Abstract
Rationale
Severe acute respiratory syndrome Coronavirus 2 (SARS CoV-2), the virus that causes COVID-19, and consequent social distancing directives have been observed to negatively impact social relationships but the impact of these changes on the quality of social relationships at a population level has not been explored.
Objective
To evaluate changes in social relationships in a U.S. population sample during a time of social distancing.
Methods
We deployed a matched, longitudinal survey design of the National Institutes of Health Adult Social Relationship Scales to assess the social aspects of emotional support, instrumental support, friendship, loneliness, perceived hostility, and perceived rejection from a time without social distancing (February 2018) to a time where social distancing directives were active (May 2020). Changes in social relationships were compared using paired t-tests, and generalized linear regression models were constructed to identify subpopulations experiencing differential changes in each subdomain of social relationships during social distancing.
Results
Within our sample population, individuals experienced an increased sense of emotional support, instrumental support, and loneliness, and decreased feelings of friendship and perceived hostility during a period of social distancing. Individuals with low self-rated health experienced a decreased sense of emotional support, and females experienced increased feelings of loneliness compared with males.
Conclusions
Social distancing measurably impacts social relationships and may have a disproportionate impact on females and individuals with lower self-rated health. If novel emergent infectious diseases become more commonplace, social interventions may be needed to mitigate the potential adverse impact of social distancing on social relationships.
Keywords: Social relationships, Loneliness, COVID-19, Social distancing, Surveys
1. Introduction
Severe acute respiratory syndrome Coronavirus 2 (SARS CoV-2), the virus that causes COVID-19, has created an international pandemic response to mitigate disease spread, ensure hospital capacity for patients in need of acute care, and prevent death (Lai et al., 2020). Uncertainty over aspects of the illness, including case fatality rate, patient ability to acquire and retain immunity, mechanisms of virus spread, and appropriate prevention measures have government officials implementing “stay-at-home” guidelines and encouraging social distancing between individuals not of the same household (Omer et al., 2020). Governmental mandates and recommendations have closed schools, offices and churches, canceled athletic seasons and leagues, and discouraged social gatherings and events. Each of these components, among others, altered normative social behaviors (Park et al., 2020).
A large amount of research exists on the link between social relationships and emotional and physical health. High levels of social support have been linked to lower likelihood of anxiety and depression (Gariépy et al., 2016; George et al., 1989), enhanced ability to self-manage chronic illness (Lui et al., 2020; Moak and Agrawal, 2010; Rees et al., 2010), and decreased all-cause and disease-specific mortality (Uchino, 2004). The social relationship concepts demonstrated to be associated with health and health outcomes at a population level include: 1) social support defined as the degree to which one views his or her social connections as available to provide support and aid in times of need (S. Cohen, 2004; Cyranowski et al., 2013); 2) companionship defined as the feeling of friendship, kinship, or fellowship through close and enduring social connection (Cyranowski et al., 2013; Thoits, 2011); and 3) social distress defined as experiences of trouble or worry across social connections (Cyranowski et al., 2013; Thoits, 2011). Loneliness, a social relationship construct that can be defined as “a distressing discrepancy between desired and actual levels of social contact” (Rubin, 2017) has been of particular concern during the COVID-19 pandemic. According to the buffering hypothesis, social relationships and social support may have a protective effect against stressful life events, and physical and mental health conditions (L. H. Cohen et al., 1984; S. Cohen, 2004; S. Cohen and Wills, 1985; Uchino, 2004). The general public has experienced a high degree of stress (Park et al., 2020) and differential psychological distress (Devaraj and Patel, 2021) related to the COVID-19 pandemic.
According to the United States (U.S.) Centers for Disease Control and Prevention, the first confirmed case of COVID-19 in the U.S. was reported on January 21, 2020 (Schuchat, 2020). From this first reported case until March of 2020, public health officials observed a rapid spread of the illness hastening the creation of both targeted and community-based mitigation efforts to slow disease transmission (Schuchat, 2020). Mitigation efforts included restrictions on travel to and from places with known high prevalence and incidence of COVID-19, recommendations to limit social events and gatherings, policies to limit or prohibit access to places housing at-risk populations including nursing homes, long-term care facilities, hospitals, and prisons, and directives for “stay-at-home” orders which closed schools and nonessential workplaces (Schuchat, 2020). Controversy exists over the potential impact of “stay-at-home” and social distancing directives on social relationships. Some researchers hypothesize that “stay-at-home” and social distancing measures may increase feelings of loneliness (Banerjee and Rai, 2020; Campbell, 2020), reduce feelings of meaningful daily activity (Campbell, 2020), reduce sense of social and emotional support (Campbell, 2020), and decrease emotional well-being (Frias et al., 2020). Conversely, a social media derived sample of Egyptian adults showed an overall increase in perceived social and family support during the COVID-19 crisis (El-Zoghby et al., 2020), which is similar to other published studies during times of other viral pandemics (El-Zoghby et al., 2020; Zhang and Ma, 2020). Although, the impact of these changes on individual characteristics of social relationships at a population level has not been explored.
In the current study, we sought to determine the changes individuals have experienced in the quality of their social relationships during a time of “stay-at-home” orders requesting social distancing. We utilized a longitudinal survey design during two time periods: a time of typical social interaction (February, 2018) and during “stay-at-home” orders (May, 2020). We deployed a validated survey toolkit (the National Institutes of Health (NIH) Adult Social Relationship Scales) to assess the changes respondents experienced across the domains of emotional support, instrumental support, friendship, loneliness, perceived hostility, and perceived rejection. We explored demographic factors associated with reported changes in the quality of social relationship constructs during the social distancing orders (2020) compared to responses during a time of typical social interaction (2018). Our analyses were exploratory in nature, but we did anticipate that subpopulations within our study may be experiencing differential changes in the domains of social support. We anticipated that we might observe changes by respondent age, gender, marital status, race, highest level of educational achievement, and self-rated health. Our findings may have implications for the development of targeted social interventions to mitigate the potential harmful effects of social distancing on social well-being.
2. Methods
2.1. Study overview
The present study was a matched, longitudinal survey of individuals who received care at one of our three main sites (Jacksonville, Florida; Rochester, Minnesota; Scottsdale, Arizona). The first survey assessment was performed in February of 2018, with a second wave of measures collected during the time of “stay-at-home” orders due to COVID-19 in May of 2020. An electronic survey tool was deployed via Qualtrics® survey software (Provo, UT). All survey responses were anonymous to the research team. This study was reviewed and approved by the Mayo Clinic Institutional Review Board (IRB).
2.2. Study population
Access to our sample population emerges from our management of patient populations for their primary, secondary, and tertiary healthcare needs. Upon becoming a patient with one of our providers, patients elect to provide contact information, including E-mail address, as well as authorization to participate in research studies as part of their registration process. We sampled individuals who received care at one of our three main Mayo Clinic campus locations in the 12 months before sampling (October 20, 2018) for participation if they met the following criteria: provided consent for participation in passive research according to the State of Minnesota policy, were between the ages of 18 and 85 years at the time of sampling and had an E-mail address in our registration files. Individuals could be under the care of our organization for any reason or condition, or be part of our primary care, longitudinal care population, and individuals did not have to be under active treatment or care by a member of our organization to be included within our sampled population. Individuals were excluded if they were identified as deceased at the time of survey sampling, or before the second survey round, if they had a diagnosis of memory impairment on file according to our medical record, or if they resided within a nursing home or hospice facility at the time of sampling. Individuals received a second wave survey if they had completed our initial survey in 2018.
2.3. Measures
Our primary measure was the NIH Adult Social Relationship Scales (Cyranowski et al., 2013) assessing multiple aspects of social relationships (Appendix 1 ). The NIH Social Relationship Scales are a series of brief, self-report assessments of three domains of social support, companionship, and social distress with six subdomains: 1) social support assessed with emotional (8 items; Example item: “I have someone who understands my problems.”) and instrumental support (8 items; Example item: ”Someone is around to make my meals if I am unable to do it myself.”); 2) companionship assessed with friendship (8 items; Example item: “I get invited to go out and do things with other people.”) and loneliness (5 items; Example item: “I feel alone and apart from others.”); and 3) social distress assessed with perceived rejection (8 items; Example item: “Please rate how often people in your life don't listen when (you) ask for help.”) and perceived hostility (8 items; Example item: “Please rate how often people in your life argue with (you).”). There are a total of 45 individual survey items across the six survey subdomains. Assessment within each domain requests the respondent to reflect on each concept “in the past month” and to rate their experience on 5-point Likert-scales. We selected this suite of tools as they were specifically designed to provide unidimensional subdomain scores with reasonable conceptual coverage of the domain concept (Cyranowski et al., 2013).
To score the Social Relationship Scales, each subdomain was scored independently by summing individual responses across the survey items contained within the subdomain, then calculating an average across the subdomain scores by dividing by the number of questions completed by the survey respondent. Cronbach's α was calculated within each subdomain to understand internal consistency of the measure. Each subdomain demonstrated high internal consistency (α range: 0.93–0.97).
Within our initial survey wave (2018), we also collected demographic information from respondents (age, gender, race, marital status, highest level of education). At that time, we requested that respondents indicate whether they have anxiety, depression, or other mental health conditions by asking “Has a doctor or other healthcare provider ever told you that you have [anxiety, depression, bipolar disorder, schizophrenia, personality disorder, other mental health condition]” with response options of “Yes/No/I don't know.” Since individuals with serious mental illness experience emotional distress differently than the general population (Hamada and Fan, 2020), individuals with self-reported bipolar disorder, schizophrenia, personality disorder, or other mental health condition were excluded (n = 83). We also asked respondents to provide a current assessment of their health as “I would rate my health to be …” with response options of “Very Good/Good/Average/Fair/Poor.” Demographic and information on mental health concerns were not reassessed in the 2020 survey wave.
2.3.1. Missing data
We assessed for two forms of missing data: attrition of individuals from the initial wave of our survey to the second survey wave, and non-response to the individual survey items within the NIH Social Relationship Scale tools. To assess for bias due to attrition, we evaluated the demographic characteristics of those who responded to our second survey wave to those who responded to our initial survey wave (Table 1 ). Overall, 50.9% of those who responded to our initial survey wave also participated in our second survey wave. Our two populations differed significantly based on age group, marital status, race, highest level of education achieved, and self-rated health status. We were not able to statistically correct these differences within our findings, which we mention as a limitation within our study.
Table 1.
Demographic characteristics of responders by survey response waves.
| Response in Wave 1 Only (N = 1922) | Responses in Waves 1 and 2 (N = 1996) | Total (N = 3918) | p-value | |
|---|---|---|---|---|
| Age Group, No. (%) | <0.0001 | |||
| 18-30 | 185 (9.6%) | 84 (4.2%) | 269 (6.9%) | |
| 31-40 | 215 (11.2%) | 177 (8.9%) | 392 (10.0%) | |
| 41-50 | 254 (13.2%) | 220 (11.0%) | 474 (12.1%) | |
| 51-60 | 452 (23.5%) | 414 (20.7%) | 866 (22.1%) | |
| 61-70 | 435 (22.6%) | 584 (29.3%) | 1019 (26.0%) | |
| 71+ | 381 (19.8%) | 517 (25.9%) | 898 (22.9%) | |
| Gender, No. (%) | 0.2529 | |||
| Female | 1247 (64.9%) | 1260 (63.1%) | 2507 (64.0%) | |
| Male | 675 (35.1%) | 736 (36.9%) | 1411 (36.0%) | |
| Marital Status, No. (%) | <0.0001 | |||
| Divorced/Separated | 152 (7.9%) | 133 (6.7%) | 285 (7.3%) | |
| Married/Life Partnership | 1401 (72.9%) | 1545 (77.4%) | 2946 (75.2%) | |
| Single | 299 (15.6%) | 222 (11.1%) | 521 (13.3%) | |
| Unknown | 2 (0.1%) | 2 (0.1%) | 4 (0.1%) | |
| Widowed | 55 (2.9%) | 90 (4.5%) | 145 (3.7%) | |
| Missing | 13 (0.7%) | 4 (0.2%) | 17 (0.4%) | |
| Race, No. (%) | <0.0001 | |||
| American Indian/Alaskan Native | 1 (0.1%) | 3 (0.2%) | 4 (0.1%) | |
| Asian | 45 (2.3%) | 27 (1.4%) | 72 (1.8%) | |
| Black/African American | 22 (1.1%) | 7 (0.4%) | 29 (0.7%) | |
| Hawaiian/Pacific Islander | 4 (0.2%) | 0 (0.0%) | 4 (0.1%) | |
| Other | 53 (2.8%) | 27 (1.4%) | 80 (2.0%) | |
| White | 1797 (93.5%) | 1932 (96.8%) | 3729 (95.2%) | |
| Highest Education Achieved, No. (%) | <0.0001 | |||
| High School or less | 165 (8.6%) | 147 (7.4%) | 312 (8.0%) | |
| Some college/Associate's degree | 549 (28.6%) | 521 (26.1%) | 1070 (27.3%) | |
| College degree | 513 (26.7%) | 583 (29.2%) | 1096 (28.0%) | |
| Post-College degree | 435 (22.6%) | 573 (28.7%) | 1008 (25.7%) | |
| Missing | 260 (13.5%) | 172 (8.6%) | 432 (11.0%) | |
| Self-Rated Health, No. (%) | <0.0001 | |||
| Very Good | 441 (22.9%) | 630 (31.6%) | 1071 (27.3%) | |
| Good | 810 (42.1%) | 911 (45.6%) | 1721 (43.9%) | |
| Average | 328 (17.1%) | 275 (13.8%) | 603 (15.4%) | |
| Fair | 208 (10.8%) | 135 (6.8%) | 343 (8.8%) | |
| Poor | 69 (3.6%) | 21 (1.1%) | 90 (2.3%) | |
| Missing | 66 (3.4%) | 24 (1.2%) | 90 (2.3%) | |
Additionally, we assessed for non-response to individual survey items within our main outcome measure, the NIH Social Relationship Scale tools. Non-response to the subdomains of the NIH Social Relationship Scale was low across our two survey waves (range 5.5%–12.2%). Only gender, education, and self-rated health were associated with the missingness with our outcomes. This information led us to believe that our data are missing at random and to use list-wise deletion of any respondents where we were unable to calculate a subdomain-level score. Respondents were included within each subdomain-level analysis where they had at least 80% of responses in both the 2018 and 2020 survey waves. These approaches are in alignment with Sidi and Harel (2018) who indicate that it is unlikely to improve the accuracy of our findings through imputation of missing data in this scenario (Sidi and Harel, 2018).
2.4. Statistical analyses
2.4.1. Study population
Descriptive statistics for our sample population were calculated as counts (n) and simple proportions (%), with missing items reported as missing. Bivariate analyses were completed using a χ2 test for Independence and Student's t-tests as appropriate. Violations of assumptions of each test type defaulted to Fischer Exact test and Wilcoxon Rank Sum test. Differences were considered significant if p < 0.01.
2.4.2. Changes in social relationships during social distancing
To detect differences in social relationship quality between our baseline period (2018) and during social distancing (2020), sample means of each social relationship subdomain between the time periods were compared using paired t-tests. We sought to explore associations in either direction (two-tailed) and considered findings statistically significant if p < 0.01.
2.4.3. Individual characteristics and changes in social relationships during social distancing
To understand if different subpopulations experienced differential changes in social relationship quality between 2018 and 2020, we constructed generalized linear models of demographic factors against a change in subdomain score between wave 1 and wave 2 in either direction. After verifying for normality of residuals, we calculated estimates, standard errors and root mean squared errors (RMSE). Factors were considered significant if p < 0.05 and RMSE>0.5.
All data management and statistical analyses were performed using Statistical Analysis Software (SAS) version 9.4 (Cary, NC).
3. Results
3.1. Study population
We had 1996 individuals complete both our 2018 and 2020 survey waves who were included within our study population (retention rate = 50.9%, 1996/3918). Our sample population had an average age of 60 years (standard deviation (SD) = 14.5) and our non-responders had an average age of 55 years (SD = 16.4). Our sample was predominantly female (63%), were in a lifetime relationship (77%), were White (97%), had a college degree or higher (58%), and were of “Good” (46%) or “Very Good” (32%) self-rated health (Table 1). Our retained sample population significantly differed from our non-responding population based on age, marital status, race, highest level of education achieved, and self-rated health status.
3.2. Changes in social relationships during social distancing
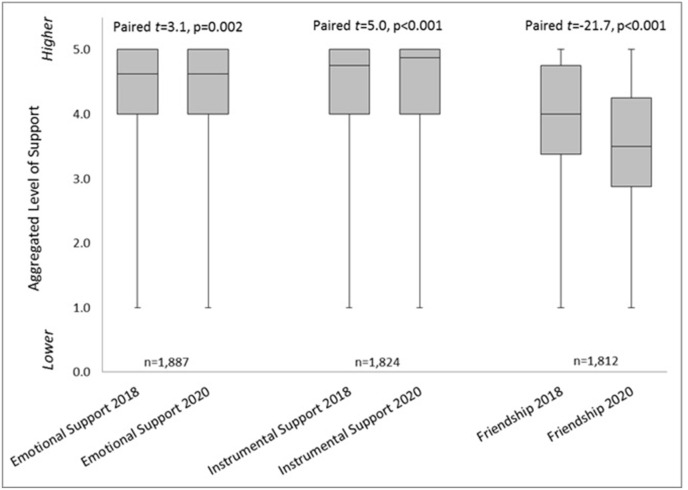
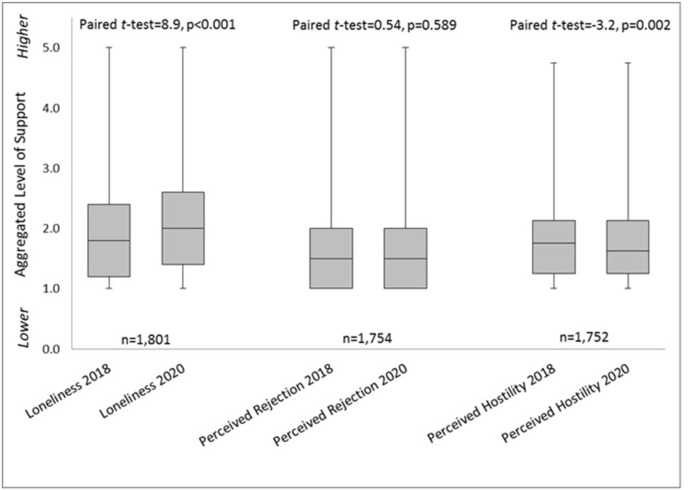
Across our sample population, we observed significant differences in all social relationship subdomains except perceived rejection (Fig. 1 , Fig. 2 ). We observed increases in mean emotional support (2018 mean = 4.3 ± 0.7; 2020 mean = 4.4 ± 0.7; paired t = 3.1, p = 0.002), instrumental support (2018 mean = 4.3 ± 0.9; 2020 mean = 4.4 ± 0.9; paired t = 5.0, p < 0.001), and feelings of loneliness (2018 mean = 1.8 ± 0.8; 2020 mean = 2.0 ± 0.8; paired t = 8.9, p < 0.001). We observed decreases in mean friendship (2018 mean = 3.9 ± 0.9; 2020 mean = 3.5 ± 0.9; paired t = 21.7, p < 0.001) and perceived hostility (2018 mean = 1.8 ± 0.6; 2020 mean = 1.7 ± 0.6; paired t = 3.2, p = 0.002). We did not observe a change in mean perceived rejection between the survey waves (2018 mean = 1.6 ± 0.7; 2020 mean = 1.6 ± 0.7; paired t = 0.54, p = 0.589).
Fig. 1.
Reported changes in social relationship quality for social relationship scales subdomains of emotional support, instrumental support, and friendship (n=1,682). Mean scores are depicted by the grey bar and are written within the bar, and the vertical lines represent standard deviations.
Fig. 2.
Reported changes in social relationship quality for Social Relationship Scales subdomains of Loneliness, Perceived Rejection and Perceived Hostility (n=1,682). Boxes depict 25th quartile, median, and 75th quartile of aggregated social relationship score. Bars represent minimum and maximum measures observed by the group.
3.3. Individual characteristics and changes in social relationships during social distancing
Among our sample population, we observed that those reporting ‘poor’ self-rated health experienced a decreased sense of emotional support compared with those reporting ‘very good’ health (estimate = −0.32, SE = 0.13, p = 0.02) (Table 2 , Table 3 ). We also observed that individuals identifying as ‘widowed’ experienced an increased sense of instrumental support compared to those identifying in a ‘life partnership or married’ (estimate = 0.21, SE = 0.09, p = 0.02), and that those identifying as ‘Black/African American’ experienced an increased sense of instrumental support compared with those identifying as ‘White’ (estimate = 0.66, SE = 0.32, p = 0.04). We did not observe any individual subpopulations of our sample reporting a significant change in the feelings of friendship.
Table 2.
Relationship Between Respondent Characteristics and Change in NIH Social Relationship Scale subdomains of Emotional Support, Instrumental Support, and Friendship.
| Emotional Support |
Instrumental Support |
Friendship |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | p-value | RMSE | Estimate | SE | p-value | RMSE | Estimate | SE | p-value | RMSE | ||
| Age Group | 0.63 | 0.79 | 0.78 | ||||||||||
| 18-30 | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| 31-40 | −0.05 | 0.08 | 0.57 | 0.02 | 0.02 | 0.88 | −0.13 | 0.11 | 0.24 | ||||
| 41-50 | −0.06 | 0.08 | 0.45 | −0.11 | −0.11 | 0.31 | −0.01 | 0.10 | 0.92 | ||||
| 51-60 | 0.01 | 0.08 | 0.90 | −0.02 | −0.02 | 0.87 | −0.07 | 0.10 | 0.49 | ||||
| 61-70 | 0.11 | 0.07 | 0.14 | 0.03 | 0.03 | 0.78 | −0.04 | 0.10 | 0.68 | ||||
| 71+ | 0.04 | 0.07 | 0.63 | −0.10 | −0.10 | 0.32 | −0.08 | 0.10 | 0.41 | ||||
| Gender | 0.63 | 0.80 | 0.78 | ||||||||||
| Female | −0.02 | 0.03 | 0.43 | 0.00 | 0.04 | 0.99 | −0.06 | 0.04 | 0.14 | ||||
| Male | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Marital Status | 0.63 | 0.79 | 0.78 | ||||||||||
| Divorced/Separated | −0.07 | 0.06 | 0.26 | 0.14 | 0.08 | 0.07 | −0.01 | 0.07 | 0.91 | ||||
| Married/Life Partnership | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Single | −0.03 | 0.05 | 0.49 | 0.09 | 0.06 | 0.12 | 0.01 | 0.06 | 0.89 | ||||
| Widowed | 0.14 | 0.07 | 0.05 | 0.21 | 0.09 | 0.02 | 0.04 | 0.09 | 0.68 | ||||
| Race | 0.63 | 0.80 | 0.78 | ||||||||||
| American Indian/Alaskan Native | 0.24 | 0.36 | 0.51 | 0.41 | 0.46 | 0.38 | 0.40 | 0.45 | 0.38 | ||||
| Asian | −0.08 | 0.13 | 0.52 | −0.13 | 0.16 | 0.43 | 0.12 | 0.16 | 0.46 | ||||
| Black/African American | 0.20 | 0.26 | 0.43 | 0.66 | 0.32 | 0.04 | 0.23 | 0.32 | 0.47 | ||||
| Other | −0.08 | 0.13 | 0.55 | −0.03 | 0.16 | 0.86 | −0.05 | 0.16 | 0.76 | ||||
| White | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Highest Education | 0.63 | 0.80 | 0.78 | ||||||||||
| High School or Less | 0.01 | 0.06 | 0.83 | −0.02 | 0.08 | 0.80 | 0.02 | 0.07 | 0.81 | ||||
| Some College/Assoc Degree | 0.00 | 0.04 | 0.91 | −0.03 | 0.05 | 0.61 | 0.06 | 0.05 | 0.20 | ||||
| College Degree | −0.03 | 0.04 | 0.39 | −0.01 | 0.05 | 0.76 | 0.00 | 0.05 | 0.98 | ||||
| Post-College Degree | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Self-Rated Health | 0.63 | 0.80 | 0.78 | ||||||||||
| Very Good | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Good | −0.06 | 0.03 | 0.07 | −0.02 | 0.04 | 0.63 | −0.06 | 0.04 | 0.16 | ||||
| Average | −0.08 | 0.05 | 0.10 | 0.11 | 0.06 | 0.06 | 0.00 | 0.06 | 0.97 | ||||
| Fair | −0.03 | 0.06 | 0.64 | 0.03 | 0.08 | 0.74 | −0.02 | 0.08 | 0.81 | ||||
| Poor | −0.32 | 0.13 | 0.02 | −0.07 | 0.17 | 0.66 | 0.10 | 0.16 | 0.55 | ||||
Assoc, Associate; SE, Standard Error; RMSE, Root Mean Square Error; Ref, Referent Group; NIH, National Institutes of Health.
Table 3.
Relationship Between Respondent Characteristics and Change in NIH Social Relationship Scale subdomains of Loneliness, Perceived Rejection, and Perceived Hostility.
| Loneliness |
Perceived Rejection |
Perceived Hostility |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | p-value | RMSE | Estimate | SE | p-value | RMSE | Estimate | SE | p-value | RMSE | ||
| Age Group | 0.72 | 0.59 | 0.54 | ||||||||||
| 18-30 | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| 31-40 | 0.02 | 0.10 | 0.88 | 0.11 | 0.08 | 0.17 | −0.03 | 0.08 | 0.74 | ||||
| 41-50 | 0.09 | 0.10 | 0.37 | 0.13 | 0.08 | 0.12 | 0.04 | 0.07 | 0.62 | ||||
| 51-60 | 0.05 | 0.09 | 0.57 | 0.10 | 0.08 | 0.19 | −0.07 | 0.07 | 0.32 | ||||
| 61-70 | −0.02 | 0.09 | 0.84 | 0.02 | 0.07 | 0.73 | −0.05 | 0.07 | 0.45 | ||||
| 71+ | −0.08 | 0.09 | 0.40 | 0.05 | 0.07 | 0.51 | −0.07 | 0.07 | 0.28 | ||||
| Gender | 0.72 | 0.59 | 0.54 | ||||||||||
| Female | 0.13 | 0.04 | <0.01 | 0.04 | 0.03 | 0.17 | −0.01 | 0.03 | 0.67 | ||||
| Male | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Marital Status | 0.72 | 0.59 | 0.54 | ||||||||||
| Divorced/Separated | 0.06 | 0.07 | 0.40 | 0.01 | 0.06 | 0.90 | −0.12 | 0.05 | 0.02 | ||||
| Married/Life Partnership | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Single | 0.07 | 0.05 | 0.21 | 0.05 | 0.04 | 0.24 | 0.06 | 0.04 | 0.16 | ||||
| Widowed | −0.11 | 0.08 | 0.18 | 0.02 | 0.07 | 0.75 | −0.01 | 0.06 | 0.93 | ||||
| Race | 0.72 | 0.59 | 0.54 | ||||||||||
| American Indian/Alaskan Native | −0.56 | 0.42 | 0.18 | 0.37 | 0.34 | 0.29 | 0.04 | 0.31 | 0.90 | ||||
| Asian | −0.12 | 0.15 | 0.45 | 0.08 | 0.13 | 0.52 | 0.06 | 0.12 | 0.62 | ||||
| Black/African American | −0.39 | 0.29 | 0.18 | −0.03 | 0.27 | 0.90 | −0.19 | 0.22 | 0.38 | ||||
| Other | −0.30 | 0.15 | 0.05 | −0.18 | 0.13 | 0.16 | −0.21 | 0.11 | 0.07 | ||||
| White | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Highest Education | 0.72 | 0.59 | 0.54 | ||||||||||
| High School or Less | 0.07 | 0.07 | 0.34 | 0.08 | 0.06 | 0.15 | −0.04 | 0.05 | 0.44 | ||||
| Some College/Assoc Degree | 0.02 | 0.04 | 0.71 | −0.03 | 0.04 | 0.40 | −0.08 | 0.03 | 0.01 | ||||
| College Degree | 0.05 | 0.04 | 0.22 | 0.01 | 0.04 | 0.87 | −0.05 | 0.03 | 0.14 | ||||
| Post-College Degree | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Self-Rated Health | 0.72 | 0.59 | 0.54 | ||||||||||
| Very Good | Ref | – | – | Ref | – | – | Ref | – | – | ||||
| Good | 0.06 | 0.04 | 0.13 | 0.04 | 0.03 | 0.22 | 0.01 | 0.03 | 0.75 | ||||
| Average | −0.04 | 0.06 | 0.52 | 0.03 | 0.05 | 0.52 | −0.05 | 0.04 | 0.21 | ||||
| Fair | −0.03 | 0.07 | 0.63 | 0.01 | 0.06 | 0.87 | 0.06 | 0.05 | 0.31 | ||||
| Poor | −0.11 | 0.15 | 0.49 | 0.19 | 0.13 | 0.13 | 0.17 | 0.12 | 0.16 | ||||
Assoc, Associate; SE, Standard Error; RMSE, Root Mean Square Error; Ref, Referent Group; NIH, National Institutes of Health.
Among our sample population, we observed that females experienced an increased sense of loneliness compared with male respondents (estimate = 0.13, SE = 0.04, p < 0.01). Additionally, those individuals identifying as ‘divorced’ or ‘separated’ reported a decreased sense of perceived hostility compared with those identifying as ‘married’ or in a ‘lifetime partnership’ (estimate = −0.12, SE = 0.05, p = 0.02). We did not observe any subpopulations within our sample reporting significant change in their feelings of perceived rejection.
4. Discussion
Within our sample population, we observed that individuals experienced an increased sense of emotional support, instrumental support, and loneliness during a period of social distancing. Our sample population also experienced decreased feelings of friendship and perceived hostility. We observed that individuals with low self-rated health experienced a decreased sense of emotional support during a time of social distancing and that females were more likely to experience increased feelings of loneliness compared with males within our population sample. Two of our subpopulations experienced an increased sense of instrumental support (those identifying as widowed, and those identifying as Black or African American). We did not observe individual subpopulations experiencing differential changes in perceived hostility or friendship, although our overall sample population did experience decreases in these social constructs.
Our observation of improved social support domains of emotional and instrumental support is consistent with previous literature and proposed hypotheses that individuals leverage social support to cope during a time of high stress. Investigating the impact of the COVID-19 pandemic on stress, coping, and individual reported adherence to the U.S. Centers for Disease Control and Prevention COVID-19 guidelines, Park et al. (2020) reported that survey respondents actively seek emotional and instrumental support to cope with feelings related to the pandemic. These findings are supported by the buffering hypothesis, which postulates that social relationships and social support may act as a “buffer” for stressful emotional, physical, or environmental events (S. Cohen and Wills, 1985). At times of high stress, individuals may enact intentional seeking behaviors to obtain emotional and instrumental support (Lau et al., 2006), or may become more conscious of the emotional and instrumental support they receive during everyday interactions (Thoits, 2011). Both of these mechanisms may have resulted in an increased sense of the social support subdomains of emotional and instrumental support we observed.
We also observed a decreased sense of friendship among our sample population. This finding should be considered in the context of the survey items comprising this subdomain. Under the social distancing directives, individuals were asked to only spend time with those within their household and to limit time spent outside of the home. Individual items within this subdomain include being invited to lunch with friends, spending time with people to have fun, and getting together with friends to relax over the prior month. Each of these items falls outside of the recommendations for social distancing measures and our finding may misrepresent or overestimate the effect of social distancing on friendships.
Loneliness is defined as a “distressing discrepancy between desired and actual levels of social contact” (Rubin, 2017). We observed an increase in loneliness among our sample population consistent with media speculation and observed in other investigations (Banerjee and Rai, 2020; Bu et al., 2020; Campbell, 2020). Abrupt changes in social norms due to the pandemic created discrepancies between actual and desired levels of social interaction, leading to feelings of increased loneliness. Early research has shown that feelings of loneliness increased during the initial days of the COVID-19 pandemic, but then decreased steadily in the following weeks (Buecker et al., 2020). We observed that females experienced increased sense of loneliness compared to males. This phenomenon has been observed among other investigations during the COVID-19 crisis (González-Sanguino et al., 2020; Losada-Baltar et al., 2020; Rosenberg et al., 2020). A survey performed by the Pew Research Center observed that women may be experiencing the impact of the COVID-19 pandemic differently than males (Pew Research Center, 2020). Compared with men, female respondents indicated higher frequency of reporting that child care responsibilities were very/somewhat difficult (men 32%, women, 37%) and that they experienced major changes in their lives related to COVID-19 (men 41%, women 47%) (Pew Research Center, 2020). The correlative and bi-directional relationship between stress and feelings of loneliness have been previously observed (Campagne, 2019).
Our sample population also experienced changes in their social relationship quality based on their report of self-rated health. Individuals with lower mental or physical health may struggle with connecting to others, which can create a cycle of deteriorating health and well-being (Moak and Agrawal, 2010). Researchers recognize the critical role of family members and caregivers in providing instrumental and emotional support among older individuals and those living with disabilities (Hado and Friss Feinberg, 2020). Social distancing directives have limited the ability of family members, caregivers, and friends to continue with typical and daily interactions. Programs such as virtual meet-up groups and virtual check-ins are promising ways to increase social connectivity for those who are homebound; and, COVID-19 presents an opportunity to address disparities in internet access that adversely affect vulnerable populations (Duong and Karlawish, 2020).
Our study has several strengths. First, we were able to deploy a longitudinal survey design, allowing us to assess for changes within individuals relating to their social relationships. This design does not require the respondents to make comparisons in a pre-/post-nature creating recall bias and allows for control of non-time-varying individual factors. Second, we deployed a validated survey instrument to assess 3 domains of social relationships (companionship, social support, social distress) with 6 subdomains. This toolset allows for a comprehensive understanding of social relationships.
Our study had several limitations. The size and quality of an individual's social relationship ties have a significant influence on received social support (Thoits, 2011). Although we did not measure the size and strength of individual social networks to understand the impact of these factors, our study intended to study the impact of the COVID-19 crisis on the change in social relationships within individual respondents over time. Our study also was limited by use of a validated self-reported history of mental health rather than validated scales. Our study also suffered from attrition bias by certain populations (age, marital status, race, educational attainment, and self-rated health status), which is not uncommon in internet survey-based research (Rübsamen et al., 2017). We observed attrition among individuals of younger age groups, unmarried individuals, individuals with lower levels of highest achieved education, and lower overall self-rated health. Our study is limited in the amount of information available on individuals who were not retained in our second survey wave limiting our ability to adjust for study attrition, but we did utilize automated survey reminders which have been demonstrated to decrease attrition effects (Rübsamen et al., 2017). Researchers anticipate that mental and emotional health impacts will differ between racial groups, particularly among Black Americans (Novacek et al., 2020). Our study experienced low representation of non-White racial groups which limits our ability to understand the impact of social distancing measures on other racial groups. Additionally, the distribution of education within our population renders our results to be more generalizable groups with more advanced education. In the future, intentional resampling of individuals within low-response groups or leveraging different modalities (e.g., follow-up phone calls, paper-based mail surveys in addition to electronic survey deployment) to gain input from low-response groups could help increase representation of varying populations. Finally, our study may suffer from selection bias based on the sampling of individuals who receive care at a major medical institution, based on being an electronically deployed survey instrument, and based on sampling only individuals who agreed to participate in research from our healthcare delivery organization. Although we did take a random sample of all individuals providing consent for research, our sample population is derived from individuals who have previously received care at our organization, which may represent a less healthy population than the general population. Additionally, deployment of an electronic survey instrument limits participation to those individuals who utilize E-mail services and can complete a web-based survey.
Technology-assisted social connection is being explored as a mechanism to ameliorate feelings of isolation and loneliness during social distancing directives, and many report leveraging email and online messaging services to stay connected with others (Anderson and Vogels, 2020). However, the same population indicates that although internet and phone-based connection helps during social distancing measures, 64% report that these technologies will not replace in-person contact (Anderson and Vogels, 2020). Research shows that internet-based connection and social networking participation have a complex and bi-directional relationship with perceptions of loneliness through mechanisms of social influence and social comparison (Nabi et al., 2013; Nowland et al., 2018; Yang, 2016), but these online platforms may be of critical need should social distancing directives occur again limiting individual ability to have meaningful face-to-face social connection.
5. Conclusions
Social distancing measurably impacts social relationships and may have a disproportionate impact on females and individuals with lower self-rated health. If novel emergent infectious diseases become more commonplace, social interventions may be needed to mitigate the potential adverse impact of social distancing on social relationships.
Funding
This study was funded by the Mayo Clinic Alix College of Medicine and Science.
Author contributions
Lindsey M. Philpot: Conceptualization, Data curation, Formal analysis, Methodology, Writing – original draft; Priya Ramar: Formal analysis, Methodology, Writing – review & editing; Daniel L. Roellinger: Formal analysis, Methodology, Writing – review & editing; Barbara A. Barry: Methodology, Writing – review & editing; Pravesh Sharma: Conceptualization, Writing – review & editing; Jon O. Ebbert: Conceptualization, Supervision, Methodology, Writing – original draft.
Declaration of competing interest
JOE has served as consultant to Nesmah outside of the present work. The remaining authors report no conflicts of interest.
Acknowledgement
We thank Libby J. Hammond and Christina M. Smith (Mayo Clinic Survey Research Center) for their help in planning, testing, and implementing the survey.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.socscimed.2021.113779.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- Anderson M., Vogels E. 2020. Americans Turn to Technology during COVID-19 Outbreak, Say an Outage Would Be a Problem. [Google Scholar]
- Banerjee D., Rai M. Social isolation in Covid-19: the impact of loneliness. Int. J. Soc. Psychiatr. 2020 Sep;66(6):525–527. doi: 10.1177/0020764020922269. Epub 2020 Apr 29. PMID: 32349580; PMCID: PMC7405628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bu F., Steptoe A., Fancourt D. Loneliness during a strict lockdown: trajectories and predictors during the COVID-19 pandemic in 38,217 United Kingdom adults. Soc. Sci. Med. 2020;265:113521. doi: 10.1016/j.socscimed.2020.113521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buecker S., Horstmann K.T., Krasko J., Kritzler S., Terwiel S., Kaiser T., et al. Changes in daily loneliness for German residents during the first four weeks of the COVID-19 pandemic. Soc. Sci. Med. 2020;265:113541. doi: 10.1016/j.socscimed.2020.113541. [DOI] [PubMed] [Google Scholar]
- Campagne D.M. Stress and perceived social isolation (loneliness) Arch. Gerontol. Geriatr. 2019;82:192–199. doi: 10.1016/j.archger.2019.02.007. [DOI] [PubMed] [Google Scholar]
- Campbell A.D. Practical implications of physical distancing, social isolation, and reduced physicality for older adults in response to COVID-19. J. Gerontol. Soc. Work. 2020:1–3. doi: 10.1080/01634372.2020.1772933. [DOI] [PubMed] [Google Scholar]
- Cohen L.H., McGowan J., Fooskas S., Rose S. Positive life events and social support and the relationship between life stress and psychological disorder. Am. J. Community Psychol. 1984;12:567–587. doi: 10.1007/BF00897213. [DOI] [PubMed] [Google Scholar]
- Cohen S. Social relationships and health. Am. Psychol. 2004;59:676–684. doi: 10.1037/0003-066X.59.8.676. [DOI] [PubMed] [Google Scholar]
- Cohen S., Wills T.A. Stress, social support, and the buffering hypothesis. Psychol. Bull. 1985;98:310–357. [PubMed] [Google Scholar]
- Cyranowski J.M., Zill N., Bode R., Butt Z., Kelly M.A., Pilkonis P.A., et al. Assessing social support, companionship, and distress: national institute of health (NIH) toolbox Adult social relationship Scales. Health Psychol. 2013;32:293–301. doi: 10.1037/a0028586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Devaraj S., Patel P.C. Change in psychological distress in response to changes in reduced mobility during the early 2020 COVID-19 pandemic: evidence of modest effects from the U.S. Soc. Sci. Med. 2021;270:113615. doi: 10.1016/j.socscimed.2020.113615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duong M.T., Karlawish J. Caregiving at a physical distance: initial thoughts for COVID-19 and beyond. J. Am. Geriatr. Soc. 2020;68:1170–1172. doi: 10.1111/jgs.16495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El-Zoghby S.M., Soltan E.M., Salama H.M. Impact of the COVID-19 pandemic on mental health and social support among adult Egyptians. J. Community Health. 2020:1–7. doi: 10.1007/s10900-020-00853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frias C.E., Cuzco C., Martín C.F., Pérez-Ortega S., Triviño López J.A., Lombraña M. Resilience and emotional support in health care professionals during the COVID-19 pandemic. J. Psychosoc. Nurs. Ment. Health Serv. 2020;58:5–6. doi: 10.3928/02793695-20200506-02. [DOI] [PubMed] [Google Scholar]
- Gariépy G., Honkaniemi H., Quesnel-Vallée A. Social support and protection from depression: systematic review of current findings in Western countries. Br. J. Psychiatry. 2016;209:284–293. doi: 10.1192/bjp.bp.115.169094. [DOI] [PubMed] [Google Scholar]
- George L.K., Blazer D.G., Hughes D.C., Fowler N. Social support and the outcome of major depression. Br. J. Psychiatry. 1989;154:478–485. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- González-Sanguino C., Ausín B., Castellanos M., Saiz J., López-Gómez A., Ugidos C., et al. Mental health consequences during the initial stage of the 2020 Coronavirus pandemic (COVID-19) in Spain. Brain Behav. Immun. 2020 doi: 10.1016/j.bbi.2020.05.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hado E., Friss Feinberg L. Amid the COVID-19 pandemic, meaningful communication between family caregivers and residents of long-term care facilities is imperative. J. Aging Soc. Pol. 2020:1–6. doi: 10.1080/08959420.2020.1765684. [DOI] [PubMed] [Google Scholar]
- Hamada K., Fan X. The impact of COVID-19 on individuals living with serious mental illness. Schizophr. Res. 2020 doi: 10.1016/j.schres.2020.05.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lai C.C., Shih T.P., Ko W.C., Tang H.J., Hsueh P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): the epidemic and the challenges. Int. J. Antimicrob. Agents. 2020;55:105924. doi: 10.1016/j.ijantimicag.2020.105924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lau J.T., Yang X., Tsui H.Y., Pang E., Wing Y.K. Positive mental health-related impacts of the SARS epidemic on the general public in Hong Kong and their associations with other negative impacts. J. Infect. 2006;53:114–124. doi: 10.1016/j.jinf.2005.10.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Losada-Baltar A., Jiménez-Gonzalo L., Gallego-Alberto L., Pedroso-Chaparro M.D.S., Fernandes-Pires J., Márquez-González M. We're staying at home". Association of self-perceptions of aging, personal and family resources and loneliness with psychological distress during the lock-down period of COVID-19. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020 doi: 10.1093/geronb/gbaa048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lui J.Z., Young N.P., Ebbert J.O., Rosedahl J.K., Philpot L.M. Loneliness and migraine self-management: a cross-sectional assessment. J Prim Care Community Health. 2020;11 doi: 10.1177/2150132720924874. 2150132720924874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moak Z.B., Agrawal A. The association between perceived interpersonal social support and physical and mental health: results from the National Epidemiological Survey on Alcohol and Related Conditions. J. Publ. Health. 2010;32:191–201. doi: 10.1093/pubmed/fdp093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nabi R.L., Prestin A., So J. Facebook friends with (health) benefits? Exploring social network site use and perceptions of social support, stress, and well-being. Cyberpsychol., Behav. Soc. Netw. 2013;16:721–727. doi: 10.1089/cyber.2012.0521. [DOI] [PubMed] [Google Scholar]
- Novacek D.M., Hampton-Anderson J.N., Ebor M.T., Loeb T.B., Wyatt G.E. Mental health ramifications of the COVID-19 pandemic for Black Americans: clinical and research recommendations. Psychol Trauma. 2020 doi: 10.1037/tra0000796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nowland R., Necka E.A., Cacioppo J.T. Loneliness and social internet use: pathways to reconnection in a digital world? Perspect. Psychol. Sci. 2018;13:70–87. doi: 10.1177/1745691617713052. [DOI] [PubMed] [Google Scholar]
- Omer S.B., Malani P., del Rio C. The COVID-19 pandemic in the US: a clinical update. Jama. 2020;323:1767–1768. doi: 10.1001/jama.2020.5788. [DOI] [PubMed] [Google Scholar]
- Park C.L., Russell B.S., Fendrich M., Finkelstein-Fox L., Hutchison M., Becker J. Americans' COVID-19 stress, coping, and adherence to CDC guidelines. J. Gen. Intern. Med. 2020:1–8. doi: 10.1007/s11606-020-05898-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center . 2020. Most Americans Say Coronavirus Outbreak Has Impacted Their Lives. [Google Scholar]
- Rees C.A., Karter A.J., Young B.A. Race/ethnicity, social support, and associations with diabetes self-care and clinical outcomes in NHANES. Diabetes Educat. 2010;36:435–445. doi: 10.1177/0145721710364419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenberg M., Luetke M., Hensel D., Kianersi S., Herbenick D. 2020. Depression and Loneliness during COVID-19 Restrictions in the United States, and Their Associations with Frequency of Social and Sexual Connections. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin R. Loneliness might Be a killer, but what's the best way to protect against it? Jama. 2017;318:1853–1855. doi: 10.1001/jama.2017.14591. [DOI] [PubMed] [Google Scholar]
- Rübsamen N., Akmatov M.K., Castell S., Karch A., Mikolajczyk R.T. Factors associated with attrition in a longitudinal online study: results from the HaBIDS panel. BMC Med. Res. Methodol. 2017;17:132. doi: 10.1186/s12874-017-0408-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schuchat A. MMWR Morb Mortal Wkly Rep: U.S. Department of Health and Human Services; 2020. Public Health Response to the Initiation and Spread of Pandemic COVID-19 in the United States, February 24–April 21, 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidi Y., Harel O. The treatment of incomplete data: reporting, analysis, reproducibility, and replicability. Soc. Sci. Med. 2018;209:169–173. doi: 10.1016/j.socscimed.2018.05.037. [DOI] [PubMed] [Google Scholar]
- Thoits P.A. Mechanisms linking social ties and support to physical and mental health. J. Health Soc. Behav. 2011;52:145–161. doi: 10.1177/0022146510395592. [DOI] [PubMed] [Google Scholar]
- Uchino B.N. Yale University Press; New Haven, CT, US: 2004. Social Support and Physical Health: Understanding the Health Consequences of Relationships. [Google Scholar]
- Yang C.C. Instagram use, loneliness, and social comparison orientation: interact and browse on social media, but don't compare. Cyberpsychol., Behav. Soc. Netw. 2016;19:703–708. doi: 10.1089/cyber.2016.0201. [DOI] [PubMed] [Google Scholar]
- Zhang Y., Ma Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in liaoning province, China: a cross-sectional study. Int. J. Environ. Res. Publ. Health. 2020;17 doi: 10.3390/ijerph17072381. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.