Abstract
Background
Maternal health services are affected by complex factors from one setting to another. Consequently, health planners should prioritize different interventions and design appropriate programs to enhance maternal health services utilization. Results of prior studies are conflicting. Furthermore, only few studies were done from antenatal to postnatal continuum of care in Ethiopia.
Objectives
This study aimed to assess prevalence and predictors of skilled maternal health services utilization at Dale-Wonsho health and demographic surveillance site of the Hawassa University, South Ethiopia, in 2019.
Methods
A community based cross sectional study was conducted from January 1–30; 2019. A total of 682 women who gave birth in the last twelve months were selected by using a two stage sampling technique. Data were collected through face to face interview. Data were entered into Epidata version 3.1. Then, they were exported and analyzed by SPSS version 22. Bi-variable logistic regression analysis was done and variables with p-value less than 0.05 were considered as candidate for multivariable logistic regression analysis. Adjusted Odds Ratios (AOR) with 95% CI were computed, and p-value less than 0.01 was computed to determine the level of significance.
Result
Prevalence of antenatal care, institutional delivery and postnatal care utilizations were 69.1%, 52.1% and 32.7% respectively. Educated women (AOR = 4.72, 95%CI,2.82,7.9), household training (AOR = 8.52,95%CI = 5.5,13.1), middle wealth quantile(AOR = 0.8,95%CI,0.4–0.7), being richest wealth quantile (AOR = 0.16;95%CI = 0.06,0.41) and pregnancy plan (AOR = 3.65,95%CI,1.67–8.0) were factors positively associated with antenatal care utilization. Husband education (AOR = 4.96,95CI,3.08–8.0), and antenatal care (AOR = 5.9; 95%CI,3.87,9.1) were factors associated with institutional delivery. Maternal education (AOR = 2.5,95CI,1.4–4.4), information about postnatal care service utilization (AOR = 3.6,95CI,2.1,6.2) and women autonomy(AOR = 6.1,95CI,3.8,9.7) were positively associated with postnatal care service.
Conclusion
Prevalence of antenatal care, institutional delivery and postnatal care services were lower than the targeted plan. Policy makers should focus on capacity building of women both economically and academically. So, women should be more autonomous to utilize health services effectively. Moreover, awareness creation among women should be enhanced about maternal health service.
Introduction
Globally, an estimated 303 million women died from complications related to pregnancy, childbirth and postpartum period in 2016 [1]. Nearly all of them were occurred in developing countries. From total maternal deaths in developing countries, more than half were happened in Sub-Saharan African countries [2]. Ethiopia is one of the top six Sub-Saharan countries with high maternal deaths. According to Ethiopian Demographic and Health Survey (EDHS) report, Maternal Mortality Ratio (MMR) was estimated as 420 per 100,000 live births in 2016 [3, 4]. In Ethiopia, more than 4 women from 5 of maternal died from complications amenable by lifesaving health interventions in health institutions [5]. Maternal deaths are occurred from pregnancy to postpartum continuum in different proportion: Pregnancy (25%), delivery (16%) and postpartum (61%) [3, 6].
Poor maternal health outcomes have been associated with underutilization of maternal health care services in most developing nations [4]. Hence, the world community focuses on maternal health nowadays [7]. Maternal health refers health of women during pregnancy, childbirth and postpartum period [8]. In Ethiopia, maternal health service utilization has been endorsed as the cost effective health approach to alleviate the burden of maternal deaths. It is one of the top priority agenda in reproductive health [9]. However, significant proportion of women were not still engaged fully in the continuum of maternal care with significant dropouts. For example, only 62% of pregnant women undergo at least one antenatal care visit, 26% of women gave birth in the health institution, and 16.5% of women received postnatal care in Ethiopia in 2016 [4]. Women with the same need should obtain the same health service. Consequently, the main concern of policies makers and health program planners is making maternal health service equally accessible everywhere [10]. Fail to access maternal health services is the predominant cause of high maternal morbidities and mortalities [11]. As a result, integrated community based maternal health services from pregnancy to postpartum period can improve maternal health outcomes [12, 13].
On the contrary, maternal health care service is affected with complex factors. For example, socio-demographic and reproductive factors are the frontline barriers for this problem [14–17]. According to behavioral model of heath service, the main influential factors were grouped under three main categories: predisposing, enabling and need related factors. These encompasses the individual and contextual dimensions [18, 19]. The context of underutilization of maternal health service varies from place to place. Hence, Compressive information on maternal health care utilization is a prerequisite to develop appropriate strategy to maximize its maternal health utilization at local national and international levels. Although many previous studies have been conducted in Ethiopia, results are still conflicting. For example, a study conducted in Enderta (Northern Ethiopia) indicates that more educated women delivered in health institution than less educated one [20]. However, another study in Holeta (Central Ethiopia) showed that more educated women were less likely to give birth in health institution [11]. Furthermore, according to a study married women utilize postnatal care less than unmarried women [21]. On the other hand, a study conducted in Jabitena Northwest Ethiopia indicated that married women are more likely to utilize postnatal care than their counterparts [22]. Besides, women of low parity utilized institutional delivery service more than their counterparts [11]. On the opposite side, women of low parity used institutional delivery service more than women of high parity [22]. Women of low monthly income utilize institutional delivery service less than women of high monthly income in Holeta, central Ethiopia [11]. On the contrary, a study conducted in South and North Ethiopia low income women utilize institutional delivery more than their counterparts [23]. But, results of studies were conflicting worldwide. For example, a study in Southern India indicated that religion has also shown association with maternal health service utilization significantly but not in some others [24]. In contrast, parity has been consistently shown to be negatively correlated with the use of skilled attendants from a study conducted in Thailand, Morocco, Kenya and Namibia [25–28]. Additionally, the above studies have reported positive association between economic status and use of institutional delivery service [24, 25]. Whereas, studies conducted in rural Guatemala and Tajistan have not found such an association between economic status and institutional delivery service [29, 30]. Furthermore, there are limited studies which assess the full skilled maternal health package. Skilled maternal health service utilizations are low coupled with inconsistent use of service from pregnancy to post-partum continuum. With this context, the country has less chance to achieve the 2030 national MMR reduction target of 70/100,000 live births. Therefore, this study aimed to assess prevalence and factors associated with maternal health care utilizations among women of reproductive age group who gave birth in the last 12 months at Hawassa University health and demographic surveillance system site, Dale and Wonsho district Health Demographic Surveillance Site (HDSS) of Hawassa university, South Ethiopia, in 2019.
Methods and materials
Study setting
This study was conducted at Dale-Wonsho HDSS (Health and Demographic Surveillance Site) of Ethiopia which is found in South region. It is controlled by Hawassa university. It was conducted from January 1–30; 2019. The study area is 330 km away from, Addis Ababa, capital city of Ethiopia. It is bordered in the North by Shabadino, in the south by Aleta-Wondo and Aleta chuko, in the east by Gorcha and in the west by Loka Abaya districts. There are a total of 43 Kebeles (the smallest administrative units in Ethiopia) in the district. Among these, 39 Kebeles are rural and 4 were urban Kebeles. According to 2015 population projection estimation, there were a total of 365,652 residents in the study area. From these, only 61,430 were women of reproductive age group (15–49 years) [31]. Maternal health services are provided by a total of 68 public health institutions in the study area. These include the following:1 general hospital and 15 health centres. Furthermore, there were about a total of 1259 health providers.
Study design and population
A community based analytical cross-sectional study was conducted from January 1–30;2019. The source population were women of the reproductive age group who gave at least one live birth in the last twelve months preceding survey. Furthermore, the study population were women of reproductive age group who gave at least one live birth in the last twelve months preceding survey, selected for this study and presented during data collection period. Women who lived less than six months in the study area, and women who were unable to communicate were excluded from this study.
Sample size calculation and sampling procedure
Sample size was calculated by using single population proportion formula in consideration of the following assumptions: Prevalence of antenatal (74.3%), skilled delivery service (28.7%) and postnatal (22.6%) [32], 95% confidence interval, Z score (1.96), and margin of error (d) 5%. Thus, sample sizes for the first objective were computed using the following formula: n = Z2(1-α/2) P(1-P)/D2. Sample sizes were computed for antenatal, skilled delivery service and postnatal care utilization as 294, 314 and 269 respectively.
We considered the design effect of 2 to minimize bias arising from not using simple random sampling technique. Furthermore, we tried to minimize errors arising from chance of noncompliance by adding 10% of the total sample sizes. In general, the total sample sizes for prevalence were calculated as: 647, 692 and 591 for antenatal care, skilled delivery care and postnatal care service uptake respectively. The sample sizes for associated factors (second objective) were calculated using Stat Cal command of epi-info software package from the same study in which sample size for prevalence was calculated. Finally, the final sample size was taken as 692 which is calculate sample size to achieve the objectives of the current study. A two stage sampling procedure was used to select the study participants. Firstly, 12 Kebeles were selected using simple random sampling which account for 20–30% of the total Kebeles in the district. There are a total of 16,800 households Kebeles in the study area.
By using HDSS data base as a sampling frame, we have identified households which contains women of the reproductive age group who gave live birth in last twelve months. Then, we applied proportional allocation to draw the study participants from each selected Kebele. Secondly, we select the study participants from each Kebele using simple random sampling. If woman was absent from the household during consecutive visits, she was regarded as non-response. For households with more than one eligible women, the index woman was selected by simple random sampling using lottery method. Neighbors were asked whether an eligible woman was present or not in the house. Revisits of two to three times were made in case where eligible respondents were not available at the time of the survey. Finally, they were considered as non-respondents.
Measurement
The dependent variables were skilled maternal health services utilization. These include the following three consecutive cares: Antenatal care service, skilled delivery care service and postnatal care service utilization. Each variable is binary outcome. Each variable was labeled as ‘0’ for non-utilization and ‘1’ for utilization of the respective service.
Independent variables were socio-demographic and reproductive health variables in this study. These explanatory variables were selected from various literatures [33–36]. The socio-demographic variables included the following charactestics: Age, educational status, occupational status, wealth index, family size, marital status and religion. Principal component analysis was done to determine wealth index. Wealth index was constructed using principal components analysis on household asset data. Individuals were classified into five wealth quintiles (poorest, poorer, medium, richer and richest). Variables included in the wealth index were ownership of selected household assets, size of agricultural land, quantity of livestock and house construction materials [37]. It was built in three consecutive steps for maximum adaptability of urban and rural areas. a subset of indicators was used to create wealth score of households in both areas in the first step. Separate factor scores were constructed for each household in both areas using specific indicators. In the third step, a nationally combined wealth index was created by combined specific scores for separate area through adjusting of area specific score with regression on a common factors score [38].
Furthermore, reproductive variables included: Antenatal care visits, time of initiating antenatal care visit, tetanus toxoid vaccine utilization, problem faced during pregnancy, reasons for antenatal care visit, place of delivery, type of health institutions visited, place of delivery, type of health providers attend, post-natal checkup, frequency of postnatal checkup and time to start postnatal checkup.
Operational definitions
Skilled attendants
Health professionals who can identify, treat and refer women with many obstetrics complications at pregnancy, delivery and postnatal period timely. These include: Doctors, midwives, nurses, health officers and emergency obstetrics and surgeons.
Proportion of antenatal care
Is defined as the proportion of complex of interventions that a pregnant woman receives from organized health care services by skilled delivery attendant at least one visit in the recent pregnancy.
Women’s autonomy
A more autonomous woman is a woman who can decide on health care spending alone with her husband. If the decision of health care spending is controlled by other than the women herself, it is considered as non-autonomous.
Proportion of safe delivery service utilization
Is the proportion of women who receive delivery care provided in the health institution by skilled health providers during a study participant’s recent birth.
Proportion of postnatal care
Is defined as the proportion of women who receive care for them and their newborn given to immediately after the birth of the placenta and for the first 42 days of life [39].
Data collection
Data were collected using the structured and pretested questionnaire via face to face interview at the participant’s home. The questionnaire was adapted from Ethiopian demographic health survey tool. It was constructed in English and then translated into local language (Sidama-afoo) and back to English to keep consistency. Inconsistent and inaccurate data were readjusted accordingly. Data were collected 8 HDSS data collectors. Furthermore, two public health experts supervised the data collection process. Training was given for data collectors and supervisors for two consecutive days. They were trained about aim of study, procedures, collection techniques, art of interviewing and ways of collecting the data. Pre-testing was done on 5% of samples on Kebeles out of the study area. Each questionnaire was checked for completeness each day after data collection by the supervisors. Finally, feedback was given for data collectors.
Data analysis
Data were entered, cleaned, coded into Epidata software version 4.2. Then, data were exported and analyzed using SPSS 22. We utilized frequencies, means and percentages to summarize the descriptive statistics. Tables and graphs were used for the data presentation. Bi-variable logistic regression analysis was done to identify variables associated with skilled maternal health service utilizations. Consequently, variables whose p-value less than 0.05 were considered as candidate variables for multivariable logistic regression analysis. In multivariable logistic regression analysis, variables with p-value less than 0.01 and adjusted odd ratios with 95% confidence interval were reported as statistically significant variables. Model fitness was checked by using Hosmer-Lemeshow test.
Ethical considerations
First, ethical clearance was obtained from institutional review board of Hawassa university college of medicine and health science. Second, a letter of support was obtained from Sidama zone health department. Third, we obtained administrative permissions from every kebele. Privacy and confidentiality of study participants was assured with a maximum effort. Then, each participant signed informed written consent. Finally, parents or guardians who live together provided written consent on behalf of study participants below 18 years old.
Result
Socio-demographic characteristics of the study participants
Table 1 of this study indicated the socio-demographic characteristics of the study participants. From a total of 692 study participants recruited for this study, only 682 study participants gave full response making response rate of 98.67%.
Table 1. Socio-demographic characteristics of study participants(n = 682) at Hawassa HDSS, South Ethiopia, in 2019.
| Variables | Categories | Frequency (%) |
|---|---|---|
| Age | 15–24 | 213 (31.2%) |
| 25–34 | 329 (48.2%) | |
| 35–49 | 140 (20.5%) | |
| Ethnicity | Sidama | 661 (96.9%) |
| Amhara | 19 (2.8%) | |
| Guarage | 2 (0.3%) | |
| Religions | Protestant | 632 (92.7%) |
| Orthodox | 17 (2.5%) | |
| Muslim | 18 (2.6%) | |
| Catholic | 15 (2.2%) | |
| Marital status | Married | 634 (93%) |
| Cohabiting | 4 (0.6%) | |
| Divorced | 38 (5.5%) | |
| Widowed | 6 (0.9%) | |
| Maternal educational status | No formal education | 132 (19.4%) |
| Educated | 550 (80.6%) | |
| Husband educational status | No formal education | 141 (20.7%) |
| Educated | 541 (79.3%) | |
| Occupation of the mother | Housewife | 631 (92.5%) |
| Government employer | 6 (0.9%) | |
| Merchant | 39 (5.7%) | |
| Occupation of the husband | Farmer | 497 (72.9%) |
| Government employer | 45 (6.6%) | |
| Merchant | 112 (16.4%) | |
| Others | 28 (4.1%) | |
| Wealth Index | Poorest | 143 (21%) |
| Poor | 125 (18.3%) | |
| Middle | 156 (22.9%) | |
| Rich | 75 (11%) | |
| Richest | 183 (26.8%) | |
| Social media access | Yes | 400 (58.7%) |
| No | 282 (41.3%) |
According to the report of this study, nearly half (48.2%) of the study participants were in the age range of 25–34 years. Most 632(93%) of the study participants were follower of protestant religion. Furthermore, majorities 634(93%) of the study participants were married. Majorities, 214(60.1%) of study participants were merchants. Furthermore, one-hundred- thirty-two (19.4%) of women and one-hundred-forty-one (20.7%) of their partners never attended formal education. Approximately one in four women was in richest wealth index. From the total of study participants, 400 (58.7%) of the study participants had access to mass media.
Reproductive health characteristics of the study participants
Table 2 indicated the reproductive health charactestics of the study participants. According to this study report, majorities 471(69.1%) of the study participants had antenatal care visits for their most recent birth. Most (79.6%) of the study participants were in the age range of 20–34 years. More than half 459 (67.3%) of the study participants planned their pregnancy. Approximately 1 from 2 women got pregnancy of more than five times. Moreover, two-third of the study participants delivered five and above times. More than half 404 (59.3%) of the study participants gave birth 1–4 times. Half 236 (50.1%) of the study participants started antenatal care in the last three months. Nearly half (47.9%) participants delivered in their home. Majorities (67.3%) of the study participants did not attend postnatal care service.
Table 2. Reproductive health characteristics of women of reproductive age group (n = 682) in Hawassa HDSS, South Ethiopia, in 2019.
| Variable | Categories | Frequency (%) |
|---|---|---|
| Antenatal care visit | Yes | 471 (69.1%) |
| No | 211 (30.9%) | |
| Age at last pregnancy | 15–19 years | 38 (5.6%) |
| 20–34 years | 543 (79.6%) | |
| 35–49 years | 101 (14.8%) | |
| pregnancy status | Planned | 459 (67.3%) |
| Unplanned | 223 (32.7%) | |
| Gravidity | 1–4 | 446 (65.4%) |
| 5 and above | 236 (34.6%) | |
| Parity | 1–4 | 404 (59.3%) |
| 5 and above | 278 (40.7%) | |
| Reason for not using antenatal care (n = 211) | No knowledge | 36 (17.1%) |
| Being in a good state | 83 (39.3%) | |
| Far from my house | 48 (22.7%) | |
| Too busy | 44 (20.9%) | |
| Time started antenatal care use | Less than 3months | 78 (16.6%) |
| 3–6 months | 157 (33.3%) | |
| More than 6 months | 236 (50.1%) | |
| Place of delivery | Health facility | 355 (52.1%) |
| Home | 327 (47.9%) | |
| Types of health facilities visited (n = 355) | Hospital | 132 (37.2%) |
| Health center | 207 (58.3%) | |
| Health post | 16 (4.5%) | |
| Reason for non-utilization of institutional delivery (n = 327) | Dislike health facility | 86 (26.3%) |
| Delay of ambulance | 119 (36.4%) | |
| No road access | 122 (37.3%) | |
| Health provider attended delivery (n = 355) | Doctors | 80 (16.5%) |
| Midwifes | 71 (15.3%) | |
| Nurse | 340 (68.3%) | |
| Others* | 7 (1%) | |
| Postnatal check up | Yes | 223 (32.7%) |
| No | 459 (67.3%) | |
| Main reason initiated postnatal care use (n = 223) | Health problem | 48 (20.9%) |
| For regular checkup | 124 (55.6%) | |
| Immunization service | 51 (22.9%) | |
| Time of PNC checkup (n = 223) | Immediately after delivery | 97 (43.5%) |
| Within 24 hours | 73 (32.7%) | |
| More than 2 days | 53 (23.8%) |
Key: Others* = health officers, emergency obstetrics and surgeon.
Prevalence of skilled maternal health services utilization
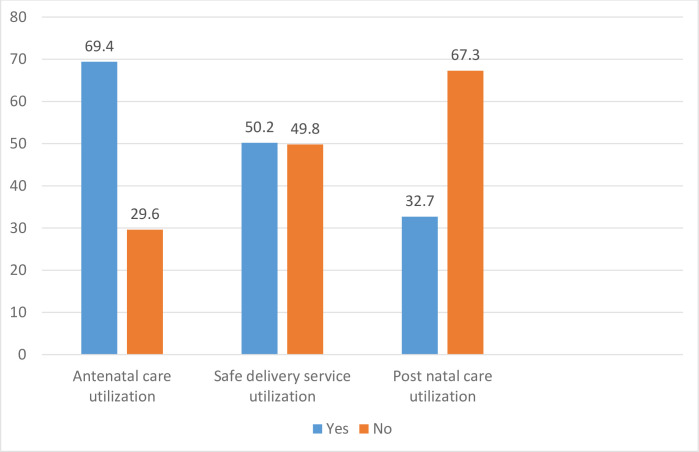
Fig 1 showed the prevalence of skilled maternal health services utilization. The prevalence of antenatal care, skilled delivery care service and postnatal care utilization among women of reproductive age group were 69.1%, 52.1% and 32.7% respectively.
Fig 1. Proportion of skilled maternal health services among women of reproductive age group (n = 682) in South Ethiopia, in 2019.
Among the total study participants, eighty-three (39.3%) of the study participants did not utilize antenatal care service as they perceived no need of care due to their well health condition. The main reasons for non-utilization of institutional delivery were lack of road access 122 (37.3%), and ambulance delay 119 (36.4%) in the current study. Half (50.1%) of the study participants started antenatal care more than six months. Among births attended in the health facilities, most 207 (58.3%) of deliveries were attended in health center. From these, majorities 340 (68.3%) of deliveries were attended by nurses. Among study participants, more than half (55%) of them came for regular checkup. Most 97 (43.5%) of women started postnatal care immediately after birth.
Factors associated with skilled maternal health service utilization
Table 3 showed that the result of bi-variable and multi-variable logistic regression analysis of antenatal care utilization. Hence, eight variables were associated with antenatal care utilization statistically. These variables were: Wealth index, maternal education, model household training, road access, plan of pregnancy, access to information on Antenatal care and counseling about pregnancy danger sign. Among these factors: wealth index, maternal education, model household training and having pregnancy plan were factors associated with antenatal care utilization in the multi-variable logistic regression. Accordingly, the odd of antenatal care utilization among women who planed current pregnancy was higher odds than their counterparts (AOR = 3.65; 95% CI = 1.6,8.0). The chance of antenatal care utilization was higher among women who had a formal education than their counterparts (AOR = 4.72, 95% CI = 2.82,7.9). In addition, compared to women who did not receive model household training, women were received model household training were more likely to use antenatal care service (AOR = 8.52; 95% CI = 5.5,13.1). The odds of women in richest wealth quantile was lower than women in poorest quantile by antenatal care utilization (AOR = 0.16; 95%CI = 0.06,0.41). However, the odds of utilization of antenatal care was increased by 4.9 times for women who had educated husbands (AOR = 4.96, 95% CI = 3.08,8.0) than their counterparts.
Table 3. Predictors of antenatal care utilization among women of reproductive age group (n = 682) in Hawassa HDSS, South Ethiopia, in 2019.
| Variables | Category | Antenatal utilization | COR | AOR | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Wealth index | Poorest | 84 | 59 | Ref. | Ref. |
| Poor | 67 | 58 | 1.23 (0.75, 2.0) | 0.94 (0.53, 1.64) | |
| Middle | 136 | 20 | 0.2 (0.12, 0.37)* | 0.09 (0.04, 0.19)** | |
| Richer | 48 | 27 | 0.8 (0.45, 1.42) | 0.47 (0.20, 1.08) | |
| Richest | 136 | 47 | 0.5(0.30, 0.78)* | 0.17 (0.07, 0.42)** | |
| Formal maternal education | Yes | 413 | 137 | 3.85 (2.59, 5.7)* | 4.72 (2.82, 7.90)** |
| No | 58 | 74 | Ref. | Ref. | |
| Model household Training | Yes | 333 | 55 | 6.84(4.75, 9.86)* | 8.52(5.52,13.15)** |
| No | 138 | 156 | Ref. | Ref. | |
| Road accessibility | Yes | 406 | 196 | 0.48(0.27, 0.86)* | 0.57 (0.27, 1.22) |
| No | 65 | 15 | Ref. | Ref. | |
| Media access | Yes | 259 | 141 | 0.61(0.43, 0.85)* | 0.69 (0.36, 1.34) |
| No | 212 | 70 | Ref. | Ref. | |
| Current pregnancy planned | Yes | 448 | 180 | 3.36 (1.90,5.91)* | 3.65 (1.67, 8.01)** |
| No | 23 | 31 | Ref. | Ref. | |
| Information about antenatal care | Yes | 427 | 170 | 2.34(1.47, 3.71)* | 1.43 (0.67, 3.05) |
| No | 44 | 41 | Ref. | Ref. | |
| Counseled about danger sign | Yes | 361 | 145 | 1.49(1.04, 2.14)* | 1.56 (0.86, 2.85) |
| No | 110 | 66 | Ref. | Ref. | |
Key: Ref: Reference categories
*: P-value < 0.05 in binary logistic regression analysis
**: P-value < 0.01 in multivariable logistic regression analysis.
According to Table 4 report, independent variables associated with institutional delivery service utilization in bi-variable logistic regression were: Age of women, the presence of maternal formal education, husband education, model household training and antenatal care utilization. However, only husband education and ANC utilization showed significant association. Based on the result, the odds of safe delivery among women who had antenatal care visit was 5.9 times higher than their counterparts (AOR = 5.9; 95% CI = 3.8,9.2) and the odds of women with uneducated husband were 80% less likely to conduct safe for delivery (AOR = 0.20; 95%CI,0.13, 0.32).
Table 4. Predictors of skilled delivery care utilization among women of reproductive age group (n = 682) in Hawassa HDSS, South Ethiopia, in 2019.
| Variables | Category | Skilled delivery service utilization | COR | AOR | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Age of women | 15–24 years | 119 | 94 | Ref. | Ref. |
| 25–34 years | 175 | 154 | 1.11 (0.71, 1.36) | 0.84 (0.55, 1.28) | |
| 35–49 years | 61 | 79 | 1.64 (1.01, 2.98)* | 0.77 (0.44, 1.38) | |
| Formal maternal education | Yes | 48 | 84 | Ref. | Ref. |
| No | 307 | 243 | 0.45 (0.31, 0.67)* | 0.87 (0.53, 1.42) | |
| Model household Training | Yes | 244 | 144 | 2.79 (2.04, 3.82)* | 1.43 (0.98, 2.08) |
| No | 111 | 183 | Ref. | Ref. | |
| Husband education | Yes | 31 | 110 | Ref. | Ref. |
| No | 324 | 217 | 0.19 (0.12, 0.29)* | 0.20 (0.13, 0.32)** | |
| Antenatal care utilization | Yes | 309 | 162 | 6.84(4.68, 9.98)* | 5.96 (3.88, 9.18)** |
| No | 46 | 165 | Ref. | Ref. | |
KEY: Ref: Indicates the reference categories
*: P-value < 0.05 in binary logistic regression
**, P-value <0.01, multiple logistic regression.
Based on Table 5 result, crude odds ratios showed that five variables were associated with postnatal care utilization significantly. Among these, only three variables were associated significantly with postnatal care utilization. These were maternal formal education, information about postnatal care and women autonomy in decision making were statistically associated with postnatal care in the final model. These association is illustrated as follows: The likelihood of postnatal care utilization was higher among educated women than their counterparts (AOR = 2.6; 95% CI = 1.4,4.4). The odd of postnatal care utilization was 3.6 times higher among women who had information about postnatal care utilization than their counterparts (AOR = 3.6; 95% CI = 2.1,6.2). Women were autonomous in decision making process on health related matters had more chance of utilizing postnatal care service than their counterparts (AOR = 6.1, 95% CI = 3.8,9.7).
Table 5. Predictors of postnatal care utilization among women of reproductive age group (n = 682) in Hawassa University Health and Demographic Surveillance Site, South Ethiopia, in 2019.
| Variables | Category | Postnatal care use | COR | AOR | |
|---|---|---|---|---|---|
| Yes | No | ||||
| Formal maternal education | Yes | 20 | 112 | Ref. | Ref. |
| No | 203 | 347 | 3.28 (1.98, 5.46)* | 2.57 (1.48, 4.44)** | |
| Current pregnancy planned | Yes | 214 | 414 | 2.58 (1.24, 5.39)* | 1.69 (0.74, 3.84) |
| No | 9 | 45 | Ref. | Ref. | |
| Information about post-natal care | Yes | 201 | 297 | 5.22 (3.20, 8.51)* | 3.66 (2.18, 6.14)** |
| No | 21 | 162 | Ref. | Ref. | |
| Place of delivery | Yes | 131 | 224 | 1.49 (1.08, 2.06)* | 1.23 (0.85, 1.76) |
| No | 92 | 235 | Ref. | Ref. | |
| Autonomy of women | Myself | 197 | 236 | 7.16(4.57, 11.2)* | 6.13 (3.86, 9.73)** |
| Others | 26 | 223 | Ref. | Ref. | |
KEY: Ref.: Indicates the reference categories
*: Indicates significant association (P-value < 0.05)
**, indicate the highly significant association (P-value <0.01).
Discussion
Poor uptake of maternal health service is one of the leading cause of maternal morbidity and mortality in the world [40]. This study is the one of the first predominant study which can resolve the preexisting conflict among findings of different studies about skilled maternal care service utilization. Leaving these conflicts unsolved at individual level can lead to miss the target point of intervention during policy making and program design. Moreover, this study provides adequate picture of the problem of poor uptake of skilled maternal care service as continuum of care from pregnancy to postpartum period. Hence, this study explored determinants of skilled maternal care mainly at a rural community. Primary health services (skilled maternal care services) inequality predominantly existed in the rural population for many years in Ethiopia.
Prevalence of antenatal care follow-up, skilled delivery care and postnatal care service utilization were estimated as 69.1%, 52.1% and 32.7% respectively. According to Mini-EDHS 2019 report, antenatal care service utilization was estimated as 69.4%(95%CI,67.6%,71.0%) during pregnancy, skilled delivery care was reported as 50.2%(95%CI,48.7%,51.7%), and post-natal care service was measured as 32% (95%CI,29.7%,34.3%) in South Nation Nationalities and Peoples Regional states of Ethiopia [41]. Based on these finding, compared with the regional proportion of skilled maternal health service, antenatal care and postnatal care utilization in this study are in line with regional proportions. However, skilled delivery service utilization was slightly higher than the regional proportion. These findings clearly indicate that maternal health service utilizations are improve active involvement of health extension workers and their community mobilization of the health development army in the rural areas. Previous evidence proved this argument that health extension workers did not achieve significant change in antenatal and postnatal care service as safe delivery service in Ethiopia [23]. On the contrary, the probable justification of increased proportion of skilled delivery care service in this study might be due to better quality antenatal care service at pregnancy by health extension workers than other parts of regions. A previous study consolidated this justification than women who had frequent visits by health extension workers were more likely to visits health institutions in Ethiopia [42]. Moreover, antenatal care service utilization was higher in this study as compared with findings of studies in other parts of Ethiopia: Debretabor, South Gondar (35.5%), East Wollega (14.4%), Dejen, East Gojjam(12%) and East Hararge (38.3%) [43–46]. This could be due to variation in study population groups, study setting and health service infrastructure. This argument was supported with an evidence proved that expansion of primary health facilities increased maternal and child health program interventions [47]. Furthermore, some cultural practices might encourage home treatment for complications during pregnancy in the study area than above study areas. prevalence of skilled delivery service uptake is consistent with finding of study done in Woldia, Northwest Ethiopia (48.3%) [48]. The possible explanation might be due to similar study population, study setting and socio-economic status of study participants. On the contrary, the this finding is more than finding of studies done in Butajera, South Ethiopia (15.7%), Banja, North West Ethiopia (37.9%) and Enderta, North Ethiopia (25%) [49–51]. The possible explanation for this discrepancy could be due to better awareness of women and strong health provider’s commitment towards birth preparedness and complication readiness plan during pregnancy in this study. Furthermore, home delivery is more cultural and religious practice in the North Ethiopia than South Ethiopia. To the opposite side, this finding is lower than findings of studies carried out in Holeta, Central Ethiopia (61.6%) and Sodo, South Ethiopia (62.2%) [52, 53]. This might be due to fact that the study participants in current study were rural dwellers than others. Consequently, rural women could not be autonomous in decision making power about their health, there might be lack of access to information and inadequate infrastructure construction in the study area. Prevalence of postnatal care utilization is higher than findings of other studies in Ethiopia: Jabitena, North West Ethiopia (20.2%), Haromaya, Eastern Ethiopia (22.6%) and North Shoa, Central Ethiopia (28.4%) [4, 16, 54, 55]. This might be due to the efforts exerted by community health workers to increase women’s awareness on the benefit of postnatal care utilization in the current study setting than others. Previous study proved that women who had better knowledge about danger sign during postpartum period were better utilized postnatal care service than their counter parts [56]. The absence of cultural belief by community members who perceives movement outside of home could exposed women for evil spirit might increase postnatal care use by restricting movement of women after delivery in the current study area than others. On the contrary, the this finding is lower than other similar studies in the Enderta, North Ethiopia (49.7%), South Ethiopia (37.2%) and Assella (72.7%) [57–59]. These discrepancies might be due to difference in socio-demographic characteristics and health seeking behaviors of women. Moreover, cultural practice and extent of urbanization among study settings might influence postnatal care service utilization.
Educational status, model household training, wealth quintile and pregnancy plan were important factors associated with antenatal care utilization in this study. Specifically, women who planned their pregnancy plan were utilized antenatal care service more than their counterparts. This finding was in line with many studies in Ethiopia. For example, a study done in Debretabor town, Wonberma and Yem woreda and South Africa [43, 60–62]. The authors argued that women who plan to have a child have better awareness of their health. As a result, they can make all the necessary arrangement to use antenatal care service effectively. This study proved that wealth index was critical determinant of antenatal care service utilization. As we go down from richest to poorest wealth index category, women had low chance of using antenatal care. Similar findings were also reported from studies conducted in the Nigeria and Ethiopia [4, 63]. The possible rational might be due to direct and indirect costs for service utilization. Even though antenatal care is free of charge currently in Ethiopia, there are indirect costs of transportation, accommodation during staying in towns, food costs and some medicine costs. An evidence has been argued that mother from poor communities or scarce resources may have difficulties to pay for the healthcare costs [64]. In addition, rich women have sufficient purchasing power to healthcare and materials of information. Previous researchers argued that rich women had tend to have personal control over resource, and being autonomous in decision making process than poor women [65]. As do many other studies, this study also indicates that educated women were more likely to utilize antenatal care than their counterparts [43, 44, 64]. The possible rational might be that as the women educated more, they tend to have good health seeking behavior, more autonomous and economically secured to utilize antenatal care service. Furthermore, education make women more positive thinker and confident.
Lack of husband education had influential effect on institutional delivery utilization in the current study. However, other studies which were done in Bangladesh and Benishangul-Gumuz of Ethiopia have disproved this hypothesis [66, 67]. The possible disparities might arise from the fact that husbands are more conservative towards their cultural practice of home delivery and women are not autonomous both in Bangladesh and Benishangul Gumuz of Ethiopia regardless of their educational status. This might indicate that education by itself might not change husbands’ behavior except massive work is done to change on their attitude. Utilization of at least one antenatal care visit increased institutional delivery service utilization in this study. Similar finding have been also reported in Benishangul-Gumuz region, Wukro and Butajera, Sodo South region and Munisa Oromia region in Ethiopia [51, 53, 66, 68]. This finding may suggest that women who have antenatal care visit prepared for birth and complication and anticipate its outcome. Previous studies also documented that birth preparedness and complication readiness plan has associated positively with institutional delivery place [69]. Maternal education was found to improve postnatal care utilization in this study. This finding is in agreement earlier works [55, 70–72]. This can be elaborated by the notion that education is an important factor in empowering women in decision making power towards postnatal care utilization, increasing awareness of fundamental health care services, and increase problem detection power of women and minimize economic dependence through employment. Consequently, women can be directed to positive health seeking behavior. This study also indicates that information access about service influenced post-natal care service positively. This finding was in agreement with findings of Dembecha, Northwest Ethiopia [73], Nigeria and Nepal [71, 72]. The observed similarities might be that informed women have good knowledge and skill of maternal health care service utilization. Finally, autonomous in decision making power was another critical factor associated with uptake of post-natal care service. Women who were more autonomous in decision making power utilized postnatal care more than their counterparts. This finding is consistent with other similar studies [74–76]. The possible reason might be due to the fact that women can increase bargaining power with their husbands on postnatal care service utilization as they become more autonomous.
Limitation
This study has several strengths. First, the rural and community based nature of the study can indicate accurate picture of the problem. Second, using simple random sampling technique, adequate sample size and standard data collection tool could yield reliable estimates. Third, each hypothesis was tested for demand side individual level variables with complete picture of the problem for maternal health care services from pregnancy to postpartum continuum.
On the contrary, the current study had few limitations. For example, recalling bias might be the source of bias. To reduce the recall bias, for instance, only women who gave birth in the last one year were selected. Furthermore, the current study did not include supply side factors of maternal health service utilization. Therefore, further studies should be conducted to assess the health institutional factors of maternal health service.
Conclusion
In general, maternal health care services are still unsatisfactory in this study compared to the target plan of local and national proportions. Maternal education, model household training, higher wealth quantile and having pregnancy plan have increased antenatal care use. Husband education and antenatal care service utilization were positively associated with skilled delivery care. Furthermore, information about postnatal care, maternal education and more autonomous status of women were associated with increased odd of postnatal care utilization. This finding warrants policymakers to formulate strategies to enhance awareness about maternal health services utilization. Ethiopia government should enhance socio-economic status of women. Furthermore, community maternal health services should be improved from pregnancy to postpartum period continuum. Moreover, women should plan their pregnancy; otherwise, use family planning method consistently.
Supporting information
(SAV)
Acknowledgments
First of all, the authors would like to thank officials of Boricha district for their permission to perform this study. Secondly, the authors are also very thankful to data collectors for their fruitful effort. Finally, we would like to thank all study participants.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Kv L.R.M.F., Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet, 2012. 380(9859): p. 2095–2128. 10.1016/S0140-6736(12)61728-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organisation (WHO), Trends in maternal mortality: 1990 to 2010. Geneva: World Health Organization, Geneva, Switzerland: 2010. [Google Scholar]
- 3.Kululanga L, J. S., Malata Aand Chirwa E, Male Involvement in Maternity Health Care in Malawi. African Journal of Reproductive Health March 2012; 16(1): 145 [PubMed] [Google Scholar]
- 4.Central Statistical Agency(CSA) [Ethiopia] and ICF, Ethiopia Demographic and Health Survey 2016: Key Indicators Report. 2016: Addis Ababa, Ethiopia, and Rockville, Maryland, USA. CSA and ICF.
- 5.Ronsmans C., Graham W.J., and L.M.S.S.s. group, Maternal mortality: who, when, where, and why. The lancet, 2006. 368(9542): p. 1189–1200. [DOI] [PubMed] [Google Scholar]
- 6.Say L, C. D., Gemmil A, et al. , Global causes of maternal death: a WHO systematic analysis,. Lancet Glob Health, 2014. 10.1016/S2214-109X(14)70227-X [DOI] [PubMed] [Google Scholar]
- 7.Gyimaha SO, T. B., Addai I, Challenges to the reproductive health needs of African women: On religion and maternal health care utilizatization in Ghana. Soc Scie Med. 62:2930–44, 2016. [DOI] [PubMed] [Google Scholar]
- 8.World Health organization (WHO), Maternal, child and adolescent health care, (WHO), Geneva, Switzerland: 2016. 10.3390/healthcare4040090 [DOI] [Google Scholar]
- 9.FMOH, National reproductive health strategy to improve maternal and child health, Addis Ababa, Ethiopia. 2016–2020.
- 10.Qian Y., et al. , An equity analysis of health examination service utilization by women from underdeveloped areas in western China. PloS one, 2017. 12(10): p. e0186837 10.1371/journal.pone.0186837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Birmeta K., Dibaba Y., and Woldeyohannes D., Determinants of maternal health care utilization in Holeta town, central Ethiopia. BMC health services research, 2013. 13(1): p. 256 10.1186/1472-6963-13-256 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borghi J, T.B., Osrin D, Jan S, Morrison J, Tamang S, Economic assessment of a women’s group intervention to improve birth outcomes in rural Nepal. Lancet. 2005; 366(9500):1882–4., 2005. 10.1016/S0140-6736(05)67758-6 [DOI] [PubMed] [Google Scholar]
- 13.Colbourn T N.B., Bondo A, Makwenda C, Tsetekani E, Makonda-Ridley A, Effects of quality improvement in health facilities and community mobilization through women’s groups on maternal, neonatal and perinatal mortality in three districts of Malawi: MaiKhanda, a cluster randomized controlled effectiveness trial. Int Health. 2013; 5(3):180–95. 10.1093/inthealth/iht011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bahilu T, A. G., Yohannes D, Factors Affecting Antenatal Care Utilization in Yem Special Woreda, Southwestern Ethiopia. Ethiop J Health Sci. 2009, 2010. [Google Scholar]
- 15.Zeine A, M. W., Shimeles O, Factors Influencing Antenatal Care Service Utilization in Hadiya Zone,. Ethiop J Health Sci. 2009, 2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.DerejeKifle T., YalemzewodAssefaGelaw and YayehiradAlemuMelsew, Maternal health care service seeking behaviors and associated factors among women in rural Haramaya District, Eastern Ethiopia,. BMC journal, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Yinager G D.A., Factors affecting utilization of postnatal care service in Jabitena district, Amhara region, Ethiopia,. Sci J Public Health. 2014, 2014,. [Google Scholar]
- 18.Ho S.C., et al. , Impact of caregiving on health and quality of life: a comparative population-based study of caregivers for elderly persons and noncaregivers. Journals of Gerontology Series A: Biomedical Sciences and Medical Sciences, 2009. 64(8): p. 873–879. 10.1093/gerona/glp034 [DOI] [PubMed] [Google Scholar]
- 19.Exavery, A., D. Klipstein-Grobusch, and C. Debpuur. Self-rated health and healthcare utilization among rural elderly Ghanaians in Kassena-Nankana District. 2010. Working paper. Presented in session 59: trends, patterns, and consequences ….
- 20.Aregay A., et al. , Factors associated with maternal health care services in Enderta District, Tigray, Northern Ethiopia: A cross sectional study. American Journal of Nursing Science, 2014. 3(6): p. 117–125. [Google Scholar]
- 21.Mbalinda S.N., et al. , Does knowledge of danger signs of pregnancy predict birth preparedness? A critique of the evidence from women admitted with pregnancy complications. Health research policy and systems, 2014. 12(1): p. 60 10.1186/1478-4505-12-60 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Workineh Y.G. and Hailu D.A., Factors affecting utilization of postnatal care service in Jabitena district, Amhara region, Ethiopia. Sci J Public Health, 2014. 23: p. 169–76. [Google Scholar]
- 23.Afework M.F., et al. , Effect of an innovative community based health program on maternal health service utilization in north and south central Ethiopia: a community based cross sectional study. Reproductive health, 2014. 11(1): p. 28 10.1186/1742-4755-11-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Navaneetham K. and Dharmalingam A., Utilization of maternal health care services in Southern India. Social science & medicine, 2002. 55(10): p. 1849–1869. 10.1016/s0277-9536(01)00313-6 [DOI] [PubMed] [Google Scholar]
- 25.Raghupathy S., Education and the use of maternal health care in Thailand. Social science & medicine, 1996. 43(4): p. 459–471. 10.1016/0277-9536(95)00411-4 [DOI] [PubMed] [Google Scholar]
- 26.Bhutta Z.A., et al. , Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: a review of the evidence. Pediatrics, 2005. 115(Supplement 2): p. 519–617. [DOI] [PubMed] [Google Scholar]
- 27.Obermeyer C.M., Culture, maternal health care, and women’s status: a comparison of Morocco and Tunisia. Studies in family planning, 1993: p. 354–365. [PubMed] [Google Scholar]
- 28.Gage A.J., Premarital childbearing, unwanted fertility and maternity care in Kenya and Namibia. Population studies, 1998. 52(1): p. 21–34. [Google Scholar]
- 29.A Glei D. and Goldman N., Understanding ethnic variation in pregnancy-related care in rural Guatemala. Ethnicity & Health, 2000. 5(1): p. 5–22. 10.1080/13557850050007301 [DOI] [PubMed] [Google Scholar]
- 30.Falkingham J., Inequality and changes in women’s use of maternal Health‐care services in Tajikistan. Studies in family planning, 2003. 34(1): p. 32–43. 10.1111/j.1728-4465.2003.00032.x [DOI] [PubMed] [Google Scholar]
- 31.CSA, Population projection of Ethiopia for all regions at wereda level from 2014–2017. 2013, CSA Addis Ababa.
- 32.Kifle D., et al. , Maternal health care service seeking behaviors and associated factors among women in rural Haramaya District, Eastern Ethiopia: a triangulated community-based cross-sectional study. Reproductive health, 2017. 14(1): p. 6 10.1186/s12978-016-0270-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ali A.A.A., et al. , Use of antenatal care services in Kassala, eastern Sudan. BMC pregnancy and childbirth, 2010. 10(1): p. 67 10.1186/1471-2393-10-67 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Teferra A.S., Alemu F.M., and Woldeyohannes S.M., Institutional delivery service utilization and associated factors among mothers who gave birth in the last 12 months in Sekela District, North West of Ethiopia: A community-based cross sectional study. BMC pregnancy and childbirth, 2012. 12(1): p. 74 10.1186/1471-2393-12-74 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abeje G., Azage M., and Setegn T., Factors associated with Institutional delivery service utilization among mothers in Bahir Dar City administration, Amhara region: a community based cross sectional study. Reproductive Health, 2014. 11(1): p. 22 10.1186/1742-4755-11-22 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Singh P.K., et al. , Determinants of maternity care services utilization among married adolescents in rural India. PloS one, 2012. 7(2): p. e31666 10.1371/journal.pone.0031666 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Rutstein S.O., The DHS Wealth Index: Approaches for rural and urban areas. 2008. [Google Scholar]
- 38.CSA-Ethiopia I., International: Ethiopia Demographic and Health Survey 2011. Central Statistical Agency of Ethiopia and ICF International Addis Ababa, Ethiopia and Calverton, Maryland, USA, 2012. [Google Scholar]
- 39.Organization, W.H., WHO technical consultation on postpartum and postnatal care. 2010, World Health Organization. [PubMed] [Google Scholar]
- 40.Wang W, S.A., Shanxiao W, Alfredo F, Levels and trends in the use of maternal health services in developing countries. DHS comparative reports. No. 26. Calverton, Maryland, USA: ICF Macro, 2016.
- 41.Central Statistical Agency Addis Ababa, E.T.D.P.I., Ethiopia demographic and health survey 2019.
- 42.Ilboudo P.G.C., et al. , Estimating the costs for the treatment of abortion complications in two public referral hospitals: a cross-sectional study in Ouagadougou, Burkina Faso. BMC Health Services Research, 2016. 16: p. 559 10.1186/s12913-016-1822-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Teshager Workneh Ayalew and Araya Mesfin Nigatu, Focused antenatal care utilization and associated factors in Debre Tabor Town, northwest Ethiopia. BMC journal, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Tekelab T, Y. B., Melka AS, Antenatal care and women’s decisionmaking power as determinants of institutional delivery in rural area of Western Ethiopia. BMC Res Notes. 2015;8(1):769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Getachew T, A. A., Aychiluhim M, Antenatal care service utilizationand associated factors in Dejen and Aneded Districts, Northwest Ethiopia. Prim Health Care,. 2014;4:4. [Google Scholar]
- 46.Zelalem Ayele D, B. B., Teji K, Admassu Ayana D, Factors affecting utilization of maternal health Care Services in Kombolcha District, eastern Hararghe zone, Oromia regional state, eastern Ethiopia,. Int Sch Res Notices. 2014;2014:7 10.1155/2014/917058 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Memirie S.T., et al. , Inequalities in utilization of maternal and child health services in Ethiopia: the role of primary health care. BMC health services research, 2016. 16(1): p. 51 10.1186/s12913-016-1296-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Worku A., Jemal M., and Gedefaw A., Institutional delivery service utilization in Woldia, Ethiopia. Science journal of public health, 2013. 1(1): p. 18–23. [Google Scholar]
- 49.AsfawosenAregay M., HuruyAssefa, WondewesonTerefe, Factors associated with maternal health care services inEnderta District, Tigray, Northern Ethiopia: A crosssectional study. 2016. [Google Scholar]
- 50.Worku A, J. M., Gedefaw A, Institutional delivery service utilization in Woldia, Ethiopia,. Sci J Public Health. 2015;1(1):18–23. [Google Scholar]
- 51.Hagos S, S. D., Assegid M, Mekonen A, Fantahun MA, Ahmed S, Utilization of institutional delivery service at Wukro and Butajera districts in the Northern and South Central Ethiopia,. BMC Pregnancy Childbirth. 2016;14:178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Birmeta K, D. Y., Woldeyohannes D, Determinants of maternal health care utilization in Holeta town, central Ethiopia,. BMC Health Serv Res. 2015;13:256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Hailemichael F, W. M., Tafese F, Predictors of institutional delivery in Sodo town, Southern Ethiopia. Afr J Prm Health Care Fam Med. 2013;5(1):9. [Google Scholar]
- 54.Matijasevich A, S. S., Silveira M, Domingues M, Barros A, Inequities in maternal postnatal visits among public and private patients: 2014 Pelotas Cohort study. BMC Public Health 9: 335 10.1186/1471-2458-9-335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Mohammed Akibu, W. T., Tewodros Megersa, and Sodere Nurgi, Prevalence and Determinants of Complete Postnatal Care Service Utilization in Northern Shoa, Ethiopia,. Hindawi Journal of Pregnancy, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Abebo T.A. and Tesfaye D.J., Postnatal care utilization and associated factors among women of reproductive age Group in Halaba Kulito Town, Southern Ethiopia. Archives of Public Health, 2018. 76(1): p. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Amane Tumbure, D. A., Elile Fantahun, Megersa Negusu, Assessment of Postnatal Care Service Utilization and Associated Factors in Asella Town, Arsi Zone, Oromiya Regional State, Ethiopia,. Global journal of reproductive health. [Google Scholar]
- 58.Gebeyehu Y, D. W., Hailu (2014) A, Factors Affecting Utilization of Postnatal Care Service in Jabitena District, Amhara Region, Ethiopia,. Science Journal of Public Health 2(3): 169–176. [Google Scholar]
- 59.Tulandi T. and Al-Fozan H., Spontaneous abortion: Risk factors, etiology, clinical manifestations, and diagnostic evaluation. UpToDate, 2011. [Google Scholar]
- 60.Joy Ebonwu, A. M., Margot Uys, Wainberg Milton L., Determinants of late antenatal care presentation in rural and peri-urban communities in South Africa: A cross-sectional study,. PLOS one, 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mulat G, K. T., Aychiluhim M, Antenatal care service utilization and its associated factors among mothers who gave live birth in the past one year in Womberma Woreda, North West Ethiopia. Epidemiology. 2015. [Google Scholar]
- 62.Tewodros B D.Y., Factors affecting antenatal care utilization in Yem special woreda, southwestern Ethiopia. Ethiop J Health Sci. 2009. 10.4314/ejhs.v19i2.69419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Emmanuel Olorunleke Adewuyi1*, A. A., Vishnu Khanal3, Olasunkanmi David Bamidele, Prevalence and factors associated with underutilization of antenatal care services in Nigeria: A comparative study of rural and urban residences based on the 2013 Nigeria demographic and health survey. PLOS one. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Gladys Buruwaa Nuamah, P. A.-B., Kofi Akohene Mensah, Daniel Boateng, Access and utilization of maternalhealthcare in a rural district in the forest belt of Ghana,. BMC Pregnancy and Childbirth, 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Chakraborty N, I.M., Chowdhury RI, Bari W, Akhter HH, Health Promot Int. 2003;18(4):327–37, Determinants of the use of maternal health services in rural Bangladesh,. [DOI] [PubMed]
- 66.Solomon Weldemariam, A.K. a.M.W., Utilization of institutional delivery service and associated factors among mothers in North West Ethiopian,. BMC Res Notes (2018) 11:194 10.1186/s13104-018-3295-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sanni Yaya, G. B., Michael Ekholuenetale, Factors associated with the utilization of institutional delivery services in Bangladesh. PLOS one, 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Amano A., Gebeyehu A., and Birhanu Z., Institutional delivery service utilization in Munisa Woreda, South East Ethiopia: a community based cross-sectional study. BMC pregnancy and childbirth, 2012. 12(1): p. 105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Nawal D. and Goli S., Birth preparedness and its effect on place of delivery and post-natal check-ups in Nepal. PloS one, 2013. 8(5): p. e60957 10.1371/journal.pone.0060957 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Lewetegn Moges, Prevalence of Intestinal Parasites among Preschool Children and Maternal Knowledge, Attitude and Practice on Prevention and Control of Intestinal Parasites in Senbete and Bete Towns, North Shoa, Ethiopia. November, 2015. [Google Scholar]
- 71.Vishnu K., A. M., Karkee R., and T, “Factors associated with the utilisation of postnatal care services among the mothers of Nepal: Analysis of Nepal Demographic and Health Survey 2011,”. BMCWomen’s Health, vol. 14, 2014. 10.1186/1472-6874-14-19 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Somefun O. D. and Ibisomi L., “Determinants of postnatal care non-utilization amongwomen inNigeria,”. BMCResearchNotes,vol. 9, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ayana Hordofa M., S.A. S., Berhanu M. G., and B.Lemiso H., “Postnatal Care Service Utilization and Associated Factors Among Women in Dembecha District, Northwest Ethiopia,”. Science Journal of Public Health, vol. 3, 2015. [Google Scholar]
- 74.Anteneh Asefa, S. G., Tamiru Messele, Yohannes Letamo, Endashaw Shibru, Mismatch between antenatal care attendance and institutional delivery in south Ethiopia: A multilevel analysis,. 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Haider MR, Q. Z., Khan MM, Effects of women’s autonomy on maternal healthcare utilization in Bangladesh: Evidence from a national survey,. Sex Reprod Healthc, 2017. 10.1016/j.srhc.2017.09.002 [DOI] [PubMed] [Google Scholar]
- 76.Adhikari R., Effect of Women’s autonomy on maternal health service utilization in Nepal: a cross sectional study. BMC women’s health, 2016. 16(1): p. 26 10.1186/s12905-016-0305-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(SAV)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.