Abstract
Background
China set out the vision to establishing a hierarchical medical system, with primary health care (PHC) facilities serving health care users’ first contact. Common ailments were listed, supported by a series of auxiliary policy measures. We aim to assess whether these policies were effective to prompt users’ preference to PHCs within these contexts.
Methods
Using data from three waves of National Health Service Survey, we examined trends in care users’ first contact with PHC facilities in Jilin, a north eastern province, during 2008–2018. We analysed trends and factors affecting care users’ choices, stratified by type of diseases and urban–rural settings.
Results
From 38 823 respondents, the survey identified 3302 health care users who sought outpatient care. 54.92% and 82.49% with diseases recommended to PHC, in urban and rural Jilin, respectively, contacted PHC facilities first. While 33.51% and 61.19% with diseases not recommended to PHC did so. Care users’ first contact with PHC facilities followed an inverse U shape during 2008–2018. Such trends were more profound among care users with hypertension and/or diabetes. Neither social health insurance coverage nor contracting with family doctors was associated with care users’ first contacts. Only 1.25% care users had referral experiences. Low perceived quality was the main barrier to choose PHC facilities.
Conclusion
Health care users sought PHC in a chaotic manner in Jilin. None of the recent efforts seemed effective in prompting their preference to PHC facilities. Without levering quality of PHC, an effective hierarchical medical system could be hardly forged in China.
Keywords: health services research, health policy, public health, cross-sectional survey, health systems
Summary box.
What is already known?
Previous studies using government statistics revealed a consistently decreasing trend in visits to primary health care (PHC) facilities in China. However, none of themanalysed health care users’ first contact by focusing on government recommended diseases to PHC facilities, nor did they assessed the recent policies and programmes that intended to forge a hierarchical medical system.
What are the new findings?
In Jilin, a province in north eastern China, 25.87% health care users with government recommended diseases did not contact PHC facilities first; however, 52.14% care users with diseases not recommended to PHC facilities did so. Care users’ first contact with PHC facilities flowed an inverse U shape during 2008–2018, with hypertension and diabetes the main driver for such a rise-and-fall pattern. Importantly, care users’ first contact to PHC facilities decreased by 19.80% and 12.80% points during 2013–2018 in urban and rural Jilin, respectively. Referrals from PHC facilitates were scant, enrolling in social health insurance and contracting with a family doctor was not associated with care users’ first contact. These evidence suggests that recent policies and programmes failed to prompt patients’ preference to PHC facilities.
What do the new findings imply?
Huge efforts are warranted in the provision of quality general practitioners who serve as ‘gatekeepers’ in the communities. Without improving quality of primary healthcare, an effective hierarchical medical system could be hardly forged in China.
Introduction
Internationally, strong primary care systems are associated with lower medical cost,1 increasing access to health care,2 lowering socioeconomic inequalities,3 4 better health system efficiency5 and population health.3 4 Historically, however, patients in China tended to bypass primary health care (PHC) facilities and concentrate in secondary or tertiary hospitals for primary care.6–8 The Outline of China’s National Health Service Delivery System Plan (2015–2020) set out the vision that PHC facilities, including community health hospitals and stations in the urban areas and township health hospitals and village clinics in the rural areas, should serve health care users’ first contact. The plan expected the percentage of health care users who first contact PHC facilities for outpatient care to reach at least 70% till 2017.9
In fact, in China’s new round of health system reform since 2009, enormous efforts have been made to revitalise the country’s primary health care, with the vision to forging a hierarchical medical system, where PHC facilities serve as ‘gatekeepers’ and secondary and tertiary hospitals provide specialised care. To this end, the government made a list of common and frequent ailments and chronic conditions that are recommended to first contact PHC facilities.10 11 In addition, China put forward a series of policies and programmes for better implementation. First, the government invested enormously to improve the capacity of PHC facilities, including targeted infrastructural investment, training of human resources for health and the launching of the National Essential Medicine Program.12 Second, the government made systemic efforts to link PHC providers and communities. In 2009, China scaled up the National Essential Public Health Service Program12 that budgeted PHC facilities to manage hypertension and diabetes in the communities, providing screening and a set of continuous services to patients with these conditions. In 2011, China launched the National Family Doctor Program, as a means to strengthening the linkage between communities and PHC facilities.13 In 2017, policies were additionally set to encourage ‘medical alliances’ within counties, to better integrate community-based PHC services with specialised care.14 Third, to incentivise use of PHC facilities, social health insurance schemes adjusted their reimbursement policy, offering 10% lower copayments to patients who sought care from PHC facilities compared with secondary or tertiary hospitals.15
Previous studies5 16 17 on the trends in the utilisation of PHC facilities in China mainly used government statistics that were aggregated from hospital records. The latest study revealed that number of PHC visits as a proportion of total outpatient volumes decreased from 62% to 53% during 2010–201117. However, hospital-based data could not measure patients’ first contact. Survey data from the demand side are, in thus, needed to examine trends, especially after the year 2011 when the government put forward enormous measures for a change. In addition, previous studies on factors affecting patients’ choice of health care facilities mostly focused on care users’ individual-level determinants such as income and educational achievement.18–24 Neither of them analysed the Chinese health care users’ utilisation patterns by focusing on specific type of diseases, nor did they assess the effects of the specific policies and programmes that were carried out recently.
Using three waves of provincially representative data from China’s National Health Services Survey (NHSS), we examined trends during 2008 and 2018 of health care users’ first contact with health providers in Jilin, a north eastern province. Focusing on the government’s recommended diseases to PHC facilities, and taking the various auxiliary policy measures into account, we provided a timely analysis on trends and factors that were affecting care users’ first contact with PHC facilities. We inform policymakers and programme managers whether recent efforts have been effective to attract care users’ preference to PHC facilities.
Methods
Settings
Jilin locates in north eastern China, with a moderate level of economic development and population size in China. For example, per capita gross domestic product of Jilin was US$8500 (exchange rate for US dollar in 2018: 6.62), which ranked 14th among the 31 provincial regions in China. The population of Jilin was 27 million, ranking in 21st in China. Jilin ranked middle in China in terms of its health care cost as well. For example, the average out-of-pocket medical cost on outpatient care in Jilin was US$30.8 in 2013 (ranking in 11/31) (online supplemental appendix 1).
bmjgh-2020-003907supp001.pdf (182KB, pdf)
Data
We used three waves of provincially representative survey data from Jilin in 2008, 2013 and 2018. Jilin’s provincial surveys were imbedded in China’s NHSS, which incepted from 1993 and were conducted every 5 years. China’s National Centre for Health Statistics and Information helped to draw the provincial samples in accordance with the national protocol. Specifically, each survey used multistage stratified random cluster sampling methods to select households, considering the four levels of administrative structure within a province, that is, city, district/county at county level, street/township at township level and community/village at community level. In the first stage, 13 districts/counties in 2008, 10 in 2013 and 12 in 2018, respectively, were selected out of a total of 60 based on their geographic location and population size. In the second stage, five streets (urban) or townships (rural) were sampled randomly from each selected district/county. In the third stage, one or two communities/villages were randomly selected in each street/township. Finally, 60 households were selected randomly from each community/village, and all members in which were invited to participate in the survey (online supplemental appendix 2). The response rate at household level was above 95% in each survey. A substantial proportion of questionnaires were answered by proxy family members, ranging between 10.78% and 27.60%. We included the proxy questionnaires in this analysis but performed additional sensitivity analysis.
The survey recruited public health doctors/nurses from community health centres/township hospitals to do the investigation, who were trained on the survey procedures, instruments and quality control standards. Data were cleaned for integrity, logical relationships within and between modules, mutual verification of key questions, identification of unreasonable and extreme values and dealing with missing values. Once problems were found, the quality control team contacted the investigators to check the original records and perform additional inquiries.
Patient and public involvement statement
Questionnaires used in the NHSS were designed in accordance with China’s Statistics Law25 and department regulations from the National Health Commission. Statistical results will be disclosed to the public in the form of report, but information about individual cases will not. Oral informed consents were obtained from household heads.
Measures
The survey investigated participants aged 15 years or above about each episode of illness that he/she were suffering during the past 2 weeks, including well-controlled hypertension and diabetes with a doctor’s diagnosis. In accordance with China’s health statistics standard, we defined outpatient care as visiting a doctor in any health care facilities.26 For each episode of illness, the survey asked the type of the first contacted health facilities and the respondents’ principal reason to make such choices. First contact for chronic conditions was referred as the most frequent consulted provider. For dependent variables, we ascertained the proportion of recent health care users’ first contact by type of health providers and the main reasons for such choices. We defined village clinics, township hospitals, community health centres, stations and other types of clinics as PHC facilities.27 We defined all county/street or above level hospitals and health centres as secondary or tertiary hospitals (online supplemental appendix 3). Private pharmacies were excluded because they were not considered as formal health care providers within China’s health system.28 We classified the main reasons for care users’ choice into six groups: transportation or travelling convenience, perceived better service quality, good relationship with staff in the facility, reasonable costs, health scheme designated facility and other reasons. The 2013 survey did not investigate these reasons.
We selected explanatory variables building on the Anderson’s conceptual framework.29 We considered type of diseases as need factors and classified them into two broad categories: diseases recommended to PHC facilities and diseases not recommended to PHC facilities.10 11 We grouped diseases recommended to PHC facilities into three subcategories: hypertension and/or diabetes, acute upper respiratory tract infections, and other ailments. The last group includes skin diseases, malnutrition or obesity, various kinds of inflammation, angina pectoris, neurological headache, appendicitis, inguinal hernia, foreign bodies in the eye and ear canal, epilepsy, and poisoning.
For enabling factors, we incorporated household income per capita (divided into tertiles for each survey separately) and social health insurance coverage. There were three types of social health insurance schemes in China; however, the eventual sample size was small for further breakdowns, and our preliminary analysis found that the specific types were not associated with the main outcomes (data not shown). We investigated the role of the National Essential Public Health Programme by analysing the association between completeness of care for hypertension and/or diabetes with care user’s first contact. In accordance with China’s national protocol,12 completeness of care was defined as full coverage of all the recommended interventions, including quarterly condition monitoring, suggestions for therapeutic regime adjustment and health education for lifestyle modification. The 2018 survey asked referral history for each episode of illness, and whether the care user had a contracted family doctor, defined as whether he/she had a formal contract with any PHC doctor within a government programme that provides regular consultation and health management services. For predisposing characteristics, we included care user’s sex, age, educational achievement and ethnicity.
Statistical analysis
We described health care users’ characteristics and graphed the completeness of care for hypertension, stratified by urban/rural settings. We used Poisson regressions, reporting robust SEs with adjustment to clusters, to analyse trends and factors that were affecting health care users’ first contact choice of PHC facilities, adjusting for the yearly trends, type of diseases, sex, age, household income per capita, educational achievement, social health insurance and ethnicity. This approach reported relative rates (RR) that were comparable to relative risks, which is straightforward for policy interpretation. The point estimates are consistent with logistic regression, and the confidence intervals (CIs) seemed to be more conservative.30 We stratified trends in utilisation by types of diseases and tabulated the principal reasons of care users’ choice of health providers. To yield provincially representative estimates, we stratified the analyses by urban and rural settings and weighted the data against each individual’s inverse sampling probabilities based on the whole survey samples. We performed χ2 tests to compare care users’ characteristics and the main reasons for choosing providers across urban/rural settings and type of providers. We performed Wald tests in the regression analysis. A two-sided p value of 0.05 or 0.001 was used as the cut-off point for statistical significance. We did all the analyses in STATA V.13.1, using the following command to define the survey: ‘svyset householdID [pweight=weight] || countyID || townshipID || villageID’ We excluded cases with missing values.
Results
The three surveys investigated 12 080, 13 739 and 13 004 participants 15 years and older in 2008, 2013 and 2018, respectively, from whom we included 3302 care users (urban 1028, rural 2274) who sought outpatient care during the past 2 weeks (table 1), with the proportion of 3.99% in 2008, 6.81% in 2013 and 14.50% in 2018, respectively. There are no missing values in the dependent variables, and only one participant was missing in household income and the other one was missing in educational achievement. Type of disease (p=0.117) and sex (p=0.954) was distributed similarly across urban and rural Jilin. Around 73% care users were suffering from diseases that were recommended to PHC facilities; in which, nearly 24% were hypertension and/or diabetes (urban 23.32%, rural 24.67%) and nearly 15% were acute upper respiratory tract infections (urban 13.56%, rural 16.01%). 36.40% care users in urban and 32.62% in rural Jilin, respectively, were suffering from diseases not recommended to PHC facilities. More than half of the care users- were women (56.71% in urban, 56.32% in rural) and aged 35–64 (53.96% in urban, 65.76% in rural). Social health insurance coverage was relatively high (urban 91.03%, rural 95.54%). Age, household income per capita, educational achievement, social health insurance and ethnicity distributed differently across urban and rural Jilin (p<0.001). According to the survey, the prevalence of hypertension and/or diabetes was 1.10%, 15.46% and 21.28% in Jilin in 2008, 2013 and 2018, respectively (online supplemental appendix 4).
Table 1.
Characteristics of recent healthcare users in Jilin China, 2008–2018, by urban and rural settings
| Characteristics | Urban | Rural | χ2 | P values | ||
| N | % | N | % | |||
| Year | 0.36 | 0.834 | ||||
| 2008 | 152 | 14.92 | 330 | 17.61 | ||
| 2013 | 297 | 26.68 | 638 | 29.10 | ||
| 2018 | 579 | 58.40 | 1306 | 53.29 | ||
| Type of diseases | 5.88 | 0.117 | ||||
| Diseases recommended to PHC facilities | 661 | 73.28 | 1519 | 73.30 | ||
| Hypertensions and/or diabetes | 250 | 23.32 | 538 | 24.67 | ||
| Acute upper respiratory tract infections | 137 | 13.56 | 374 | 16.01 | ||
| Other ailments | 274 | 26.72 | 607 | 26.70 | ||
| Diseases not recommended to PHC facilities | 367 | 36.40 | 755 | 32.62 | ||
| Sex | 0.00 | 0.954 | ||||
| Male | 446 | 43.29 | 989 | 43.68 | ||
| Female | 582 | 56.71 | 1285 | 56.32 | ||
| Age | 49.87 | <0.001 | ||||
| 15–34 | 96 | 9.15 | 200 | 9.10 | ||
| 35–64 | 561 | 53.96 | 1515 | 65.76 | ||
| 65- | 371 | 36.88 | 559 | 25.14 | ||
| Household income per capita | 686.40 | <0.001 | ||||
| Poor | 118 | 11.68 | 1018 | 46.51 | ||
| Middle | 258 | 24.99 | 829 | 35.36 | ||
| Rich | 651 | 63.33 | 427 | 18.13 | ||
| Missing | 1 | 0.10 | 0 | 0 | ||
| Educational achievement | 911.96 | <0.001 | ||||
| Primary school or below | 169 | 16.92 | 1371 | 58.48 | ||
| Junior high school | 329 | 31.69 | 713 | 32.72 | ||
| Senior high school | 335 | 32.58 | 147 | 6.75 | ||
| College and above | 195 | 18.82 | 42 | 2.05 | ||
| Missing | 0 | 0 | 1 | 0.04 | ||
| Social health insurance | 26.14 | <0.001 | ||||
| No | 92 | 8.97 | 101 | 4.46 | ||
| Yes | 936 | 91.03 | 2173 | 95.54 | ||
| Ethnicity | 87.91 | <0.001 | ||||
| Han majority | 865 | 85.63 | 2142 | 95.01 | ||
| Minorities | 163 | 14.37 | 132 | 4.99 | ||
The survey investigated 3302 adults (urban 1028, rural 2274) who sought outpatient care during the past 2 weeks of the survey. Proportions were adjusted by sampling weights to yield provincially representative estimates.
PHC facilities included community health centres and stations, township hospitals, village health centres and clinics.
Other ailments include skin diseases, malnutrition or obesity, various kinds of inflammation, angina pectoris, neurological headache, appendicitis, inguinal hernia, foreign bodies in the eye and ear canal, epilepsy, poisoning and so on.
Economic status was assessed by household income per capita and divided into three quantiles for each survey separately. The cut-off points were US$453.2 and US$906.3 for the 2008 survey, US$944.1 and US$1888.2 for the 2013 survey, and US$1007.1 and US$2323.8 for the 2018 survey respectively. 1$=6.62 RMB in 2018.
PHC, primary healthcare.
As shown in table 2 and online supplemental appendix 5, 66.66% recent health care users contacted PHC facilities first for outpatient care. The proportion of urban care users first contacting PHC facilities was lower than the rural ones (urban, 47.28%; rural, 75.42%). Proportion of recent health care users first contacting PHC facilities increased from 63.07% to 77.11% during 2008–2013 and decreased to 62.39% in 2018(p<0.001), respectively. In urban Jilin, proportion of care users first contacting PHC facilities increased from 36.18% to 62.29% during 2008 to 2013 and then decreased to 42.49% in 2018, whist in rural Jilin, proportion of patients first contacting PHC facilities increased from 75.45% to 84.01% during 2008–2013 and then decreased to 71.21% in 2018 (urban: p<0.001, rural: p<0.001). In urban Jilin, after adjusting for other factors (table 2), recent health care users’ probability of first contacting PHC facilities was 77% in 2008 of that in 2013 (RR: 0.77,0.56-1.07) and was 78% (RR: 0.78,0.60-0.99) in 2018 of that in 2013, respectively. The inverse U-shaped trends were not so obvious in rural Jilin, where proportion of patients choosing PHC facilities for outpatient care did not change significantly in 2013 (RR: 0.96,0.85-1.09) compared with 2008 but decreased by 9% (RR: 0.89,0.80-0.98) in 2018.
Table 2.
Factors affecting healthcare users’ first contact with PHC facilities in Jilin, China, 2008–2018, by urban and rural settings
| Factors | Urban | Rural | ||||
| First contacting PHC facilities, % | Crude RR (95% CI) |
Adjusted RR (95% CI)† |
First contacting PHC facilities, % | Crude RR (95% CI) |
Adjusted RR (95% CI)† |
|
| Year | ||||||
| 2008 | 36.18 | 0.61 (0.39 to 0.95)** | 0.77 (0.56 to 1.07) | 75.45 | 0.87 (0.77 to 1.00)* | 0.96 (0.85 to 1.09) |
| 2013 | 62.29 | ref | ref | 84.01 | ref | ref |
| 2018 | 42.49 | 0.67 (0.49 to 0.91)** | 0.78 (0.60 to 0.99)* | 71.21 | 0.83 (0.75 to 0.92)** | 0.89 (0.80 to 0.98)* |
| Type of diseases | ||||||
| Diseases recommended to PHC facilities | ||||||
| Hypertensions and/or diabetes | 62.40 | 1.86 (1.57 to 2.21)** | 1.67 (1.39 to 2.00)** | 86.80 | 1.42 (1.33 to 1.51)** | 1.39 (1.30 to 1.48)** |
| Acute upper respiratory tract infections | 74.45 | 2.22 (1.87 to 2.64)** | 2.11 (1.76 to 2.53)** | 92.25 | 1.51 (1.41 to 1.61)** | 1.50 (1.41 to 1.60)** |
| Other ailments | 38.32 | 1.14 (0.93 to 1.41) | 1.11 (0.90 to 1.36) | 72.65 | 1.19 (1.10 to 1.28)** | 1.17 (1.09 to 1.26)** |
| Diseases not recommended to PHC facilities | 33.51 | ref | ref | 61.19 | ref | ref |
| Sex | ||||||
| Male | 45.96 | ref | ref | 74.92 | ref | ref |
| Female | 48.28 | 1.05 (0.91 to 1.21) | 1.01 (0.89 to 1.15) | 75.80 | 1.01 (0.96 to 1.07) | 1.02 (0.97 to 1.06) |
| Age | ||||||
| 15–34 | 50.00 | ref | ref | 70.50 | ref | ref |
| 35–64 | 47.95 | 0.96 (0.77 to 1.19) | 0.97 (0.79 to 1.20) | 74.98 | 1.06 (0.97 to 1.17) | 1.08 (0.98 to 1.18) |
| 65 | 45.55 | 0.91 (0.72 to 1.15) | 0.88 (0.70 to 1.11) | 78.35 | 1.11 (1.01 to 1.23)* | 1.11 (1.00 to 1.23)* |
| Household income per capita | ||||||
| Poor | 58.47 | ref | ref | 76.52 | ref | ref |
| Middle | 58.53 | 1.00 (0.83 to 1.20) | 1.08 (0.91 to 1.29) | 74.31 | 0.97 (0.92 to 1.02) | 0.97 (0.92 to 1.02) |
| Rich | 40.86 | 0.70 (0.58 to 0.83)** | 0.83 (0.69 to 0.99)* | 74.94 | 0.98 (0.92 to 1.04) | 0.97 (0.91 to 1.03) |
| Educational achievement | ||||||
| Primary school or below | 57.99 | ref | ref | 76.51 | ref | ref |
| Junior high school | 51.37 | 0.89 (0.74 to 1.05) | 0.86 (0.73 to 1.02) | 74.61 | 0.98 (0.92 to 1.03) | 0.99 (0.94 to 1.05) |
| Senior high school | 44.18 | 0.76 (0.63 to 0.92)* | 0.75 (0.62 to 0.90)* | 74.15 | 0.97 (0.87 to 1.08) | 0.99 (0.90 to 1.09) |
| College and above | 36.41 | 0.63 (0.49 to 0.80)** | 0.69 (0.55 to 0.88)* | 59.52 | 0.78 (0.60 to 1.01) | 0.81 (0.65 to 1.02) |
| Social health insurance | ||||||
| No | 42.39 | ref | ref | 70.30 | ref | ref |
| Yes | 47.76 | 1.13 (0.88 to 1.44) | 1.25 (0.99 to 1.57) | 75.66 | 1.08 (0.95 to 1.22) | 1.07 (0.95 to 1.20) |
| Ethnicity | ||||||
| Han majority | 49.13 | ref | ref | 76.10 | ref | ref |
| Minorities | 37.42 | 0.76 (0.61 to 0.95)* | 0.81 (0.66 to 0.99)* | 64.39 | 0.85 (0.73 to 0.97)* | 0.89 (0.79 to 1.01) |
Data were weighted to yield provincially representative estimates.
Economic status was assessed by household income per capita and divided into three quantiles for each survey separately. The cut-off points were US$453.2 and US$906.3 for the 2008 survey, US$944.1 and US$1888.2 for the 2013 survey, and US$1007.1 and US$2323.8 for the 2018 survey respectively. 1$=6.62 RMB in 2018.
*p<0.05, **p<0.001.
†Adjusting for year, type of diseases, sex, age, household income per capita, educational achievement, social health insurance and ethnicity.
PHC, primary health care; ref, reference group; RR, relative rate.
For care users with diseases recommended to PHC facilities in urban and rural Jilin, 54.92% and 82.49%, respectively, contacted PHC facilities first; however, for care users with diseases that were not recommended to PHC facilities, 33.51% in the urban settings and 61.19% in the rural settings did choose PHC facilities as their first contact otherwise. As shown in table 2, type of diseases took the largest effects on care users’ first contacts with PHC facilities. Comparing to care users with diseases not recommended to PHC facilities, users with hypertension and/or diabetes were 67% and 39% more likely to first contact PHC facilities in urban and rural Jilin, respectively (urban RR: 1.67, 1.39–2.00; rural RR: 1.39, 1.30–1.48), and care users with acute upper respiratory tract infections were 111% and 50% more likely to first contact PHC facilities in urban and rural Jilin, respectively (urban RR: 2.11, 1.76–2.53; rural RR: 1.50, 1.41–1.60). However, other factors took small or insignificant effects on care users’ first contact. In particular, social health insurance coverage was not significantly associated with care users’ first contact with PHC facilities (urban RR: 1.25, 0.99–1.57; rural RR: 1.07, 0.95–1.20).
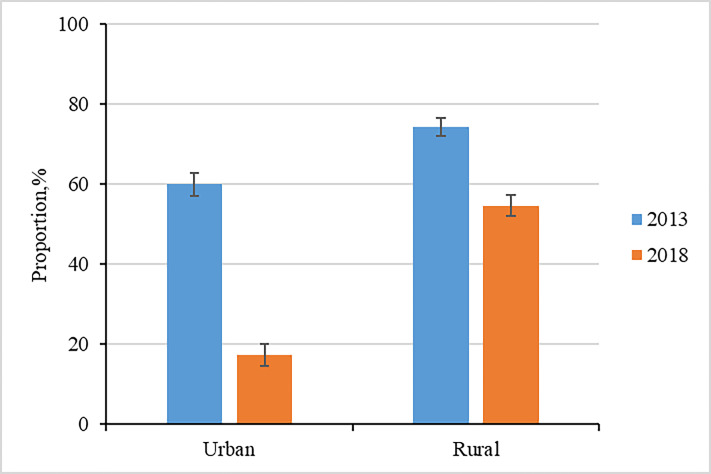
Table 3 shows the trends in recent health care users’ first contact to PHC facilities by type of diseases. Comparing to 2013, care users with diseases recommended to PHC facilities were 43%and 9% less likely to first contact PHC facilities in urban and rural Jilin, respectively (urban RR: 0.57,0.44-0.75; rural RR: 0.91,0.84-0.98) in 2008; and in 2018, they were 33%and 12% less likely to do so (urban RR: 0.67,0.58-0.77; rural RR: 0.88, 0.84–0.93). Such trends were more profound in care users with chronic conditions. Comparing to 2013, care users with hypertension and/or diabetes were 74% and 17% less likely to first contact PHC facilities in urban and rural Jilin, respectively (urban RR: 0.26, 0.11–0.62; rural RR: 0.83,0.69-0.99) in 2008; and in 2018, they were 51%and 13%less likely to do so (urban RR: 0.49,0.38-0.64; rural RR: 0.87,0.82-0.93). Notably, completeness of care in hypertension within the National EssentialPublic Health Program decreased by 42.69% and 19.63 % from 2013 to 2018, respectively (urban: 60.01% to 17.32%; rural: 74.27% to 54.64%) (figure 1). Meanwhile, the rising trends in proportion of first contacting PHC facilities among patients with acute upper respiratory tract infections were not statistically significant during 2008–2018 in either urban or rural Jilin. In addition, proportions of first contacting PHC facilities had no obvious trends among users with diseases not recommended to PHC facilities.
Table 3.
Trends in care users’ first contact to PHC facilities in Jilin, China, 2008–2018, by urban and rural settings, and type of diseases
| Diseases | Urban | Rural | ||||
| 2008 | 2013 | 2018 | 2008 | 2013 | 2018 | |
| Choice of PHC facilities, % | ||||||
| Diseases recommended to PHC facilities | 40.70 | 70.89 | 47.34 | 80.90 | 89.30 | 78.90 |
| Hypertensions and/or diabetes | 21.05 | 82.14 | 40.66 | 78.13 | 94.34 | 82.31 |
| Acute upper respiratory tract infections | 53.85 | 72.97 | 78.16 | 90.38 | 93.71 | 91.41 |
| Other ailment | 44.44 | 43.33 | 34.38 | 77.39 | 73.91 | 70.82 |
| Diseases not recommended to PHC facilities | 30.30 | 28.33 | 35.68 | 67.18 | 67.11 | 57.63 |
| Crude RR(95% CI) | ||||||
| Diseases recommended to PHC facilities | 0.57 (0.44,0.75)** | ref | 0.67 (0.58,0.77)** | 0.91 (0.84,0.98)* | ref | 0.88 (0.84,0.93)** |
| Hypertensions and/or diabetes | 0.26 (0.11,0.62)* | ref | 0.49 (0.38,0.64)** | 0.83 (0.69,0.99)* | ref | 0.87 (0.82,0.93)** |
| Acute upper respiratory tract infections | 0.74 (0.43,1.27) | ref | 1.07 (0.85,1.34) | 0.96 (0.87,1.06) | ref | 0.98 (0.92,1.04) |
| Other ailment | 1.03 (0.68,1.56) | ref | 0.79 (0.55,1.14) | 1.05 (0.90,1.21) | ref | 0.96 (0.84,1.09) |
| Diseases not recommended to PHC facilities | 1.07 (0.62,1.84) | ref | 1.26 (0.81,1.95) | 1.00 (0.85,1.18) | ref | 0.86 (0.75,0.98)* |
| Adjusted RR(95% CI)† | ||||||
| Diseases recommended to PHC facilities | 0.56 (0.43,0.74)** | ref | 0.70 (0.60,0.82)** | 0.91 (0.85,0.99)* | ref | 0.88 (0.84,0.93)** |
| Hypertensions and/or diabetes | 0.26 (0.11,0.63)* | ref | 0.61 (0.46,0.80)** | 0.82 (0.68,0.99)* | ref | 0.88 (0.83,0.94)** |
| Acute upper respiratory tract infections | 0.79 (0.48,1.33) | ref | 1.03 (0.81,1.30) | 0.99 (0.89,1.09) | ref | 0.98 (0.92,1.04) |
| Other ailments | 0.99 (0.65,1.52) | ref | 0.85 (0.58,1.25) | 1.05 (0.90,1.22) | ref | 0.94 (0.83,1.07) |
| Diseases not recommended to PHC facilities | 0.99 (0.56,1.73) | ref | 1.41 (0.89,2.25) | 1.01 (0.85,1.19) | ref | 0.87 (0.76,1.00) |
Data were weighted to yield provincially representative estimates.
*P<0.05, **p<0.001.
†Adjusting for sex, age, household income per capita, educational achievement, social health insurance and ethnicity.
PHC, primary health care; ref, reference group; RR, relative rate.
Figure 1.
Completeness of care for hypertension within the National Basic Public Health Service Program, in Jilin, China, 2013–2018, by urban and rural settings.† Completeness of care was defined as full coverage of all the recommended interventions, including quarterly condition monitoring, suggestions for therapeutic regime adjustment and health education for lifestyle modification.‡Data only available in the 2013 and 2018 survey. 95% CIs are shown.§ Adjusting for sampling, and sex, age, diseases, social health insurance, household income per capita, educational achievement and ethnicity.
In 2018, 31.22% of the urban recent health care users contracted with a family doctor, whereas 70.63% rural ones did so; however, patints’ first contact with PHC facilities seemed not be associated with whether they had a family doctor (online supplemental appendix 6). For example, in the urban setting, proportion of care users that first contacted PHC facilities for outpatient care was 45.23% and 40.78% among users contracting with and without a family doctor. In rural setting, such proportions were 73.62% and 68.93%, respectively. In addition, proportion of patients who had any referral histories was just 1.25% in 2018, and the proportion of referrals within medical alliances were just 0.45%.
Table 4 describes the principal reasons of care users’ first contact choices. The rank of principal reasons of choosing PHC facilities or secondary or tertiary facilities were similar between rural and urban settings. Over 60% care users chose PHC facilities because of distance or travelling convenience, and more than half chose secondary or tertiary facilities because of better perceived quality.
Table 4.
Principal reasons for healthcare users’ first contact health facilities in urban and rural Jilin, China, 2008 and 2018, by type of healthcare providers
| Reason | Urban | Rural | P values* | ||||||
| PHC facilities | Secondary or tertiary hospitals | PHC facilities | Secondary or tertiary hospitals | ||||||
| Number of patients | % | Number of patients | % | Number of patients | % | Number of patients | % | ||
| Transportation or travelling convenience | 178 | 59.16 | 143 | 33.65 | 770 | 65.03 | 78 | 17.27 | 0.001 |
| Perceived better service quality | 31 | 10.17 | 170 | 39.08 | 122 | 9.64 | 239 | 52.22 | |
| Good relationship with staff in the facility | 52 | 18.05 | 11 | 13.46 | 131 | 10.11 | 20 | 12.88 | |
| Reasonable cost | 27 | 8.79 | 56 | 2.71 | 83 | 7.37 | 64 | 4.72 | |
| Health scheme designated facility | 7 | 2.23 | 31 | 6.27 | 64 | 7.15 | 29 | 6.50 | |
| Other reasons | 6 | 1.60 | 19 | 4.83 | 9 | 0.70 | 27 | 6.40 | |
| P values† | <0.001 | <0.001 | |||||||
Data of principal reasons for patients’ first contact health facilities for outpatient care were only available in 2008 and 2018.
PHC facilitiesincluding community health centres and stations, township hospitals, village health centres and other clinics.
Data were weighted to yield provincially representative estimates.
*Chi-square test for difference between urban and rural settings (χ2=20.07, df=6).
†Chi-square test for difference between PHC facilities, and secondary or tertiary hospitals (urban: χ2=109.39, df=6; rural: χ2=456.65, df=6). P value of 0.001 as a cut-off point.
PHC, primary healthcare.
The same utilisation patterns were seen in the sensitivity analysis that excluded proxy answers. For example, in urban Jilin, proportion of choosing PHC facilities among care users excluding proxy cases increased from 40.87% to 62.39% during 2008–2013 and decreased to 43.10%, in 2018, respectively (online supplemental appendix 7).
Discussion
Over the past decade, the Chinese government has taken enormous measures to motivate patients’ preference to PHC facilities, aiming to build a hierarchical medical system; however, using timely survey data that were provincially representative for Jilin, a north eastern province, we found that till 2018, among recent health care users with diseases that are recommended to first contact PHC facilities—such as hypertension, diabetes and acute upper respiratory tract infections—there were still 52.66% and 21.10% choosing secondary or above hospitals as the first contact in urban and rural settings, respectively. While among care users with diseases not recommended to PHC facilities, there were about 30% and 60% in urban and rural Jilin, respectively, otherwise chose PHC facilities as their first contact. More discouragingly, care users’ first contact with PHC facilitates decreased by 19.80% and 12.80% points during 2013–2018 in urban and rural Jilin, respectively.
Primary health care plays an important role in promoting universal health coverage.31 Internationally, discussions mainly focused on how to improve service quality,32 33 the human resources for health 32–34 and the financial profiles within PHC.32–35 Literature from high-income countries reported mixed findings on the effects of gatekeeping on utilisation.33 One recent global study using data from 56 low-and middle-income countries found that hospitals are common sources of essential primary care services.36 The other study from India found that patients may bypass PHC for chronic care because of low quality.37 The other study from Latin America raised the concern on whether primary care is capable of resolving people’s health problems.38 Our case from China enriches the international discussion by reporting patients’ competitive choice of PHC providers within the context of government major health reform for a change.
Unfortunately, we found PHC facilities still failed to serve as ‘gatekeepers’ after years of health system reforms. Two-thirds of the recent healthcare users from Jilin chose PHC facilities as their first contact, which was particularly low in the urban settings (47.28%). Such performance was lower than policy-makers’ expected level of 70%.9 These findings were similar to previous reports that were conducted during 2012–2014 in urban China and the south-western region. For example, Sun et al reported a half to two-thirds patients first contacted PHC facilities in south-western China in 2014.24 Tang et al reported 62.21% patients visiting PHC facilities for outpatient care in 10 cities of urban China in 2013.22 Ye et al reported 72.62% patients chose PHC facilities for an initial visit in four counties of China in 2012.39 To our best knowledge, only two studies examined patients’ choice of health facilities by type of diseases but were all conducted before 2010, without referring to the recent developed list of recommended diseases. Specifically, Qian et al, using the NHSS data in 2008, reported 22.2% patients with acute upper respiratory tract infections seeking outpatient care first in PHC facilities in urban China.40 Yang et al reported that less than one quarter of the patients with hypertension, diabetes or chronic obstructive pulmonary disease initiated their contact with healthcare from PHC facilities in Guangdong in 2010.20 Notably, our data are the first in English literature that quantify the trends of health care users’ first contact health facilities in China during the past 10 years when major health reforms were put forward to revitalise PHC. We found that for types of diseases that are recommended to PHC facilities, the proportions of health care users that actual first contacted PHC facilities increased during 2008–2013 but decreased during 2013–2018. While for diseases that are not recommended to PHC facilities, no trends were observed. These findings suggest that recent efforts seem not to be effective in achieving its goals.
In Jilin, patients’ first contact with PHC facilities flowed an inverse U shape during 2008–2018, with hypertension and diabetes the main driver for such a rise-and-fall pattern. The Chinese government has been implementing the National Essential Public Health Program since 2009, where interventions that manage hypertension and diabetes are designated to PHC facilities.10 In the programme, PHC facilities provided screening and continuing services to residents in their catchment area free of charge.12 With rapid urbanisation and ageing, prevalence of hypertension41 and diabetes42 rose fast in China. There was a rising trend in the awareness of hypertension and diabetes in China during the past decade.41–43 Previous study found that patients with a usual source of services in PHC facilities were more satisfied with primary care.44 Thus the scaling up of free public health services may play an important role in improving patients’ preference for PHC facilities in the early stages of this programme. However, we found that completeness of care for hypertension within the National Essential Public Health Service Program decreased substantially during 2013–2018 in both urban and rural Jilin. These findings corroborated with evidence from Xinjiang and Inner Mongolia.45 As shown in recent reviews, community physicians in China were lack of systematic training with the prerequisite skills to manage chronic conditions properly, which may undermine the trust and linkage between patients and community health workers.42 46 Our data also showed that more than a quarter of the recent health care users bypassed PHC facilities for better perceived quality. Whether China’s health system reform was successful in expanding the reach of primary care services and identifying individuals in need of routine care is not known, but the compromising role of low perceived quality from PHC facilities may help explain the fall in care users’ preference for PHC facilities in recent years.
To better construct the hierarchical medical system, the government put forward a series of auxiliary policies and programmes in recent years, including differential reimbursement from social health insurance in 2010, the National Family Doctor Program in 2011 and the Medical Alliance Programs in 2017 that encourage within county referrals. However, none of these policies seems to be effective in improving users first contacting with PHC facilities. We found that social health insurance coverage was not associated with recent health care users’ first contact choice in Jilin either, which is consistent with the previous findings7 47–49 and suggests that the differential reimbursement policy was insufficient to improve first contacting of PHC facilities.7 48–50 In fact, our data showed that perceived costs were not considered by care users to make choices at all. Importantly, we found that health care users who had any referral histories were extremely low, and care users’ first contact with PHC facilities were not associated with whether or not they had any contracted family doctors either. Poor referral system between PHC facilities and secondary or above hospitals may affect continuity of service and disincentivise users’ preferences.50 Indeed, we found that only 10% patients chose PHC facilities for the reason of perceived better service quality in both urban and rural Jilin, while more than one-third patients chose secondary or above hospitals because of perceived better quality, suggesting that quality of service in PHC facilities was less attractive to health care users. Previous studies also showed that in PHC facilities quality of medical care was relatively low1 7 and the equipment was less advanced,20 51 while many drugs were unavailable.51 52 Without trust and perceived quality from PHC facilities, none of the auxiliary measures that intended to change patients’ incentives or strengthen the linkage to PHC facilities seems to be effective to make a change.
Limitations
This study has several important limitations. First, data on the main reasons for choosing healthcare facilities were only available in 2008 and 2018. We do not know why the survey designers removed these important questions; however, the missing information from 2013 largely limited our understanding to why a rise in PHC utilisation was seen in 2013. Second, our analysis was based on survey data. Although multistage stratified random cluster sampling methods were used, sampling errors might exist. For provincial representativeness, we weighted the data against the latest nationwide population census in China in 2010. Third, response rate of the surveys was high; however, nearly 10.78%–27.60% questionnaires were answered by a proxy family member. In the sensitivity analysis that excluding these cases, we had similar findings however (online supplemental appendix 7). Fourth, the survey may be encountered by recall bias, which might affect the accuracy of disease types. The NHSS recruited local public health doctors/nurses from the community to do the investigation. Misclassification in the type of providers and diseases might be low. Fifth, health insurance coverage increased quickly in our study periods and schemes varied largely; however, we could not disentangle the effects of specific type of insurance on patients’ choice, given limited sample size, for which future work is warranted.
Conclusion
Health care users sought primary care in a chaotic manner in Jilin, north eastern China. Current health system reform might be successful in expanding primary care services and identifying individuals in needs; however, none of the recent policy measures seemed to be effective in attracting health care users’ to PHC facilities. Huge efforts are warranted in the provision of quality general practitioners to serve as ‘gatekeepers’ in the communities. Without improving quality of primary health care, an effective hierarchical medical system could be hardly forged in China.
Footnotes
Handling editor: Sanni Yaya
Contributors: XLF conceived the paper. RL did the analysis under XLF’s supervision. RL and YL did the literature review. XLF made the first draft and other authors commented on the final version.
Funding: This study was supported by China National Natural Science Foundation (71761130083, 71422009).
Map disclaimer: The depiction of boundaries on this map does not imply the expression of any opinion whatsoever on the part of BMJ (or any member of its group) concerning the legal status of any country, territory, jurisdiction or area or of its authorities. This map is provided without any warranty of any kind, either express or implied.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: The data analysed in this study was obtained from a third party, the Jilin Health Information and Statistics Center. Please contact the corresponding author at fxl@bjmu.edu.cn.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Li X, Lu J, Hu S, et al. The primary health-care system in China. The Lancet 2017;390:2584–94. 10.1016/S0140-6736(17)33109-4 [DOI] [PubMed] [Google Scholar]
- 2.Kruk ME, Porignon D, Rockers PC, et al. The contribution of primary care to health and health systems in low- and middle-income countries: a critical review of major primary care initiatives. Soc Sci Med 2010;70:904–11. 10.1016/j.socscimed.2009.11.025 [DOI] [PubMed] [Google Scholar]
- 3.Macinko J, Starfield B, Shi L. The contribution of primary care systems to health outcomes within organization for economic cooperation and development (OECD) countries, 1970-1998. Health Serv Res 2003;38:831–65. 10.1111/1475-6773.00149 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kringos DS, Boerma W, van der Zee J, et al. Europe’s Strong Primary Care Systems Are Linked To Better Population Health But Also To Higher Health Spending. Health Aff 2013;32:686–94. 10.1377/hlthaff.2012.1242 [DOI] [PubMed] [Google Scholar]
- 5.Zhang L, Cheng G, Song S, et al. Efficiency performance of China's health care delivery system. Int J Health Plann Manage 2017;32:254–63. 10.1002/hpm.2425 [DOI] [PubMed] [Google Scholar]
- 6.Wang H, Gusmano MK, Cao Q. An evaluation of the policy on community health organizations in China: will the priority of new healthcare reform in China be a success? Health Policy 2011;99:37–43. 10.1016/j.healthpol.2010.07.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang HHX, Wang JJ, Wong SYS, et al. The development of urban community health centres for strengthening primary care in China: a systematic literature review. Br Med Bull 2015;116:ldv043. 10.1093/bmb/ldv043 [DOI] [PubMed] [Google Scholar]
- 8.Li H, Liu K, Gu J, et al. The development and impact of primary health care in China from 1949 to 2015: a focused review. Int J Health Plann Manage 2017;32:339–50. 10.1002/hpm.2435 [DOI] [PubMed] [Google Scholar]
- 9.State Council of the People's Republic of China Opinions on promoting the construction of hierarchical medical system, 2015. Available: http://www.gov.cn/zhengce/content/2015-09/11/content_10158.htm
- 10.State Council of the People's Republic of China Medium- and long-term plan for prevention and treatment of chronic diseases (2017-2025), 2017. Available: http://www.gov.cn/zhengce/content/2017-02/14/content_5167886.htm
- 11.The Provincial Government of Jilin Implementation plan of promoting hierarchical medical system construction in Jilin Province, 2016. Available: http://xxgk.jl.gov.cn/szf/gkml/201812/t20181205_5348277.html
- 12.State Council of the People's Republic of China Opinions on deepening the health care reform, 2009. Available: http://www.gov.cn/jrzg/2009-04/06/content_1278721.htm
- 13.State Council of the People's Republic of China Opinions on establishment of a general practitioner led primary-care, 2011. Available: http://www.gov.cn/zwgk/2011-07/07/content_1901099.htm
- 14.State Council of the People's Republic of China Opinions on promoting the construction and development of medical Consortium, 2017. Available: http://www.gov.cn/zhengce/content/2017-04/26/content_5189071.htm
- 15.State Council of the People's Republic of China Current major project on deepening health care system reform in 2010, 2010. Available: http://www.gov.cn/zwgk/2010-04/19/content_1586732.htm
- 16.Wu D, Lam TP. Underuse of primary care in China: the scale, causes, and solutions. J Am Board Fam Med 2016;29:240–7. 10.3122/jabfm.2016.02.150159 [DOI] [PubMed] [Google Scholar]
- 17.Li X, Krumholz HM, Yip W, et al. Quality of primary health care in China: challenges and recommendations. Lancet 2020;395:1802–12. 10.1016/S0140-6736(20)30122-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang HHX, Wang JJ, Wong SYS, et al. Epidemiology of multimorbidity in China and implications for the healthcare system: cross-sectional survey among 162,464 community household residents in southern China. BMC Med 2014;12:188. 10.1186/s12916-014-0188-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wang H, Liu Y, Zhu Y, et al. Health insurance benefit design and healthcare utilization in northern rural China. PLoS One 2012;7:e50395. 10.1371/journal.pone.0050395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang H, Huang X, Zhou Z, et al. Determinants of initial utilization of community healthcare services among patients with major non-communicable chronic diseases in South China. PLoS One 2014;9:e116051. 10.1371/journal.pone.0116051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hu X, Zhang H, Sun X, et al. Older adults' choices of first-contact care and related factors in Zhejiang and Qinghai Province, China. Geriatr Gerontol Int 2019;19:938–44. 10.1111/ggi.13746 [DOI] [PubMed] [Google Scholar]
- 22.Tang C, Luo Z, Fang P, et al. Do patients choose community health services (CHS) for first treatment in China? results from a community health survey in urban areas. J Community Health 2013;38:864–72. 10.1007/s10900-013-9691-z [DOI] [PubMed] [Google Scholar]
- 23.Huang M, Zhang H, Gu Y, et al. Outpatient health-seeking behavior of residents in Zhejiang and Qinghai Province, China. BMC Public Health 2019;19:967. 10.1186/s12889-019-7305-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sun X, Meng H, Ye Z, et al. Factors associated with the choice of primary care facilities for initial treatment among rural and urban residents in southwestern China. PLoS One 2019;14:e0211984. 10.1371/journal.pone.0211984 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.National Bureau of Statistics of China Statistics law of the people's Republic of China, 2009. Available: http://www.stats.gov.cn/zjtj/tjfg/tjfl/200906/t20090629_8791.html
- 26.National Health Commission of the People's Republic of China Guidance manual of the sixth National health service survey, 2018. Available: http://www.nhc.gov.cn/ewebeditor/uploadfile/2018/10/20181011142540292.pdf
- 27.State Council of the People's Republic of China Planning outline of health care system development (2015 to 2020), 2015. Available: http://www.gov.cn/zhengce/content/2015-03/30/content_9560.htm
- 28.Li J, Feng XL. Health care-seeking behaviours and health expenditures in adults aged 45 years and older in China, 2011-2013. Trop Med Int Health 2017;22:638–54. 10.1111/tmi.12865 [DOI] [PubMed] [Google Scholar]
- 29.Andersen RM Revisiting the behavioral model and access to medical care: does it matter? J Health Soc Behav 1995;36:1–10. 10.2307/2137284 [DOI] [PubMed] [Google Scholar]
- 30.Hayat MJ, Higgins M. Understanding poisson regression. J Nurs Educ 2014;53:207–15. 10.3928/01484834-20140325-04 [DOI] [PubMed] [Google Scholar]
- 31.Emma Sacks M Communities, universal health coverage and primary health care. Policy & practice 2020;98:773–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chotchoungchatchai S, Marshall AI, Witthayapipopsakul W, et al. Primary health care and sustainable development goals. Bull World Health Organ 2020;98:792–800. 10.2471/BLT.19.245613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kruk ME, Gage AD, Arsenault C, et al. High-Quality health systems in the sustainable development goals era: time for a revolution. Lancet Glob Health 2018;6:e1196–252. 10.1016/S2214-109X(18)30386-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Langlois EV, McKenzie A, Schneider H, et al. Measures to strengthen primary health-care systems in low- and middle-income countries. Bull World Health Organ 2020;98:781–91. 10.2471/BLT.20.252742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Stenberg K, Hanssen O, Bertram M, et al. Guide posts for investment in primary health care and projected resource needs in 67 low-income and middle-income countries: a modelling study. Lancet Glob Health 2019;7:e1500–10. 10.1016/S2214-109X(19)30416-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Arsenault C, Kim MK, Aryal A, et al. Hospital-provision of essential primary care in 56 countries: determinants and quality. Bull World Health Organ 2020;98:735–46. 10.2471/BLT.19.245563 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kujawski SA, Leslie HH, Prabhakaran D, et al. Reasons for low utilisation of public facilities among households with hypertension: analysis of a population-based survey in India. BMJ Glob Health 2018;3:e001002. 10.1136/bmjgh-2018-001002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Macinko J, Guanais FC, Mullachery P, et al. Gaps in primary care and health system performance in six Latin American and Caribbean countries. Health Aff 2016;35:1513–21. 10.1377/hlthaff.2015.1366 [DOI] [PubMed] [Google Scholar]
- 39.Ye T, Niehoff J-U, Zhang Y, et al. Which medical institution should perform gatekeeping in rural China? results from a cross-sectional study. Gesundheitswesen 2017;79:e10–17. 10.1055/s-0042-111824 [DOI] [PubMed] [Google Scholar]
- 40.Qian D, Lucas H, Chen J, et al. Determinants of the use of different types of health care provider in urban China: a tracer illness study of URTI. Health Policy 2010;98:227–35. 10.1016/j.healthpol.2010.06.014 [DOI] [PubMed] [Google Scholar]
- 41.Fang L, Song J, Ma Z, et al. Prevalence and characteristics of hypertension in mainland Chinese adults over decades: a systematic review. J Hum Hypertens 2014;28:649–56. 10.1038/jhh.2014.5 [DOI] [PubMed] [Google Scholar]
- 42.Li Y, Teng D, Shi X, et al. Prevalence of diabetes recorded in mainland China using 2018 diagnostic criteria from the American diabetes association: national cross sectional study. BMJ 2020;369:m997. 10.1136/bmj.m997 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Chan JCN, Zhang Y, Ning G. Diabetes in China: a societal solution for a personal challenge. Lancet Diabetes Endocrinol 2014;2:969–79. 10.1016/S2213-8587(14)70144-5 [DOI] [PubMed] [Google Scholar]
- 44.Zhang L, Li J, Ma T, et al. Usual source of care and experiences with primary care among community health service centre patients in Changchun, China: a cross-sectional survey. Health Soc Care Community 2020;28:1979–88. 10.1111/hsc.13009 [DOI] [PubMed] [Google Scholar]
- 45.Zhanchu J Study on follow-up management on patients with hypertension in two rural areas in the border regions of China. Acta Universitatis Medicinalis Nanjing 2014;14:95–9. [Google Scholar]
- 46.Yang G, Wang Y, Zeng Y, et al. Rapid health transition in China, 1990–2010: findings from the global burden of disease study 2010. The Lancet 2013;381:1987–2015. 10.1016/S0140-6736(13)61097-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Liu GG, Vortherms SA, Hong X. China’s Health Reform Update. Annu Rev Public Health 2017;38:431–48. 10.1146/annurev-publhealth-031816-044247 [DOI] [PubMed] [Google Scholar]
- 48.Niu Y, Zhang L, Ye T, et al. Can unsuccessful treatment in primary medical institutions influence patients' choice? A retrospective cluster sample study from China. BMJ Open 2019;9:e022304. 10.1136/bmjopen-2018-022304 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang L, Wang Z, Qian D, et al. Effects of changes in health insurance reimbursement level on outpatient service utilization of rural diabetics: evidence from Jiangsu Province, China. BMC Health Serv Res 2014;14:185. 10.1186/1472-6963-14-185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Jiang C, Zou M, Chen M, et al. Reliability and validity of the mandarin version of the continuity assessment record and evaluation for older people who are transferred between hospitals and nursing homes in China. Health Soc Care Community 2020;28:1180–9. 10.1111/hsc.12951 [DOI] [PubMed] [Google Scholar]
- 51.Zhou Z, Wang C, Yang H, et al. Health-Related quality of life and preferred health-seeking institutions among rural elderly individuals with and without chronic conditions: a population-based study in Guangdong Province, China. Biomed Res Int 2014;2014:1–10. 10.1155/2014/192376 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zhou XD, Li L, Hesketh T. Health system reform in rural China: voices of healthworkers and service-users. Soc Sci Med 2014;117:134–41. 10.1016/j.socscimed.2014.07.040 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2020-003907supp001.pdf (182KB, pdf)