Abstract
Cardiovascular diseases (CVDs) are a major issue in aging patients with hemophilia (PWHs). Antithrombotic agents are widely used in the general population for CVD treatment, but this recommendation is not fully applicable to PWHs. To improve treatment strategies, a prospective case–control study (COCHE) that analyzed CVD management and follow-up (2 years/patient) in PWHs was performed in France from 2011 to 2018. In total, 68 PWHs (median age: 65 years [39–89]; 48 mild, 10 moderate, and 10 severe hemophilia) were included ( n = 50 with acute coronary syndrome, n = 17 with atrial fibrillation, n = 1 with both). They were matched with 68 control PWHs without antithrombotic treatment. In our series, bleeding was significantly influenced by (1) hemophilia severity, with a mean annualized bleeding ratio significantly higher in COCHE patients than in controls with basal clotting factor level up to 20%, (2) antihemorrhagic regimen (on-demand vs. prophylaxis) in severe (hazard ratio [HR] = 16.69 [95% confidence interval, CI: 8.2–47.26]; p < 0.0001) and moderate hemophilia (HR = 42.43 [95% CI: 1.86–966.1]; p = 0 . 0028), (3) type of antithrombotic treatment in mild hemophilia, with a significantly higher risk of bleeding in COCHE patients than in controls for dual-pathway therapy (HR = 15.64 [95% CI: 1.57–115.8]; p = 0 . 019), anticoagulant drugs alone (HR = 9.91 [95% CI: 1.34–73.47]; p = 0 . 0248), dual antiplatelet therapy (HR = 5.31 [95% CI: 1.23–22.92]; p = 0 . 0252), and single antiplatelet therapy (HR = 3.76 [95% CI: 1.13–12.55]; p = 0 . 0313); and (4) HAS-BLED score ≥3 (odds ratio [OR] = 33 [95% CI: 1.43–761.2]; p = 0 . 0065). Gastrointestinal bleeding was also significantly higher in COCHE patients than in controls (OR = 15 [95% CI: 1.84–268]; p = 0 . 0141). The COCHE study confirmed that antithrombotic treatments in PWHs are associated with increased bleeding rates in function of hemophilia-specific factors and also of known factors in the general population.
Keywords: antithrombotic treatment, atrial fibrillation, cardiovascular disease, hemophilia, bleeding risk
Introduction
Hemophilia management has significantly improved in the last decades. Since the emergence of clotting factor concentrates in the 1970s, 1 the life expectancy of patients with hemophilia (PWHs) has dramatically increased from less than 30 to over 60 years in high-income countries. 2 3 4 5 6 7 8 Consequently, aging PWHs are increasingly confronted with age-related conditions, such as cardiovascular diseases (CVDs), primarily acute coronary syndrome (ACS) and atrial fibrillation (AF).
Antithrombotic treatments, mainly antiplatelet agents, play a central role in secondary CVD prevention. It is now well established that dual antiplatelet therapy (DAPT) with aspirin and P2Y12 inhibitors, such as clopidogrel, is required after drug-eluting stent (DES) implantation. 9 There are also well-defined guidelines for AF management in function of the patient's CHA 2 D 2 -VASc score. This includes the long-term use of anticoagulant drugs, mainly vitamin K antagonists (VKAs) or direct oral anticoagulants (DOAs). 10 In the case of high ischemic/thrombogenic risk, anticoagulant and antiplatelet drugs can be combined. 11 Although these drug combinations are expected to increase the bleeding risk in PWHs, this effect has not yet been demonstrated by studies with high levels of evidence. Evidence-based guidelines for the optimal management of acute CVD in PWHs or for secondary prevention are limited, as well as the published recommendations on how to handle the higher bleeding risk associated with invasive procedures that require hemostasis-interfering drugs. 12 13 14 15
As properly controlled randomized trials are not feasible in PWHs, we set up a case–control study in France to prospectively collect data on the management of coronary artery disease (CAD)/ACS or AF in PWHs, and on the consequences, particularly of antithrombotic treatments, during the 2-year follow-up.
Methods
The COCHE study is a French prospective, noninterventional, multicenter case–control registry. The study was started in July 2011 and data were collected until December 2017. The COCHE group (i.e., the cases) included PWHs A or B who started an antithrombotic treatment for ACS/CAD or for nonvalvular AF, according to the recommendations for CVD management in the general population. For each included patient, a specially designed case report form was filled at inclusion, and then all treatment changes, new cardiovascular events, and bleeding events were recorded in a follow-up form at month 1 after inclusion, and every 6 months for 2 years. The collected data included demographic features and disease characteristics, cardiovascular risk factors and antecedents, ACS/CAD or AF treatment modalities, major and minor bleeding events, and factor replacement therapy before, during, and after any cardiovascular event. According to the International Society on Thrombosis and Haemostasis recommendations, major bleeds were defined as events that required pro-hemostatic substitutive treatment, hospitalization, transfusion, or surgical/radiological interventions. 16 17
The control group included PWHs followed at the Hemophilia Treatment Centre (HTC) of Rennes, France. Each control patient was matched with one patient of the COCHE group on the basis of age (±5 years), hemophilia type and severity (±5 and ± 2% of clotting factor level for mild and moderate forms, respectively), antifactor inhibitor status, and type (on-demand or prophylaxis) of clotting factor replacement therapy (only for patients with severe hemophilia). Data for the control group were retrospectively collected from February 2016 to January 2018, for the same number of months as for the matched case. These data were extracted from the HTC medical file, HTC comprehensive daily board of hospitalization, and each patient's hemophilia diary. This allowed collecting precise information on each clotting factor infusion, hospitalization, and emergency surgery in the control group.
The mean annualized bleeding rates (ABRs) and annualized cardiovascular event rates (ACvR) during the study follow-up were calculated for both groups. For each patient, the sum of all events was divided by the exact number of months (then transformed in years) of follow-up. The mean ABR and ACvR were compared between groups and also within the COCHE group in function of the used antithrombotic treatment, antihemorrhagic regimen (prophylaxis/on-demand), hemophilia severity, clotting factor levels, and HAS-BLED score for patients with AF. Number and causes of death were recorded.
This study did not affect the normal patient management and did not lead to specific treatments or investigations. The physicians' prescribing freedom was entirely maintained. Prior to inclusion, each patient was informed about the registry procedures and provided a written consent. For the study, only anonymized data were used. This study followed the Declaration of Helsinki and local legislation. In accordance with the European and French regulations, this study was approved by the Comité consultatif sur le traitement de l'information en matière de recherche and the Commission nationale informatique et libertés on April 7, 2011 and February 1, 2012, respectively. The registry was supervised by a scientific committee that included both hematologists and cardiologists.
All statistical analyses were performed with the GraphPad Prism software (version 7.00 for Windows, GraphPad Software, La Jolla, California, United States). Categorical variables were expressed as percentages, and continuous variables as means (with lower/upper 95% confidence intervals, CIs) or medians (with minimum and maximum values). The frequency and distribution of bleeding and cardiovascular events were computed with their 95% CI. The Fischer's exact t -test was used for qualitative variables, as appropriate, and odds ratios (ORs) were determined. Hazard ratios (HRs) were used to determine the risk of bleeding from different antithrombotic treatments over time. Significance was set at p < 0.05 with 95% CI. Survival curves were drawn and analyzed using the Mantel–Cox log-rank test that computes also the chi square and HR values, including the 95% CI.
Results
Characteristics of the Study Population
Between July 2011 and December 2017, 68 patients from 26 French HTCs were included in the COCHE registry (see study flowchart in Fig. 1 and Table 1 ). A total of 1,248 months of follow-up data were collected for both COCHE and control groups, corresponding to a median of 18 months (1–24) per patient. The patients' characteristics are described in Table 1 . The reason for inclusion in the COCHE registry was ACS/CAD in 50 (73.5%) patients, AF in 17 (25%) patients, and both in one patient (simultaneous diagnosis at inclusion). Among the 50 patients with ACS/CAD, 22 had ACS (44%) (ST-elevation myocardial infarction n = 3; non-ST-elevation myocardial infarction n = 16; unstable angina n = 3), and 28 (56%) had CAD (stable angina or silent myocardial ischemia). The patient with both AF and ACS/CAD had silent myocardial ischemia without stent implantation. He had mild hemophilia (basal FVIII level: 20%). For the 18 patients with AF, the median CHA 2 D 2 -VASc score was 3 (1–7), and two patients had a score = 1. Their median HAS-BLED score was 2 (0–4). Factor VIII/IX (FVIII/FIX) replacement therapies included only standard concentrates for all patients, but for one who received recombinant activated factor VII due to presence of an anti-FVIII inhibitor. Neither extended half-life (EHL) clotting factor concentrates nor emicizumab was used because they were not available in France during this study.
Fig. 1.
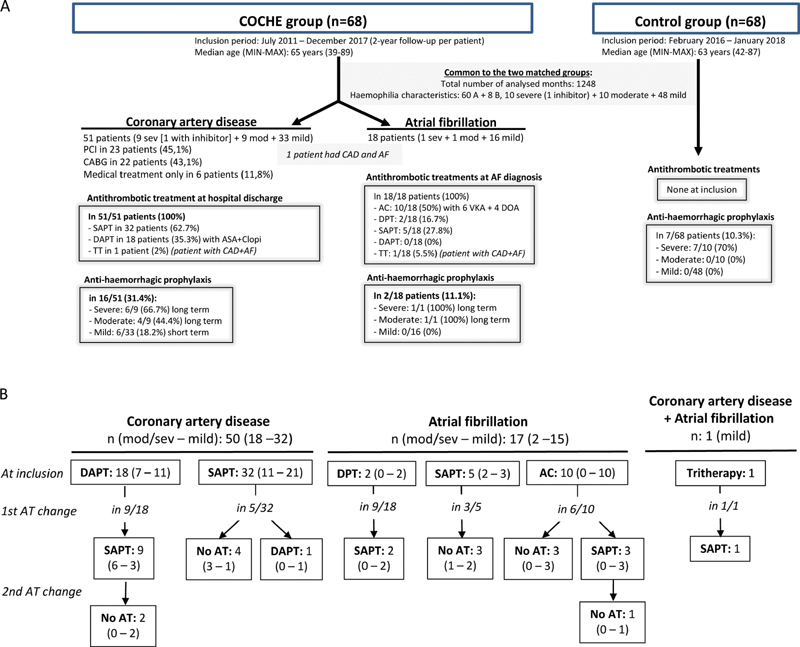
Description of patients and controls included in the COCHE study. ( A ) COCHE study flow chart. ( B ) Changes in antithrombotic treatments during the 2-year follow-up. AC, anticoagulant drug alone; ASA, aspirin; CABG, coronary artery bypass grafting; Clopi, clopidogrel; DAPT, dual antiplatelet therapy; DAPT + one anticoagulant drug; DES, drug-eluting stent; DOA, direct oral anticoagulant; DPT, dual pathway therapy (antiplatelet + anticoagulant); HA, hemophilia A; HB, hemophilia B; mod, moderate; PCI, percutaneous coronary intervention; SAPT, single antiplatelet therapy; sev, severe; TT, triple therapy; VKA, vitamin K antagonist.
Table 1. Characteristics of patients included in the COCHE study.
| COCHE group | Control group | |||||
|---|---|---|---|---|---|---|
| Total | CAD | AF | CAD + AF | |||
| N patients | 68 | 50 | 17 | 1 | 68 | |
| Median age, y [min–max] | 65 [39–85] | 64 [39–85] | 66 [51–75] | 68 | 63 [42–87] | |
| Hemophilia type n patients |
A | 60 | 43 | 16 | 1 | 60 |
| B | 8 | 7 | 1 | 0 | 8 | |
| Hemophilia severity n patients |
Mild Median factor level [min–max] |
48 17% [5–36] |
32 20.5% [5–36] |
15 16% [6–35] |
1 20% |
48 18% [6–37] |
| Moderate Median factor level [min–max] |
10 3% [1–5] |
9 3% [2–5] |
1 (1%) |
0 | 10 3.5% (2–5) |
|
| Severe | 10 1 inhibitor + |
9 1 inhibitor + |
1 | 0 | 10 | |
| Prophylaxis? n patients |
YES | |||||
| Total | 18 (26.5%) | 16 (32%) | 2 (11.8%) | 0 | 6 (8.8%) | |
| Mild | 8 (16.7%) | 8 (17.3%) | 0 | 0 | ||
| Mod/sev | 10 (50%) | 8 (44.4%) | 2 (100%) | 6 (30%) | ||
| NO | ||||||
| Total | 50 (73.5%) | 34 (68%) | 15 (88.2%) | 1 (100%) | 62 (91.2%) | |
| Mild | 40 (83.3%) | 24 (32%) | ||||
| Mod/sev | 10 (50%) | 10 (55.6%) | 15 (100%) 0 |
1 (100%) 0 |
48 (100%) 14 (70%) |
|
Abbreviations: AF, atrial fibrillation; CAD, coronary artery disease; mod/sev, moderate and severe hemophilia.
Antithrombotic Treatments and Antihemorrhagic Prophylaxis
In the COCHE group, antithrombotic treatments were started at diagnosis of ACS/CAD or AF (= inclusion) during hospitalization or consultation ( Fig. 1 ). Two patients stopped the early antithrombotic treatment during the month after inclusion because they had a CHA 2 D 2 -VASc score of 1 (one patient with AF and severe hemophilia) or because silent myocardial ischemia was detected by coronarography (one patient with CAD and mild hemophilia). The initial antithrombotic treatments comprised single antiplatelet therapy (SAPT, n = 37), DAPT ( n = 18), anticoagulant treatment alone (AC, n = 10), dual pathway therapy (DPT) with one antiplatelet and one anticoagulant drug ( n = 2), and triple therapy (TT) in which DPT was associated with another antiplatelet drug ( n = 1) (see Table 1 and Supplementary Table S1 (available in the online version) for the characteristics of the patients with initial DPT and TT). Among the 18 patients with AF, 5 ( n = 3 with mild hemophilia A, FVIII: 13–36%; n = 1 with mild hemophilia B, FIX: 28%; and n = 1 with moderate hemophilia A, FVIII: 1%) received SAPT (aspirin), as previously recommended for PWHs. During the follow-up, in 23 patients ( n = 9 with moderate/severe and n = 14 with mild hemophilia) the initial antithrombotic treatment was changed to another antithrombotic treatment ( n = 13) or completely stopped ( n = 10) ( Table 1 ).
Antihemorrhagic prophylaxis (2–3 infusions per week for FVIII concentrates, or 1–2 infusions per week for FIX concentrates) was performed in 18 patients ( Fig. 1 and Table 1 ). The cumulative duration of prophylaxis was 204 months: 108 months (mean: 11.1 months per patient) in patients with severe, 30 months (mean: 10 months per patient) in patients with moderate, and 66 months (mean: 5.5 months per patient) in patients with mild hemophilia. In patients with severe/moderate hemophilia, prophylaxis ( n = 10) was started after the introduction of the antithrombotic treatment, or was already in place before the CVD diagnosis. Conversely, in patients with mild hemophilia, prophylaxis ( n = 8) was mainly initiated after the occurrence of a bleeding event ( n = 6/8; 75%). The other two patients continued the antihemorrhagic treatment initiated for the cardiovascular procedures during hospitalization. In controls, prophylaxis was only performed in patients with severe hemophilia (6/10, 60%).
Major Bleeding Complications during the Follow-Up
Throughout the follow-up, 100 and 33 bleeding events occurred in the 68 COCHE patients and in the 68 controls, respectively. The number of patients who had at least one major bleeding event was higher in the COCHE group (29/68; 42.6%) than in the control group (14/68; 20.6%). Accordingly, the major bleeding-free survival curves were significantly different between the COCHE and control groups ( Fig. 2A ), and between patients with mild hemophilia from these two groups ( Fig. 2B ). Bleeding events were more frequent in patients receiving antiplatelet therapy (AT) than in controls regardless of the severity of hemophilia and the antithrombotic drug used, as described in Table 2 . The types of major bleeding events in the COCHE group were hemarthrosis ( n = 52; 52%) in 9 patients, hematoma ( n = 30; 30%) in 16 patients, gastrointestinal bleeding (GIB; n = 10; 10%) in 8 patients, and others ( n = 8) in 5 patients. In the control group, the 33 bleeding events were hemarthrosis ( n = 23; 69.7%) in 10 patients, hematoma ( n = 9; 27.3%) in 8 patients, and epistaxis ( n = 1). GIB episodes were significantly more frequent in the COCHE group than in controls (8/68 patients vs. 0/68 patients; OR = 15.00 [95% CI: 1.84–268]; p = 0 . 0141). GIB always occurred during an antithrombotic treatment that included an antiplatelet drug: SAPT ( n = 5 patients), TT ( n = 1 patient), and DAPT ( n = 1 patient). None of the patients with GIB received proton-pump inhibitors (PPIs).
Fig. 2.
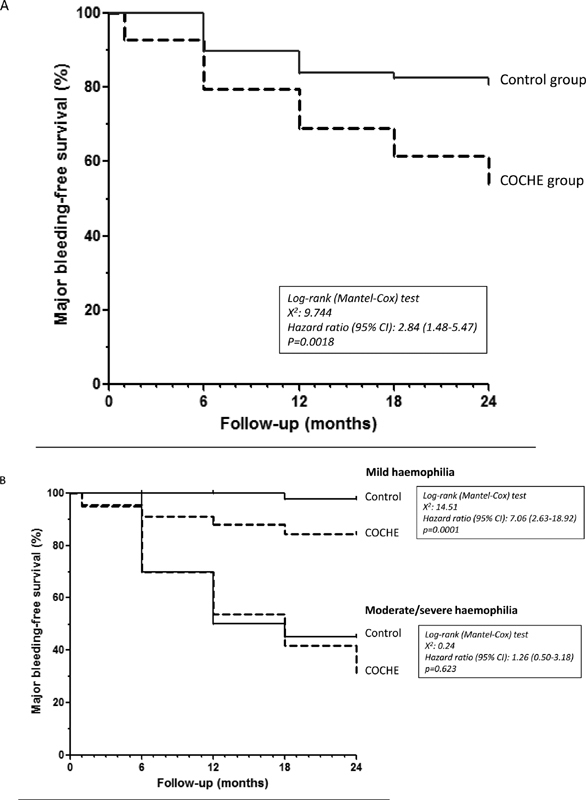
Major bleeding-free survival curves for the COCHE and control groups. ( A ) In all patients. ( B ) In function of hemophilia severity.
Table 2. Influence of antithrombotic treatments on the risk of major bleeding events in patients with hemophilia in the COCHE and control groups.
| Mean ABR (95% CI) | HR for bleeding (95% CI) | p | Cumulative number of analyzed months | n Patients | |
|---|---|---|---|---|---|
| In all patients, whatever the hemophilia severity | |||||
| Control group | 0.317 (0.226–0.408) | 1 | 1,248 | 68 | |
| COCHE total | 0.961 (0.924–0.999) | 2.64 (1.78–3.92) | <0.0001 | 1,248 | 68 |
| With AT | 1.033 (0.996–1.07) | 2.73 (1.82–4.11) | <0.0001 | 1,104 | 68 |
| Without AT a | 0.417 (0.089–0.744) | 1.78 (0.40–7.87) | 0.448 | 144 | 10 |
| In patients with moderate/severe hemophilia | |||||
| Control group | 0.86 (0.77–0.94) | 1 | 426 | 20 | |
| COCHE total | 2.22 (2.10–2.31) | 1.96 (1.21–3.18) | 0.0061 | 426 | 20 |
| With AT | 2.36 (2.17–2.53) | 2.04 (1.23–3.39) | 0.0058 | 372 | 20 |
| -SAPT | 2.76 (2.64–2.88) | 2.05 (1.16–3.62) | 0.0132 | 306 | 18 |
| -DAPT | 4.81 (2.42–13.63) | 5.58 (1.49–20.96) | 0.0109 | 60 | 7 |
| Without AT | 0.889 (0.63–1.15) | 1.52 (0.25–9.12) | 0.6475 | 54 | 4 |
| In patients with mild hemophilia | |||||
| Control group | 0.044 (0–0.09) | 1 | 822 | 48 | |
| COCHE total | 0.336 (0.273–0.432) | 4.93 (2.21–11) | <0.0001 | 822 | 48 |
| With AT b | 0.361 (0.293–0.463) | 4.97 (2.16–11.43) | 0.0002 | 732 | 48 |
| -SAPT | 0.232 (0.177–0.286) | 3.76 (1.13–12.55) | 0.0313 | 472 | 34 |
| -DAPT c | 0.517 (0.324–0.711) | 5.31 (1.23–22.92) | 0.0252 | 116 | 12 |
| -AC | 0.353 (0.01–0.606) | 9.91 (1.34–73.47) | 0.0248 | 102 | 10 |
| -DPT d | 1.143 (0.793–1.492) | 15.64 (1.57–115.80) | 0.019 | 42 | 2 |
| Without AT | 0.133 (0–0.328) | 2.39 (0.15–37.24) | 0.3173 | 90 | 6 |
Abbreviations: ABR, annualized bleeding rate; AC, anticoagulant drug alone; AT, antithrombotic treatment; DAPT, dual antiplatelet therapy; DPT, dual pathway therapy; HR, hazard ratio; SAPT, single antiplatelet therapy.
All 68 patients enrolled in the study started antithrombotic treatment, but 10 discontinued it during the follow-up period.
In this group, only 1 patient received a tritherapy (DAPT + AC) during 6 months, therefore no statistical analysis was performed for this treatment.
The occurrence of bleeding in patients receiving DAPT was significantly higher than in patients with SAPT (HR: 13.12; 95% CI: 2.99–57.48; p = 0.0006).
The occurrence of bleeding in patients receiving DPT was significantly higher than in patients with other antithrombotic treatments (HR: 8.63; 95% CI: 1.41–52.81; p = 0.0198).
In patients with moderate/severe hemophilia receiving an AT (SAPT or DAPT), the risk of bleeding was significantly higher than in controls ( Table 2 ). Furthermore, for severe hemophilia, COCHE patients without prophylaxis had a mean ABR significantly higher than COCHE patients with prophylaxis (6.875 [95% CI: 6.58–7.17] vs. 1.231 [95% CI: 0.966–1.496]; OR = 16.69 [8.20–47.26]; p < 0.0001). However, in COCHE patients with prophylaxis, the mean ABR remained threefold higher than in controls with prophylaxis (1.231 vs. 0.4 [95% CI: 0.031–0.769]; OR = 3.73 [1.11–12.56]; p = 0.0374). The beneficial effect of prophylaxis was also observed in COCHE patients with moderate hemophilia. Indeed, the mean ABR was 0.813 (95% CI: 0.6–1.03) and 0 in patients without and with prophylaxis, respectively (OR = 42.43 [1.86–966.1]; p = 0 . 0028).
In patients with mild hemophilia, more patients reported major bleeding events in the COCHE than in the control group: 17/48 patients (35.4%) and 2/48 patients (4.2%) (OR = 12.61 [95% CI: 2.72–58.52], p = 0 . 0002). The risk of major bleeding events remained high whatever the AT ( Table 2 ). Moreover, within the COCHE cohort, the risk of bleeding was significantly higher for patients taking DAPT than for patients taking SAPT (HR: 13.12; 95% CI: 2.99–57.48, p = 0.0006), and for patients taking DPT than for all other patients taking AT (HR: 8.63; 95% CI: 1.41–52.81; p = 0.0198) ( Supplementary Table S2 , available in the online version). Moreover, the mean ABR was slightly, but not significantly, higher (1.5-fold) in patients treated with AC than in those treated with SAPT. In the SAPT subgroup, the mean ABR values were comparable in patients taking aspirin and clopidogrel (0.273 and 0.2; see Supplementary Table S3 , available in the online version). In the AC group, the mean ABR of patients taking VKA and DOA could not be compared, due to their limited number ( n = 10). In the groups of patients with mild hemophilia and clotting factor levels from 6 to 20%, the percentages of patients with bleeding episodes ( Fig. 3A ) and the mean ABR values ( Fig. 3B ) were significantly higher in COCHE patients with AT but without prophylaxis than in their cross-matched controls. For basal FVIII/FIX levels >20%, no difference was observed between patients receiving an AT and controls.
Fig. 3.
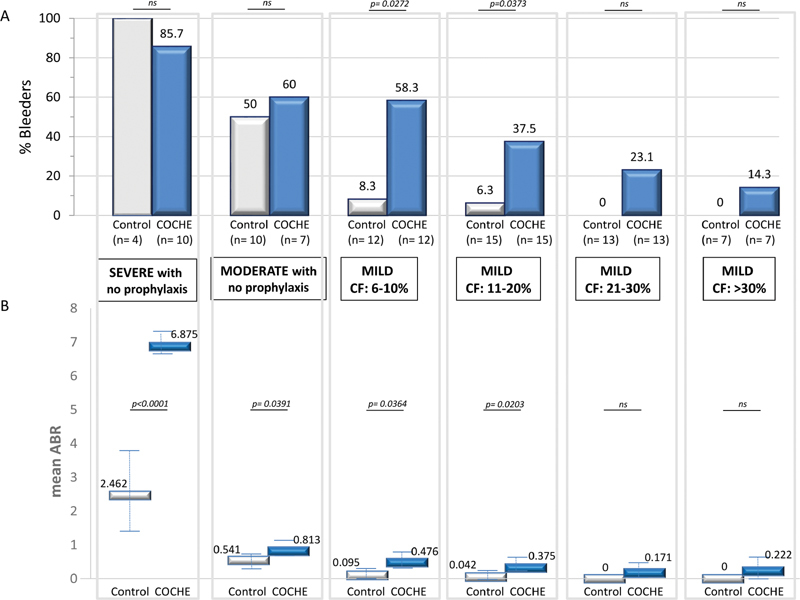
Major bleeding events in function of hemophilia severity and basal clotting factor level. ( A ) Percentage of patients who reported at least one major bleeding episode during the 2-year follow-up period. ( B ) Mean annualized bleeding rate. CF: basal clotting factor; ABR: annualized bleeding rate.
Despite the small number of patients with AF ( n = 18), the number of patients who reported bleeding episodes was significantly higher in patients with HAS-BLED score ≥3 than in those with HAS BLED score <3 (5/8 patients vs. 0/10, respectively; OR = 33 [95% CI: 1.43–761.2]; p = 0 . 0065). The median clotting factor level of patients with HAS-BLED scores ≥3 and <3 was similar (16.5% [1–36] vs. 19.5% [0–34]; p > 0.05) as well as the proportion of patients on prophylaxis (2/8 [25%] vs. 3/10 [30%]; p > 0.05).
Cardiovascular Complications
During the follow-up, a total of 13 cardiovascular events occurred in 11/68 COCHE patients (16.2%) versus only 1 in 1/68 controls (1.5%). This corresponded in COCHE patients to a mean ACvR of 0.125 (95% CI: 0.06–0.19). Cardiovascular event-free survival curves for the COCHE and control groups were significantly different ( Fig. 4 ). These cardiovascular events were ACS, recurrent or at another site ( n = 8), and mesenteric ischemia ( n = 1) in the ACS subgroup; stroke ( n = 1) in the AF subgroup; aortic valve disease aggravation ( n = 1); and cardiac decompensation ( n = 2) soon after inclusion in the patients with ACS and AF. Valve disease aggravation and cardiac decompensation led to death during the first month after inclusion. The mean ACvR was similar in patients with severe (0.121), moderate (0.054), and mild hemophilia (0.143) ( p > 0.05). Prophylaxis with clotting factors did not influence the cardiovascular event occurrence. Indeed, the mean ACvR of COCHE patients was similar during periods of prophylaxis and of on-demand treatment: 0.154 (95% CI: 0–0.381) versus 0.125 (95% CI: 0–0.421) ( p = 1) for patients with severe hemophilia, and 0 versus 0.063 (95% CI: 0–0.196) ( p > 0.05) for individuals with moderate hemophilia.
Fig. 4.
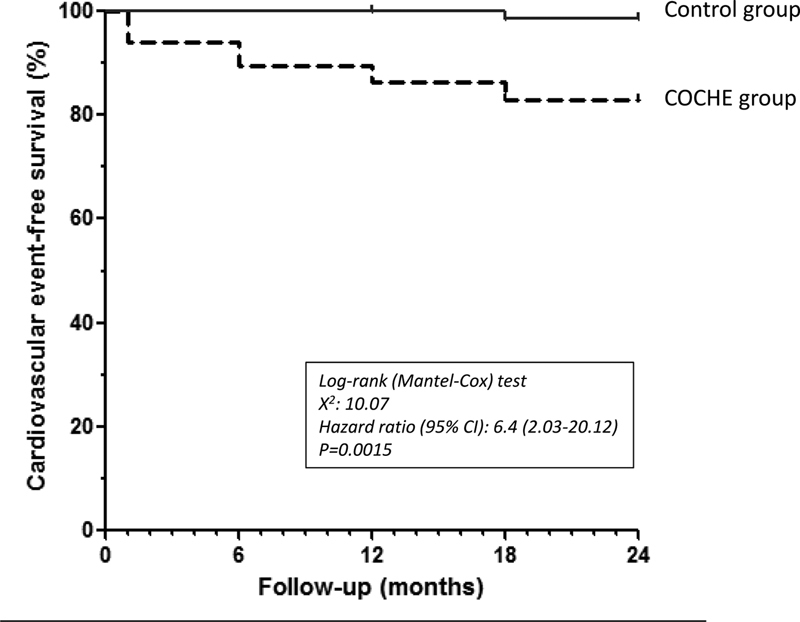
Cardiovascular event-free survival curves for the COCHE and control groups.
Discussion
The COCHE study is the first case–control study to evaluate antithrombotic treatments for CVD management in PWHs. This is also the largest prospective series with a follow-up period of 2 years after treatment initiation. Indeed, up to now, the recommendations and expert opinions were based on small series of PWHs, case reports, and authors' experience. 13 14 15 18 19 20 However, due to their increasing life expectancy, age-related diseases become more frequent in PWHs, including CVDs that require the administration of antithrombotic treatments, like in the general population. 21 22 23 24 Recommendations for CVD management in the general population are reviewed annually by the world's leading scientific societies of cardiology, based on new high-level methodological studies. 25 26 27 28 They now take into account the patient's hemorrhagic profile, whatever the cause, and constitute a major support to guide antithrombotic treatment in PWHs. Therefore, studies in this population are needed to verify or test whether these general recommendations are adapted to their specific condition. Due to the rarity of such situations in a rare hereditary disease, several results need to be confirmed. However some data could help to improve the management of these patients.
The COCHE study confirmed that antithrombotic treatments significantly increase the risk of bleeding in PWHs, regardless of hemophilia severity ( Supplementary Table S4 , available in the online version). Without antithrombotic treatment, the risk of bleeding is correlated with hemophilia severity. 29 This correlation is also observed with antithrombotic treatments. Indeed, the mean ABR progressively increased with hemophilia severity in both control and COCHE patients; however, the difference between groups was significant only up to a basal FVIII/FIX level of 20%. Above this level, the mean ABR tended to be higher in the COCHE group, but bleeding seemed mostly caused by trauma or invasive procedures. Therefore, in patients with mild hemophilia and FVIII/FIX level >20%, earlier substitution therapy after the trauma or a more systematic prophylaxis before invasive procedures (compared with the standard management of patients with mild hemophilia) could effectively prevent bleeding events. As expected, the mean ABR of COCHE patients with severe/moderate hemophilia without prophylaxis was approximately threefold higher than in controls. This result highlights the importance of prophylaxis in these patients as soon as an AT is prescribed and for the entire treatment duration.
In the subgroup of COCHE patients with AF, HAS-BLED scores ≥3 were associated with increased bleeding risk. The HAS-BLED score is an important tool to determine the basal hemorrhagic risk before and during antithrombotic treatment in the general population. 26 In the “Birmingham 3-step therapeutic strategy,” this score is the second step to assess the risk of bleeding and to adapt antithrombotic treatment in patients with AF. Here, we found that the HAS-BLED score is suitable also for PWHs and therefore, the “Birmingham 3-step strategy” could be relevant also for this population.
Over the past years, many studies demonstrated the direct influence of the antithrombotic treatment type on the bleeding risk in the general population. 11 The COCHE study found a similar influence in PWHs. Specifically, DPT was significantly associated with two- to fourfold higher bleeding risk than the other antithrombotic treatments under study. DAPT also increased the risk of bleeding by about twice compared with SAPT. These results are in line with the recommendations for antithrombotic treatments in PWHs that insist on minimizing the prescription of two or more antithrombotic drugs, such as DPT and DAPT, when possible. 13 Therefore, DPT is recommended for patients with nonvalvular AF associated with ACS, for a minimum period of 1 to 3 months, depending on the type of stent implanted (bare metal stent or DES, respectively). 11 28 The stent choice is of primary importance in PWHs. Stents that require the shortest DPT duration should be favored. 13 To reduce the bleeding risk, SAPT might be preferable to DAPT, but in the general population they are associated with higher stroke risk (1.6 times). 11 The data collected in our study do not allow concluding on this point. For PWHs with nonvalvular AF, only ACs are recommended when the CHA 2 D 2 -VASc score is ≥2, like in the general population. 25 26 VKAs are now replaced, with few exceptions, by DOAs that are associated with a twofold lower risk of fatal bleeding. 30 In COCHE patients with mild hemophilia, the bleeding risk was approximately eightfold higher in patients taking AC than in controls. Although only VKA treatment was associated with major bleeding, the COCHE study did not include enough patients treated with AC to conclude on the difference between DOA and VKA in PWHs. For patients with AF and a CHA 2 D 2 -VASc score = 1, the Canadian Cardiovascular Society (CCS) allows the use of SAPT, but only when the HAS-BLED score is high in <65-year-old patients, due to the low levels of evidence. 26 The recommendations published for all PWHs often prioritize SAPT in AF with CHA 2 D 2 -VASc score = 1, but do not take into account age and hemorrhagic score. 13 14 15 18 19 20 In the COCHE study, the small difference in the mean ABR between patients treated with AC and SAPT (∼1.5 times) suggests that both could be used in PWHs with CHA 2 D 2 -VASc = 1. However, when the HAS-BLED score is ≥3 or for patients with severe hemophilia without prophylaxis, SAPT should be preferred (as recommended by CCS).
The COCHE study confirmed that regular prophylaxis effectively protects patients with severe or moderate hemophilia from major bleeding. However, among patients with severe hemophilia receiving prophylaxis, the mean ABR was still threefold higher than among their cross-matched controls also on prophylaxis (1.231 vs. 0.4). PWHs on prophylaxis with standard FVIII concentrates, two to three times per week, have usually a FVIII trough level of 1 to 2%. 31 The same FIX trough level is obtained with standard FIX concentrates administered once or twice per week. These trough levels are certainly insufficient to effectively protect against bleeding events during antithrombotic treatments, and should be increased at least above 5% or even 10%, depending on the antithrombotic treatment type. This suggestion is supported by the mean ABR values between 0.3 and 0.5 observed in our study for mild hemophilia with FVIII/FIX levels of 6 to 10% and 11 to 20%. FVIII/FIX EHL concentrates could help to achieve these trough target levels without increasing the number of infusions. 31 32 33 In the recent guidelines for antithrombotic treatments in PWHs, the minimum FVIII/FIX trough levels for SAPT range from 1 to 5%. 13 14 15 For AC (and DAPT), the recommended FVIII/FIX trough level is ≥30%. It seems difficult to maintain this target in the long term, even with EHL concentrates, because it would require daily injections (for FVIII) or every 2 days (for FIX). In our study, the major bleeding frequency was comparable in COCHE patients with basal FVIII/FIX levels ≥20% and in controls. This threshold could be a more realistic target. In any case, antithrombotic treatment in PWHs should always be combined with a specific education program to alert the patients about the increased risk of bleeding even after a minor trauma. Multidisciplinary management is also required, including information to the cardiologist and family physician.
In our study, gastrointestinal hemorrhages were significantly more frequent in patients taking antithrombotic treatments, namely antiplatelet drugs associated or not with AC, as observed in the general population. 34 In PWHs, gastric protection with PPIs seems necessary as soon as the antiplatelet drugs are started. 35 36 Finally, the COCHE study showed that in PWHs with ischemic or thrombogenic CVD, the risk of a new cardiovascular event was at least sixfold higher than in PWHs without CVD history. Conversely, this risk of cardiovascular recurrence was independent of hemophilia severity and of prophylaxis. Therefore, antithrombotic treatment is indicated in these PWHs and should be implemented according to cardiologic recommendations adapted to hemophilia.
Given the small number of patients enrolled, we acknowledge that our results should be replicated in new studies. Furthermore, although it was a case–control study with prospective inclusion of patients, the comparison with controls who were enrolled retrospectively could potentially generate a bias.
Acknowledgment
The authors would like to thank Hasan Catovic and Diane Bracquart for their assistance in data collection and logistical organization of the COCHE study; co-investigators from the 26 French HTCs; and Elisabetta Andermarcher for her help in editing and rewriting in English.
Funding Statement
Funding The publication was sponsored by CSL Behring, France.
Conflict of Interest None declared.
Authors' Contributions
All authors contributed to the study concept and design. B.G., G.C., and J-F.S. recruited patients, analyzed and interpreted results, and wrote the manuscript. A.L., B.W., C.F., S.C., P.G., and S.C. recruited patients.
Benoît Guillet and Guillaume Cayla contributed equally to the present work.
What is known about this topic?
Age-related cardiovascular diseases (CVDs) are increasing in patients with hemophilia (PWHs) due to their longer life expectancy.
Evidence-based guidelines and medical experience on CVD optimal management in PWHs are limited, especially for antithrombotic treatments.
What does this paper add?
The major bleeding event incidence significantly increases in all PWHs taking antithrombotic treatments.
The major bleeding event incidence is directly related to hemophilia severity, presence/absence of prophylaxis, HAS-BLED score, and antithrombotic treatment type.
Gastrointestinal bleeding events are frequent in PWHs receiving antithrombotic treatments.
PWHs with CVD have an increased risk of additional cardiovascular events.
The risk of cardiovascular event recurrence in PWHs is not influenced by prophylaxis with factor VIII or IX concentrates.
Supplementary Material
References
- 1.Mannucci P M. Back to the future: a recent history of haemophilia treatment. Haemophilia. 2008;14 03:10–18. doi: 10.1111/j.1365-2516.2008.01708.x. [DOI] [PubMed] [Google Scholar]
- 2.Association of Hemophilia Clinic Directors of Canada . Walker I R, Julian J A. Causes of death in Canadians with haemophilia 1980-1995. Haemophilia. 1998;4(05):714–720. doi: 10.1046/j.1365-2516.1998.00179.x. [DOI] [PubMed] [Google Scholar]
- 3.Larsson S A. Life expectancy of Swedish haemophiliacs, 1831-1980. Br J Haematol. 1985;59(04):593–602. doi: 10.1111/j.1365-2141.1985.tb07353.x. [DOI] [PubMed] [Google Scholar]
- 4.Darby S C, Kan S W, Spooner R J. Mortality rates, life expectancy, and causes of death in people with hemophilia A or B in the United Kingdom who were not infected with HIV. Blood. 2007;110(03):815–825. doi: 10.1182/blood-2006-10-050435. [DOI] [PubMed] [Google Scholar]
- 5.Posthouwer D, Yee T T, Makris M. Antiviral therapy for chronic hepatitis C in patients with inherited bleeding disorders: an international, multicenter cohort study. J Thromb Haemost. 2007;5(08):1624–1629. doi: 10.1111/j.1538-7836.2007.02619.x. [DOI] [PubMed] [Google Scholar]
- 6.Ljung R, Petrini P, Lindgren A C, Tengborn L, Nilsson I M.Factor VIII and factor IX inhibitors in haemophiliacs Lancet 1992339(8808):1550. [PubMed] [Google Scholar]
- 7.Hay C R. The epidemiology of factor VIII inhibitors. Haemophilia. 2006;12 06:23–28. doi: 10.1111/j.1365-2516.2006.01362.x. [DOI] [PubMed] [Google Scholar]
- 8.Franchini M, Salvagno G L, Lippi G. Inhibitors in mild/moderate haemophilia A: an update. Thromb Haemost. 2006;96(02):113–118. [PubMed] [Google Scholar]
- 9.Authors/Task Force members . Windecker S, Kolh P, Alfonso F. 2014 ESC/EACTS guidelines on myocardial revascularization: the Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS) developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI) Eur Heart J. 2014;35(37):2541–2619. doi: 10.1093/eurheartj/ehu278. [DOI] [PubMed] [Google Scholar]
- 10.ESC Scientific Document Group . Kirchhof P, Benussi S, Kotecha D. 2016 ESC guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur Heart J. 2016;37(38):2893–2962. doi: 10.1093/eurheartj/ehw210. [DOI] [PubMed] [Google Scholar]
- 11.Andrade J G, Deyell M W, Wong G C, Macle L. Antithrombotic therapy for atrial fibrillation and coronary disease demystified. Can J Cardiol. 2018;34(11):1426–1436. doi: 10.1016/j.cjca.2018.08.028. [DOI] [PubMed] [Google Scholar]
- 12.Cayla G, Morange P E, Chambost H, Schved J F. Management of cardiovascular disease in haemophilia. Thromb Res. 2013;132(01):8–14. doi: 10.1016/j.thromres.2013.05.007. [DOI] [PubMed] [Google Scholar]
- 13.Ferraris V A, Boral L I, Cohen A J, Smyth S S, White G C., II Consensus review of the treatment of cardiovascular disease in people with hemophilia A and B. Cardiol Rev. 2015;23(02):53–68. doi: 10.1097/CRD.0000000000000045. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schutgens R EG, van der Heijden J F, Mauser-Bunschoten E P, Mannucci P M. New concepts for anticoagulant therapy in persons with hemophilia. Blood. 2016;128(20):2471–2474. doi: 10.1182/blood-2016-07-727032. [DOI] [PubMed] [Google Scholar]
- 15.Jabbar A Y, Baydoun H, Janbain M, Ferdinand K C. Current concepts in the management of stable ischemic heart disease and acute coronary syndrome in patients with hemophilia. Ann Transl Med. 2018;6(15):299. doi: 10.21037/atm.2018.05.29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tosetto A, Castaman G, Rodeghiero F. Bleeders, bleeding rates, and bleeding score. J Thromb Haemost. 2013;11 01:142–150. doi: 10.1111/jth.12248. [DOI] [PubMed] [Google Scholar]
- 17.Subcommittee on Control of Anticoagulation of the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis . Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non-surgical patients. J Thromb Haemost. 2005;3(04):692–694. doi: 10.1111/j.1538-7836.2005.01204.x. [DOI] [PubMed] [Google Scholar]
- 18.Mannucci P M, Schutgens R E, Santagostino E, Mauser-Bunschoten E P. How I treat age-related morbidities in elderly persons with hemophilia. Blood. 2009;114(26):5256–5263. doi: 10.1182/blood-2009-07-215665. [DOI] [PubMed] [Google Scholar]
- 19.ADVANCE Working Group . Staritz P, de Moerloose P, Schutgens R, Dolan G. Applicability of the European Society of Cardiology guidelines on management of acute coronary syndromes to people with haemophilia - an assessment by the ADVANCE Working Group. Haemophilia. 2013;19(06):833–840. doi: 10.1111/hae.12189. [DOI] [PubMed] [Google Scholar]
- 20.Martin K, Key N S. How I treat patients with inherited bleeding disorders who need anticoagulant therapy. Blood. 2016;128(02):178–184. doi: 10.1182/blood-2015-12-635094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Triemstra M, Rosendaal F R, Smit C, Van der Ploeg H M, Briët E. Mortality in patients with hemophilia. Changes in a Dutch population from 1986 to 1992 and 1973 to 1986. Ann Intern Med. 1995;123(11):823–827. doi: 10.7326/0003-4819-123-11-199512010-00002. [DOI] [PubMed] [Google Scholar]
- 22.Plug I, Van Der Bom J G, Peters M. Mortality and causes of death in patients with hemophilia, 1992–2001: a prospective cohort study. J Thromb Haemost. 2006;4(03):510–516. doi: 10.1111/j.1538-7836.2006.01808.x. [DOI] [PubMed] [Google Scholar]
- 23.Tuinenburg A, Mauser-Bunschoten E P, Verhaar M C, Biesma D H, Schutgens R E. Cardiovascular disease in patients with hemophilia. J Thromb Haemost. 2009;7(02):247–254. doi: 10.1111/j.1538-7836.2008.03201.x. [DOI] [PubMed] [Google Scholar]
- 24.Sharathkumar A A, Soucie J M, Trawinski B, Greist A, Shapiro A D. Prevalence and risk factors of cardiovascular disease (CVD) events among patients with haemophilia: experience of a single haemophilia treatment centre in the United States (US) Haemophilia. 2011;17(04):597–604. doi: 10.1111/j.1365-2516.2010.02463.x. [DOI] [PubMed] [Google Scholar]
- 25.January C T, Wann L S, Calkins H. 2019 AHA/ACC/HRS focused update of the 2014 AHA/ACC/HRS guideline for the management of patients with atrial fibrillation: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J Am Coll Cardiol. 2019;74(01):104–132. doi: 10.1016/j.jacc.2019.01.011. [DOI] [PubMed] [Google Scholar]
- 26.Proietti M, Lane D A, Boriani G, Lip G YH. Stroke prevention, evaluation of bleeding risk, and anticoagulant treatment management in atrial fibrillation contemporary international guidelines. Can J Cardiol. 2019;35(05):619–633. doi: 10.1016/j.cjca.2019.02.009. [DOI] [PubMed] [Google Scholar]
- 27.ESC Scientific Document Group . Knuuti J, Wijns W, Saraste A. 2019 ESC guidelines for the diagnosis and management of chronic coronary syndromes. Eur Heart J. 2019;00:1–71. doi: 10.1093/eurheartj/ehz425. [DOI] [PubMed] [Google Scholar]
- 28.ESC Scientific Document Group Neumann F J, Sousa-Uva M, Ahlsson A.2018 ESC/EACTS guidelines on myocardial revascularization Eur Heart J 2019400287–165.30165437 [Google Scholar]
- 29.Den Uijl I E, Mauser Bunschoten E P, Roosendaal G. Clinical severity of haemophilia A: does the classification of the 1950s still stand? Haemophilia. 2011;17(06):849–853. doi: 10.1111/j.1365-2516.2011.02539.x. [DOI] [PubMed] [Google Scholar]
- 30.Gómez-Outes A, Lagunar-Ruíz J, Terleira-Fernández A I, Calvo-Rojas G, Suárez-Gea M L, Vargas-Castrillón E. Causes of death in anticoagulated patients with atrial fibrillation. J Am Coll Cardiol. 2016;68(23):2508–2521. doi: 10.1016/j.jacc.2016.09.944. [DOI] [PubMed] [Google Scholar]
- 31.WAPPS co-investigators . Yu J K, Iorio A, Edginton A N. Using pharmacokinetics for tailoring prophylaxis in people with hemophilia switching between clotting factor products: a scoping review. Res Pract Thromb Haemost. 2019;3(03):528–541. doi: 10.1002/rth2.12204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mahlangu J. rFVIIIFC for hemophilia A prophylaxis. Expert Rev Hematol. 2018;11(12):937–943. doi: 10.1080/17474086.2018.1549478. [DOI] [PubMed] [Google Scholar]
- 33.Morfini M, Gherardini S. Pharmacokinetic-based prediction of real-life dosing of extended half-life clotting factor concentrates on hemophilia. Ther Adv Hematol. 2018;9(06):149–162. doi: 10.1177/2040620718774258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fukushi K, Tominaga K, Nagashima K. Gastroduodenal ulcer bleeding in elderly patients on low dose aspirin therapy. World J Gastroenterol. 2018;24(34):3908–3918. doi: 10.3748/wjg.v24.i34.3908. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Szabó I L, Mátics R, Hegyi P. PPIs prevent aspirin-induced gastrointestinal bleeding better than H2RAs. A systematic review and meta-analysis. J Gastrointestin Liver Dis. 2017;26(04):395–402. doi: 10.15403/jgld.2014.1121.264.hra. [DOI] [PubMed] [Google Scholar]
- 36.COMPASS Investigators . Moayyedi P, Eikelboom J W, Bosch J. Safety of proton pump inhibitors based on a large, multi-year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology. 2019;157(03):68200–69100. doi: 10.1053/j.gastro.2019.05.056. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


