Abstract
Introduction
The World Health Organization's International Classification of Functioning, Disability and Health calls on speech-language pathologists (SLPs) to provide care that impacts all aspects of an individual's experience with a communication disorder, including their participation in valued life situations. However, SLPs often report feeling unprepared to implement and document interventions that target life participation. The purpose of this article is to propose a framework to guide participation-focused intervention practices. This age- and disorder-generic framework is designed to be applicable with clients across the variety of settings in which SLPs work.
Method
In this clinical focus article, we draw on past research and clinical experience to propose a restructuring of World Health Organization's International Classification of Functioning, Disability and Health components such that participation is the primary focus and outcomes indicator for intervention. In this framework, a specific communicative participation situation is identified and assessed quantitatively, and a corresponding participation-focused goal is established through shared decision making. Following that, assessments are conducted and goals are established in the areas of communication skills, physical and social environments, and personal perspectives.
Results
The proposed framework provides a concrete organizational structure as well as assessment, goal-writing, and intervention examples to assist SLPs in translating theoretical biopsychosocial frameworks into clinical practices.
Conclusions
SLPs can and do provide holistic communication services to clients to help them achieve their life participation goals. This article provides an example as to how we can document the need for, as well as the value and impact of our important work, meeting the diverse life participation needs of clients.
Supplemental Material
Several transitions are underway in many health care fields that are intended to ensure that health care services support individual clients and their families in achieving healthy, fulfilling life participation. While there is likely little disagreement that the ethical compass of clinical care points to providing the most optimal, individualized care possible, there is a paucity of tangible roadmaps guiding clinicians in how to get from theoretical stances to concrete clinical practices. The purpose of this clinical focus article is to provide such a map that includes guidance for conducting assessments, writing goals, implementing holistic intervention, and documenting outcomes as they pertain to life participation with a communication disorder.
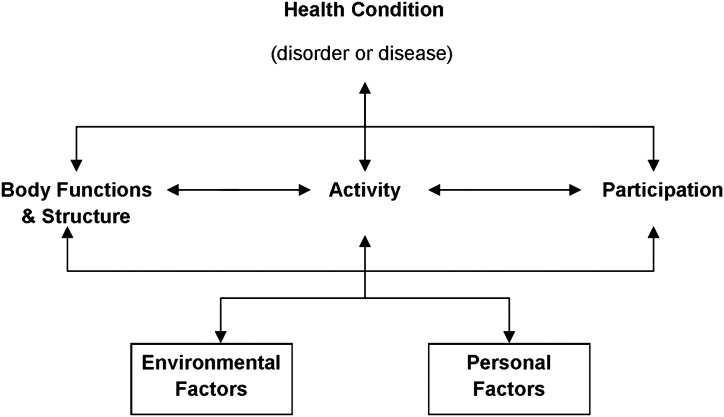
One of the foremost health care movements in recent years has been the adoption of biopsychosocial frameworks of health and disability. Biopsychosocial frameworks compel us to consider health as a complex experience that is shaped by biological elements (the physical condition and function of the body), psychological elements (emotional health), and social elements (the environment surrounding the individual; Threats, 2006; Wade & Halligan, 2017). Most prominent among these frameworks is the World Health Organization's International Classification of Functioning, Disability and Health (WHO ICF; see Figure 1) with its elements of (a) body functions and structures, (b) activities, (c) participation, and (d) environmental and personal factors (WHO, 2001). The ICF defines body functions and structures as the anatomy and physiology of the body, with the term impairment used to refer to any physical injury to the body. The ICF uses the term activities to refer to execution or performance of discreet tasks or actions. The term participation refers to an individual's engagement in real-life situations and how the individual fulfills their life roles and goals in the context of daily life. Finally, contextual factors include the environment (which can be aspects of the natural or built physical and social environments) and personal factors (which can include demographic and related personal characteristics, as well as personal experiences and coping factors).
Figure 1.
The traditional framework for the World Health Organization's International Classification of Functioning, Disability and Health (World Health Organization, 2001).
Biopsychosocial frameworks counteract traditional medical models of health, which focus almost solely on treating the physical impairment and changing the individual with the health diagnosis. While addressing the physical impairment is an important aspect of clinical care, biopsychosocial frameworks also draw our attention to principles from social models of disability, which emphasize how disability is created by barriers in the physical and social environments in which we live (Brewster, 2004; Jordan & Bryan, 2010; Oliver, 2013). Biopsychosocial frameworks remind health care providers that helping clients to navigate those barriers and advocating for environmental and societal changes that can remove disabling obstacles in the world around us are also important aspects of our clinical practices. The WHO ICF has been adopted into speech-language pathology practice patterns by the American Speech-Language-Hearing Association (ASHA), which advises that the speech-language pathology scope of practice includes a wide range of clinical services that will ultimately help clients improve their overall life participation and quality of life in the context of a communication or swallowing disorder (https://www.asha.org/policy/PP2004-00191/).
Biopsychosocial approaches to care are one component of a closely related movement in health care—that of person-centered care. Person-centered care embodies respect for client autonomy and choice, values the individual needs of each person, promotes a therapeutic alliance between health care provider and client to meet those needs, and encourages a holistic view of the client in terms of caring for physical and emotional needs (Bellon-Harn et al., 2017; DiLollo & Favreau, 2010; O'Halloran et al., 2010; Rogers, 1946). Adoption and realization of person-centered care requires a realignment of the relationships between health care professionals and their clients through shared decision making in which health care providers work collaboratively with clients and families to meet the values stated above (Kaizer et al., 2012; Parette et al., 2000; van Til et al., 2010; Wills, 2010). These influences of biopsychosocial frameworks of health, person-centered care, and shared decision making converge in the recent move toward promoting value-based clinical services. Value in health care goes beyond financial considerations. Value also means that the experience and outcomes of health care services bring about meaningful change in clients' lives such that they see the worth in having pursued that care (Rao, 2015; Rundell et al., 2015). The ideals described in these paragraphs are not unique to the field of speech-language pathology but are promoted by a wide range of rehabilitation and other health care disciplines, as well as health care policy and advocacy organizations (Baum, 2011; Cardol et al., 2002; Imms et al., 2017; Law, 2002; Magasi et al., 2009; United Nations, 2019; WHO, 2001).
While the optimal health care scenario may be represented by the concepts defined in the previous paragraphs, day-to-day clinical practice often does not meet these ideals. Speech-language pathology services in many settings still lean heavily toward a medical model of service delivery, focusing largely on addressing physical impairment and injury (e.g., language impairment or speech disfluency) and how those impairments impact the individual's performance of communication tasks (activities; Collis & Bloch, 2012; N. Miller & Bloch, 2017; Simmons-Mackie et al., 2005; Threats, 2007; Torrence et al., 2016). Clinicians certainly hope that improvements in these areas will generalize to improvements in life participation. However, associations between measures of participation and disorder severity are often weak to moderate, suggesting that impairment is likely not the only or even primary influence on participation outcomes (Bolt et al., 2016; Eadie et al., 2016). Thus, it is possible that maximal improvements in participation will not be reached unless speech-language pathologists (SLPs) look beyond the impairment to also systematically address other contributors to life participation in the context of a communication disorder, including environmental and personal factors.
Clinicians face many challenges to implementing truly person-centered, biopsychosocial care. One challenge lies in translating frameworks such as the ICF into daily clinical practices. Numerous authors have advocated for modifying the ICF because of difficulties implementing the ICF in clinical practice. Their reasons include the need to better incorporate the personal viewpoints of clients in a framework of clinical practice, to better account for the role of environment and context in health and disability, to capture more holistic quality of life or lived experiences, to clarify confusion about distinctions among constructs (e.g., activity vs. participation), and to counteract the instinct to always start analyzing from the perspective of the physical impairment since that construct occupies the first construct encountered when reading the ICF from left to right following English reading conventions (Cruice, 2008; Huber et al., 2010; Jette et al., 2007; Kagan et al., 2008; Ravenek et al., 2013; Ueda & Okawa, 2003).
Another often-cited challenge to the implementation of person-centered, biopsychosocial intervention is the lack of sufficient resources, guides, and training (Collis & Bloch, 2012; N. Miller et al., 2011; Torrence et al., 2016; Verna et al., 2009). Some initial resources have emerged. For example, the Life Participation Approach to Aphasia provides a foundational call to action emphasizing that a participation-focused approach to therapy must meet several critical criteria including the following: (a) The primary purpose of intervention is to improve life participation, (b) services should be provided not only to the person with the communication disorder but also to everyone in their circle of family and close companions who are impacted by the condition, (c) environmental and personal issues are appropriate and necessary targets for intervention, (d) people should receive services when they need assistance regardless of the stage of their condition, and (e) outcomes measures should include documentation of the impact on life participation (Chapey et al., 2000; Kagan & Simmons-Mackie, 2007; Kagan et al., 2008; Worrall, 2006). A more recent guide begins to translate the Life Participation Approach to Aphasia into concrete examples for choosing communication goals and creating collaborative, client-centered plans to address those goals (Haley et al., 2019). Even with these initial guides, however, resources are limited and are concentrated in the area of aphasia treatment for adults.
The purpose of this article is to propose a framework to guide person-centered, biopsychosocial intervention practices to help clients of all ages and disorders improve their life participation. After an introduction to the framework in the next section, subsequent sections of this article will address the individual components of the framework by defining the component, discussing options for assessing that component, and providing suggestions for writing goals and designing interventions relevant to that component. The role of shared decision making will be emphasized throughout. The text of this article is accompanied by materials that SLPs may find helpful in implementing these procedures. Appendixes A–C provide case examples using the proposed participation-focused framework with an adult with a voice disorder, a teenager with dysarthria, and a child with a developmental language disorder, respectively. In addition, Supplemental Materials S1 and S2 include a shortened guide to this information and a blank version of the treatment planning template used in the appendixes that clinicians may want to print out and fill in as they work with clients to guide their organization of information. Given space limitations, these examples cannot be exhaustive, but we hope they provide some guidance for clinicians who are looking for further suggestions. We also encourage clinicians to expand upon and adapt the ideas presented here for their specific clients.
A Framework for Participation-Focused Intervention
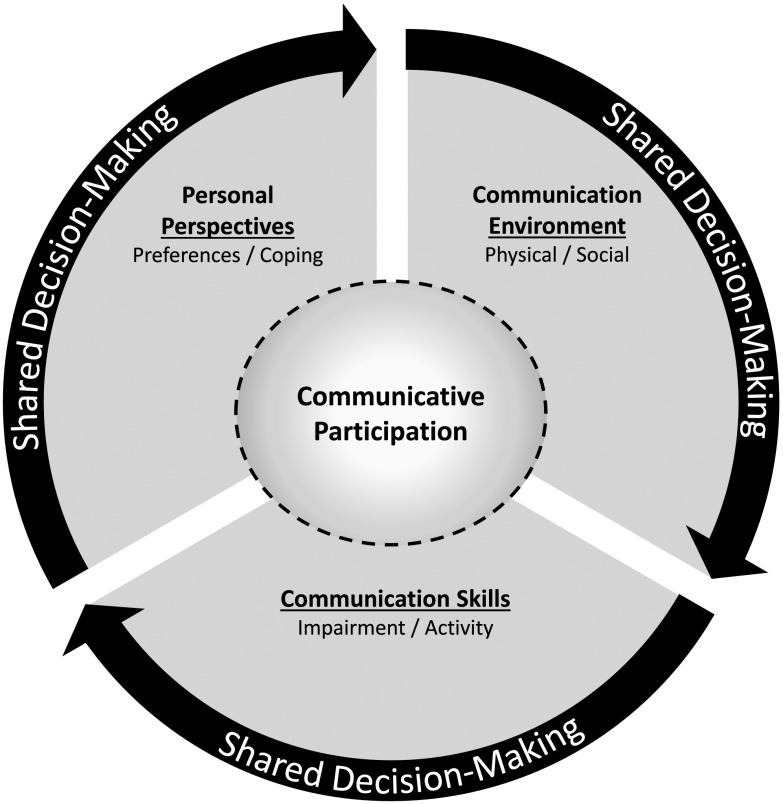
We suggest an alternative organization of the WHO ICF components to guide person-centered, biopsychosocial intervention practices (see Figure 2). This reorganization places “communicative participation,” meaning communication that occurs in the context of an individual's involvement in daily life situations (Eadie et al., 2006), at the center as the primary focus and central organizing principle of treatment planning and implementation. The elements of “communication skills,” “communication environment,” and “personal perspectives” are regarded as contributing (potentially equally) to restrictions in communicative participation, and thus each warrants full consideration in treatment planning, intervention, outcomes measurement, and documentation. The circular nature of Figure 2 is intended to represent that there is not an inherent hierarchy among communication skills, communication environment, and personal perspectives but that all warrant commensurate consideration and may influence each other. The dotted line around communicative participation represents a porous border between participation and the surrounding elements, thus acknowledging the frequent interactions among these elements and the flow of influences back and forth.
Figure 2.
The elements of the International Classification of Functioning, Disability and Health are reorganized into a participation-focused framework. In this figure, communicative participation is the central focus. As such, clinicians are urged to consider participation first and foremost. They do this by working together with their clients to first develop goals for participation for specific situations identified by the client and other key stakeholders as most important to address. This is followed by developing goals for communication skills, communication environment, and personal perspectives, which support the primary participation goal. The circular nature of the figure is intended to represent that there is not an inherent hierarchy among communication skills, communication environment, and personal perspectives but that all warrant commensurate consideration and may influence each other. The porous border between communicative participation and the surrounding elements is intended to represent the frequent interactions among these elements and the flow of influences back and forth.
The participation-focused framework presented in Figure 2 is intended to be applicable across the many communication disorders that impact individuals across the life span. The drive to create an age- and disorder-generic framework arises from several factors. First, prior research suggests that many of the life participation restrictions that adults with communication disorders face are highly similar regardless of the underlying diagnosis (Baylor et al., 2011; Garcia et al., 2002). These similarities may arise in part from common barriers to and facilitators of communicative participation in our environments. Second, restrictions in communicative participation are faced by people of all ages who have communication disorders. Examples of shared restrictions in communicative participation across different diagnoses and ages include limitations in employment or academic opportunities, loss of friends and social contacts, withdrawal from social situations, and feelings of frustration and isolation (Baylor et al., 2007; Beitchman et al., 1996a, 1996b; Bricker-Katz et al., 2009; Dalemans et al., 2008, 2010; Davidson et al., 2008; Fujiki et al., 2001; Hinckley, 2002; Hodge & Wellman, 1999; Johnson et al., 2010; Lewis et al., 2000a, 2000b; Markham et al., 2009; McNaughton et al., 2001; N. Miller et al., 2006; Northcott & Hilari, 2011; Parr, 2007; Smith et al., 1994; Walshe & Miller, 2011). Finally, as SLPs, we are trained to competently serve individuals with communication disorders across the life span. While some SLPs may specialize in a specific disorder or age group, most SLPs will be called upon to serve clients across a diverse range of ages and/or disorders throughout their careers. An age- and disorder-generic framework that SLPs can adapt to each individual client will allow SLPs to approach participation-focused intervention in a similar manner and may facilitate communication within the professional community.
Communicative Participation
Participation-focused interventions ensure that therapy is motivated by, designed for, and accountable to outcomes specifically addressing each individual's needs and preferences for attaining or maintaining fulfilling involvement in the communication aspects of their daily life (Chapey et al., 2000; Duchan, 2001; Kagan & Simmons-Mackie, 2007; Worrall, 2006; Yorkston et al., 2017b). Most clients seek clinical services (or are brought in by their families) because of concerns regarding how their communication disorder may impact what they want and need to do in their daily lives. It is the drive to fully engage in the human experience that will compel many people to strive for better, easier, and more satisfactory communication that not only allows them to function in their daily lives but also, just as importantly, reflects their identity in how they see themselves as individuals.
In Figure 2, communicative participation is the starting point for treatment planning. Participation-focused intervention must involve assessing participation as a distinct construct, writing goals specifically to address participation, and later documenting progress in actual life participation. Maintaining the traditional intervention focus on impairment and activity performance, with the motivation, hope, or intent lingering in the back of our minds or the subtext of our documentation that the intervention will, at some point, connect to real-life situations, is not, in our opinion, inherently participation focused. Participation-focused intervention starts with an understanding of what the individual needs and wants to do with communication in daily life and ends when the client has gotten as close as possible to living that experience. Interventions targeting other aspects of the WHO ICF help the client build the skills, strategies, environmental supports, and psychological resources to bridge those two points.
In the participation-focused approach to treatment planning that we are proposing in Figure 2, the “communicative participation” circle in the center represents a single, specific situation that will be the target for intervention (this process may be replicated sequentially or in parallel for multiple situations). Be sure the situation chosen for the participation goal is not too complex, grandiose, or distant into the future, all of which may be counterproductive to seeing meaningful change in a realistic timeline (Haley et al., 2019). For a child or teen, targeting “communication at school” would not make the best participation goal, largely because most school days consist of a variety of situations that involve a variety of communication needs, communication partners, and communication settings. This leads to convoluted and confounded goals and treatment data. Instead, write different participation goals for different communication situations at school. Perhaps, one goal targets “participation in conversations in group projects at school,” while another goal targets “asking questions in class,” and so forth. If the student says what they most want to focus on is talking to friends between classes, write a goal for that. Furthermore, if the timing of returning to school is unknown with a teen with a new onset of disability, focus on more immediate participation goals such as “participation in conversations with therapists during rehab sessions” or “phone conversations with family members.”
Although we want to help clients improve their communicative participation in all aspects of their lives, focusing on a single (or select few) situation(s) in therapy may have advantages, particularly if the groundwork is laid for good generalization. If the focus of intervention remains only on improving participation in a general sense across the range of different situations in a client's life, it is difficult to get specific in therapy in terms of what stimuli to practice, what environmental modifications to implement, and so forth. As a result, intervention techniques and strategies may remain vague and nonspecific, leaving it to the client to try to tailor and adapt strategies for specific situations. Some clients may be good at that, but others will struggle—hence perpetuating the risk of a disconnect between intervention and real life. In contrast, working in greater depth and detail on a specific life situation allows the client to practice highly relevant and immediately useful skills and environmental modifications using the exact stimuli and strategies that they will apply in their targeted situation.
This situation-specific focus may yield several benefits. Clients may be highly motivated by what they see as relevant and productive intervention because they can immediately experience how therapy connects to their daily lives. Motivated clients may work harder or stay engaged longer for better therapy gains. Furthermore, there may be an increased likelihood that participation in the targeted situation will improve because of the direct work on that situation—hence better outcomes. Finally, when clients (and families) see how practice, strategies, and modifications work to improve one situation, they may be empowered to generalize those strategies to new situations, thus contributing to a global improvement in life participation.
The specific situation(s) to be addressed in intervention should be chosen through a process of shared decision making with the client and key stakeholders. One of our research participants, a man with multiple sclerosis, advised us that the best starting point for intervention is to ask the client, “What is the most important conversation for you?” In this gentleman's case, he was participating in speech therapy to enhance speech intelligibility during a time in his life when he was single after a recent divorce. His “most important conversation,” or life communication situation, was meeting and dating new women. When that situation was not addressed in therapy, he felt disappointed in what he described as a “see Dick and Jane run” therapy program because of its rudimentary level of practice that bore little relevance to his daily life. This perception of speech therapy as irrelevant to daily life can also be felt by children (Merrick & Roulstone, 2011). For children, the role of the child versus the caregiver in choosing life situations to work on in therapy will be adjusted according to the age and situation of the child. When any clients are not able to easily convey the communication situation(s) they would like to focus on in therapy with appropriate communication support, other resources that might be helpful include the Life Interests and Values Cards (Haley et al., 2013) for adults and the Children's Assessment of Participation and Enjoyment and Preferences for Activities of Children (King et al., 2004) for children.
Measuring Communicative Participation
If communicative participation is to be recognized as the primary focus of intervention and key indicator of treatment success, a participation-focused approach to intervention must start by measuring communicative participation. SLPs may want to consider three key issues when selecting or designing participation measures. First, assessment of communicative participation is different than assessment of communication skills. A measure of speech intelligibility, language skills proficiency, or speech fluency, even when conducted in the target environment, does not necessarily reflect the experience of engagement or involvement that truly represents communicative participation. Participation measures need to reflect the convergence of communication skills, the environment, and personal perspectives to document whether the client is meeting their communication demands and preferences successfully and satisfactorily.
Second, when at all possible, a patient-reported outcome (PRO) should be included as a key indicator of participation restrictions and intervention outcomes (Brown et al., 2004; Law, 2002; Perenboom & Chorus, 2003; Whiteneck, 1994). Respect for client dignity and autonomy demands that clinicians document the viewpoint of the individual client (and possibly family) with regard to the extent and nature of restrictions in participation that they experience and the outcome that would be satisfactory to them—and that clinicians later document if that targeted outcome was achieved. While not all clients with significant language and cognitive impairments may be able to complete PROs, many clients are able to do so with appropriate communication support (Tucker et al., 2012), including children as young as 5 years of age (Varni et al., 2007; Young et al., 1995). When not, judicious use of proxy report may be helpful.
Finally, participation measurement should be sensitive to change with intervention. “Inventory” information such as what people communicate about in life situations, how often they do so, who they communicate with, and so forth, is important background knowledge for designing person-centered intervention. However, these constructs would serve as good measures of treatment outcomes only if the client wants or needs to change how often they participate or who is in their social network. For example, if changing the frequency of involvement is not feasible due to the nature of the situation (e.g., a school club only meets once a month) or due to the client's preference to continue with the established frequency, then frequency of participation is not a good treatment target or a good measure of treatment gains. Other constructs, such as the client's satisfaction with their participation or their judgment that they are meeting their communication needs, may be more appropriate treatment targets and thus more sensitive measures of treatment gains. This concept was illustrated by an adult participant with spasmodic dysphonia in a prior study who mentioned that she never missed a book club meeting (Baylor et al., 2005; Yorkston et al., 2008). Just as we, the interviewers, were reflecting positively on her frequent book club attendance, the participant stopped us to emphatically say, “No. I go, but I don't participate.” Her point was well taken that, to her, successful participation involved some level of engagement or involvement that could not be captured by simply measuring frequency of attendance at the event.
Considering these issues, SLPs may look to the growing repertoire of published PRO measures. A number of review articles provide examples of PROs in the areas of fluency (Franic & Bothe, 2008; Yaruss, 2010; Zraick et al., 2012), voice disorders (Francis et al., 2017; Franic et al., 2005), aphasia (de Riesthal & Ross, 2015; Irwin, 2012), and acquired dysarthria (Donovan, 2012). Other resources for PROs that are not specifically tied to communication disorders but may contain participation-related constructs are those associated with the National Institutes of Health Patient-Reported Outcomes Measurement Information System (PROMIS) and Neuro-Qol (Quality of Life in Neurological Disorders; http://www.healthmeasures.net). While communication disorder PROs provide different types of insight into the client's perspective, not all of these are considered measures of communicative participation (Eadie et al., 2006). Some instruments focus on client report of physical symptoms such as voice quality, speech fluency, or difficulty performing communication tasks. Other questionnaires elicit information about clients' feelings about their communication such as feeling embarrassed or anxious. These constructs certainly would contribute to communicative participation but do not give a complete picture of how symptoms, emotions, or other issues all come together for a summative impact on participation. In some cases, instruments have subscales that do give a more global view of communicative participation, for example, “Section IV: Quality of life” in the Overall Assessment of the Speaker's Experience of Stuttering (Yaruss & Quesal, 2006) or “Section D: How dysarthria affects my communication with others” in the Dysarthria Impact Profile (Walshe et al., 2009). The overall caution remains, however, that just because an instrument is patient reported does not guarantee it is measuring participation.
As of this writing, there are few validated measures dedicated to communicative participation, which may be related to several challenges in developing these instruments including agreeing on the definition and scope of the construct of “participation” as well as the rigorous process for developing measures demanded in the current state of measurement science (Brandenburg et al., 2015; Darling-White, 2017). Published PROs for adults include the Communicative Participation Item Bank that captures the extent to which the individual feels he or she is experiencing restrictions in daily conversational situations (Baylor et al., 2014, 2017, 2013; C. Miller et al., 2017). Options for pediatric populations include the Speech Participation and Activity Assessment of Children, which is an interview tool used to gather information about the child's participation needs and desires (McLeod, 2004). Questions on the Speech Participation and Activity Assessment of Children are geared not only toward the child but also to parents, siblings, and teachers for a more holistic view of the child's participation in a variety of contexts. Another option is the Speech Situation Checklist developed for school-age children who stutter (Brutten & Vanryckeghem, 2007).
Most of the PROs described above cover a wide range of communication situations, so they are beneficial for measuring clients' general participation during initial intake assessment or at discharge. They may also help the client–clinician team identify various situations of concern. However, per the framework presented in Figure 2 and the discussion above, intervention should focus on specific situations. Questionnaires that cover a broad range of situations might not be sufficiently sensitive to changes in the specific situation targeted in intervention. For the time being, then, this leads to the need for additional nonstandardized methods of assessment that can focus precisely on the situation(s) to be targeted to maximize sensitivity to change in a manner that is meaningful to the client.
Self-anchored rating scales are a good option for this purpose (Fox, 2012). Self-anchored scales may take the form of a Likert scale (e.g., rate on a scale of 0–10 which number represents how you feel) or a visual analog scale (VAS; e.g., the client makes a mark on a 100-mm line to represent how they feel). What makes such scales self-anchored is that the construct rated and the end points or anchors of the scales are defined using concepts and/or terminology that reflects the client's feelings (Fox, 2012). For example, a client who has identified participation in conversations in her weekly knitting group as her “most important conversation” might be asked to rate how satisfied she is with participation in conversations at a knitting club on a 100-mm VAS with 0 = not at all satisfied and 100 = very satisfied. The scale does not have to be anchored with the concept of satisfaction but could be anchored with whatever term reflects the client's viewpoint. Clients might identify more with rating an experience of “feeling left out,” “feeling isolated,” or “being a bystander in conversations” or other perspectives. Whatever format is used, this scale should be saved for this client and used again later to assess progress. See Appendix B for an example of a Likert scale being used to measure communicative participation.
Writing a Communicative Participation Goal
Once a client's current participation status in the targeted situation has been measured, the next step is to write a goal or behavioral objective to address this restriction (Hidecker et al., 2011). Setting goals can be a complex process with a diversity of viewpoints, targets, and methods to be considered (Sherratt et al., 2011). When writing a participation-focused goal, there may be some specific issues to consider. First, the goal must be about communication (or swallowing) to be within our scope of practice, but just as with assessment, it does not have to be about communication ability, proficiency, or accuracy—those issues will be addressed in the next section on communication skills. Successful communicative participation means that the client is involved and included in that communicative situation in a way that meets their needs or preferences regardless of how accurate the speech production, voice quality, or word finding might be. The participation goal should target an end point that reflects personal significance in that reaching that goal will be personally meaningful to the client (Bothe & Richardson, 2011; Northcott et al., 2015; Wyrwich et al., 2005; Zeppiere et al., 2012). Shared decision making during the goal-setting process might involve asking clients to describe what a satisfactory outcome looks like to them or, when using a quantitative measure, having them identify the number or rating that they would find to be a satisfactory outcome. We have found in our research interviews that, after acknowledging that the ideal outcome (e.g., resolution of the communication impairment) may not be likely for adults with chronic communication disorders, participants usually move fairly easily to a discussion of what would constitute a satisfactory or meaningful outcome that is feasible.
Participation-focused goals should otherwise follow conventions of SMART goals (Bovend'Eerdt et al., 2009; Torres, 2013). They should identify specific targets that are observable and measurable with a defined time frame. The smoothest transition from assessment to goal writing is to use the same scale that was used in collecting pretreatment data on the targeted situation as the method for defining goals. For example, with our hypothetical client who has identified participation in conversations in her knitting group as her “most important conversation” to work on in therapy, our goal might be as follows: “Client will report a level of satisfaction with participation in conversations at knitting club as 80 or higher on a 100-mm VAS (0 = not at all satisfied; 100 = very satisfied) by the end of 8 weeks.” Goal attainment scaling (GAS) may also be a good option for participation-focused goals. GAS is a person-centered yet standardized goal format in which levels of progress or success are defined on a 5-point scale on which −2 = the worst possible outcome, 0 = the most likely outcome, and +2 = the best possible outcome (Krasny-Pacini et al., 2016; Schlosser, 2004). During the GAS process, the client and clinician work together to operationalize each of the five levels in the scale in terms of meaningful levels of success for that individual. See Appendixes A and C for examples of GAS as it relates to communicative participation goal-setting.
Before leaving the topic of writing goals for communicative participation, we would like to highlight one additional point. In prior research (Torrence et al., 2016), we noted a fairly common practice of writing goals such as “Client will demonstrate speech intelligibility of 90% or higher at the end of 8 weeks to facilitate participation in knitting club.” We would argue that this is not a goal that specifically targets participation. This is a goal that targets speech intelligibility—a communication skill. A goal such as this states that the motivation for improving intelligibility is a life participation situation, but that is not the same as ensuring that improved participation in that situation is actually achieved. The client can even achieve 90% intelligibility at knitting club meetings, but that is not the same as knowing that the client has achieved a satisfactory level of participation (i.e., involvement or engagement) in communication at a knitting club. Even with a high level of speech intelligibility, the client's participation in a knitting club may still be restricted by factors such as negative reactions from communication partners due to her residual unnatural speech or a reluctance to participate due to feeling self-conscious about her speech. Thus, tagging a participation-related motivation on to the end of a skill-based goal does not, in our view, make it a participation goal because it does not ensure that the goal will target the full experience of participation in that communication situation.
Once the communicative participation goal has been defined, we now move to the larger circle in Figure 2 where each of the areas of communication skills, communication environment, and personal perspectives will be considered. In Figure 2, the dotted or porous border between each of these elements and communicative participation is intended to reinforce that what is addressed in each of these areas will flow together to shape the ultimate participation outcome (and we also might consider that changes in participation may have reciprocal effects in each of these areas). Much of the work in intervention will target these three components of skills, environment, and personal perspectives, but the team needs to remember to go back and measure outcomes at the level of the overall participation goal to ensure an optimal, holistic outcome has been achieved.
Communication Skills
The communication skills element in Figure 2 combines the ICF concepts of body function and structure (impairment) along with activity (defined as the discreet, noncontextualized ability to perform speech, language, or cognitive tasks). The communication skills section refers to the physical and cognitive–linguistic communication abilities of the client and is where many traditional speech, language, and cognitive skills assessments would occur to answer questions such as the following: Does this client have sufficient strength, speed, and range of motion in the speech musculature to produce intelligible speech? Does this client demonstrate accuracy with verbal expression skills such as word-finding and grammatical language formulation? Does this client demonstrate accurate recall, information processing, and other cognitive skills?” The communication skills component might also include the client's abilities to use compensatory strategies. For example, can the client access a display on a speech-generating device accurately through pointing with a finger, or is an eye-gaze system needed? Can the client program reminders into a smartphone as a strategy for taking medications on schedule?
The communication skills element of the framework is easily recognizable as forming the bulk of our traditional work. Skills-based assessment and intervention are areas where we are already highly proficient as a discipline, and this excellent work needs to continue. Thus, we will not provide examples of assessments, goals, or intervention relevant to communication skills. We would, however, like to emphasize the importance of the activities and materials used in assessment and intervention being overtly relevant to the target situation (e.g., the actual vocabulary, materials, and other stimuli used in the situation). With adults in particular, we have heard many complaints in our research interviews about the “childish,” seemingly random, and completely irrelevant therapy drills to which clients have been subjected. For example, one research participant said, “We wrote down ten phrases that I never say and practiced saying them loudly.” Too often, we seem to start with a therapy task such as a drill of labeling flash cards and then ponder how to make that drill functional for the client. Instead, perhaps we should start with the actual participation situation and work on breaking that activity into tasks to practice in therapy. Even if the client is significantly impaired and needs simplified stimuli, these can still be taken directly from the targeted participation situation and modified as needed. Therapy that is engaging for the client because of a direct and obvious relevance to their chosen life situation may be more likely to motivate clients to follow through with recommendations (Haley et al., 2019). As one of our speech-language pathology students said, we need to make therapy “come to life.”
As critical as our work is in the area of habilitation and rehabilitation of communication skills, skills alone do not necessarily guarantee successful communicative participation. Furthermore, many of our clients will not be able to attain or recover typical communication abilities or independent use of compensatory strategies. If all emphasis in clinical intervention and documentation is placed on communication skills, important ways that SLPs can and already do help people with communicative participation will go unrecognized and unaddressed. Thus, the other two sections of the large circle in Figure 2—communication environment and personal perspectives—should receive equal consideration in all aspects of clinical practice.
Communication Environment
The communication environment portion of the framework, like the environmental factors element of the WHO ICF, incorporates aspects of the physical and social environments that may impact communicative participation. The physical environment can include natural and/or human-made aspects of a setting, as well as products and technology that are used in various settings (Howe et al., 2004). Common characteristics of the physical environment that restrict communicative participation include background noise, long distances across which people need to project their speech, technology such as phones, drive-through window intercoms and smart speakers that do not transmit distorted speech well, linguistically complex printed and web-based materials, and so forth (Baylor et al., 2011; Garcia et al., 2002; Howe et al., 2008a, 2008b; Rose et al., 2003).
The social environment includes the communication partners and what they bring to communicative interactions in terms of attitudes, support and relationships, and more formal services and policies (Howe et al., 2004). There is strong evidence documenting the extent to which communication partners can be either facilitators of or barriers to communicative participation depending on how they interact with the person with the communication disorder (Baylor et al., 2011; Kagan, 1998; Merrick & Roulstone, 2011; Simmons-Mackie & Damico, 2007; Yorkston et al., 2017b, 2007, 2001). While not universal, communication partners who are more familiar to the person, who are more patient and allow sufficient time for communication, and who interact with people with communication disorders with genuine respect often facilitate participation. Conversely, communication partners who are rushed, impatient, dismissive, condescending, or unaware of how to communicate with the person can create impenetrable barriers to life participation. In recognition of the powerful role of communication partners, an increasing number of programs focused on training communication partners are emerging. Some programs target specific populations such as those with aphasia (Cruice et al., 2018; Kagan, 1998; Simmons-Mackie et al., 2010, 2016), specific age groups such as parents of young children with communication disorders (Roberts & Kaiser, 2011), or specific situations such as health care settings (Baylor et al., 2019; Burns et al., 2012; Eriksson et al., 2016; Forsgren et al., 2017; Legg et al., 2005; Simmons-Mackie et al., 2007; Sorin-Peters et al., 2010).
There are other examples of how physical and social environments can restrict communicative participation that might not be quite as direct but are important to recognize as we strive to understand the complexity of how environment shapes communication—and how we might target this in intervention. For example, in a prior study, an individual with multiple sclerosis who did not have communication impairments but who depended on a wheelchair for mobility was not able to join groups of friends for conversation during an outdoor reception where tables were placed on a grassy lawn that her wheelchair could not navigate (Yorkston et al., 2001). She considered her communicative participation restricted for reasons that had nothing to do with her speech or language abilities. While addressing mobility is not within the speech-language pathology scope of practice, it is within our scope to appreciate that these factors intersect with the social and physical environments to impact communicative participation. We should work with the client, family, and other members of the intervention team on removing communication barriers in all forms.
Assessing the Communication Environment
Standardized or published measures of communication environments, either physical or social, are lacking. Some instruments such as the Craig Hospital Inventory of Environmental Factors (Whiteneck et al., 2004) address the environment and are geared toward rehabilitation populations, but the Craig Hospital Inventory of Environmental Factors deals mostly with issues related to mobility and is likely not specific enough to serve as a sensitive outcomes measure for modifications of communication environments. Measures of social networks (Blackstone & Berg, 2003) identify the people who are involved in a client's communication environment, but a measure of the size or makeup of a social network is not necessarily a good measure of treatment outcomes unless the client's goal is specifically to change the size or membership of the network. Aspects of the social environment may be reflected in constructs such as social support, but the types of measures of social support used in most health research have been less used in speech-language pathology and may be of questionable relevance to the type of support that enables communicative participation (Eadie et al., 2018). Thus, when assessing the communication environment, clinicians need to rely largely on nonstandardized assessments at this time.
Ideally, clinicians would be able to go into the targeted participation situation with the client to observe, describe, and perhaps measure how characteristics of the physical and social environments serve as barriers to or facilitators of communicative participation. Unfortunately, feasibility limits these opportunities. This is also an area where shared decision making is critical in order to understand what aspects of the environment serve as barriers to and facilitators of participation from the client's viewpoint and what the client most wants to change. Clinicians may want to use or adapt templates such as those presented in the appendixes and Supplemental Materials S1 and S2 for both the physical and social environments that help identify, describe, and measure through client self-report the extent to which various environmental features are seen as a problem or barrier to participation. In this manner, the clinician can quickly see which environmental features are the largest problem, can have a quantitative measurement of baseline status, and can then use these data to formulate corresponding goals to target the areas of environmental modification that are of greatest concern or might have the greatest impact on participation. Clearly, conversations about key communication partners may be delicate, and clinicians need to consider if and how to include other stakeholders in these assessments.
Writing Goals Targeting the Communication Environment
When writing goals that target environmental modification and when planning intervention, we are mindful that the client may have limited control over some environments (e.g., noise in a restaurant, lack of pictures on a restaurant menu). We should counsel the client to work on reducing environmental barriers to communication for which there is a reasonably good potential to have some influence, but still, we cannot guarantee that we can resolve or remove the environmental barriers because some issues may be beyond the client's influence. There may be several ways to approach writing goals to reflect this. One option is to target a reduction of the problem per the client's report such as in the following goal: “Client will report that the extent to which background noise interferes with communication in the targeted situation of conversations at knitting club is 2 or lower (scale 0–5 with 0 = no interference and 5 = extreme interference) by the end of 3 weeks.” Another option is to focus on helping clients develop and implement strategies for managing the environment, even if those strategies do not fully resolve the problem. A goal of this nature would be as follows: “Client will implement a minimum of three strategies focused on reducing background noise in the targeted situation of communication at knitting club over the next three weeks.” Regardless of whether or not the strategies are optimally successful, through the process of developing and attempting the modifications, the client is learning skills that may lead to future improvements in or strategies for reducing environmental barriers. Note that, when writing goals addressing the social environment, rarely do we write goals in which the communication partner is the subject of the goal because most goals need to be written from the perspective of the client. However, in some situations, goals may expressly target behavior change for communication partners, particularly for children with communication disorders or for adult clients who are highly dependent on family or others for communication supports.
Intervention Addressing Environmental Modifications
Intervention to address the environment might take several approaches. One important approach is disclosure to and education of communication partners in the client's targeted situation (W. Murphy, et al., 2007; Trichon & Tetnowski, 2011). The clinician may work with the client (and possibly key communication partners) to practice and implement these strategies. SLPs also play a very important role in terms of helping to generate flexible and creative ideas for other ways that clients can gain better access to places and situations through modifications of those settings or by clients' leveraging of tools, resources, or other facilitative aspects of the environment. A key recommendation here that makes environmental modification part of therapy is that the SLP should remain engaged with the client at every step of planning and implementing environmental modifications. This does not mean handing the client a list of possible strategies and leaving the client to possibly flounder with implementing them on their own. Many clients will not feel comfortable with self-advocacy or other steps needed for environmental modification. As part of therapy sessions, SLPs can help clients explore, formulate, and implement strategies—and follow up with further problem-solving. SLPs may want to adapt approaches such as those used in self-management health programs for coaching and supporting clients (Lorig & Holman, 2003; Yorkston et al., 2017a).
Before leaving this section on the environment, it is worth pausing to reflect further on the reciprocal nature of the social environment, particularly in the context of communication disorders because communication inherently involves interactions among people. In this section, we have discussed how family, friends, coworkers, teachers, and others form the social environment for the client and how optimizing participation outcomes for the client may involve making efforts to improve the actions and behaviors of the people around them. Likewise, however, the client is part of the social environment for these other individuals. Close family members such as parents, spouses or partners, children, and others may experience challenges associated with living with and/or caring for someone with a communication disorder. The WHO ICF refers to this impact of a family member's health condition on an individual as third-party disability. Evidence is emerging documenting the third-party disability that families may experience as a result of their loved one's difficulties with communication (Grawburg et al., 2013; Mach et al., 2019). Similar literature is available relevant to families of children with disabilities that are often associated with communication disorders (Abbeduto et al., 2004; Estes et al., 2009; Guillamón et al., 2013; N. Murphy et al., 2011, 2007; Namkung et al., 2018). This is important for clinicians to recognize and address. Family members likely experience stress associated with increased caregiving burden, additional roles and responsibilities at home, financial strain, and loss of emotional closeness with the client. Placing further responsibilities on family members to learn new accommodations for the person with the communication disorder may compound that stress further. A holistic approach to improving life participation for the client must therefore consider the impact on family or other individuals close to the client and must provide relief for their needs as well using family-centered approaches to therapy (Stone, 1992).
Personal Perspectives
Returning to Figure 2, the remaining component to be considered for its role in shaping communicative participation is personal perspectives, which is reinterpreted from the personal factors component of the WHO ICF. In this component, clinicians are reminded of the critical importance of understanding the many unique characteristics that shape individual responses to living with a communication disorder (Huber et al., 2010). This is where each client represents the intersection of the many cultures to which they belong—cultures that may reflect ethnicity, geography, spirituality, gender identity, family makeup and roles, education and occupation, hobbies and interests, and so forth. In this category, we also consider how each individual approaches their experiences in terms of their life views, coping mechanisms, and priorities and values. Certainly, when it comes to personal factors, there are many aspects of an individual that we could not and should not seek to change. Respect for the individual is paramount. However, there are likely areas within this domain where we can be of help.
Assessing Personal Perspectives
Fear, anxiety, self-consciousness, or a host of other emotional reactions to a communication disorder or difference may contribute to a client's withdrawal from life situations and thus may warrant attention in and of themselves as a focus of intervention (Flasher & Fogle, 2011; Holland & Nelson, 2013; Riley, 2002). Resilience and other coping mechanisms may improve communicative participation even in the context of ongoing impairment. One such construct that has been receiving increased attention is self-efficacy. Self-efficacy refers to the confidence or belief a person has that they can accomplish a task (Bandura, 1977). Self-efficacy may contribute to communicative participation (Boyle et al., 2018) and may be related to favorable intervention outcomes in communication disorders (Babbitt & Cherney, 2010; Bray et al., 2003; Gillespie & Verdolini Abbott, 2011; Hinckley, 2006). Measures related to this construct are emerging such as the Communication Confidence Rating Scale for Aphasia (Babbitt et al., 2011) or the Self-Efficacy Scale for Adult Stutterers (Ornstein & Manning, 1985). However, given the range of other possible personal perspectives or emotional reactions that may warrant attention and the likelihood that there may not be a published measure for many issues that SLPs need to assess, clinicians will likely continue to rely on nonstandardized methods to measure personal perspectives. SLPs may identify the most salient feelings a client is experiencing through a qualitative interview and then use those client-identified terms to form self-anchored rating scales to quantify the construct, as described above (see appendixes for examples). Or the clinician may create a handful of self-anchored scales asking the client to rate different feelings about their communicative participation to find the construct that seems to resonate most with the client. The key is to measure a highly relevant perspective for the client so that it is more likely to guide intervention to meaningful issues and to be sensitive to change with intervention. Caution may be warranted about using general PROs related to constructs such as quality of life. While these are important constructs, many of the general health measures may be too broad in their scope to be sensitive to changes in one communication situation for the client.
Writing Goals for Personal Perspectives
Writing goals for personal perspectives may be very similar to writing goals for environmental modifications, as described above. Goals may target improvement in how the client feels about their participation, implementation of targeted strategies, or other approaches. Most personal perspective goals will likely rely heavily on PROs since they are about the feelings and viewpoint of the client. A good place to start with writing goals is to use the measurement scale from the assessment as an effective way to link assessment, intervention, and outcomes documentation. This is assuming that the construct that was evaluated in the assessment captures a personal perspective, feeling, or attitude with which the client identifies and wants to change. Many feelings and attitudes can be targeted, but if it is not something that is relevant to the client, the construct will not be sensitive to change, nor will any change be meaningful. Thus, goals should be phrased using terms with which the client can identify. For example, a young teen is not likely to use a clinically sounding term such as “self-efficacy” in their vocabulary but will more likely report that they “feel weird” about doing something. Careful, supportive interviewing by the clinician may help to operationalize “feeling weird” in the client's terms, and those terms can then be incorporated into both assessment ratings and corresponding goals related to personal perspectives. As an illustration, perhaps a teen with a reading impairment reports that they feel weird at school because their school requires group class work, and the client is afraid they will “stand out as being different” because of their challenges with reading. Perhaps the goal for that client is as follows: “The client will report that they feel that they stand out in a negative way due to reading difficulties in group academic activities at a level of 4 or lower on a 0–10 scale (0 = I don't feel I stand out at all; 10 = I stand out way too much) by the end of 10 weeks.” Another example of a personal perspectives goal might address implementation of coping strategies. An adult client with disfluency may experience feelings of anxiety or nervousness before entering their target situation of daily team meetings at work. One aspect of their intervention might include implementing calming strategies such as self-talk or focused breathing before entering the situation. A goal for this approach might be as follows: “The client will report implementing strategies designed to calm situational anxiety (focused breathing techniques) in at least three different team meetings at work in the next two weeks.”
Intervention for Personal Perspectives
When approaching interventions for personal coping, we should never assume that the emotional experiences of a communication disorder are commensurate with the degree of physical impairment. Furthermore, SLPs cannot ignore the emotional challenges and simply hope they will resolve by doing more speech and language drills. Even if a complete recovery from the impairment is likely, clients still have to manage the inevitable fear, distress, and concerns that arise during their recovery and that might linger thereafter. Take, for instance, a vocal performer who has vocal fold nodules. While nodules are a highly treatable condition, the diagnosis of nodules is often very distressing, particularly for professional voice users. Even after the nodules are fully resolved, these clients may be left with residual anxiety of the possibility of nodules recurring in the future, thus impacting their willingness to participate in a variety of communication situations. We need to attend to these highly personal concerns directly—and we need to document the immense value of our work in this area to stakeholders by writing goals and measuring outcomes that guide our work and clarify our impact.
The types of intervention to address personal perspectives will be highly individualized. There are many references available to assist clinicians with our long-established role of integrating counseling into intervention (Flasher & Fogle, 2011; Holland & Nelson, 2013; Riley, 2002). Techniques such as motivational interviewing (Behrman, 2006; Rollnick & Miller, 1995) and self-management (Lorig & Holman, 2003; Yorkston et al., 2017a) are additional examples of resources that clinicians may use in all aspects of participation-focused intervention.
Clinical Implications
The purpose of this article is to provide one possible framework with a concrete organizational structure, assessment ideas, and examples of goals and interventions to assist SLPs in translating theoretical biopsychosocial, person-centered constructs into tangible clinical practices. In the framework in Figure 2, the intervention planning process starts with first identifying a specific communicative participation situation that is important to the client to change, assessing participation in that situation, and then writing a corresponding participation-focused goal. Following that, assessments are conducted and goals are established as warranted in each of the areas of communication skills, physical and social environments, and personal perspectives. Conducting assessments and writing goals specifically for each of these areas allow for needs to be identified and progress to be demonstrated separately in each element that contributes to participation. This is helpful in situations where progress might be more rapid in some areas than others. For example, a client and a clinician might notice that, while impairment is improving rapidly, overall participation is not—and that might align with lack of improvement in environmental accessibility or personal perspectives—thus perhaps identifying the need to increase intervention efforts in one of these areas. Attention to each element separately holds the team accountable for exploring and addressing each relevant component that contributes to participation outcomes, while the overall participation goal ensures verification that the elements have indeed come together to culminate in the ultimate outcome of improved participation.
Many clinicians are already weaving person-centered, biopsychosocial elements into their sessions with clients. The question we ask here is if clinicians are making their work in each of these elements part of their formal assessment, documentation, and intervention processes. If we do not systematically assess, write goals for, measure outcomes of, and document our work in each area of communication skills, environmental factors, and personal perspectives related to life participation, we run a very high risk of not identifying critical areas where we could be of service to clients, of not being as helpful to our clients as we could be, and of not making it abundantly clear to other stakeholders such as referral and funding sources how valuable our work is with clients in terms of the breadth and depth of how we can bring meaningful changes to clients' lives. If we do not do these things in a value-driven health care environment, we may be undermining the value we bring to our clients and how we prove the value of our services to stakeholders. We may be selling our profession and our clients short.
In considering a participation-focused framework such as the one proposed in this article, several questions related to clinical practice might arise. Are some of these factors such as environmental and personal factors within our scope of practice? Are they within our domain of “skilled services” warranting reimbursement? We would argue not only for the importance of taking a participation-focused approach but also that a truly comprehensive and holistic approach demands the skilled services of SLPs. Our profession (along with audiology) has long been recognized as the experts in communication disorders, and that includes all aspects of communication disorders—the physical impairment and the environmental and personal factors. Clearly, there are boundaries to our scope of practice, but that does not negate the importance of our role as holistic providers caring for a diverse range of issues related to living with a communication disorder. However, if we want recognition for this holistic work, if we want to be called on to do more of this important work, and if we want to be reimbursed for that work, we need to make evident to all stakeholders, through the formal mechanisms of our goals and outcomes data, the wide-reaching and profound impact we can and do have in clients' lives.
Successful implementation of participation-focused intervention would ideally be supported by more than frameworks and guidelines. First, future research, including research that follows the principles of implementation science (Olswang & Prelock, 2015), evidence-based practice (Sackett et al., 2000), and practice-based research (Crooke & Olswang, 2015), is needed to contribute to the evidence base regarding the efficacy and effectiveness of intervention approaches such as this. Second, SLPs need additional resources to implement the diverse and creative therapy approaches required to help clients achieve their maximal possible outcomes. These resources include training, assessment and intervention materials, and funding support. Logistical aspects of clinical services such scheduling, session length, treatment location, and other features of treatment also need to be more flexible to implement patient-centered approaches. Some programs, largely in university clinics or freestanding community clinics, have been able to exercise that flexibility to initiate group programs, centers, and other community programs (Byrd et al., 2016; Elefant et al., 2012; Elman, 2016; Glista & Pollens, 2007; Mackenzie et al., 2012; Ross et al., 2006; Shih et al., 2012; Simmons-Mackie & Holland, 2011). However, we would argue that, while these are highly beneficial, participation-focused intervention does not require groups and centers. Even if SLPs are constrained to short sessions within the four walls of their one-on-one treatment rooms, they can still pursue an intervention path that starts with asking each client, “What is your most important conversation?”
Supplementary Material
Acknowledgments
This work is supported in part by a grant from the National Institute on Deafness and Other Communication Disorders (R01 DC012510, awarded to Baylor). We also acknowledge the contributions of research participants in prior studies for their insights that have driven this article.
Appendix A
Adult Example
Client background: Susanna is a 38-year-old female with vocal nodules who works full-time as a team-lead in a technical field. She works in an open floor plan office environment.
Step 1: Assess baseline overall communicative participation
Susanna's score on the general short form of the Communicative Participation Item Bank (CPIB) was T = 55. The maximum possible score on this short form, indicating no interference with participation is T = 71, so this client is scoring approximately 1.5 SDs lower than a typical adult reporting no communicative participation restrictions.
Step 2: Select a specific situation to target in intervention
Susanna wants to work on participation in social conversations with colleagues at work (going out to lunch, visiting on breaks, etc.). She reports that she is getting by ok with required work communication, but tends to hold back more than she would like from social communication with colleagues at work. She would like to change that, particularly because she sees connecting with her team members on a social basis at work as important to her success as a team lead.
Step 3: Measure baseline participation in the chosen situation and write participation-focused goals
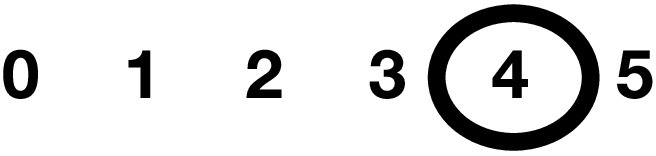
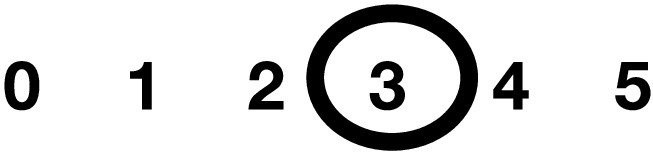
Example of baseline measurement using Goal-Attainment Scaling (client's response is circled)
| +2 | I don't feel as if I'm holding back at all from social communication at work. I feel included and I genuinely enjoy it. |
| +1 | I engage in most social interactions at work that would typically would. I enjoy them more than not, but still hold back and am not entirely comfortable. |
| 0 | I engage in social situations that I feel I ‘have to’ or that are really important, but others that I might enjoy I still avoid. I'm mostly involved but not entirely. While I don't particularly enjoy the situations, they are not miserable. |

|
Social interactions at work make me nervous and uncomfortable. I avoid most of them unless it is going to be really obvious or hurtful to someone if I avoid them. These interactions are a ‘duty’ but not enjoyable because I feel stressed. |
| −2 | I avoid all social interaction at work that I possibly can, even if it risks offending other people. I feel miserable when I think about social interactions because of feeling nervous and self-conscious. |
Goal: Client will report that she is at the “+1” level on her goal-attainment scale (see above) representing that she is engaging in most of her highly valued social communication situations at work with a moderate level of comfort by the end of 10 weeks.
Step 4: Measure baseline communication skills in the chosen situation and write skills-based goals
Baseline measurement and data: As part of a comprehensive diagnostic voice evaluation, the client's voice quality was rated using the Consensus Auditory Perceptual Evaluation of Voice (CAPE-V) (Kempster et al., 2009). This involves a 100-mm visual analog scale (0 = normal; 100 = severely impaired). Overall voice quality (rated by SLP) = 62, roughness = 45, breathiness = 55, strain = 50, pitch (low) = 25, and loudness (too quiet) = 35.
Goal: Client will demonstrate all aspects of voice quality at an SLP-judged rating of 15 or lower on the CAPE-V protocol by the end of 12 weeks.
Step 5: Measure baseline environmental barriers in the chosen situation and write relevant goals for environmental modifications
Baseline measurement and data:
Physical Environment: This table reflects client report and is completed via interview.
| Environmental feature | What works well? | What does NOT work well? | How much of a problem is this per client report? (0 = none; 5 = extreme |
|---|---|---|---|
| Noise | Noise is usually lower if we go during non-traditional lunch hour. When it is my turn to choose the restaurant I always choose the quietest one I know. | Most restaurants we go to are so noisy that I often just can't be heard. |
|
|
Space
(large rooms; outside) |
When I sit in the middle of the table—kind of the center—I feel I can be heard better than if I am way at one end. | When we have one really large table and I am at a far end, people at the other end often cannot understand me. |
|
| Phone | Not relevant to this situation | 0 1 2 3 4 5 | |
|
Other technology
(automated phone systems, drive-through intercoms, etc.) |
Not relevant to this situation other than when it is my turn to make the reservation. Most restaurants use online reservations so I don't have to call. |

|
|
|
Being able to see/be seen by communication partners
(different rooms) |
When people watch me when I am talking I think it works better—I try to use gestures and facial expression to help convey my message. | This is not a huge issue except when the food comes and people are paying attention to their plates instead of looking at who is talking, I think people understand me less well. |
|
|
Things I need to read
(computer, textbooks, etc.) |
Not relevant to this situation | 0 1 2 3 4 5 | |
|
Things I need to write
(forms, e-mails) |
Not relevant to this situation | 0 1 2 3 4 5 |
Social Environment: This table reflects client report and is completed via interview.
| Person | How do they help with communication? | What is NOT helpful for communication? | How much of a problem is this per client report? (0 = none; 5 = extreme) |
|---|---|---|---|
| Everyone | Co-workers know that in general I'm having problems with my voice and when I seem reluctant to go to lunch with them, they always encourage me to come along. They are friendly and supportive in a general way. | While they are generally supportive, they don't really pay attention to my voice problems in the situation—meaning they don't seem to be aware that they should or could change anything. |

|
| Everyone | It is a lively group. Conversations are usually fast-paced and loud. These are not quiet, shy people! |

|
|
| Kayla and Micah | They tend to dominate the conversations. They interrupt frequently so it kind of feels like ‘verbal combat’ sometimes. |

|
|
| Alejandra | She seems to ‘get it’ in terms of being aware of my problem more than anyone. Often if we end up sitting together, she and I will just visit and she kind of has this attitude of ‘ignore everyone else if they are difficult—let's just visit.’ |

|
Goals (2 examples as options):
1. Client will implement two strategies to educate communication partners about her communication needs in social situations at work by the end of 4 weeks.
2. Client will report that the extent to which group dynamics (talking over each other; fast conversations) interfere with her participation in conversations in social situations at work is at a level of 2 or lower (scale of 0–5 with 0 = no problem, 5 = extreme problem) by the end of 4 weeks.
Step 6: Measure baseline relevant coping constructs in the chosen situation and write goals
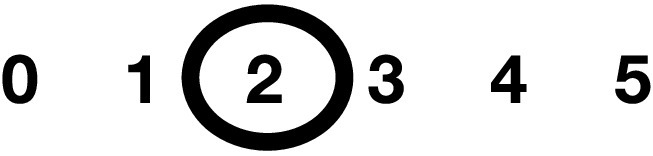
Baseline measurement and data: Susanna reports feeling very nervous about social interactions at work. She feels her nerves might be as much of an issue holding her back as her actual voice quality. We captured her baseline level through the following scale (client's response is circled):
How nervous do you feel about communicating in social activities at work (such as office lunch outings)?
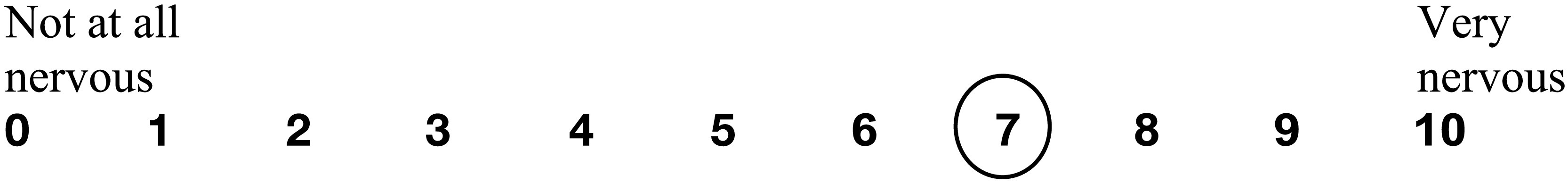
Goals (2 examples as options):
1. Client will report experiencing a level of nervousness about communicating in social interactions in work settings as a 3 or lower (scale of 0–10; 0 = not at all nervous, 10 = very nervous) by the end of 6 weeks.
2. Client will report implementing calming strategies (deep breathing, refocusing, self-talk) on at least four occasions in social conversations at work by the end of 2 weeks.
Appendix B
Teen Example
Client background: Sam is a 14-year-old female with dysarthria due to cerebral palsy. Sam recently transitioned to a new school at the start of 9th grade. Sam's parents have requested a speech evaluation as they are concerned about a perceived decline in speech intelligibility following a large growth spurt this summer. Sam's parents report that Sam seems socially isolated and lonely since starting high school. They believe this is due to Sam's speech intelligibility. Sam has a history of speech therapy but has not received services in several years.
Step 1: Assess baseline overall communicative participation
Although Sam's parents are key stakeholders, Sam is the expert and should be consulted. Using the Speech Participation and Activity Assessment of Children (SPAA-C) (McLeod, 2004) as a guide for an interview, you learn that Sam is not concerned about her speech. Sam recognizes that her speech has gotten worse recently, but she does not believe that her speech impacts her ability to be social. Sam states that her primary barrier to successful communication is her ability to type, text, and write (i.e., fine motor skills). This makes schoolwork and keeping in touch with friends outside of school difficult. Sam has also stopped participating in organized activities outside of school (e.g., sports) due to the increased academic demands of high school.
Step 2: Select a specific situation to target in intervention
Sam would like to be more involved in conversations with her friends outside of school. Sam and her friends use text based messaging apps to communicate outside of school. Because of her fine motor skills, Sam responds slowly and has difficulty keeping up with the conversation.
Step 3: Measure baseline participation in the chosen situation and write participation-focused goals
Baseline method of measurement and data:
Example using a Likert scale (Sam's responses are circled):
How satisfied are you with your involvement in conversations with your friends outside of the school setting (regardless of mode of communication)?

Goals:
1. Sam will report a level of satisfaction with communicative participation in conversations with friends outside of the school setting (regardless of the mode of communication) as an 8 or higher on a scale of 0–10 (with 0 = not at all satisfied and 10 = very satisfied) by the end of 10 weeks.
2. Using talk-to-text software, Sam will initiate conversations via text message with a friend on three separate occasions by the end of 3 weeks.
Step 4: Measure baseline communication skills in the chosen situation and write skills-based goals
Baseline method of measurement and data: Sam's speech intelligibility per the Test of Children's Speech (TOCS+; Hodge & Daniels, 2009) is 85% intelligible in sentences. When the TOCS+ is replicated with listeners rating in the context of background environmental noise (simulating a noisy community setting), sentence intelligibility drops to 70%. During a trial of talk-to-text software, Sam's intelligibility deficits result in transcription errors 60% of the time.
Goal: Using clear speech strategies, Sam will compose at least 5 messages via talk-to-text software that are each 85% accurate by the end of 6 weeks.
Step 5: Measure baseline environmental barriers in the chosen situation and write relevant goals for environmental modifications
Baseline method of measurement and data:
Physical Environment: This table reflects Sam's report and is completed in an interview.
| Environmental feature | What works well? | What does NOT work well? | How much of a problem is this per client report? (0 = none; 5 = extreme) |
|---|---|---|---|
| Noise | Not relevant to this situation | 0 1 2 3 4 5 | |
|
Space
(large rooms; outside) |
Not relevant to this situation | 0 1 2 3 4 5 | |
| Phone | We don't not talk on the phone. We only text. | 0 1 2 3 4 5 | |
|
Other technology
(automated phone systems, drive-through intercoms, etc.) |
Siri never understands me. |
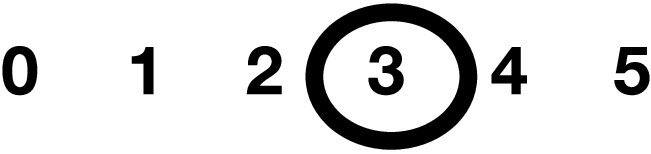
|
|
| Being able to see/be seen by communication partners | My friends and I do not video message. We only text. | 0 1 2 3 4 5 | |
|
Things I need to read
(computer, textbooks, etc.) |
Not relevant to this situation | 0 1 2 3 4 5 | |
|
Things I need to write
(forms, e-mails) |
NOTHING! | EVERYTHING! |

|
Social Environment: This table reflects Sam's report and is completed in an interview.
| Person | How do they help with communication? | What is NOT helpful for communication? | How much of a problem is this per client report? (0 = none; 5 = extreme) |
|---|---|---|---|
| Everyone | My friends don't know that it is hard for me to text. They just think I am too busy to talk. | Everyone types so fast during group texting. Once I have written a response to a comment, that conversation is over and my response doesn't make sense. |

|
Goals:
1. Sam will implement two strategies to educate friends about her communication needs when texting by the end of 3 weeks (e.g., Sam texting a single character to let friends know to wait while she composes a message; friends ask if she has something to add before they close a chat).
2. Sam will rate the negative impact of her inefficiency in texting on participation in conversations with friends at a level of 2 or lower (scale of 0–5 with 0 = no problem, 5 = extreme problem) by the end of 6 weeks because of use of smartphone supports such as word prediction.
Step 6: Measure baseline relevant coping constructs in the chosen situation and write goals
Baseline method of measurement and data: To assess Sam's personal views of her skills in oral communication vs. written communication, you might capture her baseline level through the following scales (Sam's response is circled):
How confident are you in your ability to communicate using speech?
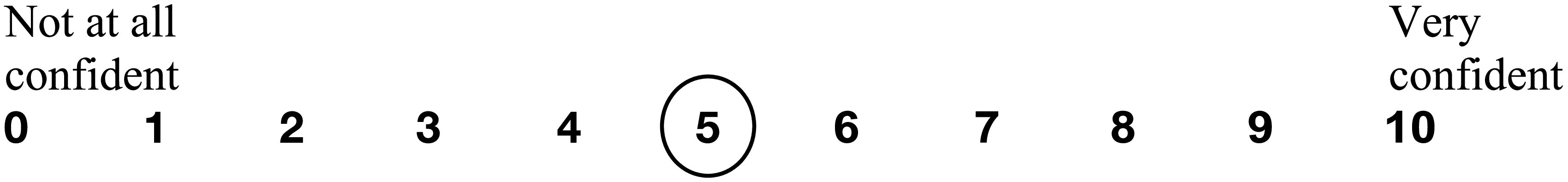
How confident are you in your ability to communicate using writing/texting?

Goals:
1. Sam will report experiencing a confidence level of 8 or higher (scale of 0–10; 0 = not at all confident, 10 = very confident) when using oral communication with her friends outside of school by the end of 6 weeks.
2. Sam will report experiencing a confidence level of 7 or higher (scale of 0–10; 0 = not at all confident, 10 = very confident) when using written/text communication with her friends outside of school by the end of 6 weeks.
Appendix C
Child Example
Client background: Our client is a 7-year-old male, Hector, with developmental language disorder and suspected dyslexia.
Step 1: Assess baseline overall communicative participation
Using the Speech Participation and Activity Assessment of Children (SPAA-C) (McLeod, 2004) as a guide for the interview, Hector's teacher reports that Hector rarely, if ever, voluntarily communicates with peers at school, and he often appears withdrawn during classroom activities. When Hector does attempt to participate, communication breakdowns happen frequently. At these times, Hector becomes frustrated and acts aggressively. Hector's teacher has noticed that Hector's self-confidence in his reading ability has decreased to the point that he now refuses to try to read independently. Hector reports that he feels sad about his ability to communicate in classroom activities via the SPAA-C child form that allows users to answer by pointing to a smiley face, a neutral face, or a sad face.
Step 2: Select a specific situation to target in intervention (replicate this process for other situations)
During the interview, Hector reports that his favorite classroom activity is when his teacher reads aloud to the students during daily story time. Hector likes listening to stories but states that his teacher reads too fast and it is hard to participate in the class discussion about the story because the other students answer questions so quickly. Hector's teacher agrees that story time is the time that Hector is most likely to attempt to participate. Given the frequency of communication breakdowns, this is often the time he is most likely to act aggressively toward other students.
Step 3: Measure baseline participation in the chosen situation and write participation-focused goals
Baseline method of measurement and data:
Example using Goal-Attainment Scaling (Hector's teacher's response is circled):
| +2 | Hector participates during story time with minimal prompting, and communication breakdowns are infrequent. Hector is able to manage his frustration by using communication repair strategies with minimal reminders. |
| +1 | Hector participates during story time with minimal prompting, but communication breakdowns are frequent. Hector is able to manage his frustration by using communication repair strategies with minimal reminders. |
| 0 | Hector participates during story time with moderate prompting. Communication breakdowns are frequent. Hector only utilizes communication repair strategies with reminders and prompts, but his frustration is low during communication breakdowns and he does not aggressively toward students. |
| −1 | Hector participates during story time with moderate prompting. Communication breakdowns are frequent. Hector only uses communication repair strategies with reminders and cues. Hector is highly frustrated during communication breakdowns but does not act aggressively toward students. |

|
Hector rarely participates during story time. When he does, communication breakdowns are frequent. Hector does not use any communication repair strategies. He becomes highly frustrated and aggressive toward students. |
Goals:
1. Hector's teacher will report a level of 0 or higher on the goal-attainment scale by the end of 10 weeks indicating that he is participating in story time with moderate prompting and using repair strategies with cues in that situation with a low level of frustration and no aggressive behaviors.
2. Hector will indicate that he was happy while participating in story time by pointing to a happy face (rather than a neutral or sad face) after 6 out of 10 story time sessions by the end of 10 weeks.
Step 4: Measure baseline and write any relevant goals for communication skills
Baseline method of measurement and data: The Test of Integrated Language and Literacy Skills (TILLS) is a norm-referenced test that is valid for the identification of language and literacy disorders (Nelson et al., 2016). Using the Identification Core score for 6- to 7-year-olds, Hector's score of 19 is consistent with the presence of a language/literacy disorder. In order to participate in class room story time, you decide to target both a language comprehension goal and a language formulation goal.
Goals:
1. Hector will answer “where” questions by pointing to the correct object in a picture book 85% of naturally occurring opportunities in 2 story-telling/joint reading sessions with the clinician with minimal cueing by the end of 4 weeks.
2. Hector will demonstrate correct verbal use of prepositions (‘beside,’ ‘under,’ etc.) in 8 out of 10 opportunities during picture description tasks with the clinician with minimal cueing by the end of 4 weeks.
Step 5: Measure baseline and write any relevant goals for environmental modifications
Baseline method of measurement and data:
Physical Environment: This table reflects input from Hector and Hector's teacher as well as SLP observation.
| Environmental feature | What works well? | What does NOT work well? | How much of a problem is this per client report? (0 = none; 5 = extreme) |
|---|---|---|---|
| Noise | Hector is able to attend to the story when only the teacher is speaking. | Other students often interrupt or talk during story time. |
|
|
Space
(large rooms; outside) |
Hector participates more frequently when given preferential seating (close to the teacher) during story time. | Hector is distracted and withdrawn when he sits far away from the teacher during story time. |
|
| Phone | Not relevant to this situation | 0 1 2 3 4 5 | |
|
Other technology
(automated phone systems, drive-through intercoms, etc.) |
Not relevant to this situation | 0 1 2 3 4 5 | |
|
Being able to see/be seen by communication partners
(different rooms) |
When Hector can maintain eye contact with his communication partner | The children are often looking at the teacher during story time and not at each other. If Hector is at the back of the story time circle, he has a harder time maintaining eye contact with the teacher. |
|
|
Things I need to read
(computer, textbooks, etc.) |
Picture books | Chapter books with few pictures and little context for vocabulary |

|
|
Things I need to write
(forms, e-mails) |
Not relevant to this situation | 0 1 2 3 4 5 |
Social Environment: This table reflects input from both Hector and Hector's teacher as well as SLP observation.
| Person | How do they help with communication? | What is NOT helpful for communication? | How much of a problem is this per client report? (0 = none; 5 = extreme) |
|---|---|---|---|
| Hector's teacher | She is aware that it is difficult for him to understand and reads at a good pace. | She often tries to finish Hector's message for him because it takes so long for him to formulate an answer. |

|
| Alysia (student in class) | Is very patient with Hector and always allows him to finish his thoughts. She never seems to have trouble understanding him. |

|
|
| Everyone | Students often talk over one another in an attempt to answer the teacher's questions about the story first. Hector does not have time to formulate an answer before everyone else jumps in. |

|
Goals:
1. Hector will be given preferential seating (close to the teacher) in 4 out of 5 daily story time sessions in the classroom by the end of 1 week.
2. Hector and his SLP will educate Hector's teacher and peers about two listener-managed strategies (e.g., maintaining eye contact, allowing ample time to formulate and finish a message, etc.) that can be utilized when communicating with Hector by the end of 2 weeks.
Step 6: Measure baseline and write any relevant goals for personal perspectives and coping
Baseline method of measurement and data: Hector's frustration related to his communication manifests in aggressive behavior toward other students. Hector's teacher reports that he exhibits at least 2 aggressive behaviors during daily story time (~10 behaviors per week).
Goals:
1. Hector will exhibit 1 or fewer aggressive behaviors (as an indication of low frustration levels) during each daily story time per teacher report by the end of 2 weeks.
Funding Statement
This work is supported in part by a grant from the National Institute on Deafness and Other Communication Disorders (R01 DC012510, awarded to Baylor).
References
- Abbeduto, L. , Seltzer, M. , Shattuck, P. , Krauss, M. , Orsmond, G. , & Murphy, M. (2004). Psychological well-being and coping in mothers of youths with autism, Down syndrome, or fragile X syndrome. American Journal on Mental Retardation, 109(3), 237–254. https://doi.org/10.1352/0895-8017(2004)109<237:PWACIM>2.0.CO;2 [DOI] [PubMed] [Google Scholar]
- Babbitt, E. , & Cherney, L. R. (2010). Communication confidence in persons with aphasia. Topics in Stroke Rehabilitation, 17(3), 214–223. https://doi.org/10.1310/tsr1703-214 [DOI] [PubMed] [Google Scholar]
- Babbitt, E. , Heinemann, A. W. , Semik, P. E. , & Cherney, L. R. (2011). Psychometric properties of the Communication Confidence Rating Scale for Aphasia (CCRSA): Phase 2. Aphasiology, 25(6–7), 727–735. https://doi.org/10.1080/02687038.2010.537347 [DOI] [PubMed] [Google Scholar]
- Bandura, A. (1977). Self-efficacy: Toward a unifying theory of behavioral change. Psychological Review, 84(2), 191–215. https://doi.org/10.1037/0033-295X.84.2.191 [DOI] [PubMed] [Google Scholar]
- Baum, C. (2011). Fulfilling the promise: Supporting participation in daily life. Archives of Physical Medicine and Rehabilitation, 92(2), 169–175. https://doi.org/10.1016/j.apmr.2010.12.010 [DOI] [PubMed] [Google Scholar]
- Baylor, C. , Burns, M. , Eadie, T. , Britton, D. , & Yorkston, K. (2011). A qualitative study of interference with communicative participation across communication disorders in adults. American Journal of Speech-Language Pathology, 20(4), 269–287. https://doi.org/10.1044/1058-0360(2011/10-0084) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , Burns, M. , McDonough, K. , Mach, H. , & Yorkston, K. (2019). Teaching medical students skills for effective communication with patients who have communication disorders. American Journal of Speech-Language Pathology, 28(1), 155–164. https://doi.org/10.1044/2018_AJSLP-18-0130 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , McAuliffe, M. , Hughes, L. , Yorkston, K. , Anderson, T. , Kim, J. , & Amtmann, D. (2014). A differential item functioning (DIF) analysis of the Communicative Participation Item Bank (CPIB): Comparing individuals with Parkinson's disease from the United States and New Zealand. Journal of Speech, Language, and Hearing Research, 57(1), 90–95. https://doi.org/10.1044/1092-4388(2013/12-0414) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , Oelke, M. , Bamer, A. , Hunsaker, E. , Off, C. , Wallace, S. , Pennington, S. , Kendall, D. , & Yorkston, K. (2017). Validating the Communicative Participation Item Bank (CPIB) for use with people with aphasia: An analysis of differential item function (DIF). Aphasiology, 31(8), 861–878. https://doi.org/10.1080/02687038.2016.1225274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , Yorkston, K. , & Eadie, T. (2005). The consequences of spasmodic dysphonia on communication-related quality of life: A qualitative study of the insider's experiences. Journal of Communication Disorders, 38(5), 395–419. https://doi.org/10.1016/j.jcomdis.2005.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , Yorkston, K. , Eadie, T. , Kim, J. , Chung, H. , & Amtmann, D. (2013). The Communicative Participation Item Bank (CPIB): Item bank calibration and development of a disorder-generic short form. Journal of Speech, Language, and Hearing Research, 56(4), 1190–1208. https://doi.org/10.1044/1092-4388(2012/12-0140) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baylor, C. , Yorkston, K. M. , Eadie, T. L. , & Maronian, N. (2007). The psychosocial consequences of BOTOX injections for spasmodic dysphonia: A qualitative study of patients' experiences. Journal of Voice, 21(2), 231–247. https://doi.org/10.1016/j.jvoice.2006.01.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behrman, A. (2006). Facilitating behavioral change in voice therapy: The relevance of motivational interviewing. American Journal of Speech-Language Pathology, 15(3), 215–225. https://doi.org/10.1044/1058-0360(2006/020) [DOI] [PubMed] [Google Scholar]
- Beitchman, J. , Wilson, B. , Brownlie, E. , Walters, H. , & Lancee, W. (1996). Long-term consistency in speech/language profiles: I. Developmental and academic outcomes. Journal of the American Academy of Child & Adolescent Psychiatry, 35(6), 804–814. https://doi.org/10.1097/00004583-199606000-00021 [DOI] [PubMed] [Google Scholar]
- Beitchman, J. , Wilson, B. , Brownlie, E. , Walters, H. , Inglis, A. , & Lancee, W. (1996). Long-term consistency in speech/language profiles: II. Behavioral, emotional, and social outcomes. Journal of the American Academy of Child & Adolescent Psychiatry, 35(6), 815–825. https://doi.org/10.1097/00004583-199606000-00022 [DOI] [PubMed] [Google Scholar]
- Bellon-Harn, M. , Azios, J. , Dockens, A. , & Manchaiah, V. (2017). Speech-language pathologists' preferences for patient-centeredness. Journal of Communication Disorders, 68, 81–88. https://doi.org/10.1016/j.jcomdis.2017.06.012 [DOI] [PubMed] [Google Scholar]
- Blackstone, S. W. , & Berg, M. H. (2003). Social networks: A communication inventory for individuals. Augmentative Communication, Inc. [Google Scholar]
- Bolt, S. , Eadie, T. , Yorkston, K. , Baylor, C. , & Amtmann, D. (2016). Variables associated with communicative participation after head and neck cancer. JAMA Otolaryngology—Head & Neck Surgery, 142(12), 1145–1151. https://doi.org/10.1001/jamaoto.2016.1198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bothe, A. , & Richardson, J. (2011). Statistical, practical, clinical, and personal significance: Definitions and applications in speech-language pathology. American Journal of Speech-Language Pathology, 20(3), 233–242. https://doi.org/10.1044/1058-0360(2011/10-0034) [DOI] [PubMed] [Google Scholar]
- Bovend'Eerdt, T. , Botell, R. , & Wade, D. T. (2009). Writing SMART rehabilitation goals and achieving goal attainment scaling: A practical guide. Clinical Rehabilitation, 23(4), 352–361. https://doi.org/10.1177/0269215508101741 [DOI] [PubMed] [Google Scholar]
- Boyle, M. , Beita-Ell, C. , Milewski, K. , & Fearon, A. (2018). Self-esteem, self-efficacy, and social support and predictors of communicative participation in people who stutter. Journal of Speech, Language, and Hearing Research, 61(8), 1893–1906. https://doi.org/10.1044/2018_JSLHR-S-17-0443 [DOI] [PubMed] [Google Scholar]
- Brandenburg, C. , Worrall, L. , Rodriguez, A. , & Bagraith, K. (2015). Crosswalk of participation self-report measures for aphasia to the ICF: What content is being measured? Disability and Rehabilitation, 37(13), 1113–1124. https://doi.org/10.3109/09638288.2014.955132 [DOI] [PubMed] [Google Scholar]
- Bray, M. A. , Kehle, T. J. , Lawless, K. A. , & Theodore, L. A. (2003). The relationship of self-efficacy and depression to stuttering. American Journal of Speech-Language Pathology, 12(4), 425–431. https://doi.org/10.1044/1058-0360(2003/088) [DOI] [PubMed] [Google Scholar]
- Brewster, S. (2004). Insights from a social model of literacy and disability. Literacy, 38(1), 46–51. https://doi.org/10.1111/j.0034-0472.2004.03801008.x [Google Scholar]
- Bricker-Katz, G. , Lincoln, M. , & McCabe, P. (2009). A life-time of stuttering: How emotional reactions to stuttering impact activities and participation in older people. Disability and Rehabilitation, 31(21), 1742–1752. https://doi.org/10.1080/09638280902738672 [DOI] [PubMed] [Google Scholar]
- Brown, M. , Dijkers, M. P. J. M. , Gordon, W. A. , Ashman, T. , Charatz, H. , & Cheng, Z. (2004). Participation objective, participation subjective: A measure of participation combining outsider and insider perspectives. The Journal of Head Trauma Rehabilitation, 19(6), 459–481. https://doi.org/10.1097/00001199-200411000-00004 [DOI] [PubMed] [Google Scholar]
- Brutten, E. , & Vanryckeghem, M. (2007). BAB: Behavior Assessment Battery for school-age children who stutter. Plural Publishing. [Google Scholar]
- Burns, M. , Baylor, C. R. , Morris, M. , McNalley, T. , & Yorkston, K. M. (2012). Training healthcare providers in patient–provider communication: What medical education and speech-language pathology can learn from one another. Aphasiology, 26(5), 673–688. https://doi.org/10.1080/02687038.2012.676864 [Google Scholar]
- Byrd, C. , Chmela, K. , Coleman, C. , Weidner, M. , Kelly, E. , Reichhardt, R. , & Irani, F. (2016). An introduction to camps for children who stutter: What they are and how they can help. Perspectives of the ASHA Special Interest Groups, 1(4), 55–69. https://doi.org/10.1044/persp1.SIG4.55 [Google Scholar]
- Cardol, M. , de Jong, B. A. , van den Bos, G. A. M. , Beelen, A. , de Groot, I. J. M. , & de Haan, R. J. (2002). Beyond disability: Perceived participation in people with a chronic disabling condition. Clinical Rehabilitation, 16(1), 27–35. https://doi.org/10.1191/0269215502cr464oa [DOI] [PubMed] [Google Scholar]
- Chapey, R. , Duchan, J. F. , Elman, R. J. , Garcia, L. J. , Kagan, A. , Lyon, J. , & Simmons Mackie, N. N. (2000). Life participation approach to aphasia: A statement of values for the future. The ASHA Leader, 5(3), 4–6. https://doi.org/10.1044/leader.FTR.05032000.4 [Google Scholar]
- Collis, J. , & Bloch, S. (2012). Survey of UK speech and language therapists' assessment and treatment practices for people with progressive dysarthria. International Journal of Language & Communication Disorders, 47(6), 725–737. https://doi.org/10.1111/j.1460-6984.2012.00183.x [DOI] [PubMed] [Google Scholar]
- Crooke, P. , & Olswang, L. (2015). Practice-based research: Another pathway for closing the research–practice gap. Journal of Speech, Language, and Hearing Research, 58(6), S1871–S1882. https://doi.org/10.1044/2015_JSLHR-L-15-0243 [DOI] [PubMed] [Google Scholar]
- Cruice, M. (2008). The contribution and impact of the International Classification of Functioning, Disability and Health on qualify of life in communication disorders. International Journal of Speech-Language Pathology, 10(1–2), 38–49. https://doi.org/10.1080/17549500701790520 [Google Scholar]
- Cruice, M. , Johansson, M. , Isaksen, J. , & Horton, S. (2018). Reporting interventions in communication partner training: A critical review and narrative synthesis of the literature. Aphasiology, 32(10), 1135–1166. https://doi.org/10.1080/02687038.2018.1482406 [Google Scholar]
- Dalemans, R. , de Witte, L. , Wade, D. T. , & van den Heuvel, W. J. A. (2008). A description of social participation in working-age persons with aphasia: A review of the literature. Aphasiology, 22(10), 1071–1091. https://doi.org/10.1080/02687030701632179 [Google Scholar]
- Dalemans, R. , de Witte, L. , Wade, D. T. , & van den Heuvel, W. J. A. (2010). Social participation through the eyes of people with aphasia. International Journal of Language & Communication Disorders, 45(5), 537–550. https://doi.org/10.3109/13682820903223633 [DOI] [PubMed] [Google Scholar]
- Darling-White, M. (2017). Towards a measure of communicative participation for children with developmental speech disorders. Seminars in Speech and Language, 38(3), 184–190. https://doi.org/10.1055/s-0037-1602837 [DOI] [PubMed] [Google Scholar]
- Davidson, B. , Howe, T. , Worrall, L. , Hickson, L. , & Togher, L. (2008). Social participation for older people with aphasia: The impact of communication disability on friendships. Topics in Stroke Rehabilitation, 15(4), 325–340. https://doi.org/10.1310/tsr1504-325 [DOI] [PubMed] [Google Scholar]
- de Riesthal, M. , & Ross, K. (2015). Patient reported outcome measrues in neurologic communication disorders: An update. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders, 25(3), 114–120. https://doi.org/10.1044/nnsld25.3.114 [Google Scholar]
- DiLollo, A. , & Favreau, C. (2010). Person-centered care and speech and language therapy. Seminars in Speech and Language, 31(2), 90–97. https://doi.org/10.1055/s-0030-1252110 [DOI] [PubMed] [Google Scholar]
- Donovan, N. (2012). Patient-reported outcomes for acquired dysarthria. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders, 22(4), 152–159. https://doi.org/10.1044/nnsld22.4.152 [Google Scholar]
- Duchan, J. F. (2001). Impairment and social views of speech-language pathology: Clinical practices re-examined. Advances in Speech-Language Pathology, 3(1), 37–45. https://doi.org/10.3109/14417040109003707 [Google Scholar]
- Eadie, T. , Kapsner-Smith, M. , Bolt, S. , Sauder, C. , Yorkston, K. , & Baylor, C. (2018). The relationship between perceived social support and patient-reported communication outcomes across communication disorders: A systematic review. International Journal of Language & Communication Disorders, 53(6), 1059–1077. https://doi.org/10.1111/1460-6984.12417 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eadie, T. , Otero, D. , Cox, S. , Johnson, J. , Baylor, C. , Yorkston, K. , & Doyle, P. (2016). The relationship between communicative participation and post-laryngectomy speech outcomes. Head & Neck, 38(S1), E1955–E1961. https://doi.org/10.1002/hed.24353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eadie, T. , Yorkston, K. , Klasner, E. R. , Dudgeon, B. J. , Deitz, J. , Baylor, C. , Miller, R. M. , & Amtmann, D. (2006). Measuring communicative participation: A review of self-report instruments in speech-language pathology. American Journal of Speech-Language Pathology, 15(4), 307–320. https://doi.org/10.1044/1058-0360(2006/030) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elefant, C. , Baker, F. , Lotan, M. , Lagesen, S. , & Skeie, G. (2012). The effect of group music therapy on mood, speech, and singing in individuals with Parkinson's disease—A feasibility study. Journal of Music Therapy, 49(3), 278–302. https://doi.org/10.1093/jmt/49.3.278 [DOI] [PubMed] [Google Scholar]
- Elman, R. J. (2016). Aphasia centers and the life participation approach to aphasia: A paradigm shift. Topics in Language Disorders, 36(2), 154–167. https://doi.org/10.1097/TLD.0000000000000087 [Google Scholar]
- Eriksson, K. , Forsgren, E. , Hartelius, L. , & Saldert, C. (2016). Communication partner training of enrolled nurses working in nursing homes with people with communication disorders caused by stroke or Parkinson's disease. Disability and Rehabilitation, 38(12), 1187–1203. https://doi.org/10.3109/09638288.2015.1089952 [DOI] [PubMed] [Google Scholar]
- Estes, A. , Munson, J. , Dawson, G. , Koehler, E. , Zhou, X.-H. , & Abbott, R. (2009). Parenting stress and psychological functioning among mothers of preschool children with autism and developmental delay. Autism, 13(4), 375–387. https://doi.org/10.1177/1362361309105658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flasher, L. , & Fogle, P. (2011). Counseling skills for speech-language pathologists and audiologists (2nd ed.). Singular Publishing. [Google Scholar]
- Forsgren, E. , Hartelius, L. , & Saldert, C. (2017). Improving medical students' knowledge and skill in communicating with people wtih acquired communication disorders. International Journal of Speech-Language Pathology, 19(6), 541–550. https://doi.org/10.1080/17549507.2016.1216602 [DOI] [PubMed] [Google Scholar]
- Fox, L. E. (2012). Self-anchored rating scales: Creating partnerships for post-aphasia change. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders, 22(1), 18–27. https://doi.org/10.1044/nnsld22.1.18 [Google Scholar]
- Francis, D. O. , Daniero, J. , Hovis, K. , Sathe, N. , Jacobson, B. , Penson, D. , Feurer, I. D. , & McPheeters, M. (2017). Voice-related patient-reported outcome measures: A systematic review of instrument development and validation. Journal of Speech, Language, and Hearing Research, 60(1), 62–88. https://doi.org/10.1044/2016_JSLHR-S-16-0022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Franic, D. M. , & Bothe, A. (2008). Psychometric evaluation of condition-specific instruments used to assess health-related quality of life, attitudes, and related constructs in stuttering. American Journal of Speech-Language Pathology, 17(1), 60–80. https://doi.org/10.1044/1058-0360(2008/006) [DOI] [PubMed] [Google Scholar]
- Franic, D. M. , Bramlett, R. E. , & Bothe, A. C. (2005). Psychometric evaluation of disease specific quality of life instruments in voice disorders. Journal of Voice, 19(2), 300–315. https://doi.org/10.1016/j.jvoice.2004.03.003 [DOI] [PubMed] [Google Scholar]
- Fujiki, M. , Brinton, B. , Isaacson, T. , & Summers, C. (2001). Social behaviors of children with language impairments on the playground: A pilot study. Language, Speech, and Hearing Services in Schools, 32(2), 101–113. https://doi.org/10.1044/0161-1461(2001/008) [DOI] [PubMed] [Google Scholar]
- Garcia, L. J. , Laroche, C. , & Barrette, J. (2002). Work integration issues go beyond the nature of the communication disorder. Journal of Communication Disorders, 35(2), 187–211. https://doi.org/10.1016/S0021-9924(02)00064-3 [DOI] [PubMed] [Google Scholar]
- Gillespie, A. , & Verdolini Abbott, K. (2011). The influence of clinical terminology on self-efficacy for voice. Logopedics Phoniatrics Vocology, 36(3), 91–99. https://doi.org/10.3109/14015439.2010.539259 [DOI] [PubMed] [Google Scholar]
- Glista, S. O. , & Pollens, R. D. (2007). Educating clinicians for meaningful, relevant and purposeful aphasia group therapy. Topics in Language Disorders, 27(4), 351–371. https://doi.org/10.1097/01.TLD.0000299889.62358.6f [Google Scholar]
- Grawburg, M. , Howe, T. , Worrall, L. , & Scarinci, N. (2013). Third-party disability in family members of people with aphasia: A systematic review. Disability and Rehabilitation, 35(16), 1324–1341. https://doi.org/10.3109/09638288.2012.735341 [DOI] [PubMed] [Google Scholar]
- Guillamón, N. , Nieto, R. , Pousada, M. , Redolar, D. , Muñoz, E. , Hernández, E. , Boixadós, M. , & Gómez‐Zúñiga, B. (2013). Quality of life and mental health among parents of children with cerebral palsy: The influence of self-efficacy and coping strategies. Journal of Clinical Nursing, 22(11–12), 1579–1590. https://doi.org/10.1111/jocn.12124 [DOI] [PubMed] [Google Scholar]
- Haley, K. , Cunningham, K. , Barry, J. , & de Riesthal, M. (2019). Collaborative goals for communicative life participation aphasia: The FOURC model. American Journal of Speech-Language Pathology, 28(1), 1–13. https://doi.org/10.1044/2018_AJSLP-18-0163 [DOI] [PubMed] [Google Scholar]
- Haley, K. , Womack, J. , Helm-Estabrooks, N. , Lovette, B. , & Goff, R. (2013). Supporting autonomy for people with aphasia: Use of the Life Interests and Values (LIV) Cards. Topics in Stroke Rehabilitation, 20(1), 22–35. https://doi.org/10.1310/tsr2001-22 [DOI] [PubMed] [Google Scholar]
- Hidecker, M. J. C. , Adamsl, J. , & Ross, S. (2011). Getting to participation: Does it matter? [Paper presentation]. American Speech-Language-Hearing Foundation Annual Convention, San Diego, CA, United States. [Google Scholar]
- Hinckley, J. (2002). Vocational and social outcomes of adults with chronic aphasia. Journal of Communication Disorders, 35(6), 543–560. https://doi.org/10.1016/S0021-9924(02)00119-3 [DOI] [PubMed] [Google Scholar]
- Hinckley, J. (2006). Finding messages in bottles: Living successfully with stroke and aphasia. Topics in Stroke Rehabilitation, 13(1), 25–36. https://doi.org/10.1310/FLJ3-04DQ-MG8W-89EU [DOI] [PubMed] [Google Scholar]
- Hodge, M. , & Daniels, J. (2009). TOCS+ Intelligibility Measures. (Version 5.3) [Computer software]. University of Alberta.
- Hodge, M. , & Wellman, L. (1999). Management of children with dysarthria. In Caruso A. & Strand E. (Eds.), Clinical management of motor speech disorders in children (pp. 209–280). Thieme. [Google Scholar]
- Holland, A. , & Nelson, R. (2013). Counseling in communication disorders: A wellness perspective (2nd ed.). Plural Publishing. [Google Scholar]
- Howe, T. , Worrall, L. , & Hickson, L. (2004). What is an aphasia-friendly environment? Aphasiology, 18(11), 1015–1037. https://doi.org/10.1080/02687030444000499 [Google Scholar]
- Howe, T. , Worrall, L. E. , & Hickson, L. M. H. (2008a). Interviews with people with aphasia: Environmental factors that influence their community participation. Aphasiology, 22(10), 1092–1120. https://doi.org/10.1080/02687030701640941 [Google Scholar]
- Howe, T. , Worrall, L. E. , & Hickson, L. M. H. (2008b). Observing people with aphasia: Environmental factors that influence their community participation. Aphasiology, 22(6), 618–643. https://doi.org/10.1080/02687030701536024 [Google Scholar]
- Huber, J. , Sillick, J. , & Skarakis-Doyle, E. (2010). Personal perception and personal factors: Incorporating health-related quality of life into the International Classification of Functioning, Disability and Health. Disability and Rehabilitation, 32(23), 1955–1965. https://doi.org/10.3109/09638281003797414 [DOI] [PubMed] [Google Scholar]
- Imms, C. , Granlund, M. , Wilson, P. , Steenbergen, B. , Rosenbaum, P. , & Gordon, A. (2017). Participation, both a means and an end: A conceptual analysis of processes and outcomes in childhood disability. Developmental Medicine & Child Neurology, 59(1), 16–25. https://doi.org/10.1111/dmcn.13237 [DOI] [PubMed] [Google Scholar]
- Irwin, B. (2012). Patient-reported outcome measures in aphasia. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders, 22(4), 160–166. https://doi.org/10.1044/nnsld22.4.160 [Google Scholar]
- Jette, A. M. , Tao, W. , & Haley, S. M. (2007). Blending activity and participation sub-domains of the ICF. Disability and Rehabilitation, 29(22), 1742–1750. https://doi.org/10.1080/09638280601164790 [DOI] [PubMed] [Google Scholar]
- Johnson, C. , Beitchman, J. , & Brownlie, E. (2010). Twenty-year follow-up of children with and without speech-language impairments: Family, educational, occupational, and quality of life outcomes. American Journal of Speech-Language Pathology, 19(1), 51–65. https://doi.org/10.1044/1058-0360(2009/08-0083) [DOI] [PubMed] [Google Scholar]
- Jordan, L. , & Bryan, K. (2010). Seeing the person? Disability theories and speech and language therapy. International Journal of Language & Communication Disorders, 36(S1), 453–458. https://doi.org/10.3109/13682820109177928 [DOI] [PubMed] [Google Scholar]
- Kagan, A. (1998). Supported conversation for adults wtih aphasia: Methods and resources for training conversation partners. Aphasiology, 12(9), 816–830. https://doi.org/10.1080/02687039808249575 [Google Scholar]
- Kagan, A. , & Simmons-Mackie, N. (2007). Beginning with the end: Outcome-driven assessment and intervention with life participation in mind. Topics in Language Disorders, 27(4), 309–317. https://doi.org/10.1097/01.TLD.0000299885.39488.bf [Google Scholar]
- Kagan, A. , Simmons-Mackie, N. , Rowland, A. , Huijbregts, M. , Shumway, E. , McEwen, S. , Threats, T. , & Sharp, S. (2008). Counting what counts: A framework for capturing real-life outcomes of aphasia intervention. Aphasiology, 22(3), 258–280. https://doi.org/10.1080/02687030701282595 [Google Scholar]
- Kaizer, F. , Spiridigliozzi, A.-M. , & Hunt, M. R. (2012). Promoting shared decision-making in rehabilitation: Development of a framework for situations when patients with dysphagia refuse diet modification recommended by the treating team. Dysphagia, 27, 81–87. https://doi.org/10.1007/s00455-011-9341-5 [DOI] [PubMed] [Google Scholar]
- Kempster, G. B. , Gerratt, B. R. , Verdolini Abbott, K. , Barkmeier-Kraemer, J. , & Hillman, R. E. (2009). Consensus auditory-perceptual evaluation of voice: Development of a standardized clinical protocol. American Journal of Speech-Language Pathology, 18(2), 124–132. https://doi.org/10.1044/1058-0360(2008/08-0017) [DOI] [PubMed] [Google Scholar]
- King, G. , Law, M. , King, S. , Hurley, P. , Hanna, S. , Kertoy, M. , Rosenbaum, P. , & Young, N. (2004). Children's Assessment of Participation and Enjoyment (CAPE) Preferences for Activities of Children (PAC). PsychCorp. [Google Scholar]
- Krasny-Pacini, A. , Evans, J. , Sohlberg, M. M. , & Chevignard, M. (2016). Proposed criteria for appraising goal attainment scales used as outcome measures in rehabilitation research. Archives of Physical Medicine and Rehabilitation, 97(1), 157–170. https://doi.org/10.1016/j.apmr.2015.08.424 [DOI] [PubMed] [Google Scholar]
- Law, M. (2002). Participation in the occupations of everyday life. The American Journal of Occupational Therapy, 56(6), 640–649. https://doi.org/10.5014/ajot.56.6.640 [DOI] [PubMed] [Google Scholar]
- Legg, C. , Young, L. , & Bryer, A. (2005). Training sixth-year medical students in obtaining case history information from adults with aphasia. Aphasiology, 19(6), 559–575. https://doi.org/10.1080/02687030544000029 [Google Scholar]
- Lewis, B. , Freebairn, L. , & Taylor, H. G. (2000a). Academic outcomes in children with histories of speech sound disorders. Journal of Communication Disorders, 33(1), 11–30. https://doi.org/10.1016/S0021-9924(99)00023-4 [DOI] [PubMed] [Google Scholar]
- Lewis, B. , Freebairn, L. , & Taylor, H. G. (2000b). Follow-up of children with early expressive phonology disorders. Journal of Learning Disabilities, 33(5), 433–444. https://doi.org/10.1177/002221940003300504 [DOI] [PubMed] [Google Scholar]
- Lorig, K. , & Holman, H. (2003). Self-management education: History, definition, outcomes, and mechanisms. Annals of Behavioral Medicine, 26(1), 1–7. https://doi.org/10.1207/S15324796ABM2601_01 [DOI] [PubMed] [Google Scholar]
- Mach, H. , Baylor, C. , Hunting Pompon, R. , & Yorkston, K. (2019). Third-party disability in family members of people with communication disorders associated with Parkinson's disease. Topics in Language Disorders, 39(1), 71–88. https://doi.org/10.1097/TLD.0000000000000172 [Google Scholar]
- Mackenzie, C. , Paton, G. , Kelly, S. , Brady, M. , & Muir, M. (2012). The Living with Dysarthria group: Implementation and feasibility of a group intervention for people with dysarthria following stroke and family members. International Journal of Language & Communication Disorders, 47(6), 709–724. https://doi.org/10.1111/j.1460-6984.2012.00180.x [DOI] [PubMed] [Google Scholar]
- Magasi, S. , Hammel, J. , Heinemann, A. W. , Whiteneck, G. , & Bogner, J. (2009). Participation: A compariative analysis of multiple rehabilitation stakeholders' perspectives. Journal of Rehabilitation Medicine, 41(11), 936–944. https://doi.org/10.2340/16501977-0450 [DOI] [PubMed] [Google Scholar]
- Markham, C. , van Laar, D. , Gibbard, D. , & Dean, T. (2009). Children with speech, language, and communication needs: Their perceptions of their quality of life. International Journal of Language & Communication Disorders, 44(5), 748–768. https://doi.org/10.1080/13682820802359892 [DOI] [PubMed] [Google Scholar]
- McLeod, S. (2004). Speech pathologists' application of the ICF to children with speech impairment. Advances in Speech-Language Pathology, 6(1), 75–81. https://doi.org/10.1080/14417040410001669516 [Google Scholar]
- McNaughton, D. , Light, J. , & Groszyk, L. (2001). “Don't give up”: Employment experiences of individuals with amyotrophic lateral sclerosis who use augmentative and alternative communication. Augmentative and Alternative Communication, 17(3), 179–195. https://doi.org/10.1080/aac.17.3.179.195 [Google Scholar]
- Merrick, R. , & Roulstone, S. (2011). Children's views of communication and speech-language pathology. International Journal of Speech-Language Pathology, 13(4), 281–290. https://doi.org/10.3109/17549507.2011.577809 [DOI] [PubMed] [Google Scholar]
- Miller, C. , Baylor, C. , Birch, K. , & Yorkston, K. (2017). Exploring the relevance of items on the Communicative Participation Item Bank (CPIB) for listeners with hearing loss. American Journal of Audiology, 26(1), 27–37. https://doi.org/10.1044/2016_AJA-16-0047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller, N. , & Bloch, S. (2017). A survey of speech-language therapy provision for people wtih post-stroke dysarthria in the UK. International Journal of Language & Communication Disorders, 52(6), 800–815. https://doi.org/10.1111/1460-6984.12316 [DOI] [PubMed] [Google Scholar]
- Miller, N. , Deane, K. , Jones, D. , Gibb, C. , & Noble, E. (2011). National survey of speech and language therapy provision for people with Parkinson's disease in the United Kingdom: Therapists' practices. International Journal of Language & Communication Disorders, 46(2), 189–201. https://doi.org/10.3109/13682822.2010.484849 [DOI] [PubMed] [Google Scholar]
- Miller, N. , Noble, E. , Jones, D. , & Burn, D. (2006). Life with communication changes in Parkinson's disease. Age and Ageing, 35(3), 235–239. https://doi.org/10.1093/ageing/afj053 [DOI] [PubMed] [Google Scholar]
- Murphy, N. , Caplin, D. , Christian, B. , Luther, B. , Holobkov, R. , & Young, P. (2011). The function of parents and their children with cerebral palsy. Physical Medicine and Rehabilitation, 3(2), 98–104. https://doi.org/10.1016/j.pmrj.2010.11.006 [DOI] [PubMed] [Google Scholar]
- Murphy, N. , Christian, B. , Caplin, D. , & Young, P. (2007). The health of caregivers for children with disabilities: Caregiver perspectives. Child: Care, Health and Development, 33(2), 180–187. https://doi.org/10.1111/j.1365-2214.2006.00644.x [DOI] [PubMed] [Google Scholar]
- Murphy, W. , Yaruss, J. S. , & Quesal, R. W. (2007). Enhancing treatment for school-age children who stutter: II. Reducing bullying through role-playing and self-disclosure. Journal of Fluency Disorders, 32(2), 139–162. https://doi.org/10.1016/j.jfludis.2007.02.001 [DOI] [PubMed] [Google Scholar]
- Namkung, E. , Greenberg, J. , Mailick, M. , & Floyd, F. J. (2018). Lifelong parenting of adults with developmetnal disabilities: Growth trends over 20 years in midlife and later life. American Journal of Intellectual and Developmental Disabilities, 123(3), 228–240. https://doi.org/10.1352/1944-7558-123.3.228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson, N. , Plante, E. , Helm-Estabrooks, N. , & Hotz, G. (2016). Test of Integrated Language and Literacy Skills (TILLS). Brookes. [DOI] [PubMed] [Google Scholar]
- Northcott, S. , Burns, K. , Simpson, A. , & Hilari, K. (2015). “Living with aphasia the best way I can”: A feasibility study exploring solution-focused brief therapy for people with aphasia. Folia Phoniatrica et Logopaedica, 67(3), 156–167. https://doi.org/10.1159/000439217 [DOI] [PubMed] [Google Scholar]
- Northcott, S. , & Hilari, K. (2011). Why do people lose their friends after a stroke? International Journal of Language & Communication Disorders, 46(5), 524–534. https://doi.org/10.1111/j.1460-6984.2011.00079.x [DOI] [PubMed] [Google Scholar]
- O'Halloran, R. , Hersh, D. , Laplante-Lévesque, A. , & Worrall, L. (2010). Person-centeredness, ethics, and stories of risk. Seminars in Speech and Language, 31(2), 81–89. https://doi.org/10.1055/s-0030-1252109 [DOI] [PubMed] [Google Scholar]
- Oliver, M. (2013). The social model of disability: Thirty years on. Disability & Society, 28(7), 1024–1026. https://doi.org/10.1080/09687599.2013.818773 [Google Scholar]
- Olswang, L. , & Prelock, P. (2015). Bridging the gap between research and practice: Implementation science. Journal of Speech, Language, and Hearing Research, 58(6), S1818–S1826. https://doi.org/10.1044/2015_JSLHR-L-14-0305 [DOI] [PubMed] [Google Scholar]
- Ornstein, A. F. , & Manning, W. H. (1985). Self-efficacy scaling by adult stutterers. Journal of Communication Disorders, 18(4), 313–320. https://doi.org/10.1016/0021-9924(85)90008-5 [DOI] [PubMed] [Google Scholar]
- Parette, H., Jr. , Brotherson, M. , & Huer, M. (2000). Giving families a voice in augmentative and alternative communication decision-making. Education and Training in Mental Retardation and Developmental Disabilities, 35(2), 177–190. [Google Scholar]
- Parr, S. (2007). Living with severe aphasia: Tracking social exclusion. Aphasiology, 21(1), 98–123. https://doi.org/10.1080/02687030600798337 [Google Scholar]
- Perenboom, R. J. M. , & Chorus, A. M. J. (2003). Measuring participation according to the International Classification of Functioning, Disability and Health (ICF). Disability and Rehabilitation, 25(11–12), 577–587. https://doi.org/10.1080/0963828031000137081 [DOI] [PubMed] [Google Scholar]
- Rao, P. (2015). Outcomes and quality: Key characteristics of a successful SLP value journey. Perspectives on Neurophysiology and Neurogenic Speech and Language Disorders, 2(3), 94–106. https://doi.org/10.1044/nnsld25.3.94 [Google Scholar]
- Ravenek, M. , Skarakis-Doyle, E. , Spaulding, S. , Jenkins, M. , & Doyle, P. (2013). Enhancing the conceptual clarity and utility of the interational classification of functioning, disability & health: The potential of a new graphic representation. Disability and Rehabilitation, 35(12), 1015–1025. https://doi.org/10.3109/09638288.2012.717582 [DOI] [PubMed] [Google Scholar]
- Riley, J. (2002). Counseling: An approach for speech-language pathologists. Contemporary Issues in Communication Science and Disorders, 29, 6–16. https://doi.org/10.1044/cicsd_29_S_6 [Google Scholar]
- Roberts, M. , & Kaiser, A. (2011). The effectiveness of parent-implemented language interventions: A meta-analysis. American Journal of Speech-Language Pathology, 20(3), 180–199. https://doi.org/10.1044/1058-0360(2011/10-0055) [DOI] [PubMed] [Google Scholar]
- Rogers, C. (1946). Significant aspects of client-centered therapy. American Psychologist, 1(10), 415–422. https://doi.org/10.1037/h0060866 [DOI] [PubMed] [Google Scholar]
- Rollnick, S. , & Miller, W. (1995). What is motivational interviewing? Behavioural and Cognitive Psychotherapy, 23(4), 325–334. https://doi.org/10.1017/S135246580001643X [DOI] [PubMed] [Google Scholar]
- Rose, T. A. , Worrall, L. E. , & McKenna, K. T. (2003). The effectiveness of aphasia-friendly principles for printed health education materials for people with aphasia following stroke. Aphasiology, 17(10), 947–963. https://doi.org/10.1080/02687030344000319 [Google Scholar]
- Ross, A. , Winslow, I. , Marchant, P. , & Brumfitt, S. (2006). Evaluation of communication, life participation and psychological well-being in chronic aphasia: The influence of group intervention. Aphasiology, 20(5), 427–448. https://doi.org/10.1080/02687030500532786 [Google Scholar]
- Rundell, S. , Goode, A. , Friedly, J. , Jarvik, J. , Sullivan, S. , & Bresnahan, B. (2015). Role of health services research in producing high-value rehabilitation care. Physical Therapy, 95(12), 1703–1711. https://doi.org/10.2522/ptj.20150033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sackett, D. L. , Straus, S. E. , Richardson, W. S. , Rosenberg, W. , & Haynes, R. B. (2000). Evidence-based medicine: How to practice and teach EBM (2nd ed.). Churchill Livingstone. [Google Scholar]
- Schlosser, R. W. (2004). Goal attainment scaling as a clinical measurement technique in communication disorders: A critical review. Journal of Communication Disorders, 37(3), 217–239. https://doi.org/10.1016/j.jcomdis.2003.09.003 [DOI] [PubMed] [Google Scholar]
- Sherratt, S. , Worrall, L. , Pearson, C. , Howe, T. , Hersh, D. , & Davidson, B. (2011). “Well it has to be language-related”: Speech-language pathologists' goals for people with aphasia and their families. International Journal of Speech-Language Pathology, 13(4), 317–328. https://doi.org/10.3109/17549507.2011.584632 [DOI] [PubMed] [Google Scholar]
- Shih, L. , Piel, J. , Warren, A. , Kraics, L. , Silver, A. , Vanderhorst, V. , Simon, D. K. , & Tarsy, D. (2012). Singing in groups for Parkinson's disease (SING-PD): A pilot study of group singing therapy for PD-related voice/speech disorders. Parkinsonism & Related Disorders, 18(5), 548–552. https://doi.org/10.1016/j.parkreldis.2012.02.009 [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie, N. , & Damico, J. S. (2007). Access and social inclusion in aphasia: Interactional principles and applications. Aphasiology, 21(1), 81–97. https://doi.org/10.1080/02687030600798311 [Google Scholar]
- Simmons-Mackie, N. , & Holland, A. (2011). Aphasia centers in North America: A survey. Seminars in Speech and Language, 32(3), 203–215. https://doi.org/10.1055/s-0031-1286175 [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie, N. , Kagan, A. , Christie, C. O. , Huijbregts, M. , McEwen, S. , & Willems, J. (2007). Communicative access and decision making for people with aphasia: Implementing sustainable healthcare systems change. Aphasiology, 21(1), 39–66. https://doi.org/10.1080/02687030600798287 [Google Scholar]
- Simmons-Mackie, N. , Raymer, A. , Armstrong, E. , Holland, A. , & Cherney, L. R. (2010). Communication partner training in aphasia: A systematic review. Archives of Physical Medicine and Rehabilitation, 91(12), 1814–1837. https://doi.org/10.1016/j.apmr.2010.08.026 [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie, N. , Raymer, A. , & Cherney, L. R. (2016). Communication partner training in aphasia: An updated systematic review. Archives of Physical Medicine and Rehabilitation, 97(12), 2202–2221. https://doi.org/10.1016/j.apmr.2016.03.023 [DOI] [PubMed] [Google Scholar]
- Simmons-Mackie, N. , Threats, T. T. , & Kagan, A. (2005). Outcome assessment in aphasia: A survey. Journal of Communication Disorders, 38(1), 1–27. https://doi.org/10.1016/j.jcomdis.2004.03.007 [DOI] [PubMed] [Google Scholar]
- Smith, E. , Nichols, S. , Lemke, J. , Verdolini, K. , Gray, S. D. , Barkmeier, J. , Dove, H. , & Hoffman, H. (1994). Effects of voice disorders on patient lifestyle: Preliminary results. NCVS Status and Progress Report, 4, 237–248. [Google Scholar]
- Sorin-Peters, R. , McGilton, K. S. , & Rochon, E. (2010). The development and evaluation of a training programme for nurses working with persons with communication disorders in a complex continuing care facility. Aphasiology, 24(12), 1511–1536. https://doi.org/10.1080/02687038.2010.494829 [Google Scholar]
- Stone, J. (1992). Resolving relationship problems in communication disorders treatment: A systems approach. Language, Speech, and Hearing Services in Schools, 23(4), 300–307. https://doi.org/10.1044/0161-1461.2304.300 [Google Scholar]
- Threats, T. (2006). Towards an international framework for communication disorders: Use of the ICF. Journal of Communication Disorders, 39(4), 251–265. https://doi.org/10.1016/j.jcomdis.2006.02.002 [DOI] [PubMed] [Google Scholar]
- Threats, T. (2007). Access for persons with neurogenic communication disorders: Influences of personal and environmental factors of the ICF. Aphasiology, 21(1), 67–80. https://doi.org/10.1080/02687030600798303 [Google Scholar]
- Torrence, J. , Baylor, C. , Yorkston, K. , & Spencer, K. (2016). Addressing communicative participation in treatment planning for adults: A survey of U.S. speech-language pathologists. American Journal of Speech-Language Pathology, 25(3), 355–370. https://doi.org/10.1044/2015_AJSLP-15-0049 [DOI] [PubMed] [Google Scholar]
- Torres, I. (2013). Make it work: Dominate your IEP data. The ASHA Leader, 18(4), 26–27. https://doi.org/10.1044/leader.MIW.18042013.26 [Google Scholar]
- Trichon, M. , & Tetnowski, J. A. (2011). Self-help conferences for people who stutter: A qualitative investigation. Journal of Fluency Disorders, 36(4), 290–295. https://doi.org/10.1016/j.jfludis.2011.06.001 [DOI] [PubMed] [Google Scholar]
- Tucker, F. M. , Edwards, D. F. , Mathews, L. , Baum, C. , & Connor, L. T. (2012). Modifying health outcome measures for people with aphasia. The American Journal of Occupational Therapy, 66, 42–50. https://doi.org/10.5014/ajot.2012.001255 [DOI] [PubMed] [Google Scholar]
- Ueda, S. , & Okawa, Y. (2003). The subjective dimension of functioning and disability: What is it and what is it for? Disability and Rehabilitation, 25(11–12), 596–601. https://doi.org/10.1080/0963828031000137108 [DOI] [PubMed] [Google Scholar]
- United Nations. (2019). Convention on the rights of persons with disabilities. https://www.un.org/development/desa/disabilities/convention-on-the-rights-of-persons-with-disabilities.html [DOI] [PubMed]
- van Til, J. , Drossaert, C. , Punter, A. , & Ijzerman, M. (2010). The potential for shared decision-making and decision aids in rehabilitation medicine. Journal of Rehabilitation Medicine, 42(6), 598–604. https://doi.org/10.2340/16501977-0549 [DOI] [PubMed] [Google Scholar]
- Varni, J. W. , Limbers, C. , & Burwinkle, T. M. (2007). How young can children reliably and validly self-report their quality of life? An analysis of 8,591 children across age subgroups with the PedsQL 4.0 Generic Core Scales. Health and Quality of Life Outcomes, 5(1), 1–13. https://doi.org/10.1186/1477-7525-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verna, A. , Davidson, B. , & Rose, T. (2009). Speech-language pathology services for people with aphasia: A survey of current practice in Australia. International Journal of Speech-Language Pathology, 11(3), 191–205. https://doi.org/10.1080/17549500902726059 [Google Scholar]
- Wade, D. T. , & Halligan, P. (2017). The biopsychosocial model of illness: A model whose time has come. Clinical Rehabilitation, 31(8), 995–1004. https://doi.org/10.1177/0269215517709890 [DOI] [PubMed] [Google Scholar]
- Walshe, M. , & Miller, N. (2011). Living wtih acquired dysarthria: The speaker's perspective. Disability and Rehabilitation, 33(3), 195–203. https://doi.org/10.3109/09638288.2010.511685 [DOI] [PubMed] [Google Scholar]
- Walshe, M. , Peach, R. K. , & Miller, N. (2009). Dysarthria Impact Profile: Development of a scale to measure psychosocial effects. International Journal of Language & Communication Disorders, 44(5), 693–715. https://doi.org/10.1080/13682820802317536 [DOI] [PubMed] [Google Scholar]
- Whiteneck, G. G. (1994). Measuring what matters: Key rehabilitation outcomes. Archives of Physical Medicine and Rehabilitation, 75, 1073–1076. https://doi.org/10.1016/0003-9993(94)90080-9 [DOI] [PubMed] [Google Scholar]
- Whiteneck, G. G. , Harrison-Felix, C. L. , Mellick, D. C. , Brooks, C. A. , Charlifue, S. B. , & Gerhart, K. A. (2004). Quantifying environmental factors: A measure of physical, attitudinal, service, productivity, and policy barriers. Archives of Physical Medicine and Rehabilitation, 85(8), 1324–1335. https://doi.org/10.1016/j.apmr.2003.09.027 [DOI] [PubMed] [Google Scholar]
- Wills, C. (2010). Sharing decisions with patients: Moving beyond patient-centered care. Journal of Psychosocial Nursing and Mental Health Services, 48(3), 4–5. https://doi.org/10.3928/02793695-20100202-03 [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2001). International Classification of Functioning, Disability and Health: ICF.
- Worrall, L. (2006). Professionalism and functional outcomes. Journal of Communication Disorders, 39(4), 320–327. https://doi.org/10.1016/j.jcomdis.2006.02.007 [DOI] [PubMed] [Google Scholar]
- Wyrwich, K. , Bullinger, M. , Aaronson, N. , Hays, R. D. , Patrick, D. L. , & Symonds, T. (2005). Estimating clinically significant differences in quality of life outcomes. Quality of Life Research, 14, 285–295. https://doi.org/10.1007/s11136-004-0705-2 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S. (2010). Assessing quality of life in stuttering treatment outcomes research. Journal of Fluency Disorders, 35(3), 190–202. https://doi.org/10.1016/j.jfludis.2010.05.010 [DOI] [PubMed] [Google Scholar]
- Yaruss, J. S. , & Quesal, R. W. (2006). Overall Assessment of the Speaker’s Experience of Stuttering (OASES): Documenting multiple outcomes in stuttering treatment. Journal of Fluency Disorders, 31(2), 90–115. https://doi.org/10.1016/j.jfludis.2006.02.002 [DOI] [PubMed] [Google Scholar]
- Yorkston, K. , Baylor, C. , & Britton, D. (2017a). Incorporating the principles of self-management into treatment of dysarthria associated with Parkinson's disease. Seminars in Speech and Language, 38(3), 210–219. https://doi.org/10.1055/s-0037-1602840 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yorkston, K. , Baylor, C. , & Britton, D. (2017b). Speech versus speaking: The experiences of people with Parkinson's disease and implications for intervention. American Journal of Speech-Language Pathology, 26(2S), 561–568. https://doi.org/10.1044/2017_AJSLP-16-0087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yorkston, K. , Baylor, C. , Deitz, J. , Dudgeon, B. J. , Eadie, T. , Miller, R. M. , & Amtmann, D. (2008). Developing a scale of communicative participation: A cognitive interviewing study. Disability and Rehabilitation, 30(6), 425–433. https://doi.org/10.1080/09638280701625328 [DOI] [PubMed] [Google Scholar]
- Yorkston, K. , Baylor, C. , Klasner, E. R. , Deitz, J. , Dudgeon, B. J. , Eadie, T. , Miller, R. M. , & Amtmann, D. (2007). Satisfaction with communicative participation as defined by adults with multiple sclerosis: A qualitative study. Journal of Communication Disorders, 40(6), 433–451. https://doi.org/10.1016/j.jcomdis.2006.10.006 [DOI] [PubMed] [Google Scholar]
- Yorkston, K. , Klasner, E. R. , & Swanson, K. M. (2001). Communication in context: A qualitative study of the experiences of individuals with multiple sclerosis. American Journal of Speech-Language Pathology, 10(2), 126–137. https://doi.org/10.1044/1058-0360(2001/013) [Google Scholar]
- Young, N. , Yoshida, K. , Williams, J. , Bombardier, C. , & Wright, J. (1995). The role of children in reporting their physical disability. Archives of Physical Medicine and Rehabilitation, 76(10), 913–918. https://doi.org/10.1016/S0003-9993(95)80066-2 [DOI] [PubMed] [Google Scholar]
- Zeppiere, G., Jr. , Lentz, T. , Atchison, J. , Indelicato, P. , Moser, M. , Vincent, K. , & George, S. (2012). Preliminary results of patient-defined success criteria for individuals with musculoskeletal pain in outpatient physical therapy settings. Archives of Physical Medicine and Rehabilitation, 93(3), 434–440. https://doi.org/10.1016/j.apmr.2011.10.007 [DOI] [PubMed] [Google Scholar]
- Zraick, R. I. , Atcherson, S. R. , & Brown, A. M. (2012). Readability of patient-reported outcome questionnaries for use with persons who stutter. Journal of Fluency Disorders, 37(1), 20–24. https://doi.org/10.1016/j.jfludis.2011.10.004 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.