Abstract
A large‐scale survey study was conducted to assess trauma, burnout, posttraumatic growth, and associated factors for nurses in the COVID‐19 pandemic. The Trauma Screening Questionnaire, Maslach Burnout Inventory, and Posttraumatic Growth Inventory‐Short Form were utilized. Factors associated with trauma, burnout, and posttraumatic growth were analysed using logistic and multiple regressions. In total, 12 596 completed the survey, and 52.3% worked in COVID‐19 designated hospitals. At the survey’s conclusion in April, 13.3% reported trauma (Trauma ≥ 6), there were moderate degrees of emotional exhaustion, and 4,949 (39.3%) experienced posttraumatic growth. Traumatic response and emotional exhaustion were greater among (i) women (odds ratio [OR]: 1.48, 95% CI 1.12–1.97 P = 0.006; emotional exhaustion OR: 1.30, 95% CI 1.09–1.54, P = 0.003), (ii) critical care units (OR: 1.20, 95% CI 1.06–1.35, P = 0.004; emotional exhaustion OR: 1.23, 95% CI 1.12–1.33, P < 0.001) (iii) COVID‐19 designated hospital (OR: 1.24, 95% CI 1.11–1.38; P < 0.001; emotional exhaustion OR: 1.26, 95% CI 1.17–1.36; P < 0.001) and (iv) COVID‐19‐related departments (OR: 1.16, 95% CI 1.04–1.29, P = 0.006, emotional exhaustion only). To date, this is the first large‐scale study to report the rates of trauma and burnout for nurses during the COVID‐19 pandemic. The study indicates that nurses who identified as women, working in ICUs, COVID‐19 designated hospitals, and departments involved with treating COVID‐19 patients had higher scores in mental health outcomes. Future research can focus on the factors the study has identified that could lead to more effective prevention and treatment strategies for adverse health outcomes and better use of resources to promote positive outcomes.
Keywords: COVID‐19 pandemic, mental health, nurses, psychological outcomes
Introduction
On 12 March 2020, the World Health Organization (WHO) declared coronavirus disease 2019 (COVID‐19) as a pandemic. Since then, millions of cases and thousands of deaths have been confirmed (World Health Organization 2020). The severity of the COVID‐19 pandemic is dire, but multiple organizations are reporting a parallel mental health pandemic in the making (Dzau et al. 2020). This large‐scale public health challenge has caused fear and physio‐psychological stress among nurses; effects are particularly severe due to anxieties with the unknown future of the disease (Spoorthy 2020). Multiple studies have revealed the psychological toll the virus has taken on healthcare providers. For example, more than 40% of healthcare personnel reported that they exhibited anxiety symptoms; more than 46% had reported depression, 32% reported insomnia, and 69% had high levels of stress (Huang et al. 2020; Lai et al. 2020; Lin et al. 2020). The WHO has reported that over 35 000 healthcare workers worldwide have been infected, and some have died because they provided care to patients with COVID‐19 (World Health Organization 2020). The United Nations Secretary‐General Antonio Guterres has called on governments across the world to focus on mental health services for their population, especially for front‐line workers (Guterres 2020).
Healthcare personnel, especially nurses, involved in COVID‐19 treatments are highly susceptible to adverse psychological outcomes, which may cause future difficulties if not diagnosed and treated appropriately (Kisely et al. 2020). Stuart’s stress adaptation model posits that coping responses are a continuum of maladaptive and adaptive responses (Stuart 2005). We hypothesize that there are additional maladaptive effects of working during the pandemic for healthcare providers. These effects include trauma exposure that could lead to posttraumatic stress disorder (PTSD), which includes sleeping, eating, and social disruptions, nightmares, and sometimes flashbacks, and burnout, including exhaustion, frustration, anger, and depression (Tominaga et al. 2019).
However, not all people who experience the pandemic have maladaptive responses. In addition to these negative outcomes, traumatic work‐related events may change individuals positively in a process known as posttraumatic growth. By saving lives and improving patient outcomes, healthcare personnel can also develop posttraumatic growth. Studies on medical rescue personnel have indicated that resilience, active coping strategies, planning, religion, seeking emotional and instrumental support, and self‐distraction abilities are positively associated with posttraumatic growth (Ogińska‐Bulik 2014; Ogińska‐Bulik & Zadworna‐Cieślak 2018).
Background
Trauma
According to the Crisis and Trauma Resource Institute (2017), ‘trauma is a wound that injures us emotionally, psychologically and physiologically’. (p. 1) (Crisis & Trauma Resource Institute 2017). The Diagnostic and Statistical Manual of Mental Disorders 5th edition (DSM 5) from the American Psychiatric Association (APA) defines trauma as ‘exposure to death, threatened death, actual or threatened serious injury, or actual or threatened sexual violence’ (APA 2013). Many people are not aware that pandemics are classified as a disaster. According to the United Nations Office for Disaster Risk Reduction (UNDRR), disaster is defined as a serious disruption of the functioning of a community or a society causing widespread human, material, economic, or environmental losses which exceed the ability of the affected community or society to cope using its own resources (UNDRR 2020). The Center for Research on the Epidemiology of Disasters (CRED) part of WHO’s Global Program for Emergency Preparedness and Response further divides disaster into 5 subgroups as: geophysical (e.g. earthquake); meteorological (e.g. storm); hydrological (e.g. flood); climatological (e.g. heatwave); and biological (e.g. epidemic)(Vos et al. 2010). DeWolfe’s description of the population exposure model shows that those who have the most exposure are the ones who are most affected by the disaster (DeWolfe 2004), whereas the population exposure model had five concentric circles going from those who are affected directly and harmed to those in the community‐at‐large. For the COVID‐19 pandemic, this concentric model can be categorized into three groups, as suggested by Xiao et al. (2020). The innermost circle contains those who are directly experiencing symptoms and traumatic treatments (dyspnoea, respiratory failure, tracheotomy). The next larger middle circle are those who are witnessing the suffering of the patients, including the other patients, family members, people who provide care and aid for the patients. The largest circle would be those experiencing realistic or unrealistic fear of infection, social isolation, financial hardships, or the community‐at‐large (Xiao et al. 2020). In the DSM 5, secondary or vicarious trauma experienced by medical professionals are part of the diagnostic criteria (APA 2013). A meta‐analysis by Hensel et al. (2015) revealed that caseload characteristics (i.e. high case volume or clinical concerns involving death or potential harm) were risk factors for traumatic stress among healthcare personnel (Hensel et al. 2015).
Epidemiological studies have demonstrated that approximately 8%–12% of people who experience a traumatic event such as those caused by a disaster develop PTSD, a common mental disorder characterized by the symptom clusters of re‐experiencing the traumatic event, negative cognitions and mood, arousal, and avoidance (Friedman et al. 2015). Definitions and criteria for PTSD diagnosis have evolved with subsequent editions of the Diagnostic and Statistical Manual of Mental Disorders (DSM) and World Health Organization’s International Classification of Diseases (ICD) with some divergence in both (Stein et al. 2014).
Burnout
Burnout is a psychological syndrome involving emotional exhaustion, depersonalization, and a feeling of reduced personal accomplishment, particularly regarding an individual’s work with clients. Emotional exhaustion refers to feeling overwhelmed. Depersonalization involves detached and impersonal feelings that seem unreal or not belonging to oneself. A lack of personal accomplishment refers to feelings of reduced self‐achievement and competence at work (Maslach et al. 1986). The consequences of burnout are dangerous to nurses, patients, and healthcare institutions. Burnout can degrade the quality of care or service provided by the nursing staff. A study on personnel caring for dengue fever revealed that 2.5%–11.7% of healthcare personnel experienced severe work burnout (Boo et al. 2018). In addition to stress caused by uncertainty and fear of the unknown, numerous studies have demonstrated that organizational support for healthcare personnel was negatively correlated with their work satisfaction, emotional response, and hostility and conflict (Marjanovic et al. 2007; Niu et al. 2019; Siu 2002). Work environment is a key factor influencing the psychological health of healthcare personnel (Sigsbee & Bernat 2014). The provision of sufficient personal protection equipment, instituting prevention policies, and a balanced workload may determine changes in work pressure among healthcare personnel (Tolomiczenko et al. 2005).
Posttraumatic growth
Posttraumatic growth entails ‘positive psychological change experienced as a result of the struggle with highly challenging life circumstances’. (Tedeschi & Calhoun 2004). Such struggles may enable individuals to identify meaning in interpersonal relationships, have a greater sense of personal strength, change their priorities, have increased appreciation for small life events, and have a richer existential or spiritual life (Tominaga et al. 2019). Personality dynamics and trauma characteristics can lead to posttraumatic growth and spirituality; moreover, social support and opportunities for emotional disclosure can buffer against mental illness and stress response (Shuwiekh et al. 2018). However, there is still uncertainty at which point after disasters or other highly challenging life circumstances, posttraumatic growth occurs as the concept is highly complex and can vary due to an individual’s circumstances, demographics, and personality traits (Collier 2016).
To our knowledge, no study has yet reported trauma, burnout, and posttraumatic growth among health personnel in the midst of the COVID‐19 pandemic, and little is known about these adaptive and maladaptive consequences amidst a pandemic. Therefore, this study assessed the occurrence of trauma, burnout, and growth among nurses involved in the COVID‐19 pandemic and the associated factors with the outcomes. Understanding the psychological sequelae of involvement in pandemic response is crucial. This can improve training and post‐pandemic interventions that may reduce the likelihood of adverse responses in front‐line workers and prevent a parallel pandemic.
Methods
A cross‐sectional large‐scale survey study was conducted using self‐report questionnaires completed online and in paper and pencil forms by nurses. The questionnaire collected data on the trauma, burnout, growth, and relevant influential factors experienced by nurses treating patients with COVID‐19. To better engaged our sampling frame of nurses, recruitment was done via specialized groups in the WeChat app and hospitals through paper surveys. The data collection period was in April 2020. Completion of the survey was completely voluntary, and confidentiality was assured. The formula for sample size N = Z 1−α/2 2 p(1 − p)/ d 2 was used where Z 1−α/2 = 1.96 (at 5% type 1 error P < 0.05), and the estimated acceptable margin of error for proportion d was 0.05; and p was based on a similar previous study on the SARS outbreak, where the actual number of those traumatized was not more than 35% (Maunder 2004). A study size of 350 was calculated from this formula. To address response bias such as social desirability, the confidential paper, and online survey form were used, which has been shown to decrease response bias (Tourangeau 2014). Online and confidential paper and pencil survey collection methods tend to offer anonymity favoured by participants and not adversely impacted by repeat or nonserious responders (Gosling et al. 2004).
Measurement tools
The demographic survey section collected variables of individual characteristics, trauma variables with the Trauma Screening Questionnaire (TSQ), burnout variables by Maslach Burnout Inventory‐General Survey (MBI‐GS), and personal growth variables with the Posttraumatic Growth Inventory‐Short Form (PTGI‐SF).
Demographic information
The demographic information survey was self‐designed based on a literature review on previous research on mental health outcomes for nurses. The study included age, sex, education level, tenure, affiliated department, and whether the participant had provided care for patients with COVID‐19.
Trauma Screening Questionnaire
Screening for trauma used the 10‐item trauma screening questionnaire. Individuals who have experienced traumatic events are asked whether they have exhibited traumatic symptoms at least twice within the past week. Participants are evaluated on the basis of their item responses (yes: 1 point; no: 0 point). Participants with scores of at least 6 may have trauma that could lead to PTSD. The questionnaire used in this study included two additional scales to measure re‐experiencing an event and arousal. Items in each scale were scored between 0 and 5; higher scores indicated more severe symptoms. Studies have demonstrated that the sensitivity, specificity, negative predictive, and positive predictive values as 0.85, 0.89, 0.98, and 0.48, respectively (Mouthaan et al. 2014; Walters et al. 2007).
Maslach Burnout Inventory‐General Survey
There are three dimensions in the Maslach burnout inventory, emotional exhaustion, depersonalization, and lack of personal accomplishment. The 22 items are scored between 0 and 6; the composite score of each scale represents a participant’s total score for each dimension. Participants with scores of 0–18, 19–26, and ≥27 in the emotional exhaustion scale exhibit low, moderate, and high levels of emotional exhaustion, respectively. Those scoring 0–5, 6–9, and >9 in the depersonalization dimension have low, moderate, and high levels of depersonalization, respectively. Items in the dimension measuring lack of personal accomplishment are reverse coded; participants with scores of 0–33, 34–39, and ≥40 exhibit a low, moderate, and high degree of lack of personal achievement, respectively. The internal consistency reliability for the burnout subscales is 0.90 for emotional exhaustion, 0.79 for depersonalization, and 0.71 for lack of personal accomplishment. The internal consistency, retest reliability, construct validity, and concept validity of the tool has been verified in numerous occupations, languages, and countries (Aguayo et al. 2011; Naude & Rothmann 2004).
Posttraumatic Growth Inventory‐Short Form
The Posttraumatic Growth Inventory‐Short Form measures the degree of positive change experienced in the aftermath of a traumatic event (Tedeschi & Calhoun 2004). The inventory consists of 21 items. Based on the dimensional structure of the inventory, numerous scholars have conducted a confirmatory factor analysis to revise the inventory into the 10‐item Posttraumatic Growth Inventory‐Short Form. Questions use a 6‐point Likert scale (1: no change to 6: a high degree of change). Scores at the 60th percentile or higher (≥32) indicate probable personal growth (Yu et al. 2010). The internal consistency coefficient of the tool is 0.89 (Taku et al. 2012). The five subscales are (1) relating to others, (2) new possibilities, (3) personal strength, (4) spiritual change, and (5) appreciation of life. Higher scores indicate greater degrees of change. According to Yu et al. (2010), participants with total scores higher than the 60th percentile have probable personal growth. There is excellent internal and test–retest reliability in both Western (Tedeschi & Calhoun 1996) and Asian samples (Solomon & Dekel 2007).
Statistical analyses
After retrieving the questionnaires, the researchers used SPSS software version 22.0 (IBM corp) for data archiving and analyses. Complete case analysis was utilized, and cases with missing outcomes were excluded. The sample characteristics were examined by descriptive analysis. Bivariate chi‐square analyses were then performed to identify associated factors. In addition, logistic and multiple linear regressions were performed to identify factors relevant to trauma, burnout, and posttraumatic growth. The variables included in the analysis are listed in the results section. In this study, all tests were two‐tailed, and alpha value of P < 0.05 indicated statistical significance.
Ethical approval
The inclusion criteria for the survey were nurses over the age of 18, who worked in hospitals in mainland China and Taiwan. Ethical approval from the ethics committee of Beijing Hospital (Approval No. 2020BJYYEC‐098‐02) and the Joint Institutional Review Board of Taipei Medical University (Approval No. N202003066) was obtained. Following ethical guidelines, informed consent was obtained from each participant after the researchers clearly described the research and explained the objectives (Lavrakas 2008; Loue 2002). Participants’ identities were anonymous, and they could withdraw from the survey at any time without providing justification. Confidentiality and privacy are additionally ensured through secure data transfers and storage.
Results
Participants characteristics
A total of 12 596 nurses were recruited, and their average age and years of experience were 33.1 and 10.4 years. A majority of participants were women (95.6%) and had a college‐level or higher education (76.5%). Of the participants, 3577 (28.4%) worked in critical care units, 660 (5.2%), 419 (3.3%), 208 (1.7%), and 702 (5.6%) worked in intensive care, pulmonary medicine, infectious disease, and emergency departments. A total of 6,585 (52.3%) were affiliated with hospitals designated for COVID‐19 treatment, and 900 (7.1%) had provided care for patients with COVID‐19. Each healthcare worker cared for an average of 1.6 patients with COVID‐19, and 247 (2.0%) personnel had cared for patients who died because of the virus (Table 1).
Table 1.
Descriptive statistics of participants (N = 12 596)
| Variables | N | % | P value |
|---|---|---|---|
| Gender | <0.001 | ||
| Male | 555 | 4.4 | |
| Female | 12 041 | 95.6 | |
| Mean | SD | ||
| Age (years)/ mean (SD) | 33.1 | 7.5 | |
| N | % | ||
| Education | <0.001 | ||
| Graduate school and above | 89 | 0.7% | |
| College or University | 9632 | 76.5 | |
| Vocational high school | 2710 | 21.5 | |
| Senior high school | 165 | 1.3 | |
| Hospital level | <0.001 | ||
| Medical centre (level 3) | 10 537 | 83.7 | |
| Regional hospital (level 2) | 1981 | 15.7 | |
| District hospital (level 1) | 78 | 0.6 | |
| Mean | SD | ||
| Tenure | 10.4 | 8.1 | |
| N | % | ||
| Department | <0.001 | ||
| ICU | 660 | 5.2 | |
| Pulmonary medicine | 419 | 3.3 | |
| Infectious disease | 208 | 1.7 | |
| ER | 702 | 5.6 | |
| Others | 10 594 | 84.2 | |
| Worked in critical care units | <0.001 | ||
| Yes | 3577 | 28.4 | |
| No | 9019 | 71.6 | |
| Worked in a COVID‐19‐designated hospital | <0.001 | ||
| Yes | 6585 | 52.3 | |
| No | 6011 | 47.7 | |
| Performed front‐line tasks for disease prevention | <0.001 | ||
| Yes | 4701 | 36.5 | |
| No | 8173 | 63.5 | |
| Provided care for patients with COVID‐19 | <0.001 | ||
| Yes | 900 | 7.1 | |
| No | 11 696 | 92.9 | |
| Mean | SD | ||
| Number of patients with COVID‐19 cared for | 1.6 | 15.3 | |
| N | % | ||
| Cared for patients with COVID‐19 who died | <0.001 | ||
| Yes | 247 | 2.0 | |
| No | 12 349 | 98.0 | |
| Mean | SD | ||
| Number of patients with COVID‐19 who died | 0.06 | 0.8 | |
| N | % | ||
| Loss of family members | <0.001 | ||
| Most | 24 | 0.2 | |
| Some | 562 | 4.5 | |
| None | 12 010 | 95.3 | |
| Financial loss | <0.001 | ||
| Considerable | 199 | 1.6 | |
| Some | 2666 | 21.2 | |
| None | 9731 | 77.2 | |
| Societal resource loss | <0.001 | ||
| Considerable | 99 | 0.8 | |
| Some | 2209 | 17.5 | |
| None | 10 288 | 81.7 | |
| TSQ ≥ 6 | <0.001 | ||
| Yes | 1681 | 13.3 | |
| No | 10 915 | 86.7 | |
| PTGI‐SF (Tedeschi & Calhoun 1996) ‡ | <0.001 | ||
| ≧60th percentile | 4949 | 39.3 | |
| <60th percentile | 7647 | 60.7 |
PTGI‐SF, Post Traumatic Growth Inventory‐Short Form; TSQ, Trauma Screening Questionnaire.
The cut‐off point for total PTGI‐SF scores was the 60th percentile to divide the population into groups with scores equal to or higher than the 60th percentile (≧32 points) and less than the 60th percentile (< 32 points).
Trauma reaction
The average trauma screening questionnaire score was 2.1 ± 2.6. The most common reactions that occurred because of COVID‐19 were the following: 34.8% of participants experienced difficulties sleeping or had poor sleep quality, 33.9% continually believed that a similar disaster would occur in the future, 28.1% became particularly nervous or frightened during unexpected events, and 27.6% exhibited symptoms of irritation or were angered easily. Furthermore, 24.6% of participants experienced unhappy thoughts or memories related to their experiences with the epidemic despite deliberately attempting to avoid them. In the subscales, the participants’ average re‐experience and arousal scores were 0.9 ± 1.2 and 1.3 ± 1.5, respectively. Higher arousal and re‐experience scores were observed among participants who were women, worked in intensive care departments, worked in a COVID‐19 designated hospital, worked in departments related to COVID‐19 treatment (i.e. intensive care, pulmonary medicine, infectious disease, and emergency departments), cared for patients with COVID‐19, and cared for patients who had died because of COVID‐19 (Table 2).
Table 2.
Descriptive and advanced statistical analysis of TSQ, MBI, and PTGI‐SF scale and subscale scores
| Trauma Screening Questionnaire (TSQ) | Maslach Burnout Inventory (MBI) | Posttraumatic Growth Inventory‐Short Form (PTGI‐SF) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total | Re‐experience | Arousal | Emotional exhaustion | Depersonalization | Lack of personal accomplishment | Total | Relating to others | New possibilities | Personal strength | Spiritual change | Appreciation of life | |
| Total | 2.1 (2.6) | 0.9 (1.2) | 1.3 (1.5) | 19.1 (10.0) | 5.5 (4.6) | 19.0 (8.4) | 28.0 (11.5) | 6.1 (2.7) | 5.8 (2.7) | 6.0 (2.7) | 4.4 (2.7) | 5.7 (2.5) |
| Gender | ||||||||||||
| Female | 2.2 (2.4)*** | 0.9 (1.2)*** | 1.3 (1.5)*** | 19.2 (10.0)* | 5.5 (4.5) | 19.1 (8.3) | 28.0 (11.4) | 6.1 (2.7) | 5.8 (2.7) | 6.0 (2.7) | 4.5 (2.7) | 5.7 (2.5) |
| Male | 1.7 (2.6) | 0.7 (1.1) | 1.0 (1.4) | 17.9 (10.9) | 5.9 (5.3) | 18.9 (9.6) | 27.8 (12.2) | 6.0 (2.9) | 5.9 (2.8) | 6.0 (2.8) | 4.2 (2.8) | 5.7 (2.7) |
| Worked in critical care units | ||||||||||||
| Yes | 2.4 (2.7)*** | 0.9 (1.3)*** | 1.4 (1.6)*** | 20.1 (10.3)*** | 5.9*** (4.9) | 19.0 (8.3) | 28.4 (11.4)* | 6.2 (2.7) | 5.9 (2.7)** | 6.1 (2.7)** | 4.5 (2.7)* | 5.8 (2.5)* |
| No | 2.1 (2.5) | 0.8 (1.2) | 1.3 (1.5) | 18.7 (9.9) | 5.4 (4.5) | 19.1 (8.4) | 27.8 (11.4) | 6.1 (2.7) | 5.7 (2.7) | 5.9 (2.7) | 4.4 (2.7) | 5.7 (2.5) |
| Worked in a COVID‐19‐related department | ||||||||||||
| Yes | 2.4 (2.7)*** | 0.9 (1.3)** | 1.4 (1.6)*** | 20.1 (10.0)*** | 6.1 (4.9)*** | 19.4 (8.3)* | 28.2 (11.6) | 6.1 (2.7) | 5.8 (2.7) | 6.1 (2.7) | 4.5 (2.7) | 5.8 (2.5) |
| No | 2.1 (2.6) | 0.8 (1.2) | 1.3 (1.5) | 18.9 (10.0) | 5.4 (4.5) | 19.0 (8.4) | 28.0 (11.4) | 6.1 (2.7) | 5.8 (2.7) | 6.0 (2.7) | 4.4 (2.7) | 5.7 (2.5) |
| Cared for patients with COVID‐19 | ||||||||||||
| Yes | 2.4 (2.6)*** | 1.0 (1.3)* | 1.5 (1.5)*** | 18.7 (9.5) | 5.2 (4.4)* | 17.6 (8.2)*** | 30.0 (11.2)*** | 6.5 (2.7)*** | 6.2 (2.6)*** | 6.5 (2.6)*** | 4.7 (2.7)* | 6.1 (2.4)*** |
| No | 2.1 (2.6) | 0.9 (1.2) | 1.3 (1.5) | 19.1 (10.1) | 5.6 (4.6) | 19.2 (8.4) | 27.8 (11.4) | 6.1 (2.7) | 5.7 (2.7) | 5.9 (2.7) | 4.4 (2.7) | 5.7 (2.5) |
| Cared for patients with COVID‐19 who died | ||||||||||||
| Yes | 2.6 (2.7)* | 1.1 (1.4)* | 1.5 (1.5)* | 18.6 (8.8) | 5.6 (4.6) | 18.3 (8.0) | 29.2 (10.4) | 6.4 (2.5) | 5.9 (2.4) | 6.4 (2.4)** | 4.5 (2.6) | 6.0 (2.3)* |
| No | 2.1 (2.6) | 0.9 (1.2) | 1.3 (1.5) | 19.1 (10.1) | 5.5 (4.6) | 19.1 (8.4) | 28.0 (11.5) | 6.1 (2.7) | 5.8 (2.7) | 6.0 (2.7) | 4.4 (2.7) | 5.7 (2.5) |
| Worked in a COVID‐19‐designated hospital | ||||||||||||
| Yes | 2.2 (2.6)*** | 0.9 (1.2)** | 1.3 (1.5)*** | 19.2(9.9) | 5.6(4.6) | 18.9 (8.3)* | 28.4 (11.5)** | 6.2 (2.7)** | 5.8 (2.7)** | 6.1 (2.7)*** | 4.5 (2.7)* | 5.8 (2.5)* |
| No | 2.1(2.5) | 0.8(1.2) | 1.2 (1.5) | 19.0(10.1) | 5.5(4.6) | 19.2(8.5) | 27.7(11.4) | 6.1(2.7) | 5.7(2.7) | 5.9(2.7) | 4.4(2.7) | 5.6(2.5) |
MBI, Maslach Burnout Inventory; PTGI‐SF, Post Traumatic Growth Inventory‐Short Form; TSQ, Trauma Screening Questionnaire.
Mean scores, Standard Deviations.
P < 0.05.
P < 0.01.
P < 0.001.
Participants were divided into two groups based on the 6‐point cut‐off. After sustaining the effects of COVID‐19, 13.3% of participants may have had traumatic responses (TSQ ≥ 6). Chi‐square analysis indicated that the proportion of nurses with traumatic responses was significantly higher for women (Women: 13.5%; Men: 10.1%), those who worked in critical care units (Yes: 15.2%; No: 12.6%), those who worked in departments related to COVID‐19 (Yes: 15.5%, No: 12.9%), and those who cared for patients with COVID‐19 (Yes: 15.2%; No: 13.2%) (Table 3).
Table 3.
Chi‐square test of variables influencing COVID‐19 effects on nurses
| Variables | TSQ | MBI | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Emotional exhaustion | Depersonalization | Lack of personal accomplishment | |||||||||||||
| <6 | ≧6 | P | Low | Moderate | High | P | Low | Moderate | High | P | Low | Moderate | High | P | |
| Gender | .021 * | .044 * | .024 * | <0.001 *** | |||||||||||
| Female | 10416 (86.5) | 1625 (13.5) | 6230 (51.7) | 3217 (26.7 a ) | 2594 (21.5) | 6921 (57.5) | 2965(24.6) | 2155 (17.9 a ) | 11635 (96.6 a ) | 278 (2.3) | 128 (1.1 a ) | ||||
| Male | 499 (89.9) | 56 (10.1) | 315 (56.8) | 125 (22.5) | 115 (20.7) | 308 (55.5) | 123 (22.2) | 124 (22.3) | 521 (93.9) | 17 (3.1) | 17 (3.1) | ||||
| Worked in critical care units | <0.001 *** | <0.001 *** | <0.001 *** | .367 | |||||||||||
| Yes | 3034 (84.8) | 543 (15.2) | 1710 (47.8 a ) | 983 (27.5) | 884 (24.7 a ) | 1933 (54.0 a ) | 888 (24.8) | 756 (21.1 a ) | 3465 (96.9) | 75 (2.1) | 38 (1.1) | ||||
| No | 7881 (87.4) | 1138(12.6) | 4835 (53.6) | 2359 (26.2) | 1825 (20.2) | 5296 (58.7) | 2200 (24.4) | 1523 (16.9) | 8691 (96.4) | 221 (2.5) | 107 (1.2) | ||||
| Worked in COVID‐19‐related departments | .002 ** | <0.001 *** | <0.001 *** | .309 | |||||||||||
| Yes | 1681 (84.5) | 308 (15.5) | 943(47.4 a ) | 578 (29.1 a ) | 468 (23.5 a ) | 1045 (52.5 a ) | 493 (24.8) | 406 (22.7 a ) | 1923 (96.7) | 39 (2.0) | 27 (1.4) | ||||
| No | 9234 (87.1) | 1373 (12.9) | 5620 (52.8) | 2764 (26.1) | 2241 (21.1) | 6184 (58.3) | 2595 (24.6) | 1828 (17.1) | 10233 (96.5) | 256 (2.4) | 118 (1.1) | ||||
| Cared for patients with COVID‐19 | .091 | .286 | .273 | .037 * | |||||||||||
| Yes | 763 (84.8) | 137 (15.2) | 483 (53.7) | 242 (26.9) | 175 (19.4) | 535 (59.4) | 219 (24.3) | 146 (16.2 a ) | 882 (98.0 a ) | 11(1.2 a ) | 7 (0.8) | ||||
| No | 10152 (86.8) | 1544 (13.2) | 6062 (51.8) | 3100 (26.5) | 2534 (21.7) | 6694 (57.2) | 2869 (24.5) | 2133 (18.2) | 11274 (96.4) | 284 (2.4) | 138 (1.2) | ||||
| Cared for patients with COVID‐19 who died | .068 | .272 | .337 | .495 | |||||||||||
| Yes | 204 (82.6) | 43 (17.4) | 133 (53.8) | 71 (28.7) | 43 (17.4 a ) | 144 (58.3) | 52 (21.1) | 51 (20.6) | 241 (97.6) | 3 (1.2) | 3 (1.2) | ||||
| No | 10711 (86.7) | 1638 (13.3) | 6412 (51.9) | 3271 (26.5) | 2666 (21.6) | 7085 (57.4) | 3036 (24.6) | 2228 (18.0) | 11915 (96.5) | 292 (2.4) | 142 (1.2) | ||||
| Worked in a COVID‐19‐designated hospital | .169 | .140 | .765 | .019 * | |||||||||||
| Yes | 5680(86.3) | 905(13.7) | 3378(51.3) | 1795(27.3) | 1412(21.4) | 3759(57.1) | 1627(24.7) | 1199(18.2) | 6382(96.9) | 141(2.1 a ) | 62(0.9) | ||||
| No | 5235(87.1) | 776(12.9) | 3167(52.7) | 1547(25.7) | 1297(21.6) | 3470(57.7) | 1461(24.3) | 1080(18.0) | 5774(96.1) | 154(2.6) | 83(1.4) | ||||
MBI, Maslach Burnout Inventory; TSQ, Trauma Screening Questionnaire.
Post hoc significance.
Data are n (%).
P < 0.05.
P < 0.01.
P < 0.001.
Burnout
The average scores of burnout for each of the three subscales were in the low‐to‐moderate range. The average emotional exhaustion score was 19.1 ± 10.0, indicating a moderate degree of emotional exhaustion. Women and personnel who worked in critical care units or departments related to COVID‐19 had significantly higher levels of emotional exhaustion (P < 0.001) (Table 2). Furthermore, the proportion of nurses with high levels of emotional exhaustion was significantly higher among those who worked in critical care units (Yes: 24.7%; No: 20.2%) and in departments related to COVID‐19 (Yes: 23.5%; No: 21.1%) (Table 3).
The average depersonalization score was 5.5 ± 4.6, indicating that participants experienced a moderate level of depersonalization. However, those who worked in critical care units or departments relate to COVID‐19 had significantly higher depersonalization scores (P < 0.001) (Table 2). The proportion of participants who experienced high levels of depersonalization was significantly higher for men (Women: 17.9%; Men: 22.3%) and those who worked in critical care units (Yes: 21.1%; No: 16.9%) and departments related to COVID‐19 (Yes: 22.7%; No: 17.1%) (Table 3).
The average score in lack of personal accomplishment score was 19.0 ± 8.4, indicating that the participants experienced a lack of personal accomplishment to a small degree (Table 2). Regardless of gender identification or whether they had cared for patients with COVID‐19 (Yes: 98.0%; No: 96.4%), the participants collectively scored low on lack of personal accomplishment (Table 3). This result indicated that the effects of COVID‐19 did not decrease the level of personal accomplishment for nurses.
Posttraumatic growth
Average posttraumatic growth score was 28.0 ± 11.5, and participants with scores at the 60th percentile or higher demonstrated personal growth due to the effects of COVID‐19. A total of 39.3% of nurses scored at the 60th percentile or higher (≥32 points).
Analysis of average scores in the five subscales was as follows: (i) relating to others (6.1 ± 2.7), (ii) new possibilities (5.8 ± 2.7), (iii) personal strength (6.0 ± 2.7), (iv) spiritual change (4.4 ± 2.7), and (v) appreciation of life (5.7 ± 2.5). Participants who had provided care in critical care units, or worked at a COVID‐19 designated hospital, or cared for patients with COVID‐19 had significantly higher total and subscale scores than those who did not serve in these hospitals, departments or provide care for patients with COVID‐19 (P < 0.05) (Table 2).
Factors associated with trauma, burnout, and posttraumatic growth among nurses
A logistic regression analysis was conducted to determine whether gender, working in critical care units, working in departments related to COVID‐19 (i.e. intensive care, pulmonary medicine, infectious disease, and emergency departments), providing care for patients with COVID‐19, and providing care for patients who died because of COVID‐19 were associated factors with respect to trauma (Fig. 1). Being a woman (odds ratio [OR]: 1.48, 95% CI 1.12–1.97; P = 0.006), working in a COVID‐19 designated hospital (OR: 1.24, 95% CI 1.11–1.38; P < 0.001), or working in critical care units (OR: 1.20, 95% CI 1.06–1.35; P = 0.004) were influential factors (Table 4). In the multiple linear regression analysis, tenure, PTGI score, emotional exhaustion, depersonalization, and lack of personal accomplishment were influential factors relating to trauma. Specifically, emotional exhaustion in the burnout dimension was the most influential factor and exhibited the highest explanatory variance (adjusted R 2 = 26%, P < 0.001) (Table 5).
Fig. 1.
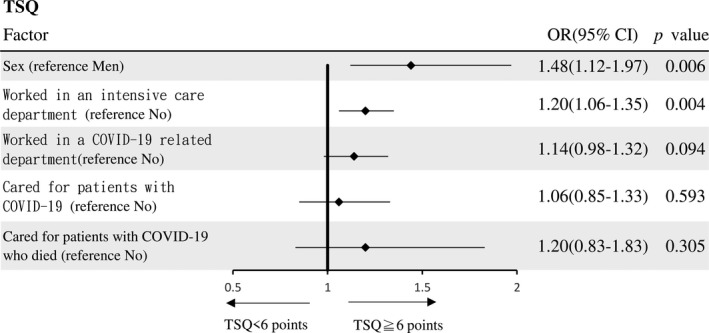
Logistic regression of TSQ by displacement status.
Table 4.
Logistic regression of influential factors of COVID‐19's effects on nurses
| Variables | TSQ (Walters et al. 2007) † | MBI‐GS (Naude & Rothmann 2004) ‡ | PTGI‐SF (Tedeschi & Calhoun 1996) § | ||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Emotional Exhaustion | Depersonalization | Lack of Personal Accomplishment | |||||||||||||||||||||||
| B | SE | OR | 95% CI | P | B | SE | OR | 95% CI | P | B | SE | OR | 95% CI | P | B | SE | OR | 95% CI | P | B | SE | OR | 95% CI | P | |
| Gender | |||||||||||||||||||||||||
| Male | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||||||||||||
| Female | 0.39 | 0.14 | 1.48 | 1.12–1.97 | 0.006 | 0.26 | 0.09 | 1.30 | 1.09–1.54 | 0.003 ** | −0.03 | 0.08 | 0.97 | 0.82–1.15 | 0.736 | −0.67 | 0.19 | 0.51 | 0.36–0.74 | <0.001 *** | −0.15 | 0.09 | 0.99 | 0.83–1.17 | 0.863 |
| Worked in critical care units | |||||||||||||||||||||||||
| vNo | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||||||||||||
| Yes | 0.18 | 0.06 | 1.20 | 1.06–1.35 | 0.004 ** | 0.20 | 0.04 | 1.23 | 1.12–1.33 | <0.001 *** | 0.14 | 0.04 | 1.15 | 1.06–1.25 | 0.001 *** | −0.17 | 0.12 | 0.84 | 0.67–1.07 | 0.160 | 0.04 | 0.04 | 1.04 | 0.96–1.14 | 0.352 |
| Worked in a COVID‐19‐related department | |||||||||||||||||||||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||||||||||||
| Yes | 0.13 | 0.08 | 1.14 | 0.98–1.32 | 0.094 | 0.15 | 0.05 | 1.16 | 1.04–1.29 | 0.006 ** | 0.18 | 0.05 | 1.20 | 1.08–1.33 | 0.001 *** | 0.02 | 0.15 | 1.02 | 0.76–1.37 | 0.887 | −0.07 | 0.06 | 0.93 | 0.84–1.04 | 0.219 |
| Cared for patients with COVID‐19 | |||||||||||||||||||||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||||||||||||
| Yes | 0.06 | 0.12 | 1.06 | 0.85–1.33 | 0.593 | −0.12 | 0.08 | 0.89 | 0.76–1.04 | 0.144 | −0.16 | 0.08 | 0.85 | 0.72–0.99 | 0.048 * | −0.70 | 0.30 | 0.50 | 0.28–0.89 | 0.019 * | 0.40 | 0.08 | 1.49 | 1.27–1.75 | <0.001 *** |
| Cared for patients with COVID‐19 who died | |||||||||||||||||||||||||
| No | Ref. | Ref. | Ref. | Ref. | |||||||||||||||||||||
| Yes | 0.21 | 0.20 | 1.23 | 0.83–1.83 | 0.305 | −0.03 | 0.15 | 0.82 | 0.72–1.30 | 0.820 | 0.04 | 0.15 | 1.04 | 0.77–1.40 | 0.790 | 0.29 | 0.51 | 1.33 | 0.49–3.59 | 0.574 | −0.25 | 0.15 | 0.78 | 0.58–1.05 | 0.779 |
| Worked in a COVID‐19‐designated hospital | |||||||||||||||||||||||||
| No | Ref. | Ref. | Ref. | Ref. | Ref. | ||||||||||||||||||||
| Yes | 0.22 | 0.06 | 1.24 | 1.11–1.38 | <0.001 *** | 0.23 | 0.04 | 1.26 | 1.17–1.36 | <0.001 *** | 0.19 | 0.04 | 1.21 | 1.12–1.31 | <0.001 *** | −0.16 | 0.11 | 0.86 | 0.69–1.07 | 0.164 | 0.03 | 0.04 | 1.03 | 0.96–1.12 | 0.405 |
MBI‐GS, Maslach Burnout Inventory‐General Survey; PTGI‐SF, Post Traumatic Growth Inventory‐Short Form; TSQ, Trauma Screening Questionnaire.
The TSQ cut‐off point was ≥6 and <6.
Emotional exhaustion, depersonalization, and lack of personal accomplishment MBI scores were classified into low and moderate‐to‐high groups.
The cut‐off point for total PTGI‐SF scores was the 60th percentile to divide the population into groups with scores equal to or higher than the 60th percentile (≧32 points) and less than the 60th percentile (<32 points).
P < 0.05.
P < 0.01.
P < 0.001.
Table 5.
Multiple linear regressions of influential factors of COVID‐19's effects on nurses
| Variables | TSQ | PTGI‐SF | ||||||
|---|---|---|---|---|---|---|---|---|
| R 2 | Adjusted R 2 | F | P | R 2 | Adjusted R 2 | F | P | |
| Tenure | 0.28 | 0.28 | 1229.02 | < 0.001 *** | 0.21 | 0.21 | 816.81 | < 0.001 *** |
| TSQ | – | – | – | – | 0.21 | 0.21 | 3.86 | < 0.001 *** |
| MBI | ||||||||
| Emotional Exhaustion | 0.26 | 0.26 | 4501.39 | < 0.001 *** | 0.20 | 0.20 | 101.97 | < 0.001 *** |
| Depersonalization | 0.28 | 0.28 | 226.67 | < 0.001 *** | 0.21 | 0.20 | 36.07 | < 0.001 *** |
| Lack of Personal Accomplishment | 0.29 | 0.29 | 74.38 | < 0.001 *** | 0.21 | 0.20 | 3090.84 | < 0.001 *** |
| PTGI‐SF | 0.29 | 0.29 | 3.86 | < 0.001 *** | – | – | – | – |
MBI, Maslach Burnout Inventory; PTGI‐SF, Post Traumatic Growth Inventory‐Short Form; TSQ, Trauma Screening Questionnaire.
P < 0.001.
In the logistic regression analysis, influential factors relating to burnout in terms of emotional exhaustion were being a woman (OR: 1.30, 95% CI 1.09–1.54; P = 0.003) working in a COVID‐19 designated hospital (OR: 1.26, 95% CI 1.17–1.36; P < 0.001), working in critical care units (OR: 1.23, 95% CI 1.12–1.33; P < 0.001), and departments related to COVID‐19 (OR: 1.16, 95% CI 1.04–1.29; P = 0.006). By contrast, influential factors relating to depersonalization were working in a COVID‐19 designated hospital (OR: 1.21, 95% CI 1.12–1.31; P < 0.001), working in critical care units (OR: 1.15, 95% CI 1.06–1.25; P = 0.001), and departments related to COVID‐19 (OR: 1.20, 95% CI 1.08–1.33; P = 0.001). Factors influencing lack of personal accomplishment were being a woman (OR: 0.51, 95% CI 0.36–0.74; P < 0.001) and never caring for patients with COVID‐19 (OR: 0.50, 95% CI 0.28–0.89; P = 0.019) (Table 4).
Participants with total scores higher than the 60th percentile were considered to have probable posttraumatic growth. The participants were divided into groups on the basis of whether their scores were equal to or higher than the 60th percentile (≧32 points) or less than the 60th percentile (<32 points). In the logistic regression, influential factors relating to posttraumatic growth scores was caring for patients with COVID‐19 (OR: 1.49, 95% CI 1.27–1.75; P < 0.001) (Table 4, Figure 2). In addition, multiple linear regression was performed to analyse whether experience, trauma score, emotional exhaustion, depersonalization, and lack of personal accomplishment influenced posttraumatic growth. Lack of personal accomplishment was a key influential factor of posttraumatic growth and had the highest explanatory power (adjusted R 2 = 20%, P < 0.001) (Table 5).
Fig. 2.
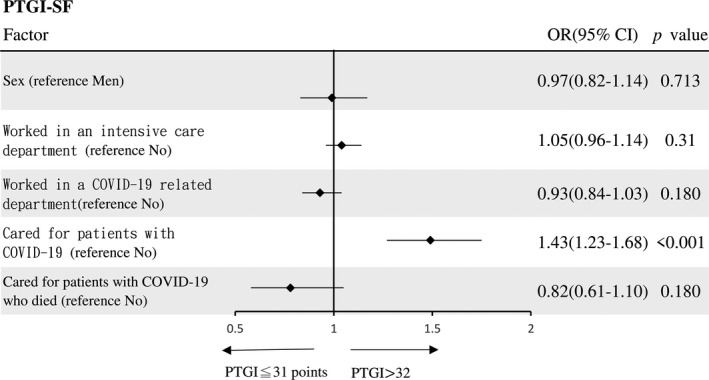
Logistic regression of PTGI‐SF by displacement status.
Discussion
It could be argued that COVID‐19 could be categorized as a new type of mass trauma. There are unique characteristics for this pandemic, which call for a new perspective about ‘what is trauma’, and what are its implications. For one thing, COVID‐19 is not only global in scope, but its impact is rippling into every aspect of society with financial setbacks, social media impact, personal and community restrictions (Horesh & Brown 2020). Healthcare professionals may also have extra concerns in pandemics, including access to appropriate personal protective equipment, fear of propagating infection, being exposed to COVID‐19 at work, and taking the infection home to their families (Kisely et al. 2020). Experiencing continuous stress can lead to psychological health problems like PTSD.
Our findings revealed that 13.3% of the participants had symptoms of trauma. Among personnel who worked in intensive care units, and those who cared for patients with COVID‐19, 15.2% exhibited symptoms of trauma. However, our results were lower in percentage than those reported in a study on nurses who cared for patients with SARS (severe acute respiratory syndrome). In the previous study, the proportion of healthcare personnel displaying symptoms of trauma was higher among those who provided care for patients with SARS (33.0%) than among those who did not (18.7%) (Su et al. 2007). Possible reasons for our result include the significantly higher death rate and disease burden associated with SARS (9.5%) and MERS or Middle East respiratory syndrome (34.4%) compared with those of the current estimates for COVID‐19 (4.3–6.9%) (Munster et al. 2020). In addition, some of the nurses working with COVID‐19 patients may have also participated in the previous SARS pandemic leading to less stress in dealing with personal protective equipment protocol and infectious disease situations (Cai et al. 2020). During a disease outbreak, organized work environments and systematic care procedures are vital for preventing infection and ensuring the safety of nurses (Chen et al. 2006).
Studies have also shown that identifying as women or men affects trauma differently. After being exposed to challenging events, women were more likely to be traumatized than men were; in this regard, our study results are consistent with those of past studies (De Stefano et al. 2018; Jones et al. 2020; Olff et al. 2007).
In terms of burnout, our findings indicate that nurses have experienced a moderate degree of emotional exhaustion, low degree of depersonalization, and a low degree in the domain of reduced personal accomplishment. Nurse respondents who were women or worked in COVID‐19 designated hospitals or in intensive care units, and cared for patients with COVID‐19 were also more likely to exhibit emotional exhaustion than men and those who did not work in COVID‐19‐related departments. Our results are consistent with previous studies that showed nurses who care for patients with infectious diseases exhibit higher levels of burnout. Specifically, their emotional exhaustion and depersonalization scores are higher than those of personnel who do not care for patients with infectious diseases (Boo et al. 2018; Qiao et al. 2016). However, a higher level of personal accomplishment was an influential factor for growth, and this may be a two‐way street where higher posttraumatic growth also influenced lower burnout and needs to be studied further. Also, previous experience of dealing with pandemics such as SARS may have increased posttraumatic growth for this population showing lower rates of burnout. According to Cai and colleagues’ study, nurses who did not have previous public health emergency treatment experience had worse mental health and resilience (Cai et al. 2020).
Our results indicated that nurses who worked in intensive care departments and provided care for patients with COVID‐19 had higher posttraumatic growth scores. This result was consistent with those of previous studies indicating the coexistence of posttraumatic growth and posttraumatic stress (Garcia et al. 2016; Ogińska‐Bulik & Zadworna‐Cieślak 2018). Stuart’s stress adaptation model theorized that not all responses to crises are negative. According to Calhoun, Cann, and Tedschi’s (2010) model of posttraumatic growth, some individuals would reinterpret their lives due to the experienced trauma and proactively adjust their self‐perceptions, relationships with others, and attitudes towards life for the better. This personal growth may have occurred because people create meaning when processing a traumatic event. Not all people who experience trauma feel despair, continually ruminate on their experience, or become devastated. A meta‐analysis showed that trauma is associated with posttraumatic growth in a linear and curvilinear relationship (Shakespeare‐Finch & Lurie‐Beck 2014). Recognizing that personality dynamics can also facilitate or impede posttraumatic growth, the independent contributions of trauma characteristics and individuals’ personality dynamics to posttraumatic growth warrant further study (Shuwiekh et al. 2018).
Limitation
Our study’s large sample size improves generalizability considerably. However, the study’s cross‐sectional design is a limitation where correlation and not causation could be inferred. Future studies should consider a longitudinal design. Self‐selection bias could also contribute to limits in the generalizability of the study results to other similar populations. Due to the sudden occurrence of the COVID‐19 pandemic, the psychological and physiological conditions of nurses before providing care for patients with COVID‐19 could not be assessed. There is also the limitation of the small percentage of personnel who care for COVID‐19 patients directly. However, as the survey was intended to gauge the reactions of medical personnel in the middle circle of the pandemic other research will have to fill in the gaps for the populations of interest in the other circles in the population exposure model.
Conclusions
This is the first large‐scale study to report the effects of COVID‐19 on healthcare workers’ trauma and burnout. Analysing the factors associated with mental health outcomes could lead to more effective prevention and treatment strategies for adverse health outcomes and better use of resources to promote positive outcomes. More psychological support should be provided for nurses who are women, those working in ICUs, COVID‐19 designated hospitals and departments involved with treating COVID‐19 patients.
Relevance for Clinical Practice
As of this writing, this is one of the first large‐scale survey studies to examine trauma, burnout, and posttraumatic growth in nurses during the COVID‐19 pandemic. Unfortunately, as evidence‐based cures and vaccines are still being developed, the degree of stress sustained by nurses could be increasing daily. In addition to providing nurses with safe and secure work environments, sufficient personal protective equipment, and clear disease prevention policies, governments must prioritize and provide for psychological support for nurses with a high risk of developing traumatic disorders. In turn, as the WHO recommends, healthcare workers should maintain self‐care, be attentive to their own mental health problems, and reflect on how their experiences may influence themselves and their loved ones. As psychological health and safety of nurses are crucial to providing quality care for the general population, identifying and instituting effective treatment strategies to improve psychological outcomes for nurses is essential.
Funding
No external funding was received for this study.
Ethics Approval
Ethical approval from the ethics committee of Beijing Hospital (Approval No. 2020BJYYEC‐098‐02) and the Joint Institutional Review Board of Taipei Medical University (Approval No. N202003066) was obtained.
Acknowledgements
We gratefully thank all the nurses who generously shared their time and experience to participate in this study during the COVID‐19 pandemic.
Chao Sun is contributed equally as first author to this manuscript.
Declaration of conflict of interest statement: The authors declare no conflict of interest.
References
- Aguayo, R. , Vargas, C. , Fuente, E. & Lozano, L. (2011). A meta‐analytic reliability generalization study of the Maslach Burnout Inventory. International Journal of Clinical and Health Psychology, 11, 343–361. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and Statistical Manual of Mental Disorders (DSM‐5®). Arlington, VA: American Psychiatric Association. [Google Scholar]
- Boo, Y. L. , Liam, C. C. K. , Lim, S. Y. et al (2018). Stress and burnout syndrome in health‐care providers treating dengue infection: A cross‐sectional study. Medical Journal of Malaysia, 73, 371–375. [PubMed] [Google Scholar]
- Cai, W. , Lian, B. , Song, X. , Hou, T. , Deng, G. & Li, H. (2020). A cross‐sectional study on mental health among health care workers during the outbreak of Corona Virus Disease 2019. Asian Journal of Psychiatry, 51, 102111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calhoun, L. G. , Cann, A. & Tedeschi, R. G. (2010). The posttraumatic growth model: Sociocultural considerations In: Weiss T. & Berger R. (Eds.), Posttraumatic Growth and Culturally Competent Practice: Lessons Learned from Around the Globe (pp. 1–14). Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Chen, R. , Chou, K. R. , Huang, Y. J. , Wang, T. S. , Liu, S. Y. & Ho, L. Y. (2006). Effects of a SARS prevention programme in Taiwan on nursing staff's anxiety, depression and sleep quality: a longitudinal survey. International Journal of Nursing Studies, 43, 215–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collier, L. (2016). Growth After Trauma (p. 48). Arlington, VA: American Psychological Association. [Google Scholar]
- Crisis and Trauma Resource Institute (2017). Trauma – Strategies for Resolving the Impact of Post Traumatic Stress. Winnipeg, MB, Canada: Crisis and Trauma Resource Institute. [Google Scholar]
- De Stefano, C. , Orri, M. , Agostinucci, J. M. et al (2018). Early psychological impact of Paris terrorist attacks on healthcare emergency staff: A cross‐sectional study. Depress Anxiety, 35, 275–282. [DOI] [PubMed] [Google Scholar]
- DeWolfe, D. J. (2004). Mental Health Response to Mass Violence and Terrorism: A Training Manual: (532512006–001). Arlington, VA: American Psychological Association. [Google Scholar]
- Dzau, V. J. , Kirch, D. & Nasca, T. (2020). Preventing a parallel pandemic — A National Strategy to protect clinicians’ well‐being. New England Journal of Medicine, 383, 513–515. [DOI] [PubMed] [Google Scholar]
- Friedman, M. J. , Keane, T. M. & Resick, P. A. (2015). Handbook of PTSD: Science and Practice. New York, NY: Guilford Publications. [Google Scholar]
- Garcia, F. E. , Cova, F. , Rincon, P. , Vazquez, C. & Paez, D. (2016). Coping, rumination and posttraumatic growth in people affected by an earthquake. Psicothema, 28, 59–65. [DOI] [PubMed] [Google Scholar]
- Gosling, S. D. , Vazire, S. , Srivastava, S. & John, O. P. (2004). Should we trust web‐based studies? A comparative analysis of six preconceptions about internet questionnaires. American psychologist, 59, 93. [DOI] [PubMed] [Google Scholar]
- Guterres, A. (2020). UN leads call to protect most vulnerable from mental health crisis during and after COVID‐19. UN News. [Google Scholar]
- Hensel, J. M. , Ruiz, C. , Finney, C. & Dewa, C. S. (2015). Meta‐analysis of risk factors for secondary traumatic stress in therapeutic work with trauma victims. Journal of Traumatic Stress, 28 (2), 83–91. [DOI] [PubMed] [Google Scholar]
- Horesh, D. & Brown, A. D. (2020). Traumatic stress in the age of COVID‐19: A call to close critical gaps and adapt to new realities. Psychological Trauma: Theory, Research, Practice, and Policy, 12, 331. [DOI] [PubMed] [Google Scholar]
- Huang, J. Z. , Han, M. F. , Luo, T. D. , Ren, A. K. & Zhou, X. P. (2020). Mental health survey of medical staff in a tertiary infectious disease hospital for COVID‐19. Journal of Industrial Hygiene and Occupational Diseases, 38, 192–195. [DOI] [PubMed] [Google Scholar]
- Jones, G. A. L. , Colville, G. A. , Ramnarayan, P. et al (2020). Psychological impact of working in paediatric intensive care. A UK‐wide prevalence study. Archives of Disease in Childhood, 105, 470–475. [DOI] [PubMed] [Google Scholar]
- Kisely, S. , Warren, N. , McMahon, L. , Dalais, C. , Henry, I. & Siskind, D. (2020). Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: rapid review and meta‐analysis. BMJ, 369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai, J. , Ma, S. , Wang, Y. et al (2020). Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Network Open, 3, e203976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavrakas, P. (2008). Survey Ethics. Encyclopedia of Survey Research Methods. Thousand Oaks, CA: Sage Publications Inc. [Google Scholar]
- Lin, K. , Yang, B. X. , Luo, D. et al (2020). The mental health effects of COVID‐19 on health care providers in China. American Journal of Psychiatry. [DOI] [PubMed] [Google Scholar]
- Loue, S. (2002). Textbook of Research Ethics: Theory and Practice. Basel: Springer US. [Google Scholar]
- Marjanovic, Z. , Greenglass, E. R. & Coffey, S. (2007). The relevance of psychosocial variables and working conditions in predicting nurses' coping strategies during the SARS crisis: an online questionnaire survey. International Journal of Nursing Studies, 44, 991–998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maslach, C. , Jackson, S. E. , Leiter, M. P. , Schaufeli, W. B. & Schwab, R. L. (1986). Maslach Burnout Inventory. Palo Alto, CA: Consulting Psychologists Press. [Google Scholar]
- Maunder, R. (2004). The experience of the 2003 SARS outbreak as a traumatic stress among frontline healthcare workers in Toronto: lessons learned. Philosophical Transactions of the Royal Society of London. Series B: Biological Sciences, 359, 1117–1125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouthaan, J. , Sijbrandij, M. , Reitsma, J. B. , Gersons, B. P. R. & Olff, M. (2014). Comparing screening instruments to predict posttraumatic stress disorder. PLoS One, 9, e97183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munster, V. J. , Koopmans, M. , van Doremalen, N. , van Riel, D. & de Wit, E. (2020). A novel coronavirus emerging in China — Key questions for impact assessment. New England Journal of Medicine, 382, 692–694. [DOI] [PubMed] [Google Scholar]
- Naude, J. L. P. & Rothmann, S. (2004). The validation of the Maslach Burnout Inventory‐Human Services Survey for emergency medical technicians in Gauteng. SA Journal of Industrial Psychology, 30, 21–28. [Google Scholar]
- Niu, S. F. , Kuo, S. F. , Tsai, H. T. , Kao, C. C. , Traynor, V. & Chou, K. R. (2019). Prevalence of workplace violent episodes experienced by nurses in acute psychiatric settings. PLoS One, 14, e0211183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogińska‐Bulik, N. (2014). The role of coping strategies in posttraumatic growth in medical rescue workers. Medycyna Pracy, 65, 209–217. [PubMed] [Google Scholar]
- Ogińska‐Bulik, N. & Zadworna‐Cieślak, M. (2018). The role of resiliency and coping strategies in occurrence of positive changes in medical rescue workers. International Emergency Nursing, 39, 40–45. [DOI] [PubMed] [Google Scholar]
- Olff, M. , Langeland, W. , Draijer, N. & Gersons, B. P. (2007). Gender differences in posttraumatic stress disorder. Psychological Bulletin, 133, 183–204. [DOI] [PubMed] [Google Scholar]
- Qiao, Z. X. , Chen, L. , Chen, M. Q. et al (2016). Prevalence and factors associated with occupational burnout among HIV/AIDS healthcare workers in China: a cross‐sectional study. BMC Public Health, 16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespeare‐Finch, J. & Lurie‐Beck, J. (2014). A meta‐analytic clarification of the relationship between posttraumatic growth and symptoms of posttraumatic distress disorder. Journal of Anxiety Disorders, 28, 223–229. [DOI] [PubMed] [Google Scholar]
- Shuwiekh, H. , Kira, I. A. & Ashby, J. S. (2018). What are the personality and trauma dynamics that contribute to posttraumatic growth? International Journal of Stress Management, 25, 181. [Google Scholar]
- Sigsbee, B. & Bernat, J. L. (2014). Physician burnout: A neurologic crisis. Neurology, 83, 2302–2306. [DOI] [PubMed] [Google Scholar]
- Siu, O. L. (2002). Predictors of job satisfaction and absenteeism in two samples of Hong Kong nurses. Journal of Advanced Nursing, 40, 218–229. [DOI] [PubMed] [Google Scholar]
- Solomon, Z. & Dekel, R. (2007). Posttraumatic stress disorder and posttraumatic growth among Israeli ex‐pows. Journal of Traumatic Stress, 20, 303–312. [DOI] [PubMed] [Google Scholar]
- Spoorthy, M. S. (2020). Mental health problems faced by healthcare workers due to the COVID‐19 pandemic‐ a review. Asian Journal of Psychiatry, 51, 102119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stein, D. J. , McLaughlin, K. A. , Koenen, K. C. et al (2014). DSM‐5 AND ICD‐11 definitions of posttraumatic stress disorder: Investigating “Narrow” and “Broad” approaches. Depression and anxiety, 31, 494–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stuart, G. W. (2005). The Stuart Stress Adaptation Model of Psychiatric Nursing Care. Principles and Practice of Psychiatric Nursing. St. Louis: Mosby Inc. [Google Scholar]
- Su, T. P. , Lien, T. C. , Yang, C. Y. et al (2007). Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. Journal of Psychiatric Research, 41, 119–130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taku, K. , Kilmer, R. P. , Cann, A. , Tedeschi, R. G. & Calhoun, L. G. (2012). Exploring posttraumatic growth in Japanese youth. Psychological Trauma‐Theory Research Practice and Policy, 4, 411–419. [Google Scholar]
- Tedeschi, R. G. & Calhoun, L. G. (1996). The Posttraumatic Growth Inventory: measuring the positive legacy of trauma. Journal of Traumatic Stress, 9, 455–471. [DOI] [PubMed] [Google Scholar]
- Tedeschi, R. G. & Calhoun, L. G. (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15, 1–18. [Google Scholar]
- Tolomiczenko, G. S. , Kahan, M. , Ricci, M. et al (2005). SARS: coping with the impact at a community hospital. Journal of Advanced Nursing, 50, 101–110. [DOI] [PubMed] [Google Scholar]
- Tominaga, Y. , Goto, T. , Shelby, J. , Oshio, A. , Nishi, D. & Takahashi, S. (2019). Secondary trauma and posttraumatic growth among mental health clinicians involved in disaster relief activities following the 2011 Tohoku earthquake and tsunami in Japan. Counselling Psychology Quarterly, 1–21. [Google Scholar]
- Tourangeau, R. (2014). Measurement properties of web surveys. Beyond traditional survey taking: adapting to a changing world. Statistics Canada. [Google Scholar]
- UNDRR (2020). Risks and Disasters. UN‐SPIDER Knowledge Portal. [Google Scholar]
- Vos, F. , Rodriguez, J. , Below, R. & Guha‐Sapir, D. (2010). Annual Disaster Statistical Review 2009: The Numbers and Trends. Centre for Research on the Epidemiology of Disasters (CRED). [Google Scholar]
- Walters, J. T. R. , Bisson, J. I. & Shepherd, J. P. (2007). Predicting post‐traumatic stress disorder: validation of the Trauma Screening Questionnaire in victims of assault. Psychological Medicine, 37, 143–150. [DOI] [PubMed] [Google Scholar]
- World Health Organization . (2020). Coronavirus disease (COVID‐2019) situation reports.
- Xiao, S. , Luo, D. & Xiao, Y. (2020). Survivors of COVID‐19 are at high risk of posttraumatic stress disorder. Global Health Research and Policy, 5, 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu, X.‐N. , Lau, J. T. F. , Zhang, J. et al (2010). Posttraumatic growth and reduced suicidal ideation among adolescents at month 1 after the Sichuan Earthquake. Journal of Affective Disorders, 123, 327–331. [DOI] [PubMed] [Google Scholar]


