Abstract
COVID-19 has rapidly spread around the world and threatened global health. Although this disease mainly affects the respiratory system, there is increasing evidence that SARS-CoV-2 also has effects on the cardiovascular system. Echocardiography is a valuable tool in the assessment of cardiovascular disease. It is cost-effective, widely available and provides information that can influence management. Given the risk of personnel infection and equipment contamination during echocardiography, leading world societies have recommended performing echocardiography only when a clinical benefit is likely, favouring focussed evaluations and using smaller portable equipment. In the past months, multiple reports have described a wide pattern of echocardiographic abnormalities in patients with COVID-19. This review summarises these findings and discusses the possible mechanisms involved.
Keywords: COVID-19, Echocardiography, Myocardial injury, Ventricular function, Systemic inflammation
Introduction
Since the World Health Organization (WHO) officially declared COVID-19 a pandemic, it has rapidly spread and caused havoc around the world. As of 11 November 2020, more than 50 million people had been infected, with over 1,000,000 deaths [1]. It is well known that SARS-CoV-2 mainly affects the respiratory system, ranging from mild upper respiratory symptoms to acute respiratory distress syndrome (ARDS) [2]. However, in the last few months an important amount of evidence has shown the cardiovascular system to be a target of this disease [3]. COVID-19 seems to affect the cardiovascular system in many ways and has manifestations that range from asymptomatic elevations of cardiac biomarkers to cardiovascular collapse and cardiac arrest [3,4]. Studies have shown that nearly 20% of this population sustains myocardial damage and that myocardial injury – with or without respiratory failure – is implicated in up to 40% of deceased subjects [3,5]. Echocardiography is a widely available, cost-effective tool for evaluating cardiac structure and function. In critically ill subjects, a focussed evaluation provides important information that can affect therapeutic decisions [6]. Given the infectiousness of COVID-19 and the potential of equipment contamination and personnel exposure, the leading echocardiographic societies have recommended performing echocardiograms only if the obtained information is likely to produce a clinical benefit; they favour smaller portable devices that are easier to disinfect and performing focussed evaluations instead of complete echocardiograms [7,8]. Over the past months, valuable information has been provided regarding the echocardiographic manifestations of COVID-19. This review aimed to summarise these findings and briefly discuss the possible mechanisms involved.
Echocardiographic Abnormalities in COVID-19
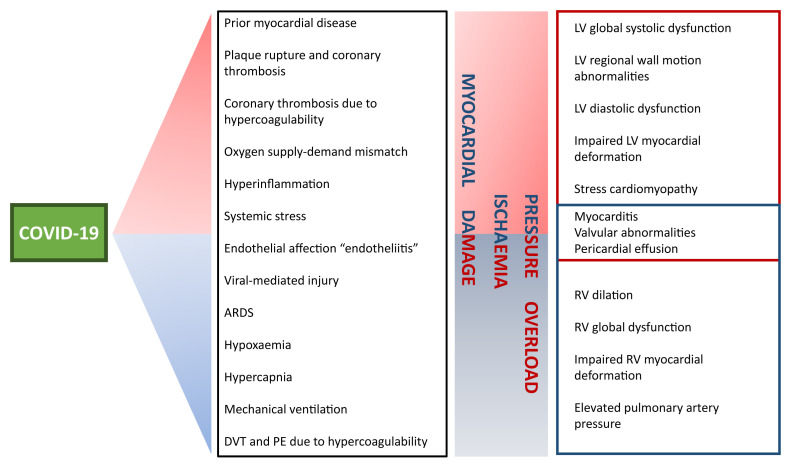
In COVID-19, cardiovascular manifestations can be the result of primary or secondary cardiac involvement, or even a worsening of previous cardiovascular disease (CVD). In each situation, echocardiography might be able to provide information about the mechanism, type and extent of the effects [9]. Multiple studies have provided information about different kinds of cardiac affection, some of them with different results regarding the frequency of right ventricular (RV) or left ventricular (LV) involvement [[10], [11], [12]]. This could be because of the diverse populations analysed in these studies. While some studies have performed echocardiograms on every subject with a diagnosis of COVID-19 [11], others have only included subjects with a clear indication for echocardiography (thoracic pain, troponin elevation, haemodynamic instability) [12]. Furthermore, subjects in some studies have been prospectively included, while other studies have conducted retrospective analysis. In addition, the disease severity has varied between studies, making the interpretation of this information complicated (Table 1 ). The following section will summarise the available data evaluating the use of echocardiography in COVID-19, dividing and discussing the possible mechanisms involved (Figure 1 ).
Table 1.
Characteristics of studies evaluating echocardiographic abnormalities in patients with COVID-19.
| Author | Study Characteristics | Indications for Echocardiography | Definitions | Comorbidities | Respiratory Status | LV Abnormalities | RV Abnormalities | Other Echocardiographic Abnormalities | Limitations |
|---|---|---|---|---|---|---|---|---|---|
| Dweck et al. [10] | 1,216 pts; prospective online survey; only patients with indications | Suspected left heart failure; suspected right heart failure; chest pain with ST-elevation; biomarker elevation; ventricular arrhythmia; suspected tamponade; cardiogenic shock | LV function: mildly impaired (55%–45%), moderately impaired (35%–45%), severely impaired (<35%). RV function: visually estimated |
HTN 37%; DM 19%; IHD 14%; HF 9%; VHD 7% | 54% severe symptoms; 19% evidence of pneumonia | 39%. LV systolic dysfunction: mildly depressed 17%, moderately depressed 12%, severely depressed 7%. MI 3%; myocarditis 3%; TS 2% | 33%. RV systolic dysfunction: mild-moderate 19%, severe 6%; RV dilation 15%; D-shape 4% | Cardiac tamponade 1%; endocarditis 1%; elevated PAP 8% | Online survey dependent on operator-reported outcomes; RV structure and function were visually estimated; selection bias |
| Jain et al. [12] | 72 pts; retrospective; only patients with indications | Haemodynamic assessment; concern for a major acute CV event; other | LV dimensions: normal mean±1.96 SD reported. Mild, moderate or severe defined by incremental addition of 1 SD. LV function: visually estimated, Simpson’s biplane when LVEF appeared abnormal. RV dimension: basal and mid diameter, or visual estimation. RV function: assessed semi-quantitatively |
HTN 66.7%; DM 43.1%; Obes 47.2%; LD 20.8%; CKD 22.2%; HFrEF 20.8%; HFpEF 2.8%; CAD 18.1%; cancer 4.2%; HT 6.9%; LVAD 1.4%; AF 2.8% | 55.6% on MV | LVEF <50% in 34.7%; LVWMA in 23.6%: 12.5% global hypokinesia, 11.1% segmental abnormalities (LAD 2.8%, RCA 1.4%, MV 1.4%, apical hypokinesia with basal sparing 5.6%) | RV dimensions: mild dilation 12.5%, moderate dilation 2.8%, and severe dilation 0. RV systolic dysfunction: mildly decreased 26.4%, moderately decreased 9.7%, severely decreased 4.2% | 1 pt AR, 2 pts MR, 4 pts TR. 12.5% with peak TR vel >2.8 m/s; 8 pts with RAP 0–5 mmHg; 2 pts 5–10 mmHg; 1 pt 10–20 mmHg; 4.2% small pericardial effusion | LV and RV parameters visually estimated; small, retrospective sample; selection bias |
| Mahamoud-Elsayed et al. [13] | 74 pts; retrospective; only patients with indication | Chest pain; arrhythmia; abnormal ECG changes; haemodynamic instability; patients only proceeded to echo if troponin-I >14 ng/L or urgent assessment needed | LV function visually estimated; RV function FAC <35%, TAPSE <17 mm; RV dimensions RV dilation if basal diameter >41 mm | HTN 42%; DM 36%; CKD 11%; stroke 7%; smoker 7%; LD 14%; CAD 9%; cancer 7% | 82% on MV | LV dimensions: small LV 20%, normal LV 76%, dilated LV 4%. LV systolic function: hyperdynamic 48%, normal 41%, mildly impaired 5%, moderately impaired 3%, severely impaired 3% | RV dimensions dilated in 41%; RV function impaired in 27% | PAH probability: low 16%, intermediate 18%, high 16%; pericardial effusion 4% | LV parameters visually estimated; small, retrospective sample; referral bias |
| Churchill et al. [14] | 125 pts prospectively enrolled after screening for study appropriateness | ___ | According to guidelines | HTN 60%; DM 41%; Obes 50% | 88% on MV | LV systolic function: hyperdynamic or normal 78%, impaired 22%, LVWMA 14% | ___ | ___ | RV not reported; selection bias |
| Sud et al. [15] | 110 pts, retrospective; only pts with clinically indicated echocardiography 24 pts with SMI (troponin-I >1 ng/mL) |
___ | ___ | CAD 21% | 42% on MV | LV dysfunction in pts with SMI: 54%, 46% LVWMA, 8% diffuse LV hypokinesia; 37% isolated LV, 17% biventricular. Pts without SMI: 19% regional or global LV dysfunction; 6% biventricular. | RV dysfunction 17% | Pericardial effusion 33% | Small, retrospective sample; selection bias |
| Szekely et al. [11] | 100 pts, prospective; all patients underwent echocardiography | ___ | Compared to reference values | IHD 16%; HF 7%; CABG 5%; AF 15%; stroke 11%; LD 11%; CKD 10%; DM 29%; HTN 57%; Obes 29%; cancer 5% | 29% with need for non-invasive O2; 10% on MV | LVEF <50% in 10%; CI <2.5 L/m2/min in 60%; SVi ≥35 mL/m2 in 72%; LAVi ≥34 mL/m2 in 32%; E/e’ >14 in 20% | RV dimensions: dilated in 39%; RV function: FAC <35% in 17%; TAPSE <17 mm in 14%; RV S’ <9.5 cm/s in 25%; Tei index >0.54 in 20% | PAT <100 ms in 60%; 1 pt MR; 2 pts AR | No ECG trace during echocardiogram |
| Van den Heuvel et al. [16] | 51 pts, cross–sectional, all pts underwent echocardiography | ___ | LV dysfunction LVEF <52% or GLS >–18; RV dysfunction TAPSE <17 mm, RV S’ <10 cm/s | HTN 41%; DM 18%; smoker 6%; stroke 4%; CKD 2%; LD 12%; CAD 8%; MI 10%; HF 0; AF 8%; VA 2%; VHD 2% | 33% required MV, none at the time of echocardiography | LV systolic dysfunction in 27%, 5.7% low LVEF, 13.5% abnormal GLS, 7.7% both impaired | RV dysfunction in 10%, 4% low TAPSE, 4% low RV S’, 2% both impaired | ___ | Small sample; time from admission to echo |
| Rath et al. [17] | 123 pts (data on echo available for 98 pts); prospective; all pts underwent echocardiography | ___ | LV dysfunction LVEF ≤50%; RV dysfunction visually assessed, TAPSE <20 mm, FAC <35% | HTN 69.9%; DLP 37.4%; DM 24.4%; smoker 0.8%; Obes 19.5%; AF 22.8%; CAD 22.8%; CKD 11.4% | No mention | LV function: mean±SD LVEF 57 (8)%; LVH in 74.2% | RV dysfunction: visually estimated, impaired RV function in 13.7%, 17.3% low TAPSE; RV dimensions RV dilation in 48.9% |
AS 5.7%; AR 11.5%; MR 26.7%; TR 26.7%; pericardial effusion 48.9% | No mention of the prevalence of LV dysfunction; RV function visually assessed in some cases |
Abbreviations: LV, left ventricle; RV, right ventricle; HTN, hypertension; DM, diabetes mellitus; IHD, ischaemic heart disease; HF, heart failure; VHD, valvular heart disease; MI, myocardial infarction; TS, Takotsubo syndrome; PAP, pulmonary artery pressure; SD, standard deviation; LVEF, left ventricular ejection fraction; Obes, obesity; LD, lung disease; CKD, chronic kidney disease; CAD, coronary artery disease; HT, heart transplant; LVAD, left ventricular assistance device; AF, atrial fibrillation; MV, mechanical ventilation; LVWMA, left ventricular wall motion abnormalities; LAD, left anterior descendent; RAC, right coronary artery; MV, multiple vessel; AR, aortic regurgitation; MR, mitral regurgitation; TR, tricuspid regurgitation; RAP, right atrial pressure; FAC, fractional area change; TAPSE, tricuspid annular plane systolic excursion; PAH, pulmonary arterial hypertension; SMI, significant myocardial injury; PAT, pulmonary artery acceleration time; GLS, global longitudinal strain; VA, ventricular arrhythmia; DLP, dyslipidaemia; LVH, left ventricular hypertrophy.
Figure 1.
Echocardiographic manifestations in COVID-19 and possible mechanisms involved.
Abbreviations: RV, right ventricular; LV, left ventricular; ARDS, acute respiratory distress syndrome; DVT, deep vein thrombosis; PE, pulmonary embolism.
The Left Ventricle in COVID-19
The largest dataset of echocardiograms in COVID-19 comes from a recently published paper by Dweck et al., who collected data from 69 countries using an online survey [10]. Echocardiograms were only performed on those patients with a clear indication. This was reported in the survey (Table 1). A total of 1,216 patients were included, and 26% had pre-existing CVD. This study found that subjects with an abnormal echocardiogram (55%) were older, with a higher prevalence of pre-existing CVD, heart failure or valvular heart disease. An affection of the LV was diagnosed in 479 (39%) subjects, with systolic dysfunction in 37.4% and biventricular affection in 14.3%. Categorisation based on the LV ejection fraction (LVEF) revealed that it was mildly depressed in 17%, moderately depressed in 12% and severely depressed in 7%. In addition, 3% had evidence of a new myocardial infarction (MI), 3% of myocarditis and 2% of findings suggestive of Takotsubo syndrome (TS). Regarding subjects without a pre-existing CVD, 46% had an abnormal echocardiogram and 25% had LV anomalies. In this study, chest pain with an ST-segment elevation and suspected left heart failure were found to be independent predictors of LV anomalies with an OR of 4.08 (2.40–6.99) and 1.63 (1.15–2.32), respectively [10].
Similarly, Jain et al. retrospectively analysed the echocardiograms of 72 patients with confirmed SARS-CoV-2 infection [12]. They found that 10% of hospitalised patients had an indication for echocardiography, with a suspected acute cardiovascular event (46%) and haemodynamic assessment (29%) being the most frequent reasons. Pre-existing coronary artery disease (CAD) was present in 18.15%, heart failure with reduced ejection fraction (HFrEF) in 20.8% and with preserved ejection fraction in 2.8%. Overall, 34.7% of these subjects had an LVEF <50%, 23.6% had evidence of LV wall motion abnormalities, with 12.5% showing global hypokinesia and 11.1% segmental abnormalities. Interestingly, four of these patients had apical dyskinesia with basal sparing, compatible with stress-induced cardiomyopathy. Increased wall thickness was present in 61.1%, being mild in 36.1% [12]. A retrospective study including 74 patients with confirmed COVID-19 who underwent echocardiography, in which 58% of subjects were on vasopressor support, found that LV systolic function was hyperdynamic or normal in 89% of the patients [13]. In their cohort, 9% of patients had prior CVD, and three patients who had a previous abnormal study were excluded. Of note, LV systolic function was visually assessed in this study and the study by Jain et al. [12,13]. The results of other studies that included patients after evaluation of study appropriateness [14,15] are described in Table 1.
Other studies have performed echocardiograms in every patient admitted with confirmed SARS-CoV-2 infection [11,16,17]. Szekely et al. reported the findings of 100 patients with confirmed COVID-19 systematically evaluated with echocardiogram during the first 24 hours after hospital admission [11]; 16% of the patients had a history of CVD and 7% had prior congestive heart failure. In this population, the LV was found to be smaller than the reference values; cardiac output (CO) and cardiac index (CI) were found to be lower; LV systolic function was impaired (LVEF <50%) in 10% of subjects; and 20% of the patients had an E/e’ ratio >14, indicative of elevated LV filling pressures. Left ventricular function and dimensions did not significantly differ between disease severity categories (with non-invasive mechanical ventilation [NIMV], invasive mechanical ventilation [IMV] or O2) [11]. Van den Heuvel et al. consecutively evaluated 51 patients admitted to hospital with SARS-CoV-2 infection and found that 14 subjects (27%) had LV systolic dysfunction [16]. In this study, even though 19 patients were admitted to the ICU and 17 required mechanical ventilation during hospitalisation, all were without mechanical ventilation or vasopressors at the time of the echocardiographic evaluation. A key fact of this study is that it used global longitudinal strain (GLS) added to LVEF to evaluate systolic function (LV dysfunction was due to LVEF in three, abnormal GLS in seven and a combination of both in four). Diastolic dysfunction, defined as an E/e’ ratio >14, was present in 6% [16].
Possible mechanisms involved in left ventricular abnormalities in COVID-19
Several mechanisms have been proposed as culprits of cardiac injury in COVD-19 [3]. It is clear since the first reports from China that myocardial injury, defined by elevation in cardiac troponins (cTn), was not only common in SARS-CoV-2 but also associated with a worse prognosis [18,19]. In one of these studies, Guo et al. showed that the mortality of subjects with underlying CVD and cTn elevations was 69.4%, and 37.5% for those without CVD, respectively [18]. Other studies have confirmed the relationship between elevations in cTn and a worse prognosis [19,20]. COVID-19 has been related to elevation of inflammatory markers in the so-called “cytokine storm” [21]. This hyperinflammatory surge has also been described in cases of Middle East respiratory syndrome (MERS) and SARS-CoV infection [22]. Some studies have shown that elevation of cTn correlates with elevations in inflammation biomarkers such as C-reactive protein (CRP), and also that the lymphocyte percentage, CD3+, CD4+, CD8+ T-cell counts, and CD16+ and CD56+ NK are independently associated with myocardial injury [18,23]. In the study by Szekely et al., CRP elevation was predictive of LV dysfunction on echocardiogram, suggesting a relationship between myocardial dysfunction and systemic inflammation [11].
As in other systemic inflammatory states, LV systolic dysfunction can be a secondary form of cardiac involvement detected by echocardiography, which in some cases might resolve [24]. This has also been found in some patients with COVID-19 who had LV systolic dysfunction that was completely resolved on subsequent evaluations [14]. Of note, in septic and unstable patients, the LV usually appears hyperdynamic with apparently preserved LVEF, but evaluation using other techniques such as GLS has shown that patients can have cardiac dysfunction even in the absence of a diminished LVEF, and this has been associated with a worse prognosis [25]. In the study by van den Heuvel et al., 27% of the patients with COVID-19 had LV systolic dysfunction but only half had a low LVEF, and the manifestation was an impaired GLS in 50% [16]. The value of GLS in detecting subtle myocardial damage in patients with COVID-19 has been confirmed by other studies [26,27]. Baycan et al. evaluated 100 patients (44 with severe and 56 with non-severe COVID-19) and 45 controls, all of them with a normal LVEF. Their results showed that GLS was significantly impaired in both non-severe and severe COVID-19 patients compared with controls: –16.7±1.3% vs –14.5±1.8% vs –19.4±1.6%, respectively (p=0.001) [26]. Similarly, Stöbe et al. demonstrated that patients with SARS-CoV-2 infection can have abnormalities in LV deformation despite normal LVEF and that the alterations can predominantly affect LV basal segments [27]. Also, hyperinflammation with catecholamine release can be related to the development of stress cardiomyopathy [28]. Some patients in the studies by Dweck et al. and Jain et al. were found to have wall motion abnormalities compatible with TS [10,12]. Other reports have described patients with confirmed COVID-19 presenting with a classic apical ballooning during echocardiography or ventriculography and no coronary lesions during angiography, confirming the diagnosis of TS in COVID-19 [29,30].
Whether myocardial involvement is the result of systemic inflammation or secondary to direct viral damage is still a matter of debate [31,32]. Multiple reports have shown that patients with COVID-19 can present several manifestations compatible with acute myocarditis, and these subjects usually have global or segmental wall motion abnormalities with reduced LVEF on echocardiogram [4]. In an autopsy study during the SARS-CoV outbreak that analysed heart samples, it was found that 35% of patients had viral RNA [33]. Given the affinity of SARS-CoV-2 to the myocardium related to the high expression level of angiotensin-converting enzyme 2 (ACE 2), direct viral damage is thought to be a possibility [32]. Some reports have even found histopathological evidence of myocarditis in endomyocardial biopsies of patients with SARS-CoV-2, and some studies have reported the presence of viral RNA in the heart tissue of a few patients [4,[34], [35], [36]].
Ischaemic cardiac injury is another possible explanation, and can be the result of multiple factors [3,4,32]. Some patients with COVID-19 eventually develop ARDS with severe hypoxaemia [2], which along with systemic stress, sympathetic activation, use of vasopressors, and underlying CAD could cause an imbalance in myocardial oxygen supply-demand, resulting in cardiac ischaemia [3]. SARS-CoV-2 infection has also been associated with a hypercoagulable state with both venous and arterial thrombotic events described [35,37]. Direct involvement of endothelial cells (endotheliitis) is another feature of this infection that could increase the risk of thrombus formation [38]. Moreover, as in other severe viral infections [39], inflammation caused by SARS-CoV-2 could affect plaque stability and cause rupture of coronary plaques, with a subsequent myocardial infarction [3]. There is evidence that acute myocardial infarction (AMI) can occur during the course or can be the initial manifestation of COVID-19 [40,41]. In a report from Italy involving 28 patients with COVID-19 and ST-segment elevation myocardial infarction, 17 had angiographic evidence of a culprit lesion that required revascularisation [40]. Some echocardiography reports in COVID-19 have shown that patients can have evidence of segmental wall motion abnormalities involving specific coronary territories [12,15]. Diastolic dysfunction is described in some patients with COVID-19 and myocardial ischaemia might be the associated mechanism [11,16].
Since CVD is common in patients with COVID-19 [32], echocardiographic abnormalities could represent the presence of prior heart disease that has remained stable or that has worsened because of the SARS-CoV-2 infection. Some studies have reported that some of their population had prior echocardiograms with LV dysfunction or wall motion abnormalities [11,12,15]. In the majority of these subsets of patients, the echocardiograms performed during SARS-CoV-2 infection showed a worsening of prior echocardiographic findings. Another mechanism that might be implicated in cardiac dysfunction during COVID-19 is downregulation of ACE2 after SARS-CoV-2 entry into the host cells. Since ACE2 inactivates angiotensin II and has beneficial effects, this downregulation could be related to progressive cardiac damage and worsening dysfunction [3,32].
Cardiac biomarkers, left ventricular echocardiographic findings and prognosis in COVID-19
It is a matter of debate whether the elevation of cardiac biomarkers in patients with COVID-19 is merely the reflection of disease severity or a manifestation of cardiac damage with cardiac structure and function alterations [42]. The report by Dweck et al. showed that biomarker elevation was one of the most frequent reasons for requesting an echocardiographic evaluation. Also, those patients with biomarker elevation (69%) were more likely to have an abnormal echocardiogram [10]. On multivariate regression models, elevations of cTn and brain natriuretic peptide (BNP) were independent predictors of an abnormal LV on echocardiogram with an OR 1.69 (1.13–2.53) and 2.9 (1.75–5.05), respectively [10]. In the study by Szekely et al., 20% of patients had cTn elevations and those with troponin-I ≥28 ng/L had a significantly lower stroke volume, CO and CI, without a difference in LVEF [11]. Also, patients with higher troponin levels more frequently had an E/e’ >14 than those with lower troponin levels. Overall, troponin levels were predictive of an altered E/e’ and an increased left atrial volume. BNP levels were predictive of a lower SV, CO, and altered E/e’ [11]. In this same study, LVEF was significantly associated with clinical deterioration (2.9 [1.1–8.1]; p=0.03 for 10% difference) and mortality (3.2 [1.01–8.1]; p=0.04 for 10% difference), while an elevated E/e’ ratio (1.08 [1.01–1.2]; p=0.03) was also associated with mortality [11]. Rath et al. showed that LVEF was significantly associated with cTn levels and N-terminal-pro-BNP [17]. They also showed that LVEF was independently related to all-cause mortality [17]. Baycan et al. showed that both elevations in cTn and D-dimer significantly correlated with a worse LV GLS (p=0.001); notably, their study also showed that an impaired LV GLS was an independent predictor of mortality, suggesting that even subtle myocardial dysfunction can be an indicator of bad prognosis [26]. Other studies showing the association between cardiac biomarkers, LV abnormalities and outcomes are summarised in Table 2 and Supplementary Table 1.
Table 2.
Biomarkers, left ventricular abnormalities and outcomes in patients with COVID-19.
| Author | Biomarkers and Left Ventricular Abnormalities | Left Ventricular Abnormalities and Outcomes |
|---|---|---|
| Dweck et al. [10] | Troponin elevation predicted LV abnormalities on the echocardiogram: OR, 1.69; 95% CI, 1.13–2.53. BNP elevation predicted LV abnormalities on the echocardiogram: OR, 2.96; 95% CI, 1.75–5.05. |
____ |
| Jain et al. [12] | Inverse correlation hs-cTn and LVEF: rho = –0.34; p=0.006. Trend towards an inverse correlation NT-proBNP and LVEF: rho = –0.29; p=0.056 |
____ |
| Szekely et al. [11] | Correlation Troponin-I and E/e’: rho=0.45; p=0.0001. Inverse correlation between BNP and SV, CO: rho= –0.43; p=0.0001 and rho= –0.21; p=0.04, respectively. Correlation between BNP and E/e’: rho=0.38; p=0.0001. Inverse correlation CRP and SV: rho= –0.22; p=0.03. Correlation CRP and E/e’: rho=0.87; p=0.0001. |
Low LVEF associated with clinical deterioration and mortality: OR, 2.9; 95% CI, 1.1–8.1 for 10% difference and OR, 3.2; 95% CI, 1.01–8.1; p=0.04 for 10% difference, respectively. Elevated E/e’ associated with mortality: OR, 1.08; 95% CI, 1.01–1.2; p=0.03. |
| Van den Heuvel et al. [16] | No difference between patients with Troponin-T >14 ng/L or ≤14 ng/L and LVEF or GLS: p=0.15 and p=0.20, respectively. No difference between patients with NT-proBNP >300 pg/L or ≤300 pg/L and LVEF or GLS: p=0.62 and p=0.53, respectively. |
____ |
| Rath et al. [17] | Inverse correlation Troponin-I and NT-proBNP and LVEF: rho= –0.367; p<0.001 and rho= –0.485; p<0.001, respectively. | LVEF independently associated with mortality: HR, 12.19; 95% CI, 2.87–51.83; p=0.001. |
| Baycan et al. [26] | Correlation between elevated hs-cTn and D-dimer and impaired LV GLS; p=0.001. | Impaired LV GLS associated with higher risk of death: OR, 1.635; p=0.010 and for a GLS >–15.20 OR, 8.342; p<0.001. A cut-off value of >–15.20% had an area under the curve of 0.83 with a sensibility of 77% and specificity of 75% for prediction of mortality. |
Abbreviations: LV, left ventricle; OR, odds ratio; CI, confidence interval; hs-cTn, high-sensitivity cardiac troponin; NT-proBNP, N terminal pro-brain natriuretic peptide; LVEF, left ventricular ejection fraction; SV, stroke volume; CO, cardiac output; CRP, C-reactive protein; GLS, global longitudinal strain; HR, hazard ratio.
The Right Ventricle in COVID-19
Since COVID-19 predominantly affects the respiratory system, some patients will eventually require ventilatory assistance such as a high-flow nasal cannula, NIMV or endotracheal intubation with IMV [43]. The acute stress caused by hypoxaemia and mechanical ventilation added to the prothrombotic state, hyperinflammatory state, direct viral damage, and ischaemic injury places the RV in a critical position during COVID-19 [44]. In the study by Dweck et al., 33% of patients had an abnormal RV on echocardiography [10]. Of these subjects, 19% had mild-to-moderate RV dysfunction and 6% had severe dysfunction. The RV was dilated in 15%, a D-shaped LV was seen in 4% and pulmonary artery pressure was elevated in 8%. In the analysis restricted to only those patients without pre-existing CVD, one-third of the patients had an abnormal RV [10]. In their analysis, 60% of the patients were in critical care and 19% had evidence of pneumonia, although there is no report of how many patients were on mechanical ventilation. Suspected right heart failure (OR, 2.65; 95% CI, 1.88–3.75) and moderate (OR, 2.34; 95% CI, 1.32–4.29) or severe (OR, 3.19; 95% CI, 1.73–6.10) COVID-19 disease were independent predictors of RV abnormalities on the echocardiogram [10]. Jain et al. found that 15.3% of the patients had an increased RV size (12.5% were mildly increased and 2.8% were moderately increased) [12]. Right ventricular systolic function was mildly decreased in 26.4%, moderately decreased in 9.7% and severely decreased in 4.2%. In this study, 20.8% of the patients had a history of asthma, chronic obstructive pulmonary disease (COPD) or interstitial lung disease, and 55.6% were on mechanical ventilation at the time of the echocardiographic evaluation. Regarding 46% of the population in whom concern of an acute major CV event was the main reason for the echocardiogram, 11% represented a suspicion of pulmonary embolism (PE); findings consistent with this diagnosis were found in the echocardiogram in four of these patients [12]. The study by Mahmoud-Elsayed et al. found a dilated RV in 41% of patients and decreased RV function in 27%. In this report, most patients had severe respiratory failure and 82% were on IMV; the use of IMV did not affect the proportion of subjects with RV dysfunction [13]. A PE was detected in 20% of subjects with RV dysfunction as compared with 2% in those without RV dysfunction (p=0.02) [13].
In the study by Szekely et al., 61% of subjects had moderate disease requiring non-invasive O2 and 10% had severe disease requiring IMV [11]. The authors found a prevalence of RV dilation of 39%, reduced fractional area change (FAC) in 28%, reduced systolic tricuspid lateral velocity (RV S’) in 25%, reduced index of myocardial performance (Tei index) in 20%, and reduced tricuspid annular plane systolic excursion (TAPSE) in 14%; all are parameters of RV systolic function [11]. Overall, the authors concluded that the most frequent echocardiographic abnormality in COVID-19 was RV dilation with or without dysfunction [11]. Also, the authors evaluated pulmonary flow acceleration time (PAT) as a measure of pulmonary vascular resistance (PVR) and found that patients with a worse clinical status had a shorter PAT, suggesting an increased RV afterload probably secondary to severe respiratory impairment [11]. Contrary to what is reported by other authors, where the RV is commonly affected during COVID-19, van den Heuvel et al. reported the presence of RV dysfunction in 10% of patients [16]. Notably, 33% of patients had IMV at some point, but none at the time of the echocardiographic evaluation [16]. Other studies that assessed RV structure and function in COVID-19 are summarised in Table 1.
Possible mechanisms involved in right ventricular abnormalities in COVID19
Studies from China have reported that 41.8% of patients who presented to a hospital with COVID-19-related pneumonia could develop ARDS, and mortality was very high [45]. In ARDS, the thin-walled RV, which usually works against low resistance, faces an abrupt increase in afterload secondary to increases in PVR, which causes ventricular dilation and eventual RV failure [46]. The incidence of RV dysfunction can be as high as 50% in ARDS and has been related to a worse prognosis [46]. Three (3) parameters have been demonstrated to be independently associated with RV dysfunction in ARDS: (1) driving pressure ≥18 cmH2O; (2) PaCO2 ≥48 mmHg; and (3) partial pressure of arterial oxygen : fraction of inspired oxygen (PaO2: FiO2) <150 mmHg [47]. Driving pressure can be used as a surrogate of transpulmonary pressure (TPP), which is known to exponentially increase PVR [48]. Hypercapnia, which occurs both as a consequence of a ventilation-perfusion mismatch and as a result of protective ventilation with low tidal volumes in ARDS, is known to increase PVR. It has been demonstrated that PaCO2 is an independent predictor of RV dysfunction in patients with ARDS and protective ventilation [49]. Low oxygen saturation, reflected in a PaO2: FiO2 <150 mmHg, during severe ARDS can also increase mean pulmonary arterial pressure and is associated with RV dysfunction [47]. In most of the studies evaluating the echocardiographic abnormalities in COVID-19, a significant number of patients were on IMV at the time of echocardiographic evaluation, although the prevalence of ARDS in each was not specified. In the study by Szekely et al., patients on IMV had a significantly lower PAT, which reflected an increased PVR associated with a worse respiratory condition; in addition, patients in the lower tertiles of PAT had significantly lower oxygen saturation (p<0.01) and FiO2. (p<0.01) [11]. Another study found no difference in the use of IMV between patients with and without RV dysfunction, although patients with RVD had lower PaO2:FiO2 and higher FiO2 [13]. Positive pressure ventilation, also commonly used in ARDS, can cause pulmonary vessel compression, increasing PVR and contributing to RV dysfunction in these subjects [46]. Patients with COVID-19 and RVD were found to have higher positive end-expiratory pressure (PEEP) compared with those without RVD, although this difference was not statistically significant [13]. The lower prevalence of RVD reported by van den Heuvel et al., where patients were off IMV, compared with the other studies where a higher proportion of patients were on IMV suggests that the stress associated with respiratory failure and ventilatory support can partly explain the RV abnormalities seen in patients during COVID-19 [16]. Increased vasoactive mediators, vascular remodelling, vascular thrombosis, and vascular compression secondary to atelectasis and oedema also contribute to RV dilation and dysfunction in ARDS caused by COVID-19 [44].
As previously mentioned, patients with COVID-19 are in a prothrombotic state that predisposes them to thromboembolic events, including deep vein thrombosis (DVT) and PE [32]. There is evidence showing that >40% of patients admitted to hospital had elevated D-dimer levels, which was associated with an increased risk of death [50]. Autopsy studies have found that >50% of the patients in whom venous thromboembolism was not suspected before death had evidence of DVT. Moreover, 33% of these patients had a PE detected as a direct cause of death [35]. Other studies using CT-pulmonary angiography have shown that 25% of patients can develop PE; furthermore, PE events can occur even with prophylactic anticoagulation [51]. In this same study, D-dimer was significantly higher in patients with PE compared with those without PE [51]. In the study by Szekely et al., patients with shorter PAT had greater levels of D-dimer as compared with those with normal PAT values. Both CRP and D-dimer were predictive of elevated PAT, suggesting a link between inflammation, thrombosis and elevated PVR [11]. Another study showed that D-dimer levels were related to RV dysfunction [13]. RV dysfunction in PE occurs because of a sudden increase in PVR secondary to pulmonary artery (PA) occlusion, and the degree of ventricular dysfunction is affected by thrombus size, the extent of PA occlusion and baseline cardiopulmonary status [52]. Echocardiography is not routinely indicated in haemodynamically stable patients with suspected PE, since the absence of signs of RVD does not exclude the diagnosis; conversely, in haemodynamically unstable patients the absence of signs of RV pressure overload can exclude PE as the cause of haemodynamic instability, while the presence of signs of pressure overload justifies reperfusion treatment [52]. In the study by Dweck et al., 33% of patients had a change in management because of findings on echocardiography; more than a third having a change in disease-specific therapy, which included therapy for PE [10]. Jain et al. described a change in management in 16.7% of patients who underwent echocardiographic evaluation; therapeutic anticoagulation was started because of signs suggestive of PE on echocardiography in four of these cases [12]. Similarly, in the study by Mahmoud-Elsayed et al., 20% of patients with RV dysfunction had a PE diagnosed by CT [13]. In the study by van den Heuvel et al., 18% of the patients had a PE diagnosed; however, the authors reported that none of these patients had echocardiographic signs of PE and all the patients included in this report were haemodynamically stable, which likely reflects the presence of low-risk PE where echocardiography can miss the diagnosis [16]. There have also been isolated reports of patients with RV clots in transit detected during echocardiography [53].
Other mechanisms that likely contribute to RV dysfunction in COVID-19 are direct myocardial damage by SARS-Cov-2, microvascular and macrovascular dysfunction associated with endotheliitis, excess of vasoactive peptides, and inflammatory damage [44]. RV dysfunction is likely the result of a combination of multiple factors: a sudden and progressive rise in PVR increases RV afterload, followed by a rise in serum catecholamines and other vasoactive peptides, which finally cause RV dilation and progress to a mismatch in myocardial oxygen supply-demand with RV ischaemia and RV dysfunction. Progressive RV failure and dilation with ventricular interdependence lead to reduced LV diastolic filling, reduced CO and eventual shock [44,46,52].
Cardiac biomarkers, right ventricular echocardiographic findings and prognosis in COVID-19
In the study by Szekely et al, patients with shorter PAT had higher levels of cTn, BNP, D-dimer, and CRP. In addition, patients with troponin-I levels ≥28 ng/L had shorter PAT, RVFAC, TAPSE, and RV S’. CRP was an independent predictor of altered PAT, Tei index, TAPSE, and RVFAC. D-dimer was predictive of an abnormal PAT, and RVFAC, while Troponin-I predicted an abnormal RVFAC [11]. In the same study, a shorter PAT was associated with clinical deterioration (2.9 [1.04–8.7]; p=0.04 for AT <100 m/s), while an increased RV end-diastolic area (1.14 [1.01–1.32]; p=0.05 for 1 cm2) and higher Tei index (1.29 [1.02–1.7]; p=0.03) were both associated with increased mortality [11]. Argulian et al. evaluated 110 patients with focussed echocardiography looking for RV dilation; in their univariate analysis they found that mechanical ventilation (p=0.003), vasoactive medication use (p=0.007) and RV enlargement (p=0.001) were associated with increased mortality [54]. In a multivariate analysis of the same study, RV enlargement was the only variable significantly associated with mortality (OR, 4.5; 95% CI, 1.5–13.7; p=0.005) [54]. Li et al. evaluated 120 patients using RV two-dimensional (2D) longitudinal strain (RVLS); they found that RVLS was a stronger predictor of mortality (HR, 1.33; 95% CI, 1.15–1.53; p<0.001) compared with RVFAC and TAPSE [55]. They found that the best cut-off value for the prediction of mortality using RVLS was –23%, with an area under the curve of 0.87 (p<0.001), sensitivity 94.4% and specificity 64.7% [55]. Other studies showing the association between cardiac biomarkers, RV abnormalities and outcomes are summarised in Table 3 and Supplementary Table 1.
Table 3.
Biomarkers, right ventricular abnormalities and outcomes in patients with COVID-19.
| Author | Biomarkers and Right Ventricular Abnormalities | Right Ventricular Abnormalities and Outcomes |
|---|---|---|
| Dweck et al. [10] | No relation between Troponin or BNP elevation and RV abnormalities on the echocardiogram: OR, 1.3; 95% CI, 0.86–1.95 and OR, 1.1; 95% CI, 0.63–1.88, respectively. | ____ |
| Mahamoud-Elsayed et al. [13] | Inverse correlation D-dimer, CRP and low FAC: rho= –0.34; p=0.003 and rho= –0.23; p=0.045, respectively. | ____ |
| Szekely et al. [11] | Inverse correlation Troponin-I, TAPSE, FAC and PAT: rho= –0.34; p=0.0006, rho= –0.32; p=0.001 and rho= –0.21; p=0.04, respectively. Inverse correlation D-dimer, PAT and FAC: rho= –0.26; p=0.008 and rho= –0.24; p=0.01, respectively. Inverse correlation CRP, PAT, TAPSE and FAC: rho= –0.52; p=0.0001, rho= –0.31; p=0.0001, rho= –0.27; p=0.01, respectively. Correlation CRP and Tei index: rho=0.6; p=0.0001. |
Shorter PAT associated with clinical deterioration: OR, 2.9; 95% CI, 1.04–8.7; p=0.04, for PAT <100 m/s. Increased RV end diastolic area and higher Tei index associated with mortality: OR, 1.14; 95% CI, 1.01–1.32; p=0.05, for 1 cm2 and OR, 1.29; 95% CI, 1.02–1.7; p=0.03, respectively. |
| Van den Heuvel et al. [16] | No difference between patients with Troponin-T >14 ng/L or ≤14 ng/L and TAPSE; p=0.44. No difference between patients with NT-proBNP >300 pg/L or ≤300 pg/L and TAPSE or RV S’: p=0.97 and p=0.8, respectively. |
____ |
| Rath et al. [17] | Inverse correlation Troponin-I, NT-proBNP and FAC: rho= –0.442; p<0.001 and rho= –0.304; p=0.006, respectively. | Impaired RV function associated with a significantly worse cumulative event-free survival, compared to patients with normal RV function. |
| Argulian et al. [54] | No differences in Troponin-I levels in patients with and without RV dilation | RV enlargement was the only variable significantly associated with mortality on multivariate analysis: OR; 4.5; 95% CI, 1.5–13.7; p=0.005. |
| Li et al. [55] | Patients in the lowest tertile of RVLS had higher levels of D-dimer and CRP compared with patients in the highest tertiles, p<0.05 for both. | RVLS, FAC and TAPSE associated with mortality in multivariate analysis: HR, 1.33; 95% CI, 1.15–1.53; p<0.001, HR, 0.90; 95% CI, 0.83–0.98; p=0.017 and HR, 0.88; 95% CI, 0.78–0.99; p=0.044, respectively. RVLS was the strongest predictor of mortality with an AUC 0.87 (p<0.001) for a cut-off value of –23%. |
| Baycan et al. [26] | Increased hs-cTn and D-dimer significantly associated with an impaired RVLS. | Impaired RVLS associated with higher risk of death: OR, 1.557; p=0.019 and for a RVLS >–18.45: OR, 6.229; p=0.011. A cut-off value of >–18.45% had an area under the curve of 0.77 with a sensibility of 72% and specificity of 66% for prediction of mortality. |
Abbreviations: BNP, brain natriuretic peptide; RV, right ventricle; OR, odds ratio; CI, confidence interval; CRP, C-reactive protein; FAC, fractional area change; TAPSE, tricuspid annular plane systolic excursion; PAT, pulmonary artery acceleration time; RVLS, right ventricular longitudinal strain; HR, hazard ratio.
Other Echocardiographic Abnormalities in COVID-19
Some of the reports have described the presence of valvular heart disease, with the majority of them comprising mitral or tricuspid regurgitation [11,12,17]. It is unclear whether these findings are associated with COVID-19 or represent prior valvular disease but are likely associated with prior diagnosed or undiagnosed disease, or with ventricular dilation. Endocarditis has been another finding in a minority of patients with COVID-19 during echocardiographic evaluation. Dweck et al. reported endocarditis in 14 (1%) patients in their study [10]. It is unclear whether this finding was associated with SARS-CoV-2 infection, or represented actual bacterial endocarditis or the presence of thrombus. Other studies have reported the presence of tricuspid vegetations that disappeared in subsequent echocardiographic evaluation in patients with negative blood cultures [56]. The presence of valve vegetations was also described in autopsy findings for SARS-CoV patients [57]. Pericardial effusion was also a common finding in the reports of patients with COVID-19; most of them were mild, with the minority of patients having signs of cardiac tamponade [10,12,13,17]. Cardiac tamponade has also been described in isolated reports, with a finding of bloody effusion during pericardiocentesis [58,59] and with the isolation of SARS-Cov-2 from pericardial fluid in one report [59].
Feasibility and Usefulness of Echocardiography in COVID-19 Patients
Echocardiographic protocols require the operators to stand close to the patients for prolonged periods, exposing them to droplets and increasing the risk of infection. Furthermore, the size of the echocardiographic equipment makes it troublesome to disinfect, increasing the risk of contamination. Since the beginning of the pandemic there have been concerns about the risk of performing echocardiograms and the need to carefully selecting patients who might benefit from echocardiography, to reduce the risk of personnel infection and increase the utility of examinations. The recommendations from echocardiography societies are to review the appropriateness of every procedure, favour the use of handheld devices that are easier to disinfect and to perform fast and focussed evaluations [7]. The American Society of Echocardiography (ASE) has provided a modified point-of-care ultrasound (POCUS) protocol for the echocardiographic evaluation of patients with suspected or confirmed COVID-19, which is likely to have an impact on patient management [8]. The adoption of protocols aimed at reducing the amount of inappropriate echocardiographic studies and guarantee that only beneficial examinations are performed have shown that the workflow in echocardiography laboratories has declined in >50% and that study appropriateness has significantly increased [60].
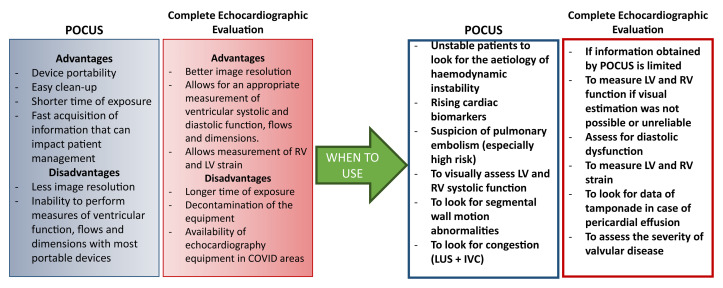
Some of the studies that have evaluated the echocardiographic abnormalities in COVID-19 have followed these recommendations, performed focussed examinations and used portable devices. Jain et al. found that an abbreviated echocardiogram protocol reduced the time of evaluation from 18 to 7 minutes. Overall, echocardiograms were considered non-diagnostic because of study quality in 5.6% of patients [12]. Other studies have demonstrated that the use of limited tablet-based echocardiograms can reduce the study time by 79% [61]. Dweck et al. demonstrated that echocardiographic evaluation had an immediate impact on the management of 33% of the patients [10], while Jain et al. reported a change in management in 16.7% [12]. It is uncertain whether POCUS will overcome a complete echocardiographic evaluation in patients with COVID-19 in terms of safety and effectiveness. POCUS has the advantage of being fast and, when used properly, it can give valuable information that can impact patient care; however, a complete echocardiogram is necessary for the accurate assessment of ventricular function, strain and other parameters that seem to have prognostic implications. Perhaps both methods are not superior to each other, but complementary (Figure 2 ). Given the important number of patients who will develop ARDS and the fact that some of them can benefit from the prone position, some reports have suggested that prone position echocardiography might be feasible, allowing RV and LV evaluation in a four-chamber view [62].
Figure 2.
POCUS vs complete echocardiographic evaluation: advantages, disadvantages and when to use.
Abbreviations: POCUS, point-of-care cardiac ultrasound; LV, left ventricle; RV, right ventricle; LUS, lung ultrasound; IVC, inferior vena cava.
Conclusions
The cardiovascular system has been affected in a significant number of patients during COVID-19. Given the high risk of personnel infection and equipment contamination during this pandemic, using focussed echocardiographic protocols and portable device echocardiograms is one of the most valuable tools for assessing patients with suspected CVD. The echocardiographic abnormalities described in the available reports are varied and there appear to be multiple mechanisms involved. Some reports have shown that biomarkers and clinical indications can help with correct selection of patients who are most likely to have echocardiographic alterations and can most benefit from the evaluation. In addition, some echocardiographic alterations appear to have prognostic implications for patients with COVID-19.
Funding Sources
None.
Conflicts of Interest
No conflict of interest to disclose.
All authors had full access to data and a role in the preparation of this manuscript.
Acknowledgements
We would like to thank Sergio Lozano-Rodríguez, M.D. for his assistance in the revision and editing of this manuscript.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.hlc.2021.02.004.
Appendices. Supplementary Data
References
- 1.WHO . 2020. Coronavirus disease (COVID-19) Weekly Epidemiological Update. [Google Scholar]
- 2.Wu Z., McGoogan J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323(13):1239–1242. doi: 10.1001/jama.2020.2648. [DOI] [PubMed] [Google Scholar]
- 3.Bavishi C., Bonow R.O., Trivedi V., Abbott J.D., Messerli F.H., Bhatt D.L. Acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog Cardiovasc Dis. 2020 doi: 10.1016/j.pcad.2020.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kang Y., Chen T. Cardiovascular manifestations and treatment considerations in Covid-19. Heart. 2020;106(15):1132–1141. doi: 10.1136/heartjnl-2020-317056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ruan Q., Yang K. Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China. Intensive Care Med. 2020;46(5):846–848. doi: 10.1007/s00134-020-05991-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cameli M., Pastore M.C. Usefulness of echocardiography to detect cardiac involvement in COVID-19 patients. Echocardiography. 2020;12 doi: 10.1111/echo.14779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirkpatrick J.N., Mitchell C., Taub C., Kort S., Hung J., Swaminathan M. ASE statement on protection of patients and echocardiography service providers during the 2019 novel coronavirus outbreak: endorsed by the American College of Cardiology. J Am Soc Echocardiogr. 2020;33(6):648–653. doi: 10.1016/j.echo.2020.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johri A.M., Galen B., Kirkpatrick J.N., Lanspa M., Mulvagh S., Thamman R. ASE statement on point-of-care ultrasound during the 2019 novel coronavirus pandemic. J Am Soc Echocardiogr. 2020;33:670–673. doi: 10.1016/j.echo.2020.04.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Agricola E., Beneduce A., Esposito A., Ingallina G., Palumbo D., Palmisano A., et al. Heart and lung multimodality imaging in COVID-19. JACC: Cardiovasc Imaging. 2020:3460. doi: 10.1016/j.jcmg.2020.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dweck M.R., Bularga A., Hahn R.T., Bing R., Lee K.K., Chapman A.R., et al. Global evaluation of echocardiography in patients with COVID-19. Eur Heart J Cardiovasc Imaging. 2020;21(9):949–958. doi: 10.1093/ehjci/jeaa178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Szekely Y., Lichter Y., Taieb P., Banai A., Hochstadt A., Merdler I., et al. Spectrum of Cardiac Manifestations in COVID-19 - a Systematic Echocardiographic Study. Circulation. 2020;142(4):342–353. doi: 10.1161/CIRCULATIONAHA.120.047971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jain S.S., Liu Q., Raikhelkar J., Fried J., Elias P., Poterucha T.J., et al. Indications for and findings on transthoracic echocardiogram in COVID-19. J Am Soc Echocardiogr. 2020;33(10):1278–1284. doi: 10.1016/j.echo.2020.06.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mahmoud-Elsayed H.M., Moody W.E., Bradlow W.M., Khan-Kheil A.M., Senior J., Hudsmith L.E., et al. Echocardiographic findings in patients with COVID-19 pneumonia. Can J Cardiol. 2020;36(8):1203–1207. doi: 10.1016/j.cjca.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Churchill T.W., Bertrand P.B., Bernard S., Namasivayam M., Churchill J., Crousillat D., et al. Echocardiographic features of COVID-19 illness and association with cardiac biomarkers. J Am Soc Echocardiogr. 2020 doi: 10.1016/j.echo.2020.05.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sud K., Vogel B., Bohra C., Garg V., Talebi S., Lerakis S., et al. Echocardiographic findings in patients with COVID-19 with significant myocardial injury. J Am Soc Echocardiogr. 2020 doi: 10.1016/j.echo.2020.05.030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.van den Heuvel F.M.A., Vos J.L., Koop Y., van Dijk A.P.J., Duijnhouwer A.L., de Mast Q., et al. Cardiac function in relation to myocardial injury in hospitalised patients with COVID-19. Neth Heart J. 2020;28(7-8):410–417. doi: 10.1007/s12471-020-01458-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rath D., Petersen-Uribe Á., Avdiu A., Witzel K., Jaeger P., Zdanyte M., et al. Impaired cardiac function is associated with mortality in patients with acute COVID-19 infection. Clin Res Cardiol. 2020:1–9. doi: 10.1007/s00392-020-01683-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo T., Fan Y., Chen M., Wu X., Zhang L., He T., et al. Cardiovascular implications of fatal outcomes of patients with Coronavirus disease 2019 (COVID-19) JAMA Cardiol. 2020;5(7):811–818. doi: 10.1001/jamacardio.2020.1017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi S., Qin M., Shen B., Cai Y., Liu T., Yang F., et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol. 2020;5(7):802–810. doi: 10.1001/jamacardio.2020.0950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Shi S., Qin M., Cai Y., Liu T., Shen B., Yang F., et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J. 2020;41:2070–2079. doi: 10.1093/eurheartj/ehaa408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhou Y., Fu B., Zheng X., Wang D., Zhao C., Qi Y., et al. Pathogenic T cells and inflammatory monocytes incite inflammatory storm in severe COVID-19 patients. Natl Sci Rev. 2020:nwaa041. doi: 10.1093/nsr/nwaa041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tisoncik J.R., Korth M.J., Simmons C.P., Farrar J., Martin T.R., Katze M.G. Into the eye of the cytokine storm. Microbiol Mol Biol Rev. 2012;76:16–32. doi: 10.1128/MMBR.05015-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Li D., Chen Y., Jia Y., Tong L., Tong J., Wang W., et al. SARS-CoV-2-induced immune dysregulation and myocardial injury risk in China: insights from the ERS-COVID-19 Study. Circ Res. 2020;127:397–399. doi: 10.1161/CIRCRESAHA.120.317070. [DOI] [PubMed] [Google Scholar]
- 24.Sato R., Nasu M. A review of sepsis-induced cardiomyopathy. J Intensive Care. 2015;3:48. doi: 10.1186/s40560-015-0112-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Orde S., Huang S.J., McLean A.S. Speckle tracking echocardiography in the critically ill: enticing research with minimal clinical practicality or the answer to non-invasive cardiac assessment? Anaesth Intensive Care. 2016;44:542–551. doi: 10.1177/0310057X1604400518. [DOI] [PubMed] [Google Scholar]
- 26.Baycan O.F., Barman H.A. Evaluation of biventricular function in patients with COVID-19 using speckle tracking echocardiography. Int J Cardiovasc Imaging. 2020:1–10. doi: 10.1007/s10554-020-01968-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stöbe S., Richter S., Seige M., Stehr S., Laufs U. Echocardiographic characteristics of patients with SARS-CoV-2 infection. Clin Res Cardiol. 2020:1–18. doi: 10.1007/s00392-020-01727-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Scally C., Abbas H., Ahearn T., Srinivasan J., Mezincescu A., Rudd A., et al. Myocardial and systemic inflammation in acute stress-induced (Takotsubo) cardiomyopathy. Circulation. 2019;139:1581–1592. doi: 10.1161/CIRCULATIONAHA.118.037975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Taza F., Zulty M., Kanwal A., Grove D. Takotsubo cardiomyopathy triggered by SARS-CoV-2 infection in a critically ill patient. BMJ Case Rep. 2020;13:e236561. doi: 10.1136/bcr-2020-236561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Meyer P., Degrauwe S., Van Delden C., Ghadri J.R., Templin C. Typical Takotsubo syndrome triggered by SARS-CoV-2 infection. Eur Heart J. 2020;41:1860. doi: 10.1093/eurheartj/ehaa306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pirzada A., Mokhtar A.T., Moeller A.D. COVID-19 and myocarditis: what do we know so far? CJC Open. 2020;2:278–285. doi: 10.1016/j.cjco.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nishiga M., Wang D.W., Han Y., Lewis D.B., Wu J.C. COVID-19 and cardiovascular disease: from basic mechanisms to clinical perspectives. Nat Rev Cardiol. 2020;17(9):543–558. doi: 10.1038/s41569-020-0413-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Oudit G.Y., Kassiri Z., Jiang C., Liu P.P., Poutanen S.M., Penninger J.M., et al. SARS-coronavirus modulation of myocardial ACE2 expression and inflammation in patients with SARS. Eur J Clin Investigat. 2009;39:618–625. doi: 10.1111/j.1365-2362.2009.02153.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bradley B.T., Maioli H., Johnston R., Chaudhry I., Fink S.L., Xu H., et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020;396(10247):320–332. doi: 10.1016/S0140-6736(20)31305-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wichmann D., Sperhake J.-P., Lütgehetmann M., Steurer S., Edler C., Heinemann A., et al. Autopsy findings and venous thromboembolism in patients with COVID-19. Ann Intern Med. 2020;173(4):268–277. doi: 10.7326/M20-2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schaller T., Hirschbühl K., Burkhardt K., Braun G., Trepel M., Märkl B., et al. Postmortem examination of patients with COVID-19. JAMA. 2020;323:2518–2520. doi: 10.1001/jama.2020.8907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Oxley T.J., Mocco J., Majidi S., Kellner C.P. Large-vessel stroke as a presenting feature of Covid-19 in the young. N Engl J Med. 2020;382(20):e60. doi: 10.1056/NEJMc2009787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Varga Z., Flammer A.J., Steiger P., Haberecker M., Andermatt R., Zinkernagel A.S., et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395:1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Warren-Gash C., Hayward A.C., Hemingway H., Denaxas S., Thomas S.L., Timmis A.D., et al. Influenza infection and risk of acute myocardial infarction in England and Wales: a CALIBER self-controlled case series study. J Infect Dis. 2012;206:1652–1659. doi: 10.1093/infdis/jis597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Stefanini G.G., Montorfano M., Trabattoni D., Andreini D., Ferrante G., Ancona M., et al. ST-elevation myocardial infarction in patients with COVID-19: clinical and angiographic outcomes. Circulation. 2020;141:2113–2116. doi: 10.1161/CIRCULATIONAHA.120.047525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Bangalore S., Sharma A., Slotwiner A., Yatskar L., Harari R., Shah B., et al. ST-segment elevation in patients with Covid-19 - a case series. N Engl J Med. 2020;382:2478–2480. doi: 10.1056/NEJMc2009020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Deng Q., Hu B., Zhang Y., Wang H., Zhou X., Hu W., et al. Suspected myocardial injury in patients with COVID-19: Evidence from front-line clinical observation in Wuhan, China. Int J Cardiol. 2020;311:116–121. doi: 10.1016/j.ijcard.2020.03.087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Berlin D.A., Gulick R.M. Severe Covid-19. N Engl J Med. 2020; May 15 doi: 10.1056/NEJMcp2009575. [DOI] [PubMed] [Google Scholar]
- 44.Park J.F., Banerjee S., Umar S. In the eye of the storm: the right ventricle in COVID-19. Pulm Circ. 2020;10(3) doi: 10.1177/2045894020936660. 2045894020936660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wu C., Chen X., Cai Y., Xia J.A., Zhou X., Xu S., et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180:1–11. doi: 10.1001/jamainternmed.2020.0994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zochios V., Parhar K., Tunnicliffe W., Roscoe A., Gao F. The right ventricle in ARDS. Chest. 2017;152:181–193. doi: 10.1016/j.chest.2017.02.019. [DOI] [PubMed] [Google Scholar]
- 47.Mekontso Dessap A., Boissier F., Charron C., Bégot E., Repessé X., Legras A., et al. Acute cor pulmonale during protective ventilation for acute respiratory distress syndrome: prevalence, predictors, and clinical impact. Intensive Care Med. 2016;42:862–870. doi: 10.1007/s00134-015-4141-2. [DOI] [PubMed] [Google Scholar]
- 48.Repessé X., Vieillard-Baron A. Right heart function during acute respiratory distress syndrome. Ann Transl Med. 2017;5:295. doi: 10.21037/atm.2017.06.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Vieillard-Baron A., Schmitt J.M., Augarde R., Fellahi J.L., Prin S., Page B., et al. Acute cor pulmonale in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implications, and prognosis. Crit Care Med. 2001;29:1551–1555. doi: 10.1097/00003246-200108000-00009. [DOI] [PubMed] [Google Scholar]
- 50.Guan W.J., Ni Z.Y., Hu Y., Liang W.H., Ou C.Q., He J.X., et al. Clinical characteristics of coronavirus disease 2019 in China. New Engl J Med. 2020;382:1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bompard F., Monnier H., Saab I., Tordjman M., Abdoul H., Fournier L., et al. Pulmonary embolism in patients with Covid-19 pneumonia. Eur Respiratory J. 2020:2001365. doi: 10.1183/13993003.01365-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Konstantinides S.V., Meyer G., Becattini C., Bueno H., Geersing G.J., Harjola V.P., et al. 2019 ESC Guidelines for the diagnosis and management of acute pulmonary embolism developed in collaboration with the European Respiratory Society (ERS) Eur Heart J. 2020;41:543–603. doi: 10.1093/eurheartj/ehz405. [DOI] [PubMed] [Google Scholar]
- 53.Sethi S.S., Zilinyi R., Green P., Eisenberger A., Brodie D., Agerstrand C., et al. Right ventricular clot in transit in COVID-19: implications for the pulmonary embolism response team. JACC Case Rep. 2020;2:1391–1396. doi: 10.1016/j.jaccas.2020.05.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Argulian E., Sud K., Vogel B., Bohra C., Garg V.P., Talebi S., et al. Right Ventricular dilation in hospitalized patients with COVID-19 Infection. JACC Cardiovasc Imaging. 2020;13(11):2459–2461. doi: 10.1016/j.jcmg.2020.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Li Y., Li H., Zhu S., Xie Y., Wang B., He L., et al. Prognostic value of right ventricular longitudinal strain in patients with COVID-19. JACC Cardiovasc Imaging. 2020;13(11):2287–2299. doi: 10.1016/j.jcmg.2020.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Vera-Pineda R., Carrizales-Sepulveda E.F., Camacho-Ortiz A., Nuzzolo-Shihadeh L., Cruz-Ramos F., Ordaz-Farias A., et al. Echocardiographic characteristics of subjects with COVID-19: a case series. Cardiol Res. 2020;11(4):260–265. doi: 10.14740/cr1084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Chong P.Y., Chui P., Ling A.E., Franks T.J., Tai D.Y., Leo Y.S., et al. Analysis of deaths during the severe acute respiratory syndrome (SARS) epidemic in Singapore: challenges in determining a SARS diagnosis. Arc Pathol Lab Med. 2004;128:195–204. doi: 10.5858/2004-128-195-AODDTS. [DOI] [PubMed] [Google Scholar]
- 58.Dabbagh M.F., Aurora L., D'Souza P., Weinmann A.J., Bhargava P., Basir M.B. Cardiac tamponade secondary to COVID-19. JACC Case Rep. 2020;2:1326–1330. doi: 10.1016/j.jaccas.2020.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Farina A., Uccello G., Spreafico M., Bassanelli G., Savonitto S. SARS-CoV-2 detection in the pericardial fluid of a patient with cardiac tamponade. Eur J Intern Med. 2020;76:100–101. doi: 10.1016/j.ejim.2020.04.045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ward R.P., Lee L., Ward T.J., Lang R.M. Utilization and appropriateness of transthoracic echocardiography in response to the COVID-19 pandemic. J Am Soc Echocardiogr. 2020;33:690–691. doi: 10.1016/j.echo.2020.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.McMahon S.R., De Francis G., Schwartz S., Duvall W.L., Arora B., Silverman D.I. Tablet-based limited echocardiography to reduce sonographer scan and decontamination time during the COVID-19 pandemic. J Am Soc Echocardiogr. 2020;33:895–899. doi: 10.1016/j.echo.2020.05.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Giustiniano E., Padua E., Negri K., Bragato R.M., Cecconi M. Echocardiography during prone-position mechanical ventilation in patients with COVID-19: a proposal for a new approach. J Am Soc Echocardiogr. 2020;33:905–906. doi: 10.1016/j.echo.2020.04.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.