Abstract
Youth involved in the child welfare system (CWS) are disproportionally impacted by the negative effects of exposure to trauma. While efforts to develop trauma-informed CWSs are accelerating, little research is available about the effects of these efforts on system capacity to respond to the needs of youth exposed to trauma. No studies evaluate longer-term effects of these efforts. In 2011, Connecticut implemented CONCEPT, a multi-year initiative to enhance capacity of the state’s CWS to provide trauma-informed care. CONCEPT used a multi-component approach including workforce development, deployment of trauma screening procedures, policy change, improved access to evidence-based trauma-focused treatments, and focused evaluation of program effects. Changes in system capacity to deliver trauma-informed care were assessed using statewide stratified random samples of child welfare staff at three time points (Year 1: N = 223, Year 3: N = 231, Year 5: N = 188). Significant improvements across nearly all child welfare domains were observed during the first 3 years of implementation, demonstrating system-wide improvements in capacity to provide trauma-informed care. These gains were maintained through the final year of implementation, with continued improvements in ratings of collaboration between child welfare and behavioral health settings on trauma-related issues observed. Responses documented familiarity with and involvement in many of the CONCEPT activities and initiatives. Staff reported greater familiarity with efforts to increase access to specific evidence-based services (e.g., TF-CBT) or to enhance trauma-related policy and practice guidelines, but less familiarity with efforts to implement new practices (e.g., trauma screening) in various sectors. Staff also reflected on the contribution of these components to enhance system capacity for trauma-informed care.
Keywords: Trauma, Child welfare, Trauma-informed, Evidence-based, System reform
Introduction
The growing body of research on the harmful effects of childhood exposure to trauma continues to spur efforts to identify trauma as a major public health concern. Exposure to potentially traumatic events (PTEs) can comprise a range of events or conditions including experiencing or witnessing physical abuse, sexual assault, violence, and loss or separation from a caregiver, exposure to other forms of household dysfunction (e.g., parental mental illness, neglect), or exposure to other stressful situations or events (e.g., natural disaster, community violence, a serious accident). More than two-thirds of adolescents in the general population report experiencing one or more PTEs in their lifetime (Finkelhor, Turner, Shattuck, & Hamby, 2015). The negative outcomes associated with childhood trauma exposure are broad and long-term, including increased risk of mental illness, physical health problems, substance abuse, suicide, academic and occupational difficulties, and greater risk of involvement with the criminal justice system (Copeland et al., 2018; Felitti et al., 1998; Fox, Perez, Cass, Baglivio, & Epps, 2015).
The prevalence of trauma exposure is especially high in the child welfare system (CWS; Ko et al., 2008). Approximately 85% of youth involved in CWS have been exposed to at least one PTE (Miller, Green, Fettes, & Aarons, 2011), and these youth are significantly more likely to have experienced multiple forms of trauma than youth not involved in the CWS (Garcia, Gupta, Greeson, Thompson, & DeNard, 2017; Stambaugh et al., 2013). For many, the precipitating event leading to CWS contact involves a PTE (e.g., child abuse or neglect, and exposure to family violence), and system contact itself (e.g., the investigation or placement process) may be perceived as traumatic (Kisiel, Fehrenbach, Small, & Lyons, 2009). Research also indicates youth in the CWS experience higher rates of posttraumatic stress disorder (PTSD) symptoms and other mental health problems compared with the general population (Burns et al., 2004; Pecora, Jensen, Romanelli, Jackson, & Ortiz, 2009; Ai, Foster, Pecora, Delaney, & Rodriguez, 2013).
Increasing efforts to prevent and address childhood trauma exposure are being made across child-serving systems, including child welfare (Bunting et al., 2019; Child Welfare Information Gateway 2015; Ko et al., 2008). Variation exists with respect to how such an approach is operationalized, at least in part out of recognition that trauma-informed services should be individualized and tailored to the unique needs of the service population and of service providers (Berliner & Kolko, 2016; Murphy, Moore, Redd, & Malm, 2017).
Despite this variability, most systems change efforts include a core set of components including workforce development (e.g., training, supervision, and support), enhanced screening and identification, delivery of trauma-focused services, and organizational and environmental supports (e.g., service coordination, safe physical environment, written policies; Hanson & Lang, 2016). Workforce development efforts are necessary to educate child welfare staff about the impact of trauma on children and families and promote use of trauma-informed practices that reduce the effects of traumatic experiences or prevent further exposure (Conners-Burrow et al., 2013; Kramer, Sigel, Conners-Burrow, Savary, & Tempel, 2013). Programs and supports to address secondary traumatic stress are critical to reduce staff burnout and turnover (Sprang, Craig, & Clark, 2011). Screening for trauma at key points within the child welfare system ensures proper identification of children suffering negative effects of PTE exposure (Conradi, Wherry, & Kisiel, 2011; Lang et al., 2017) and can facilitate referral to evidence-based trauma-informed services, which is critical for the effective treatment of trauma-related behavioral health concerns (Berliner et al., 2015; Greer, Grasso, Cohen, & Webb, 2014).
A number of multi-year statewide and other large-scale efforts to create trauma-informed CWSs have been supported through federal grants from the Administration for Children and Families and SAMHSA’s National Child Traumatic Stress Network, including Massachusetts, Kentucky, Washington, and others (Akin, Strolin-Goltzman, & Collins-Camargo, 2017; Bartlett et al., 2018; Kerns et al., 2016; Murphy et al., 2017). Initial results from these initiatives show promise for development of trauma-informed CWSs, primarily with specific components of “trauma-informed systems” such as implementing trauma screening, improving access to trauma-focused evidence-based treatments (EBTs), workforce development, and policy change (Bartlett et al., 2018; Campbell, Lang, & Zorba, 2018; Crandal, Hazen, & Reutz, 2017; Kerns et al., 2016; Lang et al., 2017). However, little is still known about the long-term effects of a comprehensive system-wide trauma-informed approach on the broader CWS.
This study examines the first five years of a statewide initiative to create a trauma-informed CWS in Connecticut to determine the extent to which a multi-pronged approach results in systemic and sustained change. These analyses provide a follow-up to previous evaluation results of the Connecticut Collaborative on Effective Practices for Trauma (CONCEPT) in the third year of implementation (Lang, Campbell, Shanley, Crusto, & Connell, 2016). These prior analyses demonstrated significant improvements in measures of trauma-informed care and cross-system collaboration using a stratified random sample of child welfare workers. The current study extends this work to evaluate the extent to which improvements were sustained through year 5 of implementation and to assess staff perceptions of the effects of program components on changes at the system level.
Method
This section provides a brief overview program details, as well the methods used to evaluate system-wide change over the five-year implementation period.
State Context
Connecticut’s Department of Children and Families (DCF) is an integrated state agency charged with managing the child protection, child welfare, children’s behavioral health, juvenile justice (at the time of this initiative), and prevention-related needs of the State’s children and youth. DCF employs approximately 3,200 staff across 14 area offices in six regions as well as psychiatric residential treatment facilities, a children’s psychiatric hospital, and a secure juvenile detention facility (which subsequently closed). In 2017, DCF completed CPS investigations (including alternative response) for approximately 24,400 children and provided placement services for over 5,600 youth in foster care (U.S. Department of Health & Human Services, 2019a, 2019b). The state also contracted for outpatient care services for nearly 24,000 children and youth both in and out of DCF custody.
Beginning in the early 2000s, DCF made significant investments in dissemination and implementation of child-focused EBTs, in part to address needs identified as part of a federal consent decree in the late 1980s. As a result, prior to CONCEPT, DCF had already begun disseminating Trauma-Focused Cognitive Behavioral Therapy (TF-CBT; Cohen, Mannarino, & Deblinger, 2006; Lang, Franks, Epstein, Stover, & Oliver, 2015), an EBT for children experiencing symptoms following exposure to PTEs, and had piloted the NCTSN Child Welfare Trauma Training Toolkit (Trauma Toolkit; Child Welfare Collaborative Group & National Child Traumatic Stress Network, 2013). In addition, identification of trauma-informed care as one of the seven cross-cutting themes for DCF initiatives beginning in 2010 was instrumental to preparing the department for CONCEPT-related activities beginning in 2011.
CONCEPT Components
Below, we summarize the primary components implemented by CONCEPT during the first five years of the initiative. A timeline depicting implementation of program components during the five-year grant is provided in Fig. 1. Components generally fell into the following areas: (a) workforce development, (b) trauma screening, (c) secondary traumatic stress supports, (d) dissemination of trauma-focused EBTs, and (e) development of trauma-informed policy and practice guides. Additional details regarding program components are available in a prior publication (Lang et al., 2016).
Fig. 1.
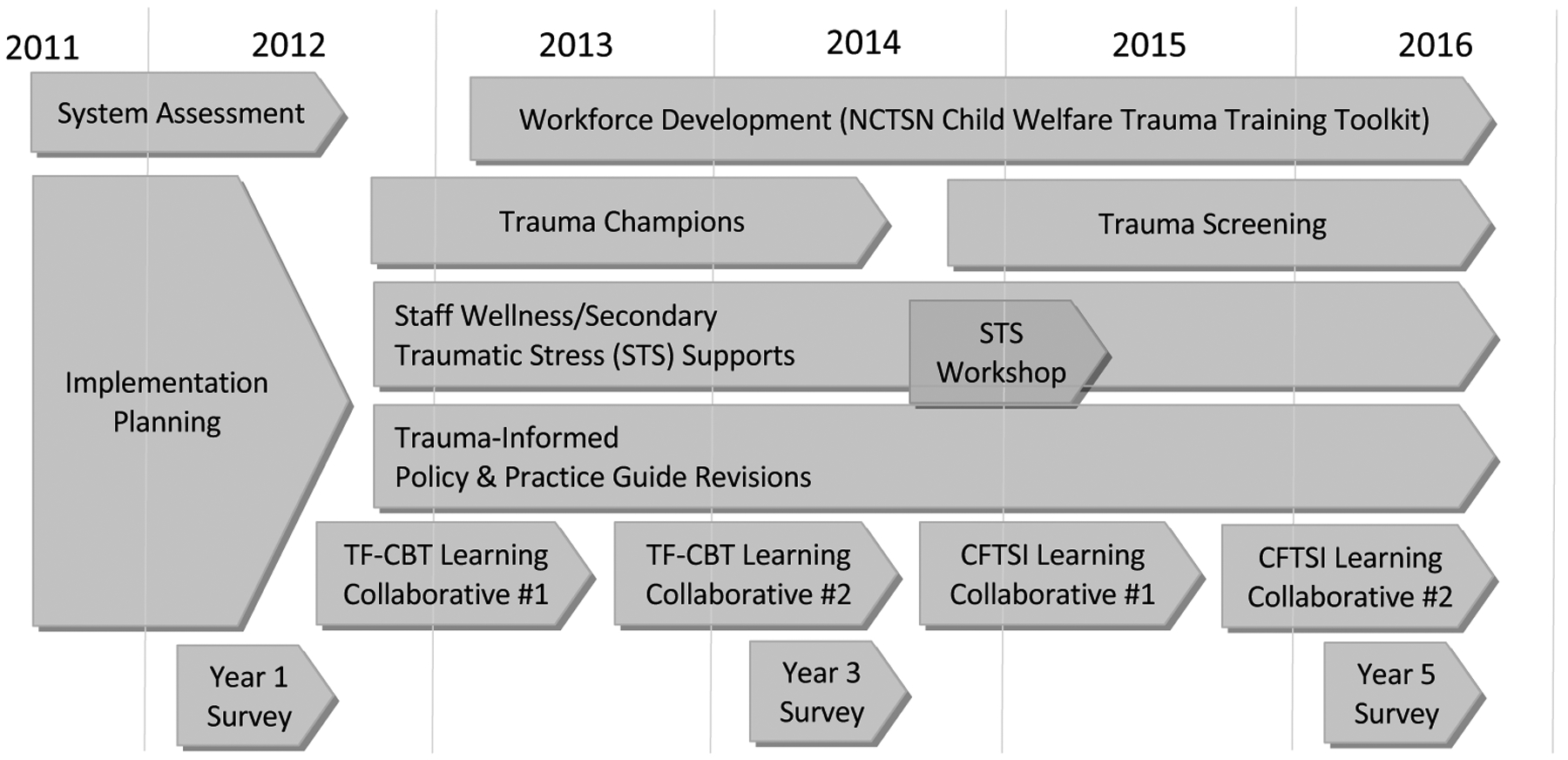
Timeline of key CONCEPT activities.
Workforce Development
Workforce development activities included two primary activities: (a) identification of a cohort of “trauma champions” to serve as liaisons to local area offices and function as early adopters of trauma-focused activities, and (b) implementation of trauma-focused pre- and in-service training, system-wide, for the child welfare workforce. A third area (dissemination of trauma-focused EBTs) also addressed training of the broader child welfare and behavioral health workforce and is described separately.
Trauma champions were identified in each area office and facility on a volunteer basis (typically two to four individuals) and reflective of frontline, supervisory, and managerial roles. Trauma champions met quarterly as a statewide group to identify trauma resources and plan methods for supporting trauma-informed practice within their local communities. Champions were to provide at least one monthly trauma-focused in-service activity through their area office. The trauma champion role was phased out in the third year after the initial goals of developing expertise and resources within each office were met, and as trauma-informed practices became more ingrained in daily child welfare operations. Some of these roles were also assumed by other functions (e.g., area office wellness groups).
The NCTSN Trauma Toolkit (2013) was implemented as a core component of pre- and in-service trauma training for child welfare staff. The Trauma Toolkit was conducted as a two-day session designed to improve knowledge about child trauma and promote trauma-informed practice change across organizational levels within the child welfare workforce. Training was provided to 487 managers and supervisors across 23 cohorts during the spring of 2013 and to 1164 caseworkers and clinical staff across 53 cohorts during the fall of 2013. The Trauma Toolkit was added as an ongoing pre-service training requirement for all new hires beginning in 2014.
Trauma Screening
Preliminary efforts to disseminate a screening tool, described in a previous paper (Lang et al., 2016), involved developing and testing a brief tool to document exposure to PTEs and associated traumatic stress reactions with a small cohort of child welfare workers. In year 3 of the grant, the CONCEPT team developed and validated an empirically derived brief screening tool—the Child Trauma Screen (CTS; Lang & Connell, 2017, 2018). In year 4, the screening tool was integrated into the Multidisciplinary Evaluation (MDE) for all children ages seven and up who were placed into DCF care, and a pilot implementation of the tool was conducted in an urban area office to assess its utilization by caseworkers for their ongoing cases (Lang et al., 2017). A total of 1,894 children were screened with the child trauma screen from its initial implementation through the fall of 2018. Subsequent to the period reported in this paper, a young child version (caregiver report for ages three to six years) was developed that has been integrated into the MDE process.
Secondary Traumatic Stress Supports
Funds were allocated for use by the DCF Area Offices, facilities, and Central Office to support staff wellness and to mitigate secondary traumatic stress. Area offices were given an annual budget (ranging from $2,500 to $5,000, roughly proportional to the number of employees in the office) to be used to support approved health, wellness, and staff recognition materials or activities (e.g., support for STS training or presentation, development of STS-focused informational materials, creation of a “staff wellness” room, and facilitation of “staff wellness fairs”). In year 4, funds were used to conduct a statewide two-day training workshop for DCF staff and support regionally based follow-up consultation on vicarious trauma initiatives that was conducted by a nationally recognized expert.
Trauma-Informed Policy & Practice Guide Revisions
Based on integration of trauma-informed care to the agency mission, the DCF Commissioner mandated departmental review of all policies (i.e., legislative and administrative directives) and practice guides (i.e., procedure and resource manuals related to program and policy areas) to integrate trauma-informed guidance. CONCEPT facilitated a policy workgroup, including relevant DCF staff, who conducted a systematic review and revision of 37 child welfare policies and practice manuals (of 44 overarching policy areas—some areas such as fiscal or engineering services were not reviewed), as well as an additional 34 policies related to the state’s juvenile training school. The policy workgroup developed a policy review tool based on Chadwick’s essential elements of a trauma-informed system (Chadwick Trauma-Informed Systems Project, 2013). Campbell et al. (2018) provide a more thorough overview of the policy review and revision process, as well as the results with respect to promulgation of new policy and procedure language within the department. Within DCF, recommendations for changes were made and accepted for 22 policies or practice guides reviewed by the policy workgroup. In addition, the workgroup produced a guide for trauma-informed practices to provide information and additional resources about trauma-informed child welfare practice to support sustainability of ongoing policy and practice reviews, which were subsequently reviewed and approved by the DCF Policy Unit and the DCF Commissioner and were disseminated to agency staff.
EBT Dissemination
CONCEPT implemented a series of four community-based multi-agency learning collaborative cohorts to disseminate two trauma-focused EBTs: TF-CBT (Cohen et al., 2006) and Child and Family Traumatic Stress Intervention (CFTSI; Berkowitz, Stover, & Marans, 2011). Learning collaboratives were based on the Breakthrough Series Collaborative quality improvement methodology (Ebert, Amaya-Jackson, Markiewicz, Kisiel, & Fairbank, 2012; Kilo, 1998) and brought together four to six local community teams comprised of staff from selected community-based behavioral health agencies reflecting clinical, supervisory, and managerial staff to support dissemination of each service model. Consistent with adaptation of the learning collaborative model developed by Saunders and Hanson (2014), CONCEPT learning collaborative teams also included staff from the local DCF area office for each agency team to promote cross-system collaboration and to improve access to trauma-informed care for children in the CWS.
A competitive RFQ process was used to select agencies for participation in EBT learning collaboratives. Thirteen community-based outpatient behavioral health providers (seven to eight participants per site), their DCF area office partners (six participants per site), and a family partner (one to two per site) participated in two year-long learning collaborative cohorts to implement TF-CBT, bringing the total number of agencies trained in the model to more than 30 across the state. In addition, 42 clinicians in seven agencies were trained to provide CFTSI as a preventive intervention for children experiencing recent trauma exposure. Selected clinics were given a small stipend ($12,000/year) to offset costs for participating in learning collaborative activities. During the grant, over 2,000 children were referred to TF-CBT and over 200 received CFTSI through CONCEPT providers.
System-Level Evaluation Procedures
Lang et al. (2016) described evaluation results of agency-wide change in DCF staff perception of the agency’s capacity for trauma-informed care during the first three years of CONCEPT. The present study extends the evaluation of system-level change through the fifth year of the initiative. System-wide random samples reflecting DCF staff, stratified by area office or facility (e.g., central office, residential facility setting), were identified for each of the survey periods (years 1, 3, and 5). Samples were selected from rosters reflecting all agency staff in leadership, supervisory, and caseworker/clinical roles. The sampling rate was approximately 20% of all eligible DCF personnel (493 in year 1, 497 in year 3, 553 in year 5). Samples were intended to represent contemporary workforce makeup in each year of the grant; the primary interest was to reflect system-wide changes in perceptions, rather than individual-level change. Thus, individuals were not enrolled longitudinally and responses were not linked over time. Staff were excluded if they currently were active in learning collaborative activities to minimize survey burden among DCF staff. Selected staff were invited to participate in the online survey via email and were informed that survey responses were anonymous. The email included a participant-specific link to the consent and staff survey using Qualtrics web-based survey software (Qualtrics, 2016). Individuals completing the survey were entered into weekly random drawings to receive a $20 gift card in exchange for their participation and received periodic (e.g., weekly) prompts via email to encourage participation over a five- to seven-week period of data collection each year. All CONCEPT evaluation activities were reviewed and approved by Yale University School of Medicine and Connecticut Department of Children and Families Institutional Review Boards.
Participants
Response rates for the three survey periods were as follows: year 1 (n = 233, 45.2% response rate), year 2 (n = 231, 46.5% response rate), and year 5 (n = 185, 33.5% response rate). Table 1 summarizes and compares survey respondent characteristics across the three waves of survey administration. Survey participant characteristics generally have remained consistent for each year of the survey. This may be due, in part, to relatively low rates of turnover in Connecticut’s child welfare workforce, which has been reported at 8% or less annually compared with national estimates between 23 and 60% (Strand, Spath, & Bosco-Ruggiero, 2010). The primary difference among sample waves was in the mean number of years respondents had worked in the child welfare field, increasing from an average of 13.5 years (SD = 6.7) to 15.5 years (SD = 8.4) in year 5 (F2,636 = −3.96, p = .02). Differences in representation of roles over time did not reach statistical significance, with approximately 3 to 5 percent of participants in director/administrator roles, 25 to 35 percent in manager or supervisory roles, 52 to 58 percent in caseworker or clinical roles, and 9 to 16 percent in other roles such as case aide, consultant, or medical service roles. Respondent child welfare sector representation (e.g., intake, ongoing services, and foster and adoptive services), caseload, education, and demographic characteristics (i.e., gender and race or ethnicity) all remained stable over survey administrations.
Table 1.
Respondent characteristics by year
| CWS staff characteristics | Time 1 (N = 223) | Time 3 (N = 231) | Time 5 (N = 188) | Comparison | |||
|---|---|---|---|---|---|---|---|
| Mean | SD | Mean | SD | Mean | SD | ||
| Mean years in child welfare | 13.5a | 6.7 | 14.8a,b | 6.9 | 15.5b | 8.4 | F2,636 = −3.96, p = .02 |
| Mean caseload (if applicable) | 16.0 | 16.3 | 15.8 | 18.1 | 15.7 | 19.3 | F2,443 = 0.01, p = .99 |
| N | % | N | % | N | % | ||
| Agency role | |||||||
| Director/Administrator | 6 | 2.7 | 7 | 3.0 | 10 | 5.3 | X2(6) = 11.87, p = .07 |
| Manager/Supervisor | 62 | 27.8 | 56 | 24.2 | 65 | 34.6 | |
| Caseworker/Clinical staff | 129 | 57.8 | 131 | 56.7 | 97 | 51.6 | |
| Other | 26 | 11.7 | 37 | 16.0 | 16 | 8.5 | |
| Child welfare sector (check all) | |||||||
| Intake & disposition (CPS) | 35 | 15.7 | 49 | 21.2 | 35 | 18.6 | X2(2) = 2.29, p = .32 |
| Intake & disposition (FAR) | 18 | 8.1 | 29 | 12.6 | 25 | 13.3 | X2(2) = 3.45, p = .18 |
| Ongoing services | 87 | 39.0 | 81 | 35.1 | 75 | 39.9 | X2(2) = 1.22, p = .54 |
| Area resource group | 16 | 7.2 | 14 | 6.1 | 12 | 6.4 | X2(2) = 0.24, p = .89 |
| Foster care and adoption services | 16 | 7.2 | 26 | 11.3 | 12 | 6.4 | X2(2) = 3.87, p = .14 |
| Administration & Quality improvement | 13 | 5.8 | 13 | 5.6 | 14 | 7.5 | X2(2) = 0.68, p = .71 |
| Child welfare facility | 21 | 9.4 | 17 | 7.4 | 25 | 13.3 | X2(2) = 4.19, p = .12 |
| Other | 42 | 18.8 | 39 | 16.9 | 26 | 13.8 | X2(2) = 1.85, p = .40 |
| Education | |||||||
| Doctoral (MD, Ph.D.) | 7 | 3.1 | 4 | 1.7 | 4 | 2.2 | X2(6) = 11.15, p = .08 |
| Licensed masters | 30 | 13.5 | 31 | 13.4 | 43 | 23.2 | |
| Masters | 79 | 35.4 | 83 | 35.9 | 52 | 28.1 | |
| Bachelors or lower | 107 | 48.0 | 113 | 48.9 | 86 | 46.5 | |
| Gender (Female) | 171 | 77.0 | 178 | 78.4 | 138 | 76.8 | X2(2) = 0.84, p = .66 |
| Race/Ethnicity | |||||||
| African American | 53 | 24.4 | 47 | 20.5 | 39 | 21.2 | X2(6) = 3.23, p = .78 |
| Caucasian | 124 | 57.1 | 129 | 56.3 | 111 | 60.3 | |
| Hispanic | 25 | 11.5 | 36 | 15.7 | 21 | 11.4 | |
| Other | 15 | 6.9 | 17 | 7.4 | 13 | 7.1 | |
CPS, child protective services; FAR, family assessment response.
Cells with different subscripts within row are statistically significantly different from one another (p < .05) based on pairwise post hoc comparisons.
Measures
In years 1 and 3, a 90-item version of the Trauma System Readiness Tool (TSRT; Hendricks, Conradi, & Wilson, 2011; Lang et al., 2016) was used to assess staff perceptions of individual and system understanding of and capacity to use trauma-informed principles and practices to support children, families, and the child welfare workforce. The TSRT was initially developed by the Chadwick Trauma-Informed Systems Project (CTISP); Sullivan, Preisler, Ake, Potter, and Beck (2012) developed an adaptation of the TSRT that reduced items, streamlined the response set, and maintained coverage of key domains. To reduce survey burden among DCF staff, a briefer version of the TSRT was developed for the year 5 administration, using respondent data from the first two administrations to inform the revision. Specifically, factor analyses were conducted using data from year 1, and the four to six items with the highest factor loadings were used to generate a briefer version of that subscale. Resulting scales were then re-assessed using data from year 3 to determine whether the items had acceptable reliability and were correlated with the full subscale scores. In addition, we assessed replicability of full-scale longitudinal effects using the briefer survey format. The revised results mirrored those of our previous publication (Lang et al., 2016), supporting use of the TSRT short form (TSRT-SF). The revised version paralleled the constructs of the initial TSRT, and as items were identical to previous administrations, we were able to assess change over the five-year grant period using the revised instrument. As with the original instrument, items were rated on a 5-point Likert-type scale from “Strongly Disagree” to “Strongly Agree.” A mean score for each domain was created, with higher scores reflecting more favorable ratings of individual or agency-level capacity for that survey scales. Table 2 summarizes TSRT-SF structure and reliability.
Table 2.
Trauma system readiness tool—short form (TSRT-SF) items and reliability (years 1, 3, and 5)
| TSRT-SF Domain (Item Count) | Scale Description | Cronbach’s α | ||
|---|---|---|---|---|
| Yr 1 | Yr 3 | Yr 5 | ||
| 1. Trauma training exposure (5) | Personal exposure to key aspects of the effects of trauma on children | .92 | .93 | .94 |
| 2. Individual trauma knowledge and practice (3) | Personal understanding and use of trauma-related principles and practices | .82 | .86 | .84 |
| 3. Staff trauma knowledge (8) | Agency-level staff understanding of trauma-related principles and practices | .93 | .93 | .93 |
| 4. Staff trauma practice (7) | Agency-level staff use of trauma-related principles and practices | .90 | .93 | .93 |
| 5. Trauma supervision and support (3) | Agency-level supports to address trauma among children and families as well as secondary traumatic stress | .86 | .86 | .83 |
| 6. Staff supports child relationships (5) | Staff efforts to support for maintenance of key child relationships | .87 | .87 | .89 |
| 7. Birth families trauma support (4) | Staff use of trauma-informed practices with children’s birth families | .87 | .85 | .84 |
| 8. Resource family trauma support (5) | Staff use of trauma-informed practices with resource caregivers | .91 | .90 | .90 |
| 9. Staff address child psychological safety (3) | Staff practices to address psychological safety | .87 | .90 | .86 |
| 10. Agency trauma assessment (4) | Accessibility and trauma-focused content of behavioral assessments for children and youth in the area | .94 | .94 | .95 |
| 11. Access to trauma-informed services (2) | Staff- and community-level access to trauma-informed services and supports for children in their caseloads | .93 | .92 | .89 |
| 12. Local agency collaboration (general; 3) | Collaboration around general practice | .84 | .86 | .88 |
| 13. Local agency collaboration (trauma; 3) | Joint commitment to providing trauma-informed care | .82 | .81 | .84 |
For year 5 administration, an additional set of questions were asked of participants reflecting awareness of and participation in 12 key CONCEPT components, as well as staff perceptions of the contribution of each component to the overall rating of changes in system capacity for trauma-informed care associated with the grant initiative. Awareness was rated on a 3-point scale (0-not aware, 1-somewhat aware, and 2-aware). Level of involvement in activities was rated on a 5-point scale (0 = not aware, 1 = somewhat aware, 2 = aware). Level of involvement in activities was rated on a 4-point scale (0 = not aware/not at all, 1 = a little bit, 2 = somewhat, 3 = quite a bit, and 4 = very much); only those elements providing opportunity for involvement were assessed for this item. Finally, staff rated the overall extent to which they perceived the agency had become “more trauma-informed” over the five-year grant (0-not at all to 4-very much) and the extent to which each of the 12 program components had contributed to changes in system-wide capacity for trauma-informed care using the same scale.
Data Analysis
Changes in agency staff perceptions of individual and system-level readiness and capacity to deliver trauma-informed care were assessed using regression with robust standard errors (Verardi & Croux, 2009) to account for clustering by area office or facility; all analyses were conducted using Stata 14.2 (StataCorp LLC, 2015). Multilevel modeling (MLM) was considered but no office-level (level 2) effects were included in models and intra-class coefficients by area office were typically very low (i.e., <.001). All models were replicated using MLM, and results were not demonstrably different (available upon request). For consistency with previous analyses of years 1 and 3 (Lang et al., 2016), regression results using robust standard errors are presented in Table 3. All models controlled for respondent report of years in child welfare field and role (i.e., manager/supervisor vs. frontline staff/other). The overall F-test for time assesses the linear effect of time from years 1 to 5, and separate contrasts were assessed for the change from years 1 to 3 and from years 3 to 5. Unstandardized betas (B) for each time comparison reflect the change in TSRT-SF domain scores after controlling for years in the field and respondent role.
Table 3.
Changes in readiness and capacity for trauma-informed care in years 1, 3, and 5 of CONCEPT implementation
| TSRT-SF domain | Year 1 | Year 3 | Year 5 | Time model | Time 1–2 Effect [95% CI] | Time 2–3 Effect [95% CI] | |||
|---|---|---|---|---|---|---|---|---|---|
| M | SE | M | SE | M | SE | ||||
| 1. Trauma training exposure | 3.80a | 0.06 | 4.19b | 0.04 | 4.15b | 0.06 | F = 12.66, p < .001 | 0.39 [0.25–0.53] | −0.04 [−0.19–0.12] |
| 2. Individual trauma knowledge and practice | 3.47a | 0.05 | 3.89b | 0.05 | 4.02b | 0.05 | F = 20.56, p < .001 | 0.42 [0.27–0.57] | 0.14 [−0.02–0.29] |
| 3. Staff trauma knowledge | 3.67a | 0.04 | 3.99b | 0.05 | 4.02b | 0.06 | F = 15.37, p < .001 | 0.32 [0.17–0.48] | 0.02 [−0.14–0.19] |
| 4. Staff trauma practice | 3.62a | 0.05 | 3.81b | 0.04 | 3.91b | 0.03 | F = 5.00, p = .007 | 0.19 [0.04–0.34] | 0.09 [−0.04–0.22] |
| 5. Trauma supervision and support | 2.48a | 0.08 | 3.04b | 0.07 | 3.08b | 0.06 | F = 10.88, p < .001 | 0.57 [0.33–0.80] | 0.03 [−0.15–0.22] |
| 6. Staff supports child relationships | 3.57a | 0.05 | 3.82b | 0.05 | 3.85b | 0.04 | F = 15.65, p < .001 | 0.24 [0.08–0.41] | 0.03 [−0.11–0.17] |
| 7. Birth families trauma support | 2.76a | 0.06 | 3.30b | 0.06 | 3.30b | 0.05 | F = 37.71, p < .001 | 0.54 [0.36–0.72] | 0.00 [−0.21–0.21] |
| 8. Resource family trauma support | 2.96a | 0.05 | 3.47b | 0.04 | 3.53b | 0.05 | F = 15.67, p < .001 | 0.52 [0.38–0.66] | 0.06 [−0.06–0.18] |
| 9. Staff address child psychological safety | 3.60a | 0.06 | 3.73a,b | 0.05 | 3.84b | 0.05 | F = 5.22, p = .006 | 0.13 [−0.04–0.30] | 0.11 [−0.06–0.29] |
| 10. Agency trauma assessment | 3.28a | 0.07 | 3.68b | 0.06 | 3.69b | 0.05 | F = 7.61, p = .001 | 0.39 [0.20–0.58] | 0.02 [−0.15–0.18] |
| 11. Access to trauma-informed services | 2.47a | 0.09 | 3.00b | 0.06 | 3.15b | 0.08 | F = 7.06, p = .001 | 0.53 [0.29–0.76] | 0.14 [−0.01–0.30] |
| 12. Local agency collaboration (general) | 3.45a | 0.03 | 3.48a | 0.04 | 3.62b | 0.05 | F = 2.04, p = .13 | 0.02 [−0.10–0.14] | 0.14 [0.01–0.27] |
| 13. Local agency collaboration (trauma) | 3.33a | 0.06 | 3.65b | 0.04 | 3.83c | 0.05 | F = 16.02, p < .001 | 0.32 [0.15–0.50] | 0.18 [0.03–0.33] |
Cells with different superscripts (within row) differ statistically from one another, p < .05.
Time model refers to overall linear effect of time assessed via regression with robust standard errors to adjust for clustering by area office/facility. All models controlled for years in child welfare field and role (manager/director and clinician/frontline staff positions); df reflects number of setting clusters (4,18).
Results
Baseline ratings of individual and agency capacity for trauma-informed care were largely positive, ranging from 3.3 to 3.8 for most domains. The top-rated domains reflected trauma training exposure (M = 3.80), staff knowledge (M = 3.67), and staff practice domains (M = 3.62). The lowest rated domains, each rated below three on the 5-point scale, were trauma supervision and support (M = 2.48), access to trauma-informed services (M = 2.487), and support for birth family trauma-related needs (M = 2.76).
Overall model effects demonstrated significant improvements in ratings of capacity for trauma-informed care across each of the TSRT-SF domains. Examination of the separate time increments (years 1 to 3 and years 3 to 5) reveals a generally consistent pattern of significant increase during the first half of the CONCEPT grant, followed by a period of maintenance for the second half of the grant. Among the strongest trends following this pattern were increases noted in two of the areas initially rated least favorably. The improvement in trauma supervision and support, for example, was quite large at year 3 (B = 0.57) and then remained stable from years 3 to 5 (B = 0.03). This pattern was also observed for birth family trauma supports, access to trauma-informed services, and resource family trauma supports. Most other scales showed more modest increases (typically in the 0.24 to 0.42 range for the first half and largely stable, non-significant trends during the second half of the initiative.
A few exceptions to this pattern were observed. Two domains demonstrated a delayed effect in observed change. Ratings of staff capacity to address child psychological safety did not increase significantly across successive waves (years 1 to 3: B = 0.13, years 3 to 5: B = 0.11), but the overall trend revealed a significant increase in ratings by year 5 (p = .001). Ratings of general collaboration with local community-based agencies did not increase from years 1 to 3 (B = 0.02) but did increase significantly during the latter half of the initiative (B = 0.14). Finally, trauma-focused collaboration with local community-based agencies continued to increase across each successive wave of assessment (years 1 to 3: B = 0.32, years 3 to 5: B = 0.18).
Next, staff in the final wave of assessment were asked to rate awareness, involvement, and contribution of 12 CONCEPT activities toward the overall rating of system capacity for trauma-informed care. Most staff (at least 50%) reported some level of familiarity with each of the program components assessed (see Fig. 2). Nearly all staff (greater than 90%) reported some level of familiarity with four of the components, including availability of trauma-focused treatments, integration of trauma with policy and practice guides, regional wellness committee initiatives, and integration of trauma with the DCF mission. Similar levels were also reported for the Trauma Toolkit and TF-CBT learning collaborative activities. Three areas rated the lowest with respect to awareness were the CFTSI learning collaborative, deployment of the trauma screen in area offices, and inclusion of the trauma screen in MDE reports. Each of these activities took place during the latter half of the CONCEPT initiative and involved fewer total staff who participated directly in each.
Fig. 2.
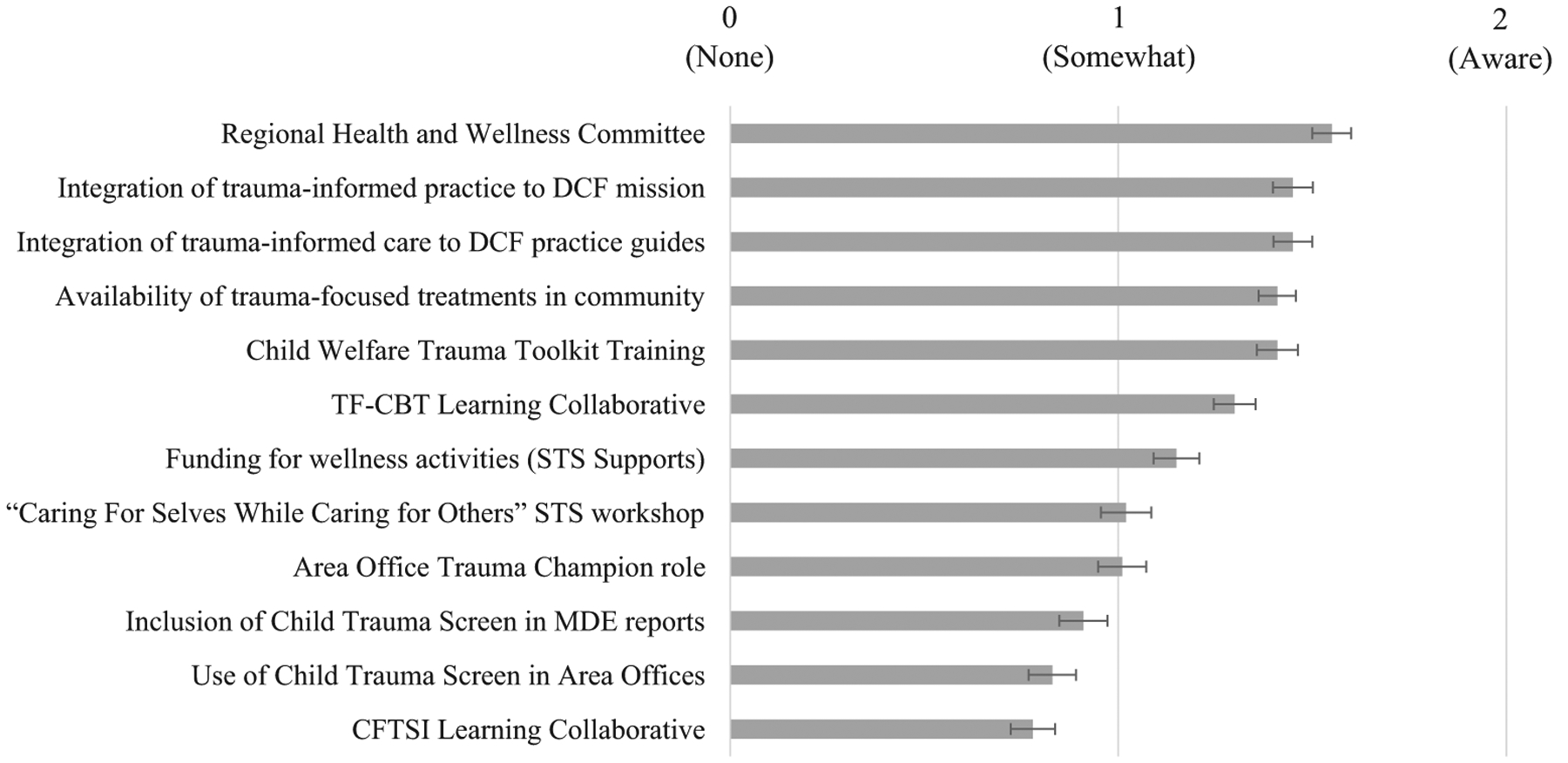
Staff awareness of CONCEPT activities. Note. Error bars represent standard error of the mean.
Figure 3 depicts staff involvement in those activities with which they were familiar. A majority of staff (greater than 50%) reported some level of involvement with only three activities: regional health and wellness initiatives and Trauma Toolkit both had greater than 60 percent of respondents indicate some level of involvement, and the TF-CBT learning collaborative exceeded 50 percent, though this likely reflects knowledge of the collaboratives or referral of cases to these teams, rather than direct involvement for most respondents. Level of involvement was generally lower in each of the other CONCEPT activities.
Fig. 3.
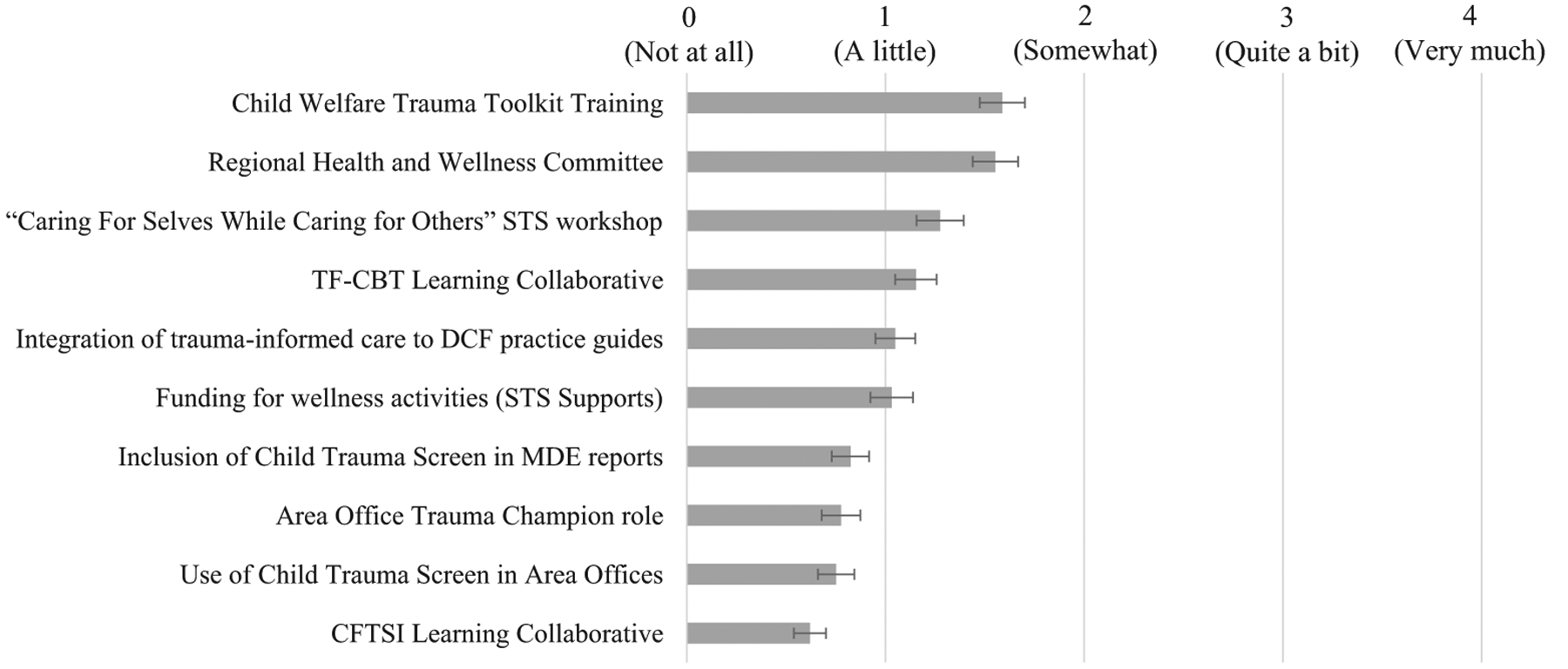
Staff involvement in CONCEPT activities. Note. Error bars represent standard error of the mean.
Finally, staff rated their perceptions of the extent to which DCF had become a “more trauma-informed” agency over the previous five years of grant activities and the degree to which they perceived each of the core components had contributed to that change in capacity (see Fig. 4). All staff noted at least some level of change in capacity: a little (6.7%), somewhat (27.4%), quite a bit (47.0%), and very much (18.9%). The three mostly favorably rated contributors included the increased availability of trauma-focused treatments in the community, integration of trauma-informed care into DCF practice guides, and integration of trauma-informed practice to the DCF mission. Next most favorably rated contributors include Trauma Toolkit training, regional health and wellness initiatives, and the TF-CBT learning collaboratives. Lowest rated activities contributing to changes in system capacity included the CFTSI learning collaboratives, use of the trauma screen (personally or within the MDE), and the STS workshop and consultation process.
Fig. 4.
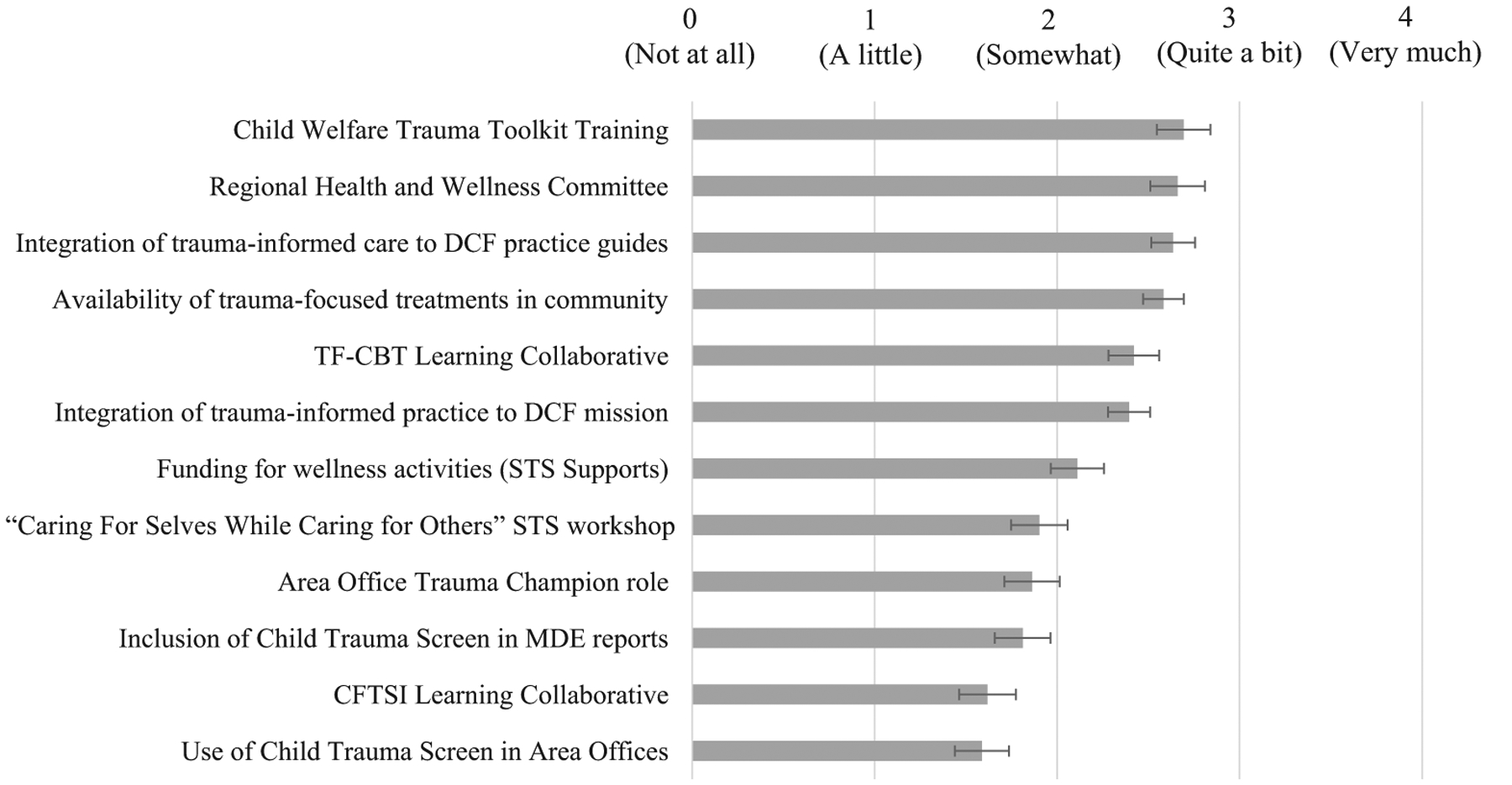
Staff perceived contribution of CONCEPT activities to system-wide trauma-informed capacity. Note. Error bars represent standard error of the mean.
Discussion
Federal agencies have provided significant resource support to advance the cause of trauma-informed child welfare systems. These include funding of three “trauma-grant” cohorts involving more than 15 different state, tribal, or community-based initiatives through the Children’s Bureau of the Administration for Children and Families, as well as several dozen grants through SAMHSA’s NCTSN to develop and disseminate trauma-informed services and supports in states and communities across the United States. Although definitions of what comprises a trauma-informed CWS vary across agencies and grantees, a consistent theme of these initiatives is to prevent further trauma exposure and to identify and support children exposed to trauma in all areas of intersection with the CWS. This type of change effort usually involves a multi-pronged approach consisting of formal workforce development and training efforts (including efforts to reduce STS or vicarious trauma reactions), changes in agency policy and practice, deployment of screening and assessment tools to identify children in need of trauma-informed care, and dissemination of trauma-focused EBTs (Hanson & Lang, 2016; Ko et al., 2008; SAMHSA 2014).
Despite the growing interest and funding for trauma-informed CWSs, little is known about the long-term impact on system capacity for trauma-informed care. Our study addresses this research gap and provides evidence of the potential for system-wide efforts to increase CWS capacity to improve trauma-informed care for children, families, and the CWS workforce. To our knowledge, this is the first such study to examine these types of effects over a sustained follow-up period using representative samples within a statewide CWS. The results build on earlier findings reported in Lang et al. (2016). With continued implementation of program components, as well as the addition of new initiatives, our results reveal sustainment of initial gains in perceived capacity, but little additional gains across assessed dimensions. The marked gains that emerged during the initial phase of program implementation largely coincided with system-wide efforts at workforce development and dissemination of a well-known EBT to a wide array of agencies working in concert with local DCF area offices, while later activities may have served to maintain those activities or deploy components that were less widely visible. Screening deployment, for example, involved a small number of contracted MDE providers, rather than CWS staff; the second round of EBT learning collaboratives did not involve DCF staff as central members of learning collaborative teams; and Trauma Toolkit trainings were conducted primarily as pre-service training with new employees, rather than as part of a statewide workforce training experience. Yet, despite the potential decreased visibility of these efforts for the agency workforce, ratings of system capacity continued to maintain early gains. Further, three domains continued to show improvements—ratings of staff attendance to child psychological safety needs and ratings of both general and trauma-specific collaboration with local community-based agencies.
Staff ratings of awareness and involvement with CONCEPT components at the conclusion of the 5th year revealed significant variability across activities. A majority of staff reported at least some level awareness with each component, though involvement and perceived impact of specific components were less so for activities that may have offered less opportunity for direct involvement (e.g., activities involving training of other systems such as CFTSI learning collaboratives, or implementation of tools in other sectors such as the MDE child trauma screening). Despite limited ratings of direct involvement in many CONCEPT components, child welfare staff did report positive improvements on the overall capacity of the system with respect to providing trauma-informed care to children, families, and the child welfare workforce. Key drivers of these gains, reflected in ratings of each component, parallel reports of awareness and involvement.
Two surprising findings emerged with respect to the awareness and perceived contribution of core program components. First, limited awareness of child trauma screening tool implementation within the MDE for cases opening to child welfare was not anticipated. Implementation of trauma screening is viewed as a critical component of trauma-informed care within child-serving systems (Conradi et al., 2011; Hanson & Lang, 2016; Ko et al., 2008). Trauma screening is important as a means of identifying youth at risk of an adverse reaction to PTE exposure, as well as for identifying youth in need of referral for additional assessment or access to trauma-informed services. Limited awareness, in this case, may reflect decisions about where to deploy screening within the CWS. The initial strategy proposed by CONCEPT was to implement a child trauma screen by caseworkers within the intake and disposition sector (e.g., for appropriate youth coming into contact with CPS or family assessment). Concern was expressed by CWS leadership, however, that integration of additional screening, coupled with other practice model requirements, would place significant burden on CPS workers. As a result, trauma screening was implemented within the MDE process for children removed from care because (a) cases reaching the MDE were likely to have higher levels of need than cases at intake, which may be screened out or not require departmental involvement, (b) the MDE had an established framework for integrating the trauma screen within an existing assessment and case planning process for ongoing cases, and (c) these youth would have caseworker involvement to support appropriate referrals for subsequent assessment and treatment. CONCEPT also piloted use of the trauma screen among area office caseworkers in one location, but the practice was not implemented statewide. Limited awareness, therefore, may reflect that many of the survey respondents represented sectors (e.g., intake and disposition, area resource groups, and foster care and adoption) that did not directly engage with the MDE at the time of case opening.
An additional factor related to awareness and perceived impact may be the age range of children eligible for trauma screening. We have detailed the development and considerations of trauma screening in previous publications (Lang & Connell, 2017, 2018). One challenge is the limited number of validated tools that assess both trauma exposure and trauma-related stress symptoms, particularly for young children. As a result, CONCEPT developed and validated the Child Trauma Screen, beginning first with a tool that could be used by parents and youth over age six (age seven for child self-report). Subsequent development extended a parallel instrument down to age 3 based on caregiver report, but that tool was not implemented prior to year 5 of CONCEPT. It may be, therefore, that ongoing expansion of trauma screening practices provides greater opportunity for awareness and utilization of screening results to inform case practice.
The second area that was surprising was limited perceived impact of STS supports, including the statewide STS workshop and post-workshop consultation, as well as (to a lesser extent) funding to support wellness activities. Support for workforce experiences of STS was not initially a part of the CONCEPT work plan, but was added in response to feedback from participants in surveys and focus group activities conducted during the initial planning year of the initiative. Although offered statewide, the two-day STS workshop had limited capacity, involving key representatives from each region, with the primary emphasis on providing a process for developing regionally tailored response to STS-related needs and post-workshop consultation on this development and implementation. It may be that these activities varied with respect to regional implementation, attenuating the perceived impact of these activities. Notably, ratings of overall support for the workforce through trauma-related supervision and other activities did show significant increase during the first half of CONCEPT, which may be the result of other activities (e.g., Trauma Toolkit implementation with managers and supervisors).
Limitations
A number of limitations of this evaluation are important to identify. As was indicated previously, the response rate among child welfare staff was between 33 and 50 percent across the three waves of data collection, raising the potential of a biased response pattern (i.e., that respondents held different views than those who chose not to complete a survey). Our previous analyses demonstrated that respondents reflected the overall workforce makeup with respect to sector and role (Lang et al., 2016), and our present results demonstrate that the makeup of the participant sample has remained relatively stable over each of the reporting years, minimizing this potential concern. Another limitation is the reliance on self-report to assess perceptions of trauma-related individual and system capacity, as well as ratings of the particular CONCEPT components and their impact on system capacity. It is critical that future research incorporates additional independent indicators of knowledge or practice change associated with trauma-informed care components. These might be reflected, for example, in assessment of specific information learned through workforce development initiatives; changes in rates of referral for screening, assessment, or treatment; and independent reviews of supervisor practices. It is important to note that separate evaluation activities were linked to many CONCEPT components, and further research on initiative effects at the child and workforce level is underway. We also recognize that more research is needed to develop valid and reliable indicators of trauma-informed care within child-serving systems.
Other limitations are related to the overall study design. We are unable to attribute causal effects of CONCEPT components to observed changes in trauma-related system capacity. All activities were implemented system-wide, rather than in the context of a randomized or phased rollout design, so a rigorous comparison condition was not available. Despite this limitation, however, our use of a stratified random sample reflecting the child welfare workforce at key points of implementation does provide greater confidence than reliance on a convenience sample of respondents. This limitation is relatively common in evaluating system-level initiatives within the child welfare system (Bunting et al., 2019), whether due to concerns about with-holding resources to those in need or concern about potential spillover of exposure to information and resources when deployed in communities across a state system.
We also recognize that results may not fully generalize to other child welfare settings. As we discussed in a previous publication, the Connecticut workforce is very stable (with more than 13 to 15 years in the field, on average), relative to other state child welfare systems. It may be that efforts to develop capacity for trauma-informed care face additional barriers in systems marked by higher rates of turnover. In addition, Connecticut’s child welfare system is relatively centralized, even though area offices and regions provide some local control. States with stronger county or regional administrative structures may experience greater variability in the impact of initiatives to change overall system culture and practice. Further, because Connecticut’s child welfare system provides some funding for outpatient children’s services, implementation may have benefitted from relationships that already existed between child welfare offices and behavioral health providers. Future research should continue to examine the structural and administrative factors that impact capacity-building efforts to increase access to trauma-informed care within child- and family-serving systems.
Conclusions and Recommendations
Beyond the quantitative data demonstrating system improvements, we also have heard from numerous colleagues and staff within the CWS that there has been a noticeable cultural shift toward embracing trauma-informed care as a fundamental value since the project began. Example of this can be seen across the system, from increasing recognition about workers’ secondary traumatic stress following the death of a child to increasing utilization of trauma-focused behavioral health services to changes to the intake process and implementation of a differential response system. The continued importance of a trauma-informed approach through the recent transition to a new Commissioner and administration suggests that the cultural shift has been embedded within the CWS and will continue. In addition, other state agencies (e.g., juvenile justice, education) have begun pursuing a trauma-informed approach in part through learning about DCF’s success.
Based on our experience with CONCEPTs’s challenges and success, we make several recommendations for other CWSs seeking to implement a trauma-informed approach. First, the comprehensive readiness and capacity assessment that was provided (and required) by the grant in the first year offered a much-needed opportunity to carefully plan for implementation based on the CWS’s capacity and needs, including soliciting input from hundreds of CWS staff across the state and ensuring buy-in and commitment from leadership. Second, we recommend a multi-component approach that addresses immediate, concrete needs of CWS staff (e.g., high-quality training in trauma, a brief screening tool, increased access to trauma-focused EBTs for children in the CWS) as well as opportunities to more permanently embed changes into the system (e.g., policy change, building internal capacity/expertise in trauma). Finally, the importance of a multidisciplinary leadership and implementation team, including a range of CWS staff, an intermediary organization, an academic researcher, community-based providers, and a consumer, was a strong driver for CONCEPT’s success. We recommend that CWSs seeking to implement a trauma-informed approach search inside and outside the CWS to develop similar partnerships for a governance and implementation team.
Finally, as noted in Lang et al. (2016), state and federal policy efforts may impact the need for systems to adopt more trauma-informed approaches, potentially accelerating the pace with which state systems work to promote increased capacity and access to trauma-informed care. Since that time, congress enacted the Families First Act of 2018, which includes a number of requirements related to evidence-based and trauma-informed services. Specifically, in order for states to be reimbursed for extended stays in congregate care, facilities must meet criteria for a “qualified residential treatment program,” and one criterion for this designation includes the use of trauma-informed treatment model. The law also allows states to use funds derived from Title IV-E of the Social Security Act be used for “time-limited services” to prevent out-of-home placement, providing such services have a demonstrated level of efficacy. Many core trauma-focused interventions (e.g., TF-CBT, EMDR, CPP) meet high standards of evidence (well-supported or supported) and numerous others (e.g., CFTSI, AF-CBT, TARGET-A) are rated as promising practices by the California Evidence-based Clearing-house for Child Welfare (www.cebc4cw.org), consistent with the guidelines of the Act. As these and other policies are implemented, support for trauma-informed and evidence-based treatments will likely follow—prompting still greater attention on the need for workforce training, appropriate screening and assessment, and other system-development efforts to support growth of trauma-informed child-serving systems of care.
Highlights.
Evaluated changes in child welfare system capacity for trauma-informed care over 5-year initiative
Initial gains in perceived capacity for trauma-informed care were sustained during implementation.
Workforce development, wellness supports, and accessible treatments contributed to improvements.
ACKNOWLEDGMENTS
CONCEPT was funded by a cooperative agreement from the Department of Health and Human Services, Administration for Children and Families, Children’s Bureau, Grant #0169. The authors would like to acknowledge the contributions of Kim Campbell, Marilyn Cloud, Cindy Crusto, Doriana Vicedomini, Paul Shanley, Bert Plant, Maegan Genovese, Emily Melnick, Tanisha Mair, Aliza Lipman, Jodi Hill-Lilly, Joette Katz, Mary Cummins, Tracy Davis, Michelle Delaney, Carrie Epstein, Robert Franks, Victoria Gasca, Carla Stover, Tiffany Franceschetti, Karen Grayson, Rita Pelaggi, Carol O’Connor, Laurie Valentine, Jeffrey Vander-ploeg, and all of the provider organizations, staff, and families who participated in CONCEPT activities.
Footnotes
Conflict of Interest
The authors declare they have no conflict of interest.
Compliance with Ethical Standards
The authors of this manuscript have complied with APA ethical principles in their treatment of individuals participating in the research, program, or policy described in the manuscript. This study received Institutional Review Board approval from Yale University School of Medicine and Connecticut Department of Children and Families.
References
- Ai AL, Foster LJJ, Pecora PJ, Delaney N, & Rodriguez W (2013). Reshaping child welfare’s response to trauma: Assessment, evidence-based intervention, and new research perspectives. Research on Social Work Practice, 23(6), 651–668. [Google Scholar]
- Akin BA, Strolin-Goltzman J, & Collins-Camargo C (2017). Successes and challenges in developing trauma-informed child welfare systems: A real-world case study of exploration and initial implementation. Children and Youth Services Review, 82, 42–52. [Google Scholar]
- Bartlett JD, Griffin JL, Spinazzol J, Fraser JG, Norona CR, Bodian R, & Barto B (2018). The impact of a statewide trauma-informed care initiative in child welfare on the well-being of children and youth with complex trauma. Children and Youth Services Review, 84, 110–117. 10.1016/j.childyouth.2017.11.015. [DOI] [Google Scholar]
- Berkowitz SJ, Stover CS, & Marans SR (2011). The child and family traumatic stress intervention: Secondary prevention for youth at risk of developing PTSD. Journal of Child Psychology and Psychiatry, 52, 676–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berliner L, Fitzgerald MM, Dorsey S, Chaffin M, Ondersma SJ, & Wilson C (2015). Report of the APSAC Task Force on evidence-based service planning guidelines for child welfare. Child Maltreatment, 20, 6–16. [DOI] [PubMed] [Google Scholar]
- Berliner L, & Kolko DJ (2016). Trauma informed care: A commentary and critique. Child Maltreatment, 21, 168–172. [DOI] [PubMed] [Google Scholar]
- Bunting L, Montgomery L, Mooney S, MacDonald M, Coulter S, Hayes D, & Davidson G (2019). Trauma informed child welfare systems—A rapid evidence review. International Journal of Environmental Research and Public Health, 16, 2365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burns BJ, Phillips SD, Wagner HR, Barth RP, Kolko DJ, Campbell Y, & Landsverk J (2004). Mental health need and access to mental health services by youths involved with child welfare: A national survey. Journal of the American Academy of Child & Adolescent Psychiatry, 43, 960–970. [DOI] [PubMed] [Google Scholar]
- Campbell K, Lang JM, & Zorba B (2018). Policy change to support trauma informed care in child welfare. APSAC Advisor, 30, 75–89. [Google Scholar]
- Chadwick Trauma-Informed Systems Project (2013). Creating trauma-informed child welfare systems: A Guide for administrators (2nd edn). San Diego, CA: Author. [Google Scholar]
- Child Welfare Collaborative Group & National Child Traumatic Stress Network. (2013). Child welfare training toolkit: 3rd edition: Trainer’s guide. Los Angeles & Durham, NC: National Center for Child Traumatic Stress. [Google Scholar]
- Child Welfare Information Gateway (2015). Developing a trauma-informed child welfare system. Washington, DC: U.S. Department of Health & Human Services, Children’s Bureau. [Google Scholar]
- Cohen JA, Mannarino AP, & Deblinger E (2006). Treating trauma and traumatic grief in childhood and adolescence. New York: Guilford Press. [Google Scholar]
- Conners-Burrow NA, Kramer TL, Sigel BA, Helpenstill K, Sievers C, & McKelvey L (2013). Trauma-informed care training in a child welfare system: Moving it to the front line. Children and Youth Services Review, 35, 1830–1835. 10.1016/j.childyouth.2013.08.013. [DOI] [Google Scholar]
- Conradi L, Wherry J, & Kisiel C (2011). Linking child welfare and mental health using trauma-informed screening and assessment practices. Child Welfare, 90, 129–147. [PubMed] [Google Scholar]
- Copeland WE, Shanahan L, Hinesley J, Chan RF, Aberg KA, Fairbank JA, & Costello EJ (2018). Association of childhood trauma exposure with adult psychiatric disorders and functional outcomes. JAMA Network Open, 1, e184493–e184493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crandal BR, Hazen AL, & Reutz JR (2017). Identifying trauma-related and mental health needs: The implementation of screening in California’s child welfare systems. Advances in Social Work, 18, 335–348. [Google Scholar]
- Ebert L, Amaya-Jackson L, Markiewicz JM, Kisiel C, & Fairbank JA (2012). Use of the breakthrough series collaborative to support broad and sustained use of evidence-based trauma treatment for children in community practice settings. Administration and Policy in Mental Health and Mental Health Services Research, 39, 187–199. 10.1007/s10488-011-0347-y. [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, & Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults - The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14, 245–258. 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, & Hamby SL (2015). Prevalence of childhood exposure to violence, crime, and abuse: Results from the national survey of children’s exposure to violence. Jama Pediatrics, 169, 746–754. [DOI] [PubMed] [Google Scholar]
- Fox BH, Perez N, Cass E, Baglivio MT, & Epps N (2015). Trauma changes everything: Examining the relationship between adverse childhood experiences and serious, violent and chronic juvenile offenders. Child Abuse & Neglect, 46, 163–173. [DOI] [PubMed] [Google Scholar]
- Garcia AR, Gupta M, Greeson JK, Thompson A, & DeNard C (2017). Adverse childhood experiences among youth reported to child welfare: Results from the national survey of child & adolescent wellbeing. Child Abuse & Neglect, 70, 292–302. [DOI] [PubMed] [Google Scholar]
- Greer D, Grasso DJ, Cohen A, & Webb C (2014). Trauma-focused treatment in a state system of care: Is it worth the cost? Administration and Policy in Mental Health and Mental Health Services Research, 41, 317–323. [DOI] [PubMed] [Google Scholar]
- Hanson RF, & Lang J (2016). A critical look at trauma-informed care among agencies and systems serving maltreated youth and their families. Child Maltreatment, 21, 95–100. [DOI] [PubMed] [Google Scholar]
- Hendricks A, Conradi L, & Wilson C (2011). The trauma system readiness tool. San Diego, CA: Chadwick Center for Children and Families. [Google Scholar]
- Kerns SE, Pullmann MD, Negrete A, Uomoto JA, Berliner L, Shogren D, & Putnam B (2016). Development and implementation of a child welfare workforce strategy to build a trauma-informed system of support for foster care. Child Maltreatment, 21, 135–146. [DOI] [PubMed] [Google Scholar]
- Kilo CM (1998). A framework for collaborative improvement: Lessons from the Institute for Healthcare Improvement’s Breakthrough Series. Quality Management in Health Care, 6, 1–13. [DOI] [PubMed] [Google Scholar]
- Kisiel C, Fehrenbach T, Small L, & Lyons JS (2009). Assessment of complex trauma exposure, responses, and service needs among children and adolescents in child welfare. Journal of Child & Adolescent Trauma, 143–160. [Google Scholar]
- Ko SJ, Ford JD, Kassam-Adams N, Berkowitz SJ, Wilson C, Wong M, & Layne CM (2008). Creating trauma-informed systems: Child welfare, education, first responders, health care, juvenile justice. Professional Psychology-Research and Practice, 39, 396–404. 10.1037/0735-7028.39.4.396. [DOI] [Google Scholar]
- Kramer TL, Sigel BA, Conners-Burrow NA, Savary PE, & Tempel A (2013). A statewide introduction of trauma-informed care in a child welfare system. Children and Youth Services Review, 35, 19–24. 10.1016/j.childyouth.2012.10.014. [DOI] [Google Scholar]
- Lang JM, Ake G, Barto B, Caringi J, Little C, Baldwin MJ, & Connell CM (2017). Trauma screening in child welfare: Lessons learned from five states. Journal of Child & Adolescent Trauma, 10, 405–416. [Google Scholar]
- Lang JM, Campbell K, Shanley P, Crusto CA, & Connell CM (2016). Building capacity for trauma-informed care in the child welfare system: Initial results of a statewide implementation. Child Maltreatment, 21, 113–124. 10.1177/1077559516635273. [DOI] [PubMed] [Google Scholar]
- Lang JM, & Connell CM (2017). Development and validation of a brief trauma screening measure for children: The Child Trauma Screen. Psychological Trauma-Theory Research Practice and Policy, 9, 390–398. 10.1037/tra0000235. [DOI] [PubMed] [Google Scholar]
- Lang JM, & Connell CM (2018). The child trauma screen: A follow-up validation. Journal of Traumatic Stress, 31, 540–548. 10.1002/jts.22310. [DOI] [PubMed] [Google Scholar]
- Lang JM, Franks RP, Epstein C, Stover C, & Oliver JA (2015). Statewide dissemination of an evidence-based practice using Breakthrough Series Collaboratives. Children and Youth Services Review, 55, 201–209. 10.1016/j.childyouth.2015.06.005. [DOI] [Google Scholar]
- Miller EA, Green AE, Fettes DL, & Aarons GA (2011). Prevalence of maltreatment among youths in public sectors of care. Child Maltreatment, 16, 196–204. 10.1177/1077559511415091. [DOI] [PubMed] [Google Scholar]
- Murphy K, Moore KA, Redd Z, & Malm K (2017). Trauma-informed child welfare systems and children’s well-being: A longitudinal evaluation of KVC’s bridging the way home initiative. Children and Youth Services Review, 75, 23–34. 10.1016/j.childyouth.2017.02.008. [DOI] [Google Scholar]
- Pecora PJ, Jensen PS, Romanelli LH, Jackson LJ, & Ortiz A (2009). Mental health services for children placed in foster care: An overview of current challenges. Child welfare, 88, 5–26. [PMC free article] [PubMed] [Google Scholar]
- Qualtrics. (2016). Qualtrics survey software. Provo, UT. [Google Scholar]
- Saunders BE, & Hanson RF (2014). Innovative methods for implementing evidence-supported interventions for mental health treatment of child and adolescent victims of violence In Reece RM, Hanson RF & Sargent J (Eds.), Treatment of child abuse: Common ground for mental health, medical, and legal practitioners (2nd edn, pp. 235–245). Baltimore, MD: Johns Hopkins University Press. [Google Scholar]
- Sprang G, Craig C, & Clark J (2011). Secondary traumatic stress and burnout in child welfare workers: a comparative analysis of occupational distress across professional groups. Child Welfare, 90, 149–168. [PubMed] [Google Scholar]
- Stambaugh L, Ringeisen H, Casanueva C, Tueller S, Smith K, & Dolan M (2013). Adverse childhood experiences in NSCAW. (OPRE report 2013–26) Washington, DC: Office of Planning, Research and Evaluation, Administration for Children and Families, U.S. Department of Health and Human Services. [Google Scholar]
- StataCorp LLC. (2015). Stata data analysis and statistical software (Version 14.2) College Station, TX: StataCorp LLC [Google Scholar]
- Strand VC, Spath R, & Bosco-Ruggiero S (2010). So you have a stable child welfare workforce - What’s next? Children and Youth Services Review, 32, 338–345. 10.1016/j.childyouth.2009.10.002. [DOI] [Google Scholar]
- Substance Abuse and Mental Health Services Administration. (2014). SAMHSA’s concept of trauma and guidance for a trauma-informed approach. HHS Publication No. (SMA) 144884. Rockville, MD: Substance Abuse and Mental Health Services Administration. [Google Scholar]
- Sullivan K, Preisler J, Ake GS, Potter D, & Beck D (2012). North Carolina child welfare trauma readiness assessment. Raleigh, NC: North Carolina Department of Health and Human Services, Division of Social Services, Funded by the Department of Health and Human Services, Administration for Children, Youth and Families, Children’s Bureau Grant #90CO1058. [Google Scholar]
- U.S. Department of Health & Human Services. (2019a). Adoption foster care analysis reporting system (AFCARS) FY2008–2017. Submissions as of 08/10/2018. Available from: https://www.acf.hhs.gov/cb/resource/trends-in-foster-care-and-adoption [last accessed August 10 2018]
- U.S. Department of Health & Human Services. (2019b). Child maltreatment 2017. Available from: http://www.acf.hhs.gov/programs/cb/research-data-technology/statistics-research/child-maltreatment [last accessed June 2019]
- Verardi V, & Croux C (2009). Robust regression in Stata. The Stata Journal, 9, 439–453. [Google Scholar]


