Key Readings Index
Structure and Function, 324
Dysfunction/Responses to Injury, 331
Portals of Entry/Pathways of Spread, 339
Defense Mechanisms/Barrier Systems, 342
Disorders of Domestic Animals, 344
Disorders of Horses, 386
Disorders of Ruminants (Cattle, Sheep, and Goats), 391
Disorders of Pigs, 401
Disorders of Dogs, 406
Disorders of Cats, 410
E-Glossary 7-1 Glossary of Abbreviations and Terms
AAEC—Attaching and effacing Escherichia coli = EPEC
Abdominocentesis—Needle puncture of the abdomen to obtain fluid for analysis
Aboral—Moving away from the oral cavity
Acanthotic—Thickening of the stratum spinosum
Achalasia—Primary esophageal motility disorder with an absence of esophageal peristalsis
Achlorhydric—Absence of hydrochloric acid from gastric secretions
Achlorophyllic—Absence of chlorophyll
Afferent—Leading into
Agalactia—Absence of milk production
Aganglionic—Lacking ganglia
Agenesis—Failure of formation
AHV—Alcelaphine herpesvirus
AIDA—Adhesin involved in diffuse adherence
AIDS—Acquired immunodeficiency syndrome
Amalgam—Dental cavity filling
Amelanotic—Lacking melanin
Amelogenesis—Enamel formation
Amphophilic—Stains with both acid and basic dyes
Aneurysm—Balloon-like bulging of a vascular wall
Angiotoxin—Toxin affecting vasculature
Anion channel—A protein (porin) that allows formation of transmembrane channels
Ankyloglossia—“Tongue-tied”; a lingual frenulum limiting tongue movement
Anoikis—Apoptosis as a result of separation from the extracellular matrix
Anorexia—Loss of appetite
Antecedent—Preceding
Anthelmintic—Drug used to expel parasites
Anthrolysin—Pore-forming, cholesterol-dependent cytolysin secreted by Bacillus anthracis
Antimesenteric—Intestinal surface opposite the mesenteric attachment
Antrum—Initial portion of the gastric pylorus
Apoptosis—Programmed cell death
Argentaffin—Stains with silver
Arteriovenous shunt—An abnormal connection between an artery and a vein
Arthropod—Insects, spiders, centipedes, shrimp, and crayfish; all with exoskeletons
Arthus—Type III hypersensitivity reaction
Artiodactyl—Even-toed ungulates
Ascites—Accumulation of fluid in the peritoneal cavity
Atony—Lack of tone or energy; muscular weakness
Bacteremia—Bacteria in the blood
Bacteriocins—Bacterial toxins that inhibit the growth of other bacteria
Bacteriophage—Virus that infects bacteria
Basophilic—Cells accepting a basic dye (e.g., hematoxylin)
Bifid—Split or cleft
Biotype—Individuals having the same enteric bacterial makeup
Birefringent—Double refraction of light
Bombesin—Hormone present in the intrinsic nerves of the gastrointestinal tract that stimulates the release of gastrin and pancreatic enzymes and causes contraction of the gallbladder
Botryoid—Grapelike clusters
BoTV—Bovine torovirus
Brachydont—Teeth with short crowns and well-developed roots that do not continue to grow throughout life
Brachygnathia—Short mandible as compared to the maxillae
Broken mouth—Uneven dental wear with tooth loss
Bruxism—Grinding of the teeth
Buccal—Mucosal lining of the cheeks and lips
Bullae—Fluid-filled sacs
BVD—Bovine viral diarrhea
C1, C2, C3—Gastric compartments of New World camelids
Cachexia—Physical wasting
cAMP—A second messenger important in many biologic processes (cyclic adenosine monophosphate)
CAR—Coxsackievirus and adenovirus receptor
Carcinoid—Neuroendocrine tumor
Carcinomatosis—Metastases of tumors within the peritoneal cavity
Caries—Tooth decay
Catarrhal—Mucoid
Catecholamines—Epinephrine and norepinephrine
Caveat—A cautionary detail that should be considered
Cellulolytic—Ability to hydrolyze cellulose
Cercariae—Free-swimming larval stage of a parasitic trematode
Cestode—Tapeworm
CFTR—Cystic fibrosis transmembrane regulator
cGMP—A cyclic nucleotide that acts as a second messenger (cyclic guanosine monophosphate)
Chalones—Polypeptides produced by a tissue that inhibit mitosis in the cells of that tissue
Cheiloschisis—Cleft lip
Chief cell—Gastric cell that releases pepsinogen and chymosin
Chloroplasts—Organelles in plant cells and eukaryotic algae that conduct photosynthesis
Choke—Clinical disease caused by an obstructed esophagus
Cholecystokinin—Hormone that stimulates the gallbladder to contract
Chyle—Fluid within the lacteals consisting of an emulsion of lymph and chylomicrons
Claudin—Transmembrane protein of tight junctions
Colicins—Bacteriocins from E. coli
Collagenolysis—Dissolution or digestion of collagen
Commensal—Relationship between two organisms where one organism benefits from the other without affecting it
Complement—Protein cascade that aids inflammation
Cotransporter—Protein that aids in the active transport of sodium, potassium, and chloride into and out of cells
CpHV—Caprine herpesvirus
Cricopharyngeal—Muscle of upper esophageal sphincter
CXC—Chemokines
Cytochrome P450—Family of isozymes that biotransform xenobiotics
Cytokeratin—Keratin-containing intermediate filament in epithelial cells
Cytokine—Small cellular protein important in cell signaling
Cytopathic—Virus-induced structural changes in host cells
Cytotoxins—Agents or processes that kills cells
Darkfield—Microscope illumination technique that is used on unstained tissue or cells
Defensins—Antibiotic polypeptides in neutrophils that kill bacteria via membrane damage
Deglutition—Swallowing
Dentine/Dentin—Mineralized tissue denser than bone that forms the bulk of the tooth
Denuded—With the epithelium removed
DIC—Disseminated intravascular coagulopathy
Digesta—Gastrointestinal contents being digested
Diverticulosis—Outpouching of the intestinal mucosa into and sometimes through the muscularis
Dysautonomia—Malfunction of the autonomic nervous system
Dysbiosis—Microbial imbalance in the gut
Dysentery—Bloody diarrhea
Ectasia—Dilation of a tubular structure
Ecthyma—Ulcerative pyoderma
Effacement—Shortening, thinning, or replacement of a tissue
Efferent—Coming away from
EGF—Epidermal growth factor
EHEC—Enterohemorrhagic E coli
EIEC—Enteroinvasive E. coli
Elementary body—Infectious particle of a microorganism
ELISA—Enzyme-linked immunosorbent assay
Endocrine—Secretes hormones into the blood
Endotoxin—Lipopolysaccharide in the wall of a (usually) Gram-negative bacteria
Enteroendocrine—Neuroendocrine cells of the intestine
Enteroglucagon—Glucagon-like hyperglycemic agent from the mucosa of the small intestine
Enteroinvasive—Organisms that penetrate into enterocytes
Enterolith—Intestinal concretion
Enteropathogen—Organism that causes disease in the intestinal tract
Enterotoxigenic—Organism containing or producing an enterotoxin
Enterotoxin—Protein released from a microorganism that damages the intestine
Enterotype—Bacterial ecosystem in the gut microbiome
Enzootic—A disease constantly present in an animal population
Eosinophilic—Tissues accepting an eosin dye
EOTRH—Equine odontoclastic tooth resorption and hypercementosis
EPEC—Enteropathogenic E. coli = AAEC
Epitheliogenesis imperfecta—Incomplete formation of skin
Epitheliotropic—Affinity for epithelium
Epizootic—An outbreak of disease in an animal population
Epulis—Tumor-like masses in the oral mucosa
Erosion—Superficial loss of lining epithelium
Eructation—Belching
Erythropoiesis—Red blood cell formation
ETEC—Enterotoxic E. coli
Exacerbate—Make worse
Exanthema—Skin eruption
Excreta—Feces
Exotoxin—A toxin secreted by a live bacteria
ExPEC—Extraintestinal pathogenic E. coli
Exsanguination—The process of bleeding out
Fauna—Animal life in a defined area
FeLV—Feline leukemia virus
Fetid—Odorous
Fimbriae—Fringe
FIP—Feline infectious peritonitis
FIV—Feline immunodeficiency virus
Flaccid—Atonal
Flagella—Whiplike external organelle
Floating—Mechanical leveling of hypsodont teeth
Flora—Plant life in a defined area
Florid—Fully developed
Fomite—Carrier of infectious organisms
Foveola—Gastric pit
GALT—Gut-associated lymphoid tissue
G cells—Gastrin-producing cells
GCP—Granulocyte chemotactic protein
GI—Gastrointestinal
GIST—Gastrointestinal stromal tumor
Glossitis—Inflammation of the tongue
Glucose-dependent insulotropic peptide—Small intestinal hormone that contributes to insulin release based on blood glucose concentrations
Gluten—Grain protein
Glycocalyx—Glycoprotein-polysaccharide surface layer
Glycoconjugate—Carbohydrates covalently linked to other chemical species
Glycosuria—Glucose in the urine
Gnotobiotic—Germ-free
Granulopoiesis—Segmented leukocyte production
Halitosis—Bad breath
Helminthes—Parasitic worms
Hematemesis—Vomiting of blood
Hematochezia—Fresh blood in the feces
Hematogenous—Blood borne
Hematoxylinophilic—Affinity for the basophilic stain hematoxylin
Hemoabdomen—Free blood in the abdominal cavity
Hemolysins—Toxins that destroy red blood cell membranes
Hemothorax—Free blood in the thoracic cavity
Hermaphrodite—Organism with male and female sex organs
Hiatal—An abnormal opening such as in the diaphragm.
Histamine—Protein produced by mast cells and basophils that functions in inflammation
HLA—Human leukocyte antigen
Horizontal spread—Disease-causing organism that spreads among an animal population
Hydropic—Swelled with water
Hypokalemia—Low potassium level in the blood
Hypsodont—Continues growing throughout life
Iatrogenic—Disease caused by treatment
Idiopathic—Of unknown cause
IHC—Immunohistochemistry
Immunohistochemistry—Use of antibodies to detect antigens in tissue sections
Immunostaining—Use of antibodies to detect proteins/antigens
Immunotolerance—Failure to mount an immune response to a particular antigen
Impaction—Blockage
Inappetence—Lack of appetite
Infarction—Tissue death due to a thrombus
Influx—Inrush
Infundibulum—Funnel-shaped cavity
Ingesta—Substances eaten
In situ—In its original place
Integrins—Transmembrane receptors
Intercurrent—Occurring at the same time
Interferon—Signaling proteins released by host cells in response to pathogens
Intermediate host—A host in which a parasite goes through its developmental stages
Intestinal emphysema—Gas-dilated intestinal lymphatic vessels
Intimin—A bacterial outer membrane protein
Intractable—Uncontrollable
Intrinsic factor—Protein necessary for absorbing vitamin B12
Intussusceptiens—Outer portion of an intussusception
Intussusception—Telescoping of intestine one portion into another
Intussusceptum—Enveloped portion of an intussusception
In utero—In the womb/uterus
Ischemia—Lack of blood circulation
Kallikrein—Serine proteases that cleave kininogens to form kinins
Keratoconjunctivitis—Inflammation of the cornea and conjunctiva
Ketonuria—Ketone bodies in the urine
Langhans giant cell—Multinucleated macrophage
Laparoscopy—Examination of a body cavity via use of a laparoscope inserted through a small incision
Leiomyometaplasia—Intestinal muscular ceroidosis
Leproma—Granulomatous nodule due to acid-fast bacteria
Leukoclastic—Neutrophilic debris in vessel walls
Leukoplakia—White patches on a mucosal membrane
Leukotrienes—Eicosanoid inflammatory mediators produced in leukocytes, mastocytes, and other cells
Ligand—An antibody, hormone, or drug that binds to a receptor
LPS—Lipopolysaccharide
Lymphangiectasia—Pathologic dilation of lymphatic vessels
Lysins—Hydrolytic bacteriophage enzymes
Lysozyme—Glycoside hydrolase that damages bacterial cell walls
Macrogamete—The larger (female) gamete involved in conjugation
Macroglossia—Large tongue
Macromolecule—Large molecules, including nucleic acids, proteins, carbohydrates, lipids, and macrocycles
Macule—Circumscribed alteration in skin color
Major histocompatibility complex—Group of genes that code for proteins on cell surfaces that enable the immune system to recognize foreign antigens
Malabsorption—Defect in absorbing nutrients from the intestinal tract
Malacia—Tissue softening
Maldigestion—Impaired breakdown of nutrients
Malocclusion—Abnormal tooth positioning
Margo plicatus—Dividing line between the gastric and nongastric parts of the equine stomach
-
M
cells—Highly specialized epithelial cells overlying lymphoid follicles of the small and large intestine
MDR—Multidrug-resistant gene
Meconium—Fetal feces
Megaesophagus—Dilated esophagus
Melena—Digested blood in the feces
Merozoite—Cells produced by fission in the asexual stage of certain protozoa
MHC—Major histocompatibility complex
Microarray—DNA spots attached to a solid surface
Microbiota—Microbe population of the intestine
Microgamete—The smaller (male) gamete involved in conjugation
Microglossia—Small tongue
Microphthalmia—Small eye
Microvilli—Brush border surface of some epithelial cells
Molt/Moult—To shed hair, skin, or feathers
Monozygotic—Produced from a single ovum
Morbidity—Incidence of disease in a population
Mortality—Frequency of deaths in a population
MBNL2—Gene that encodes a C3H-type zinc finger protein (muscleblind-like protein 2)
Mucocele/Mucocoele—Accumulation of mucus (saliva) outside of the salivary gland
Mummified—Desiccated
Mural—Wall
NAD(P)H—The reduced form of NADP
Nasal planum—Nonhaired tip of the nose
Nematodes—Roundworms
Neurohormone—Hormone produced and released by neuroendocrine cells
Neutropenia—Low number of neutrophils
NK—Natural killer
nm—Nanometer
Noncytopathic—Does not damage host cells
Nosocomial—Hospital acquired
Notch signaling—Highly conserved cell signaling system of most multicellular organisms
NSAIDs—Nonsteroidal antiinflammatory drugs
NSP—Nonstructural protein
Obligate—By necessity
Occludin—Integral plasma-membrane tight junction protein
Occlusal—Grinding or biting surface of teeth
Odontoclast—A cell that reabsorbs tooth roots
Odontogenesis—Tooth formation
Odontoma—Dental hamartoma
OvHV—Ovine herpesvirus
Oocyst—Encysted sporozoan zygote
Operculum—Small covering or lid
Opportunistic—Exploits opportunities
Osteolysis—Dissolution of bone
P450—Detoxification enzymes
Palatoschisis—Cleft palate
Palliative—Alleviating a problem but not the underlying cause
Papillae—Nipple-like projections
Paracrine—Cell-cell communication in which a cell produces a signal to induce changes in nearby cells
Paradental—Around a tooth
Paradox—A statement that is logically unacceptable
Paraffin—Waxlike substance used to embed fixed tissue
Parakeratosis—Retention of nuclei in the stratum corneum
Parietal cell—Acid-secreting cell of the stomach
Parturient—Pertaining to birth
PAS—Periodic acid–Schiff
Patent—Open
Pathophysiology—Disordered physiology associated with disease
PCAD—Porcine circovirus–associated disease
PCR—Polymerase chain reaction
PCV—Porcine circovirus
Pedunculated—Having a stalk or peduncle
PEDV—Porcine epidemic diarrhea virus
PEG—Percutaneous endoscopic gastrostomy
Pelage—Hair coat
Peptidase—Proteolytic enzyme
Percussion—Tapping a surface to determine the underlying structure
Periodontal—Supporting tooth structures
Peristalsis—Contractile movements of the intestine
Perissodactyl—Even-toed ungulates
Peyer's patch—Intestinal lymphoid nodules
PGE2—Prostaglandin E2 lipid compounds having diverse hormone-like effects
Phage—Virus that infects bacteria
Phytobezoar—Plant mass in stomach
Pilus—Hairlike appendage
Plaque—Deposit on teeth
Plasmid—Extrachromosomal DNA
Pneumoperitoneum—Air within the abdominal cavity
Polymyositis—Inflammatory muscle disease
Polyserositis—Inflammation of serous surfaces
Poor doers—Unthrifty
Porphyrin—Hemoglobin cofactor
Postparturient—After pregnancy
Postprandial—Post eating
Proctoscopy—Endoscopic evaluation of the rectum and colon
Proglottid—Tapeworm segment
Prognathia—Protruding mandible
Proptosis—Bulging eyes
Prostaglandins—Cyclic fatty acid compounds with hormone-like effects
Pruritus—Itchiness
Pseudomembrane—Membrane-like mucosal coating consisting of coagulated fibrin, bacteria, and leukocytes
Ptyalism—Salivating
Radiomimetic—Imitates the effects of radiation
Ranula—Dilated salivary duct
Reflux—Regurgitation
Refractory—Resistant
Regurgitation—Reflux
Reperfusion—Restoring blood flow
Resorption—Lysis and assimilation of a substance
Rests of Malassez—Odontogenic epithelial cells in the periodontal ligament
Retroperitoneal—Situated behind the peritoneum
Rhabditiform—Early developmental larval stages (first and second) of soil-borne nematodes
RT-PCR—Reverse transcription polymerase chain reaction
Rugae—Folds and ridges
Scaffold—Framework
Schizonts—Cells formed from a trophozoite that divides to become a merozoite
Schwartzman reaction—Generalized reaction following two intravenous injections of endotoxin given 24 hours apart, resulting in disseminated intravenous coagulopathy
Secretin—Duodenal hormone that regulates secretions of the stomach and pancreas
Septicemia—Bacterial toxemia
Serositis—Inflammation of serous surfaces
Serotonin—Neurotransmitter produced by intestinal tissue, central nervous tissue, and platelets
Sialo—Salivary
Siderophore—Iron-chelating compounds secreted by microorganisms
Somatostatin—Pancreatic and pituitary hormone that inhibits gastric secretion and somatotropin release
SPI—Salmonella pathogenicity island
Spindloid—Elongate with tapered ends
Splendore-Hoeppli reaction—Amorphic, eosinophilic, hyaline material surrounding some pathogens
Sporangiospores—Fungal spores in a fruiting body
Sporozoites—Infective stage of some sporozoans
Squamoid—Flattened
Steatitis—Inflammation of fat
Steatorrhea—Lipid in the stool
Stellate—Star shaped
Stenosis—Narrowing
Step mouth—Markedly uneven wear of cheek teeth
Stricture—Narrowing of a canal
Supernumerary—Extra
Syncytial—Multinucleate mass of cytoplasm
Synergism—Combination greater than the sum of individual effects
Temperate—Mild or moderate
Tenesmus—Straining to defecate
TGE—Transmissible gastroenteritis
TGF-α—Transforming growth factor-α
Thrombocytopenia—Platelet deficiency
Tiger striping—Congestion and hemorrhage of colonic and rectal ridges
Tight junctions—Epithelial cell connections
TLRs—Toll-like receptors
TNF—Tumor necrosis factor
Toll-like receptor—Single, membrane-spanning sentinel cell receptor of macrophages and dendritic cells that recognizes structurally conserved molecules derived from microbes
Torsion—Rotation of an organ on its long axis
Toxemia—Circulating toxins
Transcription—Copying of DNA into RNA via RNA polymerase
Transduction—The vector transfer of genetic material from one organism to another
Transferrin—Iron-binding blood protein
Translucent—Semitransparent
Transmural—Throughout the entire wall of a luminal organ
Trematodes—Flukes; flatworms
Tricellulin—Tight junctional protein
Trichobezoar—Mass of hair in the stomach
Trophozoite—An elongated cell that develops from a sporozoite or a merozoite of an apicomplexan parasite
Tropism—Specificity
TRP—Tyrosinase-related protein
Tumor necrosis factor—Cytokines that can cause cell death (apoptosis)
Tympany—A low-pitched, resonant, drumlike sound from a gas filled organ
Ubiquitous—Pervasive
Ulcer—Full-thickness loss of epithelium of a luminal surface to the basement membrane
Ungulate—Hoofed mammal
Uroperitoneum—Urine within the abdominal cavity
VapA—Virulence-associated protein A
Verminous—Parasite related
Verotoxic—Lethal to African green monkey cell cultures
Vertical spread—Transmitted from the mother to the embryo/fetus
Vesiculation—Blistering
Virulence—Degree of pathogenicity
Volvulus—Rotation of a luminal viscus on its mesenteric axis
VTEC—Verotoxic E. coli
Waterhouse-Friderichsen syndrome—Hemorrhagic adrenalitis often secondary to endotoxic shock and DIC
Wnt—Signal transduction pathway proteins that pass signals from outside of cell via cell surface receptors to the inside of the cell
Zona occludens—Tight junctions
Zoonosis—Disease-causing agent that passes from an animal to human beings
Zygote—Fertilized ovum
Zymogen pepsin—Enzyme from the chief cells of the stomach
Introduction
The alimentary system is a long and complex tube that varies in its construction and function among animal species. For example, herbivores need a fermentation chamber (either a rumen or an expanded cecum) for the digestion of cellulose, a feature not present in carnivores. Although a large variety of gastrointestinal (GI) disturbances are clinically important in all species of animals, the predominant form of disease varies from species to species. Pet carnivores, partly because of their long life span, effective vaccines, and a lifestyle and diet similar to that of human beings, develop alimentary neoplasia far more often than herbivores. Meat-, milk-, and fiber-producing animals (ruminants and pigs) are host to a variety of infectious diseases that are largely resistant to vaccines. These pathogens may have evolved as a result of the herding instinct of these animals, giving the pathogens an opportunity to mutate within a large socially structured host population. Horses are most prone to displacements of alimentary viscera.
In general the alimentary system, including the salivary glands, pancreas, and liver, functions by adding water, electrolytes, and enzymes to ingested matter and then mixing and grinding it to facilitate its breakdown to water-soluble nutrients for absorption across mucous membranes into the blood circulation and subsequent distribution through the body. Although the alimentary tract is open ended, most ingested substances and secretions produced by the GI system are absorbed.
A large part of the practice of veterinary medicine is devoted to the diagnosis and treatment of alimentary disorders. Many of the newer molecular and imaging methods have been designed specifically to increase the clinician's ability to make accurate diagnoses of the various conditions of the alimentary system. Additionally, every physical examination includes the opportunity for a fecal analysis that allows the clinician a window into the functioning of the alimentary system as a whole.
The polymerase chain reaction (PCR) is a tool that allows the opportunity to rapidly diagnose an infectious cause of enteritis without having to culture the organism in the traditional manner. Diagnosis of the cause of an infectious disease of the alimentary system can also be made from examination of a biopsy sample by histologic and immunohistochemical staining or by in situ hybridization that allows demonstration of the pathogen within target cells.
Through the use of fiberoptic endoscopes inserted through the mouth or anus or through a small incision in the abdominal wall (laparoscopy), a thorough clinical examination of most of the alimentary system can be made. This knowledge is now a necessity in clinical practice because GI mucosa from the oral cavity, through the esophagus, stomach, duodenum, and the large colon and rectum and the entire serosal surface of the abdominal viscera can be viewed and sampled directly in the live animal.
For convenience of discussion and illustration, the alimentary system has been divided into the following anatomic subunits: oral cavity; teeth; tonsils; salivary glands; tongue; esophagus; rumen, reticulum, and omasum; stomach and abomasum; intestine; and the peritoneum, omentum, mesentery, and peritoneal cavity.
Structure and Function
The most important point to keep in mind when examining the alimentary system is that normal mucosal and serosal surfaces should be smooth and shiny (although there may be normal papilla, folds, and ridges). The exception to this rule is the rumen, whose papillae may normally have a roughened, dull surface appearance. When serosal and mucosal surfaces are not smooth and shiny, animals should be examined thoroughly to determine the reason.
The function of the alimentary system as a whole is to take ingested feedstuffs, grind them and mix them with a variety of secretions from the oral cavity, stomach, pancreas, liver, and intestines (digestion), and then to absorb the constituent nutrients into the bloodstream and lacteals. Undigested ingesta, effete neutrophils, fresh (hematochezia) or digested (melena) blood, and excess secretions are passed from the body into the alimentary lumen and thus become a component of the feces. The quality and quantity of the feces and clinical signs, such as regurgitation and vomiting, are often early indicators of alimentary dysfunction.
Oral Cavity
The physiologically normal oral mucosa is smooth, shiny, and pink. It is composed of variably keratinizing, stratified squamous epithelium (mucous membranes). In animals in which the oral mucosa is heavily pigmented (melanosis), assessment of circulatory function (capillary refill time) and color as an indicator of red blood cell concentration (packed cell volume) can be difficult. In these cases, examination of conjunctiva and rectal and urogenital mucosa can be substituted. The oral cavity is where ingested materials are masticated; mixed with digestive enzymes, such as those in saliva; and passed on through the oropharynx to the esophagus.
Teeth
Teeth provide mechanical advantage for prehension, tearing, and/or mastication of food. Among domestic animals there are differences in the growth pattern and numbers of teeth. Hypsodont teeth, such as in the horse, continue to grow throughout life, and appropriate leveling of the occlusive surfaces (floating) may be a necessary procedure to prevent malocclusion and sharp edges that can lacerate the adjacent buccal mucosa and interfere with appropriate mastication as the horse ages. Brachydont teeth, such as in carnivores, do not continue to grow after they are fully erupted. Most species of mammals have deciduous teeth that are replaced near maturity by permanent teeth. In many species the approximate age of the animal may be determined by eruption date and examination of wear patterns and shape of the teeth.
Molar teeth in general are designed for grinding feedstuffs, whereas incisors in ruminants (mandibular only) are for cropping forage. Canine teeth are designed for tearing flesh. Brachydont teeth consist of a crown, which is the portion above the gingiva; the neck, which is slightly constricted; and, just below the gingiva, the roots, which are embedded in the bony socket (alveolus) of the jaw. Enamel covers the crown, cementum covers the roots, and both cover the dentin. Besides carnivores, the incisor (lower) teeth of ruminants and porcine teeth, except the canines of the boar, are brachydont.
Hypsodont teeth have an elongated body, but the neck and roots may form later in life. Cementum covers the tooth, and enamel is beneath the cementum. Beneath the enamel is the dentin. The cementum and enamel invaginate into the dentin, forming the infundibula. Enamel crests result from normal wear, with enamel being the hardest of the layers. The cheek teeth of ruminants, tusks of boars, and the teeth of horses are hypsodont.
In simple-toothed animals, such as carnivores, the tooth root is not covered by enamel. Receding gingiva therefore expose the dentin, resulting in pain and invasion by bacteria. Domestic animal species seldom get caries, although buildup of plaque can result in gingival infections, osteolysis, and tooth loss.
Tonsils
The palatine tonsils are pharyngeal lymphoid structures covered by stratified squamous epithelium. Their function is uncertain, although it is likely they serve in lymphocyte production and antibody formation (see Chapters 5 and 13). In carnivores they are found in crypts or recesses at the dorsolateral aspect of the caudal oropharynx. In pigs they are flat and recognized by tiny pores in the surface epithelium of the caudal soft palate. Horses, ruminants, and pigs have lingual tonsils in addition to palatine tonsils.
Salivary Glands
Salivary glands are found in a variety of locations in the head and neck regions and vary in number and location from species to species. They arise from oral ectoderm. In all species the major salivary glands include the parotid, mandibular, and sublingual. Carnivores have a zygomatic gland as well. Minor salivary glands include buccal, labial, lingual, palatine, and others similarly named by location.
Most salivary glands are discrete aggregates of compound tubuloalveolar tissue. Saliva is a mixture of serous and mucoid secretions. Saliva lubricates the mouth and esophagus and moistens ingesta. Saliva also dissolves water-soluble components of food so the taste buds can function. The mucus in saliva binds to masticated food and creates a bolus that is more easily swallowed. Salivary mucus also coats the epithelium of the mouth, preventing mechanical damage to the tissue. Saliva, through its flushing action, reduces bacterial populations. Saliva contains a lysozyme that lyses bacteria. Carbohydrate digestion begins in the oral cavity as a result of the presence of α-amylase, which changes starch into maltose. There are very small quantities of this enzyme in carnivores and cattle. Saliva also is an effective buffer, especially in ruminants, whose forestomachs have no glands. In carnivores, evaporation of saliva is a major mechanism of thermoregulation.
Tongue
The tongue is a muscular organ covered by stratified epithelium and is functionally connected to the esophagus via the epiglottis. It is necessary for prehension, mastication, and swallowing of feedstuffs and water. The epithelial covering of the tongue is stratified squamous with various degrees of keratinization dorsally, but ventrally the epithelium is not keratinized and the tongue attaches to the floor of the oral cavity by a frenulum. Keratinized papillae are most prominent in ruminants and cats. There are various types of papillae, some with secondary lamellae. Vallate papillae, for example, are on the dorsal surface of the tongue near its origin and are flat structures completely surrounded by a cleft. Some surface macroscopic papillae contain taste buds. The tongue is a highly vascular (functioning in heat loss in many animals, especially carnivores that have no sweat glands) and sensitive organ containing a variety of serous and mucus glands and sensory cells (taste buds). The muscular part of the tongue is striated in randomly arranged bundles. A cordlike structure enclosed in dense collagen extending lengthwise near the ventral central surface of the tongue of carnivores is called the lyssa. Porcine and equine tongues have a similar structure. The lyssa appears to be a structure without a function. Historically the lyssa was removed as “prevention” for rabies. Lyssa bodies are synonymous with Negri bodies, and rabies used to be called lyssa. Adipose tissue becomes more abundant in the caudal part of the tongue in most species.
Esophagus
Under normal circumstances the esophageal lumen is a potential space. The wall collapses when the esophagus is not transporting ingesta. The esophagus extends from the aboral end of the oropharynx, passes through the mediastinum and the diaphragmatic hiatus, and ends at the stomach. The esophagus is lined by nonkeratinizing stratified squamous epithelium in carnivores and is keratinized in pigs, horses, and ruminants. Keratinization is greatest in ruminants, less in horses, and least in pigs. Longitudinal and oblique mucosal folds are present to varying degrees. Transverse, herringbone-like folds are present in the cat.
The tunica muscularis is completely striated in ruminants and dogs. In the horse the distal third of the esophagus contains smooth muscle. The pig is similar to the horse, except that the middle third of the esophagus contains a mixture of smooth and striated muscle. In cats, opossums, and primates, the distal two-thirds of the esophagus is composed of smooth muscle. The smooth muscle is arranged as an inner circular layer and an outer longitudinal layer. Horses are unable to vomit.
Mixed mucinous glands are present in the tunica submucosa of pigs and dogs. In pigs the glands are most abundant in the cranial half of the esophagus, and in dogs they are present throughout. Glands are present in cats, horses, and ruminants only at the junction of the esophagus and pharynx.
It is important to remember that unlike the rest of the tubular digestive tract, the esophagus is unique in that it lacks a serosa in all but the abdominal portion. This means that there is no serosa to leak serum and fibrin to seal a puncture wound from a perforation of a foreign body or a surgical incision. Likewise, sutures are not likely to seal an incision. Combine this with the strong muscular peristaltic contractions that characterize this organ and it is easy to understand why esophageal surgery is not often performed and is even less often successful. For the same anatomic reasons, perforating foreign bodies of the esophagus do not seal themselves off.
Esophageal innervation is from the vagus nerves. Esophageal smooth muscle contains myenteric ganglia. Striated muscle is innervated by motor end-plates via efferent fibers of the hypoglossal nerve along with contributory neurofibers from cranial nerves V, IX, and X, which control voluntary lingual function.
Rumen, Reticulum, and Omasum
The forestomachs of ruminants and camelids are dilations and modifications of the esophagus. They are designed to house the digestive flora responsible for breaking down cellulose into short-chain fatty acids. The rumen has small papillae that vary by diet up to 1.5 cm in length. Their length, shape, and degree of keratinization are affected by diet; they are longer with high-roughage diets and shorter with more concentrates in the ration. These changes are most obvious in the ventral compartment—the ventral ruminal sac. The reticulum has a honeycomb appearance, and the omasum consists of a series of approximately 100 longitudinal folds similar to the pages of a book. The non-glandular stratified squamous mucosa of the reticulum, rumen, and omasum can be acutely inflamed when their contents have an acid pH and the abnormal milieu permits bacterial and mycotic overgrowth.
The epithelial lining of the forestomach functions as a protective barrier for the forestomach and for the metabolism of ingesta and the absorption of volatile fatty acids, Na+, and Cl-. Because the reticulo-omasal orifice is more dorsal than the floor of the compartments, the reticulum can trap foreign bodies, especially dense metallic ones. These can irritate or penetrate the mucosa (“hardware disease”). Problems with motility and imbalances of rumen flora and fauna are the most frequent abnormalities of forestomach function. Often the changes in flora and fauna are precipitated by a change in ingested substrate, promoting the growth of particular organisms. These changes alter ruminal pH and thus affect the integrity of the mucosal lining of the compartments of the forestomach or cause the production of excessive gas, resulting in ruminal distention.
Parts of compartment one (C1) and C2 and C3 of the camelid forestomach are lined by mucinous glandular epithelium. Concretions of ingesta are sometimes found within the saccules that contain the glands. The saccules are also the sites of water and other solutes. The nonglandular portions of C1 and C2 are lined by nonkeratinized stratified squamous epithelium without papillae. The forestomach of New World camelids contracts at two to three times the rate of ruminants (and in reverse order), and with each cycle, the saccules empty and refill. This results in high digestive efficiency across the saccules.
Stomach and Abomasum
The gastric mucosa of simple-stomached animals contains numerous folds or rugae that are flattened when the stomach is distended. Foveolae or gastric pits communicate with the lumen of the stomach and transport gastric cell secretions. The glandular stomach functions in the enzymatic and hydrolytic digestion of ingested food substances. The epithelial covering is one cell thick, and the cell types include columnar mucus and bicarbonate-secreting surface epithelial cells, mucous neck cells arranged in tubuloalveolar glands, acid-secreting parietal cells, pepsinogen-secreting chief cells, and neuroendocrine (enterochromaffin, argentaffin) cells that secrete gastrin, enteroglucagon, and somatostatin (Fig. 7-1 ). The neuroendocrine cells do not communicate with the gastric lumen. The mucous neck cells are the precursor cells for all the other epithelial types in the stomach and are responsible for the replacement of surface epithelial cells as they are lost, either at the end of their normal life span or from some type of insult.
Figure 7-1.

Microanatomy of the Stomach.
Multiple submucosal lymphoid patches are present in monogastric animals. In ruminants a single lymphoid patch is present at the fold separating the omasum and abomasum.
In some species, such as the horse and rat, the cranial or orad part of the stomach (nonglandular part or pars nonglandularis) is lined by stratified squamous epithelium, whereas the distal portion (pars glandularis) is lined by glandular epithelium. In the horse the dividing line between the two is called the margo plicatus. The pars nonglandularis in the pig is a small square to rectangular area of stratified squamous epithelium surrounding the esophageal opening.
Although some differences exist, the stomachs of the simple-stomached animals and the abomasum of ruminants (third compartment of New World camelids) are very similar in structure and function. A fundus and body make up the cranial portion lined by numerous spiral folds and produce acid and pepsin. The aboral portion, the pyloric part, is lined by epithelium with mucous-secreting glands and G cells that produce gastrin. Stomachs have an indigenous flora. Most of these organisms cannot be cultured by traditional methods. C3 of New World camelids is more tubular than the abomasum, with more peristalsis-like rather than mixing motility. The first two-thirds of C3 is fermentative with a pH of approximately 6.5. At the caudal flexure the mucosa thickens to 7 to 10 mm and the pH is around 2.0. The final portion surrounding the torus pyloricus has an alkaline pH.
Intestine
The intestines might be thought of as a tube within the body cavity that carries material (ingesta/digesta) through the body. The overall anatomic and histologic organization of this digestive tube is illustrated in Figure 7-2 . By the action of enzymes, resident flora, and added secretions from the liver and pancreas, ingesta are broken down, nutrients are absorbed into the body, and waste products are excreted. To perform these functions the intestine needs a very large surface area, which is accomplished by the following three means:
-
1.
The intestine is coiled in the abdomen.
-
2.
Numerous intestinal folds contain villi that notably increase the number of cells contacting the ingesta (Fig. 7-3, A and B ).
-
3.
Each enterocyte has a microvillous border, further increasing the surface area available for digestive and absorptive processes (see Fig. 7-3, C).
Figure 7-2.

Anatomic and Histologic Organization of the Digestive Tube.
A, Entire digestive tube. B, Higher magnification of the jejunum and ileum.
Figure 7-3.

Organization of the Intestine.
The digestive and absorptive surfaces of the intestine are markedly increased by the presence of villi and microvilli on the enterocytes. A, Intestinal villi. Villus epithelial cells are present on a basement membrane (not seen) on a core of lamina propria. Hematoxylin and eosin (H&E) stain. B, Small intestine, intestinal villi, scanning electron microscopy. Carbon sputter coat. C, Enterocyte microvilli. Transmission electron microscopy (TEM). Uranyl acetate and lead citrate stain.
(From Damjanov I, Linder J: Anderson's pathology, ed 10, St. Louis, 1996, Mosby.)
Herbivores have longer intestines than carnivores or omnivores and need a fermentation vat, either the rumen or cecum, to digest cellulose. Within the smooth muscle layers and villi are the neural network of the enteric nervous system.
The intestinal mucosa is composed of three layers—a single-cell-thick layer of epithelial cells lining the intestinal lumen, mesenchymal cells of the lamina propria, and the muscularis mucosa. Damage to any of these structures or to their innervation can result in digestive dysfunction and resultant diarrhea.
The epithelial cells function as a selectively permeable barrier allowing nutrient, electrolyte, and water absorption, while excluding pathogens, toxins, and other antigens. An understanding of these cell types and their functional roles in digestion and absorption is important in understanding the mechanisms of intestinal disease. Similarly, an understanding of the biology of these cell types is important in predicting clinical outcomes and designing therapeutic strategies for treating intestinal disease.
Epithelial Cells
There are six major types of polarized epithelial cells lining the intestine, all of which are produced by progenitor cells in the crypts via notch signaling. Notch and Wnt signals in combination are necessary for proliferation of enterocyte precursors, but differentiation of cell types is independent of Wnt. Wnt and notch synergy appears to induce intestinal adenomas. Notch pathways are used by cells (i.e., cell-cell communication) to regulate, via their genes, cell differentiation processes that occur during embryonic and adult life. In the gut, notch pathways influence whether intestinal epithelial stem cells differentiate into cells with secretory or absorptive functions. These pathways involve typical ligand-receptor interactions, in which the ligand is a transmembrane protein expressed in one cell type (see Chapter 1) that binds with a notch receptor (i.e., notch protein) present on or in the cell membrane of another cell type. This binding interaction results in modifications of gene expression in the cell expressing the receptor, such as facilitating its differentiation into an absorptive enterocyte. This ligand-receptor binding appears to result in cells organizing into groups of cell types as needed for their differentiation into specific tissues and organs.
The epithelial cells are enterocytes, undifferentiated or crypt epithelial cells, goblet cells, Paneth cells, enterochromaffin (neuroendocrine, argentaffin) cells, and microfold (M) cells (Fig. 7-4 ).
Figure 7-4.

Epithelial Cell types of the Small Intestine.
Progenitor cells, located in the intestinal crypts, give rise to all other epithelial cell types lining the crypt and covering the villi.
Enterocytes are tall and columnar with luminal microvilli. They contain a surface glycocalyx that houses the digestive and absorptive enzymes. The mature cells do not proliferate, but they provide feedback inhibition of mitosis to the crypt cells by chalones. The cells are attached to each other by tight junctions composed of more than 40 proteins anchored to actin filaments, the most predominant of which are occludin, junctional adhesion molecules, and claudins. Many nutrients are absorbed through the lateral intercellular spaces between cells. Enterocytes move up the crypt and intestinal villus to the extrusion zone at the villus tip, where effete enterocytes are discarded into the fecal mass by an apoptotic mechanism called anoikis. The turnover rate for enterocytes is the most rapid of any fixed-cell population in the body. In neonatal pigs, for example, the turnover rate is 7 to 10 days. In 3-week-old pigs that have achieved a mature or climax flora, that rate accelerates to 2 to 3 days. Enterocytes are pinocytotic in the neonate, which is important in colostrum uptake and transfer of passive immunity from the dam. Enterocytes contain class II major histocompatibility complex (MHC) molecules and a complement of biotransformation enzymes important in metabolizing xenobiotics. Inflammatory bowel disease in human beings is accompanied by downregulation of genes encoding some of these enzymes, such as colonic enterocyte cytochrome P450. Enterocytic microvilli shed receptor-laden alkaline phosphatase and catalase-containing vesicles, thus potentially interacting with pathogens that are subsequently shed in the feces. This is one means of intestinal protection from pathogens.
The microbiota/microbiome of the lower GI system consists of 100 trillion bacteria (10 times the number of cells in an animal) and 3.3 million genes (150 times the number of genes in an animal). These bacteria secrete bacteriocins (i.e., proteinaceous toxins that inhibit the growth of other bacteria) and compete for nutrients and for attachment sites, thus limiting potential pathogen growth. The microbiota promotes immune system maturation and contains biotransformation enzymes such as β-glucuronidases, β-glucosidases, demethylases, hydrolases, and reductases. It has been recently discovered that there are three enterotypes (i.e., types of bacteriologic ecosystems of the GI microbiome) in animals and that these biotypes may be in part responsible for susceptibility or resistance to certain diseases.
Undifferentiated crypt epithelial cells have little or no digestive capability. They are the progenitor cells that replace all of the other epithelial cell types. They have short, sparse microvilli. Crypt cells are the source of secretory component that acts as a receptor for immunoglobulin A (IgA) and immunoglobulin M (IgM) produced by plasmacytes in the intestinal lamina propria. The migration rate of crypt cells up the villus depends on several factors, one of which is an adaptation to gut microflora. In germ-free or gnotobiotic animals the enterocyte replacement rate is similar to that of the neonate. Crypt cells are a source of chloride ion secretion into the intestinal lumen.
Goblet cells secrete mucus. They occur in both villous and crypt regions. Their numbers tend to increase aborally throughout the length of the intestine. Mucus exerts a variety of protective effects, including trapping of bacteria with resultant passage in the fecal mass and lessening of shear forces of particulate matter on the enterocytes.
Paneth cells are located near the crypt base in some species, notably primates, horses, and rodents. It is not certain if Paneth cells are present in pigs. Unlike all the other cells of the intestinal surface, these cells migrate toward the crypts rather than the villus tips. Paneth cells are considered to have both secretory and phagocytic functions. Experimentally, Paneth cell function and microbial composition vary among strains of mice suggesting a genetic influence of the host.
Paneth cells produce cryptdins, lysins, peptidases and lysozymes. Some of these substances are toxic to bacteria and probably protect the proliferating crypt cells from infection. Paneth cells also act in a paracrine manner by opening anion channels in enterocytes, causing chloride secretion from crypt enterocytes. It has been suggested that Paneth cells play a role in elimination of heavy metals because they are selectively damaged by methylmercury. Collectively, Paneth cells constitute a cellular mass similar to that of the pancreas.
Enteroendocrine cells are also known as enterochromaffin cells and argentaffin cells because of their affinity for silver stains. The GI system is the largest endocrine organ in the body (Box 7-1 ). Enteroendocrine cells reside primarily in the crypts and produce serotonin, glucose-dependent insulotropic peptide, catecholamines, gastrin, somatostatin, serotonin, cholecystokinin, secretin, bombesin, enteroglucagon, and likely others in response to chemical and mechanical stimuli. They secrete these products into the tissue rather than the gut lumen and thus are truly endocrine. Serotonin, for example, activates both the intrinsic and extrinsic primary afferent neurons initiating peristalsis and secretory reflexes that are transmitted to the central nervous system (CNS). Occasionally enteroendocrine cells form neoplasms called carcinoids.
Box 7-1. Enterochromaffin (Enteroendocrine, Argentaffin) Cells of the Gastrointestinal System.
Stomach
| Gastrin | Stimulates parietal cells to release HCl, ↑ motility |
| Ghrelin | Appetite regulator |
| Neuropeptide Y | ↑ Food intake |
| Somatostatin | ↓ Rate of gastric emptying and ↓ smooth muscle contractions and blood flow within the intestine |
| ↓ Release of gastrin, cholecystokinin, motilin, secretin, vasoactive intestinal peptide, gastric inhibitory polypeptide | |
| Enteroglucagon | ↓ Release of pancreatic hormones |
| ↓ Exocrine secretory action of the pancreas | |
| Histamine | ↑ Gastric acid secretion |
| Endothelin | Smooth muscle contraction |
| Glicentin | ↑ Glycogenolysis in the liver |
| Glucagon | ↑ Concentration of glucose in the blood |
Intestine
| Serotonin (90% of body's total from GI tract) | Mood, appetite, sleep |
| Cholecystokinin | Gallbladder emptying, pancreatic secretion, satiety |
| Bombesin | Negative feedback for eating |
| Secretin | Regulates secretions of stomach, pancreas and water balance |
| Enteroglucagon | Delays gastric emptying |
| Enterogastrone—Brunner's gland | ↓ HCl from stomach |
| Gastrin | Stimulates parietal cells to release HCl, ↑ motility |
| Fibroblast growth factor 19 | Effects on liver (bile acid production, glucose, glycogen) |
| Substance P | Stimulates emetic center |
| Vasoactive intestinal polypeptide | Relaxes smooth muscle of stomach, esophageal and gastric sphincters, and gallbladder while also inducing contraction of enteric smooth muscle |
| Increases water secretion, inhibits gastrin, and stimulates pancreatic secretion of bicarbonate | |
| Gastric inhibitory peptide = glucose-dependent inhibitory peptide | ↓ Gastrin, ↑ insulin |
| Motolin | Stimulates peristalsis |
| Peptide YY | ↓ Motility |
| Neurotensin | ↑ Pancreatic secretion, ↑ blood flow, ↓ motility |
| Glucagon-like peptide | ↑ Insulin, ↓ gastric emptying, ↓ gastric secretion |
| Glicentin | ↑ Glycogenolysis in the liver |
| Glucagon | ↑ Concentration of glucose in the blood |
| Urogastrone | ↓ HCl |
| Oxyntomodulin | ↓ Gastric secretion, ↓ intestinal mucosal growth |
| Enkephalins | ↑ Smooth muscle contraction, ↓ secretion of water and electrolytes |
GI, Gastrointestinal; HCl, hydrogen chloride.
M cells (microfold [membranous] cells) occur in most species. These cells are located in the dome or follicle-associated epithelium of Peyer's patches or gut-associated lymphoid tissue (GALT). They are important in the uptake of antigens, including particulate toxins (e.g., asbestos) from the intestinal lumen, and transport to the lymphatic system. M cells have basal recesses that house lymphoid cells that allow more rapid interaction with phagocytosed antigens. They also allow bidirectional movement of lymphocytes between the lamina propria and intestinal lumen. M cells are exploited for the entry of a variety of pathogens such as Salmonella, Yersinia, Rhodococcus, and some viruses (bovine virus diarrhea). Figure 7-5 illustrates the anatomic and mechanistic relationships of M cells to the underlying lymphoid tissue.
Figure 7-5.

Gut-Associated Lymphoid Tissue (GALT).
DC, Dendritic cell; IEL, intraepithelial lymphocyte; M, microfold; MC, mast cell; N, neutrophil; NK, natural killer.
Mesenchymal Cells
The intestinal lymphoid tissue is 25% of the body's lymphoid mass (Fig. 7-6 ) and consists of lymphoid cells in the lamina propria and the GALT. This volume is larger than that of the spleen. In spite of the fact that the average person ingests 700 tons of antigens in a lifetime, the gut is adept at not responding to these food antigens. Laminal propria lymphocytes also play a role in intestinal crypt cell differentiation. Data are beginning to accumulate identifying the different effector and regulatory T lymphocyte types in the lamina propria and the functional organization of the GALT (see Fig. 7-5).
Figure 7-6.

Normal Gut-Associated Lymphoid Tissue (GALT), Intestine, Pig.
The lymphoid tissue on the antimesenteric surface of the intestine is outlined by arrows and makes up one-quarter of the animal's total lymphoid mass.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
The classification and functions of innate immune cells are currently being elucidated. They arise from the same progenitor cell as natural killer (NK) T lymphocytes, do not contain T lymphocyte receptors, and produce a plethora of interleukins and other soluble mediators that parallel those of the antigen-specific immune effector cells. Current theory holds that the innate lymphoid cells hold infections in check until specific immune responses can be generated. Dendritic cells may be group 3 innate lymphoid cells and along with macrophages have toll-like receptors.
Mesenchymal cells reside in the lamina propria. They arise from primitive mesenchyme rather than from ectoderm or endoderm. Among these cells is a resident population of lymphocytes that increase with exposure to antigens, especially the microbiota. The immune system and microbiota have profound influences on each other in maintaining intestinal homeostasis.
Neutrophils are transient within the lamina propria of the intestine. Neutrophils are short-lived in the blood and tissues; their normal route of removal from the body is to migrate through the wall of the alimentary tract to the lumen and be digested or excreted from the body via feces. Human neutrophils spend approximately 5 days in the bloodstream and approximately 2 days in tissues. However, there is marked variation in neutrophil life span among species. In mice, for example, neutrophils live approximately 0.75 days.
Eosinophils, when present in the intestinal lamina propria and submucosa, indicate a hypersensitivity reaction, often to food antigens or parasites.
Mast cells comprise 2% to 3% of the cells of the lamina propria and under normal conditions help regulate the intestinal epithelial barrier. Intestinal mast cells differ in important ways from mast cells in other portions of the body. They lack membrane-bound immunoglobulin E (IgE) and release proinflammatory mediators through paracrine cytokines. Mast cells are very important in maintaining intestinal integrity and perform such functions as regulating the epithelial barrier, controlling blood flow, coagulation, smooth muscle contraction, stimulation of the enteric nervous system, peristalsis, and antibody-dependent recognition of parasites and microorganisms.
Globule leukocytes are large granular lymphocytes that are interepithelial or within the lamina propria. They are most common in parasitic infections. They are found in all species and occasionally form neoplasms, most notably in the cat. The normal function of these cells is unknown. Likewise, their origin is unknown. Theories include derivation from mast cells, plasma cells, large granular lymphocyte lineages, or from a distinct precursor.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
The peritoneum is a membrane composed of a connective tissue stroma and a mesothelial cell component separated by a basement membrane. Mesothelial cells are permeable and function as a dialysis membrane. Their rapid regeneration after injury may be misinterpreted as neoplasia. It is speculated that mesothelial regeneration occurs from stem cells in the subserosal tissues rather than proliferation of adjacent uninjured mesothelial cells. Thus repair of a damaged peritoneum occurs across the whole of the damaged surface rather than from the edges such as occurs on epithelial-lined mucous membranes and skin. The peritoneum lines the abdominal cavity (parietal peritoneum) and reflects around and covers the visceral organs and scrotal cavity (visceral peritoneum). The omentum, mesenteries, and ligaments are doubled sheets of peritoneum that connect the visceral peritoneum to the parietal peritoneum. Nerves and vessels course through these structures into the various visceral structures. The visceral and parietal peritoneum receive afferent innervation from different sources. The visceral innervation is autonomic, responding with dull pain sensation to pressure and traction. In contrast, the parietal peritoneum receives afferent nerves from somatic and visceral sources, resulting in sharp pain when stimulation occurs. The peritoneal structures are an important site of fat storage and a site of serous atrophy when the animal is in negative energy balance. The kidneys are covered by peritoneum on only one surface and are thus termed retroperitoneal. Like other serous surfaces, peritoneal structures are smooth and shiny when not diseased.
Omenta (greater and lesser) connect the stomach to other organs or to the body wall. Ligaments course from the body wall to an organ or from organ to organ. A mesentery in its broad definition runs from the abdominal wall to the intestine or female reproductive system. The peritoneum and its connected structures produce a small amount of fluid, which is useful in lubrication of mesothelial surfaces. This fluid does not contain fibrinogen and therefore does not clot on exposure to air, except in pigs and camelids.
The omenta are capable of localizing infection and serve as an important source of revascularization of surgically altered tissues. Unfortunately, they also serve as a blood supply to metastatic tumors (i.e., carcinomatosis). Horses in general have a small omentum and thus are less able to wall off peritoneal infections than are ruminants. Omentectomy does not appear to have an adverse effect on general health.
Pacinian Corpuscles
Pacinian corpuscles are baroreceptors that are commonly present in the pancreatic interstitium (see Fig. 8-87) and in the mesentery of cats. They are often visible macroscopically and may whorl in a fingerprint pattern (E-Fig. 7-1) or appear as solid masses resembling parasites (see Fig. 8-87).
E-Figure 7-1.

Pacinian Corpuscle, Pancreas, Cat.
Pacinian corpuscles are sometimes present in a whorled or “fingerprint” configuration. H&E stain.
(Courtesy Dr. C. Löhr, College of Veterinary Medicine, Oregon State University.)
Dysfunction/Responses to Injury
Gastrointestinal Aging
Aging changes in the alimentary system are generally subtle and not of clinical significance and are most often recognized in dogs. In the oral cavity, significant changes occurring with aging are lacking with the exception of plaque buildup, which is generally more severe and more prone to advance to periodontitis in smaller breeds of pet carnivores. A variety of factors may account for this, including dental crowding, softer diets, and malocclusions. The end result may be alveolar bone resorption and dental loss.
In the intestinal tract, especially in dogs, increasing age results in decreased secretion of saliva and gastric acids. Hyperplasia of the mucus glands of the esophagus and leiomyometaplasia of the intestinal smooth muscle are most commonly seen in dogs. Villus size tends to decrease, gastric emptying and intestinal turnover slows, motility decreases, and there are changes in the microbiota. These changes, however, are not generally related to the digestive or absorptive functions of the gut. Experimentally, lifelong calorie restriction results in increased longevity in a variety of species, including dogs.
Oral Cavity
The oral cavity serves an important function in preventing many harmful xenobiotic substances (i.e., foreign chemical substances within an organism that are not produced by or expected to be present in the organism) from entering the body. It does this through “mouth feel” and taste. Caustic substances, heat, and electricity may result in chemical erosions or ulcerations of the oral mucosa, but mucous membranes in general heal rapidly.
Antibiotic use may kill normal flora within the oral cavity. This change and/or high blood glucose concentrations via intravenous fluid administration or metabolic disturbance such as diabetes mellitus may allow for colonization by organisms not generally present. This outcome may result in a condition, sometimes called thrush, caused by a surface growth of Candida spp. (Figs. 7-7 and 7-8 ).
Figure 7-7.

Thrush (Oral Candidiasis), Tongue, Foal.
A, Hyphae of Candida albicans are growing in the superficial keratin of the tongue. H&E stain. B, Same specimen as A. Gomori's methenamine silver stain.
(Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Figure 7-8.

Thrush, Tongue, Foal.
A pseudomembrane of hyphae of candida is present on the dorsal surface. It has been scraped off the rostral end of the tongue (top) to reveal normal mucosa beneath the fungal mat.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Saliva contains electrolytes such as sodium, potassium, calcium, magnesium, chloride, bicarbonate, and phosphate; as well as iodine; mucus, which serves as a lubricant; antibacterial compounds such as thiocyanate and hydrogen peroxide; secretory IgA; epidermal growth factor (EGF); and the digestive enzymes α-amylase, lipase, and kallikrein. Antimicrobial enzymes secreted include lysozyme, lactoperoxidase, proline-rich proteins, class A and B acid phosphatases, N-acetylmuramoyl-l-alanine amidase, the reduced form of nicotinamide adenine dinucleotide phosphate (NAD[P]H) dehydrogenase (quinone), superoxide dismutase, glutathione transferase, class 3 aldehyde dehydrogenase, and glucose-6-phosphate isomerase. Saliva also contains a bacteria-rich flora and at least in human beings, opiorphin, an analgesic.
Teeth
Enamel is the only substance in the body incapable of turnover and repair. Advertisements by makers of toothpaste and other dental remedies notwithstanding, enamel is incapable of healing. Because enamel is deposited on teeth during amelogenesis (i.e., developmental formation of enamel on teeth) and is fully formed at the time of tooth eruption, pathogens and dietary supplementation such as those containing fluoride will not weaken or strengthen enamel once the tooth is erupted. Acid etching of enamel from vomition of gastric acid or eating and drinking of acidic substances such as carbonated beverages produces permanent loss of enamel.
In those species with hypsodont teeth, continual growth throughout life theoretically results in renewed occlusal surfaces to ensure grinding ability. In practice, however, continual growth has disadvantages such as uneven wear and the formation of ridges. For well-kept animals, this problem, especially in horses, is alleviated by mechanical evening of occlusal surfaces, a process known as “floating.” The current popularity of motorized tools for this purpose has resulted in inexperienced and/or unlicensed operators causing considerable damage by overzealous application. In those species with brachydont dentition, loss of occlusal surfaces is irreversible.
Tonsils
Because the tonsils lack afferent lymphatic vessels, they do not act as a lymphoid filter for oral structures. Infections may be blood borne or by direct contact with substances dissolved in saliva. Therefore the tonsils may serve as antigen samplers and may be affected by pathogens in blood or oral secretions. The initial multiplication of some enteric viruses (e.g., feline parvovirus) occurs within the tonsillar tissues. Most neoplasms that develop in the tonsils are either from the epithelium (squamous cell carcinomas) or the lymphoid tissue (lymphoma).
Salivary Glands
Injury to the salivary gland is accompanied by incomplete regeneration, principally from ductular epithelium. There are often atrophy, fibrosis, and squamous metaplasia of secretory epithelium, sometimes resulting in blockage of ducts.
Tongue
The tongue is an important part of the oral cavity and provides for the mixing action of saliva with xenobiotics so that the taste buds can determine if the ingested material is worthy of swallowing. Likewise, nerve endings in the tongue provide data about the digestibility of ingesta.
Esophagus
Horses are unable to vomit, which is an important mechanism for eliminating toxic or otherwise undesirable ingesta from the alimentary system. Esophageal healing is relatively rapid; the normal epithelial turnover rate is 5 to 8 days.
Rumen, Reticulum, and Omasum
The three compartments of the ruminant forestomach are the reticulum, rumen, and omasum. Folds and compartments subdivide the forestomach. Normal forestomach motility, and thus innervation, is critical in maintaining digestive homeostasis. The ruminant forestomachs are aglandular. The resident flora and fauna are responsible for digestion and fermentation of cellulose. In general, the rumen is a large fermentation vat where microorganisms break down ingesta by mechanical and chemical action into short-chain fatty acids that are directly absorbed across the epithelial lining into the blood. These fatty acids supply more than half of the energy from nutrients absorbed by the alimentary tract. The reticulum and omasum act mechanically to further reduce the ingesta to fine particles.
Stomach and Abomasum
The gastric epithelial layer is one cell thick, and the turnover rate is 2 to 4 days. The parietal cells produce rennin that coagulates milk protein, intrinsic factor for vitamin B12 absorption, and hydrogen chloride (HCl). The low luminal pH destroys many ingested pathogens, but there is a resident bacterial flora that cannot be cultured by conventional methods. Chief cells produce zymogen and pepsin involved in digestion of feedstuffs, and enteroendocrine cells produce serotonin, gastrin, ghrelin, somatostatin, endothelin, histamine, enteroglucagon, and others involved in hormonal regulation (see Box 7-1). Mucus cells produce bicarbonate and an unstirred protective layer on the cell surface
Intestine
Inflammation
Chronic injury of the lamina propria that results in dense cellular infiltration can cause diarrhea in a variety of ways, none of which are completely understood. These mechanisms include simple physical impairment of mucosal diffusion by space-occupying cells, with resultant disruption of the overlying epithelium causing increased permeability. Examples of these diseases in domestic animals are canine histiocytic ulcerative colitis (boxer colitis), Johne's disease (paratuberculosis) of ruminants, amyloidosis, and lymphoma.
Necrotizing Processes
Primary necrotizing processes of the lamina propria generally involve necrosis of the GALT with extension to the overlying epithelium. Examples of diseases with these lesions include bovine viral diarrhea (BVD) of cattle and Rhodococcus equi infection of horses.
Lymphangiectasia
Dilation of lacteals is idiopathic or secondary to obstruction of flow. These lesions are seen most commonly as part of the syndrome resulting from space-occupying lesions of the lamina propria, such as occurs in Johne's disease and in lymphoma. In both cases there is obstruction to outflow of lymph—a granulomatous lymphangitis and lymphadenitis in Johne's disease and tumors in the lamina propria and lymph nodes in lymphoma. Endotoxemia that results in vascular damage and disseminated intravascular coagulopathy can cause thromboemboli in small vessels and hemorrhage, necrosis, and ulceration of the intestine.
Disorders of Innervation
Agangliosis and dysautonomia, malfunction of the cranial nerves, spinal nerves, ganglia, and/or autonomic nervous system, can have profound influences on intestinal motility. There are a great variety of agents that cause these changes, ranging from botulinum toxin to inflammatory diseases. Many cases are idiopathic or may be hereditary. In addition, there is a bidirectional neurohormonal interchange between intestinal microbiota and the brain. Thus alteration of the microbiota may result in changes in the gut-brain axis. Dysbiosis (also known as dysbacteriosis), a state of microbial imbalances in the alimentary system, has effects on early brain development in mice, irritable bowel syndrome, Crohn's disease, ulcerative colitis, demyelination in multiple sclerosis, hepatic encephalopathy, and psychiatric disorders such as early-onset autism. Finally, the interstitial cells of Cajal are of mesenchymal origin and are the pacemakers of the gut. Inflammation or loss of these cells affects coordinated movement of the alimentary system.
Diarrhea
Diarrhea is defined as secretion of abnormally fluid feces accompanied by an increased volume of feces and an increased frequency of defecation. Pathogens causing diarrhea fall into three major categories: those that induce intestinal secretion, such as enterotoxic, or enterotoxigenic, Escherichia coli (ETEC) (noninflammatory or secretory diarrhea); those that induce inflammation, such as Lawsonia; and those that are invasive, such as Salmonella. To simplify this further, there are two mechanistic “types” of diarrhea, noninflammatory and inflammatory. Noninflammatory diarrheas are produced by organisms that disrupt the absorptive or secretory mechanisms of the enterocytes without destroying the cells. Usually, but not always, noninflammatory diarrheas affect the more proximal portions of the bowel (enterotoxic E. coli, rotavirus, and Cryptosporidium parvum). Inflammatory diarrheas are produced by organisms that produce cytotoxins or are invasive and activate cytokines that initiate inflammatory cascades. The inflammatory diarrheas generally affect the ileum, cecum, or colon (Salmonella, Brachyspira, and Lawsonia). Combinations of these mechanisms are present in most enteric diseases and are as follows:
-
•
Malabsorption with or without fermentation leads to osmotic diarrhea whether the cause is loss of digestive enzmes secondary to microvillus disruption, crypt or villus enterocyte death, or space-occupying lesions of the lamina propria. Generally this outcome is a problem of the small intestine, but secondary colonic malfunction can occur because of malabsorption of bile salts and fatty acids that stimulate fluid secretion in the large intestine. As examples, malabsorption occurs in rotavirus and coronavirus infections of neonates.
-
•
Chloride (Cl−) hypersecretion by the cystic fibrosis transmembrane regulator (CFTR) of a structurally intact mucosa. CFTR is regulated by kinases, which are dependent on cyclic adenosine monophosphate (cAMP), which acts as a second messenger. Prostanoids, bacterial toxins, and protein kinases all increase cAMP, thus increasing Cl− secretion. Calcium ion (Ca2+) also plays a role in opening Cl− channels by increasing acetylcholine interaction with epithelial muscarinic receptors via cholenergic nerves in intestinal plexi. Through a different mechanism but also involving the CFTR, bicarbonate secretion is also increased. This osmotic activity results in a net efflux of fluid and electrolytes independent of permeability changes, absorptive capacity, or exogenously generated concentration gradients (i.e., osmotic diarrhea). As examples, chloride hypersecretion occurs in enterotoxic E. coli diarrhea.
-
•
Exudation caused by an increased capillary permeability (protein-losing enteropathy) by leaky tight junctions between enterocytes. As examples, exudation occurs in some parasitic infections in which opening of the tight junctions allows macromolecules (antibodies) into the intestinal lumen.
-
•
Hypermotility generally is involved in diarrhea but usually not as a primary mechanism in domestic animals. Hypermotility is defined as an increased rate, intensity, or frequency of peristalsis. Theoretically, with decreased mucosal contact time, digestion and absorption of nutrients and water should be less efficient. It is suspected that decreased motility in some diseases allows for increased bacterial proliferation (Fig. 7-9 ). Conversely, some enterotoxins can stimulate intestinal motitlity in some motility disorders of human beings such as achalasia, Hirschsprung's disease, and inflammatory bowel disease. Diarrhea occurs when there is an alteration in the network of interstitial cells of Cajal within the smooth muscle of the bowel wall. Whether this is a cause or effect of bowel motility disorders is not known.
-
•
Toll-like receptors (TLRs) and related molecules produced by enterocytes and leukocytes are very important in the regulation of intestinal inflammation and in the host's response to intestinal pathogens. Intestinal inflammation can lead to neoplasia.
-
•
M cells regulate the presentation of antigens to GALT.
-
•
Other factors (prostaglandins, leukotrienes, and platelet-activating factor) act on enteric nerves to induce neurotransmitter-induced intestinal secretion by crypt cells.
-
•
Cell damage is possibly a consequence of inflammation mediated by T lymphocytes or proteases and oxidants produced by mast cells. T lymphocytes also may affect epithelial cell maturation, causing villous atrophy and crypt hyperplasia.
-
•
Cell death can result from pathogen invasion into enterocytes, multiplication of the pathogen, and extrusion of the affected enterocytes. These changes lead to notable distortion of villus architecture with a lack of mature absorptive enterocytes accompanied by nutrient malabsorption and osmotic diarrhea.
-
•
Mast cells of the lamina propria are in close association with enteric neurons and the enteric vasculature. They release histamine, prostaglandins, 5-hydroxytryptamine (5-HT), and proteolytic enzymes that play a role in diarrhea production.
Figure 7-9.

Mechanism of How Intestinal Bacterial Overgrowth Causes Malabsorption and Diarrhea.
1, Bacterial overgrowth results from a combination of increased ingestion of bacteria, dysfunction of intestinal loops, and reduced clearance of bacteria. These processes result in excessive multiplication of bacteria and thus bacterial overgrowth in the intestines. 2, Malabsorption and diarrhea occur as a result of bacterial overgrowth leading to bile salt deficiencies, excessive bacterial toxins, and overconsumption of resources by bacteria.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University; and Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
The nuts and bolts of the mechanisms listed are of course much more complicated. Pathogens enter or attach to enterocytes and may release enterotoxins. This action triggers the enterocytes to release cytokines (interleukin [IL]-8), which activate resident macrophages and recruit new blood-borne macrophages (e.g., monocytes) into the lamina propria. The activated macrophages release soluble factors (histamine, serotonin, adenosine) that increase intestinal secretion of chloride and water and inhibit absorption (Figs. 7-10 and 7-11 ). Recruitment of inflammatory cells to areas of injury results in release of a chemical milieu of cytokines (Fig. 7-12 ). Other factors (prostaglandins, leukotrienes, platelet-activating factor) act on enteric nerves to induce neurotransmitter-mediated intestinal secretion and hypermotility. The subsequent cell damage is possibly a consequence of inflammation mediated by T lymphocytes or proteases and oxidants secreted by mast cells (see Fig. 7-12). T lymphocytes also affect epithelial cell growth, producing villus atrophy and crypt hyperplasia. Cell death results from pathogen invasion, multiplication, and extrusion. The end result is marked distortion of villus architecture accompanied by nutrient malabsorption and osmotic diarrhea.
Figure 7-10.
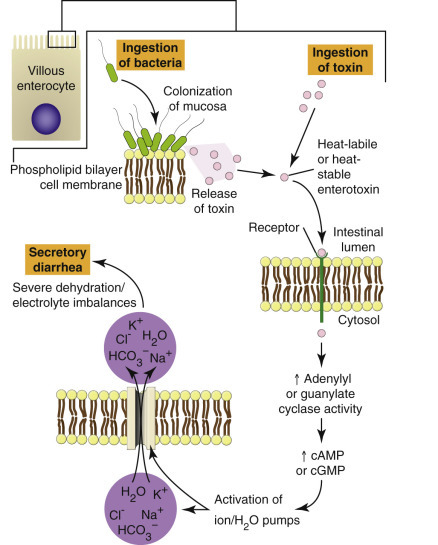
Mechanism of Action for Enterotoxin-Mediated Bacterial Diarrhea.
cAMP, Cyclic adenosine monophosphate; cGMP, cyclic guanosine monophosphate.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University; and Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Figure 7-11.
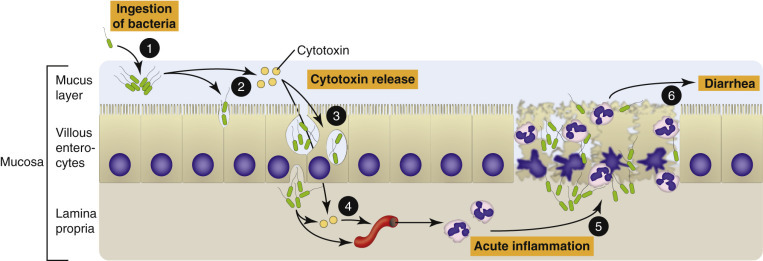
Mechanism of Invasive and Cytotoxin-Mediated Bacterial Inflammation.
1, Colonization of the mucosa. 2, Local production of cytotoxins and invasion of the mucosa by bacteria. 3, Bacteria replicate in large numbers and spread to adjacent epithelial cells. 4, Bacterial cytotoxins are released and injure adjacent mucosal endothelial cells and cause acute inflammation. 5, Acute inflammation results in necrosis of the mucosa. 6, Mucosal necrosis and bacterial toxins cause diarrhea.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University; and Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Figure 7-12.

Chemotactic Factors Active during Intestinal Inflammation.
ECF, Eosinophil chemotactic factor; IFN-γ, interferon-γ; IL, interleukin; LTB4, leukotriene B4; PAF, platelet-activating factor; TGF-β, transforming growth factor-β.
There are nonintestinal causes of diarrhea that must be considered in addition to diseases of the intestine. Among this group are hyperthyroidism, Addison's disease, pancreatic insufficiency, pancreatitis, chronic renal failure, and others. These diseases are discussed in their respective chapters of this book.
Consequences.
Normal feces are 75% water. Diarrheal feces are greater than 85% water. The consequence of excess fluid loss in the feces through diarrhea is dehydration. Dehydration results in hypovolemia. Hypovolemia results in hemoconcentration that results in inadequate tissue perfusion. Energy therefore is generated in tissue by anaerobic glycolysis. The resultant hypoglycemia leads to ketoacidosis. Acidosis is, by definition, a reduction in blood and tissue pH. Acidosis causes a reduction in pH-dependent enzyme system functions. Acidosis is compounded by fecal bicarbonate loss in diarrhea and the results of inadequate renal excretion of hydrogen ions and inadequate absorption of bicarbonate, which is a late effect of inadequate renal perfusion. The resultant electrolyte imbalance results in an increase in intracellular hydrogen ion concentration and a decrease in intracellular potassium ion concentration. The imbalances decrease neuromuscular control of myocardial contraction, leading to a further decrease in tissue perfusion. A vicious cycle results, culminating in hypovolemic shock.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
Ascites
Ascites or hydroperitoneum is defined as excess fluid in the peritoneal cavity. The quality of the fluid varies by cause from thick and syrupy in feline infectious peritonitis (FIP) to thin and watery in cases of hypoproteinemia (see Fig. 3-3). Ascites is nonspecific and can result from any cause of hypoproteinemia such as heart (see Fig. 10-6 and E-Fig. 10-10), liver, or kidney failure, protein-losing enteropathies such as Johne's disease, lymphangiectasia (Figs. 7-13 and 7-14, A, B ), lymphatic blockage, ruptured lymph ducts, bladder rupture (uroperitoneum), and hypertension. Evaluation of fluid obtained by abdominocentesis is very helpful in the live animal in sorting out the various causes.
Figure 7-13.

Ascites, Abdomen, Emaciation, Dog, Doberman Pinscher.
Protein-losing enteropathy, secondary to idiopathic intestinal lymphangiectasia resulted in hypoproteinemia and then ascites.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-14.

Lymphangiectasia, Jejunum, Dog.
A, Intestinal villi are expanded by ectasia of the lymphatic vessels (raised white areas). Lymphangiectasia can be a congenital developmental disorder of the lymphatic vessels, or it can be acquired secondary to lymph vessel obstruction caused by granulomatous or neoplastic diseases. B, Lacteals are dilated (asterisks), thus resulting in diminished lymph absorption by lacteals in the lamina propria and subsequent loss of protein (hypoproteinemia) and other nutrients into the intestinal lumen. H&E stain.
(A courtesy College of Veterinary Medicine, University of Illinois. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Fat Necrosis
There are four main categories of fat necrosis. They are nutritional, pancreatic, traumatic, and idiopathic, as follows:
-
•
Nutritional fat necrosis, also called steatitis or yellow fat disease, results in peroxidation of lipids, including those in cell membranes. It is most common in cats but occurs in a variety of species. The free radicals produced evoke an inflammatory response. The inciting cause is generally a diet very high in lipids and low in vitamin E or other tocopherols. Although steatitis of cats has historically been a sequela of fish-based diets, anecdotal evidence suggests that it may also be caused by some unconventional diets being used today.
-
•
Pancreatic or enzymatic fat necrosis is initiated by pancreatic enzyme release (lipase) from pancreatic necrosis (pancreatitis). Lipase converts triglycerides into fatty acids and glycerol. The fatty acids combine with calcium, magnesium, and sodium ions, forming soaps resulting in chalky white deposits (see Figs. 1-38 and 8-90). This is a painful condition, and free lipid droplets are sometimes seen in fluids recovered from abdominocentesis.
-
•
Traumatic fat necrosis results from direct, usually blunt, trauma to adipose tissue and is a relatively uncommon occurrence. Rupture of adipocytes releases triglycerides, which are hydrolyzed by tissue and/or serum lipases.
-
•
Idiopathic fat necrosis can be focal or massive and occurs in all species of mammal but is seen primarily in large animal species, especially in sheep, horses (Fig. 7-15 ), and obese dairy cattle. With massive necrosis in cattle the hard lumps of dense necrotic fat can envelop intestinal loops, resulting in stricture and functional blockage of ingesta. The cause of this condition is unknown but may relate in some way to nutritional imbalances.
Figure 7-15.

Idiopathic Fat Necrosis, Ventral Parietal Peritoneum, Horse.
This cross section of necrotic fat is mottled by a mixture of areas of saponification and normal adipocytes. The cause of this sporadic condition is unknown.
(Courtesy College of Veterinary Medicine, Cornell University.)
Damaged and necrotic adipose tissue frequently has a white, chalky or gritty appearance and texture caused by saponification and mineralization. Inflammatory cell presence and density vary based on the various causes of tissue damage and the area of fat sampled.
Inflammation: Peritonitis
Inflammation of the peritoneum, or peritonitis, is caused by a variety of agents varying from viral (feline infectious peritonitis) (Fig. 7-16 ) to bacterial (Fig. 7-17 ) to parasitic (ascarid migrations) (Fig. 7-18 ) to mechanical (hardware disease) to sterile (bile peritonitis) to organ rupture (Fig. 7-19 ). Peritonitis is also called serositis, and when multiple serous membranes like those of the meninges, joints, pleura, pericardium, peritoneum, and scrotum are affected, it is called a polyserositis. Glasser's disease of pigs is an example of a polyserositis (see Fig. 7-17). Different species vary in their stoicism and survival in the face of peritonitis, with horses showing the most pain and intolerance, whereas cattle and cats may live a long time with severe disease. The nature of the exudate includes those covered in Chapter 3 that result in suppurative peritonitis (Fig. 7-20 ) or fibrinous peritonitis (Fig. 7-21 ), as examples. Cytologic examination and bacterial culture are instrumental in determining a cause in the live animal. As in other diseases, the peritoneum responds to injury via acute inflammation (Fig. 7-22 ) and if needed, chronic inflammation (Fig. 7-23 ) and/or granulomatous inflammation (Fig. 7-24 ), if the source of the injury remains unresolved.
Figure 7-16.

Fibrinous Polyserositis, Abdomen, Cat.
Fibrin strands between viscera and mats of fibrin on organ surfaces are characteristic of the “wet form” of feline infectious peritonitis. The mesentery (below and left of the liver) has numerous white linear serpentine tracts, which are inflamed (type III hypersensitivity, immune complex) capillaries and venules. Note the small nodules (pyogranulomas) on the intestinal serosa and on the surface of the kidney.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-17.

Fibrinous Polyserositis, Abdomen, Pig.
Strands and clumps of fibrin are scattered throughout serosal surfaces. A milk-spotted liver is also present. Bacteria such as Haemophilus suis/parasuis (Glasser's disease), Actinobacillus suis, Streptococcus suis, or Escherichia coli can cause polyserositis.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-18.

Fibrinous Peritonitis, Abdomen, Pig.
The presence of fibrin in this pig's abdomen indicates that the intestinal rupture occurred antemortem. Ascarids are also present but do not help determine the time of rupture.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-19.

Fibrinous Peritonitis, Abdomen, Horse.
The presence of fibrin and ingesta adherent to serosal surfaces indicates antemortem perforation or rupture of the intestine.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-20.

Acute Suppurative Peritonitis, Bacterial Infection, Pig.
The surface of the peritoneum is rough and granular and covered with gray/white-yellow flecks of pus and fibrin. Red areas are indicative of active hyperemia and hemorrhage.
(Courtesy College of Veterinary Medicine, University of Illinois.)
Figure 7-21.

Fibrinous Peritonitis, Acute Inflammation, Bacterial Infection, Cow.
This lesion was the result of extensive damage to capillaries in the peritoneum leading to leakage of fibrinogen and polymerization to fibrin on peritoneal surfaces.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-22.

Acute Peritonitis, Peritoneum, Dog.
The mesothelial cells are swollen, vacuolated, and misshapen (arrowheads), indicating their response to injury. Capillaries under the mesothelial cells are dilated (active hyperemia and leukocyte adhesion cascade). Neutrophils are migrating through endothelial cell junctions and in the interstitium to reach the inflammatory stimulus in the abdominal cavity. Note the microabscesses in junctional spaces (arrows). H&E stain.
(Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Figure 7-23.

Chronic Peritonitis, Peritoneum, Cow.
Because the inflammatory stimulus in the abdominal cavity has persisted, the inflammatory response has shifted to a chronic exudate in an attempt to resolve the damage. Note the abundance of immature collagen fibers (arrows) in the areolar tissue of the peritoneum. H&E stain.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-24.

Granulomatous Peritonitis, Peritoneum, Tuberculosis, Cow.
In long-standing cases of tuberculosis, granulomas can form on the peritoneum.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Parasitic Peritonitis.
Aberrant migration of nematodes and trematodes in most species of animals can cause focal fibrosis in peritoneum and mesenteries when larvae travel through the abdominal cavity (see Fig. 8-52). Setaria, as an example, are nematodes that are sometimes found in the peritoneal cavity of ungulates and may cause mild focal peritonitis and rarely significant damage. Furthermore, a variety of cestodes may be found in the abdominal cavity of many animals. Some, such as Echinococcus granulosus (hydatid cysts) are zoonotic and may take 20 to 30 years to cause clinical signs in human beings. Mesocestoides and Porocephalus (pentastomiasis) are found in carnivores, where their migration may induce a pyogranulomatous reaction (Fig. 7-25 ).
Figure 7-25.

Mesocestoides Infection, Peritoneum, Dog.
Encysted larval cestodes (asterisks) have elicited a granulomatous inflammatory reaction (arrow) in the peritoneum of this dog. H&E stain.
(Courtesy Dr. C. Löhr, College of Veterinary Medicine, Oregon State University.)
Pneumoperitoneum
Spontaneous pneumoperitoneum is secondary to perforation of the GI or reproductive tracts. Causes include neoplasia, nonsteroidal antiinflammatory drugs (NSAIDs), and steroids. Traumatic pneumoperitoneum is caused by penetrating projectiles (e.g., bullets, knives, arrows), vehicular trauma, penetrating bite wounds, iatrogenic (surgery, peritoneal dialysis, positive pressure ventilation, urinary catheterization with penetration, penetrating gastrotomy, or percutaneous endoscopic gastrostomy [PEG] tubes), and idiopathic causes. Unless removed mechanically, it takes approximately 30 days for the air to be absorbed.
Portals of Entry/Pathways of Spread
There are limited numbers of ways that pathogenic agents gain entry into the alimentary system (Box 7-2 ). The most common, of course, is through ingestion. However, under certain circumstances, pathogens may be coughed up from the lungs into the pharynx and swallowed (R. equi in horses). Systemic blood-borne infections of viruses (viremia), bacteria (bacteremia), and systemic toxins (septicemia and toxemia) may make their way through the bloodstream and attach to specific receptors on the epithelial lining cells of the alimentary system. Parasites may migrate through various regions of the body to find a home within the mucosa or roam free in the lumen of the alimentary tract.
Box 7-2. Portals of Entry in the Alimentary System.
-
•
Ingestion
-
•
Coughed up from the lungs and swallowed
-
•
Systemic blood-borne infections
-
•
Parasite migration
Oral Cavity
Any substance placed in the oral cavity has the opportunity to affect the mucosa. The fact that oral infections are relatively rare is evidence supporting the efficacy of oral secretions and the epithelial barrier. Mechanical penetration of oral mucosa allows pathogens the opportunity to spread through submucosal tissues and enter vascular channels or draining lymphatic vessels. Although most pathogens are halted and killed during their travels, some need epithelial surfaces (bovine viral diarrhea virus) or lymphoid tissues (parvoviruses of carnivores) to multiply.
Teeth
Enamel is inert and thus does not play a role in pathogen multiplication or spread, nor can it heal. Domestic animal species seldom develop caries, but plaque accumulation and periodontal disease can lead to gum loss, inflammation, bone resorption, and loss of teeth.
Tonsils
Tonsils do not possess afferent lymphatic vessels and do not serve as lymph filters. Therefore only primary (or direct) or hematogenous infections occur (tonsillitis) (Fig. 7-26 ), as well as primary neoplasms of either the lymphoid (lymphoma) (Fig. 7-27 ) or epithelial (squamous cell carcinoma) (Fig. 7-28 ) components. In many viremias of mammals, such as pseudorabies of pigs, virus may be isolated from the tonsils.
Figure 7-26.

Necrotizing Tonsillitis, Tonsils, Dog.
The palatine tonsils are enlarged and discolored. The right tonsil is covered by a diphtheritic membrane (arrow), and the left tonsil is extensively ulcerated. Because there are no afferent lymphatic vessels to the tonsils, infection is either primary (by direct spread) or hematogenous.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-27.

Lymphoma (Lymphosarcoma), Tonsil, Dog.
Proliferation of malignant lymphocytes has expanded the tonsils so that they now protrude beyond their crypts and are pink-red because they are well vascularized.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-28.

Squamous Cell Carcinoma, Tonsil, Cat.
The right tonsil has been replaced by a large expansile neoplasm. The left tonsil is normal and remains in its crypt.
(Courtesy Dr. R. Storts, College of Veterinary Medicine, Texas A&M University.)
Salivary Glands
Salivary glands are generally affected by blood-borne pathogens, direct penetration by foreign objects, obstruction of the excretory ducts, or bite wounds. An important pathogen, rabies virus, is spread through saliva. In human beings, ascending infections from the salivary ducts occur, but there is no evidence that this occurs in domestic animals. The serous portions of the salivary glands are radiosensitive.
Tongue
Epitheliotropic viruses, many of which are foreign to the United States, such as foot-and-mouth disease, replicate in the epithelium of the oral cavity, including the tongue. Loss of lingual epithelium and exposure of nerves may result in pain, inappetence, ptyalism, and bruxism.
Esophagus
Materials, including caustic chemicals, from the oral cavity pass via the esophagus to the stomach or rumen. In the thoracic cavity, penetration or obstruction by foreign objects is the most common portal of entry into the mediastinum (Fig. 7-29 ). Some parasites spend part or all of their life cycles in the esophagus. Iatrogenic puncture of the esophagus is a not uncommon sequela to passage of stomach tubes. Gastric reflux is an additional portal of entry into the esophagus.
Figure 7-29.

Foreign Body with Necrosis, Esophagus, Dog.
A ham bone lodged in this dog's esophagus dorsal to the base of the heart has caused esophageal dilation and pressure necrosis of the esophageal mucosa.
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Rumen, Reticulum, and Omasum
The forestomachs in ruminants and camelids are dilations and modifications of the esophagus. They are designed to house a digestive flora necessary for producing short-chain fatty acids from forage that are subsequently directly absorbed into the bloodstream along with sodium and chloride. Most clinical disease of the forestomachs relates to disruptions in coordinated motility and changes in pH. Camelid forestomachs have glandular sacculations. Horses have stomachs that are divided into anterior stratified and aboral glandular portions. Pigs have only a small stratified portion that directly surrounds the esophageal os. The abomasum and C3 (a compartment comparable to the abomasum) of camelids function similarly to the stomachs of monogastric mammals.
Stomach and Abomasum
Gastric and abomasal ulcers occur in all species. Although the cause of ulcers, other than caustic agents and those caused by bacteria that can survive the extremely low pH of the stomach (Helicobacter spp.), is imprecisely understood, conditions necessary for ulcer development include local disturbances or trauma to the mucosal epithelial barrier, normal or high gastric acidity, and local disturbances to blood flow, including stress-induced and sympathetic nervous system–mediated arteriovenous shunts leading to ischemia. These physiologic changes allow pepsin and HCl into the submucosa. In addition, exogenous or endogenous steroids and NSAIDs depress prostaglandin E1 (PGE1) and prostaglandin E2 (PGE2), decreasing phospholipid secretions, which are gastroprotective, thus causing erosions and ulcers.
Intestine
Targets for Microbial Colonization or Destruction of Intestinal Mucosae
Mucosal targets include absorptive enterocytes, undifferentiated crypt cells, microvilli and glycocalyx, apical junctional complexes, unknown or nonspecific structures, and the lamina propria as illustrated in Figure 7-30 .
Figure 7-30.
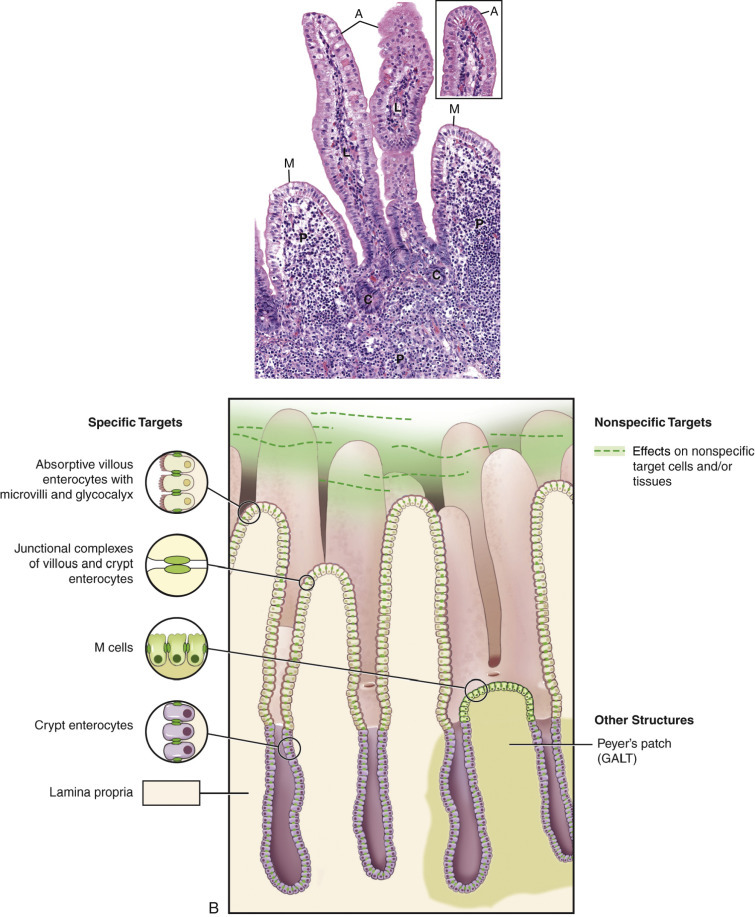
Targets for Microbial Infection in the Intestine.
A, Photomicrograph of small intestinal mucosae identifying targets for infection. Compare with schematic diagram illustrated in B.Inset, Higher magnification of villus tip enterocytes with a microvillus border. B, Schematic diagram illustrating targets for infection. A, Absorptive enterocyte; C, undifferentiated crypt cells; GALT, gut-associated lymphoid tissue; L, lamina propria: M, M cells; P, Peyer's patch.
(A and inset courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Diseases of the Intestinal Epithelium
A number of diseases are characterized by colonization or destruction of the epithelial components of the intestinal mucosa. Although the disease-producing effects of pathogens are complex and multifactorial, a simplified understanding of the principal cell under attack is helpful in predicting disease outcome and managing treatment.
Diseases of the Absorptive Enterocytes.
A number of agents have a tropism for the absorptive cells lining the intestinal villi. These agents include viruses such as rotavirus, enteric coronavirus, and the coronavirus of transmissible gastroenteritis of pigs. Intracellular bacteria and parasites can likewise invade and multiply in absorptive epithelial cells. Examples include the agents of swine dysentery (Brachyspira hyodysenteriae), coccidia, and cryptosporidium.
Some pathogens with a tropism for absorptive lining cells of the intestine cause destruction of these cells. This results in loss of enterocytes and at least temporary villous atrophy. The loss of the absorptive-digestive villous enterocytes causes maldigestion, and malabsorption results. Furthermore, because ingesta and normal alimentary secretions are unabsorbed, they are degraded further and fermented in the intestine by bacteria, increasing the osmolality of intestinal contents, with a subsequent increase in the fluid content of the bowel.
Because the regenerative crypt cells are not attacked by pathogens with tropism for villous enterocytes, diseases with villous enterocyte damage are not necessarily fatal. The denuded basement membrane contracts, causing villous atrophy. This contraction may be a function of the smooth muscle in the lamina propria. The functionally immature migrating crypt cells cover the villi. Often these immature cells become squamoid in an effort to cover the maximum area of basement membrane. However, if naked basement membranes contact each other, they will adhere, resulting not only in villous blunting but also in villous fusion, preventing the reformation of normal villi.
Diseases of Undifferentiated Crypt Cells.
Loss of the undifferentiated epithelial cells in the base of the crypts means loss of the cells capable of mitosis, and thus regeneration of the epithelium is impaired. Therefore the clinical effect of crypt cell loss can be delayed for several days because the villi are initially still covered by enterocytes. This type of loss is more severe and often fatal, compared with villous enterocyte loss. Agents that target and destroy crypt cells are called radiomimetic because they mimic the effects of radiation on the rapidly dividing enterocytes. Examples of these agents include the parvoviruses of carnivores, bovine viral diarrhea virus, rinderpest virus, and some mycotoxins such as vomitoxin.
Enterotoxic E. coli infection of neonatal pigs, calves, lambs, and human beings causes what is known as a secretory diarrhea. These bacteria are able to colonize the small intestinal enterocytes by way of their surface or pilus antigens, which anchor them to the enterocytes. Different pilus antigens adhere to glycoconjugate receptors on enterocytes in different regions of the small intestine. Thus these bacteria are not washed out by peristalsis. Because the enterocytes are not damaged, no lesions are observed, although microscopically the bacteria can be seen attached to the epithelial surface. The bacteria produce a toxin that causes enterocytes to secrete water and electrolytes. Although cAMP and cyclic guanosine monophosphate (cGMP) mediate this process, the exact mechanism by which this secretion occurs is unknown. Some secretions, especially those of Cl−, occur via the crypt cells. Intestinal secretion exceeds the ability of the colon to absorb the surplus fluid. The net result is diarrhea.
Abnormalities of the Microvilli and Glycocalyx.
Because the microvilli and glycocalyx on villous enterocytes are largely responsible for the immense surface area and the enzymes responsible for nutrient digestion and absorption, it follows that damage to either of these structures can result in intestinal malfunction and resultant diarrhea. A prime example of this is human lactose intolerance. Such persons lack lactase in the glycocalyx. Because of this lack, they are unable to digest lactose from dairy products. The lack of lactase results in failure of uptake of milk sugar, and the lactose is fermented by bacteria in the colon. This results in an osmotic drain of fluid into the gut with resultant diarrhea. Thus the malabsorption in this case is limited to a single substrate. Histologically the intestine is normal.
Some bacteria, such as attaching and effacing E. coli, damage microvilli by their attachment. This attachment disrupts enzyme systems housed in microvilli and the glycocalyx and causes diarrhea. The antibiotic neomycin can similarly cause fragmentation of microvilli and destruction of the glycocalyx with resultant diarrhea. Cessation of neomycin therapy results in a return to normal structure and function.
Diseases in Which the Epithelial Targets Are Unknown or Nonspecific.
In a number of enteric diseases the targeted epithelial cell is unknown or nonspecific. Clostridium perfringens type C is a pathogen of neonatal pigs, lambs, calves, and foals. Unlike enterotoxic E. coli, which produces a toxin affecting enterocytes, C. perfringens produces a nonspecific cytotoxin. This toxin causes necrosis of villous absorptive cells, which then extends to the lamina propria and blood vessels. The result is massive and acute necrohemorrhagic enteritis.
Separation of Apical Junctional Complexes.
Apical junctional complexes, also called tight junctions or zona occludens, join enterocytes to each other. Transmembrane proteins, such as claudin, occludin, tricellulin, junction-associated molecules, and the coxsackievirus and adenovirus receptor (CAR), form tight junctions. Normally these junctions are a barrier to macromolecular transepithelial transport. In certain diseases, such as ostertagiasis, Salmonella typhimurium in vitro, C. perfringens, alimentary anthrax, and enterohemorrhagic E. coli, these tight junctions are pathologically opened through effects of bacterial toxins and products on transmembrane proteins, allowing transport of macromolecules into the intestinal (abomasal) lumen. This opening of tight junctions is also important in allowing macromolecules, such as immunoglobulin, into the lumen, where the pathogen can be attacked.
Diseases of the Lamina Propria
Lesions within the lamina propria can be infiltrative, necrotizing, or vascular, all of which can cause diarrhea even though the epithelium is not the primary cell type injured.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
Most infections of the peritoneal cavity are traumatic in origin from a rupture in the alimentary, urinary, or reproductive systems. Extension from organ infection or neoplasia is another common source of introduction of foreign agents into the peritoneum. Traumatic injury to a body wall, such as by a projectile, can introduce foreign material or air (pneumoperitoneum). Traumatic injury to a vessel or to an organ or rupture from a tumor or ingestion or administration of anticoagulants may cause hemoperitoneum. The liver is particularly prone to rupture when infiltrated by fat or amyloid.
Defense Mechanisms/Barrier Systems
Considering the types of materials that are ingested by domestic animals, it is significant that they are not constantly ill. This resistance to disease occurs because the alimentary system is well suited to protect itself against most potentially pathogenic insults (Box 7-3 ). These protective mechanisms include oral secretions, such as saliva; “normal” resident flora and fauna; the gastric pH; opening of tight junctions between intestinal cells to allow macromolecules, such as immunoglobulins, into the lumen; vomiting; secretions from the liver and pancreas; intestinal proteolytic enzymes, macrophages, and other effector cells, such as neutrophils, within the submucosa, which are exuded into the alimentary lumen; the high rate of epithelial turnover; increased peristalsis resulting in diarrhea; Paneth cells; and the immune system. Paneth cells produce antimicrobial peptides and proteins, including lysozyme and secretory phospholipase A2. They also produce α-defensins (cryptdins).
Box 7-3. Defense Mechanisms in the Alimentary System.
-
•
Taste buds
-
•
Vomiting
-
•Saliva
-
•Flushing action so potential pathogens are cleared from the oropharynx
-
•Protective coating of the mucosa
-
•Contains antimicrobial lysozyme, lactoferrin, lactoperoxidase, and immunoglobulins
-
•
-
•
Gastric pH
-
•Microbiota/microbiome—lower GI tract (damaged by toxicants; carcinogen activation)
-
•100 trillion (anaerobic) bacteria (10 × host); 3.3 million genes (150 × host)
-
•Bacteriocins
-
•Compete for nutrients
-
•Compete for attachment sites
-
•Promote immune system maturation
-
•Biotransformation
-
•Enterotype
-
•
-
•
Secreted immunoglobulins
-
•Extraintestinal secretions from the liver and pancreas
-
•Lactoferrins
-
•Peroxidase
-
•
-
•
Intestinal proteolytic enzymes
-
•
Intestinal biotransforming and metabolic enzymes
-
•
Phagocytes and other effector cells within the submucosa
-
•
High rate of epithelial turnover
-
•
Shedding of receptor-laden ALP and catalase-containing vesicles from microvilli
-
•
Large surface area
-
•
Dilution with ingesta
-
•
Increased peristalsis resulting in diarrhea
-
•
Mucus—contains phages that destroy bacteria > 1 × 104
-
•
Paneth cells (antimicrobial peptides, lysozymes, phospholipase A2, defensins-cryptdins)
-
•
Innate lymphoid cells
-
•
Adaptive immune system
-
•
Kupffer cells (liver)
-
•
Genetic polymorphisms (HLA) and host gene expression.
ALP, Alkaline phosphatase; GI, gastrointestinal; HLA, human leukocyte antigen.
Oral Cavity
Defense mechanisms of the oral cavity include the stratified epithelial surface that is resistant to trauma and some irritants; taste buds, which reject potentially toxic materials based on taste and tongue feel; an indigenous bacterial flora that occupy attachment sites that would otherwise be available to pathogens; and saliva. Saliva provides a flushing action, so potential pathogens are cleared from the oropharynx and swallowed. Saliva also forms a protective coating of the mucosa and contains antimicrobial lysozyme in the zymogen granules of serous cells and immunoglobulins, especially IgA, in a manner analogous to cryptal enterocytes of the intestine, through the production of a secretory component. Migration through the alimentary tract, including the oral cavity, eliminates neutrophils at the end of their life span. In their absence, stomatitis results.
Teeth
In spite of the biophysical resistance of enamel and cementum to most pathogens, plaque accumulates on dental surfaces and may cause regression of gingiva (gingival recesses) as a result of bacterial colonization and inflammation (see Disorders of Domestic Animals, Teeth, Periodontal Disease).
Tonsils
The tonsils sample antigens dissolved in saliva and develop immune responses similar to other lymphoid tissues in the body. Barrier protection to the tonsils is provided by nonkeratinizing, stratified squamous epithelium.
Salivary Glands
Saliva contains electrolytes such as sodium, potassium, calcium, magnesium, chloride, bicarbonate and phosphate; iodine; mucus, which serves as a lubricant; antibacterial compounds such as thiocyanate and hydrogen peroxide; secretory immunoglobulin A; EGF; and the digestive enzymes α-amylase, lipase, and kallikrein. Antimicrobial enzymes secreted include lysozyme, lactoperoxidase, proline-rich proteins, class A and B acid phosphatases, N-acetylmuramoyl-l-alanine amidase, NAD(P)H dehydrogenase (quinone), superoxide dismutase, glutathione transferase, class 3 aldehyde dehydrogenase, and glucose-6-phosphate isomerase. Saliva also contains a bacteria-rich flora and at least in human beings, opiorphin, an analgesic.
Tongue
The thick, nonabsorptive, nonkeratinizing, stratified squamous epithelial barrier of the tongue is protective against most xenobiotics. Epitheliotropic viruses, direct penetrating wounds, and caustic agents can damage the epithelium. The tongue also manually removes substances from oral surfaces.
Esophagus
The lining stratified squamous epithelium of the esophagus is keratinized in pigs, horses, and ruminants and nonkeratinized in dogs and cats (carnivores). The epithelial cell turnover rate is 5 to 8 days; therefore healing is relatively rapid. The muscularis is striated in ruminants and dogs, smooth in horses (distal third), which are unable to vomit, and variably mixed in other species. Submucosal mucus glands are present throughout the esophagus in pigs and dogs and at the pharyngeal junction in cats, horses, and ruminants.
Rumen, Reticulum, and Omasum
A thick keratinizing stratified squamous epithelial lining provides protection against xenobiotics, including ingested roughage in the rumen, reticulum, and omasum. There is no secretory apparatus (i.e., goblet cells) in ruminant forestomachs such as in the abomasum, but absorption of volatile fatty acids occurs across the epithelium. The rich “normal” flora (i.e., microbiota) and alkaline pH provide a mechanism for preventing colonization by and multiplication of pathogens.
Stomach and Abomasum
The gastric mucosal barrier is significant in preventing autodigestion and bacterial overgrowth. There is, however, a resident flora that is difficult to grow on artificial media. Microorganismal overgrowth is prevented under normal physiologic conditions by abomasal or gastric motility, PGE2, a protective layer of mucus and bicarbonate, secretory IgA, transforming growth factor-α (TGF-α), epidermal growth factor, an extremely acid luminal pH, and an effective pyloric sphincter that prevents regurgitation into the stomach or abomasum of duodenal, hepatic, and pancreatic secretions. An intact epithelial layer and adequate blood flow also prevent acid-induced damage.
Intestine
Defense mechanisms of the intestinal tract are diverse. They include indigenous (nonpathogenic) bacterial flora, intestinal and extraintestinal secretions, gastric acidity, intestinal motility, epithelial cell turnover, bile salts, immunologic mechanisms, and although a secondary mechanism, the Kupffer cells of the liver.
Secretions of the oral cavity, saliva, and intestine, called mucins, inhibit the adherence of organisms to the mucosa of the alimentary system. In addition to physically trapping pathogens, intestinal mucus serves to cover glycolipid and glycoprotein receptors on the surface of enterocytes (unstirred layer), thus preventing pathogen attachment and damage by toxins. Mucins are viscous and thus aid in protecting the epithelium from the shear forces of particulates driven against them by peristaltic waves. Because they are extensively glycosylated, mucins can cross-link and trap bacteria, making them more amenable to clearance by passage through the alimentary system. Mucus also contains bacteriophages (i.e., viruses that infect and replicate within bacteria) that destroy bacteria, reducing the population by more than 1 × 104.
Normal gastric acidity kills many organisms before they have the chance to reach the small intestine. Very young animals are achlorhydric; thus they may be more susceptible to some organisms such as pathogenic E. coli. Helical bacteria in the stomach are the single greatest cause of gastric ulcers in human beings. Although similar organisms occur in the stomachs of domestic animals, particularly carnivores, their role in gastritis of animals is less certain. Normal gastric acidity apparently does not kill all potentially pathogenic bacteria (helical bacteria) in the stomach and proximal small intestine of domestic animals.
Indigenous (nonpathogenic) bacterial flora (microbiota) competitively bind to putative attachment sites on the enterocytes, thus preempting pathogen attachment. These prokaryotic symbionts coevolved with their hosts and are an integral part of homeostatic mechanisms. Killing of these bacteria through the use of antibiotics sometimes allows pathogens to colonize the intestine and produce disease. Thus gnotobiotic animals are more susceptible to infection. The microbiome enhances the host's genome in contributing to normal physiologic functioning and disease resistance and susceptibility. Bacteria in the intestine outnumber the total somatic and germ cells of the body by approximately a factor of 10. Probiotics are “friendly bacteria” that are sometimes used therapeutically or prophylactically in a variety of products and nutraceuticals. These “friendly bacteria” also compete for substrate with pathogens, alter the microenvironmental pH, making the growth of competitive bacteria difficult, and produce short-chain fatty acids and inhibitory growth substances (bacteriocins) that are toxic to other bacteria. Colicins are bacteriocins produced by E. coli. Bacterial growth is also inhibited by lactoferrin and peroxidase from the pancreas and lysozyme and defensins from Paneth cells. Transferrin in serum and lactoferrin produced by enterocytes and neutrophils at sites of infection serve to sequester iron that is necessary for bacterial growth.
Intestinal peristalsis is protective in that loss of motility may lead to bacterial overgrowth in the intestine and increased susceptibility of enterocytes to toxins that are not moved out of the gut. Diarrhea can be in part a defense mechanism that rids the body of bacteria and toxins. Conversely, some bacteria secrete toxins that impair intestinal motility, thus allowing pathogens a greater opportunity to attach to enterocytes.
Epithelial cells of the intestine have the greatest turnover rate of any fixed-cell population in the body. In effect, this means that pathogens with a life cycle that exceeds that of the enterocytes will likely not be successful because their host cell will slough before the pathogen can reproduce. In addition, experimental evidence indicates that enterocyte microvilli form unilaminar vesicles containing digestive enzymes such as catalase and alkaline phosphatase on their surface. These vesicles are shed into the intestinal lumen, where they may interact with the pathogen(s), thus preventing contact of pathogens with enterocyte receptors because these vesicles are passed in the feces.
Bile salts inhibit the growth of many organisms. Kupffer cells of the liver act as a secondary line of defense. Because all the blood from the intestine enters the portal vein and percolates through the hepatic sinusoids, the Kupffer cells are perfectly positioned to phagocytose bacteria and endotoxins with which they come in contact. In pigs, goats, and cattle (artiodactyls), these functions are performed by intravascular pulmonary macrophages.
Secretory IgA and IgM constitute very important mechanisms of humoral immunity and function largely to prevent attachment of pathogens to intestinal epithelium. Crypt epithelial cells produce the secretory component of IgA. IgA functions through adhesion to M cells that regulates transepithelial movement of antigens while masking certain other antigens (Fig. 7-31 ).
Figure 7-31.

Immunoglobulin Secretion in the Intestine.
Dimeric immunoglobulin A (dIgA), produced by plasma cells via interaction with polymeric IgR (PIgR) is transported across the intestinal epithelium in association with secretory component, which is a portion of PIgR secreted into the intestinal lumen. IgG transport is mediated by major histocompatibility complex class I (neonatal Fc receptor [FcRn]). IgG transport is bidirectional; IgA is not. M, Microfold.
Although in its infancy, research indicates that genetic polymorphisms of the host, including human leukocyte antigen (HLA), likely play a role in disease susceptibility and resistance.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
Mesothelial cells produce a lubricant to allow serosal surfaces to slide easily against each other and prevent tumor cell adhesion. Mesothelial cells are also actively phagocytic, transport fluid and cells across serosal surfaces, and play a role in antigen presentation, inflammation, tissue repair, coagulation, and fibrinolysis.
Disorders of Domestic Animals2
Oral Cavity
The oral cavity is one of the places that can be examined directly by the clinician and pathologist and where they can use the same criteria for determining abnormality. The same can be said of the rectal mucosa.
Developmental Anomalies
There are a wide variety of developmental abnormalities in the oral cavity. Some are incompatible with life unless surgically corrected. Only a few of these congenital lesions have a proven hereditary component. Most are idiopathic. Thorough physical examination of neonates must include examination of the oral cavity for these defects.
Palatoschisis, or cleft palate, and cheiloschisis, or cleft lip, are among the most common developmental abnormalities of the oral cavity. Cheiloschisis is sometimes referred to as hare lip because this is a normal feature of the rabbit. It is a failure of fusion of the upper lip along the midline or philtrum. Palatoschisis can be genetic or toxic in origin. It results from a failure of fusion of the lateral palatine processes. It can be caused by steroid administration during pregnancy in primates, including human beings. Depending on the size of the defect, which may involve only the soft palate or both the soft and hard palates (Fig. 7-32 ), the lesion may be surgically correctable. It is a matter of some ethical concern whether to correct such defects without also sterilizing the patient because of the potential for cleft palate to have a genetic cause. Important sequelae to the host from cleft palate are starvation, as the result of the inability of the nursing animal to create a negative pressure in the mouth with a resultant failure to suckle, and aspiration pneumonia, because no effective separation is present between the oral and nasal cavities.
Figure 7-32.

Palatoschisis and Cheiloschisis, Hard and Soft Palate, Puppy.
The lateral palatine processes have failed to fuse during the first trimester of gestation (palatoschisis). In dogs, palatoschisis has been attributed to genetic abnormalities, excessive intake of vitamin A during gestation, and the administration of cortisone during gestation. The upper lip is also cleft (cheiloschisis).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Stomatitis and Gingivitis
Stomatitis and gingivitis refer to inflammation of the mucous membranes of the oral cavity and gingiva, respectively. Because the oral cavity is constantly bombarded with ingested substances that are moved around by the tongue, the final result of a variety of insults to the lining of the oral cavity is a loss of mucosa—erosions, ulcerations, and necrosis. Thus, although inflammation is apparent, clues as to the initiating process may be absent. Lesions may be at different stages and are commonly classified as macules, papules, vesicles, erosions, abscesses, granulomas, and ulcers. These lesions can be caused by infectious agents, particularly viruses; chemical injury; trauma; intoxicants; or autoimmune or systemic disease. They often result in anorexia caused by painful mastication. Hypersalivation (ptyalism) is also apparent, whether from overproduction or a failure to swallow. In the cat, gingivitis is the first and most consistent sign of feline immunodeficiency virus (FIV) infection (immune system failure) associated with a reduction in CD4 lymphocytes, thymic atrophy, and lymph node atrophy.
Vesicular Stomatitides—Viral Diseases
Although vesicular stomatitis correctly refers to oral vesicles and blisters, the term is generally reserved for those lesions caused by epitheliotropic viruses. The vesicular stomatitides are listed in Table 7-1 . Their genesis is from virus-induced epithelial cytolysis attended by fluid accumulation and subsequent rupture of the resultant vesicle. Blistering or vesiculation of the oral epithelium is present early in the course of these diseases. All of these diseases are virus induced, and all have identical appearances at gross and histopathologic examination. None of these conditions is fatal. They produce great economic loss because of poor weight gain in affected animals and sometimes abortions in gravid females. The exact cause of the abortions is unknown, but it is probably related to the stress induced by the painful oral, cutaneous, and pedal (hoof or foot) lesions. Secondary bacterial invaders, both Gram-negative and Gram-positive, of these lesions can result in endotoxemia. Several diseases, such as foot-and-mouth disease and vesicular exanthema, affect the coronary bands of the digits and interdigital clefts, resulting in lameness. Some of these diseases (foot-and-mouth disease, vesicular exanthema, and swine vesicular disease) are exotic to the United States and thus are reportable to state or federal authorities, or both, if the clinician or pathologist suspects the disease. This requirement is due to the great expense involved in eradicating these diseases from the United States and their potential use as agents of agroterrorism. Nontariff export/import barriers designed to prevent the introduction of highly contagious agents, such as foot-and-mouth disease, into animal populations of countries with which we trade, are often put in place.
Table 7-1.
Vesicular Stomatitides
| Disease | Cause | Ruminant | Pigs | Horses |
|---|---|---|---|---|
| Foot-and-mouth disease | Picornavirus | + | + | − |
| Vesicular stomatitis | Rhabdovirus | ++ | + | + |
| Vesicular exanthema of swine | Calicivirus (vesivirus) | − | ++ | − |
| Swine vesicular disease | Enterovirus | − | ++ | − |
+, Species in which disease occurs; −, species in which disease does not occur.
The gross lesions of the vesicular stomatitides are epithelial. Fluid-filled vesicles are present in the oral cavity, lips, rostral palate, tongue, and planum nasale (Fig. 7-33, A ). Entry of virus in these cases is most likely oral into areas of temporary loss of mucosa as the result of normal mastication and trauma. The viruses are cytolytic, and the resultant release of virus from cells infects neighboring cells. The lesions enlarge centripetally, forming vesicles. Bullae result from coalescence, resulting in erosions and ulcers. These ulcers are typically hyperemic (see Fig. 7-33, B). Viremia, often transient, sometimes occurs.
Figure 7-33.

Cutaneous Vesicles, Vesicular Exanthema, Snout, Pig.
A, Vesicles, both intact (upper vesicle) and ruptured (lower vesicle), are present on the planum nasale and are caused by the infection of injured mucosal epithelial cells with vesicular exanthema of swine virus, a calicivirus (vesivirus). B, Ruptured vesicles with cutaneous ulceration, vesicular exanthema (later stage of the disease). Note the ruptured vesicles, which can cause pain, resulting in inappetence.
(A from Gelberg H, Lewis RM: Vet Pathol 19:424-443, 1982. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Similar vesicular lesions occur in the nasal mucosa, particularly in pigs with vesicular exanthema and in the proximal epithelium of the alimentary system (esophagus and rumen) of cattle with foot-and-mouth disease. Some animals have conjunctivitis and vesicular dermatitis of the teats and vulva. The microscopic lesions of these four diseases (foot-and-mouth disease, vesicular stomatitis, vesicular exanthema, and swine vesicular disease) are similar. Virus-induced, intracellular edema progresses to swelling of the cells of the stratum spinosum, cell lysis and intercellular edema, and resultant vesicles. The epithelium overlying the virus-rich vesicular fluid is thin, and even slight friction can rupture vesicles and bullae, creating an ulcer. Healing of the ulcer progresses from the usual fibrin- and/or neutrophil-rich acute stages (scab) to the more chronic stages of granulation.
Lesions and signs of the vesicular stomatitides include vesicles, bullae, and detachment of patches of epithelium with resultant raw ulcers, ptyalism, lameness, fever, and anorexia. Besides the lesions that develop from the initially infected cells, the virus spreads centripetally to adjacent susceptible epithelium, causing repeated episodes of this infectious, lytic cycle. The vesicular stomatitides are tentatively diagnosed based on the clinical signs and lesions resulting from oral and nasal ulceration, conjunctivitis, and ulceration of the genitalia and mammary glands. Lameness is secondary to hoof involvement that is focused at the coronary band. Definitive diagnosis is important and performed at federal laboratories equipped to rapidly respond to suspected outbreaks. Federal quarantine of infected herds is an important control mechanism, followed by eradication, slaughter, and carcass disposal.
Foot-and-Mouth Disease.
Vesicular Stomatitides
Vesicular Stomatitis.
Vesicular stomatitis is common in calves, pigs, and some wildlife species but does not occur in sheep or goats. It is the only vesicular disease to which horses are susceptible. In northern latitudes, it is generally a warm weather disease, suggesting that insects act as vectors. As the name implies, vesicles in the oral cavity characterize the disease. Clinically the disease is often recognized by inappetence in the affected animal, accompanied by ptyalism.
Other Vesicular Stomatitides.
Vesicular exanthema is a specific disease of pigs that is indistinguishable clinically and pathologically from foot-and-mouth disease. This disease is uniquely American and was believed eradicated from pigs in 1956 through enactment of federal laws requiring the cooking of garbage fed to pigs. The evidence indicates that vesicular exanthema of pig serovars are variants of San Miguel sea lion virus. This latter marine calicivirus (vesivirus) occurs in coastal sea lion and fur seal populations from California to Alaska (E-Fig. 7-2). Swine vesicular disease is indistinguishable from the other vesicular stomatitides and is exotic to the United States. Efforts are underway to develop DNA microarrays to facilitate rapid identification of specific vesicular diseases from a single sample.
E-Figure 7-2.

Cutaneous Vesicles, San Miguel Sea Lion Virus Infection, Foreflippers, Northern Fur Seal.
On the nonhaired portion of the foreflipper are vesicles both intact (arrow) and ruptured, caused by the infection of injured mucosal epithelial cells with San Miguel sea lion virus, a calicivirus (vesivirus). These vesicles will rupture with trauma, resulting in cutaneous erosion and ulceration.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Erosive and Ulcerative Stomatitides
Erosions are defined by a loss of part of the thickness of the surface epithelium, whereas ulcers are full-thickness epithelial losses exposing the basement membrane. Thus erosions may progress to ulcers, which in hollow organs may become perforating ulcers. Erosive and ulcerative stomatitis can have a variety of causes. Agents responsible include the viruses of bovine viral diarrhea (Fig. 7-34 ), rinderpest, malignant catarrhal fever (Fig. 7-35 ), feline calicivirus, and bluetongue, and in horses, NSAIDs. Other causes include uremia (Fig. 7-36 ); ingested foreign bodies, such as foxtail awns; the feline eosinophilic granuloma complex; and vitamin C deficiency in primates and guinea pigs (E-Fig. 7-3). Often the oral lesions must be evaluated in the context of the clinical signs, together with histopathologic findings and ancillary testing, to arrive at a definitive diagnosis. Additionally, the vesicular stomatitides can progress to ulceration secondary to abrasion to the point that they cannot be distinguished from the ulcerative stomatitides.
Figure 7-34.

Erosions and Ulcers, Bovine Viral Diarrhea (BVD) Virus Infection, Hard Palate, Cow.
Erosions and ulcers (small red areas on mucosal surface) caused by this pestivirus are particularly evident on the mucosal epithelial surface of the caudal hard palate. These lesions are characteristic of the ulcerative stomatitides, which, unlike the vesicular disease viruses, do not form vesicles.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-35.

Erosions and Ulcers, Malignant Catarrhal Fever, Hard Palate, Dental Pad and Buccal Papillae, Cow.
The erosions and ulcers (red areas on mucosal surface) are due to malignant catarrhal fever virus, a herpesvirus, but are characteristic of many ulcerative stomatitides.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-36.

Uremic Ulcers, Hard Palate, Dog.
Ulcers present on the transverse palatine ridges and periodontal gingiva are secondary to vascular damage associated with increased concentrations of plasma blood urea nitrogen and creatinine from kidney failure. Affected animals often have an ammoniacal or uremic odor to the breath.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
E-Figure 7-3.

Ulcerative Gingivitis Secondary to Scurvy (Vitamin C Deficiency), Gingiva, Monkey.
There is a deep ulcer at the commissure of the mouth and smaller ulcers periodontally. Vitamin C deficiency in primates and guinea pigs can result in gingival erosions and ulcers and even tooth loss.
(Courtesy College of Veterinary Medicine, University of Illinois.)
Parapox Stomatitides
Necrotizing Stomatitides
Necrotizing stomatitis occurs in cattle, sheep, and pigs. In cattle it is sometimes referred to as calf diphtheria (Fig. 7-37 ). Necrotizing stomatitis is the end stage of all other forms of stomatitis when they are complicated by infection with Fusobacterium necrophorum, a filamentous-to-rodlike-to-coccoid, Gram-negative anaerobe. Bacterial toxins are responsible for the extensive lesions. Necrotizing stomatitis is characterized by yellow-gray, round foci surrounded by a rim of hyperemic tissue in the oral cavity, larynx, pharynx, or tongue. Well-demarcated foci of coagulation necrosis typify the histologic appearance of necrotizing stomatitis. As might be expected in foci of inflammation, there is a circumferential rim of leukocytes and hyperemia. Clinical signs include swollen cheeks, inappetence, pyrexia, and halitosis. Infection may become systemic if severe, resulting in lesions throughout the alimentary system and associated lymphoid tissue.
Figure 7-37.

Necrotizing Stomatitis, Calf Diphtheria, Tongue, Calf.
The dorsal surface of the tongue is ulcerated, and the ulcers are covered by a yellow-white diphtheric membrane. Calf diphtheria is caused by infection with the bacterium Fusobacterium necrophorum secondary to abrasion and/or trauma to the mucosal epithelium of the oral cavity or larynx.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Noma is a severe form of oral ischemic necrosis with lesional spirochetes and fusiform bacteria. Although rare, it is seen most often in primates, including human beings, and dogs. It is characterized by severe necrotizing gingivitis that can extend into adjacent bone, causing osteolysis and sometimes death.
Ulcerative gingivitis (trench mouth), caused by anaerobic spirochetes, affects human beings, some nonhuman primates, and rarely, puppies. In addition to Fusobacterium spp., Borrelia vincentii may be causative. Debilitated animals and those with intercurrent infections are at increased risk for these secondary invaders, which may be part of normal oral flora. Similar clinically to necrotizing stomatitis, ulcerative gingivitis is characterized by acute inflammation and necrosis, oral ulceration and pain, halitosis, a fragile oral mucosa, and ptyalism. The morphologic diagnosis is an acute, necrotizing gingivitis. Unlike the case in necrotizing stomatitis, the causative agents are readily identified by tissue smears or by culture.
Eosinophilic Stomatitides
Oral granulomas or ulcers (“rodent ulcers”) occur frequently in cats. Similar lesions occur sporadically in a variety of canine breeds. In cats they are termed oral eosinophilic granulomas. Although the cause of this condition is unknown, the histologic appearance of lesions suggests an immune-mediated mechanism, possibly a hypersensitivity reaction to an unknown antigen. Antibodies to intercellular material can often be demonstrated in affected cats. In the majority of cases of both dogs and cats, an increase in circulating eosinophils is present.
In cats, lip lesions are commonly visible near the philtrum and may extend through the adjacent haired skin (Fig. 7-38 ). Oral lesions may occur anywhere in the mouth, including the gingiva, hard and soft palates, oral and nasal pharynx, tongue, and occasionally draining lymphoid tissues, excluding the tonsils, which do not have afferent lymphatic vessels (see Fig. 17-22, C). In dogs, eosinophilic granulomas typically are raised, fungating masses on the ventral and lateral lingual epithelium and palate. Collagenolysis (because collagen is acellular, it cannot undergo necrosis) is characteristically central in the lesion. The surrounding inflammatory tissue contains mixed inflammatory cells with increased numbers of eosinophils, mast cells, and multinucleated giant cells (see E-Fig. 3-10). Lesions grouped as the eosinophilic granuloma complex of cats include eosinophilic ulcer, linear (collagenolytic) granulomas, and eosinophilic plaques. The latter two lesions are strictly cutaneous and do not affect the oral cavity. No proven etiologic link has been established among these cutaneous conditions (linear granulomas and eosinophilic plaques) and oral eosinophilic granulomas. The cause of the canine lesions is unknown.
Figure 7-38.

Eosinophilic Granuloma, Skin, Upper Lip, Cat.
Bilateral ulceration of the upper lip is present. The upper left lip is more extensively affected (arrow).
(Courtesy Dr. Ann M. Hargis, DermatoDiagnostics.)
Lymphoplasmacytic Stomatitis
Lymphoplasmacytic stomatitis is an idiopathic condition of the cat named on the basis of the histologic appearance of the lesions (Fig. 7-39 ). Associations have been hypothesized between this condition and the presence of bacteria or calicivirus associated with feline leukemia virus (FeLV) and/or FIV infection. It is a chronic condition characterized by red, inflamed gums, a fetid breath, and inappetence. The oral mucosa may be hyperplastic and ulcerated. An inefficient immune response may be responsible for the persistence of oral bacteria and the accumulation of lymphocytes and plasma cells.
Figure 7-39.

Lymphoplasmacytic Stomatitis, Gingiva, Cat.
This chronic condition of cats is characterized by red, inflamed gums, fetid breath, and inappetence. The oral mucosa can also be hyperplastic and ulcerated. Inset, There is a florid infiltrate of mixed inflammatory cells, including many lymphocytes and plasma cells in the submucosa beneath the epithelium. H&E stain.
(Figure courtesy Dr. C. Patrick Ryan, Veterinary Public Health, Los Angeles Department of Health Services; and Noah's Arkive, College of Veterinary Medicine, University of Georgia. Inset courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Chronic Ulcerative Paradental Stomatitis
Chronic ulcerative paradental stomatitis, a condition of dogs also known as ulcerative stomatitis and lymphocytic-plasmacytic stomatitis, is caused by apposition of “kissing ulcers” to dental plaque. The condition is painful with resultant inappetence and anorexia. Affected dogs drool and have halitosis. This condition occurs in older dogs of any breed, but Maltese dogs and Cavalier King Charles spaniels are particularly susceptible. The lymphocytic-plasmacytic lesions noted on histologic examination are suggestive of an inflammatory rather than infectious cause, possibly caused by mediators released from the plaque. If untreated, bone resorption may occur.
Oral Mucosal Hyperplasia and Neoplasia
Hyperplastic Diseases.
Gingival hyperplasia is a simple overgrowth of gum tissue, principally the fibrous submucosa. The hyperplasia can become severe enough to bury incisor teeth (Fig. 7-40 ). Gingival hyperplasia is most common in brachycephalic dog breeds and is present in 30% of boxer dogs older than 5 years.
Figure 7-40.

Gingival Hyperplasia, Gingiva, Dog.
Hyperplastic gingiva (asterisk) has enveloped the lower incisor teeth. Dental calculus (tartar, brown) is also present on both upper and lower incisor, canine, and molar teeth.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Grossly, gingival hyperplasia can be indistinguishable from an epulis (Fig. 7-41 ). Epulis is a nonspecific term that designates a growth of the gingiva. The several kinds of epulides can only be distinguished by histopathologic examination. These include fibromatous epulis of periodontal ligament origin—a benign tumor of dental mesenchyme. This distinction is not just an academic exercise because, although all epulides are considered benign, one form, acanthomatous epulis or acanthomatous ameloblastoma, invades bone and can be quite destructive. This growth arises from the epithelial rests of Malassez or epithelial tooth germ. Fortunately, this type of epulis can be managed therapeutically. Whether the epulides represent fibrous and epithelial hyperplasia or benign neoplasms of tooth germ is controversial.
Figure 7-41.

Fibromatous Epulis, Left Mandible, Molar Teeth, Dog.
This growth is an epulis (fibromatous type); however, epulides are often grossly indistinguishable from gingival hyperplasia. Epulis is a term used to designate a growth of the gingiva that is firm, periodontal, and usually solitary, in contrast to gingival hyperplasia. This distinction is not just an academic exercise because, although all epulides are considered benign, one form, acanthomatous ameloblastoma, is locally invasive. It invades bone and can be quite destructive.
(Courtesy Dr. J. King, College of Veterinary Medicine, Cornell University.)
Neoplasia.
In the dog 70% of tumors of the alimentary system are in the oral cavity and oropharynx. These tumors run the gamut of biologic behavior from simple epithelial hyperplasia to malignant neoplasms with metastases to distant sites. Squamous cell carcinomas occur in the oral cavity, particularly in old cats, in which they account for 60% of oral neoplasms. They generally occur on the ventrolateral surface of the tongue and tonsils. Lingual squamous cell carcinomas occur more commonly in cats, and tonsillar squamous cell carcinomas are more common in dogs. Although often appearing histologically aggressive, only a small percentage of lingual neoplasms metastasize, most commonly to draining lymph nodes, the mandibular and medial retropharyngeal. Unfortunately, most tonsillar carcinomas metastasize, initially to regional lymph nodes and then to distant sites.
Squamous cell carcinomas vary both in size and in gross appearance—from flat to proliferative (Fig. 7-42 ). These tumors are often quite aggressive locally, invading subjacent tissues. Some tumors contain more differentiated cells, keratin, often in whorls (keratin pearls) and visible desmosomes (intercellular bridges), whereas others are less well differentiated but with significant mitotic activity. In these latter cases, intracellular immunohistochemical markers for cytokeratin are useful in determining a definitive diagnosis. The amount of fibrous tissue within an individual tumor is variable. Some carcinomas induce a scirrhous response, whereas others have areas of necrosis caused by rapid tumor growth, “collision necrosis,” of the tightly packed proliferating cells and loss of contiguity with the blood supply.
Figure 7-42.

Squamous Cell Carcinoma, Palate, Woodchuck.
A mass of proliferating neoplastic squamous epithelial cells has displaced and replaced the mucosa and underlying tissue of the left hard palate and gingiva.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Ninety percent of melanomas of the oral cavities of dogs are malignant. A breed predilection exists for Scottish terriers, Airedales, cocker spaniels, golden retrievers, Bedlington terriers, Duroc pigs, and others. Most melanomas contain copious intracellular pigment and are visibly black. Some melanomas without pigment, termed amelanotic melanomas, present a greater diagnostic challenge to both the clinician and pathologist (Fig. 7-43 ). Immunohistochemical staining for tyrosinase-related proteins (TRP-1, TRP-2), Melan-A, and melanocytic antigen PNL2 are useful for immunohistochemically identifying amelanotic tumors. Melanomas are composed of melanocytes and are of neural crest origin. Cellular morphologic features within melanomas vary from spindloid to epithelioid. Thus some neoplasms are histologically difficult to differentiate from squamous cell carcinomas and others from fibrosarcomas.
Figure 7-43.

Amelanotic Melanoma, Mandibular Symphysis, Dog.
A proliferative, ulcerated, nonpigmented mass is present on the oral mucosa at the mandibular symphysis and protrudes into the oral cavity, likely resulting in malocclusion. Incisor teeth have been lost. Note the absence of pigmentation (melanin) in this tumor.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Canine oral papillomatosis is a papovavirus-induced, transmissible condition that usually occurs in animals younger than 1 year. The lesions usually regress spontaneously. Immunity is long lasting. The lesions are papilliform or cauliflower-like and can become quite numerous. They are generally white and friable and occur on the mouth, tongue, palate, larynx, and epiglottis. These oral tumors are usually multiple, white to gray, raised, and pedunculated with a keratinized surface and a stromal core. The epithelial cells constituting the lesion can be acanthotic, hyperplastic, and rest on a hyperplastic, folded, connective tissue stroma. The stratum spinosum is also hyperplastic and ballooned. Cytoplasmic inclusion bodies are sometimes present.
Oral extramedullary plasmacytomas may occur anywhere in the mucous membranes of the oral cavity, and in the esophagus or intestine. In the oral cavity they are slow-growing neoplasms and in spite of often-recognized anisokaryosis, mitoses, and multinucleate cells, they rarely invade surrounding tissues and have not been reported to metastasize. Histologic examination is required for accurate diagnosis (see Fig. 13-84).
Fibrosarcomas arise from the collagen-producing cells (fibroblasts) of the oral cavity. Fibrosarcomas are most common in the cat, accounting for 20% of oral neoplasia in that species. They may occur anywhere in the oral cavity. In large-breed dogs, histologically benign-appearing fibrosarcomas of the oral cavity invade bone and metastasize.
Teeth
Malocclusions
Abnormal development and positioning of the teeth may affect dental function. Malocclusion refers to a failure of the upper and lower incisors to oppose properly. This feature is “normal” for some dogs, particularly the brachycephalic breeds. In the extreme, malocclusions can lead to difficulty in the prehension and mastication of food. Malocclusions are named according to the position of the mandible. Protrusion of the lower jaw is termed prognathia (Fig. 7-44 ), whereas a short lower jaw with resultant protrusion of the upper jaw is termed brachygnathia and sometimes hypognathia. Sometimes these terms are incorrectly used, referring to brachygnathia as superior prognathia and prognathia as superior brachygnathia.
Figure 7-44.

Prognathia, Head, Horse.
The mandible is elongated when compared to the maxilla.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Malocclusions result from abnormal jaw conformation or rarely from abnormal tooth eruption patterns. In some animals, such as rodents and rabbits, the teeth continue to grow throughout the animal's lifetime. If these animals are not provided with sufficient roughage in their diets, the teeth (both incisors and cheek teeth) overgrow and either “lock” the jaw or because of a lack of occlusal grinding surfaces, prevent the animal from receiving proper nutrition (E-Fig. 7-4).
E-Figure 7-4.

Overgrown Teeth, Head, Guinea Pig.
The incisors and molars are longer than normal and the tongue is entrapped by the lower molar teeth, which will lead to starvation unless corrected.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Anomalies of Tooth Development
In simple-toothed animals and rarely in other animals, agenesis of a tooth or teeth occurs and is generally of no clinical significance (see Fig. 17-37). Supernumerary tooth development is less common than tooth agenesis and is similarly of little clinical significance. Some animals, such as elasmobranches (sharks), continue to produce row on row of teeth as the outermost rows are lost. Dental dysgenesis may be primarily due to dysplasia of the enamel-forming organ or secondary to trauma, infection and hyperthermia, toxicosis, or other metabolic irregularities during odontogenesis.
Dentigerous cysts result from dental dysgenesis, and epithelial-lined, cystic structures in tissue, including the bone of the jaw, result. Dentigerous cysts develop from abnormal proliferation of the cell rests of Malassez. They appear as variably sized, sometimes fluctuant swellings of the mandible or maxilla. In the maxilla they sometimes invade the nasal sinuses. Although rare, dentigerous cysts are often painful, and although not usually neoplastic, they can destroy the jaw. Dentigerous cysts are epithelial lined and may become impacted with keratin. Rudimentary, malformed teeth may be found within these cysts, and painful fistulas may develop, especially in horses. These draining tracts are seen most often rostral and ventral to the ear (“ear tooth”).
Segmental enamel hypoplasia occurs before eruption of the permanent teeth of dogs as a result of hyperthermia and viral infection, most often by canine distemper virus infection. Enamel is fully formed when the teeth erupt; therefore virus infection of ameloblasts must occur during enamel formation, which is before the dog is 6 months of age, if enamel hypoplasia is to occur. Canine distemper virus infection causes necrosis and disorganization of the enamel organ. After the virus is cleared, structure and function of the enamel organ return to normal. Thus segmental enamel hypoplasia results from the lack of enamel formation during the period of virus infection (Fig. 7-45 ). A similar condition in calves is caused by in utero bovine viral diarrhea virus infection.
Figure 7-45.

Enamel Hypoplasia, Permanent Incisor Teeth, Dog.
There is a lack of enamel formation with resultant discrete deep pits and exposure of the dentin (light yellow to beige areas of the teeth), the result of infection with canine distemper virus and necrosis of the ameloblasts during enamel formation. Permanent adult teeth (shown in illustration) are infected with virus before their eruption and while they are still within their sockets (dental alveoli).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Chemicals, most notably tetracycline antibiotics ingested during the process of enamel mineralization, can cause yellowish, permanent discoloration (see Fig. 1-59). Congenital porphyria, a defect in red blood cell production, may result in incorporation of porphyrins into dentin, resulting in pink discoloration of the teeth (“pink tooth”) (E-Fig. 7-5). Both tetracycline and porphyrins fluoresce under ultraviolet light, dramatically demonstrating these lesions.
E-Figure 7-5.

Pink Tooth, Congenital Porphyria Teeth, Adult Ox.
The teeth are discolored brown from the accumulation of porphyrins in the dentin.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Fluoride incorporation into the enamel and dentin occurs in fluoride toxicosis, particularly in cattle and sheep. A relationship exists in beef cattle between fluorosis and selenium supplementation, with selenium supplementation being protective in high fluoride areas such as those downwind from aluminum smelters or with high concentrations of fluoride in groundwater. Excessive dietary concentrations of fluorine during odontogenesis (from 6 to 36 months of age) may result in incorporation of the fluoride in the enamel and dentin of the permanent teeth. The result is soft, chalky, discolored enamel, usually yellow, dark brown, or black (E-Fig. 7-6). Occlusal grinding of affected soft teeth against more normal enamel results in rapid dental wear to the extent that severely affected sheep may have almost completely worn down their incisors. One wonders therefore about the cumulative effect of fluoride supplementation in municipal drinking water, vitamins with added fluoride, fluoride-supplemented toothpaste, fluoride treatment of teeth, reconstituted and bottled soft drinks made with fluoridated water, and so forth. It is difficult to calculate the total fluoride load ingested by individuals or what the effects may be of that fluoride supplementation.
E-Figure 7-6.

Fluorosis, Cheek Teeth, Cow.
The enamel is chalky and weak, and the teeth are rapidly worn down.
(Courtesy Dr. L. Krook, College of Veterinary Medicine, Cornell University.)
Lesions Caused by Attrition and Abnormal Wear
Loss of normal dental structure and function often results from rapid and irregular and/or abnormal wear of occlusal surfaces in many species of domestic animals. In those species with hypsodont teeth, attention to the dentition as the animal ages is often a major factor in overall body conditioning and health (Fig. 7-46 ). Aggressive treatment of occlusal surface irregularity by filing of high points in the dental arcade (floating) can notably prolong an animal's life. Rock chewing or other compulsive oral behaviors in dogs may result in accelerated dental wear. Similarly, cribbing in horses and herbivorous animals grazing on sandy soils can cause premature dental wear. In all species, exposure of dentin or the pulp canal may lead to dental infection with serious consequences.
Figure 7-46.

Dental Attrition, Molar Teeth, Antelope.
Age-associated dental wear results in improper mastication of feedstuffs and malnutrition. This condition occurs most commonly in horses and is referred to as “step mouth” or “broken mouth.”
(Courtesy College of Veterinary Medicine, University of Tennessee.)
Miscellaneous Dental Disorders
Feline External Resorptive Neck Lesions.
See Disorders of Cats.
Equine Odontoclastic Tooth Resorption and Hypercementosis.
See Disorders of Horses.
Infundibular Impaction
Impaction of the infundibulum, also known as infundibular necrosis or infundibular caries, may cause serious dental disease in ruminants and more rarely in horses. Incomplete infundibular cementum formation before the tooth erupts likely predisposes to infundibular impaction. The pathogenic mechanism is comparable to dental caries in simple-toothed animals, which is uncommon in domestic animals. Feed material is ground into the infundibulum, where bacteria metabolize it to form acid, which causes demineralization. Bacterial enzymes digest the organic matrix of enamel and dentin. As a result of this destruction, the pulp cavity becomes exposed and infected, resulting in pulpitis and endodontitis. Dental abscesses and fistulous tracks may develop and rupture into the paranasal sinuses. The inflamed infundibular cavities often continue to become impacted with feed, creating a vicious cycle.
Periodontal Disease
More than 200 species of bacteria and fungi have been associated with dental plaque (a film of an organic matrix, food particles, and bacteria on the tooth surface). This plaque often becomes mineralized (tartar or dental calculus). The mineralized material contributes to atrophy and inflammation of the gingival mucosa and supporting stroma by acting as a nidus for additional plaque accumulation. Bacteria resident in films on the tooth surface produce acids and enzymes that may damage their enamel substrate (cavities) and also destroy the subjacent gingival tissue and periodontal ligament (periodontal disease).
The initial site for destructive inflammation is in the gingival crevice–forming pockets where bacteria lodge. With time, this inflammation spreads distally along the tooth, resulting in gingival-epithelial attachment only on the root of the tooth, deep in the alveolar socket. Progression of inflammation may destroy the connective tissue of the periodontal ligament, resulting in loosening of the tooth. The infection can spread, causing alveolar osteomyelitis and pulpitis and can result in apical abscesses and bacteremia. There is significant oral pain, reluctance to masticate, and halitosis. Periodontal disease is common in carnivores and human beings. Mildly abrasive diets and brushing of the teeth of pet carnivores, combined with regular dental examination, is preventive as it is in human beings.
Dental Neoplasia
Proliferative, cystic, or neoplastic diseases of the dental arcade can originate from cell rests that form from the dental lamina or the enamel organ (the cell rests of Malassez). Dental neoplasms usually arise close to the teeth, either deeply in the jaw or from the oral epithelium. There is a relatively precise method of naming dental neoplasms based on the tissue or cell of origin and the extent of differentiation and odontogenesis present within the neoplastic tissue. The histologic appearance of these neoplasms is complex; pathologists with considerable experience in differentiating these uncommon neoplasms should be consulted when a precise diagnosis is indicated.
Odontomas are hamartomas originating in the enamel organ and are usually seen in puppies and foals (Fig. 7-47 ). They usually contain well-recognizable dentin and enamel, as well as ameloblasts, odontoblasts, and dental pulp.
Figure 7-47.

Odontoma, Incisor Teeth, Cow.
This is a hamartoma (a benign tumor-like nodule) of the enamel organ that in this case has expanded bilaterally on the rostral mandibles. There is extensive hemorrhagic ulceration over the tumor. Diagnosis can be confirmed by radiographic and histopathologic examination.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Ameloblastoma is a term applied to epithelial neoplasms of enamel organ origin. Several subtypes, distinguished histologically, are ameloblastic fibroma, ameloblastic odontoma, calcifying epithelial odontogenic tumor, peripheral odontogenic fibroma, and other rare tooth neoplasms. Ameloblastoma appears randomly in the dental arcade, usually in adult dogs. These neoplasms are often osteolytic and thus are locally invasive. Histologic examination by an expert is often necessary to distinguish ameloblastoma from acanthomatous epulis (acanthomatous ameloblastoma) and squamous cell carcinoma.
Tonsils
Tonsillitis is relatively rare in domestic species. Because they lack afferent lymphatic vessels, tonsils do not become secondarily affected by lymphatic drainage from infections elsewhere in the oral cavity. Tonsillitis may occur, however, as a result of saliva- and blood-borne agents such as infectious canine hepatitis and hog cholera. Epithelial tumors (squamous cell carcinomas) and lymphoid neoplasms occur in all species.
Salivary Glands
Inflammatory Diseases
Sialoadenitis, inflammation of a salivary gland, is relatively rare in veterinary medicine. Although diagnosis of systemic diseases is not made by examining the salivary gland, rabies and canine distemper are two very important diseases that cause inflammation of the salivary glands. Saliva is a particularly important medium of spread, by bite wounds, of the rhabdovirus that causes rabies. There are focal necrosis, mononuclear cell inflammation, and sometimes inclusions (Negri bodies) in the nuclei of ganglion cells. In the rat a coronavirus termed sialodacryoadenitis virus is responsible for inflammation of the salivary gland and some adnexal ocular glands. Salmonella typhisuis has caused suppurative parotid sialoadenitis in pigs.
Gross lesions of sialoadenitis are subtle and include swelling and edema. Sialoadenitis can be accompanied by pain on palpation. Abscesses occasionally occur, sometimes secondary to the migration of foreign bodies (grass awns), and are especially noticeable when they occur in the retrobulbar zygomatic gland where they may cause ocular protrusion (proptosis).
Miscellaneous Disorders
Changes in the salivary glands are uncommon in domestic animal species. A ranula is a cystic saliva-filled distention of the duct of the sublingual or submaxillary salivary gland that occurs on the floor of the mouth alongside the tongue (Fig. 7-48 ). It is thus epithelial lined. The cause is generally unknown, although some cases are due to sialoliths. A salivary mucocele, in contrast, is a pseudocyst not lined by epithelium but filled with saliva. The cause of this lesion is also unknown, but it may occur secondary to traumatic rupture of the duct of a sublingual salivary gland with resultant leakage and encapsulation of saliva by reactive connective tissue.
Figure 7-48.

Ranula, Mandibular Salivary Duct, Dog.
This is a cystic distention of the left mandibular salivary duct along the ventral-lateral aspect of the tongue.
(Courtesy Dr. P. Stromberg, College of Veterinary Medicine, The Ohio State University.)
Sialoliths are rare in domestic animal species. When they do occur, they are considered to be caused by inflammation of the salivary gland with sloughed cells or inflammatory exudate forming a nidus for mineral accretion (Fig. 7-49 ). Thus they are one cause of ranula formation.
Figure 7-49.

Sialolith, Horse.
Pressure necrosis from this large stonelike mass (arrows) has destroyed the gland in which it formed.
(Courtesy Dr. B. Cooper, College of Veterinary Medicine, Oregon State University.)
Neoplasia
Salivary gland neoplasms, both benign and malignant, are uncommon but occur in all species (Fig. 7-50 ). They are composed of glandular or ductular elements or a combination of epithelial and mesenchymal components similar to those in mixed mammary neoplasms. A grossly appearing similar condition, salivary gland infarction, occurs infrequently in cats and rarely in dogs. The cause of the infarction is unknown. The gross appearance of firmness and swelling of an infarcted gland must be distinguished microscopically from neoplasia (E-Fig. 7-7). In salivary gland infarction there are discrete foci of parenchymal necrosis with peripheral hemorrhage and inflammatory cells. Attempted incomplete regeneration of the gland from ductal epithelium can be mistaken for neoplasia unless one is familiar with the former condition.
Figure 7-50.

Salivary Gland Carcinoma, Left Parotid Salivary Gland, Cat.
A large proliferative carcinoma of the salivary gland has replaced the normal gland.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
E-Figure 7-7.

Salivary Gland Infarction, Salivary Gland, Cat.
Note the areas that lack cell definition (necrosis) secondary to infarction (arrows). Normal salivary gland is present in the right third of this illustration. Inset, Abortive regeneration as evidenced by hyperplasia of surviving salivary duct epithelial cells (arrows). H&E stain.
(Figure and Inset courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Tongue
Developmental Anomalies
Congenital diseases of the tongue include epithelial defects such as fissures, epitheliogenesis imperfecta, macroglossia and microglossia, bifid tongue, and hair growing from the tongue (choristoma) (E-Fig. 7-8). Lethal glossopharyngeal defect, or bird tongue of dogs, is characterized by a pointed tongue that cannot wrap around a nipple and create the negative pressure required for nursing, and without intervention, starvation results. Ventral ankyloglossia, fusion of the tongue to the floor of the oral cavity, has been reported in related Anatolian shepherd dogs. The cause of these congenital lesions is not known, but they sometimes occur in association with other defects. As in the case of other congenital defects, ingestion of unknown teratogenic substances by the dam during gestation is an etiologic possibility, as is mutation of T-box genes.
E-Figure 7-8.

Choristoma (“Hair Tongue”), Tongue, Dog.
Dysplastic hair is growing from the choristoma in the tongue.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Disease agents that principally target the tongue are relatively rare. The exception to this rule is Actinobacillus lignieresii, a Gram-negative bacillus that is a normal inhabitant of the oral cavity. It is an opportunistic invader of damaged lingual tissue, principally in cattle and occasionally in horses and small ruminants. The granulomas resulting from infection contain centrally located actinobacilli rimmed by radiating amorphic, eosinophilic, and clublike structures composed of immunoglobulin molecules from lesion plasmacytes (Fig. 7-51 ). Mixed mononuclear inflammatory cells, including multinucleated Langhans giant cells, often surround these foci (Splendore-Hoeppli phenomenon), and infection may drain and cause similar inflammation in submaxillary and retropharyngeal lymph nodes. The amount of fibrous tissue present depends on the duration of the inflammation and the swelling. Inflammation and fibrosis cause increased firmness and enlargement of the tongue called “wooden tongue” (Fig. 7-52 ). Horses are rarely affected by A. lignieresii infections, but when they are, lesions are cutaneous or lymph node abscesses, mastitis, and occasional glossitis.
Figure 7-51.

Actinobacillosis (Wooden Tongue), Tongue, Cow.
Splendore-Hoeppli reaction (colony of bacteria with surrounding radiating “clubs” of immunoglobulin) is surrounded by suppurative inflammation. H&E stain.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-52.

Actinobacillosis, Tongue, Cow.
A, Dorsal surface. Proliferative and ulcerative chronic-active inflammatory lesions containing neutrophils mixed with mononuclear inflammatory cells (lymphocytes, macrophages, plasma cells) and fibrous tissue are present in the tongue. B, Chronic actinobacillosis (wooden tongue). Chronic inflammation results in loss of muscle of the tongue and its replacement by fibrous tissue during healing. Note the white interwoven bands of fibrous tissue (arrowheads) and the focus of granulomatous inflammation (arrow).
(A courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee. B courtesy Dr. R.J. Panciera, School of Veterinary Medicine, Oklahoma State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
Systemic Disease: Secondary Involvement of the Tongue
Thrush is a Candida albicans (yeast) infection of intact mucous membranes of the tongue and esophagus (see Fig. 7-7). It occurs principally in ungulates but has also been seen in carnivores. Thrush is not a primary disease but often indicates an underlying debility, particularly in young animals. It occurs as a result of antibiotic treatment that kills normal flora, increased serum glucose concentrations as a result of diabetes mellitus, a high-sugar diet, or intravenous glucose therapy. The availability of iron is a limiting factor for the indigenous bacteria, which compete with yeast for mucosal colonization. Immunodeficiency states also contribute to the development of thrush. All of these scenarios provide tissue conditions suitable for the proliferation of yeast forms. Rarely, systemic infection may result. Factors predisposing to systemic infections include multiple antibiotic usage, indwelling catheters, and endotracheal tubes. This infection presents as a gray-green pseudomembrane that is easily scraped off the intact underlying mucosal surface (see Fig. 7-8).
Often, lingual lesions are manifestations of systemic diseases, such as bovine viral diarrhea, foot-and-mouth disease, multisystemic amyloidosis, and uremia (Fig. 7-53 ; also see Fig. 11-21). These diseases are discussed in more detail in this and other chapters of this book.
Figure 7-53.

Ulcerative Glossitis, Uremia (Uremic Glossitis), Tongue, Cat.
There is extensive ulceration of the mucosal epithelium of the tongue associated with increased concentrations of serum blood urea nitrogen and creatine from kidney failure.
(Courtesy Drs. R.L. Fredrickson and R.A Doty, College of Veterinary Medicine, University of Illinois.)
Hyperplastic and Neoplastic Conditions
Lingual (glossal) neoplasms are rare but when they occur are generally of epithelial origin. Squamous cell carcinomas are most common (Fig. 7-54 ; also see Fig. 6-10), but papillomas (Fig. 7-55 ), rhabdomyomas, rhabdomyosarcomas, fibrosarcomas, melanomas, and granular cell tumors have all been reported in domestic animals.
Figure 7-54.

Squamous Cell Carcinoma, Tongue (Dorsal Surface), Dog.
Note the proliferative, ulcerated, and hemorrhagic neoplasm growing transversely across the surface of the tongue.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-55.

Papillomas, Tongue (Ventral Surface), Cow.
Papillomas, often caused by bovine papillomavirus, are present on the ventral surface of the tongue. The virus infects traumatized mucosal epithelial cells and induces epithelial cell proliferation.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Parasites
Parasites of the tongue are uncommon, with the exception of those that reside in muscles, such as Sarcocystis spp. in most species and Trichinella spiralis in pigs and occasionally in carnivorous wildlife such as polar bears. Gongylonema spp. can be present in the lingual mucosa of pigs and ruminants and are of no clinical significance.
Esophagus
Developmental Anomalies
Achalasia.
Esophageal motility disorders are termed achalasia. In this condition the sequential contractility of the esophagus is defective, and the lower cricopharyngeal sphincter fails to function properly. Achalasia results in difficulty in swallowing and may be responsible for regurgitation and weight loss.
Cricopharyngeal achalasia is a congenital, possibly neurogenic, disorder of the upper esophageal (cricopharyngeal) sphincter. It occurs in young, small-breed dogs, particularly terriers, cocker spaniels, and miniature poodles. Postweaning dysphagia and regurgitation after a meal of solid food is characteristic of this functional disorder. Liquids are generally swallowed without incidence. Gagging or choking behavior of the patient after swallowing is a good indicator in the appropriately aged dog of this condition.
Acquired canine achalasia is extremely uncommon. In this condition there is often a visible abnormality of the musculature of deglutition (cricopharyngeus). There does not appear to be a characteristic change in the affected musculature. Esophageal myotomy of the appropriate cricopharyngeal sphincter muscle is palliative for these idiopathic conditions.
Megaesophagus
Megaesophagus or esophageal ectasia is dilation of the esophagus because of insufficient, absent, or uncoordinated peristalsis in the mid and cervical esophagus. It has been described in dogs, cats, cows, ferrets, horses, and New World camelids. Causes include innervation or denervation disorders and partial physical obstructions and stenosis, secondary to inflammatory diseases of esophageal musculature or persistence of the right aortic arch. Many cases are idiopathic.
Congenital megaesophagus is usually due to partial blockage of the lumen of the esophagus by a persistent right fourth aortic arch. Because of the persistence of the arch, a vascular ring forms around the esophagus and trachea, preventing full dilation of the esophagus. The ring is formed by the aorta, pulmonary artery, and ductus arteriosus. This form of megaesophagus is unique in that the esophageal obstruction, and thus dilation, occurs cranial to the heart because of the location of the obstructing vascular ring (Fig. 7-56 ; also see Fig. 10-37. Persistent right aortic arch is likely hereditary in German shepherds, Irish setters, and greyhounds. All other forms of megaesophagus result in dilation cranial to the stomach.
Figure 7-56.

Megaesophagus from a Persistent Right Aortic Arch, Esophagus, Dog.
Dilation of the esophagus cranial to the heart (H) is the result of failure of the right fourth aortic arch to regress during embryonic life (vascular ring abnormality).
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Congenital megaesophagus also occurs as an idiopathic denervation of the esophagus, most notably in great Danes, Irish setters, miniature schnauzers, Labrador retrievers, wire hair fox terriers, shar-peis, Newfoundlands, Siamese cats, and in some cases of vagal indigestion, in cattle. Some cases of myasthenia gravis (see later discussion) are congenital and may be of genetic origin.
Acquired megaesophagus (esophageal achalasia) is the result of failure of relaxation of the distal esophageal (cardiac) sphincter of the stomach. The obstruction and thus dilation occurs cranial to the stomach (Fig. 7-57 ). Although the gross appearance of acquired megaesophagus in animals is similar to that of human beings, the cause of the condition in animals does not involve the cardiac sphincter. Causes are idiopathic or secondary to polymyositis (inflammation of the esophageal muscle), myasthenia gravis (a congenital or autoimmune disease directed against acetylcholine receptors of the neuromuscular junction), hypothyroidism (which can result in muscle atrophy and denervation disease), congenital myopathy, lead and thallium poisoning (via effect on innervation), peripheral neuropathies, vagal indigestion, esophagitis, and recurrent gastric dilation. Increased risk in dogs is seen in German shepherds, golden retrievers, and Irish setters.
Figure 7-57.

Megaesophagus, Thoracic Esophagus, Dog.
A notably dilated thoracic esophagus cranial to the diaphragm has displaced the right lung caudally and ventrally. This form of megaesophagus is often attributable to an abnormality (mass, foreign body, innervation disorder) affecting the cardiac sphincter.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Megaesophagus is recognized clinically by regurgitation after ingestion of solid food. Thus congenital megaesophagus is often recognized at weaning. Often animals are thin and may have aspiration pneumonia. Radiographically, the esophagus is dilated anterior to the lesion and retains radiopaque dyes (E-Fig. 7-9). Dilation may vary from diffuse to locally extensive, depending on its cause. Putrid ingesta are sometimes found in the dilated, atonic portions of the esophagus. Although degenerate nerve fibers are occasionally found within vagus nerves, megaesophagus can occur without detectable histologic lesions.
E-Figure 7-9.
Megaesophagus, Thoracic Radiograph, Dog.
Swallowed radiopaque imaging agent (barium sulfate) demonstrates dilation of the esophagus cranial to the diaphragm.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Hiatal Hernia
Protrusion of the abdominal esophagus and cardia of the stomach through the diaphragm into the thoracic cavity is termed a hiatal hernia. This inversion is generally into the esophageal lumen and is self-reducing. Sometimes a gastroesophageal intussusception results.
Eosinophilic Esophagitis
Eosinophilic esophagitis is an emerging disease in human beings. In a single dog, clinical signs include regurgitation, dysphagia, and cough, accompanying a diffusely affected, friable, hyperemic, ulcerated, esophageal mucosa visible by endoscopy. Inflammation is dominated by granulocytes—half of which are eosinophils. Diagnosis is by elimination of other causes of inflammatory esophagitis. Seventy percent of human beings and the single dog described had concurrent allergic skin disease.
Esophageal Parasites
With notable exceptions, parasitic diseases of the esophagus are generally of no clinical importance. The more common parasites of the esophagus are Gongylonema spp., which affect ruminants, pigs, horses, primates, and occasionally rodents. These nematodes reside in the esophageal mucosa and are characteristically thin, red, and serpentine. They can be 10 to 15 cm in length and are easily visible (Fig. 7-58 ). The intermediate hosts are cockroaches and dung beetles.
Figure 7-58.

Gongylonemiasis, Esophagus, Cow.
The red-white serpentine intramucosal nematodes are characteristic of Gongylonema, a nematode of the superfamily Spiruroidea.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Gasterophilus spp. occur in horses. These fly larvae have interesting life cycles because their eggs are laid on the skin in varying locations. The warmth and moisture from licking activates them. The larvae burrow into the oral mucosa, molt, and then migrate down the esophagus. They occur in both the distal esophagus and the stomach, where they attach to the mucosa via oral hooks. They eventually detach, leaving craters at the site of attachment, and pass in the feces.
Hypoderma lineatum is the larvae of the warble fly of ruminants. These parasites eventually migrate to the esophageal adventitia and then to the subcutaneous tissue of the back.
Spirocerca lupi of dogs is probably the most pathogenic of the esophageal parasites. These nematodes reach the esophageal submucosa after migrating from the stomach. They penetrate through the gastric mucosa to reach the adventitia of arteries and then migrate in the adventitia to the abdominal aorta and aborally to the caudal aorta, where they form a granuloma in the adventitia. From here they migrate to the adjacent esophageal submucosa. A passage forms between the esophageal lumen and the granuloma containing the parasite, allowing discharge of ova into the lumen of the alimentary system and eventually into the feces. Clinical sequelae of infestation include dysphagia, aortic aneurysms, hemothorax, and rarely esophageal fibrosarcomas or osteosarcomas (Fig. 7-59 ). Occasionally, chronic aortic granulomas will extend into the adjacent thoracic vertebral bodies of chronically affected dogs to cause spondylosis deformans adjacent to the aortic granulomas. S. lupi infestations occur in warmer climates. The intermediate hosts are dung beetles, and the paratenic hosts are chickens, reptiles, and rodents.
Figure 7-59.
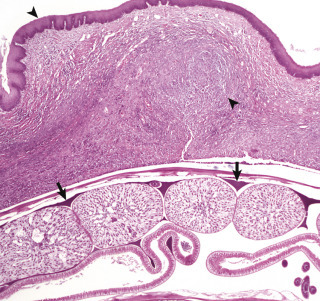
Fibrosarcoma, Esophagus, Dog.
Spirocerca lupi (longitudinal section) (arrows) is present in the esophageal submucosa deep to the fibrosarcoma, which it has induced (arrowheads). H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Miscellaneous Esophageal Disorders
Idiopathic muscular hypertrophy of the distal esophagus is a lesion peculiar to horses and pigs that can be quite spectacular at necropsy (Fig. 7-60 ) but usually is of no clinical significance. The esophageal musculature can be several centimeters thick, and the lesion can extend along the distal quarter of the esophagus. Rarely this condition plays a role in esophageal impaction. Similarly, dilation of the esophageal glands present throughout the esophagus of aged dogs can be a spectacular gross lesion of no clinical consequence. It is therefore important to carefully evaluate these lesions either at necropsy or by endoscopy in the live animal to determine whether what appear to be erosions and ulcers are instead mucosal elevations caused by glands filled with mucus. Because the lesions are subepithelial, the overlying mucosa is smooth and shiny. Dilated esophageal glands vary in number and location but are generally only a few millimeters in diameter (Fig. 7-61 ). They are most numerous in the distal esophagus.
Figure 7-60.

Muscular Hypertrophy, Distal Esophagus, Horse.
Longitudinal (left) and transverse (right) sections of the esophagus demonstrate the marked increase in the thickness of the smooth muscle in the tunica muscularis of the distal esophagus.
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Figure 7-61.

Cystic Esophageal Glands, Distal Esophagus, Dog.
Multiple white mucosal cysts are present in the esophageal glands of the mucosa and submucosa. These cysts are common and insignificant findings in aged dogs.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Esophageal erosions and ulcers are relatively common and have a variety of causes. One of the more common causes of esophageal erosions and ulcers is reflux of stomach acid. This reflux of gastric acids causes chemical burning of the distal or aboral esophagus and is commonly called acid reflux esophagitis (Fig. 7-62 ) or clinically, heartburn in human beings. Other causes of esophageal ulcers include improper use of stomach tubes, which cause linear scraping on the crests of the longitudinal folds of the esophageal mucosa (Fig. 7-63 ), foreign bodies such as bones in dogs and infectious diseases, such as bovine viral diarrhea (Fig. 7-64 ), which cause mucosal injury in other locations as well.
Figure 7-62.

Acid Reflux Esophagitis, Esophagus, Horse.
The dark red streaks on the surface of the esophagus are areas of epithelial loss secondary to gastric acid reflux. The white streaks and vertically linear areas on the surface of the esophagus are areas of unaffected and likely hyperplastic mucosal epithelium. As would be expected, erosions are most severe in the esophageal mucosa adjacent to the cardia and extend orad. This distribution is diagnostic of acid reflux esophagitis.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-63.

Trauma-Induced Esophageal Ulceration, Esophagus, Horse.
These red linear ulcers are the result of abrasion from improper stomach tubing, either from an overly large diameter tube, from a too-vigorous insertion, or from a tube with a roughened edge.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-64.

Ulcerative Esophagitis, Bovine Viral Diarrhea (BVD), Esophagus, Cow.
Note the multiple variably sized (millimeter range) and variably shaped esophageal mucosal ulcers caused by the pestivirus of bovine viral diarrhea.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Leukoplakia of the esophagus and stomach is characterized by discrete, flat, white mucosal elevations (epithelial plaques) of no clinical significance and of unknown cause. They are sometimes mistaken for thrush lesions or neoplasia. Unlike thrush lesions, they do not scrape off easily, and their regularity, number, and location distinguish them from neoplasms. Histologically, the stratum basale and prickle cell layers are notably thickened, and the surface cells have pyknotic nuclei and some parakeratosis. In human beings approximately 5% of these lesions become cancerous. They are present in the oral cavity and esophagus of human beings and are believed related to chronic irritation most often associated with smoking or chewing tobacco. Alcohol consumption and restorative dental amalgams may also predispose to leukoplakia.
Choke
Choke is a clinical term referring to esophageal obstruction subsequent to stenoses or blockage. Choke most often occurs in anatomic locations in which the esophagus cannot fully expand. These locations are dorsal to the larynx, cranial to the first rib at the thoracic inlet, the base of the heart, and the diaphragmatic hiatus. Choke occurs most frequently as a result of ingestion of large foreign bodies, such as potatoes, apples, bones (Fig. 7-65 ), corn cobs (Fig. 7-66 ), or medicaments, such as large gelatin-filled capsules or tablets (dry boluses). If these bodies are lodged against the epithelium for longer than 2 days, the interaction often results in circumferential pressure necrosis of the esophageal mucosa (Fig. 7-67 ), which forms strictures during healing. These strictures then can cause reflex regurgitation after ingestion of food with possible starvation or aspiration pneumonia resulting.
Figure 7-65.

Ulcers and Perforation, Foreign Body, Esophagus, Dog.
The esophagus has been perforated by an ingested chicken bone. Note that the end of the bone opposite the perforation site has caused a deep ulcer (arrow). There are also several chronic ulcers caudal to the perforation, presumably from abrasion by other bones as they moved down the esophagus.
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Figure 7-66.

Foreign Body (Choke), Esophagus, Cow.
A corn cob has lodged in the esophagus subjacent to the larynx.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-67.

Foreign Body (choke), Esophagus, Horse.
Pressure necrosis of the proximal esophageal mucosa adjacent to the larynx has occurred secondary to lodgment of a foreign body (compacted chaff). As a general rule, pressure necrosis usually occurs if the foreign body remains in place against the mucosal epithelium for longer than 2 days.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
In older horses, poor dentition causes feed to be incompletely masticated, resulting in impaction in the esophagus. Neoplastic or inflammatory lesions of the esophagus or periesophageal tissues also cause obstruction. Persistence of the right aortic arch has already been discussed as a cause of esophageal stenosis and megaesophagus.
Neoplasia
Neoplasms of the esophagus are rare. Bracken fern (Pteridium aquilinum) consumption, sometimes in association with papilloma viruses, has been associated with squamous cell carcinomas in cattle. The clinical signs are similar to those of other causes of esophageal blockage and include dysphagia, regurgitation, weight loss, and dilation of the esophagus proximal to the mass. Tumors of the esophagus are occasionally palpable but are most often intraluminal rather than mural. Epithelial tumors include papillomas (Fig. 7-68 ) and squamous cell carcinomas. The latter have wide metastatic potential. Smooth muscle tumors of the esophagus, whether benign or malignant, are also rare but may result in similar clinical signs (Fig. 7-69 ). Esophageal fibrosarcomas of dogs often develop in areas with S. lupi infestation. Esophageal lymphoma occurs sporadically in most species (Fig. 7-70 ).
Figure 7-68.

Papillomatosis, Bovine Papillomavirus, Esophagus, Bull.
Multiple papillomas, characteristic of this viral-induced disease, occur following trauma to the esophageal mucosa and infection of mucosal epithelial cells. Oral papillomas may be present concurrently.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-69.

Leiomyoma, Esophagus, Dog.
A mass consisting of submucosal proliferation of smooth muscle cells bulges into the distal esophageal lumen, causing obstruction.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-70.

Lymphoma (Lymphosarcoma), Esophagus, Dog.
Masses of submucosal proliferating malignant lymphocytes bulge into the esophageal lumen, causing partial obstruction. Note that the mucosal epithelium is intact (smooth and shiny).
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Rumen, Reticulum, and Omasum
Stomach and Abomasum
Gastric Dilation and Volvulus
Simple gastric dilation occurs in a variety of animals (Fig. 7-71 ). In dogs, particularly in the large, deep-chested breeds, the acute gastric dilation and volvulus syndrome occurs. This lesion is life threatening and should not be confused with simple gastric dilation, which is common in young puppies after overeating. Predisposing factors to acute gastric dilation include a source of distending gas, fluid, or feed; obstruction of the cardia that prevents eructation and emesis; and obstruction of the pylorus that prevents passage of gastric contents into the small intestine. The source of gas is not well understood. Theories include gas production by C. perfringens, spores of which are present in the feed, carbon dioxide from physiologic mechanisms of digestion, or simple aerophagia.
Figure 7-71.

Simple Gastric Dilation, Stomach, Rabbit.
The stomach is markedly dilated and filled with gas. Dilation occurs most commonly following aerophagia or overeating and is relieved by eructation or vomiting.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
The result of repeated episodes of gastric dilation is stretching and relaxation of the gastrohepatic ligament. Recurrent dilation, combined with overfeeding, postprandial exercise, and perhaps a hereditary predisposition, results in gastric rotation. Gastric rotation is recognized by splenic displacement and a twisted esophagus and results in vascular compression and decreased venous drainage and hypoxemia (Figs. 7-72 and 7-73 ). The stomach generally is rotated clockwise on the ventrodorsal axis when the abdomen is viewed from the ventral surface. Rotation is 180 to 360 degrees. The combination of gastric hypoxemia, acid-base imbalance, obstruction of the pylorus and cardia, and increased intragastric pressure leads to antiperistaltic waves followed by atony, cardiovascular ischemia, arrhythmias, and shock. Decreased portal venous return leads to pancreatic ischemia and release of myocardial depressant factor, cardiac collapse, and death.
Figure 7-72.

Gastric Dilation and Volvulus, Stomach, Dog.
The stomach is distended with food and gas (top example). It rotates (arrow) on the mesenteric axis (bottom example) clockwise (180, 270, or 360 degrees on a ventrodorsal axis when the abdomen is viewed from the ventral surface), resulting in a gastric volvulus with an obstructed esophagus that prevents eructation and thus further contributes to gastric dilation. The spleen, attached to the stomach by the gastrosplenic ligament, rotates with the stomach and is thus folded back upon itself and located in the right cranial abdomen against the diaphragm (bottom example). The splenic vein is compressed, resulting in a congested spleen, because the arterial blood supply remains patent longer than venous drainage.
(Modified from Van Kruiningen HJ, Gregoire K, Meuten DJ: J Am Anim Hosp Assoc 10:294-324, 1974.)
Figure 7-73.

Gastric Dilation and Volvulus, Abdomen, Dog.
The stomach is filled with gas and its serosa is congested (dark red). The duodenum and engorged spleen have been displaced to the right.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Epidemiologic evidence suggests that dry dog foods that list oils or fats among the first four ingredients increase the risk for the gastric dilation and volvulus syndrome. Gastric dilation and volvulus is sometimes associated with gastric eversion or intussusception into the distal esophagus. This latter condition can also occur independently of gastric dilation and volvulus.
Abomasal Displacement
Gastric Dilation and Rupture
Gastric dilation occurs in horses as a result of the ingestion of fermentable feeds or grain, a situation analogous to grain overload with lactic acidosis in cattle. Acute gastric dilation and rupture in horses occurs most frequently as a terminal event in intestinal obstruction and displacement. Because gastric dilation and rupture can occur after death, the diagnostic challenge is to determine if the rupture occurred ante mortem or post mortem. The only reliable indicator of the time of rupture, in relation to the death of the animal, is the presence of hemorrhage and evidence of inflammation, such as fibrin strands, along the margins of the rupture (usually the greater curvature) because such inflammatory responses occur only in live animals (Figs. 7-74 and 7-75 ).
Figure 7-74.

Rupture, Abomasum, Calf.
Multifocal hemorrhages along the upper margin of the tear and subserosally adjacent to the greater curvature indicate that the rupture occurred antemortem.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-75.

Rupture, Stomach, Horse.
The hemorrhage visible on the right margin of the rupture indicates that the rupture occurred antemortem. Note also that the rent through the tunica muscularis is longer than that through the mucosa, which still covers the ingesta on the left and right sides. The mucosal and serosal surfaces are congested.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
In Northern Europe, acute gastric dilation occurs in horses on pasture as part of the syndrome called grass sickness or dysautonomia. The esophagus and stomach are often dilated and atonic. Although serologic evidence suggests an association of grass sickness with C. perfringens type A enterotoxin, noninflammatory degeneration of associated autonomic ganglia has also been described. This condition can be experimentally produced in the horse with whole blood from affected animals, suggesting that a soluble toxin may be the cause.
Chronic gastric dilation is also associated with ingestion of poorly digestible substances. Habitual cribbing and aerophagia may also be contributory.
Dysautonomia also occurs in pet carnivores secondary to ganglionic death in cranial nerves, spinal nerves, and autonomic nerves. Associated ganglionic peptide levels are reduced in an amount consistent with the functional aberrations. Ganglioneuritis creates a similar syndrome to dysautonomia in a variety of species and is infrequently diagnosed. GI signs of dysautonomia include xerostomia, decreased anal tone, vomiting, and regurgitation. See Chapter 14 for a description of the histologic lesions.
Chronic abomasal and/or ruminal dilation may occur in cows with overeating disease, dystocia, exhaustion, poor-quality or frozen feedstuffs, abomasal ulcers with or without abomasal lymphoma, and vagal indigestion. A sequela of abomasitis may be a mycotic infection similar to that which occurs in the rumen (Fig. 7-76 ).
Figure 7-76.
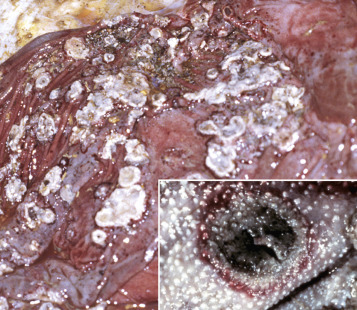
Mycotic Abomasitis and Omasitis, Calf.
The mucosal surface of the abomasum has discrete and coalescing ulcers covered by yellow-white diphtheritic membranes and a red outer margin of active hyperemia and inflammation. These lesions are indicative of infarcts and are likely secondary to vasculitis and thrombosis by angioinvasive fungi such as Aspergillus, Mucor, Rhizopus, Absidia, and Mortierella spp. The diphtheritic membranes are a mixture of necrotic cellular debris from the infarct, inflammatory cells, and hyphae from the inciting fungus. Inset, Mycotic omasitis. The lesion is similar to the one in the abomasum. The diphtheritic membrane has been lost because of omasal peristalsis, but the necrotic center (infarct) and red outer margin of active hyperemia and inflammation are prominent.
(Figure courtesy College of Veterinary Medicine, University of Illinois. Inset courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
In monkeys an increased frequency of acute gastric dilation often occurs during weekends, when there may be changes in feeding behavior secondary to unfamiliar keepers. Studies have implicated C. perfringens overgrowth secondary to an increase in fermentable feed consumption in the pathogenesis of gastric dilation in primates.
Chronic gastric dilation in dogs is usually secondary to gastric ulcer, mural gastric lymphomas, uremia affecting gastric structure and function, pyloric stenosis or obstruction, acute gastric dilation, intervertebral disk disease, or vagotomy. Chronic gastric dilation is characterized by reduced feed intake, diminished gastric motility, and increased gastric gas accumulation sometimes resulting in abdominal distention similar to that of bloat.
Abomasal Dilation and Tympany
Impaction
Impaction of the monogastric stomach and abomasum has a variety of causes. Intrathoracic lesions, such as pneumonia, pleuritis, lymphadenopathy, and lymphoma of mediastinal lymph nodes, can infiltrate and damage the vagal nerves, resulting in a problem with abomasal/gastric motility and emptying. Roughage, hairballs, and other foreign materials also cause impaction. Gastric trichobezoars and phytobezoars of monogastric animals are similar to those that occur in the rumen (E-Fig. 7-10).
E-Figure 7-10.

Trichobezoar, Stomach, Rabbit.
The stomach is impacted with ingested hair.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Abomasal emptying defect can also cause impaction. It is principally a condition of Suffolk sheep 2 to 6 years of age. It is characterized by an impacted, dilated abomasum. Clinical signs include anorexia, weight loss, and increased ruminal chloride concentrations. The latter feature is believed to be secondary to abomasal reflux. Scattered chromatolysis and neuronal necrosis in the celiac and mesenteric ganglia are consistent changes from a neurotoxicosis. The process is likely mediated by excitotoxins, although viruses have not been ruled out. Clusters of affected animals in a single flock are suggestive of an environmental cause. Inflammation is minimal. Abomasal emptying defect may be a form of acquired dysautonomia.
Inflammatory Diseases
Inflammation of the simple stomach or abomasum is designated as gastritis and abomasitis, respectively, and must be differentiated from simple hyperemia and petechiae, which are often nonspecific agonal lesions. Gastritis is often associated clinically with vomiting, dehydration, and metabolic acidosis. Hemorrhage, edema, increased amounts of mucus, abscesses, granulomas, foreign body penetration, parasites, inflammatory cells of various types, erosions, ulcerations, and necrosis characterize the changes in the mucosal surface and subsequent inflammatory reaction.
Clostridium septicum is a cause of hemorrhagic abomasitis with submucosal emphysema of sheep and cattle, a disease known as braxy. Although this disease is most common in the United Kingdom and Europe, it occurs in North America as well. Generally, the disease follows ingestion of frozen feeds contaminated with the causative Clostridium spp. The lesions are produced by the exotoxin of the bacteria, and death therefore is due to an exotoxemia.
Sarcina-like organisms have been reported in association with abomasal bloat in several calves. Sarcinas are anaerobic, Gram-positive, nonmotile cocci found in rafts or packets. They are suspected gastric pathogens in a variety of animal species. The lesions are similar to braxy.
In many septicemias of pigs, bacterial emboli lodge in the vessels of the gastric submucosa and cause thrombosis, resulting in hyperemia, hemorrhage, infarction, and ulceration. This occurs in salmonellosis (Fig. 7-77 ), swine dysentery, Glasser's disease, and colibacillosis. Certain intoxicants such as vomitoxin produced by Fusarium spp. can cause similar lesions.
Figure 7-77.

Acute “Hemorrhagic Gastritis,” Stomach, Pig.
The fundus of the stomach is hemorrhagic. This type of gastric change is often seen in the pig in acute septicemia, for example, from salmonella, and the severe congestion is attributed to venous infarction from endotoxemia. E, Esophageal os; P, pylorus.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
A deep mycosis that causes a granulomatous gastritis is due to Histoplasma capsulatum (see intestinal diseases of carnivores). Very rarely, Mycobacterium tuberculosis causes granulomatous gastritis in a variety of species. In granulomatous gastritis, epigastric discomfort after eating (postprandial), emesis, progressive cachexia, weakness, vomiting of blood (hematemesis), and pyloric obstruction caused by the space-occupying inflammatory reaction occur. In both histoplasmosis and tuberculosis, regional (gastric, splenic, and hepatic) lymph nodes may be affected. Nodular or diffusely thickened gastric and lymphoid lesions contain predominantly macrophages. Mononuclear inflammatory cells, fibroblasts, granulocytes (including eosinophils), and multinucleate giant cells are also present. Often the causative organisms can be demonstrated within the granulomatous inflammation, but special stains, such as acid-fast for mycobacteria and periodic acid–Schiff (PAS) reaction, or Gomori's methenamine silver stain may be necessary to demonstrate fungi.
Eosinophilic gastritis is uncommon in all species of domestic animals but has been reported in pet carnivores. In general, the etiologic basis for this condition is poorly understood. The three types of gastritis characterized by an influx of eosinophils are as follows:
-
•
A characteristic focal eosinophilic infiltrate is sometimes associated with trapped, intramural nematode larvae, especially Toxocara canis. Larvae of T. canis pass to nursing puppies through the milk, through fecal soiling of bedding, or from dirt or other fomites harboring eggs or larvae. After ingestion the parasite's larval sheath, feces, and saliva are antigenic. In dogs and cats, tissue reaction to these larvae in the mucosal and submucosal intestine and gastric epithelial cell is hyperplasia, resulting in a polyp-like proliferation of the antral mucosa. Pyloric obstruction sometimes results.
-
•
In other cases of eosinophilic gastritis the infiltration of eosinophils is more diffuse and is believed to be a hypersensitivity reaction. The offending antigen is not known. In many of these cases there is a peripheral eosinophilia, especially when associated with eosinophilic infiltration of the small intestine (eosinophilic gastroenteritis). This form of eosinophilic gastritis may become transmural, with necrosis and scarring.
-
•
The third type, scirrhous eosinophilic gastritis of dogs and cats, for the most part has unknown causes. The fibrosis associated with scirrhous changes in the stomach and lymph nodes results in persistent emesis, weight loss, and malnutrition.
The gross lesions of eosinophilic gastritis are rather nonspecific and consist of diffuse or nodular mural thickenings. Microscopic lesions are characterized by infiltrates of eosinophils in the mucosa and the submucosa and are seen extensively through the muscularis of the stomach. Similar lesions are sometimes present in segments of the small intestine and colon. In the dog there is sometimes necroproliferative eosinophilic perivasculitis and eosinophilic lymphadenopathy. In the scirrhous form the eosinophilic infiltrate is followed by transmural fibroplasia and scarring.
Hypertrophic or Hyperplastic Gastritis
Hypertrophic gastritis, characterized by thickened rugae, is the result of hyperplasia of the gastric glands. This effect is believed to be a response to chronic retention of gastric fluid and reflux of intestinal bile. Similar mucosal glandular changes are seen in immune-mediated lymphoplasmacytic gastritis of dogs. Hypertrophic gastritis has also been described in primates, horses, pigs, and rodents. The nematode Nochtia nocti causes this lesion in the stomachs of monkeys. Equine hypertrophic gastritis is a focal lesion or more diffuse lesion associated with the nematodes Habronema spp. and Trichostrongylus axei, respectively.
Chronic giant hypertrophic gastropathy of dogs affects the basenji, beagle, boxer, and bull terrier breeds, among others. The disease is similar to Ménétrier's disease in human beings. Clinical signs include weight loss, diarrhea, vomiting, and hypoproteinemia. The chronic gastritis results in increased mucosal permeability to serum proteins with subsequent protein-losing gastropathy. Unlike normal gastric mucosal folds, in giant hypertrophic gastropathy the mucosa does not flatten with distention of the organ (Fig. 7-78 ). Microscopically, the mucosa is hypertrophic and hyperplastic. The incorporation of folds of submucosa and muscularis mucosa is variable, as is the presence of inflammatory cells, principally lymphocytes and plasma cells. The cause of this condition is unknown.
Figure 7-78.

Chronic Giant Hypertrophic Gastropathy, Stomach, Dog.
A cerebriform mass of redundant mucosa is present in the center of the gastric mucosa. Chronic inflammation in the mass results in increased mucosal permeability to serum proteins and a subsequent protein-losing gastropathy.
(Courtesy College of Veterinary Medicine, Cornell University.)
Ulcers—Mucosal Defects
An ulcer is a mucosal defect in which the entire epithelial thickness, down to or through the basement membrane, has been lost. Penetration through the remaining tissue layers to the peritoneal cavity is termed a perforating ulcer. Partial-thickness epithelial loss is termed an erosion. Chronic ulcers differ from acute ulcers by the presence of an indurated rim caused by fibrosis and attempts at epithelial regeneration. The identification of gastric ulcers is not challenging, either at necropsy or by endoscopy. They are sharply bordered cavities, often coated with exudate. Thrombosis of blood vessels is sometimes adjacent to ulcers in ruminants with mycotic vasculitis secondary to ruminal lactic acidosis. Thus it is an infarct.
The pathogenesis of most gastric and duodenal ulcers in human beings has been demonstrated to be a result of infection with a helical bacterium, Helicobacter pylori. The same bacterium has been epidemiologically linked to gastric adenocarcinoma. Helicobacter mustelae acts similarly in ferrets. Although similar, gastric Helicobacter-like organisms are readily demonstrated in dogs and cats, their relationship with ulcer formation or neoplasia is not established. It appears that the stomachs of as many animals without gastritis or ulcers are as heavily colonized by these bacteria as are those of animals with ulcers (Fig. 7-79 ). More than 90% of cats are infected with two Helicobacter spp. Helicobacter felis can be cultured in vitro, but the noncultivatable Helicobacter heilmannii is the more frequent. Pathologic and clinical outcomes appear to depend on a number of bacterial virulence factors as well as on the host response to these agents. Investigations suggest there may be a link between the presence of Helicobacter and other diseases, including coronary and neurologic disease.
Figure 7-79.

Helicobacter spp. Infection, Stomach, Cat.
Numerous spiral bacteria (arrows) are present in the superficial mucous layer. There is no inflammation in the adjacent mucosa; however, in some areas the epithelium is hyperplastic. H&E stain. Inset, The helical shape of the helicobacter organisms is demonstrated with a Steiner's silver stain.
(Figure courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University. Inset courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Theories abound as to the causes of most gastric ulcers in animals. None have been proved. There may be a heritable component to ulcer susceptibility. The conditions necessary for ulcer development boil down to an imbalance between acid secretion and mucosal protection. This imbalance occurs as a result of the following:
-
•
Local disturbances or trauma to the mucosal epithelial barrier; this injury can be due to back flush of bile salts from the duodenum or ingestion of lipid solvents such as alcohol
-
•
Normal or high gastric acidity
-
•
Local disturbances in blood flow (stress-induced and sympathetic nervous system–mediated arteriovenous shunts) resulting in ischemia
-
•
Steroids and NSAIDs that depress prostaglandin formation (PGE2, PGI1) or concentration, thus decreasing phospholipid secretions, which are protective
All of these mechanisms allow pepsin and hydrochloric acid into the submucosa. Severe gastric hyperacidity and gastric ulcers are sometimes associated with the presence of islet cell tumors producing gastrin. Some of these gastrin-producing tumors arise in the duodenum, but the majority originate in the pancreas. These neoplasms release histamine into the bloodstream, which binds to receptors on parietal cells of the stomach, increasing HCl secretion. The gastric ulceration produced associated with these tumors is known as Zollinger-Ellison syndrome.
In dogs, gastric ulceration causes vomiting, inappetence, abdominal pain, and anemia secondary to gastric bleeding (Fig. 7-80 ). Melena (digested blood in feces) may also be present if the ulceration persists, and significant amounts of blood are lost to the GI system. Gastric ulcers in dogs and cats are generally idiopathic but can occur in those animals with mast cell tumors that stimulate gastric HCl secretion through histamine release and its effect on the surrounding blood vessels or other neoplasia that infiltrate and weaken the gastric wall.
Figure 7-80.

Ulcer, Stomach, Dog.
The stomach contains a large volume of clotted and unclotted blood from a gastric ulcer (idiopathic) with rounded edges visible in the left side of the photograph. The hemorrhage was so severe that the dog died from exsanguination.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Ulcers are idiopathic in foals. Foals with gastric ulcers may have abdominal pain, bruxism (grinding of the teeth), ptyalism, and gastric reflux and may lie in dorsal recumbency. Gastric ulcers associated with administration of NSAIDs are common in horses and to a lesser extent in other species (Fig. 7-81 ). Equine gastric ulcer syndrome occurs in 40% to 90% of competitive and performance horses, with the most severe ulcers occurring in those animals that are worked the hardest. More than one-third of horses used less strenuously develop mild ulcers.
Figure 7-81.

Gastric Ulcers, Stomach, Horse.
Administration of nonsteroidal antiinflammatory drugs has caused extensive ulceration of the stratified squamous epithelium (S) of the nonglandular mucosa. The ulceration extends from the cardia (center) to the margo plicatus (right).
(Courtesy College of Veterinary Medicine, Cornell University.)
Cattle with abomasal ulcers have partial or complete anorexia, decreased milk production, palpable discomfort on pressure applied to the right xiphoid area, and melena. In any species the vomiting of coffee grounds–like material (hematemesis) or passage of melena is highly suggestive of gastric ulcer disease. Abomasal ulcers of ruminants vary in significance from subclinical to fatal (Figs. 7-82 and 7-83 ). In calves, ulcers are associated with dietary changes or mechanical irritation of the abomasum by roughage. Dietary changes involve substitution of roughage for milk or milk replacer, together with the associated stress. In dairy cattle, ulcers are associated with heavy grain feeding (lactic acidosis) at the time of parturition, displacement of the abomasum, bovine viral diarrhea, impaction, torsion, and gastric lymphoma. Because cattle have an effective omentum that seals abomasal ulcers, they may live for a long time unless a large perforation occurs, resulting in septic peritonitis.
Figure 7-82.

Ulcers, Abomasum, Cow.
The ulcers consist of a central dark red-gray area of necrosis surrounded by an outer red margin characteristic of active hyperemia and inflammation. The discrete rounded outline of these ulcers suggests that they are infarcts, possibly from vasculitis and thrombosis caused by angioinvasive fungi.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-83.

Perforating Ulcer, Abomasum, Cow.
The rounded borders of the ulcer indicate an attempt at repair and therefore chronicity. Death was due to peritonitis.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
In pigs, gastric ulcers are common and occur in penned pigs fed finely ground grain. These ulcers always are limited to the stratified squamous epithelium of the esophageal portion of the gastric mucosa that surrounds the cardia (Fig. 7-84 ). Death can result from exsanguination into the gastric lumen. Evidence suggests that a high-carbohydrate diet alone is not sufficient to produce erosions and ulcers but rather that the appropriate diet in combination with fermentative commensal bacteria, such as Lactobacillus and Bacillus spp., produces lesions. Lesions progress from parakeratosis to hyperkeratosis through keratolysis to erosive gastritis or perforation of the stomach.
Figure 7-84.

Gastric Ulcer (Pars Esophagea), Stomach, Pig.
This type of gastric ulcer occurs exclusively in pigs and most commonly in confined growing pigs. The lesion is limited to the stratified squamous epithelium surrounding the cardia (pars esophagea). Ulcers in this location characteristically have a multifactorial cause, including the ingestion of finely ground grain or pelleted feed (possibly deficient in vitamin E), fermentation of sugars in the feed, and stress of confinement rearing. These ulcers frequently bleed and can cause exsanguination.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Miscellaneous Disorders
Uremic gastritis occurs most frequently in carnivores as a result of chronic renal disease (Fig. 7-85 ; also see Figs. 1-39, 11-22, and 11-231-3911-2211-23). In ungulates it is a rare event and is usually secondary to obstructive kidney disease (postrenal uremia). Uremic gastritis is characterized by mineralization of the glands, vessels, and lamina propria of the gastric mucosa and sometimes results in ulcer formation.
Figure 7-85.
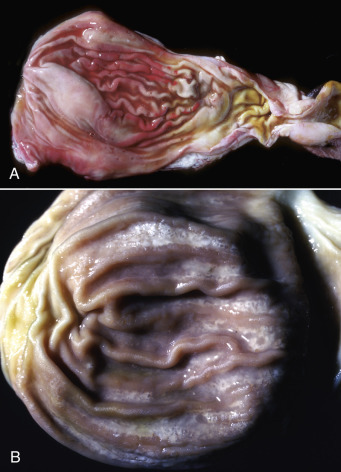
Uremic Gastropathy (Also Called Uremic Gastritis), Stomach, Cat.
A, The major lesion is congestion and edema of the gastric mucosa caused by injury to capillaries within the lamina propria associated with elevated concentrations of nitrogen-derived metabolic waste products in the systemic circulation from kidney failure. B, With chronicity, there is mineralization of the gastric mucosa, visible as fine white stippling and lines in the mucosa.
(A courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee. B courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Amyloidosis occasionally is present in the stomach concomitant with systemic amyloid infiltrates. Generalized amyloid A (AA) amyloidosis with gastric deposits of amyloid has been reported in bats, Siamese and Abyssinian cats, goats, rhesus monkeys, sheep, and Siberian tigers.
Pyloric stenosis can be anatomic or physiologic because of an inability of the pyloric sphincter to function properly. This condition may be congenital or acquired. This lesion occurs most often in dogs (particularly brachycephalic breeds), Siamese cats, horses, and human beings. Congenital pyloric stenoses may be hereditary, at least in human beings. Pyloric stenosis is often first recognized in recently weaned animals by projectile vomiting, retention of gastric contents, gastromegaly, and the presence of strong gastric peristaltic waves (E-Fig. 7-11). Pyloric muscular hypertrophy, variable submucosal edema, vascular ectasia, and degeneration of myenteric ganglion cells (dysautonomia) may be identified histologically in some cases. Functional pyloric stenosis can be a feature of vagus indigestion of ruminants. In general the many causes of pyloric stenosis are not well understood.
E-Figure 7-11.

Pyloric Stenosis, Stomach, Horse.
The probe passes through the narrowed pyloric canal.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Giant hypertrophic pyloric gastropathy, not to be confused with giant hypertrophic gastropathy of basenjis and other dogs, is an idiopathic condition seen most often in older small-breed dogs. To the uninitiated the gross and microscopic features of this pyloric lesion strongly imitate those of carcinoma (Fig. 7-86 ). Microscopically, there is notable foveolar and glandular hyperplasia with variable hypertrophy of pyloric smooth muscle, small mucosal erosions, and ulcerations. There is usually a lymphoplasmacytic infiltrate of variable degree in the lamina propria.
Figure 7-86.

Giant Hypertrophic Pyloric Gastropathy, Stomach, Dog.
The mass of hyperplastic glandular tissue (arrow) at the pylorus could be mistaken for a neoplasm.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Neoplasia
Gastric neoplasia, although uncommon, manifests in different ways in domestic animals. Leiomyoma and more rarely leiomyosarcoma arise from the tunica muscularis (Fig. 7-87 ). Lymphoma can be primary, metastatic, or multicentric in origin (Figs. 7-88 and 7-89 ); also see Fig. 13-94). In cattle, lymphoma is often caused by the bovine leukemia virus and has a predilection for the abomasum, the right atrium, and uterus (Fig. 7-90 ). Squamous cell carcinoma of the stratified squamous (esophageal) portion of the stomach is relatively common in the horse (Fig. 7-91 ). Glandular neoplasms, adenomas, and adenocarcinomas occur in all species but are seen most often in dogs and cats. Dogs and rarely cats occasionally develop gastric mast cell tumors.
Figure 7-87.

Leiomyoma, Stomach, Dog.
This tumor (arrow) arose from smooth muscle in the tunica muscularis and is covered by intact mucosa.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-88.

Lymphoma, Stomach, Cat.
A large expansile white mass is present in the submucosa of the stomach (top edge) and is covered by an intact mucosal epithelium. Note the other lymphomatous white mass, which is ulcerated (lower right). This latter lesion is somewhat atypical of this disease, because ulceration is uncommon and occurs in late-stage disease when the mass is quite large and protrudes into the gastric lumen. In most cases of gastric lymphoma the mucosal epithelium is intact and not ulcerated.
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Figure 7-89.

Lymphoma, Stomach, Horse.
Large smooth-surfaced submucosal nodules (arrows), two of which have a central hemorrhagic ulcer, are present in the glandular portion of the stomach. Ulcers in the stratified squamous portion (white-gray areas) of the stomach are sites of Gasterophilus intestinalis attachment.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-90.
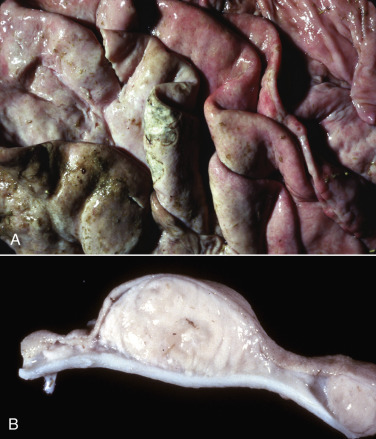
Lymphoma, Abomasum, Cow.
A, Mucosal surface of abomasal folds. Note the folds are thickened and have a pale white-pink color resulting from the infiltration of neoplastic lymphocytes. Overlying mucosae are eroded and ulcerated. B, Transverse section. This cross section demonstrates a white, space-occupying submucosal mass. The intact mucosa is located at the top of the specimen.
(A courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-91.

Squamous Cell Carcinoma, Stomach, Horse.
A large proliferative, ulcerative mass has arisen from the epithelium of the nonglandular (squamous) mucosa of the stomach.
(Courtesy Dr. A. Paulman, College of Veterinary Medicine, University of Illinois.)
Intestine
Developmental Anomalies
Atresia.
Occlusion of the intestinal lumen as the result of anomalous development of the intestinal wall is called atresia (Fig. 7-92 ). Atresia is generally named for the part of the bowel that is occluded, such as atresia ani or atresia coli. The causes of atresia in domestic animals are not completely understood, but they can be a result of mechanical lesions to fetal blood vessels in a portion of the gut, such as caused by malpositioning, that compromise circulation and results in vascular accidents and ischemia. Release of meconium into the abdominal cavity of the fetus may result in sterile peritonitis and may be responsible for some cases of atresia such as in cystic fibrosis of human beings. In still other cases the embryonic cells that normally occlude the lumen fail to break down, resulting in atresia. The end result is segmental atresia in which a segment of the bowel is either entirely missing or completely occluded because of a lack of epithelial development and confluence between two contiguous portions (Figs. 7-93 and 7-94 ).
Figure 7-92.
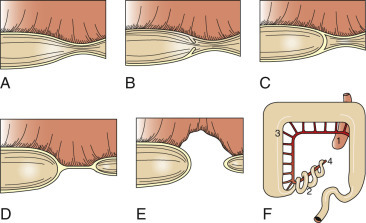
Types of Stenosis And Atresia.
A, Stenosis. B, Stenosis with partial membrane. C, Membrane atresia. D, Cord atresia. E, Blind-end atresia. F, Christmas tree atresia (1, jejunum; 2, ileum; 3, colon; 4, ileocolic artery).
(Modified from van der Gaag I, Tibboel D: Vet Pathol 17(5):565-574, 1980.)
Figure 7-93.

Abdominal Distention, Atresia Coli, Feeder Pig.
This pig has been unable to defecate since birth because of an atretic developmental malformation of the distal colon. Note the greatly distended abdomen.
(Courtesy Dr. J. King, College of Veterinary Medicine, Cornell University.)
Figure 7-94.

Atresia Coli, Colon, Cow.
There is a blind-ended atretic segment of the spiral colon. The smaller segment at the right of the photograph is distal, the terminal part of the colon.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Meckel's Diverticulum.
Meckel's diverticulum is a remnant of the omphalomesenteric duct. Generally it disappears after the first trimester of gestation, but it can persist in all mammalian species. It is near the termination of the ileum, represents the stalk of the yolk sac, and because of its location and being blind ended, can be confused with the cecum.
Megacolon.
Megacolon, as its name implies, is a large, usually fecal-filled colon (Figs. 7-95 and 7-96 ) that can be congenital or acquired. The congenital form occurs in pigs, dogs, cats, overo foals, and human beings from a developmental lack of myenteric plexuses (Hirschsprung's disease) secondary to the failure of migration of neuroblasts from the neural crest to the colorectal myenteric plexuses.
Figure 7-95.

Megacolon, Colon, Cat.
This disease may be congenital due to a lack of intestinal innervation or atresia of the distal colon or anus. It can also be acquired secondary to nerve injury.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-96.

Megacolon, Colon, Dog.
The large colon from the cecum (C) to the anus is dilated with feces. In dogs, this disease has pathogeneses similar to those described in cats (see Fig. 7-95).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
The equine overo pattern of spotting is defined by white patches of epidermis on the ventral or lateral abdomen and extends dorsally up to but not including the dorsal midline. The epidermis is also nonpigmented on the lateral neck and flank. The overo pattern typically includes at least one pigmented leg. Affected foals are white and appear normal at birth. They do not pass meconium; subsequently they develop colic and die usually by 72 hours after birth. These white foals are nonperistaltic because of absence of the myenteric (Auerbach's) plexus or submucosal (Meissner's) plexus, particularly in the colon and rectum. Thus these anomalies can be termed aganglionosis. A congenital aganglionic megacolon is contracted and nonperistaltic. Dilation or megacolon occurs proximal to the aganglionic section of the gut. Acquired megacolon is secondary to damage to the colonic innervation. Such events are usually traumatic and most common in carnivores struck by automobiles. Atresia ani can also result in megacolon.
Intestinal Obstruction
Mechanical obstruction of the intestinal tract occurs in all species of domestic and wild animals. Although foreign bodies of all types have been removed from animals at surgery, the long-term systemic effects of some foreign bodies are also important. These include copper and zinc toxicosis from ingestion of coins in dogs, seals, ruminants, and horses and lead poisoning in cattle from ingestion of old batteries. Primates caged in outdated facilities with lead paint or lead bars can also succumb to lead poisoning. Pythium insidiosum infection has caused intestinal obstruction in a puppy because of inflammation associated with the infection.
Enteroliths and Impaction.
Enteroliths are rare in species other than the horse. The Arabian breed has an increased incidence. Generally, affected animals are more than 4 years old. The stones are usually formed by ammonium magnesium phosphate (struvite) and collect around a small central nidus, often a metallic foreign body (E-Fig. 7-12). Enteroliths vary greatly in size from several centimeters in diameter to greater than 20 cm, and they can weigh several kilograms. They generally lodge at the pelvic flexure or transverse colon. Diets high in magnesium and phosphorus predispose to enterolith formation. In the past, millers' horses (grain and feed mills) had access to large amounts of inexpensive bran, and thus their horses were more prone to enteroliths. In California the feeding of high-protein, magnesium-rich alfalfa hay may partially explain the higher incidence of enteroliths in California horses.
E-Figure 7-12.

Enterolith, Horse.
This cross section demonstrates concentric laminations. A metallic nidus was present in the center of the enterolith.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
The presence of aggregated ingesta that cannot move along the intestinal tract (impaction) occurs in all species. It is especially common in horses after anthelmintic administration and is the result of the rapid die-off of large numbers of nematodes, particularly ascarids (E-Fig. 7-13). Cecal impaction occurs in old horses because of a high-roughage (indigestible) diet, debility, or poor dentition caused by a lack of mechanical leveling of the teeth (floating). Fibrous ingesta can also result in ileal impaction. Large amounts of ingested sand can accumulate anywhere in the equine colon, resulting in impaction (sand colic).
E-Figure 7-13.

Ascarid Impaction, Jejunum, Horse.
Impaction was the result of a rapid “die-off” of the ascarids as the result of administration of an anthelmintic.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Strictures with Obstruction.
Strictures are the result of narrowing of the lumen of a canal, which in the present case is the intestinal canal. They are generally the result of healing with scarring of penetrating and nonpenetrating wounds of all kinds or of a vascular injury causing infarction, followed by healing with fibrosis (Fig. 7-97 ). For example, rectal stricture is a sequela of salmonellosis in pigs and is the result in part of thrombosis of the cranial hemorrhoidal artery and lack of collateral circulation (Fig. 7-98 ) that could otherwise allow the intestinal segment to remain viable. Renal strictures obstruct the intestine.
Figure 7-97.

Stricture, Intestine, Horse.
The dilated intestine (D) is proximal to the stricture. Such strictures can be caused by penetrating or nonpenetrating wounds of all kinds from the luminal surface or secondary to vascular injury.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-98.

Stricture, Colon, Pig.
This lesion (between arrows) in pigs has been attributed to thrombosis of the cranial hemorrhoidal artery from vasculitis and thrombosis caused by salmonella.
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Intussusception.
When one segment of intestine becomes telescoped into the immediately distal segment of intestine, the lesion is called an intussusception (Figs. 7-99 and 7-100 ). The intussusceptum is the trapped segment, and the intussuscipiens is the enveloping portion of the intestine. The cause is generally unknown but is thought to be associated with intestinal irritability and hypermotility. Irritability and hypermotility can occur secondary to enteritis, irritation caused by parasites of all sorts, and general debility. Foreign bodies, neoplasms, and some parasites, such as the nodular worm of sheep (Oesophagostomum spp.), by means of the subserosal nodules it produces, can provide a toehold for the intestine to telescope into itself. In the dog, intussusception of the intestine has been related to, or caused by, handling of the small intestine during surgery, hypertrophied lymphoid nodules, granulomas secondary to inflammatory and parasitic diseases, linear foreign bodies (string) (Fig. 7-101, A ), and ascarids.
Figure 7-99.

Intussusception.
A, Schematic diagram showing the anatomic positioning of small intestinal segments in an intussusception. B, Longitudinal section of small intestinal intussusception demonstrating the position of the intussusceptum (trapped segment) and the intussuscipiens (the enveloping portion) of the small intestine.
(A redrawn with permission from Dr. T. Boosinger. B courtesy Dr. T. Boosinger, College of Veterinary Medicine, Auburn University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
Figure 7-100.

Ileocecal Intussusception, Ileum, Horse.
The necrotic intussuscipiens is present in the lumen of the opened cecum.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-101.
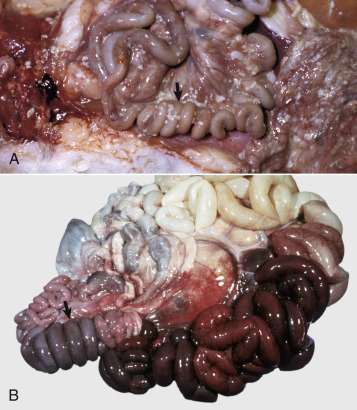
Accordion-Folded Intestines.
A, Small intestine, cat. A linear foreign body (roast beef string) has caused the accordion-folded appearance of the small intestine (arrow). Peristalsis of the intestine over the string, which is taut, in the intestinal lumen causes a sawing, abrasive effect and perforation of the intestine resulting in peritonitis. A white exudate is present on serosal surfaces. B, Intussusception, intestine, pig. The accordion-folded intussusception (arrow) is contiguous with infarcted red to dark red bowel, the result of vascular strangulation.
(A courtesy College of Veterinary Medicine, University of Illinois. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
In cattle and horses, tumors, abscesses, and granulomas may be causes of intussusceptions. In horses, verminous arteritis may uniquely cause intussusceptions. Ileoileal, ileocecal, cecocecal, and cecocolic intussusceptions are sometimes associated with Anoplocephala perfoliata. Rarely, duodenogastric and gastroesophageal intussusceptions occur.
Clinical features of intussusception are similar to those of intestinal obstruction. In small animals with thin abdominal walls, they can sometimes be palpated. Intussusceptions are enlarged, thickened segments of intestine that vary in length. Intussusceptions are grossly swollen, doughy-feeling segments of the intestine. They resemble the folds of an accordion (see Fig. 7-101, B). Red to black discoloration depends on the degree of vascular compromise, ranging from congestion to hemorrhage and necrosis. The mesenteric attachment of the intussusceptum may be seen extending from the lesion. This occurs as the vascular mesentery gets pulled into the intussuscipiens compressing first the thinner-walled veins and then the arteries. Fibrin exudation, ischemic necrosis, congestion, and edema may occur in both the intussusceptum and intussuscipiens. On rare occasions, antemortem intussusceptions spontaneously reduce by sloughing of the infarcted intussusceptum, which then passes in the feces. Often the site of sloughing is replaced with fibrous tissue, and a circumferential scar or stricture forms. Because peristalsis continues after death, intestinal invaginations can occur post mortem. Before attributing death to intestinal obstruction caused by intussusception, there is a need to determine if the intussusception took place before or after death. Because inflammation occurs only in the living organism, postmortem invaginations are easily reduced because there are no adhesions and they are not accompanied by hyperemia or fibrin on the peritoneal surfaces, which remain smooth and glistening.
Ileus.
Paralytic ileus (adynamic ileus) is a nonmechanical hypomotility resulting in a functional obstruction of the bowel (pseudo-obstruction). It can be due to paralysis of the bowel wall (generally the result of bowel manipulation at surgery), peritonitis from any cause, shock, severe pain, abnormal stimulation of splanchnic nerves, toxemia, electrolyte imbalances (especially hypokalemia), vitamin B–complex deficiency, uremia, tetanus, diabetes mellitus, or heavy-metal poisoning.
The gut is not paralyzed, but because of continuous nerve discharge, it becomes refractory, resulting in lack of tonic stimulation of the bowel musculature. In most cases of paralytic ileus, there are no gross lesions other than perhaps atonic dilation of the intestine. It occurs in most animal species.
Grass sickness of horses in Europe, southern South America, and rarely the United States is associated with dysphagia, GI hypomotility, and subsequent colic. Degenerative lesions of this idiopathic condition are present in the autonomic ganglia, suggesting it is an acquired dysautonomia. An occasional outbreak in horses is associated with the temporospatial occurrence of similar lesions in rabbits. Ingestion of Clostridium botulinum type C with subsequent toxin production is suspected to be the cause of this condition.
Intestinal Displacements
Intestinal displacements include herniations that lead to incarcerations (fixation) of the displaced bowel and finally strangulations (interference with blood flow) of the incarcerated segment of intestine and are categorized as internal or external. Internal herniations are displacements of intestine through a normal or pathologic foramen in the abdominal cavity. The most common of these displacements occur in horses and include herniation through the epiploic foramen and through mesenteric tears. The dorsal border of the epiploic foramen is formed by the caudate lobe of the liver and the caudal vena cava. The ventral boundary is the right lobe of the pancreas, the gastropancreatic ligament, and the portal vein. The cranial boundary is the hepatoduodenal ligament, and the caudal boundary is the junction of the pancreas and mesoduodenum. The epiploic cavity is only a potential space. It is proposed that in older horses the caudate lobe of the liver atrophies, enlarging the foramen and allowing loops of intestine to slip through and become incarcerated and strangulated (E-Fig. 7-14).
E-Figure 7-14.

Herniation of Small Intestine through the Epiploic Foramen, Abdomen, Horse.
An enlarged epiploic foramen has allowed the small intestine to herniate through the foramen, become incarcerated, and then strangulated (dark red intestine).
(Courtesy Dr. J. King, College of Veterinary Medicine, Cornell University.)
External hernias are formed when a hernial sac, formed by a pouch of parietal peritoneum, penetrates outside the abdominal cavity. Types of external herniation include umbilical, ventral, diaphragmatic (Fig. 7-102 ), hiatal, inguinal, scrotal (Fig. 7-103 ), and perineal, named for the location of the displaced viscera. Perineal hernias are seen in old male dogs with prostate gland enlargement and obstipation. Some of these herniations (diaphragmatic, perineal) are more correctly termed eventrations (protrusion of the intestine through the abdominal wall or diaphragm) because they are not accompanied by a peritoneal pouch. Postoperative wound dehiscence of a ventral abdominal incision also causes eventration. It should be noted that umbilical hernias are generally caused by a defect in the abdominal wall and not by the chewing on the umbilical cord by the dam. Umbilical hernias may have a genetic basis, so it may be a matter of some ethical concern whether to surgically repair these hernias in show and breeding animals. In calves, umbilical infections are also associated with an increased risk for hernia development.
Figure 7-102.

Diaphragmatic Hernia, Abdomen, Cat.
Traumatic rupture of the diaphragm has allowed intestine, stomach (S), and liver into the thoracic cavity, resulting in displacement and compression of the thoracic viscera and consequently compromise of cardiopulmonary function. K, Kidney.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-103.
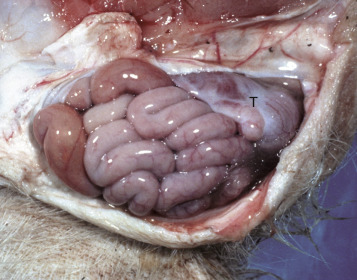
Scrotal Hernia, Scrotum, Pig.
Loops of intestine within the scrotum entered through the inguinal canal to lie in the scrotal cavity and have displaced the testis (T) caudally.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Rectal prolapse may occur secondary to tenesmus or excessive postpartum straining (Fig. 7-104 ).
Figure 7-104.

Prolapsed Rectum, Anus, Cat.
Tenesmus caused the rectum to prolapse.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Volvulus and Torsion.
A volvulus is a twisting of the intestine on its mesenteric axis. A torsion is a rotation of a tubular organ along its long axis. The latter is most common in the cecum of cattle and horses and occasionally of the abomasum of calves (E-Fig. 7-15). Both volvulus and torsion result in compression of the mesenteric veins and arteries, resulting in ischemia initially followed by obstruction—veins first and later as the pressure on the mesenteric vessels increases, the arteries. Infarction is a result of occlusion of the thin-walled mesenteric veins. Because the mesenteric arterial supply is anatomically more resistant to occlusion, blood is pumped into the twisted segment but cannot drain. Edema, congestion, hemorrhage, and eventual necrosis result (Figs. 7-105 and 7-106 ). It is probable that the mechanism of intestinal twisting is secondary to movement of the walls of the abdominal cavity (i.e., the intestine stays still and the horse rolls or otherwise moves around the static intestine).
E-Figure 7-15.

Volvulus, Abomasum, Calf.
The volvulus took place at the omasal-abomasal junction, compromising the abomasum's venous return and resulting in severe passive congestion of the abomasal mucosa.
(Courtesy Dr. J. King, College of Veterinary Medicine, Cornell University.)
Figure 7-105.

Infarction, Small Intestine, Horse.
Volvulus of the intestine has resulted in vascular compromise and infarction (dark red intestine) of several loops of bowel.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-106.

Torsion, Large Colon, Horse.
A, Rotation of the colon on its long axis has resulted in severe colic with strangulation (arrow). Note the red to blue discoloration of the colon distal to the torsion caused by obstruction of venous blood flow. B, Note the sharp line of demarcation (point where the torsion occurred) between viable colon (to the right) and nonviable colon (to the left) caused by obstruction of venous blood flow. In this case, the torsion was not found at the time of necropsy; however, a torsion will commonly untwist itself (reduce itself) during transport of the cadaver to the postmortem room.
(A courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University. B courtesy Dr. M.D. McCracken, College of Veterinary Medicine, University of Tennessee.)
At surgery or necropsy the twisted segment of intestine is distended with gas and fluid and is discolored either dark red or black (see Fig. 2-40). There is usually a sharp line of demarcation between the affected and normal intestine. This line marks the site for surgical resection. A volvulus may result in a rotation of the intestine up to 720 degrees, either clockwise or counterclockwise on its mesenteric axis. Therefore surgical correction of a volvulus may be difficult and complex. It is very important to determine the viability of the bowel after reduction of a volvulus. The affected segment of intestine is often necrotic, congested, and hemorrhagic. Intestinal stasis and toxemia and/or bacteremia may result from bacterial overgrowth and anoxic bowel necrosis. Reperfusion injury may also occur. Toxemia and intestinal rupture may result in death.
Volvulus of the equine large intestine occurs most commonly in the left colon. In horses the left ventral colon is an extension of the right ventral colon beginning at the sternal flexure. The left ventral colon doubles back on itself in the pelvic inlet to form the left dorsal colon. This pelvic flexure can be palpated rectally. The left dorsal colon becomes the right dorsal colon at the diaphragmatic flexure. The diaphragmatic flexure lies cranial to the sternal flexure and usually contacts the ventral body wall. The left dorsal colon is sacculated with one taenia; the left ventral colon is sacculated with four taeniae. When twisting occurs, it is usually clockwise around the mesocolon and is thus a volvulus. Torsion of the large colon of mares accounts for half of their intestinal displacements in the peripartum period.
A peculiar type of intestinal strangulation occurs in horses in which lipomas, which are pedunculated, wrap around the intestinal mesentery or the bowel, causing ischemia, colic, and death (Fig. 7-107 ). Pedunculated lipomas may rotate about their pedicle, cutting off their own blood supply. When this occurs, they undergo mineralization and sometimes ossification. The stalk may become necrotic and break, leaving a free-floating lipoma within the abdominal cavity, where it apparently does no harm. However, most mesenteric lipomas are of no clinical consequence. Rarely, intestinal strangulation by pedunculated lipomas has been reported in the dog.
Figure 7-107.

Pedunculated Lipomas.
A, Intestinal strangulation by pedunculated lipomas, small intestine, horse. Two lipomas (arrows) have wrapped around the mesentery and strangled the bowel resulting in infarction (dark red intestine).B, Mesentery, horse. Closer view of a pedunculated lipoma.
(A courtesy College of Veterinary Medicine, Cornell University. B courtesy College of Veterinary Medicine, University of Illinois.)
Miscellaneous Disorders
Cecal or large intestinal rupture occurs most commonly in postparturient mares (see Fig. 7-19) but can also result from impaction and as a complication of anesthesia. The sites of rupture vary, and the mechanisms are unknown. Iatrogenic rectal tearing may occur secondary to rectal palpation (Fig. 7-108 ). The presence of blood on a rectal sleeve after palpation is cause for concern because peritonitis may be the result of penetration of the peritoneal cavity, especially if the tear occurs ventrally.
Figure 7-108.

Ulceration, Rectum, Horse.
Hemorrhage, ulcers, and tears in the rectum are often caused by inexperienced persons or overly vigorous rectal palpation.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Diverticula (sing. diverticulum) are epithelium-lined cavities that are derived from mucosal epithelium that extend through the muscularis mucosa, submucosa, and muscularis and often reach the serosa, where they sometimes rupture, causing peritonitis (Figs. 7-109 and 7-110 ; E-Fig. 7-16). This can occur in any part of the tubular gut, including the esophagus and cecum.
Figure 7-109.

Diverticula, Cecum, Horse.
Diverticula are mucosal outpouchings into the subjacent smooth muscle layers of the colon. They are filled with ingesta and lined by intact mucosa.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-110.

Diverticulum, Colon, Cow.
A diverticulum (D) lined by superficial mucosa has penetrated through the submucosa to lie next to the muscularis. H&E stain.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
E-Figure 7-16.

Mesodiverticulum, Ileum, Horse.
An intestinal mucosal outpouch has penetrated the wall of the intestine and extended into the mesentery (red nodule).
(Courtesy Dr. J. King, College of Veterinary Medicine, Cornell University.)
Muscular hypertrophy of the distal ileum is an idiopathic condition of horses and pigs. Although generally an incidental finding, hypertrophy of the tunica muscularis can lead to impaction and rupture of the ileum. The lesion in horses is sometimes segmental, affecting the ileum and variably the jejunum. Often the lesion is a sequela of muscular hypertrophy caused by a damaged or stenotic ileocecal valve. Muscular hypertrophy of horses may also affect the duodenum and jejunum in association with diverticula in those gut segments. Horses with muscular hypertrophy of the distal ileum may have mild colic, occasional diarrhea, and weight loss. Often muscular hypertrophy is asymptomatic. Muscular hypertrophy of the ileum in pigs generally occurs as an idiopathic, asymptomatic lesion. Muscular hypertrophy of the tunica muscularis associated with diverticulosis of the ileum has been recorded in young Yorkshire pigs and in Romney Marsh and Hampshire sheep. The lesion is suspected to be secondary to a functional obstruction of the ileocecal valve. Diverticulosis and/or intestinal rupture may result.
Cats can have a severe hypertrophy of the inner, circular layer of the tunica muscularis of the ileum and sometimes the jejunum. In cats with hypereosinophilic syndrome, a disease characterized by intramural eosinophil infiltrates, hypertrophy of the gastric antrum and small intestinal musculature can occur. Muscular hypertrophy of the intestine and medial hyperplasia of the pulmonary arteries occur in cats given large oral doses of Toxocara cati larvae. These conditions are often accompanied by diarrhea and eosinophilic enteritis. Fibrosis of the lamina propria and hypertrophy of the inner layer of the tunica muscularis may result in a stiff, thickened intestine.
Another unique lesion in the horse is hemomelasma ilei. These lesions are pink to black plaques that vary in length from several millimeters to many centimeters and can occur anywhere in the intestinal subserosa but are generally limited to the ileum (Fig. 7-111 ; also see Fig. 3-38). They are attributed to larval migrations of strongyles (usually Strongylus edentatus) and are located on the antimesenteric serosal surface. However, parasites have never been reported in the lesions, and therefore the cause of hemomelasma ilei is unknown. The lesions are generally of no clinical consequence but can on occasion lead to intestinal strictures and intermittent colic.
Figure 7-111.

Hemomelasma Ilei, Ileum, Horse.
Hemorrhagic and siderotic (yellow-brown) fibrovascular plaques on the antimesenteric serosa are attributed to strongyle larval migration (Strongylus edentatus), but this association has never been demonstrated.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Intestinal ceroidosis or leiomyometaplasia is also called brown dog gut. The discolored intestinal smooth muscle may occur in association with chronic enteritis and pancreatitis. Experimentally, leiomyometaplasia can be produced in dogs by vitamin E deficiency, in association with excess dietary lipids. The dietary requirement for vitamin E is proportional to the concentration of polyunsaturated fatty acids in the diet. Intestinal ceroidosis probably does not cause clinical signs but may be an indicator of a metabolic or nutritional disorder. In this condition the intestinal serosa varies from tan to dark brown (Fig. 7-112 ). The stomach and large bowel are variously affected, as is the small intestine. Accumulation of brown, granular, acid-fast–staining ceroid in the perinuclear lysosomes of the leiomyocytes is characteristic of this condition.
Figure 7-112.

Leiomyometaplasia, Intestine, Dog.
“Brown dog gut” is a rare condition caused by the accumulation of a brown pigment now known to be ceroid (formerly called lipofuscin) in the lysosomes of smooth muscle cells of the tunica muscularis. It is a dietary condition associated with vitamin E deficiency.
(Courtesy Dr. L. Borst, College of Veterinary Medicine, University of Illinois.)
Amyloidosis occasionally is present in the intestinal and vascular walls of the lamina propria and muscularis in association with systemic amyloid A infiltrations in a variety of animal species of all ages.
Tiger striping is a nonspecific congestion of colonic ridges secondary to diarrhea and/or tenesmus (E-Fig. 7-17). The red and pale longitudinal stripes are formed by the congested tips of the folds alternating with the uncongested mucosa between them.
E-Figure 7-17.

Tiger Striping, Colon, Dog.
Nonspecific congestion and hemorrhage of the colonic ridges is due to tenesmus and/or diarrhea.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Small Intestinal Intoxicants
Because most toxins enter the body through ingestion, those that are irritants can cause contact lesions in the oral cavity, esophagus, stomach, and intestine. The lesions that result are generally those of hemorrhage and inflammation. In many cases of intoxication, induction of vomiting is contraindicated because what burns going down will also burn coming up. For some intoxicants, multidrug resistance (MDR1) gene products of enterocytes are part of the detoxification process. In addition, P450 enzymes are present on villus enterocytes, although in much lesser amounts than in the liver. They are in highest concentration in the jejunum and decrease aborally. In human beings, ingestion of grapefruit juice interferes with the function of these enzymes, sometimes resulting in enhanced oral drug availability.
The numbers and types of chemicals and intoxicants animals are exposed to make a listing of them a monumental undertaking. A few examples are phosphorus, arsenic, bracken fern (cattle), mercury, oak, copper, nitrate, thallium, and blister beetles. Blister beetles, a specific toxicity, are sometimes incorporated into crimped hay (Fig. 7-113 ). They contain a topical irritant called cantharidin. Lesions include sloughing of the epithelium of the stomach and enterocytes of the proximal small intestine (Fig. 7-114 ). In addition, cantharidin can cause hemorrhagic ulcers of the urinary bladder and myocardial necrosis.
Figure 7-113.

Striped Blister Beetles.
Numerous species of blister beetles (Epicauta spp.), such as gray, black, and striped, can be found throughout the United States. They contain a vesicant (blister-causing substance) that causes inflammation and blistering of mucosal surfaces when they are ingested. Usually these beetles are trapped and crushed in crimped hay.
(Courtesy Dr. W. Crowell, College of Veterinary Medicine, University of Georgia; and Noah's Arkive, College of Veterinary Medicine, University of Georgia.)
Figure 7-114.

Acute necrohemorrhagic Enteritis, Small Intestine, Horse.
The severe necrosis with sloughing of intestinal mucosa is the result of cantharidin, a toxin contained in ingested blister beetles.
(Courtesy Dr. R. Panciera, School of Veterinary Medicine, Oklahoma State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
Although not generally considered an intoxicant, corticosteroids cause colonic perforation in some treated dogs and can delay GI healing. They do this by decreasing cell turnover, decreasing mucus production, and stimulating gastrin secretion, leading to increased acid production. NSAIDs can cause right dorsal colitis in horses. This colitis is characterized by necrosis, resulting in erosions and ulcers. Epithelial loss may be severe, with only regenerating, rounded islands of normal mucosa remaining. The massive edema of the denuded intestine causes rupture of the submucosa in an elongated diamond-like pattern. The mechanism of injury is direct by topical application (oral administration) and through inhibition of prostaglandin synthesis. Neutrophils play a role by increasing synthesis of tumor necrosis factor-α, leukotriene B4, and upregulation of leukocyte adhesion molecules.
Vascular Diseases of the Intestine
Strongylus Vulgaris.
See Disorders of Horses.
Lymphangiectasia
Lymphangiectasia (i.e., pathologic dilatation of lymphatic vessels) may be congenital as a result of vascular malformations or acquired secondary to space-occupying lesions of the lamina propria. Most often it is idiopathic. It results in malabsorption, steatorrhea, and protein-losing enteropathy.
Innervation Disorders
See Dysfunction/Responses to Injury, Intestine, Disorders of Innervation.
Diseases Caused by Specific Pathogens
A number of pathogens affect different animal species in similar ways. The mechanism of damage is similar among these animal species and pathogens. Therefore it is useful to discuss the diseases caused by these organisms across species. Specific diseases that do not have analogues in other species are described later in this chapter. Depending on the mechanism of injury and repair, the morphologic types of infectious enteritis include necrotizing, hemorrhagic, fibrosing, lymphoplasmacytic, eosinophilic, granulomatous, proliferative, catarrhal, pseudomembranous, or combinations of these.
Viral Diseases
Group A Rotavirus Enteritis.
Rotaviruses are ubiquitous pathogens present everywhere in the environment, including air and water. Each species of animal has its specific rotavirus, and although broad similarities exist in pathogenesis among viral infection of individual species, in general the viruses are not cross-infective among species. These viruses are important pathogens. Human group A rotavirus, for example, kills a million children a year in the developing countries of the world. In all species these viruses cause disease in association with other enteropathogens of neonates.
In calves the disease is most important during the first week of life and in piglets in the first 7 weeks of life. These ages correspond to the reduction of colostral and milk-associated antirotavirus antibody titers that occur after weaning. Specific diagnosis of these diseases is difficult for a variety of reasons. The virus is ubiquitous and therefore can be isolated or detected in many animals, most of whom do not have clinical disease. Additionally, because the viruses are cytolytic, some animals with viral diarrhea can be negative for viruses because the cells harboring the virus have been shed previously in the feces.
Rotaviruses are approximately 70 nm in diameter and are trilayered. Only the complete triple-layered virion is infectious. Rotaviruses have double-stranded RNA at their core, and protein spikes project from the surface. The complete particle looks like a wheel, thus the appellation rotavirus. The route of infection is oral, and the target cells are villus enterocytes. Piglets and calves with rotavirus disease are dehydrated, have yellow, watery diarrhea, and are weak and depressed. Production of clinical disease depends on the amount of villous epithelium that is lost. This varies by host species.
Pathogenesis.
The epithelial cells over the upper two-thirds of the affected villi of the proximal small intestine are infected first in those species that suffer with severe diarrhea from rotavirus infection (E-Fig. 7-18). Sloughing of villous cells results in shortening and sometimes fusion of villi, if basement membranes are exposed (Fig. 7-115 ). Interestingly, besides causing a malabsorptive diarrhea, rotaviruses produce a secretory enterotoxin nonstructural protein (NSP4) that increases chloride secretion through a calcium-dependent mechanism. This toxin also activates the enteric nervous system and blocks the intestinal sodium/glucose cotransporter. All of these increase fluid and the rate of peristalsis in the intestinal lumen. Depending on the degree of enterocyte loss, recovery may be delayed or incomplete, depending on the amount of absorptive surface that is permanently lost. When death occurs, it is generally associated with intercurrent infections with those organisms that also target villous epithelial cells such as coronavirus, Cryptosporidium, E. coli, coccidia, and others.
E-Figure 7-18.

Rotavirus Enteritis, Jejunum, Piglet.
Infected enterocytes contain large amounts of viral antigen (brown). Note that infected enterocytes are those that cover the tips and upper sides of intestinal villi. Antirotavirus immunoperoxidase stain.
(Courtesy Dr. H. Gelberg.)
Figure 7-115.
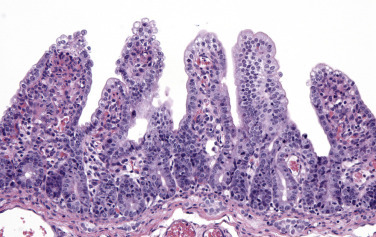
Rotavirus Enteritis, Jejunum, Piglet.
There is notable blunting and fusion of intestinal villi secondary to virus-induced cytolysis of enterocytes covering the tips and sides of intestinal villi. H&E stain.
(Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Coronavirus Enteritis.
Coronaviruses responsible for calfhood enteritis (at 100 to 120 nm) are larger than rotaviruses. Their genetic core is single-stranded RNA. Peplomers project from the surface, resulting in the appearance of a corona, such as created by the sun; hence the appellation coronavirus. The clinical course of the disease, histologic lesions, mechanism of diarrhea production, and age of affected calves are very similar to those of rotavirus enteritis, although somewhat prolonged. Virus infection is more virulent than in rotavirus enteritis, and death is more common. Colitis occurs in addition to small intestinal involvement, but the principal disease signs and pathogenicity are related to the small intestinal lesions. In the colon, similar to the small intestine, enterocytes when lost are initially replaced by less mature and often squamoid cells.
Although generally a mild and self-limiting disease of neonates, feline enteric coronavirus has been associated with fatal enteritis in a series of cats. Lesions consist of degeneration and loss of enterocytes from jejunal villous tips. Cats 2 months to 7 years old are affected.
Pathogenesis.
Unlike in rotavirus enteritis, crypt lumens contain cell debris and crypt cells may be focally hyperplastic, indicating attempts at enterocyte replacement and villus repair. The lamina propria and draining lymph nodes often contain increased numbers of inflammatory cells. A hemorrhagic form of the disease with extensive colitis has been reported.
Adenovirus Enteritis.
Adenoviral infection occurs in cattle, sheep, pigs, goats, Spanish ibex, cervids, horses, and inland bearded dragons. Each species-specific virus causes inapparent respiratory disease and under some circumstances, clinical enteric disease. Other organs may also be affected, such as the liver and kidneys. Endothelial cells are often affected. In Arabian horses and Arabian crossbreeds, adenovirus enteritis occurs in association with combined immunodeficiency. Adenovirus is transmitted by aerosols, feces, and fomites. When enteritis is produced, characteristic basophilic to amphophilic intranuclear inclusion bodies are present in villous enterocytes, usually in young animals that are immunosuppressed. Endothelial cells also are affected and have similar inclusions. Loss of enterocytes results in villous blunting and fusion. In general, adenovirus infection is subclinical, although severe enteric disease may occur in calves.
Bacterial Diseases
Escherichia coli Diseases (Colibacillosis).
Coliform bacteria arrive early among the normal flora that colonizes the intestinal tract of virtually all animals. Young animals are at highest risk for coliform diarrhea, especially pigs and calves. There is interplay of many intrinsic and extrinsic factors that act together to determine if disease will be produced by infection. Some of the factors are the genetic makeup of the host animals, the passive transfer of specific antibodies in the colostrums, the constant bathing of the intestine with milk-associated antibodies from nursing, environmental contamination, and the nutritional plane of the host. Environmental stressors predisposing to disease production include temperature extremes, crowding, and intercurrent infections with rotavirus, coronavirus, Cryptosporidium, coccidia, and others. The development of unique serotypes of E. coli may cause problems in individual environments. E. coli has a large number of mobile genetic elements. Gain or loss of these elements is responsible for the adaptability of E. coli as a commensal and pathogenic agent. In the past, autogenous vaccines, made to order for these environments, have been reasonably effective in controlling some disease outbreaks. Probiotics containing several E. coli types and/or Lactobacillus spp. have shown promise as a preventive in calves. Lytic phages have also been promising in eliminating infection.
There are a variety of classification schemes for the E. coli enteritides. They include enterotoxic (ETEC), septicemic (EIEC), edema disease (enterotoxemic), postweaning, enterohemorrhagic (EHEC), enteroinvasive, and enteropathogenic/attaching and effacing (EPEC/AAEC), among others (also see Chapter 4).
E. coli attaches to cells by a variety of pili or fimbriae (Fig. 7-116 ). Enterotoxic E. coli may have fimbrial antigens F4 (K88), F5 (K99), F6 (987P), 18, or 41 and may also produce up to three enterotoxins and Shiga toxins (STa, STb, LT). Fimbrial and nonfimbrial adhesins, such as adhesins involved in diffuse adherence (AIDA-1), may also be present. Many E. coli produce verotoxins (verotoxic E. coli [VTEC]) important in disease pathogenesis. More than 200 serotypes of verotoxic E. coli have been isolated from cattle alone. Diagnosis of toxin-producing E. coli is by selective culture properties of the bacteria, immunomagnetic separation, and other monoclonal-based immunoassays for the verotoxins and Shiga toxins. A more recent development is the use of real-time PCR to detect pathogenic gene sequences. Many of the virulence factors of E. coli can be exchanged among E. coli and other bacterial species by phages, as well as plasmids.
Figure 7-116.
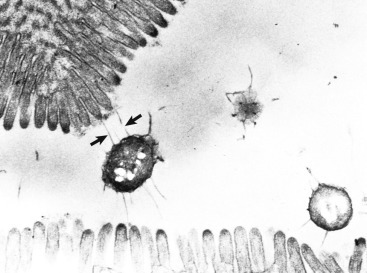
Colibacillosis, Intestine, Piglet.
Escherichia coli pili (arrows) are attached to enterocytes. TEM. Uranyl acetate and lead citrate stain.
(Courtesy Dr. R. Isaacson, College of Veterinary Medicine, University of Minnesota.)
Enterotoxic Colibacillosis.
Enterotoxic, or enterotoxigenic, colibacillosis (ETEC) (F18ac) occurs most often in animals 2 days to 3 weeks of age. Calves and piglets are most often affected. Why enterotoxic colibacillosis is a disease of neonates is not well understood. Some speculation is that enteric bacterial colonization is a function of gastric acidity and that the low pH of the stomach of postneonatal animals kills the bacteria.
The diarrhea that occurs is largely a function of bacterial endotoxin-induced cGMP-dependent and cyclic guanosine monophosphate-adenosine monophosphate (cGAMP)-dependent kinase-induced sodium and chloride secretion into the intestinal lumen. Water is drawn into the intestine to normalize the resultant sodium chloride. Thus the diarrhea is termed secretory. Diarrhea is voluminous, yellow to white, and watery to pasty. At necropsy the small intestine is dilated, flaccid, and filled with translucent, yellow fluid and sometimes gas. Chyle is present in the mesenteric lymphatic vessels similar to animals without enteric disease, indicating that unlike the malabsorptive diseases of the small intestine, absorption proceeds normally in cases of enterotoxic colibacillosis. Microscopically, the intestine is also normal. Diagnosis can be made by light microscopic examination in freshly dead animals by noting the presence of bacteria lining the luminal surface of the enterocytes (Fig. 7-117 ). Inflammation is absent. Affected animals are dehydrated, with a “tucked-up” abdomen. Subsequent to dehydration the eyes of affected animals may be recessed deeply into their sockets (sunken eyeballs). Animals that die from enterotoxic E. coli infection are often emaciated and have diarrheic feces pasted around their perineum.
Figure 7-117.

Enterotoxic Colibacillosis, Jejunum, Piglet.
Mats (arrows) of Escherichia coli are attached to the microvillous surface of the enterocytes. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Septicemic Colibacillosis.
Septicemic or enteroinvasive colibacillosis (EIEC) is a disease of newborn calves, lambs, and occasionally foals that have not received sufficient colostrum to develop immunity. Although the lesions produced are generally those of septicemia, similar to those caused by other organisms, infection can localize in the intestine, causing enteritis. Diagnosis is generally made by finding fibrin in any location in the body such as the eye, joints, abdomen, heart sac, meninges, and/or thorax. The bacteria gain entry to the body through the respiratory system, oral cavity, or umbilicus. Fibrinous arthritis, ophthalmitis, serositis, meningitis (polyserositis), and white-spotted kidneys (cortical abscesses) characterize the septicemia (see Fig. 11-63). Mixed bacterial infections often occur with enterotoxic E. coli.
Edema Disease.
See Disorders of Pigs.
Postweaning Colibacillosis.
See Disorders of Pigs.
Enterohemorrhagic Colibacillosis.
Enterohemorrhagic colibacillosis (EHEC) is described in human beings, laboratory animals, and occasionally cattle and pigs. It has not been reported as a field problem in livestock. The pathogenesis of the disease is similar to that of other invasive bacteria such as Salmonella spp. In human beings the colon is affected. A Shiga toxin gene, a locus for enterocyte effacement, and a plasmid encoding for hemolysin are produced by E. coli, which result in hemorrhagic colitis and sometimes the hemolytic uremic syndrome. These strains are also called verotoxic E. coli, which are strains based on the Vero (African green monkey kidney) cell line on which the bacteria are sometimes grown. Outbreaks of enteroinvasive colibacillosis in human beings are often food-borne illnesses. These organisms are pathogenic because of their acid resistance and ability to survive transport through the stomach. Shiga toxin–producing enterohemorrhagic E. coli O157:H7 rarely causes naturally occurring disease in domestic livestock but often contaminates ground beef. Surveys have indicated that the seroprevalence of E. coli O157:H7 in dairy herds is 38.5%, with an individual cow prevalence of 6.5%, and is most often isolated from the skin surface. This finding is an important reason not to eat undercooked ground beef. Steaks are a different matter because bacterial contamination is only a surface phenomenon, and bacteria are killed by surface searing of meat.
Experimentally, calves may develop necrohemorrhagic or mucohemorrhagic diarrhea. Human disease can be serious, resulting in hemorrhagic colitis, thrombocytopenic purpura, and the hemolytic uremic syndrome. Deer, sheep, cattle, horses, dogs, and rabbits, including laboratory rabbits, may be carriers. Stable flies and fecal contamination of a variety of substances may create fomites.
Attaching and Effacing Escherichia coli.
Attaching and effacing E. coli (AAEC), also called enteropathogenic E. coli (EPEC), has been infrequently reported in rabbits, calves, pigs, lambs, dogs, and human beings. The actual incidence of this disease in domestic animals is unknown. Lesions are characterized by E. coli attachment to the microvillous border of enterocytes and gallbladder epithelium via cups and pedestals (E-Fig. 7-19). Intimin, a bacterial outer membrane protein, facilitates bacterial attachment to the host cell's membrane, resulting in attachment and effacement. These bacteria also alter a variety of tight junction proteins and therefore cause leakage of enterocyte tight junctions. Gross lesions are not present except that the intestine is dilated and fluid filled. Colonization of the epithelium by attaching and effacing E. coli is relatively common; disease occurs most often in association with other enteropathogens of calves of this age, namely rotavirus, C. parvum, enterotoxic E. coli, coronavirus, bovine viral diarrhea virus, and coccidia. In contrast to enterotoxic E. coli infection, in attaching and effacing E. coli infection the brush border of the enterocytes is disrupted and can be seen on select enterocytes in hematoxylin and eosin (H&E)-stained tissue sections. Microvillous disruption results in loss of the glycocalyx digestive enzymes, resulting in maldigestion, malabsorption, and diarrhea. Attaching and effacing E. coli also stimulates enterocyte apoptosis, Cl− and mucus secretion, and toxin production. Attaching and effacing E. coli flagellin TLR5 stimulates interleukin (IL)-8 release by enterocytes, which initiates an inflammatory response resulting in cell death and fluid secretion.
E-Figure 7-19.

Attaching and Effacing Escherichia coli, Intestine, Rabbit.
Bacterial rods have attached to and effaced the microvillous border of enterocytes. TEM. Uranyl acetate and lead citrate stain.
(From Thulin J, Kuhlenschmidt M, Gelberg H: Lab Invest 54:719-731, 1991.)
Extraintestinal Pathogenic Escherichia coli.
Extraintestinal pathogenic E. coli (ExPEC) are gut inhabitants with virulence genes that differ from strains of E. coli that are enteropathogens or commensal organisms of the intestine. They contain fimbrial adhesins for attachment, cytotoxins and hemolysins responsible for tissue necrosis and hemorrhage, and siderophore receptors to sequester iron. Extraintestinal pathogenic E. coli can be isolated from the feces of many healthy animals, particularly dogs and cats. When the animals are stressed, such as in group housing in shelters, aerosolized bacteria may be inhaled, resulting in fulminating necrohemorrhagic pleuropneumonia. Septicemia can result in urogenital infections. In addition, meningitis has been reported in human beings. There is concern about the zoonotic potential of these organisms.
Salmonellosis.
Salmonella spp. are enteroinvasive bacteria. All known species of Salmonella are pathogenic, and salmonellosis is an important zoonosis and nosocomial infection. Salmonellosis is a significant cause of acute and chronic diarrhea and death in numerous animal species and in human beings. S. typhimurium is the second most common food-borne pathogen in human beings. In veterinary medicine, salmonellosis can occur epizootically, enzootically, or sporadically. The serovars most often isolated from diseased animals include S. typhimurium, Salmonella enterica, Salmonella dublin, Salmonella choleraesuis, and Salmonella typhosa.
The salmonellas are Gram-negative, aerobic to facultatively anaerobic, and motile. They survive and multiply within phagocytic cells, resulting in granulomatous inflammation. One way that they survive in the hostile environment of the phagosomes of professional phagocytes is by producing a nitrite transporter through their pathogenicity island (SPI-2) that neutralizes nitric oxide production by the phagocytosing cell. The form of salmonellosis that occurs—septicemic, acute enteric, or chronic enteric—depends on the challenge dosage of the bacterium, previous exposure to the bacterium, and stress factors such as overcrowding, transport, cold temperatures, feed changes, pregnancy, parturition, surgery, anesthesia, and antibiotic administration. Some recovered animals become carriers and shed the organism in their feces, particularly after stress. This may make diagnosis by culture difficult because carriers may not be ill. Conversely, antibiotic treatment of ill animals may create false-negative bacterial cultures. Although dogs and cats rarely get clinical salmonellosis, 10% are carriers and can infect their human companions. It has been documented that fatal salmonellosis may occur in cats in association with homemade, raw-meat diets.
The most common route of bacterial entry is fecal-oral. Effective hand washing is thus of paramount importance for food handlers (“typhoid Mary”). Besides being present in contaminated feed, water, and aerosols, salmonella can be transmitted by flies and fomites. Transplacental infection may also occur. After ingestion, salmonella may colonize regional lymphoid tissue in the oral cavity and gut through dendritic cells by means of pathogenicity islands, which are clusters of plasmid genes coding for virulence factors such as fimbriae, motility, lipopolysaccharide (LPS), and other secreted proteins. Some species of Salmonella are enteroinvasive.
S. choleraesuis and typhimurium in pigs have been shown to adhere to apical membranes of M cells, enterocytes, goblet cells, and sites of cellular extrusion. Salmonellas produce disease via enterotoxins, cytotoxins (verotoxins), and endotoxins, some of which block closure of Cl− channels. In addition, inflammatory cells upregulate PGE2, which results in hypersecretion of chloride. Secretory diarrhea results, as well as malabsorptive diarrhea from enterocyte death. Experimental infections of calves with S. typhimurium demonstrate upregulation of CXC chemokines (IL-8, growth-related oncogene-α [GRO-α], and granulocyte chemotactic protein-2 [GCP-2]), IL-1β, IL-1 receptor-α (IL-1Rα), and IL-4 associated with a neutrophilic influx. Once in contact with macrophages of the lamina propria or Peyer's patches, the organisms are phagocytosed and transported to regional lymph nodes or by way of the portal circulation to the liver. The organisms colonize the small intestine, colon, mesenteric lymph nodes, and gallbladder, which may serve as reservoirs in carrier animals. Salmonellosis infects the young more frequently; the young are more severely affected than are adults; and the young are more likely to succumb to septicemia.
Peracute Salmonella Septicemia.
Peracute Salmonella septicemia is a disease of calves, foals, and pigs. Young animals are generally at greater risk than older animals, although the reasons for this difference are not understood. In foals the feces of affected animals are typically green. The serovar of Salmonella most often involved in septicemic salmonellosis is S. choleraesuis. Gross lesions of animals dying of peracute Salmonella septicemia are minimal and are caused by fibrinoid necrosis of blood vessels (Fig. 7-118 ). Necrosis of blood vessels causes widespread petechiation and a blue discoloration (cyanosis) of the extremities and ventrum of white pigs. Fibrinous polyserositis may be present. Peracute Salmonella septicemia is usually fatal in animals 1 to 6 months of age. Death is usually attributable to disseminated intravascular coagulopathy secondary to the generalized Shwartzman reaction.
Figure 7-118.
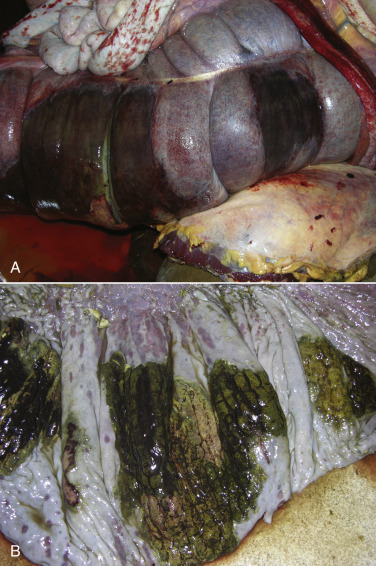
Peracute to Acute Salmonellosis, Colon, Horse.
A, Serosal surfaces. Note the areas of hemorrhage and necrosis affecting multiple sacculations. This pattern is consistent with colonic infarcts secondary to ischemia caused by vascular thrombosis, which can occur with peracute and/or acute salmonellosis. B, Mucosal surfaces. Note the extensive mucosal edema and gray-white areas of mucosal necrosis. The green-stained tissue is postmortem imbibition. Mucosal erosions and ulcerations are also present.
(Courtesy Dr. A. Gillen, College of Veterinary Medicine, University of Illinois.)
Acute Enteric Salmonellosis.
Acute enteric salmonellosis is caused most frequently by S. typhimurium and occurs in cattle, pigs, and horses. Carnivores are rarely affected. Characteristic of the disease is diffuse catarrhal enteritis with diffuse fibrinonecrotic ileotyphlocolitis. Intestinal contents are malodorous and contain mucus, fibrin, and occasionally blood. The feces have a septic tank odor. Salmonella are enteroinvasive through specific surface bacterial fimbrial (pilus adhesin) antigens. Receptor-mediated endocytosis then occurs. Membrane-bound vacuoles then translocate the bacteria to macrophages in the lamina propria. The intact Salmonella induce secretory diarrhea through interference with Cl− channels. They also induce enterocyte apoptosis and recruit neutrophils. Endotoxins induce thrombosis. All these adherence and inflammatory changes are regulated by pathogenicity islands. Multiple foci of hepatocellular necrosis and hyperplasia of Kupffer cells (paratyphoid nodules), when present, are characteristic of acute enteric salmonellosis (see Fig. 8-54). Mesenteric lymphadenopathy is usually present. Fibrinous cholecystitis at necropsy is pathognomonic for acute enteric salmonellosis in calves (see Fig. 8-85).
Chronic Enteric Salmonellosis.
Chronic enteric salmonellosis occurs in pigs, cattle, and horses. Lesions are seen principally in pigs that have discrete foci of necrosis and ulceration, principally in the cecum and colon. These are termed button ulcers (Figs. 7-119 and 7-120 ). Because salmonellosis causes vascular thrombosis and pigs have poor or no collateral blood supply to the rectum (cranial hemorrhoidal artery), in affected animals, rectal strictures develop, with resultant abdominal distention secondary to fecal retention.
Figure 7-119.

Button Ulcers, Colon, Pig.
Multiple foci of necrosis (infarcts [arrows]) due to chronic enteric salmonellosis are termed button ulcers and are pathognomonic for this disease in North America and in other areas in which hog cholera has been eradicated. The morphologic features of this lesion are attributable to bacterial toxin-induced vasculitis and thrombosis of blood vessels in the lamina propria and submucosa resulting in focal intestinal infarcts.
(Courtesy Dr. D. Driemeier, Federal University of Rio Grande do Sul, Brazil.)
Figure 7-120.

Chronic Enteric Salmonellosis, Colon, Pig.
Multiple foci of mucosal necrosis (arrow) are termed button ulcers and are pathognomonic for chronic enteric salmonellosis in hog cholera–free areas. Also see Figure 7-119. H&E stain.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Clostridial Enteritis.
Clostridial organisms cause many diseases that affect animals and human beings. This discussion is limited to those clostridia that produce diarrheal disease. All clostridial enteritides produce enterotoxemias.
C. perfringens is a Gram-positive, anaerobic bacillus that normally inhabits the GI tract and is ubiquitously present in the environment. It is the most important cause of clostridial enteritis in domestic animals. At least 17 exotoxins have been described, but only 4 are believed to be involved in the pathogenesis of disease. Toxin genes are often present on plasmids. These spore-forming bacilli produce their toxins when circumstances provide them with an excess of nutrients that promote bacterial growth in an anaerobic environment. The four major toxins—α (CPA), β (CPB), ε (ETX), and ι (ITX)—are used to classify the toxigenic types of C. perfringens into five major groupings, A through E. The toxins are protein exotoxins, some of which are proenzymes, whereas others have enzymatic activity. C. perfringens type A produces the α-toxin responsible for necrotic enteritis of birds, enterotoxemia of calves and lambs, necrotizing enterocolitis of piglets, canine hemorrhagic enteritis, and possibly equine colitis. Type B produces α-, β-, and ε-toxins and the diseases lamb dysentery, hemorrhagic enteritis of neonatal calves and foals, and hemorrhagic enterotoxemia of sheep. Type C produces α- and β-toxins and necrotic enteritis of birds, hemorrhagic enterotoxemia of neonatal farm animal species, and struck of sheep. Type D produces α- and ε-toxins and pulpy kidney disease of lambs and enterocolitis of goats of all ages. Type E produces α- and ι-toxins and enteritis of lagomorphs and possibly enterotoxemia in calves and lambs.
Enterotoxigenic strains of C. perfringens, particularly type A, are responsible for clostridial food poisoning. This generally occurs when cooked foods are improperly stored, and spores that survive the cooking environment germinate and produce enterotoxin.
Enterotoxemia.
Enterotoxemia is produced by one of the five C. perfringens types described previously. Type D occurs most often. Clostridial enterotoxemia most often affects the better-fleshed animals within a group. Outbreaks often follow an abrupt change in the amount or quality of feed such as occurs in an animal being “finished” for sale or slaughter. In foals, enterotoxemia has been associated with feeding materials rich in carbohydrates and proteins. This diet leads to a change in the intestinal microbial balance. C. perfringens proliferates and produces abundant toxin. Clinical signs may be absent before death or may include diarrhea, sometimes with blood. Glycosuria occurs only in lambs with enterotoxemia and is a helpful feature in preliminary necropsy diagnosis. Enzyme-linked immunosorbent assay (ELISA) kits are available for toxin typing (CPA, CPB, ETX) and for the bacteria.
The small intestine, the target organ of clostridial enterotoxemia, typically has serosal and mucosal petechiae, ecchymoses, and paintbrush or diffuse hemorrhage similar in appearance to those of intestinal strangulation. The intestines are atonic and dilated. Emphysematous enteritis is variably present, as is coagulative necrosis of skeletal muscle. Congestive splenomegaly is present. On exposure to enterotoxin, villous tip enterocytes and midvillous enterocytes degenerate and are sloughed into the intestinal lumen, leaving denuded basement membranes. The exposed basement membranes allow fluid leakage and attract leukocytes into the lamina propria. Death is usually rapid.
Clostridium perfringens Type A.
C. perfringens type A is the most frequently occurring clostridium in mammals and birds. It is also the most common clostridium found in the environment. C. perfringens type A produces enteric disease in a great variety of animals. These diarrheal diseases are generally mild with minimal damage to the intestinal mucosa. In addition to enteritis, infection produces gas gangrene and other anaerobic wound infections. In the western United States, it causes hemorrhagic abomasitis in young ruminants, often accompanied by severe diarrhea. In the Pacific Northwest, principally in Washington and Oregon, a condition called yellow lamb disease is associated with C. perfringens type A. Death is rapid and accompanied by clinical and pathologic signs of hemolysis, hence the yellow discoloration of the carcass.
Clostridium perfringens Type B.
Clostridium perfringens Type C.
Enterotoxic hemorrhagic enteritis affects calves, lambs, and foals during the first few days of life and piglets during the first 8 hours of life. Adult horses may also be affected. Susceptibility of neonates is partially attributed to the antitrypsin activity of colostrum because β-toxin is susceptible to trypsin. Some foods also have antitrypsin effects, and trypsin is sometimes lacking in pancreatic disease. Clinical signs vary from none to bloody diarrhea. When piglets are affected, the whole litter dies. Lesions at necropsy include hemorrhagic or necrotizing enteritis of the small intestines, sometimes with gas in the lumen and within the walls of the intestine (Figs. 7-121 and 7-122 ). In piglets it has been demonstrated that β-toxin induces endothelial damage that is important in disease pathogenesis. Struck, which is also caused by C. perfringens type C, affects adult sheep, goats, and feedlot cattle in winter and early spring and is characterized by hemorrhagic enteritis with ulceration, ascites, and peritonitis.
Figure 7-121.

Enterotoxemia, Small Intestine, Piglet.
The entire small intestinal mucosa is hemorrhagic. Necrosis can extend through the muscularis mucosa and is caused by toxins of the Clostridium perfringens type C group acting directly on the intestinal mucosa in the intestinal lumen. The entire litter of piglets was affected.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-122.

Clostridial Enteritis, Small Intestine, Pig.
Nonspecific necrotizing enteritis results from the toxins produced by Clostridium perfringens type C. Note the disorganization, shortening, and pale staining (with H&E stain) of intestinal villi. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Clostridium perfringens type D.
Clostridium perfringens type E.
Case reports of necrohemorrhagic diarrhea associated with C. perfringens type E infection are poorly documented. It is safest to state that C. perfringens type E may rarely cause enterotoxemia of lambs, calves, and rabbits.
Peracute Hemorrhagic Gastroenteritis of Dogs.
See Disorders of Dogs.
Lincomycin or Antibiotic Enteritis.
Lincomycin or antibiotic enteritis is associated with antibiotic administration and is seen most commonly in rabbits and horses; both are cecal fermenters. It has been suggested but not proved that antibiotic administration causes death of normal enteric flora, which allows overgrowth of C. perfringens type A. Clinical signs and gross and microscopic lesions are similar to those observed in animals with Clostridium spp. enteritis, but bacterial organisms are often lacking.
Clostridium piliforme.
Clostridium piliforme infects multiple mammalian species and is commonly called Tyzzer's disease. The target organs of C. piliforme vary among affected animals. Although pathogen entry is usually via the intestine, the principal target is the liver, but lesions also occur in the intestine and heart. Intestinal involvement is variable and most common in rodents and rabbits. The enteric manifestations of Tyzzer's disease are generally in the distal small intestine, particularly the ileum. Colitis occurs in some cats. Mucosal necrosis and edema extend into the muscularis. Definitive diagnosis is made by finding the causative bacillus (best done with silver stains such as Dieterle's or Steiner's) in the characteristic hepatic lesions (Fig. 7-123 ; also see Fig. 8-53).
Figure 7-123.

Tyzzer's Disease, Liver, Foal.
Criss-crossed bacilli (arrow) resembling Chinese characters or pickup sticks are diagnostic of infection with Clostridium piliforme. Warthin-Starry stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Clostridium difficile.
Clostridium difficile spores are common in the environment and in the intestinal tract of many mammals. They cause pseudomembranous colitis in primates, including human beings, hemorrhagic necrotizing enterocolitis in foals, necrotizing typhlocolitis in horses (colitis X) and possibly cats, and enteritis in a variety of laboratory animals. C. difficile also affects suckling pigs in outbreaks characterized by mesocolonic edema and typhlocolitis. Dogs, especially those hospitalized, may also shed the organism. The disease-producing ability of C. difficile in the dog is not understood, but its zoonotic potential may be important. The induction of disease by C. difficile is likely dose related, but the reasons for bacterial overgrowth, apart from those caused by oral antibiotic administration, are not known. The lesions are similar to those produced by C. perfringens infection.
Lawsoniasis.
Lawsonia intracellularis is the cause of a proliferative segmental enteropathy in a variety of species, including human beings. Lawsonia are curved, Gram-negative, motile, and obligate intracellular bacteria that cannot be grown on artificial media. Lesions of proliferative enteropathy have been reported in pigs, dogs, horses, sheep, rabbits, guinea pigs, hamsters, rats, ferrets, foxes, cervids, monkeys, ostriches, and emus. In the dog the majority of cases occur in puppies younger than 3 months. The mechanism of enterocyte proliferation may relate to Lawsonia-induced altered transcription of host “alarm response” genes that affect regulation of the cell cycle and cell differentiation. Lesions consist of surface erosions and proliferation of cryptal enterocytes with the presence of bacteria in the apical cytoplasm of affected cells. Diagnosis depends on characteristic histologic findings of crypt cell proliferation and on the presence of comma-shaped bacteria in the intestinal crypt epithelial cytoplasm. Clinically, diarrhea is of 5 to 15 days' duration. The diarrhea is mucoid or watery, with or without blood, and is accompanied by partial anorexia, vomiting, and a slight fever.
Campylobacter.
Campylobacter infections from asymptomatic poultry (Campylobacter jejuni) and pigs (Campylobacter coli) are an important issue in food safety and thus an important emerging zoonotic disease. Although C. jejuni is present in a high percentage of dogs without clinical signs, it has been associated with mild enterocolitis in kennels.
Yersiniosis.
Yersinia are Gram-negative aerobic to facultative anaerobic coccobacilli. The species enterocolitica and pseudotuberculosis are normal gut inhabitants that may cause mild to severe diarrhea, septicemia, or lymphadenitis, primarily in ruminants. Pigs, cervids, horses, wild ungulates, poultry, and human beings (food borne) are also susceptible to infection and disease. Carrier states exist in many species, including dogs and cats, and cool climates support bacterial growth and environmental contamination. The bacteria invade the intestine through M cells overlying GALT via bacterial invasins and cell-associated β1 integrins and then spread systemically. Microabscesses and granulomas, including giant cells, occur randomly in the intestinal lamina propria and crypts, and there is widespread lymphoid necrosis. The bacteria are extracellular and intracellular, and there is massive recruitment of host neutrophils. Histologic diagnosis with bacterial isolation is definitive.
Intestinal Mycobacteriosis.
Intestinal tuberculosis, caused by M. tuberculosis and Mycobacterium bovis, is an uncommon disease in cattle, nursing calves, nonhuman primates, and human beings. Although historically associated with drinking unpasteurized milk, more recently, intestinal tuberculosis is an important acquired immunodeficiency syndrome (AIDS)-associated disease in human beings. The bacteria are ingested and then taken up by the M cells of the GALT, particularly in the distal ileum. Like Johne's disease of cattle, intestinal tuberculosis is a chronic wasting disease characterized by a roughened, rugae-like appearance to the intestine.
In small animals it is sometimes clinically possible to palpate the thickened intestine. A thickened colon is sometimes palpable rectally in large animals. Granulomatous lymphadenopathy is often present, sometimes with mineralization and necrosis. The intestinal lamina propria and submucosa, as in Johne's disease, are enlarged and the architecture distorted by epithelioid macrophages and giant cells. Fewer acid-fast organisms are present as compared with Johne's disease. In most cases of Mycobacterium avium-intracellulare–induced intestinal tuberculosis, lepromatous (noncaseating) granulomatous inflammation occurs similar to that of Johne's disease of small ruminants.
Pigs often contract intestinal tuberculosis as a result of the husbandry practice of feeding them avian litter as an inexpensive protein source. As might be expected, early lesions develop in the retropharyngeal lymph nodes.
Alimentary Anthrax.
Anthrax occurs worldwide, principally in ruminants, but any mammal, including human beings, can be affected. In the United States it is a reportable disease and a potential agent of bioterrorism and agroterrorism. Most birds, along with amphibians, reptiles, and fish, are resistant to disease. Herbivores contact the disease by ingesting spore-contaminated vegetation, through a cutaneous wound, or by inhaling spores, whereas carnivores are usually infected by ingesting contaminated carcasses. Biting flies can also transmit the causative bacterium, Bacillus anthracis, or its spores. In peracute disease, generally in ruminants, bacteremia and septicemia result, and the blood may fail to clot because of toxin production from the bacteria. The spleen is often very large and bloody (blackberry jam spleen), and unclotted blood may ooze from any orifice. Blood or exudate smears often demonstrate the organisms as short chains of bacterial cells, thus avoiding the necessity of a necropsy. The spores are very resistant to environmental extremes and are infective. They have been known to survive the tanning process of hides. Pulmonary anthrax in human beings is also called woolsorter's disease. The type of infection that occurs is directly related to the route of infection: cutaneous, respiratory, or GI.
Alimentary anthrax is most common in horses, pigs, dogs, and cats and may be oropharyngeal or intestinal. The oropharyngeal type is characterized by oral or esophageal ulcers with infection of associated lymph nodes. The clinical signs are swelling, dyspnea, and dysphagia. The intestinal form is most severe in the terminal ileum or cecum and is characterized by abdominal pain, hematemesis, and fever. Mechanistically, alimentary infection requires that vegetative bacteria cross the intestinal epithelium. In vitro, anthrolysin O produced by B. anthracis disrupts the intestinal tight junction protein occludin. Cattle may develop ulcerative hemorrhagic abomasitis or small intestinal enteritis, as well as similar lesions in the large intestine (Fig. 7-124 ). The spleen and lymph nodes and mesentery are edematous and hemorrhagic. Pigs are relatively resistant to anthrax; they generally develop pharyngeal and neck swelling, but necrohemorrhagic enteritis may occur. Live attenuated livestock vaccines are safe and generally provide approximately 9 months of immunity.
Figure 7-124.

Necrohemorrhagic Enteritis, Intestine, Alimentary Anthrax, Cow.
A, Note the massive transmural hemorrhage and necrosis caused by anthrax toxin. B, Tissue impression. The light blue bacilli in the debris are Bacillus anthracis bacteria. Some bacilli have blunted ends (presumably spores). H&E stain. C, Tissue impression. Note the dark blue bacilli (Gram-positive) in the debris. Gram stain.
(A courtesy Dr. D. Driemeier, Federal University of Rio Grande do Sul, Brazil. B and C courtesy Drs. V. Valli and J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Parasitic Diseases.
Parasites of the intestinal tract are legion in the various domestic animal species. Refer to a parasitology textbook for specific information regarding the life cycles and identification of the various species. Diagnosis of enteric parasitism is generally performed via fecal flotation or intestinal scrapings.
Amebiasis.
Entamoeba spp. are obligate intracellular parasites with a direct life cycle. The portal of entry is oral. Trophozoites are produced that dwell in the intestinal lumen. They may also invade through the intestinal wall and go to many other organs, such as the liver, brain, and lung, especially in human beings, in whom microabscesses may form. Cysts are excreted with formed feces and continue their life cycle when ingested by another host. Trophozoites are more likely seen in diarrheic feces. Because cysts are the infective form, diarrheic feces of dogs are not usually considered to be especially dangerous to human beings or other animals. The trophozoites vary from 12 to 30 µm in diameter, and the cysts vary from 10 to 20 µm with four nuclei. Contact of ameba and host cells is likely mediated by adhesins. Soluble factors produced by the parasite mediate pathogenicity.
Entamoeba histolytica is zoonotic in human beings, other primates, dogs, cats, and other animals. Disease is serious in human beings. Lesions include colonic congestion, petechia, and ulceration (ulcerative colitis). This colitis may be acute or chronic, bloody or mucoid. In tissue, the amebas may be as large as 50 µm and often form typical flask-shaped ulcers spanning the mucosa and submucosa of the colon. After penetrating the surface mucus and adhering to the colonic enterocytes, E. histolytica releases amebapores (channel-forming peptides) that lyse the enterocytes without killing the ameba.
Balantidiasis (Balantidium coli).
See Disorders of Pigs.
Trichomoniasis.
Tritrichomonas foetus is a sexually transmitted pathogen of cattle. Cats, however, especially those less than a year of age housed in groups, have a tendency toward large bowel diarrhea when infected with this flagellate. Diagnosis is often made by visualization of motile flagellates on fecal wet mounts. Histologic diagnosis is most accurate when at least six biopsy sections of colon containing surface mucus are examined. PCR on paraffin-embedded tissue has also been successful, even in the absence of histologic evidence of the parasite. Infection occurs in the ileum, cecum, and colon. Lesions include mild to moderate colitis, with microabscesses and occasional extension of infection into the lamina propria. There may be colonic enterocyte attenuation and/or increased mitotic activity in the crypts. The 5- by 7-µm teardrop-shaped parasites can often be seen in surface mucus, within colonic glands, and occasionally within macrophages and lymphatic vessels. Thus the parasite is enteroinvasive under certain circumstances. Flagella are not visible on H&E staining. There is no effective treatment. The diarrheal disease in cats generally resolves within 2 years of onset.
Coccidiosis.
Coccidia are exquisitely host- and tissue-specific protozoa. They are obligate intracellular pathogens. Lesions vary from proliferative in sheep and goats (Fig. 7-125 ) to hemorrhagic in dogs, cats, and cattle (Fig. 7-126 ). In pigs a fibrinonecrotic pseudomembrane, without blood, in 5- to 7-day-old animals is characteristic of enteric coccidiosis (Fig. 7-127 ). Eimeria macusaniensis is a relatively common cause of sickness and death in New World camelids of all ages. Gross lesions, even in heavily infested animals, are minimal to absent. In many cases, results of fecal examinations are negative.
Figure 7-125.

Multifocal Proliferative Enteritis, Small Intestine, Goat.
Proliferative nodules (also see Fig. 7-129) in the small intestinal mucosa are characteristic of ovine and caprine coccidiosis. Sporozoites and merozoites infect enterocytes and replicate, stimulating hyperplasia of enterocytes.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-126.

Necrohemorrhagic Enteritis, Small Intestine, Calf.
Coccidiosis in cattle, dogs, and cats is characterized by intestinal hemorrhage. Hemorrhagic diarrheic feces may be visible on the perineum and hind legs. In severe cases there may be anemia, which will be evident as pale external mucous membranes.
(Courtesy College of Veterinary Medicine, Cornell University.)
Figure 7-127.

Fibrinonecrotic Enteritis, Small Intestine, Pig.
Pseudomembranes are characteristic of porcine coccidiosis.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Most species of Eimeria and Isospora infect villous or crypt epithelial cells, more rarely lacteals, the lamina propria, and regional lymph nodes. The coccidia undergo one or more asexual reproductive cycles within enterocytes. The resulting sporozoites produce schizonts containing merozoites, which infect additional enterocytes.
Merozoites produce gamonts that differentiate into microgametes and macrogametes (Fig. 7-128 ). Microgametes fertilize macrogametes, producing zygotes that develop into oocysts. When a small number of coccidia parasitize the intestine of otherwise healthy young growing animals, little disease results. However, when animals are in crowded conditions associated with poor sanitation, fecal-oral transmission of large numbers of organisms can occur. It is in these circumstances, compounded by malnutrition and intercurrent infections or parasitism, that clinical disease results. Enterocyte rupture occurs in all stages of the parasite's life cycle. Clinical disease depends on parasitic load and varies by animal species. Because of diminished epithelial turnover in young animals, they are most susceptible to disease.
Figure 7-128.

Sexual Stages of Intestinal Coccidiosis, Small Intestine, Cow.
Note that the mucosal epithelial cells are distended with microgametes (arrow) and macrogametes (arrowhead). H&E stain.
(Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Gross lesions of coccidiosis are variable by host species, parasite species, and intestinal location. Bleeding is variably present both within species and among species. Coccidiosis in sheep and goats is characterized by enterocyte proliferation that is visible grossly as mucosal nodules (Fig. 7-129 ). The large schizonts of some species are sometimes grossly visible as well. Eimeria leuckarti of horses is asymptomatic. In dogs and cats a slightly different organism, Cystoisospora, is responsible for disease. Intestinal toxoplasmosis of cats is an important zoonotic concern, especially for pregnant women.
Figure 7-129.

Proliferative Enteritis, Small Intestine, Goat.
Coccidia-induced enterocyte hyperplasia results in nodule formation (area identified by dashed lines) as seen in Figure 7-125. Note the hyperplastic enterocytes lining crypts within the nodule. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
“Poor doing” associated with diarrhea is characteristic of clinical coccidiosis. Depending on the host species and the region of intestine that is affected, infected fresh blood may be present in the feces. The presence of tenesmus is variable. Oocysts are usually demonstrable in the feces.
Cryptosporidiosis.
C. parvum is a ubiquitous protozoan pathogen of mammals. Often waterborne, it is a significant cause of municipal water contamination. Although it causes a self-limiting infection in immunocompetent animals, the very young or immunocompromised individuals, such as acquired immunodeficiency syndrome patients, suffer from intractable diarrhea. When treating calves, veterinarians and veterinary students are at particular risk for infection. Cryptosporidia attach to surface epithelial cells of the stomach, small intestine, or colon. The protozoa displace the microvilli and are enclosed by surface cell membranes. Thus the parasite lives in a unique environment described as intracellular but extracytoplasmic (E-Fig. 7-20). Microgametes, macrogametes, schizonts, trophozoites, meronts, merozoites, and oocysts can be demonstrated in the intestine adjacent to, or attached to, epithelial cells. Oocysts are 4 to 5 µm in diameter and are shed in the feces. Studies have indicated that there are species-specific tropisms or biotypes of cryptosporidia. Previously, fecal contamination of water supplies by ruminants was believed to be the cause of most human outbreaks. Molecular typing of the organism has shown in many disease outbreaks that contamination with human feces and human-specific cryptosporidia causes most human epidemics.
E-Figure 7-20.

Cryptosporidiosis, Small Intestine.
A, Cow. Cryptosporidia (arrow) are attached to the microvillus border of the enterocyte membrane. Plastic-embedded, toluidine blue–stained section. B, Rabbit. The cryptosporidia form a trilaminated enveloping membrane on fusion with the enterocyte membrane. Their location is thus intracellular but extracytoplasmic. Microvilli are effaced. TEM. Uranyl acetate and lead citrate stain.
(A courtesy Dr. A.R. Doster, University of Nebraska; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Oocysts can be identified in feces by Sheather's sucrose flotation and a modified acid-fast stain. Cryptosporidiosis causes subacute or chronic, sometimes bloody, watery diarrhea. The mechanism of diarrhea involves more than just cell loss. Prostaglandins, perhaps secreted by macrophages, increase anion (Cl−) secretion through cAMP and inhibit sodium absorption and thus water absorption. In addition, C. parvum interferes with interferon-γ (IFN-γ) gene expression of host cells, thus contributing to immune evasion by the parasite. There is associated dehydration and electrolyte loss. Although the disease can be fatal, particularly in the presence of other pathogens, it is often self-limiting in immunocompetent individuals. In these cases the illness resolves spontaneously in approximately a week.
Affected portions of the GI tract are diffusely reddened and have fluid contents. The organisms appear as tiny blue (hematoxylinophilic) dots attached to the epithelial cells of affected segments. In addition to the dot forms, ring- and banana-shaped organisms are readily seen in Giemsa-stained sections. The lesions of enteritis or colitis consist of decreased mucosal (villous) height, irregular mucosal thickness, crypt necrosis, hyperemia, and an increase in lymphocytes and plasma cells in the lamina propria. Villous atrophy and fusion of the villi of the small intestine are the end result. Because of the intracellular, extracytoplasmic location of the parasite, chemotherapeutic intervention is ineffective. There are few chemicals that can decontaminate the environment. Clorox, for example, is used experimentally to purify the parasites.
Giardiasis.
Giardiasis has been reported in many species, including human beings, dogs, cats, horses, cattle, rabbits, guinea pigs, hamsters, rats, mice, chinchillas, and parakeets. In clinical veterinary practice, giardiasis is frequently recognized in puppies and kittens and causes concern among owners because of its zoonotic potential. Prevalence of the parasite in human beings in the developed world is estimated at 2% to 5%. Giardiasis is caused by a pear-shaped protozoan with posterior flagella, a ventral sucker, and four nuclei, two of which resemble eyes (Fig. 7-130 ). Giardia lamblia (Giardia intestinalis, Giardia duodenalis) parasitizes the small intestine, particularly the duodenum. Giardia attach to the microvillous border of epithelial cells, producing membrane damage. Although generally asymptomatic, diarrhea may result in very young animals or in animals otherwise immunologically deficient.
Figure 7-130.

Giardiasis, Small Intestine, Dog.
A single pear-shaped flagellated protozoa is readily visible in the intestinal lumen (arrow). H&E stain.
(Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Giardia spp. have been shown to induce apoptosis of enterocytes, thus increasing membrane permeability. In large numbers the parasites decrease the absorption of simple sugars and disaccharides secondary to microvillous destruction. Ingesta are then fermented by bacterial flora, creating gas and osmotically drawing water into the intestinal lumen. An enterotoxin stimulates intestinal Cl− secretion. Clinical cases of giardiasis have brown, fluid diarrhea and abdominal discomfort without fever, weight loss, melena, and/or steatorrhea. The diagnosis is made by demonstrating Giardia in preparations of fresh feces or in histologic sections by identifying the organisms either with H&E or Giemsa stains.
Ascariasis.
Ascarids are easily recognized as proximal-intestinal, luminal nematodes that are smooth and white. They are round on cross section, thus giving them the appellation of roundworms together with the other nematodes. They vary greatly in length; the larger the host species, the larger the ascarids. They are 3 to 4 cm long in small animals and attain lengths of 40 to 50 cm in pigs and horses. Ascarids of domestic animals belong to the genera Ascaris (pigs), Parascaris (horses), and Toxocara (dogs, cats, and human beings). The young of these species acquire larval ascarids by intrauterine transmission during the last 7 to 10 days of gestation, through the milk of the dam, and later in life through parasite ova contamination of the environment. After ingestion, infective larvae penetrate the intestine and migrate to the liver via the portal circulation. From there the larvae migrate via the caudal vena cava to the lungs. After leaving the circulation and entering the alveoli, the larvae undergo development and are coughed into the pharynx and swallowed. Development to adults occurs in the intestine. Ova passed in the feces complete the life cycle.
Alternatively, Toxascaris leonina of dogs and cats is ingested via an intermediate host. Hepatopulmonary migration does not occur. Lesions produced by ascarid larval migration include canine multifocal eosinophilic gastroenteritis and visceral larva migrans. Animals affected with heavy ascarid burdens lose weight, grow poorly as a result of competition for nutrients between luminal parasites and the host, and often have a pear-shaped abdomen when held vertically. Adult worms may be vomited or passed in the diarrheic feces. A hacking cough termed thumping is a sign of pulmonary larva migrans, especially in pigs. Anthelmintic administration can cause a rapid die-off of adult ascarids, resulting in intestinal occlusion (see E-Fig. 7-13). Ascarids continue to migrate after the death of the host and may be found in aberrant locations such as the bile duct, stomach, oral cavity, pancreatic duct, and abdomen (see Fig. 7-18).
Hookworm Disease.
Parasitism by hookworms varies from asymptomatic to fatal based on the challenge dose of parasites, the host's age, nutritional status, and likely its immunologic state. When death occurs, it is by exsanguination because hookworms are blood eaters (Fig. 7-131 ). Challenge dosage is often exacerbated by poor nutritional and sanitary conditions, mild climatic conditions, and moisture. Hookworms are generally small nematodes, 1 to 1.5 cm long. Their habitat is usually the proximal small intestine. Genera include Ancylostoma and Uncinaria in dogs, Bunostomum in ruminants, Globocephalus in pigs, and Ancylostoma and Necator in human beings. Ancylostoma caninum in dogs has zoonotic potential. Environmental contamination occurs from the large number of eggs produced in the intestine. The first- through third-stage larvae feed on environmental bacteria. Third-stage larvae are infective and enter the host either by ingestion or direct dermal penetration. From either point of entry, they migrate through the pulmonary system, through somatic tissue to the uterus, or through mucosal tissue. Larvae may also be present in colostrum. The final destination is the intestine, where eggs are produced, completing the life cycle.
Figure 7-131.

Hookworms, Hemorrhagic Enteritis, Small Intestine, Dog.
Where hookworms have detached, hemorrhage is present.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Because prenatal infections with hookworms do not become patent for 11 days, fecal examination results may be negative. Otherwise, fecal examination, especially in young animals with anemia, is diagnostic of this disease. Adult hookworms bury into the villous, ingesting tissue, mucus, and blood (Fig. 7-132 ). When the worm moves to another attachment site, blood may continue to flow from the wound for 30 minutes.
Figure 7-132.

Hookworm Enteritis, Intestine, Dog.
A hookworm has burrowed deep into and attached to the mucosa. H&E stain.
(Courtesy College of Veterinary Medicine, Cornell University.)
Trichuriasis.
Trichurids, or whipworms, are long and slender at their anterior ends and may be numerous within the cecum and colon. Trichurids have a direct life cycle. The name Trichuris translates to “whip-tail,” which is a misnomer because the parasite actually has a “whip-head” that invades and attaches to the mucosa of the cecum, colon, and rectum. Although the parasite ingests blood, anemia is rarely a clinical symptom. Bloody diarrhea may be present. Different species are parasites of carnivores, ruminants, pigs, and human beings. The disease in each species is similar. The horse does not have a whipworm.
Trichuris eggs are elongate, or football shaped, with an operculum at either end, and are very resistant to environmental conditions. Most infections are asymptomatic, and the complete life cycle may take up to 3 months. Therefore repeated dewormings are necessary to eliminate infection, even in the absence of fecal ova. Symptoms may be vague, with only paroxysmal diarrhea. Gross enteric lesions vary from mild to erosive and ulcerative.
Strongyloidosis.
Strongyloides spp. are unique in having free-living and parasitic forms. Rhabditiform larvae may develop parthenogenetically. Free-living parasites are both male and female and undergo sexual reproduction. Enteritis can be severe; larvae or larvated eggs are in the feces of infected animals.
Strongyloides stercoralis of dogs is zoonotic. Strongyloides spp. also infect horses, pigs, and cats. Geographic differences in parasite populations account for differences in virulence within host species. Hyperinfection and autoinfection may occur, adding to the parasite burden. Larvae may enter the host by skin penetration, or less often by ingestion. Strongyloides spp. infection may be acquired in utero and through colostrum and milk. Larvae migrate to the bloodstream and lungs. When they gain access to alveoli, they subsequently migrate to airways, where they are carried, via the mucociliary elevator, to the pharyngeal cavity and are swallowed. Small intestinal parasitism is characterized by larvae residing within superficial mucosa (E-Fig. 7-21). Epithelial destruction by the parasites may result in villous atrophy and crypt hyperplasia. The nonspecific clinical signs include diarrhea, hypoproteinemia, weight loss, and dehydration. Rhabditiform dermatitis may also occur.
E-Figure 7-21.

Strongyloidosis, Small Intestine, Horse.
Cross sections of the parasite (Strongyloides westeri) (arrows) are present in the superficial mucosa. Note the mild chronic inflammatory response with some eosinophils in the lamina propria. H&E stain.
(Courtesy Dr. C.S. Patton, College of Veterinary Medicine, University of Tennessee.)
Pinworms.
Oxyuris equi is the most common pinworm of domestic animals. The parasites occupy the lumen of the distal intestine of horses and occasionally cause rectal pruritus by laying their eggs on the perineal region. Enterobius vermicularis is the pinworm of primates and great apes. It is not zoonotic and is generally of little clinical consequence.
Cestodes.
Tapeworms, although frequently found in the alimentary system, are generally of little clinical significance. They require two and sometimes three hosts, often including arthropods and other invertebrates, to complete their life cycles. Tapeworms attach to the gut wall by means of their anterior scolex, which may have hooks in addition to four suckers (Fig. 7-133 ). Although they can cause some damage at the site of attachment, generally they compete with the host for nutrients. Lacking an alimentary system, they absorb nutrients through their surface. Tapeworms are flat, segmented, and hermaphroditic, reproducing by addition of segments or proglottids. Examples of tapeworms are Anoplocephala spp. in horses, Moniezia spp. in ruminants, and Diphyllobothrium and Dipylidium spp. in dogs and cats. Mesocestoides spp. can infect dogs and cats. In some cases this parasite can perforate through the intestine and proliferate in the peritoneal cavity (see Fig. 7-25).
Figure 7-133.

Cestodiasis, Small Intestine, Fur Seal.
Segmented tapeworms are present in this otherwise normal intestine.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Taenia and Echinococcus spp. are the most destructive of the cestodes. Although carnivores are the definitive hosts, the larval forms reside in the viscera and body cavities of the intermediate hosts, usually ruminants, pigs, horses, or rodents (see Fig. 8-59). Human beings can also become infected, and sometimes it takes 20 or 30 years for clinical disease to appear. The damage in the intermediate hosts may be quite severe.
Trematodes.
Trematodes are uncommon parasites of the alimentary tract. Nanophyetus salmincola uses a snail and a fish as intermediate hosts. It carries the rickettsia responsible for salmon poisoning in the Northwestern United States. Lesions of the intestine are hemorrhagic enteritis.
Alaria spp. can attach to the small intestine of dogs and cats but are generally innocuous. The mesocercariae can cause tissue damage during their migrations through body organs of the host. Paratenic hosts are frogs, snakes, and mice.
Schistosomiasis of ruminants, pigs, horses, and dogs can cause granulomatous intestinal lesions with protein loss secondary to the parasite's presence in mesenteric veins after migration through the liver. Parasites are acquired by direct penetration of the skin by cercariae.
Acanthocephalans.
The thorny-headed worm of pigs, Macracanthorhynchus hirudinaceus, is a small intestinal parasite with a soil-based arthropod intermediate host such as dung beetles. They are thus more common, as are many other parasites in a variety of mammalian species, in “free-range” animals. They are occasionally misidentified as tapeworms, which they superficially resemble. However, they are not truly segmented parasites. They occasionally penetrate the bowel wall at the site of parasite attachment, causing peritonitis. Prosthenorchis spp. are acanthocephalans of primates. Cockroaches are the intermediate hosts.
Intestinal Neoplasia
Neoplasms of various types occur in the GI system of domestic animals. Those of the oral cavity and stomach have already been discussed. Intestinal neoplasms are diagnosed most frequently in dogs and cats, in large part because of their longer life spans. Additionally, pets live in close harmony with their human companions, and thus it is possible that some of the same environmental factors that may contribute to human cancer may cause similar problems in animals.
In dogs, benign neoplasms of the intestinal tract are most commonly adenomas or polyps (see Fig. 6-4), and their malignant counterparts adenocarcinomas. Dogs and cats infrequently develop intestinal mast cell tumors and plasmacytomas. Smooth muscle neoplasms termed leiomyomas and leiomyosarcomas arise from existing intestinal muscular layers. An important caveat in diagnosing these spindle cell tumors is that some of them when examined immunohistochemically are composed of undifferentiated cells with an uncertain histogenesis. These neoplasms have been reported in dogs, horses, rats and primates. They are termed GI stromal tumors (GISTs). Supposition exists that these neoplasms arise from the interstitial cells of Cajal, which normally become the pacemaker cells of the gut. Most are KIT (CD117) positive (proto-oncogene c-kit).
Lymphoma can be solitary, metastatic, or multicentric. In cats the most common neoplasms include alimentary lymphoma (Fig. 7-134 ); mastocytomas (Fig. 7-135 ), which are associated with ulceration; adenomas; adenocarcinomas; and carcinoids. In dogs 5% to 7% of lymphomas are GI. Those of the GI tract are epitheliotropic and primarily T lymphocyte in origin. In human beings, most GI lymphomas are B lymphocyte in origin. In sheep, adenocarcinomas of the intestine are fairly common and are virus induced. In cows, alimentary lymphoma is most common. Horses rarely have intestinal neoplasms develop.
Figure 7-134.

Lymphoma (Lymphosarcoma), Colon, Cat.
Numerous submucosal nodules contain neoplastic lymphocytes. Note that the mucosal epithelium is intact (smooth and shiny) and not ulcerated.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-135.

Mast Cell Tumor, Small Intestine, Cat.
The submucosal nodule (N) contains neoplastic mast cells.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Algae
Chlorellosis and Protothecosis.
Unicellular and sometimes achlorophyllic algae have been reported to opportunistically cause cutaneous or widely disseminated granulomatous disease in a variety of species, including human beings, dogs, cats, dromedaries, gazelle, a beaver, cattle, and sheep. These algae are found in a variety of environmental locales, including both fresh and marine water. Primary infection is believed to be in the alimentary tract with chronic bloody diarrhea or through cutaneous wounds. Lesions are often tinted green if the algae contain chlorophyll. In the intestine the transmural lesions are those of granulomatous enteritis and lymphadenitis. Intracellular algae measuring 5 to 11 µm, including those in giant cells, are visualized by Gomori's methenamine silver or PAS staining of the thick capsule. Chlorella, unlike Prototheca, which is considered to be its achlorophyllous mutant, contains starch bodies and chloroplasts that are birefringent in H&E sections, PAS positive, and diastase negative. Internal septation of the organisms is present with 2 to 20 sporangiospores.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
Parasitic Diseases
Aberrant migration of nematodes and trematodes in most species of mammals can cause focal fibrosis when they travel through the abdominal cavity (see Fig. 8-33). Setaria are nematodes that are sometimes found in the peritoneal cavity of ungulates and rarely cause significant damage in this location. Mild focal peritonitis is sometimes the result of their travels. A variety of cestodes may be found in the abdominal cavity of many species of mammal. Some, such as E. granulosus (hydatid cysts) are zoonotic. Mesocestoides and Porocephalus (pentastomiasis) are found in carnivores, in which their presence may induce a pyogranulomatous reaction (see Fig. 7-25).
Neoplasia
Primary neoplasms of the peritoneum are uncommon with the exception of lipomas, which may become pedunculated and result in intestinal strangulation (see Fig. 7-107). Mesotheliomas occur sporadically in animals and more commonly in human beings (Fig. 7-136 ). In human beings, mesotheliomas are associated with asbestosis and other fibers with similar physicochemical properties and are considered an occupational hazard for some industries. Great efforts have been made to reduce occupational exposure to asbestos. Mesotheliomas have been reported in calves as a congenital disease. Tumors of mesothelial origin are all considered malignant because they may spread transcoelomically. They seldom metastasize to draining lymph nodes or distal sites. They are quite pleomorphic and vary from papillary and adenocarcinoma-appearing to spindloid and fibrosarcoma-like. It is extremely difficult to distinguish neoplastic mesothelium from hyperplastic, reactive mesothelium.
Figure 7-136.

Mesothelioma, Abdominal Cavity, Rat.
Raised nodules (arrows) of neoplastic mesothelial cells are present on serosal surfaces of the abdominal organs.
(Courtesy College of Veterinary Medicine, University of Illinois.)
Disorders of Horses
For disorders occurring in two or more species of animals, see Disorders of Domestic Animals.
Oral Cavity
Teeth
See Disorders of Domestic Animals, Teeth, Infundibular Impaction.
Equine Odontoclastic Tooth Resorption and Hypercementosis
Equine odontoclastic tooth resorption and hypercementosis (EOTRH) is an idiopathic disorder that affects incisor and canine teeth of aged horses. It is often painful with attendant periodontitis and resorption and/or proliferation of mineralized dental tissues. As the name implies, osteoclasts are mechanistically responsible for resorption, which is followed by hypercementosis (Fig. 7-137 ).
Figure 7-137.

Equine Odontoclastic Tooth Resorption and Hypercementosis, Oral Cavity, Horse.
This idiopathic disorder affects incisor and canine teeth of aged horses. It is often painful with attendant periodontitis (arrowheads) and resorption and/or proliferation of mineralized dental tissues (arrows).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Tonsils
Salivary Glands
Sialoadenitis is associated with strangles in horses.
Tongue
Esophagus
Choke
Stomach
Intestine
Intestinal Displacements
Renosplenic Entrapment.
Renosplenic entrapment of the large colon in horses is due to left dorsal displacement of the left dorsal colon or left ventral colon between the spleen and left body wall. Entrapment occurs dorsally over the renosplenic ligament that runs between the left kidney and the spleen. The cause of the displacement is unknown but could occur secondary to rolling behavior in horses or gaseous distention of the large colon. If not corrected either by rolling the horse or by surgery, intestinal rupture and death may result.
Right Dorsal Displacement.
In the equine condition right dorsal displacement, the left dorsal and ventral colons are displaced to the right of the cecum and may result in torsion with signs of colic. It is a surgically correctable disease.
Bacterial Diseases
Rhodococcus equi Enteritis.
R. equi is a soil saprophyte and a normal inhabitant of the equine intestine. The disease caused by this large, potentially zoonotic, Gram-positive, and facultatively anaerobic rod is often characterized by pulmonary pyogranulomas in foals under 6 months of age (see Fig. 9-82) and in immunocompromised adult horses and human beings, or those with intercurrent disease (acquired immunodeficiency syndrome patients). The bacterium is not resistant to neutrophil-mediated destruction but can resist the intracellular environment of macrophages. All pathogenic R. equi isolated from horses but not human beings have a large plasmid and the encoded surface-expressed lipoprotein VapA, which is associated with virulence. The frequent intercurrence of helminths and R. equi infection suggests that migrating larvae aid in distributing the bacterium through the body of the foal. Stringent control of helminth infections may therefore help to reduce or eliminate R. equi infections.
Equine abortion, pneumonia, and placentitis have been associated with infection, as have sporadic infections, sometimes fatal, of a wide variety of mammalian species. R. equi can be isolated from a large number of otherwise healthy mammals of different species.
When coughed up and swallowed in large numbers, the bacteria enter the intestinal M cells overlying the GALT, resulting in pyogranulomatous lymphadenitis of GALT and lymph nodes and pyogranulomatous ulcerative enterotyphlocolitis.
Intestinal infection commences in Peyer's patches, which are ultimately replaced by granulomatous inflammation, abscess formation, and necrotic tissue, and the patches are ulcerated. Infection then spreads to mesenteric lymph nodes with a similar result. Macrophages, often laden with intact bacteria, fill the intestinal lamina propria and submucosa, resulting in a markedly thickened, corrugated intestine. The grossly observable abscesses and foci of necrosis and ulceration often correspond to the distribution of GALT (Fig. 7-138 ).
Figure 7-138.

Multifocal Ulcerative Colitis, Colon, Horse.
Rhodococcus equi infection causes multiple mucosal ulcers centered over gut-associated lymphoid tissue.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Mesenteric, cecal, and colonic lymph nodes are enlarged, firm, and gray (Fig. 7-139 ). They, along with the spleen, may contain granulomas and abscesses (see Fig. 13-68). The large number of macrophages and multinucleated giant cells within the lamina propria and lymphoid tissue is characteristic of this infection. Bacteria may be seen within these cells with Giemsa and tissue Gram stains. The florid inflammatory infiltrate expands the intestinal villi and may distort the crypts of the entire intestinal tract.
Figure 7-139.

Mesenteric Lymphadenitis, Colon, Horse.
Infection of colic lymph nodes with Rhodococcus equi causes pyogranulomatous lymphadenomegaly.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Contamination of skin wounds by R. equi may result in cutaneous ulcerative lymphangitis in horses. Swine cervical lymphadenopathy may also be a result of infection.
Parasitic Diseases
Many parasites cause disease of the stomach, especially in ungulates.
Equine Bots.
Equine bots, Gasterophilus intestinalis and Gasterophilus nasalis, are commonly seen in animals on inadequate deworming regimens (Fig. 7-140 ). Both species migrate in the tissues of the oral cavity and often reside in infected spaces adjacent to teeth. G. intestinalis colonizes the stratified portion of the stomach. The adult fly lays eggs on the hairs of the distal limbs of the horse. G. nasalis lays its eggs around the nose of the horse. The larvae hatch after being moistened and warmed by licking. They are swallowed and live in the glandular stomach and duodenum. Both species attach to the mucosa via their anterior pincers. The larvae pass in the feces, pupate, and develop into flies.
Figure 7-140.

Gasterophiliasis, Stomach, Horse.
Fly larvae (bots) of Gasterophilus intestinalis are attached to the epithelium of the nonglandular portion of the stomach. Note the muscular hypertrophy of the distal esophagus (arrows). Although not shown in this illustration, Gasterophilus nasalis, another similar equine gastric parasite, attaches to the epithelium of the glandular portion of the stomach.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Draschia.
Draschia megastoma is found in “brood pouches” in the glandular mucosa adjacent to the margo plicatus (Fig. 7-141 ). Infection is sometimes referred to as habronemiasis, based on antiquated taxonomic nomenclature in which these nematodes were classified as Habronema spp. Eggs produced in the cysts are extruded through a pore in the brood pouch to the gastric lumen. The eggs pass out with the feces and are consumed by fly larvae that are the intermediate hosts. Both Draschia and Gasterophilus spp. can cause gastric ulcers. Considering their location and means of survival in the stomach, it is remarkable that they do not cause serious damage more often.
Figure 7-141.

Focal Granulomatous Gastritis, Draschia Brood Pouch, Stomach, Horse.
A large parasitic brood pouch is present in the glandular mucosa (right center of illustration) adjacent to the margo plicatus (top right of illustration). Nematodes have been squeezed from the pouch and are visible on the surface (arrow). Histologically, the mucosa is expanded by focal granulomatous inflammation containing clusters of adult Draschia megastoma.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Cyathostomiasis.
In ponies and horses under 5 years of age in temperate climates, sudden emergence of massive numbers of fourth- and fifth-stage cyathostome larvae from the cecum and colon results in necroulcerative hemorrhagic typhlocolitis. Ova are generally not detected in feces, but larvae are often visible.
Rickettsial Diseases
Equine Monocytic Ehrlichiosis.
Equine monocytic ehrlichiosis, also known as Potomac horse fever, was first reported in 1983. It appears that the disease was present for at least the previous 5 years. First described in the Potomac River valley of Maryland, Virginia, and Pennsylvania, it is now found throughout the United States and elsewhere. The common denominator is a proximity of horses to slow-moving bodies of water.
The causative agent, Neorickettsia risticii—an intracytoplasmic rickettsial pathogen of epithelial cells, macrophages, and monocytes—is found in trematodes in freshwater snails. A reduction in pollution levels of the Potomac River basin is believed to have resulted in an increase in the number of freshwater snails. Mayflies and caddis flies have been implicated in transmission. Horses are believed to become infected by eating the dead flies that may accumulate in water buckets and feed troughs, particularly those under artificial light. Rickettsia are often transmitted by arthropods, and this disease is seasonal in northern latitudes (May through September). Without treatment, one-third of cases with diarrhea die as a result of dehydration.
Experimental evidence indicates that N. risticii may be abortigenic. The gross lesions of Potomac horse fever are subtle, consisting of congestion, petechiae, and edema, primarily in the cecum and colon. There is a variable superficial necrotizing enterocolitis. Sometimes the small intestine is affected. Intestinal contents are tan, watery, and malodorous.
Because the experimental reproduction of clinical disease in germ-free animals has not been done, the microscopic appearance of lesions is not certain. Intercurrent bacteria may be responsible for some of the reported lesions. Interestingly, horses with Potomac horse fever have a mild necrotizing typhlocolitis similar in distribution to colitis X and enteric salmonellosis. The nature of the gross lesions is somewhat controversial because experimental infections produce variable results. Like hog cholera, Potomac horse fever is sometimes associated with concurrent Salmonella infection, perhaps accounting for the Salmonella-like lesions. Monocytes and macrophages in all layers of the intestine can be demonstrated with stains, such as Giemsa, to contain Neorickettsia organisms.
Clinical signs associated with Potomac horse fever include fever, watery diarrhea, depression, dehydration, variable colic, laminitis, and subcutaneous edema of the thorax, abdomen, and hind legs. Equine monocytic ehrlichiosis is apparently the same disease known as churrido equino (equine scours), which has been present for more than a century in Uruguay and Brazil.
Idiopathic Disorders
Equine Granulomatous Enteritis.
Equine granulomatous enteritis is characterized by wasting and hypoalbuminemia and has been reported most often in thoroughbred and standardbred horses younger than 5 years of age. The pathogenesis of the disease is unknown. In a few cases Mycobacterium avium was isolated from lesions. The disease is characterized by diffuse or segmental transmural noncaseating granulomatous inflammation of the small and occasionally large intestines. Giant cells are present in approximately half the cases. The result is a notably thickened bowel (Figs. 7-142 and 7-143 ).
Figure 7-142.

Equine Granulomatous Enteritis, Small Intestine (Formalin Fixed), Horse.
The lamina propria (asterisks) is greatly thickened by granulomatous inflammatory cells.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-143.

Equine Granulomatous Enteritis, Small Intestine, Horse.
Mononuclear inflammatory cells (macrophages, lymphocytes, plasma cells) and multinucleate giant cells (arrows) are present in the lamina propria and submucosa. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Clostridial Enteritis (Colitis X).
The severe diarrhea seen in cases of colitis X contains no blood and is rapidly fatal. The cause is unknown. However, the disease is associated with certain environmental and clinical variables. These include exhaustion; shock or other stressors; enterotoxemia, perhaps associated with overgrowth of C. perfringens type A (antibiotic enteritis); Clostridium cadaveris; C. difficile; anaphylaxis; or high protein–low cellulose diets. Lesions are limited to the mucosa of the cecum and colon and consist of edema, congestion, and hemorrhage (Fig. 7-144 ). The location and nature of these lesions overlap with those of acute enteric salmonellosis and equine monocytic ehrlichiosis. Therefore elimination of Salmonella spp. and N. risticii as causes is necessary before a diagnosis of colitis X can be made. Thus colitis X is a diagnosis made by exclusion of other causes. Appropriate lesions such as gelatinous edema of the intestinal wall, combined with variable intestinal congestion and hemorrhage, green, variably bloody diarrhea, and submucosal thromboses and detection of A-B toxins, are diagnostic. At necropsy, in addition to the intestinal lesions, evidence of endotoxic shock, such as disseminated intravascular coagulopathy, thrombosis, and hemorrhage of the adrenal cortices (Waterhouse-Friderichsen syndrome) can be present, as in salmonellosis and other septicemic diseases.
Figure 7-144.

Clostridial Enteritis, Colon, Horse.
Commonly called colitis X, this disease is characterized by mucosal edema, congestion, and hemorrhage. The lesions are attributed to endotoxemia caused by several species of clostridia, most likely Clostridium difficile. Note the punctate mucosal erosions and ulcerations. s, Serosa; m, mucosa.
(Courtesy Drs. V. Hsiao and A. Gillen, College of Veterinary Medicine, University of Illinois.)
Hemorrhagic Fibrinonecrotic Duodenitis–Proximal Jejunitis.
In hemorrhagic fibrinonecrotic duodenitis–proximal jejunitis, also known as anterior enteritis and gastroduodenojejunitis, the morphologic description of the lesions is the same as the name of this idiopathic disease. The disease is characterized microscopically by submucosal edema and a neutrophilic infiltrate of the submucosa and lamina propria. Salmonella and clostridial infections are suspected as the cause. This disease occurs in horses older than 9 years, and the definitive diagnosis is made at necropsy by the characteristic hemorrhagic necrotizing lesions in the small intestine. The duodenum is always involved; jejunal involvement is variable.
Chronic Eosinophilic Gastroenteritis and Multisystemic Eosinophilic Epitheliotropic Disease.
Soft stools accompanied by weight loss characterize chronic eosinophilic gastroenteritis and multisystemic eosinophilic epitheliotropic disease, which are uncommon conditions. The inflammatory reaction consists of eosinophils among other inflammatory cells in both nodular and diffuse accumulations within all portions and layers of the GI system, salivary glands, and mesenteric lymph nodes (Fig. 7-145 ). A circulating eosinophilia may be present. The histologic findings of the condition, especially the presence of eosinophils, suggest a hypersensitivity reaction that in at least one instance was associated with Pythium spp. infection. With the exception of the rare cases with a specific etiologic agent, affected horses die. The disease is associated with an upregulated T helper lymphocyte type 2 response and increased IL-5 production.
Figure 7-145.

Eosinophilic Enteritis, Small Intestine, Horse.
Eosinophils are numerous within the deep lamina propria, mucosal/submucosal interface, and superficial submucosa. Except in rare cases in which an etiologic agent is diagnosed and treated successfully, affected horses die. Inset, The lamina propria contains a mixture of eosinophils, lymphocytes, macrophages, and fibroblasts. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Clinical signs relating to the GI system may include watery diarrhea and hypoproteinemia secondary to protein-losing enteropathy. In human beings and occasionally in horses the lymphoplasmacytic infiltrates in this condition are precursors to lymphoma.
Idiopathic Focal Eosinophilic Enteritis.
Idiopathic focal eosinophilic enteritis is characterized by infiltration of eosinophils along with macrophages and fibroblasts in the mucosa and transmurally to the serosa (see Fig. 7-145). The cause of the condition is unknown and is associated with obstructive colic. Resection of the affected portion of the intestine is curative in most cases.
Cranial Cecal Impaction.
In this uncommon condition, impaction of cecal cupula (cecal base) occurs without other cecal or intestinal involvement. Type I impactions are due to dry digesta; Type II are secondary to motility disorders such as ileus. Typical signs include mild colic without abnormalities being detected by rectal examination. Successful treatment is by typhlotomy and removal of the impacted material.
Anaphylactoid Purpura.
Leukocytoclastic vasculitis associated with numerous discrete foci of necrosis and hemorrhage throughout the intestine and in the mucosa of the larynx and skeletal muscles is termed anaphylactoid purpura in the horse and Henoch-Schönlein purpura in human beings (see Fig. 15-32). Anecdotal evidence suggests that an Arthus-like hypersensitivity reaction to a streptococcal respiratory infection is the mechanism of lesion production.
Parasitic Enteritides
See Disorders of Domestic Animals, Intestine, Diseases Caused by Specific Pathogens, Parasitic Diseases.
Vascular Diseases of the Intestine
Strongylus vulgaris.
In horses Strongylus vulgaris fourth-stage larvae are present in the wall of the cranial mesenteric artery, resulting in arteritis. So-called aneurysms (some with osseous metaplasia and bone marrow) and mural thromboses develop (Fig. 7-146 ; also see Fig. 10-73). In many cases even complete occlusion of the anterior mesenteric artery (see Fig. 2-25) does not result in bowel infarction because collateral circulation will develop if the vascular occlusion develops slowly (Fig. 7-147 ). Therefore it is important to ascertain if the colonic arteries are thrombosed before assigning the cause of bowel death to S. vulgaris. Severe colic and death often result from bowel infarction secondary to verminous arteritis and thrombosis.
Figure 7-146.

Verminous Arteritis, Cranial Mesenteric Artery (C), Horse.
Chronic proliferative arteritis and mural thrombosis have resulted from the migration of Strongylus vulgaris fourth-stage larvae through and within the vessel wall at or near its origin from the aorta (A). The arteritis can lead to mural thrombosis, formation of aneurysms (lower right), arterial mineralization, and infarction of the bowel.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-147.

Infarcts, Small Intestine, Horse.
Thromboemboli from sites of verminous arteritis in the cranial mesenteric artery will often lodge in end arteries of segments of the small intestine, resulting in sudden vascular occlusion and bowel infarction (areas of red to dark red mucosa).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Third-stage larvae are ingested and molt to fourth-stage larvae in the small intestine. They then invade small arterioles on their way to the anterior mesenteric artery. It takes 3 to 4 months in this location until fifth-stage larvae are produced and migrate through the blood vessels to the cecocolonic subserosa. They may be walled off similarly to Oesophagostomum spp. in ruminants and pigs. In the lumen of the large intestine, adults develop. The entire cycle takes up to 6 months or more. Thus the prepatent period in foals is considerable, and by the time ova appear in the feces, significant vascular damage may have occurred. Modern deworming regimens have been quite effective and will hopefully succeed in making this disease of historic significance only.
Intestinal Neoplasia
See Disorders of Domestic Animals, Intestine, Intestinal Neoplasia.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
See Disorders of Domestic Animals; Peritoneum, Omentum, Mesentery, and Peritoneal Cavity.
Disorders of Ruminants (Cattle, Sheep, and Goats)
For disorders occurring in two or more species of animals, see Disorders of Domestic Animals.
Oral Cavity
Viral Diseases
Foot-and-Mouth Disease.
Foot-and-mouth disease is an extremely important disease and disease threat of artiodactyls worldwide but has not appeared in U.S. livestock since 1929, when it was eradicated after an outbreak in California. Virus spreads rapidly and principally by aerosol. The disease is characterized in its early stages by vesicles in the planum nasale, in the oral cavity, and tongue. The picornavirus of foot-and-mouth disease attaches to susceptible cells via integrins on the cell surface. Fluid from ruptured vesicles spreads to areas of abraded skin, for example, skin of a mammary gland. When coronary bands and hooves are affected, coronary band vesiculation may eventually lead to sloughing of the hoof. Although this disease is not fatal, the pain and accompanying inappetence lead to weight loss. If allowed to heal, the hoof will regrow into a ball-like structure. Young animals with foot-and-mouth disease frequently have a viral myocarditis without other signs. Vaccination is short-lived (6 months) and takes time to become effective in individual animals; thus immediate protection is not provided. Persistent infections occur in water buffalo and infected cattle that have been previously vaccinated.
Vesicular Stomatitides.
See Disorders of Domestic Animals, Oral Cavity, Vesicular Stomatitides—Viral Diseases.
Erosive and Ulcerative Stomatitides.
See Disorders of Domestic Animals, Oral Cavity, Erosive and Ulcerative Stomatitides.
Parapox Stomatitides.
The two major diseases in this category, bovine papular stomatitis and contagious ecthyma, are zoonotic. Bovine papular stomatitis is recognized by papules on the nares, muzzle, gingiva, buccal cavity, palate, and tongue (Fig. 7-148 ). Lesions also occur in the esophagus, rumen, and omasum. Microscopically, acantholysis is responsible for the macule and ballooning degeneration of these cells, which may contain intracytoplasmic eosinophilic parapoxvirus inclusions at a later stage (Fig. 7-149 ; also see Fig. 1-11). Erosion of the infected cells accompanied by a neutrophilic infiltrate heals readily from the unaffected basal epithelium. The disease is more common in immunosuppressed animals such as those persistently infected with bovine viral diarrhea virus. In human beings the disease is called milker's nodules and is characterized by papules of the hands and arms.
Figure 7-148.

Epithelial Plaques, Papular Stomatitis, Hard Palate Mucosa, Calf.
Virus-induced (parapoxvirus) epithelial plaques and papules are present on the mucosal epithelium of the hard palate and adjacent gingiva (arrows).
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Figure 7-149.

Hydropic Change, Papular Stomatitis, Hard Palate Mucosa, Cow.
There is massive cytoplasmic swelling (arrows) of the epithelial cells of the stratum spinosum. At an earlier stage, these cells may contain intracytoplasmic eosinophilic parapoxvirus inclusions (not visible here). H&E stain.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Contagious ecthyma, sore mouth or infectious pustular dermatitis, is a condition of sheep and goats characterized by progression of the stages typical of poxviruses—macules, papules, vesicles, pustules, scabs, and scars in areas of skin abrasions, including the corners of the mouth (Fig. 7-150 ; also see Fig. 17-65), mouth, udder, teats, coronary bands, and anus. Occasionally the mucosa of the esophagus and rumen also can be affected. The virus is quite hardy and can survive for 50 to 60 days in the summer and longer in cold weather. At room temperature, scabs containing virus can be infective after 10 years. Eosinophilic cytoplasmic inclusion bodies are visible at microscopic examination of lesions early in the course of disease. The condition in human beings is called orf.
Figure 7-150.

Contagious Ecthyma, Oral Mucous Membranes, Lamb.
Note crusts around nose and lips. Multiple pustules and coalescing ruptured pustules covered by scabs are present on the skin. The parapoxvirus induces epithelial proliferation (acanthosis), followed by vesicle formation. These vesicles rupture and are quickly covered by scabs. Lesions develop at the sites of trauma, such as occur with a nursing lamb, where damage to the superficial oral epithelium allows entry of the virus into skin.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Teeth
Tonsils
See Disorders of Domestic Animals, Tonsils.
Bovine viral diarrhea and rinderpest viruses multiply in the tonsils.
Salivary Glands
Tongue
Esophagus
Rumen, Reticulum, and Omasum
Bloat (Ruminal Tympany)
Ruminal tympany, or bloat, is by definition an overdistention of the rumen and reticulum by gases produced during fermentation. Mortality of affected animals is approximately 50%. A hereditary predisposition to bloat might exist in cattle because cases are on record of bloat in monozygotic twins. Bloat can be divided into primary tympany and secondary tympany.
Primary tympany is also known as legume bloat, dietary bloat, or frothy bloat. It generally occurs up to 3 days after animals begin a new diet. Certain legumes, such as alfalfa, ladino clover, and grain concentrates, promote the formation of stable foam. The nonvolatile acids of legume and ruminal fermentation lower the rumen pH to between 5 and 6, which is optimal for formation of bloat. Foam mixed with rumen contents physically blocks the cardia, preventing eructation and causing the rumen to distend with the gases of fermentation. Clinical signs include a distended left paralumbar fossa, a distended abdomen (see E-Fig. 1-8), increased respiratory and heart rates, and late in the disease, decreased ruminal movements. When death occurs, it is attributable to distention of the abdomen, which compresses the diaphragm, moving it cranially (orad), with resultant decreased pleural cavity size and respiratory embarrassment. There is also increased intraabdominal and intrathoracic pressure, resulting in decreased venous return to the heart and ultimately generalized congestion cranial to the thoracic inlet.
The lesions of primary tympany are often difficult to detect if there is an interval between death and postmortem examination because the foam can collapse. Conversely, fermentation can occur after death in a nonbloated animal, resulting in the production of abundant gas. The most reliable postmortem indicator of antemortem bloat is the sharp line of demarcation most evident in the mucosa between the pale, bloodless esophagus distal to the thoracic inlet and the congested proximal esophagus cranial (orad) to it. This line may sometimes form even after death before the blood clots. This division is known as a bloat line (Fig. 7-151 ).
Figure 7-151.

Bloat Line, Esophagus and Trachea at the Thoracic Inlet, Cow.
There is a sharp demarcation between the caudal (blanched) and the cranial (congested) mucosa of the esophagus (arrow). This demarcation is caused by compromised venous return, the result of a grossly distended rumen displacing the diaphragm cranially and causing increased intrathoracic pressure, thus preventing the flow of venous blood into the thorax. In this illustration, a similar demarcation can be seen on the mucosa of the trachea. The subcutaneous tissues of the neck and head are also congested.
(Courtesy Department of Veterinary Pathology, Cornell University.)
Secondary tympany is caused by a physical or functional obstruction or stenosis of the esophagus, resulting in failure to eructate. Examples of physical causes are esophageal papilloma, lymphoma, esophageal foreign bodies, and enlarged mesenteric or tracheobronchial lymph nodes, usually from lymphoma or tuberculosis. Vagus indigestion or other innervation disorders are examples of functional disorders.
It is questionable if New World camelids bloat.
Foreign Bodies
Foreign bodies can collect or lodge in the rumen. These include trichobezoars (hairballs) and phytobezoars (plant balls). Trichobezoars are sometimes a sequela to a habit of bucket-fed calves sucking on the skin of each other to satisfy their nursing instincts. Trichobezoars can form in utero because of hair circulating in the amniotic fluid and being swallowed by the fetus. Phytobezoars result from an excess of indigestible roughage. Ingestion of nails and wire, common where straw and hay bales are bound by wire, can result in perforation of the wall of the reticulum with resultant reticulitis, peritonitis, or eventually possible pericarditis (hardware disease) (Fig. 7-152 ). Often, in areas in the United States in which ruminants are at high risk for hardware disease because of farming practices, magnets are placed in rumens to prevent the ingested wires and nails from penetrating the reticular mucosa. Occasionally ruminants ingest plates from storage batteries and suffer lead poisoning.
Figure 7-152.

Traumatic Reticulitis, Reticulum, Cow.
Several ingested wires have perforated the wall of the reticulum (arrow) and lodged in the tunica muscularis. Each wire is surrounded by a sinus tract draining to the surface of the reticulum. A chronic ulcer has formed around each area penetrated by the wires.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Inflammatory Diseases
Inflammation of the rumen, rumenitis, is generally considered synonymous with lactic acidosis. Lactic acidosis is synonymous with grain overload, rumen overload, carbohydrate engorgement, and chemical rumenitis. All ruminants are susceptible. The pathophysiologic process of lactic acidosis usually involves a sudden dietary change to an easily fermentable feed or a change in the feed volume consumed. The latter scenario is most likely to occur during weather changes, especially among feedlot cattle, when a sudden cooling rainstorm will stimulate food intake of cattle that had previously lost appetite because of high environmental temperatures and humidity.
Ruminal microflora is generally rich in cellulolytic Gram-negative bacteria necessary for the digestion of hay. A sudden change to a highly fermentable, carbohydrate-rich feed promotes the growth of Gram-positive bacteria, Streptococcus bovis, and Lactobacillus spp. The lactic acid produced by the fermentation of ingested carbohydrates decreases the ruminal pH below 5 (normal, 5.5 to 7.5). This acidic pH eliminates normal ruminal flora and fauna and damages ruminal mucosa. Increased concentrations of dissociated fatty acids lead to ruminal atony. When death occurs, it is due to dehydration secondary to the increased osmotic effect of ruminal solutes (organic acids), causing movement of fluids across the damaged ruminal mucosa into the rumen, acidosis (from absorption of lactate from the rumen), and circulatory collapse. Mortality among animals with lactic acidosis ranges from 25% to 90% and usually occurs within 24 hours.
At necropsy the ruminal and intestinal contents are watery and acidic. Often, abundant grain is found in the rumen. The mucosa of the ruminal papillae is brown and friable and detaches easily, especially from the ventral ruminal sac. Caution must be exercised in interpreting this latter finding as a lesion because the ruminal mucosa often detaches easily in animals that have been dead for even a few hours at high environmental temperatures. Hydropic change and coagulative necrosis of the ruminal epithelium followed by an influx of neutrophils are common microscopic lesions. Animals surviving lactic acidosis develop stellate scars that are visible because of their color difference from the unaffected surrounding ruminal mucosa. Scars are pale; unaffected mucosa may be light to dark brown to black, depending on the original diet.
New World camelids appear to be more sensitive than ruminants to high-carbohydrate diets. Although their compartments do not have papillae, widespread ulceration of the squamous mucosa occurs in cases of lactic acidosis. New World camelids retain feed in their stomach longer than ruminants, possibly increasing fermentation and acid production. They rely on emptying of fluid to preserve milieu. High-energy feeds may quickly impede motility, promoting a drop in pH.
Bacterial rumenitis generally occurs secondary to lactic acidosis or mechanical injury to the ruminal mucosa. Bacteria that colonize the damaged ruminal wall can be transported into the portal circulation and to the liver, resulting in multiple abscesses. Arcanobacterium (Corynebacterium) pyogenes is a common cause of bacterial abscesses in the liver. F. necrophorum, also transported from the rumen to the liver, results in necrobacillosis, which has distinctive liver lesions.
Mycotic infections of the rumen also occur secondary to the damage to the ruminal mucosa caused by lactic acidosis and mechanical injury. Mycotic rumenitis also results from the administration of antibiotics, usually in calves but also in adult cattle, which reduce the numbers of normal flora and allow fungi to proliferate. In cases of mycotic rumenitis, lesions are generally circular and well delineated and are caused principally by infarction from thrombosis secondary to fungal vasculitis (Fig. 7-153 ). Offending fungi include Aspergillus, Mucor, Rhizopus, Absidia, and Mortierella spp. These fungi can spread to the placenta hematogenously and cause mycotic placentitis, which leads to abortions.
Figure 7-153.

Mycotic Rumenitis, Rumen, Calf.
Note the numerous well-demarcated red foci of necrosis and hemorrhage (infarcts) in the ruminal mucosa that can be caused by angioinvasive fungi such as Aspergillus, Mucor, Rhizopus, Absidia, and Mortierella spp. This type of mycotic infection is usually preceded by a chemical (lactic acid) rumenitis (overeating).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Ruminal candidiasis occurs as an incidental finding at necropsy. There is usually an underlying debilitating condition, glucose therapy, milk-replacer overload (sour rumen), or an antibiotic-induced kill-off of resident flora and fauna. Ruminal candidiasis is seldom diagnosed in a live animal.
Miscellaneous Disorders
Ruminal papillae vary in length, becoming longer with high-roughage diets (Fig. 7-154 ). Such diets also can cause the papilla to become tongue or leaf shaped. Animals consuming diets with less than 10% roughage can develop ruminal parakeratosis. These rumens have hard, brown, often clumped, papillae. This lesion has little to no clinical consequence.
Figure 7-154.

Parakeratosis, Reticulorumen, Calf.
A diet that was almost devoid of roughage has resulted in atrophy and parakeratosis of ruminal papillae. Normal papillae are leaf shaped, but some of these papillae have become finger shaped, cauliflower shaped, or clumped. The parakeratotic epithelium has been stained brown to black by components of the feed because of the lack of abrasion by the ground feed. These lesions are most marked on the ventral floor of the ventral sac of the rumen.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Ruminal papillomas are papillomavirus induced in some cases, but in certain countries, bracken fern has been implicated as a cofactor in these forestomach neoplasms (Fig. 7-155 ).
Figure 7-155.

Papillomas, Rumen, Cow.
Smooth-surfaced, squamous papillomas are present on the dorsal wall.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Vagal Indigestion
Vagal indigestion results in a functional outflow problem from the forestomach. Damage to the vagus nerve can occur anywhere along its length and can result in functional pyloric stenosis and omasal dilation. Causes of vagal indigestion include damage to the vagus nerve due to traumatic reticuloperitonitis, liver abscesses with secondary peritonitis, volvulus of the abomasum, and bronchopneumonia. Mechanical obstruction of the forestomach or abomasal outflow can be due to abomasal lymphoma or papillomas or from blockage after ingestion of indigestible or foreign materials. Diet and dwarfism are sometimes associated with vagus indigestion. Many cases are idiopathic. Clinical signs include ruminoreticular distention. The presence of abomasal distention depends on the precise location of the damage to the vagus nerve. Vagal indigestion is divided into the following four types, based on the anatomic location of the functional obstruction.
-
•
Type I is usually caused by inflammatory lesions around the vagal nerve at any location and is a failure of eructation, resulting in bloat.
-
•
Type II is a functional or anatomic condition that results in failure of omasal transport into the abomasum. Usual causes are adhesions and abscesses on the medial wall of the reticulum associated with or secondary to traumatic reticuloperitonitis. Abomasal lymphoma and physical obstruction of the omasal canal (e.g., neoplasia or ingested placenta) may also be causative.
-
•
Type III is caused by physical impaction of the abomasum by roughage and thus is dietary in origin. Abomasal displacements and volvulus are also potential causes.
-
•
Type IV is pregnancy related, perhaps as a result of shifting of position of the abomasum secondary to the expanding uterus, causing compression of the abdominal branches of the vagus nerve.
Ruminal Parasitism
Paramphistomiasis is a fluke infestation of the ruminant forestomach in warmer latitudes around the world. These trematodes are in the genera Paramphistomum, Calicophoron, and Cotylophoron. They are similar in size and appearance to ruminal papillae (Fig. 7-156 ). Although the presence of adult organisms in the forestomach is usually of no clinical significance, heavy infestations of larvae in the proximal small intestine, before migration to the rumen and reticulum, can cause hypoproteinemia, anemia, and death. Larvae burrow deeply into and sometimes through the wall of the small intestine and can be found in the peritoneal cavity. The intermediate host is a snail. Cercariae encyst on aquatic vegetation and are eaten by the ruminant.
Figure 7-156.

Paramphistomiasis, Rumen, Cow.
The pink conical structures located in the center of the illustration are paramphistomes (ruminal flukes). They are considered to be innocuous, but massive numbers of immature flukes in the duodenum may cause a severe catarrhal duodenitis. Note the normal leaf-shaped ruminal papillae, indicative of a high-roughage diet.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Abomasum
Abomasal Displacement
Normally the abomasum lies over the xiphoid process at the abdominal ventral midline. Abomasal displacement is usually to the left side, although right-sided displacements also occur (Fig. 7-157 ). Left-sided displacement of the abomasum is a generally nonfatal entity seen in high-producing dairy cattle during the 6 weeks after parturition. Strenuous activity can predispose nonpregnant cows to displacement. In the postcalving period, abomasal atony can occur as a result of heavy grain feeding (volatile fatty acids decrease motility) and hypocalcemia. Meanwhile, the gravid uterus may have displaced the rumen and abomasum cranially and to the left, rupturing the attachment of the greater omentum to the abomasum. The abomasum then occupies the cranial left quadrant of the abdomen and displaces the rumen medially. This change leads to partial obstruction of abomasal outflow. Metabolic alkalosis contributes to rumen atony and impaired movement of ingesta. The associated hypochloremia is a result of HCl secretion and is common along with hypokalemia. Abomasal ulcers and peritoneal adhesions can result in cases of chronic displacement.
Figure 7-157.

Two Possible Modes of Rotation of the Omasum, Abomasum, and Cranial Part of the Duodenum in Volvulus.
1, Normal relations; 2, simple dilation and displacement on the right; 3, 180-degree volvulus around the longitudinal axis of the lesser omentum, counterclockwise as seen from the rear; 2′, 90-degree rotation of the abomasum in a sagittal plane, counterclockwise as seen from the right; 3′, 180-degree rotation of the abomasum and omasum around the transverse axis of the lesser omentum, drawing the duodenum cranially, medial to the omasum; 4, 360-degree counterclockwise volvulus, final stage resulting from either mode of rotation. D, Duodenum; E, esophagus; G, greater omentum; L, lesser omentum; O, omasum; P, pylorus; Q, reticulum; R, rumen.
(Modified from Habel RE, Smith DF: J Am Vet Med Assoc 179:447-455, 1981.)
Fifteen percent of abomasal displacements are right sided. The abomasum can be overdistended, displaced dorsally, and rotated on its mesenteric axis, and 20% of these cases develop abomasal volvulus. Right-sided displacements occur in postparturient dairy cows and in calves.
Clinical features of displaced abomasums, whether right sided or left sided, include anorexia, cachexia, dehydration, lack of feces, ketonuria, and a characteristic high-pitched ping subsequent to percussion over the abomasum. Idiopathic abomasal volvulus occurs occasionally in ruminants and calves (see E-Fig. 7-15).
Abomasal Dilation and Tympany
Abomasal dilation and tympany is a syndrome of young cattle that occurs most commonly in dairy breeds with a history of one or more of the following: only a single milk feeding per day, cold milk or milk replacer, lack of free choice water, inconsistency of feeding time, dosing with high-energy oral electrolyte solutions, and sometimes failure of passive transfer of immunity. The pathophysiologic process is presumed to be abomasal fermentation of high-energy ingesta by gas-producing bacteria. Hyperglycemia and a resultant glycosuria are present. Hemorrhage, edema, necrosis, and sometimes emphysema of the abomasum and other compartments of the forestomach are found at necropsy.
Abomasal Emptying Defect
See Disorders of Domestic Animals, Stomach and Abomasum, Impaction.
Braxy (Clostridium septicum)—Inflammatory Diseases
See Disorders of Domestic Animals, Stomach and Abomasum, Inflammatory Diseases.
Intestine
Viral Diseases
Bovine Viral Diarrhea.
Bovine viral diarrhea, also known as mucosal disease, affects cattle of all ages but is most common in animals 8 months to 2 years of age. In this respect, clinical cases are typically younger than animals susceptible to Johne's disease. Animals, including New World camelids, infected in utero or early in life with noncytopathic bovine viral diarrhea pestivirus develop a persistent infection as a result of immunotolerance. They shed virus throughout their lives. Later in life, if exposed to cytopathic pestivirus, they may develop disease. Multifocal, sharply demarcated erosions and ulcers in the tongue, gingiva, palate (see Fig. 7-35), esophagus (Fig. 7-158 ), rumen, abomasum, and coronary bands of the hooves characterize bovine viral diarrhea. In the intestine the characteristic lesion is sharply demarcated foci of necrosis in the epithelium over the GALT (Figs. 7-159 and 7-160 ). Lesions in the stratified squamous epithelium begin in the stratum spinosum. Necrosis of the epithelium is soon followed by the formation of erosions and ulcerations. Villous and crypt enterocytes become necrotic. There is lympholysis in the GALT. Follicular medullary regions of intestinal lymphoid tissue may be filled with cell debris and dead enterocytes. There is commonly a fibrinonecrotic pseudomembrane over the damaged GALT.
Figure 7-158.

Acute Multifocal Ulcers, Esophagus, Cow.
A, Grossly, there are multiple sharply demarcated ulcers (vertically linear red streaks) and similar areas covered by diphtheritic membranes (vertically linear yellow-brown streaks). The cause is the pestivirus of bovine viral diarrhea. B, Microscopically, there is a focus of necrosis (arrows) of cells of the stratum basale and stratum spinosum caused by the pestivirus of bovine viral diarrhea. H&E stain.
(A courtesy Department of Veterinary Biosciences, College of Veterinary Medicine, The Ohio State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia. B courtesy Dr. J.S. Haynes, College of Veterinary Medicine, Iowa State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
Figure 7-159.

Bovine Viral Diarrhea, Ileum, Mucosa, Cow.
Peyer's patches and the overlying epithelium are necrotic (red to dark red elliptical area) and covered with suppurative exudate (yellow-white granular material).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-160.

Multifocal Ulcerative Colitis, Bison, Colon.
Multiple mucosal ulcers were caused by bovine viral diarrhea virus.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Clinical signs may include anorexia, depression, profuse watery diarrhea with staining of the perineum and tail, agalactia, pyrexia, rumen atony, ptyalism, lacrimation, and a mucopurulent nasal discharge. Calves infected in utero may have cerebellar hypoplasia, cataracts, microphthalmia, or renal dysplasia and other congenital defects develop. Abortions, stillbirths, and mummified fetuses can also result from in utero infection in New World camelids, cervids, sheep, goats, and cattle. Aborted calves often have enlarged hemal lymph nodes. Morbidity in a herd varies from 2% to 50%. All affected animals die.
A more common outcome from bovine viral diarrhea infection occurs in immunocompetent animals that are seronegative at the time of exposure to either the cytopathic or noncytopathic virus. Variable signs develop, but they are mostly mild or subclinical. Most cattle in the United States have serologic evidence of exposure to nonvaccine bovine viral diarrhea virus. Exotic ruminants may also become infected. Under certain circumstances pigs may become subclinically infected. This is of interest because the viruses of bovine viral diarrhea and hog cholera are antigenically closely related. This may cause confusing serologic results when testing hogs for cholera. New World camelids may also succumb to bovine viral diarrhea infection, although infections are often subclinical. The diagnosis of persistent infection is by immunohistochemical examination of skin biopsies because calves shed large amounts of virus through the skin. Feedlot cattle that are persistently infected are believed to be more susceptible to mannheimiosis, chronic pneumonia and polyarthritis syndrome, salmonellosis, infectious bovine rhinotracheitis, bovine respiratory syncytial virus, and mycoses. Other diagnostic means are virus isolation, reverse transcription PCR (RT-PCR), and antigen-capture ELISA.
Rinderpest.
Lesions similar to those of bovine viral diarrhea occur in cattle with rinderpest. The morbillivirus associated with rinderpest infects cattle, sheep, goats, pigs, water buffalo, giraffes, wildebeest, and other wild ruminants. Disease spread is via aerosolization and contact with other body secretions. Initial virus replication is in tonsils and pharyngeal and mandibular lymph nodes, resulting in viremia. Acute necrosis is typically severe in all lymph nodes and the epithelial lining of the alimentary, respiratory, and reproductive systems, including erosions and ulcers of the oral cavity and nasal planum. These lesions are particularly severe in regions of GALT, similar to bovine viral diarrhea. Pale eosinophilic, cytoplasmic, and perinuclear inclusion bodies surrounded by a halo are sometimes seen in epithelia and lymphoid tissue macrophages. Intranuclear inclusions are visible less often. The signature lesion is characteristic multinucleate enterocytes in epithelial tissues, including the intestinal lesions that do not occur in bovine viral diarrhea. Postinfection immunity is likely lifelong. Rinderpest does not occur in the United States or Europe but is a significant disease in Africa and Asia and is believed to be on the verge of eradication through effective vaccination. In immunologically naïve populations of animals, morbidity and mortality may be high.
Peste des Petits Ruminants.
Peste des petits ruminants is a distinct morbillivirus disease of sheep and goats that causes ulcerative and pseudomembranous lesions of the oral cavity, similar to rinderpest, along with necrotizing tonsillitis, fibrinohemorrhagic enteritis, and bronchointerstitial pneumonia. Syncytial cells and nuclear and cytoplasmic inclusion bodies of epithelial and lymphoid tissues similar to those found in rinderpest are also present. Peste des petits ruminants is enzootic in the Middle East, the Indian subcontinent, and North Africa.
Border Disease.
The pestivirus causing border disease in sheep and goats is antigenically related to the noncytopathic biotype of bovine viral diarrhea virus. Border disease is usually a congenital infection associated with reproductive failure or birth of abnormal lambs and kids. When subsequently infected with a cytopathic virus, they develop lesions similar to bovine viral diarrhea of cattle. Border disease has been reported in the British Isles, Australia, New Zealand, and the United States.
Malignant Catarrhal Fever.
Malignant catarrhal fever, which is caused by closely related rhadinoviruses (γ-herpesviruses), occurs in a variety of species of ruminants, including cervids and bison. Persistent infection is common in host species, and disease occurs as a result of cross-species transmission. The African form of the disease, caused by alcelaphine herpesvirus 1 is common in wildebeests and other ruminants. In the United States and worldwide, ovine herpesvirus 2 (OvHV-2), caprine herpesvirus 2, and white-tailed deer herpesvirus are most often reported in ruminants. The respiratory form of the disease, associated with keratoconjunctivitis, is most commonly seen in cattle in the United States.
Lesions include widespread lymphadenomegaly, mucosal necrosis, lymphoplasmacytic necrotizing arteritis and phlebitis of the subcutis, and especially in the rete mirabile surrounding the base of the pituitary gland. Hoof walls may be shed. Coagulation necrosis is found in lymph nodes, and lymphoplasmacytic infiltrates are present in the retina, myocardium, brain, spinal cord, and meninges. The alimentary form of the disease is characterized as multifocal ulcerative stomatitis (see Fig. 7-35), glossitis, esophagitis, abomasitis, and enterotyphlocolitis associated with vasculitis. Hemorrhagic cystitis may also be present.
Winter Dysentery.
Winter dysentery is a somewhat enigmatic, acute, generally nonfatal disease of adult cattle. Although its cause is unknown, a coronavirus has been implicated as causative and can sometimes be demonstrated immunohistochemically in colonic basal enterocytes of affected animals. As the disease progresses in a herd, virtually all members become ill. As the name implies, it is a seasonal disease and additionally occurs only in northern latitudes. Catarrhal ileitis and jejunitis characterize this highly contagious disease.
Mild lesions are noted in the rare animal that dies of winter dysentery. The intestinal mucosa is intact, but there is variable congestion and petechiae of the abomasum and small intestine. The intestine may be atonic. The colon may have congestion and hemorrhage of the colonic mucosal folds, a nonspecific lesion associated with tenesmus (tiger striping) (see E-Fig. 7-17).
Acute onset of profuse diarrhea, decreased milk production in dairy cattle, variable depression, and anorexia are characteristic. Malodorous green to black (melena) diarrhea lasts for up to 4 days and may contain fresh blood and mucus. Immunity in dairy herds is protective for years. Older animals are more severely affected than are younger ones. Calves appear to be refractory to disease development. Diagnosis is generally made by epizootic information, clinical signs, its seasonal occurrence, and lack of significant mortality.
Bovine Torovirus Diarrhea.
The shedding of bovine torovirus (BoTV), or Breda virus, has been associated with diarrhea of neonatal veal calves. BoTV is a single-stranded, enveloped RNA virus, which currently cannot be grown in cell culture. BoTV is associated with the presence of other enteropathogens of neonates, including rotavirus, coronavirus, Cryptosporidium, Salmonella, and Giardia. Although it is not uncommon to have intercurrent infections producing diarrhea in calves, especially in the presence of immunosuppression, malnutrition, and other stressors, BoTV may cause disease independently. Necrosis and sloughing of enterocytes on the middle and lower villi, extending into the crypts, are noted on histologic examination. Diagnosis is confirmed by antigen-capture ELISA or RT-PCR in feces in the absence of evidence of other enteric pathogens. Death, when it occurs, is due to dehydration.
Coronavirus Colitis of Beef Calves.
Recently a hemorrhagic and sometimes fatal colitis was reported from postweaning beef calves in Nebraska. A bovine coronavirus (clade 2) was associated with these lesions and was similar to clade 2 coronavirus isolated from the respiratory system of postweaned beef calves with pulmonary disease or without clinical symptoms.
Bacterial Diseases
Clostridium perfringens Type B.
C. perfringens type B is the cause of lamb dysentery. This is generally a disease of very young lambs, although older animals may be affected in prolonged disease outbreaks. Unexpected death is usual, but occasionally there is antecedent anorexia and abdominal pain with or without severe bloody diarrhea. Other young ruminants and foals may also be affected. This disease occurs sporadically in the United States but is more common in Europe, South Africa, and the Middle East.
Clostridium perfringens Type D.
C. perfringens type D affects fattening sheep, goats, and calves. The disease is diet related and associated with grain overload or “overeating disease.” The sudden change in diet promotes growth of organisms in the small intestine. The disease is often characterized by unexpected death, sometimes preceded by CNS signs or “blind staggers.” Endothelial cell damage is produced by a bacterial toxin (angiotoxin). This lesion can result in bilateral symmetric encephalomalacia, which in sheep is similar in its regional distribution to edema disease of pigs (swine cerebral angiopathy) (see Fig. 14-96). Lesions of C. perfringens type D infection are multisystem hemorrhages, particularly of serosal surfaces. Fibrinonecrotic enterocolitis can also occur in association with the β-2 toxin, at least in goats. Pericardial effusion is present along with mild gastroenteritis. The angiotoxin produces “pulpy kidney disease” of sheep (see Fig. 11-42).
Paratuberculosis (Johne's Disease).
Paratuberculosis, or Johne's disease, has been described in numerous ruminant species. Ruminants are infected from feces-contaminated soil. In cattle the disease is characterized by intractable diarrhea, emaciation, and hypoproteinemia in animals older than 19 months. In the average infected herd, 32% to 42% of animals are infected. In small ruminants (sheep and goats), the clinical disease is similar to that observed in cattle except that diarrhea does not occur. The pygmy goat is an exception to the course of disease in small ruminants in that some pygmy goats develop explosive diarrhea and die unexpectedly. In other ruminants the disease has a protracted course and is considered a wasting disease because of the loss of body mass (Fig. 7-161 ). The causative bacterium is Mycobacterium avium subsp. paratuberculosis.
Figure 7-161.

Granulomatous Enteritis, Johne's Disease (Mycobacterium avium subsp. paratuberculosis), Cow.
There is chronic wasting and diarrhea in this 18-month-old heifer. The age at which this cow showed clinical signs is not typical of the disease. Signs usually occur 2 or more years after initial infection.
(Courtesy College of Veterinary Medicine, Cornell University.)
The causative organisms are very resistant to environmental stressors, particularly in regions with acid soils. After ingestion the bacilli are transported through M cells and taken up by macrophages. Lesions in the lamina propria of the intestines, particularly in the ileum, include the accumulation of macrophages. There is little correlation between the severity of the gross lesions and the severity of clinical disease. An age-related immune resistance to infection and disease develops in animals older than 2 months. Fetuses can be infected, but disease is delayed until the animals are much older. Isolation of newborns from fecal contamination is a useful measure to reduce the incidence of infection in a particular herd.
Diagnosis is made by observing clinical signs together with the signalment. The gross lesion in Johne's disease is a chronic, segmental thickening of the ileum, cecum, and proximal colon (Fig. 7-162 ). The ileocecal valve region is usually affected. Affected segments have a variably thickened, rough, rugose mucosa, often with multiple foci of ulceration. There is mesenteric lymphadenopathy.
Figure 7-162.

Granulomatous Enteritis, Johne's Disease (Mycobacterium avium subsp. paratuberculosis).
A, Ileum, sheep. There is notable thickening of the mucosa, which is smooth and shiny (intact) and not ulcerated. B, Small intestine, cow. The lamina propria of the intestine is markedly expanded by granulomatous inflammatory cells (arrows = macrophages), which compress the crypts and eventually result in their loss (atrophy). H&E stain. C, Small intestine, cow. Mycobacterium-containing macrophages distend the lamina propria. Mycobacterium stain red with Ziehl-Neelsen stain.
(A courtesy Dr. M.D. McCracken, College of Veterinary Medicine, University of Tennessee; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia. B and C courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Noncaseating granulomas contain numerous foamy macrophages with large numbers of acid-fast organisms (see Fig. 7-162; also see Figs. 3-25 and 13-82). In contrast, sheep, goats, and deer may have tuberculoid (caseating) granulomas in the intestines, lymphatic vessels, and lymph nodes. These granulomas are sometimes mineralized and contain whorled accumulations of epithelioid macrophages with variable numbers of Langhans-type giant cells. It is more difficult to find acid-fast mycobacteria in these mature granulomas.
M. avium ssp. paratuberculosis can be isolated from feces of affected animals, from diseased intestines and regional lymph nodes, and sometimes from a variety of other tissues and fluids, including the liver, uterus, fetus, milk, urine, and semen. Acid-fast bacteria in rectal mucosal scrapings are found in 60% of the cases. Hepatic microgranulomas occur in approximately 25% of affected animals. Aortic and endocardial mineralization (arteriosclerosis), when it occurs in association with the clinical signs and lesions of paratuberculosis, is specific for Johne's disease in cattle (see Figs. 10-22 and 10-53). The pathogenesis of this vascular lesion is not well understood but is associated with the severe cachexia associated with the disease. The epizootiology of Johne's disease leads many to believe it is one of the most important diseases facing the dairy industry. Speculation has existed for many years that Johne's disease is zoonotic and somehow causative of Crohn's disease in human beings.
Hemorrhagic Bowel Syndrome of Dairy Cattle.
Hemorrhagic bowel syndrome, also known as fatal jejunal hemorrhage syndrome, intraluminal-intramural hemorrhage of the small intestine, and jejunal hematoma, is characterized by intraluminal hemorrhage resulting in blood clots that lead to intestinal obstruction. It is characterized by dark, clotted blood in the feces; variable and multifocal distention of the small intestine; small intestinal ileus; and necrohemorrhagic jejunitis or enteritis (Fig. 7-163 ). This peracute fatal disease of dairy cattle during early lactation is tentatively associated with infections caused by C. perfringens type A and/or Aspergillus fumigatus. The clinical history usually includes a sudden loss of appetite, decreased milk production, abdominal distention, and melena. Usually the history includes a change in feed to a highly digestible, low-fiber ration.
Figure 7-163.

Necrohemorrhagic Enteritis, Hemorrhagic Bowel Syndrome, Small Intestine, Cow.
A, The massive small intestinal hemorrhage and necrosis is characteristic of clostridial infections of the intestine. B, Note the horizontal linear “band” of acute coagulative necrosis affecting the superficial half of the mucosa (light pink zone) of the intestine caused by clostridial toxins. H&E stain.
(A courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee. B courtesy Dr. C.W. Qualls, College of Veterinary Medicine, Oklahoma State University, and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
Chlamydial Diseases
Chlamydiosis.
Bovine chlamydia (Chlamydophila pecorum) has been recovered from spontaneous enteritis of young calves. After experimental inoculation, newborn calves develop fever and diarrhea within 24 hours and become moribund within 4 to 5 days. Grossly the ileum is most severely affected, but the jejunum and large intestine also have lesions. In diseased segments the mucosa is congested and marked with petechiae. The intestinal wall and mesentery are edematous. The lumen contains watery, yellow fluid mixed with a yellow, tenacious, fibrin-rich material attached to the surface. Colonic ridges are hyperemic and have small erosions. Bleeding from petechiae and ecchymoses of the colonic or rectal ridges occurs infrequently. Regional lymph nodes are enlarged. Microscopically, villous epithelial cells, enterochromaffin cells, goblet cells, macrophages, fibroblasts of the lamina propria, and endothelial cells of lacteals are parasitized by the chlamydia. The chlamydia are endocytosed and multiply in epithelial cell apices. They subsequently are liberated into the lamina propria. Villi are enlarged by dilated lacteals and infiltrates of mononuclear cells and neutrophils. Crypts of both small and large intestines are dilated and have sloughed epithelial cells and inflammatory exudate (colitis cystica superficialis). The centers of lymphoid follicles of Peyer's patches are necrotic. The mucosa and submucosa of the intestines are thickened by a diffuse granulomatous reaction. The abomasum also has lesions, and in some calves, foci of inflammation extend transmurally, thereby causing focal peritonitis. Affected calves have diarrhea, fever, anorexia, and depression.
Parasitic Diseases
Haemonchus contortus.
Haemonchus contortus, known as the barber's pole worm, is relatively common in ruminant abomasums. The common name of this parasite is related to the macroscopically visible entwining of the blood-filled intestine and white uterus in the female worm (Fig. 7-164 ). Hyperinfested pastures containing numerous third-stage larvae are the source of infection. Lambs are particularly at risk. Larvae on grasses are ingested by the host and enter the abomasum, where they may lie dormant within the gastric glands. After development to adults, they exit to the abomasal surface and attach via a buccal tooth. Eggs pass in the feces, completing the life cycle. Haemonchus are blood feeders and can cause severe anemia, hypoproteinemia, and resultant edema. This edema is characteristically present in the intermandibular space, resulting in a physical resemblance to a bottle (“bottle jaw”). As with any process resulting in anemia and hypoproteinemia, there are pale mucous membranes, stunting, and diarrhea. Diagnosis is by fecal egg counts and at necropsy by semiquantification of abomasal parasite load along with the attendant lesions of anemia and hypoproteinemia. At necropsy the carcass is pale and has generalized edema and fluid in all body cavities secondary to hypoproteinemia. Abomasal contents are fluid and discolored from free blood. Foci of mucosal hemorrhage are present at sites of worm attachment.
Figure 7-164.

Haemonchus contortus, Abomasum, Sheep.
The white spiral reproductive tract wrapped around the blood-filled intestine is responsible for the striped appearance, hence the common name “barber's pole worm.”
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Ostertagiasis.
In temperate climates, ostertagiasis is considered the most important parasitic disease in cattle (Ostertagia ostertagi) and small ruminants (Ostertagia circumcincta). Affected animals are unthrifty. Ostertagia spp. have a direct life cycle similar to that of Haemonchus spp. The nematodes are smaller than those of Haemonchus and are uniformly brown. Third-, fourth-, and fifth-stage larvae reside in the abomasal gastric glands. Ostertagia spp. are often present along with Trichostrongylus spp. in other GI locations. Intercurrent GI parasitism with other trichostrongyles has an additive effect on the clinical signs. Unthriftiness, lack of proper mentation, diarrhea, hypoproteinemia, and ventral edema may result. The multinodular appearance of the abomasum of heavily infested animals resembles morocco leather (Fig. 7-165 ). This cobblestone appearance is due to enlargement of the gastric glands because of mucous cell hyperplasia and hyperplasia of lymphoid nodules in the abomasal submucosa elevating the overlying mucosa. Abomasitis produced by Ostertagia spp. is characterized by an infiltration of mononuclear inflammatory cells and eosinophils in the lamina propria. There are also increased numbers of globule leukocytes, a decrease in the number of parietal and chief cells, and hyperplasia of abomasal mucous cells. Differential diagnoses include lymphoma.
Figure 7-165.

Ostertagiasis, Abomasum, Cow.
The granular morocco leather appearance of the abomasal mucosa is characteristic of chronic ostertagiasis and is due to epithelial hyperplasia of the gastric glands, which may contain Ostertagia larvae and lymphoid hyperplasia.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Coccidiosis.
Abomasal coccidiosis has been reported in a sheep. Mucosal lesions are nodular and hemorrhagic with hyperplasia of mucous neck cells, parietal cell atrophy, and lymphoplasmacytic fibrosis of the lamina propria associated with giant schizonts of uncertain taxonomy.
Trichostrongylosis.
Trichostrongyles are small nematodes that parasitize the small intestine of ruminants. Mild climates promote clinical disease. These parasites have a direct life cycle. Third-stage larvae are rendered infective in the acid environment of the abomasum. The larvae burrow in between crypt enterocytes but do not generally penetrate the basement membrane. Paradoxically, crypt hyperplasia is followed by villous atrophy. As with most other parasitisms, crowding, poor sanitation, and inadequate nutrition potentiate disease. Protein leakage into the intestinal lumen together with absorptive enterocyte loss leads to diarrhea, cachexia, and its metabolic consequences, which can be severe and widespread through many organ systems.
Nematodirosis.
Nematodirus nematodes are parasites of the cranial small intestine of ruminants. The life cycle is direct. Unlike the case with other strongyles, Nematodirus larvae within ova are resistant to cold temperatures. In fact, the ova must overwinter to be infective. This is evolutionally interesting because it allows for a new crop of susceptible hosts, particularly lambs and calves each year. Fourth- and fifth-stage larvae reside in deeper layers of the mucosa than do the trichostrongyles. Villous atrophy of the cranial small intestine is the predominant histologic lesion. Nematodirus spp. do not generally cause disease except in association with other parasites. Signs include green diarrhea, weight loss, and hypoproteinemia secondary to weight loss and inappetence.
Cooperiasis.
A small intestinal parasite of ruminants, Cooperia nematodes—unlike other trichostrongyles—do not burrow into the intestine. Rather, they reside between villi, causing pressure necrosis. Their life cycle and clinical signs are similar to those of the other strongyles already described.
Oesophagostomum.
The nodular worms of ruminants (Oesophagostomum columbianum, Oesophagostomum radiatum) and pigs (Oesophagostomum dentatum) cause subserosal mineralized nodules that are characteristic of the disease. These nodules generally are of no clinical significance, but they make the intestines unsuitable for use as sausage casings. Occasionally they are associated with, and can be the cause of, intussusceptions.
Third-stage larvae of O. columbianum of sheep are ingested, penetrate deeply into the small intestinal wall, excyst, and molt to fourth-stage larvae, which mature in the colon. They may encyst in the colonic wall and become mineralized subserosal nodules or may mature to adults. Disease is more severe in nutritionally debilitated animals. Most infestations are asymptomatic. O. radiatum of cattle may produce inappetence, hypoproteinemia from damaged enterocyte tight junctions, and anemia and hemorrhage from consumptive coagulopathy induced by the parasites. Nodules may also form, as in sheep. Oesophagostomiasis in pigs is usually asymptomatic, although ill thrift and malaise secondary to typhlocolitis may occur.
Intestinal Neoplasia
Alimentary lymphoma is the most common alimentary neoplasm of ruminants. It has a propensity to develop in the abomasum. See Chapter 6 for more information.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
See Disorders of Domestic Animals, Peritoneum, Omentum, Mesentery, and Peritoneal Cavity.
Disorders of Pigs
For disorders occurring in two or more species of animals, see Disorders of Domestic Animals.
Oral Cavity
See Disorders of Domestic Animals, Oral Cavity.
Viral Diseases
Vesicular Stomatitides.
See Disorders of Domestic Animals, Oral Cavity, Vesicular Stomatitides—Viral Diseases.
Tonsils
Pseudorabies (Aujeszky's Disease)
The virus of Aujeszky's disease, or pseudorabies, initially replicates in the tonsils, which can be sampled to determine viral presence. See Chapter 4 for more information.
Salivary Glands
Tongue
Epithelial hyperplasia of the lateral edges of the tongue is common in piglets before nursing, when the fringelike epithelium is rubbed off (E-Fig. 7-22).
E-Figure 7-22.

Lingual Epithelial Hyperplasia, Tongue, Neonatal Pig.
The lateral surfaces of the tongue are covered by a hyperplastic epithelial fringe. This fringe is normal at birth and will be lost through mechanical trauma to the fringe during nursing.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Esophagus
Stomach
See Disorders of Domestic Animals, Stomach and Abomasum.
In pigs, gastric ulcers are common and occur in penned pigs fed finely ground grain. These ulcers always are limited to the stratified squamous epithelium of the esophageal portion of the gastric mucosa that surrounds the cardia (see Fig. 7-84).
Intestine
Enteric diseases of pigs are a major cause of economic loss. Rapid and accurate on-farm diagnosis is critical in controlling disease outbreaks. If one takes into account the epizootiology of the outbreak, the age of the affected animals, and the location and nature of lesions, one can generally be fairly accurate in rendering an on-farm diagnosis, pending laboratory confirmation. This listing of specific infectious causes of enteritis in pigs is exclusive of those agents already discussed. When formulating a differential diagnosis, one must consider all causes of enteritis, including intestinal displacements, colibacillosis, rotavirus, Salmonella, clostridia, parasites, toxins, and so on.
Viral Diseases
Transmissible Gastroenteritis.
Transmissible gastroenteritis (TGE) is an important disease in pigs younger than 10 days. Older animals apparently can compensate for the small intestinal damage through fluid and short-chain fatty acid absorption in the large intestine. The coronavirus that causes this disease cross-reacts with, but is distinct from, the coronavirus that causes feline infectious peritonitis. The virus is inactivated by sunlight; therefore transmissible gastroenteritis disease occurs mostly in winter. Target cells for the virus are villous enterocytes; therefore lesions consist of notable atrophy of villi of the small intestine (Fig. 7-166 ). In piglets, epithelial replacement time is much longer than in more mature animals, accounting for the high mortality. Diagnosis is by positive immunostaining of intestinal sections in piglets acutely ill with the disease.
Figure 7-166.
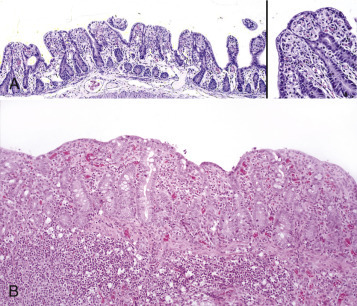
Transmissible Gastroenteritis, Small Intestine, Piglet.
A, Early stage of the disease. Transmissible gastroenteritis virus targets epithelial cells of the tips and upper sides of intestinal villi, causing necrosis of the enterocytes and atrophy of the villi. These cells are sloughed and replaced by flattened epithelial cells migrating up the basement membrane from progenitor cells in the crypts. Inset, Note the flattened epithelial cells covering the tips and sides of the atrophic villi and the fusion of the adjacent villi. Inflammation is minimal. H&E stain. B, Later stage of the disease. There is severe blunting (marked villus atrophy) of intestinal villi with fusion of their basement membranes. Chronic inflammation is prominent in the lamina propria and submucosa. H&E stain.
(A courtesy Dr. B.G. Harmon, College of Veterinary Medicine, The University of Georgia; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Similar to rotavirus or non–transmissible gastroenteritis coronavirus infections, the virus is lytic, and sloughed enterocytes carry virus into the feces. The difference in pathogenicity between rotavirus and non–transmissible gastroenteritis coronavirus infections and transmissible gastroenteritis is the number of villous enterocytes destroyed by a virus. In transmissible gastroenteritis, most of the villous enterocytes are destroyed, and therefore the clinical disease is more severe.
The diarrhea contains odoriferous undigested milk. The loss of the majority of villous enterocytes results in continued significant intestinal malabsorption. Because of fusion of adjacent villi, the enterocyte mass may never fully be restored. Affected surviving animals remain chronic “poor doers.”
Piglets dead from transmissible gastroenteritis are dehydrated, and their perineum is stained with liquid, yellow, fecal material. The small intestine is dilated and thin walled because of the loss of enterocytes and contains yellow fluid and gas (Fig. 7-167 ). Mesenteric lymph vessels are devoid of chyle as a result of malabsorption. The diagnosis is partially based on the presence of villous atrophy. The decrease in villous height to crypt depth ratio is marked and may be appreciated subgrossly (Fig. 7-168 ). Colibacillosis, coccidiosis, cryptosporidiosis, rotavirus infection, and non–transmissible gastroenteritis coronavirus infection are among the differential diagnoses.
Figure 7-167.
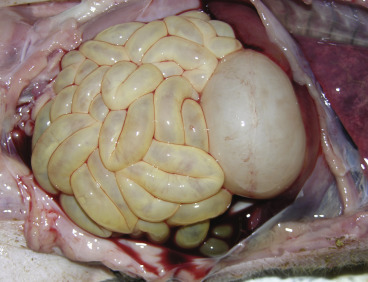
Transmissible Gastroenteritis, Small Intestine, Piglet.
The small intestine is dilated by gas, is thin walled, and contains undigested milk.
(Courtesy Dr. V. Hsiao, College of Veterinary Medicine, University of Illinois.)
Figure 7-168.

Wet Mount, Intestinal Villi, Transmissible Gastroenteritis, Small Intestine, Piglet.
There is notable villous atrophy (bottom) compared with normal intestine (top).
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Piglets suffer from acute diarrhea, weight loss, vomiting, and dehydration. Morbidity and mortality, especially in neonates, approach 100% in susceptible herds. Death occurs within 48 hours to 5 days after the commencement of clinical signs. In feeder pigs, transmissible gastroenteritis virus infection causes transient clinical signs with eventual recovery. Sows are susceptible to the virus, and morbidity among the sows is 100%, but the clinical signs are mild and transient (fever, vomiting, inappetence, and agalactia), and none die. Immunity is solid.
Porcine Epidemic Diarrhea.
Porcine epidemic diarrhea virus (PEDV) was first recognized in China in 2010 and rapidly spread worldwide, including at least 10 states in the Unites States in 2013. Porcine epidemic diarrhea virus is a coronavirus similar to the virus that causes transmissible gastroenteritis. Morbidity in naïve herds is 100%, and mortality among suckling and recently weaned piglets ranges from 50% to 100%. Transmission among pigs is rapid (36 hours) and by a variety of methods, including fecal-oral, fomites, and wind borne. Clinical signs are vomiting, inappetence, and watery, fetid diarrhea in all age pigs. Typical lesions are small intestinal atrophy with occasional epithelial syncytia. Severity of disease is variable and dependent on age with older animals having low mortality.
Porcine Circovirus Enteritis.
Porcine circovirus (PCV) is ubiquitous in pigs worldwide. The small, single-stranded, nonenveloped, DNA genome of the virus is circular. Although PCV type 1 has been recognized as a nonpathogenic laboratory culture contaminant since 1982, in 1998 pathogenic variants emerged in commercial pigs and were designated PCV2 a and b. They were associated with a clinical syndrome termed postweaning multisystemic wasting syndrome. Porcine circovirus–associated disease (PCVAD) refers to the different disease manifestations associated with PCV2 infection, including enteritis. Seropositivity for PCV2 is ubiquitous and does not equate with clinical disease.
In confirmed clinical cases of porcine circovirus–associated disease, histologic lesions of lymphoid depletion and/or lymphohistiocytic to granulomatous inflammation must be present in affected organs and PCV2 must be identified within lesions by PCR or immunohistochemistry (IHC). The organs affected and the clinical signs vary greatly and are exacerbated by intercurrent infections by a variety of infectious agents.
Lesions in the intestine include depletion of germinal centers in GALT with replacement by histiocytes and multinucleated giant cells. Macrophages in Peyer's patches may contain botryoid, basophilic, intracytoplasmic inclusion bodies. Lymphohistiocytic to granulomatous inflammation may extend from GALT to the intestinal lumen of both the large and small intestines. In some cases the lesions are similar to those of Lawsonia infection. Virus is spread horizontally within a herd by all body secretions.
Bacterial Diseases
Edema Disease.
Edema disease, also known as enterotoxemic colibacillosis, is an E. coli (F18ab) infection that is specific for pigs. Edema disease is caused by a bacterial enterotoxin (verotoxin) produced in the small intestine and spread hematogenously via induction of IL-8. This interleukin attracts neutrophils that carry the toxin throughout the body. It is generally a disease of pigs 6 to 14 weeks of age and is usually associated with dietary changes at weaning. It is often noted that the best pigs in a group are the ones affected. Edema disease is characterized by neurologic signs, including incoordination, poor balance, weakness, tremors, and convulsions.
Hemolytic E. coli proliferates in the small intestine subsequent to dietary changes and produces a heat-labile exotoxin called the edema disease principle. This systemic toxin (angiotoxin) causes generalized vascular endothelial injury of arterioles and arteries (see Fig. 10-69), resulting in fluid loss and edema. The edema can be found anywhere but is most characteristic in the gastric submucosa (see Fig. 10-79), eyelids (Fig. 7-169 ), forehead, gallbladder, and mesentery of the spiral colon (Fig. 7-170 ). In the brain, arterial damage causes focal malacia in the medulla, thalamus, and basal ganglia. These nervous tissue lesions are collectively known as focal symmetric encephalomalacia or swine cerebral angiopathy and are responsible for the variety of clinical signs. Death is due to an endotoxic shocklike syndrome. Some animals suffer from a Shwartzman-like bilateral renal cortical necrosis. Morbidity within a herd is approximately 35%, and all affected animals die.
Figure 7-169.

Edema Disease, Head, Pig.
The skin of the eyelids, snout, and submandibular area are edematous as a result of production of angiotoxin by Escherichia coli, which increases the permeability of capillaries.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-170.

Edema Disease, Spiral Colon, Pig.
Edema of the mesentery is a result of an angiotoxin produced by Escherichia coli.
(Courtesy Drs. W. Hascheck-Hock and L. Borst, College of Veterinary Medicine, University of Illinois.)
Postweaning Colibacillosis.
Postweaning colibacillosis is another specific disease of pigs caused by a hemolytic E. coli. The disease appears identical to enterotoxic colibacillosis of the neonate in that it produces a secretory diarrhea and therefore no lesions in the intestine, although gastric infarcts are common. It is a distinct strain of E. coli, however, and is associated with feed and management changes at weaning.
Swine Dysentery.
Unlike most of the other diseases of the porcine gut, swine dysentery is generally confined to the large intestine. The causative bacterium, Brachyspira hyodysenteriae, previously known as Treponema and Serpulina, is a Gram-negative, flagellated, and anaerobic spirochete that acts synergistically with anaerobic colonic flora, such as F. necrophorum or Bacteroides vulgatus, to produce disease. This synergism is believed to be partially responsible for the age restriction (8 to 14 weeks old) of the disease because neonatal animals have not yet developed the appropriate anaerobic gut flora. B. hyodysenteriae produces a cytotoxic hemolysin, which is a virulence determinant.
The gross lesions of the disease closely approximate those of acute enteric salmonellosis except that bloody feces are more usual in dysentery. Weanling pigs 8 to 14 weeks old are usually affected, and the disease spreads rapidly through a herd. Morbidity approaches 90%, and mortality is around 30%. Lesions of mucohemorrhagic enteritis are present in the spiral colon, colon, cecum, and rectum. The intestine often has a fibrinonecrotic pseudomembrane that correlates with the severe diarrheic feces that contains blood, mucus, and fibrin (Fig. 7-171 ). The diarrhea and electrolyte loss that occur are caused by colonic absorptive failure.
Figure 7-171.

Necrohemorrhagic Enterocolitis, Swine Dysentery, Spiral Colon, Pig.
There is marked necrosis and hemorrhage of the intestinal mucosa caused by the bacterium Brachyspira hyodysenteriae.
(Courtesy Department of Veterinary Biosciences, College of Veterinary Medicine, The Ohio State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
B. hyodysenteriae is identified by impression smear (Fig. 7-172 ), dark-field microscopy, immunolabeling techniques, and PCR. It is assumed that a carrier state exists because the disease is enzootic in affected herds.
Figure 7-172.

Swine Dysentery, Colon, Pig.
This impression smear contains a few enterocytes and numerous bacteria. Note the spiral bacteria (arrows) consistent with Brachyspira spp. Diff-Quik stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Lawsonia Enteritis.
Lawsonia enteritis manifests in a variety of ways, as indicated by the number of names applied to it: proliferative enteropathy, proliferative ileitis, intestinal adenomatosis, distal ileal hypertrophy, terminal ileitis, and proliferative hemorrhagic enteropathy. The genus of the causative agent has undergone several recent changes in nomenclature. For many years this disease was believed to be caused by Campylobacter spp. (Campylobacter mucosalis, C. jejuni, Campylobacter hyointestinalis). Newer methods of bacterial classification caused the name to be changed to Ileobacter and now L. intracellularis, the only species in the genus. Pigs older than 4 weeks of age are susceptible; thus this condition is a postweaning disease. Disease is believed to be caused by an unknown interaction of Lawsonia with normal gut flora. The nature of the lesions is a function of the extent of intestinal mucosal necrosis. The disease begins as a bacteria-induced stimulation of small intestinal crypt epithelial cells, particularly in the ileum (Figs. 7-173 and 7-174 ), where lesions are generally most severe. With time the lesions progress to necrosis of the proliferating crypt cells with hemorrhage (Fig. 7-175 ). Thus the morphologic appearance of the lesions varies from case to case. The mechanism of lesion production is not well understood. Infection results in immunosuppression with a reduction in CD8+ T and B lymphocytes. In the proliferative form of the disease, the causative bacteria may be seen in apical cytoplasm of enterocytes. The mechanism of enterocyte proliferation may relate to Lawsonia-induced altered transcription of host “alarm response” genes that affect regulation of the cell cycle and cell differentiation. The enterocyte hyperplasia that results may cause release of cytokines that attract macrophages. With severe disease, bacteria are present in macrophages in the lamina propria. This may cause release of tumor necrosis factor-α (TNF-α), resulting in vascular permeability and hemorrhage.
Figure 7-173.

Proliferative Enteritis, Ileum, Pig.
Note the marked mucosal expansion, the result of Lawsonia-induced epithelial hyperplasia.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Figure 7-174.

Lawsonia Enteritis, Ileum, Pig.
There is notable hyperplasia of enterocytes, resulting in distortion of normal architecture and “collision necrosis” of tightly packed proliferating enterocytes. Also see Figure 7-173. H&E stain.
(Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Figure 7-175.

Lawsonia Enteritis, Ileum, Pig.
A, Hemorrhagic bowel form. Note the prominent folds of hyperplastic mucosa and the concurrent hemorrhage forming a luminal cast. B, Necroproliferative form. Note the prominent necrosis of the ileal mucosa and its diphtheritic membrane (luminal cast) formed by cellular debris and inflammatory exudate.
(A courtesy Dr. D.D. Harrington, School of Veterinary Medicine, Purdue University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia. B courtesy Dr. D. Driemeier, Federal University of Rio Grande do Sul, Brazil.)
At clinical and necropsy examination, variable amounts of blood and intestinal casts are present in the feces. Microscopically, the comma-shaped bacteria are made visible with special stains, such as Steiner's, within the mitotically active cells of the small intestinal crypts (Fig. 7-176 ). The massive mitoses of crypt cells and resultant cryptal crowding and necrosis prevent maturation to absorbent villous enterocytes. There is resultant villous shortening. Mitosis can be so intense that the histologic features suggest neoplasia and a diagnosis of “intestinal adenomatosis.”
Figure 7-176.

Proliferative Enteritis, Ileum, Pig.
Curved Lawsonia spp. bacteria (arrow) are present in the apical cytoplasm of enterocytes. There is proliferation of crypt enterocytes. Warthin-Starry stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Morbidity within a herd is 10% to 15%; mortality is around 50%. In fatal cases, affected pigs usually die within a day of the appearance of clinical signs. Pigs that recover are generally “poor-doers.” A similar organism with associated intestinal proliferation is found in horses, hamsters, ostriches, cervids, sheep, ferrets, rats, and macaques.
Chlamydial Diseases
Chlamydiosis.
Chlamydia has been found in enterocytes of normal pigs and pigs with diarrhea. In gnotobiotic pigs, Chlamydia trachomatis and Chlamydia suis infection result in villous atrophy and villous-tip necrosis. These lesions are most severe in the distal jejunum and ileum. Colonic infection has also been reported.
Parasitic Diseases
Balantidiasis (Balantidium coli).
Balantidium coli is a normal inhabitant of the cecum and colon of primates, including human beings, and pigs. It is large (50 to 60 µm × 25 to 45 µm) and ciliated. Dogs with whipworm infestation may become infested after contact with infected pigs. In general, Balantidium is an opportunistic pathogen associated with enteric disease (Fig. 7-177 ).
Figure 7-177.

Balantidium coli, Colon, Pig.
B. coli is an opportunistic flagellated protozoan that is normally present in the pig intestine (arrows). This pig had concurrent proliferative (Lawsonia) enteritis. H&E stain. Inset, Higher magnification of B. coli. H&E stain.
(Courtesy Dr. C. Löhr, College of Veterinary Medicine, Oregon State University. Insert, Courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
Hyostrongylus rubidus.
Hyostrongylus rubidus of pigs is a gastric parasite that causes a thickening of the mucosa, with mucus accumulation and mucous cell hyperplasia and inflammation of the lamina propria by lymphocytes, plasma cells, and eosinophils. The parasite is threadlike and red. Clinically, hyostrongylosis is associated with the “thin sow syndrome.” Grossly, the gastric mucosa is thickened, catarrhal, and somewhat cobblestone, similar to ostertagiasis of ruminants. Microscopically, there is mucous metaplasia of parasitized and adjacent gastric glands. Submucosal lymphoid follicles develop in chronic infections.
Oesophagostomum.
See Disorders of Ruminants (Cattle, Sheep, and Goats), Intestine, Parasitic Diseases, Oesophagostomum.
Miscellaneous Disorders
Intestinal Emphysema.
Intestinal emphysema (pneumatosis cystoides intestinalis) of pigs and rabbits translates to gas-dilated lymphatic vessels of the intestinal serosa and mesentery. The cause of this condition is unknown, and it is not associated with clinical disease (Fig. 7-178 ).
Figure 7-178.

Intestinal Emphysema, Intestines, Pig.
Gas bubbles dilate serosal and mesenteric lymphatic vessels.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Intestinal Neoplasia
See Disorders of Domestic Animals, Intestine, Intestinal Neoplasia.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
Glasser's Disease
Glasser's disease is characterized by fibrinous polyserositis (pleuritis, pericarditis, peritonitis, arthritis, and leptomeningitis). Although not generally a diarrheal disease, it causes inflammation of the intestinal serosa (serositis). Lesions range from arthritis to peritonitis to leptomeningitis, depending on the serous surface infected. Glasser's disease generally occurs in 5- to 12-week-old pigs. Mortality of affected animals within a herd is high, but morbidity is low. Although classic Glasser's disease is caused by either Haemophilus suis or Haemophilus parasuis, porcine polyserositis can be caused by Mycoplasma hyorhinis, Streptococcus suis type II (zoonotic), septicemic salmonellosis, and septicemic E. coli (see Fig. 7-17).
Disorders of Dogs
For disorders occurring in two or more species of animals, see Disorders of Domestic Animals.
Oral Cavity
See Disorders of Domestic Animals, Oral Cavity.
Eosinophilic Stomatitides
See Disorders of Domestic Animals, Oral Cavity, Eosinophilic Stomatitides.
Teeth
Tonsils
Salivary Glands
Tongue
Esophagus
Achalasia
See Disorders of Domestic Animals, Esophagus, Developmental Anomalies, Achalasia.
Stomach
Parasitic Diseases
Several genera of nematodes, principally Ollulanus, Gnathostoma, and Cylicospirura, cause gastritis in dogs and cats, but these infections are rare. Physaloptera spp. are often thought of as gastric parasites of carnivores because they are sometimes found in the stomach on endoscopic examination or at necropsy. They are occasionally responsible for vomiting. They appear similar to ascarids but generally attach by anterior hooks to the proximal duodenal mucosa at the gastric valve (Fig. 7-179 ). Intermediate hosts are coprophagous beetles.
Figure 7-179.

Physalopteriasis, Stomach, Dog.
Stout coiled nematodes, Physaloptera canis are firmly attached to the gastric mucosa by dentate pseudolabia.
(Courtesy Dr. M.D. McGavin, College of Veterinary Medicine, University of Tennessee.)
Intestine
Lymphangiectasia
Lymphangiectasia, or lacteal dilation, is the most commonly reported cause of protein-losing enteropathy in dogs. Clinical signs include diarrhea, steatorrhea, hypoproteinemia, and ascites (see Fig. 7-13). Lymphangiectasia can be due to a congenital developmental disorder of the lymphatic vessels, or it can be acquired secondary to lymph vessel obstruction caused by granulomatous or neoplastic diseases. An inherited cause is suspected in some canine breeds. A special case is lipogranulomatous lymphangiectasia of the dog, the name of which is descriptive of the lesions present. Most cases of acquired lymphangiectasia are idiopathic. Gross and microscopic lesions are those of lymphangiectasia and include a thickened intestinal mucosa with dilated lymphatic vessels and lacteals (see Fig. 7-14). There are variable increases in lymphocyte and plasma cell numbers in affected tissue.
Viral Diseases
Parvovirus Enteritis.
Also see Disorders of Cats, Intestine, Viral Diseases, Parvovirus Enteritis.
Parvovirus enteritis of dogs (and cats) is a severe, usually fatal disease. Because the target cells are those that are rapidly dividing, in the intestine the crypt cells are principally affected. This tropism is called radiomimetic. Initial virus replication occurs in lymphoid tissue. Although there is much overlap in the disease syndrome in dogs and cats, the dissimilarities warrant independent discussion of each species. To complicate matters further, there is a high mutation rate among canine and feline parvoviruses, and genetic recombination between the two viruses has been documented.
Canine parvovirus enteritis first appeared in Europe and the United States in 1978. The disease was initially recognized because the gross and microscopic lesions were identical to those of feline parvovirus enteritis. Panleukopenia vaccines were effective in preventing this disease in dogs and were used extensively until canine-specific parvovirus vaccines were developed. Rottweilers and Doberman pinschers, which are genetically related, are at increased risk for parvovirus disease even if properly vaccinated.
Canine parvovirus disease initially was described as occurring in three distinct syndromes. Puppies younger than 2 weeks of age had generalized disease with focal areas of virus-induced necrosis in those tissues with rapidly dividing cells. Thus multiple organs and tissues, such as the liver, kidney, heart, vessels, bone marrow, intestine, and lung, were affected. Puppies 3 to 8 weeks of age would sometimes have myocarditis develop for the same reason. Often, initial infection would go undetected, and these animals would die unexpectedly up to 5 months later because of myocardial scarring and conduction failure (see Fig. 10-81). In puppies 8 weeks or older, the disease is identical to that in the cat. Congenital cerebellar hypoplasia has not been induced in puppies.
At necropsy the dilated, fluid-filled, flaccid, and hemorrhagic small intestine with serositis similar to that of panleukopenia is quite characteristic (Fig. 7-180 ). The contents of the small intestine are brown to red-brown and fluid with a fibrinous exudate, with or without hemorrhage (also see Fig. 7-185, B). Mesenteric lymphadenomegaly with variable hemorrhage is present. The bone marrow is depleted. Dogs but not cats may have coagulative lymphadenitis associated with severe lymphoid infection.
Figure 7-180.

Parvovirus Enteritis, Small Intestine, Dog.
A, Segments of the small intestine are diffusely reddened (active hyperemia of the mucosa), and the serosal surface is roughened, faintly granular, and petechiated. B, The mucosa of the small intestine is necrotic. Note the roughened, granular, focally petechiated, and focally sloughing mucosa.
(A courtesy College of Veterinary Medicine, University of Illinois. B courtesy Department of Veterinary Biosciences, College of Veterinary Medicine, The Ohio State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia.)
Figure 7-185.

Panleukopenia Virus Enteritis, Small Intestine, Cat.
A, Villi are denuded of epithelium and are atrophic. Note that because of the loss of epithelial cells in the crypts, they have collapsed, obliterating their lumens. Some crypts are dilated. H&E stain. B, Higher magnification of crypts. Note the sloughed necrotic epithelial cells in the crypt lumens and the lining of the crypts by squamoid epithelial cells and hyperplastic cells (some with intranuclear inclusion bodies) (arrow), all indicative of attempts at epithelial repair and regeneration. Chronic inflammatory cells are present in the lamina propria. H&E stain.
(A and B courtesy Dr. J.F. Zachary, College of Veterinary Medicine, University of Illinois.)
The intestinal lesion is necrosis of crypt epithelial cells. Surviving epithelial cells are not targets of the virus, but their morphologic configuration changes to squamoid to cover the surface of the denuded crypts and later to temporarily cover the denuded villous basement membrane, because replacement cells are not being produced, even though senile epithelial extrusion continues to occur from the villous tips. Severe lesions consist of partially denuded villi over debris-filled crypts, some of which lack an epithelial lining. Because the villous basement membrane is exposed during the continuing extrusion process, villous fusion occurs, resulting in lack of a scaffold for enterocyte replacement once the crypts recover. This results in permanent villous distortion and atrophy. Entrapped, hyperplastic crypt epithelium may therefore be present. Inclusion bodies are not present in lymphoid tissue. In bone marrow, erythropoiesis is normal, but granulopoiesis is reduced. Necrotizing colitis may occur but is much less important than the small intestinal lesions. Dogs with hemorrhagic parvovirus enteritis have bloody diarrhea and die from shock within 24 hours. Secondary bacterial infections with endotoxemia are believed to be associated with this syndrome.
Circovirus.
Canine circovirus (dog CV) is associated with vomiting, hematochezia, hemorrhagic gastroenteritis, necrotizing vasculitis, and granulomatous lymphadenitis. Histologic lesions in pigs infected with porcine circovirus include viral inclusion bodies in macrophages and multinucleated giant cells, features not reported in dogs. Virus has been isolated from outbreaks of canine diarrhea, from heathy dogs, from dogs with a variety of other problems such as thrombocytopenia or neutropenia fever of unknown origin, and from some animals with tick bites. The virus is nonenveloped and round with a core of single-stranded, circular DNA. It is speculated that intercurrent pathogens potentiate disease in dog CV infections.
Minute Virus of Dogs.
Canine parvovirus type 1 produces myocarditis and respiratory disease in young pups. The virus is widely distributed in the canine population, but disease is only diagnosed sporadically. The virus is spread via the oronasal route. Fetal death and embryo absorption occur between 25 and 35 days of gestation. Microscopically, intestinal lesions consist of enterocyte hyperplasia with eosinophilic or amphophilic intranuclear inclusion bodies in the enterocytes of the villous tips of the duodenum and jejunum. Crypt necrosis characteristic of canine parvovirus type 2 infection is not present.
Bacterial Diseases
Clostridial Enteritis
Peracute Hemorrhagic Gastroenteritis of Dogs.
The cause of peracute hemorrhagic gastroenteritis of dogs, also known as canine hemorrhagic gastroenteritis, is undiscovered but is considered likely a result of infection with C. perfringens of unknown type. The disease most often occurs in dogs of toy and miniature breeds younger than 2 years. Blood is observed at the anus before death. As the name of the disease denotes, there is hemorrhagic necrosis of the GI mucosa anywhere from the stomach caudally. Numerous clostridial organisms are present in the intestinal debris but are not attached to intact mucosa. Unlike parvoviral enteritis, in which crypts are preferentially destroyed, the crypts are spared in peracute hemorrhagic gastroenteritis.
Histiocytic Ulcerative Colitis.
Because of its occurrence in boxer dogs and the genetically related French bulldog, histiocytic ulcerative colitis has been called boxer colitis. Granulomatous colitis is another term for this disease, although true granulomas are not present. It generally occurs in dogs younger than 2 years. Dogs can have soft feces, but often no diarrhea or weight loss is observed. In some cases mucus and blood appear in the stool. The lesions, which are visible by proctoscopy, are raised ulcerative nodules (Fig. 7-181 ). Microscopically, the colon is ulcerated and has marked infiltration by macrophages containing PAS-positive material.
Figure 7-181.

Histiocytic Ulcerative Colitis, Colon, Boxer Dog.
There are numerous round and coalescing ulcers in the colon in this case of “boxer colitis.” Research suggests Escherichia coli as the causative agent of boxer colitis.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Large macrophages with abundant foamy eosinophilic cytoplasm are present in the colonic lamina propria and submucosa early in the disease process. There may be lesser numbers of smaller, mononuclear inflammatory cells, principally lymphocytes and plasmacytes. The PAS-positive material in macrophages has been visualized by tissue Gram stains, electron microscopy, and immunohistochemistry. They likely contain bacteria and the phagolysosomal remnants of digested cells. Evidence suggests that the bacteria are probably E. coli. The massive numbers of engorged macrophages within the lamina propria results in a space-occupying lesion that affects the overlying enterocytes. Enterocyte necrosis results in colonic erosion and ulceration. There is lymphadenopathy, both regional and generalized, characterized by an influx of foamy macrophages in the lymphatic sinuses.
Citrobacter freundii Enteritis.
Bacteremia and septicemia associated with Citrobacter freundii have been reported to cause mucohemorrhagic diarrhea in dogs with hemorrhagic lesions in the small intestine and colon. It is believed to be a condition of puppies and immunocompromised dogs. Being bacteremic and/or septicemic, many organs and tissues are affected besides the gut. The condition is more common in human beings as a nosocomial infection with a high mortality rate. In human beings the route of infection is through the urinary tract, gallbladder, GI tract, or cutaneous wounds. Citrobacter infections should be considered potentially zoonotic.
Fungal Diseases
Canine Histoplasmosis.
Canine histoplasmosis occurs most often in the Ohio and Mississippi river valleys. This zoonotic systemic fungus can infect the intestine, but pneumonia is more common. Thus the route of infection is inhalation or ingestion. The reservoir is believed to be soil and bird feces. The yeast invades tissue, causes necrosis, and replicates in macrophages. Granulomatous lesions may be present in pulmonary, intestinal, lymphoid, hepatic, and other tissue. At necropsy or biopsy the intestine has a thickened and corrugated mucosa with ulceration. There is hepatomegaly and mesenteric lymphadenopathy and lymphadenomegaly. Scattered pulmonary granulomas may be present.
In the affected ileum and colon the lamina propria is widened by macrophages that contain H. capsulatum (Fig. 7-182 ). With time, infection may extend transmurally through the intestine and to the lymphoid system. There is hyperplasia of regional lymph nodes, and lymphoid sinuses contain numerous macrophages (see Figs. 13-59, 13-91, and 13-92Fig. 13-59Fig. 13-91Fig. 13-92). Multifocal granulomas with intracellular fungi are in the liver, presumably arriving via the portal vein (see Fig. 8-56).
Figure 7-182.
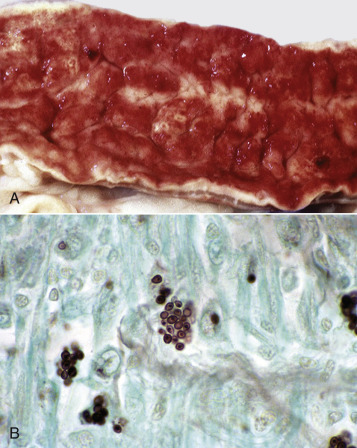
Histoplasmosis, Granulomatous Enteritis, Intestine, Dog.
A, The mucosa is congested and greatly thickened from granulomatous inflammation that has expanded the lamina propria. B, Clusters of 3- to 5-µm Histoplasma capsulatum organisms (stained black) with a central nucleoid are in macrophages. Grocott-Gomori's methenamine silver stain.
(A courtesy Dr. R. Panciera, School of Veterinary Medicine, Oklahoma State University; and Noah's Arkive, College of Veterinary Medicine, The University of Georgia. B courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Signs of intestinal histoplasmosis in the dog include intractable chronic diarrhea with anorexia and its attendant weight loss, lethargy, poor pelage, and anemia. Respiratory signs and peripheral lymphadenitis may be present.
Rickettsial Diseases
Salmon Poisoning.
Salmon poisoning is an acute and fatal hemorrhagic granulomatous enterocolitis of the dog and fox that results from consuming salmon carrying the fluke Nanophyetus salmincola. When this trematode harbors Neorickettsia helminthoeca, a 0.3-µm coccoid rickettsia, disease may result. Lesions may extend from the pylorus to the anus. The enteric lesions consist of hemorrhage at sites of GALT necrosis, especially near the ileocecal valves. In the small intestine, trematodes may be embedded in the mucosa. Diagnosis is confirmed by visualizing macrophages in many tissues, including the lymph nodes, lamina propria, and brain, containing Giemsa- or Gram-stained elementary bodies (E-Fig. 7-23).
E-Figure 7-23.

Salmon Poisoning, Mesenteric Lymph Node, Dog.
This acute and fatal disease of the dog and fox results from consuming salmonid fish carrying the fluke Nanophyetus salmincola. When this trematode harbors Neorickettsia helminthoeca, a 0.3-mm coccoid rickettsia, disease may result. Numerous elementary bodies (arrow) are present in phagocytic cells of this Gram-stained section of lymph node.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Six to eight days after eating parasitized fish, affected dogs become febrile and depressed. There is an oculonasal discharge, severe diarrhea, emesis, anorexia, and splenolymphadenopathy characterized by enlarged tonsils, spleen, and lymph nodes. The mesenteric lymph nodes are often more severely affected than peripheral nodes. Unless treated, affected animals die within 10 days.
Parasitic Diseases
Canine Multifocal Eosinophilic Gastroenteritis.
Canine multifocal eosinophilic gastroenteritis is an uncommon disease of dogs generally younger than 4 years. It is caused by migrating larvae of T. canis. Therefore this disease occurs in association with poor parasite management.
Larvae of T. canis are ingested, invade the mucosa of the stomach and small intestine, and then become trapped and localized in their self-induced inflammation. Dormant larvae migrate into the uterus and fetuses during late pregnancy. Postpartum, larvae are secreted in the milk of the bitch or ingested from environmental feces. Ingested larvae penetrate the gastric and small intestinal mucosa, enter lymph vessels or the portal vein, and travel to the liver and lungs. They then develop into third-stage larvae and are coughed up and swallowed. In the GI tract they mature to adult ascarids. In the majority of puppies, ascarid larvae complete their life cycle in several weeks. Alternatively, the larvae are enveloped in granulomas that kill the parasite secondary to immune reactivity. These granulomas may occur anywhere along the parasite's migration tracts, including most abdominal organs, eyes, brain, and the lungs. Eosinophils are a prominent component of the inflammatory reaction and are attracted to the site of parasite entrapment by the waste products of the larvae. There may be subsequent mineralization of larvae, or they may remain viable for up to 4 years. This condition is especially common in aberrant host species and is called visceral larval migrans. It is an environmental danger where children play in sand or dirt contaminated by feces of infected animals. The ova are relatively resistant to environmental extremes.
Lesions are microscopic to macroscopic and may be quite numerous. As in other inflammatory diseases, there may be regional lymphadenopathy with or without nodules that vary from principally granulomatous to eosinophilic or a mix of the two. Larvae, when present, are surrounded by an eosinophilic, amorphous, fringed material that stains PAS positive (the Splendore-Hoeppli phenomenon).
In general, canine multifocal eosinophilic gastroenteritis is asymptomatic. However, chronic diarrhea, moderate weight loss, intermittent or persistent eosinophilia, and elevated serum γ-globulin concentrations may characterize this disorder. Serum albumin concentration and results of absorption tests and small bowel contrast radiographs usually are normal.
Immunologic Disorders
Inflammatory Bowel Disease.
In dogs and cats inflammatory bowel disease is microscopically a lymphoplasmacytic enteritis. Diagnosis is made by biopsy. Breeds with a predilection for this disease include the basenji and the German shepherd. The cause is unknown, but the presence of numerous lymphocytes and plasma cells suggests an immunologic problem. Malabsorption and chronic protein-losing enteropathy can result from the marked infiltrate of lymphocytes and plasmacytes in the lamina propria. In dogs there are increased numbers of both B and T lymphocytes in the lamina propria of the small intestine (Fig. 7-183 ). In cats, but not dogs, dietary antigens cause some cases of inflammatory bowel disease; therefore control of the disease can be achieved by regulation of the diet. Anecdotal evidence suggests that lymphocytic plasmacytic enteritis in the cat can be a prelude to intestinal lymphoma.
Figure 7-183.

Lymphoplasmacytic Enteropathy, Intestine, Dog.
The lamina propria is widened with lymphocytes and plasma cells. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Diffuse Eosinophilic Gastroenteritis.
Although diffuse eosinophilic gastroenteritis has a predilection for the German shepherd breed, it occurs in other breeds of dogs and in cats. It is characterized by recurrent episodes of diarrhea associated with tissue and circulating eosinophilia. The increased concentration of eosinophils in the circulation and within lesions suggests a hypersensitivity reaction to some ingested substance or to parasites. The cause has not been identified. There are no gross lesions. Eosinophils, along with lymphocytes and plasma cells, heavily infiltrate all layers of the mucosa of the stomach and intestine (Fig. 7-184 ).
Figure 7-184.

Diffuse Eosinophilic Enteritis, Small Intestine, Dog.
Numerous eosinophils are present in the deep lamina propria and the mucosal-submucosal interface (bottom quarter of image). The cause of this hypersensitivity reaction is not known. H&E stain.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Wheat-Sensitive Enteropathy of Irish Setters.
Wheat-sensitive enteropathy, a hereditable condition similar to gluten-sensitive enteropathy of human beings, is the first described dietary-induced enteropathy of dogs. It is characterized initially by increased numbers of intraepithelial lymphocytes and goblet cells and later by partial villous atrophy, particularly of the jejunum. Dietary therapy is palliative.
Idiopathic Disorders
Canine Senile Gastrointestinal Amyloidosis.
Amyloid located in and around vessels of the submucosal and muscular layers of the alimentary tract and within the mesentery has been reported in dogs. The mechanism and chemical nature of the amyloid deposition have not been determined. Dysfunction of the alimentary tract has not been reported to occur with canine senile GI amyloidosis.
Parasitic Enteritides
See Disorders of Domestic Animals, Intestine, Diseases Caused by Specific Pathogens, Parasitic Diseases.
Intestinal Neoplasia
See Disorders of Domestic Animals, Intestine, Intestinal Neoplasia.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
See Disorders of Domestic Animals, Peritoneum, Omentum, Mesentery, and Peritoneal Cavity.
Sclerosing Encapsulating Peritonitis
Sclerosing encapsulating peritonitis is uncommon in dogs and rare in cats. Serous surfaces of the abdominal cavity are covered with granulation tissue and/or fibrous tissue, often encapsulating and sometimes distorting viscera. Multiple adhesions are present. In clinical patients it is sometimes possible to palpate the affected organs. Affected animals vomit, experience abdominal pain, and have ascites. The abdominal fluid contains variable numbers of erythrocytes, macrophages, mixed inflammatory cells, reactive mesothelial cells, and fibroblasts. The etiology in those cases that are not idiopathic includes steatitis, foreign bodies, and chronic bacterial infections.
Disorders of Cats
For disorders occurring in two or more species of animals, see Disorders of Domestic Animals.
Oral Cavity
Eosinophilic Stomatitides
See Disorders of Domestic Animals, Oral Cavity, Eosinophilic Stomatitides.
Feline rhinotracheitis and feline calicivirus may cause oral ulceration.
Teeth
Feline External Resorptive Neck Lesions
Cats suffering from feline external resorptive neck lesions often have pain upon chewing that may be reflected by inappetence and/or abnormal masticatory movements. External neck resorption of the cheek teeth of otherwise dentally normal cats is caused by odontoclastic resorption of cementum, particularly in the neck area or root of the tooth. Osteoclast ingrowths partially or completely line the resorption cavity. The resultant cavity may harbor bacterial plaque, resulting in intense inflammation and further osteoclastic resorption of dental tissue, including dentin and the root canal. The primary cause of this condition is not known.
Tonsils
Salivary Glands
Tongue
See Disorders of Domestic Animals, Tongue and Disorders of Cats.
Esophagus
Stomach
Intestine
Viral Diseases
Parvovirus Enteritis.
Also see Disorders of Dogs, Intestinal Disorders, Viral Diseases, Parvovirus Enteritis.
In the cat, mink, and raccoon, panleukopenia, cat distemper, feline enteritis, and mink enteritis are synonyms for this important disease. Early lesions in the course of the disease are lymphoid depletion and thymic involution. Later, lesions include flaccid, segmentally reddened intestine with serositis. Lesions are generally limited to the small intestine, but colitis occurs in some cats. Villous atrophy occurs secondary to crypt cell destruction (Fig. 7-185 ). Basophilic intranuclear inclusion bodies are present in enterocytes and lymphocytes early in infection. In germ-free cats with a low enterocyte turnover, the disease caused by feline parvovirus is much less severe. Intrauterine infection causes congenital cerebellar hypoplasia of kittens. The virus is cytolytic and infects dividing cells and thus alters the differentiation of layers in the cerebellum during organogenesis. The clinical disease is characterized by dehydration, depression, and diarrhea and vomiting. Because the bone marrow is a rapidly dividing tissue, panleukopenia dominates the clinical pathologic findings.
Immunologic Disorders
See Disorders of Dogs, Intestinal Disorders, Immunologic Disorders, Diffuse Eosinophilic Gastroenteritis.
Idiopathic Disorders
Inflammatory Bowel Disease.
See Disorders of Dogs.
Feline Ulcerative Colitis.
Feline ulcerative colitis is grossly and histologically analogous to its canine counterpart, histiocytic ulcerative colitis (Fig. 7-186 ). The cause is unknown.
Figure 7-186.

Feline Ulcerative Colitis, Colon, Cat.
There are numerous round ulcers in the mucosa of this idiopathic disease.
(Courtesy Dr. H. Gelberg, College of Veterinary Medicine, Oregon State University.)
Parasitic Enteritides
See Disorders of Domestic Animals, Intestine, Diseases Caused by Specific Pathogens, Parasitic Diseases.
Intestinal Neoplasia
See Disorders of Domestic Animals, Intestine, Intestinal Neoplasia.
Peritoneum, Omentum, Mesentery, and Peritoneal Cavity
Viral Diseases
Feline Infectious Peritonitis.
Feline infectious peritonitis is a uniformly fatal disease of cats. A nearly identical coronaviral disease has been described in ferrets. Although it affects cats of all ages, the disease is principally found in the young and old. Twelve percent of feline deaths are associated with feline infectious peritonitis. The cause of the disease is a coronavirus related to the coronavirus of transmissible gastroenteritis of pigs. The coronavirus of feline infectious peritonitis in cats is believed to be a mutated enteric coronavirus. After entry into the body, the first round of viral replication takes place in the lymphoid system. Macrophages are infected and carry the virus systemically. Endothelial cells are activated secondary to upregulation of major histocompatibility complex class II. Observations suggest that activated monocytes are critical for development of vasculitis. Lesions are multifocal, and most organs, including the CNS, may be affected (see Figs. 14-105 and 14-106). The lesions in the vasculature of the eye are sometimes useful in making a tentative diagnosis of feline infectious peritonitis in the live cat, but other diseases, such as toxoplasmosis and systemic fungi, may cause similar lesions (see E-Figs. 21-11 and 21-75). The “wet form” of the disease is characterized by fibrinous polyserositis (see Fig. 7-16); the “dry form” is without the effusive process. Why one form develops rather than the other is not completely understood but may relate to the major type of immune effector cell. The disease often clusters in households, and virus spreads among cats by saliva on shared bowls and utensils or by mutation of an endogenous coronavirus.
Because of the presence of a nonneutralizing antibody, immune complexes develop and Arthus reactions localize in the vasculature. Complement is fixed, and inflammatory cell chemoattractants are produced. Vasculitis results in protein effusion. Thus lesions are vasocentric. The prodromal course of feline infectious peritonitis is shortened, and the development and extent of lesions are accelerated in seropositive cats. Feline infectious peritonitis is usually characterized by progressive wasting because of protein loss. It is unusual for a virus to result in pyogranulomatous lesions, but in feline infectious peritonitis the vasocentric deposition of immune complexes results in pyogranulomas. These lesions are single to multiple, white, and raised. On the surface of the kidney they often are linear, clearly following the renal surface vasculature (see Fig. 11-68). In its “wet form,” feline infectious peritonitis is characterized by variable of amounts of thick, stringy, high-protein effusion in body cavities. When placed between gloved fingers, this transudate may be drawn out in strings as the fingers are separated. The transudate is sterile, eliminating most other causes of fibrinous peritonitis. The granulomas are translucent and less than 2 mm in diameter. The “dry form” of the disease is identical to the wet but contains only pyogranulomas and not the exudates.
Suggested Readings
Suggested Readings are available at www.expertconsult.com .
Footnotes
For a glossary of abbreviations and terms used in this chapter see E-Glossary 7-1.
See Necropsy Techniques in E-Appendix 7-1 for information on postmortem examination of the alimentary system.
Suggested Readings
- Adaska JM, Aly SS, Moeller RB. Jejunal hematoma in cattle: a retrospective case analysis. J Vet Diag Invest. 2014;26:96–103. doi: 10.1177/1040638713517696. [DOI] [PubMed] [Google Scholar]
- Bellows J, Colitz CMH, Daristotle L. Common physical and functional changes associated with aging in dogs. J Am Vet Med Assoc. 2015;246:67–89. doi: 10.2460/javma.246.1.67. [DOI] [PubMed] [Google Scholar]
- Brodersen BW. Bovine viral diarrhea virus infections: manifestations of infection and recent advances in understanding pathogenesis and control. Vet Pathol. 2014;51:453–464. doi: 10.1177/0300985813520250. [DOI] [PubMed] [Google Scholar]
- Collins SM, Surette M, Bercik P. The interplay between the intestinal microbiota and the brain. Nat Rev Microbiol. 2012;10:735–742. doi: 10.1038/nrmicro2876. [DOI] [PubMed] [Google Scholar]
- Diab SS, Rodriguez-Bertos A, Uzal FA. Pathology and diagnostic criteria of Clostridium difficile enteric infection in horses. Vet Pathol. 2013;50:1028–1036. doi: 10.1177/0300985813489039. [DOI] [PubMed] [Google Scholar]
- Gelberg H. Comparative anatomy, physiology and mechanisms of disease production of the esophagus, stomach and small intestine. Toxicol Pathol. 2014;42:54–66. doi: 10.1177/0192623313518113. [DOI] [PubMed] [Google Scholar]
- Gyles C, Boerlin P. Horizontally transferred genetic elements and their role in pathogenesis of bacterial disease. Vet Pathol. 2014;51:328–340. doi: 10.1177/0300985813511131. [DOI] [PubMed] [Google Scholar]
- Kamanda N, Seo SU, Chen GY. Role of gut microbiota in immunity and disease. Nat Rev Immunol. 2013;13:321–335. doi: 10.1038/nri3430. [DOI] [PubMed] [Google Scholar]
- Mueller K, Ash C, Pennisi E. The gut microbiota. Science. 2012;336:1245–1247. doi: 10.1126/science.336.6086.1245. [DOI] [PubMed] [Google Scholar]
- Naveneethan U, Giannella RA. Mechanisms of infectious diarrhea. Nat Clin Pract Gastroenterol Hepatol. 2008;5:637–647. doi: 10.1038/ncpgasthep1264. [DOI] [PubMed] [Google Scholar]
- Shifrin DA, McConnell RE, Nambiar R. Enterocyte microvillus-derived vesicles detoxify bacterial products and regulate epithelial-microbial interactions. Curr Biol. 2012;22:627–631. doi: 10.1016/j.cub.2012.02.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson GW, Hoang H, Schwartz KJ. Emergence of porcine epidemic diarrhea virus in the United States: clinical signs, lesions, and viral genome sequences. J Vet Diag Invest. 2013;25:649–654. doi: 10.1177/1040638713501675. [DOI] [PubMed] [Google Scholar]
- Vannucci FA, Gebhart CJ. Recent advances in understanding the pathogenesis of Lawsonia intracellularis infections. Vet Pathol. 2014;51:465–477. doi: 10.1177/0300985813520249. [DOI] [PubMed] [Google Scholar]
E-Appendix 7-1 Necropsy Techniques
The intestinal mucosa is a labile tissue; postmortem autolysis occurs rapidly after death. The early loss of microvilli post mortem increases the difficulty of histologic visualization of pathogens such as cryptosporidia and attaching effacing Escherichia coli. Small animals can be refrigerated (not frozen) and cooled relatively rapidly, but larger animals, regardless of one's refrigeration capacity, frequently suffer mucosal decomposition. This problem is exacerbated in warm weather and delays in discovering and transporting the cadavers and performing necropsy examinations. Field necropsies are often imperative in facilitating a histologic diagnosis. At the same time, chilling excised intestine facilitates meaningful bacterial culture, bacterial toxin, and pathogen identification. Frozen tissue and intestinal content can be used for these purposes as well.
There are similarities in postmortem examination of the alimentary system regardless of species. Sometimes for small laboratory animals and pocket pets, intraluminal in situ formalin infusion is best, especially when the animal is so small that its size precludes meaningful gross examination. The correct anatomic positioning of the various parts of the intestinal tract is important, especially in horses that are most prone to displacements. In larger species, after in situ examination it is useful to remove the esophagus with the pluck and the stomach, duodenum, and intestines as a single unit. The entire intestine can then be examined following the flow of ingesta. In companion carnivores and horses the mesentery can be severed and the intestines laid out in a straight line. In ruminants and pigs, with the exception of the spiral colon, a similar dissection can be performed. Lesions and obstructions can be accurately located, measured, and described using this technique. The intestine is then opened along its antimesenteric borders and appropriate samples placed in buffered neutral formalin. Formalin will not penetrate closed lumens. A common error among students and practitioners is placing too much tissue in too little formalin. Regardless of the size of the animal, formalin will only penetrate approximately a quarter of an inch.
In the absence of lesions it is wise to take representative tissue samples from a variety of anatomic sites. In addition, because some pathogens, such as the parvoviruses of carnivores, produce “skip” lesions, more than one sample per anatomic region may be appropriate. The varying areas of the stomach should be sampled, especially fundus, antrum, and pylorus; the duodenum, including the biliary and pancreatic papillae; jejunum; ileum; cecum; and colon. These samplings are particularly important in pigs and horses because lesion distribution of many of their infectious diseases aids in diagnosis. Likewise, the ileocecocolic junction of ruminants is a prime site for mycobacteria.


