Abstract
Background
The care of children with cancer creates emotional, financial, and social impacts for their families. Information on the impact of childhood cancer (CC) on the family is scarce in Bangladesh. Thus, the study was set out to assess the impact of CC on the families in the local context.
Methods
This cross-sectional study was conducted from January to June 2018 in three purposively selected tertiary hospitals. All the children diagnosed and treated at those hospitals during the study period were eligible for this study. Children undergoing bone marrow transplantation, or those who were seriously ill, or those transferred to another hospital, or those who died were excluded or whose parents were not willing to participate. A total of 242 children were enrolled in the study and their parents were included in the interview. Measures included socio-demographic attributes, financial burden, personal strain, social impact, mastery, and treatment cost. Informed written consent was obtained from the parents and a face-to-face interview was conducted using a semi-structured questionnaire based on (i) About you and your-family and (ii) the Impact-On-Family (IOF) scale. High scores of the scale correlated to high impact. Medical records were reviewed to collect data on the pattern of CC and treatment costs.
Results
Major CCs included leukemia (36.0%), blastoma (18.2%), sarcoma (14.9%), and lymphoma (12.4%). The weighted score was highest for mastery (3.63) followed by financial burden (3.33), personal strain (3.27), and social impact (3.21) domains. The difference of IOFS score was significant by family type (p < 0.05), father's occupation (p < 0.05), type (p < 0.01) and duration of cancer (p < 0.01), and treatment cost (p˂0.01). Families adopted diverse coping strategies including changed lifestyle (98.3%), sought social support (86.0%), rely more on religion (98.8%), and reduced family investment (83.9%) to adjust the impact.
Conclusion
The impact of CC on the family is evident at many levels. In particular, mean scores of financial burden, personal strain, social impact, and mastery domains of the IOF scale were significantly associated with the employment status of parents, residing place, treatment cost, type, and duration of cancer. The study findings could contribute to devising impact-reducing intervention programs in Bangladesh.
Keywords: Childhood cancer, Family, Financial burden, Impact, Mastery, Personal strain, Social impact, Treatment cost, Bangladesh
Childhood cancer, Family, Financial burden, Impact, Mastery, Personal strain, Social impact, Treatment cost, Bangladesh
1. Introduction
Childhood cancer (CC) is emerging as a major cause of death among children, and it became 2nd leading cause of death among children beyond the age of 1 year [1]. Prevention of CC is a challenging task, so that, early and accurate diagnosis followed by effective treatment is mandatory to prevent the worst impacts of CC. The cure rate of children with cancer was found more than 80% in high-income countries but only 20% in low and middle-income countries [2].
International Agency for Research on Cancer (IARC) collates cancer data from around the world to estimate national, regional, and global cancer burden following the definitions of the International Classification of Diseases. Quantifying global and regional cancer burden is challenging because the majority of the world's population is not adequately covered by vital registration, cancer surveillance systems, or both [3].
In Bangladesh, the burden of CC is unknown due to the nonexistence of countrywide cancer registries and surveillance systems [4]. The proportion of CC is higher in Bangladesh because a larger segment (around 30%) of the total population is children under fifteen years [5]. The numbers of pediatric cancer cases are expected to increase in the country by the next few decades. Health services for the people are delivered at three levels in the country; primary, secondary, and tertiary. Specialized health facility for assessments and treatment of cancer is not available in primary and secondary levels, where most of the total population reside. At the tertiary level, there are very limited cancer service facilities including the four largest public hospitals having pediatric oncology departments and a few private specialized hospitals to serve the CC patients of the whole country. The health care delivery system encounters a severe shortage of infrastructure and trained health personnel for effective management of CC [6].
Diagnosis of CC is an extremely distressing experience for the families as it requires a higher degree of support, coping, and adaptation [7]. CC invites increased caregiving responsibility of the families and imposes a physical, emotional, and financial burden. Families' ability to cope up with the financial burden may have a long-term effect on their quality of life [1]. Several studies have found that having a child in the family with cancer can induce feelings of stress, impairs psychological and social adjustments [8].
Treatment cost of CC comprises of direct and indirect costs. Direct costs include the cost of hospitalization, treatment, medication, diagnosis, travel; accommodation, and food [9]. Indirect costs include loss of income, unofficial payment, family costs, and attendant. Some of the families fall into improvised poverty for catastrophic health care expenditure of CC [1].
Parents and families continue to experience the worst impacts of CC as demonstrated significantly higher impact scores in all negative domains. The factors that contributed to this higher impact were single parenthood, lower-income, and greater distance needed to travel to the hospital [10].
Bangladesh confronts s higher incidence rate of CC (13000 new cases per year) [11]. The families of children with CC suffer from high levels of anxiety, depression, psychological distress, financial impact, and extensive worry for the children [12]. The actual scenario of the impact of CC on the family is unknown in the country.
Around 67% of the health care expenditure is out of pocket, and nearly 6.0 million people are pushed into poverty because of out-of-pocket payments every year in Bangladesh. The country is experiencing a 15% catastrophic expenditure [13]. National health policy suggested a substantial increase in budgetary allocation for health care to ensure health equity and financial risk protection through achieving Universal Health Coverage (UHC) [14].
The catastrophic treatment cost of CC imposes a financial burden on the families. This present study intended to determine the impacts of CC on the family in terms of personal strain, mastery, social, and financial burden. The study findings would contribute to implementing national policy for establishing financial risk protection through UHC.
2. Materials and methods
2.1. Study setting
We conducted this cross-sectional study in three purposively selected tertiary hospitals in Dhaka city. Two were public hospitals: National Institute of Cancer Research & Hospital (NICRH) and Dhaka Medical College Hospital (DMCH), and another one was a quasi-public hospital: Bangabandhu Sheikh Mujib Medical University (BSMMU). All these hospitals have specialized facilities for diagnosis and treatment of CC at the pediatric oncology departments. Different health facilities throughout the country refer children with cancer to those hospitals for assessment and treatment.
2.2. Study design, study population, and sample size
This cross-sectional study was performed from 1 January to 30 June 2018. All children aged <18 years diagnosed and treated for cancer at the selected tertiary hospitals during the study period were eligible for the study. The study excluded children undergoing bone marrow transplantation, or those who were seriously ill, or those transferred to another hospital, or those who died after diagnosis, or whose parents were not willing to participate. We targeted all the children enrolled in the hospitals during the study period and completed treatment of cancer for at least one month. Based on the selection criteria, the study enrolled 242 children and their parents (either father or mother or both) as the study participants to take part in the interview. Among the participants, 164 were both father and mother, 36 were the only mother, and 42 were the only father.
2.3. Data collection
Data were collected at the hospital setting by interviewing the parents of the children who were undergoing treatment for CC. A face-to-face interview was conducted for data collection using a semi-structured pre-tested questionnaire based on (i) About-you and your-family and (ii) IOF scale (IOFS) [15]. First part of the questionnaire contained socio-demographic attributes while the second part was based on the IOFS. There was no validated Bangla (local language of Bangladesh) version of IOFS. We adopted the scale linguistically and contextually. Considering the local context, we translated the scale into Bangla and back-translated it into English to make it meaningful similar to the original version in English. We finalized the Bangla version of IOFS through necessary corrections and modifications following the findings of the pre-testing. One interviewer was employed for conducting the interviews in the same language, sequence, and technique to ensure the reliability of data. This scale consists of a 24-item questionnaire measuring 4 domains of impact; financial burden; social impact; personal strain; and mastery. Financial burden refers to the economic consequences for the family. Social impact concerns the level of disruption of social interaction for the family. Personal strain assesses the psychological burden experienced by the primary caretaker for the child with cancer. Mastery refers to the coping strategies employed by the family [15]. Cronbach's alpha reliabilities for the 4 dimensions of the IOFS are 0.72, 0.86, 0.81, 0.60, respectively, and 0.88 for the total score [16]. A total score for the IOFS was obtained by the summation of scores of all 24 items as a general measure of impact, where a higher score indicates a greater impact. Treatment cost was estimated monthly by calculating both direct and indirect costs of CC. The objectives and procedure of the study were explained followed by informed written consent was obtained from each participant before the interview. Measures were taken to ensure data quality; inconsistency and irrelevance of data were checked and corrected.
2.4. Statistical analysis
Data were analyzed using necessary statistical tools and techniques. The normality of the variables was tested with the Shapiro Wilk test/Kolmogorov Smirnov tests of Normality. Descriptive statistics included mean, frequency, and percentage. Continuous data such as age, number of a family member, monthly family income, direct cost, indirect cost, total cost, and scores of domains of IOFS, etc. were presented in the form of mean with 95% confidence interval (CI). Categorical data like gender, residence, educational qualification, family type, occupation of the father, occupation of the mother were reported as counts and percentages. Inferential statistics included comparisons of the mean IOFS scores by socio-demographic attributes, types and duration of CC, and treatment costs using the relevant statistical test of significance. We performed multiple statistical tests to find out significant differences in mean IOF scores (dependent variable) by different independent variables. Independent sample ‘t’ tests were done to determine any significant differences between two mean IOF scores, and ANOVA tests were done to find any significant differences among three or more mean scores. We considered p-value <0.05 with 95% CI as significant. All the statistical tests were two-sided and were performed at a significance level of α = 0.05. To correct the experiment-wise error rate for using multiple 't' tests and a procedure to correct the family-wise error rate following analysis of variance (ANOVA), we used Bonferroni adjusted probability (p), which sets the alpha value for the entire set of ‘n’ comparisons equal to ‘α’ by taking the alpha value for each comparison equal to α/n. Explicitly, given ‘n’ tests ‘Ti’ for hypotheses ‘Hi’ (1≤i ≤ n) under the assumption ‘Ho’ that all hypotheses ‘Hi’ are false, and if the individual test critical values are ≤α/n, then the experiment-wide critical value is ≤α. In equation form, if p(Ti passes | Ho) ≤ α/n. To get the adjusted p-value, we divided the original α-value by the number of analyses on the dependent variable.
2.5. Ethical considerations
Ethical clearance was obtained from the Institutional Ethics Committee (IEC) of NIPSOM Mohakhali, Dhaka, Bangladesh (Reference No. NIPSOM/IRB-IEC/2018/20/3, Date: 18.01.2018). Informed consent was obtained from the parents by informing the purpose and procedure, expected duration, nature, and anticipated physical and psychological risks (no typical financial or commercial) and benefits of participating. Confidentiality of data and privacy of the participants was strictly maintained.
3. Results
3.1. Enrollment of children with CC and their parents
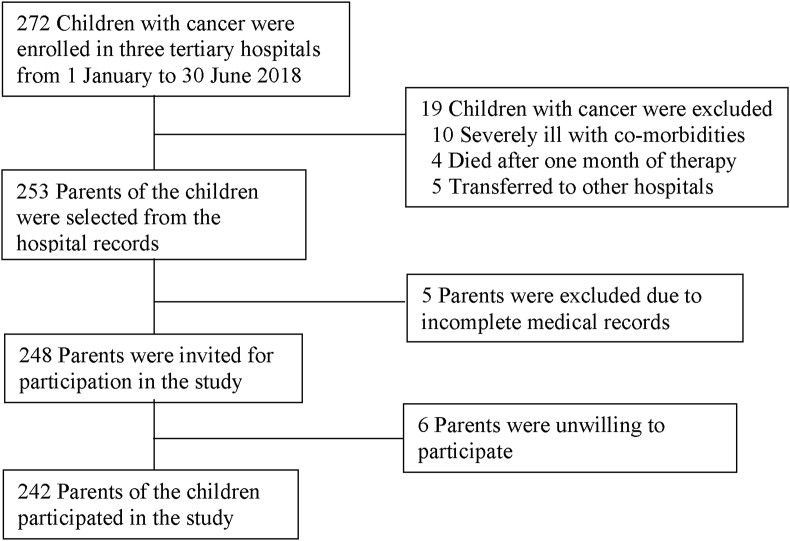
Of the 272 children, 10 were severely ill, 4 died within one month of therapy, 5 were transferred to other hospitals, 5 had missing medical records. Among the remaining 248 parents of children, 6 were unwilling to participate in the interview (Figure 1).
Figure 1.
Flow chart of study participants.
3.2. Socio-demographic attributes of the children
The mean age of the children was 8.97 (±4.75) years. Male children were predominant (60.7%), and the majority were from rural areas (67.5%) and the nuclear family (60.7%). More than one-fourth of fathers (27.7%) were farmers while most (94.2%) of the mothers were housewives (Table 1).
Table 1.
Socio-demographic attributes of the children and families.
| Attributes | No. (%) | Mean (95% CI) | |
|---|---|---|---|
| Age (Years) | 2–5 | 75 (31.0) | 8.97 (8.37–9.57) |
| 6–10 | 61 (25.2) | ||
| 11–17 | 106 (43.8) | ||
| Gender | Male | 147 (60.7) | |
| Female | 95 (39.3) | ||
| Residence | Urban | 83 (34.3) | |
| Rural | 159 (65.7) | ||
| Educational Qualification | Pre-school | 76 (31.4) | |
| Primary | 103 (42.6) | ||
| Secondary | 63 (26.0) | ||
| Family Type | Nuclear | 147 (60.7) | |
| Joint | 95 (39.3) | ||
| Number of Family Member | 3–5 | 138 (57.0) | 5.83 (5.59–6.08) |
| 6–8 | 82 (33.9) | ||
| 9–12 | 22 (9.1) | ||
| Occupation of the Father | Service (Govt. & Private employees) | 57 (23.6) | |
| Business | 60 (24.8) | ||
| Farmer | 67 (27.7) | ||
| Day labor | 45 (18.6) | ||
| Unemployed | 13 (5.4) | ||
| Occupation of the Mother | Service (Govt. & Private employees) | 14 (5.8) | |
| Housewife | 228 (94.2) | ||
| Monthly Family Income (TK.) | 7000–10000 | 54 (22.3) | 18262 (17281–19243) |
| 10001–20000 | 123 (50.8) | ||
| 20001–40000 | 65 (26.9) | ||
No.: Number; SD: Standard Deviation; TK.: Taka, Currency of Bangladesh.
3.3. Types of childhood cancer
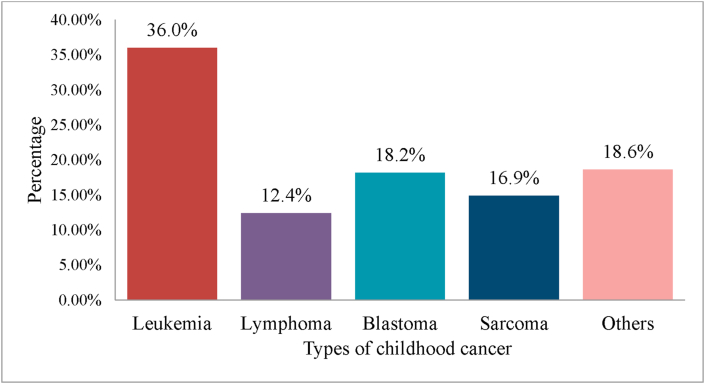
Major CCs included leukemia (36.0%) followed by blastoma (18.2%), sarcoma (14.9%), lymphoma (12.4%) and others (18.6%) (Figure 2).
Figure 2.
Distribution of children by types of cancer.
Leukemia: Acute Lymphoblastic Leukemia, Acute Myeloid Leukemia; Lymphoma: Hodgkin's Lymphoma, Non-Hodgkin's Lymphoma, Burkit Lymphoma; Blastoma: Retinoblastoma, Neuroblastoma, Medulloblastoma, Hepatoblastoma; Sarcoma: Ewing's Sarcoma, Soft Tissue Sarcoma, Chondrosarcoma, Fibrosarcoma; Others: Carcinoma Rectum, Bone Tumor, Wilm's Tumor, Germ Cell Tumor, Round Cell Tumor, Yolk Sac Tumor, Primitive Neur-oectodermal Tumor.
3.4. Treatment cost of CC
Regarding the treatment costs of CC, the direct cost was TK.64938 (±33053), the indirect cost was TK.8601 (±4943), and the average cost was TK.73494 (±34008). Drug cost and the family cost were the leading direct and indirect costs respectively (Table 2).
Table 2.
Treatment costs of CC incurred by the families.
| Type of cost | No. | Mean (95% CI) | |
|---|---|---|---|
| Direct cost (TK.) | Consultation fee | 160 | 1990 (1707–2272) |
| Travel cost | 242 | 3923 (3341–4505) | |
| Drug cost | 242 | 34262 (30855–37669) | |
| Hospital cost | 217 | 8200 (6873–9526) | |
| Investigation cost | 242 | 1211 (11034–13188) | |
| Food cost | 242 | 5701 (5326–6076) | |
| Tips | 141 | 384 (320–448) | |
| Average direct cost | 242 | 64938 (60753–69124) | |
| Indirect Cost (TK.) | Loss of income | 28 | 5678 (4394–6962) |
| Family cost | 242 | 7835 (7274–8396) | |
| Attendant's cost | 02 | 2000 (2000–2000) | |
| Unofficial payment | 48 | 358 (277–439) | |
| Average indirect cost | 242 | 8576 (7947–9205) | |
| Total cost (TK.) | Average treatment cost | 242 | 73469 (69174–77763) |
No.: Number; SD: Standard Deviation; TK.: Taka, Currency of Bangladesh.
3.5. Impact of CC on the family
Out of the 4 domains, the mastery (3.63) domain shared the highest weighted score followed by financial burden (3.3), personal strain (3.27), and social impact (3.21) domains, and the mean score of all the domains was 80.0 (Table 3).
Table 3.
Summary of mean (95% CI) scores of domains of IOFS in Bangladeshi children.
| Domain | No. of items | Mean (95% CI) score | Weighted mean score | Minimum | Maximum |
|---|---|---|---|---|---|
| Financial impact | 4 | 13.33 (13.13–13.52) | 3.33 | 9 | 16 |
| Social impact | 9 | 28.89 (28.49–29.29) | 3.21 | 20 | 36 |
| Personal strain | 6 | 19.63 (19.37–19.90) | 3.27 | 12 | 23 |
| Mastery | 5 | 18.15 (17.93–18.38) | 3.63 | 12 | 20 |
| Total | 24 | 80.0 (±79.40–80.60) | 68 | 89 |
No: Number; SD: Standard deviation.
Based on significance at p < 0.05, the differences in mean scores of IOFS and its social impact domain were significant by family type and fathers' occupation. The mean score of the financial burden domain was significantly different by age of children, residing place, and fathers' occupation (p < 0.05). Differences in mean scores of personal strain and mastery domains were significant by family income (p < 0.05) and fathers' occupation (p < 0.05). Based on significance at adjusted ‘p’ value (0.008), no difference of IOFS and its domains was revealed (Table 4).
Table 4.
Mean scores of the domains of IOFS by socio-demographic attributes.
| Attributes | Financial burden |
Social impact |
Personal strain |
Mastery |
Total IOFS score |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | p-value | Mean | p-value | Mean | p-value | Mean | p-value | Mean | p-value | ||
| Age | 2–5 | 13.00 | 0.009b | 28.77 | 0.600b | 19.56 | 0.083b | 18.31 | 0.657b | 79.64 | 0.403b |
| 6–10 | 13.80 | 28.64 | 20.13 | 18.11 | 80.69 | ||||||
| 11–18 | 13.28 | 29.11 | 19.40 | 18.07 | 79.86 | ||||||
| Gender | Male | 13.22 | 0.173a | 28.72 | 0.303a | 19.80 | 0.113a | 18.02 | 0.171a | 79.77 | 0.344a |
| Female | 13.49 | 29.15 | 19.37 | 18.35 | 80.36 | ||||||
| Residence | Urban | 12.99 | 0.013a | 29.12 | 0.407a | 19.66 | 0.870a | 18.14 | 0.958a | 79.92 | 0.84a |
| Rural | 13.50 | 28.77 | 19.62 | 18.16 | 80.04 | ||||||
| Type of Family | Nuclear | 13.38 | 0.495a | 28.52 | 0.022a | 19.52 | 0.314a | 18.10 | 0.530a | 79.52 | 0.048a |
| Joint | 13.24 | 29.46 | 19.80 | 18.24 | 80.75 | ||||||
| Father's occupation | Service (Govt. and Private employees) | 12.86 | 0.021b | 28.65 | 0.045b | 19.35 | 0.313b | 17.72 | 0.019b | 78.58 | 0.021b |
| Business | 13.70 | 28.43 | 20.12 | 18.72 | 80.97 | ||||||
| Farmer | 13.57 | 29.10 | 19.55 | 18.27 | 80.49 | ||||||
| Day labor | 13.11 | 29.91 | 19.44 | 17.93 | 80.40 | ||||||
| Unemployed | 13.15 | 27.38 | 19.69 | 17.62 | 77.85 | ||||||
| Monthly family income | 7000–10000 | 13.54 | 0.374b | 29.19 | 0.111b | 19.02 | 0.033b | 18.63 | 0.070b | 80.37 | 0.569b |
| 10001–20000 | 13.33 | 28.48 | 19.90 | 17.97 | 79.68 | ||||||
| 20001–40000 | 13.14 | 29.42 | 19.63 | 18.11 | 80.29 | ||||||
∗Significant at corrected p < 0.008.
Independent sample t-test.
One-way ANOVA (F-test).
The differences in the mean score of IOFS by direct cost and type and duration of CC were significant (p < 0.01). The difference in the mean score of the financial burden domain by the duration of CC was significant (p < 0.01). The differences in the mean score of the social impact domain were significant by type and duration of cancer, direct, indirect, and total treatment costs (p < 0.01). The mean score of the personal strain domain was significantly different by duration (p < 0.01) of cancer and direct treatment cost (p < 0.01). The differences in the mean scores of mastery domain were significant by type and duration of cancer, indirect, and total treatment costs (p < 0.01) (Table 5).
Table 5.
Comparison of mean scores of the domains of IOFS by treatment cost, type, and duration of cancer.
| Attributes | Financial burden |
Social impact |
Personal strain |
Mastery |
Total IOFS score |
||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean | p-value | Mean | p-value | Mean | p-value | Mean | p-value | Mean | p-value | ||
| Type of cancer | Leukemia | 13.15 | 0.370b | 27.71 | 0.000b∗ | 19.10 | 0.055b∗ | 17.75 | 0.001b∗ | 77.71 | 0.000b∗ |
| Lymphoma | 13.70 | 29.20 | 19.77 | 17.53 | 80.20 | ||||||
| Blastoma | 13.32 | 29.81 | 20.05 | 18.87 | 82.05 | ||||||
| Sarcoma | 13.17 | 29.00 | 19.83 | 18.44 | 80.44 | ||||||
| Others | 13.56 | 29.96 | 20.00 | 18.42 | 80.00 | ||||||
| Duration of cancer (Months) | 1–6 | 12.89 | 0.000b∗ | 27.86 | 0.000b∗ | 19.19 | 0.000b∗ | 17.86 | 0.002b∗ | 77.80 | 0.000b∗ |
| 7–12 | 14.0 | 30.67 | 20.44 | 18.73 | 83.84 | ||||||
| 13–18 | 14.24 | 30.12 | 19.94 | 18.18 | 82.47 | ||||||
| Direct cost | 1500–50000 | 13.14 | 0.408b | 27.76 | 0.000b∗ | 19.18 | 0.002b∗ | 18.35 | 0.178b | 78.43 | 0.001b∗ |
| 50001–100000 | 13.42 | 29.56 | 19.66 | 17.96 | 80.61 | ||||||
| 100001–200000 | 13.40 | 28.93 | 20.73 | 18.47 | 81.53 | ||||||
| Indirect cost |
1000–10000 | 13.30 | 0.699a | 28.37 | 0.000a∗ | 19.60 | 0.699a | 18.38 | 0.001a∗ | 79.65 | 0.052a |
| 10001–20000 | 13.39 | 30.34 | 19.72 | 17.53 | 80.98 | ||||||
| Total cost | 20000–50000 | 13.12 | 0.397b | 27.74 | 0.000b∗ | 19.38 | 0.084b | 18.61 | 0.033b | 78.84 | 0.054b |
| 50001–100000 | 13.43 | 29.54 | 19.57 | 17.93 | 80.47 | ||||||
| 100001–200000 | 13.36 | 28.67 | 20.28 | 18.13 | 80.44 | ||||||
∗Significant at corrected p < 0.01.
Independent sample t-test.
One-way ANOVA (F-test).
3.6. Coping strategies adopted by the families
To adapt to the impact of CC, families adopted diverse coping strategies like changing lifestyle (98.3%), seeking social support (86.0%), relying on religion (98.8%), and reducing family investment (83.9%). Under changing lifestyle strategy, around two-third of families reduced educational expenses and minimized food expenses of the family while under social support strategy, most of the families obtained support from relatives. Under the religious strategy, more than four-fifth of families started a regular prayer, four-fifth of families accepted the event as a part of fate. Under minimizing family investment, more than two-fifth of families reduced deposition of provident fund and business investment (Table 6).
Table 6.
Coping strategies and ways of coping adopted by the families.
| Coping strategies | Ways of coping | No. (%) |
|---|---|---|
| Changing lifestyle (98.3%) | Reducing recreational expenses | 63 (26.5) |
| Reducing educational expenses | 158 (66.4) | |
| Minimizing clothing expenses | 127 (53.4) | |
| Reducing travel expenses | 54 (22.7) | |
| Minimizing food expenses | 151 (63.4) | |
| Social support (86.0%) | Support from relatives | 196 (94.2) |
| Support from friends | 65 (31.3) | |
| Support from neighbors | 53 (25.5) | |
| Support from social welfare | 35 (16.8) | |
| Arranging fund raising events | 04 (1.9) | |
| Religious activity (98.8%) | Regular prayer | 204 (85.4) |
| Spending time in holy places | 43 (18.0) | |
| Donation to poor & distressed people | 54 (22.6) | |
| Arranging religious program at home | 57 (23.8) | |
| Mode of acceptance (100%) | Fate | 212 (87.6) |
| Bad luck | 26 (10.7) | |
| Self-negligence | 04 (1.7) | |
| Minimizing family investment (83.9%) | Reducing monthly deposit in Bank | 67 (33.0) |
| Reducing investment in business | 82 (40.4) | |
| Reducing amount in provident fund | 89 (43.8) |
No.: Number; %: Percentage.
4. Discussion
Although CC has been a greater concern of clinical medicine, empirical research on its impact on the families has hardly been conducted in Bangladesh. As a pioneering work, this study laid the foundation for further large scale investigations into the impact of CC.
Around one-third of children with cancer enrolled in the current study were in the age group 2–5 years. Another institution-based study conducted in Singapore revealed a similar finding [7]. It could be explained by the fact that the clinical features of CC are mostly manifested and diagnosed at an early age (within five years) of the children. Accordingly, the families attend the health facilities for treating cancer at an early age of the children. More than two-fifth of children were male and from the nuclear family, and around two-third were from a rural setting. Another study conducted in Bangladesh depicted similar findings [1]. Arguably we could mention that in a developing country like Bangladesh, rural parents are fond of male children and are more concerned about their health and treatment. Accordingly, the parents take care of male children more than their counterpart female children with cancer. Moreover, poor education, less awareness of health, exposure to the unhygienic environment, unhealthy diet, and poor access to health services make the rural children more susceptible to diverse CC. Fathers' occupation comprised of agriculture (27.7%) and business (24.8%) while most (94.2%) of the mothers were housewives. This difference in parent's occupation could be justified by social, cultural, and religious norms of the country, where women are still less empowered and employed. Lower family income evidenced by the study could be explained by the fact that Bangladesh is a lower-middle-income country, and the majority of the families had small-scale agriculture and small business as tiny sources of income.
Major CCs were leukemia (36.0%), lymphoma (12.40%) and blastoma (18.20%). Two other studies conducted in Bangladesh support this finding [1, 11] but the study of Ward et al [17] found ALL (26%) and brain tumors (21.0%) as major contributors. These differences could be due to variations of the study place and period between the two studies.
Treatment costs of CC included total cost, Tk.73494; direct cost, Tk.64938; and indirect cost, Tk.8601. But the costs estimated by Islam S et al [1] in Bangladesh were comparatively lower. It indicates that the treatment cost of CC is increasing abruptly and posing a financial burden to the families of the children.
Mean IOFS score (80.0 ± 4.72) was significantly higher in children with 7–12 than 1–6 months' duration of CC (F-test, p˂0.001). It indicates that the higher impact on the family correlates with the longer duration of CC. The present study found the highest weighted scores in mastery (3.63) domain followed by financial burden (3.33), personal strain (3.27), social impact (3.21) domains but the study in Singapore [7] found the highest weighted score in social impact (3.80) domain and lowest score in mastery (1.45) domain. These differences could be justified by the fact that better economic status and healthcare facilities reduce the impact of CC on the families in Singapore than in Bangladesh. Moreover, the families in Bangladesh confront the incremental financial burden of CC along with their existing poor financial capacity. Scores of the financial burden and mastery domains were significantly higher in fathers who were businessmen. It could be argued that fathers have to reduce investment in the business to adjust the financial burden of CC and confront incremental impact. The score of the social impact domain was higher in joint families, and it could be justified by the realities that the joint families have to deal with diverse needs of other family members and tackle different social affairs and responsibilities, which aggravates the impact of CC.
Higher scores of financial, social, and mastery domains were associated with a longer duration of CC. A longer duration of CC incurs more treatment costs, which require diverse coping strategies and social supports and worsen the impact on the families. The score of the personal strain domain was higher in the first year of diagnosis of CC. It could be argued by the fact that the psychological stress of CC on the families remains extreme immediately after diagnosis followed by it declines by adaptation and adoption of diverse coping strategies.
Higher scores of social, financial, personal, and mastery domains were also associated with total, direct, and indirect treatment costs. The financial burden and psychological stress of CC worsen the impact on the families. It could be argued that higher treatment cost aggravates the financial burden and mental stress of the parents, and reduces their mastery capacity. To adjust to the impact of CC, families adopt diverse coping strategies like changed lifestyle, sought social support, religious dependency, and reduction in family investment. It could be claimed that the social, religious, economic, and moral states of the local context compelled the families to adopt these strategies.
4.1. Policy implications
The health care managers could use the study findings for devising effective strategies to make health services for CC available at all levels of health service delivery in Bangladesh. The study could contribute to minimizing the impact of CC on the families by establishing financial risk protection under the UHC throughout the country. The study findings also expect to open an avenue for policy-makers and health managers in the country and elsewhere in the developing world to comprehend the social and psychological impacts of CC considering the coping strategies adopted by the families.
4.2. Limitations of the study
The study result might not reflect the real picture of the country as it included only those children who enrolled in the selected tertiary care hospitals for diagnosis and treatment during a specific time period. Children who were treated at home and private hospitals could not be included in this study. Moreover, many children with cancer in Bangladesh reside in rural communities and never attend the tertiary hospitals for assessment and treatment. The original version of the IOF scale was not validated in the local context. Data were collected from the parents of children undergoing cancer treatment at the hospitals, which might have little influence on the responses.
5. Conclusion
Despite a few limitations, the study revealed the impact of CC on the family in many dimensions, such as financial burden, personal strain, social impact, and mastery. The mean scores of the domains of the IOF scale were significantly different by the employment status of parents, residing place, treatment cost, type, and duration of cancer. The families of children adopted diverse coping strategies like taking social support, performing a religious activity, minimizing family investment, changing lifestyle, and consolation as a consequence of fate. The cancer treatment facility is very scarce at primary and secondary levels of health service delivery in Bangladesh. Holistic medical and psychosocial measures are essential to strengthen the coping capacity for the families to accommodate the impact of CC. The study findings could contribute to devising effective interventions and programs to ensure financial risk protection and impact reduction for the families of children with CC within the UHC policy of Bangladesh.
Declarations
Author contribution statement
M.Z. Islam: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Wrote the paper.
S. Farjana: Conceived and designed the experiments; Analyzed and interpreted the data; Wrote the paper.
S.S. Efa: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
Data will be made available on request.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
Acknowledgements
The authors are indebted to the director of NIPSOM for technical and organizational supports; and all those who were involved in this research project: the co-investigators for their active contribution; administrative personnel and other workers at the tertiary hospitals for their sincere cooperation; and parents for their participation.
References
- 1.Islam S., Zafreen F., Karim S., Islam M.Z. Strategies adopted by families to overcome financial burden of childhood cancer. J. Armed Forces Med. Coll. Bangladesh. 2017;13(2):25–28. [Google Scholar]
- 2.World Health Organization Cancer in children. https://www.who.int/news-room/fact-sheets/detail/cancer-in-children Available online:
- 3.Johnston W.T., Erdmann F., Newton R., Steliarova-Foucher E., Schüz J., Roman E. Childhood cancer: estimating regional and global incidence. Canc. Epidemiol. 2020 Jan 8:101662. doi: 10.1016/j.canep.2019.101662. [DOI] [PubMed] [Google Scholar]
- 4.Magrath I., Steliarova-Foucher E., Epelman S., Ribeiro R.C., Harif M., Li C.K., Kebudi R., Macfarlane S.D., Howard S.C. Paediatric cancer in low-income and middle-income countries. Lancet Oncol. 2013 Mar 1;14(3):e104–e116. doi: 10.1016/S1470-2045(13)70008-1. [DOI] [PubMed] [Google Scholar]
- 5.Choudhury N.A., Selimuzzaman M., Belayet M. Childhood cancer a big burden of low middle income settings in Bangladesh: evidence from cross sectional study in Dhaka, Bangladesh. IOSR J. Dent. Med. Sci. 2019 May 15;18(5):52–61. [Google Scholar]
- 6.Hussain S.A., Sullivan R. Cancer control in Bangladesh. Jpn. J. Clin. Oncol. 2013 Dec 1;43(12):1159–1169. doi: 10.1093/jjco/hyt140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Aung L., Saw S.M., Chan M.Y., Khaing T., Quah T.C., Verkooijen H.M. The hidden impact of childhood cancer on the family: a multi-institutional study from Singapore. Ann. Acad. Med. Singapore. 2012 Apr 1;41(4):170. [PubMed] [Google Scholar]
- 8.Jackson A.C., Stewart H., O’Toole M., Tokatlian N., Enderby K., Miller J., Ashley D. Pediatric brain tumor patients: their parents’ perceptions of the hospital experience. J. Pediatr. Oncol. Nurs. 2007 Mar;24(2):95–105. doi: 10.1177/1043454206296030. [DOI] [PubMed] [Google Scholar]
- 9.Mardakis S., Arora R.S., Bakhshi S., Arora A., Anis H., Tsimicalis A. A qualitative study of the costs experienced by caregivers of children being treated for cancer in New Delhi, India. Canc. Rep. 2019 Jun;2(3):e1149. [Google Scholar]
- 10.Heath J.A., Lintuuran R.M., Rigguto G., Tikotlian N., McCarthy M. Childhood cancer: its impact and financial costs for Australian families. Pediatr. Hematol. Oncol. 2006 Jan 1;23(5):439–448. doi: 10.1080/08880010600692526. [DOI] [PubMed] [Google Scholar]
- 11.Khasru A.A. Childhood cancer: a situation analysis and challenges, Bangladesh perspective. Bangladesh J. Child Health. 2017;41(3):140–142. [Google Scholar]
- 12.Castellano-Tejedor C., Blasco-Blasco T., Pérez-Campdepadrós M., Capdevila L. The hidden sufferers: parental reactions to childhood cancer during treatment and at survival. Spanish J. Psychol. 2017;20 doi: 10.1017/sjp.2017.26. [DOI] [PubMed] [Google Scholar]
- 13.Fahim S.M., Bhuayan T.A., Hassan M.Z., Zafr A.H.A., Begum F., Rahman M.M., Alam S. Financing health care in Bangladesh: policy responses and challenges towards achieving universal health coverage. Int. J. Health Plann. Manag. 2019 Jan;34(1):e11–e20. doi: 10.1002/hpm.2666. [DOI] [PubMed] [Google Scholar]
- 14.Joarder T., Chaudhury T.Z., Mannan I. Universal health coverage in Bangladesh: activities, challenges, and suggestions. Adv. Publ. Health. 2019;(3):1–12. doi: 10.1155/2019/4954095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Knapp C., Madden V., Shenkman F. Institute for Child Health Policy, University of Florida; USA: 2006-2007. Children’s Medical Services Network, Partners in Care: Together for Kids; pp. 1–38. [Google Scholar]
- 16.Kolk A.M., Schipper J.L., Hanewald G.J., Casari E.F., Fantino A.G. The Impact-On-Family Scale: a test of invariance across culture. J. Pediatr. Psychol. 2000 Jul 1;25(5):323–329. doi: 10.1093/jpepsy/25.5.323. [DOI] [PubMed] [Google Scholar]
- 17.Ward E., DeSantis C., Robbins A., Kohler B., Jemal A. Childhood and adolescent cancer statistics, 2014. CA A Cancer J. Clin. 2014 Mar;64(2):83–103. doi: 10.3322/caac.21219. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available on request.