Abstract
Objective
In phase II and III trials, anifrolumab, a human monoclonal antibody that binds type I interferon receptor subunit 1, has shown efficacy in adults with moderate to severe SLE. We evaluated the safety and tolerability of anifrolumab using data pooled from these trials to more precisely estimate the rate and severity of adverse events (AEs).
Methods
Data were pooled from patients receiving monthly intravenous anifrolumab 300 mg or placebo in MUSE, TULIP-1 and TULIP-2. Key safety endpoints included percentages and exposure-adjusted incidence rates (EAIRs) of patients who experienced AEs, serious AEs (SAEs), AEs leading to discontinuation and AEs of special interest.
Results
During treatment, 86.9% of patients receiving anifrolumab 300 mg (n=459) experienced AEs (≥1) versus 79.4% receiving placebo (n=466), and 4.1% versus 5.2% experienced an AE leading to discontinuation of investigational product. SAEs (≥1) were experienced by 11.8% and 16.7% of patients receiving anifrolumab and placebo, respectively (EAIR risk difference (95% CI) −7.2 (−12.5 to –1.9)), including lupus exacerbations classified as SAEs (1.5% and 3%, respectively). Infections occurred in 69.7% and 55.4% of patients receiving anifrolumab and placebo, respectively; difference in reported rates was driven by herpes zoster (HZ) and mild and moderate respiratory (excluding pneumonia) infections. The risk of HZ was increased with anifrolumab versus placebo (6.1% vs 1.3%, respectively; EAIR risk difference (95% CI) 5.4 (2.8 to 8.4)); most HZ events were mild or moderate, cutaneous and resolved without treatment discontinuation. Serious infections occurred in 4.8% and 5.6% of patients receiving anifrolumab and placebo, respectively.
Conclusions
In this pooled analysis of 925 patients with moderate to severe SLE, monthly intravenous anifrolumab 300 mg was generally well tolerated over 52 weeks with an acceptable safety profile. Anifrolumab was associated with an increased incidence of HZ and respiratory tract infections and lower reported rate of SLE worsening as SAEs.
Keywords: lupus erythematosus, systemic, biological products, interferon type I, therapeutics, outcome assessment, health care
Key messages.
What is already known about this subject?
In phase II and III trials, anifrolumab, a human monoclonal antibody that binds the type I interferon receptor subunit 1, has shown efficacy in adults with moderate to severe SLE, including global disease activity improvement, SLE flare reduction and the ability to permit glucocorticoid dosage tapering.
What does this study add?
We evaluated the safety and tolerability of anifrolumab using data from these phase II and III trials to more precisely characterise the safety profile.
In this pooled analysis of 925 patients with moderate to severe SLE, monthly intravenous anifrolumab 300 mg was generally well tolerated over 52 weeks with a manageable safety profile.
Anifrolumab was associated with an increased incidence of herpes zoster and respiratory tract infections and a lower reported rate of SLE worsening.
How might this impact on clinical practice or future developments?
Taken together with the previously reported efficacy results in phase II and III trials, anifrolumab has a positive benefit–risk profile and is a potential new treatment option for a disease with few therapeutic options.
Introduction
SLE is a chronic, multisystemic autoimmune disease associated with substantial morbidity and mortality.1 2 Compared with the general population, studies of patients with SLE also indicate 1.6-fold to 7.8-fold higher rates of several comorbidities, including infections/pneumonia, malignancy, cardiovascular (CV) mortality, ischaemic stroke, myocardial infarction, depression and suicidality.3–11 Standard-of-care (SOC) therapies for SLE, such as antimalarials, immunosuppressants and glucocorticoids are associated with deleterious effects that include retinopathy, CV disease, osteoporosis, cataracts, metabolic abnormalities and increased risk of infections.12–14
Anifrolumab is a human monoclonal antibody that binds the type I interferon (IFN) receptor subunit 1 (IFNAR1). This results in blockade of receptor-mediated type I IFN signalling and subsequent inhibition of IFN-responsive gene expression and downstream inflammatory and immunologic sequelae.15 Potential safety concerns related to IFNAR blockade include those associated with immunomodulation, such as opportunistic infections, viral infections (including reactivation) and malignancy.16 Protein-based infusions also pose risks of hypersensitivity reactions and other infusion-related reactions, independent of the drug’s mechanism of action.17
Anifrolumab has been studied for the treatment of adults with moderate to severe SLE in three randomised, double-blind, placebo-controlled, 52-week trials: the MUSE (NCT01438489) phase II trial and the TULIP-1 (NCT02446912) and TULIP-2 (NCT02446899) phase III trials.18–20 In all three studies, monthly intravenous anifrolumab 300 mg was associated with increased rates of response compared with placebo in British Isles Lupus Assessment Group-based Composite Lupus Assessment response rates at week 52. A consistent benefit was also observed with anifrolumab across a range of other clinically significant efficacy endpoints, including sustained glucocorticoid dosage reduction, reduction in severity of skin disease and reduction in flares.
Understanding the safety profile of anifrolumab and its impact on SLE comorbidities is essential for evaluation of its potential utilisation in the SLE treatment paradigm. Therefore, extensive safety monitoring and evaluation was incorporated into the design of the MUSE, TULIP-1 and TULIP-2 studies (details provided in online supplemental appendix).
lupus-2020-000464supp001.pdf (265.9KB, pdf)
The aim of this analysis was to evaluate the safety and tolerability of anifrolumab 300 mg intravenous every 4 weeks relative to placebo, using data pooled from three similarly designed trials (although with differing primary endpoints) to provide more precise estimates of treatment effect on safety than in the individual trials. These trials encompass a population representative of the SLE population with moderate to severe disease despite SOC therapy who are generally seen in clinical practice, with the exception of exclusions (eg, chronic infections, hepatitis and immunodeficiency) to minimise confounding of the safety evaluation.
Methods
Study design and patients
The detailed methods for each study have been previously reported.18–20 MUSE, TULIP-1 and TULIP-2 were randomised, double-blind, 52-week trials that each included evaluation of anifrolumab 300 mg (intravenous every 4 weeks for 48 weeks) or placebo, in patients with moderate to severe SLE despite SOC treatment. MUSE and TULIP-1 also included a higher (1000 mg) and lower (150 mg) dose, respectively. Data from patients who received anifrolumab 300 mg intravenous monthly or placebo in MUSE, TULIP-1 and TULIP-2 were pooled. Because of differences in data collection between MUSE and TULIP, some pooled analyses only included data from the anifrolumab 300 mg arms in TULIP-1 and TULIP-2 (details provided in online supplemental appendix).
The extensive safety evaluation mechanisms incorporated into the anifrolumab clinical development programme included a data safety monitoring board in all three clinical trials (MUSE, TULIP-1 and TULIP-2), as well as the following in TULIP-1 and TULIP-2: Cardiovascular Event Adjudication Committee, Columbia Suicide Severity Rating Scale (C-SSRS) at every visit and Personal Health Questionnaire Depression Scale-8 (PHQ-8) at day 1 and weeks 12, 24, 36 and 52. Further details are provided in the online supplemental appendix.
Safety evaluations and statistical analysis
Safety endpoints analysed from all three studies included percentages and exposure-adjusted incidence rates (EAIRs) of patients receiving placebo or anifrolumab 300 mg who experienced any adverse events (AEs), serious AEs (SAEs), AEs leading to discontinuation of investigational product and AEs of special interest (AESIs) (details provided in online supplemental appendix methods and table S1). A patient with an event that met the criteria for more than one AE category was counted once in each category. Patients with multiple events in the same category are counted only once in that category.
The safety analysis set comprised all patients who received ≥1 dose of anifrolumab or placebo, and patients were analysed according to the treatment they received. Details of the statistical analysis are provided in the supplementary appendix.
Results
Study population
In this integrated safety analysis, 459 and 466 patients received ≥1 dose of anifrolumab 300 mg or placebo, respectively, and comprise the safety analysis set. Additionally, 93 patients received ≥1 dose of anifrolumab 150 mg in TULIP-1 and 105 patients received anifrolumab 1000 mg in MUSE. The latter group included one patient assigned to placebo who erroneously received one dose of anifrolumab 1000 mg.
Baseline demographics, SLE disease severity, SLE treatment and prevalence of CV risk factors and CV disease were similar between patients receiving anifrolumab 300 mg and placebo (online supplemental appendix table S2 and S3). Most patients were female (~93% in both treatment groups) and were predominantly white (59% and 61% in the anifrolumab and placebo groups, respectively), with a mean age of 41 years. African-American patients comprised 14% and 13% of the anifrolumab and placebo groups, respectively, and Asian patients comprised approximately 10% of patients in both treatment groups. Approximately 28% of patients in both treatment groups were of Hispanic or Latino ethnicity.
At baseline in pooled TULIP trials data, 80.8% and 83.0% of patients in the anifrolumab 300 mg and placebo groups, respectively, were receiving glucocorticoids, with approximately half in each treatment group receiving prednisone ≥10 mg/day or equivalent (online supplemental appendix table S3). In both treatment groups, approximately 70% were receiving antimalarials and approximately half of the patients were receiving immunosuppressants including azathioprine, methotrexate, mycophenolate and mizoribine (online supplemental appendix table S3). SLE medication use at baseline in the MUSE trial was similar to that in the TULIP trials (online supplemental appendix table S3).
In all three studies, non-SLE medications taken during the 52-week studies were similar across treatment groups; the most common included paracetamol, omeprazole and folic acid. In TULIP-1 and TULIP-2, where this information was available, the most commonly reported comorbidities at baseline were hypertension (30.7%), gastro-oesophageal reflux disease (15.7%), depression (15.6%), insomnia (14.2%), anxiety (11.7%), hypothyroidism (11.0%), Raynaud’s phenomenon (10.7%), fibromyalgia (10.3%), secondary Sjögren’s syndrome (10.2%) and migraine (10.1%).
Baseline CV risk factors in all three studies combined are listed in online supplemental appendix table S2. The percentages of patients with diabetes or hypertension at baseline were 5.7% and 33.8%, respectively, among patients receiving anifrolumab 300 mg, and 3.6% and 28.8% respectively, among patients receiving placebo. In the pooled TULIP trials, percentages of patients with a history of CV disease at baseline among anifrolumab treated and placebo groups, respectively, were: acute myocardial infarction (0% and 1.4%), unstable angina (0% and 0.3%), coronary revascularisation (0.3% and 0.8%) and heart failure (1.1% and 0.5%).
Fewer patients in the anifrolumab 300 mg group prematurely discontinued treatment compared with patients who discontinued placebo (16.1% vs 26.0%). This held true for each of the most common reasons for discontinuation, including withdrawal by patient (5.4% vs 9.0%), AE (4.4% vs 6.4%) and lack of efficacy (1.1% vs 4.5%). Time to discontinuation for patients receiving anifrolumab and placebo is shown in online supplemental appendix figure S1). More patients in the anifrolumab 300 mg group were exposed to at least 48 weeks of treatment compared with the placebo group (84.3% vs 75.3%), and total patient-years of exposure was slightly greater (419.4 and 403.0 years, respectively).
Adverse events
The percentage of patients with ≥1 AE during study duration was greater in the anifrolumab 300 mg group (86.9% (399/459)) than in the placebo group (79.4% (370/466)) (table 1). Most AEs were mild or moderate in intensity (36.6% and 41.2%, respectively, among patients receiving anifrolumab, and 38.4% and 33.0%, respectively, among patients receiving placebo). In the anifrolumab group, the most frequently reported AEs were nasopharyngitis, upper respiratory tract infection, urinary tract infection, bronchitis and infusion-related reaction (table 2). AEs that were more common in the anifrolumab group than in the placebo group (ie, ≥5% difference or ≥5% incidence in the anifrolumab group and at least twice the rate of the placebo group) were nasopharyngitis, upper respiratory tract infection, bronchitis, and herpes zoster (HZ). No clinically meaningful differences were observed in the frequency or pattern of AEs for patients receiving anifrolumab and classified at baseline as interferon gene signature (IFNGS) high (76.2% with any AE above the reporting threshold of 2% (227/298)) versus IFNGS low (77.4% (48/62)) in pooled data from TULIP-1 and TULIP-2.
Table 1.
AEs in patients during treatment in pooled MUSE, TULIP-1 and TULIP-2 data
| Anifrolumab 300 mg (n=459) |
Placebo (n=466) |
EAIR risk difference (anifrolumab 300 mg – placebo) (95% CI) | |||
| n (%) | EAIR | n (%) | EAIR | ||
| Any AE* | 399 (86.9) | 290.1 | 370 (79.4) | 225.2 | NR |
| SAE | 54 (11.8) | 13.6 | 78 (16.7) | 20.7 | −7.2 (−12.5 to −1.9) |
| Death | 2 (0.4) | 0.5 | 0 | 0 | 0.5 (−0.5 to 1.7) |
| DAE | 19 (4.1) | 4.5 | 24 (5.2) | 6.0 | −1.4 (−4.7 to 1.7) |
| AESI†‡ | 61 (13.3) | 15.5 | 47 (10.1) | 12.2 | 3.3 (–1.5 to 8.2) |
| Non-opportunistic serious infections | 22 (4.8) | 5.4 | 26 (5.6) | 6.6 | −1.3 (−4.7 to 2.1) |
| Opportunistic infections | 1 (0.2) | 0.2 | 1 (0.2) | 0.2 | −0.0 (−1.2 to 1.1) |
| Anaphylaxis | 0 | 0 | 0 | 0 | 0 |
| Malignancy | 3 (0.7) | 0.7 | 3 (0.6) | 0.7 | −0.0 (−1.5 to 1.4) |
| Herpes zoster | 28 (6.1) | 6.9 | 6 (1.3) | 1.5 | 5.4 (2.8 to 8.4) |
| Active TB | 0 | 0 | 0 | 0 | 0 |
| Latent TB§ | 4 (0.9) | 1.0 | 1 (0.2) | 0.2 | 0.7 (−0.5 to 2.2) |
| Influenza | 12 (2.6) | 2.9 | 9 (1.9) | 2.3 | 0.6 (−1.7 to 3.0) |
| Non–SLE-related vasculitis | 0 | 0 | 2 (0.4) | 0.5 | −0.5 (−1.8 to 0.4) |
| Major adverse cardiovascular event | 1 (0.2) | 0.2 | 3 (0.6) | 0.7 | −0.5 (−2.0 to 0.7) |
EAIR was reported per 100 patient-years and calculated as the number of patients with an event/[sum of time at risk in days/(365.25×100)].
*AEs were coded by MedDRA V.22.1. An AE during intervention period was defined as an AE with a date of onset on or after the day of the first dose of anifrolumab or placebo and on or before the day of the last dose of anifrolumab or placebo plus 28 days.
†AESIs differed from the individual MUSE and TULIP trials and were identified using standardised MedDRA queries and custom preferred term groupings.
‡Hypersensitivity was included as an AESI in MUSE but not in the TULIP trials and is not included in this table.
§Patients with latent TB (not active TB) were interferon gamma release assay positive without radiographic or clinical manifestations of active TB.
AE, adverse event; AESI, AE of special interest; DAE, AE leading to discontinuation of investigational product; EAIR, exposure-adjusted incidence rate; MedDRA, Medical Dictionary for Regulatory Activities; NR, not reported; SAE, serious AE; TB, tuberculosis.
Table 2.
AEs reported by ≥2% of patients in pooled MUSE, TULIP-1 and TULIP-2 data
| AE* | Anifrolumab 300 mg (n=459) | Placebo (n=466) |
| n (%) | n (%) | |
| Nasopharyngitis† | 75 (16.3) | 44 (9.4) |
| Upper respiratory tract infection† | 71 (15.5) | 45 (9.7) |
| Urinary tract infection | 55 (12.0) | 63 (13.5) |
| Bronchitis† | 45 (9.8) | 20 (4.3) |
| Infusion-related reaction | 43 (9.4) | 33 (7.1) |
| Headache | 37 (8.1) | 45 (9.7) |
| Herpes zoster† | 28 (6.1) | 6 (1.3) |
| Back pain | 24 (5.2) | 20 (4.3) |
| Sinusitis | 24 (5.2) | 24 (5.2) |
| Cough | 23 (5.0) | 15 (3.2) |
| Arthralgia | 22 (4.8) | 9 (1.9) |
| Pharyngitis | 21 (4.6) | 17 (3.6) |
| Vomiting | 18 (3.9) | 12 (2.6) |
| Nausea | 17 (3.7) | 25 (5.4) |
| Oral herpes | 17 (3.7) | 12 (2.6) |
| Pneumonia | 15 (3.3) | 13 (2.8) |
| Diarrhoea | 14 (3.1) | 25 (5.4) |
| Respiratory tract infection | 14 (3.1) | 2 (0.4) |
| Depression | 13 (2.8) | 8 (1.7) |
| Gastroenteritis | 13 (2.8) | 14 (3.0) |
| Hypersensitivity | 13 (2.8) | 3 (0.6) |
| Influenza | 12 (2.6) | 9 (1.9) |
| Gastroenteritis (viral) | 11 (2.4) | 7 (1.5) |
| Gastro-oesophageal reflux disease | 11 (2.4) | 12 (2.6) |
| Pain in extremity | 11 (2.4) | 3 (0.6) |
| Anxiety | 10 (2.2) | 8 (1.7) |
| Dizziness | 10 (2.2) | 12 (2.6) |
| Fatigue | 10 (2.2) | 9 (1.9) |
| Peripheral oedema | 10 (2.2) | 4 (0.9) |
| SLE | 10 (2.2) | 14 (3.0) |
| Insomnia | 9 (2.0) | 19 (4.1) |
EAIR was reported per 100 patient-years and calculated as the number of patients with an event/[sum of time at risk in days/(365.25×100)].
*AEs were coded by MedDRA V.22.1. An AE during the intervention period was defined as an AE with a date of onset on or after the day of the first dose of anifrolumab or placebo and on or before the day of the last dose of anifrolumab or placebo plus 28 days.
†AEs more common in the anifrolumab 300 mg group than in the placebo group (ie, ≥5% difference, or ≥5% incidence in the anifrolumab group and at least twice the reported rate of the placebo group).
AE, adverse event; MedDRA, Medical Dictionary for Regulatory Activities.
A total of 54/459 patients (11.8%) receiving anifrolumab 300 mg and 78/466 (16.7%) receiving placebo experienced ≥1 SAE during treatment (table 1). SAEs included infections (anifrolumab: 22 (4.8%) and placebo: 26 (5.6%), of which pneumonia accounted for eight (1.7%) and nine (1.9%), respectively), as well as worsening of SLE that met criteria for an SAE (7 (1.5%) and 14 (3.0%), respectively).
Discontinuations due to AEs and deaths
AEs led to discontinuation of investigational product in 19 (4.1%) patients receiving anifrolumab 300 mg and 24 (5.2%) receiving placebo. During the three 52-week controlled studies, there were two deaths among patients treated with anifrolumab 300 mg, both due to pneumonia, with one case considered by the investigator to be related to the investigational product (day 221) and one (day 64) considered not related. There was also one death in a patient treated with anifrolumab 1000 mg (due to colitis (day 34), considered unrelated to treatment), and one death in a patient receiving placebo (due to encephalitis (day 35); not shown in table 1 as it occurred during the follow-up period).
AEs of special interest
AESIs that occurred in patients receiving placebo and anifrolumab 300 mg are summarised in table 1.
Infections
Infections overall during treatment, as categorised using the Medical Dictionary for Regulatory Activities (MedDRA) System Organ Class infections and infestations were reported in a greater percentage of patients in the anifrolumab 300 mg group than in the placebo group (69.7% (320/459) vs 55.4% (258/466)). Most infections in both treatment groups were mild or moderate in intensity, were not classified as SAEs and did not result in discontinuation of anifrolumab or placebo. The difference between the reported rates of infection was driven by differences in the incidence of mild and moderate infections involving the respiratory tract, excluding pneumonia (which was similar between both treatment groups) and separately by HZ. Non-opportunistic serious infection rates were similar and occurred in 4.8% and 5.6% of patients receiving anifrolumab and placebo, respectively (table 1).
Three opportunistic infections were reported: one anifrolumab patient had a non-serious AE with preferred term (PT) mycobacterium avium complex infection that led to treatment discontinuation, and two placebo patients had opportunistic infections (PT oropharyngeal candidiasis, PT meningitis cryptococcal). The rate of influenza was similar between groups, and no cases of active TB were reported.
Herpes zoster
Patients in the anifrolumab 300 mg group had an increased risk of HZ compared with patients in the placebo group (6.1% and 1.3%, respectively; EAIR risk difference (95% CI) 5.4 (2.8 to 8.4)) (table 3). In TULIP-1, HZ occurred in 5.4% and 1.6% of patients receiving anifrolumab 150 mg (n=93) and placebo (n=184), respectively. The rate of HZ was greater for patients receiving anifrolumab 1000 mg (n=105) in MUSE, 8.6% versus 1.0% for placebo (n=101) (online supplemental appendix table S4).
Table 3.
Herpes zoster events in patients during treatment with anifrolumab 300 mg versus placebo in pooled MUSE, TULIP-1 and TULIP-2 data
| Anifrolumab 300 mg (n=459) n (%) |
EAIR (per 100 PY) |
Placebo (n=466) n (%) |
EAIR (per 100 PY) |
EAIR (per 100 PY) risk difference (anifrolumab 300 mg − placebo) (95% CI) |
|
| Any AE | 28 (6.1) | 6.9 | 6 (1.3) | 1.5 | 5.4 (2.8 to 8.4) |
| Any AE with outcome of death | 0 | 0 | 0 | 0 | 0 |
| Any SAE | 2 (0.4) | 0.5 | 0 | 0 | 0.5 (−0.5 to 1.7) |
| Any DAE | 2 (0.4) | 0.5 | 0 | 0 | 0.5 (−0.5 to 1.7) |
| Any AE by maximum reported intensity | |||||
| Mild | 9 (2.0) | 2.2 | 1 (0.2) | 0.3 | - |
| Moderate | 17 (3.7) | 4.1 | 5 (1.1) | 1.2 | - |
| Severe | 2 (0.4) | 0.5 | 0 | 0 | - |
EAIR was reported per 100 PY and defined as the number of patients with the specific event divided by the total exposure time in years and then multiplied by 100. The exposure time was defined as the time from the date of first administration of investigational product to the date of first event, death, end of treatment plus 28 days or end of study, whatever came first.
AE, adverse event; DAE, AE leading to discontinuation of investigational product; EAIR, exposure-adjusted incidence rate; PY, patient-years; SAE, serious AE.
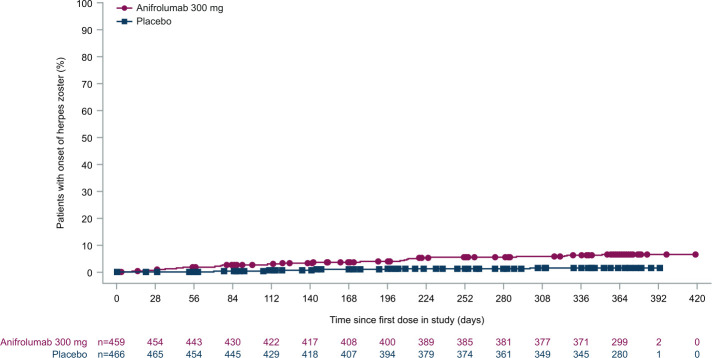
Across the placebo and anifrolumab 300 mg groups from all three studies, in the 34 patients with HZ AEs, 32 patients had mild or moderate cases and two patients had a severe case (table 3); most cases were cutaneous. Two patients treated with anifrolumab 300 mg had HZ SAEs. One patient receiving anifrolumab 300 mg discontinued treatment due to transverse myelitis with a positive PCR test for HZ in the cerebrospinal fluid and no cutaneous presentation. This patient responded to antiviral and high-dose glucocorticoid treatment and fully recovered without sequela. The patient had received two doses of anifrolumab and was also receiving concomitant treatment with immunosuppressants. This AE was assessed by the investigator to be unrelated to treatment. All patients in the anifrolumab 300 mg group and four of six patients in the placebo group with HZ AEs received antiviral treatment and all cases resolved. Of the 34 patients with HZ AEs, 32 continued in the study; AEs leading to discontinuation were non-serious, with the exception of the transverse myelitis case. Among patients for whom data regarding dermatome involvement were available (TULIP-1 and TULIP-2), four cases involved three or more dermatomes (anifrolumab 300 mg: n=3; placebo: n=1). Time to first onset of HZ was slightly shorter in the anifrolumab 300 mg than in the placebo group (figure 1). Among patients for whom data regarding history of HZ prior to study enrolment were available (TULIP-1 and TULIP-2) and in whom HZ occurred during treatment, 4 of the 23 patients receiving anifrolumab 300 mg and one of the five patients receiving placebo had a history of HZ prior to study enrolment.
Figure 1.
Time to first onset of herpes zoster during treatment with anifrolumab 300 mg versus placebo in pooled MUSE, TULIP-1 and TULIP-2 data. If a patient had no herpes zoster during treatment, the time to first onset was censored at the date of last administration of investigational product plus 28 days.
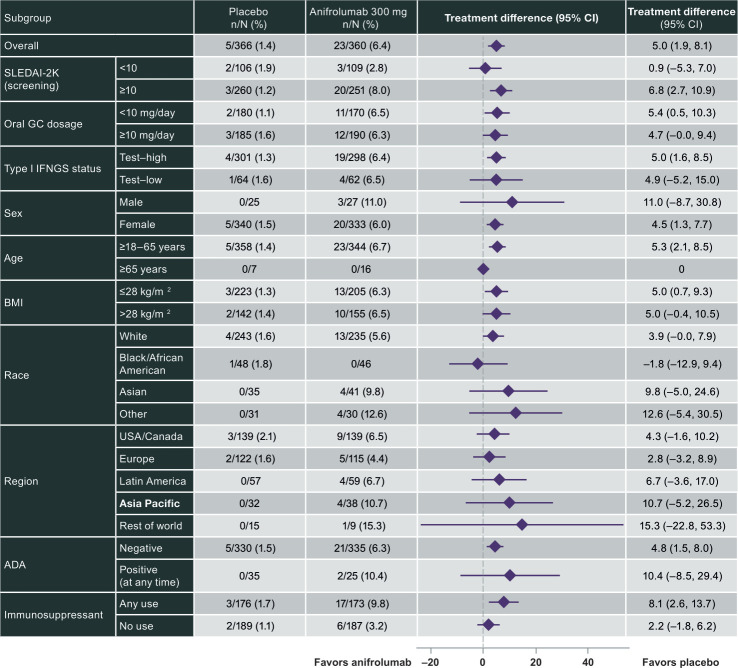
Subgroup analyses of pooled data available from TULIP-1 and TULIP-2 did not suggest any clear trends in HZ cases by demographics, baseline disease characteristics or SLE-related medication use (figure 2). However, the rate of HZ events was greater in the anifrolumab 300 mg group among patients who received immunosuppressant (9.8%, n=17) than those who did not receive immunosuppressant (3.2%, n=6).
Figure 2.
Adjusted difference in cumulative proportions of patients with herpes zoster events in subgroups of patients treated with anifrolumab 300 mg versus placebo in pooled TULIP-1 and TULIP-2 data. ADA, antidrug antibody; BMI, body mass index; IFNGS, interferon gene signature; GC, glucocorticoid; SLEDAI-2K, Systemic Lupus Erythematosus Disease Activity Index 2000. Immunosuppressant use is defined at baseline. Left and right bars indicate the lower and upper limit of the 95% CI. Numbers under ‘(%)’ indicate the cumulative proportion.
Malignancy
Malignancies, including nonmelanoma skin cancers, were reported in six patients (1.3% (6/459)) receiving anifrolumab 300 mg and three patients (0.6% (3/466)) receiving placebo. Excluding non-melanoma skin cancers, malignancies were reported in three patients (0.65%) receiving anifrolumab (two invasive ductal breast carcinoma and one B cell lymphoma, the latter existing before first dose of anifrolumab) and in three patients (0.6%) receiving placebo (one carcinoid tumour, one squamous cell carcinoma of the cervix and one uterine cancer).
Other AESIs
Among patients in TULIP-1 and TULIP-2, adjudicated major adverse cardiovascular events were reported in one patient receiving anifrolumab 300 mg (non-fatal myocardial infarction) and in no patients in the placebo group. In the MUSE study, in which events were not adjudicated, no CV events were reported among patients receiving anifrolumab 300 mg (n=99), and three were reported among patients receiving placebo (two ischaemic strokes and one cerebral infarction). Non-SLE-related vasculitis was not observed in any anifrolumab-treated patients.
Anaphylaxis, hypersensitivity and infusion-related reactions
Hypersensitivity reactions were reported by 2.6% (12/459) and 0.6% (3/466) of patients receiving anifrolumab 300 mg and placebo, respectively. These events were predominantly mild or moderate in intensity and occurred during the first 12 weeks (ie, first three to four infusions). One patient receiving anifrolumab 300 mg experienced a serious hypersensitivity event, which was treated, and anifrolumab treatment was continued. Anaphylaxis was not reported among any patients receiving anifrolumab 300 mg but was reported in one patient receiving anifrolumab 150 mg; this patient was treated, the condition resolved and the patient discontinued study treatment.
Infusion-related reactions occurred in 43/459 patients (9.4%) receiving anifrolumab 300 mg and 33/466 (7.1%) receiving placebo. All were mild or moderate in intensity, and most occurred in the first 24 weeks of treatment. In data available only for the pooled TULIP trials, the most common infusion-related reaction symptoms among patients receiving anifrolumab were headache, nausea, vomiting and fatigue.
Other safety events
In pooled data available only for the TULIP trials, there was no evidence of increased risk for suicidality per assessment with the C-SSRS or reported AEs, or for depression based on PHQ-8 scores and the standardised MedDRA queries depression (excluding suicide and self-injury) narrow search (details provided in online supplemental results).
In both TULIP-1 and TULIP-2, fewer patients had Cushingoid features at week 52 compared with baseline across all treatment groups. In TULIP-1, most notable decreases from baseline observed with anifrolumab versus placebo were for features of moon face (from 17.8% to 9.4% vs 18.5% to 14.1%), easy bruising (21.1% to 15.0% vs 19.0% to 13.6%) and acne (7.2% to 1.1% vs 4.9% to 1.6%). In TULIP-2, the most notable decreases from baseline observed with anifrolumab versus placebo were for features of moon face (13.9% to 7.2% vs 17.6% to 9.3%) and hirsutism (5.6% to 0.6% vs 2.2% to 1.1%).
Among 837 patients with SLE exposed to anifrolumab during the anifrolumab SLE clinical programme, there were 20 patients with one or more pregnancies despite the requirement to use contraception during study participation. No drug-associated congenital anomalies or drug-associated AEs were observed among these pregnancies (details provided in online supplemental appendix).
Laboratory, electrocardiogram and vital sign results
In the integrated analysis of data from TULIP-1 and TULIP-2, mean haematology and clinical chemistry values were generally similar between patients receiving anifrolumab 300 mg and placebo at baseline and at week 52 (online supplemental appendix table S5), and no clinically meaningful differences were noted between treatment groups over time.
No differences in mean blood pressure values or heart rate were noted between anifrolumab 300 mg and placebo groups, nor clinically meaningful trends in change from baseline values at 52 weeks. No clinically meaningful shifts in ECG parameters from normal to abnormal were reported.
In TULIP-1 and TULIP-2, there were no clinically important differences among treatment groups in mean changes from baseline to week 52 in body weight (TULIP-1: anifrolumab +1.43 kg, placebo +0.71 kg; TULIP-2: anifrolumab +1.54 kg, placebo +0.35 kg).
Immunogenicity
Anifrolumab administered as an intravenous infusion was associated with low levels of antidrug antibodies (ADAs) in patients with moderate to severe SLE. Among patients in whom ADAs were detected, there was no clinically relevant impact on pharmacokinetics, pharmacodynamics or safety. The percentage of patients ADA positive at any point and persistently ADA positive21 in pooled data from TULIP-1 and TULIP-2 was 7.0% and 1.2%, respectively, for anifrolumab 300 mg and 9.6% and 2.0%, respectively, for placebo (online supplemental appendix table S6). The screening and confirmatory cut-point factors used in the assay to detect ADAs were determined from 419 baseline SLE serum samples from patients enrolled in the TULIP-1 study. Drug tolerance assessments evaluated the effect of anifrolumab on the detection of ADAs. These data showed that 125 ng/mL of affinity purified polyclonal anti-anifrolumab idiotype antibody could be detected in the presence of 25 µg/mL of drug indicating that the ADA assay was sensitive and drug tolerant making false negative results unlikely. However, the selection of the low cut-points made detection of false positive results possible. The number, temporal response, titre, and all other categories of ADA assessments conducted never favoured anifrolumab (as compared with placebo) supporting the conclusion that anifrolumab is very poorly immunogenic when administered intravenously to patients with SLE.
Discussion
Morbidity in patients with SLE results from the combined deleterious effects of disease activity and treatment. Most patients with SLE require combination treatment and many of the agents currently recommended have either multiple, or non-specific, mechanisms of action, making AEs both more likely and less predictable.22 The potential introduction of a new immune-targeting drug as an add-on therapy for SLE requires comprehensive assessment of safety for its risk–benefit, and therefore its place in the therapeutic armamentarium, to be determined. Anifrolumab, which specifically targets the common receptor for all type I IFN signalling proteins, has been shown to suppress IFN gene signatures and deliver efficacy in active SLE across three phase II and III trials.18–20 Although safety data for each of these studies have been reported separately, the integrated safety analysis reported here allows for assessment of the rate and severity of both common and less common AEs.
These analyses were focused on reporting of the safety in the anifrolumab 300 mg group because this is the recommended dose for anifrolumab. The anifrolumab 150 mg dose in TULIP-1 had suboptimal efficacy and pharmacokinetics, and the 1000 mg dose in MUSE was associated with a higher rate of HZ.18 19 These analyses of pooled data indicate that anifrolumab 300 mg was generally well tolerated by patients with SLE. The most commonly reported AEs were mild to moderate in severity and included nasopharyngitis, upper respiratory tract infection, urinary tract infection, bronchitis and infusion-related reactions. AEs leading to discontinuation of investigational product were infrequent and were balanced between the groups. During the three 52-week studies, there were three deaths among patients treated with anifrolumab (two with 300 mg and one with anifrolumab 1000 mg) and one death in a patient receiving placebo. There was a lower reported rate of SAEs in patients receiving anifrolumab versus placebo. Lupus affects multiple organs, and anifrolumab has demonstrated efficacy for disease activity and reduction of flares,18–20 which may explain the lower rate of SAEs in the anifrolumab group of these trials. Among SAEs, infections including pneumonia were most common and were similar between anifrolumab (4.8%) and placebo (5.6%) groups. The rate of worsening of SLE as an SAE was greater in patients receiving placebo (3.0% vs 1.5% with anifrolumab), concordant with the numerically lower flare rates observed with anifrolumab 300 mg versus placebo in all three studies.18–20
Compared with patients receiving placebo, more patients in the anifrolumab 300 mg group experienced an AE in the System Organ Class of infections and infestations (69.7% vs 55.4%). The percentages of infections in treatment and placebo groups in patients with SLE were each comparable with those reported in clinical trials of the monoclonal antibodies to B cell activating factor tabalumab and belimumab and for epratuzumab, a monoclonal antibody to CD22.23–25 Most infections in both anifrolumab and placebo groups were mild or moderate in intensity, were not classified as SAEs and did not result in discontinuation of investigational product. The difference in rates was driven by differences in the incidence rates of mild and moderate respiratory tract infections (excluding pneumonia) and by HZ. Overall, the rate of serious infections was low with anifrolumab and similar to that in the placebo group.
There was an increased risk of HZ with anifrolumab versus placebo (6.1% and 1.3%, respectively; EAIR risk difference 5.4). However, HZ event characteristics, including duration and severity, were similar between treatment groups. Most HZ events were mild or moderate, cutaneous and resolved with antiviral treatment and without treatment discontinuation. One patient had an SAE of transverse myelitis during the MUSE study.18 The patient had a positive PCR test for HZ in spinal fluid, there were no cutaneous manifestations of HZ, and they responded following treatment with both antivirals and glucocorticoids. We cannot determine whether the underlying cause was HZ or a manifestation of SLE. This transverse myelitis case was not considered by investigators to be related to treatment, and the patient made a full recovery with no observed long-term disability. This analysis did not reveal any patient or treatment characteristics predictive of HZ reactivation, although these were numerically more common in patients receiving immunosuppressants as part of SOC therapy. As patients with SLE are known to have an increased baseline risk of HZ reactivation, it may be valuable to evaluate strategies to vaccinate this patient population prior to receipt of immunosuppressive therapies in both the clinic and clinical trial setting.26 This strategy is supported by recently updated EULAR guidelines on vaccination in autoimmune inflammatory rheumatic diseases, which recommend considering HZ vaccination in patients considered high risk.27
Infusion-related reactions were uncommon, although the rate of AEs reported as hypersensitivity and infusion-related reactions was greater with anifrolumab-treated patients (2.6% and 9.4%, respectively) than placebo (0.6% and 7.1%, respectively); most occurred early and were mild or moderate in intensity. Hypersensitivity SAE was observed in one patient receiving anifrolumab 300 mg, and one patient receiving anifrolumab 150 mg had an anaphylactic reaction. The rates of hypersensitivity/infusion-related reactions are comparable with those reported in patients with SLE in 52-week phase III trials of tabalumab and belimumab.24 25
Exposure to anifrolumab, a fully humanised monoclonal antibody, administered as an intavenous infusion to patients with SLE was minimally immunogenic. Among patients in whom ADAs were detected, there was no clinically relevant impact on pharmacokinetics, pharmacodynamics or safety. The subgroups of patients positive for ADA were small; thus, these results should be interpreted with caution. The selection of low assay cut-points also made detection of false positive results possible. The number, temporal response, titre and all other categories of ADA assessments conducted never favoured anifrolumab (as compared with placebo) supporting the conclusion that anifrolumab is very poorly immunogenic when administered intravenously to patients with SLE.
In patients treated with anifrolumab, flares of SLE as AEs were less common, despite protocol-determined glucocorticoid tapering in all three studies. The harmful effects of glucocorticoids, both in general and in the setting of SLE, are well known and include increased risk of irreversible organ damage and susceptibility to infection.28 29 Furthermore, fewer patients had Cushingoid features at week 52 compared with baseline across all treatment groups, with notable decreases with anifrolumab versus placebo. Therefore, the sustained glucocorticoid reduction achieved with anifrolumab represents a potential safety benefit.
The safety profile in these trials of anifrolumab is broadly comparable with that reported in phase III programmes of other treatments for patients with SLE.23–25 The patient populations selected in the MUSE, TULIP-1 and TULIP-2 trials were intended to reflect the real-world population of patients with moderate to severe SLE despite SOC therapy; however, certain exclusion criteria were necessary to minimise confounding in safety evaluations. Therefore, the future reporting of real-world safety experience with anifrolumab treatment in patients with SLE will be important.
These analyses have several limitations, including a duration of only 1 year. However, 218 patients who completed MUSE were enrolled in a long-term extension study, 139 of who completed 3 years of treatment. This long-term observational study reported that the rate and patterns of SAEs and AEs of special interest over the 3 years were consistent with those reported for 1 year of treatment in the primary MUSE study.30 A further placebo-controlled long-term observational extension study of patients enrolled in the TULIP-1 and TULIP-2 trials is ongoing and will provide additional long-term safety data. Another limitation was that patients with severe renal lupus and neuropsychiatric disorders were excluded from the TULIP-1, TULIP-2 and MUSE trials, and therefore, the efficacy and safety of anifrolumab in these patient subgroups still needs to be studied. A phase II study of anifrolumab in patients with lupus nephritis is ongoing.
The decision to use any medication requires a patient-focused shared decision-making process balancing benefit and risk. The current analysis shows that anifrolumab 300 mg intravenous monthly had an acceptable safety profile during 52 weeks of treatment in adult patients who had moderate to severe SLE despite SOC therapy. Taken together with the previously reported efficacy based on global disease activity improvement, glucocorticoid dosage tapering and SLE flare reduction,18–20 anifrolumab has a positive benefit–risk profile and is a potential new treatment option for a disease with few therapeutic options.
Acknowledgments
The authors would like to thank Claire Morgan, MD, Lisa Beth Ferstenberg, MD, Lijin Zhang, PhD, Ihor Hupka, MD, Pranita Kabadi, PhD and Marta Pujol, PhD for their assistance in these analyses. The authors would also like to thank the patients, study sites and investigators who participated in these clinical trials and also appreciate all members of the global academic steering committee and local steering committees. Writing and editing assistance was provided by Angela Cimmino, PharmD, and Luke Burke, PhD, of JK Associates Inc, a Fishawack Health Company. This support was funded by AstraZeneca.
Footnotes
Contributors: All authors contributed to the development of the manuscript, including interpretation of results, substantive review of drafts, and approval of the final draft for submission. GA led the statistical analyses.
Funding: This study was supported by AstraZeneca (Gaithersburg, Maryland, USA).
Competing interests: RT, GA, LP, MAM and RNK are employees of AstraZeneca. RAF has received grant/research support and consulting fees from AstraZeneca. EM has received grant support from, was a consultant for and was a speaker at a speaker bureau for AstraZeneca; received grant support and consulting fees from AbbVie, BMS, Eli Lilly, GSK, Janssen, Merck Serono and UCB; received grant support from BMS; and received consulting fees from Amgen, Biogen, CSL Inc, Neovacs and Wolf Biotherapeutics.
Patient consent for publication: Not required.
Ethics approval: The MUSE, TULIP-1 and TULIP-2 trials were conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonisation Guidelines for Good Clinical Practice, and all patients provided written informed consent in accordance with local requirements.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data underlying the findings described in this manuscript may be obtained in accordance with AstraZeneca’s data sharing policy described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.Bruce IN, O'Keeffe AG, Farewell V, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus: results from the systemic lupus international collaborating clinics (SLICC) inception cohort. Ann Rheum Dis 2015;74:1706–13. 10.1136/annrheumdis-2013-205171 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Jorge AM, Lu N, Zhang Y, et al. Unchanging premature mortality trends in systemic lupus erythematosus: a general population-based study (1999-2014). Rheumatology 2018;57:337–44. 10.1093/rheumatology/kex412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Arkema EV, Svenungsson E, Von Euler M, et al. Stroke in systemic lupus erythematosus: a Swedish population-based cohort study. Ann Rheum Dis 2017;76:1544–9. 10.1136/annrheumdis-2016-210973 [DOI] [PubMed] [Google Scholar]
- 4.Choi MY, Flood K, Bernatsky S, et al. A review on SLE and malignancy. Best Pract Res Clin Rheumatol 2017;31:373–96. 10.1016/j.berh.2017.09.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hermansen M-L, Lindhardsen J, Torp-Pedersen C, et al. The risk of cardiovascular morbidity and cardiovascular mortality in systemic lupus erythematosus and lupus nephritis: a Danish nationwide population-based cohort study. Rheumatology 2017;56:kew475–15. 10.1093/rheumatology/kew475 [DOI] [PubMed] [Google Scholar]
- 6.Zhang L, Fu T, Yin R, et al. Prevalence of depression and anxiety in systemic lupus erythematosus: a systematic review and meta-analysis. BMC Psychiatry 2017;17:70. 10.1186/s12888-017-1234-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tektonidou MG, Wang Z, Dasgupta A, et al. Burden of serious infections in adults with systemic lupus erythematosus: a national population-based study, 1996-2011. Arthritis Care Res 2015;67:1078–85. 10.1002/acr.22575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gergianaki I, Bertsias G. Systemic lupus erythematosus in primary care: an update and practical messages for the general practitioner. Front Med 2018;5:161. 10.3389/fmed.2018.00161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.González LA, Alarcón GS. The evolving concept of SLE comorbidities. Expert Rev Clin Immunol 2017;13:753–68. 10.1080/1744666X.2017.1327353 [DOI] [PubMed] [Google Scholar]
- 10.Pego-Reigosa JM, Nicholson L, Pooley N, et al. The risk of infections in adult patients with systemic lupus erythematosus: systematic review and meta-analysis. Rheumatology 2021;60:60–72. 10.1093/rheumatology/keaa478 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yazdany J, Pooley N, Langham J, et al. Systemic lupus erythematosus; stroke and myocardial infarction risk: a systematic review and meta-analysis. RMD Open 2020;6:e001247. 10.1136/rmdopen-2020-001247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Al Sawah S, Zhang X, Zhu B, et al. Effect of corticosteroid use by dose on the risk of developing organ damage over time in systemic lupus erythematosus-the Hopkins lupus cohort. Lupus Sci Med 2015;2:e000066. 10.1136/lupus-2014-000066 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Oglesby A, Shaul AJ, Pokora T, et al. Adverse event burden, resource use, and costs associated with immunosuppressant medications for the treatment of systemic lupus erythematosus: a systematic literature review. Int J Rheumatol 2013;2013:1–9. 10.1155/2013/347520 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Popa R, Lautaru LA, Lucretiu R, et al. Therapy side effects in systemic lupus erythematosus. Curr Health Sci J 2018;44:316–21. 10.12865/CHSJ.44.03.18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Peng L, Oganesyan V, Wu H, et al. Molecular basis for antagonistic activity of anifrolumab, an anti-interferon-α receptor 1 antibody. MAbs 2015;7:428–39. 10.1080/19420862.2015.1007810 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Crow MK, Ronnblom L. Type I interferons in host defence and inflammatory diseases. Lupus Sci Med 2019;6:e000336. 10.1136/lupus-2019-000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Akarsu A, Soyer O, Sekerel BE. Hypersensitivity reactions to biologicals: from bench to bedside. Curr Treat Options Allergy 2020;7:71–83. 10.1007/s40521-020-00242-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Furie R, Khamashta M, Merrill JT, et al. Anifrolumab, an Anti-Interferon-α receptor monoclonal antibody, in moderate-to-severe systemic lupus erythematosus. Arthritis Rheumatol 2017;69:376–86. 10.1002/art.39962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Furie RA, Morand EF, Bruce IN, et al. Type I interferon inhibitor anifrolumab in active systemic lupus erythematosus (TULIP-1): a randomised, controlled, phase 3 trial. Lancet Rheumatol 2019;1:e208–19. 10.1016/S2665-9913(19)30076-1 [DOI] [PubMed] [Google Scholar]
- 20.Morand EF, Furie R, Tanaka Y, et al. Trial of anifrolumab in active systemic lupus erythematosus. N Engl J Med 2020;382:211–21. 10.1056/NEJMoa1912196 [DOI] [PubMed] [Google Scholar]
- 21.Shankar G, Arkin S, Cocea L, et al. Assessment and reporting of the clinical immunogenicity of therapeutic proteins and peptides-harmonized terminology and tactical recommendations. Aaps J 2014;16:658–73. 10.1208/s12248-014-9599-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fanouriakis A, Kostopoulou M, Alunno A, et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann Rheum Dis 2019;78:736–45. 10.1136/annrheumdis-2019-215089 [DOI] [PubMed] [Google Scholar]
- 23.Clowse MEB, Wallace DJ, Furie RA, et al. Efficacy and safety of epratuzumab in moderately to severely active systemic lupus erythematosus: results from two phase III randomized, double-blind, placebo-controlled trials. Arthritis Rheumatol 2017;69:362–75. 10.1002/art.39856 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merrill JT, van Vollenhoven RF, Buyon JP, et al. Efficacy and safety of subcutaneous tabalumab, a monoclonal antibody to B-cell activating factor, in patients with systemic lupus erythematosus: results from ILLUMINATE-2, a 52-week, phase III, multicentre, randomised, double-blind, placebo-controlled study. Ann Rheum Dis 2016;75:332–40. 10.1136/annrheumdis-2015-207654 [DOI] [PubMed] [Google Scholar]
- 25.Wallace DJ, Navarra S, Petri MA, et al. Safety profile of belimumab: pooled data from placebo-controlled phase 2 and 3 studies in patients with systemic lupus erythematosus. Lupus 2013;22:144–54. 10.1177/0961203312469259 [DOI] [PubMed] [Google Scholar]
- 26.Mok CC Herpes zoster vaccination in systemic lupus erythematosus: the current status. Hum Vaccin Immunother 2019;15:45–8. 10.1080/21645515.2018.1514228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Furer V, Rondaan C, Heijstek MW, et al. 2019 update of EULAR recommendations for vaccination in adult patients with autoimmune inflammatory rheumatic diseases. Ann Rheum Dis 2020;79:39–52. 10.1136/annrheumdis-2019-215882 [DOI] [PubMed] [Google Scholar]
- 28.Apostolopoulos D, Morand EF. It hasn't gone away: the problem of glucocorticoid use in lupus remains. Rheumatology 2017;56:i114–22. 10.1093/rheumatology/kew406 [DOI] [PubMed] [Google Scholar]
- 29.Apostolopoulos D, Kandane-Rathnayake R, Louthrenoo W, et al. Factors associated with damage accrual in patients with systemic lupus erythematosus with no clinical or serological disease activity: a multicentre cohort study. Lancet Rheumatol 2020;2:e24–30. 10.1016/S2665-9913(19)30105-5 [DOI] [PubMed] [Google Scholar]
- 30.Chatham WW, Furie R, Saxena A, et al. Long‐term safety and efficacy of anifrolumab in adults with systemic lupus erythematosus: results of a phase 2 open‐label extension study. Arthritis Rheumatol 2020. 10.1002/art.41598 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
lupus-2020-000464supp001.pdf (265.9KB, pdf)