Abstract
Of the hypothesized causes of Gulf War Illness (GWI), a chronic multi-symptom illness afflicting approximately 25% of military personnel deployed to the 1991 Gulf War, exposure to depleted uranium (DU) munitions has attracted international concern. Past research has not tested the potential association of GWI with inhaled DU nor used isotope mass spectrometry of sufficient sensitivity to rigorously assess prior DU exposure. We applied a standard biokinetic model to predict the urinary concentration and uranium isotopic ratios for a range of inhalation exposures. We then applied sensitive mass spectrometry capable of detecting the predicted urinary DU to 154 individuals of a population-representative sample of U.S. veterans in whom GWI had been determined by standard case definitions and DU inhalation exposures obtained by medical history. We found no difference in the 238U/235U ratio in veterans meeting the standard case definitions of GWI versus control veterans, no differences by levels of DU inhalation exposure, and no 236U associated with DU was detected. These findings show that even the highest likely levels of DU inhalation played no role in the development of GWI, leaving exposure to aerosolized organophosphate compounds (pesticides and sarin nerve agent) as the most likely cause(s) of GWI.
Subject terms: Environmental sciences, Biomarkers, Diseases, Mass spectrometry
Introduction
Thirty years have passed since the 1990 invasion of Kuwait by Iraq and the subsequent 1991 Persian Gulf War that liberated Kuwait. During or shortly after the 1991 conflict, an estimated 25%1 of the approximately 700,000 deployed U.S. (and additional allied) military personnel developed an unusual chronic multi-symptom illness, referred to as Gulf War Illness (GWI)2, manifested by fatigue, fever and night sweats, memory and concentration problems, pathogen-free diarrhoea, sexual dysfunction, chronic body pain and other symptoms compatible with autonomic nervous system dysfunction3 and dysfunction of the brain’s cholinergic system4. Investigations into the causes have considered potential war theatre exposures including low-level chemical warfare nerve agent(s), pyridostigmine bromide anti-nerve-agent medication, pesticides, multiple immunizations, depleted uranium (DU), and combat stress. The possibility of toxic effects from DU, first raised after the first large scale use of DU munitions in the Gulf War, have stimulated international concern because of potential exposure of civilian populations from the Gulf War and from later conflicts in Kosovo, Bosnia, the Persian Gulf and others. Studies attempting to address this concern have failed to generate a consensus because of limitations in the sensitivity of tests for DU in urine and the lack of any investigation of DU in veterans meeting accepted case definitions of GWI.
DU is uranium depleted isotopically in the more fissile 235U isotope which is separated by isotope enrichment methods to produce enriched 235U for use in nuclear reactors and nuclear weapons. Instead of remaining as unused nuclear waste, it has been made into dense armour-piercing munitions used in military conflicts in 1991 and 2003 onwards as well as in tank armour. In a hard target impact a DU-containing projectile efficiently penetrates the target’s armour, partially fragments the DU core, and ignites a brief intense fire, combusting and oxidizing DU into aerosolized oxides. Humans may then internalize DU by inhalation of aerosolized DU oxides, oral ingestion of DU oxide particles that settle in the environment, or retention of DU in metallic form in shrapnel fragments in body wounds.
Adverse effects of significant intake are hypothesized to result from heavy metal toxicity and alpha particle radiation from DU mainly in the lungs, kidneys and bone where it is concentrated. Despite numerous studies demonstrating long-term urinary excretion of DU from industrial exposure and prediction of possible adverse effects on the basis of doses of heavy metal and alpha radiation5–8, no actual adverse effects in humans have been described, though serious effects may be masked because of major gaps in research9. Nevertheless, DU continues to be considered a plausible cause of GWI10 and courts in the UK and Italy have attributed illness and death to inhalation exposure to DU11,12.
The 1991 Gulf War presents an opportunity to study the health effects of inhaled DU. Approximately 300 tonnes of DU-munitions were fired by tanks, artillery and aircraft mainly at targets in southern Iraq and especially along the Basra Road where Iraqi tanks were destroyed in large numbers by DU munitions. In addition to combat-related exposures, in July 1991 a post-war explosion and fire at an ammunition storage site within U.S. Army Camp Doha, Kuwait, resulted in a series of explosions involving several tonnes of DU munitions, causing DU-related aerosols to be released into the dense smoke plume from the fire to which many personnel were exposed during containment and clean-up13.
Natural uranium (NU) is composed of 238U (99.27%), 235U (0.72%) and 234U (0.0054% in minerals, 0.005–0.02% in water sources), with a 238U/235U ratio of 137.80–137.881,14. In the production of nuclear fuel, enriched uranium (EU) high in 235U is extracted from NU leaving the residual DU strongly depleted in 235U and thus with a greatly increased 238U/235U ratio of approximately 5008,15. Aside from fission of 235U in power generation, nuclear reactions also include neutron capture by 235U generating 236U, which is absent in NU; when re-enriched during nuclear fuel recycling, the resulting DU acquires this rare isotope. While EU has variable and significant amounts of 236U, DU contains 236U in low proportions (~ 0.003%)15. The large differences in isotope composition among EU, NU and DU can be exploited by mass spectrometry to quantify even small proportions of DU in humans and the environment16,17.
NU occurs naturally in food, water and soil. A portion (~ 2%) of ingested or inhaled uranium is absorbed into the bloodstream, concentrated and stored in bone and kidney, and excreted slowly in urine over many years. A large intake of NU, EU or DU can usually be detected by a urine assay for total uranium concentration [U]. Total [U] values above 43 ng/g of creatinine—the 95th percentile of the US population18,19—indicate an excess body load of uranium, but highly sensitive mass spectrometry is required to determine whether the excess is due to NU, EU, DU or some combination. Two methods of mass spectrometry have been used to detect DU in human urine samples: lower precision sector-field mass spectrometry (SF-ICP-MS) has been used to differentiate DU from NU in Gulf War veterans at 238U/235U ratios above 166; whereas, higher precision multi-collector mass spectrometry (MC-ICP-MS) applied to chemically purified U can detect DU at 238U/235U ratios as low as 140.
A series of studies between 1993 and 2009 was conducted to determine whether an exposure to DU in the 1991 Gulf War resulted in enough absorption to detect in urine years later5. At first, small numbers of U.S. soldiers who had been involved in friendly fire explosions and, later, U.S. veterans who wanted to be tested provided urine samples for assay. All of the studies attempted to identify DU by measuring the total [U]. Some, but not all, veterans with X-ray-documented DU fragments retained in their bodies were found to have extremely high total [U] levels, far above the 95th percentile of the U.S. population—the cut point for distinguishing DU—and no veterans with inhalation exposures but no retained shrapnel did. In recent studies20,21, however, measurements with low precision SF-ICP-MS identified 3 veterans out of 1,700 with 238U/235U ratio above the cut point of 166 confirming DU in their urine, but 2 of these 3 had total [U] below the cut point for DU and the third was right at the cut point; whereas, 29 veterans with no evidence of DU by SF-ICP-MS were nevertheless above the cut point by total [U], and other veterans who recalled inhalation exposures had far lower total [U] levels. Thus, while these studies demonstrated that a few veterans with retained shrapnel excrete very high levels of DU in their urine, the method was too imprecise to evaluate excretion from inhalation exposures. More importantly, since none of the studies measured the veterans’ continuing symptoms or applied the standard GWI case definitions, no study has yet addressed the question of whether the symptoms of GWI could be due to DU exposure.
In this paper we extend prior work to measurement of DU excretion in U.S. veterans with or without GWI who reported information on possible DU exposures. We first calculated the urinary DU concentrations expected as a function of time since exposure to plausible DU oxide levels from aerosol inhalation scenarios in the 1991 Gulf War6,8,22 based on the Human Respiratory Tract Model (HRTM) relating absorption and excretion23. We then evaluated the capability of the following 3 bioassay methods to detect the subtle DU excretion in urine expected from inhalation absorption: (1) screening for excess total [U]; (2) measurement of 238U/235U ratio with high sensitivity multi-collector mass spectrometry (MC-ICP-MS) on chemically purified U; and finally, bivariate analysis of the 236U/238U and 235U/238U isotopic ratios. We applied these methods to a highly studied population-representative sample of both theatre-deployed and non-deployed Gulf War-era U.S. veterans in whom Gulf War Illness (GWI) had been determined by standard case definitions, whose wartime DU exposures had been ascertained by interview, and who provided a 24-h urine sample 18–20 years after the war. We compared these measured values to those predicted to be found 18–20 years after exposure to medically meaningful DU levels in the war. The goal was to provide the best chance of finding DU if potential disease-causing inhalation exposure had occurred and for the first time provide high confidence in a negative finding.
Results
Predicted values of DU excretion from historic inhalation exposures
Inhaled fine particulates of DU oxide have the potential to lodge deep in the lung, decompose slowly into solution into the blood stream, and become stored in bone, kidney and other organs to be excreted over time with organ and bone re-working, all while undergoing slow radioactive decay. The rate of dissolution is a key parameter that underpins the notion that DU can be detected in urine many years after exposure.
To test whether DU plays any role in GWI, it is first necessary to predict the concentration of DU expected in a urine sample for a given DU aerosol inhalation exposure as a function of the dose and oxide type of the original DU exposure, the time since exposure, and likely dietary intakes of NU in the run up to urine collection. Without this prediction, it is impossible to know whether a negative test is due to an inconsequential exposure or an insensitive urine assay method—a valid criticism of past research on this problem.
The defining studies by the U.S. Department of Defense6, the World Health Organisation22 and the British Royal Society8, classified battlefield situations of potential DU aerosol exposure into 3 standard exposure levels likely to occur in combat situations: level I-high, level II-medium, and level III-low. Exposure level I includes direct inhalation of an impact aerosol; level II, inhalation of resuspended impact aerosol or oral ingestion within a contaminated vehicle; and level III, inhalation of an aerosol plume at a distance from an impact or fire or resuspension from ground contamination. Doses in milligrams of DU taken into the body in each of these situations were estimated with evidence from other studies, including field studies involving measurements during destruction of vehicles with DU penetrators (Table 1)6.
Table 1.
Current ranges of urinary total [U] and U isotopic ratios that identify DU estimated from different levels of DU inhalation exposure during the 1991 Gulf War, time since exposure, and daily dietary intake of natural uranium running up to urine sample collection.
| Parameters specified in the prediction model | Ranges of parameters expected 18 years after specified DU inhalation exposure | Can expected levels of DU be detected by criteria used in prior studies? | ||||||
|---|---|---|---|---|---|---|---|---|
| Standard DU exposure level | Estimated DU intake (mg) for the exposure level in 1991 Gulf Wara | Daily dietary U excretion (ng) in run-up to testing | Total [U] (ng U/g creatinine) | 238U/235U | 236U/238U × 10–6 | Method 1: total [U] > 50 ng U/g creatinineb | Method 2: 238U/235U > 166 by SF-ICP-MSc | Method 3: 238U/235U > 140 by MC-ICP-MSd |
| Level I | 250 | 2 | 14.5–74.5 | 367–467 | 25.9–29.2 | Rarely | Yes | Yes |
| 8 | 20.5–80.5 | 247–397 | 18.3–27.0 | Rarely | Yes | Yes | ||
| Level II | 10 | 2 | 2.5–4.9 | 161–241 | 6.0–17.8 | No | Yes | Yes |
| 8 | 8.5–10.9 | 144–171 | 1.8–8.0 | No | No | Yes | ||
| Level II | 5 | 2 | 2.3–3.5 | 150–198 | 3.3–12.6 | No | No | Yes |
| 8 | 8.3–9.5 | 141–155 | 0.9 -4.6 | No | No | Yes | ||
| Level III | 2 | 2 | 2.1–2.6 | 143–165 | 1.4–6.7 | No | No | Yes |
| 8 | 8.1–8.6 | 139–145 | 0.4–2.0 | No | No | Yes | ||
aNumerical values are derived from calculations of8,23,24 as illustrated in Fig. 1, described in more detail in on-line methods.
bIn the most recent study of DU in Gulf War veterans, Dorsey et al.20 screened urine total [U] for DU by this criterion.
cDorsey et al.20 identified the presence of DU with the 238U/235U ratio measured by lower precision sector field–inductively coupled plasma-mass spectrometry (SF-ICP-MS).
dThe present study identified the presence of DU with the 238U/235U ratio measured by the high precision multiple collector–inductively coupled plasma-mass spectrometry (MC-ICP-MS).
We used the modelling of8,22,24 to estimate the urinary excretion of uranium on the basis of an inhalation dose. We considered intake doses representing each of the Royal Society’s exposure levels at 18 years after exposure and at 2 likely dietary intake levels of NU in the run up to urine collection to predict current excretion rates of DU oxides (UO2, U3O8, etc.) in a range of excretion levels determined by the level of uncertainty in the ICRP models (Fig. 1). The model output8,24 allowed calculation of the current expected ranges of the following 3 parameters most used for detecting past DU exposure from urinary assays: total [U], the 238U/235U isotopic ratio, and the 236U/238U ratio, given in Table 1.
Figure 1.
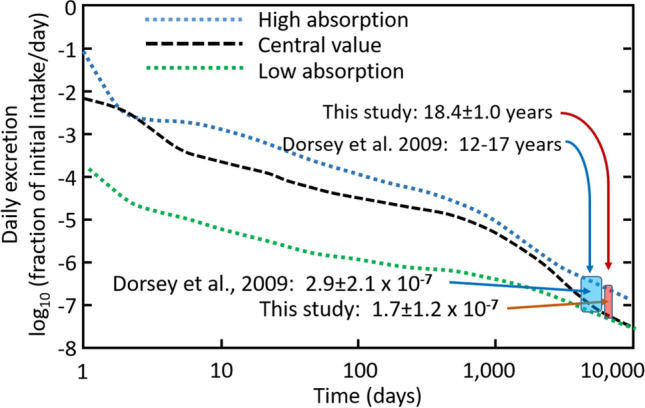
Estimation of current urinary DU excretion from DU oxides absorbed 18 years earlier. From the Human Respiratory Track Model (HRTM) for inhalation of uranium oxides we estimated the daily urinary excretion of DU, expressed as a fraction of the original inhaled dose (log scale), and plotted as a function of days since inhalation (log scale). In the sample of veterans studied, the duration between potential inhalation (in the first half of 1991 during the conflict) and the urine collection (November 2008–June 2010) was 6720 ± 365 days or 18.4 ± 1.0 years, shown as the width of the small red box. The analogous region from Dorsey et al.20 discussed in the text is shown in the larger blue box. Three curves showing fractional uranium excretion predicted by the combined dissolution-storage-excretion function of the HRTM for uranium oxide particulates are shown; these represent “Low” and “High” absorption curves during dissolution and metabolism of compounds of uranium oxide with contrasting chemical form and solubilities. The figure is modified from8,24 using the HRTM model with aerosol and oxide physicochemical characteristics summarized8 and taking into account the uncertainty in the HRTM model parameters23.
Comparison of the ability of three methods to distinguish DU from NU in urine
Total [U]
Applying the criterion of finding > 50 ng U/g creatinine of total [U] in urine will detect only veterans excreting the very highest total [U] in those with Level I inhalation exposures in the Gulf War, but would be unable to distinguish any with Level II or III exposures from NU excretion (Table 1).
238U/235U measured by SF-ICP-MS
The relatively low precision SF-ICP-MS method would be able to differentiate DU from NU in all veterans with Level I exposures in the Gulf War and most in the upper half with Level II exposures but only if they are consuming a diet low in NU (average 2 ng NU per day) so that DU is ≥ 25% of the total U excreted. It would thus be unable to differentiate most with Level II and all with Level III exposures from NU excretion (Table 1).
238U/235U measured by MC-ICP-MS after rigorous chemical purification of U (this study)
The high precision MC-ICP-MS method combined with chemical separation and purification of U from urine, allows the detection of excreted DU at a rate of > 0.068 ng/day, our methodological DU detection limit. Our prediction model indicates that it would detect an initial inhalation exposure of as little as 0.40 mg of DU from the 1991 Gulf War. Thus, it would be able to identify DU in all veterans with Gulf War exposures far less than the lowest Level III exposure (2 mg DU inhaled during the Gulf War) even if consuming a diet relatively high in NU before urine collection (Table 1). It follows then that only mass spectrometry with high precision MC-ICP-MS is capable of detecting DU from inhalation exposure in the Gulf War or confirming its absence in most Gulf War veterans.
Cohort of GWI cases and controls and battlefield deployment
We measured the uranium isotope composition in urine samples from a nested case–control sample of Gulf War veterans selected in a 3-stage stratified random sample of the 1991 U.S. military population studied in the U.S. Military Health Survey (USMHS). The methods of sample selection at the 3 stages have been published3,25. The first stage involved a computer-assisted telephone interview (CATI) survey (N = 8020) which included questions covering battlefield situations likely to involve inhalation of various levels of DU, from which we assigned the standard DU exposure levels. The second stage involved blood collection from all veterans whose symptoms met the 3 widely used case definitions of GWI (cases) and an approximately 15% random sample of those not meeting it (controls), including both deployed and not deployed to the Kuwaiti Theatre of Operations. The third stage constituted a smaller representative sample selected from the larger stage 2 sample, and included 106 who met the 3 standard case definitions of GWI2,26,27 in which cases comprised of 31 with syndrome variant 1 (“impaired cognition”); 42 with syndrome variant 2 (“confusion-ataxia”); 33 with syndrome variant 3 (“central pain”)2; and 47 control veterans comprised of 26 deployed to the war theatre and 21 non-deployed not meeting the case definitions. Between November 2008 and June 2010, the 154 veterans in the stage 3 sample were studied extensively in a 7-day clinical research protocol in which each travelled to Dallas, Texas (USA) to be hospitalized in the University of Texas Southwestern Medical Center’s Clinical and Translational Research Center. In addition to diverse neuropsychological, autonomic and neuroimaging studies, a 24-h urine sample was collected in urine containers prewashed with nitric acid to remove any trace uranium; creatinine was measured on an aliquot shortly after collection.
Effectiveness of total [U] of urine to rule out past DU exposure
The first method we used to detect evidence of past DU exposure was to screen the 154 GWI cases and control subjects’ urine for an increase in total [U] excretion (Table 2). The distribution of total [U] was similar to that of the U.S. population19, and no values exceeded its 95th percentile (Fig. 2a). The geometric mean of total [U] of the cases meeting the 3 case definitions of GWI was 1.78 ng U/g creatinine, statistically indistinguishable from the combined deployed and non-deployed controls (geometric mean 1.57 ng U/g creatinine, t test P = 0.18). These values of total [U] are consistent with lack of DU contamination but do not exclude the possibility of the small amounts of DU expected from our prediction model with Level II and III inhalation exposures (Table 1). Although continuing dissolution of DU shrapnel in metallic form retained in the body usually increases total [U] beyond the population’s 95% percentile, as concluded by20, our findings further confirm that screening of total [U] is not useful for detecting the far smaller intake doses and the time-limited exposure situations involved in inhalation exposures to DU aerosols (Table 1).
Table 2.
Urinary excretion rate of total U by Gulf War veterans’ clinical group.
| Clinical group | Sample size | Total [U] | Total [U] adjusted for creatinine | ||||
|---|---|---|---|---|---|---|---|
| Mean | 95% CI | 5th and 95th percentile | Range | Median | Mean | ||
| Non-deployed controls | 21 | 2.37 | − 1.04/+ 1.86 | 0.24–11.2 | 0.2–30.2 | 1.25 | 1.24 |
| Deployed controls | 27 | 3.80 | − 1.60/+ 2.78 | 0.42–50.2 | 0.32–96.4 | 2.16 | 1.87 |
| GWI syndrome 1 | 31 | 2.53 | − 0.78/+ 1.12 | 0.58–10.7 | 0.22–13.3 | 1.38 | 1.41 |
| GWI syndrome 2 | 42 | 4.00 | − 1.25/+ 1.81 | 0.77–21.7 | 0.70–28.8 | 2.05 | 2.15 |
| GWI syndrome 3 | 33 | 3.33 | − 1.05/+ 1.54 | 0.65–12.0 | 0.44–15.1 | 1.95 | 1.74 |
| All controls | 49 | 2.98 | − 0.98/+ 1.45 | 0.36–25.9 | 0.17–96.4 | 1.86 | 1.57 |
| All GWI | 106 | 3.30 | − 0.57/+ 0.69 | 0.69–16.2 | 0.13–23.9 | 1.84 | 1.78 |
| All samples | 154 | 3.24 | − 0.56/+ 0.68 | 0.57–17.6 | 0.17–96.4 | 1.84 | 1.71 |
Figure 2.
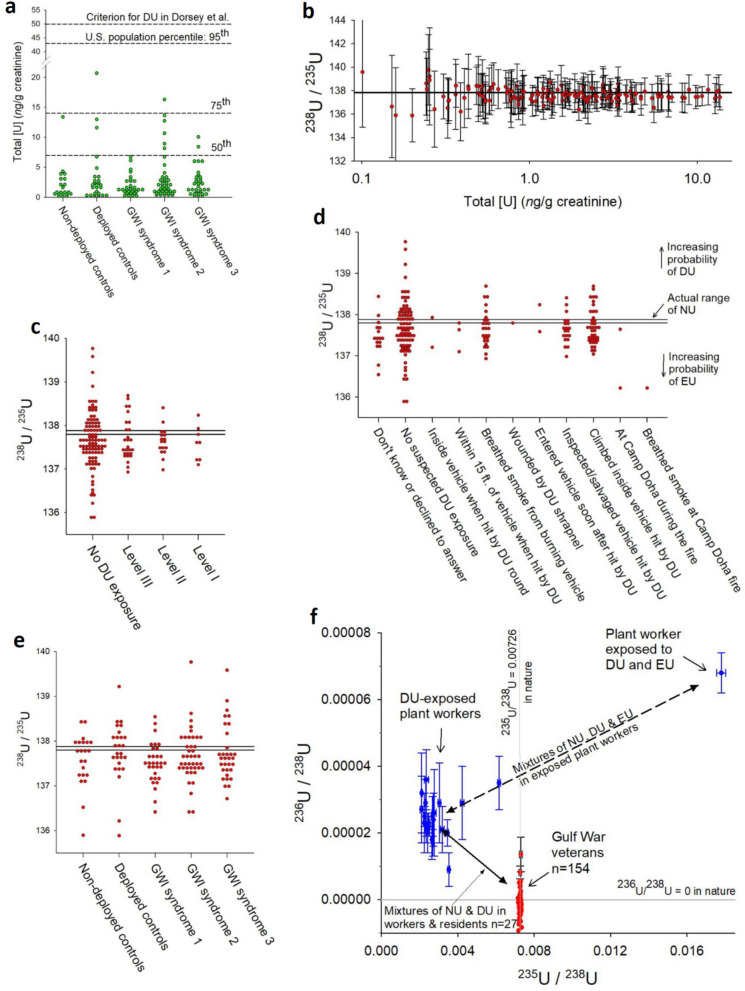
Exposure levels, incidents, and GWI clinical classification. (a) Total [U] (ng/g of creatinine) by veterans’ GWI clinical classification; horizontal lines indicate the 50th, 75th and 95th percentiles of the distribution of urine U concentrations in the US population18,19 and the lower limit for detecting DU of20. (b) Veterans’ 238U/235U ratios with individual measurement uncertainty intervals by total [U], demonstrating how the uncertainty intervals and variance increase at lower total [U]. All certainty intervals overlap natural U (horizontal lines). (c–e) Distributions of veterans’ 238U/235U ratios by standard classification of DU exposure levels8, (c) by specific DU exposure situations (d), and by GWI clinical classification (e). The horizontal reference lines indicate the range of the 238U/235U ratio of natural U (137.80–137.88), above which values suggest mixtures of natural U and DU and below which, mixtures of natural and enriched U; individual measurement uncertainties of ~ 1% are omitted for clarity. (f) Bivariate scatterplot of 236U/238U ratio by 235U/238U ratio for the sample of Gulf War veterans (red symbols), overlaid by those of workers in a DU plant in the town of Colonie, New York, known to have had substantial occupational inhalation DU exposures7,28. The horizontal reference line at 236U/238U = 0 emphasizes that natural U contains no 236U. The ratios from subjects with various exposure levels of DU would fall along the solid line; whereas, subjects with mixed exposure to DU and enriched U would fall in the upper right where one such DU worker is shown. Six of the Gulf War veterans had elevated 236U/238U ratios with certainty intervals that do not overlap zero, but their 235U/238U ratios are not reduced, which is incompatible with DU and EU; this is caused by an isobaric interference on mass 236 and is explained in the online methods and the text. The standard DU exposure levels range from level III (lowest) to level I (highest)8 The GWI clinical classification includes syndrome 1 (impaired cognition), syndrome 2 (confusion-ataxia) and syndrome 3 (central pain)2.
Use of high precision 238U/235U to determine significant inhalation exposure
The second method we used to detect past DU exposure was analysis of the 238U/235U isotopic ratio measured by the high precision MC-ICP-MS method (Table 3). The uncertainty in the 238U/235U ratio, measured by its 95% confidence interval, increases (precision decreases) as the urinary total [U] decreases (Fig. 2b), but it was less than ± 1% for 95% of the samples (Fig. 2b). For urine samples with total [U] above 1 ng/g creatinine and a ± 1% uncertainty, values of the 238U/235U ratio above 139–140 including their lower uncertainty bound are considered likely to represent the presence of DU (Fig. 2b). This threshold of 139–140 for confirmation of DU is more robust and > 10 times more sensitive than the threshold of 166 applied by Dorsey et al. using the lower precision SF-ICP-MS (Table 1)20.
Table 3.
Urinary uranium isotope ratios by Gulf War veterans’ clinical group.
| Clinical group | Sample size | 238U/235U | 236U/238U | |||
|---|---|---|---|---|---|---|
| Median | Meana | 95% CIa | Meana,c | 95% CIa | ||
| Undeployed controls | 21 | 137.79 | 137.62 | 0.26 | < LOD | n/a |
| Deployed controls | 27 | 137.84 | 137.75 | 0.25 | < LOD | n/a |
| GWI syndrome 1 | 31 | 137.50 | 137.51 | 0.16 | < LOD | n/a |
| GWI syndrome 2 | 42 | 137.62 | 137.68 | 0.16 | < LOD | n/a |
| GWI syndrome 3 | 33 | 137.62 | 137.71 | 0.19 | < LOD | n/a |
| All controls | 49 | 137.79 | 137.70 | 0.18 | < LOD | n/a |
| All GWI | 106 | 137.55 | 137.64 | 0.10 | < LOD | n/a |
| All samples | 154 | 137.63 | 137.66 | 0.09 | < LOD | n/a |
| In house urine no IRMM184d | 4 | 137.70 | 137.68 | 0.27 | < LOD | n/a |
| 2 ppb IRMM184 + 233Ue | 125 | 137.70 | 137.71 | 0.05 | 1.11E−07 | 1.3E−08 |
| IRMM184 certifiedf | 137.70 | 0.04 | 1.25E−07 | 5.3E−10 | ||
| Natural uranium | 137.82 | ~ 0.06 | < 10–8 | n/a | ||
| DU in munitions | ~ 500 | ~ 0.000030 | ||||
DU depleted uranium, IRMM European Commission's Institute for Reference Materials and Measurements, LOD limit of detection, n/a not applicable, U uranium.
aGeometric means with 95% CI.
bSince 238U/235U uncertainties are not significantly asymmetrical and are reported as a single value.
cThe 236U/238U ratios were overwhelmingly below the 0.0000015 limit of detection after all corrections and uncertainty propagations were made.
dThe 4 analyses of in-house urine that had no additional IRMM184 added.
eIRMM184+ 233U values reported are corrected for very minor contributions of other isotopes in the 233U that was added.
fIRMM certified value from https://crm.jrc.ec.europa.eu/p/40454/40475/By-application-field/Nuclear/IRMM-184-URANIUM-238-NATURAL-ISOTOPIC-NITRATE-SOLUTION/IRMM-184.
Exposure situations
When predictions of DU excretion are applied to groups of veterans with different standard levels of DU inhalation exposures, the 238U/235U ratios are below 139 for veterans with all 3 inhalation exposure levels (Fig. 2c; Kruskal–Wallis test P = 0.74). The 3 veterans with outlying values nearest the threshold between 139 and 140 all had very low values of total [U] and thus very wide uncertainty intervals that generously overlap the 238U/235U of NU (~ 137.8). When the battlefield exposure situations from which the standard exposure levels were generated were broken out, the distributions of the 238U/235U ratios showed no pattern suggesting any departure from NU outside of methodological uncertainty (Fig. 2d).
GWI symptoms
Likewise, veterans who continue to have potentially disabling symptoms of GWI had distributions of the 238U/235U ratio that did not differ from the deployed and non-deployed control veterans (Fig. 2e), and none had values that differed from NU. Moreover, the distribution of the 238U/235U ratios in the 3 GWI syndrome variant groups combined was similar to those of the deployed and non-deployed control groups (Kruskal–Wallis test P = 0.16).
Bivariate analysis of the 236U/238U and 235U/238U as a further test of DU exposure
As a further test for the possibility of DU in these veterans, we studied their location on the bivariate distribution of the veterans’ ratios of both 236U/238U and 235U/238U isotopic ratios. This is an important procedure because, since 236U is found only in EU and DU but not in NU, it provides a further direct method of distinguishing DU from NU and from ascertaining whether EU may also have been involved. Since 236U constitutes only ~ 0.003% of DU used in munitions, it can only be measured by high precision MC-ICP-MS and thus has not previously been measured in research on GWI.
We applied this approach to our representative sample of Gulf War veterans in the context of prior studies7,15,28 of groups of U.S. civilians exposed to DU (and EU) aerosol pollution in New York State from a uranium fabrication plant in the 1960s and 1970s29 and in part studied with MC-ICP-MS of urine samples using the same methods as in our study7. These studies demonstrated that significant doses of DU aerosols inhaled by factory workers and residents living nearby can be detected in urine ≥ 25 years after the plant was closed7,28, broadly consistent with predictions of the HRTM model.
In the bivariate plot in Fig. 2f, an individual excreting pure NU would be located at the point where 235U/238U = 0.00726 and 236U/238U = 0, reflecting the usual amount of 235U and the absence of 236U in natural U. A theoretical individual excreting pure DU would be located at a point defined by 235U/238U ≈ 0.002 and 236U/238U ≈ 0.00003, but most DU-exposed workers excrete a combination of DU and NU, which displaces them downward and to the right; whereas, EU added to the mix would displace them upward and to the right. Using published analyses of workers from the plant, mixtures of NU and DU had lower 235U and higher 236U, locating them along the solid line. Mixtures of NU and EU would have 235U/238U above that of NU (235U/238U > 0.00726), indicating substantially increased 235U, and variably increased 236U. Mixtures of NU, DU and EU would appear along the dashed line in the diagram.
Published studies of the DU plant workers and local town residents with proven non-military DU aerosol exposure7,28 are shown to illustrate where subjects with proven inhalation exposure to DU typically fall. All but 6 of the Gulf War veterans in our study are located in a narrow zone located exactly at 235U/238U = 0.00726, the value of natural U, and with 236U/238U ratios within the uncertainty zone around 236U/238U = 0 (Fig. 2f). The 6 exceptions have slightly elevated 236U/238U ratios and values of the 235U/238U incompatible with both DU and EU, indicating an artefact of measurement from organic molecule interference in these samples (see explanation in Supplemental materials, mass spectrometry).
Veteran with a Level I battlefield exposure and DU shrapnel wound
One Gulf War veteran in our study was standing on an Abrams tank when it was hit in a “friendly fire” accident by a DU round which destroyed the tank, threw the individual several meters, peppered him with a mix of sand, pebbles and shrapnel, tattooing his skin and embedding 2 pea-sized pieces of DU shrapnel under his skin. He breathed the hot gases from the explosion for several minutes. Upon return to his base in the U.S. 4 months later, the shrapnel was removed. During his wartime deployment to the war theatre, however, he was also exposed to low-level sarin nerve agent, took pyridostigmine tablets, and has moderately low PON1 type Q isoenzyme level, which are typical risk factors for GWI30–32. The veteran had symptoms satisfying the case definitions of GWI, subclassified as variant syndrome 1 (“cognitive impairment”), but his urine showed a total [U] of 1.35 ng/g creatinine, a 238U/235U ratio of 137.8, and a 236U/238U ratio below detection limit (< 0.000001)—all typical of natural U with no DU. If residual DU were present it was being excreted at a rate of < 0.068 ng/day, our limit of detection, and our prediction model indicates that he could have absorbed no more than 0.40 mg of DU from the Gulf War from both inhalation and DU shrapnel.
Discussion
Our findings, using high precision mass spectrometry MC-ICP-MS on chemically purified U that detects even the lowest level of DU exposure capable of causing illness, demonstrate that a sample of veterans drawn from a large population-representative sample of Gulf War veterans, meeting the case definitions of GWI and reporting a range of inhalation exposures to DU in friendly fire accidents, did not absorb even the smallest amount of DU capable of producing chronic adverse effects on health. The past studies of DU in Gulf War veterans have shown clear evidence of DU absorption into the body only in individuals with chunks of DU in metallic form as shrapnel retained in tissues from friendly fire wounds. The methods of detecting DU used in those studies—total [U] and limited use of U isotope ratios measured by the less precise SF-ICP-MS mass spectroscopy method—however, had insufficient precision to differentiate the lower levels of DU absorption likely with inhalation exposures from dietary NU absorption. Moreover, no past study has tested the association of urinary DU excretion measurements with GWI defined by the standard case definitions. Consequently, past studies did not address the question more widely concerning to Gulf War veterans and others of whether inhalation of DU in the war caused, or contributed to, the GWI. Our study, however, found no DU excretion in either veterans meeting the case definitions of GWI or control veterans not meeting them. Given the high precision of our methods, our results not only show an absence of evidence for an association but evidence for the absence of that association.
The element of our study design that gives meaning to a negative finding is that we first developed estimates of the amount of DU that would still be excreted in urine 18 years after exposure to amounts of DU found through simulation studies to result from various situations where soldiers inhaled DU oxides from explosions of DU munitions. We then tested urine from a representative sample of ill and well Gulf War veterans with the high precision mass spectrometry method, not used in prior testing of large samples of veterans, that is capable of detecting the levels of DU excretion predicted by the model. We based the predictions on the best estimates of the bodily absorption of DU that results from various exposure events and the modelling on the most widely accepted approach of the International Commission on Radiological Protection’s (ICRP) Human Respiratory Tract Model8,23,24. This study design provided the best chance of finding evidence of DU exposure if it exists but also provides a high degree of confidence in a negative finding as well.
A limitation of our study is that we included only Gulf War-era veterans who were potentially exposed to inhalation of DU from infrequent, very brief, though often intense, friendly fire accidents and sporadic inhalation of dust potentially contaminated with DU particulates over a 4–5 month period. While study of these Gulf War veterans addresses the question of whether short-term and potentially intense inhalation exposures produce enough systemic absorption to cause chronic illness, it may not adequately address the wider implications of decades of continuous exposure to DU-containing dust faced by the populations in war zones where DU munitions have been deployed. The design of our study applying high precision mass spectroscopy to urine samples could readily be adapted to study residents of former war zones to identify ongoing DU excretion as a quantitative biomarker of true DU absorption. Any effects of this exposure on health could then be addressed with clinical studies comparing sensitive measures of adverse health effects in persons with DU-positive and DU-negative test results.
For now, however, Gulf War veterans need no longer be concerned that a connection between their chronic illnesses and DU exposure in the Gulf War has been inadequately addressed by insensitive methods of measuring DU excretion and studies not relating DU measurements directly to GWI. If DU had been an important cause of GWI, our study, applying the most precise measure of DU to a representative sample of Gulf War veterans meeting the standard case definitions, was sensitive enough to have found it. From our negative results, we conclude that inhalation of DU during the Gulf War was not an important contributor to the GWI. Now scientific attention must be focused even more intensely on the remaining likely causes, particularly the widespread exposure to cholinesterase-inhibiting toxicants including low-level sarin nerve gas known to have been widely dispersed during destruction of chemical weapons stores by Allied bombing of Iraqi chemical weapons storage depots32,33, as well as pesticides and pyridostigmine, for which considerable evidence exists31.
Methods
Subjects
The 154 Gulf War-era U.S. military veterans who participated in this study were selected by a 3-stage statistical sampling plan as a representative sample of those who served in the U.S. armed forces during the 1991 Persian Gulf War, the target population. The first stage involved a computer-assisted telephone interview (CATI) survey of a stratified random sample of the target population, known as the U.S. Military Health Survey (USMHS). The sample was selected from the computer personnel file of the Gulf War-era military population between August 2, 1990 and July 1, 1991, obtained from the Defense Manpower Data Center (DMDC, Seaside, CA), stratified by the following design parameters: a flag indicating deployment to the Kuwaiti Theatre of Operations (KTO), age (< 49 years, ≥ 49 years), sex, race/ethnicity (non-Hispanic white, other), military rank during the war (officer, enlisted), military component (active duty, Reserve/Guard), military occupation (air flight crew, aircraft maintenance, army special operations, other), location in KTO on 20 January 1991 (deployed only), and 3 special study samples (twin pairs, member of 24th Reserve Naval Mobile Construction Battalion, and parent of a child with Goldenhar complex birth defect). Of the full USMHS sample (n = 8020), 6497 were deployed to the KTO, and 1523 were non-deployed. With 74.9% of the selected veterans located and contacted and 80.2% of these agreeing to participate, the overall response rate was 60.1%. The methods, extensive pilot testing and initial findings of the USMHS were described in detail elsewhere25.
The standardized interview included questions on specific in-theatre scenarios previously defined by the U.S. Army’s DU Capstone project for calculating the 4 levels of DU exposure recommended for epidemiologic studies by6,8. It also contained all questions required to define the 3 most often used case definitions of GWI: the Factor2, CDC26, and Modified Kansas27 definitions. The Factor case definition was developed with principal components analysis of symptom scales to identify groups of veterans with similar patterns related to deployment and was extensively validated25,34. All deployed personnel were present for the 5-week air war and the 5-day ground war in January and early February 1991.
The second stage involved selection of all veterans who met any of the 3 case definitions and an approximately 15% random sample of all who did not. The resulting sample included 2103 veterans, from whom samples of peripheral blood serum, plasma, DNA and RNA were collected by trained phlebotomists in or near subjects’ homes, shipped overnight to the UT Southwestern laboratory, and archived for later studies.
The third stage selected a subset (n = 154) of those who participated in the second stage and were randomly selected as a representative sample of Gulf War-era veterans with and without GWI. These were hospitalized between late 2008 and June 2010 in the UT Southwestern Medical Center’s Clinical and Translational Research Center for a 7-day research protocol involving 25 clinical neurological, neuroimaging, EEG and genetic studies of GWI. This protocol included the collection of a 24-h timed urine collection supervised and timed by professional research nurses in the hospital’s clinical research center. The urine samples were collected in urine collection bottles that had been pre-washed with an HCL solution to remove any trace of uranium. Urine samples thus post-date potential DU exposure by approximately 18 years. At the completion of collection, the volume of each 24 h urine sample was measured and recorded, and an aliquot was sent to Quest Laboratories for creatinine determination. The urine samples were then stored at 4 °C. In late 2017, a 500 ml aliquot was taken from each well shaken urine sample, and sent to the University of Portsmouth in the U.K. for uranium isotope analysis with generic sample numbers for blind analysis. All participants gave written informed consent according to a protocol approved by the institutional review board of the University of Texas Southwestern Medical Center and methods followed relevant guidelines and regulations.
Calculation of inhalation exposure and excretion of inhaled uranium
The predictions of urinary DU concentrations from DU absorbed 18 years earlier, shown in Fig. 1, are based on information in the annexes to the comprehensive study by the Royal Society report on DU [annexes C, G, H of 8; 22,24]. These sources describe the absorption of inhaled material from the respiratory tract and how this can be modelled in terms of accumulation in kidney and bone and excretion in urine over time, dependent upon the type and solubility of uranium oxide particles. These are based upon the Human Respiratory Tract Model (HRTM) of the International Commission on Radiological Protection23 and8, the latter providing available information on absorption characteristics (i.e. lung solubility) of particulate DU from DU penetrator impact and combustion in fires. Because relatively insoluble UO2 and U3O8 are the predominant oxides from DU6,35, they have the slowest dissolution rate constants, approximately 0.0012–0.00035 and 0.0015–0.00049 for U3O8 and UO2, respectively.
The modelling8,24 using the Human Respiratory Tract Model23 is shown in Fig. 1 for inhalation of U oxides of various types and illustrates daily excretion as a fraction of the original intake as a function of time. The red box of Fig. 1 uses 18.4 ± 1.0 years as the duration between inhalation and urine collection, and the fractional excretion of inhaled DU is 1.7 ± 1.2 × 10–7. An analogous blue box is shown for the Dorsey et al. study20. Using a range of initial inhalation doses of DU from 250 down to 2 mg, we calculated the DU excretion during the time window of urine collection and added two contrasting ranges of daily dietary excretion of natural U of 2 and 8 ng/day of U. For these calculations the 238U/235U and 236U/238U for DU were 500 and 30 × 10–6, and for natural U 137.82 and 0, respectively. From these excretion rates, we calculated (Supplemental Material, indicative calculation) the fractional amount of DU in urine, and the corresponding isotope ratios of 238U/235U and 236U/238U; this allows assessment of measurement capabilities and limits of detection for DU for our method and that of all previous urinary U isotope measurements of US Gulf War veterans20, which used a less sensitive SF-ICP-MS methodology.
The predicted isotope ratios 238U/235U and 236U/238U were calculated from Eqs. (1) and (2), using end member DU of 238U/235U = 500 and 236U/238U = 30 × 10–6, (2) NU 238U/235U = 137.82 and 236U/238U = 0, and the fraction of excretion that is DU (fDU).
| 1 |
| 2 |
The sensitivity threshold for positive detection of DU using 238U/235U measurements was 139–140 for our method (described below) and 166 according to the methods used by20. Because we could not detect DU if its proportion was < 2%, corresponding to a 238U/235U of 140, we calculate that based on the mean rate of excretion of 3.4 ng/day, the maximum amount of DU excreted would be < 0.068 ng/day. Using the HRTM-based calculation, this leads to a maximum inhalation dose 0.4+1.0/−0.2 mg during the Gulf War.
Chemical and isotope measurement procedures
Samples were measured blind at the University of Portsmouth in that they had generic sample numbers without any information as to subject criteria in terms of deployed, not deployed, Gulf War Illness positive or negative—information which was confidentially retained at the University of Texas Southwestern Medical Center. Upon receipt of samples at the University of Portsmouth, weights of samples were measured and stored for subsequent analysis in a restricted access class 100 laboratory. The general procedures used to measure the concentration and isotope composition of uranium from urine are adapted from prior publications7,36 and followed methods in accordance with regulations. Particular variations to published methods are described below and in the Supplemental Material. The procedure involved a full chemical separation and purification of uranium extracted by calcium phosphate co-precipitation from 150 ml of urine using pre-cleaned reagents (see Supplemental Material, reagents) in a class-100 clean laboratory and multiple collector inductively coupled plasma mass spectrometry (MC-ICP-MS). The study used a Nu Instruments MC-ICP-MS with multiple faraday and ion counting detectors, extensive analysis of a 2 ng/g solution of certified IRMM184 (Institute of Reference Materials and Measurement, Geel, Belgium) uranium solution almost identical with natural uranium to which a high isotopic purity 233U tracer was added (238U/233U ~ 100), repeated analysis of an in-house urine to which IRMM184 was partly added, and routine measurement of mass 237 important for making time-dependent corrections to 236U/238U related to mass abundance sensitivity (down-mass tailing corrections) arising from pressure variations within the mass spectrometer and trace amounts of organic molecular ion interference at masses 236.8 and 235.8 (Supplemental Material, mass spectrometry). The method resulted in a LOD on the 236U/238U of 0.000015 or 11 counts/sec on the 236 mass. The uranium introduced during the chemical procedure was 11–38 pg averaging 8–12 pg during each batch. Once all of these corrections were made, the analyses of the IRMM184 reference solution yielded 234U/238U, 235U/238U and 236U/238U values of 5.344 × 10–5 ± 2.0 × 10–6, 0.0072614 ± 0.0000025 and 1.1 × 10–7 ± 0.1 × 10–7, respectively, in agreement with the certified values. The mean 235U/238U measurement uncertainty and its standard deviation for 154 sample and 125 IRMM184 measurements was 0.66 ± 0.46% and 0.44 ± 0.19%, respectively, with individual analyses available in Supplemental Material Tables S3 and S4.
Supplementary Information
Acknowledgements
The U.S. Military Health Survey in a representative sample of Gulf War-era veterans and the followup nested case–control studies in which the participants of this study were recruited and studied were planned under Grant DAMD17-01-1-0741 from the US Army Medical Research and Materiel Command. The epidemiologic and clinical data and the urine samples analysed in this study were collected under funding through the Indefinite Delivery Indefinite Quantity contract VA549-P-0027, awarded and administered by the Department of Veterans Affairs Medical Center, Dallas, Texas, and by Grant UL1RR024982-05, titled North and Central Texas Clinical and Translational Science Initiative, to UT Southwestern Medical Center from the National Center for Research Resources, a component of the National Institutes of Health (NIH) and NIH Roadmap for Medical Research. A research proposal, approved by the local Merit Review Committee and Institutional Review Board in 2009, for uranium isotope measurement of the urine samples by high precision MC-ICP-MS was rejected by the Department of Veterans Affairs because funding was contingent on use of the lower precision SF-ICP-MS used in prior and ongoing U.S. Government studies. Consequently, measurements of U isotope ratios by high precision MC-ICP-MS were funded by departmental support from the School of Earth and Environmental Sciences, University of Portsmouth. Manuscript writing was supported in part by the Perot Foundation of Dallas. The content does not necessarily reflect the position or the policy of the U.S. federal government or the sponsoring agencies, and no official endorsement should be inferred.
Author contributions
R.R.P. developed the analytical procedures, refined methods of mass spectrometry for these samples, conducted all of the chemical extractions and mass spectrometric measurements. R.W.H. designed the GWI study and Gulf War veteran sample selections, and obtained and provided aliquots of urine samples. R.R.P. and R.W.H. co-wrote the manuscript.
Funding
The funding agencies had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript. Gerald Kramer assisted with sample archiving and aliquoting at UT Southwestern Medical Center, and J Dunlop is thanked for help with NuPlasma MC-ICP-MS mass spectrometry at Portsmouth. Parrish thanks S. Noble, M. Horstwood and N. Atkinson of the British Geological Survey for advice in the analysis of samples. A large research team of survey specialists at RTI International contributed importantly to the design and performed the field work for the national CATI survey of Gulf War era veterans. Research leaders included Kathleen A. Considine, Vincent G. Iannacchione, Jill A. Dever, Christopher P. Carson, Heather Best, Carla Bann, Darryl Creel, Barbara Alexander, Amanda Lewis-Evans, Lily Trofimovich, Kirk Pate, Anne Kenyon, Jeremy Morton, Craig Hill and Robert E. Mason.
Competing interests
The authors declare no competing interests.
Footnotes
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
The online version contains supplementary material available at 10.1038/s41598-021-82535-3.
References
- 1.Research Advisory Committee on Gulf War Veterans' Illnesses. Gulf War Illness and the Health of Gulf War Veterans: Scientific Findings and Recommendations.https://www.va.gov/RAC-GWVI/docs/Committee_Documents/GWIandHealthofGWVeterans_RAC-GWVIReport_2008.pdf (2008).
- 2.Haley RW, Kurt TL, Hom J. Is there a Gulf War syndrome? Searching for syndromes by factor analysis of symptoms. J. Am. Med. Assn. 1997;277:215–222. doi: 10.1001/jama.1997.03540270041025. [DOI] [PubMed] [Google Scholar]
- 3.Haley RW, et al. Cholinergic autonomic dysfunction in veterans with Gulf War illness: Confirmation in a population-based sample. J. Am. Med. Assn. Neurol. 2013;70:191–200. doi: 10.1001/jamaneurol.2013.596. [DOI] [PubMed] [Google Scholar]
- 4.Haley RW, et al. Abnormal brain response to cholinergic challenge in chronic encephalopathy from the 1991 Gulf War. Psychiatry Res. 2009;171:207–220. doi: 10.1016/j.pscychresns.2008.05.004. [DOI] [PubMed] [Google Scholar]
- 5.McDiarmid MA, et al. The US Department of Veterans' Affairs depleted uranium exposed cohort at 25 years: Longitudinal surveillance results. Environ. Res. 2017;152:175–184. doi: 10.1016/j.envres.2016.10.016. [DOI] [PubMed] [Google Scholar]
- 6.Parkhurst, M. A. et al. Capstone Depleted Uranium Aerosols: Generation and Characterization, Pacific Northwest National Laboratory-14168. https://www.pnnl.gov/main/publications/external/technical_reports/PNNL-14168.pdf (2004).
- 7.Parrish RR, et al. Depleted uranium contamination by inhalation exposure and its detection after approximately 20 years: Implications for human health assessment. Sci. Total Environ. 2008;390:58–68. doi: 10.1016/j.scitotenv.2007.09.044. [DOI] [PubMed] [Google Scholar]
- 8.Royal Society. The health hazards of depleted uranium munitions: Part I (2001).
- 9.Bruess, E. & Snell, J. War and the environment: The disturbing and under-researched legacy of depleted uranium weapons. Bull At Sci. https://thebulletin.org/2020/07/war-and-the-environment (2020).
- 10.Faa A, et al. Depleted uranium and human health. Curr. Med. Chem. 2018;25:49–64. doi: 10.2174/0929867324666170426102343. [DOI] [PubMed] [Google Scholar]
- 11.ANSA (Agenzia Nazionale Stampa Associata). Depleted Uranium Caused Italy Soldiers' Cancer—Probe. https://www.ansa.it/english/news/2018/02/07/depleted-uranium-caused-italy-soldiers-cancer-probe_3bfc785c-4e95-4bd1-975a-79fb167a9188.html (2018).
- 12.Telegraph. Soldier Died from Exposure Depleted Uranium During Gulf War. https://www.telegraph.co.uk/news/uknews/defence/6168039/Soldier-died-from-exposure-depleted-uranium-during-Gulf-War.html (2009).
- 13.Laboratory PNN. Camp Doha Report. Washington, DC: U.S. Department of Defense; 2000. [Google Scholar]
- 14.Hiess J, Condon DC, McLean N, Noble SR. 238U/235U systematics in terrestrial uranium-bearing minerals. Science. 2012;335:1610–1614. doi: 10.1126/science.1215507. [DOI] [PubMed] [Google Scholar]
- 15.Lloyd NS, Parrish RR, Horstwood MSA, Chenery SR. Precise and accurate isotopic analysis of microscopic uranium-oxide grains using LA-MC-ICP-MS. J. Anal. Atom. Spectrom. 2009;24:752–758. doi: 10.1039/b819373h. [DOI] [Google Scholar]
- 16.Lloyd NS, Chenery SR, Parrish RR. The distribution of depleted uranium contamination in Colonie, NY, USA. Sci. Total Environ. 2009;408:397–407. doi: 10.1016/j.scitotenv.2009.09.024. [DOI] [PubMed] [Google Scholar]
- 17.Oliver IW, Graham MC, MacKenzie AB, Ellam RM, Farmer JG. Assessing depleted uranium (DU) contamination of soil, plants and earthworms at UK weapons testing sites. J. Environ. Monit. 2007;9:740–748. doi: 10.1039/b700719a. [DOI] [PubMed] [Google Scholar]
- 18.National Center for Environmental Health. Third National Report on Human Exposure to Environmental Chemicals. https://clu-in.org/download/contaminantfocus/pcb/third-report.pdf (2005).
- 19.Ting BG, et al. Uranium and thorium in urine of United States residents: Reference range concentrations. Environ. Res. 1999;81:45–51. doi: 10.1006/enrs.1998.3951. [DOI] [PubMed] [Google Scholar]
- 20.Dorsey CD, Engelhardt SM, Squibb KS, McDiarmid MA. Biological monitoring for depleted uranium exposure in US Veterans. Environ. Health Perspect. 2009;117:953–956. doi: 10.1289/ehp.0800413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McDiarmid MA, et al. Surveillance results of depleted uranium-exposed Gulf War I veterans: Sixteen years of follow-up. J. Toxicol. Environ. Health Part A. 2009;72:14–29. doi: 10.1080/15287390802445400. [DOI] [PubMed] [Google Scholar]
- 22.WHO (World Health Organisation). Depleted uranium: Sources, Exposure and Health Effects. Geneva World Health Organization. https://apps.who.int/iris/handle/10665/66930 (2001).
- 23.Bair WJ, et al. Human respiratory tract model for radiological protection. A report of a Task Group of the International Commission on Radiological Protection. Ann. ICRP. 1994;24:1–482. doi: 10.1016/0146-6453(94)90029-9. [DOI] [PubMed] [Google Scholar]
- 24.Etherington, G. The Solubility of Inhaled DU and Its Influence on Urine Excretion. Depleted Uranium Oversight Board. https://drive.google.com/file/d/1Z56XXc51IAUw8qWwMetPOIhPedLWBuVO/view?usp=sharing (2004).
- 25.Iannacchione VG, et al. Validation of a research case definition of Gulf War illness in the 1991 US military population. Neuroepidemiology. 2011;37:129–140. doi: 10.1159/000331478. [DOI] [PubMed] [Google Scholar]
- 26.Fukuda K, et al. Chronic multisymptom illness affecting Air Force veterans of the Gulf War. J. Am. Med. Assn. 1998;280:981–988. doi: 10.1001/jama.280.11.981. [DOI] [PubMed] [Google Scholar]
- 27.Steele L. Prevalence and patterns of Gulf War illness in Kansas veterans: Association of symptoms with characteristics of person, place, and time of military service. Am. J. Epidemiol. 2000;152:992–1002. doi: 10.1093/aje/152.10.992. [DOI] [PubMed] [Google Scholar]
- 28.Arnason JG, Pellegri CN, Moore JL, Lewis-Michl EL, Parsons PJ. Depleted and enriched uranium exposure quantified in former factory workers and local residents of NL Industries, Colonie, NY USA. Environ. Res. 2016;150:629–638. doi: 10.1016/j.envres.2016.04.006. [DOI] [PubMed] [Google Scholar]
- 29.Agency for Toxic Substances and Disease Registry. Health Consultation: Colonie site, Albany County, New York. https://www.atsdr.cdc.gov/HAC/pha/ColonieSite100504-NY/ColonieSite100504HC-NY.pdf (2004).
- 30.Haley RW, Billecke S, La Du BN. Association of low PON1 type Q (type A) arylesterase activity with neurologic symptom complexes in Gulf War veterans. Toxicol. Appl. Pharmacol. 1999;157:227–233. doi: 10.1006/taap.1999.8703. [DOI] [PubMed] [Google Scholar]
- 31.Michalovicz LT, Kelly KA, Sullivan K, O'Callaghan JP. Acetylcholinesterase inhibitor exposures as an initiating factor in the development of Gulf War Illness, a chronic neuroimmune disorder in deployed veterans. Neuropharmacology. 2020;171:108073. doi: 10.1016/j.neuropharm.2020.108073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tuite JJ, Haley RW. Meteorological and intelligence evidence of long-distance transit of chemical weapons fallout from bombing early in the 1991 Persian Gulf War. Neuroepidemiology. 2013;40:160–177. doi: 10.1159/000345123. [DOI] [PubMed] [Google Scholar]
- 33.Haley RW, Tuite JJ. Epidemiologic evidence of health effects from long-distance transit of chemical weapons fallout from bombing early in the 1991 Persian Gulf War. Neuroepidemiology. 2013;40:178–189. doi: 10.1159/000345124. [DOI] [PubMed] [Google Scholar]
- 34.Haley RW, Luk GD, Petty F. Use of structural equation modeling to test the construct validity of a case definition of Gulf War syndrome: Invariance over developmental and validation samples, service branches and publicity. Psychiatry Res. 2001;102:175–200. doi: 10.1016/S0165-1781(01)00241-4. [DOI] [PubMed] [Google Scholar]
- 35.Lloyd NS, et al. The morphologies and compositions of depleted uranium particles from an environmental case-study. Mineral. Mag. 2009;73:495–510. doi: 10.1180/minmag.2009.073.3.495. [DOI] [Google Scholar]
- 36.Parrish RR, et al. Determination of MC-ICP-MS 238U/235U, 236U/238U and uranium concentration in urine using SF-ICP-MS and MC-ICP-MS: An interlaboratory comparison. Health Phys. 2006;90:127–138. doi: 10.1097/01.HP.0000174809.43871.54. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.