Abstract
OBJECTIVE:
Anterior cervical discectomy and fusion (ACDF) is the most common procedure for the treatment of degenerative cervical conditions. The objective of this study is to determine time-dependent trends in patient outcomes following ACDF for degenerative disease from 2006 to 2016.
METHODS:
We used the National Surgical Quality Improvement Program (NSQIP) database to retrospectively review all patients who underwent elective ACDF between 2006 and 2016. A descriptive statistical analysis followed by time trend analysis was performed on demographics, comorbidities, perioperative, and outcome variables. Primary outcomes were reoperation and readmission rates. Secondary outcomes were medical and surgical complications reported within 30 days of operation.
RESULTS:
A total of 36,854 patients underwent elective ACDF from the 2006 to 2016 NsQIP database. Mean age increased from 48.19 years [standard error: 1.49] in 2006 to 54.08 years [standard error: 0.12] in 2016 (P < 0.001). There was a significantly greater number of outpatient procedures from 2012 to 2016 (P < 0.001). The proportion of patients with American Society of Anesthesiologists classes 3/4 significantly increased over time (P < 0.001, P < 0.001, P = 0.005, respectively). Readmission risk, first documented in NSQIP in 2011, increased over time from 2011 to 2016 (P < 0.001). Unplanned reoperations have remained consistent at about 1.4%. Postoperative complications varied over time with no discernable patterns or trends.
CONCLUSIONS:
Since the establishment of the NSQIP database, there have been no considerable improvements in reoperation or postoperative complication rates based on available data, however, there have been increased rates of readmission. Changes in data collection and an aging patient population with greater burden of comorbidities could confound these trends.
Keywords: Anterior cervical discectomy and fusion, Degenerative spine disease, NSQIP, Outcomes, Readmission, Reoperation, Trends
INTRODUCTION
Operations for degenerative cervical spine disease are among the most common elective surgical operations performed in the United States.1 Anterior cervical discectomy and fusion (ACDF) is the most frequently performed surgery for degenerative cervical disease.2 ACDF, a procedure involving decompression of the spinal cord and fusion between vertebrae to decrease movement, has been shown to decrease symptoms and significantly increase health-related quality of life.2,3 Rates of spinal surgery for cervical disease have been consistently increasing over the last 4 decades.1,4-6 As more individuals continue to undergo these procedures, it is paramount to continuously improve patient outcomes.
Large administrative databases can provide significant patient information and outcome data on surgical trends at a national level. The American College of Surgeons' National Surgical Quality Improvement Program (NSQIP) is a national, outcomes-based and risk-adjusted database designed to measure and improve surgical care.7 The NSQIP database, launched initially for the National Veterans Affairs Surgical Risk Study in 1992, was expanded nationally in 2004, adding novel data points and participating hospitals annually, representing 680 hospitals by the year 2016.8,9 NSQIP provides risk-adjusted 30-day outcomes data, in turn supplying a method for unbiased comparisons between a wide variety of participating hospitals. Ultimately, the main objective of NSQIP is to improve cost efficiency and patient safety for all surgical procedures performed in the United States.9 Studies have revealed a substantial decrease in morbidity and mortality since the development of NSQIP.8 However, despite the significant numbers of studies published on ACDF from the NSQIP database, there is a paucity of literature on the effect that NSQIP has had on ACDF outcomes over time.10-17
The NSQIP database has been fundamental to large-scale, national research. Many studies have specifically analyzed NSQIP to identify factors and related surgical outcomes following ACDF. One of the aims of NSQIP and other national databases is to identify modifiable risk factors that influence rates of readmission and reoperation. When these factors are understood and modified, then there is an opportunity to improve outcomes and rates of readmission in the future. The objective of this study is to determine trends in patient level factors and outcomes, primarily reoperation and readmission following ACDF, since NSQIP has been established in 2006.
MATERIALS
Data Source
The NSQIP database is a nationwide program compiling data on major surgical procedures in both the outpatient and inpatient settings. Patients are selected by billable Current Procedural Terminology (CPT) code and given an International Classification of Diseases, Ninth Revision (ICD-9) and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) code corresponding to the postoperative diagnosis from the operative or pathology reports. Trained surgical clinical reviewers collect data on the perioperative period and up to 30 days after the procedure using a standardized sampling method.18-20 Several variables were added, dropped, or changed in the NSQIP database since its inception. The definitions of ethnicity and race were revised in 2008 to comply with the Centers for Medicare and Medicaid Services and other federal agencies. Data from national participant use files from 2006 to 2016 were compiled and all patients undergoing single or multilevel ACDF were identified. The number of participating sites continues to increase each year; in 2006, a total of 121 health centers reported data, which grew to 680 by 2016. The NSQIP database is publicly available and dei-dentified, thus Institutional Review Board or informed consent were waived.
Patient Selection
We retrospectively reviewed the NSQIP database from 2006 to 2016 for adult patients aged 18–89 years and queried for 5 primary CPT codes: 22551 (Anterior or Anterolateral Approach Technique Arthrodesis Procedures on the Spine [Vertebral Column] single level), 22552 (Anterior or Anterolateral Approach Technique Arthrodesis Procedures on the Spine [Vertebral Column] additional levels), 22554 (Arthrodesis, anterior interbody technique, including minimal discectomy to prepare interspace [other than for decompression]), 22856 (ACDF code prior to 2010), and 63075 (ACDF code prior to 2010). The CPT coding for ACDF changed over the study period. In 2010 and the years prior, the CPT code 63075 was used in concert with 22554 for representing anterior discectomy and subsequent fusion. In 2011, these 2 codes were combined into 1 code: 22551 for first fusion and discectomy level (with code 22552 for additional levels).21 Only patients with ICD-9 or ICD-10 codes appropriate for ACDF in an elective case were evaluated. Cases were excluded if they were emergent; did not provide pertinent demographic data such as sex, height, or weight; or had disseminated cancer. Furthermore, cases undergoing revision surgery or fusion extending to the thoracic, lumbar, or pelvis were excluded: 22800, 22802, 22804, 22808, 22810, 22849, 22850, and 22855.
Independent Variables
Demographic variables, comorbidities, and perioperative variables were analyzed across time. Demographic variables included age, sex, body mass index (BMI), race, and ethnicity. Comorbidities included smoking, ventilator dependency, history of chronic obstructive pulmonary disease, ascites, diabetes, history of cardiac heart failure, use of hypertensive medications, renal failure, dialysis, wound infection, steroids, recent 10% weight loss, bleeding disorder, dyspnea, functional status before surgery, and sepsis. Perioperative variables collected were inpatient versus outpatient procedure, American Society of Anesthesiologists (ASA) class, total operation duration, and total length of hospital stay, as well as symptoms of radiculopathy and myelopathy. Radiculopathy and myelopathy were considered present if respective ICD-10 diagnostic codes were explicitly mentioned.
Outcome Variables
The primary outcome variables were reoperation and readmission within 30 days of surgery. The readmission variable was added in 2011, whereas reoperation was available since the inception of NSQIP in 2006. Although readmission was not reported until 2011, we recognize the importance of tracking this variable and describing the trend with the data available, which is a meaningful time period of 5 years. For readmission, ICD-9 and ICD-10 codes were summarized. Secondary outcome variables included medical and surgical complications within 30-days such as surgical-site infections, dehiscence, pneumonia, reintubation, venous thromboembolism events, failure to wean off of the ventilator within 48 hours, progressive renal insufficiency, acute renal failure, urinary tract infection, stroke or cerebrovascular accident, cardiac arrest requiring resuscitation, myocardial infarction, or requiring transfusion.
Statistical Analysis
IBM SPSS Statistics, Version 24 (IBM Corp., Armonk, New York, USA) was used to perform all statistics. Descriptive statistics are given as either n (%) or mean value ± standard error (SE) where appropriate. Categorical variables were analyzed by the χ2 test and continuous variables were analyzed using analysis of variance. A time trend analysis was performed using the χ2 test for trend and ordinary linear regression, for categorical and continuous variables, respectively. Nonparametric tests, including the Kruskal–Wallis H test and Jonckheere–Terpstra test, were implemented for cell counts less than 10 and non-normally distributed data.
RESULTS
Population Characteristics
A total of 36,854 patients met our inclusion criteria for elective ACDF (Figure 1). Overall, 50.2% of patients were female and the mean age was 53.56 [SE: 0.06] years (Table 1).
Figure 1.
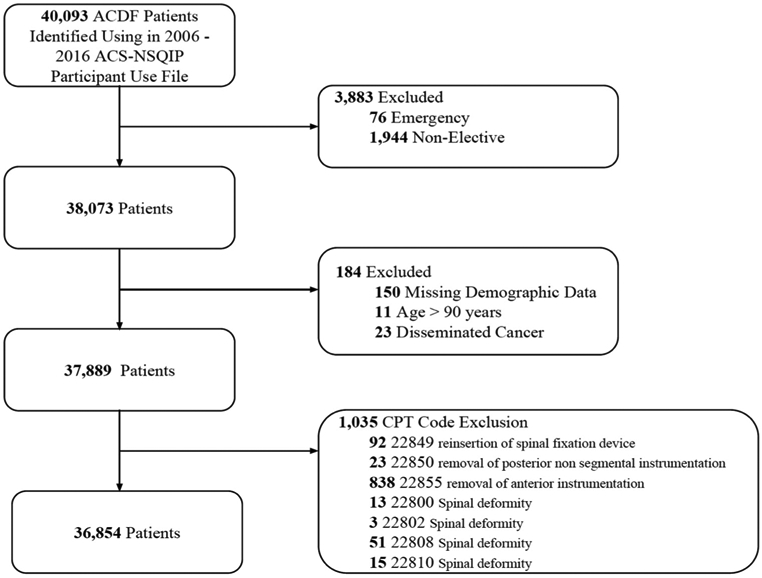
Attrition figure for included patients undergoing ACDF surgery from the 2006 to 2016 ACS-NSQIP database. ACDF, anterior cervical discectomy and fusion; ACS-NSQIP, American College of Surgeons National Surgical Quality Improvement Program database; CPT, Current Procedural Terminology.
Table 1.
Patient Characteristics and Intraoperative Variables in Patients Undergoing ACDF from ACS-NSQIP 2006 to 2016
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | P Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Total ACDF | 31 | 211 | 538 | 848 | 183 | 373 | 3853 | 5725 | 6577 | 8578 | 9937 | |
| Demographics | ||||||||||||
| Age | 48.2 [1.5] | 51.4 [0.8] | 52.5 [0.5] | 52.1 [0.4] | 52.1 [0.9] | 52.7 [0.6] | 53.3 [0.2] | 53.6 [0.2] | 53.3 [0.1] | 53.7 [0.1] | 54.1 [0.1] | <0.001 |
| BMI | 29.4 [1.3] | 29.6 [0.4] | 29.8 [0.3] | 30.0 [0.2] | 30.3 [0.5] | 30.1 [0.4] | 30.3 [0.1] | 30.1 [0.1] | 30.3 [0.1] | 30.4 [0.1] | 30.5 [0.1] | 0.003 |
| Male | 14 (45.2%) | 88 (41.7%) | 250 (46.5%) | 417 (49.2%) | 90 (49.2%) | 195 (57.4%) | 1850 (48.4%) | 2717 (47.7%) | 3289 (50.3%) | 4251 (49.9%) | 2768 (50.4%) | 0.001 |
| Race | <0.001 | |||||||||||
| White | NA | 0 | 395 (73.4%) | 679 (80.1%) | 135 (73.8%) | 268 (10.5%) | 3195 (82.9%) | 4604 (82.2%) | 5338 (81.2%) | 6887 (80.3%) | 7947 (80.0%) | |
| Black | NA | 1 (0.5%) | 54 (10.0%) | 67 (7.9%) | 28 (15.3%) | 56 (15.0%) | 357 (9.3%) | 493 (8.6%) | 615 (9.4%) | 878 (10.2%) | 991 (10.0%) | |
| Asian | NA | 0 | 7 (1.3%) | 5 (0.6%) | 2 (1.1%) | 9 (2.4%) | 61 (1.6%) | 117 (2.0%) | 128 (1.9%) | 172 (2.0%) | 174 (1.8%) | |
| American Indian/Alaska Native | NA | 0 | 16 (3.0%) | 21 (2.5%) | 0 | 0 | 7 (0.2%) | 35 (0.6%) | 64 (1.0%) | 82 (1.0%) | 59 (0.6%) | |
| Native Hawaiian/Pacific Islander | NA | 0 | 0 | 0 | 0 | 1 (0.3%) | 13 (0.3%) | 18 (0.3%) | 35 (0.5%) | 29 (0.3%) | 38 (0.4%) | |
| Ethnicity | <0.001 | |||||||||||
| Hispanic | NA | 0 | 32 (5.9%) | 35 (4.1%) | 9 (4.9%) | 21 (5.6%) | 170 (4.4%) | 239 (4.2%) | 316 (4.8%) | 417 (4.9%) | 465 (4.7%) | |
| Non-Hispanic | NA | 1 (0.5%) | 506 (94.1%) | 813 (95.9%) | 166 (90.7%) | 325 (87.1%) | 3507 (91.0%) | 5183 (90.5%) | 5758 (87.5%) | 7542 (87.9%) | 8583 (86.4%) | |
| Comorbidities | ||||||||||||
| Diabetes (with insulin) | 1 (3.2%) | 8 (3.8%) | 15 (2.8%) | 35 (4.1%) | 14 (7.7%) | 27 (7.2%) | 161 (4.2%) | 269 (4.7%) | 354 (5.4%) | 439 (5.1%) | 539 (5.7%) | <0.001 |
| Current smoker (within 1 year) | 18 (58.1%) | 82 (38.9%) | 183 (34.0%) | 280 (33.0%) | 53 (29.0%) | 114 (30.6%) | 1157 (30.0%) | 1692 (29.6%) | 1831 (27.8%) | 2261 (26.4%) | 2633 (26.5%) | <0.001 |
| Dyspnea | <0.001 | |||||||||||
| Dyspnea with moderate exertion | 8 (25.8%) | 11 (5.2%) | 33 (6.1%) | 38 (4.5%) | 17 (9.3%) | 15 (4.0%) | 235 (6.1%) | 302 (5.3%) | 289 (4.4%) | 379 (4.4%) | 421 (4.2%) | |
| Dyspnea at rest | 0 | 0 | 3 (0.6%) | 1 (0.1%) | 0 | 20 (0.5%) | 20 (0.5%) | 9 (0.2%) | 10 (0.2%) | 14 (0.2%) | 34 (0.3%) | |
| Functional status | 0.054 | |||||||||||
| Partially dependent | 0 | 10 (4.7%) | 10 (1.9%) | 21 (2.5%) | 5 (2.7%) | 10 (2.7%) | 58 (1.5%) | 63 (1.1%) | 72 (1.1%) | 93 (1.1%) | 129 (1.3%) | |
| Totally dependent | 0 | 2 (0.9%) | 2 (0.4%) | 1 (0.1%) | 1 (0.5%) | 0 (0.0%) | 8 (0.2%) | 2 (0.0%) | 6 (0.1%) | 6 (0.1%) | 9 (0.1%) | |
| COPD | 2 (6.5%) | 4 (1.9%) | 16 (3.0%) | 24 (2.8%) | 6 (3.3%) | 10 (2.9%) | 129 (3.4%) | 253 (4.4%) | 282 (4.3%) | 337 (3.9%) | 410 (4.1%) | 0.052 |
| Hypertension requiring medication | 12 (38.7%) | 84 (39.8%) | 226 (42.0%) | 358 (42.2%) | 78 (42.6%) | 157 (42.10%) | 1648 (42.8%) | 2453 (42.8%) | 2847 (43.3%) | 3784 (44.1%) | 4439 (44.7%) | 0.332 |
| On dialysis | 0 | 0 | 0 | 0 | 1 (0.5%) | 3 (0.8%) | 16 (0.4%) | 8 (0.1%) | 13 (0.2%) | 10 (0.1%) | 20 (0.2%) | 0.005 |
| Open wound or wound infection | 0 | 0 | 1 (0.2%) | 1 (0.1%) | 3 (1.6%) | 1 (0.3%) | 17 (0.4%) | 11 (0.2%) | 9 (0.1%) | 21 (0.2%) | 18 (0.2%) | 0.055 |
| Steroid use | 1 (3.2%) | 9 (4.3%) | 11 (2.0%) | 26 (3.1%) | 4 (2.2%) | 20 (5.4%) | 119 (3.1%) | 166 (2.9%) | 183 (2.8%) | 274 (3.2%) | 274 (3.2%) | 0.055 |
| >10% weight loss in <6 months | 0 | 2 (0.9%) | 1 (0.2%) | 7 (0.8%) | 1 (0.5%) | 1 (0.3%) | 4 (0.1%) | 10 (0.2%) | 10 (0.2%) | 10 (0.1%) | 12 (0.1%) | 0.818 |
| Bleeding disorders | 0 | 3 (1.4%) | 4 (0.7%) | 10 (1.2%) | 0 | 5 (1.3%) | 29 (0.8%) | 51 (0.9%) | 64 (1.0%) | 84 (1.0%) | 111 (1.1%) | 0.614 |
| Sepsis | 0.766 | |||||||||||
| SIRS | 1 (3.2%) | 1 (0.5%) | 4 (0.7%) | 3 (0.4%) | 1 (0.5%) | 2 (0.5%) | 6 (0.2%) | 8 (0.1%) | 11 (0.2%) | 15 (0.2%) | 20 (0.2%) | |
| Sepsis | 0 | 0 | 0 | 1 (0.1%) | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Preoperative transfusion RBC | 0 | 0 | 0 | 0 | 1 (0.0%) | 0 (0.0%) | 1 (0.0%) | 0 (0.0%) | 1 (0.0%) | 2 (0.0%) | 0 (0.0%) | 0.943 |
| Inpatient vs. outpatient | <0.001 | |||||||||||
| Inpatient | 22 (71.0%) | 175 (82.9%) | 460 (85.5%) | 719 (84.8%) | 154 (84.2%) | 323 (86.6%) | 2974 (77.2%) | 4347 (75.9%) | 4916 (74.7%) | 6187 (72.1%) | 7012 (70.6%) | |
| Outpatient | 9 (29.0%) | 36 (17.1%) | 78 (14.5%) | 129 (15.2%) | 29 (15.8%) | 50 (13.4%) | 879 (22.8%) | 1378 (24.1%) | 1661 (25.3%) | 2391 (27.9%) | 2925 (29.4%) | |
| Radiculopathy | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 5 | 837 | 3543 | <0.001 |
| Myelopathy | 5 (16.1%) | 75 (35.5%) | 172 (32.0%) | 274 (32.3%) | 174 (95.1%) | 350 (93.8%) | 1111 (28.8%) | 1754 (30.6%) | 2055 (31.2%) | 2454 (28.6%) | 2184 (22.0%) | <0.001 |
| ASA class | <0.001 | |||||||||||
| I: no disturbance | 0 | 20 (9.5%) | 24 (4.5%) | 46 (5.4%) | 13 (7.1%) | 15 (4.0%) | 177 (4.6%) | 241 (4.2%) | 294 (4.5%) | 368 (4.3%) | 402 (4.0%) | |
| II: mild disturbance | 21 (67.7%) | 123 (58.3%) | 327 (60.8%) | 498 (58.7%) | 93 (50.8%) | 214 (57.4%) | 2240 (58.1%) | 3339 (58.3%) | 3760 (57.2%) | 4846 (56.5%) | 5308 (53.4%) | |
| III: severe disturbance | 10 (32.3%) | 59 (28.0%) | 175 (32.5%) | 292 (34.4%) | 75 (41.0%) | 139 (37.3%) | 1366 (35.5%) | 2058 (35.9%) | 2427 (36.9%) | 3231 (37.7%) | 4060 (40.9%) | |
| IV: life threatening | 0 | 8 (3.8%) | 11 (2.0%) | 11 (1.3%) | 2 (1.1%) | 5 (1.3%) | 63 (1.6%) | 75 (1.3%) | 90 (1.4%) | 125 (1.5%) | 154 (1.5%) | |
| Operation time | 143.3 [11.4] | 150.8 [4.7] | 137.5 [3.0] | 130.5 [2.2] | 133.2 [4.4] | 130.8 [3.4] | 124.3 [1.1] | 122.1 [0.9] | 124.3 [0.8] | 124.0 [0.7] | 124.5 [0.7] | 0.003 |
| Hospital variables | ||||||||||||
| Total hospital length of stay | 1.7 [0.3] | 2.1 [0.3] | 1.9 [0.1] | 2.0 [0.1] | 1.9 [0.6] | 6.1 [2.0] | 1.6 [0.1] | 1.4 [0.0] | 1.6 [0.0] | 1.5 [0.0] | 1.5 [0.0] | <0.001 |
| Days from operation to discharge | 1.6 [0.2] | 1.9 [0.2] | 1.7 [0.1] | 1.8 [0.1] | 1.5 [0.6] | 2.1 [0.2] | 1.6 [0.1] | 1.5 [0.0] | 1.5 [0.0] | 1.5 [0.0] | 1.5 [0.0] | <0.001 |
Data are displayed as n (%) or mean [standard deviation].
ACDF, anterior cervical discectomy and fusion; ACS-NSQIP, American College of Surgeons National Surgical Quality Improvement Program database; BMI, body mass index; NA, not available; COPD, chronic obstructive pulmonary disease; SIRS, systemic inflammatory response syndrome; RBC, red blood cell; ASA, American Society of Anesthesiologists.
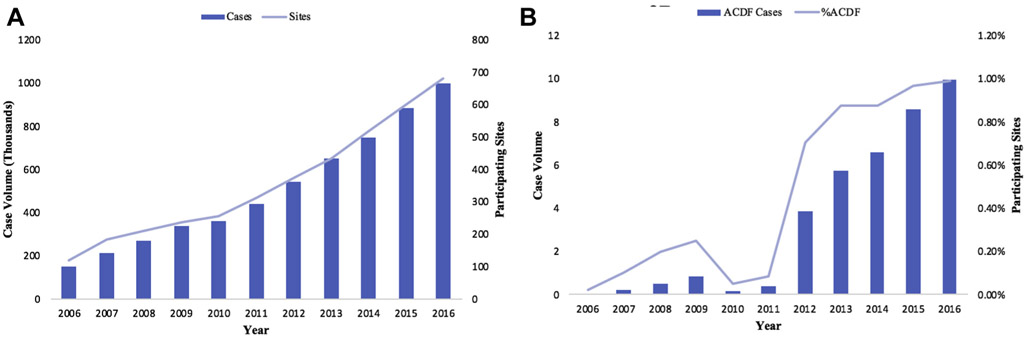
The total number of ACDF procedures significantly increased even when adjusted for total surgical cases reported to NSQIP since 2006 (Figure 2). Over the 11-year period, there were more female patients (P < 0.001) and procedures performed as outpatient surgery, consistently increasing from 2012 to 2016 (P < 0.001). Mean age increased from 48.19 [SE: 1.49] in 2006 to 54.08 [SE: 0.12] in 2016 (P < 0.001). BMI was statistically significantly (P < 0.001) but not clinically relevant (29.4 in 2006 to 30.5 in 2016). Patients reporting symptoms of myelopathy varied significantly across years (P < 0.001). Radiculopathy was based on the ICD-10 code and was first recorded in 2014, with only 5 cases (0.10%) documented as having radiculopathy present in 2014, rising to 3,542 (35.70%) cases in 2016.
Figure 2.
Trends in ACDF procedure volume over time by participating sites from the NSQIP database from 2006 to 2016. (A) Sites indicate number of participating health care sites in the ACS-NSQIP database. (B) %ACDF indicates percentage of procedures coded as ACDF procedures compared with all procedures in the ACS-NSQIP. ACDF, anterior cervical discectomy and fusion; NSQIP, National Surgical Quality Improvement Program database; ACS, American College of Surgeons.
Baseline comorbidity of patients differed throughout the analyzed time period. The number of patients with diabetes was significantly different across years (P < 0.001). The proportion of patients with ASA classes 3 and 4 increased over time (P < 0.001). When stratified by inpatient versus outpatient status, the percentage of patients undergoing inpatient ACDF with low ASA classification (1 and 2) decreased from 80% in 2007 and 66% in 2016, as did those with ASA classification scores of 3 and 4 (88% in 2007 to 76% in 2016, respectively). These trends were significant over the study period (P < 0.05). In addition, more patients had dyspnea at moderate exertion and at rest (P < 0.001) and were on dialysis (P = 0.005) between 2006 and 2016. The proportion of smokers within year of operation significantly decreased between 2006 and 2016 (P < 0.001). The functional status of patients did not worsen over time (P = 0.054).
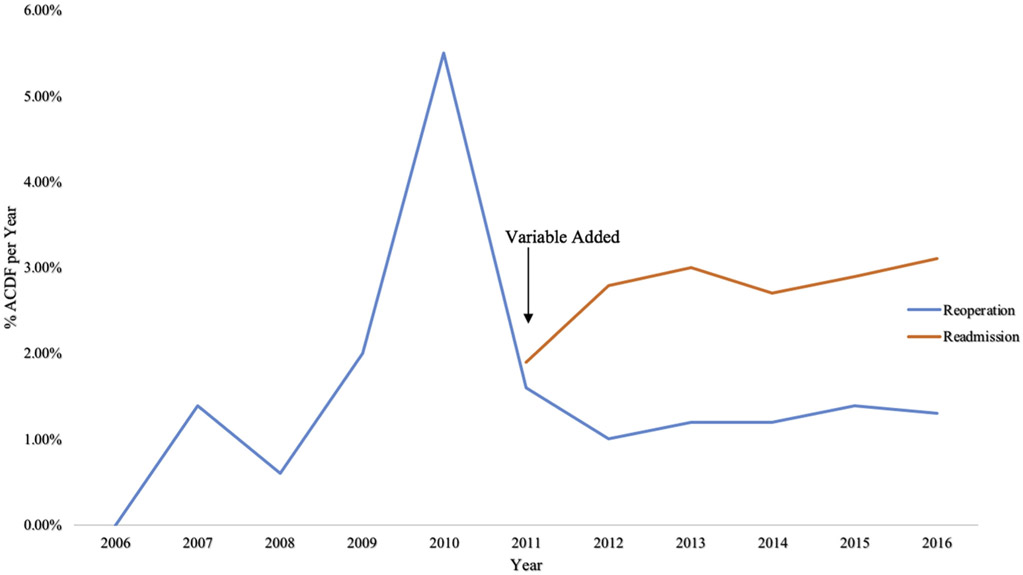
Patient Outcomes
Readmission risk, first documented in NSQIP in 2011, increased slightly from 1.9% to 3.1% from 2011 and 2016 (P < 0.001, Figure 3). By manual entry, the most common readmission causes were pneumonia (n = 66, 0.20%), followed by deep surgical-site infection (n = 29, 0.10%) and pulmonary embolism (n = 25, 0.10%). The most common causes of readmission by ICD-9-CM codes were the following: hematoma complicating a procedure (n = 42, 0.10%), dysphagia (n = 29, 0.10%), and other acute postoperative pain (n = 18, <0.01%). The most common reason for readmission by ICD-10 codes was dysphagia (n = 24, 0.10%). The majority of readmission causes were not reported (manually entry n = 36,103 [98.0%], ICD-9 n = 36,553 [99.2%], and ICD-k n = 36,659 [99.5%]).
Figure 3.
Time trends in reoperation and readmission following ACDF procedure over time from 2006 to 2016. %ACDF per year indicates the percentage of all NSQIP ACDF operations per year. ACDF, anterior cervical discectomy and fusion; NSQIP, National Surgical Quality Improvement Program database.
There were no obvious trends in unplanned reoperations between 2006 and 2016, but the percentage varied over time (P < 0.001, Figure 3). The most commonly documented postoperative diagnoses were intervertebral disc disorders (n = 7850, 21.30%), cervical spondylosis with myelopathy (n = 4512, 12.20%), and spondylosis without myelopathy (n = 4120, 11.20%).
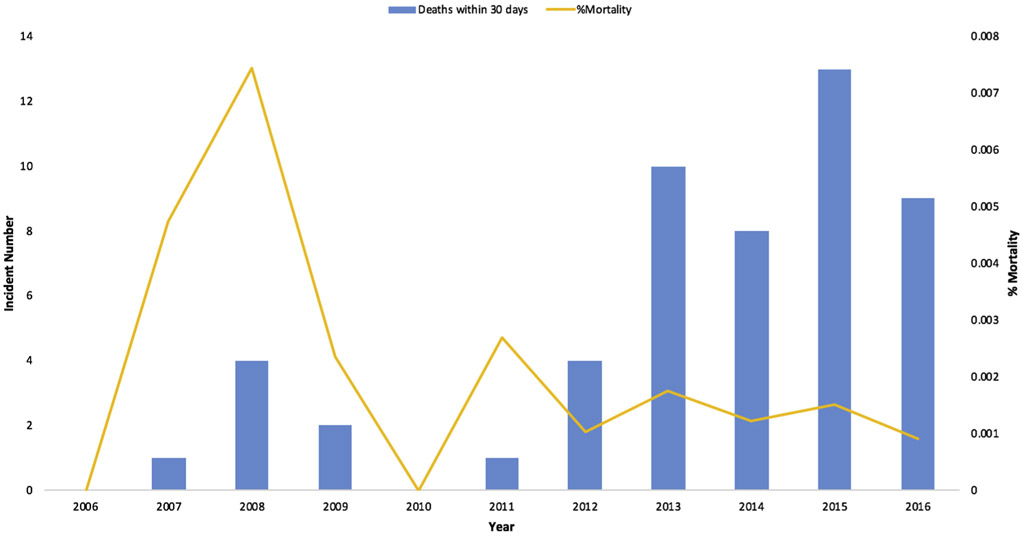
When adjusted for sex, age, inpatient versus outpatient status, and BMI, operation time decreased significantly between 2006 (143.3 ± 63.7 minutes; 95% confidence interval [CI] 119.9–166.6) and 2016 (124.5 ± 65.24 minutes, 95% CI 123.3–125.8, P = 0.009). Length of stay also differed significantly between 2006 (1.7 ± 1.4 days, 95% CI 1.3–2.3) and 2016 (1.5 ± 2.5 days, 95% CI 1.5–1.6) with no clear trends (P < 0.001). There were differences in discharge destination with no discernable trend over time (P < 0.001). There was a total of 52 reported deaths within 30 days of operation over the 11 years (Figure 4).
Figure 4.
Percent mortality and death within 30 days following ACDF over time. %Mortality indicates the percentage of mortality as reported in NSQIP in individuals undergoing ACDF. ACDF, anterior cervical discectomy and fusion; NSQIP, National Surgical Quality Improvement Program database.
Rates of postoperative complications varied throughout the study period but there were no significant differences in failure to wean, defined as on ventilator greater than 48 hours, pulmonary embolism or deep venous thrombosis requiring therapy, pneumonia, progressive renal insufficiency, or urinary tract infections (see Table 2). In addition, there were no significant differences in rates of superficial, deep, or organ space incisional surgical infections, or wound disruption. Between 2006 and 2016, there was also no significant difference in rates of serious medical complications including systemic infections (Table 2).
Table 2.
Outcomes Following ACDF Procedures from ACS-NSQIP 2006–2016
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | P Value | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Unplanned reoperation | 0 | 3 (1.4%) | 3 (0.6%) | 17 (2.0%) | 10 (5.5%) | 6 (1.6%) | 38 (1.0%) | 69 (1.2%) | 80 (1.2%) | 123 (1.4%) | 134 (1.3%) | <0.001 |
| Readmission | NA | NA | NA | NA | NA | 0 | 107 (2.8%) | 169 (3.0%) | 180 (2.7%) | 252 (2.9%) | 309 (3.1%) | <0.001 |
| Superficial SSI | 0 | 2 (0.9%) | 1 (0.2%) | 4 (0.5%) | 1 (0.5%) | 0 | 12 (0.3%) | 14 (0.2%) | 21 (0.3%) | 20 (0.2%) | 33 (0.3%) | 0.623 |
| Deep incisional SSI | 0 | 1 (0.5%) | 0 | 2 (0.2%) | 1 (0.5%) | 0 | 4 (0.1%) | 8 (0.1%) | 9 (0.1%) | 12 (0.1%) | 14 (0.1%) | 0.802 |
| Organ space SSI | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 (0.1%) | 8 (0.1%) | 4 (0.0%) | 10 (0.1%) | 0.564 |
| Wound disruption | 0 | 0 | 0 | 0 | 0 | 0 | 1 (0.0%) | 5 (0.1%) | 5 (0.1%) | 4 (0.0%) | 3 (0.0%) | 0.896 |
| Pneumonia | 0 | 1 (0.5%) | 5 (0.9%) | 6 (0.7%) | 2 (1.1%) | 3 (0.8%) | 21 (0.5%) | 31 (0.5%) | 30 (0.5%) | 37 (0.4%) | 61 (0.6%) | 0.679 |
| Unplanned intubation | 0 | 3 (1.4%) | 2 (0.4%) | 3 (0.4%) | 2 (1.1%) | 5 (1.3%) | 20 (0.5%) | 24 (0.4%) | 26 (0.4%) | 26 (0.3%) | 41 (0.4%) | 0.041 |
| Pulmonary embolism | 0 | 0 | 1 (0.2%) | 2 (0.2%) | 0 | 1 (0.3%) | 8 (0.2%) | 8 (0.1%) | 12 (0.2%) | 12 (0.1%) | 17 (0.2%) | 0.993 |
| Deep vein thrombosis requiring therapy | 0 | 0 | 4 (0.7%) | 2 (0.2%) | 1 (0.5%) | 0 | 6 (0.2%) | 13 (0.2%) | 7 (0.1%) | 17 (0.2%) | 24 (0.2%) | 0.146 |
| On ventilator >48 hours | 0 | 1 (0.5%) | 4 (0.7%) | 4 (0.5%) | 1 (0.5%) | 4 (1.1%) | 9 (0.2%) | 15 (0.3%) | 14 (0.2%) | 22 (0.3%) | 23 (0.2%) | 0.062 |
| Renal failure | 0 | 1 (0.5%) | 0 | 0 | 0 | 0 | 0 | 0 | 4 (0.1%) | 6 (0.1%) | 1 (0.0%) | 0.010 |
| UTI | 0 | 1 (0.5%) | 2 (0.4%) | 5 (0.6%) | 2 (1.1%) | 3 (0.8%) | 14 (0.4%) | 19 (0.3%) | 26 (0.4%) | 41 (0.5%) | 43 (0.4%) | 0.800 |
| Stroke/cerebral vascular incident | 0 | 0 | 1 (0.2%) | 2 (0.2%) | 0 | 0 | 6 (0.2%) | 3 (0.1%) | 6 (0.1%) | 10 (0.1%) | 5 (0.1%) | 0.582 |
| Cardiac arrest | 0 | 0 | 1 (0.2%) | 1 (0.1%) | 0 | 2 (0.5%) | 5 (0.1%) | 7 (0.1%) | 9 (0.1%) | 5 (0.1%) | 8 (0.1%) | 0.360 |
| Myocardial infarction | 0 | 0 | 0 | 1 (0.1%) | 0 | 0 | 6 (0.2%) | 7 (0.1%) | 3 (0.0%) | 11 (0.1%) | 14 (0.1%) | 0.845 |
| Transfusion | 0 | 0 | 0 | 0 | 0 | 4 (1.1%) | 17 (0.4%) | 29 (0.5%) | 12 (0.2%) | 14 (0.2%) | 14 (0.1%) | <0.001 |
| Sepsis | 0 | 1 (0.5%) | 1 (0.2%) | 1 (0.1%) | 1 (0.5%) | 0 | 7 (0.2%) | 9 (0.2%) | 15 (0.2%) | 10 (0.1%) | 17 (0.2%) | 0.780 |
| Septic shock | 0 | 0 | 1 (0.2%) | 0 | 0 | 1 (0.3%) | 0 | 6 (0.1%) | 6 (0.1%) | 4 (0.0%) | 5 (0.1%) | 0.428 |
| Still in hospital >30 days | NA | NA | NA | NA | NA | 0 | 1 (0.0%) | 2 (0.0%) | 1 (0.0%) | 5 (0.1%) | 5 (0.1%) | <0.001 |
| Death | 0 | 1 (0.0%) | 4 (0.0%) | 2 (0.0%) | 0 | 1 (0.0%) | 4 (0.0%) | 10 (0.0%) | 8 (0.0%) | 13 (0.0%) | 9 (0.0%) | 0.017 |
Renal failure is defined as progressive renal insufficiency/acute renal failure requiring dialysis. Cardiac arrest is defined as intraoperative or postoperative cardiac arrest requiring cardiopulmonary resuscitation. Myocardial infarction is defined as intraoperative or postoperative myocardial infarction. Transfusion is defined as red blood cell transfusion within 72 hours surgery start time.
ACDF, anterior cervical discectomy and fusion; ACS-NSQIP, American College of Surgeons National Surgical Quality Improvement Program database; NA, not available; SSI, surgical-site infection; UTI, urinary tract infection.
DISCUSSION
This is the first study to analyze trends of ACDF surgery in the context of the NSQIP database since its inception in 2006. The total number of ACDF surgeries performed in the United States, even when adjusted for the total surgical volume reported to NSQIP, is increasing, which is consistent with current literature.1,4-6 The readmission rates reported in NSQIP have slightly increased over time, and there have been no significant decreases in postoperative complications aside from decreased intraoperative red blood cell transfusions from 2011 to 2016. In contrast to the trend of increasing readmission rates and higher rates of outpatient ACDF procedures identified in this study, based on current literature it might be expected that readmission rates should be decreasing with increased outpatient operations.11,22 We hypothesized that the population selected for outpatient procedures would be expected to have fewer medical comorbidities. We did observe an increase frequency of lower ASA classification scores since the inception of NSQIP, but this this trend did not translate into fewer 30-day readmissions. The lack of improvement could potentially be confounded by severity of patient disease among participating sites as the proportion of patients with ASA 3 and 4 increased overtime from 2006 to 2016, in addition to increased age, which has been shown to be associated with increased risk of readmission.23
In terms of patient selection, there has been a tendency not to operate on patients who are active smokers. In this study, the frequency of current smoking status continues to decrease since 2006. There is more evidence that insurance companies will deny financial coverage for patients who smoke,24 but these finding also can be linked to the association of smoking with increased rates of pseudarthrosis and pulmonary complications that likely influence patient selection.14,25
Our findings also demonstrate an increased rate of outpatient ACDF. This trend can be explained by the safety of outpatient ACDF on select patients11,22,26 and the adoption of outpatient surgery in many centers in conjunction with the evolution of surgery-centers over the past decade.27 Our study demonstrates a trend toward decreased operative time and length of stay. This may be explained by improvement in efficiency and comfort with the surgical technique by the surgeon and the surgical team. Decreased length of stay can be explained by many potential factors, such as early mobilization, increased social work efficiency in placement, and better postoperative pain control.28-30
There is a paucity of data on time trends in patient outcomes from the NSQIP database among patients undergoing elective ACDF surgeries. The NSQIP database, designed to collect and provide data to enhance cost effectiveness and patient safety of surgical procedures, has been shown to effectively improve morbidity and mortality in all surgical procedures at both high-performing and low-performing hospitals over time.8-31 Contrary to these findings, there were no significant improvement trends in surgical outcomes aside from decreased red blood cell transfusion rate over time for patients undergoing ACDF and this may be due to the increase proportion of patients with ASA 3 and 4 undergoing this operation. However, postoperative medical and surgical complications may be underreported in large databases such as NSQIP, especially more minor and indirect surgical complications, therefore limiting interpretation of morbidity associated with ACDF procedures. Moreover, data elements have evolved substantially over time, with new factors being added and removed annually, and therefore the ability to analyze trends is limited. Many studies have published recommendations on methodologies to improve patient care following ACDFs,10-17 but further collective evidence is needed to provide clear recommendations on how to improve patient outcomes.
The NSQIP database has a significant amount of valuable data that provides unique, important information on trends and outcomes of increasingly common procedures such as ACDF. It must be emphasized that NSQIP only consists of direct surgical outcomes and does not aim to directly report on clinical or functional results. However, the lack of substantial improvements that can be inferred from the direct surgical outcomes over time, despite this growing data resource, suggests that although many studies have used this database to reveal insights into surgical outcomes, the application of these findings in clinical practice has been limited. Therefore, to improve patient outcomes and fully use available data, we propose regular review and procedure specific updates on outcomes and trends be reported to these national databases. Ideally, there would be standardized method of reporting that could be compared over time and be made easily accessible to clinicians.
Between 2006 and 2016, the morbidity and mortality associated with ACDF procedures recorded in NSQIP has remained exceedingly small and highly varied. It is likely that the proportion of patients experiencing complications following ACDF maybe small and highly heterogenous that the data elements collected may not generate meaningful insights to guide changes in clinical management. More specific neurosurgical quality improvement and outcome databases would be more useful in guiding interventions that lead to improvements in clinical care, such as the Quality Outcomes Database (https://www.codetechnology.com/n2qod-outcomes-database/). In addition, the majority of readmission causes were not reported, potentially due to being unknown by those submitting the data, further limiting the ability of NSQIP to identify clinically relevant and applicable information to help reduce 30-day readmissions.
This study has several important limitations such as the heterogeneity in the care, record keeping, and management between sites and surgeons, but these variables were not captured in this database. In addition, our primary outcome, readmission, was first recorded in 2011, limiting inference to time of data collection and was subject to small sample bias. In addition, causes for readmission were not reported in the majority of readmission variables, limiting our ability to infer trends on etiologies. Many other factors, such as radiculopathy, relied only on ICD-10 coding and was a recent addition, further limiting disease specific inference. Additionally, adjusting for important confounders in medically complex patients was not performed in this trend analysis.
CONCLUSIONS
Since the establishment of the NSQIP database, the proportion of ACDF surgery to all other NSQIP procedures has increased, yet we did not identify significant trends in reoperation or postoperative complications, except increased readmission risk. Data elements have changed significantly. One of the primary purposes of the NSQIP database is to provide data for study to improve patient safety. Future efforts to more effectively translate NSQIP studies on ACDF procedures to clinical practice is warranted.
Acknowledgments
Conflict of interest statement: Dr. Roxanna Garcia serves as the StrokeNet research fellow under grant U24 NS107233-01 and Fogarty Global Health Trainee. Research reported in this publication was supported by the Fogarty International Center and National Institute of Mental Health, of the National Institutes of Health under award number D43 TW010543. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Abbreviations and Acronyms
- ACDF
Anterior cervical discectomy and fusion
- ASA
American Society of Anesthesiologists
- BMI
body mass index
- CI
Confidence interval
- CPT
Current Procedural Terminology
- ICD-9
International Classification of Diseases, Ninth Revision
- ICD-10
International Statistical Classification of Diseases and Related Health Problems, Tenth Revision
- NSQIP
National Surgical Quality Improvement Program
- SE
Standard error
REFERENCES
- 1.Oglesby M, Fineberg SJ, Patel AA, Pelton MA, Singh K. Epidemiological trends in cervical spine surgery for degenerative diseases between 2002 and 2009. Spine (Phila Pa 1976). 2013;38:1226–1232. [DOI] [PubMed] [Google Scholar]
- 2.Kani KK, Chew FS. Anterior cervical discectomy and fusion: review and update for radiologists. Skeletal Radiol. 2018;47:7–17. [DOI] [PubMed] [Google Scholar]
- 3.Schroeder GD, Boody BS, Kepler CK, et al. Comparing health-related quality of life outcomes in patients undergoing either primary or revision anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2018;43:E752–E757. [DOI] [PubMed] [Google Scholar]
- 4.Gray DT, Deyo RA, Kreuter W, et al. Population-based trends in volumes and rates of ambulatory lumbar spine surgery. Spine (Phila Pa 1976). 2006;31:1957–1963 [discussion: 1964]. [DOI] [PubMed] [Google Scholar]
- 5.Patil PG, Turner DA, Pietrobon R. National trends in surgical procedures for degenerative cervical spine disease: 1990-2000. Neurosurgery. 2005;57:753–758 [discussion: 753-758]. [PubMed] [Google Scholar]
- 6.Davis H Increasing rates of cervical and lumbar spine surgery in the United States, 1979-1990. Spine (Phila Pa 1976). 1994;19:1117–1123 [discussion: 1123-1124]. [DOI] [PubMed] [Google Scholar]
- 7.Jones RS, Brown C, Opelka F. Surgeon compensation: “Pay for performance,” the American College of Surgeons National Surgical Quality Improvement Program, the Surgical Care Improvement Program, and other considerations. Surgery. 2005;138:829–836. [DOI] [PubMed] [Google Scholar]
- 8.Fuchshuber PR, Greif W, Tidwell CR, et al. The power of the National Surgical Quality Improvement Program—achieving a zero pneumonia rate in general surgery patients. Perm J. 2012;16:39–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.McNelis J, Castaldi M. “The National Surgery Quality Improvement Project” (NSQIP): a new tool to increase patient safety and cost efficiency in a surgical intensive care unit. Patient Saf Surg. 2014;8:19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fu MC, Gruskay JA, Samuel AM, et al. Outpatient anterior cervical discectomy and fusion is associated with fewer short-term complications in one- and two-level cases: a propensity-adjusted analysis. Spine (Phila Pa 1976). 2017;42:1044–1049. [DOI] [PubMed] [Google Scholar]
- 11.McGirt MJ, Godil SS, Asher AL, Parker SL, Devin CJ. Quality analysis of anterior cervical discectomy and fusion in the outpatient versus inpatient setting: analysis of 7288 patients from the NSQIP database. Neurosurg Focus. 2015;39:E9. [DOI] [PubMed] [Google Scholar]
- 12.Phan K, Kim JS, Kim JH, et al. Anesthesia duration as an independent risk factor for early postoperative complications in adults undergoing elective ACDF. Global Spine J. 2017;7:727–734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Samuel AM, Fu MC, Toy JO, et al. Most 30-day readmissions after anterior cervical discectomy and fusion are not due to surgical site-related issues: an analysis of 17,088 patients. Spine (Phila Pa 1976). 2016;41:1801–1807. [DOI] [PubMed] [Google Scholar]
- 14.Purvis TE, Rodriguez HJ, Ahmed AK, et al. Impact of smoking on postoperative complications after anterior cervical discectomy and fusion. J Clin Neurosri. 2017;38:106–110. [DOI] [PubMed] [Google Scholar]
- 15.Bhashyam N, De la Garza Ramos R, Nakhla J, et al. Thirty-day readmission and reoperation rates after single-level anterior cervical discectomy and fusion versus those after cervical disc replacement. Neurosurg Focus. 2017;42:E6. [DOI] [PubMed] [Google Scholar]
- 16.Phan K, Kim JS, Lee NJ, Kothari P, Cho SK. Relationship between ASA scores and 30-day readmissions in patients undergoing anterior cervical discectomy and fusion. Spine (Phila Pa 1976). 2017;42:85–91. [DOI] [PubMed] [Google Scholar]
- 17.Gruskay JA, Fu M, Basques BA, et al. Factors affecting length of stay and complications after elective anterior cervical discectomy and fusion: a study of 2164 patients from the American College of Surgeons National Surgical Quality Improvement Project Database (ACS NSQIP). Clin Spine Surg. 2016;29:E34–E42. [DOI] [PubMed] [Google Scholar]
- 18.Khuri SF. The NSQIP: a new frontier in surgery. Surgery. 2005;138:837–843. [DOI] [PubMed] [Google Scholar]
- 19.Khuri SF, Henderson WG, Daley J, et al. Successful implementation of the Department of Veterans Affairs’ National Surgical Quality Improvement Program in the private sector: the Patient Safety in Surgery study. Ann Surg. 2008;248:329–336. [DOI] [PubMed] [Google Scholar]
- 20.Khuri SF, Daley J, Henderson W, et al. The Department of Veterans Affairs’ NSQIP: the first national, validated, outcome-based, risk-adjusted, and peer-controlled program for the measurement and enhancement of the quality of surgical care. National VA Surgical Quality Improvement Program. Ann Surg. 1998;228:491–507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ellis S Surgery Center Coding Guidance: Anterior Cervical Diskectomy and Fusion Procedures. ASC Review. Available at: https://www.beckersasc.com/asc-coding-billing-and-collections/surgery-center-coding-guidance-anterior-cervical-diskectomy-and-fusion-procedures.html Accessed March 25, 2020. [Google Scholar]
- 22.Khalid SI, Adogwa O, Ni A, Cheng J, Bagley C. A comparison of 30-day hospital readmission and complication rates after outpatient versus inpatient 1 and 2 level anterior cervical discectomy and fusion surgery: an analysis of a Medicare patient sample. World Neurosurg. 2019;129:e233–e239. [DOI] [PubMed] [Google Scholar]
- 23.Lovecchio F, Hsu WK, Smith TR, Cybulski G, Kim B, Kim JYS. Predictors of thirty-day readmission after anterior cervical fusion. Spine (Phila Pa 1976). 2014;39:127–133. [DOI] [PubMed] [Google Scholar]
- 24.Lee M, Grossnickle P. On the Oregon Health Authority’s recent ban on elective surgery for smokers with Medicaid: an ethical analysis. J Healthc Ethics Admin. 2017;3:40–50. [Google Scholar]
- 25.Bydon M, De la Garza-Ramos R, Abt NB, et al. Impact of smoking on complication and pseudarthrosis rates after single- and 2-level postero-lateral fusion of the lumbar spine. Spine (Phila Pa 1976). 2014;39:1765–1770. [DOI] [PubMed] [Google Scholar]
- 26.Yerneni K, Burke JF, Chunduru P, et al. Safety of outpatient anterior cervical discectomy and fusion: a systematic review and meta-analysis. Neurosurgery. 2020;86:30–45. [DOI] [PubMed] [Google Scholar]
- 27.Sivaganesan A, Hirsch B, Phillips FM, McGirt MJ. Spine surgery in the ambulatory surgery center setting: value-based advancement or safety liability? Neurosurgery. 2018;83:159–165. [DOI] [PubMed] [Google Scholar]
- 28.Adogwa O, Elsamadicy AA, Fialkoff J, Cheng J, Karikari IO, Bagley C. Early ambulation decreases length of hospital stay, perioperative complications and improves functional outcomes in elderly patients undergoing surgery for correction of adult degenerative scoliosis. Spine (Phila Pa 1976). 2017;42:1420–1425. [DOI] [PubMed] [Google Scholar]
- 29.Bradywood A, Farrokhi F, Williams B, Kowalczyk M, Blackmore CC. Reduction of inpatient hospital length of stay in lumbar fusion patients with implementation of an evidence-based clinical care pathway. Spine (Phila Pa 1976). 2017;42:169–176. [DOI] [PubMed] [Google Scholar]
- 30.Carli F, Kehlet H, Baldini G, et al. Evidence basis for regional anesthesia in multidisciplinary fast-track surgical care pathways. Reg Anesth Pain Med. 2011;36:63–72. [DOI] [PubMed] [Google Scholar]
- 31.Hall BL, Hamilton BH, Richards K, Bilimoria KY, Cohen ME, Ko CY. Does surgical quality improve in the American College of Surgeons National Surgical Quality Improvement Program: an evaluation of all participating hospitals. Ann Surg. 2009;250:363–376. [DOI] [PubMed] [Google Scholar]