Abstract
Background
Globally, post-partum depression is a major public health problem and is associated with a harmful effect on the infant, child, and mothers’ mental, physical, and social health. Although a few post-partum depression studies have been published, we still lack an accurate estimated pooled prevalence of national PPD and associated factors.
Objectives
This study aims to show the estimated pooled prevalence of PPD and associated factors in Ethiopia.
Methods
We conduct the extensive search of articles as indicated in the guideline (PRISMA), reporting systematic review and meta-analysis. Databases like MEDLINE, PubMed, psych INFO, Web of Science, EMBASE, CINAHL, Scopus, and The Cochrane Library. All publications and grey literature were addressed by using MeSH terms and keywords. The pooled estimated effect of post-partum depression and associated factors was analyzed using the random effect model meta-analysis, and 95% CI was also considered.
Protocol and registration
PROSPERO 2020 CRD42020176769 Available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020176769.
Result
A total of 11 studies with 7,582 participants were included in this meta-analysis. The estimated pooled prevalence of post-partum depression (PPD) was 22.08%, with a 95% CI (17.66%, 26.49). For factors associated with post-partum depression, a random effect size model was used during meta-analysis; unplanned pregnancy [(OR = 2.84; 95% CI (2.04, 3.97)], domestic violence [OR = 3.14; 95% CI (2.59, 3.80)], and poor social support [OR = 3.57;95% CI (2.29,5.54) were positively associated factors with post-partum depression.
Conclusion and recommendation
The estimated pooled prevalence of post-partum depression was high in Ethiopia. Unplanned pregnancy, poor social support, and domestic violence were factors affecting PPD. Therefore, the Ethiopian policymakers and health personnel better give more emphasis to mothers who had a history of unplanned pregnancy, domestic violence, and poor social support
Introduction
Depression is a major public health problem that women are around twofold greater than men to experience depression during their lifetime [1–3].
Globally, depressive disorders are common, chronic, and a principal source of disability among women. In the US, approximately 12 million women experience clinical depression each year [1].
In low- and middle-income countries, the estimated prevalence of depression among women ranges from 15 to 28% in Asia and Africa [4,5].
Post-partum depression (PPD) is a mood disorder that involves the brain and affects behavior and physical health after delivery [6]. Worldwide, depression is the leading cause of disability [7], and it affects one in five women after giving birth [8]. Post-partum depression is the most common psychiatric illness, and it is the major public problem that is as twice as common in women as men during the childbearing years [9].
Globally, severe postnatal onset depression rates are three times higher than in other periods of women’s lives [9]. Parenting stress and mother-child interaction problems are common in postnatal depressive mothers [10].
In the world, depression after delivery affects women. It increases poorer self-care and maternal morbidity and negatively affects infants, children, and families as well [5,11]. The disorder is often unrecognized and untreated, despite the potentially deleterious effects of PPD on the mother, infant, and children [9,12]. Because of the stigma of depression, the mother may refuse to seek professional help [13]. Maternal PPD has short-term negative effects on young children’s emotional, cognitive, behavioral, and interpersonal development [9].
In a worldwide review, the prevalence of PPD ranges from 4.0 to 63.9% [14]. In 56 countries, the pooled prevalence of PPD was 17.7% [15]. In India, the systematic review and metanalysis of the pooled prevalence of PPD was 22% [16]. In another review, the pooled prevalence was 20% [17]. In Iran, a systematic review and meta-analysis, the pooled prevalence was 25.3% [18]. In a systematic review in Denmark, up to 15% of the mother were affected with post-partum depression [19].
In low and middle-income countries, there are large gaps in the knowledge of the long-term effects of post-partum depression in physical, psychological, and social [10] and PPD is under-recognized and under-treated [19].
In different literature reviews; factors associated with PPD were unplanned pregnancy [20–22], a having history of depression [18,23–25], perceived lack of support from husband [25], domestic violence and lack of support [16,22], poor social support from the partner [26], birth complications [27], dissatisfaction about family [28], violence from husband [29–31] and poor social support [9,23,32].
Although mothers after delivery are at a critical period for the incidence of depression, little attention is still given in terms of prevention and treatment. Showing the pooled prevalence and factors associated with PPD by systematic review and meta-analysis is very important to health policymakers to pertain attention for these vulnerable women. Therefore, the present study reviews accessible epidemiological publications on post-partum depression and related factors in Ethiopian women to help health workers and policymakers design preventive strategies and further research.
Our two purposes in this study
What is the estimated pooled prevalence of post-partum depression in Ethiopia?
What are the associated factors for post-partum depression in Ethiopia?
Intervention(s), exposed(s); postnatal mothers who considered depression as screened by depression screening tools
Comparator(s)/control; postnatal mothers who have considered no depression by depression screening tools
Materials and methods
Search process and study selection
Literature search; Our search strategy and selection of publication for the review were conducted according to the PRISMA guideline [33]. The literature on post-partum depression among Ethiopian women was retrieved through searching the scientific search engines Database like MEDLINE, PubMed, psych INFO, Web of Science, EMBASE, CINAHL Scopus, and The Cochrane Library. All publications and grey literature were addressed by using keywords that were used in PubMed. In PubMed, MeSH terms were used (incidence OR prevalence OR magnitude OR epidemiology) AND (postnatal depression OR depression OR post-partum depression OR depressive disorder OR maternal mental health OR emotional distress OR puerperal disorder OR low mood disorder OR psychological distress) AND (after childbirth OR after delivery) AND (associated factors OR risk factors OR predictors OR determinants) AND Ethiopia, January 2010 to January 2020.
For the other databases, we employed specific subject headings as advised for each database. Furthermore, to identify other related literature, we manually searched the reference lists of eligible articles.
Protocol and registration; PROSPERO 2020 CRD42020176769 Available from https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020176769.
Eligible criteria
Inclusion criteria
Study design type-cross-sectional
Article published in the English language
Studies that reported the prevalence of post-partum depression in the health institution and in the community
A study done in Ethiopia
Publication date from 1 January 2010 to 1 January 2020
All publications which fulfilled more than 90% of the criteria were included
Exclusion criteria
Reviews, letters and international studies, and duplicated studies were excluded.
Methods for data extraction and quality assessment
Three reviewers (TAZ, WG, and ZTT) evaluated the relevant articles using the title and the abstract prior to retrieval of the full-text articles. Retrieved full-text articles were further screened according to prespecified inclusion and exclusion criteria. We resolved the arguments by a discussion with the fourth reviewer (KG).
The standardized form of the data extraction method was used for identified studies. The following information was extracted for each included study: first author, year of publication, study design, associated factors, sample size, study settings, adjusted for risk estimate (OR), and the 95% confidence interval. Data extraction from source documents was done independently by four investigators. The disagreement was resolved with discussion.
The quality of the included studies was evaluated using the Newcastle-Ottawa Scale(NOS) [34]. Sample representativeness and size, comparability between participants, ascertainment of post-partum depression, and statistical quality were the domains of NOS used to assess each study’s quality. Actual agreement and agreement beyond chance (unweighted Kappa) were used to evaluate four reviewers’ agreement. We consider the value 0 as poor agreement, 0.01 to 0.02 as slight agreement, 0.21 to 0.4 as a fair agreement, 0.41 to 0.60 as moderate agreement, 0.61 to 0.80 as substantial agreement, and 0.81 to 1.00 as almost perfect agreement [35]. In this review, the actual agreement beyond chance was ranged from 0.88 to 1 is almost perfect agreement.
Data synthesis and analysis
STATA version 14 software was used for meta-analysis. Forest plots that showed combined estimates with 95% CI. The heterogeneity was evaluated using Q and I2 statistics [36]. For the variables, the random effect size (OR) model was used. The magnitude of statistical heterogeneity between studies was assessed using I2 statistics and considered value 25% as low, 50% as a medium, and 75% as high [37]. In this review data, the value of the I2 statistics was 95.1% with a p-value ≤of 0.001, which showed there was high heterogeneity. Therefore, the overall pooled prevalence was estimated by the random effect model meta-analysis [36]. Meta-regression was made to explore the probable source of heterogeneity. We also carried a leave-one-out sensitivity analysis to assess the key studies that significantly impact between-study heterogeneity.
Variables; post-partum depression yes/no
Independent variables were unplanned pregnancy vs. planned pregnancy, poor social support vs. strong social support, and domestic violence vs. no domestic violence.
Result
Identification of the studies
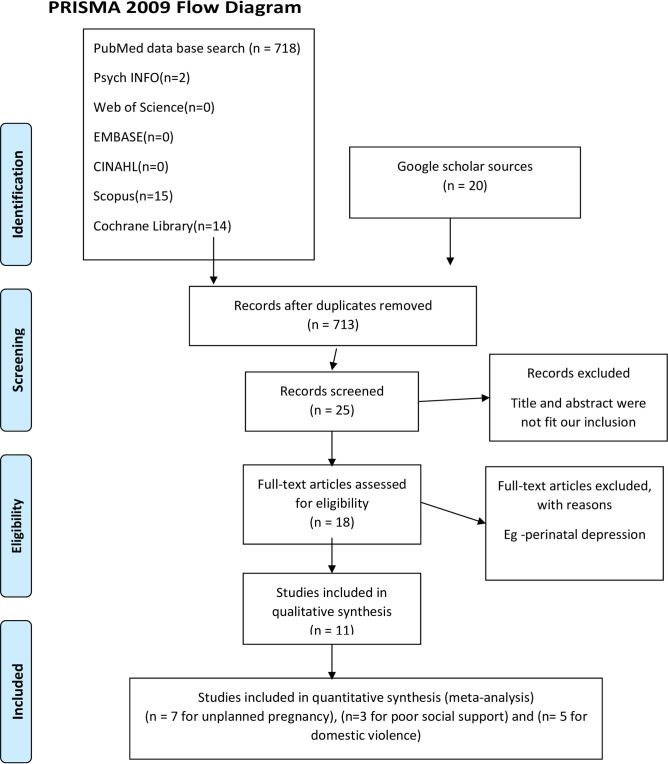
Our search strategy and selection of publication for the review was conducted in accordance with the PRISMA. In the database search, 718 articles were found. Of these, 688 articles were excluded because the title and the abstract were not fit the inclusion criteria. Eighteen articles were retrieved for full screening. However, seven studies were excluded because there was perinatal depression. Therefore, eleven studies were included in this systematic review and meta-analysis guideline (Fig 1).
Fig 1. Flow chart showing how was the research articles were searched, 2020.
Characteristics of the studies
In this systematic review and meta-analysis, 11 articles were included. The included studies were conducted from 1 January 2010 to 1 January 2020. All studies were conducted with a cross-sectional study design in Ethiopia. Post-partum depression was assessed by using EPDS (eight studies), PHQ-9 (two studies), and K-10 score (one study). Six studies were conducted in the community; the rest were in the health institution (Table 1).
Table 1. The prevalence of post-partum depression among women related to the study area in Ethiopia, 2020.
| Author | Publication year | Study area | Site | Study design | PPD | sample | case | prevalence | Tool |
|---|---|---|---|---|---|---|---|---|---|
| Asaye MM. [38] | 2020 | Gondar town | Community | cross-sectional | YES | 526 | 129 | 25 | EPDS |
| Fantahun A. [39] | 2018 | Addis Ababa | Health institution | cross-sectional | YES | 618 | 144 | 23.3 | EPDS |
| Teshome H [40] | 2016 | Addis Ababa | Health institution | cross-sectional | YES | 295 | 82 | 27.8 | K-10 score. |
| Abadiga M. [41] | 2019 | Nekemte Town | Community | cross-sectional | YES | 287 | 60 | 20.9 | EPDS |
| Shewangzaw A. [42] | 2018 | Harar Town | Health institution | cross-sectional | YES | 122 | 16 | 13.11 | EPDS |
| Azale T [43] | 2018 | Sodo district | Community | cross-sectional | YES | 3147 | 385 | 12.2 | PHQ-9 |
| Shitu S. [44] | 2019 | Ankesha district | Community | cross-sectional | YES | 596 | 141 | 23.7 | EPDS |
| Abebe A. [45] | 2019 | Bahir Dar Town | Health institution | cross-sectional | YES | 511 | 113 | 22.1 | EPDS |
| Kerie S. [46] | 2018 | Mizan Tepi Town | Health institution | cross-sectional | YES | 408 | 138 | 33.8 | EPDS |
| Toru T. [47] | 2018 | Mizan Aman Town | Community | cross-sectional | YES | 456 | 102 | 22.4 | PHQ-9 |
| Mariam D. [48] | 2016 | Eastern Zone of Tigray | Community | cross-sectional | YES | 616 | 117 | 19 | EPDS |
Qualities of included studies
The Newcastle-Ottawa Scale (NOS) was used to assess the quality of the studies methodologically. In the evaluation, we concluded that 11 studies satisfy the quality assessment in terms of selection, outcome measurement, and non-response bias. The risk of bias in each study was assessed by using kappa values, which range from 0.88 to 1, almost perfect (Table 2).
Table 2. The quality and agreed level of bias and level of agreement on the method qualities included articles in a meta-analysis based on sample, outcome, objective, responses rate and analysis method.
| Author | Publication year | Study area | Percentage of agreement | Kappa value | Level of agreement | NOS quality(0 9) |
|---|---|---|---|---|---|---|
| Asaye MM. | 2020 | Gondar town | 100 | 1 | Almost perfect | 9 |
| Fantahun A. | 2018 | Addis Ababa | 100 | 1 | Almost perfect | 9 |
| Teshome H | 2016 | Addis Ababa | 88 | 0.88 | Almost perfect | 8 |
| Abadiga M. | 2019 | Nekemte Town | 100 | 1 | Almost perfect | 9 |
| Shewangzaw A. | 2018 | Hrarar Town | 100 | 1 | Almost perfect | 9 |
| Azale T | 2018 | Sodo district | 100 | 1 | Almost perfect | 9 |
| Shitu S. | 2019 | Ankesha district | 100 | 1 | Almost perfect | 9 |
| Abebe A. | 2019 | Bahir Dar Town | 100 | 1 | Almost perfect | 9 |
| Kerie S. | 2018 | Mizan Tepi Town | 100 | 1 | Almost perfect | 9 |
| Toru T. | 2018 | Mizan Aman Town | 100 | 1 | Almost perfect | 9 |
| Mariam D. | 2016 | Eastern Zone of Tigray | 100 | 1 | Almost perfect | 9 |
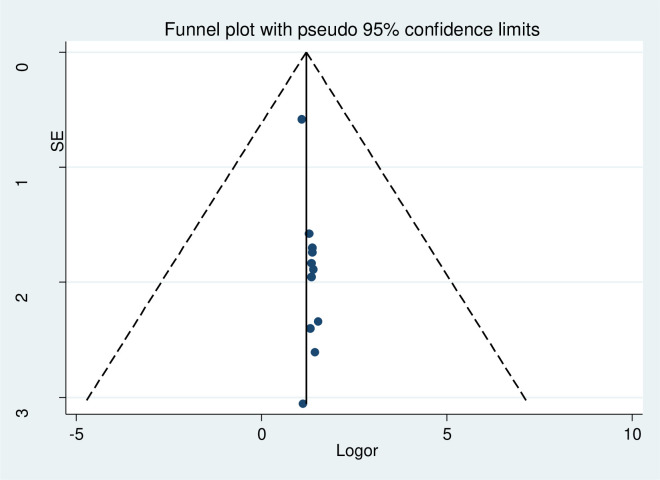
Publication bias
No evidence of publication bias was found by the funnel plot and Egger’s regression test of post-partum depression (Fig 2).
Fig 2. Forest plot presenting of publication bias of post-partum depression among after child giving mothers, Ethiopia, 2020.
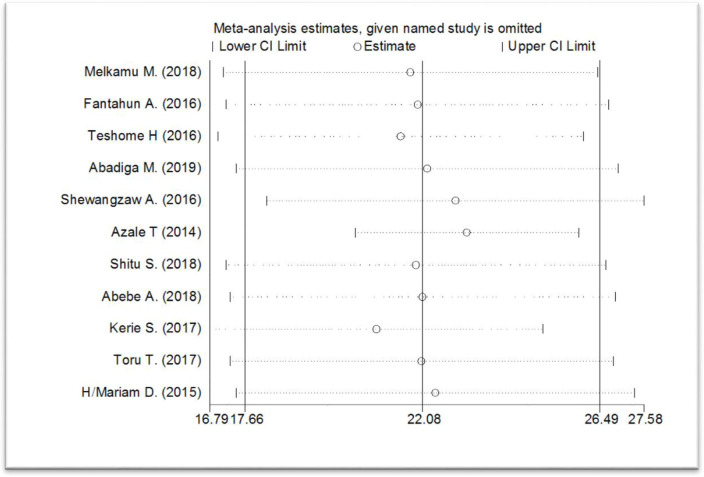
Sensitivity analysis
In the sensitivity analysis, there is no single study that is influencing the overall meta-analysis estimate (Fig 3)
Fig 3. Forest plot presenting to show not having a single study influences the overall meta-analysis estimated of post-partum depression among after child giving mothers, Ethiopia, 2020.
The result of estimated a pooled meta-analysis
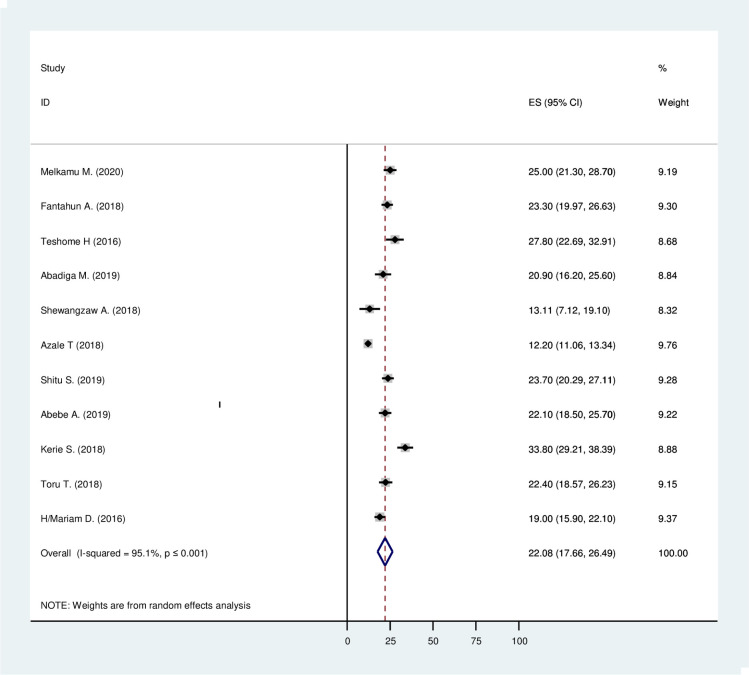
Prevalence of post-partum depression
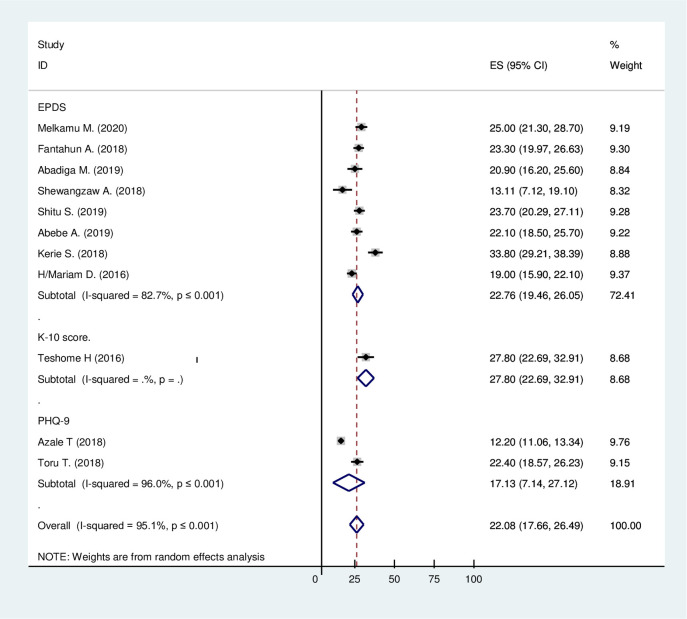
A total of 11 studies with 7,582 participants were included in this meta-analysis. In Ethiopia, the prevalence of post-partum depression was ranged from 12.2% to 33.8% (Table 1). The random-effect model was used to combine the 11 articles to show the estimated pooled prevalence of post-partum depression. The estimated pooled prevalence of post-partum depression (PPD) among mothers was 22.08%, with 95% CI (17.66%, 26.49). The studies’ heterogeneity was significant (I2 = 95.1%; Q = 204.06 df = 10 and p≤0.001) (Fig 4).
Fig 4. The estimated pooled prevalence of post-partum depression among mothers after giving birth in Ethiopia, 2020.
Subgroup analysis by assessment tools
Around eight articles were conducted with EPDS, two articles were with PHQ-9, and one study was conducted with a K-10 score. The prevalence of PPD by using EPDS, PHQ-9, and K-10 Score was 27.76% with 95% CI (19.46, 26.05), 17.13% with 95% CI (7.14, 27.12), and 27.80% with 95% CI (22.69, 32.91) respectively. The heterogeneity of each tool, EPDS, and PHQ-9, was significant (I2 = 82.7, Q = 40.38, df = 7, p≤0.001), and (I2 = 96.0, Q = 25.06, df = 1, p≤0.001) respectively. In all assessment tools; the prevalence of PDD were similar. Since the study conducted by the K-10 assessment tool was a single study, there was no heterogeneity test (Fig 5).
Fig 5. Forest plot presenting of subgroup analysis of the pooled estimated prevalence of post-partum depression based on tools in Ethiopia, 2020.
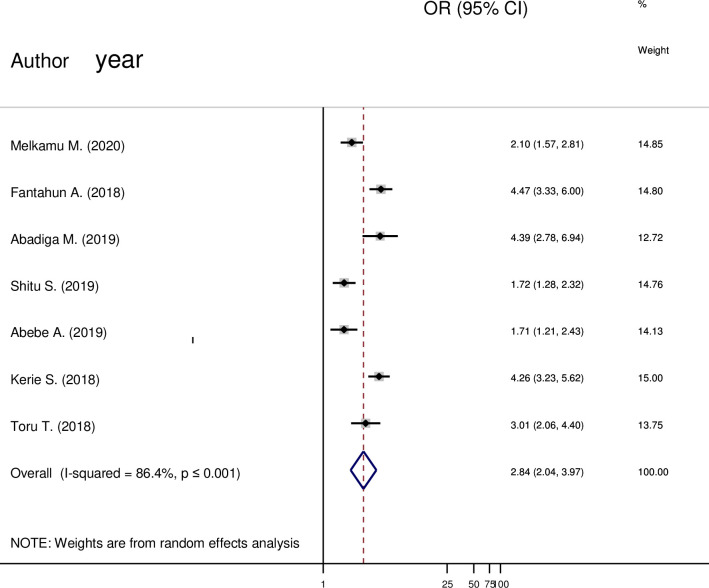
Unplanned pregnancy and post-partum depression
From (Fig 6) a total of seven articles were included in the analysis. There was a significant association between unplanned pregnancy and post-partum depression. Mothers who had a history of unplanned pregnancy were about 3(OR = 2.84; 85% CI 2.04 to 3.97) times more likely to have depression when compared to a planned pregnancy.
Fig 6. Forest plot pooled random effect size (OR) of unplanned pregnancy-related to planned pregnancy in post-partum depression among mothers in Ethiopia, 2020.
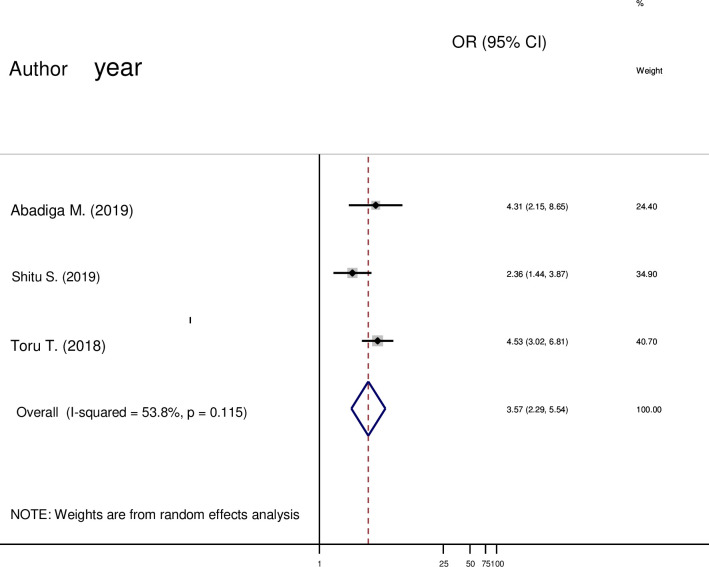
Social support and post-partum depression
Three studies were carried out in this meta-analysis. The pooled odds ratio (OR) demonstrated that the odds of PPD were significantly higher in mothers who had poor social support than mothers’ who had strong social support (OR = 3.57; 95% CI 2.29 to 5.54) (Fig 7).
Fig 7. Forest plot pooled random effect size (OR) of poor social support related to strong social support in post-partum depression among mothers in Ethiopia, 2020.
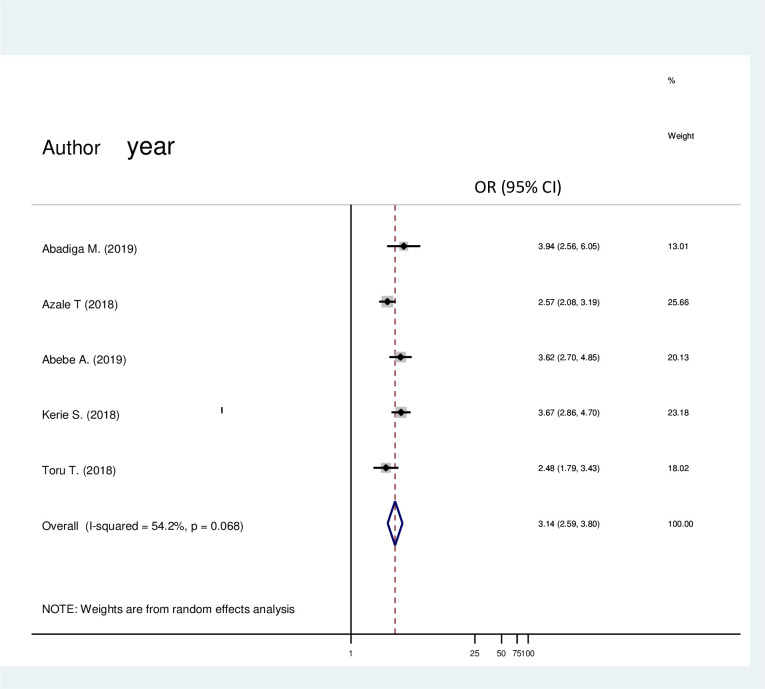
Domestic violence and post-partum depression
In (Fig 8) a total of five articles were comprised in this analysis. There was a significant association between domestic violence and post-partum depression. Having domestic violence was about 3 (OR = 3.14; 95% CI 2.59, 3.80) times more likely to have post-partum depression than not having domestic violence.
Fig 8. Forest plot pooled random effect size (OR) of domestic violence related to no domestic violence in post-partum depression among mothers in Ethiopia, 2020.
Discussion
The pooled prevalence of post-partum depression in Ethiopia in our meta-analysis was 22.08%, with a 95% CI (17.66%, 26.49). Post-partum depression is strongly linked to life stress events (socio-economic factors), physical and emotional demands of childbearing and caring for new babies, and change in hormones after delivery [49]. In low and middle-income countries, post-partum depression is even more prevalent; the reason might be biological factors like (illness, and biological predisposition); psychosocial aspects (greater exposer to violence, the difficulty of living conditions, childhood maltreatment, social exclusion, and unplanned pregnancy), and economical (poverty and food insecurity) [10]. Another study showed that individuals who are living in low-income countries experienced more stressors associated with depression and anxiety than high-income countries [50].
This finding was consistent with other systematic findings. A systematic review of studies in 56 countries showed that the pooled prevalence of PPD was 17.7% [15]. In India, the systematic review and metanalysis, the pooled prevalence of PPD was 22% [16]; in another review, the pooled prevalence was 20% [17]. In Iran, a systematic review and meta-analysis, the pooled prevalence was 25.3% [18]. These estimates in low income and middle-income countries are similar to this finding, and taken together; they support a disagreement for placing more importance on maternal post-partum depression as part of overall efforts to maternal, infant, and child health. However, the current finding was significantly higher than the prevalence of 15% derived from a systematic review of studies from Denmark [19]. The discrepancy might be due to the absence of an awareness of PPD by health experts; there are issues that may be barriers to early recognition and management of post-partum depression [51–53].
Article review revealed that the following factors affect post-partum depression: unplanned pregnancy, social support, and domestic violence.
Postnatal mothers who had poor social support were about 4 [OR = 3.57; 95% CI (2.29,5.54)] times more likely to have depression when compared to mothers who had strong social support. Poor social support refers to perceived lack of support from husband [25], poor social support from the partner [26], poor social support [9,23,32], lack of support from the family [16,22] and dissatisfaction from family [28]. The reason might be that living with a supportive person halves stress. Social support is significant for maintaining good mental and physical health, and it related to resilience [54]. Good social support has been shown to be a consistent protective factor for mothers with high distress. The mothers who reported consistent opportunities to interact and talk with people were more likely to report a reduction in distress [55].
Mothers who had a history of domestic violence were about 3 [OR = 3.14; 95% CI (2.59,3.80)] times more likely to have depression than their counterparts. Other studies revealed that mothers who had a history of violence and abuse from husband [29–31] and domestic violence from the family members [16,22] were associated with post-partum depression. Violence has a negative effect on mental health. Mothers who are violent had feelings of helplessness and then had depression; they are also high risk for suicide to end their life [56].
Women whose pregnancy was unplanned were 3[(OR = 2.84; 95% CI (2.04, 3.97)] times more likely to have depression when compared with mothers who gave birth after a planned pregnancy. Having unplanned pregnancy, unwanted delivery, and unwanted pregnancy were factors affecting post-partum depression [20–22]. The reason might be during the conception period; psychological preparedness is very important to the mother, otherwise there will be mental health problems. Unplanned pregnancy leads the mother to feel unhappy and have negative thoughts, consequently depression develops [57]. Mothers e with unplanned pregnancy had the earliest parenting stress [58]. The mother also perceived poor social support and less satisfaction with marriage life [59].
Strengths and limitations
In this study, the authors used different databases to search the articles to minimize reviewers’ bias and quality evaluation by four reviewers. Showing estimated pooled prevalence and pooled associated factors and conducting subgroup analysis based on assessment tools.
Limitation
In this study, only English language articles were included. A disproportional number of studies were included in the subgroup analysis of screening tools that minimize the estimated value’s precision.
Implication of this finding
The finding has implications for the future researcher, clinicians, and policymakers; for the future researcher, the prevalence of post-partum depression is increasing in the current finding. Therefore, it needs further investigation to know the reason why PPD is increasing and better management. Clinicians should screen the mother for depression when they present in the institution and the community. Our study should assist policymakersin design prevention and treatment strategies both in the community and in health institution.
Conclusion
Postpartum depression was high in Ethiopia. Unplanned pregnancy, poor social support, and domestic violence were factors affecting PPD. Therefore, the Ethiopian policymakers and health personnel better emphasize mothers who had a history of unplanned pregnancy, domestic violence, and poor social support.
Supporting information
(DOC)
(DOCX)
Acknowledgments
The authors would like to thank all authors of the research paper included in this systematic review and meta-analysis.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The authors received no specific funding for this work.
References
- 1.Kessler RC, McGonagle KA, Swartz M, Blazer DG, Nelson CB. Sex and depression in the National Comorbidity Survey I: Lifetime prevalence, chronicity and recurrence. Journal of affective disorders. 1993;29(2–3):85–96. 10.1016/0165-0327(93)90026-g [DOI] [PubMed] [Google Scholar]
- 2.Noble RE. Depression in women. Metabolism. 2005;54(5):49–52. 10.1016/j.metabol.2005.01.014 [DOI] [PubMed] [Google Scholar]
- 3.Robertson E, Celasun N, Stewart D. Maternal mental health & Child health and development. World health organization http://www who int/mental_health/prevention/suicide/mmh% 26chd_c hapter_1 pdf. 2008;5:2016. [Google Scholar]
- 4.Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B. Depression, chronic diseases, and decrements in health: results from the World Health Surveys. The Lancet. 2007;370(9590):851–8. [DOI] [PubMed] [Google Scholar]
- 5.Wachs TD, Black MM, Engle PL. Maternal depression: a global threat to children’s health, development, and behavior and to human rights. Child Development Perspectives. 2009;3(1):51–9. [Google Scholar]
- 6.Wisner KL, Parry BL, Piontek CM. Post-partum depression. New England Journal of Medicine. 2002;347(3):194–9. [DOI] [PubMed] [Google Scholar]
- 7.Murray C, Barber R, Foreman K, Abbasoglu Ozgoren A, Abd-Allah F, Abera S, et al. GBD 2013 DALYs and HALE Collaborators. Global, regional, and national disability-adjusted life years (DALYs) for 306 diseases and injuries and healthy life expectancy (HALE) for 188 countries, 1990–2013: quantifying the epidemiological transition. Lancet. 2015;386(10009):2145–91. 10.1016/S0140-6736(15)61340-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fisher J, Mello MCd, Patel V, Rahman A, Tran T, Holton S, et al. Prevalence and determinants of common perinatal mental disorders in women in low-and lower-middle-income countries: a systematic review. Bulletin of the World Health Organization. 2012;90:139–49. 10.2471/BLT.11.091850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stewart DE, Robertson E, Dennis C-L, Grace SL, Wallington T. Postpartum depression: Literature review of risk factors and interventions Toronto: University Health Network Women’s Health Program for Toronto Public Health; 2003. [Google Scholar]
- 10.Herba CM, Glover V, Ramchandani PG, Rondon MB. Maternal depression and mental health in early childhood: an examination of underlying mechanisms in low-income and middle-income countries. The Lancet Psychiatry. 2016;3(10):983–92. 10.1016/S2215-0366(16)30148-1 [DOI] [PubMed] [Google Scholar]
- 11.Stein A, Pearson RM, Goodman SH, Rapa E, Rahman A, McCallum M, et al. Effects of perinatal mental disorders on the fetus and child. The Lancet. 2014;384(9956):1800–19. 10.1016/S0140-6736(14)61277-0 [DOI] [PubMed] [Google Scholar]
- 12.Weissman MM, Pilowsky DJ, Wickramaratne PJ, Talati A, Wisniewski SR, Fava M, et al. Remissions in maternal depression and child psychopathology: a STAR* D-child report. Jama. 2006;295(12):1389–98. 10.1001/jama.295.12.1389 [DOI] [PubMed] [Google Scholar]
- 13.Dennis CL, Chung‐Lee L. Postpartum depression help‐seeking barriers and maternal treatment preferences: A qualitative systematic review. Birth. 2006;33(4):323–31. 10.1111/j.1523-536X.2006.00130.x [DOI] [PubMed] [Google Scholar]
- 14.Arifin SRM, Cheyne H, Maxwell M. Review of the prevalence of postnatal depression across cultures. AIMS public health. 2018;5(3):260 10.3934/publichealth.2018.3.260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hahn-Holbrook J, Cornwell-Hinrichs T, Anaya I. Economic and health predictors of national post-partum depression prevalence: a systematic review, meta-analysis, and meta-regression of 291 studies from 56 countries. Frontiers in psychiatry. 2018;8:248 10.3389/fpsyt.2017.00248 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Upadhyay RP, Chowdhury R, Salehi A, Sarkar K, Singh SK, Sinha B, et al. Postpartum depression in India: a systematic review and meta-analysis. Bulletin of the World Health Organization. 2017;95(10):706 10.2471/BLT.17.192237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McCoy SJB, Beal JM, Shipman SBM, Payton ME, Watson GH. Risk factors for post-partum depression: a retrospective investigation at 4-weeks postnatal and a review of the literature. Journal of the American Osteopathic Association. 2006;106(4):193 [PubMed] [Google Scholar]
- 18.Veisani Y, Delpisheh A, Sayehmiri K, Rezaeian S. Trends of post-partum depression in iran: a systematic review and meta-analysis. Depression research and treatment. 2013;2013 10.1155/2013/291029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pearlstein T, Howard M, Salisbury A, Zlotnick C. Postpartum depression. American journal of obstetrics and gynecology. 2009;200(4):357–64. 10.1016/j.ajog.2008.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Abdollahi F, Zain A. The mode of delivery and some selected obstetric factors as predictors of post-partum depression. Caspian Journal of Reproductive Medicine. 2015;1(2):13–21. [Google Scholar]
- 21.Kalar MU, Fatima I, Nabila K, Zainab A, Wardah G, Zara R, et al. Prevalence and predictors of postnatal depression in mothers of Karachi. International Journal of Collaborative Research on Internal Medicine & Public Health. 2012;4(5):830–839. [Google Scholar]
- 22.Tikmani SS, Soomro T, Tikmani P. Prevalence and determinants of post-partum depression in a tertiary care hospital. Austin Journal of Obstetrics and Gynecology. 2016;3(2):1. [Google Scholar]
- 23.O’hara MW, Swain AM. Rates and risk of post-partum depression—a meta-analysis. International review of psychiatry. 1996;8(1):37–54. [Google Scholar]
- 24.Ay F, Tektaş E, Mak A, Aktay N. Postpartum depression and the factors affecting it: 2000–2017 study results. Journal of Psychiatric Nursing. 2018;9(3):147–52. [Google Scholar]
- 25.Al Dallal F, Grant I. Postnatal depression among Bahraini women: prevalence of symptoms and psychosocial risk factors. EMHJ-Eastern Mediterranean Health Journal, 18 (5), 439–445, 2012. 2012. [PubMed] [Google Scholar]
- 26.Dlamini LP, Mahanya S, Dlamini SD, Shongwe MC. Prevalence and factors associated with post-partum depression at a primary healthcare facility in Eswatini. South African Journal of Psychiatry. 2019;25(1):1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kunwar D, Corey E, Sharma P, Risal A. Screening for Postpartum Depression and Associated Factors among Women who Deliver at a University Hospital, Nepal. Kathmandu University Medical Journal. 2015;13(1):44–8. [DOI] [PubMed] [Google Scholar]
- 28.Do TKL, Nguyen TTH, Pham TTH. Post-partum depression and risk factors among Vietnamese women. BioMed research international. 2018;2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Patel HL, Ganjiwale JD, Nimbalkar AS, Vani SN, Vasa R, Nimbalkar SM. Characteristics of post-partum depression in Anand district, Gujarat, India. Journal of tropical pediatrics. 2015;61(5):364–9. 10.1093/tropej/fmv046 [DOI] [PubMed] [Google Scholar]
- 30.Nasreen HE, Edhborg M, Petzold M, Forsell Y, Kabir ZN. Incidence and risk factor of post-partum depressive symptoms in women: a population based prospective cohort study in a rural district in Bangladesh. J Depress Anxiety. 2015;4(1000180):2167–1044.1000180. [Google Scholar]
- 31.Ongeri L, Wanga V, Otieno P, Mbui J, Juma E, Vander Stoep A, et al. Demographic, psychosocial and clinical factors associated with post-partum depression in Kenyan women. BMC psychiatry. 2018;18(1):1–9. 10.1186/s12888-017-1517-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.World Health Organization. Maternal mental health & child health and development Department of Mental Health and Substance Abuse Geneva: WHO; 2008. [Google Scholar]
- 33.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Annals of internal medicine. 2009;151(4):264–9. 10.7326/0003-4819-151-4-200908180-00135 [DOI] [PubMed] [Google Scholar]
- 34.Wells G, Shea B, O’Connell D, Peterson J, Welch V, Losos M, et al. NewCastle–Ottawa quality assessment scale—case control studies. 2017. [Google Scholar]
- 35.Landis JR, Koch GG. The measurement of observer agreement for categorical data. biometrics. 1977:159–74. [PubMed] [Google Scholar]
- 36.Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed‐effect and random‐effects models for meta‐analysis. Research synthesis methods. 2010;1(2):97–111. 10.1002/jrsm.12 [DOI] [PubMed] [Google Scholar]
- 37.Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. Bmj. 2003;327(7414):557–60. 10.1136/bmj.327.7414.557 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Asaye MM, Muche HA, Zelalem ED. Prevalence and Predictors of Postpartum Depression: Northwest Ethiopia. Psychiatry Journal. 2020;2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Fantahun A, Cherie A, Deribe L. Prevalence and Factors Associated with Postpartum Depression Among Mothers Attending Public Health Centers of Addis Ababa, Ethiopia, 2016. Clinical practice and epidemiology in mental health: CP & EMH. 2018;14:196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Teshome H. Postpartum Depression and Associated Factors Among Mothers: the Case of Nifas Silk Lafto Sub City Woreda 1 and 2 Health Centers: Addis Ababa University; 2006. [Google Scholar]
- 41.Abadiga M. Magnitude and associated factors of post-partum depression among women in Nekemte town, East Wollega zone, west Ethiopia, 2019: A community-based study. PloS one. 2019;14(11). 10.1371/journal.pone.0224792 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shewangzaw1a A, Tadesse B, Ashani T, Misgana T, Shewasinad S. Prevalence of Postpartum Depression and Associated Factors among Postnatal Women Attending At Hiwot Fana Specialized University Hospital, Harar, East Ethiopia.
- 43.Azale T, Fekadu A, Hanlon C. Postpartum depressive symptoms in the context of high social adversity and reproductive health threats: a population-based study. International journal of mental health systems. 2018;12(1):42 10.1186/s13033-018-0219-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Shitu S, Geda B, Dheresa M. Postpartum depression and associated factors among mothers who gave birth in the last twelve months in Ankesha district, Awi zone, North West Ethiopia. BMC Pregnancy and Childbirth. 2019;19(1):435 10.1186/s12884-019-2594-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Abebe A, Tesfaw G, Mulat H, Hibdye G. Postpartum depression and associated factors among mothers in Bahir Dar Town, Northwest Ethiopia. Annals of general psychiatry. 2019;18(1):19 10.1186/s12991-019-0244-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kerie S, Menberu M, Niguse W. Prevalence and associated factors of post-partum depression in Southwest, Ethiopia, 2017: a cross-sectional study. BMC research notes. 2018;11(1):623 10.1186/s13104-018-3730-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Toru T, Chemir F, Anand S. Magnitude of post-partum depression and associated factors among women in Mizan Aman town, Bench Maji zone, Southwest Ethiopia. BMC pregnancy and childbirth. 2018;18(1):442 10.1186/s12884-018-2072-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Mariam D, Dessalegn B, Tadesse Z, Siyoum D. Assessment of prevalence and associated factors of post-partum depression among post-partum mothers in Eastern zone of Tigray. Eur J Pharm Med Res. 2016;10(3):54–60. [Google Scholar]
- 49.United states Department of Health and Health Service. Perinatal Depression. NationalI nstitute of Mental Health; 2019. [Google Scholar]
- 50.Carbone-López K, Kruttschnitt C, Macmillan R. Patterns of intimate partner violence and their associations with physical health, psychological distress, and substance use. Public health reports. 2006;121(4):382–92. 10.1177/003335490612100406 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Mannava P, Durrant K, Fisher J, Chersich M, Luchters S. Attitudes and behaviours of maternal health care providers in interactions with clients: a systematic review. Globalization and health. 2015;11(1):36 10.1186/s12992-015-0117-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Keng SL. Malaysian midwives’ views on postnatal depression. British journal of midwifery. 2005;13(2):78–86. [Google Scholar]
- 53.Goldsmith ME. Post-partum depression screening by family nurse practitioners. Journal of the American Academy of Nurse Practitioners. 2007;19(6):321–7. 10.1111/j.1745-7599.2007.00232.x [DOI] [PubMed] [Google Scholar]
- 54.Ozbay F, Johnson DC, Dimoulas E, Morgan III C, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry (Edgmont). 2007;4(5):35 [PMC free article] [PubMed] [Google Scholar]
- 55.Berkman L. The role of social support in reducing psychological distress. International Journal of Mental Health Promotion. 2014;5(10):19–33. [Google Scholar]
- 56.Delara M. Mental health consequences and risk factors of physical intimate partner violence. Mental health in family medicine. 2016;12(1):119–25. [Google Scholar]
- 57.Barton K, Redshaw M, Quigley MA, Carson C. Unplanned pregnancy and subsequent psychological distress in partnered women: a cross-sectional study of the role of relationship quality and wider social support. BMC pregnancy and childbirth. 2017;17(1):1–9. 10.1186/s12884-016-1183-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Nelson JA, O’Brien M. Does an unplanned pregnancy have long-term implications for mother–child relationships? Journal of Family Issues. 2012;33(4):506–26. 10.1177/0192513X11420820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yanikkerem E, Ay S, Piro N. Planned and unplanned pregnancy: effects on health practice and depression during pregnancy. Journal of Obstetrics and Gynaecology Research. 2013;39(1):180–7. 10.1111/j.1447-0756.2012.01958.x [DOI] [PubMed] [Google Scholar]