Abstract
Background:
Atrial fibrillation is the most common arrhythmia in post-industrialized populations. Older age, hypertension, obesity, chronic inflammation, and diabetes are significant atrial fibrillation risk factors, suggesting that modern urban environments may promote atrial fibrillation.
Objective:
Here we assess atrial fibrillation prevalence and incidence among tropical horticulturalists of the Bolivian Amazon with high levels of physical activity, a lean diet, and minimal coronary atherosclerosis, but also high infectious disease burden and associated inflammation.
Methods:
Between 2005–2019, 1314 Tsimane aged 40–94 years (52% female) and 534 Moseten Amerindians aged 40–89 years (50% female) underwent resting 12-lead electrocardiograms to assess atrial fibrillation prevalence. For atrial fibrillation incidence assessment, 1059 (81% of original sample) Tsimane and 310 Moseten (58%) underwent additional ECGs (mean time to follow up 7.0, 1.8 years, respectively).
Findings:
Only one (male) of 1314 Tsimane (0.076%) and one (male) of 534 Moseten (0.187%) demonstrated atrial fibrillation at baseline. There was one new (female) Tsimane case in 7395 risk years for the 1059 participants with >1 ECG (incidence rate = 0.14 per 1,000 risk years). No new cases were detected among Moseten, based on 542 risk years.
Conclusion:
Tsimane and Moseten show the lowest levels of atrial fibrillation ever reported, 1/20 to ~1/6 of rates in high-income countries. These findings provide additional evidence that a subsistence lifestyle with high levels of physical activity, and a diet low in processed carbohydrates and fat is cardioprotective, despite frequent infection-induced inflammation. Findings suggest that atrial fibrillation is a modifiable lifestyle disease rather than an inevitable feature of cardiovascular aging.
Introduction
Atrial fibrillation (AF) is the most common arrhythmia in the post-industrialized world [1,2]. It is associated with a five-fold increase in the risk of stroke [3], which is the second leading cause of death in many industrialized nations [4]. AF is also associated with a three-fold increase in risk of heart failure and two-fold increases in risk of dementia and all-cause mortality [3,4]. The incremental cost of atrial fibrillation to the health care system has been estimated at 6–26 billion dollars per year in the United States alone [5].
AF prevalence is increasing worldwide due to its greater incidence among older adults and the aging of the global population [6,7]. AF prevalence in the U.S. is expected to increase up to 45% by 2030, to over 12 million cases [8], and to 14–17 million cases across Europe [9]. The increasing prevalence of potentially modifiable AF risk factors contributes to its growing prevalence [6]. AF risk factors include older age, hypertension, congestive heart failure, diabetes, peripheral vascular and coronary artery disease, valvular heart disease, alcohol excess, sleep apnea, systemic inflammation, male sex, and other cardiovascular disease risk factors (e.g. low high-density lipoprotein, HDL) [3,4,6,10]. Correlates of AF observed on a 12-lead electrocardiogram (ECG) include first-degree atrioventricular blocks, increased QRS duration, and bundle branch blocks [11].
Given the widespread and increasing prevalence of AF in post-industrialized populations, and its detection worldwide [12], AF has been considered a natural consequence of cardiovascular aging [13]. However, most estimates to date have been derived from high-income countries with more sedentary lifestyles. Prevalence and incidence rates appear to be generally lower in low-income countries, although country-level differences are not well explained by development status [12]. Thus, the relative roles of lifestyle and the biology of aging in AF incidence across diverse environments remain unclear.
Study Goals and Hypotheses
To assess the extent to which lifestyle factors influence AF risk, we evaluate AF prevalence and incidence in the Tsimane and Moseten, two subsistence-based populations of lowland Bolivia with active lifestyles [14]. The Tsimane are an indigenous population of approximately 17,000 who fish, hunt, farm with hand tools, and forage for their food; they have minimal access to electricity, clean water, and public sanitation [15]. The Moseten (population ~3,000) are a genetically and ethno-linguistically related Bolivian population of horticulturalists who live in close proximity to Tsimane but who began acculturation into broader Bolivian society decades earlier [16]. The Tsimane mostly inhabit the Maniqui River basin area in the municipality of San Borja, while the Moseten territory is adjacent but closer to the Andes foothills west of the Tsimane area in the municipality of Palos Blancos. There is limited inter-marriage between Tsimane and Moseten, as their territories do not overlap. While Tsimane are largely endogamous, the Moseten in recent decades have intermarried with highland migrants to the region. Working with the Tsimane and Moseten to assess AF provides a rare opportunity to evaluate the extent to which lifestyle and environment might effectively reduce AF, beyond that of healthy subjects in industrialized nations. Tsimane have the lowest levels of coronary atherosclerosis ever observed, based on non-contrast X-ray computed tomography (CT) to evaluate coronary artery calcification [17]. Tsimane exhibit few other atherosclerotic risk factors, including hypertension [18], obesity, type 2 diabetes, and hyperlipidemia [17,19]. Tsimane diet is rich in fiber, polyunsaturated fatty acids, potassium, magnesium, and selenium [16], and low in saturated fat and preservatives. They have high physical activity levels beginning early in life [14].Though endurance-trained athletes show evidence of increased frequency of paroxysmal AF [20], the Tsimane do not typically engage in very high levels of vigorous activity. Instead, the Tsimane engage in high levels of low and moderate activity, and thus are rarely sedentary, throughout the day [14]. They show no evidence of lower extremity peripheral atherosclerosis as assessed by Ankle-Brachial Indices [21]. However, two AF risk factors that are prevalent among Tsimane include elevated levels of systemic inflammation, and low levels of high-density lipoproteins (HDL) [17,21]. Inflammation has been associated with increased AF prevalence in numerous studies [22,23,24], and the Tsimane experience frequent infections, which increases systemic inflammation and immune activation throughout life [25,26]. Low HDL is also a significant AF risk factor [27], and over half of Tsimane adults age 40+ years show HDL levels < 40 mg/dL [17].
Compared to Tsimane, Moseten lifestyle is more acculturated: Moseten have more schooling, have greater access to clean water and electricity, and many no longer speak the indigenous Moseten language but instead are monolingual Spanish speakers. Moseten also engage more often in cash cropping than Tsimane and have greater access to labor-saving technology, like chainsaws. Likely as a result of these differences, the Moseten show higher rates of obesity and type 2 diabetes, and have more processed foods and additives in their diet [16]. Nevertheless, compared to populations in high-income countries, Moseten lifestyle as subsistence farmers is still closer to that of the horticultural-forager Tsimane in terms of physical activity level and other AF risk factors. Investigating Moseten AF thus represents an opportunity to explore the role of lifestyle change on AF in a genetically related population inhabiting a similar rural environment within Bolivia.
Our aims are to (1) assess risk factors for AF among Tsimane and Moseten; and (2) estimate their AF prevalence and incidence and compare against other world populations.
Methods
Risk factors
Baseline demographic information was collected by a mobile biomedical team along with measurements of the following risk factors: height, weight, waist circumference, blood lipids (total cholesterol, LDL, HDL and triglycerides) from fasting morning samples, inflammatory markers (high sensitivity C-reactive protein [hs-CRP], erythrocyte sedimentation rate [ESR], interleukin-6 [IL6]), and systolic and diastolic blood pressure (see 17, 18 for detailed procedures) [17,18]. Hypertension and diabetes were classified according to clinical guidelines [28].
AF Prevalence and Incidence
Trained Bolivian physicians (RQG, ECL, DER) conducted a resting standard 12-lead electrocardiogram (ECG). Tsimane ECGs were reviewed by two cardiologists (CJR and KT) blinded to subject information and independently evaluated by three cardiologists (GST, MIM, LSW). Moseten ECGs were reviewed by one of the same cardiologists (CJR) and an additional cardiologist (MAE). ECGs were coded as either positive or negative for AF. There was no disagreement in diagnoses among coders. ECG measures of PR and QRS were also recorded.
To assess AF prevalence, at least one ECG was performed from 2005–2019 on 1314 Tsimane aged 40+ years, which at the time represented 70% of the adult population in that age range (Table 1; Figure S1 for STROBE sample flow chart). AF was defined as in the 2006 ACC/AHA/ESC guidelines [29]. Participants also underwent routine medical screening by a mobile medical team consisting of internists, medical technicians, and biochemists. A patient’s first ECG was used to assess AF prevalence, and 81% (n = 1059) of the sample underwent at least one subsequent ECG to assess incidence. Between 2015 to 2018, one ECG was performed on 534 Moseten aged 40+ years by the same team and using the same protocol, covering 95% of the eligible population aged 40+. A second ECG was collected among 310 (58%) of these Moseten participants (Table 2, Figure S2).
Table 1.
Tsimane sample composition and distribution of AF risk factors. Standard deviations and standard errors are given in parentheses (for means and proportions, respectively). Significance column provides p-values for testing differences across age groups based on ANOVA.
| AGE GROUP (YEARS) | N | 39–49 | 50–59 | 60–69 | 70–79 | ≥ 80 | TOTAL | SIGNIFICANCE |
|---|---|---|---|---|---|---|---|---|
| N with baseline ECG | 670 | 328 | 204 | 90 | 22 | 1314 | ||
| Proportion Male | 0.52 | 0.51 | 0.55 | 0.49 | 0.36 | 0.52 | ||
| Anthropometric measures | ||||||||
| Height cm | 1307 | 157.0 (7.2) | 155.8 (7.7) | 155.1 (7.4) | 151.6 (7.9) | 149.9 (6.2) | 155.9 (7.5) | <0.001 |
| Weight kg | 1307 | 60.4 (9.6) | 58.4 (10.3) | 56.3 (9.4) | 53.2 (8.7) | 47.8 (7.9) | 58.5 (10.0) | <0.001 |
| BMI kg/m2 | 1306 | 24.4 (3.1) | 24.0 (3.6) | 23.3 (3.1) | 23.1 (3.4) | 21.2 (2.2) | 24.0 (3.3) | <0.001 |
| % BMI > 30 kg/m2 | 1306 | 5.0 (0.8) | 5.2 (1.2) | 3.5 (1.3) | 4.4 (2.2) | 0.0 (0.0) | 4.7 (0.6) | 0.362 |
| Waist Circ. in | 1049 | 34.9 (3.3) | 35.0 (4.1) | 35.2 (3.7) | 35.6 (4.0) | 33.5 (2.4) | 35.0 (3.6) | 0.732 |
| % Waist Circ. High | 1049 | 24.6 (1.9) | 26.0 (2.7) | 31.1 (3.7) | 25.0 (5.3) | 5.9 (5.9) | 25.6 (1.4) | 0.938 |
| Lipid profiles | ||||||||
| Total Cholesterol mg/dL | 1112 | 142.9 (27.6) | 146.8 (30.6) | 140.9 (26.9) | 137.8 (27.6) | 139.6 (26.5) | 143.3 (28.4) | 0.064 |
| % Cholesterol > 240 mg/dL | 1112 | 0.35 (0.25) | 0.68 (0.48) | 0.0 (0.0) | 0.0 (0.0) | 0.0 (0.0) | 0.36 (0.18) | 0.498 |
| LDL mg/dL | 1032 | 86.6 (25.7) | 89.7 (27.9) | 85.0 (25.6) | 80.3 (25.3) | 82.5 (21.7) | 86.7 (26.2) | 0.045 |
| % LDL > 130 mg/dL | 1032 | 5.28 (0.97) | 6.77 (1.54) | 4.52 (1.67) | 5.97 (2.92) | 0.00 (0.00) | 5.52 (0.71) | 0.714 |
| HDL mg/dL | 1035 | 37.2 (7.5) | 38.0 (6.7) | 37.1 (6.4) | 38.0 (7.6) | 37.1 (9.6) | 37.5 (7.2) | 0.045 |
| Triglycerides mg/dL | 1117 | 109.0 (46.9) | 113.9 (52.7) | 106.1 (45.9) | 105.9 (41.0) | 105.6 (22.6) | 109.6 (47.8) | 0.519 |
| % Triglycerides > 200 mg/dL | 1117 | 4.20 (0.84) | 4.76 (1.24) | 4.29 (1.59) | 1.37 (1.37) | 0.00 (0.00) | 4.12 (0.59) | 0.289 |
| Inflammatory Markers | ||||||||
| hs-CRP mg/dL | 758 | 2.4 (1.8) | 2.6 (2.3) | 3.1 (2.3) | 2.3 (1.6) | 4.4 (2.7) | 2.6 (2.0) | <0.001 |
| % hs-CRP > 3 mg/dL | 758 | 37.0 (2.5) | 42.9 (3.4) | 53.8 (4.6) | 45.5 (7.6) | 66.7 (14.2) | 42.2 (1.8) | <0.001 |
| ESR mm/h | 1304 | 27.1 (15.1) | 30.3 (15.1) | 38.8 (20.9) | 43.7 (22.3) | 58.4 (19.0) | 31.4 (17.9) | <0.001 |
| % Elevated ESR | 1304 | 45.6 (1.9) | 59.3 (2.7) | 72.3 (3.2) | 76.4 (4.5) | 95.5 (4.6) | 56.1 (1.4) | <0.001 |
| IL6 (pm/mL) | 740 | 1.6 (0.7) | 1.6 (0.5) | 1.6 (0.9) | 1.6 (1.6) | 1.5 (1.3) | 1.6 (0.8) | <0.001 |
| Blood Pressure and Hypertension | ||||||||
| Heart Rate (BPM) | 1314 | 51.1 (26.0) | 48.1 (27.6) | 49.2 (28.4) | 55.9 (29.5) | 57.6 (26.4) | 50.5 (27.1) | 0.640 |
| Systolic Blood Pressure mmHg | 1305 | 111.1 (8.0) | 114.4 (10.2) | 118.0 (12.7) | 121.9 (16.4) | 121.5 (24.0) | 113.9 (11.1) | <0.001 |
| % SBP > 120 mmHg | 1305 | 11.3 (1.2) | 19.9 (2.2) | 34.2 (3.4) | 45.6 (5.3) | 38.1 (10.9) | 19.8 (1.1) | <0.001 |
| Diastolic Blood Pressure mmHg | 1305 | 69.7 (5.8) | 70.8 (6.1) | 71.6 (7.9) | 70.8 (7.8) | 68.2 (9.8) | 70.3 (6.5) | 0.004 |
| % DBP > 80 mmHg | 1305 | 3.3 (0.7) | 6.8 (1.4) | 11.4 (2.2) | 7.8 (2.8) | 4.8 (4.8) | 5.8 (0.6) | 0.002 |
| % Hypertensive (>130/80 mmHg) | 1305 | 3.8 (0.7) | 8.9 (1.6) | 20.3 (2.8) | 26.7 (4.7) | 9.5 (6.6) | 9.3 (0.8) | <0.001 |
| ECG Measures | ||||||||
| PR ms | 1312 | 162 (19) | 162 (19) | 162 (18) | 162 (20) | 160 (21) | 162 (19) | 0.990 |
| % PR > 200 ms | 1312 | 1.79 (0.5) | 2.44 (0.9) | 2.46 (1.1) | 3.37 (1.9) | 4.56 (4.6) | 2.21 (0.4) | 0.328 |
| QRS ms | 1313 | 103 (12) | 103 (12) | 104 (17) | 104 (18) | 99 (14) | 103 (14) | 0.999 |
| % QRS > 120 ms | 1313 | 7.6 (1.0) | 5.8 (1.3) | 10.3 (2.1) | 10.0 (3.2) | 4.6 (4.6) | 7.7 (0.7) | 0.316 |
| Coronary Calcium scores from CT scan | ||||||||
| % CAC > 100 AU | 823 | 0.5 (0.38) | 3.5 (1.2) | 8.5 (2.34) | 4.4 (3.1) | 30.8 (13.3) | 3.5 (0.6) | <0.001 |
Note: Sample sizes vary, especially for serum biomarker analyses, due to logistical complications in the field (e.g., inability to store serum). CT sample sizes are smaller because of stratified sampling for ages 40–54.
Table 2.
Moseten sample composition and distribution of AF risk factors. Standard deviations are given in parentheses (for means), standard error (for proportions). “Total” column provides sample means age-standardized to Tsimane sample age distribution. Significance column provides p-values for testing differences across age groups based on ANOVA.
| AGE GROUP (YEARS) | N | 40–49 | 50–59 | 60–69 | 70–79 | ≥ 80 | TOTAL (AGE-ADJUSTED) | SIGNIFICANCE |
|---|---|---|---|---|---|---|---|---|
| N with baseline ECG | 208 | 155 | 121 | 39 | 10 | 534 | ||
| Proportion Male | 0.47 | 0.5 | 0.54 | 0.62 | 0.4 | 0.5 | ||
| Anthropometric Measures | ||||||||
| Height cm | 527 | 156.1 (7.1) | 154.8 (6.7) | 153.3 (8.0) | 151.8 (9.5) | 150.6 (7.1) | 154.8 (7.4) | <0.001 |
| Weight kg | 523 | 64.5 (12.4) | 62.6 (11.1) | 58.2 (13.0) | 58.2 (15.0) | 60.5 (9.0) | 62.4 (12.4) | <0.001 |
| BMI kg/m2 | 523 | 26.5 (5.1) | 26.1 (4.2) | 24.6 (4.7) | 25.1 (5.3) | 26.6 (3.3) | 26.0 (4.8) | 0.002 |
| % BMI > 30 kg/m2 | 523 | 21.2 (2.9) | 18.2 (3.1) | 10.2 (2.8) | 21.1 (6.7) | 10.0 (10.0) | 18.3 (1.7) | 0.088 |
| Lipid Profile | ||||||||
| Total Cholesterol mg/dL | 368 | 157.9 (30.1) | 162.4 (37.8) | 157.2 (35.2) | 161.9 (24.9) | 158.3 (34.5) | 159.2 (33.0) | 0.873 |
| % Cholesterol > 240 mg/dL | 368 | 2.9 (1.4) | 4.5 (2.0) | 2.3 (1.6) | 0.0 (0.0) | 0.0 (0.0) | 3.0 (0.9) | 0.28 |
| LDL mg/dL | 363 | 106.3 (35.7) | 108.8 (37.9) | 99.9 (35.8) | 107.3 (27.4) | 106.3 (30.3) | 105.9 (35.7) | 0.286 |
| % LDL > 130 mg/dL | 363 | 19.9 (3.4) | 24.6 (4.1) | 19.3 (4.2) | 26.1 (9.4) | 33.3 (21.1) | 21.7 (2.2) | 0.991 |
| HDL mg/dL | 363 | 37.6 (9.1) | 36.5 (9.1) | 39.2 (9.3) | 37.8 (9.1) | 35.1 (3.4) | 37.6 (9.1) | 0.193 |
| Triglycerides mg/dL | 365 | 137.9 (74.6) | 134.2 (81.1) | 113.0 (59.8) | 135.0 (71.0) | 103.1 (25.5) | 131.8 (73.2) | 0.047 |
| % Triglycerides > 200 mg/dL | 365 | 15.4 (3.1) | 15.3 (3.4) | 10.2 (3.3) | 16.7 (7.8) | 0.00 (0.00) | 14.3 (1.9) | 0.431 |
| Inflammatory Markers | ||||||||
| hs-CRP mg/dL | 109 | 2.6 (2.7) | 2.5 (2.1) | 2.9 (3.0) | 3.5 (1.9) | 7.3 (0.0) | 2.6 (2.7) | 0.315 |
| % hs-CRP > 3 mg/dL | 109 | 47.4 (8.2) | 42.1 (8.1) | 50.0 (9.3) | 50.0 (50.0) | 100.0 (NA) | 47.6 (5.9) | 0.275 |
| ESR mm/h | 449 | 29.6 (17.3) | 33.8 (20.4) | 38.5 (22.0) | 46.9 (24.1) | 39.0 (21.3) | 33.6 (19.6) | <0.001 |
| % Elevated ESR | 449 | 49.7 (3.9) | 60.2 (4.3) | 64.4 (4.7) | 84.9 (6.3) | 70.0 (15.3) | 57.8 (2.4) | <0.001 |
| IL6 (pm/mL) | 114 | 1.6 (0.3) | 1.6 (1.1) | 1.6 (0.9) | 7.8 (8.8) | 13.3 (0.0) | 1.6 (1.1) | 0.259 |
| Blood Pressure and Hypertension | ||||||||
| Heart Rate (BPM) | 533 | 64.0 (9.0) | 65.3 (9.9) | 64.4 (9.2) | 69.5 (16.1) | 67.8 (10.1) | 64.9 (10.0) | 0.019 |
| Systolic Blood Pressure mmHg | 526 | 116.9 (12.6) | 118.9 (15.9) | 125.0 (15.1) | 130.8 (16.5) | 144.8 (25.3) | 120.3 (14.5) | <0.001 |
| SBP > 120 mmHg | 526 | 35.8 (3.4) | 39.2 (4.0) | 55.4 (4.5) | 71.1 (7.5) | 90.0 (10.0) | 43.5 (2.1) | <0.001 |
| Diastolic Blood Pressure mmHg | 527 | 74.9 (10.1) | 76.8 (11.6) | 78.9 (10.2) | 81.5 (9.3) | 92.2 (15.2) | 76.9 (10.6) | <0.001 |
| % DBP > 80 mmHg | 527 | 26.5 (3.1) | 33.1 (3.8) | 39.7 (4.5) | 47.4 (8.2) | 80.0 (13.3) | 32.9 (2.0) | <0.001 |
| % Hypertensive (>130/80 mmHg) | 527 | 29.4 (3.2) | 37.0 (3.9) | 45.5 (4.6) | 55.3 (8.2) | 100.0 (0.0) | 37.3 (2.1) | <0.001 |
| ECG Measures | ||||||||
| PR ms | 528 | 150 (19) | 152 (20) | 153 (20) | 145 (21) | 158 (33) | 151 (20) | 0.937 |
| % PR > 200 ms | 528 | 1.5 (0.8) | 2.0 (1.1) | 1.7 (1.2) | 0.0 (0.0) | 11.1 (11.1) | 1.7 (0.6) | 0.565 |
| QRS ms | 533 | 104 (13) | 102 (10) | 106 (17) | 104 (15) | 96 (8) | 104 (13) | 0.872 |
| % QRS > 120 ms | 533 | 4.3 (1.4) | 4.5 (1.7) | 10.7 (2.8) | 15.4 (5.9) | 0.0 (0.0) | 6.2 (1.0) | 0.018 |
To assess Tsimane incidence, all follow-up ECGs (n = 1059 individuals totaling 7395 risk years) were examined with an average time to follow-up of 7.0 years (Table 3). Moseten incidence is based on a smaller follow-up sample (n = 310 totaling 542 risk years; average time to follow-up = 1.8 years). Tsimane and Moseten adults age 40+ years not sampled in the prevalence phase or missed during the incidence phase show minimal differences in AF risk factors (Supplementary Table S1).
Table 3.
Crude prevalence and incidence of atrial fibrillation.
| AGE GROUP (YEARS) | 40–49 | 50–59 | 60–69 | 70–79 | ≥ 80 | TOTAL |
|---|---|---|---|---|---|---|
| TSIMANE | ||||||
| Number of individuals | 670 | 328 | 204 | 90 | 22 | 1314 |
| Number of AF cases | 0 | 0 | 0 | 1 | 0 | 1 |
| AF prevalence (per 1,000) | 0 | 0 | 0 | 11.11 | 0 | 0.76 |
| N with >1 ECG | 541 | 286 | 157 | 60 | 15 | 1059 |
| Total Person-Years | 3726 | 2190 | 1074 | 335 | 70 | 7395 |
| Average Risk Years per Person | 6.89 | 7.66 | 6.84 | 5.59 | 4.67 | 6.98 |
| Number of new AF cases | 0 | 0 | 0 | 0 | 1 | 1 |
| AF incidence (per 1,000 person years) | 0 | 0 | 0 | 0 | 14.29 | 0.14 |
| MOSETEN | ||||||
| Number of individuals | 208 | 156 | 121 | 39 | 10 | 534 |
| Number of AF cases | 0 | 0 | 0 | 1 | 0 | 1 |
| AF prevalence (per 1,000) | 0 | 0 | 0 | 25.64 | 0 | 1.87 |
| N with > 1 ECG | 96 | 92 | 88 | 25 | 9 | 310 |
| Total Person-Years | 170 | 162 | 153 | 43 | 14 | 542 |
| Average Risk Years per Person | 1.78 | 1.76 | 1.74 | 1.73 | 1.55 | 1.75 |
| Number of new AF cases | 0 | 0 | 0 | 0 | 0 | 0 |
| AF incidence (per 1,000 person years) | 0 | 0 | 0 | 0 | 0 | 0 |
Verbal Autopsies
We recognize that our estimates of AF prevalence and incidence may be biased due to potentially higher case fatality rates, given the limited medical treatment in the region. To investigate this possibility, one THLHP physician (RQG) and Tsimane assistant conducted verbal autopsies for all Tsimane deaths occurring between October 2008 and December 2013 (n = 209 deaths) using the 2012 World Health Organization Verbal Autopsy Instrument [30].
Statistical Analysis
Crude prevalences were determined by dividing the number of cases diagnosed with AF by the total number of participants undergoing their initial ECG. Crude incidence rates were calculated by dividing the total number of new cases diagnosed from the follow-up ECG by the number of risk years between baseline and last ECG (if all were negative) or between the negative and positive ECGs (if a new incidence occurred).
To compare AF prevalence across populations, we selected papers reporting AF prevalence in rural subsistence-level samples (Ghana and Tanzania) [31,32] and among indigenous groups living in industrialized nations (Indigenous Australians and Native Americans) [33,34,35,36]. We also selected studies in industrialized populations that were population representative, used similar methodology for AF diagnosis, and provided age-specific AF rates so that age-standardized rates could be calculated [37,38,39,40]. Lastly, we included recently published AF prevalences for Global Burden of Disease (GBD) world regions based on 184 studies, that used similar inclusion and exclusion criteria, and so may also include atrial flutter and paroxysmal AF [12]. We employ indirect standardization using age-specific AF prevalences from the GBD sample to compute comparable estimates of AF prevalence across populations (Figure 1). This was done to account for the different age ranges among samples, which prevented us from directly standardizing the age-specific prevalences of each sample to a standard population structure.
Figure 1.
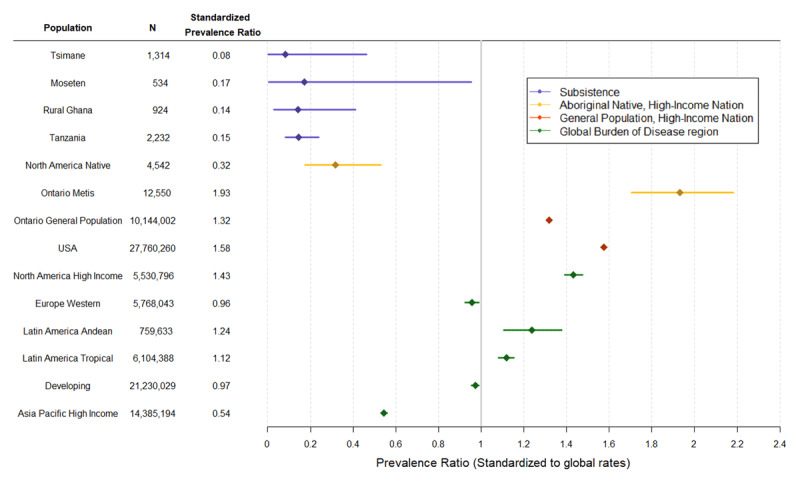
Age-standardized atrial fibrillation prevalence ratios, with 95% CIs. Ratios compare the observed prevalence in each population with the expected prevalence if that population had the average age-specific AF prevalences of a global GBD sample (2010 total prevalence of 1366/100,000), as reported by Chugh et al [12].
Ethics Statement
All phases of the study were approved by the Institutional Review Boards of the University of New Mexico Health Sciences Center and the University of California, Santa Barbara. Additionally, the Tsimane government (Gran Consejo Tsimane), village leaders, and study participants approved all protocols.
Results
AF Risk Factors
Tsimane and Moseten adults are short in stature (mean = 156 and 155 cm, respectively) with a corresponding low body weight (mean ~59 and 62 kg, respectively) (Tables 1, 2). Mean body mass index (BMI) for Tsimane is 24 kg/m2 and 5% of adults are obese (BMI ≥ 30 kg/m2). Moseten show larger mean BMI (26.0 kg/m2) and higher obesity prevalence (18%).
Tsimane total fasting cholesterol levels are low (mean = 143 mg/dL, and < 1% have an elevated value ≥ 240 mg/dL. Low-density lipoproteins (LDLs) and triglycerides are also low (mean = 87 and 110 mg/dL, respectively). Only 5.5% had LDL ≥ 130 mg/dL and 4% had triglycerides ≥ 200 mg/dL. HDL values were also low (mean = 37.5 mg/dL). Moseten show higher levels of most blood lipids: mean total cholesterol is 159 mg/dL (3% with levels ≥ 240 mg/dL), mean LDL is 106 (22% ≥ 130 mg/dL), mean triglycerides are 132 mg/dL (14% ≥ 200 mg/dL). Only Moseten HDLs (mean = 37.6 mg/dL) are similar to Tsimane levels.
Inflammatory markers are elevated among both Tsimane and Moseten. Median levels of hs-CRP are 2.6 mg/dL for both populations, and nearly half of adults show values > 3.0 mg/dL. ESR is also high and increases with age in both populations: 56% of Tsimane and 58% of Moseten show elevated ESR levels. Interleukin-6 (IL-6) levels are also high, especially at older ages among Moseten (Table 2). Blood pressure (BP) among the Tsimane participants is low, with mean systolic and diastolic BP being 114 mmHg and 70 mmHg, respectively (see also Gurven, Blackwell, Eid, Stieglitz, and Kaplan) [18]. Tsimane hypertension (> 130 mmHg systolic and/or 80 mmHg diastolic) is minimal (9% prevalence) compared to Moseten (37% prevalence).
Prevalence of first-degree block (PR > 200 ms) was rare in both Tsimane and Moseten populations (2%). Across both populations, 6–8% had QRS > 120 ms. Resting heart rates are relatively low, averaging 50.5 and 64.9 beats per minute among Tsimane and Moseten, respectively.
Coronary artery disease as assessed by non-contrast CT scan of coronary calcium (CAC) is largely absent among Tsimane. Mean CAC values range from < 2 Agaston units (AU) for adults aged 40–49 to 68 AU for adults aged 80+ years. Overall, only 3.5% of Tsimane aged 40+ years have a CAC score over 100 AU (considered moderate risk) [17]. Analysis of CAC among Moseten is currently underway.
Only a minority of Tsimane and Moseten, mostly men, smoked regularly. The majority of people who did smoke only smoked a few cigarettes per month. We estimate that the average Tsimane ‘smoker’ smoked < 0.3 pack years in their lifetime. Smoking is more common among Moseten: 39% reported smoking regularly, and the average Moseten smoker smoked 2.6 pack years in their lifetime.
AF Prevalence and Incidence
Tsimane
Only one of 1314 ECGs demonstrated AF (Table 2), yielding a crude prevalence rate of 0.076%, or < 1 person per 1,000 (Table 3). There was one new AF case in 7395 risk years from 1059 adults with > 1 ECG. This represents a crude incidence rate of 0.14 per 1,000 risk years.
Moseten
Only one of 534 ECGs demonstrated AF (Table 2), representing a crude prevalence of 0.187% (1.87 per 1,000). There were no new AF cases in 542 risk years from 311 adults with > 1 ECG (Table 3). Despite observing only one case of AF, we report three observations of premature atrial contractions, which are believed to play a critical role in AF pathogenesis in other populations [41,42]. No cases of atrial flutter were observed among either the Moseten or Tsimane.
Clinical Characteristics of All Three AF Cases
Case 1 (observed in Tsimane prevalence phase): The only person with AF on his first ECG was a 70-year-old man in 2010. At last contact with the study in 2019, he was 79 years of age. Echocardiography demonstrated no valvular or structural heart disease and a normal ejection fraction. No other obvious AF risk factors were observed (BMI = 23 kg/m2, BP: 100/65 mmHg, total cholesterol = 137 mg/dL, LDL = 77 mg/dL, HbA1c = 5.6%). He has had five ECGs conducted by our project physicians from 2010 to 2019, and AF was observed in all of them, consistent with permanent AF.
Case 2 (observed in Tsimane incidence phase): The only adult who developed AF in the incidence phase was an 85-year-old woman whose first medical contact with our project was in 2010. She underwent a standard medical evaluation by a project physician, including an ECG and echocardiogram which demonstrated moderate aortic stenosis. She again received medical attention in August of 2016 for evaluation of an undiagnosed illness. Repeat echocardiography showed severe aortic stenosis and new AF based on the ECG. Three days later she went into pulseless electrical activity and died from end stage aortic stenosis; both prior ECGs showed normal sinus rhythm without left ventricular hypertrophy. Prior observations also showed no obvious AF risk factors (BMI = 20.1 kg/m2, BP: 100/60 mmHg, pulse: 68 bpm, total cholesterol = 94.9 mg/dL, LDL = 45.2 mg/dL).
Case 3 (observed in Moseten prevalence phase): The only resident of a Moseten community with AF was a 72-year-old man. Though he resides in a Moseten village, he and his family migrated there from the Bolivian highlands and he is not of Moseten descent. AF was confirmed on two visits separated by two years (July 2016, July 2018), suggestive of long-standing persistent AF. Echocardiography demonstrated mild to moderate aortic stenosis in 2016. He was obese (BMI = 40.9 kg/m2, total body fat percentage = 38%), diabetic (fasting blood glucose = 241 mg/dL in 2016, and was 122 mg/dL in 2018 after treatment), hypertensive (110/97 mmHg), had elevated resting heart rate (> 90 bpm on multiple occasions), but had low cholesterol (total cholesterol =132 mg/dL, LDL=70.4 mg/dL).
Mortality Selection: One possibility for low AF prevalence and incidence is that the Tsimane or Moseten might experience a high AF case fatality rate given limited treatment options. However, our verbal autopsies revealed at most only two suspected cases where deaths could potentially be attributed to undiagnosed AF: an 88-year-old woman who died of a possible stroke, and a 75-year-old man who died of an apparent myocardial infarction. Both of these individuals were in our ECG sample but had normal rhythm without conduction defects and no evidence of significant pathology prior to their death. It is therefore unlikely that mortality selection could account for the low AF prevalence and incidence rates we report here.
Tsimane and Moseten AF in Comparative Perspective
In order to compare the Tsimane prevalence of AF to other populations, Figure 1 uses indirect standardization to compute age-standardized risk ratios of observed AF prevalence in diverse populations relative to the expected prevalence in those same populations if they had the average age-specific AF prevalences of a 2010 global reference sample from the Global Burden of Disease study of AF [12]. The first cluster (in blue) represents four subsistence populations: the Tsimane, Moseten, and rural samples from Ghana and Tanzania [31,32]. Prevalence rates across all four subsistence populations are exceedingly low, approximately 0.08–0.17 (1/12–1/6 as high as the global average), with overlapping confidence intervals.
The second cluster represents aboriginal and native populations in the U.S., Canada and Australia, who no longer practice a subsistence-based lifestyle. While one Native American sample from the Strong Heart Study [33] shows a relatively low prevalence ratio, about 1/3 of the global reference, it is still 2–4 times higher than observed in subsistence populations. Two additional studies report higher AF prevalence among Native Americans. Ontario Métis natives show highly elevated prevalence (~50% higher) compared to non-native Canadians [35,36,43]. A larger sample of Native Americans from the Veteran’s Administration in 1999, though restricted to men, shows a much higher prevalence among Native Americans than what we report in Figure 1, similar to whites in that study [34]. More recent data show Native Americans of California to have higher incident AF than all other U.S. ethnic groups, attributed in part to excess chronic kidney disease and diabetes [44]. Australian Aborigines living in urban areas exhibit highly elevated AF prevalence, compared to the subsistence populations and global reference analyzed here, though this Aboriginal sample comes from urban hospital admissions over a 10-year period (and hence is not shown in Figure 1) [36]. In that study, Aborigines showed higher AF prevalence at younger ages (< 60 y) and lower AF prevalence at older ages (> 70 y) than non-indigenous Australians.
As a regional comparison, we include tropical and Andean regions of Latin America. Both regions show rates 12–24% higher than the global reference. Western Europe and the GBD designation for ‘developing’ countries show similar AF prevalences as the global reference. North American AF prevalence is 43% higher, and the U.S. specifically is 58% higher, than the global reference. The Asia Pacific region shows the lowest AF prevalence for all post-industrialized countries, at 54% of the global reference.
Discussion
AF is exceedingly rare among Tsimane and Moseten Amerindians of Bolivia: we found just one AF case in the prevalence phase of each population and one case in the incidence phase of the Tsimane. AF prevalence was therefore 8–18% that of Western Europe, and 5–11% that of the United States. It is also 15–31% that of Asia Pacific, which is the GBD world region with the lowest rates of AF [12]. The combined crude incidence rate of AF for Tsimane and Moseten is 0.13 per thousand risk years.
Tsimane and Moseten exhibit minimal AF despite having several traditional risk factors, including elevated inflammatory biomarkers (e.g., CRP, IL-6, ESR [22]), and low HDL. The fact that AF is almost absent among Tsimane and Moseten suggests that the source of inflammation itself may play a role in AF etiology [17,26]. In rural Bolivia, most inflammation comes from diverse infections (bacterial, parasitic, viral) that afflict individuals from a young age, while among many sedentary industrialized populations, the combination of obesity, cigarette smoking, air pollution, and other factors promotes chronic low-grade inflammation [45]. Given the heavy chronic infectious burden amongst the Tsimane and Moseten, and potential links between pathogen burden and the development of AF [46], one would expect to have found more cases of AF than observed. This interesting finding calls into question the particular inflammatory pathways that lead to AF. In industrialized populations, low HDL is also considered a moderate risk factor for AF [27]; this does not appear to be the case for Tsimane and Moseten, where over half of all individuals have low HDL but also low LDL and negligible AF risk.
AF has an exceptionally low prevalence in the four subsistence populations where it has been measured (Figure 1) [31,32]. While many traditional AF risk factors were low in these populations, the two African populations showed higher levels of hypertension, suggesting that hypertension alone is insufficient to increase AF risk. Despite being the most common medical condition associated with AF worldwide [6], hypertension likely must interact with other cardiovascular disease risk factors like dyslipidemia, diabetes, and sedentary lifestyle to increase AF susceptibility. Low AF risk among the two African populations, and in sub-Saharan African countries more generally, are also noteworthy given high reported stroke incidences in the region [47]. AF patients in sub-Saharan Africa also tend to be younger than in other world regions, and experience high case fatality and rheumatic valvular heart disease [48]. AF incidence is expected to increase substantially in sub-Saharan Africa over the next few decades [12,48], highlighting the need for more research on AF etiology in the region. The Tsimane and Moseten also exhibit greater systemic inflammation and lower HDL than other subsistence populations, but this does not appear to lead to greater AF prevalence. These observations in subsistence populations suggest that multiple risk factors in concert may be necessary to increase AF risk.
Despite the fact that Moseten lead a more modernized lifestyle than Tsimane, they do not manifest significantly higher AF prevalence or incidence. As most lifestyle differences among Moseten have occurred in the past three decades, it is possible that older Moseten have largely had similar cumulative exposures as age-matched Tsimane. Our results therefore suggest that lifecourse, or perhaps particularly early life, exposures warrant consideration beyond biomarkers assessed in later adulthood. An expectation is that differences in AF incidence, and presumably CVD, diabetes, and related comorbidities, will increasingly manifest in younger adults over time.
Limitations
In order to reduce measurement bias when assessing AF prevalence, we took steps to make sure that people who were not sampled (n = 68 individuals, 4.6% of the study population) were not missed due to illness or other comorbidities that could be associated with AF. However, people not sampled were likely among the healthiest, either traveling to other villages or locations during team visits, or too busy working that they declined medical attention (very few individuals, Figure S1, S2).
While mortality selection might explain why indigenous Australians have higher AF prevalence than non-indigenous Australians only before age 60 years [36], it does not explain the low levels of AF risk we report among Tsimane and Moseten. Consistent with what we report for verbal autopsies, an earlier study examining retrospective causes of death among Tsimane similarly reported minimal evidence of strokes or infarcts [49]. A study of stroke incidence among another Bolivian Amazonian population (Chiquitano) also reported very low incidence (174/100,000) over a one-year period [50].
Another potential weakness is that we only performed resting 12-lead ECGs, which sample 10 seconds at a time. With our methodology, it would be difficult to detect cases of intermittent or paroxysmal AF. It has been proposed that paroxysmal AF may be more common in some ethnicities than the persistent AF usually reported for Caucasians, especially among ethnicities with higher stroke risk [51]. Thus, it is possible that we and others using similar methods may be underestimating AF. Indeed, the use of higher-sensitivity detection methods has been shown to reduce ethnic differences in AF prevalence [52]. Nevertheless, the comparative data from other population-level studies relied on similar ECG methodology, and so our results are comparable to most studies reported in Figure 1.
Lastly, we acknowledge that ~140 genetic loci affecting AF have been identified to date among participants mostly of European descent [53]. Genetic risk prediction of AF is still in its infancy, and the relevance of these loci and ancestry-specific rare variants in contributing to the low AF prevalence among Tsimane, Moseten, and other subsistence populations remains to be determined.
Conclusion
Our findings of exceptionally low AF prevalence and incidence among rural Bolivian horticulturalists suggest that a subsistence lifestyle with high rates of physical activity and a diet relatively low in processed carbohydrates and harmful fats can be heart-healthy despite high levels of inflammation and low HDLs. Some lifestyle alterations associated with incipient modernization may be insufficient to increase AF risk, as suggested here by similar AF prevalences among Tsimane and Moseten. AF prevalence is higher among indigenous populations that are no longer living a traditional subsistence lifestyle, suggesting that combined changes in physical activity, diet, and other risk factors associated with marginalization, discrimination, and lifestyle disruption can increase vulnerability to AF, especially when coupled with low access to quality healthcare. Rather than being viewed as an inevitable feature of cardiovascular aging, it appears that AF is better viewed as a modifiable lifestyle disease with ample scope for prevention.
Data Accessibility Statement
Code and anonymized, disguised data are provided to recreate Tables 1, 2, 3 and Supplementary Table S1: https://github.com/babeheim/tsimane-afib. Undisguised but anonymous data, however, can be shared upon reasonable request to the corresponding author.
Additional Files
The additional files for this article can be found as follows:
STROBE Diagram for Tsimane subject recruitment. N = 1871 refers to all Tsimane who were at least age 40 years from 2005–2019, considering that the THLHP medical team sampled adults age 40+ throughout the entire study period (i.e. not only at baseline). N = 1314 adults had at least one ECG. 557 adults were not sampled, either because ECGs were not measured on all medical rounds (most common, largely due to damaged equipment, lack of electricity, and in some cases lack of time), or because adults were either not present in the village during visits when ECGs assessed (common reason), or were present in the community but did not show up for their clinical visit (less common). 255 adults were lost to follow-up, due either to not being in the village during follow-up visits (most common), being present but not showing up for their clinical visit (less common), or being seen by project physicians but refusing an ECG (rare).
STROBE Diagram for Moseten subject recruitment. The prevalence phase is based on one medical round in 2015–2016; incidence phase is based on a follow-up visit in 2017–2018. Of the 561 eligible Moseten aged 40+ years, 20 were either not present in the community during THLHP visits (most common), or were present but did not visit our mobile clinic (less common). Loss to follow-up during the second visit was due to not revisiting all of the same villages seen during the prevalence phase, and slightly poorer attendance at our clinic.
Potential sample bias in prevalence and incidence phases. Biomarker comparisons between those who received or did not receive an ECG during the prevalence phase, and those who did or did not receive a follow-up ECG in the incident phase. Mean values are compared using student t-tests. Blue color indicates lower AF risk among unsampled adults, whereas red color indicates higher AF risk. In the prevalence phase, unsampled Tsimane and Moseten are similar or show lower AF risk than those sampled with an ECG. In the incidence phase, Tsimane from the prevalence phase who were lost to follow-up ECG showed only slightly higher AF risk than those sampled (2.1 years older, 2.6 mg/dL lower HDL, 1.8 mmHg higher systolic blood pressure, 6.5 mm/hr higher ESR), though also show lower AF risk for LDL (14 mg/dL lower) and total cholesterol (13.3 mg/dL lower). Among Moseten, those lost to follow-up showed only slightly higher BMI (0.9 kg/m2 higher).
Acknowledgements
We thank the Tsimane and Moseten for their continuing hospitality, collaboration, support, and friendship over the years. Special thanks to THLHP personnel for their herculean efforts and dedication. We also thank the HORUS research team for their deep involvement. JS acknowledges IAST funding from the French National Research Agency under the Investments for the Future (Investissements d’Avenir) programme (ANR-17-EURE-0010).
Funding Statement
The Tsimane Health and Life History Project (THLHP) is funded by the National Institute on Aging within the National Institutes of Health (RF1AG054442; R01AG024119, R56AG024119).
Contributor Information
Gregory S. Thomas, Email: GThomas1@memorialcare.org.
Hillard S. Kaplan, Email: hkaplan@chapman.edu.
Michael D. Gurven, Email: gurven@anth.ucsb.edu.
Ethics and Consent
All phases of the study were approved by the Institutional Review Boards of the University of New Mexico Health Sciences Center and the University of California, Santa Barbara. Additionally, the Tsimane government (Gran Consejo Tsimane), village leaders, and study participants approved all protocols.
Funding Information
The Tsimane Health and Life History Project (THLHP) is funded by the National Institute on Aging within the National Institutes of Health (RF1AG054442; R01AG024119, R56AG024119).
Competing Interests
The authors have no competing interests to declare.
Author Contributions
CJR, HK, MG, BT, and GT contributed to the conception of the paper. DER, ECL, RQG, and JCA collected the data. CJR, GST, KT, LSW, ME, and MIM evaluated ECGs. BB, DC, ES, and TK organized databases and curated the data. ES and BB analyzed data. MG, CJR, and HK wrote the paper. BT, GT, ME, and JS critically revised the paper. MG and GT led efforts to complete the paper from start to finish. All authors gave final approval and agreed to be accountable for all aspects of work, ensuring integrity and accuracy. All authors had access to the data and a role in writing the manuscript.
References
- 1.Schnabel RB, Yin X, Gona P, et al. 50 year trends in atrial fibrillation prevalence, incidence, risk factors, and mortality in the Framingham Heart Study: A cohort study. The Lancet. 2015; 386(9989): 154–162. DOI: 10.1016/S0140-6736(14)61774-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Go A. Prevalence of atrial fibrillation in adults: National implications for rhythm management and stroke prevention: The ATRIA Study. JAMA. 2001; 285(18): 2370 DOI: 10.1001/jama.285.18.2370 [DOI] [PubMed] [Google Scholar]
- 3.Chugh S, et al. Epidemiology and natural history of atrial fibrillation: Clinical implications. JACC. 2001; 37(2): 371 DOI: 10.1016/S0735-1097(00)01107-4 [DOI] [PubMed] [Google Scholar]
- 4.January CT, Wann LS, Alpert JS, et al. 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation. Journal of the American College of Cardiology. 2014; 64(21): e1 DOI: 10.1016/j.jacc.2014.03.022 [DOI] [PubMed] [Google Scholar]
- 5.Mea K. Estimation of total incremental health care costs in patients with atrial fibrillation in the United States. Circulation: Cardiovascular Quality and Outcomes. 2011; 4: 313–320. DOI: 10.1161/CIRCOUTCOMES.110.958165 [DOI] [PubMed] [Google Scholar]
- 6.Rahman F, Kwan GF, Benjamin EJ. Global epidemiology of atrial fibrillation. Nature Reviews Cardiology. 2014; 11(11): 639–54. DOI: 10.1038/nrcardio.2014.118 [DOI] [PubMed] [Google Scholar]
- 7.Lippi G, Sanchis-Gomar F, Cervellin G. Global epidemiology of atrial fibrillation: An increasing epidemic and public health challenge. International Journal of Stroke. 2020. DOI: 10.1177/1747493019897870 [DOI] [PubMed] [Google Scholar]
- 8.Colilla S, Crow A, Petkun W, Singer DE, Simon T, Liu X. Estimates of current and future incidence and prevalence of atrial fibrillation in the U.S. adult population. American Journal of Cardiology. 112(8): 1142–1147. DOI: 10.1016/j.amjcard.2013.05.063 [DOI] [PubMed] [Google Scholar]
- 9.Zoni-Berisso M, Lercari F, Carazza T, Domenicucci S. Epidemiology of atrial fibrillation: European perspective. Clinical Epidemiology. 2014; 6: 213–220. DOI: 10.2147/CLEP.S47385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Aviles RJ, Martin DO, Apperson-Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003; 108(24): 3006–3010. DOI: 10.1161/01.CIR.0000103131.70301.4F [DOI] [PubMed] [Google Scholar]
- 11.El-Chami MF, Brancato C, Langberg J, Delurgio DB, Bush H, Brosius L, Leon AR. QRS duration is associated with atrial fibrillation in patients with left ventricular dysfunction. Clinical Cardiology. 2010; 33(3): 132–8. DOI: 10.1002/clc.20714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chugh SS, Havmoeller R, Narayanan K, et al. Worldwide epidemiology of atrial fibrillation: A Global Burden of Disease 2010 Study. Circulation. 2014; 129(8): 837–847. DOI: 10.1161/CIRCULATIONAHA.113.005119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Schnabel R, et al. Development of a risk score for atrial fibrillation in the community: The Framingham heart study. Lancet. 2009; 373(9665): 739–45. DOI: 10.1016/S0140-6736(09)60443-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gurven M, Jaeggi AV, Kaplan H, Cummings D. Physical activity and modernization among Bolivian Amerindians. PLoS ONE. 2013; 8(1): e55679 DOI: 10.1371/journal.pone.0055679 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gurven M, Stieglitz J, Trumble BC, et al. The Tsimane health and life history project: Integrating anthropology and biomedicine. Evolutionary Anthropology. 2017. DOI: 10.1002/evan.21515 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kraft TS, Stieglitz J, Trumble BC, Martin M, Kaplan H, Gurven M. Nutrition transition in 2 lowland Bolivian subsistence populations. The American Journal of Clinical Nutrition. 2018; 108(6): 1183–1195. DOI: 10.1093/ajcn/nqy250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kaplan H, Thompson R, Trumble BC, et al. Indigenous South American Tsimane demonstrate the lowest levels of coronary atherosclerosis. Lancet. 2017; S0140(6736): 30752–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gurven M, Blackwell A, Eid D, Stieglitz J, Kaplan H. Does blood pressure inevitably rise with age? Longitudinal evidence among forager-horticulturalists. Hypertension. 2012; 60(1). DOI: 10.1161/HYPERTENSIONAHA.111.189100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Vasunilashorn Sea. Blood lipids, infection and inflammatory markers in the Tsimane of Bolivia. Journal of Human Biology. 22: 731–740. DOI: 10.1002/ajhb.21074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Sanchis-Gomar F, Perez-Quilis C, Lippi G, et al. Atrial fibrillation in highly trained endurance athletes—Description of a syndrome. International Journal of Cardiology. 2017; 226: 11–20. DOI: 10.1016/j.ijcard.2016.10.047 [DOI] [PubMed] [Google Scholar]
- 21.Gurven M, Kaplan H, Winking J, et al. Inflammation and infection do not promote arterial aging and cardiovascular disease among lean Tsimane forager-horticulturalists. PLoS ONE. 2009; 4(8): e6590 DOI: 10.1371/journal.pone.0006590 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hu Y-F, Chen Y-J, Lin Y-J, Chen S-A. Inflammation and the pathogenesis of atrial fibrillation. Nature Reviews Cardiology. 2015; 12(4): 230 DOI: 10.1038/nrcardio.2015.2 [DOI] [PubMed] [Google Scholar]
- 23.Chung MK, Martin DO, Sprecher D, et al. C-reactive protein elevation in patients with atrial arrhythmias. Circulation. 2001; 104(24): 2886 DOI: 10.1161/hc4901.101760 [DOI] [PubMed] [Google Scholar]
- 24.Aviles RJ, Martin DO, Apperson-Hansen C, et al. Inflammation as a risk factor for atrial fibrillation. Circulation. 2003; 108(24): 3006 DOI: 10.1161/01.CIR.0000103131.70301.4F [DOI] [PubMed] [Google Scholar]
- 25.Blackwell AD, Martin M, Kaplan H, Gurven M. Antagonism between two intestinal parasites in humans: The importance of co-infection for infection risk and recovery dynamics. Proceedings of the Royal Society B: Biological Sciences. October 22, 2013; 280(1769). DOI: 10.1098/rspb.2013.1671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blackwell AD, Trumble BC, Maldonado Suarez I, et al. Immune function in Amazonian horticulturalists. Annals of Human Biology. 2016:1–45. DOI: 10.1080/03014460.2016.1189963 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chamberlain AM, Agarwal SK, Ambrose M, Folsom AR, Soliman EZ, Alonso A. Metabolic syndrome and incidence of atrial fibrillation among blacks and whites in the Atherosclerosis Risk in Communities (ARIC) Study. American Heart Journal. 2010; 159(5): 850–856. DOI: 10.1016/j.ahj.2010.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Whelton PK, Carey RM, Aronow WS, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: A report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Journal of the American College of Cardiology. 2017; 24430 DOI: 10.22141/2307-1257.7.1.2018.122220 [DOI] [PubMed] [Google Scholar]
- 29.Fuster V, Rydén LE, Cannom DS, et al. Guidelines for the management of patients with atrial fibrillation: A report of the American College Of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology committee for practice guidelines: Developed in collaboration with the European Heart Rhythm Association and the Heart Rhythm Society. Circulation. 2006; 114(7): e257–e354. [DOI] [PubMed] [Google Scholar]
- 30.World Health Organization. Verbal autopsy standards: 2012 WHO Verbal Autopsy Instrument. 2012. [Google Scholar]
- 31.Koopman JJ, van Bodegom D, Westendorp RG, Jukema JW. Scarcity of atrial fibrillation in a traditional African population: A community-based study. BMC Cardiovascular Disorders. 2014; 14(1): 87 DOI: 10.1186/1471-2261-14-87 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Dewhurst MJ, Adams PC, Gray WK, et al. Strikingly low prevalence of atrial fibrillation in elderly Tanzanians. Journal of the American Geriatrics Society. 2012; 60(6): 1135–1140. DOI: 10.1111/j.1532-5415.2012.03963.x [DOI] [PubMed] [Google Scholar]
- 33.Oopik AJ, Dorogy M, Devereux RB, et al. Major electrocardiographic abnormalities among American Indians aged 45 to 74 years (the Strong Heart Study). American Journal of Cardiology. 1996; 78(12): 1400–1405. DOI: 10.1016/S0002-9149(96)00642-X [DOI] [PubMed] [Google Scholar]
- 34.Borzecki AM, Liebschutz JM, Berlowitz DR. Racial differences in the prevalence of atrial fibrillation among males. Journal of the National Medical Association. 2008; 100(2): 237 DOI: 10.1016/S0027-9684(15)31212-8 [DOI] [PubMed] [Google Scholar]
- 35.Atzema CL, Khan S, Lu H, et al. Cardiovascular disease rates, outcomes, and quality of care in Ontario Métis: A population-based cohort study. PLoS One. 2015; 10(3): e0121779 DOI: 10.1371/journal.pone.0121779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Wong CX, Brooks AG, Cheng Y-H, et al. Atrial fibrillation in Indigenous and non-Indigenous Australians: A cross-sectional study. BMJ Open. 2014; 4(10): e006242 DOI: 10.1136/bmjopen-2014-006242 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Heeringa J, van der Kuip DA, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: The Rotterdam study. European Heart Journal. 2006; 27(8): 949–953. DOI: 10.1093/eurheartj/ehi825 [DOI] [PubMed] [Google Scholar]
- 38.Majeed A, Moser K, Carroll K. Trends in the prevalence and management of atrial fibrillation in general practice in England and Wales, 1994–1998: Analysis of data from the general practice research database. Heart. 2001; 86(3): 284–288. DOI: 10.1136/heart.86.3.284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Marcolino MS, Palhares DM, Benjamin EJ, Ribeiro AL. Atrial fibrillation: Prevalence in a large database of primary care patients in Brazil. EP Europace. 2015; 17(12): 1787–1790. DOI: 10.1093/europace/euv185 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Naccarelli GV, Varker H, Lin J, Schulman KL. Increasing prevalence of atrial fibrillation and flutter in the United States. American Journal of Cardiology. 2009; 104(11): 1534–1539. DOI: 10.1016/j.amjcard.2009.07.022 [DOI] [PubMed] [Google Scholar]
- 41.Dewland TA, Vittinghoff E, Mandyam MC, et al. Atrial ectopy as a predictor of incident atrial fibrillation: A cohort study. Annals of Internal Medicine. 2013; 159(11): 721–728. DOI: 10.7326/0003-4819-159-11-201312030-00004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Hoffmann E, Sulke N, Edvardsson N, et al. New Insights into the initiation of atrial fibrillation. Circulation. 2006; 113(16): 1933–1941. DOI: 10.1161/CIRCULATIONAHA.105.568568 [DOI] [PubMed] [Google Scholar]
- 43.McGrady M, Krum H, Carrington MJ, et al. Heart failure, ventricular dysfunction and risk factor prevalence in Australian Aboriginal peoples: The Heart of the Heart Study. Heart. 2012; 98(21): 1562–1567. DOI: 10.1136/heartjnl-2012-302229 [DOI] [PubMed] [Google Scholar]
- 44.Sanchez JM, Jolly SE, Dewland TA, et al. Incident atrial fibrillation among American Indians in California. Circulation. 2019; 140(19): 1605–1606. DOI: 10.1161/CIRCULATIONAHA.119.042882 [DOI] [PubMed] [Google Scholar]
- 45.Gurven MD, Trumble BC, Stieglitz J, et al. Cardiovascular disease and type 2 diabetes in evolutionary perspective: A critical role for helminths? Evolution, Medicine, and Public Health. 2016; 2016(1): 338–357. DOI: 10.1093/emph/eow028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gundlund A, Olesen JB, Butt JH, et al. One-year outcomes in atrial fibrillation presenting during infections: A nationwide registry-based study. European Heart Journal. 2020; 41(10): 1112–1119. DOI: 10.1093/eurheartj/ehz873 [DOI] [PubMed] [Google Scholar]
- 47.Owolabi MO, Akarolo-Anthony S, Akinyemi R, et al. The burden of stroke in Africa: A glance at the present and a glimpse into the future. Cardiovasc J Afr. Mar-Apr 2015; 26(2 Suppl 1): S27–S38. DOI: 10.5830/CVJA-2015-038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Stambler BS, Ngunga LM. Atrial fibrillation in sub-Saharan Africa: epidemiology, unmet needs, and treatment options. International Journal of General Medicine. 2015; 8: 231 DOI: 10.2147/IJGM.S84537 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Gurven M, Kaplan H, Supa AZ. Mortality experience of Tsimane Amerindians of Bolivia: Regional variation and temporal trends. American Journal of Human Biology. 2007; 19(3): 376–398. DOI: 10.1002/ajhb.20600 [DOI] [PubMed] [Google Scholar]
- 50.Heckmann J, Kolominsky-Rabas P, Heuschmann P, Erbguth F, Neundörfer B, Galeote J. Low incidence of stroke in the Chiquitanos tribe in the Bolivian lowlands. Stroke. 2000; 31(9): 2266 DOI: 10.1161/01.STR.31.9.2266-d [DOI] [PubMed] [Google Scholar]
- 51.Soliman EZ, Prineas RJ, Case LD, Zhang Z-m, Goff DC, Jr. Ethnic distribution of ECG predictors of atrial fibrillation and its impact on understanding the ethnic distribution of ischemic stroke in the Atherosclerosis Risk in Communities (ARIC) study. Stroke. 2009; 40(4): 1204–1211. DOI: 10.1161/STROKEAHA.108.534735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Prineas RJ, Soliman EZ, Howard G, et al. The sensitivity of the method used to detect atrial fibrillation in population studies affects group-specific prevalence estimates: Ethnic and regional distribution of atrial fibrillation in the REGARDS study. Journal of Epidemiology. 2009: 0906190091–0906190091. DOI: 10.2188/jea.JE20081032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Roselli C, Rienstra M, Ellinor PT. Genetics of atrial fibrillation in 2020: GWAS, genome sequencing, polygenic risk, and beyond. Circulation Research. 2020; 127(1): 21–33. DOI: 10.1161/CIRCRESAHA.120.316575 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
STROBE Diagram for Tsimane subject recruitment. N = 1871 refers to all Tsimane who were at least age 40 years from 2005–2019, considering that the THLHP medical team sampled adults age 40+ throughout the entire study period (i.e. not only at baseline). N = 1314 adults had at least one ECG. 557 adults were not sampled, either because ECGs were not measured on all medical rounds (most common, largely due to damaged equipment, lack of electricity, and in some cases lack of time), or because adults were either not present in the village during visits when ECGs assessed (common reason), or were present in the community but did not show up for their clinical visit (less common). 255 adults were lost to follow-up, due either to not being in the village during follow-up visits (most common), being present but not showing up for their clinical visit (less common), or being seen by project physicians but refusing an ECG (rare).
STROBE Diagram for Moseten subject recruitment. The prevalence phase is based on one medical round in 2015–2016; incidence phase is based on a follow-up visit in 2017–2018. Of the 561 eligible Moseten aged 40+ years, 20 were either not present in the community during THLHP visits (most common), or were present but did not visit our mobile clinic (less common). Loss to follow-up during the second visit was due to not revisiting all of the same villages seen during the prevalence phase, and slightly poorer attendance at our clinic.
Potential sample bias in prevalence and incidence phases. Biomarker comparisons between those who received or did not receive an ECG during the prevalence phase, and those who did or did not receive a follow-up ECG in the incident phase. Mean values are compared using student t-tests. Blue color indicates lower AF risk among unsampled adults, whereas red color indicates higher AF risk. In the prevalence phase, unsampled Tsimane and Moseten are similar or show lower AF risk than those sampled with an ECG. In the incidence phase, Tsimane from the prevalence phase who were lost to follow-up ECG showed only slightly higher AF risk than those sampled (2.1 years older, 2.6 mg/dL lower HDL, 1.8 mmHg higher systolic blood pressure, 6.5 mm/hr higher ESR), though also show lower AF risk for LDL (14 mg/dL lower) and total cholesterol (13.3 mg/dL lower). Among Moseten, those lost to follow-up showed only slightly higher BMI (0.9 kg/m2 higher).
Data Availability Statement
Code and anonymized, disguised data are provided to recreate Tables 1, 2, 3 and Supplementary Table S1: https://github.com/babeheim/tsimane-afib. Undisguised but anonymous data, however, can be shared upon reasonable request to the corresponding author.


