan-tropomyosin receptor kinases (Pan-TRKs) inhibitor. J Med Chem. 2016;59:3392–3408. doi: 10.1021/acs.jmedchem.6b00064. [DOI] [PubMed] [Google Scholar]
- 85.Ardini E., Menichincheri M., Banfi P., Bosotti R., de Ponti C., Pulci R. Entrectinib, a pan-TRK, ROS1, and ALK inhibitor with activity in multiple molecularly defined cancer indications. Mol Canc Therapeut. 2016;15:628–639. doi: 10.1158/1535-7163.MCT-15-0758. [DOI] [PubMed] [Google Scholar]
- 86.Roche . June 18 2019. Japan becomes the frst country to approve Roche's per sonalised medicine Rozlytrek.https://www.roche.com/media/releases/med-cor-2019-06-18 Available from: [Google Scholar]
- 87.Lewis R.T., Bode C.M., Choquette D.M., Potashman M., Romero K., Stellwagen J.C. The discovery and optimization of a novel class of potent, selective, and orally bioavailable anaplastic lymphoma kinase (ALK) inhibitors with potential utility for the treatment of cancer. J Med Chem. 2012;55:6523–6540. doi: 10.1021/jm3005866. [DOI] [PubMed] [Google Scholar]
- 88.Weiss G., Sachdev J., Infante J., Mita M., Natale R., Arkenau H.T. Phase (Ph) 1/2 study of TSR-011, a potent inhibitor of ALK and TRK, including crizotinib-resistant ALK mutations. J Clin Oncol. 2014;32 e19005–e05. [Google Scholar]
- 89.Albanese C., Alzani R., Amboldi N., Degrassi A., Festuccia C., Fiorentini F. Anti-tumour efficacy on glioma models of PHA-848125, a multi-kinase inhibitor able to cross the blood–brain barrier. Br J Pharmacol. 2013;169:156–166. doi: 10.1111/bph.12112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Albanese C., Alzani R., Amboldi N., Avanzi N., Ballinari D., Brasca M.G. Dual targeting of CDK and tropomyosin receptor kinase families by the oral inhibitor PHA-848125, an agent with broad-spectrum antitumor efficacy. Mol Canc Therapeut. 2010;9:2243–2254. doi: 10.1158/1535-7163.MCT-10-0190. [DOI] [PubMed] [Google Scholar]
- 91.Brasca M.G., Amboldi N., Ballinari D., Cameron A., Casale E., Cervi G. Identification of N,1,4,4-tetramethyl-8-{[4-(4-methylpiperazin-1-yl)phenyl]amino}-4,5-dihydro-1H-pyrazolo[4,3-h]quinazoline-3-carboxamide (PHA-848125), a potent, orally available cyclin dependent kinase inhibitor. J Med Chem. 2009;52:5152–5163. doi: 10.1021/jm9006559. [DOI] [PubMed] [Google Scholar]
- 92.Thress K., MacIntyre T., Wang H., Liu Z.Y., Hoffmann E., Wang T. 574 Poster identification and preclinical characterization of AZ-23, a novel, selective, and orally bioavailable inhibitor of the TRK kinase pathway. Eur J Cancer Supplements. 2008;6:180. doi: 10.1158/1535-7163.MCT-09-0036. [DOI] [PubMed] [Google Scholar]
- 93.Fancelli D., Moll J., Varasi M., Bravo R., Artico R., Berta D. 1,4,5,6-Tetrahydropyrrolo[3,4-c]pyrazoles: identification of a potent Aurora kinase inhibitor with a favorable antitumor kinase inhibition profile. J Med Chem. 2006;49:7247–7251. doi: 10.1021/jm060897w. [DOI] [PubMed] [Google Scholar]
- 94.Lippa B., Morris J., Corbett M., Kwan T.A., Noe M.C., Snow S.L. Discovery of novel isothiazole inhibitors of the TRKA kinase: structure−activity relationship, computer modeling, optimization, and identification of highly potent antagonists. Bioorg Med Chem Lett. 2006;16:3444–3448. doi: 10.1016/j.bmcl.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 95.Hyeonjeong C., Son Y., Byun B., Choi S., Lee K. Identification of pyrrole[3,4-c]pyrazoles as potent tropomyosin receptor kinase A (TRKA) inhibitors. Bull Kor Chem Soc. 2016;37:1378–1380. [Google Scholar]
- 96.Han S.Y., Lee C.O., Ahn S.H., Lee M.O., Kang S.Y., Cha H.J. Evaluation of a multi-kinase inhibitor KRC-108 as an anti-tumor agent in vitro and in vivo. Invest N Drugs. 2012;30:518–523. doi: 10.1007/s10637-010-9584-2. [DOI] [PubMed] [Google Scholar]
- 97.Stachel S.J., Sanders J.M., Henze D.A., Rudd M.T., Su H.P., Li Y. Maximizing diversity from a kinase screen: identification of novel and selective pan-TRK inhibitors for chronic pain. J Med Chem. 2014;57:5800–5816. doi: 10.1021/jm5006429. [DOI] [PubMed] [Google Scholar]
- 98.Carboni J.M., Wittman M., Yang Z., Lee F., Greer A., Hurlburt W. BMS-754807, a small molecule inhibitor of insulin-like growth factor-1R/IR. Mol Canc Therapeut. 2009;8:3341–3349. doi: 10.1158/1535-7163.MCT-09-0499. [DOI] [PubMed] [Google Scholar]
- 99.Wenglowsky S.M., Brooijmans N., Miduturu C.V., Bifulco N., inventors. Blueprint Medicines Co., assignee . 2017 Mar 02. Compounds and compositions useful for treating disorders related to NTRK. [Google Scholar]
- 100.Wenglowsky S.M., Miduturu C.V., Bitfulco N., Kim J.L., inventors. Blueprint Medicines Co., assignee . 2017 May 26. Compounds and compositions useful for treating disorders related to NTRK. [Google Scholar]
- 101.Zhu L., Hu Y.D., Wu W., Dai L.G., Duan X.W., Yang Y.Q., inventors. Chia Tai Tianqing Pharmaceutical Group Co. Ltd., assignee . 2018 May 03. Amino pyrazolopyrimidine compound used as a neurotrophic factor tyrosine kinase receptor inhibitor. [Google Scholar]
- 102.Liu H., Tan H., He C., Wang X.L., Liu Q.H., Li Z.F., inventors. Fochon Pharmaceuticals Ltd., assignee . 2019 Sept 19. Substituted (2-azabicyclo[3.1.0]hexan-2-yl)pyrazolo[1,5-a]pyrimidine and imidazo[1,2-b]pyridazine compounds as TRK kinases inhibitors. [Google Scholar]
- 103.Li J., Zhang D., Wang Z., Pan L.C., Wang Q., inventors. Hitgen Inc., assignee . 2019 June 27. Imidazo[1,2-b]pyridazinemacrocyclic kinase inhibitor. [Google Scholar]
- 104.Albaugh P., Fan Y., Mi Y., Sun F., Adrian F., Li N. Discovery of GNF-5837, a selective TRK inhibitor with efficacy in rodent cancer tumor models. ACS Med Chem Lett. 2012;3:140–145. doi: 10.1021/ml200261d. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Yakes F.M., Chen J., Tan J., Yamaguchi K., Shi Y., Yu P. Cabozantinib (XL184), a novel MET and VEGFR2 inhibitor, simultaneously suppresses metastasis, angiogenesis, and tumor growth. Mol Canc Therapeut. 2011;10:2298–2308. doi: 10.1158/1535-7163.MCT-11-0264. [DOI] [PubMed] [Google Scholar]
- 106.Lieberman H., Yang D.L., Philbrook M., Santos M., Ho C., inventors. Genzyme Co., assignee . 2016 Jun 23. Pharmaceutical formulations of tropomyosin related kinase (TRK) inhibitors. [Google Scholar]
- 107.Skerratt S.E., Andrews M., Bagal S.K., Bilsland J., Brown D., Bungay P.J. The discovery of a potent, selective, and peripherally restricted pan-TRK inhibitor (PF-06273340) for the treatment of pain. J Med Chem. 2016;59:10084–10099. doi: 10.1021/acs.jmedchem.6b00850. [DOI] [PubMed] [Google Scholar]
- 108.Lieberman H., Yang D.L., Philbrook C.M., Santos M., Ho C., inventors. Genzyme Co., assignee . 2019 Mar 05. Pharmaceutical formulations of tropomyosin related kinase (TRK) inhibitors. [Google Scholar]
- 109.El Zein N., D'Hondt S., Sariban E. Crosstalks between the receptors tyrosine kinase EGFR and TRKA and the GPCR, FPR, in human monocytes are essential for receptors-mediated cell activation. Cell Signal. 2010;22:1437–1447. doi: 10.1016/j.cellsig.2010.05.012. [DOI] [PubMed] [Google Scholar]
- 110.Wang T., Yu D., Lamb M.L. TRK kinase inhibitors as new treatments for cancer and pain. Expert Opin Ther Pat. 2009;19:305–319. doi: 10.1517/13543770902721261. [DOI] [PubMed] [Google Scholar]
- 111.Hong S., Kim J., Seo J.H., Jung K.H., Hong S.S., Hong S. Design, synthesis, and evaluation of 3,5-disubstituted 7-azaindoles as TRK inhibitors with anticancer and antiangiogenic activities. J Med Chem. 2012;55:5337–5349. doi: 10.1021/jm3002982. [DOI] [PubMed] [Google Scholar]
- 112.Stachel S.J., Egbertson M., Brnardic E., Jones K.G., Sanders J.M., Henze D., Merck S., Dohme C., inventors. Merck Sharp and Dohme Corp., assignees. TRKA kinase inhibitors, 2015 Nov 10. Compositions and methods thereof. [Google Scholar]
- 113.Tomizawa M., Nishi H., Tanaka H., Aoki M., inventors. Chugai Pharmaceutical Co. Ltd., assignee . 2017 May 04. Dihydronaphtho[2,3-b]benzofuran derivative. [Google Scholar]
- 114.Tanaka H., Sase H., Tsukaguchi T., Hasegawa M., Tanimura H., Yoshisa M. Selective TRK inhibitor CH7057288 against TRK fusion-driven cancer. Mol Canc Therapeut. 2018;17:2519–2529. doi: 10.1158/1535-7163.MCT-17-1180. [DOI] [PubMed] [Google Scholar]
- 115.Bailey J.J., Jaworski C., Tung D., Wängler C., Wängler B., Schirrmacher R. Tropomyosin receptor kinase inhibitors: an updated patent review for 2016–2019. Expert Opin Ther Pat. 2020;30:325–339. doi: 10.1080/13543776.2020.1737011. [DOI] [PubMed] [Google Scholar]
- 116.Chung V., Wang L., Fletcher M.S., Massarelli E., Reckamp K.L., Cristea M.C. First-time in-human study of VMD-928, an allosteric and irreversible TRKA selective inhibitor, in patients with solid tumors or lymphoma. J Clin Oncol. 2019;37(15_suppl):TPS3146. [Google Scholar]
- 117.Subramanian G., Johnson P.D., Zachary T., Roush N., Zhu Y., Bowen S.J. Deciphering the allosteric binding mechanism of the human tropomyosin receptor kinase A (hTRKA) inhibitors. ACS Chem Biol. 2019;14:1205–1216. doi: 10.1021/acschembio.9b00126. [DOI] [PubMed] [Google Scholar]
- 118.Cee V.J., Albrecht B.K., Geuns Meyer S., Hughes P., Bellon S., Bready J. Alkynylpyrimidine amide derivatives as potent, selective, and orally active inhibitors of Tie-2 kinase. J Med Chem. 2007;50:627–640. doi: 10.1021/jm061112p. [DOI] [PubMed] [Google Scholar]
- 119.Allen S., Andrews S.W., Blake J.F., Condroski K.R., Hass J., Huang L., inventors. Array Biopharma Inc., assignee. 2012 Nov 22. Pyrrolidinyl urea and pyrrolidinyl thiourea compounds as TRKA kinase inhibitors. [Google Scholar]
- 120.Su H.P., Rickert K., Burlein C., Narayan K., Bukhtiyarova M., Hurzy D.M. Structural characterization of nonactive site, TRKA-selective kinase inhibitors. Proc Natl Acad Sci U S A. 2017;114:e297–e306. doi: 10.1073/pnas.1611577114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Paiva S.L., Crews C.M. Targeted protein degradation: elements of PROTAC design. Curr Opin Chem Biol. 2019;50:111–119. doi: 10.1016/j.cbpa.2019.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Zou Y., Ma D., Wang Y. The PROTAC technology in drug development. Cell Biochem Funct. 2019;37:21–30. doi: 10.1002/cbf.3369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Fang Y., Liao G.H., Yu B. Small-molecule MDM2/X inhibitors and PROTAC degraders for cancer therapy: advances and perspectives. Acta Pharm Sin B. 2020;10:1253–1278. doi: 10.1016/j.apsb.2020.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Zhao B., Burgess K. TRKC-targeted kinase inhibitors and PROTACs. Mol Pharm. 2019;16:4313–4318. doi: 10.1021/acs.molpharmaceut.9b00673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Du J.T., Guo J., Kang D.W., Li Z.H., Wang G., Wu J.B. New techniques and strategies in drug discovery. Chin Chem Lett. 2020;31:1695–1708. [Google Scholar]