Abstract
Background
It is important to understand whether the potential impact of pyrethroid resistance on malaria control can be mitigated by switching between different pyrethroids or whether cross-resistance within this insecticide class precludes this approach.
Methods
Here we assess the relationships among pyrethroids in terms of their binding affinity to, and depletion by, key cytochrome P450 enzymes (hereafter P450s) that are known to confer metabolic pyrethroid resistance in Anopheles gambiae (s.l.) and An. funestus, in order to identify which pyrethroids may diverge from the others in their vulnerability to resistance. We then investigate whether these same pyrethroids also diverge from the others in terms of resistance in vector populations.
Results
We found that the type I and II pyrethroids permethrin and deltamethrin, respectively, are closely related in terms of binding affinity to key P450s, depletion by P450s and resistance within vector populations. Bifenthrin, which lacks the common structural moiety of most pyrethroids, diverged from the other pyrethroids tested in terms of both binding affinity to key P450s and depletion by P450s, but resistance to bifenthrin has rarely been tested in vector populations and was not analysed here. Etofenprox, which also lacks the common structural moiety of most pyrethroids, diverged from the more commonly deployed pyrethroids in terms of binding affinity to key P450s and resistance in vector populations, but did not diverge from these pyrethroids in terms of depletion by the P450s. The analysis of depletion by the P450s indicated that etofenprox may be more vulnerable to metabolic resistance mechanisms in vector populations. In addition, greater resistance to etofenprox was found across Aedes aegypti populations, but greater resistance to this compound was not found in any of the malaria vector species analysed. The results for pyrethroid depletion by anopheline P450s in the laboratory were largely not repeated in the findings for resistance in malaria vector populations.
Conclusion
Importantly, the prevalence of resistance to the pyrethroids α-cypermethrin, cyfluthrin, deltamethrin, λ-cyhalothrin and permethrin was correlated across malaria vector populations, and switching between these compounds as a tool to mitigate against pyrethroid resistance is not advised without strong evidence supporting a true difference in resistance.
Introduction
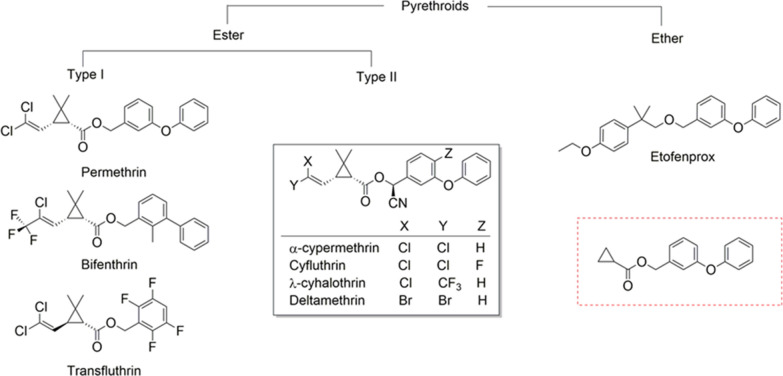
The primary malaria control intervention in high-burden countries is the deployment of long-lasting insecticide-treated nets (LLINs) impregnated with pyrethroids, alone or in combination with a second active ingredient or synergist [1, 2]. Widespread and increasing resistance to pyrethroids is, therefore, a serious potential threat to malaria control [3, 4]. Because the options for LLINs are limited, it is essential to understand whether the impact of resistance can be mitigated by switching between different pyrethroids or whether cross-resistance within this insecticide class precludes this approach. ‘Cross-resistance’ often refers to the instance where resistance is conferred to two or more classes of insecticide, is commonly assumed within an insecticide class. Evidence for divergence in resistance within an insecticide class may, however, be relevant especially given the reliance on a single insecticide class, the pyrethroids. Pyrethroids listed by the World Health Organization (WHO) for malaria control are differentiated into two groups based on biological activity that is associated with the absence (type I) or presence (type II) of an alpha-cyano group (Fig. 1). Type II pyrethroids are more lethal to insects because of their higher potency to the voltage-gated sodium channel (VGSC) in nerve membranes, the primary target site of pyrethroids [5, 6]. The higher potency of type II pyrethroids, such as deltamethrin and α-cypermethrin, translates into much lower doses being required to treat vector control products compared with type I pyrethroids, such as permethrin. This has led to increased deployment of alpha-cyano pyrethroids, in particular α-cypermethrin, which is currently used in 28% of the prequalified vector control products [2]. Generally, the pyrethroids used in vector control possess the common structural motif of phenoxybenzyl alcohol coupled with a cyclopropane ring via an ester bond, except for bifenthrin and etofenprox (Fig. 1). This narrow spectrum of chemical variation among pyrethroids makes it likely that cross-resistance will occur in malaria vector populations.
Fig. 1.
Chemical structure of pyrethroid insecticides used for malaria vector control. The common scaffold of pyrethroids, boxed in red, was identified by searching 230 million compounds available in the ZINC database (https://zinc.docking.org)
The high-burden countries where LLINs are deployed are concentrated in Africa where the most important vectors are Anopheles gambiae (s.l.) and Anopheles funestus [7]. Pyrethroid resistance in malaria vectors is primarily associated with target-site insensitivity due to mutations in the Vgsc gene known as knockdown resistance (kdr) and increased detoxification activity known as metabolic resistance. Metabolic mechanisms of resistance are found in all African malaria vectors, whereas kdr mutations are common in species of the Anopheles gambiae complex but not in the An. funestus subgroup [8–14]. There are multiple amino acid substitutions that cause target-site insensitivity resulting in pyrethroid resistance [15]. This includes a mutation, M918T, that produces a super-knockdown (s-kdr) phenotype in houseflies. Structure modelling studies in M918T phenotypes indicate that the highest degree of resistance in s-kdr houseflies depends on the chemical structure of the insecticide, which is positively correlated with the presence of an α-cyano group coupled with a phenoxybenzyl moiety in the larger type II pyrethroid molecules, such as deltamethrin and fenvalerate [16]. By comparison, the most common Vgsc resistance allele in west African An. gambiae populations, L1014F, is not influenced by pyrethroid chemical structure when expressed alone in house flies [17].
Although kdr mutations are common in An. gambiae (s.l.), they may have a relatively modest impact on resistance, and they are absent from highly pyrethroid-resistant An. funestus populations, suggesting that metabolic mechanisms may have a greater impact in African malaria vectors [18–20]. Metabolic resistance is most commonly mediated by elevated levels of cytochrome P450 (CYP) enzymes (hereafter referred to as P450s) [21]. Transcriptome-wide studies of gene expression in resistant and susceptible mosquito strains have found that upregulation of several cytochrome P450 genes is associated with resistance to both a type I pyrethroid (permethrin) and a type II pyrethroid (deltamethrin). For example, upregulation of the CYP6P3 gene and its orthologues CYP6P9a and CYP6P9b and of the CYP6AA1, CYP6Z1 and CYP6Z3 genes is associated with resistance to both of these pyrethroids in An. gambiae/An. coluzzii and An. funestus [22–32]. In addition, upregulation of the CYP6Z2 gene in An. gambiae and An. coluzzii, and of the CYP6M7 gene in An. funestus, is also associated with resistance to both pyrethroids [23–25, 27, 28, 30–32]. These findings from studies of gene expression in resistant and susceptible strains provide evidence for P450-mediated pyrethroid cross-resistance in Anopheles populations, particularly to deltamethrin and permethrin; however, associations among resistance to more than one pyrethroid have not always been found, a limited range of pyrethroids has been tested and these studies do not give an indication of whether cross-resistance is stronger between some pyrethroids than others. Like the Anopheles vectors, target-site mutations and metabolic resistance are also thought to be the main resistance mechanisms in Aedes mosquitoes [33, 34].
An assessment of the impact of individual structural variation within the pyrethroid class on resistance in the field is required to inform the best use of different compounds. A previous study assessed resistance in malaria vector populations at more than 1000 sites in Africa and showed that when spatio-temporal trends were separated from noise in the susceptibility test data, strong associations among the resistance trends for three structurally similar pyrethroids (deltamethrin, ʎ-cyhalothrin and permethrin) were found [35]. The variance in the mean percent mortality values was 28 for the west Africa model and 23 for the east Africa model, reflecting the noisiness of the mortality data. This study also noted that the prevalence of resistance to permethrin was typically higher than that to deltamethrin; however, caution is needed when interpreting differences found using susceptibility test data because they may be due to real differences in the prevalence of resistance or differences in the calibration of the diagnostic dose, or both. Diagnostic doses currently recommended for use were calculated by doubling the dose of a compound which kills 100% of a susceptible strain of a species, or doubling the LC99 (lethal concentration that incurs 99% mortality) in this strain [36, 37]. A robust recommendation should be based on data from multiple strains in different testing centres, but where this is not possible doses may not be well calibrated between compounds. It is clear that differences in resistance between individual pyrethroids cannot be generally assumed, but it remains unclear whether meaningful differences can occur, particularly when a wider range of pyrethroid chemistries is considered.
In the study reported here, we took a new approach to assess variation in resistance among pyrethroids. We first assessed differences in pyrethroid chemistry that influence inhibition of the key enzymes that confer metabolic resistance in African malaria vectors, and the rate of depletion of each pyrethroid by these enzymes [38]. Of the primary resistance genes, the P450 superfamily is most frequently associated with metabolic resistance to pyrethroids in malaria vectors. Therefore, we assessed the relative differences among six pyrethroids in terms of their molecular interactions with P450s from the major African malaria vectors by constructing a P450s structure–activity relationship model (P450s-SAR). We focussed on α-cypermethrin, deltamethrin and permethrin as most relevant for recommendations regarding the current LLIN options. However, for broader future consideration, we included bifenthrin, etofenprox, cyfluthrin and λ-cyhalothrin, all structurally varied pyrethroids that are also in the WHO’s prequalified list for malaria vector control (Fig. 1) [2]. We then analysed resistance to these pyrethroids in multiple vector populations to determine whether the relative differences found by P450s-SAR studies translated into relative differences in resistance within wild populations. This was supplemented by an analysis of resistance in arbovirus vector populations. Finally, the resistance associations found across insecticide classes were also analysed in order to put the relationships found within the pyrethroids into the wider context of cross-resistance generally and to further investigate whether cross-resistance predicted by laboratory studies can be detected as general trends in the field data.
Material and methods
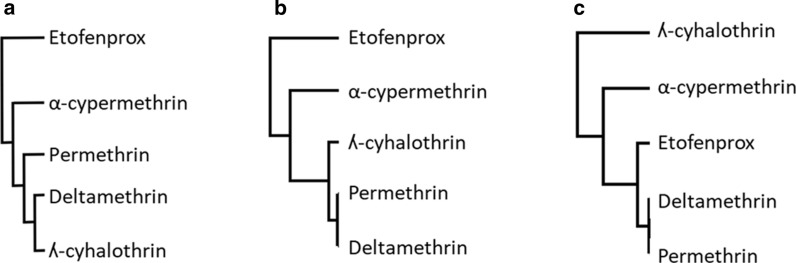
In order to test whether relationships identified by SAR studies can be detected in the field, we constructed dendrograms for the hierarchical relationships between pyrethroids found by a series of molecular and field studies, and then compared the dendrograms obtained.
Relationships among pyrethroids in terms of functional activity data
Cytochrome P450 inhibition assays using fluorogenic probe substrates have become commonplace in drug discovery screening cascades and are a rapid method of screening for insecticide interactions with mosquito P450s to predict insecticide binding, metabolism, cross-resistance and synergism [38–41]. In this study, the half maximal inhibitory concentration (IC50), which provides a value for inhibition of each P450 by each pyrethroid (also referred to as ‘binding affinity’), and the percentage depletion, which gives a value for metabolism of each pyrethroid by each P450 (also referred to as vulnerability to metabolic attack), were both included as parameters to establish a P450s structural activity relationship model. This model was used to understand both the chemistry of the pyrethroids and the interaction with mosquito P450s that function as monooxygenases in metabolic resistance, to predict cross-resistance liabilities in vivo. A low IC50 value indicates that the pyrethroid being assessed is a potent inhibitor that may be able to counter resistance mediated by P450s. A low percentage depletion indicates low metabolism of the pyrethroid, which means that it may be less vulnerable to resistance mediated by P450s.
The IC50 values for permethrin, etofenprox and bifenthrin (type I) and deltamethrin, λ-cyhalothrin and α-cypermethrin (type II) pyrethroids that were exposed to recombinant P450s from the An. gambiae Kisumu strain (CYP6Z2, =6M2, -6P2, -6P3 and -9J5) and the An. funestus FUMOZ strain (CYP6P9a) were extracted from two studies [38, 41]. In addition, inhibition activity data for these pyrethroids exposed to CYP6Z3 from the An. gambiae Kisumu strain were also generated (Additional file 1).
The values for percentage depletion (metabolism) of each pyrethroid by three of the enzymes CYP6M2, CYP6P3 and CYP6P9a, which were expressed in a single plasmid construct, were also extracted from the same sources and used for the comparative analysis.
The two datasets were analysed using hierarchical clustering of rows (insecticide) and columns (P450) by Perseus v1.6.14.0 to produce two visual heat maps representing the clustered matrices for relative insecticide binding affinity and insecticide vulnerability to metabolic attack. The clustered matrices for functional activity data for these six pyrethroids against these seven P450s were then used to construct dendrograms for the hierarchical relationships among the pyrethroids.
Relationships among pyrethroids in terms of susceptibility test mortality in malaria vector populations
We accessed a published database of insecticide resistance in African malaria vectors [14] and identified all instances in which a mosquito sample from the field had been tested using two or more pyrethroids. Pairs of results were extracted, rather than instances in which a sample had been divided between tests of three or more pyrethroids, because there were insufficient data from studies testing > 2 pyrethroids against a single mosquito collection. Each data point provided paired susceptibility test data from a single collection sampled at a given time and place that was subdivided and subsequently tested under identical experimental conditions, with the aim of addressing the question ‘for a given time, place, species/complex and method, does higher resistance to pyrethroid A indicate higher resistance to pyrethroid B?’. A total of 3153 pairs of WHO susceptibility test results from samples of the An. gambiae complex were obtained. Only data that detected resistance to at least one pyrethroid were included; that is, results from samples that demonstrated 100% mortality to all of the pyrethroids tested were excluded.
We conducted a series of correlation analyses to assess how closely associated each pair of pyrethroids is in terms of resistance. The mean value for the Pearson’s correlation coefficient was calculated across 1000 bootstrapped samples for each pyrethroid pair using SPSS Statistics v25 (IBM Corp., Armonk, NY, USA). A Holm-Bonferroni correction was applied to identify significant correlations among the multiple tests conducted while avoiding false positives [42]. The mean correlation coefficients generated were ranked to identify the most and least closely correlated pyrethroids, respectively. These bootstrap mean correlation coefficients were used to construct a dendrogram of the hierarchical relationships among pyrethroids using the unweighted pair-group method with arithmetic mean [43], where the highest correlation coefficient indicated the most closely related pair.
The analyses conducted using data from An. gambiae (s.l.) samples were repeated using data from the An. funestus subgroup, An. arabiensis, An. coluzzii, An. funestus and An. gambiae samples (Additional file 2). The same approach was also used for susceptibility test data from Aedes albopictus and Ae. aegypti to investigate whether the same relationships could be detected in these vectors of arboviruses, as detailed in Additional file 3. There were much lower data volumes for the individual Anopheles species, compared to An. gambiae (s.l.), and a limited selection of pyrethroid pairs could be tested so no dendrograms were constructed from these data. Finally, the correlations between resistance to deltamethrin and resistance to insecticides from other classes were calculated in order to put the relationships found within the pyrethroids into the broader context of cross-resistance.
Results
Relationships among pyrethroids in terms of functional activity data
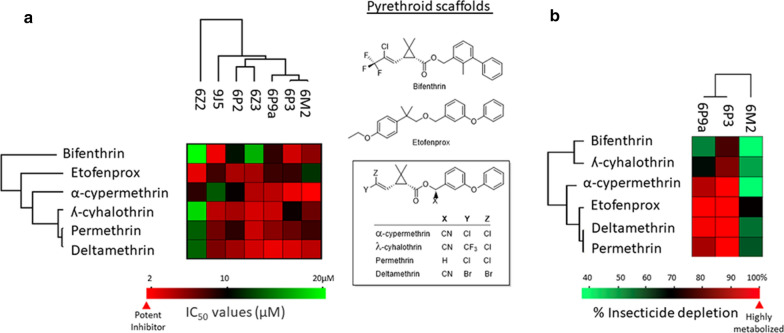
The six pyrethroids were categorised according to their inhibition of diethoxyfluorescein metabolism by P450s as potent (IC50 < 1 μM), moderate (IC50 1–10 μM) and weak inhibitors (IC50 > 10 μM) [44]. Accordingly, all pyrethroids investigated showed low to moderate binding to the P450 panel (Fig. 2a; Additional file 1: Table S2). Bifenthrin had the lowest binding to the P450s panel examined (Fig. 2a; Additional file 1: Table S2).
Fig. 2.
Cluster analysis of functional activity data for six pyrethroids against cytochrome P450 (CYP) enyzmes (P450s) from African malaria vectors. a Inhibition data from the screening of six pyrethroids (scaffold structures indicated on the right of data panels) against a set of P450s are presented as a heat map. Target enzymes are arrayed along the x-axis, and each of the pyrethroids is arrayed along the y-axis. Colours indicate the inhibition potency of pyrethroids with an indicated variable scaffold for a designated target P450. Potent (hot) inhibitors are assigned a red colour, and weak or ineffective (cold) inhibitors are given a light-green colour. b Pyrethroid metabolism by the P450s most widely associated with resistance from Anopheles gambiae (CYP6M2 and CYP6P3) and An. funestus (CYP6P9a) is clustered and presented as a heat map. Pyrethroids susceptible to metabolism are assigned a red colour, and weak metabolism is denoted light green. Dendrograms were obtained by hierarchical clustering and indicate the degree of similarity as a function of the height of the lines connecting the profiles
CYP6P3, -6M2 and -6P9a were selected for comparative metabolism analysis because they are commonly associated with pyrethroid resistance, are among the earliest pyrethroid resistance markers to be functionally validated and are most heavily used for in vitro screening [29, 41, 45, 46]. All of the pyrethroids, with the exception of bifenthrin, were strongly metabolised by CYP6P3 and its orthologue CYP6P9a expressed from An. gambiae and An. funestus, respectively (Fig. 2b; Additional file 1: Table S3). However, lower metabolism profiles were observed with CYP6M2 expressed from An. gambiae (Fig. 2b; Additional file 1: Table S3). Notably, etofenprox was strongly metabolised by CYP6P3, CYP6M2 and CYP6P9a. Overall, the metabolism data presented in Fig. 2b and Additional file 1: Table S3 ranked etofenprox, deltamethrin and permethrin as the most vulnerable insecticides for metabolic attack by the three enzymes, followed by α-cypermethrin and ʎ-cyhalothrin; bifenthrin demonstrated the lowest vulnerability.
The dendrograms indicate that, in terms of inhibition of P450s and metabolism by P450s, permethrin and deltamethrin are closely related whereas bifenthrin diverges from these pyrethroids, (Fig. 2).
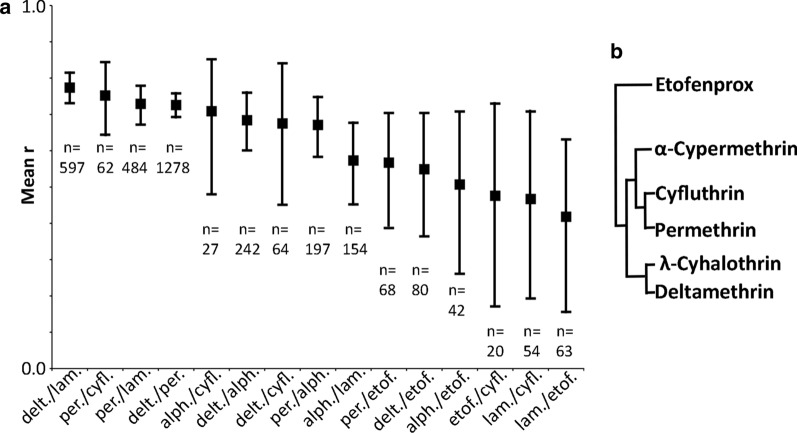
Relationships among pyrethroids in terms of susceptibility test mortality in malaria vector populations
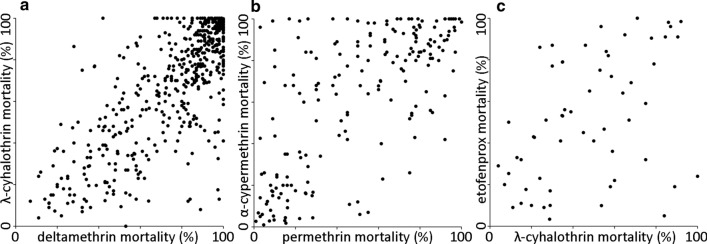
Each of the 15 pairs of values for pyrethroid resistance within An. gambiae (s.l.) was significantly correlated (Table 1). That is, populations with a higher prevalence of resistance to one pyrethroid tended to have a higher prevalence of resistance to the others (Fig. 3; Additional file 2: Figure S2). The pyrethroid pairs were ranked from the most closely correlated pair, deltamethrin versus λ-cyhalothrin, to the most divergent pair, etofenprox versus λ-cyhalothrin (Table 1; Fig. 4a). The correlation coefficients were used to construct a dendrogram of the hierarchical relationships among these pyrethroids (Fig. 4b). Deltamethrin, λ-cyhalothrin, permethrin, cyfluthrin and α-cypermethrin were closely related whereas etofenprox diverged from the other five pyrethroids.
Table 1.
Correlations in resistance to seven pyrethroids in the Anopheles gambiae complex
| Rank | Pyrethroid paira | Paired sample size (N) | Mean r |
|---|---|---|---|
| 1 | Deltamethrin vs λ-cyhalothrin | 597 | 0.774* |
| 2 | Permethrin vs cyfluthrin | 62 | 0.752* |
| 3 | Permethrin vs λ-cyhalothrin | 484 | 0.729* |
| 4 | Deltamethrinvs permethrin | 1278 | 0.726* |
| 5 | α-Cypermethrin vs cyfluthrin | 27 | 0.709* |
| 6 | Deltamethrin vs α-cypermethrin | 242 | 0.684* |
| 7 | Deltamethrin vs cyfluthrin | 64 | 0.675* |
| 8 | Permethrin vs α-cypermethrin | 197 | 0.671* |
| 9 | λ-Cyhalothrin vs α-cypermethrin | 154 | 0.573* |
| 10 | Permethrin vs etofenprox | 68 | 0.567* |
| 11 | Deltamethrin vs etofenprox | 80 | 0.549* |
| 12 | α-Cypermethrin vs etofenprox | 42 | 0.507* |
| 13 | Etofenprox vs cyfluthrin | 20 | 0.476* |
| 14 | λ-Cyhalothrin vs cyfluthrin | 54 | 0.467* |
| 15 | λ-Cyhalothrin vs etofenprox | 63 | 0.418* |
r, Pearson’s correlation coefficient
*Significant results (at the 0.05 level with a Holm-Bonferroni correction)
aThe most closely correlated pair is ranked first
Fig. 3.
Distributions of values for three example pyrethroid pairs. a The most closely related pyrethroid pair in terms of resistance in wild mosquito populations (deltamethrin and λ-cyhalothrin), b a mid-ranked pyrethroid pair (permethrin and α-cypermethrin), c the least closely related pyrethroid pair (λ-cyhalothrin and etofenprox). Each point represents the results from a single An. gambiae (s.l.) sample that was subdivided between two susceptibility tests. The plots for all pairs are shown in Additional file 2: Figure S2
Fig. 4.
Relationships among pyrethroids defined by correlations in resistance within An. gambiae complex mosquitoes. a The mean correlation coefficient for each pyrethroid pair ranked from the most closely correlated to the most divergent. alph. α-Cypermethrin, cyfl. cyfluthrin, delt. deltamethrin, etof. etofenprox, lamb. λ-cyhalothrin, per. permethrin. The bars represent the upper and lower 95% bootstrap confidence interval and the sample size for each pair is given below these bars. b The hierarchical relationships among pyrethroids defined using the correlation coefficients shown in a
Comparison of pyrethroid relationships seen in the molecular and field studies
The three dendrograms using data for (i) resistance in field populations, (ii) P450 inhibition and (iii) depletion by P450s were re-constructed incorporating only the five pyrethroids that were included in all three analyses (Fig. 5). The dendrograms for P450 inhibition (also referred to as binding affinity) and vector population resistance both show that deltamethrin, λ-cyhalothrin, permethrin are most closely related to each other, followed by α-cypermethrin, with etofenprox as the most divergent (Fig. 5a, b). The dendrogram constructed using values for insecticide depletion (also referred to as vulnerability to metabolic attack) by CYP6P3, CYP6M2 and CYP6P9a reveals different relationships among these pyrethroids, although permethrin and deltamethrin are still closely related (Fig. 5c).
Fig. 5.
Hierarchical relationships among pyrethroids defined using data on resistance in vectors and functional activity data. The dendrograms were constructed using correlations in mortality across African malaria vector populations (Pearson’s correlation coefficient) (a), binding affinity values (IC50) (b) and insecticide depletion values (%) (c)
Correlations in pyrethroid resistance within malaria vector species
Across An. funestus subgroup communities, there were significant correlations between resistance to deltamethrin and λ-cyhalothrin, permethrin and λ-cyhalothrin, and deltamethrin and permethrin, and the same was true for the four species tested (Table 2; Additional file 2: Figures S3 and S4). There were insufficient data to test the other pyrethroid combinations for the African malaria vector species. Across Ae. aegypti populations, resistance to cyfluthrin, deltamethrin, λ-cyhalothrin and permethrin was significantly correlated, whereas there were no significant correlations between these four pyrethroids and etofenprox (full results are given in Additional file 3).
Table 2.
Correlations between resistance to different pyrethroids in African malaria vector species.
| Pyrethroid combination | Paired sample size (N) | r |
|---|---|---|
| Deltamethrin vs λ-cyhalothrin | ||
| Anopheles funestus subgroup | 46 | 0.818* |
| Anopheles funestus | 24 | 0.865* |
| Anopheles arabiensis | 28 | 0.946* |
| Anopheles coluzzii | 18 | 0.863* |
| Anopheles coluzzii/gambiaea | 19 | 0.603* |
| Anopheles gambiae | 19 | 0.418 n.s. |
| Permethrin vs λ-cyhalothrin | ||
| Anopheles funestus subgroup | 26 | 0.786* |
| Anopheles funestus | 16 | 0.845* |
| Anopheles arabiensis | 31 | 0.859* |
| Anopheles coluzzii | 14 | 0.740* |
| Anopheles coluzzii/gambiaea | 17 | 0.790* |
| Anopheles gambiae | 4 | Not tested |
| Deltamethrin vs permethrin | ||
| Anopheles funestus subgroup | 113 | 0.608* |
| Anopheles funestus | 69 | 0.726* |
| Anopheles arabiensis | 116 | 0.840* |
| Anopheles coluzzii | 48 | 0.793* |
| Anopheles coluzzii/gambiaea | 63 | 0.714* |
| Anopheles gambiae | 75 | 0.782* |
n.s., non-significant results (at the 0.05 level with a Holm-Bonferroni correction)
*Significant results (at the 0.05 level with a Holm-Bonferroni correction)
aAnopheles coluzzii/gambiae refers to mosquito samples that were undifferentiated between An. coluzzii (M form) and An. gambiae (S form), before they were recognised as two species
In order to put the relationships found within the pyrethroids into the wider context of cross-resistance across the insecticide classes used for malaria vector control, the correlations between deltamethrin and six commonly used non-pyrethroid insecticides were also calculated. Significant correlations with the prevalence of resistance to dichlorodiphenyltrichloroethane (DDT) were found for species within the An. gambiae complex but not for An. funestus (Additional file 2: Table S4, Figure S5). No significant correlations were found between the prevalence of resistance to deltamethrin and that to bendiocarb or propoxur (carbamates), malathion, fenitrothion or pirimiphos-methyl (organophosphates) for species within the An. gambiae complex or An. funestus.
Variation in pyrethroid resistance within populations of African malaria vector species
The results presented above show significant correlations in resistance among the pyrethroids tested, but this result does not preclude the possibility that the prevalence of resistance is generally higher in one pyrethroid compared to the others across populations with differing levels of pyrethroid resistance. The insecticide depletion data presented above indicates that some pyrethroids are potentially more vulnerable to P450 attack; this is particularly the case for etofenprox which was most depleted by the three P450s (Additional file 1: Table S3). This leads to the question of whether higher levels of resistance to this compound can be detected in wild mosquito populations. An analysis of the paired data from An. gambiae (s.l.) samples collected across Africa provides no evidence that the prevalence of resistance is consistently higher for etofenprox compared to the other pyrethroids in An. gambiae (s.l.) (Additional file 2: Figure S6), but mortality was significantly lower after Ae. aegypti populations were exposed to etofenprox compared to mortality following exposure to deltamethrin, cyfluthrin, λ-cyhalothrin and permethrin (Additional file 3: Table S7).
To put the mortality differences found among pyrethroids (Additional file 2: Figures S7–S8) into the wider context of cross-resistance, the prevalence of resistance to deltamethrin was compared to the prevalence of resistance to six non-pyrethroid insecticides in paired susceptibility tests (Additional file 2: Figure S9). A reversal in the differences between resistance to deltamethrin and to the organochlorine DDT was found, with An. gambiae (s.l.) species having significantly higher resistance to DDT whereas An. funestus had significantly higher resistance to deltamethrin. In all species tested, mortality was lower following deltamethrin exposure compared to exposure to bendiocarb and propoxur (carbamates), malathion, fenitrothion and pirimiphos-methyl (organophosphates), respectively.
Discussion
The results of this study highlight which of the pyrethroids used in malaria control are closely related in terms of inhibition of and depletion by P450s. Other studies of structurally diverse pyrethroids have also shown variation in P450 metabolism of pyrethroids with different structures. An in vivo study of the An. funestus strain, FUMOZ-R, which is characterised by upregulated P450 levels without any target-site mutations, found that transfluthrin, which contains a polyfluorobenzyl alcohol, was effective in the absence of the generic P450 inhibitor, piperonyl butoxide (PBO), whereas the other pyrethroids that contain the common phenoxybenzyl moiety, including cypermethrin, ß-cyfluthrin, deltamethrin and permethrin, were only effective when partnered with PBO [47]. This effect was associated with an inability of detoxifying enzymes to bind to the uncommon structure of transfluthrin. A similar observation was reported earlier from agriculture studies where an isogenic metabolic resistance strain isolated from a pyrethroid-resistant field population of Helicoverpa armigera showed significant cross-resistance between pyrethroids characterised by having both the phenoxybenzyl and aromatic acid moieties whereas the substitution of the phenoxybenzyl group with a polyfluorobenzyl group, as occurs in tefluthrin, benfluthrin and transfluthrin, overcame most of this resistance [48]. These studies support the aim of identifying pyrethroids that are active against resistant populations when P450-mediated resistance plays a major role. In our study, bifenthrin diverged from the other pyrethroids in terms of both inhibition of, and depletion by, P450s, but no susceptibility test data were available for resistance to bifenthrin in populations of African malaria vectors. Susceptibility test data were available for etofenprox, and this pyrethroid was found to diverge from the more commonly deployed pyrethroids in terms of inhibition of An. gambiae and An. funestus P450s and in terms of resistance in An. gambiae (s.l.) and Ae. aegypti populations.
The susceptibility test data from these populations show strong associations between resistance to the most commonly used pyrethroids (deltamethrin, λ-cyhalothrin, permethrin and α-cypermethrin), in agreement with the results for binding affinity and with earlier studies of spatio-temporal trends in An. gambiae (s.l.) [3, 35]. The correlations in resistance among these pyrethroids, which were demonstrated in all the major African malaria vectors, suggest that if differences in resistance to these pyrethroids (as well as to the less commonly deployed cyfluthrin) are found using susceptibility tests conducted on a small number of field samples of malaria vectors, further evidence should be obtained before any decision is made to switch between them.
Greater differentiation was found for resistance to bifenthrin in terms of both inhibition of, and depletion by, P450s. The results for bifenthrin are interesting because they show that (i) this pyrethroid differs from the other pyrethroids in terms of P450 binding and metabolism and that (ii) it may be less susceptible to common P450 enzymes. Bifenthrin is the active ingredient in one indoor residual spray (IRS), Bistar 10WP [2, 49], which is used in India. Bifenthrin IRS was trialled in Nigeria in 2006 and Zambia in 2011 [50–52], but it has not been widely deployed in Africa where concerns about the duration of residual activity have been raised [52–54]. There are no field data from susceptibility tests on African malaria vectors conducted using bifenthrin, presumably because this compound is rarely deployed and because there is no recommended diagnostic dose for use in a susceptibility test. One study of Anopheles sinensis in Korea collected blood-fed adults in the field and exposed subsets of the F1 larvae to each of the pyrethroids considered in our study. Resistance ratios using LC50 values were calculated from a susceptible strain, and the results revealed that the larvae were most susceptible to bifenthrin, cyfluthrin and etofenprox, in that order, and least susceptible to permethrin [55]. Further evidence comes from studies of Aedes vectors, including three studies that tested bifenthrin [34]. One study in Mexico tested seven populations of Aedes aegypti with eight pyrethroids and compared the concentrations required for 50% knockdown (KC50) and mortality (LC50) to the same values obtained using a susceptible strain to give a resistance ratio (RR) [56]. Across the seven populations, resistance to deltamethrin, lambda-cyhalothrin, permethrin and α-cypermethrin were highly correlated (in terms of both RRKC50 and RRLC50), indicating the existence of strong cross-resistance. However, the resistance values for bifenthrin were not correlated with any of those for the other four compounds, and the authors of the study concluded that bifenthrin could be an alternative insecticide for Ae. aegypti in Mexico. Two independent studies in Thailand tested three Ae. aegypti and three Ae. albopictus populations, respectively, and calculated the diagnostic doses for each pyrethroid, including bifenthrin, using a susceptible strain [57, 58]. In both studies, the population with the highest deltamethrin resistance also had the highest bifenthrin resistance, so no evidence for divergence in resistance was observed for these two species in Thailand. Given the known data noise in susceptibility test results, caution is needed when interpreting the results from a single study at a small number of sites. It is also worth noting that bifenthrin’s relative immunity to depletion by CYP6M2, CYP6P3 and CYP6P9a described here was not found when tested previously [28]. Metabolism assays carried out in two earlier studies showed that CYP6M7, CYP6P9a and CYP6P9b from An. funestus metabolised bifenthrin (62, 68 and 71%, respectively) as well as permethrin, deltamethrin and λ-cyhalothrin (ranging from 46 to 81% depletion). Field tests for bifenthrin resistance in malaria vector populations are needed before a firm conclusion can be reached on whether bifenthrin can be recommended in situations where resistance to other pyrethroids has been found.
The analyses of binding affinity data and of field data from malaria vector populations both show that resistance to etofenprox diverges, to a degree, from resistance to the more commonly deployed pyrethroids. This result is backed up by data from studies of resistance in Ae. aegypti. However, the depletion activity data suggest that etofenprox is more vulnerable to P450 metabolism and that if resistance to this compound is found to be greater in malaria vector populations, then a switch would not be advised. A trend for higher resistance to etofenprox was not seen in the data from malaria vector populations but it was found in the data from Ae. aegypti populations, although caution is needed when interpreting differences found using susceptibility test data (particularly tests using diagnostic doses that have not been calibrated for Aedes species [34]). Etofenprox is the active ingredient in two WHO prequalified products, namely a kit for insecticide-treated nets (Vectron 10EW) and an IRS formulation (Vectron20WP) [2]. The latter product is listed by the Global Fund, but etofenprox is not widely deployed in Africa and was last reported as the active ingredient used for IRS in 2012 in parts of Zambia [51, 52].
We found some variation in the relationships among pyrethroids when different types of evidence were considered. In particular, the results for insecticide depletion were largely not repeated in the findings for resistance in mosquito populations. The results for both insecticide inhibition and insecticide depletion depend on which enzymes are included in the activity tests. Seven P450s (three for the depletion analysis) were included in the present study, whereas at least 14 have been implicated in An. gambiae (s.l.) and An. funestus resistance to date [21, 22, 24–32, 46, 59–73] and many more in Aedes vectors [34]. It is also important to note that detoxification by P450s is not the only mechanism of resistance found in these vector species. Target-site mutations are common in many of these species [9–13], upregulation of other detoxifying enzymes is also linked to pyrethroid resistance [74] and there is some evidence for cuticular thickening in resistant mosquitoes [75]. Upregulation of the GSTE2 gene is associated with resistance to both permethrin and deltamethrin, as well as DDT, in An. gambiae and An. coluzzii [70, 72, 76], An. funestus [29, 71, 74] and Ae. aegypti [77–79], and allele frequencies for target-site mutations in the voltage-gated sodium channel gene, Vgsc, have been shown to be useful partial predictors of resistance in An. gambiae (s.l.) [35]. Thus, we would not expect the findings from molecular studies of P450 activity alone to be exactly replicated in field populations, except in instances where P450-mediated metabolic resistance dominates in a mosquito population.
The results for pyrethroid cross-resistance within individual species reported here match our knowledge of other mechanisms of resistance found in these species. Mutations in the Vgsc gene (kdr mutations) confer cross-resistance to pyrethroids and DDT, and are partial predictors of patterns of resistance to these compounds in the An. gambiae complex, but they have not been found in An. funestus or other members of the An. funestus subgroup [3, 8–14, 35]. In our study, correlations between pyrethroid and DDT resistance were found for members of the An. gambiae complex but not for the An. funestus subgroup or species. No correlations were found between pyrethroid resistance and resistance to the carbamates or organochlorines, underlining the finding that it is cross-resistance within the pyrethroids, as well as between the pyrethroids and DDT, that is most important. Some metabolic resistance mechanisms do confer cross-class resistance, for example between the pyrethroids and DDT and/or the carbamates [24, 30, 32, 73], but the impact of these mechanisms within the array of resistance types that co-occur is more nuanced, and no cross-class resistance other than the aforementioned pyrethroid–DDT resistance in An. gambiae (s.l.) was detected here.
In conclusion, we have shown that the type I and type II pyrethroids permethrin and deltamethrin, respectively, are closely related, as exemplified by (i) the close associations between the binding affinities of permethrin and deltamethrin to a range of anopheline P450s, (ii) the close associations between depletion of permethrin and deltamethrin by these P450s and (iii) correlations in resistance to permethrin and deltamethrin in populations of An. arabiensis, An. coluzzii, An. gambiae and An. funestus. Importantly, a population with higher resistance to one of the pyrethroids incorporating the common structural motif of phenoxybenzyl alcohol coupled with a cyclopropane ring (the primary target for metabolic oxidation) is likely to have higher resistance to the others, and these cross-resistance trends could be detected despite the noise in the susceptibility test data. It is unlikely that resistance to those pyrethroids most commonly deployed for malaria control diverges within vector populations, and it would be unwise to switch between these compounds based on the results from a small number of susceptibility tests alone. There are, however, pyrethroids that are not commonly deployed that show greater potential for true divergence in resistance, such as bifenthrin and possibly etofenprox. Bifenthrin diverged from the other pyrethroids tested in terms of both binding affinity to key P450s and depletion by P450s, but resistance to bifenthrin has rarely been tested in vector populations and was not analysed here. Etofenprox diverged from the more commonly deployed pyrethroids in terms of binding affinity to key P450s and resistance in vector populations, but was closely related to these pyrethroids in terms of depletion by anopheline P450s in the laboratory. The analysis of pyrethroid depletion by the P450s indicates that etofenprox may be particularly vulnerable to metabolic resistance mechanisms in vector populations. In addition, greater resistance was found across Ae. aegypti populations, but greater resistance to etofenprox was not found in any of the malaria vector species analysed. It is worth noting that there are still significant correlations between resistance in malaria vector populations to etofenprox and resistance to the pyrethroids in common use, and it is possible that a correlation could also be found for bifenthrin once data from multiple vector populations are available to answer this question. Systematic SAR analyses of these more structurally diverse pyrethroids are required to estimate the effect of structural diversity on pyrethroid resistance, and these findings need to be verified by studies of resistance in wild populations.
Supplementary Information
Additional file 1. Further details of the functional activity data including Table S1. Primers used for amplification of CYP6Z3 and in vitro functional characterisation. Figure S1. Fe2+-CO vs. Fe2+ difference spectrum of E. coli membranes expressing AgCYP6Z3. Table S2. IC50 values (μM) of pyrethroid insecticides. Table S3. Pyrethroid metabolism by mosquito P450s.
Additional file 2. Additional results from the population resistance comparisons including Figure S2. The distributions of paired pyrethroid susceptibility test mortality values for An. gambiae s.l. Figure S3. The distributions of paired pyrethroid susceptibility test mortality values for the An. funestus subgroup. Figure S4. The distributions of paired pyrethroid susceptibility test mortality values for four species. Figure S5. The distributions of paired susceptibility test mortality values for four species exposed to deltamethrin and a non-pyrethroid insecticide. Figure S6. Comparisons between resistance to etofenprox and five other pyrethroids in the An. gambiae complex and the An. funestus subgroup. Figure S7. Comparison of resistance to three pyrethroids within the An. gambiae complex and An. funestus subgroup. Figure S8. Comparisons of resistance to three pyrethroids in four malaria vector species. Figure S9. Comparison of resistance to deltamethrin and six insecticides from other classes. Table S4. Correlations between resistance to deltamethrin and non-pyrethroid insecticides in four African malaria vector species.
Additional file 3. Further details of the analyses of resistance in Aedes populations including Table S5. Diagnostic doses and data volumes for each pyrethroid. Table S6. Correlations in resistance to different pyrethroids in Ae. aegypti samples. Table S7. Comparisons of mean mortality between pairs of pyrethroids.
Additional file 4. A csv file containing the full data for pairs of pyrethoid susceptibility test results in each species.
Acknowledgements
Natalie Lissenden is acknowledged for searching the literature and laboratory data for measurements of quantitative toxicity of pyrethroids against malaria and dengue vectors.
Authors' contributions
CLM and HMI conceived the study. CLM, CY, KJW, KH, FO, MJIP and HMI generated the data and conducted the analyses. All authors contributed to the interpretation of the results and preparation of the manuscript. All authors read and approved the final manuscript.
Funding
This work was funded by a Global Fund contract awarded to RSL, a NIAID Grant Number R01AI116811 awarded to DW, a European Union Seventh Framework Programme FP7 (2007–2013) Grant Agreement No. 265660 AvecNet that funded MJIP, CY and KH and a Wellcome Grant Number 108440/Z/15/Z awarded to CLM.
Availability of data and materials
All susceptibility test data analysed during this study are included in Additional file 4.
Ethics approval and consent to participate
Not applicable.
Consent for publication
All authors provided their consent for publication.
Competing interests
The authors confirm they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
C. L. Moyes, Email: catherinemoyes@gmail.com
H. M. Ismail, Email: Hanafy.Ismail@lstmed.ac.uk
Supplementary Information
The online version contains supplementary material available at 10.1186/s13071-021-04609-5.
References
- 1.World Health Organization: World malaria report 2019. Geneva: World Health Organization; 2019.
- 2.World Health Organization: Prequalified lists. 2020. https://www.who.int/pq-vector-control/prequalified-lists/en/. Accessed 11 August 2020.
- 3.Hancock PA, Hendriks CJM, Tangena JA, Gibson H, Hemingway J, Coleman M, et al. Mapping trends in insecticide resistance phenotypes in African malaria vectors. PloS Biol. 2020;18:6. doi: 10.1371/journal.pbio.3000633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moyes CL, Athinya DK, Seethaler T, Battle KE, Sinka M, Hadi MP, et al. Evaluating insecticide resistance across African districts to aid malaria control decisions. Proc Natl Acad Sci USA. 2020;117(36):22042–22050. doi: 10.1073/pnas.2006781117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soderlund DM. Molecular mechanisms of pyrethroid insecticide neurotoxicity: recent advances. Arch Toxicol. 2012;86(2):165–181. doi: 10.1007/s00204-011-0726-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Narahashi T. Nerve membrane ionic channels as the primary target of pyrethroids. Neurotoxicology. 1985;6(2):3–22. [PubMed] [Google Scholar]
- 7.Sinka ME, Golding N, Massey NC, Wiebe A, Huang Z, Hay SI, et al. Modelling the relative abundance of the primary African vectors of malaria before and after the implementation of indoor, insecticide-based vector control. Malar J. 2016;15:42. 10.1186/s12936-016-1187-8. [DOI] [PMC free article] [PubMed]
- 8.Kawada H, Dida GO, Ohashi K, Komagata O, Kasai S, Tomita T, et al. Multimodal Pyrethroid Resistance in Malaria Vectors, Anopheles gambiae ss, Anopheles arabiensis, and Anopheles funestus ss in Western Kenya. PLoS One. 2011;6:8. doi: 10.1371/journal.pone.0022574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Camara S, Koffi AA, Alou LPA, Koffi K, Kabran JPK, Kone A, et al. Mapping insecticide resistance in Anopheles gambiae (s.l.) from Cote d’Ivoire. Parasites Vectors. 2018;11:19. 10.1186/s13071-017-2546-1. [DOI] [PMC free article] [PubMed]
- 10.Foster GM, Coleman M, Thomsen E, Ranson H, Yangalbe-Kalnone E, Moundai T, et al. Spatial and temporal trends in insecticide resistance among malaria vectors in Chad highlight the importance of continual monitoring. PLoS One. 2016;11:5. doi: 10.1371/journal.pone.0155746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kawada H, Futami K, Komagata O, Kasai S, Tomita T, Sonye G, et al. Distribution of a knockdown resistance mutation (L1014S) in Anopheles gambiae s.s. and Anopheles arabiensis in Western and Southern Kenya. PLoS ONE. 2011;6:9. doi: 10.1371/journal.pone.0024323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ndiath MO, Cailleau A, Orlandi-Pradines E, Bessell P, Pages F, Trape JF, et al. Emerging knock-down resistance in Anopheles arabiensis populations of Dakar, Senegal: first evidence of a high prevalence of kdr-e mutation in West African urban area. Malar J. 2015;14:364. doi: 10.1186/s12936-015-0898-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Reddy MR, Godoy A, Dion K, Matias A, Callender K, Kiszewski AE, et al. Insecticide resistance allele frequencies in Anopheles gambiae before and after anti-vector interventions in continental Equatorial Guinea. Am J Trop Med Hyg. 2013;88(5):897–907. doi: 10.4269/ajtmh.12-0467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moyes CL, Wiebe A, Gleave K, Trett A, Hancock PA, Padonou GG, et al. Analysis-ready datasets for insecticide resistance phenotype and genotype frequency in African malaria vectors. Sci Data. 2019;6:121. doi: 10.1038/s41597-019-0134-21Zxza. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rinkevich FD, Du Y, Dong K. Diversity and convergence of sodium channel mutations involved in resistance to pyrethroids. Pestic Biochem Physiol. 2013;106(3):93–100. doi: 10.1016/j.pestbp.2013.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Khambay BPS, Farnham AW, Beddie DG. Relationships between pyrethroid structure and level of resistance in houseflies (Musca domestica L). In: Briggs GG, editor. Advances in the chemistry of insect control III; 1994. Cambridge: Royal Society of Chemistry; p. 117–26.
- 17.Davies TGE, Williamson M. Interactions of pyrethroids with the voltage-gated sodium channel. Bayer Crop Sci J. 2009;62:9. [Google Scholar]
- 18.Awolola TS, Adeogun A, Olakiigbe AK, Oyeniyi T, Olukosi YA, Okoh H, et al. Pyrethroids resistance intensity and resistance mechanisms in Anopheles gambiae from malaria vector surveillance sites in Nigeria. PLoS One. 2018;13:12. doi: 10.1371/journal.pone.0205230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hemingway J, Vontas J, Poupardin R, Raman J, Lines J, Schwabe C, et al. Country-level operational implementation of the Global Plan for Insecticide Resistance Management. Proc Natl Acad Sci USA. 2013;110(23):9397–9402. doi: 10.1073/pnas.1307656110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Irving H, Wondji CS. Investigating knockdown resistance (kdr) mechanism against pyrethroids/DDT in the malaria vector Anopheles funestus across Africa. BMC Genet. 2017 doi: 10.1186/s12863-017-0539-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.David JP, Ismail HM, Chandor-Proust A, Paine MJI. Role of cytochrome P450s in insecticide resistance: impact on the control of mosquito-borne diseases and use of insecticides on Earth. Phil Trans R Soc Lond B Biol Soc. 2013;368:1612. doi: 10.1098/rstb.2012.0429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amenya DA, Naguran R, Lo TCM, Ranson H, Spillings BL, Wood OR, et al. Over expression of a cytochrome P450 (CYP6P9) in a major African malaria vector, Anopheles funestus, resistant to pyrethroids. Insect Mol Biol. 2008;17(1):19–25. doi: 10.1111/j.1365-2583.2008.00776.x. [DOI] [PubMed] [Google Scholar]
- 23.Barnes KG, Irving H, Chiumia M, Mzilahowa T, Coleman M, Hemingway J, et al. Restriction to gene flow is associated with changes in the molecular basis of pyrethroid resistance in the malaria vector Anopheles funestus. Proc Natl Acad Sci USA. 2017;114(2):286–291. doi: 10.1073/pnas.1615458114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kwiatkowska RM, Platt N, Poupardin R, Irving H, Dabire RK, Mitchell S, et al. Dissecting the mechanisms responsible for the multiple insecticide resistance phenotype in Anopheles gambiae ss, M form, from Vallee du Kou, Burkina Faso. Gene. 2013;519:98–106. doi: 10.1016/j.gene.2013.01.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Muller P, Donnelly MJ, Ranson H. Transcription profiling of a recently colonised pyrethroid resistant Anopheles gambiae strain from Ghana. BMC Genomics. 2007;8:36. doi: 10.1186/1471-2164-8-36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ngufor C, Nuessan R, Fagbohoun J, Subramaniam K, Odjo A, Fongnikin A, et al. Insecticide resistance profile of Anopheles gambiae from a phase II field station in Cove, southern Benin: implications for the evaluation of novel vector control products. Malar J. 2015;14:464. doi: 10.1186/s12936-015-0981-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nikou D, Ranson H, Hemingway J. An adult-specific CYP6P450 gene is overexpressed in a pyrethroid-resistant strain of the malaria vector Anopheles gambiae. Gene. 2003;318:91–102. doi: 10.1016/s0378-1119(03)00763-7. [DOI] [PubMed] [Google Scholar]
- 28.Riveron JM, Ibrahim SS, Chanda E, Mzilahowa T, Cuamba N, Irving H, et al. The highly polymorphic CYP6M7 cytochrome P450 gene partners with the directionally selected CYP6P9a and CYP6P9b genes to expand the pyrethroid resistance front in the malaria vector Anopheles funestus in Africa. BMC Genomics. 2014;15:817. doi: 10.1186/1471-2164-15-817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Riveron JM, Irving H, Ndula M, Barnes KG, Ibrahim SS, Paine MJI, et al. Directionally selected cytochrome P450 alleles are driving the spread of pyrethroid resistance in the major malaria vector Anopheles funestus. Proc Natl Acad Sci USA. 2013;110(1):252–257. doi: 10.1073/pnas.1216705110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thomsen EK, Strode C, Hemmings K, Hughes AJ, Chanda E, Musapa M, et al. Underpinning sustainable vector control through informed insecticide resistance management. PLoS One. 2014;9:6. doi: 10.1371/journal.pone.0099822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Vontas J, Grigoraki L, Morgan J, Tsakireli D, Fuseini G, Segura L, et al. Rapid selection of a pyrethroid metabolic enzyme CYP9K1 by operational malaria control activities. Proc Natl Acad Sci USA. 2018;115(18):4619–4624. doi: 10.1073/pnas.1719663115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ibrahim SS, Ndula M, Riveron JM, Irving H, Wondji CS. The P450 CYP6Z1 confers carbamate/pyrethroid cross-resistance in a major African malaria vector beside a novel carbamate-insensitive N485I acetylcholinesterase-1 mutation. Mol Ecol. 2016;25(14):3436–3452. doi: 10.1111/mec.13673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Weetman D, Kamgang B, Badolo A, Moyes CL, Shearer FM, Coulibaly M, et al. Aedes Mosquitoes and Aedes-Borne Arboviruses in Africa: Current and Future Threats. Int J Environ Res Public Health. 2018;15:2. doi: 10.3390/ijerph15020220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Moyes CL, Vontas J, Martins AJ, Ng LC, Koou SY, Dusfour I, et al. Contemporary status of insecticide resistance in the major Aedes vectors of arboviruses infecting humans. PLoS Negl Trop Dis. 2017;11:7. doi: 10.1371/journal.pntd.0005625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Hancock PA, Wiebe A, Gleave KA, Bhatt S, Cameron E, Trett A, et al. Associated patterns of insecticide resistance in field populations of malaria vectors across Africa. Proc Natl Acad Sci USA. 2018;115(23):5938–5943. doi: 10.1073/pnas.1719663115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.WHO Expert Committee on Vector Biology and Control & World Health Organization. Vector resistance to pesticides: fifteenth report of the WHO Expert Committee on Vector Biology and Control. World Health Organisation; 1992. https://apps.who.int/iris/handle/10665/37432. [PubMed]
- 37.World Health Organization/Department of Communicable Disease Prevention, Control and Eradication. Test procedures for insecticide resistance monitoring in malaria vectors, bio-efficacy and persistance of insecticides on treated surfaces. World Health Organisation; 1998. https://www.who.int/whopes/resources/who_cds_cpc_mal_98.12/en/.
- 38.Yunta C, Hemmings K, Stevenson B, Koekemoer LL, Matambo T, Pignatelli P, et al. Cross-resistance profiles of malaria mosquito P450s associated with pyrethroid resistance against WHO insecticides. Pestic Biochem Physiol. 2019;161:61–67. doi: 10.1016/j.pestbp.2019.06.007. [DOI] [PubMed] [Google Scholar]
- 39.Kalliokoski T, Kramer C, Vulpetti A, Gedeck P. Comparability of mixed IC50 data—a statistical analysis. PLoS One. 2013;8:4. doi: 10.1371/journal.pone.0061007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.McLaughlin LA, Niazi U, Bibby J, David JP, Vontas J, Hemingway J, et al. Characterization of inhibitors and substrates of Anopheles gambiae CYP6Z2. Insect Mol Biol. 2008;17(2):125–135. doi: 10.1111/j.1365-2583.2007.00788.x. [DOI] [PubMed] [Google Scholar]
- 41.Yunta C, Grisales N, Nasz S, Hemmings K, Pignatelli P, Voice M, et al. Pyriproxyfen is metabolized by P450s associated with pyrethroid resistance in An gambiae. Insect Biochem Mol Biol. 2016;78:50–57. doi: 10.1016/j.ibmb.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Holm S. A simple sequentially rejective multiple test procedure. Scand J Stat. 1979;6(2):65–70. [Google Scholar]
- 43.Sokal RR, Michener CD. A statistical method for evaluating systematic relationships. Univ Kans Sci Bull. 1958;38:1409–1438. [Google Scholar]
- 44.Krippendorff BF, Lienau P, Reichel A, Huisinga W. Optimizing classification of drug-drug interaction potential for CYP450 isoenzyme inhibition assays in early drug discovery. J Biomol Screen. 2007;12(1):92–99. doi: 10.1177/1087057106295897. [DOI] [PubMed] [Google Scholar]
- 45.Muller P, Warr E, Stevenson BJ, Pignatelli PM, Morgan JC, Steven A, et al. Field-caught permethrin-resistant Anopheles gambiae overexpress CYP6P3, a P450 that metabolises pyrethroids. PLoS Genet. 2008;4:1000286. doi: 10.1371/journal.pgen.1000286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Stevenson BJ, Bibby J, Pignatelli P, Muangnoicharoen S, O'Neill PM, Lian LY, et al. Cytochrome P450 6M2 from the malaria vector Anopheles gambiae metabolizes pyrethroids: Sequential metabolism of deltamethrin revealed. Insect Biochem Mol Biol. 2011;41(7):492–502. doi: 10.1016/j.ibmb.2011.02.003. [DOI] [PubMed] [Google Scholar]
- 47.Horstmann S, Sonneck R. Contact Bioassays with Phenoxybenzyl and Tetrafluorobenzyl Pyrethroids against Target-Site and Metabolic Resistant Mosquitoes. PLoS One. 2016;11:e0149738. doi: 10.1371/journal.pone.0149738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Tan JG, McCaffery AR. Efficacy of various pyrethroid structures against a highly metabolically resistant isogenic strain of Helicoverpa armigera (Lepidoptera : Noctuidae) from China. Pest Manag Sci. 2007;63(10):960–968. doi: 10.1002/ps.1419. [DOI] [PubMed] [Google Scholar]
- 49.The Global Fund: List of indoor residual sprays (IRS) that meet GF QA requirements for use against malaria vector. https://www.theglobalfund.org/media/5857/psm_indoorresidualsprayirsgf_list_en.pdf?u=636679306830000000 (2020). Accessed 12 Aug 2020.
- 50.Okwa OO. The current trends in integrated prevention and control of malaria. A case study of some Nigerian communities. Glob Adv Res J Med Med Sci. 2012;2:104–107. [Google Scholar]
- 51.Tangena JAA, Hendriks CMJ, Devine M, Tammaro M, Trett AE, Williams I, et al. Indoor residual spraying for malaria control in sub-Saharan Africa 1997 to 2017: an adjusted retrospective analysis. Malar J. 2020;19:1. doi: 10.1186/s12936-020-03216-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chanda E, Kandyata A, Chanda J, Phiri FN, Muzia L, Kamuliwo M. The efficacy of Vectron 20 WP, etofenprox, for indoor residual spraying in areas of high vector resistance to pyrethroids and organochlorines in Zambia. Int Scholary Res Notices. 2012;2013:e371934. doi: 10.5402/2013/371934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Ozumba N, Onyido A, Nwosu E, Ekwunife E, Amadi E. Field trial tests on the efficacy and residual effects of Bistar® 10wp on mosquitoes and other household arthropod pests. Internet J Trop Med. 2008;6:9. [Google Scholar]
- 54.RTI International. Rwanda spraying performance report. Research Triangle Park: RTI International; 2007.
- 55.Chang KS, Yoo DH, Shin EH, Lee WG, Roh JY, Park MY. Susceptibility and resistance of field populations of Anopheles sinensis (Diptera: Culicidae) collected from Paju to 13 insecticides. Osong Public Health Res Perspect. 2013;4(2):76–80. doi: 10.1016/j.phrp.2013.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Flores AE, Ponce G, Silva BG, Gutierrez SM, Bobadilla C, Lopez B, et al. Wide spread cross resistance to pyrethroids in Aedes aegypti (Diptera: Culicidae) from Veracruz State Mexico. J Econ Entomol. 2013;106(2):959–969. doi: 10.1603/ec12284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Juntarajumnong W, Pimnon S, Bangs MJ, Thanispong K, Chareonviriyaphap T. Discriminating lethal concentrations and efficacy of six pyrethroids for control of Aedes aegypti in Thailand. J Am Mosq Control Assoc. 2012;28(1):30–37. doi: 10.2987/11-6203.1. [DOI] [PubMed] [Google Scholar]
- 58.Thanispong K, Sathantriphop S, Malaithong N, Bangs MJ, Chareonviriyaphap T. Establishment of diagnostic doses of five pyrethroids for monitoring physiological resistance in Aedes albopictus in Thailand. J Am Mosq Control Assoc. 2015;31(4):346–352. doi: 10.2987/moco-31-04-346-352.1. [DOI] [PubMed] [Google Scholar]
- 59.Djouaka RF, Bakare AA, Coulibaly ON, Akogbeto MC, Ranson H, Hemingway J, et al. Expression of the cytochrome P450s, CYP6P3 and CYP6M2 are significantly elevated in multiple pyrethroid resistant populations of Anopheles gambiae ss from Southern Benin and Nigeria. BMC Genomics. 2008;9:538. doi: 10.1186/1471-2164-9-538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Munhenga G, Koekemoer LL. Differential expression of cytochrome P450 genes in a laboratory selected Anopheles arabiensis colony. Afr J Biotechnol. 2011;10:59. doi: 10.5897/ajb11.363. [DOI] [Google Scholar]
- 61.Nardini L, Christian RN, Coetzer N, Koekemoer LL. DDT and pyrethroid resistance in Anopheles arabiensis from South Africa. Parasites Vectors. 2013;6:229. doi: 10.1186/1756-3305-6-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Jones CM, Haji KA, Khatib BO, Bagi J, Mcha J, Devine GJ, et al. The dynamics of pyrethroid resistance in Anopheles arabiensis from Zanzibar and an assessment of the underlying genetic basis. Parasites Vectors. 2013;6:343. doi: 10.1186/1756-3305-6-343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Abdalla H, Wilding CS, Nardini L, Pignatelli P, Koekemoer LL, Ranson H, et al. Insecticide resistance in Anopheles arabiensis in Sudan: temporal trends and underlying mechanisms. Parasites Vectors. 2014;7:213. doi: 10.1186/1756-3305-7-213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Main BJ. Complex and evolving insecticide resistance spans species barriers in Anopheles coluzzii. Am J Trop Med Hyg. 2015;93(4):363–364. [Google Scholar]
- 65.Main BJ, Lee Y, Collier TC, Norris LC, Brisco K, Fofana A, et al. Complex genome evolution in Anopheles coluzzii associated with increased insecticide usage in Mali. Mol Ecol. 2015;24(20):5145–5157. doi: 10.1111/mec.13382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Ibrahim SS, Riveron JM, Stott R, Irving H, Wondji CS. The cytochrome P450 CYP6P4 is responsible for the high pyrethroid resistance in knockdown resistance-free Anopheles arabiensis. Insect Biochem Mol Biol. 2016;68:23–32. doi: 10.1016/j.ibmb.2015.10.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lucas ER, Rockett KA, Lynd A, Essandoh J, Grisales N, Kemei B, et al. A high throughput multi-locus insecticide resistance marker panel for tracking resistance emergence and spread in Anopheles gambiae. Sci Rep. 2019;9:13335. doi: 10.1038/s41598-019-49892-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ibrahim SS, Amvongo-Adjia N, Wondji MJ, Irving H, Riveron JM, Wondji CS. Pyrethroid resistance in the major malaria vector Anopheles funestus is exacerbated by overexpression and overactivity of the P450 CYP6AA1 across Africa. Genes. 2018;9:3. doi: 10.3390/genes9030140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Barnes KG, Weedall GD, Ndula M, Irving H, Mzihalowa T, Hemingway J, et al. Genomic footprints of selective sweeps from metabolic resistance to pyrethroids in African malaria vectors are driven by scale up of insecticide-based vector control. PLoS Genet. 2017;13:2. doi: 10.1371/journal.pgen.1006539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Toe KH, N'Fale S, Dabire RK, Ranson H, Jones CM. The recent escalation in strength of pyrethroid resistance in Anopheles coluzzi in West Africa is linked to increased expression of multiple gene families. BMC Genomics. 2015;10.1038/s41598-019-49892-6:146. doi: 10.1186/s12864-015-1342-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Gregory R, Darby AC, Irving H, Coulibaly MB, Hughes M, Koekemoer LL, et al. A de novo expression profiling of Anopheles funestus, malaria vector in Africa, using 454 pyrosequencing. PLoS One. 2011;6:2. doi: 10.1371/journal.pone.0017418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.David JP, Strode C, Vontas J, Nikou D, Vaughan A, Pignatelli PM, et al. The Anopheles gambiae detoxification chip: A highly specific microarray to study metabolic-based insecticide resistance in malaria vectors. Proc Natl Acad Sci USA. 2005;102(11):4080–4084. doi: 10.1073/pnas.0409348102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Edi CV, Djogbenou L, Jenkins AM, Regna K, Muskavitch MAT, Poupardin R, et al. CYP6 P450 enzymes and ACE-1 duplication produce extreme and multiple insecticide resistance in the malaria mosquito Anopheles gambiae. PLoS Genet. 2014;10:3. doi: 10.1371/journal.pgen.1004236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Riveron JM, Yunta C, Ibrahim SS, Djouaka R, Irving H, Menze BD, et al. A single mutation in the GSTe2 gene allows tracking of metabolically based insecticide resistance in a major malaria vector. Genome Biol. 2014;15:2. doi: 10.1186/gb-2014-15-2-r27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Balabanidou V, Kefi M, Aivaliotis M, Koidou V, Girotti JR, Mijailovsky SJ, et al. Mosquitoes cloak their legs to resist insecticides. Proc R Soc Biol Sci. 2019;286:1907. doi: 10.1098/rspb.2019.1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ding YC, Ortelli F, Rossiter LC, Hemingway J, Ranson H. The Anopheles gambiae glutathione transferase supergene family: annotation, phylogeny and expression profiles. BMC Genomics. 2003;4:35. doi: 10.1186/1471-2164-4-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Lumjuan N, Rajatileka S, Changsom D, Wicheer J, Leelapat P, Prapanthadara LA, et al. The role of the Aedes aegypti Epsilon glutathione transferases in conferring resistance to DDT and pyrethroid insecticides. Insect Biochem Mol Biol. 2011;41(3):203–209. doi: 10.1016/j.ibmb.2010.12.005. [DOI] [PubMed] [Google Scholar]
- 78.Strode C, Wondji CS, David JP, Hawkes NJ, Lumjuan N, Nelson DR, et al. Genomic analysis of detoxification genes in the mosquito Aedes aegypti. Insect Biochem Mol Biol. 2008;38(1):113–123. doi: 10.1016/j.ibmb.2007.09.007. [DOI] [PubMed] [Google Scholar]
- 79.Lumjuan N, McCarroll L, Prapanthadara LA, Hemingway J, Ranson H. Elevated activity of an Epsilon class glutathione transferase confers DDT resistance in the dengue vector, Aedes aegypti. Insect Biochem Mol Biol. 2005;35(8):861–871. doi: 10.1016/j.ibmb.2005.03.008. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1. Further details of the functional activity data including Table S1. Primers used for amplification of CYP6Z3 and in vitro functional characterisation. Figure S1. Fe2+-CO vs. Fe2+ difference spectrum of E. coli membranes expressing AgCYP6Z3. Table S2. IC50 values (μM) of pyrethroid insecticides. Table S3. Pyrethroid metabolism by mosquito P450s.
Additional file 2. Additional results from the population resistance comparisons including Figure S2. The distributions of paired pyrethroid susceptibility test mortality values for An. gambiae s.l. Figure S3. The distributions of paired pyrethroid susceptibility test mortality values for the An. funestus subgroup. Figure S4. The distributions of paired pyrethroid susceptibility test mortality values for four species. Figure S5. The distributions of paired susceptibility test mortality values for four species exposed to deltamethrin and a non-pyrethroid insecticide. Figure S6. Comparisons between resistance to etofenprox and five other pyrethroids in the An. gambiae complex and the An. funestus subgroup. Figure S7. Comparison of resistance to three pyrethroids within the An. gambiae complex and An. funestus subgroup. Figure S8. Comparisons of resistance to three pyrethroids in four malaria vector species. Figure S9. Comparison of resistance to deltamethrin and six insecticides from other classes. Table S4. Correlations between resistance to deltamethrin and non-pyrethroid insecticides in four African malaria vector species.
Additional file 3. Further details of the analyses of resistance in Aedes populations including Table S5. Diagnostic doses and data volumes for each pyrethroid. Table S6. Correlations in resistance to different pyrethroids in Ae. aegypti samples. Table S7. Comparisons of mean mortality between pairs of pyrethroids.
Additional file 4. A csv file containing the full data for pairs of pyrethoid susceptibility test results in each species.
Data Availability Statement
All susceptibility test data analysed during this study are included in Additional file 4.