Abstract
As an awardee of the Centers for Disease Control and Prevention’s Colorectal Cancer Control Program, the California Department of Public Health partnered with Neighborhood Healthcare to implement evidence-based interventions and provider incentives (incentives offered to support staff, e.g., medical assistants, phlebotomists, front office staff, lab technicians) to improve colorectal cancer screening uptake. The objective of this study was to evaluate the effectiveness and cost of the provider incentive intervention implemented by Neighborhood Healthcare to increase colorectal cancer screening uptake. We collected and analyzed process and cost data to assess fecal immunochemical test (FIT) kit return rates to the health centers and the number of completed FIT kits. We estimated the costs of the preexisting interventions and the new interventions. Analyses were conducted for two time periods: preimplementation and implementation. Most Neighborhood Healthcare health centers experienced an increase in the percentage of FIT kit returns (average of 3.6 percentage points) and individuals screened (an average increase of 111 FIT kits per month) from the baseline period through the implementation period. The cost of the incentive intervention for each additional screen was $66.79. In conclusion, the results indicate that incentive programs can have an overall positive impact on both the percentage of FIT kits returned and the number of individuals screened.
Keywords: colorectal cancer, California, cancer screening, federally qualified health centers, economic evaluation, provider incentives
BACKGROUND
In California, 70.8% of men and women aged 50 to 75 are up to date with colorectal cancer (CRC) screening (Centers for Disease Control and Prevention [CDC], National Cancer Control Program, 2017). However, the percentage varies by sociodemographic characteristics, such as race, ethnicity, and insurance status. The percentage of Black and White residents who report up-to-date CRC screening is 77.5% and 77.3%, respectively, whereas the screening rate for Hispanic or Latino residents is 55.6% (CDC, 2017). The CRC screening rate among people without insurance is approximately half the screening rate of people with insurance: 34.4% versus 67.3% (CDC, 2017).
To decrease disparities in CRC screening uptake, in 2015, the CDC (2018) funded 30 awardees (states, universities, and tribal health organizations) to implement evidence-based interventions (EBIs) to increase CRC screening uptake as part of its Colorectal Cancer Control Program (additional detail on the Colorectal Cancer Control Program is provided in a companion article in this journal; Tangka et al., 2020). One Colorectal Cancer Control Program awardee was the California Department of Public Health. As an awardee, the California Department of Public Health began the California Colon Cancer Control Program and worked with several federally qualified health centers (FQHCs) to improve CRC screening uptake through the implementation of EBIs.
One of the FQHCs in partnership with the California Department of Public Health is Neighborhood Healthcare, located in San Diego and Riverside Counties, and with a patient profile that is, on average, 36% Hispanic. Neighborhood Healthcare implemented an incentive system with its support staff using its own internal funding in conjunction with additional EBIs, which were under way at the health centers. There is a lack of research on the effectiveness of incentives in promoting CRC screening, and due to insufficient evidence, The Community Guide has not recommended it as an intervention (Community Preventive Services Task Force, 2013). The objective of this study is to evaluate the effectiveness and cost of the support staff incentive intervention (payments were offered to support staff at the clinics when predetermined screening target were met) implemented by Neighborhood Healthcare to increase CRC screening uptake.
METHOD
Interventions to Increase CRC Screening Uptake
To improve its CRC screening uptake, Neighborhood Healthcare decided to supplement its ongoing efforts and implement two types of incentives for its support staff. One incentive was given to all support staff at a health center (e.g., medical assistants, phlebotomists, front office staff, lab technicians) when its CRC screening uptake moved one 5-percentage point interval (e.g., from 45% to 50%). A second incentive was given to all support staff at the health center when a health center’s fecal immunochemical test (FIT) kit return rate for the month was 75% or higher. Each incentive was $25 per month per measure to each support staff.
Before initiating the incentive program, Neighborhood Healthcare had already instituted provider and patient reminders within health centers’ electronic medical record systems. Also, to reduce structural barriers, the health centers gave patients picture-based educational materials and instructions available in English, Arabic, and Spanish. If patients required a different language, the health centers used translation services. In addition, health centers provided prestamped and prelabeled envelopes to make returning the kits easier and had a drop box to return kits in the waiting areas.
These multicomponent EBIs were in place before July 2015, but health centers varied in how they implemented them. Starting in January 2016, the process of implementing the EBIs was streamlined and EBI implementation was generally standardized across the centers. The bonus payments for both CRC screening uptake and FIT kit return rates were implemented in July 2016.
Data Collection
We reported on nine of Neighborhood Healthcare’s 11 health centers. The nine health centers were the centers that participated in the CDC’s Colorectal Cancer Control Program. A detailed description of data collection and methodology is provided in a companion article in this journal.
The health centers collected process measures (e.g., number of FIT kits distributed and the number returned within 2 months) to assess implementation of the incentive program. FIT kits were distributed to average-risk, asymptomatic, age-eligible (age 50–75) patients. Neighborhood Healthcare tracked the amount of bonus payments for CRC screening uptake increase, as well as FIT kit return rates made to each center on a monthly basis. We captured the cost of all EBIs implemented by the health system and the costs of the CRC screening process. Provider reminders and approaches to reduce structural barriers had negligible ongoing cost (as resources are required to initially modify the electronic medical record systems and translate materials). We then focused on estimating cost for the patient reminders (e.g., staff time making reminder calls) to highlight the cost of existing interventions. We collected cost data from three representative health centers that were able to collect the data to estimate the cost of conducting patient reminders. We used a combination of health center staff interviews and time-and-motion assessments to estimate the time spent on each key activity per patient. The health centers participating in this study provided time spent in the implementation phase.
Analyses
We analyze data for two time frames. The preimplementation period was July 2015 to June 2016, and the implementation period was July 2016 to December 2017. These time frames were selected to reflect the implementation of the provider incentives, which is the intervention evaluated in this study. We analyze the data in 6-month increments across the study period.
We report the percentages of FIT kits returned and the number screened by each health center in 6-month increments from July 2015 to December 2017 to evaluate overall trends. For the percentage of FIT kits returned, we conducted significance testing using t tests comparing by health center whether the changes from the preimplementation period to the end of the implementation period reported were significant.
Using cost data reported, we calculated the per-person cost of the initial contact to provide the FIT kit, tracking and reminders, laboratory processing of the kits, and following up with patients after a positive FIT kit using the activity-based cost data from the health centers. We also reported the total cost of incentives and the cost of the incentives per additional person screened. Using this information, we calculated an estimate of the bonus payments to screen one additional person.
RESULTS
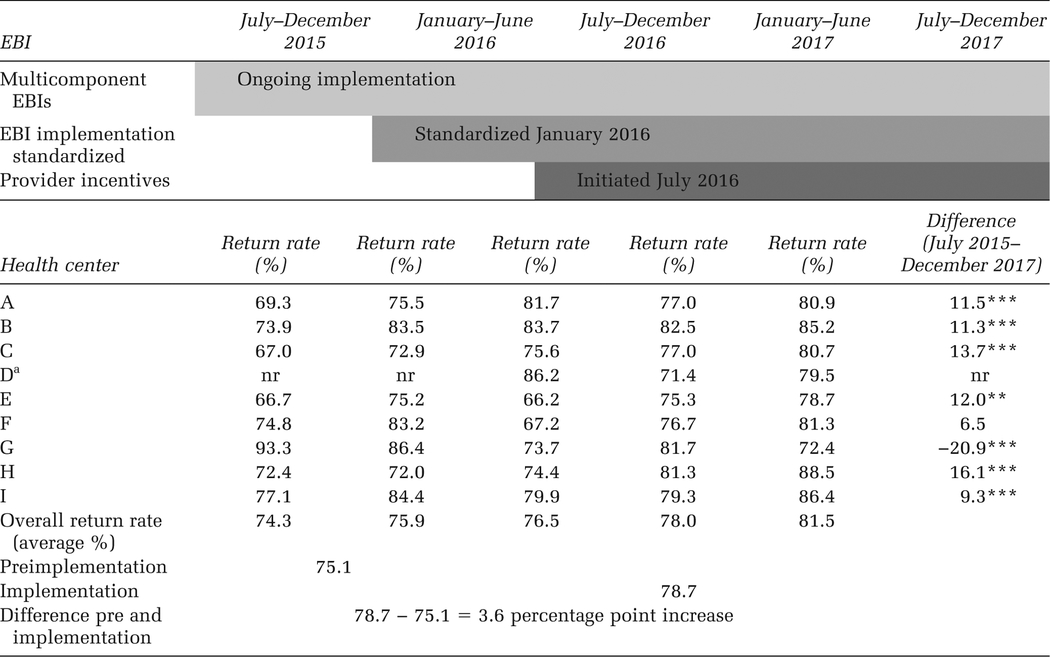
Most health centers experienced an increase in the percentage of FIT kit returns from the preimplementation period (July 2015–June 2016) through the implementation period (July 2016–December 2017; Table 1). In 6-month intervals, the average percentage change across all centers showed a consistently increasing pattern of FIT kit return rates from 74.3% in the first 6-month period to 81.5% in the last 6-month period. Overall, the average percentage of FIT kit returns was 75.1% during preimplementation; the percentage of returns increased to 78.7% during implementation, for an increase of 3.6 percentage points. By individual health center, the change ranged from a decrease of 20.9 percentage points to an increase of 16.1 percentage points.
TABLE 1.
Fecal Immunochemical Test Return Rate by Health Center
|
Note. Multicomponent EBIs are interventions where more than one intervention can be implemented at different levels. EBI = evidence-based intervention; nr = not reported.
Health Center D has data beginning March 2016 and is not reported in the January–June 2016 period because of small cell size.
p < .01.
p < .05.
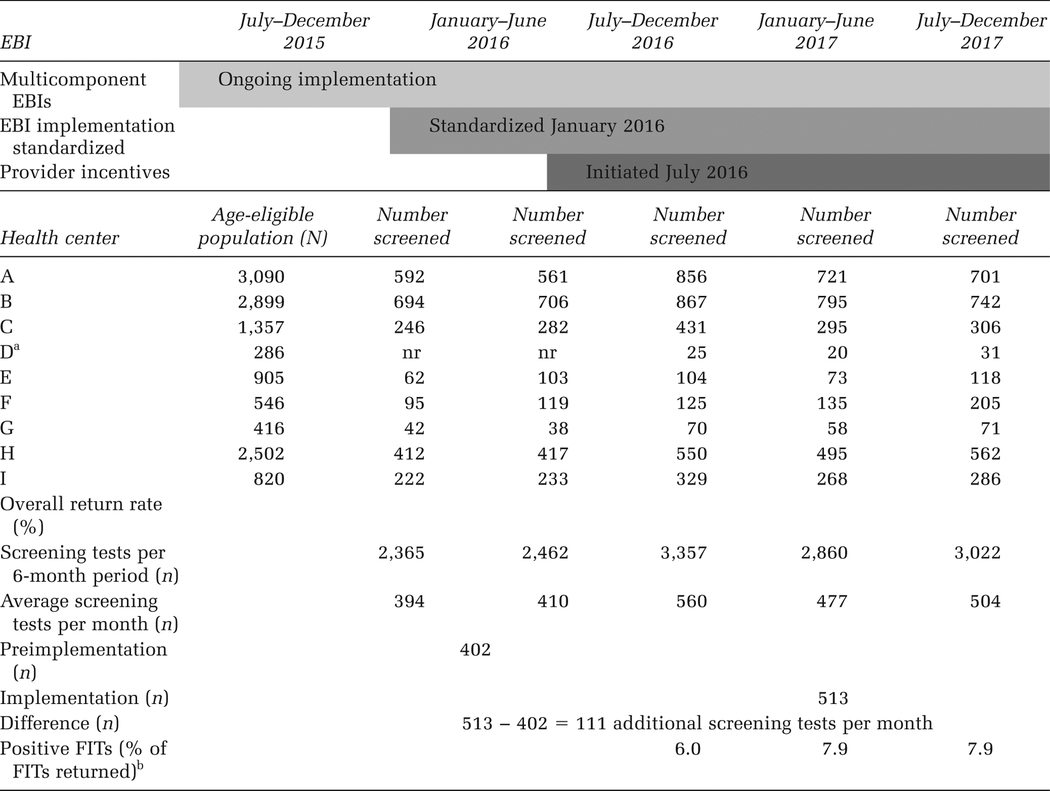
The number of CRC screening tests by health center generally increased by period (Table 2). The number of CRC screening tests increased from 2,365 for the period July to December 2015 to 3,022 for the period July to December 2017. The 6-month period with the highest number of screens was July to December 2016, with 3,357 individuals returning FIT kits; these are the months immediately after the implementation of the incentive program. The average number of CRC screening tests per month was 402 during the pre-implementation period and 513 during the implementation period; this was an average increase of 111 additional CRC screening tests per month. Of the FITs returned during implementation, on average, 7.3% were positive.
TABLE 2.
Total Number of Colorectal Cancer Screening Tests by Health Center
|
Note. Multicomponent EBIs are interventions where more than one intervention can be implemented at different levels. EBI = evidence-based intervention; FIT = fecal immunochemical test; nr = not reported.
Health Center D has data beginning March 2016 and is not reported in the January–June 2016 period because of small cell size.
Follow-up colonoscopies were not consistently reported back to Neighborhood Healthcare.
The cost estimates for the CRC screening processing, including the patient reminders, and the incentive program are shown in Table 3. The average cost per patient was $5.88 for contacting patients, purchasing FIT kits, and distributing them; $3.51 for tracking patients and reminding them to return FIT kits; $1.89 for processing the FIT kits; and $7.84 for follow-up activities after a positive FIT, which included referral for a diagnostic colonoscopy. The cost of the new intervention and incentive program totaled $133,447.30, which included $2,172.30 for processing incentives and $131,275.00 for the bonuses. Most of the incentive payment was for the FIT return rate bonus ($113,225.00), whereas only a small proportion was for the CRC screening bonus ($18,050.00). The cost of the incentive intervention for each additional screening test (based on 1,998 screening tests) was $66.79.
TABLE 3.
Cost Estimates for Preexisting and New Interventions
| Cost estimates, $ | |||
|---|---|---|---|
| Cost category | Description | Average per patient | Range per patient |
| Cost of patient reminders and CRC screening process | |||
| Patient contact and FIT distribution | Initial contact with patient; provide patient with a prelabeled FIT kit along with instructions, collection date, and prestamped envelope; if patient has colonoscopy, obtain signed release form and fax to specialist; includes cost of FIT kit | 5.88 | 3.17–8.49 |
| Patient tracking and reminders | Follow-up with patients, reminder calls and letters, outreach to return kits | 3.51 | 2.27–6.21 |
| Process laboratory tests | Personnel and indirect cost associated with processing FIT kits | 1.89 | — |
| Follow-up after positive FIT | Educate patient and refer to diagnostic colonoscopy; refer for treatment and follow-up | 7.84 | 5.41–11.07 |
| Total cost, $ | Range per heath center, $ | ||
| Cost of incentives (18-month period) | |||
| FIT return rate bonus | 113,225.00 | 1,500–27,875 | |
| CRC screening rate bonus | 18,050.00 | 500-$6,725 | |
| Cost to process incentives | 2,172.30 | — | |
| Total cost of Incentives | 133,447.30 | — | |
| Additional screening tests (111 screening tests per month × 18 months), n | 1,998 | ||
| Cost of the incentives per additional screening test | 66.79 | ||
Note. FIT = fecal immunochemical test; CRC = colorectal cancer.
DISCUSSION
Neighborhood Healthcare’s incentive program overall increased both the percentage of FIT kit returns and the number of individuals screened. During the study period, from July 2015 to December 2017, all health centers, except for one, experienced an increase in FIT kit return rates. In prior analyses, our team reported a wide range in the percentage of FIT kit returns at health centers from 31.0% to 81.6% (Conn et al., 2020; Kemper et al., 2018); the percentage of FIT kit returns in Neighborhood Healthcare centers was definitely on the high end of this range with percentages from 72.4% to 88.5% during the 6 months from July to December 2017. The percentage of FIT kit returns was already quite high, 75.1%, before the incentive program, which could be a result of the multicomponent interventions already implemented in the clinics. Despite this, average FIT kit returns during the implementation period increased to 78.7%, and during the last 6-month period, the average percentage was 81.5%. Additionally, the incentive program substantially increased the overall volume of individuals screened. On average, an additional 111 patients per month received CRC screening after the bonus payments were implemented.
The increase in screening was achieved at an intervention cost of about $67 per additional person screened. The cost of the overall initial screening process (from FIT kit distribution to return) in Neighborhood Healthcare centers was approximately $8. This was based on $5.88 for initial contact and $3.51 for reminders and tracking; we assumed that two thirds of the patients required reminders. Overall, the percentage of FIT kits returned was 80%, and the cost per person successfully screened was calculated to be approximately $10 ($8 ÷ 80%). The laboratory processing cost was $1.89 for each returned kit, and follow-up referral was $7.84 per person with a positive finding. Because only 7% of tests had a positive result, this amounted to less than $1 in cost per average person successfully screened. Adding the incentive payment of $67 per person screened to these screening-related costs, the total cost per additional person successfully screened by the health system was about $80. In prior studies, the incremental cost per person successfully screened has ranged from $13 to as high as $2,602; therefore, the costs from this study fall in the lower end of the range (Lairson et al., 2014; Liss et al., 2016; Misra et al., 2011; Phillips et al., 2015). Additionally, researchers have reported similar costs to the present study. In a recent study among rural health centers in West Virginia, the average cost per FIT kit returned was $60.18 (not including cost of FIT kits or lab processing fees; Conn et al., 2020). Using a simulation-based study from randomized trials, researchers concluded that the cost per completed FIT kit ranged from $45 to $74 (includes cost of FIT kit [$5.03] and processing of returned kits [$2.20]; Liss et al., 2016).
Among the two bonus payments implemented, a much higher proportion of cost was incurred for the FIT return rate bonus than the CRC screening uptake bonus. This was likely because it was much more difficult to consistently increase screening uptake by 5–percentage point intervals compared with maintaining FIT return rates at levels higher than 75%. In this study, the implementation of the incentive payments and their impacts were assessed over an 18-month period. It is not known whether the long-term impact of the bonus payments will remain the same, especially given the challenges of increasing screening uptake as the overall level of screening uptake increases across the health centers. The 18-month data show that the largest increase in screening uptake occurred during the first 6 months of the intervention, but the numbers screened were also higher for the next 12 months compared with the pre-implementation period. Over the long term, it may be more appropriate to use incentives as a onetime booster rather than as a continuous intervention.
There are a few limitations to the analysis presented in this study. First, the increase in screening uptake varied across the health centers. We hypothesized that the type of patient served at a health center can affect screening uptake, with those serving more transient clientele experiencing higher levels of variation in FIT return rates. Second, we estimated cost data based on information collected from three of the nine health centers. Although efforts were made to standardize the interventions and screening procedures, there could have been variations across the health centers that we did not capture. Third, because of inadequate follow-up data, we could not report on the completion of follow-up colonoscopies for those with positive FITs. Fourth, we assessed the impact of the incentives over an 18-month period, and the long-term effectiveness may differ. Neighborhood Healthcare is continuing to monitor the incentive intervention and plans to implement adjustments and further adaptations to the incentive payments based on ongoing study findings.
IMPLICATIONS FOR PRACTICE AND/OR POLICY AND RESEARCH
We found that incentive payments provided to support staff at health centers increased CRC screening uptake and complemented multilevel EBI interventions. Although CRC screening uptake at Neighborhood Healthcare was already at 75%, the interventions increased CRC screening uptake even more at a reasonable cost per additional person screened.
These findings add to the evidence base on cost-effective implementation of provider incentive programs in health care systems. Future research may examine the optimal schedule and duration, as well as sustainability, of offering support staff incentives. Lessons learned from Neighborhood Healthcare’s practices may inform other FQHCs interested in implementing staff/provider incentives as part of a broad strategy to improve CRC screening uptake.
Acknowledgments
We thank staff of Neighborhood Healthcare for their support in compiling the data for this study. Special thanks to LeeAnn Velasquez at the California Department of Public Health for support in managing the California Colon Cancer Control Program, maintaining the billing invoices for the contracted health centers, and facilitating the partnership with Neighborhood Healthcare. Funding support for RTI International was provided by the Centers for Disease Control and Prevention (CDC; Contract No. 200-2014-61263 Task 4, to RTI International). The findings and conclusions in this article are those of the authors and do not necessarily represent the official position of the CDC.
REFERENCES
- Centers for Disease Control and Prevention. (2018, December 3). Colorectal Cancer Control Program (CRCCP): About program. https://www.cdc.gov/cancer/crccp/index.htm
- Centers for Disease Control and Prevention, National Cancer Control Program. (2017). Quick facts: Colorectal cancer (CRC) screening in California. https://www.cdc.gov/cancer/ncccp/screening-rates/pdf/colorectal-cancer-screening-california-508.pdf
- Community Preventive Services Task Force. (2013). Increasing cancer screening: Client incentives. Task force finding and rationale statement. https://www.thecommunityguide.org/sites/default/files/assets/Cancer-Screening-Client-Incentives.pdf
- Conn ME, Kennedy-Rea S, Subramanian S, Baus A, Hoover S, Cunningham C, & Tangka FKL (2020). Cost and effectiveness of reminders to promote colorectal cancer screening uptake in rural federally qualified health centers in West Virginia. Health Promotion Practice, 21(6), XX–XX. 10.1177/1524839920954164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemper KE, Glaze BL, Eastman CL, Waldron RC, Hoover S, Flagg T, Tangka F, & Subramanian S (2018). Effectiveness and cost of multilayered colorectal cancer screening promotion interventions at federally qualified health centers in Washington State. Cancer, 124(21), 4121–4129. 10.1002/cncr.31693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lairson DR, Dicarlo M, Deshmuk AA, Fagan HB, Sifri R, Katurakes N, Cocroft J, Sendecki J, Swan H, Vernon SW, & Myers RE (2014). Cost-effectiveness of a standard intervention versus a navigated intervention on colorectal cancer screening use in primary care. Cancer, 120(7), 1042–1049. 10.1002/cncr.28535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liss DT, French DD, Buchanan DR, Brown T, Magner BG, Kollar S, & Baker DW (2016). Outreach for annual colorectal cancer screening: A budget impact analysis for community health centers. American Journal of Preventive Medicine, 50(2), e54–e61. 10.1016/j.amepre.2015.07.003 [DOI] [PubMed] [Google Scholar]
- Misra S, Lairson DR, Chan W, Chang YC, Bartholomew LK, Greisinger A, McQueen A, & Vernon SW (2011). Cost effectiveness of interventions to promote screening for colorectal cancer: A randomized trial. Journal of Preventive Medicine and Public Health, 44(3), 101–110. 10.3961/jpmph.2011.44.3.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips L, Hendren S, Humiston S, Winters P, & Fiscella K (2015). Improving breast and colon cancer screening rates: A comparison of letters, automated phone calls, or both. Journal of the American Board of Family Medicine, 28(1), 46–54. 10.3122/jabfm.2015.01.140174 [DOI] [PubMed] [Google Scholar]
- Tangka FKL, Subramanian S, Hoover S, DeGroff A, Joseph D, Wong FL, & Richardson LC (2020). Economic evaluation of interventions to increase colorectal cancer screening at federally qualified health centers. Health Promotion Practice, 21(6), XX–XX. 10.1177/1524839920954168 [DOI] [PMC free article] [PubMed] [Google Scholar]


