Abstract
Background:
Due to inherent challenges in maintaining physical distancing in hemodialysis units, the Canadian Society of Nephrology has recommended peritoneal dialysis as the preferred modality for patients requiring maintenance dialysis during the coronavirus disease 19 (COVID-19) pandemic. However, pursuing peritoneal dialysis is not without risk due to the requirement for in-person contact during catheter insertion and training, and there is a paucity of data regarding the experience of peritoneal dialysis during the early phases of the pandemic.
Objective:
To examine the incidence and outcomes of peritoneal dialysis between March 17 and June 01, 2020 compared to the same time period in preceding years.
Design:
Retrospective observational study.
Setting:
British Columbia, Canada. After the pandemic was declared on March 17, 2020, patients continued to be trained in peritoneal dialysis. In an effort to limit time spent in hospital, patients were preferentially trained in continuous ambulatory peritoneal dialysis, training times were truncated for some patients, and peritoneal dialysis catheters were inserted by a physician at the bedside whenever feasible.
Patients:
All patients aged >18 years who started chronic maintenance dialysis during the period March 17 to June 01 in the years 2018 to 2020 inclusive. The time period was extended to include the years 2010 to 2020 inclusive to evaluate longer term trends in dialysis incidence.
Measurements:
A provincial clinical information system was used to capture the date of commencing dialysis, dialysis modality, and complications including peritonitis. Overall uptake of peritoneal dialysis included new starts and transitions to peritoneal dialysis from in-center hemodialysis during the observation period.
Methods:
The incidence of dialysis during the specified time period, overall and by modality, was calculated per million population using census figures for the population at risk. Patients were followed for a minimum of 30 days from the start of peritoneal dialysis to capture episodes of peritonitis and COVID-19.
Results:
A total of 211 patients started maintenance dialysis between March 17 and June 01, 2020. The incidence dialysis rate (41.3 per million population) was lower than that expected based on the 10-year trend from 2010 to 2019 inclusive (expected rate 45.7 per million population, 95% confidence interval 41.7 to 50.1). A total of 93 patients started peritoneal dialysis, including 32 patients who transitioned from in-center hemodialysis, contributing to a higher overall uptake of peritoneal dialysis compared to preceding years. The incidence rate for peritoneal dialysis of 18.2 per million population was higher than that expected (16.3 per million population, 95% confidence interval 14.0 to 19.0). Half of patients (48%) underwent a bedside peritoneal dialysis catheter insertion by a physician. During 30 days of follow-up, 2 (2.2%) patients experienced peritonitis and no patients were diagnosed with COVID-19.
Limitations:
Results are short term and generalizable only to regions with similarly low community rates of transmission of severe acute respiratory syndrome coronavirus 2.
Conclusions:
These preliminary findings indicate that peritoneal dialysis can be safely started and perhaps expanded as a means of mitigating the anticipated surge in in-center hemodialysis during the COVID-19 pandemic. Important contributors to the uptake of peritoneal dialysis in British Columbia were bedside catheter insertions and expediting transitions from in-center hemodialysis to peritoneal dialysis.
Keywords: coronavirus disease 19, hemodialysis, incidence, peritoneal dialysis, peritonitis
Introduction
The coronavirus disease 19 (COVID-19) pandemic has had a profound impact on the delivery of kidney replacement therapy world-wide. An abrupt decline in transplantation activity1 has restricted the modality choices usually available to patients with kidney failure and raised concerns that the demand for in-center hemodialysis may exceed supply. Reports of infectious outbreaks in hemodialysis units,2 and high rates of adverse outcomes in hemodialysis patients with COVID-19,3,4 have amplified this concern for patients and their families. An expansion in peritoneal dialysis (PD) is an appealing alternative; however, the decision to pursue PD is not without risk given the requirement for direct patient contact for catheter insertion and during training. On the basis that the benefits are likely to outweigh the risks, the Canadian Society of Nephrology has recommended PD as the preferred modality for patients requiring maintenance dialysis during the pandemic.5
The Canadian province of British Columbia has a population of approximately 5 million individuals, of whom some 3500 receive dialysis across the 6 health authorities in the province. Care for these patients is delivered by BC Renal, a governmental branch of the Provincial Health Services Authority. After the pandemic was declared on March 17, 2020, the executive committee of BC Renal, representing medical directors from each health authority, made the decision to continue training patients in PD. In an effort to limit time spent in the hospital environment, patients preferentially received training in continuous ambulatory peritoneal dialysis (CAPD), training times were truncated for suitable patients, and PD catheters were inserted at the bedside by a nephrologist whenever feasible. Herein, we describe our experience of PD in British Columbia between March 17 and June 1, 2020, during which time approximately 2500 cases of COVID-19 were diagnosed in the province.
Methods
This was a retrospective observational study of patients initiating chronic maintenance dialysis in British Columbia during the time period March 17 to June 1, 2020. All patients who are resident in British Columbia and receive kidney replacement therapy are automatically registered in a province-wide clinical information system, which records data on dialysis start date, dialysis modality, procedures including PD catheter insertion, and complications such as infection. The incidence rate of dialysis during the study period was calculated per million population using census figures for the population at risk, and 95% confidence intervals were calculated assuming a Poisson distribution. Overall uptake of PD included patients who started PD as their first dialysis therapy, as well as patients who transitioned to PD from in-center hemodialysis during the observation period. The incidence of dialysis, overall and by modality, was compared to that in the same 10-week period in 2019 and 2018. Follow-up was extended to July 1 of each year to capture events of peritonitis in the first 30 days of initiating PD. To further evaluate the observed dialysis incidence rate in 2020, the expected incidence rate for March 17 to June 1, 2020 was estimated from the trend observed in the same 10-week period in the years 2010 to 2019 inclusive, using a Poisson regression model.
Results
Between March 17 and June 1, 2020, a total of 211 patients were initiated on maintenance dialysis, representing an incidence rate of 41.3 per million population (pmp). This rate was broadly comparable to that observed in the same 10-week period in 2019 (n = 246, 48.7 pmp) and 2018 (n = 195, 39.1 pmp; Table 1). Based on the 10-year trend in dialysis incidence between 2010 and 2019, the observed rate in 2020 was lower than that expected (45.7 pmp, 95% confidence interval 41.7 to 50.1). A total of 61 patients started PD as their first dialysis therapy and a further 32 patients transitioned to PD from in-center hemodialysis, contributing to a higher overall uptake of PD compared to that observed in the same time period in preceding years (Figure 1). The observed incidence of PD of 18.2 pmp was higher than that expected based on the trend from 2010 to 2019 (16.3 pmp, 95% confidence interval 14.0 to 19.0). A total of 45 (48%) patients underwent a bedside PD catheter insertion by a physician. During 30 days of follow-up, 2 (2.2%) cases of peritonitis were encountered, compared to 2 (2.5%) cases in 2019 and 2 (2.8%) cases in 2018. No cases of COVID-19 were diagnosed among patients who initiated PD.
Table 1.
Incidence of Chronic Dialysis in British Columbia From March 17 to June 1, 2020 Compared to the Same Time Period in 2019 and 2018.
| 2018 | 2019 | 2020 | ||||
|---|---|---|---|---|---|---|
| N | % | N | % | N | % | |
| HD Initiation | 144 | 74 | 186 | 76 | 150 | 71 |
| Out-patient | 46 | 24 | 72 | 29 | 53 | 25 |
| In-patient | 98 | 50 | 114 | 46 | 97 | 46 |
| PD Initiation | 51 | 26 | 60 | 24 | 61 | 29 |
| Training | 31 | 16 | 43 | 17 | 49 | 23 |
| Out-patient | 18 | 9 | 13 | 5 | 12 | 6 |
| In-patient | 2 | 1 | 4 | 2 | 0 | 0 |
| Total | 195 | 100 | 246 | 100 | 211 | 100 |
| Incident Dialysis Rate PMP | 39.1 | 48.7 | 41.3 | |||
| Incident HD Rate PMP | 28.9 | 36.8 | 29.4 | |||
| Incident PD Rate PMP | 10.2 | 11.9 | 11.9 | |||
Note. HD = hemodialysis; PD = peritoneal dialysis; PMP = per million population.
Figure 1.
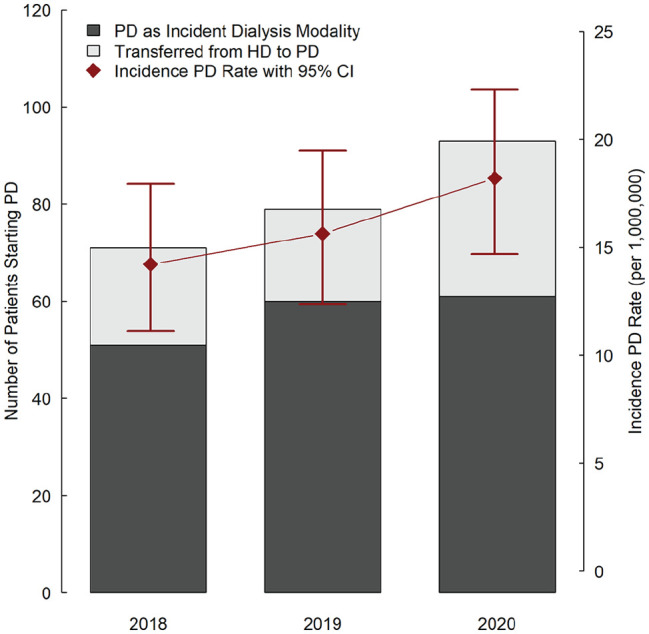
Uptake of peritoneal dialysis in British Columbia from March 17 to June 1, 2020 compared to the same time period in 2019 and 2018.
Note. CI = confidence interval; HD = hemodialysis; PD = peritoneal dialysis.
Discussion
In this study of patients initiating maintenance dialysis in British Columbia during the first 10 weeks of the COVID-19 pandemic between March 17 and June 1, 2020, the uptake of PD was successfully maintained through a combination of new PD starts and transitions to PD from in-center hemodialysis. Reassuringly, no patient contracted severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) during catheter insertion or in-person training, and there was no apparent signal of higher rates of early peritonitis among incident PD patients compared to previous years. The overall incidence of dialysis was lower than that expected based on temporal trends between 2010 and 2019, perhaps indicating a reluctance among patients to pursue medical attention during the early stages of the pandemic.
The reliability of protocols and clinical pathways for the optimal delivery of care to patients with kidney disease have been severely tested since the onset of the COVID-19 pandemic. It is therefore imperative that different jurisdictions share their learning experiences and outcomes, so that individual programs can refine and adapt their response within the context of local resources. These preliminary findings indicate that PD can be safely started, and perhaps the capacity of PD expanded, during a time when modality options are restricted for patients due to a decrease in kidney transplantation. In British Columbia, this was achieved through a number of initiatives undertaken at the onset of the pandemic. Perhaps most importantly, patients waiting for PD catheter insertion were identified and their procedures expedited, including patients receiving in-center hemodialysis who subsequently transitioned to PD. Approximately half of patients had their catheter inserted by a physician at the bedside. Despite operating rooms being closed for elective procedures, clinicians in each health authority argued strongly for the remainder of patients to undergo surgical catheter placement on the basis that proceeding with surgery could offset future risk of hospitalization for acute hemodialysis and mitigate exposures between patients and staff in dialysis units. To reduce in-person training times, training in CAPD was prioritized and training times were truncated for suitable patients on a case-by-case basis at the discretion of the treating physician. Beyond successfully training patients in PD, there are many unanswered questions related to how best to support patients in their home environment, remotely monitor treatment delivery, and manage complications.6 While this represents a significant challenge, the urgent need for innovative solutions to these problems has the potential to change treatment paradigms for home therapies in the future.7
Our study has a number of limitations. Community transmission rates of SARS-CoV-2 were comparatively low in British Columbia during the period of interest and personal protective equipment was widely available, therefore our results are only generalizable to regions with similar characteristics. The results are short term and we did not capture catheter-related complications other than peritonitis. Nevertheless, our findings suggest that insertion of PD catheters and training of patients can continue to be undertaken safely and effectively. Given the increasing recognition that containment measures will be required for some time in hemodialysis units, with attendant resource implications, an expansion in PD capacity could play an important role in mitigating the anticipated surge in facility-based hemodialysis.
Footnotes
Ethics Approval and Consent to Participate: This report was undertaken under the auspices of BC Renal, which is accountable for care and data related to kidney services in British Columbia. This data is reported to provincial committees as part of their regular work for ongoing surveillance and monitoring, and is regularly presented in the public domain. As such, ethics approval was not specifically required for this report.
Consent for Publication: All authors provide their consent for publication.
Availability of Data and Materials: All relevant data are provided in the manuscript. Please contact the corresponding author for questions or clarifications.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Mark Canney  https://orcid.org/0000-0002-4308-3083
https://orcid.org/0000-0002-4308-3083
References
- 1. Loupy A, Aubert O, Reese PP, Bastien O, Bayer F, Jacquelinet C. Organ procurement and transplantation during the COVID-19 pandemic [published online ahead of print May 11, 2020]. Lancet. doi: 10.1016/S0140-6736(20)31040-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Corbett R, Blakey S, Nitsch D, et al. Epidemiology of COVID-19 in an urban dialysis centre. J Am Soc Nephrol. 2020;31:1815-1823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goicoechea M, Sánchez Cámara LA, Macías N, et al. COVID-19: clinical course and outcomes of 36 hemodialysis patients in Spain. Kidney Int. 2020;98:27-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Wu J, Li J, Zhu G, et al. Clinical features of maintenance hemodialysis patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. Clin J Am Soc Nephrol. 2020;15:1139-1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Home Dialysis Workgroup Members, Copland M, Hemmett J, et al. Canadian Society of Nephrology COVID-19 rapid response team home dialysis recommendations. Can J Kidney Health Dis. 2020;7:1-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Wilkie M, Davies S. Peritoneal dialysis in the time of COVID-19. Perit Dial Int. 2020;40:357-358. [DOI] [PubMed] [Google Scholar]
- 7. Brown EA, Perl J. Increasing peritoneal dialysis use in response to the COVID-19 pandemic: will it go viral. J Am Soc Nephrol. 2020;31:1928-1930. [DOI] [PMC free article] [PubMed] [Google Scholar]


