Abstract
Aim
To define both competencies and envisaged outcomes for registered nurses in expanded roles in Swiss nursing homes to be implemented and evaluated within a new model of care.
Background
In regions where Advanced Practice Nurses are rare or absent, registered nurses take up clinical leadership and expanded roles. To allow effective implementation, monitoring and evaluation of these nurses, stakeholders need a shared understanding of the competencies they require and what outcomes they should achieve.
Design
RAND/UCLA Appropriateness Method – a modified Delphi method.
Methods
A critical literature review and case studies were conducted to identify possible competencies and outcomes for registered nurses in expanded roles. In 2017, a two‐round rating process and an in‐person panel discussion was completed by a group of multi‐professional stakeholders.
Findings
Two rounds generated 190 competencies and 72 outcomes relevant to registered nurses in expanded roles.
Conclusion
The relevant competencies and outcomes of registered nurses in expanded roles indicate their support for care teams and development of nursing care in nursing homes. Their geriatric expertise allows them to function as role models and innovators, reinforcing overall perceptions of nursing as a profession. These nurses are especially important in countries and settings where Advanced Practice Nurses are scarce or unavailable.
Impact
The identified competencies clarify the duties of expanded‐role registered nurses, thereby differentiating them from other care providers. Although conducted in the Swiss healthcare system, our methods and findings can be adapted to other healthcare settings. The results of this study will guide the development of an educational programme in a multi‐centre study to reduce avoidable hospitalizations, while the defined outcomes guide the evaluation of their impact.
Keywords: competencies, Delphi, expanded role, model of care, nurse, nursing homes, outcomes, RAND UCLA
Abstract
目的
定义在瑞士养老院中,在新型护理模式下所实施并评估的,角色拓展的注册护士的能力和设想结果。
背景
在高级执业护士稀缺或缺乏的地区,注册护士充当了临床领导以及各种拓展的角色。为了能够有效实施、监测、评估这些护士,相关人员需要就他们所需的能力和应取得的结果达成共识。
设计
RAND/UCLA适当方法——改进的德尔菲法
方法
进行关键文献综述及个案研究,以识别注册护士的合理能力和结果,这些护士充当了各种拓展的角色。2017年,一组多专业的相关人员完成了两轮评分程序,并亲自参加了一场专题讨论会。
发现
两轮评分程序产生了190种能力和72种结果,均和充当了各种扩展角色的注册护士相关。
结论
充当各种扩展角色的注册护士,就其相关能力和结果而论,表明了他们在护理团队和养老院护理发展中的支撑作用。他们对老年人的专业知识使其成为榜样和创新者,巩固了护理作为一种职业的整体看法。在高级执业护士稀缺或缺乏的城市中,这些护士更为重要。
影响
这些能力可明确充当各种扩展角色的注册护士职责,将其区别于其他护理提供者。尽管是在瑞士医疗系统中进行,我们的方法和发现同样可适用于其他医疗环境。可利用本研究结果指导制定多中心研究的教育计划,减少可避免的住院治疗,并且,明确的结果将可适用于影响评估。
1. INTRODUCTION
Globally rising numbers of older persons are forcing fundamental changes in primary care provision. Nursing homes (NHs) are especially challenged to provide high quality and care at costs affordable to residents, many of whom are chronically ill and frail (Colombo et al., 2011; World Health Organization, 2015). In this context, geriatric‐trained healthcare professionals working in interprofessional teams are developing new models of care (Berwick et al., 2008; Colombo et al., 2011; McGilton et al., 2016; World Health Organization, 2015).
As these models often require competencies beyond those of normal registered nurses (RNs), some countries fill the new roles with primary care nurse practitioners, for example, Advanced Practice Nurses (APNs), to manage NH residents (Maier et al., 2017; Mezey et al., 2005). However, in most European countries APNs are not well established (World Health Organization, 2020). Consequently, RNs' roles are being re‐examined and re‐designed (Lamb et al., 2015; Smolowitz et al., 2015). Growing evidence indicates that, in collaboration with other primary care practitioners, expanded‐role RNs are ideally positioned to manage older people with chronic conditions (Bodenheimer & Mason, 2017; Martin‐Misener & Bryant‐Lukosius, 2014; McGilton et al., 2016; Smolowitz et al., 2015).
This study's purpose was to define relevant competencies and outcomes to be achieved by RNXs working in a new Swiss NH care model that aims to reduce unplanned hospitalizations. The results will guide the development of a structured educational programme and associated outcome evaluation in eleven intervention NHs, while supporting RNXs' sustainability and scalability.
1.1. Background
1.1.1. RNXs in nursing homes
In the NH context, resident care demands interprofessional teams of geriatric‐trained healthcare professionals (Berwick et al., 2008; Colombo et al., 2011; McGilton et al., 2016; World Health Organization, 2015). However, with care needs outstripping available staffing, resources are stretched to their limits. The ratio of primary care practitioners – that is, professionals authorized to diagnose, treat and bill for their services – to patients is currently insufficient for the NH population (Colombo et al., 2011; McGilton et al., 2016; World Health Organization, 2015). To fill this gap, other professionals must be prepared to oversee and deliver primary care within new models of care.
These new models of care can benefit hugely from the addition of RNXs to NHs' interprofessional care teams (Bauer & Bodenheimer, 2017; Bodenheimer & Mason, 2017; Smolowitz et al., 2015). The roles they take on differ importantly from those of regular RNs or licensed practical nurses (LPNs). As clinical leaders, RNXs with additional geriatric care training can improve the quality of chronic care management and care coordination, while guiding and facilitating interprofessional collaboration towards person‐centred care and empowering care staff (Bauer & Bodenheimer, 2017; Donald et al., 2013; McGilton et al., 2016; Smolowitz et al., 2015). Lastly, they can both leverage primary practitioners' resident visit time and provide an attractive next step in a long‐term care nursing career.
In recent decades, as neither assistant/associate physicians nor APNs roles are yet fully established or regulated, many Swiss NHs have employed RNXs with various educational backgrounds to address the need for geriatric expertise in NHs. In fact, 70% of European countries have no experience with APNs (World Health Organization, 2020). In Switzerland, for example, as of the end of 2015, while 328 APNs had graduated from the Swiss master's‐level programme; nearly all were practicing in hospitals, not NHs (Maier et al., 2017). Instead, in NHs, many RNs had upgraded their qualifications via certificates, diplomas, or Masters of Advanced Studies in areas such as geriatrics, dementia, or palliative care to assume the necessary expanded roles. Others took up those roles based on field experience enriched by ongoing training, education and local NH needs (Ryan, 2003).
1.1.2. Development of RNXs
Swiss NHs developed their first RNXs ad hoc, with limited public or professional oversight. As a result, neither have their competencies ever been comprehensively catalogued nor is there evidence on their effectiveness. Competencies include attributes such as knowledge, acquired through experience and study and psychomotor (e.g., delivering injections) and affective skills (e.g., attitudes and feelings) needed to deliver care (International Council of Nurses, 2005). We expect specific competencies to be related to specific target patient outcomes (Donabedian, 1988).
While work has been conducted to establish competencies related specifically to care for older people (American Association of Colleges of Nursing, 2020), such definitions usually consider APNs with master's‐level education working in broadly understood primary care rather than in NH‐specific contexts. Others include definitions of competencies for care of older people by RNs without expanded roles (Bing‐Jonsson et al., 2015; Kiljunen et al., 2017). In collaboration with stakeholders, clear definition of RNXs' competencies and target outcomes is essential both to monitor and evaluate their effectiveness and to disambiguate them from other professionals. It also supports the building of an attractive career pathway in the NH setting, which increases the status of nursing work in this area (Bryant‐Lukosius & DiCenso, 2004; Maier et al., 2017). Lastly, clearly defining RNXs' roles could add to their sustainability both by guiding geriatric curriculum development to match specific NH needs and by enabling international comparison (Peters et al., 2013).
2. THE STUDY
2.1. Aim
This study aims to define both RNXs' competencies and the envisaged outcomes of their clinical work. The results will support the definition of RNXs embedded in a new Swiss model of nursing home care. This, in turn, will guide the development of a structured educational curriculum.
2.2. INTERCARE intervention
This study is part of the INTERCARE project, which will introduce a new care model that will rely on RNXs, who will be called INTERCARE nurses (Zúñiga et al., 2019). The INTERCARE model aims to improve the quality of NH care and interprofessional collaboration while reducing unplanned resident hospitalizations. To guarantee the new care model's sustainability and scalability, both the necessary RNXs and the structured educational programme will be implemented and evaluated regarding its effectiveness in eleven NHs. By consulting with a broad stakeholder group, it will also adhere at every stage to the principles of Public Patient Involvement (Involve, 2012).
2.3. Design
To define relevant competencies and outcomes for nursing‐home RNXs, the RAND/UCLA method – a modified Delphi method – was used iteratively and independently in two rating rounds with stakeholders (Fitch et al., 2000). To define a clear set of competencies and make them comparable, we divided all competencies into seven core areas following the Hamric model (Hamric, 2015) and stratified all outcomes onto four levels (Figure 1). The study consists of two phases: (a) development of the questionnaire survey; and (b) two expert rating rounds based on RAND/UCLA (Figure 1).
FIGURE 1.
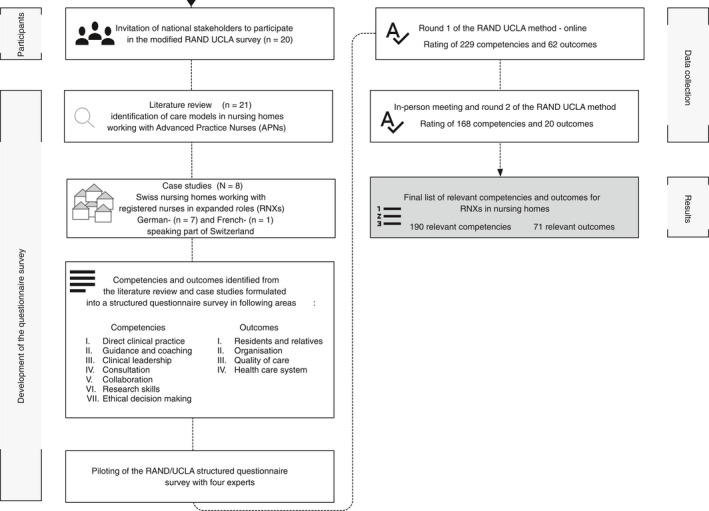
Flow chart of the RAND/UCLA method – a modified Delphi method
2.4. Participants
A purposive sample was used. Twenty national stakeholders (60% female) from 20 organizations were invited to participate in the modified RAND/UCLA survey (Table 1). A stakeholder was eligible if he/she was directly or indirectly involved in any Swiss healthcare sector for older adults – as a patient representative, healthcare provider, other professional or policymaker and understood German (Concannon et al., 2012). To include contextual variations, we assured the representation of each of Switzerland's three (German, French and Italian) language regions.
TABLE 1.
Overview of stakeholders from Swiss institutions invited to participate and included in the RAND/UCLA method – a modified Delphi method
| Institutions represented | Sex a | 1st round b | 2nd round b |
|---|---|---|---|
| Patients, residents and older persons groups | |||
| Federal (n = 2) | |||
| Swiss Organisation for Patient Protection SPO | F | Y | Y |
| Swiss Alzheimer Association | F | Y | N |
| Cantonal level (n = 1) | |||
| Dementia network of both cantons of Basel | M | N | Y |
| Professionals | |||
| Physician (n = 3) | |||
| Swiss Society of General Internal Medicine | M | Y | Y |
| Swiss Society for Geriatrics SFGG – a nursing home‐based geriatrician | M | Y | Y |
| Swiss Society for Geriatrics SFGG – an acute geriatric care geriatrician | M | ‐ | ‐ |
| Educational institutions (n = 1) | |||
| Swiss Association of Education Centers. Health and Social Affairs | M | Y | N |
| Nursing stakeholders and other care worker representatives (n = 6) | |||
| Academic Society for Gerontological Nursing | F | Y | Y |
| Swiss Interest Group of Nurse Aides | F | Y | Y |
| Swiss Association for Nursing Science | F | Y | N |
| Swiss professional association for long‐term care | F | Y | Y |
| Professional Association Palliative ch, nursing expert group | M | Y | Y |
| Healthcare providers | |||
| Nursing homes representatives (n = 4) | |||
| Curaviva Switzerland – Swiss Association of Institutions for Persons Requiring Support | F | Y | Y |
| Curaviva Baselland – Cantonal Association of Institutions for Persons Requiring Support | F | Y | Y |
| Friborg Association of Institutions for the Elderly (AFIPA‐VFA) | M | ‐ | ‐ |
| Swiss association of economically independent retirement and care homes – Senesuisse | M | ‐ | ‐ |
| Nursing management (n = 1) | |||
| Swiss Nurse Leaders | F | ‐ | ‐ |
| Policy makers | |||
| Federal and cantonal level (n = 2) | |||
| Federal Office of Public Health | F | Y | Y |
| Swiss Conference of Cantonal Health Directors | F | Y | Y |
| Total | 12 F (60%) | 15 (75%) | 13 (65%) |
F: female, M: male.
Y: participation, N: no participation.
2.5. Development of the questionnaire survey
2.5.1. Literature review
To systematically define possible competencies and outcomes for the nursing‐home RNXs, we conducted a critical literature review (Grant & Booth, 2009). As studies on RNXs effectiveness in NHs are rare, we aimed to identify APN competencies and outcomes in that context. The search strategy and screened sources can be found in supplementary files (Tables S1 and S2). We included 21 studies (Figure S1) describing NH models of care working with APNs of any type who effectively improved outcomes for residents (Holtz et al., 2015; Ouslander et al., 2014; Rantz et al., 2017; Stolle & Hillier, 2002). From the identified studies and resources, relevant APN role competencies and outcomes were extracted.
2.5.2. Case studies
In comparison to RNXs, few APNs practice in Swiss NHs [8]. We intended to validate findings from international studies and identify additional, context‐specific competencies. Therefore, we conducted case studies in the local Swiss context (Yin, 2009). Purposive and snowball sampling were applied to identify NHs employing RNXs who fulfilled our pre‐defined criteria (Table S3). Eight NHs (seven Swiss‐German and one Swiss‐French) participated. Data collection included: (a) the administration of structured questionnaires to RNXs to capture their competencies and outcomes (Abdallah et al., 2005; Canadian Nurse Practitioner Initiative, 2006; Donald et al., 2011; Mick & Ackerman, 2000; Müller, 2013); and (b) on‐site visits with semi‐structured interviews of the RNXs, their supervisors (e.g., director of nursing) and responsible physicians, with a self‐developed interview guide to assess further RNX‐relevant competencies and outcomes.
2.5.3. Piloting of the RAND/UCLA structured questionnaire survey
Competencies and outcomes identified from the literature review and case studies were formulated into a structured questionnaire survey (Hamric, 2015). To check the questionnaire's face validity and completeness, we consulted a primary healthcare physician, a geriatrician, a researcher specialized in new care models and APNs and an expert in healthcare staffing regarding its wording and clarity. Their suggestions were discussed in the research group and adaptations made accordingly.
2.6. Data collection
The relevance of each RNX competency and outcome was rated on a 9‐point Likert‐type scale (1 very irrelevant – 9 very relevant) in two rounds and analysed for disagreement (Fitch et al., 2000). The stakeholders were asked to rate: (a) the relevance of each competency for the RNXs; and (b) the relevant outcomes to be reached with the relevant competencies. Additionally, stakeholders could suggest modifying or adding items. The two‐round rating process took place between September and November 2017 (Figure 1).
2.6.1. Round 1
The first rating round was conducted online over a three‐week time span. To provide background information and explain the rating process, the studies collected via the literature review, summaries of our case studies, a glossary of terms used in the structured questionnaire survey and a short video explaining the rating process were sent along with the questionnaire survey per email.
2.6.2. In‐person meeting and round 2
After the first round, a full‐day in‐person meeting took place to identify and exchange underlying reasons for dispersion of ratings and not clearly written items from the first round, allowing participants to re‐evaluate their voting. Prior to the meeting, each stakeholder was emailed an overview of the first‐round results, showing their own scores in relation to the medians (as required by the RAND/UCLA methodology) for all items (Fitch et al., 2000). At the meeting, all stakeholders received a new rating questionnaire for the second round. This included: (a) items rated with disagreement in the first round; (b) items rated as uncertain; (c) re‐worded items based on first‐round input; and (d) new items suggested by stakeholders. Items with median ratings below 4 and no disagreement were discarded after round one. Before rating began, an open discussion was led by an experienced facilitator (Fitch et al., 2000).
2.7. Ethical considerations
Expert surveys that use no health‐related data do not require approval from Swiss ethics committees. The data collected are not of a sensitive nature and provide no foreseeable risk to participants. The study was conducted according to accepted guidelines for ethical conduct in Human Research (Swiss Academy of Medical Sciences, 2015). Participation in both the survey and the in‐person meeting was by ‘opt‐in’; informed consent was implied through survey completion. Since the participants are public figures, demographic information was not collected (to protect their identity). The implementation and evaluation of the INTERCARE model has been approved by the local ethical committee (EKNZ 2018‐00501) and registered at clinicaltrials.gov (NCT03590470).
2.8. Data analysis
After each rating round, per‐item medians were computed and three relevance categories assigned: 1–3: not relevant; 4–6: uncertain; and 7–9: relevant (Fitch et al., 2000). Agreement was calculated based on statistical measures of ratings' dispersion across the three scoring categories (Fitch et al., 2000). Disagreement was indicated when the unadjusted interpercentile range (IPR) was greater than the IPR adjusted for asymmetry (IPRAS), i.e., IPR > IPRAS. Items producing disagreement/variation in the first round were rerated in the second. Additionally, competencies identified by stakeholders as unclear in the first round would be reworded and rerated in the second. After each round, items with median ratings of 7–9 and no disagreement were included in the final set (Fitch et al., 2000). Analyses were performed using R software, version 3.5.1 (R Development Core Team, 2018).
2.9. Validity and reliability
We combined data from our literature review and case studies to develop the survey questionnaire, which was rated by a heterogeneous group of stakeholders. As for its reliability, participants were encouraged to revise existing competencies and outcomes in round one and during the in‐person meeting. Confounding variables – known in Delphi terminology as group thinking, dominant personalities, or other influences – were reduced by conducting the first rating round online with no exchange among participants; and discussion in the second round was led by an experienced facilitator who had not been involved in any other stage of the study (Hsu & Sandford, 2007; Humphrey‐Murto et al., 2017).
3. RESULTS
3.1. First round
Of the 20 stakeholders we contacted, 15 responded (75% response rate) for the first round (Table 1). This round started with 229 competencies and 62 outcomes. Of the competencies, 130 (57%) were rated 7–9 (relevant) with no disagreement and were included in the final set; 2 (1%) were judged non‐relevant (1–3) and removed; 91 (40%) were re‐rated in the second round due to disagreement or a need for rewording; and six (3%) were divided into 14 new items. Regarding outcomes, the first round ended with 52 items (84%) gauged relevant/included, 1 (2%) rated uncertain and re‐allocated and nine (14%) re‐allocated due to changes of wording. Based on stakeholders' suggestions, 63 new competencies and 10 outcomes were added after round 1. The added competency items mostly involved extension of the topics for which RNXs should provide education, resulting in a set of 168 competencies (105 from the first round and 63 new) and 20 (10 from the first round and 10 new) outcomes to be rated in the second round.
3.2. Second round and the final set
Thirteen stakeholders (65%) participated in the second round (Table 1). After this round, 60 (35%) competencies and 19 (95%) outcomes were found relevant (median 7–9) with no disagreement, making them eligible for inclusion in the final set.
In total, the final set included 190 competencies (130 from the first round, 60 from the second) and 71 relevant outcomes (52 from the first round, 19 from the second round). Tables 2 and 3 provide examples of included competencies and outcomes. The complete list of relevant competencies and outcomes (with their ratings) is available in supplementary files (Table S4).
TABLE 2.
Number and examples of rated competencies in seven competency areas
| Competency areas | 1st Round rated (included) a | 2nd Round rated (included) a | Final number included | Examples of final competencies |
|---|---|---|---|---|
| Clinical‐geriatric competencies | 90 (18) | 84 (31) | 49 |
|
| Guidance and coaching | 43 (37) | 62 (19) | 56 |
|
| Clinical and professional leadership | 45 (31) | 18 (7) | 38 |
|
| Consultation | 3 (3) | ‐ | 3 |
|
| Collaboration | 23 (19) | 6 (3) | 22 |
|
| Research competencies | 6 (5) | 1 (0) | 5 |
|
| Ethical decision making | 19 (17) | 2 (0) | 17 |
|
| Total | 229 (130) | 173 (60) | 190 |
ADL, activities of daily leaving; IADL, instrumental activities of daily living; RNXs, Registered nurses in expanded roles.
The number in brackets indicates how many competencies in a given set were rated as relevant after each round.
TABLE 3.
Number and examples of rated outcomes in four areas
| Area | 1st round rated (included) a | 2nd round rated (included) a | Final number included | Examples of final outcomes |
|---|---|---|---|---|
| Residents and relatives | 12 (12) | 3 (3) | 15 |
|
| Organization | 15 (5) | 17 (16) | 21 |
|
| Quality of care | 14 (14) | ‐ | 14 |
|
| Healthcare system | 21 (21) | ‐ | 21 |
|
| Total | 62 (52) | 20 (19) | 71 |
The number in brackets indicates how many outcomes in a given set were rated as relevant after each round.
3.3. Survey rounds 1 and 2 and in‐person meeting
3.3.1. Relevant competencies
Among (a) clinical‐geriatric competencies, the most discussed and important for RNXs were conducting elements of a comprehensive geriatric assessment (including physical, functional, and cognitive status). As for (b) guidance and coaching, the stakeholders agreed that RNXs should provide formal and informal training to care staff on geriatric‐specific topics. Regarding educating residents and their families, stakeholders emphasized that, because this is part of regular RNs' competencies, taking over this duty could lead to de‐skilling of the regular RN role; therefore, except in complex situations and/or if an RN requests support, RNXs should limit involvement in educating residents/relatives. Concerning (c) clinical and professional leadership, RNXs should support the care teams to understand and adhere to clinical guidelines. Stakeholders upheld the principle that RNXs should not prescribe medications (median 1–3 (not relevant)). This mainly reflected legal concerns and a lack of appropriate education; however, monitoring of medication was rated as relevant. In terms of (d) consultation, as exchange with other RNXs or care experts plays a pivotal role in nurses' professional development, it was agreed that RNXs should consult with others in similar roles both within and outside their workplaces. With regard to (e) collaboration, RNXs are important facilitators and coordinators of interprofessional collaboration with other professionals. For (f) research competencies, activities such as conducting literature searches of evidence‐based nursing and developing guidelines were found relevant. Finally, for competencies relating to (g) ethical decision‐making, RNXs should manage institutional efforts for pro‐active advance care planning. However, the ability to independently document them was not considered relevant.
3.3.2. Relevant outcomes
The classification of a competency as relevant implies the ability of its holder to achieve targeted outcomes. At (a) the level of residents and relatives, for example, improvement of patient‐centred care or empowerment are reasonable goals. For this context, we defined empowerment as a process of enhancing residents' independence and feelings of autonomy, including participating in decision‐making about care processes. This can be measured explicitly via a standardized residents' questionnaire about autonomy and participative decision‐making (Morris et al., 2018), or implicitly with the availability of advance care planning. At (b) the organizational level, given consistent professional support from RNXs, low staff turnover, increases in care staff job satisfaction on all levels and empowerment would be expected. We understood the empowerment of RNXs as an increase in their nursing expertise, improvement of knowledge and skills, increased confidence and independence in executing nursing tasks, as well as taking leadership roles in interdisciplinary situations. Following feedback from the first rating round, we separated RNX‐specific empowerment‐linked outcomes from those of other care staff (additional second‐round outcomes). Outcomes indicating increased confidence in care staff could be measured with standardized self‐efficacy questions (Bandura, 1977). An increase in RNs' independence could be measured in relation to the number and level of RNX involvements in coaching situations and their possibility to move on to other themes after the introduction of the target knowledge and skills to a care team. One outcome, ‘The care institution is certified with a quality label’, was rated with uncertainty in both rounds. Stakeholders argued that certification should be an overall aim of NHs, not solely of RNXs; therefore, it was excluded from the final set. Furthermore, (c) quality of care could be improved, for example, via increased continuity of care and improved pain management. For example, the RNX will support care workers in acute care situations by guiding them as necessary to contact the physician, by preparing transfers, by sharing crucial clinical information about the resident's needs and functional capacities and by keeping contact with the hospital during hospitalizations (Cummings et al., 2020). Depending on the existing skill set on the unit, RNX could also handle the physician visit or initiate contact with a physiotherapist to align care goals. The outcome could be measured via the care team members' perceptions of interprofessional collaboration (Kenaszchuk et al., 2010). And at (d) the healthcare system level, a reduction of avoidable hospitalizations – and therefore of associated costs – could be achieved by applying the relevant competencies. For continuous evaluation, the number of hospitalizations per 1,000 resident days could be monitored and the transfer reasons explored in root‐cause analyses (Ouslander et al., 2016).
4. DISCUSSION
We used the RAND/UCLA modified Delphi method to define 190 relevant competencies and 71 outcomes for RNXs, that is, RNs with additional (but not APN master‐level) education for NHs (Fitch et al., 2000; Hsu & Sandford, 2007). The two‐pronged aim of this development process was first to support the definition of RNXs in a new model of care for Swiss NHs, then to use the results to guide development of a structured educational curriculum.
With their unique geriatric expertise, RNXs can serve as role models and innovators, empowering NH care staff and residents alike. However, while role expansion offers RNs professional development, little international evidence exists regarding the value they add in NHs. Therefore, it is crucial to define specific competencies and outcomes to monitor, evaluate and gather evidence on these roles. Further, engagement of diverse stakeholders is pivotal in the development and sustainability of this group's expanded roles.
4.1. RNXs and APNs
APNs' and RNXs' training and educational curricula should include blueprints for the models of care within which they will work. While nurse practitioners (NPs) have a rather medical focus, RNXs are more active in roles often performed by Clinical Nurse Specialists (CNSs) – although without a master's level education—and focus more on organizational factors, for example, staff empowerment through coaching and clinical leadership or improving NHs' care efficiency, quality, and accessibility of care (Klaasen et al., 2009; Rantz et al., 2017).
In practice, RNXs' roles can very effectively complement those of APNs. This is the case within the OPTIMISTIC model in the US, where NPs collaborate with RNXs (Hickman et al., 2020).
Two recent reports confirm that, especially in countries where APN roles are not yet established or regulated, RNXs are becoming central to primary care provision (Bodenheimer & Mason, 2017; Martin‐Misener & Bryant‐Lukosius, 2014). And as increasing numbers of RNs consider expanded‐role nursing as an interesting and fulfilling career step, this path adds to the overall attractiveness of nursing as a profession (Auerbach et al., 2011, 2013).
4.2. Number of competencies
We defined 190 competencies applicable to nursing‐home RNXs. Their broad range reflects the complexity of NH residents' needs, for example, multimorbidity, chronic conditions, dementia, and premature hospital discharge (Colombo et al., 2011; Martin‐Misener & Bryant‐Lukosius, 2014; World Health Organization, 2015). As long as no standardized education for RNXs exists, NH administrators can adapt a selection of these competencies based on their available resources and the training of their current RNs. This will allow them to achieve the best possible fit in response to their quality of care issues, resident needs assessments, case mixes, short‐ and long‐term institutional goals and financial, personal and organizational resources (e.g., availability of physicians). In the US, for example, the Evercare project has developed a 112‐competency APN profile to fulfil their project goal of reducing unplanned NH resident hospitalizations (Abdallah et al., 2005).
To increase the uptake of RNXs in NHs, the list of defined competencies can inform the development of training and educational curricula. A core set was used within a training programme in the INTERCARE study measuring/testing RNXs' effectiveness. After this programme's evaluation, an ongoing set of courses could be launched as a postgraduate programme embedding those competencies and outcomes evaluated as core themes. This is a vital step in promoting RNXs' success and sustainability beyond the INTERCARE study (Zúñiga et al., 2019).
4.3. Specific competencies
We learned from stakeholders that alongside clinical leadership, coaching is deemed a core RNX competency. Focusing on the empowerment of all‐level care staff via regular bedside coaching can reduce staff burden considerably (Mezey et al., 2005; Rantz et al., 2017). As is common elsewhere, 40% of Switzerland's NH care personnel are nursing aids with little or no professional education, 35% are LPNs and only 25% are RNs (Bundesamt für Statistik, 2020; Harrington et al., 2012). As the rising complexity of resident caseloads is quickly outstripping this group's training, clinical leadership, and empowerment in daily practice play pivotal roles in ensuring and improving quality of care (Flesner & Rantz, 2004). Based on discussion with stakeholders, RNXs would work alongside RNs, who often supervise the care of 20–30 residents each. An RNX with a full‐time equivalent position would support several RNs and the care workers under their supervision, with a range of 60–80 residents. They could also support the introduction of clinical guidelines to simplify and support decision making (Zarowitz et al., 2018). And as inappropriate prescribing is commonly associated with adverse outcomes, RNXs could also conduct regular medication reviews to be discussed in multidisciplinary team meetings (Kapoor et al., 2019; Nazir et al., 2013).
4.4. Stakeholder involvement
The stakeholder group's survey responses guided our definition of RNXs competencies and outcomes (Concannon et al., 2012). Regarding the new designation's implementation and sustainability in real‐life contexts, stakeholder discussions helped identify context‐, leadership‐ and process‐related factors that might function as barriers. Consistent with international literature, these include opposition from professional staff – especially nurses – and poorly‐defined distinctions between RNXs and other nurses (Delamaire & Lafortune, 2010; Fealy et al., 2015). Based on these insights, the INTERCARE study developed several implementation strategies to facilitate the new role's integration into daily practice (Powell et al., 2015).
4.5. Defining and monitoring outcomes
Quantifying RNXs' impact will require evidence (Backhaus et al., 2014). Gathering that evidence will require definition of attributable outcomes, that is, results of interactions between their education (structure) and their competencies (processes) (Donabedian, 1988). Such definitions have at least three uses: (a) On an individual or aggregated level, they can be implemented to evaluate relevant impacts; (b) they identify redundancies and gaps regarding other professional disciplines; and (c) they allow inter‐setting quality‐of‐care comparisons (National Quality Forum, 2017). Data on outcomes sensitive to extended‐practice nurses' input will both highlight their contributions and provide a starting point from which to establish their role internationally (Alexandrov & Brewer, 2010).
4.6. Limitations
The RAND UCLA method's chief strengths are its combination of different data sources and its insistence on stakeholder engagement – which must be clear in both their comments and their written feedback. However, as the included case studies were from Switzerland's German‐ and French‐speaking region, cultural bias is possible: our results would require further evaluation before their application internationally or even across national regions. Furthermore, the RAND/UCLA method is not commonly used to rate new roles but to define clinical procedures' appropriateness. Thus, its contextual appropriateness warrants further testing. In addition, the identified competencies and outcomes should be further tested regarding feasibility, acceptability and reliability. Our list should be adapted to reflect both each residential NH's context and available RNXs' backgrounds and training. And finally, as the instrument assessing RNXs' competencies is unvalidated and our list of defined competencies and outcomes is not exhaustive.
5. CONCLUSIONS
According to the competencies' ratings, RNXs are considered to have a positive impact on supporting care staff in direct clinical geriatric practice while coaching/ empowering all‐level nursing staff. Further, they promote quality of care by facilitating system change and evidence‐ based practice through clinical leadership. And, particularly where APNs are unavailable, RNXs with additional education are well‐positioned to develop care locally. Equally importantly, given the growing shortage of nurses, the possibility of RNs assuming expanded roles reinforces nursing as a profession. The value RNXs add to their contexts is assessed in the INTERCARE research project. Ultimately, this study's findings will support development of a sustainable educational and training programme that will continue long after the study itself, increasing nursing homes' uptake of RNXs.
CONFLICTS OF INTEREST
No conflict of interest has been declared by the author(s).
AUTHOR CONTRIBUTIONS
All authors have agreed on the final version of this manuscript. KB involved in data acquisition, analysis and interpretation, wrote the original draft and revised it. FZ and MS involved in conceptualization and design, data analysis and interpretation, critically revised the manuscript. NIHW, AZ, and RWK, critically revised the manuscript for important intellectual content. Each author participated sufficiently in the work to take public responsibility for appropriate portions of the content; and agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Peer Review
The peer review history for this article is available at https://publons.com/publon/10.1111/jan.14644.
Supporting information
Supplementary Material
ACKNOWLEDGEMENTS
The authors thank our stakeholders for participating in this time‐consuming rating process, Nikola Engelhard for moderating the workshop, and the entire INTERCARE research team for contributing so much of their time and energy.
Basinska K, Wellens NIH, Simon M, Zeller A, Kressig RW, Zúñiga F. Registered nurses in expanded roles improve care in nursing homes: Swiss perspective based on the modified Delphi method. J. Adv. Nurs. 2021;77:742–754. 10.1111/jan.14644
Funding information
This work was supported by the Swiss National Science Foundation (SNSF) as a part of the National Research Programme ‘Smarter Health Care’ (NRP 74) (Grant 407440_167458); Nurse Science Foundation Switzerland; Ebnet – Stiftung, Switzerland.
Contributor Information
Kornelia Basinska, @KorneliaBas.
Michael Simon, @msimoninfo.
Franziska Zúñiga, Email: franziska.zuniga@unibas.ch, @fzuniga300.
REFERENCES
- Abdallah, L. , Fawcett, J. , Kane, R. , Dick, K. , & Chen, J. (2005). Development and psychometric testing of the EverCare Nurse Practitioner Role and Activity Scale (ENPRAS). Journal of the American Academy of Nurse Practitioners, 17(1), 21–26. 10.1111/j.1041-2972.2005.00006.x [DOI] [PubMed] [Google Scholar]
- Alexandrov, A. W. , & Brewer, B. B. (2010). The role of outcomes in evaluating practice change In Melnyk B. & Finout‐Overholt E. (Eds.), Evidence‐based practice in nursing and health: A guide for translating research evidence into practice (2nd ed., pp. 226–237). : Wolters Kluwer, Lippincott Williams & Wilkins. [Google Scholar]
- American Association of Colleges of Nursing . (2020). Educational resources. Retrieved from https://www.aacnnursing.org/Education‐Resources/Curriculum‐Guidelines [Google Scholar]
- Auerbach, D. I. , Buerhaus, P. I. , & Staiger, D. O. (2011). Registered nurse supply grows faster than projected amid surge in new entrants ages 23–26. Health Affairs, 30(12), 2286–2292. 10.1377/hlthaff.2011.0588 [DOI] [PubMed] [Google Scholar]
- Auerbach, D. I. , Staiger, D. O. , Muench, U. , & Buerhaus, P. I. (2013). The nursing workforce in an era of health care reform. New England Journal of Medicine, 368(16), 1470–1472. 10.1056/NEJMp1301694 [DOI] [PubMed] [Google Scholar]
- Backhaus, R. , Verbeek, H. , van Rossum, E. , Capezuti, E. , & Hamers, J. P. (2014). Nurse staffing impact on quality of care in nursing homes: A systematic review of longitudinal studies. Journal of the American Medical Directors Association, 15(6), 383–393. 10.1016/j.jamda.2013.12.080 [DOI] [PubMed] [Google Scholar]
- Bandura, A. (1977). Self‐efficacy: Toward a unifying theory of behavior change. Psychology Review, 84(2), 191–251. [DOI] [PubMed] [Google Scholar]
- Bauer, L. , & Bodenheimer, T. (2017). Expanded roles of registered nurses in primary care delivery of the future. Nursing Outlook, 65(5), 624–632. 10.1016/j.outlook.2017.03.011 [DOI] [PubMed] [Google Scholar]
- Berwick, D. M. , Nolan, T. W. , & Whittington, J. (2008). The triple aim: Care, health, and cost. Health Affairs, 27(3), 759–769. 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- Bing‐Jonsson, P. C. , Bjork, I. T. , Hofoss, D. , Kirkevold, M. , & Foss, C. (2015). Competence in advanced older people nursing: Development of ‘nursing older people–competence evaluation tool’. International Journal of Older People Nursing, 10(1), 59–72. 10.1111/opn.12057 [DOI] [PubMed] [Google Scholar]
- Bodenheimer, T. , & Mason, D. (2017). Registered nurses: Partners in transforming primary care. Proceedings of a conference sponsored by the Retrieved from New York. [Google Scholar]
- Bryant‐Lukosius, D. , & DiCenso, A. (2004). A framework for the introduction and evaluation of advanced practice nursing roles. Journal of Advanced Nursing, 48(5), 530–540. 10.1111/j.1365-2648.2004.03235.x [DOI] [PubMed] [Google Scholar]
- Bundesamt für Statistik . (2020). Pflegepersonal 2018. Retrieved from https://www.bfs.admin.ch/bfs/de/home/aktuell/neue‐veroeffentlichungen.gnpdetail.2020‐0494.html [Google Scholar]
- Canadian Nurse Practitioner Initiative . (2006). Implementation and evaluation toolkit for nurse practitioner in Canada. Retrieved from https://nurseone.ca/~/media/nurseone/files/en/toolkit_implementation_evaluation_np_e.pdf?la=en
- Colombo, F. , Llena‐Nozal, A. , Mercier, J. , & Tjadens, F. (2011). Help wanted?: Providing and paying for long‐term care. Paris: OECD Health Policy Studies, OECD Publishing; 10.1787/9789264097759-en [DOI] [Google Scholar]
- Concannon, T. W. , Meissner, P. , Grunbaum, J. A. , McElwee, N. , Guise, J.‐M. , Santa, J. , Conway, P. H. , Daudelin, D. , Morrato, E. H. , & Leslie, L. K. (2012). A new taxonomy for stakeholder engagement in patient‐centered outcomes research. Journal of General Internal Medicine, 27(8), 985–991. 10.1007/s11606-012-2037-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings, G. G. , McLane, P. , Reid, R. C. , Tate, K. , Cooper, S. L. , Rowe, B. H. , Estabrooks, C. A. , Cummings, G. E. , Abel, S. L. , Lee, J. S. , Robinson, C. A. , & Wagg, A. (2020). Fractured care: A window into emergency transitions in care for LTC residents with complex health needs. Journal of Aging and Health, 32(3–4), 119–133. 10.1177/0898264318808908 [DOI] [PubMed] [Google Scholar]
- Delamaire, M. L. , & Lafortune, G. (2010). Nurses in advanced roles: A description and evaluation of experiences in 12 developed countries. 10.1787/5kmbrcfms5g7-en [DOI]
- Donabedian, A. (1988). The quality of care: How can it be assessed? JAMA Internal Medicine, 260(12), 1743–1748. 10.1001/jama.260.12.1743 [DOI] [PubMed] [Google Scholar]
- Donald, F. , Martin‐Misener, R. , Carter, N. , Donald, E. E. , Kaasalainen, S. , Wickson‐Griffiths, A. , Lloyd, M. , Akhtar‐Danesh, N. , & DiCenso, A. (2013). A systematic review of the effectiveness of advanced practice nurses in long‐term care. Journal of Advanced Nursing, 69(10), 2148–2161. 10.1111/jan.12140 [DOI] [PubMed] [Google Scholar]
- Donald, F. , Martin‐Misener, R. , Ploeg, J. , DiCenso, A. , Brazil, K. , Kaasalainen, S. , Bryant‐Lukosius, D. (2011). Understanding the individual, organizational, and system factors influencing the integration of the nurse practitioner role in long‐term care settings in Canada. Retrieved from https://www.ryerson.ca/apnltc/pdf/FinalReport.pdf
- Fealy, G. M. , Rohde, D. , Casey, M. , Brady, A.‐M. , Hegarty, J. , Kennedy, C. , McNamara, M. , O'Reilly, P. , & Prizeman, G. (2015). Facilitators and barriers in expanding scope of practice: Findings from a national survey of Irish nurses and midwives. Journal of Clinical Nursing, 24(23–24), 3615–3626. 10.1111/jocn.12980 [DOI] [PubMed] [Google Scholar]
- Fitch, K. , Bernstein, S. J. , Aguilar, M. D. , Burnand, B. , LaCalle, J. R. , Lázaro, P. , Kahan, J. P. (2000). The Rand/UCLA appropriateness method user's manual (0–8330‐2918‐5). Retrieved from https://www.rand.org/content/dam/rand/pubs/monograph_reports/2011/MR1269.pdf
- Flesner, M. K. , & Rantz, M. J. (2004). Mutual empowerment and respect: Effect on nursing home quality of care. Journal of Nursing Care Quality, 19(3), 193–196. 10.1097/00001786-200407000-00004 [DOI] [PubMed] [Google Scholar]
- Grant, M. J. , & Booth, A. (2009). A typology of reviews: An analysis of 14 review types and associated methodologies. Health Information & Libraries Journal, 26(2), 91–108. 10.1111/j.1471-1842.2009.00848.x [DOI] [PubMed] [Google Scholar]
- Hamric, A. B. (2015). Advanced practice nursing. An integrative approach (5th ed.). St. Louis, Mo.: Saunders/Elsevier. [Google Scholar]
- Harrington, C. , Choiniere, J. , Goldmann, M. , Jacobsen, F. F. , Lloyd, L. , McGregor, M. , Stamatopoulos, V. , & Szebehely, M. (2012). Nursing home staffing standards and staffing levels in six countries. Journal of Nursing Scholarship, 44(1), 88–98. 10.1111/j.1547-5069.2011.01430.x [DOI] [PubMed] [Google Scholar]
- Hickman, S. E. , Parks, M. , Unroe, K. T. , Ott, M. , & Ersek, M. (2020). The role of the palliative care registered nurse in the nursing facility setting. Journal of Hospice and Palliative Nursing, 22(2), 152–158. 10.1097/NJH.0000000000000634 [DOI] [PubMed] [Google Scholar]
- Holtz, L. R. , Maurer, H. , Nazir, A. , Sachs, G. A. , & Unroe, K. T. (2015). OPTIMISTIC: A program to improve nursing home care and reduce avoidable hospitalizations In Malone M. L., Capezuti E. A., & Palmer R. M. (Eds.), Geriatrics models of care: Bringing ‘best practice’ to an aging America (pp. 287–292). Springer International Publishing. [Google Scholar]
- Hsu, C. C. , & Sandford, B. A. (2007). The Delphi technique: Making sense of consensus. Practical Assessment, Research & Evaluation, 12(10), 10.7275/pdz9-th90 [DOI] [Google Scholar]
- Humphrey‐Murto, S. , Varpio, L. , Gonsalves, C. , & Wood, T. J. (2017). Using consensus group methods such as Delphi and Nominal Group in medical education research. Medical Teacher, 39(1), 14–19. 10.1080/0142159X.2017.1245856 [DOI] [PubMed] [Google Scholar]
- International Council of Nurses . (2005). Regulation terminology. Retrieved from http://www.icn.ch/regterms.htm [Google Scholar]
- Involve . (2012). Briefing notes for researchers: Involving the public in NHS, public health and social care research. Retrieved from http://www.invo.org.uk/wp‐content/uploads/2012/04/INVOLVEBriefingNotesApr2012.pdf [Google Scholar]
- Kapoor, A. , Field, T. , Handler, S. , Fisher, K. , Saphirak, C. , Crawford, S. , Fouayzi, H. , Johnson, F. , Spenard, A. , Zhang, N. , & Gurwitz, J. H. (2019). Adverse events in long‐term care residents transitioning from hospital back to nursing home. JAMA Internal Medicine, 179(9), 1254–1261. 10.1001/jamainternmed.2019.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenaszchuk, C. , Reeves, S. , Nicholas, D. , & Zwarenstein, M. (2010). Validity and reliability of a multiple‐group measurement scale for interprofessional collaboration. BMC Health Services Research, 10, 83 10.1186/1472-6963-10-83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiljunen, O. , Valimaki, T. , Kankkunen, P. , & Partanen, P. (2017). Competence for older people nursing in care and nursing homes: An integrative review. International Journal of Older People Nursing, 12(3), e12146 10.1111/opn.12146 [DOI] [PubMed] [Google Scholar]
- Klaasen, K. , Lamont, L. , & Krishnan, P. (2009). Setting a new standard of care in nursing homes. The Canadian Nurse, 105(9), 24–30. [PubMed] [Google Scholar]
- Lamb, G. , Newhouse, R. , Beverly, C. , Toney, D. A. , Cropley, S. , Weaver, C. A. , Kurtzman, E. , Zazworsky, D. , Rantz, M. , Zierler, B. , Naylor, M. , Reinhard, S. , Sullivan, C. , Czubaruk, K. , Weston, M. , Dailey, M. , & Peterson, C. (2015). Policy agenda for nurse‐led care coordination. Nursing Outlook, 63(4), 521–530. 10.1016/j.outlook.2015.06.003 [DOI] [PubMed] [Google Scholar]
- Maier, C. B. , Aiken, L. H. , & Busse, R. (2017). Nurses in advanced roles in primary care: Policy levers for implementation. OECD Health Working Papers, No. 98(OECD Publishing, Paris). 10.1787/a8756593-en [DOI]
- Martin‐Misener, R. , & Bryant‐Lukosius, D. (2014). Optimizing the role of nurses in primary care in Canada. Final report. Retrieved from https://www.cna‐aiic.ca/~/media/cna/page‐content/pdf‐en/optimizing‐the‐role‐of‐nurses‐in‐primary‐care‐in‐canada.pdf?la=en [Google Scholar]
- McGilton, K. S. , Bowers, B. J. , Heath, H. , Shannon, K. , Dellefield, M. E. , Prentice, D. , Siegel, E. O. , Meyer, J. , Chu, C. H. , Ploeg, J. , Boscart, V. M. , Corazzini, K. N. , Anderson, R. A. , & Mueller, C. A. (2016). Recommendations from the international consortium on professional nursing practice in long‐term care homes. Journal of the American Medical Directors Association, 17(2), 99–103. 10.1016/j.jamda.2015.11.001 [DOI] [PubMed] [Google Scholar]
- Mezey, M. , Greene Burger, S. , Bloom, H. G. , Bonner, A. , Bourbonniere, M. , Bowers, B. , Burl, J. B. , Capezuti, E. , Carter, D. , Dimant, J. , Jerro, S. A. , Reinhard, S. C. , & Ter Maat, M. (2005). Experts recommend strategies for strengthening the use of advanced practice nurses in nursing homes. Journal of the American Geriatrics Society, 53(10), 1790–1797. 10.1111/j.1532-5415.2005.53556.x [DOI] [PubMed] [Google Scholar]
- Mick, D. J. , & Ackerman, M. H. (2000). Advanced practice nursing role delineation in acute and critical care: Application of the strong model of advanced practice. Heart and Lung, 29(3), 210–221. 10.1067/mhl.2000.106936 [DOI] [PubMed] [Google Scholar]
- Morris, J. N. , Declercq, A. , Hirdes, J. P. , Finne‐Soveri, H. , Fries, B. E. , James, M. L. , Geffen, L. , Kehyayan, V. , Saks, K. , Szczerbińska, K. , & Topinkova, E. (2018). Hearing the voice of the resident in long‐term care facilities‐an internationally based approach to assessing quality of life. Journal of the American Medical Directors Association, 19(3), 207–215. 10.1016/j.jamda.2017.08.010 [DOI] [PubMed] [Google Scholar]
- Müller, M. (2013). Nursing competence: Psychometric evaluation using Rasch modelling. Journal of Advanced Nursing, 69(6), 1410–1417. 10.1111/jan.12009 [DOI] [PubMed] [Google Scholar]
- National Quality Forum . (2017). Measuring performance: NQF‐Endorsed® Standards. Retrieved from https://www.qualityforum.org/Measuring_Performance/Measuring_Performance.aspx [Google Scholar]
- Nazir, A. , Unroe, K. , Tegeler, M. , Khan, B. , Azar, J. , & Boustani, M. (2013). Systematic review of interdisciplinary interventions in nursing homes. Journal of the American Medical Directors Association, 14(7), 471–478. 10.1016/j.jamda.2013.02.005 [DOI] [PubMed] [Google Scholar]
- Ouslander, J. G. , Bonner, A. , Herndon, L. , & Shutes, J. (2014). The Interventions to Reduce Acute Care Transfers (INTERACT) quality improvement program: An overview for medical directors and primary care clinicians in long term care. Journal of the American Medical Directors Association, 15(3), 162–170. 10.1016/j.jamda.2013.12.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ouslander, J. G. , Naharci, I. , Engstrom, G. , Shutes, J. , Wolf, D. G. , Alpert, G. , Rojido, C. , Tappen, R. , & Newman, D. (2016). Root cause analyses of transfers of skilled nursing facility patients to acute hospitals: Lessons learned for reducing unnecessary hospitalizations. Journal of the American Medical Directors Association, 17(3), 256–262. 10.1016/j.jamda.2015.11.018 [DOI] [PubMed] [Google Scholar]
- Peters, D. H. , Tran, N. T. , & Adam, T. (2013). Implementation research in health: A practical guide (9789241506212). Retrieved from https://www.who.int/alliance‐hpsr/resourcesimplementationresearchguide/en/ [Google Scholar]
- Powell, B. J. , Waltz, T. J. , Chinman, M. J. , Damschroder, L. J. , Smith, J. L. , Matthieu, M. M. , Proctor, E. K. , & Kirchner, J. A. E. (2015). A refined compilation of implementation strategies: Results from the Expert Recommendations for Implementing Change (ERIC) project. Implementation Science, 10(1), 21 10.1186/s13012-015-0209-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team . (2018). R: A language and environment for statistical computing (Version 3.5.1).
- Rantz, M. J. , Popejoy, L. , Vogelsmeier, A. , Galambos, C. , Alexander, G. , Flesner, M. , Crecelius, C. , Ge, B. , & Petroski, G. (2017). Successfully reducing hospitalizations of nursing home residents: Results of the Missouri quality initiative. Journal of the American Medical Directors Association, 18(11), 960–966. 10.1016/j.jamda.2017.05.027 [DOI] [PubMed] [Google Scholar]
- Ryan, J. (2003). Continuous professional development along the continuum of lifelong learning. Nurse Education Today, 23(7), 498–508. 10.1016/S0260-6917(03)00074-1 [DOI] [PubMed] [Google Scholar]
- Smolowitz, J. , Speakman, E. , Wojnar, D. , Whelan, E. M. , Ulrich, S. , Hayes, C. , & Wood, L. (2015). Role of the registered nurse in primary health care: Meeting health care needs in the 21st century. Nursing Outlook, 63(2), 130–136. 10.1016/j.outlook.2014.08.004 [DOI] [PubMed] [Google Scholar]
- Stolle, E. , & Hillier, L. (2002). The Ontario nurse practitioner in long‐term care facilities pilot project – Interim evaluation. Retrieved from http://www.health.gov.on.ca/en/common/ministry/publications/reports/nurseprac02/np_report_022302.pdf [Google Scholar]
- Swiss Academy of Medical Sciences . (2015). Research with human subjects. A manual for practitioners. Retrieved from https://www.samw.ch/en/Ethics/Topics‐A‐to‐Z/Research‐ethics.html
- World Health Organization . (2015). World report on ageing and health. Retrieved from http://apps.who.int/iris/bitstream/10665/186463/1/9789240694811_eng.pdf?ua=1 [Google Scholar]
- World Health Organization . (2020). State of the world's nursing 2020: Investing in education, jobs and leadership. Retrieved from https://apps.who.int/iris/bitstream/handle/10665/331677/9789240003279‐eng.pdf [Google Scholar]
- Yin, R. K. (2009). Case study research: Design and methods (4th ed., Vol. 5). SAGE. [Google Scholar]
- Zarowitz, B. J. , Resnick, B. , & Ouslander, J. G. (2018). Quality clinical care in nursing facilities. Journal of the American Medical Directors Association, 19(10), 833–839. 10.1016/j.jamda.2018.08.008 [DOI] [PubMed] [Google Scholar]
- Zúñiga, F. , De Geest, S. , Guerbaai, R. A. , Basinska, K. , Nicca, D. , Kressig, R. W. , Zeller, A. , Wellens, N. I. H. , De Pietro, C. , Vlaeyen, E. , Desmedt, M. , Serdaly, C. , & Simon, M. (2019). Strengthening geriatric expertise in Swiss nursing homes: INTERCARE implementation study protocol. Journal of the American Geriatrics Society, 67(10), 2145–2150. 10.1111/jgs.16074 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Material


