To the Editor:
A sudden influx in unplanned intensive care unit (ICU) admissions due to a pandemic or disaster could place substantial strain on the health care system.1–3 Without coordination of resources at the state and national level, an unexpected increase in critical illness could lead to mismatched supply and demand. To better understand the implications of this problem, we evaluated US population-level critical care bed supply.
Methods:
Critical care bed data from the 2007 Centers for Medicare and Medicaid Healthcare Cost Report Information System (HCRIS) were linked to 2007 adult (15 and over) US Census population projections. Critical care beds were defined as any intensive care (including neurological), surgical intensive care, coronary care, or burn unit bed. Population estimates were obtained at the level of the census block group (Claritus, Ithaca NY). Regional boundaries were defined using Dartmouth Atlas Hospital Referral Regions (HRRs). Hospitals and block groups were exactly sited in geographic space by either address (hospitals) or geographic centroids (block groups) and assigned to an HRR if their latitude and longitude fell within HRR borders (ESRI, Redlands CA). For each HRR, the number of critical care beds per 10000 population and the percentage of adult patients with simultaneous critical illness required to exceed regional resources were calculated using a range of potential values as might occur in a severe disaster or pandemic (Stata 11.0, College Station TX). The analysis was repeated categorizing HRRs by tertiles of population density and US census region.
Results
In 2007, there were 4634 acute care hospitals, 3228 of which contained ICU beds, and a total of 67357 critical care beds. The total adult population was 240.6 million, resulting in 2.80 critical care beds per 10000 for the United States as a whole. Within each HRR (N=306), ICU beds ranged from 1.01 to 5.95 per 10000 (Figure), with a median of 2.77 per 10000 (interquartile range, 2.20 – 3.43).
Figure.
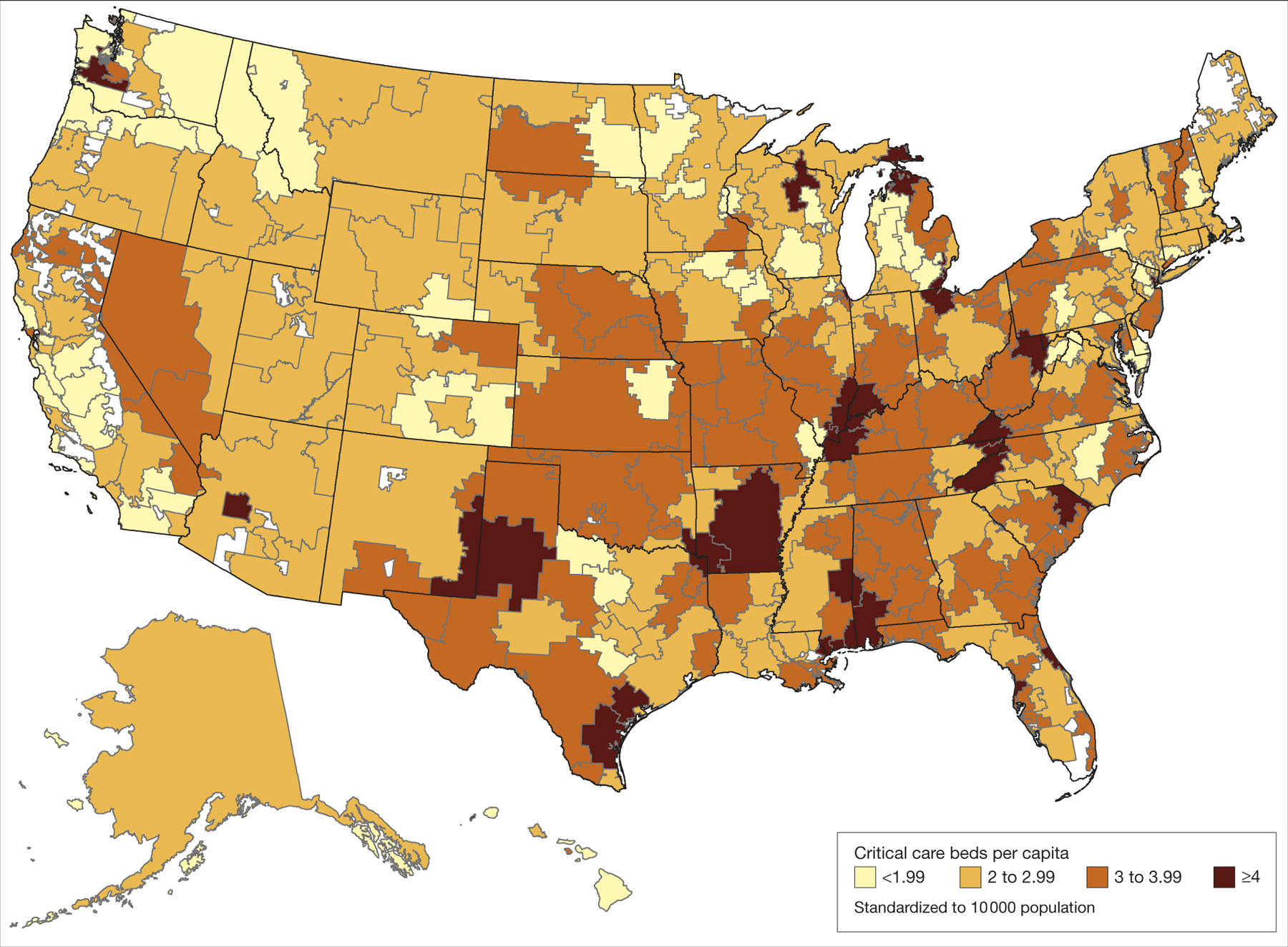
Critical care beds per capita in the United States by Dartmouth Atlas Hospital Referral Region.
A simultaneous episode of critical illness in a small percentage of the population would exceed regional resources in a substantial number of HRRs, with greater effect in high density (more urban) areas and in the northeast and western United States (Table). For reference, 0.02% of the population equals approximately 200 individuals in a city the size of Tampa, Florida (2007 adult HRR population = 1,025,516) or approximately 400 individuals in a city the size of Portland, Oregon (2007 adult HRR population 2,082,544).
Table.
Dartmouth Atlas Hospital Referral Regions (HRRs) exceeding critical care capacity in the event of a sudden surge in critical illnessa
| HRRs exceeding critical care capacity, % | ||||||
|---|---|---|---|---|---|---|
| Percentage of population experiencing sudden critical illness | ||||||
| ICU beds per 10000 population | 0.01 | 0.02 | 0.03 | 0.04 | 0.05 | |
| All HRRs (N=306) | 2.80 | 0 | 16.7 | 58.8 | 90.9 | 97.4 |
| HRRs by population densitya | ||||||
| Lowest tertile (n=102) | 2.97 | 0 | 12.8 | 53.9 | 89.2 | 96.1 |
| Middle tertile (n=102) | 2.84 | 0 | 17.7 | 56.9 | 92.2 | 98.0 |
| Highest tertile (n=102) | 2.71 | 0 | 19.6 | 65.7 | 91.2 | 98.0 |
| HRRs by US Census Regionb | ||||||
| Northeast (n=48) | 2.72 | 0 | 18.8 | 75 | 97.9 | 97.9 |
| Southeast (n=89) | 3.17 | 0 | 2.2 | 37.1 | 83.2 | 96.6 |
| Midwest (n=81) | 2.93 | 0 | 19.8 | 55.6 | 91.4 | 98.7 |
| West (n=88) | 2.45 | 0 | 27.3 | 75 | 94.3 | 96.6 |
Abbreviations: ICU, intensive care unit
Calculated by dividing total 2007 adult population by total HRR area. Lowest tertile = 0.3 to 23.2 adults per km2; middle tertile = 23.2 to 73.4 adults per km2; highest tertile = 75.4 to 9218.7 adults per km2.
HRRs classified into United States Census regions by the state of the primary HRR city from the Dartmouth Atlas.
Comment
There is substantial variability in critical care resources across the United States, and a pandemic or disaster affecting a small proportion of the population could quickly exceed critical care capacity in some areas while leaving resources idle in others. This reflects the limitations of a private health system in which planning occurs primarily from the hospital perspective.
Our study has several limitations. We did not include pediatric hospitals, governmental hospitals (which contain approximately 2% of all ICU beds), or chronic care facilities with ICU capacity, all of which might play a role in a pandemic or disaster; nor could we calculate ventilator-capable beds. Due to the complexity of quantifying critical care capacity, the true number of ICU beds may vary by methodology and study. We could not account for regional or temporal variation in a pandemic or patient transfer outside an HRR.
These results do not necessarily mean that more ICU beds are needed. There is little consensus about the optimal number of ICU beds per capita,4 and overexpansion could lead to long-term inefficiencies. Instead, the findings highlight a need for comprehensive national health care planning to better coordinate critical care capacity across regions,5 echoing the Institute of Medicine’s vision for “coordinated, regionalized, and accountable” emergency care from a population perspective.6
ACKNOWLEGEMENTS
Disclosure: Dr Carr reported receiving grant funding from the National Institutes of Health, the Agency for Healthcare Research and Quality, and the American Heart Association. Dr Kahn reported receiving speaking honoraria from the American Thoracic Society and grant funding from the National Institutes of Health and the Society of Critical Care Medicine. Mr Addyson reported no disclosures.
Funding: Dr Carr is supported by a career development award from the Agency for Healthcare Research and Quality (K08HS017960). Dr Kahn is supported by a career development award from the National Heart Lung and Blood Institute (K23HL082650).
Role of the Sponsors: The sponsors had no role in study design, data collection, analysis or interpretation, or the decision to publish the manuscript.
References
- 1.Kumar A, Zarychanski R, Pinto R, et al. Critically ill patients with 2009 influenza A(H1N1) infection in Canada. JAMA. 2009;302:1872–1879. [DOI] [PubMed] [Google Scholar]
- 2.White DB, Angus DC. Preparing for the Sickest Patients With 2009 Influenza A(H1N1). JAMA. 2009;302:1905–1906. [DOI] [PubMed] [Google Scholar]
- 3.Farmer JC, Carlton PK, Jr. Providing critical care during a disaster: the interface between disaster response agencies and hospitals. Crit Care Med. 2006;34:S56–59. [DOI] [PubMed] [Google Scholar]
- 4.Wunsch H, Angus DC, Harrison DA, et al. Variation in critical care services across North America and Western Europe. Crit Care Med. 2008;36:2787–2793. [DOI] [PubMed] [Google Scholar]
- 5.Barnato AE, Kahn JM, Rubenfeld GD, et al. Prioritizing the organization and management of intensive care services in the United States: the PrOMIS Conference. Crit Care Med. 2007;35:1003–1011. [DOI] [PubMed] [Google Scholar]
- 6.Institute of Medicine. Hospital-based emergency care: at the breaking point. Washington: National Academies Press; 2007. [Google Scholar]


