Abstract
Background
Appendicectomy is a common emergency operation. The aim of this analysis was to study the effect of preoperative delay on disease progression, and whether a novel scoring system (Atema score) could be useful in predicting complicated appendicitis.
Methods
Patients with uncomplicated acute appendicitis on CT and who underwent appendicectomy in 2014–2015 were analysed for patient characteristics, preoperative delay and outcomes.
Results
Of 837 patients with uncomplicated appendicitis on CT, 187 (22.3 per cent) were found to have complicated appendicitis at surgery. The median time estimate for perforation was 25.4 h after CT, with an hourly rate of perforation of 2 per cent. Patients with an Atema score of 6 or less and those with no appendicolith on CT and a C-reactive protein level below 51 mg/l were the slowest to develop perforation, reaching a perforation rate of 5 per cent in 7.1 and 7.6 h respectively.
Conclusion
A substantial proportion of patients with uncomplicated acute appendicitis on CT have complicated appendicitis at surgery. However, in patients with no risk factors, surgery can be postponed safely for up to 7 h.
Of a total of 837 patients with uncomplicated appendicitis diagnosed on CT, 187 (22.3 per cent) were found to have complicated appendicitis at surgery. The median time estimate for perforation was 25.4 h after CT, with an hourly rate of perforation of 2 per cent. Patients with low Atema score, low C-reactive protein level and no appendicolith had lower perforation rates.
Resumen
Antecedentes
La apendicectomía es una operación que frecuentemente se practica con carácter de urgencia. El objetivo de este análisis fue estudiar el efecto del retraso preoperatorio sobre la progresión de la enfermedad y si un nuevo sistema de puntuación (puntuación Atema) podría ser útil para predecir la apendicitis complicada.
Métodos
Se analizaron las características, el retraso preoperatorio y los resultados de los pacientes con apendicitis aguda no complicada diagnosticados mediante tomografía computarizada (TC) y sometidos a apendicectomía durante los años 2014-2015.
Resultados
De los 837 pacientes con apendicitis no complicada en la tomografía computarizada, se encontró que 187 (22,3%) tenían apendicitis complicada en la cirugía. La mediana de tiempo estimado para la perforación fue de 25,4 horas después de la tomografía computarizada, con una tasa de perforación por hora del 2%. Los pacientes con puntuación de Atema ≤ 6 y los pacientes sin apendicolito en la TC y un valor de la PCR < 50 mg/L fueron los más lentos en desarrollar la perforación, alcanzando una tasa de perforación del 5% en 7,1 horas y 7,6 horas, respectivamente.
Conclusión
Una proporción sustancial de pacientes con apendicitis aguda no complicada en las imágenes de TC tienen apendicitis complicada durante la cirugía. Sin embargo, en pacientes sin factores de riesgo, la cirugía puede posponerse de forma segura hasta 7 horas.
Introduction
When simple appendicitis proceeds to perforation, the prognosis worsens significantly, predisposing the patient to a prolonged hospital stay, use of broad-spectrum antibiotics, and increased morbidity. Traditionally, early appendicectomy has been accepted as the optimal approach to prevent perforation, and a low level of perforation in an institution has been viewed as a sign of high-quality care, based on an assumption that the in-hospital delay from admission to operation influences the incidence of perforation.
It is widely recognized that increasing delay from the onset of symptoms to operation leads to a higher incidence of perforation1–5, and that most perforations have already occurred by the time the patient arrives at the hospital2,5,6. A meta-analysis7 of 152 314 patients concluded that delaying appendicectomy for presumed uncomplicated appendicitis for up to 24 h does not increase the risk of complicated appendicitis, surgical-site infection or morbidity. In contrast, it was found that in children with uncomplicated appendicitis on CT a delay of more than 9 h from CT to surgery resulted in a 6-fold increase in perforation compared with a shorter delay8. As non-operative treatment of uncomplicated appendicitis has increased in popularity, the accuracy of CT in differentiating uncomplicated from complicated appendicitis has become an important guide to management9,10. The only available meta-analysis11 found 10 informative CT features, nine of which showed high specificity but low sensitivity, making them unsafe in determining which patients might be treated conservatively. In 2015, Atema and colleagues12 published a scoring system (referred to here as the Atema score) to calculate the probability of complicated appendicitis according to clinical assessment, laboratory parameters, and features on either ultrasound imaging or CT, in the hope that this might prove more reliable in predicting complicated appendicitis than CT alone.
The aim of the present study was to investigate the length of time for which adults with uncomplicated acute appendicitis on CT might safely wait for their operation without risk of perforation, and whether the Atema score could provide additional value for these patients.
Methods
This was an observational cohort study performed in two major abdominal surgery departments at Helsinki University Hospital. The study was approved by the institutional review board (reference number 9/2016).
All patients aged 18 years or above with Nordic Medico-Statistical Committee (NOMESCO) classification codes JEA00 or JEA01 and a diagnosis of acute appendicitis (ICD-10 code K35.X) presenting between January 2014 and December 2015 were identified from an electronic database of surgical operations. Hospital records of these patients were examined manually. Data regarding demographics, laboratory parameters, vital signs, clinical status, CT findings, preoperative and postoperative antibiotic treatments, intraoperative findings, histopathological findings, length of symptoms, length of time between CT and operation, length of stay and postoperative complications were obtained from electronic patient records.
Abdominal CT was performed with intravenous contrast. Several different multidetector CT devices were used, partly because some patients had already been scanned before arriving at the operating hospital. Images were not reanalysed for this study, although special attention was paid to terms indicative of perforation or abscess.
The Atema score was calculated for each patient; scoring points are shown in Table 1. The maximum score is 22 points; the higher the score, the greater the probability of complicated appendicitis, and a score of 0–6 is considered indicative of uncomplicated appendicitis.
Table 1.
The Atema score for clinical and CT features
| Points scored | |
|---|---|
| Age ≥ 45 years | 2 |
| Body temperature (°C) | |
| ≤37.0 | 0 |
| 37.1–37.9 | 2 |
| ≥38.0 | 4 |
| Duration of symptoms ≥ 48 h | 2 |
| WBC count > 13×109/l | 2 |
| C-reactive protein (mg/l) | |
| ≤50 | 0 |
| 51–100 | 2 |
| >100 | 3 |
| Extraluminal free air on CT | 5 |
| Periappendiceal fluid on CT | 2 |
| Appendicolith on CT | 2 |
| Maximum score | 22 |
WBC, white blood cell.
In the present study, uncomplicated appendicitis was defined as simple or gangrenous without perforation, similar to American Association for the Surgery of Trauma (AAST) grades I and II13. Appendicitis with perforation or abscess formation was defined as complicated appendicitis (AAST grades III– V). Additional appendicular conditions such as benign or malignant tumours did not affect this categorization. Pre-CT delay was defined as the time from the symptom onset to CT. Preoperative delay was defined as the time from CT to surgery. The total time delay is the combination of these two time intervals. Postoperative complications occurring during the 30-day period after operation were recorded and categorized using the Clavien–Dindo classification14.
Statistical analysis
Categorical risk factors for complicated appendicitis were analysed; the χ2 test was performed, and odds ratios (ORs) with 95 per cent c.i. were calculated. For continuous variables, a receiver operating characteristic (ROC) curve analysis was performed, the area under ROC curve (AUROC) with 95 per cent c.i. was reported, and P values were obtained using the Mann–Whitney U test.
The impact of the preoperative delay on complications was determined by using the Kaplan–Meier analysis. The time of the start of the operation was used to represent the time of perforation, because the exact time of perforation was impossible to know. After categorizing patients according to different risk factors, Kaplan–Meier analysis with the log rank pairwise comparison test was used. A multivariable analysis was undertaken using the Cox regression model to assess the effect of different risk factors on complications during the preoperative delay. Statistical analysis was done with SPSS® Statistics version 25 (IBM, Armonk, NY, USA).
Results
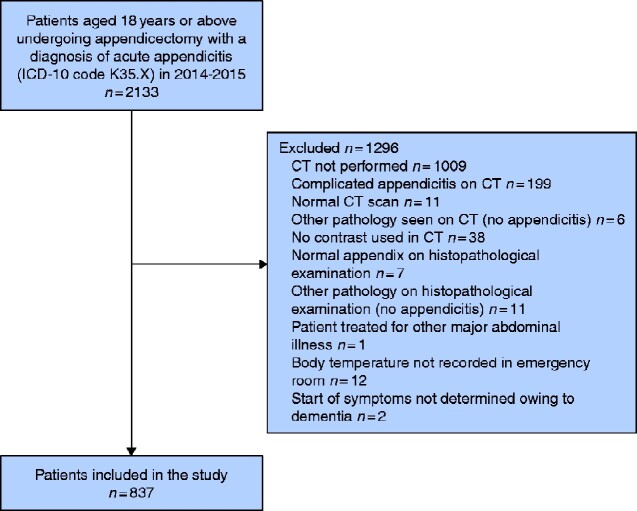
Of 2133 patients operated on for acute appendicitis, 1009 who did not undergo CT and 199 who had complicated appendicitis diagnosed by CT were excluded. Of the remainder, a further 88 patients were excluded for the reasons shown in Fig. 1, leaving a total of 837 patients with uncomplicated appendicitis on CT who subsequently underwent appendicectomy with a diagnosis of appendicitis. Some 685 patients (81.8 per cent) were operated on laparoscopically.
Fig. 1.
Flow diagram of patient inclusion in the study
There were 402 men (48.0 per cent) and 435 women (52.0 per cent). The median age was 47 (i.q.r. 33–60) years. All 837 patients were considered to have uncomplicated appendicitis according to the CT findings. At operation, 187 patients (22.3 per cent) had complicated appendicitis. Of 537 patients with no risk factors on CT, 75 (14.0 per cent) had complicated appendicitis. Demographics and risk factors for perforation are shown in Table 2. All risk factors included in the Atema score were associated with complicated appendicitis. An Atema score greater than 6 was best at differentiating uncomplicated and complicated appendicitis, although the sensitivity for complicated appendicitis was only 69.0 (95 per cent c.i. 65.9 to 72.3) per cent and specificity was 71.8 (68.8 to 75.0) per cent.
Table 2.
Basic demographics and risk factors for complicated appendicitis
| Uncomplicated appendicitis (n = 650) | Complicated appendicitis (n = 187) | AUROC† | Odds ratio† | P § | |
|---|---|---|---|---|---|
| Age (years)* | 44 (33–56) | 55 (41–67) | 0.655 (0.610, 0.700) | < 0.001¶ | |
| Age 45 years or more | 321 (49.4) | 131 (70.1) | 2.40 (1.69, 3.40) | < 0.001 | |
| Male sex | 314 (48.3) | 88 (47.1) | 0.95 (0.69, 1.32) | 0.763 | |
| Laparoscopic surgery | 542 (83.4) | 143 (76.5) | 0.65 (0.44, 0.96) | 0.031 | |
| Pre-CT delay (h)* | 28.7 (16.5–45.4) | 38.6 (24.6–58.2) | 0.632 (0.586, 0.678) | < 0.001¶ | |
| Preoperative delay (h)* | 9.3 (5.5–14.2) | 7.8 (4.8–12.9) | 0.446 (0.400, 0.493) | 0.026¶ | |
| Total delay (h)* | 38.7 (27.1–55.7) | 50.6 (34.3–69.8) | 0.620 (0.574, 0.667) | < 0.001¶ | |
| Pre-CT delay over 48 h | 154 (23.7) | 81 (43.3) | 2.46 (1.75, 3.46) | < 0.001 | |
| Appendicolith on CT | 159 (24.5) | 93 (49.7) | 3.06 (2.18, 4.28) | < 0.001 | |
| Periappendiceal fluid on CT | 40 (6.2) | 32 (17.1) | 3.15 (1.92, 5.18) | < 0.001 | |
| Extraluminal air on CT | 5 (0.8) | 6 (3.2) | 4.28 (1.29, 14.17) | 0.010 | |
| Any risk factor‡ on CT | 188 (28.9) | 112 (59.9) | 3.67 (2.62, 5.15) | < 0.001 | |
| No risk factor‡ on CT | 462 (71.1) | 75 (40.1) | 0.27 (0.18, 0.38) | < 0.001 | |
| WBC count (109/l)* | 12.0 (9.1–14.7) | 12.6 (9.8–15.8) | 0.559 (0.512, 0.607) | 0.013¶ | |
| WBC count >13×109/l | 256 (39.4) | 89 (47.6) | 1.40 (1.01, 1.94) | 0.044 | |
| CRP (mg/l)* | 35 (9–79) | 78 (37–158) | 0.696 (0.653, 0.739) | < 0.001¶ | |
| CRP >50 mg/l | 267 (41.1) | 123 (65.8) | 2.76 (1.96, 3.87) | < 0.001 | |
| CRP >100 mg/L | 105 (16.2) | 80 (42.8) | 3.88 (2.72, 5.55) | < 0.001 | |
| Body temperature (°C)* | 37.1 (36.7–37.5) | 37.5 (37.1–38.0) | 0.687 (0.643, 0.731) | < 0.001¶ | |
| Body temperature >37.0°C | 342 (52.6) | 141 (75.4) | 2.76 (1.91, 3.98) | < 0.001 | |
| Body temperature ≥38.0°C | 64 (9.8) | 56 (29.9) | 3.91 (2.61, 5.87) | < 0.001 | |
| Atema score* | 4 (4–7) | 9 (6–11) | 0.775 (0.736, 0.814) | < 0.001¶ | |
| Atema score >6 | 183 (28.2) | 129 (69.0) | 5.68 (3.98, 8.09) | < 0.001 | |
| Antibiotics started before entering theatre | 396 (60.9) | 155 (82.9) | 3.11 (2.06, 4.69) | < 0.001 | |
| Antibiotics administered >2 h before surgery | 369 (56.8) | 138 (73.8) | 2.15 (1.50, 3.08) | < 0.001 | |
| Time from CT to first antibiotic dose (h)* | 3.3 (1.8–6.6) | 2.2 (0.3–4.4) | 0.374 (0.327, 0.422) | < 0.001¶ | |
| Time from first antibiotic dose to surgery (h)* | 4.0 (0.0–10.0) | 4.4 (1.8–9.5) | 0.552 (0.509, 0.595) | 0.027¶ | |
| Proportion of time from start of antibiotics to surgery from preoperative delay (%)* | 56.6 (0–82.3) | 71.4 (37.3–93.0) | 0.627 (0.582, 0.672) | < 0.001¶ | |
| Transfer from another hospital for surgery | 124 (19.1) | 31 (16.6) | 0.843 (0.547, 1.299) | 0.438¶ |
Values in parentheses are percentages unless indicated otherwise;
*values are median (i.q.r.); †values in parentheses are 95 per cent confidence intervals.
‡Appendicolith, periappendiceal fluid or extraluminal air. AUROC, area under receiver operating characteristic (ROC) curve; WBC, white blood cell; CRP, C-reactive protein.
§Pearson’s χ2 test, except
¶Mann–Whitney U test.
Median pre-CT delay, preoperative delay and total delay was 30.1 (i.q.r. 17.5–50.7) h, 8.8 (5.4–13.9) h and 42.2 (28.4–60.0) h respectively. The delay from symptom onset to surgery was significantly longer in patients with complicated appendicitis. In contrast, the time interval from CT to operation was shorter in patients with complicated appendicitis. A number of risk factors were associated with perforation and with a shorter delay to operation (Table S1).
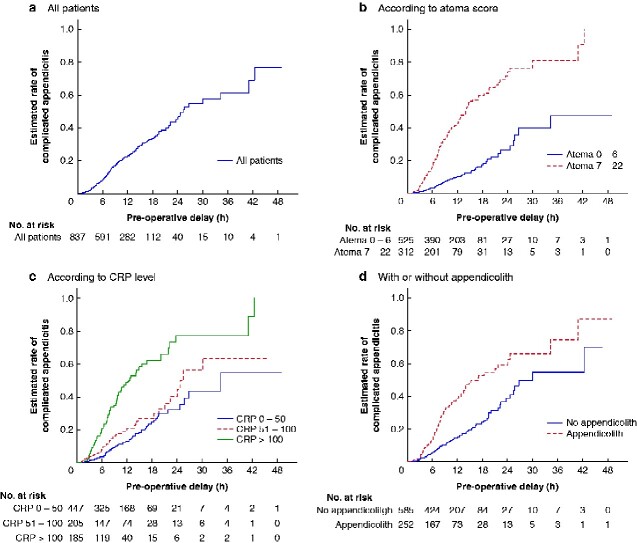
The median time estimate for perforation was 25.4 (95 per cent c.i. 21.1 to 29.7) h after CT (Fig. 2a). When patients were categorized according to the Atema score, the perforation rate was significantly lower in patients with a low Atema score (Fig. 2b). Patients with a C-reactive protein (CRP) level of 100 mg/l or less (Fig. 2c) and patients without an appendicolith on CT (Fig. 2d) had significantly reduced perforation rates.
Fig. 2.
Kaplan–Meier one minus survival curves estimating the rate of complicated appendicitis
a All patients; b patients according to Atema score 0-6 or 7-22; c patients divided according to C-reactive protein (CRP) level of 0-50, 51-100 or more than 100 mg/l; d patients with or without appendicolith on CT. b P<0.001; c P<0.001 (CRP >100 versus CRP 0-50 and CRP 51-100), P=0.044 (CRP 0-50 versus CRP 51-100); d P<0.001 (log rank test).
Of a total of 837 patients with uncomplicated appendicitis diagnosed on CT, 187 (22.3 per cent) were found to have complicated appendicitis at surgery. The median time estimate for perforation was 25.4 h after CT, with an hourly rate of perforation of 2 per cent. Patients with low Atema score, low C-reactive protein level and no appendicolith had lower perforation rates.
Kaplan–Meier analysis provided estimations of the preoperative delay for different proportions of complicated appendicitis. Table 3 shows time intervals for 5, 25 and 50 per cent rate estimates of complicated appendicitis. Patients with an Atema score of 6 or less, and those with an appendicolith on CT and a CRP level below 51 mg/l were slowest to develop perforation, reaching a perforation rate of 5 per cent in 7.1 and 7.6 h respectively.
Table 3.
Estimated preoperative delay until proportion with complicated appendicitis reached 5, 25 and 50 per cent, and perforation rate of appendicitis per h according to Kaplan–Meier analysis
| n | Estimated preoperative delay (h) |
Perforation rate (% per h) | |||
|---|---|---|---|---|---|
| 5% complicated appendicitis | 25% complicated appendicitis | 50% complicated appendicitis | |||
| All patients | 837 | 4.4 | 12.9 | 25.4 | 2 |
| Atema score ≤6 | 403 | 7.1 | 21.7 | – | 1 |
| Atema score >6 | 434 | 3.1 | 7.3 | 13.7 | 3 |
| CRP 0–50 mg/l | 447 | 6.8 | 17.7 | 26.7 | 1 |
| CRP 51–100 mg/l | 205 | 4.0 | 14.0 | 24.6 | 2 |
| CRP >100 mg/l | 185 | 3.1 | 7.1 | 12.2 | 3 |
| Appendicolith on CT | 252 | 3.2 | 7.8 | 15.3 | 3 |
| Appendicolith on CT and CRP >100 mg/l | 61 | 2.7 | 4.3 | 8.0 | 6 |
| No appendicolith on CT | 585 | 5.6 | 17.7 | 26.7 | 2 |
| No appendicolith on CT and CRP ≤100 mg/l | 461 | 6.9 | 19.5 | – | 1 |
| No appendicolith on CT and CRP ≤50 mg/l | 305 | 7.6 | 19.2 | – | 1 |
CRP, C-reactive protein.
Cox regression analysis showed that age over 60 years, pre-CT delay greater than 48 h, body temperature of 38.0°C or above, white blood cell count over 13×109/l, CRP concentration above 100 mg/l, periappendiceal fluid on CT, and appendicolith on CT were all independently associated with complicated appendicitis (Table 4). Increasing delay of antibiotic administration after CT had a lower hazard of developing complicated appendicitis.
Table 4.
Cox regression analysis of risk factors for complicated appendicitis
| Hazard ratio | P | |
|---|---|---|
| Age (years) | ||
| <45 | 1.00 (reference) | 0.004 |
| 45–60 |
1.45
(0.99, 2.12) |
0.055 |
| >60 |
1.85
(1.28, 2.66) |
0.001 |
| Pre-CT delay (h)* | ||
| <24 | 1.00 (reference) | < 0.001 |
| 24–48 |
0.97
(0.63, 1.48) |
0.877 |
| >48 |
2.05
(1.32, 3.20) |
0.001 |
| Body temperature (°C) | ||
| ≤37.0 | 1.00 (reference) | < 0.001 |
| 37.1–37.9 |
1.51
(1.04, 2.20) |
0.029 |
| ≥38.0 |
2.38
(1.56, 3.65) |
< 0.001 |
| WBC count > 13×109/l |
1.40
(1.03, 1.88) |
0.030 |
| C-reactive protein (mg/l) | ||
| ≤50 | 1.00 (reference) | 0.021 |
| 51–100 |
1.15
(0.75, 1.75) |
0.526 |
| >100 |
1.75
(1.14, 2.67) |
0.009 |
| Extraluminal free air on CT |
1.47
(0.60, 3.56) |
0.398 |
| Periappendiceal fluid on CT |
2.11
(1.39, 3.19) |
< 0.001 |
| Appendicolith on CT |
2.71
(2.01, 3.64) |
< 0.001 |
| Time from CT to antibiotics started (h) |
0.94
(0.90, 0.97) |
< 0.001 |
Values in parentheses are 95 per cent confidence intervals.
*Pre-CT delay is time from CT to start of operation; time to event is time from CT to surgery. WBC, white blood cell.
Patients with complicated appendicitis had a longer hospital stay after surgery: mean difference 2 days and 14 h (95 per cent c.i. 2 days 5 h to 3 days 0 h) (P < 0.001). Patients operated on for complicated appendicitis had more frequent complications than those who had surgery for uncomplicated appendicitis (Table 5).
Table 5.
Postoperative outcomes
| Uncomplicated appendicitis (n = 650) | Complicated appendicitis (n = 187) | Odds ratio† | P ‡ | |
|---|---|---|---|---|
| Length of postoperative hospital stay (days)* | 1.08 (0.75–1.55) | 3.56 (2.14–5.13) | < 0.001§ | |
| Length of postoperative antibiotic treatment (days)* | 0.50 (0.50–1.09) | 10.11 (8.32–12.08) | < 0.001§ | |
| Clavien–Dindo grade at 30 days | ||||
| No complications | 612 (94.2) | 160 (85.6) | 0.37 (0.22, 0.62) | < 0.001 |
| I | 6 (0.9) | 8 (4.3) | 4.80 (1.64, 14.00) | 0.002 |
| II | 25 (3.8) | 10 (5.3) | 1.41 (0.67, 3.00) | 0.366 |
| III | 7 (1.1) | 7 (3.7) | 3.57 (1.24, 10.32) | 0.012 |
| IV | 0 (0) | 2 (1.1) | – | 0.008 |
| V | 0 (0) | 0 (0) | – | – |
| Surgical-site infection | ||||
| None | 629 (96.8) | 174 (93.0) | 0.45 (0.22, 0.91) | 0.023 |
| Superficial | 8 (1.2) | 5 (2.7) | 2.21 (0.71, 6.82) | 0.160 |
| Deep | 0 (0) | 1 (0.5) | 0.22 (0.20, 0.25) | 0.062 |
| Organ space | 13 (2.0) | 7 (3.7) | 1.91 (0.75, 4.85) | 0.169 |
Values in parentheses are percentages unless indicated otherwise;
*values are median (i.q.r.); †values in parentheses are 95 per cent confidence intervals.
‡Pearson’s χ2 test, except
§Mann–Whitney U test.
Discussion
This study has shown that patients with uncomplicated appendicitis on CT have a substantial risk of being diagnosed with complicated appendicitis at surgery. Although appendicolith, periappendiceal fluid and extraluminal air are CT features associated with a greater probability of complicated disease11, even in the absence of these risk factors the rate of complicated appendicitis was high (14.0 per cent). The limitations of CT in discriminating complicated appendicitis from uncomplicated disease have been identified previously9. A recent study15 with similar design to the present study found that 12 per cent of patients had an intraoperative diagnosis of complicated appendicitis after uncomplicated appendicitis had been diagnosed on preoperative CT. A more accurate identification of patients with uncomplicated appendicitis is possible by excluding patients with appendicolith on CT10.
The Atema score was designed to identify patients with complicated appendicitis, taking into account the CT appearances along with clinical and laboratory findings. This study provides some external validation of this score. Unfortunately, in discriminating uncomplicated from complicated appendicitis, the overall sensitivity of the Atema score was only 69.0 per cent, indicating that it is not accurate enough to rule out complicated appendicitis in clinical practice. The Atema score might be a useful a tool for the surgeon to decide on the urgency of operation for a specific patient.
A number of studies1–5,16,17 have shown that increasing the time from symptom onset is associated with an increasing proportion of complicated appendicitis. Conflicting results have been found, however, regarding the impact of in-hospital delay8,15,18,19,20,21. Inevitably, observational studies have a risk of selection bias influencing in-hospital delay. Patients with more severe pain6 or those with several risk factors21 are usually operated on earlier, as was the case in the present series. A prospective study16 of 171 patients showed that only the total delay from the start of the symptoms to surgery correlated with the proportion of complicated appendicitis, whereas hospital delay did not. In the present study, analyses to estimate the risk of developing perforation after uncomplicated appendicitis on CT indicated that delaying appendicectomy in patients with uncomplicated appendicitis on CT may be harmful, and every 1 h of delay increased the risk of perforation by 2 per cent. However, in patients with a low Atema score or low CRP concentration without appendicolith on CT, a delay of up to 7 h was still associated with only a 5 per cent rate of perforation, indicating that a distinct subset of patients can be identified, if case prioritization is necessary.
Among patients with minor to moderate symptoms of acute appendicitis, antibiotics are usually started during induction of anaesthesia. When symptoms are more severe or when surgery is significantly delayed for some reason, clinicians often start antimicrobial therapy sooner. Studies9,10 investigating non-operative treatment of appendicitis rely on antibiotics as an alternative to surgery. In the present study, the use of preoperative antibiotics was more common and prolonged among patients who had a final diagnosis of complicated appendicitis. This casts doubt about the ability of antibiotics to prevent perforation in acute appendicitis.22
In the present study, the Atema score with clinical, laboratory and CT features did not reach the sensitivity (90.2 per cent) reported in the original publication12 for discriminating complicated from uncomplicated appendicitis. There may be a number of reasons for this. The present study excluded patients considered to have complicated appendicitis according to the radiology report. Gangrenous non-perforated appendicitis was considered uncomplicated in this study, in contrast to the original publication. In the present study, patients had a fairly long (over 8 h) median preoperative delay after CT, which might explain the worse results; unfortunately the duration of in-hospital delay was not provided in the original publication.
This study has other limitations. Although the sample size was large, it does not represent consecutive patients with appendicitis, because nearly half of the patients did not have preoperative CT. As the study hospitals used the Adult Appendicitis Score in selecting patients for imaging studies, many patients would be those presenting with equivocal findings on clinical examination.23,24 Owing to the retrospective nature of the study, the scores were not recorded and available in all patients. There is also a possibility that some patients may have had complicated appendicitis at baseline, not diagnosed by CT. The exact time of perforation was not possible to measure, so the time of perforation was set to the beginning of the surgery. This may represent systematic bias, overestimating the time from CT to perforation. Despite these limitations, patients with uncomplicated appendicitis on CT have a substantial risk of complicated disease by the time of surgery, if this is delayed. A delay of up to 7 h may be safe in patients with a low Atema score or in those with a low CRP concentration and no appendicolith on CT.
Funding
Governmental competitive funds
Supplementary Material
Acknowledgements
This study was funded by governmental competitive funds for medical research.
Disclosure. The authors declare no conflicts of interest.
Supplementary material
Supplementary material is available at BJS Open online
References
- 1. Ditillo MF, Dziura JD, Rabinovici R. Is it safe to delay appendectomy in adults with acute appendicitis? Ann Surg 2006;244:656–660 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Augustin T, Cagir B, Vandermeer TJ. Characteristics of perforated appendicitis: effect of delay is confounded by age and gender. J Gastrointest Surg 2011;15:1223–1231 [DOI] [PubMed] [Google Scholar]
- 3. Hansson LE, Laurell H, Gunnarsson U. Impact of time in the development of acute appendicitis. Dig Surg 2008;25:394–399 [DOI] [PubMed] [Google Scholar]
- 4. Bickell NA, Aufses AH, Rojas M, Bodian C. How time affects the risk of rupture in appendicitis. J Am Coll Surg 2006;202:401–406 [DOI] [PubMed] [Google Scholar]
- 5. Temple CL, Huchcroft SA, Temple WJ. The natural history of appendicitis in adults. A prospective study. Ann Surg 1995;221:278–281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Sammalkorpi HE, Leppäniemi A, Mentula P. High admission C-reactive protein level and longer in-hospital delay to surgery are associated with increased risk of complicated appendicitis. Langenbecks Arch Surg 2015;400:221–228 [DOI] [PubMed] [Google Scholar]
- 7. van Dijk ST, van Dijk AH, Dijkgraaf MG, Boermeester MA. Meta-analysis of in-hospital delay before surgery as a risk factor for complications in patients with acute appendicitis. Br J Surg 2018;105:933–945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Bonadio W, Brazg J, Telt N, Pe M, Doss F, Dancy L et al. Impact of in-hospital timing to appendectomy on perforation rates in children with appendicitis. J Emerg Med 2015;49:597–604 [DOI] [PubMed] [Google Scholar]
- 9. Vons C, Barry C, Maitre S, Pautrat K, Leconte M, Costaglioli B et al. Amoxicillin plus clavulanic acid versus appendicectomy for treatment of acute uncomplicated appendicitis: an open-label, non-inferiority, randomised controlled trial. Lancet 2011;377:1573–1579 [DOI] [PubMed] [Google Scholar]
- 10. Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis. JAMA 2015;313:2340–2349 [DOI] [PubMed] [Google Scholar]
- 11. Kim HY, Park JH, Lee YJ, Lee SS, Jeon J-J, Lee KH. Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology 2018;287:104–115 [DOI] [PubMed] [Google Scholar]
- 12. Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg 2015;102:979–990 [DOI] [PubMed] [Google Scholar]
- 13. Tominaga GT, Staudenmayer KL, Shafi S, Schuster KM, Savage SA, Ross S et al. The American Association for the Surgery of Trauma grading scale for 16 emergency general surgery conditions: disease-specific criteria characterizing anatomic severity grading. J Trauma Acute Care Surg 2016;81:593–602 [DOI] [PubMed] [Google Scholar]
- 14. Dindo D, Demartines N, Clavien P-A. Classification of surgical complications. Ann Surg 2004;240:205–213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Hanson KA, Jacob D, Saleh AA, Dissanaike S. In-hospital perforation risk in acute appendicitis: age matters. Am J Surg 2020;219:65–70 [DOI] [PubMed] [Google Scholar]
- 16. Foul SA, Egozi E, Assalia A, Kluger Y, Mahajna A. Is early appendectomy in adults diagnosed with acute appendicitis mandatory? A prospective study. World J Emerg Surg 2019;14:1–4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Kim JW, Shin DW, Kim DJ, Kim JY, Park SG, Park JH. Effects of timing of appendectomy on the risks of perforation and postoperative complications of acute appendicitis. World J Surg 2017;42:1295–1303 [DOI] [PubMed] [Google Scholar]
- 18. Omundsen M, Dennett E. Delay to appendicectomy and associated morbidity: a retrospective review. ANZ J Surg 2006;76:153–155 [DOI] [PubMed] [Google Scholar]
- 19. Papandria D, Goldstein SD, RheeD, Salazar JH, ArlikarJ, GorgyA, et al. Risk of perforation increases with delay in recognition and surgery for acute appendicitis. J Surg Res 2013;184:723–729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Busch M, Gutzwiller FS, AelligS, KuettelR, MetzgerU, Zingg U. In-hospital delay increases the risk of perforation in adults with appendicitis. World J Surg 2011;35:1626–1633 [DOI] [PubMed] [Google Scholar]
- 21. Drake FT, Mottey NE, Farrokhi ET, Florence MG, Johnson MG, MockC et al Time to appendectomy and risk of perforation in acute appendicitis. JAMA Surg 2014;149:837–844 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Park HC, Kim MJ, Lee BH. Randomized clinical trial of antibiotic therapy for uncomplicated appendicitis. Br J Surg 2017;104:1785–1790 [DOI] [PubMed] [Google Scholar]
- 23. Sammalkorpi HE, MentulaP, Leppäniemi A. A new adult appendicitis score improves diagnostic accuracy of acute appendicitis – a prospective study. BMC Gastroenterol 2014;14:910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Sammalkorpi HE, Mentula P, Savolainen H, Leppäniemi A. The introduction of adult appendicitis score reduced negative appendectomy rate. Scand J Surg 2017;106:196–201 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.