Abstract
Background:
Egg allergy is common in young children (<5 years) and has significant negative impacts on quality of life.
Objective:
The objective of this study was to characterize egg allergy prevalence, severity, baked egg tolerance, and other associated factors in a large US cohort.
Methods:
A national cross-sectional survey was administered from October 2015-September 2016, resulting in complete parent-proxy responses for 38,408 children. Weighted proportions were estimated to compare egg allergy prevalence and characteristics between key subpopulations.
Results:
Overall prevalence of current, convincingly egg allergy was 0.9% among all children and 1.3% among children <5 years. Black children were over-represented among children with egg allergy, accounting for 23.4% (95% CI: 13.1–38.4) of egg-allergic children despite comprising 13.2% (12.3-14-2) of the US pediatric population. Among children with egg allergy, 64.2% reported baked egg tolerance and 60.2% had allergy to other foods, with 29.3% having peanut allergy. Asthma was more prevalent in children with an egg allergy than children with other top 8 food allergies (46.5%, (35.8–57.4) vs 33.2% (29.6–37.0), p<0.05). Among children with current egg allergy, those with baked egg tolerance reported that their food allergy resulted in significantly reduced psychosocial burden, relative to their baked egg-allergic counterparts (M=3.1 (2.9–3.3) vs M=3.7 (3.5–3.9).
Conclusion:
Egg allergy is common amongst young children. Nearly two-thirds of children with egg allergy reported baked egg tolerance. Increased efforts are needed to ensure children with egg allergy are appropriately evaluated as many have comorbid allergic disease and determination of baked egg tolerance may improve QoL.
Keywords: Food allergy, atopy, egg allergy, prevalence, pediatrics
Introduction
Food allergies affect 7.6% of children in the U.S.1 and are associated with substantial economic burden2 as well as significant decreases in quality of life for children and their caregivers.3 Past studies report allergy to hen’s egg specifically affects 0.8% of all children1 and 1.3% of children under <5 years, making it the second most common allergy in this cohort after cow’s milk allergy.1, 4, 5 Furthermore, in a recent evaluation of anaphylaxis in infants <12 months of age, egg was found to be the most common food trigger.6 While the severity of reactions to egg can vary, past studies have found that in children with asthma, anaphylaxis triggered by egg can be life-threatening.7–9
There are five known egg proteins that have been implicated in IgE-mediated reactions.4 As some of these proteins are known to become denatured when heated,10 a subset of patients with egg allergy can tolerate egg that has been extensively heated (“baked egg” heated ≥350° for >30 minutes).10–12 In previous studies, tolerance to baked egg has been reported in 60–80% of children who have allergy to raw or lightly cooked egg.13 There is also some evidence that suggest consumption of baked egg may increase tolerance to all forms of egg by inducing immunologic changes.10 For example, baked egg-allergic infants were much more likely to have persistent egg allergy (OR>5) at 24 months, while infants who consumed baked egg between 12 and 24 months had a positive association with egg allergy resolution by 24 months.14
Among the top nine food allergens (peanut, tree nut, milk, shellfish, egg, wheat, soy, fish, and sesame), egg is one of the most commonly outgrown. One past study showed 50% of US children outgrowing the allergy by age 6,15 while another study reported that only 12% outgrew their egg allergy by age 6 but 68% did so by age 16.16 Furthermore, the Healthnuts cohort reported remarkably high rates of allergy to raw egg at 1 year (9.5% of their population-based cohort), which dropped to 1.2% among the same children when reassessed at 4 years.17 For those who do not outgrow their allergy, avoidance of egg is the main form of management which is challenging as egg is a common ingredient in many foods.4 Further characterization of egg allergy severity, baked-egg tolerance, and allergy-related quality of life among US children is needed. The goal of this study is to evaluate the prevalence, symptoms, and severity of egg allergy with a specific focus on those with baked egg tolerance and other associations via a large, population-based study of U.S. households.
Methods
A US population-based, cross-sectional survey was administered to a sample of 53,575 US households from October 2015 to September 2016. The study protocol was approved by the institutional review boards of Northwestern University and NORC at the University of Chicago.
Study Participants and Recruitment
Eligible study participants included adults (≥18 years old) who resided in a US household and able to complete the survey in English or Spanish via web or telephone. Similar to our 2009–2010 national survey,18 this study relied upon a nationally-representative household panel to support population-level inference. Study participants were first recruited from NORC at the University of Chicago’s, nationally-representative, probability-based AmeriSpeak Panel, with a survey completion rate of 51.2% (7218 responses of 14 095 invitees). Each child was assigned a base, study-specific sampling weight equal to their responding parent’s non-response adjusted AmeriSpeak sampling weight. Child-specific weights were further adjusted to account for random selection of up to three children/household and raked to external pediatric population totals. Parental weights were reconciled with external population totals associated with age, sex, education, race/ethnicity, housing tenure, telephone status, and Census Division via iterative proportional fitting to improve external validity. In order to increase precision of population parameter estimates, the population-weighted AmeriSpeak responses were then augmented via iterative proportional fitting with calibration-weighted, non-probability-based responses obtained through Survey Sampling International. The complex survey development, sampling, weighting, and analysis procedures utilized here are detailed in Gupta et al 2018.1
Outcome Measures
The primary outcome measure for the present study was the prevalence of pediatric egg allergy. Parent-reported egg allergies were only considered convincing if the most severe reaction reported to that food included at least one symptom on the stringent symptom list developed by our expert panel, even if such allergies were reported to be physician-diagnosed (Figure 1). Convincing egg allergies for which parents reported a doctor’s diagnosis were considered physician-confirmed. A severe reaction history to egg was indicated by parent-report of multiple specific stringent symptoms occurring within two or more of the following four organ systems (skin/oral mucosa, gastrointestinal, cardiovascular, and respiratory) in response to the question “Think back to the most severe allergic reaction to egg that your child has ever had. What were [his/her] symptoms?” Both current and outgrown egg allergies were assessed, as was the ability to tolerate baked egg. Complete description of survey development, testing, categorization of allergy type has been published previously.1 The text of survey items used in the present analyses are provided in Appendix 1, in the Online Repository Text.
Figure 1.
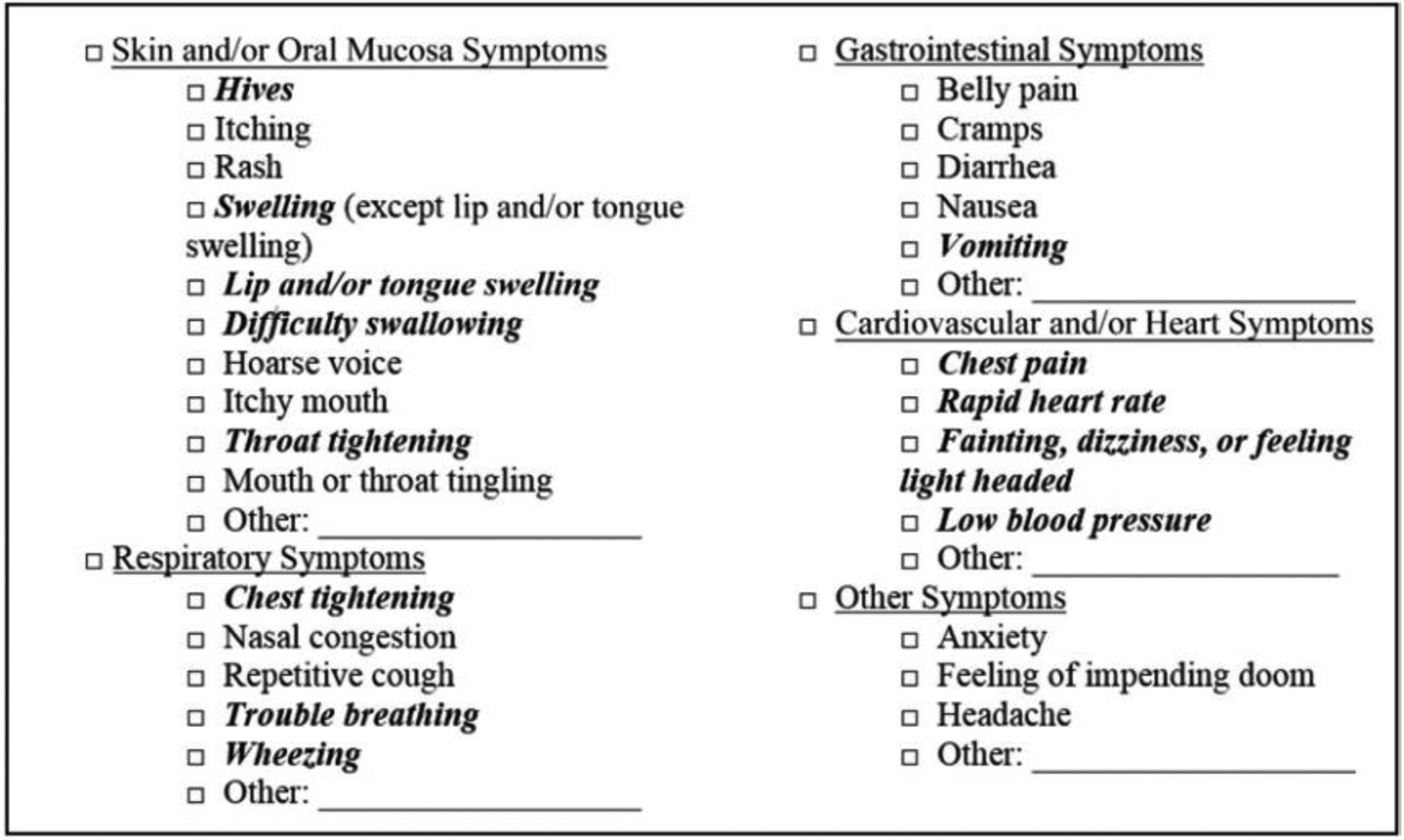
Specific Reaction Symptoms used to Characterize “Convincing” Egg Allergy List of allergic reaction symptoms highlighting stringent symptoms indicative of convincing food allergy. All symptoms listed are offered as answer choices in the survey. Symptoms in bold italics comprised our expert panel’s stringent symptom list. A convincing food allergy required the patient report of at least 1 stringent symptom during the child’s most severe reaction to a given food. A severe reaction consisted of a parent report of at least 2 stringent symptoms from 2 different body systems during a child’s most severe reaction to a given food.
To assess the psychosocial burden of living with a food allergy the food allergy independent measure (FAIM; provided in Appendix B in the Online Repository Text) was administered to all respondents reporting a current food allergy. This validated parent-report measure is comprised of 6 questions, which are scored on a 1 to 7 point scale with higher scores indicative of greater psychosocial burden and lower quality of life (QoL).19 FAIM scores for the parent-proxy child form (<13 years) and parent-proxy teen form (13–17 years) were calculated as described by the scale authors.19
Statistical Analysis
Complex survey-weighted means and proportions were calculated to estimate US population prevalence of pediatric egg allergy and other characteristics using STATA 14 svy: prefix. Cluster robust standard errors accounted for clustering of multiple children within the same household. The food allergy independent measure exhibited excellent internal consistency (Chronbach’s α >.8) and confirmatory factor analysis of the food allergy independent measure concluded that a two-factor solution exhibited excellent fit to the data (Confirmatory Fit Index [CFI]≥.950; Root Mean Square Error of Approximation [RMSEA]<.08).20 Two-sided hypothesis tests were utilized, with 2-sided P < .05 considered to be statistically significant.
Results
Egg Allergy Prevalence and Demographic Characteristics
Across the United States 53,575 households were surveyed and complete parent-proxy responses were collected for 38,408 children. Overall prevalence of convincing egg allergy was 0.9% in all children and 1.3% of young children (<5 years). Demographic characteristics of parent-reported egg allergy were evaluated (Table 1) and showed that Black children made up a larger portion of children with an egg allergy compared to the proportion of Black children in the general population (23.4%, (13.1–38). vs 13.2% (12.3–14.2 4), p<0.05). Conversely, White, non-Hispanic children made up a smaller proportion. (40.8%, (31.8–50.5) vs 52.8%, (51.2–54.4), p<.05). Compared to children with other top 8 food allergies, a greater proportion of egg allergy patients were young children 1–2 years of age [19.6% (12.7–29.1) vs 12.5% (9.4–16.4)] and 3–5 years of age [22.3 (16.4–29.6) vs. 15.7(13.0–18.8)]. Age-specific prevalence of egg-allergy peaks between 1–2 years of age—with 2% meeting convincing symptom-report criteria and gradually declines across childhood, dropping to 0.5% of 14–17 year olds with convincing egg allergy (Figure 2).
TABLE 1.
Demographics and Comorbid Allergic Disease
| Variable | All children (95% CI) | Children with Egg Allergy (95% CI) | Children with Other Allergies† (95% CI) |
|---|---|---|---|
| Race/ethnicity | |||
| Asian, non-Hispanic | 3.2 (2.8–3.7) | 3.6 (1.8–6.9) | 2.8 (2.1–3.6) |
| Black, non-Hispanic | 13.2 (12.3–14.2) | 23.4 (13.1–38.4) | 15.0 (12.7–17.7) |
| White, non-Hispanic | 52.8 (51.2–54.4) | 40.8 (31.8–50.5) | 48.3 (44.3–52.2) |
| Hispanic | 24.1 (22.5–25.7) | 22.6 (15.9–31.0) | 27.6 (23.6–31.9) |
| Multiple/other | 6.6 (6.1–7.3) | 9.6 (5.6–16.1) | 6.9 (5.4–8.7) |
| Born in the US | |||
| Yes | 97.7 (97.3–98.0) | 95.1 (88.9–97.9) | 98.7 (98.0–99.2) |
| No | 2.3 (2.0–2.7) | 4.9 (2.1–11.2) | 1.3 (.8–2.0) |
| Sex | |||
| Female | 48.9 (47.8–50.0) | 47.9 (37.5–58.6) | 54.9 (42.2–49.7) |
| Male | 51.1 (50.0–52.2) | 52.1 (41.4–62.6) | 54.1 (50.3–57.8) |
| Age | |||
| <1 year | 5.3 (4.8–5.9) | 2.2 (1.2–4.0) | 2.1 (1.5–3.0) |
| 1–2 year | 10.6 (10.0–11.3) | 19.6 (12.7–29.1) | 12.5 (9.4–16.4) |
| 3–5 year | 16.2 (15.5–17.0) | 22.3 (16.4–29.6) | 15.7 (13.0–18.8) |
| 6–10 year | 27.9 (26.9–28.8) | 26.3 (19.9–33.9) | 30.7 (27.4–34.2) |
| 11–13 year | 16.6 (15.9–17.4) | 17.6 (12.2–24.8) | 16.9 (14.1–20.0) |
| 14–17 year | 23.4 (22.4–24.4) | 12.0 (8.4–16.8) | 22.2 (19.3–25.3) |
| Household income, $ | |||
| <25,000 | 16.1 (14.9–17.3) | 12.7 (7.1–21.8) | 14.9 (12.2–18.1) |
| 25,000–49,000 | 22.2 (20.9–23.5) | 20.3 (14.1–28.3) | 22.5 (19.5–25.9) |
| 50,000–99,999 | 31.1 (29.8–32.5) | 38.7 (28.0–50.6) | 32.0 (28.8–35.4) |
| 100,000–149,000 | 19.2 (18–20.5) | 21.3 (15.7–28.2) | 20.8 (17.2–25.0) |
| ≥150,000 | 11.4 (10.3–12.6) | 7.0 (4.3–11.3) | 9.7 (7.5–12.5) |
| Other Conditions | |||
| Asthma | 12.2 (11.4–13.0) | 46.5 (35.8–57.4) | 33.2 (29.6–37.0) |
| Eczema | 5.9 (5.3–6.5) | 19.0 (12.2–28.2) | 15.7 (12.7–19.1) |
| Environmental Allergies | 12.8 (12.0–13.6) | 38.2 (30.7–46.4) | 30.3 (27.0–34.0) |
| Eosinophilic Esophagitis | 0.2 (0.1–0.2) | 1.2 (0.5–2.7) | 0.7 (.4–1.2) |
Note: These are weighted proportions
The other top 8 food allergies (peanut, tree nut, milk, wheat, soy, fish, shellfish, sesame)
Figure 2.
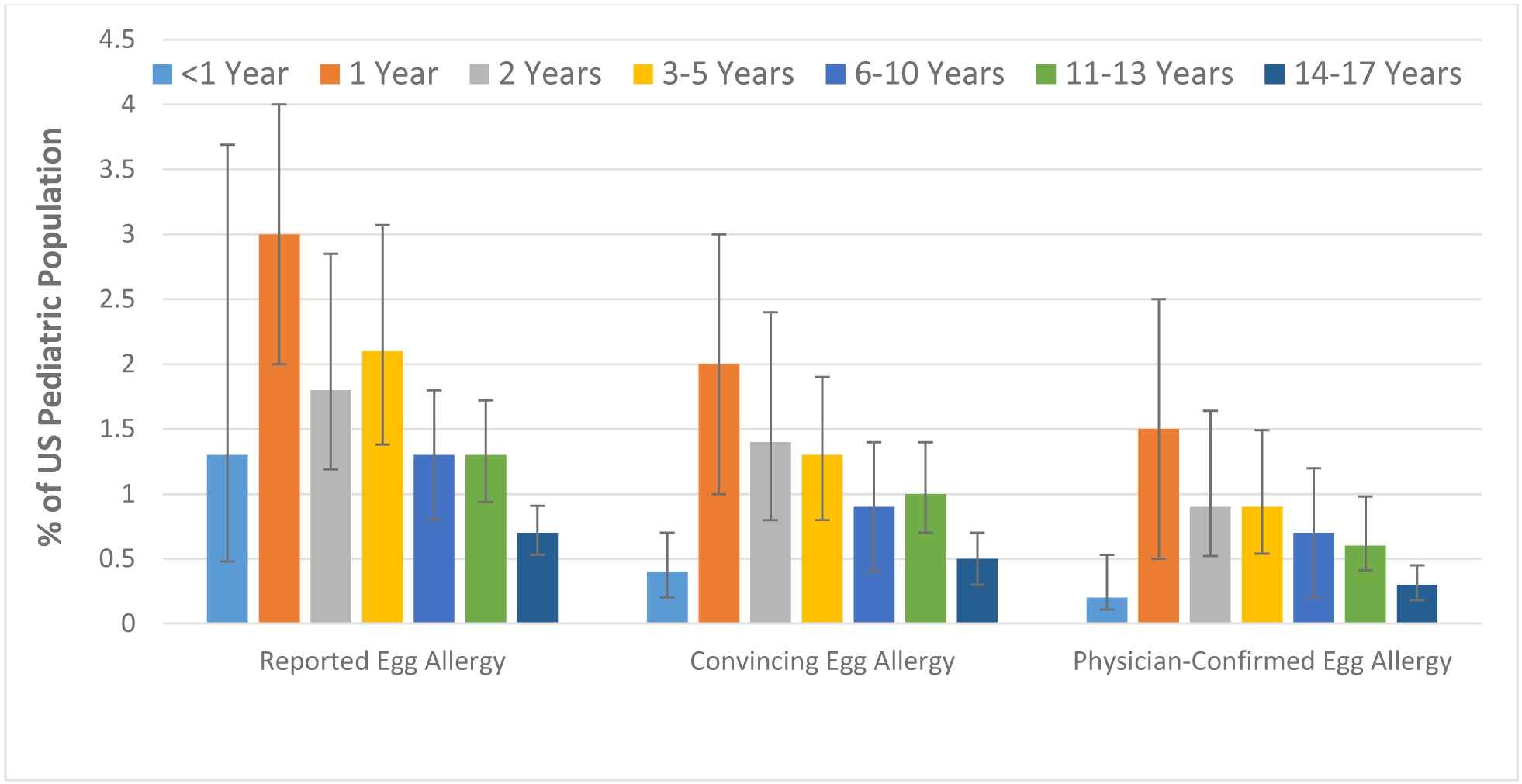
Age-specific Prevalence of Current Egg Allergy by Food Allergy Category
Co-Morbid Atopic Conditions
When compared to the general population, egg allergic children were more likely to have atopic comorbid conditions such as eczema (19.0% (12.2–28.2) vs 5.9% (5.3–6.5), p<0.05), asthma (46.5%, (35.8–57.4) vs 12.2% (11.4–13.0), p<0.05), environmental allergies (38.2%, (30.7–46.4) vs 12.8%, (12.0–13.6), p<0.05), and eosinophilic esophagitis (1.2%, (.5–2.7) vs 0.2 (0.1–0.2), p<0.05). Asthma was more prevalent in egg-allergic children than children with other top 8 food allergies (46.5%, (35.8–57.4) vs 33.2% (29.6–37.0), p<0.05).
Baked Egg Tolerance
Baked egg tolerance was reported among 64.2% of the children with egg allergy. Children whose parents reported they could not tolerate baked egg were more likely to be allergic to milk than children with baked egg tolerance (51.3%, (29.5–72.6) vs 26.3%, (19.6–34.4), p=0.03). Children whose parents reported they could not tolerate baked egg were also somewhat more likely to be allergic to multiple food allergens relative to children with baked egg tolerance (81.8, (69.0–90.1) vs 72.4%, (64.3–79.2), p=0.18). Differences in reaction symptomatology and outcomes between egg-allergic children who can vs. cannot tolerate baked egg products are summarized in Figure 3.
Figure 3. Comparison of Outcomes between Baked Egg Tolerant vs Baked Egg Allergic Children.
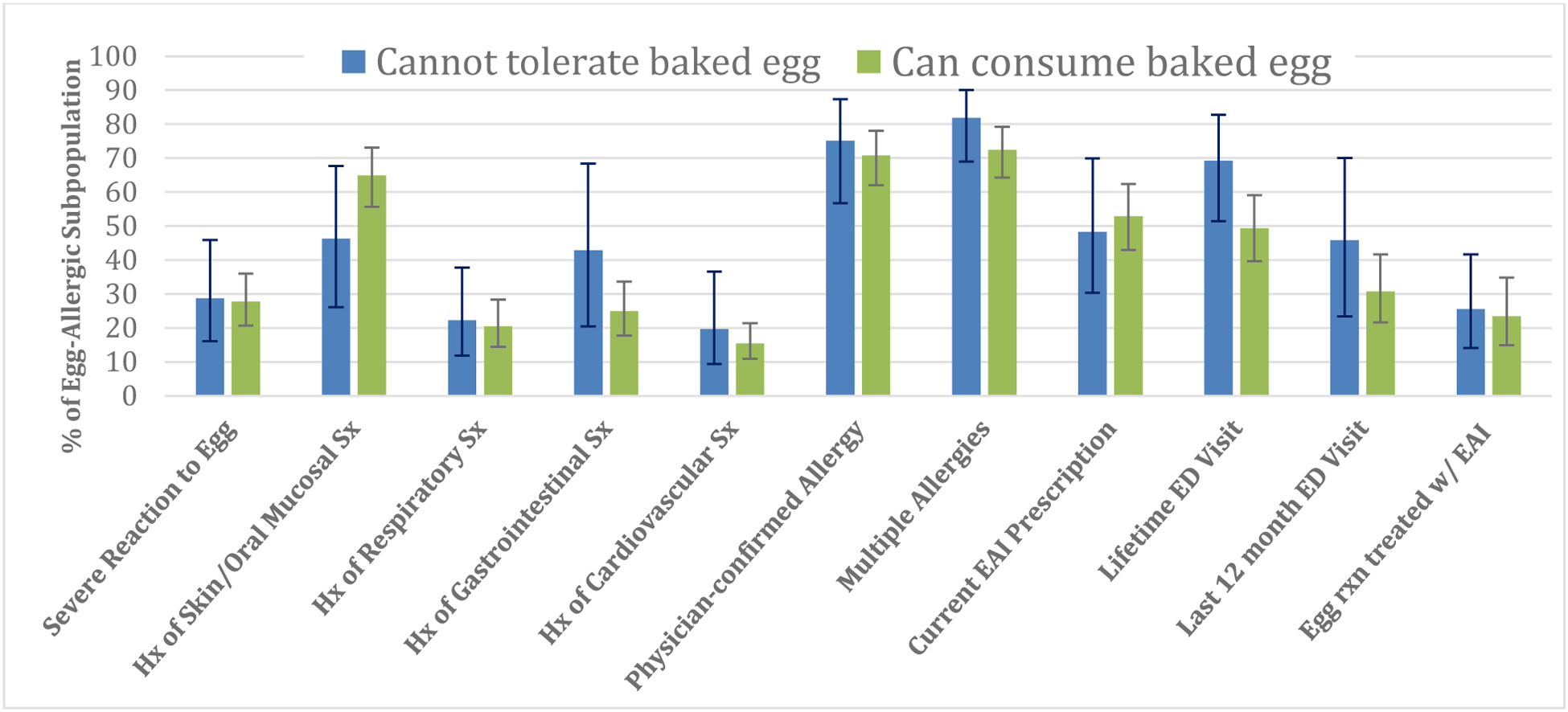
Hx: History
Sx: Symptoms
Rxn: Reaction
W/ EAI: With Epinephrine Auto Injector
Egg Allergy and Other Major Food Allergens
Amongst egg-allergic children, 60.2% had a comorbid allergy with one of the other top eight food allergens, with milk (35.2% (24.6–47.5) and peanut (29.3% (22.0–37.7) being the most common (Table 2). Sesame [6.1%, (3.5–10.3) vs 3.0 % (2.2–4.2), p=0.03] and soy [13.2%, (7.3–22.9) vs 6.9 % (5.0–9.5), p=0.05] allergies were roughly twice as prevalent among egg-allergic children compared to children with the other top 8 food allergens. Among children with a parent-reported egg-allergic reaction occurring within the first year, prevalence rates of convincing peanut allergy were 21.5% (12.1–35.1), while only 9.8% (6.3–14.9) of children with reactions to cow’s milk in the first year of life had convincing peanut allergy. However, children with reported soy or wheat-allergic reactions—the other most common food allergies reported during the first year of life—had a comparable prevalence of peanut allergy to those reporting early egg allergy (soy=18.9% (9.7–33.0); wheat=26.1% (12.1–47.5).
TABLE II.
Comorbid Food Allergies in Children with Egg Allergy
| Variable | Among Children with Egg Allergy | Among Children with Top 8 Food Allergies besides Egg† | P-value |
|---|---|---|---|
| Baked Egg Tolerance | 64.2 (51.9–74.9) | -- | |
| Top 8 Food Allergy (besides Egg) | 60.2 (53.0–67.0) | -- | |
| Comorbid Food Allergies | |||
| Peanut | 29.3 (22.0–37.7) | 37.9 (34.2–41.7) | 0.07 |
| Milk | 35.2 (24.6–47.5) | 31.4 (27.6–35.5) | 0.53 |
| Shellfish | 15.9 (10.8–23.0) | 22.2 (19.4–25.3) | 0.1 |
| Tree nuts | 17.5 (12.3–24.2) | 20.3 (17.8–23.1) | 0.41 |
| Wheat | 11.5 (7.5–17.1) | 7.7 (5.6–10.6) | 0.14 |
| Soy | 13.2 (7.3–22.9) | 6.9 (5.0–9.5) | 0.05 |
| Fin fish | 11.7 (7.0–18.9) | 8.5 (6.6–10.8) | 0.25 |
| Sesame | 6.1 (3.5–10.3) | 3.0 (2.2–4.2) | 0.03 |
The other top 8 food allergies (peanut, tree nut, milk, wheat, soy, fish, shellfish, sesame)
Reaction Severity
Overall, 28.1% (21.5–36.0) children with egg allergy reported having experienced a severe allergic reaction (allergic symptoms in egg-allergic children compared to children with other allergies is summarized in Table E1, in the Online Repository File). Egg-allergic children were more likely to have gone to the emergency department (ED) in their lifetime for any food allergy reaction (not necessarily a reaction to egg), than children with the other top eight food allergies (56.4% (46.6–65.8) vs 43.7% (39.9–47.6), p=0.02). This also held true for ED visits within the last 12 months for egg-allergic children vs. children with allergy to the other top eight food allergens (36.1% (25.0–48.9) vs 18.0% (14.7–21.8), p=0.001). Children with baked egg tolerance were less likely to report food allergy-related emergency department visits than their baked-egg allergic counterparts—both over their lifetime (49.3% (39.6–59.1) vs 48.2% (27.1–69.9), p=0.05), and within the last year (30.7% (21.6–41.6) vs 45.8% (23.4–70.0), p=0.26). Allergic symptoms in each cohort are summarized in Table E2, in the Online Repository File).
Physician Diagnosis
A physician diagnosis did not occur in 27.8% of children with convincing egg allergy. Egg- allergic children with baked egg tolerance lacked a physician-diagnosis 25% of the time vs 29% in egg allergic children without baked egg tolerance (p=.63). Furthermore, 34% of egg allergic children with history of severe reactions and 25% of egg allergic children without a history of severe reactions lacked a physician-diagnosis (p=.24). There were no differences found in those with a physician diagnosis vs those without with respect to mean age, sex, race, or ethnicity. Of the children with convincing egg allergy whose allergy was physician-diagnosed, 61.7% reported skin prick testing (SPT), 46.7% serum IgE blood testing and 20.9% reported receiving an oral egg challenge.
Both reporting a current EAI prescription [32.2 (21.0–45.9) vs. 58.4 (43.4–72.0%) p<.01] and a history of EAI use to treat an egg-allergic reaction [13.6% (8.0–22.2%) vs 28.1% (18.6–40.1%); p=.02] were less common among children without physician vs physician-confirmed egg allergy.
Outgrowth
In this survey, 418 children reported having a current convincing egg allergy and 152 reported having outgrown a convincing egg allergy (Table 3). Amongst children who had outgrown an egg allergy, 70.5% could tolerate baked egg prior to outgrowing their allergy (vs 64% with current egg allergy) and 46.3% had multiple concurrent food allergies compared to 75.8% (68.7–81.7) with current egg allergy. In comparison to children with a current egg allergy, children who outgrew their egg allergy were somewhat less likely to have physician-diagnosed asthma (46.5% (35.8–57.4) vs 32.2% (21.4–45.3) p=.09).
TABLE III.
Outgrown Egg Allergy
| Variable | Characteristics of Children who Outgrew an Egg Allergy† |
|---|---|
| Age | |
| 1–2 y | 4.1 (1.8–8.9) |
| 3–5 y | 20.9 (12.1–33.6) |
| 6–10 y | 45.8 (31.3–60.9) |
| 11–13 y | 10.2 (6.0–16.8) |
| 14–17 y | 18.8 (11.6–29.0) |
| Has Multiple Current Food Allergies | 46.3 (27.6–66.0) |
| Baked Egg Tolerance | 70.5 (58.2–80.4) |
| Race/ethnicity | |
| Asian, non-Hispanic | 4.8 (2.2–10.1) |
| Black, non-Hispanic | 4.8 (2.1–10.5) |
| White, non-Hispanic | 53.3 (38.6–67.5) |
| Hispanic | 30.0 (16.6–48.0) |
| Multiple/other | 7.1 (3.7–13.2) |
| Sex | |
| Female | 42.4 (28.4–57.6) |
| Male | 57.6 (42.4–71.6) |
| Other Conditions | |
| Asthma | 32.2 (21.4–45.3) |
| Eczema | 22.4 (13.6–34.7) |
| Environmental Allergies | 30.7 (20.5–43.4) |
| Eosinophilic Esophagitis | 4.0 (1.2–12.6) |
| Organ System Involved: | |
| Skin/mucosal tissue | 76.2 (57.0–88.5) |
| GI | 26.9 (14.2–45.1) |
| Respiratory | 16.5 (9.1–28.0) |
| Cardio | 7.6 (4.0–13.7) |
Comparison of children with egg allergy and the children with top 9 allergies besides egg
Food Allergy-related Quality of Life
Children with convincing egg allergy who reported they could consume baked egg products reported better food allergy-related QoL (assessed by FAIM) relative to baked egg-allergic children (MFAIM=3.13 vs 3.69; p<.01) (Table 4). This difference was also significant when these unadjusted analyses were restricted to children with only egg allergy and no other comorbid food allergies (MFAIM=3.23 vs 2.64; p<.01). Furthermore, these observed differences in FAIM scores remained statistically significant after adjustment for a variety of potential confounders including age, sex, race/ethnicity, income, history of severe reactions to egg, emergency department visits, physician-diagnosis of egg allergy, epinephrine use, having an epinephrine prescription, and country of birth. Survey item-level scores are summarized in Table 4, each of which indicated greater burden among baked egg-allergic children.
TABLE IV.
FAIM Scores among Egg-Allergic Children
| Egg allergic children with baked egg tolerance [Mean (95% CI)] | Egg allergic children with baked egg allergy [Mean (95% CI)] | |
|---|---|---|
| Mean FAIM | 3.1 (2.9–3.3) | 3.7 (3.5–3.9) |
| Q1 | 2.4 (2.1–2.7) | 2.8 (2.1–3.5) |
| Q2 | 2.8 (2.5–3.1) | 3.2 (2.8–3.5) |
| Q3 | 1.8 (1.5–2.1) | 2.0 (1.5–2.4) |
| Q4 | 1.9 (1.6–2.1) | 2.2 (1.8–2.6) |
| Q5 | 2.3 (2.0–2.6) | 3.1 (2.7–3.6) |
| Q6 | 1.6 (1.3–1.8) | 2.9 (2.3–3.3) |
FAIM: Food Allergy Independent Measure
Discussion
To our knowledge, this is the first study to comprehensively describe current egg allergy prevalence among children from a large, representative sample of US households. Our study found that egg allergy is a common allergy primarily among young children, affecting 1.3% of children < 5 years of age, with disease burden amongst black children and children with comorbid atopic conditions. Overall, egg-allergic children had high rates of comorbid food allergies, with 60.2% reporting an allergy to one of the other top eight food allergens—primarily peanut and milk. Over one-third of the children with egg allergy reported they could not tolerate baked egg, and reported higher rates of comorbid food allergy and food allergy-related ED visits. Furthermore, those with baked egg tolerance reported better food allergy-related QoL. Thus, while the majority of children with egg allergy reported having a physician diagnosis, greater promotion of physician evaluation, including assessing baked egg tolerance, may be helpful for families managing this food allergy.
While there are well-acknowledged limitations to cross-sectional parent-report prevalence survey data, it is notable that the present egg allergy prevalence estimates are largely consistent with data from high-quality international cohort studies. For example, our point prevalence estimate of 1.4% among US 2 year-old children is similar to the rate of 1.2% reported among 2 year-old children in the 9 country Europrevall consortium.21 Our point prevalence estimate of 1.3% among 3–5 year-olds is also remarkably similar to challenge-confirmed point prevalence estimates among 4 year-olds reported from the Australian population-based HealthNuts study (1.2%),17 as well as estimates from 4 year old participants in the Isle of Wight birth cohort (1.1–1.4%).22 Furthermore, the distribution of prevalence rates across the pediatric age spectrum is consistent with longitudinal data published by Savage, who found that 50% of egg allergic infants outgrew their egg allergy by age 9 and two-thirds by age 16. This was the case irrespective of the definition used for egg allergy—parent reported, convincing, or physician-confirmed. While US population-based birth cohort studies would provide much-needed validation of the current survey-based prevalence measures, the similarity between prevalence estimates gleaned from the present cross-sectional questionnaire and the aforementioned European and Australian birth cohort studies support the utility of parent-proxy survey-based approaches to food allergy prevalence estimation in young children.
Egg allergy has been used as an important predictor of atopy among infants and young children. For example, the HealthNuts study also found that egg allergy is associated with 2-fold higher risk for asthma regardless of whether egg allergy was transient or persistent.23 Similarly, our data support the idea that egg-allergic children may be particularly atopic, given that rates of asthma (46.5% vs 33.2%), eczema (19.0% vs 15.7%), and allergic rhinitis (38.2% vs 30.3%) were all higher among egg-allergic children, relative to children with other top 8 food allergies (Table 1). Furthermore, just over 60% of convincingly egg-allergic children in our study had a comorbid food allergy, with milk and peanut being the most common.
Given that the LEAP criteria utilize the presence of egg allergy during the first year as an indicator of increased peanut allergy risk, the present study examined the prevalence of peanut allergy in those reporting an egg-allergic reaction by 11 months. Among these individuals, 1 in 5 developed a peanut allergy, a ten-fold increase in risk over those who didn’t report such reactions. This suggests that egg-allergic reactions during infancy are considerably more predictive of peanut allergy than cow’s milk reactions, where only 1 in 10 went on to develop a peanut allergy. However, when all children are considered (not just infants), data show that a lower proportion of egg-allergic children had comorbid peanut allergy than did those with other top 8 allergies. Additionally, our data also suggests that early life soy or wheat-allergic reactions may be similarly predictive of subsequent peanut allergy development, given that convincing peanut allergy was also prevalent among 1 in 5 individuals reporting reactions to either food.
In this study, over 25% of children with egg allergy were reported to have experienced a severe allergic reaction with egg exposure. A recent review of egg allergy studies reported that egg was the trigger for 7–12% of pediatric anaphylaxis presentations.24 Specifically, amongst infants however, a recent study found that egg was the most common food trigger for anaphylaxis, accounting for 38% of the cases.6 Notably, children with egg allergy in our study reported more frequent ED visitations for food allergy concerns compared to children without egg allergy. While the survey did not elicit detailed information to determine whether ED visits were specifically to address allergic reactions triggered by egg, these data nevertheless suggest that this population of children may benefit from increased attention and education.
Two-thirds of children with egg allergy in this study reported tolerating baked egg. This is consistent with a prospective study reporting 63% of children with egg allergies passed an observed baked egg oral challenge.25 In another study, children with known baked egg tolerance were more likely to pass native egg oral food challenge compared to children who could not tolerate baked egg or had not previously been exposed to egg.26 Furthermore, even in those who reacted to raw egg, these reactions occurred at higher doses of raw egg and required epinephrine less often. This is consistent with our findings that children who reported baked egg tolerance had less severe anaphylactic reactions and reduced likelihood of reporting food allergy-related emergency department visits. Our study also demonstrated that the ability to eat baked egg products is associated with higher food allergy- related QoL and greater likelihood of reporting a previously outgrown egg allergy.
Nearly three-quarters of children who had a convincing history of egg allergy had their diagnosis confirmed by a physician, and our study found many reasons to continue encouraging potentially egg-allergic children to seek formal physician diagnosis. The general risks of not having confirmatory evaluation are many, including lack of education and preparedness with emergency medications to treat allergic reactions. Errors in allergen avoidance places the child at risk for potentially severe reactions, as well as unnecessary over-restriction of foods which can negatively affect growth and nutrition.27, 28 Furthermore, specific to egg allergy, evaluation may lead to a determination of baked egg tolerance as well as evaluation of other possible food allergies and atopic diseases. One previous study reported that a ovomucoid skin prick test is greater than 11mm had a positive-predictive value of 100% for baked-egg intolerance,25 thus children with SPT <11mm will need to discuss the risk and benefits of an oral baked egg challenge with their Allergist. Understanding which egg protein a child is allergic to also aids in this discussion, as not all egg allergens are affected by heat.10
Compared to other allergens like peanut, tree nuts, shellfish, and finfish, egg is a highly ubiquitous allergen that can be particularly difficult to avoid since it is not only a known ingredient in many baked goods, it is also frequently present as a “hidden” ingredient. For example, eggs are frequently used as clarifying agents, as components of soup stocks, cocktails, and as a wash on bread products to improve their appearance.29 Recent analysis of a prospective case series of 500 food-allergic infants followed over a three-year period estimated that nearly 1 in 5 allergic infants experienced an egg-allergic reaction. Nearly all (87%) resulted from accidental exposure.30 Therefore, it is perhaps unsurprising that individuals with the ability to tolerate baked egg reported significantly greater food allergy-related QoL in our study, which was primarily influenced by reductions in reported allergen avoidance and concomitant adverse social impacts.
There were several limitations to this study. This was a survey-based study which is subject to responder recall bias. Furthermore, data on the frequency and reproducibility of reaction symptoms were not collected. Since roughly 1 in 4 children with egg allergy did not report physician-confirmation of their egg allergy and few had undergone food challenges, underestimation of baked egg tolerance is possible. Lastly, while our prevalence findings are consistent with cohort studies, another limitation is that our estimates for physician diagnosis, allergy testing, and ED visits were based on parental reports and not medical records. Despite these limitations, this study reports on egg allergy in a large, nationally-representative sample and used stringent criteria developed in collaboration with an expert panel to exclude adverse responses not likely to be IgE-mediated food allergy. These rigorous criteria yielded a prevalence estimate similar to other population-based prevalence studies utilizing clinical confirmation of disease over a similar time period.17, 22 Our study also reinforces the importance of formal evaluation by a physician as egg allergy may be a marker of greater atopic burden. Understanding the higher prevalence in young children, the strong association with comorbid food allergy, and the improved quality of life for those with baked egg tolerance provides important data for clinicians caring for these children.
Conclusions
Egg allergy is common amongst young children, with a peak prevalence of 2% in children age 1–2 years of age. Children with egg allergy have higher rates of asthma, eczema, and allergic rhinitis relative to children with the other top 8 allergies. While peanut and milk were the most common comorbid food allergies, children with egg allergy were also twice as likely to report comorbid sesame and soy allergies, than were children with the other top 8 allergies. Nearly two-thirds of children with egg allergy were reported to be tolerant to baked egg products, which was associated with improved QoL and fewer food allergy-related emergency department visits. Increased efforts are needed to ensure children with egg allergy are appropriately evaluated in order to assess for co-morbid food allergy, other atopic disease, and baked egg tolerance.
Supplementary Material
Highlights Box:
-
What is already known about this topic?
Past studies found that egg allergy affects 0.8% of US children; further characterization of egg allergy among US children is necessary to help create appropriate management guidelines.
-
What does this article add to our knowledge?
Egg allergy prevalence is 0.9% among all children and 1.3% among children <5 years. Among egg allergic children, 64.2% reported baked egg tolerance and 60.2% had allergy to other foods. Additionally, baked egg tolerance was associated with a significant higher quality of life.
-
How does this study impact current management guidelines?
Increased efforts are needed to ensure children with egg allergy are appropriately evaluated in order to assess for co-morbid food allergy, other atopic disease, and baked egg tolerance.
Acknowledgements
We would like to thank Julia Ross for her help with analysis of the data.
Funding source: This study was supported by grant R21AI135702-PI from the National Institute of Allergy and Infectious Disease (Dr Gupta).
Conflict of Interest:
J Wang receives research support from National Institute of Allergy and Infectious Diseases, Aimmune, DBV Technologies, and Regeneron, and consultancy fees from ALK Abello, and DBV Technologies. R. S. Gupta reports receiving grants from the National Institutes of Health (grant nos. R21 ID # AI135705, R01 ID# AI130348, and U01 ID # AI138907), Rho Inc, Stanford Sean N. Parker Center for Allergy Research, UnitedHealth Group, Thermo Fisher Scientific, Genentech, and the National Confectioners Association; and serves as a medical consultant/advisor for Before Brands, Kaléo Inc, Genentech, Institute for Clinical and Economic Review, Food Allergy Research & Education, Aimmune Therapeutics, and DBV Technologies. The rest of the authors declare that they have no relevant conflicts of interest.
Abbreviations:
- QoL
Quality of Life
- IgE
Immunoglobulin E
- FAIM
Food Allergy Independent Measure
- ED
Emergency Department
- EAI
Epinephrine Auto Injector
References
- 1.Gupta RS, Warren CM, Smith BM, Blumenstock JA, Jiang J, Davis MM, et al. The Public Health Impact of Parent-Reported Childhood Food Allergies in the United States. Pediatrics. 2018;142(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gupta R, Holdford D, Bilaver L, Dyer A, Holl JL, Meltzer D. The economic impact of childhood food allergy in the United States. JAMA Pediatr. 2013;167(11):1026–31. [DOI] [PubMed] [Google Scholar]
- 3.Warren CM, Otto AK, Walkner MM, Gupta RS. Quality of Life Among Food Allergic Patients and Their Caregivers. Curr Allergy Asthma Rep. 2016;16(5):38. [DOI] [PubMed] [Google Scholar]
- 4.Caubet JC, Wang J. Current understanding of egg allergy. Pediatr Clin North Am. 2011;58(2):427–43, xi. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sicherer SH, Sampson HA. 9. Food allergy. J Allergy Clin Immunol. 2006;117(2 Suppl Mini-Primer):S470–5. [DOI] [PubMed] [Google Scholar]
- 6.Samady W, Trainor J, Smith B, Gupta R. Food-induced anaphylaxis in infants and children. Ann Allergy Asthma Immunol. 2018;121(3):360–5. [DOI] [PubMed] [Google Scholar]
- 7.Tariq SM, Matthews SM, Hakim EA, Arshad SH. Egg allergy in infancy predicts respiratory allergic disease by 4 years of age. Pediatr Allergy Immunol. 2000;11(3):162–7. [DOI] [PubMed] [Google Scholar]
- 8.Gaffin JM, Sheehan WJ, Morrill J, Cinar M, Borras Coughlin IM, Sawicki GS, et al. Tree nut allergy, egg allergy, and asthma in children. Clinical pediatrics. 2011;50(2):133–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wang J, Liu AH. Food allergies and asthma. Current opinion in allergy and clinical immunology. 2011;11(3):249–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Leonard SA, Caubet JC, Kim JS, Groetch M, Nowak-Wegrzyn A. Baked milk- and egg-containing diet in the management of milk and egg allergy. J Allergy Clin Immunol Pract. 2015;3(1):13–23; quiz 4. [DOI] [PubMed] [Google Scholar]
- 11.Lemon-Mule H, Sampson HA, Sicherer SH, Shreffler WG, Noone S, Nowak-Wegrzyn A. Immunologic changes in children with egg allergy ingesting extensively heated egg. J Allergy Clin Immunol. 2008;122(5):977–83.e1. [DOI] [PubMed] [Google Scholar]
- 12.Lieberman JA, Huang FR, Sampson HA, Nowak-Wegrzyn A. Outcomes of 100 consecutive open, baked-egg oral food challenges in the allergy office. J Allergy Clin Immunol. 2012;129(6):1682–4.e2. [DOI] [PubMed] [Google Scholar]
- 13.Osborne NJ, Koplin JJ, Martin PE, Gurrin LC, Lowe AJ, Matheson MC, et al. Prevalence of challenge-proven IgE-mediated food allergy using population-based sampling and predetermined challenge criteria in infants. J Allergy Clin Immunol. 2011;127(3):668–76.e1–2. [DOI] [PubMed] [Google Scholar]
- 14.Peters RL, Dharmage SC, Gurrin LC, Koplin JJ, Ponsonby AL, Lowe AJ, et al. The natural history and clinical predictors of egg allergy in the first 2 years of life: a prospective, population-based cohort study. J Allergy Clin Immunol. 2014;133(2):485–91. [DOI] [PubMed] [Google Scholar]
- 15.Sicherer SH, Wood RA, Vickery BP, Jones SM, Liu AH, Fleischer DM, et al. The natural history of egg allergy in an observational cohort. J Allergy Clin Immunol. 2014;133(2):492–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Savage JH, Matsui EC, Skripak JM, Wood RA. The natural history of egg allergy. J Allergy Clin Immunol. 2007;120(6):1413–7. [DOI] [PubMed] [Google Scholar]
- 17.Peters RL, Koplin JJ, Gurrin LC, Dharmage SC, Wake M, Ponsonby AL, et al. The prevalence of food allergy and other allergic diseases in early childhood in a population-based study: HealthNuts age 4-year follow-up. J Allergy Clin Immunol. 2017;140(1):145–53.e8. [DOI] [PubMed] [Google Scholar]
- 18.Gupta RS, Springston EE, Warrier MR, Smith B, Kumar R, Pongracic J, et al. The prevalence, severity, and distribution of childhood food allergy in the United States. Pediatrics. 2011;128(1):e9–17. [DOI] [PubMed] [Google Scholar]
- 19.van der Velde JL, Flokstra-de Blok BM, Vlieg-Boerstra BJ, Oude Elberink JN, DunnGalvin A, Hourihane JO, et al. Development, validity and reliability of the food allergy independent measure (FAIM). Allergy. 2010;65(5):630–5. [DOI] [PubMed] [Google Scholar]
- 20.Kline RB. Principles and Practice of Structural Equation Modeling (2nd Edition ed.): New York: The Guilford Press; 2005. [Google Scholar]
- 21.Xepapadaki P, Fiocchi A, Grabenhenrich L, Roberts G, Grimshaw KE, Fiandor A, et al. Incidence and natural history of hen’s egg allergy in the first 2 years of life-the EuroPrevall birth cohort study. Allergy. 2016;71(3):350–7. [DOI] [PubMed] [Google Scholar]
- 22.Venkataraman D, Erlewyn-Lajeunesse M, Kurukulaaratchy RJ, Potter S, Roberts G, Matthews S, et al. Prevalence and longitudinal trends of food allergy during childhood and adolescence: Results of the Isle of Wight Birth Cohort study. Clin Exp Allergy. 2018;48(4):394–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Vermeulen EM, Koplin JJ, Dharmage SC, Gurrin LC, Peters RL, McWilliam V, et al. Food Allergy Is an Important Risk Factor for Childhood Asthma, Irrespective of Whether It Resolves. J Allergy Clin Immunol Pract. 2018;6(4):1336–41.e3. [DOI] [PubMed] [Google Scholar]
- 24.Tan JW, Joshi P. Egg allergy: an update. J Paediatr Child Health. 2014;50(1):11–5. [DOI] [PubMed] [Google Scholar]
- 25.Tan JW, Campbell DE, Turner PJ, Kakakios A, Wong M, Mehr S, et al. Baked egg food challenges - clinical utility of skin test to baked egg and ovomucoid in children with egg allergy. Clin Exp Allergy. 2013;43(10):1189–95. [DOI] [PubMed] [Google Scholar]
- 26.Capucilli P, Cianferoni A, Fiedler J, Gober L, Pawlowski N, Ram G, et al. Differences in egg and milk food challenge outcomes based on tolerance to the baked form. Ann Allergy Asthma Immunol. 2018;121(5):580–7. [DOI] [PubMed] [Google Scholar]
- 27.Mehta H, Ramesh M, Feuille E, Groetch M, Wang J. Growth comparison in children with and without food allergies in 2 different demographic populations. J Pediatr. 2014;165(4):842–8. [DOI] [PubMed] [Google Scholar]
- 28.Beck C, Koplin J, Dharmage S, Wake M, Gurrin L, McWilliam V, et al. Persistent Food Allergy and Food Allergy Coexistent with Eczema Is Associated with Reduced Growth in the First 4 Years of Life. J Allergy Clin Immunol Pract. 2016;4(2):248–56.e3. [DOI] [PubMed] [Google Scholar]
- 29.Wang J Egg allergy: Management. UpToDate. 2019. [Google Scholar]
- 30.Fleischer DM, Perry TT, Atkins D, Wood RA, Burks AW, Jones SM, et al. Allergic reactions to foods in preschool-aged children in a prospective observational food allergy study. Pediatrics. 2012;130(1):e25–e32. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


