Abstract
Introduction:
Some Muslim religious councils in Indonesia have ruled that measles vaccines contain haram, i.e., forbidden, materials. This study (1) evaluates changes in measles vaccination coverage between 1991 and 2017, and (2) compares vaccination coverage between Muslims and non-Muslims in Indonesia.
Methods:
Seven cross-sectional in-person surveys of mothers from 1991–2017 in Indonesia were analyzed in 2019. Participants were asked about religion in 1991–2007, and 100 datasets of religion were imputed for 2012 and 2017. In this multiple imputation analysis, binomial regression models output prevalence differences adjusted for wealth, education, child’s sex, and mother’s age. A quadratic term for year (year*year) and an interaction term between year and religion evaluated changes in vaccination over time by religion.
Results:
The seven datasets included 23,106 children 12–23 months old, with the proportion Muslim ranging between 85% to 89% across survey years. Between 1991 and 2017, measles vaccination coverage increased from 57% to 79% for non-Muslims and 59% to 79% among Muslims. In the multivariable regression model, measles vaccination coverage increased 1.6% each year (with a quadratic term of −0.05%, indicating some leveling over time). At baseline in 1991, non-Muslims had a vaccination coverage 6.2% higher than Muslims, but this disparity decreased by −0.2% each year.
Conclusions:
Measles vaccination increased in both Muslims and non-Muslims in Indonesia but has stagnated in recent years. Because of increased attention among Muslim groups on haram materials in vaccines since 2017, future studies should continue to examine the relationship between religion and vaccine uptake in Indonesia.
Keywords: Islam, Indonesia, measles vaccine, vaccination coverage
INTRODUCTION
Over recent decades, global vaccination coverage has been increasing.1 However, vaccination coverage is not uniform across different socioeconomic groups,2 and vaccine uptake can be impacted by access, affordability, and acceptance.3 Indonesia has a large annual birth cohort of around 5 million – the fifth largest in the world after India, China, Nigeria, and Pakistan – and it has been able to progressively increase vaccination coverage, with uptake of diphtheria-tetanus-pertussis vaccine dose 3 (DTP3) reaching 83% in 2012.1
Indonesia’s estimated population as of 2017 was 260 million.4 Overall, 87% of Indonesians identify as Muslim, although several provinces have non-Muslim majorities (four being majority Christian and one majority Hindu).5 According to the 2010 census, Aceh has the highest percentage of Muslims compared to all other Indonesian provinces,5 and, as of 2005, is the only Indonesian province officially allowed to practice Shari’ah Law.6
The relationship between religion and vaccination acceptance, and therefore uptake, has recently come to the forefront in Indonesia. In response to community concerns of vaccines, specifically that immunization may interfere with an individual’s destiny, and that vaccines may contain haram, i.e. forbidden, material, the Indonesian Council of Ulama issued a fatwa about vaccination in 2016.7 In Indonesia, fatwas are rulings under Islamic law that are not legally binding but highly influential among the Muslim population.8 The ruling stated that immunizations were allowed but that vaccines should be certified as halal. In response to a new measles vaccine (a measles-rubella combination vaccine) introduced in 2017, the Indonesian Council of Ulama issued a fatwa that the new vaccine was haram because some porcine components are used in the manufacturing process.9 In case of a medical emergency or recommendation by a doctor, they argued it permissible to get a measles vaccine. The fatwa also stated that because there is no halal alternative of the vaccine, the version produced with pork is an acceptable vaccine for the time being. However, it is important to consider that, globally, other Muslim organizations have issued statements promoting vaccines. For example, in 2017, the Dakar Declaration of Vaccination signed by African Islamic Leaders explains why parents need to vaccinate their children.10 It directly states that vaccines do not cause sterility – a concern among some Muslim groups. The declaration does nevertheless support the creation of a certification body to determine which vaccines should be considered halal. However, religious expression may not necessarily have a negative impact on health.11 Practicing religion may give women, often the primary medical-decision makers within families, space to express spirituality and ideas. Rinaldo argues that the Islamic revival in Indonesia has led to economic and social opportunities for Muslim women.12 However, the association between religion and public health, and vaccination specifically, is understudied.
Previous studies have examined vaccination coverage in Indonesia,13 but instead of considering religion have focused on other explanatory variables, like urbanicity.14 Using several waves of the Indonesia Demographic and Health Surveys (DHS), this study (1) describes changes in demographic make-up between Muslims and non-Muslims in Indonesia over time, and (2) characterizes the impact of religion on measles vaccination coverage in Indonesia.
METHODS
Study population
Cross-sectional data from the Demographic and Health Survey (DHS) program in was analyzed in 2019. Between 1987 and 2017, there have been 8 Indonesia DHSs conducted: 1987, 1991, 1994, 1997, 2002, 2007, 2012, and 2017. The 1987 survey lacks certain variables including measles vaccination, and so was excluded from this analysis. The United States Agency for International Development (USAID) funds the DHS program. The DHSs are designed to generate national and sub-national estimates of vital statistics as well as maternal and child health characteristics through a two-stage cluster design: the first level are Census Enumeration Areas, and the second stage are households selected from an updated list of households in that Enumeration Area. DHSs are available for many countries. For example, one recent publication details differences in vaccination coverage between Muslims and Christians in African countries.15 Details about the survey, and access to the survey data, are available from: https://dhsprogram.com. The results in this study are limited to children 12–23 months old who were alive at the time of the study. The surveys are not necessarily conducted within the same communities, and it is not known if individuals were re-sampled over time. Additionally, not all provinces and areas are included in every year: East Timor became independent and was therefore not in any dataset from 2002 on, and Aceh, Maluku, and Papua were not included in 2002 because of security concerns. A sensitivity analysis was conducted by removing East Timor and the year 2002 from the dataset, and the results were substantially the same as the main analysis.
Derived variables
The variables used in this study include religion, wealth index, child’s sex, and respondent’s (mother’s) education and age. Most of these variables are directly available on the DHS questionnaire with the following exceptions. Wealth index was not calculated in 1991, 1994, and 1997. The index in these years was created by conducting a principle components analysis on the following variables (not all variables were available for all datasets): source of drinking water, source of non-drinking water, electricity, radio, television, refrigerator, bicycle, motorcycle or boat, automobile, main floor material, main wall material, and main roof material, and type of stove. Religion was asked in 1991–2007, but not in 2012 and 2017. For these years, 100 values were imputed for every individual, where the respondents’ religious affiliation (Muslim vs. non-Muslim) was randomly generated based on the distribution of Muslims in that respondent’s province according to the 2007 DHS. In comparing the imputed and observed values in the 2007, the imputation method is highly sensitive – 87.8% of those Muslim were imputed to be Muslim. Moreover, a majority (56.3%) of those non-Muslim were identified as such. Religious affiliation was based on the mothers’ self-report; inter-faith marriages are relatively rare in Indonesia.16
The outcome, measles vaccination, was determined from either the mother’s report or from vaccination cards provided by community health centers, or Puskesmas. Puskesmas were first introduced in the late 1960s,17 and have been the primary source of vaccinations, since the national immunization program was started in 1977. The vaccination program initially included polio, diphtheria-tetanus-pertussis (DTP), and measles vaccines. In 1997, the hepatitis B was brought into the program at the national level, and in 2013, the pentavalent vaccine (diphtheria-tetanus-pertussis-hepatitis B-Haemophilus influenzae type b) was introduced.18 All these vaccines are freely available in the Puskesmas. Indonesia switched from using a measles to a measles-rubella vaccine in 2017, and that a national measles mass vaccination campaign was on-going in 2017 and 2018, with over 60 million children targeted for vaccination.19 Vaccinations administered during mass campaigns were counted (but had not been differentiated from routine vaccinations) in this analysis. Records of measles vs measles-rubella vaccination were not distinguished in the dataset. DTP or pentavalent dose 3 vaccination coverage is also tabulated as an example of a vaccine used in many cross-country comparisons.1
Statistical analysis
Observed measles vaccination coverage in 2017 was mapped by province. Estimates of vaccination coverage were modeled with a binomial regression model in a Generalized Estimating Equations (GEE) framework clustered by household and the survey cluster, and accounting for an independent covariance matrix. Two sets of models were estimated. The first set only included religion and wealth index. Estimates of vaccine coverage by survey year were derived from the intercept of the model and are graphically depicted along with 95% confidence intervals (CIs). The second set was another binomial regression model which included year, religion, child’s sex, mother’s age, mother’s education level, and the family wealth index. A quadratic term for year (year*year) and an interaction term between year and religion evaluated changes in vaccination over time by religion.
The code used to generate the derived variables and to conduct the statistical analysis is available on figshare: https://figshare.com/articles/Indonesia_DHS_code/12042855.
Ethical approval
This study was limited to a secondary data analysis. It has been deemed exempt and not regulated by the University of Michigan Health Sciences and Behavioral Sciences Institutional Review Board (HUM00162698).
RESULTS
Across the seven datasets there were 122,068 children 0–59 months old who had mothers 15–49 years old who were interviewed (15,708 in 1991, 18,196 in 1994, 17,444 in 1997, 16,206 in 2002, 18,645 in 2007, 18,021 in 2012, and 17,848 in 2017). In total, 97,826 children who were not 12–23 months old were excluded (by year: 12,553, 14,755, 13,921, 12,967, 15,008, 14,406, and 14,215), and 1,136 children who had died were also removed (by year: 239, 200, 194, 142, 150, 113, and 98). The remaining dataset included 23,106 children, with the proportion Muslim ranging between 85% to 89% across survey years (Table 1). Socioeconomic status improved over this time frame, but was generally lower among non-Muslims. For example, the proportion of mothers without any education in 1991 was 22% among non-Muslims and 12% among Muslims. By 2017, these numbers were shifted to 2% and 1%, respectively. For wealth index, a greater proportion of non-Muslims were in the poorest category compared to Muslims (31% vs 17% in 1991), with this disparity slightly increasing by 2017 (38% of non-Muslims in poorest category compared to 17% of Muslims).
Table 1.
Demographic characteristics, stratified by religion, among children 12–23 months old and their mothers, Indonesia DHS.
| 1991 n=2915 |
1994 n=3241 |
1997 n=3329 |
2002 n=3097 |
2007 n=3487 |
2012 n=3502 |
2017 n=3535 |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Non-Muslim | Muslim | Non-Muslim | Muslim | Non-Muslim | Muslim | Non-Muslim | Muslim | Non-Muslim | Muslim | Non-Muslim | Muslim | Non-Muslim | Muslim | |
| Overall (row %) | 13% | 87% | 13% | 87% | 13% | 87% | 11% | 89% | 15% | 85% | 14% | 86% | 13% | 87% |
| Proportion female | 51% | 50% | 54% | 50% | 53% | 52% | 50% | 48% | 48% | 47% | 47% | 49% | 48% | 50% |
| Respondent’s age | ||||||||||||||
| 15–24 years | 25% | 36% | 23% | 33% | 24% | 34% | 21% | 33% | 19% | 31% | 27% | 25% | 22% | 22% |
| 25–34 years | 56% | 48% | 58% | 50% | 55% | 48% | 53% | 50% | 57% | 50% | 51% | 54% | 53% | 52% |
| 35–49 years | 19% | 16% | 19% | 17% | 21% | 18% | 27% | 17% | 24% | 19% | 22% | 21% | 24% | 27% |
| Respondent’s education | ||||||||||||||
| None | 22% | 12% | 15% | 10% | 14% | 8% | 6% | 4% | 6% | 2% | 6% | 1% | 2% | 1% |
| Primary | 45% | 66% | 43% | 62% | 38% | 59% | 38% | 45% | 33% | 42% | 29% | 30% | 25% | 24% |
| Secondary | 26% | 20% | 35% | 25% | 41% | 30% | 48% | 46% | 49% | 48% | 53% | 57% | 55% | 59% |
| Tertiary | 7% | 2% | 8% | 3% | 7% | 4% | 7% | 6% | 12% | 9% | 12% | 13% | 18% | 16% |
| Wealth index | ||||||||||||||
| Poorest | 31% | 17% | 29% | 10% | 30% | 9% | 47% | 20% | 42% | 17% | 39% | 17% | 38% | 17% |
| Poorer | 15% | 21% | 15% | 19% | 15% | 17% | 11% | 19% | 15% | 20% | 22% | 22% | 19% | 20% |
| Middle | 14% | 18% | 16% | 22% | 17% | 20% | 10% | 21% | 14% | 22% | 18% | 20% | 16% | 20% |
| Richer | 16% | 22% | 11% | 23% | 14% | 27% | 11% | 21% | 13% | 22% | 11% | 21% | 14% | 22% |
| Richest | 24% | 22% | 28% | 26% | 23% | 27% | 20% | 19% | 16% | 20% | 11% | 20% | 12% | 20% |
| Child had DTP3 vaccine | 55% | 56% | 64% | 59% | 67% | 65% | 63% | 59% | 57% | 69% | 68% | 73% | 76% | 77% |
| Child had measles vaccine | 57% | 59% | 67% | 63% | 75% | 71% | 70% | 73% | 73% | 78% | 75% | 81% | 79% | 79% |
Notes:
DHS, Demographic and Health Surveys; DTP3, 3rd dose diphtheria-tetanus-pertussis (or pentavalent) vaccine
Overall, measles and DTP3 vaccination coverage increased between 1991 and 2017. For measles vaccination, it increased from 58% in 1991 to 53% in 1994, 72% in 1997, 73% in 2002, 77% in 2007. Thereafter gains were minimal (80% in 2012 and 79% in 2017). DTP3 vaccination followed a similar pattern (at the seven time points: 56%, 60%, 65%, 59%, 67%, 73%, and 77%).
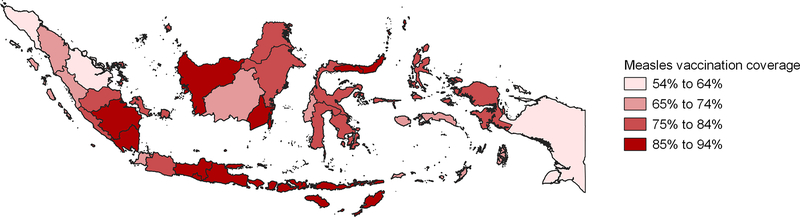
Between 1991 and 2017, the crude, unadjusted measles vaccination coverage increased from 57% to 79% for non-Muslims and 59% to 79% among Muslims. Figure 1 shows the geographical distribution of measles vaccination coverage in 2017. Overall, measles vaccination coverage was 79%, but this ranged from 54% in Aceh and 55% in Riau to 91% in South Kalimantan, 92% in Gorontalo and 94% in North Sulawesi.
Figure 1.
Measles vaccination coverage in children 12–23 months by Indonesian province, 2017 Demographic and Health Survey.
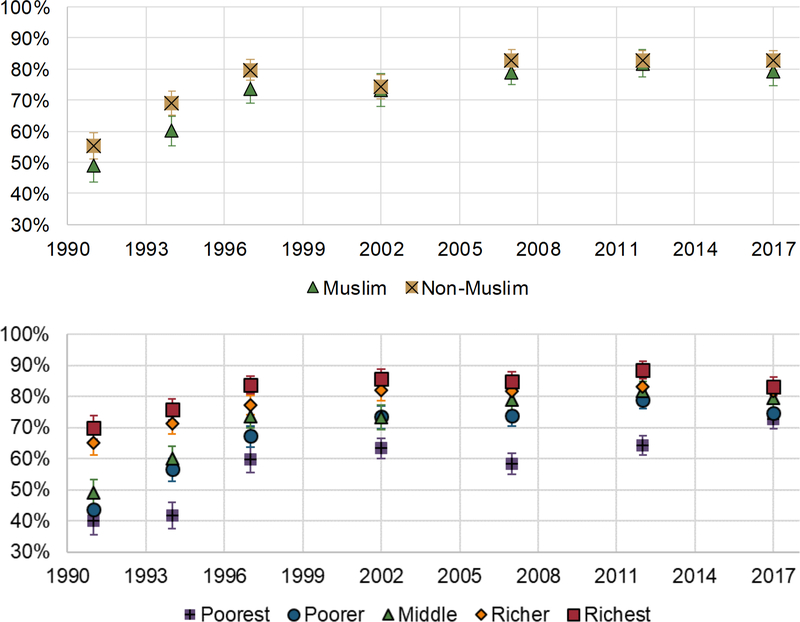
Estimated disparities by religion and wealth index, according to models adjusted for both variables, are shown in Figure 2. There is a substantial reduction in disparities across wealth index over time. In the poorest quintile, vaccination coverage increased steadily from 40% to 73% over time. In the richest quintile, coverage increased from 70% to 84% between 1991 and 1997, and has since hovered between 83% and 86%. Among non-Muslims, vaccination coverage increased from 55% in 1991 to 83% in 2007 on. For Muslims, vaccination coverage increased from 49% in 1991 to 82% in 2012, before decreasing to 79% in 2017.
Figure 2.
Measles vaccination coverage in children 12–23 months old over time and by religion and wealth index. Estimates from binomial models conditioned on religion and wealth index.
In the multivariable regression model (Table 2), measles vaccination coverage increased 1.6% each year (95% CI: 1.4%, 1.9%), with a quadratic term of −0.05% (95% CI: −0.05%, −0.04%) indicating some leveling over time. At baseline in 1991, non-Muslims had a vaccination coverage 6.2% higher than Muslims (95% CI: 3.8%, 8.6%), but this disparity decreased by −0.2% each year (95% CI: −0.4%, 0.0%).
Table 2.
Measles vaccination coverage in Indonesian children 12–23 months old, 1991–2017 DHS.
| Across all available data (n=23,106)a | Excluding 2002 and East Timor (n=19,672)a | ||||
|---|---|---|---|---|---|
| Variables | β | 95% Confidence Interval | P-value | β | P-value |
| Intercept | 69.3% | (67.0%, 71.5%) | <.0001 | 68.9% | <.0001 |
| Years since 1991 (continuous) | 1.6% | (1.4%, 1.9%) | <.0001 | 1.6% | <.0001 |
| Years * Years | −0.05% | (−0.05%, −0.04%) | <.0001 | 0.0% | <.0001 |
| Non-Muslim vs Muslim | 6.2% | (3.8%, 8.6%) | <.0001 | 7.0% | <.0001 |
| Non-Muslim * Years | −0.2% | (−0.4%, 0.0%) | 0.0309 | −0.2% | 0.0257 |
| Child's sex: male vs female | −0.2% | (−1.2%, 0.9%) | 0.7757 | −0.4% | 0.5527 |
| Respondent’s age (ref: 25–34 years) | |||||
| 15–24 years | −0.7% | (−2.0%, 0.6%) | 0.2736 | −0.1% | 0.8757 |
| 35–49 years | −2.9% | (−4.3%, −1.4%) | 0.0002 | −2.9% | 0.0004 |
| Educational attainment (ref: secondary school) | |||||
| No formal education | −26.6% | (−29.5%, −23.8%) | <.0001 | −26.5% | <.0001 |
| Primary | −12.2% | (−13.6%, −10.8%) | <.0001 | −11.6% | <.0001 |
| Tertiary | 1.1% | (−0.6%, 2.9%) | 0.2105 | 0.6% | 0.5519 |
| Respondent’s wealth index (ref: middle) | |||||
| Poorest | −9.3% | (−11.1%, −7.4%) | <.0001 | −10.2% | <.0001 |
| Poorer | −2.3% | (−4.1%, −0.4%) | 0.0153 | −2.8% | 0.0045 |
| Richer | 3.8% | (2.1%, 5.6%) | <.0001 | 3.7% | 0.0001 |
| Richest | 5.7% | (3.9%, 7.4%) | <.0001 | 5.8% | <.0001 |
Note: Boldface indicates statistical significance (p<0.05).
Multivariable binomial regression model, 100 multiple imputations to account for missing data on religion in the 2012 and 2017 surveys
Mother’s age, education, and wealth index were also significant predictors of a child’s vaccination coverage. Respondents 35–49 years old had −2.9% (95% CI: −4.3%, −1.4%) lower coverage than respondents 25–34 years old. There was a dose-response relationship by education, whereas coverage was substantially lower among those with no education compared to a secondary education (−26.6%, 95% CI: −29.5%, −23.8%), with an attenuated disparity between those with primary and a secondary education (−12.2%, 95% CI: −13.6%, −10.8%). Those in the poorest quintile had −9.3% lower coverage compared to those in the middle quintile (95% CI: −11.1%, −7.4%), whereas those in the richest quintile were 5.7% higher (3.9%, 7.4%) compared to those in the middle quintile.
DISCUSSION
Across almost three decades’ worth of vaccination and religion data in Indonesia, there was a substantial increase in vaccination coverage, although uptake in the past ten years was stagnant among higher wealth groups and among Muslims, and there was a slight decline in Muslims between 2012 and 2017.
The disparity of vaccination coverage by wealth index shrank from 1991 to 2017, wealth index and mother’s education were positively associated with a child’s measles vaccination coverage during this time period. Associations between socioeconomic factors and immunization status may have attenuated over time because of a strong network of public clinics, the Puskesmas, in Indonesia which freely offer vaccines to all children.20 That there still is a disparity by wealth index could be a function of time costs and convenience – how many hours a day or how many days a week a Puskesmas is open can vary across the country,21 and could explain low vaccination coverage in some more remote regions. Parents in certain socioeconomic strata may also be more hesitant towards vaccination. A study of parents in Malaysia found employment status, but not educational level or monthly household income, to be associated with vaccine hesitancy.22 In Indonesia, a study in Aceh found socioeconomic status to be associated with acceptance of a hypothetical dengue vaccine23 while another study in West Sumatra and Aceh found that having a diploma certificate was associated with non-hesitant vaccine attitudes among parents.24 Finally, it is possible that certain vaccination providers at Puskesmas may consider some vaccines to be more of a priority than other vaccines.25
Overtime the disparity in measles vaccination coverage between Muslims and non-Muslims decreased. For 2002 this may have resulted from some provinces excluded from sampling that year. Measles vaccination coverage among Muslims stagnated between 2012 (81%) and 2017 (79%). This coincides with the issuance of the fatwa in 2016, although it excludes the more recent fatwa in 2018. There is also large variation in the proportion of children who received the measles vaccine by province in 2017. Aceh, the only province allowed to practice Shari’ah Law, had the lowest measles vaccination coverage at 54%. Further research will be needed to understand the potential link between the fatwa and the decline in measles vaccination among Muslims after the more recent fatwa in 2018, as well as the low coverage in Aceh. This relationship may be more discernible in the future. Understanding parental attitudes towards vaccination will be useful for understanding if the fatwa and concerns that the measles vaccine is haram had any bearing on the decision to vaccinate.
The experiences of other Muslim-majority countries in the region show diversity in the presentation of vaccine hesitancy and the relationship between religion and vaccination uptake. Malaysia, which neighbors Indonesia, has had high vaccination coverage, but childhood vaccines are not compulsory,26 and the prevalence of vaccine hesitancy was 11.6% among Malaysian parents in 2016.22 Interestingly, the study in Malaysia found hesitancy higher in non-Muslims compared to Muslims. More parents received information about vaccines from the internet than from doctors.22 Pakistan, which has the world’s second largest Muslim population after Indonesia, has recently struggled with polio eradication, as its citizens are wary of the oral polio vaccine (OPV) due to rumors spread by local news. Some common rumors have religious undertones and include OPV causes sterilization and it contains porcine products, so is not halal.27,28 Small outbreaks of polio have been seen since.28 In Saudi Arabia, an Islamic theocracy, parents in one survey were highly confident in vaccines. And even vaccine hesitant parents did not see religion as prohibiting vaccination.29 A study of religion and vaccination in African countries found that in most countries, vaccination coverage was higher among Christians than Muslims, but the reverse was true in other countries and there was substantial diversity in coverage between countries.15 The findings from these countries show that it may not be possible to generalize the relationship between religion and vaccination beyond one country.
The nature of Islam in Indonesia is complex and changing, although at its basis, religion is a core part of identity for many in Indonesia, as symbolized by the national identification card stating the citizen’s religion.6 Indonesia in some respects has experienced a rise in religiosity, specifically in Islam. An increasing number of mosques has coincided with “faith politics” becoming more popular in recent elections.30 While Indonesia on a national level is not a theocracy, the government does ban blasphemy, and in 2008 decided to punish members of the Islamic movement Ahmadiyya from spreading their religious ideas.6 However, this rise in Islam has overlapped with improved social positioning of women. For example, the proportion of women who have control over their own earnings is relatively high and has increased in recent years, from 65% in 2012 to 73% in 2017.31 Other countries in Asia with large Muslim populations show a much lower proportion for this number: 49% in Pakistan,32 32% in Bangladesh,33 and 26% among Muslims in India.34 Indonesia is diverse, not only in terms of religion, but also with language, ethnicity, and cultural backgrounds. A multitude of factors beyond religion could be impacting perceptions of vaccines.
It is also important to recognize that, despite improvements over time, vaccine coverage in 2017 for both Muslims and non-Muslims in Indonesia was far lower than the 90% goal outlined in the World Health Organization’s Global Vaccine Action Plan.35 Both Muslim and non-Muslim communities in Indonesia are potentially at risk of a measles outbreak, such as the one experienced by Papua in 2017 and 2018.36 The government has already enlisted religious and community leaders to promote vaccines,19 and continued efforts to improve vaccination coverage in both Muslims and non-Muslims will be needed to protect against such outbreaks. Integration of religious leaders into the promotion of new vaccines could mitigate future conflicts with religious councils.37
Strengths and limitations
This study has a number of limitations. More in-depth questions based on religion and adherence to religious guidelines could have been added. Further questions regarding women’s empowerment and health education could be beneficial to providing stronger connections between vaccination, religions, and maternal autonomy. Additionally, other mediators of the relationship between religion and vaccination status, for example, family size or birth order, may be important. The absence of surveying religion from 2012 onwards is also limiting. Although multiple imputation was able to recapture some of this data, the underlying assumptions (using province-level data related to religion from 2007 to project onto 2012 and 2017) may be overly simplistic, and power to detect differences in 2012 and 2017 was lost. Imputed data in 2012 and 2017 may not reflect changing religious trends over time in different areas. Although all non-Muslims were combined into one category for this analysis, Indonesia is a religiously diverse country, with Christians, Hindus, Buddhists, and Confucians having a presence in the Indonesian Archipelago for hundreds of years. A 2010 estimate puts Muslims as the majority (87.2%) with Protestants (7%), Roman Catholics (2.9%), and Hindus (1.7%) as the predominant religious groups.38 Over time, there are a number of other trends which could affect vaccination coverage, for instance declines in infant mortality, particularly in the vaccinated group.
This study also has a number of strengths including the use of DHS, a set survey used nationally that asks in-depth questions on daily life and health. This survey is an accurate depiction of the viewpoints of survey participants nationwide, and allows for comparisons across regions of the country.
Conclusions
In the past few decades in Indonesia, measles vaccination coverage has increased. Disparities across socioeconomic status and religion may have diminished over time: individuals in the lowest quintile of wealth have seen extraordinary gains in measles vaccine uptake. There is evidence that this disparity is decreasing also between Muslims and non-Muslims, although recent fatwas issued regarding haram content in vaccines may reduce vaccination coverage in the near future. The picture of immunization in Indonesia is complex, with geography and socioeconomic status, including religion, playing a role. Ultimately, understanding religious influence in a parent’s decision to vaccinate their child will be important to ensure coverage rates increase, and vaccine manufacturer’s should consider the use of halal products.
Acknowledgements
We appreciate the work of the data collectors who work in the Demographic and Health Surveys Program.
ALW’s salary was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number K01AI137123. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The study sponsor did not have any role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Conflict of interest: ALW’s salary was supported by the National Institute of Allergy and Infectious Diseases of the National Institutes of Health under Award Number K01AI137123. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. The study sponsor did not have any role in study design; collection, analysis, and interpretation of data; writing the report; or the decision to submit the report for publication.
Footnotes
Financial disclosure: No financial disclosures were reported by the authors of this paper.
REFERENCES
- 1.VanderEnde K, Gacic-Dobo M, Diallo MS, Conklin LM, Wallace AS. Global Routine Vaccination Coverage — 2017. MMWR Morb Mortal Wkly Rep. 2018;67(45):1261–1264. doi: 10.15585/mmwr.mm6745a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ndwandwe D, Uthman OA, Adamu AA, et al. Decomposing the gap in missed opportunities for vaccination between poor and non-poor in sub-Saharan Africa: A Multicountry Analyses. Hum Vaccin Immunother. 2018;14(10):2358–2364. doi: 10.1080/21645515.2018.1467685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Thomson A, Robinson K, Vallée-Tourangeau G. The 5As: A practical taxonomy for the determinants of vaccine uptake. Vaccine. 2016;34(8):1018–1024. doi: 10.1016/j.vaccine.2015.11.065 [DOI] [PubMed] [Google Scholar]
- 4.CIA. CIA Factbook World Population 2017. http://www.idai.or.id/artikel/klinik/imunisasi/jadwal-imunisasi-2017 Published 2019.
- 5.Indonesia Census. Population According to Region and Religion Advised Indonesia. https://sp2010.bps.go.id/index.php/site/tabel?tid=321&wid=0 Published 2010. Accessed July 30, 2019.
- 6.U.S. Commission on International Religious Freedom. United States Commission on Religious Freedom Report. https://www.uscirf.gov/sites/default/files/2019USCIRFAnnualReport.pdf Published 2019. Accessed July 30, 2019.
- 7.Majelis Ulama Indonesia. Fatwa Majelis Ulama Indonesia (MUI) tentang imunisasi. http://www.mui.or.id Published 2016.
- 8.The University of Melbourne. What is a fatwa and what does it mean for Indonesian policy? https://indonesiaatmelbourne.unimelb.edu.au/what-is-a-fatwa-and-what-does-it-mean-for-indonesian-policy/ Published 2016. Accessed December 2, 2019.
- 9.Rochmyaningsih D Indonesian fatwa causes immunization rates to drop. Science (80-). 2018;362(6415):628–629. doi: 10.1126/science.362.6415.628 [DOI] [PubMed] [Google Scholar]
- 10.WHO. Dakar Declaration on Vaccination. https://afro.who.int/sites/default/files/2017-09/ReligiousLeadersDeclaration.pdf Published 2014. Accessed July 30, 2019.
- 11.Foege WH. Positive and Negative Influences of Religion, Culture, and Tradition in Public Health. Am J Public Health. 2019;109(3):378–378. doi: 10.2105/ajph.2018.304921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rinaldo R The Islamic revival and women’s political subjectivity in Indonesia. Womens Stud Int Forum. 2010;33(4):422–431. doi: 10.1016/j.wsif.2010.02.016 [DOI] [Google Scholar]
- 13.Brown DW, Gacic-Dobo M. Home-based record prevalence among children aged 12–23 months from 180 demographic and health surveys. Vaccine. 2015;33(22):2584–2593. doi: 10.1016/j.vaccine.2015.03.101 [DOI] [PubMed] [Google Scholar]
- 14.Fernandez RC, Awofeso N, Rammohan A. Determinants of apparent rural-urban differentials in measles vaccination uptake in Indonesia. Rural Remote Health. 2011;11(3):1–14. [PubMed] [Google Scholar]
- 15.Costa JC, Weber AM, Darmstadt GL, Abdalla S, Victora CG. Religious affiliation and immunization coverage in 15 countries in Sub-Saharan Africa. Vaccine. 2020;38(5):1160–1169. doi: 10.1016/j.vaccine.2019.11.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Refugee Review Tribunal. RRT Research Response: IDN34011. https://www.refworld.org/pdfid/4b6fe1fe25.pdf Published 2008. Accessed June 9, 2020.
- 17.Benotti E, Hirschhorn L, Sugiyarso S, Ahmad J. Indonesia: Puskesmas and the Road to Equity and Access | PHCPI. https://improvingphc.org/indonesia-puskesmas-and-road-equity-and-access Accessed June 9, 2020.
- 18.Hadisoemarto PF, Reich MR, Castro MC. Introduction of pentavalent vaccine in Indonesia: A policy analysis. Health Policy Plan. 2016;31(8):1079–1088. doi: 10.1093/heapol/czw038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pronyk P, Sugihantono A, Sitohang V, et al. Vaccine hesitancy in Indonesia. Lancet Planet Heal. 2019;3(3):e114–e115. doi: 10.1016/S2542-5196(18)30287-0 [DOI] [PubMed] [Google Scholar]
- 20.Holipah Maharani A, Kuroda Y. Determinants of immunization status among 12- to 23-month-old children in Indonesia (2008 – 2013): a multilevel analysis. BMC Public Health. 2018;18:288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.World Bank Group, Australian Aid, The Global Fund, Gavi The Vaccine Alliance. Is Indonesia Ready to Serve? doi: 10.1596/30623 [DOI] [Google Scholar]
- 22.Mohd Azizi FS, Kew Y, Moy FM. Vaccine hesitancy among parents in a multi-ethnic country, Malaysia. Vaccine. 2017;35(22):2955–2961. doi: 10.1016/j.vaccine.2017.04.010 [DOI] [PubMed] [Google Scholar]
- 23.Harapan H, Anwar S, Setiawan AM, Sasmono RT. Dengue vaccine acceptance and associated factors in Indonesia: A community-based cross-sectional survey in Aceh. Vaccine. 2016;34(32):3670–3675. doi: 10.1016/j.vaccine.2016.05.026 [DOI] [PubMed] [Google Scholar]
- 24.Yufika A, Wagner AL, Nawawi Y, et al. Parents’ hesitancy towards vaccination in Indonesia: A cross-sectional study in Indonesia. Vaccine. 2020;38(11):2592–2599. doi: 10.1016/j.vaccine.2020.01.072 [DOI] [PubMed] [Google Scholar]
- 25.Seale H, Sitaresmi MN, Atthobari J, et al. Knowledge and attitudes towards rotavirus diarrhea and the vaccine amongst healthcare providers in Yogyakarta Indonesia. BMC Health Serv Res. 2015;15(1):528. doi: 10.1186/s12913-015-1187-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Binti Mustafa Khan NJ, Binti Zulkipli ZN. COMPULSORY VACCINATION FOR CHILDREN IN MALAYSIA: LEGISLATION AND REALISATION. Yuridika. 2018;33(3):402. doi: 10.20473/ydk.v33i3.9826 [DOI] [Google Scholar]
- 27.Basharat S, Shaikh BT. Polio immunization in Pakistan: ethical issues and challenges. Public Health Rev. 2017;38(1):6. doi: 10.1186/s40985-017-0049-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Bin Atta B. Polio eradication : Our culture is the biggest impediment. https://www.dawn.com/news/1491880/polio-eradication-our-culture-is-the-biggest-impediment Published 2019. Accessed January 10, 2020.
- 29.Alshammari TM, Subaiea GM, Hussain T, Moin A, Yusuff KB. Parental perceptions, attitudes and acceptance of childhood immunization in Saudi Arabia: A cross sectional study. Vaccine. 2018;36(1):23–28. doi: 10.1016/j.vaccine.2017.11.050 [DOI] [PubMed] [Google Scholar]
- 30.Beech H Faith Politics on the Rise as Indonesian Islam Takes a Hard-Line Path. https://www.nytimes.com/2019/04/15/world/asia/indonesia-election-islam.html?login=email&auth=login-email Published 2019. Accessed July 30, 2019.
- 31.DHS. Indonesia Demographic and Health Survey 2017. https://dhsprogram.com/pubs/pdf/FR342/FR342.pdf Published 2017. Accessed January 10, 2020.
- 32.DHS. Pakistan. https://dhsprogram.com/pubs/pdf/FR354/FR354.pdf Published 2017. Accessed July 30, 2019.
- 33.DHS. Bangladesh. https://dhsprogram.com/pubs/pdf/FR311/FR311.pdf Published 2016. Accessed July 30, 2019.
- 34.DHS. India. https://dhsprogram.com/pubs/pdf/FR339/FR339.pdf Published 2017. Accessed January 10, 2020.
- 35.World Health Organization. Global Vaccine Action Plan: 2011–2020. Geneva, Switzerland: World Health Organization; 2011. [Google Scholar]
- 36.The Straights Times. Indonesia declares end to deadly Papua measles outbreak. https://www.straitstimes.com/asia/se-asia/indonesia-declares-end-to-deadly-papua-measles-outbreak Published 2018. Accessed March 27, 2020.
- 37.Padmawati RS, Heywood A, Sitaresmi MN, et al. Religious and community leaders’ acceptance of rotavirus vaccine introduction in Yogyakarta, Indonesia: a qualitative study. BMC Public Health. 2019;19(1):368. doi: 10.1186/s12889-019-6706-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Central Intelligence Agency. Indonesia. https://www.cia.gov/library/publications/the-world-factbook/geos/id.html Published 2020. Accessed June 9, 2020.