Key Points
Question
What is the prevalence of eyeglass use compliance among preschool children from low-income families, and what factors are associated with this compliance?
Findings
In this longitudinal cross-sectional study of 188 preschool students, 133 (71%) were consistently compliant with eyeglass wear during the 2017 to 2018 school year. Baseline uncorrected visual acuity was significantly associated with consistent eyeglass wear.
Meaning
Among preschoolers receiving free glasses through a school-based program, compliance with eyeglass wear was relatively stable throughout the school year, and compliance was solely associated with poor baseline visual acuity.
Abstract
Importance
Despite growing support for early school-based vision screening and eyeglass provision, few studies have rigorously monitored the compliance of eyeglass wear among preschool-aged children who receive eyeglasses through such programs.
Objective
To assess the prevalence and factors associated with eyeglass wear compliance among preschoolers from low-income families who receive eyeglasses through the See Well to Learn program.
Design, Setting, and Participants
Longitudinal cross-sectional study of eyeglass wear compliance patterns among 188 children 3 to 5 years of age from 51 Bay Area Head Start preschools in San Francisco, California. The study conducted during the 2017 to 2018 school year included students with a failed vision screening who met predetermined refractive criteria following cycloplegic refraction and received eyeglasses through the See Well to Learn program.
Exposures
Eyeglass distribution.
Main Outcomes and Measures
Eyeglass wear compliance, measured by a school-year’s worth of weekly teacher reports, was a longitudinal measure of consistent eyeglass wear, defined by eyeglass wear for more than 50% of every school day (compliance score of 4).
Results
Of 188 students (91 boys [49%]; 94 girls [51%]; mean [SD] age, 3.89 [0.5] years), 133 (71%; 95% CI, 64%-77%) maintained a mean compliance score throughout the school year of 4 or higher. Compliance prevalence was relatively stable throughout the school year, ranging from 139 students (74%) to 164 students (87%). Baseline uncorrected visual acuity in both the better-seeing and worse-seeing eyes was the only assessed factor that was associated with compliance. In the better-seeing eye, the mean uncorrected visual acuity of students with eyeglass wear compliance was 0.473 logMAR (95% CI, 0.433-0.514) (Snellen equivalent, 20/60) compared with 0.394 logMAR (95% CI, 0.334-0.454) (Snellen equivalent, 20/50) for students with noncompliance (P = .03). In the worse-seeing eye, the mean uncorrected visual acuity of students with compliance was 0.576 logMAR (95% CI, 0.530-0.623) (Snellen equivalent, 20/75) compared with 0.492 logMAR (95% CI, 0.433-0.551) (Snellen equivalent, 20/62) for students with noncompliance (P = .03). In the better-seeing eye, the difference between students with compliance vs noncompliance was 0.079 logMAR (95% CI, 0.009-0.150) (5 Snellen letter difference) compared with 0.084 logMAR (95% CI, 0.007-0.160) (5 Snellen letter difference) in the worse-seeing eye.
Conclusions and Relevance
This study found that nearly 3 of 4 preschool students consistently wore their glasses at school during their first year of use, supporting the continued implementation of preschool-based vision screening programs. These findings suggest that programs involving school-based screening and eyeglass delivery may lessen disparities in accessing pediatric vision care. Consistent with previous studies, students with poorer uncorrected baseline visual acuity were found to be more likely to wear eyeglasses compliantly.
This cross-sectional study assesses the prevalence and factors associated with eyeglass wear compliance for a school year among preschool children who have a failed vision screening, are from low-income families, and receive eyeglasses through the See Well to Learn program.
Introduction
Uncorrected refractive errors account for the majority of visual impairment experienced by children across the world, including the United States.1 Although most refractive errors can be cost-effectively corrected with eyeglasses, low compliance with early eyeglass wear can limit visual development and ability.
Among children in particular, the impact of visual impairment extends well beyond eyesight, showing detrimental associations with social and behavioral development,2 future literacy,2 academic success,3 and the quality of everyday life.3 Although refractive errors affect children from all backgrounds and regions, the impact associated with poor vision can be further compounded by social inequities and barriers to care faced by children of low-income families. Previous studies have shown that disparities in visual impairment are disproportionately observed among urban minority youth, further widening gaps in academic achievement.4
Given the importance of timely diagnosis and treatment of refractive errors, support for early school-based vision screening programs has been growing internationally. Despite growing numbers of mobile eye programs that screen and deliver eyeglasses at school, few studies have consistently monitored the compliance of preschool-aged children who receive glasses through such programs. Previous studies report compliance based on 1 or 2 unannounced observations at school or on students’ self-report.5,6 The definition of compliance itself has varied among prior studies, ranging from simply carrying eyeglasses to being observed wearing them.
There is a wide range of reported compliance among school-aged children, from 13.4% among children in a study conducted in Mexico7 to 70.8% among children of low-income families in an urban study conducted in the United States.8 Previous reviews have found that factors associated with compliance are largely context specific, highlighting the importance of local follow-up and investigation.6 In our present study, we defined compliance with eyeglass wear rigorously by collecting data at regular, weekly intervals from preschool teachers. The purpose of this study is thus to investigate the prevalence and factors associated with compliance among preschoolers who recently received glasses through an onsite preschool screening program in San Francisco, California, and to better understand trends in eyeglass use compliance during the course of a school year.
Methods
This was a cross-sectional analysis examining the factors associated with eyeglass wear compliance during the 2017 to 2018 school year. This study received approval from the institutional review board of the University of California, San Francisco, and was conducted in accordance with the Health Insurance Portability and Accountability Act. Written parental informed consent was obtained in a manner consistent with the Declaration of Helsinki9 at the eye examination.
Program Overview
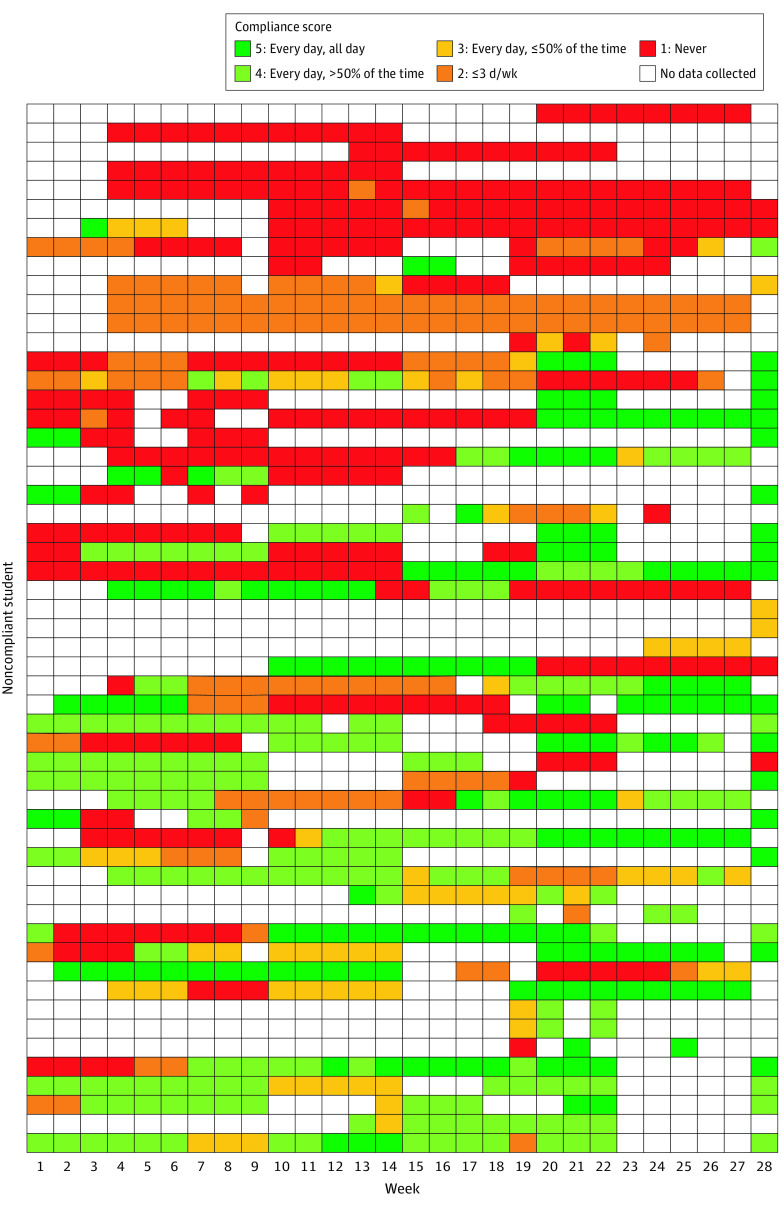
The See Well to Learn (SWTL) program was established in 2012 by Prevent Blindness Northern California, a community nonprofit 501(c)(3), to address vision problems and school readiness for preschool children from low-income families in Northern California. As depicted in Figure 1, the SWTL program includes school-based vision screenings, on-site eye exams, free eyeglasses, and referrals to pediatric ophthalmologists as needed.10,11 Support for eyeglasses was available through in-kind donation of lenses from the Essilor Vision Foundation and no-cost replacement glasses through the University of California, San Francisco Augie Fund.
Figure 1. See Well to Learn Program Components.
Participants
We selected 51 Head Start preschools in the San Francisco region for this study. Preschoolers aged 3 to 5 years with failed results on vision screening in the fall of 2017 received a complete ophthalmological examination on the SWTL eye bus, including cycloplegic refraction. The program followed preestablished age-appropriate guidelines for eyeglass prescription.10 Children diagnosed as having refractive errors received 2 pairs of glasses and a replacement pair as needed. At the time of their examination, participants chose from 7 frame options in a variety of colors. Eyeglasses were provided at no cost and were delivered to students at their respective schools within approximately 2 weeks.
Neither parents nor students were given additional incentives to participate in the study. The SWTL staff informed parents that they would follow up with a telephone call in the parents’ preferred language within 3 weeks of eyeglass delivery to ask whether the child was adjusting to glasses and to answer questions. The SWTL staff requested to call back within 2 months for a total of 3 support calls made to consenting parents. These calls used motivational interview techniques and followed a script to elicit honest feedback from the parents on challenges that they were facing in having their children wear new glasses. Parents received a printed copy of advice and tips as well as a sticker chart to help their child adjust to glasses. These documents were provided in parents’ primary spoken language. A total of 188 students who met refractive criteria and received glasses were included in this study.
Compliance Scoring
Teachers were asked to record weekly observations of student eyeglass wear compliance during the 2017 through 2018 school year (eFigure 1 in the Supplement). Teachers were given information on amblyopia, hyperopia, myopia, and astigmatism to reinforce the importance of consistent eyeglass wear in school. Teachers who submitted the weekly logs were entered into a monthly raffle for a $50 gift card for classroom supplies. Eyeglass wear was checked formally on daily arrival to the classroom and informally during the course of the day to allow teachers to determine each student’s weekly compliance report. These observations were converted to a 5-point compliance scale, and the mean calculated for the school year for each student (Table 1). Students with a mean compliance score of 4 or higher were considered to be eyeglass wear compliant. A compliance score of 4 or higher corresponded to those who consistently wore their glasses at least every day, for more than half of the 8-hour school day. A preliminary analysis of individual trends in compliance score over time was conducted to determine whether eyeglass wear tended to increase or decrease during the course of the school year.
Table 1. Compliance Scores Based on Teacher Observations Throughout School Year.
| Observation | Score | No. | No./total No. (%) |
|---|---|---|---|
| Compliant | |||
| Every day | |||
| All day | 5 | 67 | 133 (71) |
| >50% Of the time | 4 | 66 | |
| Noncompliant | |||
| Every day, ≤50% of the time | 3 | 25 | 55 (29) |
| ≤3 Days a week | 2 | 17 | |
| Never | 1 | 13 |
Sociodemographic data, including age, sex, and race/ethnicity, were reported by schools (Table 2). A complete history was taken at the time of the mobile eye examination; data on the primary language spoken at home, insurance status, previous eye examinations, and family history of eye conditions were collected from these records in addition to baseline uncorrected visual acuity.
Table 2. Demographic and Clinical Characteristics of Preschool Student Participants.
| Characteristic | No. (%) of participantsa | P valueb | |
|---|---|---|---|
| Compliant (n = 133) | Noncompliant (n = 55) | ||
| Age, mean (SD), y | 3.92 (0.47) | 3.88 (0.69) | .58c |
| Sex | |||
| Male | 68 (52) | 23 (43) | .32 |
| Female | 64 (48) | 30 (57) | |
| Race/ethnicity | |||
| Latino | 91 (71) | 42 (78) | .35 |
| Non-Latino | 37 (29) | 12 (22) | |
| Language spoken at home | |||
| English | 35 (27) | 15 (28) | .68 |
| Spanish | 72 (55) | 32 (60) | |
| Mandarin | 11 (8) | 1 (2) | |
| Other, multilingual | 14 (10) | 5 (10) | |
| Insurance | |||
| Public | 77 (77) | 37 (86) | .26 |
| Private | 22 (22) | 6 (14) | |
| Visual acuity, logMAR (Snellen equivalent) | |||
| Better-seeing eye | 0.473 (20/60) | 0.394 (20/50) | .03c |
| Worse-seeing eye | 0.576 (20/75) | 0.492 (20/62) | .03c |
| Family history of glasses | |||
| Yes | 73 (73) | 30 (73) | .98 |
| No | 27 (27) | 11 (27) | |
| Family history of blindness | |||
| Yes | 6 (6) | 0 | .11 |
| No | 94 (94) | 42 (100) | |
| Family history of “lazy eye” | |||
| Yes | 13 (14) | 9 (21) | .24 |
| No | 83 (86) | 33 (79) | |
| Prior eye examination | |||
| Yes | 57 (59) | 29 (69) | .25 |
| No | 40 (41) | 13 (31) | |
| Noticed problems with your child’s vision? | |||
| Yes | 27 (28) | 7 (18) | .20 |
| No | 70 (72) | 33 (82) | |
The denominators of calculated percentages vary owing to missing demographic information of certain variables of some respondents.
Reported P values of χ2 tests for independence.
Reported P value of unpaired t test.
Statistical Analysis
Visual acuity in the best-seeing and worse-seeing eyes was converted to the logarithm of the minimum angle of resolution (logMAR) for analyses. Pearson χ2 and unpaired t tests were used to examine associations between compliance status and demographic factors, visual acuity, and family history (Table 2). We used t tests to analyze the continuous variables of visual acuity (logMAR) and age. Reported P values are 2-sided and were not adjusted for multiple comparisons; P < .05 was considered statistically significant. Data analysis was completed using Stata statistical software, version 16.2 (StataCorp).
Results
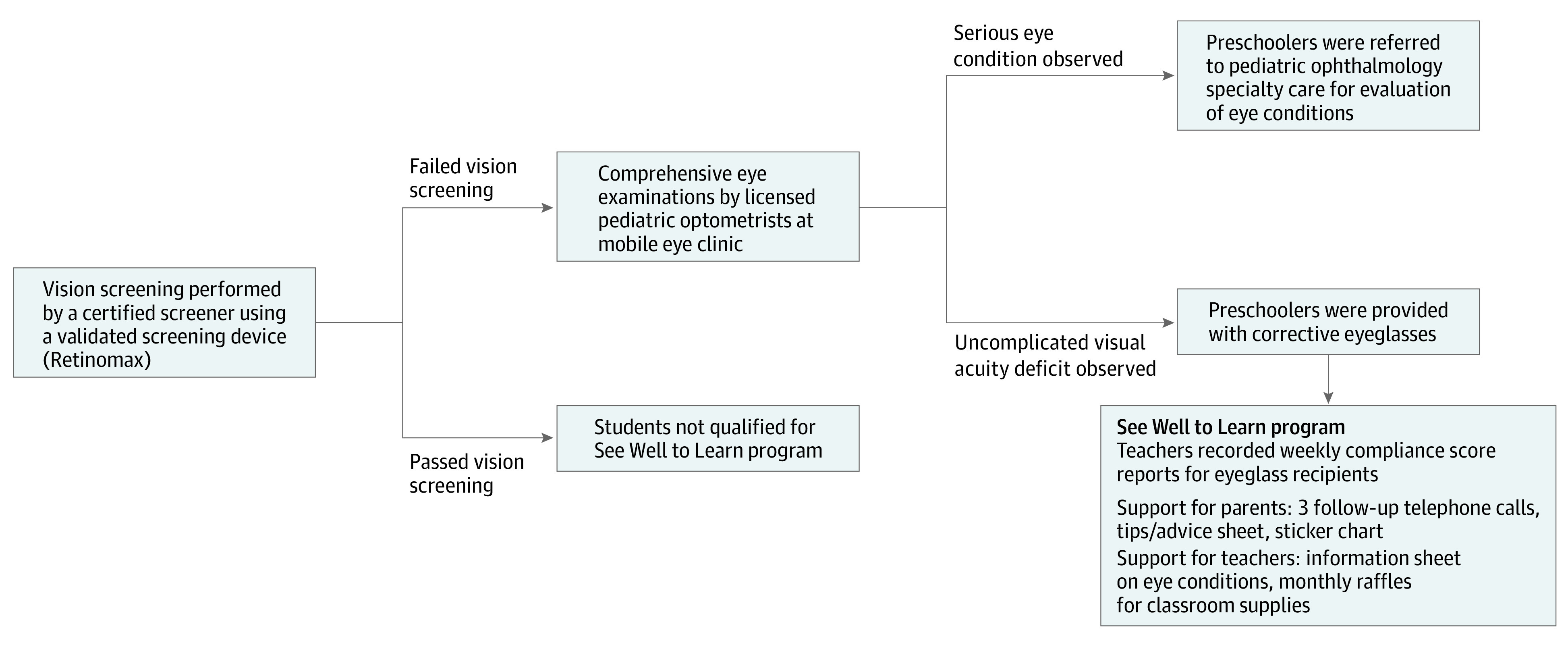
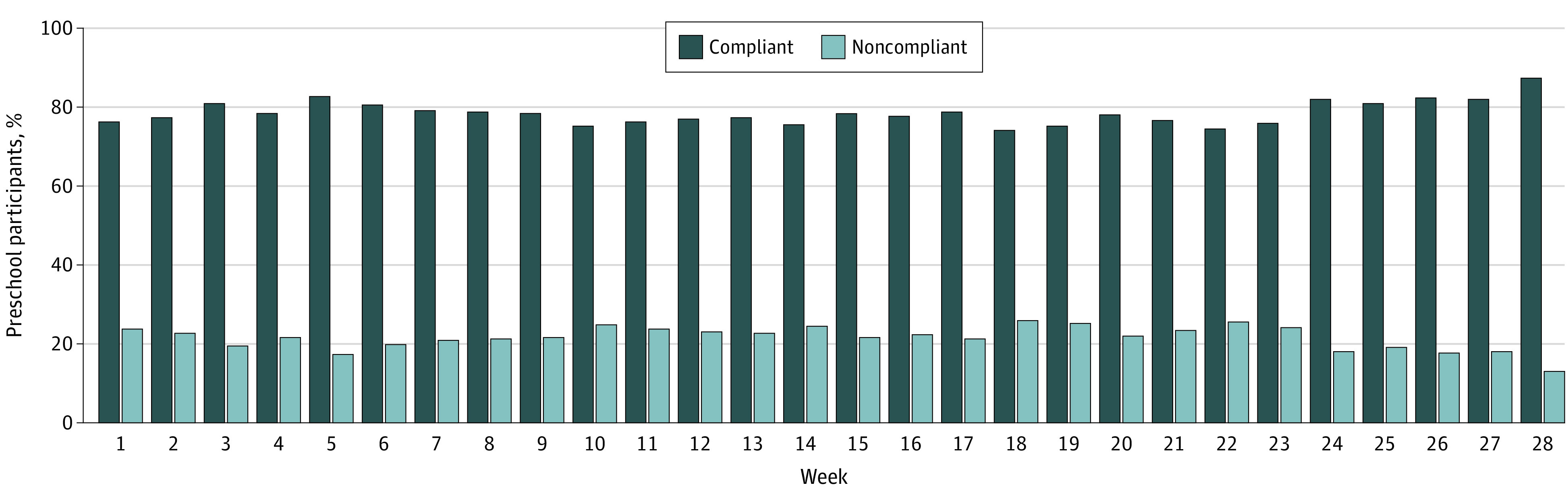
Of 188 students included in this study (91 boys [49%]; 94 girls [51%]; mean [SD] age, 3.89 [0.5] years), 133 (71%; 95% CI, 64%-77%) scored 4 or higher on their mean compliance rating during the school year (Table 1). The annual mean score of 133 students compliant with eyeglass use was 4.73 (95% CI, 4.67-4.79) vs 2.78 (95% CI, 2.54-3.01) among 55 students noncompliant with eyeglass use. Because teachers recorded weekly observations of students’ eyeglass wear, these compliance score means for the school year provided a robust measure of consistent eyeglass wear. The distribution of these weekly compliance scores is depicted in Figure 2, which shows that the prevalence of compliant eyeglass wear was relatively stable throughout the school year, during the 28 weeks from October 2017 to April 2018. In any given week, between 139 students (74%) and 164 students (87%) were observed to wear their glasses every day, for at least 50% of the time. In total, 133 students (71%) were able to maintain consistent eyeglass adherence throughout their first year of spectacle wear.
Figure 2. Trends in Compliant vs Noncompliant Eyeglass Wear Among Students From October 2017 to April 2018.
The remaining 55 students (29%) were deemed noncompliant with eyeglass wear because their weekly mean compliance scores were lower than 4. The weekly compliance scores of these 55 students are shown in Figure 3, plotted in an effort to detect any patterns underlying noncompliant eyeglass wear. Among those 55 students, those with lower compliance scores tended to start the school year with infrequent eyeglass wear. Relatively few of those 55 students started the school year with frequent eyeglass wear that decreased as the weeks progressed. For the majority of 188 participants, those who began the school year with compliant eyeglass wear were able to maintain adherence to eyeglass wear throughout the school year. This pattern is further shown in eFigure 2 in the Supplement, which portrays the weekly compliance scores of 133 students with compliant eyeglass use.
Figure 3. Weekly Compliance Scores of 55 Students With Noncompliant Eyeglass Use (Mean School Year Compliance Score <4).
The white boxes in Figure 3 and eFigure 2 in the Supplement depict the weeks that student data were not collected. Out of 28 potential weekly compliance scores, a mean (SD) of 14 (7) scores were recorded for students who were compliant vs 16 (8) scores for students with noncompliance (P = .10). During our study, approximately 25% of students required a replacement pair of eyeglasses.
Table 2 provides various demographic characteristics assessed for their association with adherence to eyeglass wear in school during the school year. The sociodemographic factors assessed, including age, sex, home language, and insurance status, did not differ between students who were vs were not compliant with eyeglass use. Although a greater percentage of female (48% [n = 64] vs 57% [n = 30]) and Latino (71% [n = 91] vs 78% [n = 42]) students were observed to be noncompliant with eyeglass use compared with their respective counterparts compliant with eyeglass use, these differences were not significant. Similarly, students who spoke Mandarin at home were more likely be compliant with eyeglass use (8% [n = 11] vs 2% [n = 1]) although this difference was not significant.
Baseline uncorrected visual acuity was associated with eyeglass compliance. Students with more severe uncorrected baseline visual acuity were more likely to wear their glasses consistently. The mean uncorrected acuity in the better-seeing eye was 0.473 logMAR (95% CI, 0.433-0.514) (Snellen equivalent, 20/60) among students compliant with eyeglass use, compared with 0.394 logMAR (95% CI, 0.334-0.454) (Snellen equivalent, 20/50) for students noncompliant with eyeglass use (P = .03). Similarly, in the worse-seeing eye, the mean logMAR of students compliant with eyeglass use was 0.576 (95% CI, 0.530-0.623) (Snellen equivalent, 20/75) compared with 0.492 (95% CI, 0.433-0.551) (Snellen equivalent, 20/62) for students noncompliant with eyeglass use (P = .03). The association between lower visual acuity and higher compliance was thus consistent across comparisons of individual participants’ stronger eyes and weaker eyes. In the better-seeing eye, the difference between students compliant and noncompliant with eyeglass use was 0.079 logMAR (95% CI, 0.009-0.150) (5 Snellen letter difference) compared with 0.084 logMAR (95% CI, 0.007-0.160) (5 Snellen letter difference) in the worse-seeing eye.
We examined whether the presence of eye disorders in the family was associated with student eyeglass compliance. Notably, 73% of students compliant and 73% of students noncompliant with eyeglass use had a family member who wore glasses at home, suggesting that familial eyeglass wear was not associated with compliance behaviors at school. Similarly, a family history of blindness or “lazy eye” was not associated with eyeglass use compliance. Although the analysis was limited by small sample size, all 6 students with a family history of blindness were compliant with eyeglass wear at school.
In total, less than 25% of parents (for 34 of 188 students) had noticed something wrong with their child’s vision or the way the children held their head by the time they received failing vision screening scores. This factor was not associated with compliance.
Discussion
Of the various factors analyzed, visual acuity of the worse-seeing eye and visual acuity of the better-seeing eye were associated with consistent eyeglass wear compliance at school. The notion that preschool students who are having a harder time seeing will be more likely to wear their glasses is a plausible one. These findings, while locally relevant to the low-income preschool population we studied in San Francisco, are also consistent with previous studies of adolescents in diverse settings. From Bangalore5 to Botswana,12 similar patterns have been observed: poorer visual acuity is associated with higher eyeglass use compliance.
Our present study was unique in several ways. Although nearly all prior studies of pediatric eyeglass compliance include adolescents or teenagers from 5 to 19 years of age,6 our participants were notably younger, from 3 to 5 years of age. Factors associated with compliance likely differ among various stages of child development, and it is worthwhile to note that among preschoolers in the present study, sex was not a significant factor associated with compliance. This differs from a handful of adolescent studies, several of which observed that girls were more compliant than boys with eyeglass wear but also face social barriers to compliance, including increased bullying and greater concern of appearances.6
In addition to studying preschool students, our study was unique in its rigorous monitoring of compliance. Rather than observe compliance at 1 or 2 points during the school year, we monitored compliance with weekly observations collected from teachers, which were averaged during the school year for each student. This reassured us that our observations were relatively robust and not influenced strongly by 1 or 2 “off days” that a child may have had.
The overall rate of compliance (71%) was relatively high, given that our participants were preschool-aged children receiving glasses for the first time. We found that compliance did not fluctuate much throughout the school year for the majority of participants. Those who started out with compliance scores of 4 or higher in the fall were largely able to maintain consistent eyeglass wear throughout the winter and spring, suggesting that once a child develops the habit of wearing glasses, further resources may not be required to encourage continued compliance throughout the school year. To increase cost-effectiveness, additional interventions ought to be focused on noncompliance. Overall rates of eyeglass use compliance were more likely to improve rather than deteriorate as the school year progressed.
Several factors were likely associated with the high prevalence of successful eyeglass wear, including the child’s ability to select the frames. Prior studies have suggested that allowing students to pick their frames increases their engagement and adherence to eyeglass wear.3,13 After selecting an eyeglass frame, each child in the present study was given 2 pairs of eyeglasses and a third replacement as needed, which allowed many students to keep a pair at school and maintain consistent compliance even after damaging or losing a pair. Previous studies have established that breaking or losing one’s eyeglasses are major reasons for pediatric spectacle use noncompliance. In a recent study of 206 students, 66% of students required replacements after initially receiving 2 pairs of glasses.13 During the present study, approximately 1 in 4 students received replacement pairs after breaking or misplacing their eyeglasses. Proactively providing our SWTL participants with more than 1 pair of glasses likely mitigated the negative impact of wear and tear that is to be expected among preschoolers wearing glasses for the first time.
Fewer than a quarter of parents had suspected that their child’s vision was impaired by the time the child received failing scores on the vision screening, further highlighting the importance of early school-based vision testing to detect refractive errors in the first place. By providing school-based exams and delivering eyeglasses at no cost, the SWTL program circumvents logistical barriers to eyecare access that may otherwise have delayed or prevented proper eyeglass wear. Continued support was provided to families in the form of follow-up telephone calls conducted in parents’ preferred spoken language. Conducted by SWTL staff, these telephone calls served not only to reinforce eyeglass compliance at home but also to provide strategies to support eyeglass wear and elucidate reasons for nonwear. Members of our team plan to conduct a qualitative analysis of the content of these parental telephone calls to further investigate potential factors associated with eyeglass compliance.
Although financial, transport, and language barriers continue to be observed disproportionately among low-income families,13,14,15 the SWTL program has been successful in early vision intervention, thus creating more opportunity for these preschoolers to see better, in the hopes of ultimately promoting greater scholastic and social development. Among the present population of children enrolled in an early education program for low-income families, sociodemographic factors, such as students’ home language, race/ethnicity, or insurance status, were not ultimately associated with whether or not they wore their glasses. The only factor we assessed that was associated was visual acuity. This supports the notion that the delivery of the SWTL program may help reduce disparities in access to vision screening and eyeglass wear among preschoolers from low-income families. By connecting with eyecare resources through their schools, fewer patients are lost to follow-up as well.
Limitations
Although our results are promising regarding the positive observations associated with SWTL, they ought to be interpreted with some caution. As described previously, our robust measure of compliance as a longitudinal variable was a method strength of this study. However, as shown by the notable presence of white boxes in Figure 3, our study was limited by missing data because many students’ compliance scores were not recorded every week. Annual compliance scores were thus determined by as many weeks of data that were collected per student. During the study, teachers recorded a mean of 14 scores vs 16 scores per student with compliant wear vs noncompliant wear (P = .10). This lack of difference in the number of observations of compliance and noncompliance is somewhat reassuring because it suggests that teachers did not neglect to observe students with poor eyeglass adherence. Intermittent student and teacher absences from school may account for some of these missing data points. Students with missing data points were not excluded from the study, thus limiting our analysis to the assumption that eyeglass wear during these unreported weeks did not differ from reported weeks. The amount of missing data reaffirms the need to ensure that all teachers are engaged with the SWTL program, and further investigation into the causes of missing data is warranted. This study was also limited in its relatively short follow-up time of 1 school year.
Another limitation of our study was that we were not able to analyze compliance data by individual Head Start preschools owing to the small number of children requiring glasses in each school. However, this analysis could have potentially captured whether specific schools or teachers were factors associated with student eyeglass use compliance. It is also unclear whether teachers were actively encouraging students to wear their glasses while in school. Students were not told that their teachers were observing their eyeglass wear, thus mitigating the potential of the Hawthorne effect.
In the future, it may be worthwhile to collect qualitative data from students themselves to better appreciate individual factors that may be associated with a child’s adherence or lack thereof. Although we asked parents whether anyone else at home wears glasses, we did not ask whether participants had a close friend who also wears glasses. Given that compliance behaviors were observed in school, having eyeglass-wearing peers may have been a factor associated with compliance.13
Conclusions
In the context of the current coronavirus disease 2019 pandemic, virtual learning has blurred the line between school and home settings, with the potential of disrupting consistent eyeglass wear habits developed in school. This further highlights the importance of monitoring and encouraging compliant eyeglass wear both in school and at home, requiring support from parents and teachers alike. Overall, our observation that nearly 3 of 4 preschool students were consistently wearing their glasses at school during their first year of wear provides support for the continued implementation and development of preschool-based vision screenings and eyeglass distribution in low-income neighborhoods.
eFigure 1. Weekly Eyeglass Compliance Observation Reports Completed by Teachers
eFigure 2. Tracking Weekly Compliance Scores of Compliant Students (Yearlong Average Compliance Score ≥4)
References
- 1.Flaxman SR, Bourne RRA, Resnikoff S, et al. ; Vision Loss Expert Group of the Global Burden of Disease Study . Global causes of blindness and distance vision impairment 1990-2020: a systematic review and meta-analysis. Lancet Glob Health. 2017;5(12):e1221-e1234. doi: 10.1016/S2214-109X(17)30393-5 [DOI] [PubMed] [Google Scholar]
- 2.Zaba JN. Social, emotional, and educational consequences of undetected children’s vision problems. J Behavl Optom. 2001;12(3):66-70. [Google Scholar]
- 3.Dudovitz RN, Izadpanah N, Chung PJ, Slusser W. Parent, teacher, and student perspectives on how corrective lenses improve child wellbeing and school function. Matern Child Health J. 2016;20(5):974-983. doi: 10.1007/s10995-015-1882-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Basch CE. Vision and the achievement gap among urban minority youth. J Sch Health. 2011;81(10):599-605. doi: 10.1111/j.1746-1561.2011.00633.x [DOI] [PubMed] [Google Scholar]
- 5.Morjaria P, Evans J, Gilbert C. Predictors of spectacle wear and reasons for nonwear in students randomized to ready-made or custom-made spectacles: results of secondary objectives from a randomized noninferiority trial. JAMA Ophthalmol. 2019;137(4):408-414. doi: 10.1001/jamaophthalmol.2018.6906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Morjaria P, McCormick I, Gilbert C. Compliance and predictors of spectacle wear in schoolchildren and reasons for non-wear: a review of the literature. Ophthalmic Epidemiol. 2019;26(6):367-377. doi: 10.1080/09286586.2019.1628282 [DOI] [PubMed] [Google Scholar]
- 7.Castanon Holguin AM, Congdon N, Patel N, et al. Factors associated with spectacle-wear compliance in school-aged Mexican children. Invest Ophthalmol Vis Sci. 2006;47(3):925-928. doi: 10.1167/iovs.05-0895 [DOI] [PubMed] [Google Scholar]
- 8.Alvi RA, Justason L, Liotta C, et al. The Eagles Eye Mobile: assessing its ability to deliver eye care in a high-risk community. J Pediatr Ophthalmol Strabismus. 2015;52(2):98-105. doi: 10.3928/01913913-20150216-02 [DOI] [PubMed] [Google Scholar]
- 9.World Medical Association . World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191-2194. doi: 10.1001/jama.2013.281053 [DOI] [PubMed] [Google Scholar]
- 10.Lowry EA, de Alba Campomanes AG. Cost-effectiveness of school-based eye examinations in preschoolers referred for follow-up from visual screening. JAMA Ophthalmol. 2016;134(6):658-664. doi: 10.1001/jamaophthalmol.2016.0619 [DOI] [PubMed] [Google Scholar]
- 11.Lowry EA, de Alba Campomanes AG. Efficient referral thresholds in autorefraction-based preschool screening. Am J Ophthalmol. 2015;159(6):1180-1187.e3. doi: 10.1016/j.ajo.2015.02.012 [DOI] [PubMed] [Google Scholar]
- 12.McCormick I, Morjaria P, Mactaggart I, et al. Spectacle compliance and its determinants in a school vision screening pilot in Botswana. Ophthalmic Epidemiol. 2019;26(2):109-116. doi: 10.1080/09286586.2018.1523441 [DOI] [PubMed] [Google Scholar]
- 13.Huang AH, Guo X, Mudie LI, et al. Baltimore Reading and Eye Disease Study (BREDS): compliance and satisfaction with glasses usage. J AAPOS. 2019;23(4):207.e1-207.e6. doi: 10.1016/j.jaapos.2019.01.018 [DOI] [PubMed] [Google Scholar]
- 14.Zhang X, Elliott MN, Saaddine JB, et al. Unmet eye care needs among U.S. 5th-grade students. Am J Prev Med. 2012;43(1):55-58. doi: 10.1016/j.amepre.2012.01.032 [DOI] [PubMed] [Google Scholar]
- 15.Grant R, Gracy D, Goldsmith G, Sobelson M, Johnson D. Transportation barriers to child health care access remain after health reform. JAMA Pediatr. 2014;168(4):385-386. doi: 10.1001/jamapediatrics.2013.4653 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eFigure 1. Weekly Eyeglass Compliance Observation Reports Completed by Teachers
eFigure 2. Tracking Weekly Compliance Scores of Compliant Students (Yearlong Average Compliance Score ≥4)