Summary
Adequate resuscitation of acute burn patients is important to ensure end organ perfusion and oxygenation. The ideal marker to the endpoint of burn resuscitation is still not established. We aimed to evaluate the role of blood lactate and lactate clearance in burn resuscitation and their association with mortality and sepsis in burn patients. The retrospective study included patients (18-50 years) with thermal and scald burns with total body surface area of 30% to 60% over a period of 9 months who had achieved target urine output of at least 0.5ml/kg/hr within 24 hours of resuscitation. Patients were divided based on their admission blood lactate levels (Group A < 2 mmol/L and Group B > 2 mmol/L). Group B was further subdivided into Group B1 in whom blood lactate levels reached less than 2 mmol/L within 24 hours of burn resuscitation and Group B2 in whom it did not. Total patients included were 203. Mortality (M) and sepsis (S) rates in subgroup B2 were higher (M=57.9%; S=43.5%) and rates in subgroup B1 (M=25.8%; S=27.4%) were comparable to Group A (M=27.8%; S=26.4%). Persistent lactic acidosis at 24 hours was independently associated with significantly increased mortality and sepsis. Our data suggests a correlation of blood lactate levels and lactate clearance within 24 hours of admission with mortality and sepsis related to burn injury.
Keywords: burns, blood lactate, lactate clearance, mortality, prognostic biomarker, sepsis
Abstract
Un remplissage vasculaire adapté est nécessaire afin de préserver la perfusion et l’oxygénation tissulaires des brûlés. Le marqueur idéal de sa qualité reste à trouver. Nous avons évalué la lactatémie et l’élimination des lactates dans ce but, ainsi que leur corrélation avec la mortalité et le sepsis. Nous avons étudié rétrospectivement, sur 9 mois, 203 patients de 18 à 50 ans, brûlés sur 30 à 60% de SCT, ayant eu une diurèse horaire de plus de 0,5 mL/kg/h dans les 24 premières heures suivant leur brûlure. Le groupe A avait moins de 2 mmol/L de lactate à l’admission, le groupe B plus. Ce dernier groupe a été subdivisé en B1 (lactate redescendant à moins de 2 mmol/L dans les 24 premières heures) et B2 ne le faisant pas. La mortalité de B2 était plus élevée (57,8%) que A (27,8%) et B1 (25,8%), ces 2 derniers groupes étant comparables. De même, un sepsis survenait chez 43,5% des patients de B2 contre 27,4% pour B1 et 26,4% pour A. Plus que leur valeur initiale, c’est l’absence de décroissance dans les 24 premières heures des lactates qui est un marqueur de mauvais pronostic chez le brûlé.
Introduction
Burn injury results in severe hemodynamic derangements that initially start as rapid depletion of intravascular volume primarily caused by severe capillary leak. Burn shock to begin with is hypovolemic and is manifested by marked hemodynamic changes comprising diminished cardiac output, plasma volume and urinary output with sequentially elevated systemic vascular resistance subsequently leading to reduced peripheral blood flow.1 To counteract these hemodynamic changes and to restore homeostasis, fluid resuscitation should be initiated at the earliest. Resuscitation of these critical burn patients is targeted by a blend of clinical assessments, blood investigations and invasive monitors. The end point of the exercise of resuscitation is to restore the circulating volume, establish cellular oxygenation, aerobic end organ metabolism and correct the acidosis ensued during the injury.2 The ideal marker to the endpoint of burn resuscitation is still not established. Blood lactate has been studied as one such end point marker of resuscitation in shock. The correlation between blood lactate and cellular hypoxia has been established in the trauma and burn setting. 3,4 In contrast to the existing evidence, data on blood lactate and lactate clearance in burn shock in the Indian subcontinent is not available and for the rest of the world it is sparse. The aim of this study was to evaluate if blood lactate and lactate clearance is a valuable parameter in the evaluation of mortality and sepsis in burn patients.
Methodology
Study setting
The study was retrospective in design and was conducted from January to September 2019 at the Department of Burns, Plastic & Maxillofacial Surgery, VM Medical College & Safdarjung Hospital, Delhi, a tertiary burn care centre in India.
Study population
Patients who presented to the Department of Burns and Plastic Surgery from January to September 2019 with thermal or scald burns involving total body surface area of 30-60% and who achieved a target urine output of at least 0.5ml/kg/hr within 24 hours of resuscitation were included in the study. The exclusion criteria included associated trauma other than burns, presentation to our burn care facility after 24 hours from time of burn, organ failure, pre-existing comorbidities and documented infection pre burn.
Data and definitions
Data were collected using Microsoft Excel 2010 (Microsoft, USA) for eligible patients at the time of admission.
Fluid resuscitation was done using institutional protocol: first 24 hours: 2ml/kg/% burns (lactated ringer) + 50ml/kg/day (dextrose normal saline) was calculated. Half of the calculated volume was administered in the first 8 hours post-burn injury and the remaining half of the calculated volume was administered in the following 16 hours. For the second 24 hours: 1ml/kg/% burns (lactated ringer) + 50ml/kg/day (dextrose normal saline) was administered. After 48 hours: 40ml/kg/day + (25+body surface area burnt) x body surface area x 24 (dextrose normal saline) was calculated and given.5
Blood lactate values were assessed using Radiometer ABL 800 flex analyser every 4 hours in the first 24 hours, every 6 hours in the next 24 hours and every 12 hours in the next 24 hours post burn/normalisation of two consecutive blood lactate values, whichever was earlier.
Sepsis was defined by the presence of 3 or more of the following criteria: 1) tachycardia (heart rate >90 beats/min), 2) tachypnea (respiratory rate >20 breaths/min), 3) fever or hypothermia (temperature >38 or <36 °C), 4) leukocytosis or leukopenia (white blood cells >1,2000/mm3 or <4,000/mm3 respectively) along with documented infection or clinical suspicion of infection.6
Statistical analysis
The population was divided based on admission blood lactate levels. Group A consisted of patients with blood lactate levels less than 2 mmol/L and Group B with blood lactate levels more than 2 mmol/L. Group B was further subdivided into Group B1 in whom blood lactate levels reached less than 2 mmol/L within 24 hours of burn resuscitation and Group B2 in whom blood lactate levels did not fall below 2 mmol/L within 24 hours of burn resuscitation. General population characteristics were analysed between the groups. Data were analysed for any association between the groups and sub groups with mortality and sepsis. Mean and median were used to represent the skewed data. The continuous variables were compared using t test. A p value <0.05 was considered statistically significant.
Results
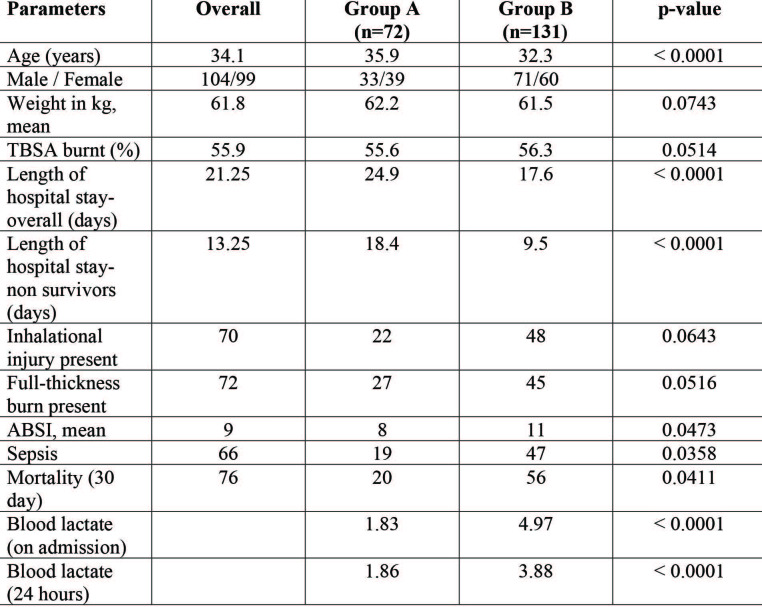
A total of 203 patients were included in the study. The mean age of the study population was 34.1 years (18-50 years). Fifty-two percent of the patients were in the age group of 20-35 years and 51% of the patients were male. Mean total body surface area (TBSA) involved was 55.9% (30-60%). The mean duration of hospital stay was 21.25 days (11-45 days). Seventy patients had inhalational burns. Sixty-six patients developed sepsis during their hospital stay. Mortality within 30 days post burn was seen in 76 patients (Table I).
Table I. Population characteristics.
Seventy-two patients had blood lactate levels at admission less than 2 mmol/L (Group A) and their mean abbreviated burn severity index (ABSI) was 8. Sepsis was clinically detected in 19 patients and 20 patients expired during the first post burn month. The average duration of hospital stay was 24.9 days. Group B included 131 patients with blood lactate levels at admission greater than 2 mmol/L and their mean ABSI was 11. Sepsis was clinically detected in 47 patients and 56 patients expired during the first post burn month. The average duration of hospital stay was 17.6 days.
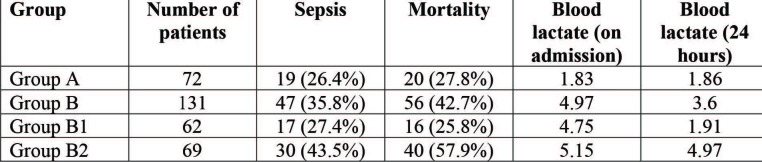
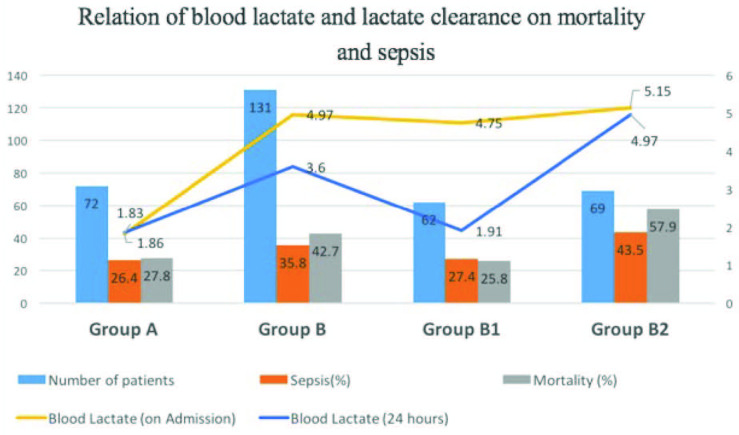
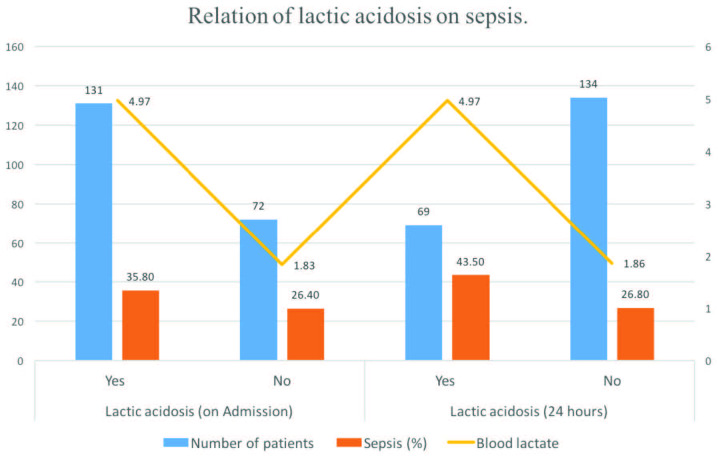
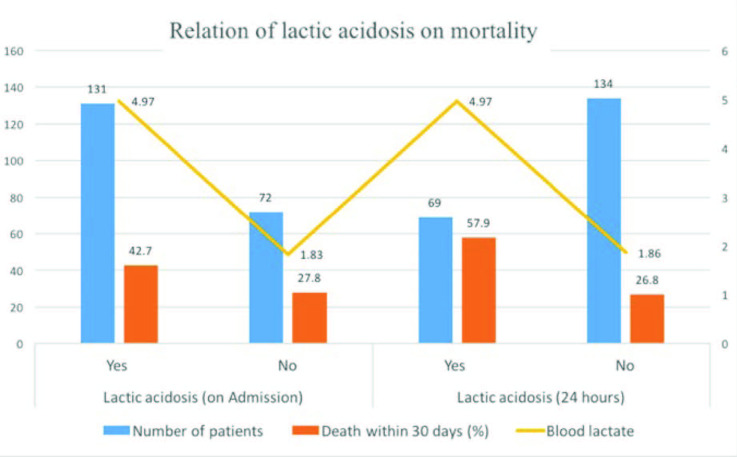
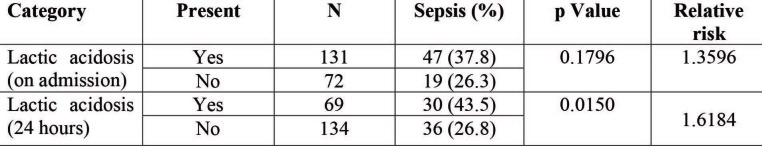
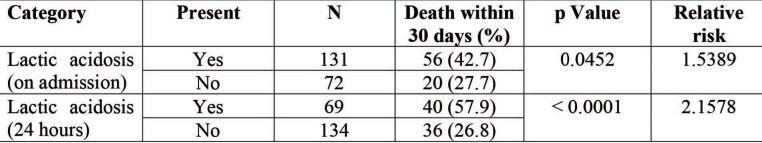
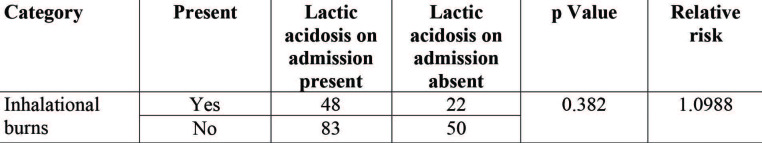
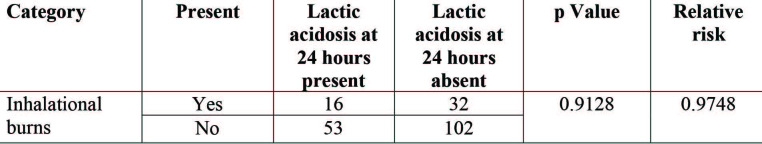
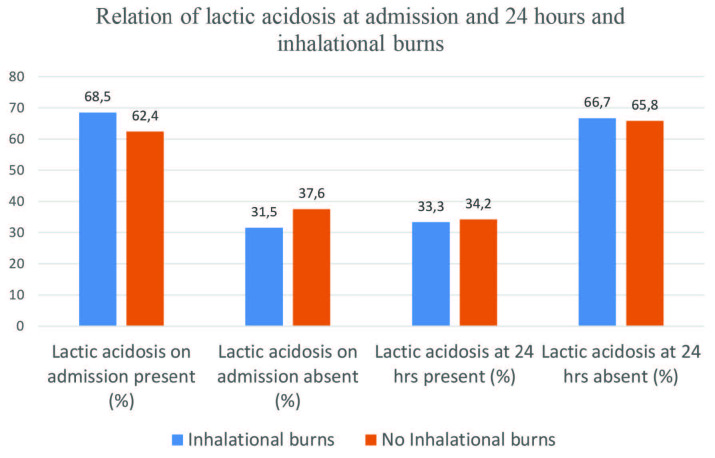
Subgroup analysis was done for patients in Group B with relation to blood lactate clearance at 24 hours. In subgroup B1 the blood lactate reached values <2 mmol/L at 24 hours and in subgroup B2 the values persisted to be elevated >2 mmol/L at 24 hours. The mortality rate in subgroup B1 and B2 was 25.8% and 57.9% respectively. The sepsis rate in subgroup B1 and B2 was 27.4% and 43.5% respectively. The mortality and sepsis rates in subgroup B2 were higher and the rates in subgroup B1 were comparable to Group A (Table II) (Fig. 1). The difference in mortality and sepsis rates in subgroups of group B was statistically significant. Lactic acidosis on admission and at 24 hours was studied for associated mortality and sepsis. Persistent lactic acidosis at 24 hours was independently associated with significantly increased mortality and sepsis (Figs. 2 and 3). The overall relative risk of mortality and sepsis in the presence of lactic acidosis at 24 hours was 2.1578 and 1.6184 respectively (Tables III and IV). Another subgroup analysis was done to understand the relationship between inhalational burns and lactic acidosis. The overall relative risk of lactic acidosis on admission and at 24 hours with inhalational burns was 1.0988 and 0.9748 respectively. The association was not statistically significant (Tables V and VI) (Fig. 4).
Table II. Relation of blood lactate and lactate clearance on mortality and sepsis.
Fig. 1. Relation of blood lactate and lactate clearance on mortality and sepsis.
Fig. 2. Relation of lactic acidosis on sepsis.
Fig. 3. Relation of lactic acidosis on mortality.
Table III. Relation of lactic acidosis on sepsis.
Table IV. Relation of lactic acidosis on mortality.
Table V. Relation of lactic acidosis on admission and inhalational.
Table VI. Relation of lactic acidosis at 24 hours and inhalational.
Fig. 4. Relation of lactic acidosis at admission and 24 hours and inhalational burns.
Discussion
Adequate fluid resuscitation has been found to reduce mortality in burn patients. The best marker for monitoring adequacy of burn resuscitation is still under question. An ideal marker would require it to be accurate, reproducible and adequately reflect dynamic changes during resuscitation.7 In fluid resuscitation of acute burns, conventionally used markers such as blood pressure and urine output, though commonly used, are not reliable.8 Stress response to catecholamines tends to maintain blood pressure in the face of decreasing circulating volume over variable periods of time.9 Invasive monitoring often leads to over resuscitation with fluids and is labour intensive. 10 Lactic acidosis in burns occurs as a result of both increased production and decreased clearance of lactate. Anaerobic metabolism induced by cellular hypoxia as a result of hypo-perfusion causes increased production of lactate. Hepatic clearance of lactate is also reduced in shock scenarios.11 In the setting of septic and hemorrhagic shock, blood lactate has been found to correlate with clinical outcome.12 Blood lactate levels have been used as an indicator in sepsis.13 Blood lactate levels are shown to predict microcirculation and global tissue hypoxia. Lactic acidosis can decrease cardiac contractibility, cardiac output, increase arrhythmogenicity and decrease responsiveness to catecholamines.14 Lactate levels and base deficit have been found to be associated with burn mortality.7,15,16
In this retrospective study of 203 patients, we intended to demonstrate blood lactate as a marker to predict outcomes in burns. Mean ABSI was higher in Group B patients. Overall 30-day mortality was 37.4% in our cohort, which is higher than that reported in other studies.7,15,16 Inhalational injury was present in 34.4% of cases. The rates of inhalational injury were higher in Group B; the difference was not statistically significant. It is known that the associated mortality rates are higher in inhalational injury; hence a subgroup analysis was done to know the association of lactic acidosis and inhalational injury. In our study, there was no statistically significant increased risk in the inhalational burn subgroup to develop lactic acidosis. In their study, Mokline et al. did not find inhalational injury to be an independent predictor of mortality.17 In Group B, mean hospital stay was lower, mainly because of the higher mortality rates. These deaths occurred much earlier during their hospital course (9.5 vs 18.4 days).
Group A patients had significantly lower occurrence of sepsis (26.3%) and 30-day mortality (27.7%) than Group B (sepsis - 35.8%, mortality - 42.7%). Cochran et al. demonstrated that burn patients who died had significantly increased lactate levels in the first 48 hours, but they did not find a specific threshold value in their study.15 Herero et al. showed that there was 31.3% mortality for patients with a blood lactate at admission of ≥2 mmol/l versus 6% in patients with a blood lactate at admission of <2 mmol/L.18 Average time for lactate clearance in survivors was significantly less than in non survivors (2.02 vs 4.6 days, p<0.02). In their study of 80 burn patients Mokline et al. suggested that initial lactate levels provided the best sensitivity (88%) and specificity (79%) for predicting sepsis (ROC- 0.82). Blood lactate for prediction of mortality had a good sensitivity (86%) and specificity (92%) in their study.17 However, Cochrane et al. found no association between lactate levels on admission with mortality.15 In our study we found that patients who cleared lactate within the first 24 hours had significantly lower mortality (25.8%) and sepsis rates (27.4%) than those who did not clear lactate. In fact, the rates of mortality and sepsis in the group who cleared lactate within the first 24 hours was comparable to patients who had baseline lactate levels of <2 mmol/L. Blood lactate levels did not correlate with total burn surface area. Both Groups A and B had similar TBSA. In our study, average total body surface area burned was 55.9%, which is similar to other studies evaluating the role of lactate in burns.15 Lactate clearance has been demonstrated in a few studies to be a good marker of resuscitation in burns and other types of shock.12,19 In patients with sepsis and trauma, lactate clearance has shown improved outcomes.12,19 In addition, it has been proposed as an early predictor of death in patients with burn injuries. Kamolz et al. prospectively evaluated lactate levels in 166 burn patients. They observed that survivors and non survivors could be separated based on initial lactate level. Moreover, patients who cleared lactate within 24 hours had a 68% chance of survival compared to patients who had a lactate of >2mmol/L (27% chance of survival).7 For each 10% increase in lactate clearance, an 11% decrease in mortality occurs.19
In spite of many studies reiterating the importance of blood lactate and lactate clearance in predicting mortality in burn patients, the role of these markers in the titration of therapy is ambiguous. Overzealous fluid resuscitation may cause fluid overload and acute respiratory distress syndrome. Also, there is not much regional data available to establish the importance of blood lactate and lactate clearance. We demonstrated the association of blood lactate level at the time of admission and lactate clearance with mortality and sepsis. However, to establish the causal relationship, further large multicenter prospective studies are required.
Conclusion
Traditional end points of burn resuscitation are being extensively used clinically. However these end points of resuscitation are not the ideal markers. The high-end resource extensive devices are not easily available in resource-restricted environments. Our data suggest a correlation of blood lactate levels and lactate clearance within 24 hours of admission with mortality and sepsis related to burn injury. Hence directing measures to normalize lactate levels in addition to the traditional resuscitation end points might lead to better outcomes in burn patients. Our study is limited due to its retrospective nature and limited population. Further prospective studies with larger study populations are required to establish blood lactate and lactate clearance as endpoint in resuscitation of burn patients and its clinical application to improve the outcomes in care of burn patients. Although we have studied inhalational injury and its association with lactic acidosis, there could be other confounding variables that have not been extensively studied in this study.
References
- 1.Shirani KZ, Vaughan GM, Mason AD, Pruitt BA. Update on current therapeutic approaches in burns. Shock. 1996;5:4–16. [PubMed] [Google Scholar]
- 2.Schiller WR. The relationship between oxygen delivery and oxygen consumption during fluid resuscitation of burn related shock. J Burn Care Rehab. 2000;21:391–393. [PubMed] [Google Scholar]
- 3.Holm C. Resuscitation in shock associated with burns. Tradition or evidence based medicine? Resuscitation. 2000;44:157–164. doi: 10.1016/s0300-9572(00)00159-3. [DOI] [PubMed] [Google Scholar]
- 4.Klein D, Einspanier R, Bolder U, Jeschke MG. Differences in the hepatic signal transcription pathway and cytokine expression between thermal injury and sepsis. Shock. 2003;20:536–543. doi: 10.1097/01.shk.0000093345.68755.98. [DOI] [PubMed] [Google Scholar]
- 5.Bedi MK, Sarabahi S, Agrawal K. New fluid therapy protocol in acute burn from a tertiary burn care centre. Burns. 2019;45:335–340. doi: 10.1016/j.burns.2018.03.011. [DOI] [PubMed] [Google Scholar]
- 6.Balk RA. Severe sepsis and septic shock. Definitions, epidemiology, and clinical manifestations. Crit Care Clin. 2000;16:179–192. doi: 10.1016/s0749-0704(05)70106-8. [DOI] [PubMed] [Google Scholar]
- 7.Kamolz LP, Andel H, Schramm W, Meissl G. Lactate: early predictor of morbidity and mortality in patients with severe burns. Burns. 2005;31:986–990. doi: 10.1016/j.burns.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 8.Dries DJ, Waxman K. Adequate resuscitation of burn patients may not be measured by urine output and vital signs. Crit Care Med. 1991;19:327–329. doi: 10.1097/00003246-199103000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Wo CC, Shoemaker WC, Appel PL, Bishop MH. Unreliability of blood pressure and heart rate to evaluate cardiac output in emergency resuscitation and critical illness. Crit Care Med. 1993;21:218–223. doi: 10.1097/00003246-199302000-00012. [DOI] [PubMed] [Google Scholar]
- 10.Holm C, Mayr M, Tegeler J, Horbrand F. A clinical randomized study on the effects of invasive monitoring on burn shock resuscitation. Burns. 2004;30:798–807. doi: 10.1016/j.burns.2004.06.016. [DOI] [PubMed] [Google Scholar]
- 11.Kraut JA, Madias NE. Lactic acidosis. N Engl J Med. 2014;371:2309–2319. doi: 10.1056/NEJMra1309483. [DOI] [PubMed] [Google Scholar]
- 12.McNelis J, Marini CP, Jurkiewicz A, Szomstein S. Prolonged lactate clearance is associated with increased mortality in the surgical intensive care unit. Am J Surg. 2001;182:481–485. doi: 10.1016/s0002-9610(01)00755-3. [DOI] [PubMed] [Google Scholar]
- 13.Lee SM, An WS. New clinical criteria for septic shock: serum lactate level as new emerging vital sign. J Thorac Dis. 2016;8:1388–1390. doi: 10.21037/jtd.2016.05.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kimmoun A, Novy E, Auchet T, Ducrocq N. Hemodynamic consequences of severe lactic acidosis in shock states: from bench to bedside. Crit Care. 2015;19:175. doi: 10.1186/s13054-015-0896-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cochran A, Edelman LS, Saffle JR, Morris SE. The relationship of serum lactate and base deficit in burn patients to mortality. J Burn Care Res. 2007;28:231–240. doi: 10.1097/BCR.0B013E318031A1D1. [DOI] [PubMed] [Google Scholar]
- 16.Jeng JC, Jablonski K, Bridgeman A, Jordan MH. Serum lactate, not base deficit, rapidly predicts survival after major burns. Burns. 2002;28:161–166. doi: 10.1016/s0305-4179(01)00098-5. [DOI] [PubMed] [Google Scholar]
- 17.Mokline A, Abdenneji A, Rahmani I, Gharsallah L. Lactate: prognostic biomarker in severely burned patients. Ann Burns Fire Disasters. 2017;30:35–38. [PMC free article] [PubMed] [Google Scholar]
- 18.Herrero, EH, Sánchez M, Cachafeiro L, Agrifoglio A. Lactate in the burn patient. Critical Care. 2015;19(1):145. https://doi.org/10.1186/cc14225 . [Google Scholar]
- 19.Nguyen HB, Rivers EP, Knoblich BP, Jacobsen G. Early lactate clearance is associated with improved outcome in severe sepsis and septic shock. Crit Care Med. 2004;32:1637–1642. doi: 10.1097/01.ccm.0000132904.35713.a7. [DOI] [PubMed] [Google Scholar]