Abstract
Purpose
This study aimed to assess the direct and indirect impact of COVID-19-related aspects on self-reported sleep quality, considering the moderator role of some psychological variables.
Methods
During the first weeks of the lockdown in Italy, 2286 respondents (1706 females and 580 males; age range: 18–74 years) completed an online survey that collected sociodemographic information and data related to the experience with the COVID-19 pandemic. Some questionnaires assessed sleep quality, psychological well-being, general psychopathology, Post-Traumatic Stress Disorders symptoms, and anxiety. The path analysis was adopted.
Results
The study confirms a direct effect of some aspects ascribable to the pandemic, with a mediator role of the psychological variables. Lower sleep quality was directly related to the days spent at home in confinement and the knowledge of people affected by the COVID-19. All the other aspects related to the COVID-19 pandemic influenced sleep quality through the mediator effect of psychological variables.
Conclusion
This study highlighted that the psychological condition of the population has been influenced by the COVID-19 pandemic and the government actions taken to contain it, but it has also played an important role in mediating the quality of sleep, creating a vicious circle on people’s health. The results suggest that a health emergency must be accompanied by adequate social support programs to mitigate the fear of infection and promote adequate resilience to accept confinement and social distancing. Such measures would moderate psychological distress and improve sleep quality.
Keywords: COVID-19, pandemic, sleep quality, psychological distress, home confinement, social isolation
Introduction
The Coronavirus disease 2019 (COVID-19) pandemic severely impacted the worldwide population, involving aspects closely related to physical health, political, social, economic, and psychological conditions.1–3 Italy was one of the first and most affected countries. The rapid spread of the virus led the Italian government to implement exceptional containment measures of social distancing, including social isolation and home confinement, between March and May 2020.4,5 Likewise, several governments have adopted the same measures.4
COVID-19 pandemic affected the psychological well-being of the general population. Several studies documented the mental-health outcomes of the pandemic, particularly reporting an increase of distress,6–8 Post-Traumatic Stress Disorders’ symptoms (PTSD),9,10 anxiety,11,12 mood diseases,11,12 and sleep disorders.8,13 In Italy, different authors confirmed similar trends about the psychological impact of the pandemic.14–20 Moreover, pandemic caused changes in daily habits and lifestyles (eg, eating habits, physical activity, and leisure activity21–23) linked to the more or less severe containment measures that exacerbated the impact of COVID-19 on mental health.23
One of the aspects highly affected by the pandemic was sleep.16,24,25 Different studies evidenced alteration in both sleep quality and quantity. A recent meta-analysis reported a prevalence of 32.2% of sleep disorders among the general population.26 During the pandemic, modifications in sleep patterns, such as increased sleep medication use, higher prevalence of insomnia, and a general decrease of perceived sleep quality were reported in association with lifestyle changes due to the confinement.16,24,25. Moreover, sleep disturbances were associated with higher levels of anxiety and depression and a greater incidence of psychiatric disorders.26
In Italy, an online survey conducted during the first 2 weeks of lockdown reported poor sleep quality in about six respondents out of ten (57.1%).16 Moreover, the mean scores of the questionnaire for the self-assessment of sleep quality (Pittsburgh Sleep Quality Index)27, adopted by the study, indicated greater sleep disturbances in the respondents’ sample than normative data from the general population. Other Italian studies reported similar results.15,20,24,28–30 For example, Marelli et al15 reported increased sleep disturbances and insomnia, particularly in students and workers. Cellini and colleagues24 highlighted an alteration in sleep quality related to the changes in habits due to the home confinement, especially when high levels of depression, anxiety, and stress symptomatology were reported. Furthermore, Salfi and colleagues28 underlined that the Italian population transversely presented significant sleep disturbance after the stressful lockdown period due to the pandemic.
It is well known that sleep pattern is associated with mental health. Sleep quality has a bidirectional relationship with stress, anxiety, and mood alteration.31 On the one hand, sleep disturbances exacerbate psychological distress; on the other hand, anxiety and depression impair the usual sleep habits.31,32
Many studies have assessed the different aspects of sleep by providing important information about its association with the pandemic33 – such as the prevalence of sleep disturbance in different populations8,15,34 and the potential risk factors for poor sleep quality during lockdown (eg, gender, level of education, occupational condition, social capital).35,36, However, no research has integrated the psychological variables into a model capable to associate the pandemic dimensions and the quality of sleep.
Moreover, it has never been clarified whether COVID-19-related variables (such as the diagnosis, the confinement, etc.) influenced sleep quality directly or indirectly and whether other aspects (such as mental-health variables) modulated it. The COVID-19 and the consequent measures taken to contain it could directly or indirectly alter sleep quality. Many psychological dimensions could play a relevant role in this relationship. Understanding indirect associations of COVID-19 pandemic, more than direct ones, would allow scheduling, specific interventions to improve the general population’s sleep quality.
Accordingly, this study aimed to assess the association between COVID-19-related aspects (ie, the diagnosis of COVID-19; the contact with people affected by the virus; the day of confinement at home during the lockdown) and sleep quality, considering the moderator role of some psychological variables identified by previous studies on the effect of pandemic (ie, psychological well-being, anxiety, psychopathological symptoms, PTSD symptoms).11,14,16,18
We hypothesized that COVID-19-related aspects influenced both directly and indirectly via psychological variables the sleep quality. A worse sleep condition should be associated with higher COVID-19 exposure (ie, personal infection or direct contact with infected people) and home confinement due to the pandemic spread. Furthermore, the quality of sleep should be affected by the deterioration of the respondents’ psychological state, also influenced by the COVID-19 pandemic and its consequences, such as confinement and social distancing.
Materials and Methods
Study Design and Participants
Data from the Italian population were collected by a web-based cross-sectional survey that was broadcasted through different platforms and mainstream social media between March 18th and April 2nd. After a brief presentation about the study aims, electronic informed consent was requested from each participant before starting the survey. A short questionnaire collected information on some demographic and COVID-19-related information, then standardized questionnaires to evaluate psychological dimensions and sleep quality were administered. The survey lasted about 30 minutes, and all the data from respondents who completed the survey in less than 20 min were excluded to ensure a standard quality of questionnaires. The only inclusion criteria adopted were a minimum age of 18 years and being Italian. If a participant withdrew from the survey before the end, no data were saved. The 98% of the total respondents, who started the survey signing the consent (2.286 participants out of 2.332), completed it and were considered for the statistical analyses. Participants were 1706 females and 580 males with a mean age of 29.61 (standard deviation: 11.42) and an age range between 18 and 74 years. More specific information of the sample can be found in the previous study.17
Instrument and Measure
Demographic Information
To collect data on gender, age, education, occupation, Territorial Areas (north, center or south of Italy), number of inhabitants in own city (<2000; 2000–10,000; 10,000–100,000; >100,000), a questionnaire including socio-demographic information was administered.
COVID-19-Related Information
A section aimed to evaluate the personal experience with COVID-19 infection was included. If the respondents had a COVID-19 diagnosis (options: “yes”, “no”, “I don’t know”), and the number of days spent at home consequently to the Italian government measures was reported. Moreover, three dichotomous (yes/no) questions were focused on detecting the knowledge of people (1) affected by COVID-19, (2) admitted in intensive care units (ICU) due to COVID-19, (3) dead for COVID-19. These three responses were converted into 1 (yes) and 0 (no) values and added together to obtain a global index.
Psychological Variables
Psychological Well-Being
The Psychological General Well-Being Index (PGWB-I)37,38 consists of 22 items (6-point Likert scale), divided into six dimensions: Anxiety, Depressed mood, Positive well-being, Self-control, General health, and Vitality, and a global score of well-being. Higher scores indicating greater well-being and lower distress. The internal consistency of the questionnaire is adequate (alpha value higher than 0.74).
Psychological Symptomatology
The Symptom Checklist-90 (SCL-90)39,40 was administered to assess psychological symptomatology. The items are rated on a 5-point Likert scale, ranging from `not at all’ (0) to `extremely’ (4). Nine primary symptomatic dimensions are measured: Somatization, Obsessive-Compulsive, Interpersonal Sensitivity, Depression, Anxiety, Anger-Hostility, Phobic Anxiety, Paranoid Ideation, and Psychoticism. A Global Severity Index provides measures of the overall psychological distress. Higher scores indicate greater distress and psychopathological symptomatology. The internal consistency of SCL-90 is good for all its subscales (an alpha value ranging between 0.70 and 0.96).
State and Trait Anxiety: the State-Trait Anxiety Inventory (STAI)41,42 includes 40-items. The items are rated on 4-point Likert scales, ranging from 1 (not at all) to 4 (very much so). In both the State and Trait anxiety scales, higher scores indicate greater anxiety levels. In the present study, only State anxiety was considered. The reliability of the STAI is adequate (alpha values ranging between 0.90 and 0.93).
COVID-19 PTSD related symptoms: the Post-Traumatic Stress Disorder related to COVID-19 (COVID-19-PTSD)17 was adopted. The questionnaire includes 19 items structured on a 5-point Likert scale (from 0= not at all to 4= extremely). Higher scores indicate a higher risk of PTSD occurrence. The COVID-19 PTSD demonstrated excellent internal consistency (alpha value= 0.94).
Sleep Quality
Sleep characteristics have been assessed through the Pittsburgh Sleep Quality Index (PSQI),27,43 an 18-items questionnaire. The PSQI includes items evaluating sleep quality, sleep duration, sleep latency, habitual sleep efficiency, sleep disorders, the use of sleeping medications, and daytime dysfunctions. A global score indicates general sleep quality/sleep disturbance. Higher scores indicate poor sleep quality. The PSQI shows a high internal consistency (alpha= 0.83).
Ethical Consideration
The study was conducted in accordance with the Declaration of Helsinki and was approved by the Ethics Committee of the Department of Dynamic and Clinical Psychology, “Sapienza” University of Rome (protocol number: 0000266). To guarantee anonymity, no data which could allow the identification of participants were collected.
Statistical Analysis
Descriptive statistics of demographic variables were reported. The Structural equation modeling (SEM) was performed in R studio software to estimate a path model that can explain the direct relation between COVID-19-related variables and sleep quality and the possible moderator effect of psychological variables.
To check the adequate sample size for the study, previous studies were analyzed, and power analysis was conducted. According to some authors,44 a sample of 2.000 participants for the Structural Equation Modeling (SEM) analysis was considered a large sample condition. Moreover, a power analysis conducted specifically for survey online (CL: 95.5%; CI: 5), considering the target population (ie, adults between 18 and 74 years of age with internet access),45 confirmed that 2000 respondents represent an adequate sample size for statistical analyses.
The robust maximum likelihood estimator (MRL) was used for parameter estimation because it is most robust to the normality assumption violations.
We also controlled the model for age and gender as possible confounding variables. The χ2, the comparative fit index (CFI), Tucker-Lewis Index (TLI), and the root-mean-square error of approximation (RMSEA) indices were employed to determine whether the models fit the data. Good model fit was determined by the cut-off of 0.90 value for CFI and TLI and 0.08 for the RMSEA.
Results
Demographic Characteristics
Demographic characteristics of the respondents are reported in Table 1. The sample included 74.6% of women. The age range most represented was 18–29 years (68.6%), and the respondents presented generally high levels of education. The 51.4% of the respondents are settled in the South, 25% in the Centre, and 23.6.% in the North of Italy.
Table 1.
Demographic Characteristics of the Sample
| Total Sample (N= 2286) | |
|---|---|
| Sex, n (%) | |
| Man | 580 (25.4) |
| Woman | 1706 (74.6) |
| Age, n (%) | |
| 18–29 years old | 1568 (68.6) |
| 30–49 years old | 485 (21.2) |
| >50 years old | 233 (10.2) |
| Education, n (%) | |
| Until middle School | 97 (4.2) |
| High School | 1135 (49.6) |
| Undergraduate | |
| Health care | 246 (10.8) |
| Other | 658 (28.8) |
| Post-graduated | |
| Health care | 63 (2.8) |
| Other | 87 (3.8) |
| Occupation, n (%) | |
| Student | 1071 (46.8) |
| Employed | 687 (30.1) |
| Unemployed | 278 (12.2) |
| Self-Employed | 222 (9.7) |
| Retired | 28 (1.22) |
| Territorial areas | |
| North Italy | 540 (23.6) |
| Centre Italy | 571 (25.0) |
| South Italy | 1175 (51.4) |
| Number of inhabitants in own city, n (%) | |
| < 2.000 | 124 (5.4) |
| 2.000–10.000 | 451 (19.7) |
| 10.000–100.000 | 936 (50.0) |
| > 100.000 | 775 (33.9) |
| Quarantine experience, n (%) | |
| Alone | 2054 (89.9) |
| Others | 232 (10.1) |
| Infection by the virus | |
| Yes | 9 (0.4) |
| No | 1703 (74.5) |
| Do not know | 574 (25.1) |
| Direct contact with people infected by COVID-19 | |
| Yes | 40 (1.7) |
| No | 1438 (63.0) |
| Do not know | 808 (35.3) |
| Knowledge of people infected by COVID-19 | |
| Yes | 549 (24.0) |
| No | 1737 (76.0) |
| Knowledge of people in ICU for COVID-19 | |
| Yes | 177 (7.7) |
| No | 2109 (92.3) |
| Knowledge of people died for COVID-19 | |
| Yes | 112 (4.9) |
| No | 2174 (95.1) |
Note: From: Forte et al 2020.10
Abbreviation: ICU, intensive care unit.
Path Model
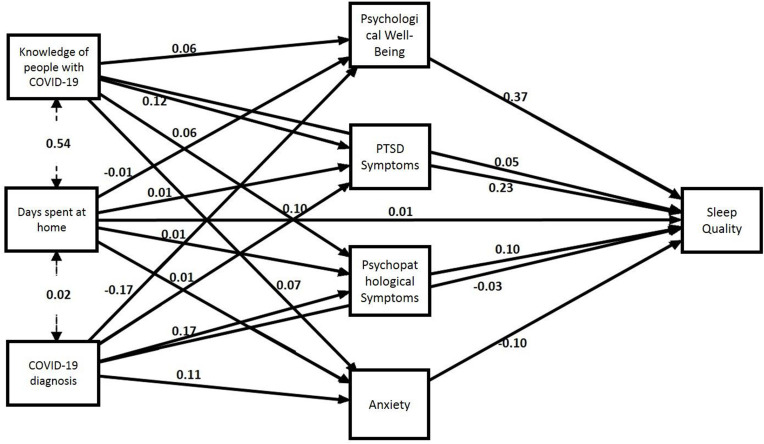
The path model fit adequately the overall data, χ2 (df= 14)= 314.42, p< 0.0001, CFI= 0.95, TLI= 92, RMSEA= 0.08, 90% CI [0.07, 0.09].
The analysis revealed that lower sleep quality was directly related to the days spent in confinement at home (p= 0.01) and the knowledge of people affected by the COVID-19 (p= 0.03), but not to a COVID-19 diagnosis (p= 0.51) (see Table 2).
Table 2.
The Direct Effect of COVID-19-Related Variables on Sleep Quality
| Estimate | Std.Err | z-value | p | |
|---|---|---|---|---|
| Infected by COVID-19 -> Sleep Quality | −0.03 | 0.03 | −0.065 | 0.51 |
| Days spent at home in confinement -> Sleep Quality | 0.01 | 0.003 | 3.89 | 0.001 |
| Knowledge of people infected by COVID-19* -> Sleep Quality | 0.05 | 0.02 | 2.09 | 0.03 |
Note: *Infected, in ICU or dead because of COVID-19.
Considering the total indirect effects, all the three variables COVID-19-related were significantly associated with lower sleep quality (all p< 0.05) (see Table 3). In particular, the presence of COVID-19 infection in respondents determined low sleep quality through all the psychological variables (all p< 0.05), except for the State Anxiety (p= 0.06). The days spent at home influenced the sleep quality through the mediation of PTSD symptomatology (p< 0.05) and general psychological symptomatology (p< 0.05), while there is no mediation role of psychological distress (p= 0.10) and state anxiety (p= 0.15). The effect of knowledge of people affected by COVID-19 on sleep quality was significantly mediated by psychological distress (p< 0.05) and PTSD symptomatology (p< 0.001), but not by state anxiety (p= 0.06) and general psychological symptomatology (p= 0.10) (see Table 4). We also controlled the model for age and gender, considered as confounding variables, but these variables did not produce significant changes in the texted model.
Table 3.
The Global Indirect Effect of COVID-19-Related Variables on Sleep Quality
| Estimate | Std. Err | z-value | p | |
|---|---|---|---|---|
| Infected by COVID-19 -> Sleep Quality | 0.09 | 0.2 | 3.24 | 0.001 |
| Days spent at home in confinement -> Sleep Quality | 0.005 | 0.002 | 2.23 | 0.02 |
| Knowledge of people infected by COVID-19* -> Sleep Quality | 0.05 | 0.02 | 2.63 | 0.01 |
Note: *Infected, in ICU or dead because of COVID-19.
Table 4.
Indirect Effects of COVID-19-Related Variables on Sleep Quality
| Estimate | Std. Err | z-value | p | |
|---|---|---|---|---|
| Affection by COVID-19 -> Psychological Well-Being -> Sleep Quality | 0.06 | 0.01 | 3.30 | 0.001 |
| Affection by COVID-19 -> COVID-PTSD -> Sleep Quality | 0.02 | 0.01 | 1.91 | 0.04 |
| Affection by COVID-19 -> State Anxiety -> Sleep Quality | −0.01 | 0.005 | −1.90 | 0.06 |
| Affection by COVID-19 -> Psychological Symptomatology-> Sleep Quality | 0.02 | 0.007 | 2.28 | 0.02 |
| Days spent at home -> Psychological Well-Being -> Sleep Quality | 0.002 | 0.001 | 1.63 | 0.10 |
| Days spent at home -> COVID-PTSD -> Sleep Quality | 0.002 | 0.001 | 2.22 | 0.02 |
| Days spent at home -> State Anxiety -> Sleep Quality | −0.001 | 0.002 | −1.44 | 0.15 |
| Days spent at home -> Psychological Symptomatology-> Sleep Quality | 0.001 | 0.001 | 2.21 | 0.02 |
| Knowledge of people infected by COVID-19* -> Psychological Well-Being -> Sleep Quality | 0.02 | 0.01 | 1.89 | 0.04 |
| Knowledge of people infected by COVID-19* -> COVID-PTSD -> Sleep Quality | 0.03 | 0.01 | 3.26 | 0.001 |
| Knowledge of people infected by COVID-19* -> State Anxiety -> Sleep Quality | −0.01 | 0.01 | −1.89 | 0.06 |
| Knowledge of people infected by COVID-19* -> Psychological Symptomatology-> Sleep Quality | 0.01 | 0.01 | 1.63 | 0.10 |
Note: *Infected, in ICU or dead because of COVID-19.
Figure 1 reports the path diagram.
Figure 1.
The path diagram.
Discussion
This study aimed to assess the association between COVID-19-related aspects and sleep quality, considering the moderator role of some psychological variables in this relationship.
Many studies have shown a worsening of sleep quality and a high prevalence of sleep disorders during the first phase of the COVID-19 pandemic spread.8,11,16,25 Lower sleep quality and increased sleep disturbances were confirmed by Italian15,16,19,24,28 and international8,13,25 studies. However, no study has clarified whether this impairment of sleep quality was directly determined by the variables associated with COVID-19 (eg, the risk of infection; the confinement at home) or whether it was due to the altered psychological condition caused by the pandemic. Accordingly, this study examined the role of different psychological variables (psychological well-being, COVID-19 PTSD related symptoms, psychological symptomatology, and state of anxiety) as potential mediators of the relationship between some aspects specifically related to the COVID-19 pandemic (ie, to have a COVID-19 diagnosis, number of days spent at home after the confinement measures, knowledge of people affected at different degrees by COVID-19) and self-reported sleep quality in an Italian sample during the lockdown. The principal objectives were to clarify whether some COVID-19-related aspects, directly and indirectly, affect sleep quality during this health emergency through their influence on psychological states.
Results confirm a direct effect of some aspects ascribable to the pandemic.16,18 The first period of the pandemic spread in Italy and, consequently, the first phase of the lockdown, the confinement at home, and the consequential social distancing, directly impaired the participants’ sleep quality. COVID-19-related aspect and the confinement at home also affected the participants’ psychological condition, confirming a mediator role of psychological distress (PGWB), PTSD symptoms (COVID-19-PTSD), and psychological symptoms (SCL-90) on self-reported sleep quality.
Although a high level of anxiety during the emergency was reported, it does not appear to play a modulator role in sleep quality.16,18,34 This result is surprising and unexpected. It is proved that anxiety negatively affects sleep quality;46 however, this role did not emerge in our model. This result may depend on the weight assumed by other psychological variables such as distress or PTSD symptoms COVID-19 related. Accordingly, many Italians experienced the first period of the pandemic spread and the lockdown as a traumatic event. In fact, in this period, a high percentage of PTSD symptomatology (29.5%) was found in the Italian population.17,18
Generally, evidence of an impairment of sleep quality and increased sleep disturbances during the COVID-19 pandemic has been reported in the general population and specific conditions (eg, health care workers).15,16,19,24,47,48 This worsening was described in heterogeneous samples (eg, university students, health care professionals, people subjected to the quarantine dispositions, general population), and it was often associated with other psychological conditions, such as anxiety or PTSD symptomatology.
Our previous work16 highlighted that some aspects related to COVID-19 would represent possible risk factors for sleep disturbances, specifically the uncertainty regarding direct contact with individuals infected by COVID-19 and the knowledge of people that died because of COVID-19. Accordingly, a recent study reported that fear of contagion impacts individuals’ mental health, including consequences on the quality of sleep.49 Our current study added some information on this aspect. It seems that there are multiple aspects associated with the pandemic experience that appears to affect sleep quality in different ways. The uncertainty or the confirmation of a COVID-19 diagnosis indirectly influences, via psychological dimensions, sleep quality. However, other aspects related to this exceptional event, as the days spent in confinement at home (ie, social isolation) and the knowledge of people affected at different severities by the COVID-19, including also dead people (ie, the fear of the impact of the infection) directly influences sleep quality.
Considering the moderator effects of psychological variables, some interesting considerations can be addressed. The high post-traumatic symptomatology associated with the COVID-19 experience appears to have a mediating role in sleep quality. This result would confirm previous findings that have shown high PTSD symptoms in conditions of severe emergencies, epidemics, and, more recently, the COVID-19 pandemic.16–18,50 Moreover, these symptoms would be directly related to sleep quality.51,52 These results appear important and need to be considered from a clinical perspective given the findings that detected high rates of COVID-related PTSD in the worldwide and Italian populations.9,18,53,54
A similar trend was reported considering the psychological symptomatology measured with SCL-90. The COVID-19 emergency exacerbates the psychopathological symptoms, in line with previous evidence that compared psychopathological symptoms measured during the COVID-19 pandemic with normative data from the general population.18 In this study, we underlined the influence of the psychopathological condition on sleep quality without ignoring the role of COVID-19 experience and reporting a strong link between the environmental situation and the psychological condition.
The general psychological well-being that, inversely, can be considered as an index of psychological distress, again, acts as a mediator of the relationship between COVID-19 variables and sleep quality. The worsening of psychological well-being during the COVID-19 emergency impacted sleep quality and sleep disturbances.
Although this study reported some interesting findings, certain limitations should be highlighted. First, the sample’s recruitment was carried out with an online survey, and the poor control of self-reported measures represents a limit in the path model generalizability. The cross-sectional design is another limit because it did not allow understanding the causal nature of the relationship and whether this relationship is confirmed or modulated over time and with the changes in the pandemic situation. However, the study aimed to highlight the Italian population’s state in the first days after the lockdown; therefore, a longitudinal design was impossible to use. Furthermore, greater control of potentially confounding variables such as gender, occupational status, age, medical conditions, lifestyle changes involving health behavior (eg, sedentary behavior, maladaptive eating habits) should be done according to the results of previous studies highlighting the role of certain demographic or lifestyle variables as possible risk factors for sleep quality.9 Moreover, the adoption of a self-report measure to evaluate the quality and quantity of sleep might represent a limit in reliability and may not highlight specific characteristics of the sleep pattern during a pandemic. Similarly, the adoption of a questionnaire to assess psychological variables could not identify mental illnesses, representing a further limitation of the study.
Conclusions
In the face of an unprecedented medical emergency, which has directly impacted the fear of contagion and the indirect risks associated with it, the present findings highlight the importance of also considering the psychological effects.
The COVID-19 spread has undoubtedly influenced the people’s psychological state, but it has also played a mediating role in the pandemic consequences. In this study, the central focus was on the quality of sleep, which directly influences many daily activities, and it is involved, at multiple levels, in the psychological,55,56 cognitive57,58 and physical59 well-being of individuals. Interventions to promote a good quality of sleep and reduce sleep disorders in these critical phases cannot ignore aspects such as distress, psychological symptoms, and PTSD symptoms. All these aspects, being influenced by the COVID-19 experience and being mediators of the impact on sleep quality, must be well evaluated before implementing interventions to solve sleep diseases related to this extraordinary event, both in the medium and long terms.
To counteract the increase in sleep disturbances and the worsening of sleep quality due to pandemic, it would be useful to adopt countermeasures, such as general sleep hygiene programs (eg, maintaining sleep and waking times, adequate physical activity, proper nutrition, good organization of the day, avoiding overexposure to news COVID-19 related, especially in the evening). However, our results show that this emergency and the social distancing and confinement at home norms lead to psychological diseases that worsen sleep quality. Therefore, governments should provide clinical and counseling centers and online platforms consisting of psychologists and sleep experts to improve the psychological condition and provide adequate sleep hygiene support.
Acknowledgments
This work was supported by a grant from the “Sapienza” University of Rome.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Serafini G, Parmigiani B, Amerio A, Aguglia A, Sher L, Amore M. The psychological impact of COVID-19 on the mental health in the general population. QJM. 2020;113(8):531–537. doi: 10.1093/qjmed/hcaa201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ali I, Alharbi OM. COVID-19: disease, management, treatment, and social impact. Sci Total Environ. 2020;728:138861. doi: 10.1016/j.scitotenv.2020.138861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saladino V, Algeri D, Auriemma V. The psychological and social impact of Covid-19: new perspectives of well-being. Front Psychol. 2020;11:2550. doi: 10.3389/fpsyg.2020.577684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.World Health Organization. Coronavirus disease (COVID-2019) situation reports. 2020. Available from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports/. Accessed November20, 2020.
- 5.Istituto Superiore di Sanità. Epicentro. Coronavirus. 2020. Available from: https://www.epicentro.iss.it/coronavirus/. Accessed November20, 2020.
- 6.Qiu J, Shen B, Zhao M, Wang Z, Xie B, Xu Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33(2). doi: 10.1136/gpsych-2020-100213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Petzold MB, Bendau A, Plag J, et al. Risk, resilience, psychological distress, and anxiety at the beginning of the COVID-19 pandemic in Germany. Brain Behav. 2020;10(9):e01745. doi: 10.1002/brb3.1745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fu W, Wang C, Zou L, et al. Psychological health, sleep quality, and coping styles to stress facing the COVID-19 in Wuhan, China. Transl Psychiatry. 2020;10(1):1–9. doi: 10.1038/s41398-020-00913-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Liu N, Zhang F, Wei C, et al. Prevalence and predictors of PTSS during COVID-19 outbreak in China hardest-hit areas: gender differences matter. Psych Res. 2020;112921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Karatzias T, Shevlin M, Murphy J, et al. Posttraumatic stress symptoms and associated comorbidity during the COVID-19 pandemic in Ireland: a population-based study. J Trauma Stress. 2020;33(4):365–370. doi: 10.1002/jts.22565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Salari N, Hosseinian-Far A, Jalali R, et al. Prevalence of stress, anxiety, depression among the general population during the COVID-19 pandemic: a systematic review and meta-analysis. Glob Health. 2020;16(1):1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rajkumar RP. COVID-19 and mental health: a review of the existing literature. Asian J Psychiatr. 2020;102066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Voitsidis P, Gliatas I, Bairachtari V, et al. Insomnia during the COVID-19 pandemic in a Greek population. Psych Res. 2020:113076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mazza C, Ricci E, Biondi S, et al. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: immediate psychological responses and associated factors. Int J Environ Res. 2020;17(9):3165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Marelli S, Castelnuovo A, Somma A, et al. Impact of COVID-19 lockdown on sleep quality in university students and administration staff. J Neurol. 2020;1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Casagrande M, Favieri F, Tambelli R, Forte G. The enemy who sealed the world: effects quarantine due to the COVID-19 on sleep quality, anxiety, and psychological distress in the Italian population. Sleep Med. 2020;75:12–20. doi: 10.1016/j.sleep.2020.05.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Forte G, Favieri F, Tambelli R, Casagrande M. COVID-19 Pandemic in the Italian Population: validation of a Post-Traumatic Stress Disorder Questionnaire and Prevalence of PTSD Symptomatology. Int J Environ Res Public Health. 2020;17(11):4151. doi: 10.3390/ijerph17114151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Forte G, Favieri F, Tambelli R, Casagrande M. The Enemy Which Sealed the World: effects of COVID-19 Diffusion on the Psychological State of the Italian Population. J Clin Med. 2020;9(6):1802. doi: 10.3390/jcm9061802 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gualano MR, Lo Moro G, Voglino G, et al. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health. 2020;17(13):4779. doi: 10.3390/ijerph17134779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rossi R, Socci V, Talevi D, et al. COVID-19 pandemic and lockdown measures impact on mental health among the general population in Italy. Front Psychiat. 2020;11:790. doi: 10.3389/fpsyt.2020.00790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Di Renzo L, Gualtieri P, Pivari F, et al. Eating habits and lifestyle changes during COVID-19 lockdown: an Italian survey. J Transl Med. 2020;18(1):1–15. doi: 10.1186/s12967-020-02399-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Carriedo A, Cecchini JA, Fernandez-Rio J, Méndez-Giménez A. COVID-19, psychological well-being and physical activity levels in older adults during the nationwide lockdown in Spain. Am J Geriatr Psychiatry. 2020;28(11):1146–1155. doi: 10.1016/j.jagp.2020.08.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jacob L, Tully MA, Barnett Y, et al. The relationship between physical activity and mental health in a sample of the UK public: a cross-sectional study during the implementation of COVID-19 social distancing measures. Ment Health Phys Act. 2020;19:100345. doi: 10.1016/j.mhpa.2020.100345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cellini N, Canale N, Mioni G, Costa S. Changes in sleep pattern, sense of time and digital media use during COVID-19 lockdown in Italy. J Sleep Res. 2020;e13074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jahrami H, BaHammam AS, Bragazzi NL, Saif Z, Faris M, Vitiello MV. Sleep problems during COVID-19 pandemic by population: a systematic review and meta-analysis. J Clin Sleep Med. 2020;jcsm–8930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sher L. COVID-19, anxiety, sleep disturbances and suicide. Sleep Med. 2020;70:124. doi: 10.1016/j.sleep.2020.04.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Buysse DJ, Reynolds III CF, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psych Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4 [DOI] [PubMed] [Google Scholar]
- 28.Salfi F, Lauriola M, Amicucci G, et al. Gender-related time course of sleep disturbances and psychological symptoms during the COVID-19 lockdown: a longitudinal study on the Italian population. Neurobiol Stress. 2020;13:100259. doi: 10.1016/j.ynstr.2020.100259 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Morin CM, Carrier J. The acute effects of the COVID-19 pandemic on insomnia and psychological symptoms. Sleep Med. 2020;S1389–9457(20):30261–30266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Franceschini C, Musetti A, Zenesini C. Poor quality of sleep and its consequences on mental health during COVID-19 lockdown in Italy. Psyarxiv Preprint. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Friedrich A, Schlarb AA. Let’s talk about sleep: a systematic review of psychological interventions to improve sleep in college students. J Sleep Res. 2018;27(1):4–22. doi: 10.1111/jsr.12568 [DOI] [PubMed] [Google Scholar]
- 32.Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: a review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23(4):2324–2332. doi: 10.1111/jcmm.14170 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Altena E, Baglioni C, Espie CA, et al. Dealing with sleep problems during home confinement due to the COVID-19 outbreak: practical recommendations from a task force of the European CBT-I academy. J Sleep Res. 2020;e13052. [DOI] [PubMed] [Google Scholar]
- 34.Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psych Res. 2020;288:112954. doi: 10.1016/j.psychres.2020.112954 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Xiao H, Zhang Y, Kong D, et al. The effects of social support on sleep quality of medical staff treating patients with coronavirus disease 2019 (COVID-19) in January and February 2020 in China. Med Sci Monit. 2020;26:e923549–1. doi: 10.12659/MSM.923921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ernstsen L, Havnen A. Mental health and sleep disturbances in physically active adults during the COVID-19 lockdown in Norway: does change in physical activity level matter? Sleep Med. 2020. doi: 10.1016/j.sleep.2020.08.030 [DOI] [PubMed] [Google Scholar]
- 37.Dupuy HJ, Wenger NK, Mattson ME, Fuberg CP. Assessment of Quality of Life in Clinical Trials of Cardiovascular Therapies. New York: Le Jacq; 1984. [DOI] [PubMed] [Google Scholar]
- 38.Grossi E, Mosconi P, Groth N, Niero M, Apolone G. Questionario Psychological General Well.-Being Index: Versione Italiana. Milano: Istituto Farmacologiao Mario Negri; 2002. [Google Scholar]
- 39.Derogatis LR, Cleary PA. Confirmation of the dimensional structure of the SCL‐90: a study in construct validation. J Clin Psych. 1977;33(4):981–989. doi: [DOI] [Google Scholar]
- 40.Cassano GB, Conti L, Levine J. SCL-90 In Repertorio Delle Scale di Valutazione in Psichiatria. Firenze, Italy: SEE; 1999:325–332. [Google Scholar]
- 41.Spielberger CD. State-Trait Anxiety Inventory for Adults. Palo Alto, CA: Mind Garden; 1983. [Google Scholar]
- 42.Pedrabissi L, Santinello M. Verifica Della Validità Dello STAI forma Y di Spielberger. Firenze, Italy: Giunti Organizzazioni Speciali; 1989. [Google Scholar]
- 43.Curcio G, Tempesta D, Scarlata S, et al. Validity of the Italian version of the Pittsburgh sleep quality index (PSQI). Neurol Sci. 2013;34(4):511e9. doi: 10.1007/s10072-012-1085-y [DOI] [PubMed] [Google Scholar]
- 44.Sivo SA, Fan X, Witta EL, Willse JT. The search for” optimal” cutoff properties: fit index criteria in structural equation modeling. J Exp Educ. 2006;74(3):267–288. doi: 10.3200/JEXE.74.3.267-288 [DOI] [Google Scholar]
- 45.Istituto Nazionale di Statistica. Datie Microdati Popolazione Italiana. Available from: https://www.istat.it/it/popolazione-e-famiglie. Accessed November20, 2020.
- 46.Cox RC, Olatunji BO. A systematic review of sleep disturbance in anxiety and related disorders. J Anxiety Disord. 2016;37:104–129. doi: 10.1016/j.janxdis.2015.12.001 [DOI] [PubMed] [Google Scholar]
- 47.Majumdar P, Biswas A, Sahu S. COVID-19 pandemic and lockdown: cause of sleep disruption, depression, somatic pain, and increased screen exposure of office workers and students of India. Chronob Int. 2020;1–10. [DOI] [PubMed] [Google Scholar]
- 48.Zhuo K, Gao C, Wang X, et al. Stress and sleep: a survey based on wearable sleep trackers among medical and nursing staff in Wuhan during the COVID-19 pandemic. Gen Psych. 2020;33(3). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychol Trauma. 2020;12(S1):17–21. doi: 10.1037/tra0000924 [DOI] [PubMed] [Google Scholar]
- 50.Brooks SK, Webster RK, Smith LE, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395(10227):912–920. doi: 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Germain A, Hall M, Krakow B, et al. A brief sleep scale for posttraumatic stress disorder: Pittsburgh sleep quality index addendum for PTSD. J Anxiety Disord. 2005;19(2):233–244. doi: 10.1016/j.janxdis.2004.02.001 [DOI] [PubMed] [Google Scholar]
- 52.Strasshofer DR, Pacella ML, Irish LA, et al. The role of perceived sleep quality in the relationship between PTSD symptoms and general mental health. Mental Health Prev. 2017;5:27–32. doi: 10.1016/j.mhp.2017.01.001 [DOI] [Google Scholar]
- 53.Tang W, Hu T, Hu B, et al. Prevalence and correlates of PTSD and depressive symptoms one month after the outbreak of the COVID-19 epidemic in a sample of home-quarantined Chinese university students. J Affect Disord. 2020;274:1–7. doi: 10.1016/j.jad.2020.05.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fekih-Romdhane F, Ghrissi F, Abbassi B, et al. Prevalence and predictors of PTSD during the COVID-19 pandemic: findings from a Tunisian community sample. Psychiatry Res. 2020;290:113131. doi: 10.1016/j.psychres.2020.113131 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Saunders EF, Fernandez-Mendoza J, Kamali M, et al. The effect of poor sleep quality on mood outcome differs between men and women: a longitudinal study of bipolar disorder. J Affect Disord. 2015;180:90–96. doi: 10.1016/j.jad.2015.03.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tkachenko O, Olson EA, Weber M, et al. Sleep difficulties are associated with increased symptoms of psychopathology. Exp Brain Res. 2014;232(5):1567–1574. doi: 10.1007/s00221-014-3827-y [DOI] [PubMed] [Google Scholar]
- 57.Nebes RD, Buysse DJ, Halligan EM, et al. Self-reported sleep quality predicts poor cognitive performance in healthy older adults. J Gerontol. 2009;64B(2):180–187. doi: 10.1093/geronb/gbn037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Porter VR, Buxton WG, Avidan AY. Sleep, cognition and dementia. Curr Psych Rep. 2015;17(12):97. doi: 10.1007/s11920-015-0631-8 [DOI] [PubMed] [Google Scholar]
- 59.Gothe NP, Ehlers DK, Salerno EA, et al. Physical activity, sleep and quality of life in older adults: influence of physical, mental and social well-being. Behav Sleep Med. 2019;1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]