Sir,
In order to promote equitable and efficient allocation of coronavirus disease 2019 (COVID-19) vaccines, the World Health Organization (WHO) Strategic Advisory Group of Experts on Immunization (WHO-SAGE-I) has published a ‘Roadmap for Prioritizing Uses of COVID-19 Vaccines in the Context of Limited Supply’, outlining which groups should be prioritized under various supply scenarios [1].
Healthcare workers (HCWs) at high or very high risk of acquiring and transmitting severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) are included in Stage I when supply is very limited.
Wang et al. (2020) [2] estimated the target population sizes of priority groups for vaccination, including HCWs. However, their estimate was based on the number of doctors, nurses and midwives alone, and they did not attempt to stratify by risk. The present study expanded the definition of an HCW to match the WHO definition more closely, and compared risk across key HCW groups to determine which occupations are associated with the highest risk. The findings suggest that the majority of HCWs (approximately 70–90%) could be considered at high risk, and sparsity of country-level data means that effective risk stratification would be challenging to implement at programmatic level.
WHO defines HCWs as ‘all people engaged in work actions whose primary intent is to improve health’ [1]. This is intended to include not only health professionals, but health management and support personnel [3]. For this analysis, all those classified as health professionals (Sub-major Group 22) and health associate professionals (Sub-major Group 32) in the International Standard Classification of Occupations (ISCO-08) were included. For the 111 countries which report values for these two categories in ILOSTAT [4], the healthcare workforce constitutes, on average, <1% [0.80%, interquartile range (IQR) 0.39–1.53] of the national population [5].
The definition of high risk in the WHO-SAGE-I Roadmap is based on exposure to suspected or confirmed cases of COVID-19, or risk of exposure to aerosols with SARS-CoV-2. However, several studies have reported comparable or even higher infection rates in HCWs on general wards compared with COVID-19 wards [6], and others have reported higher risk of severe COVID-19 in medical support staff compared with health professionals [7]. These findings suggest that access to personal protective equipment and testing capacity may have a more substantial impact on risk than exposure to confirmed cases of COVID-19, given the risk posed by patients with asymptomatic or undiagnosed infection.
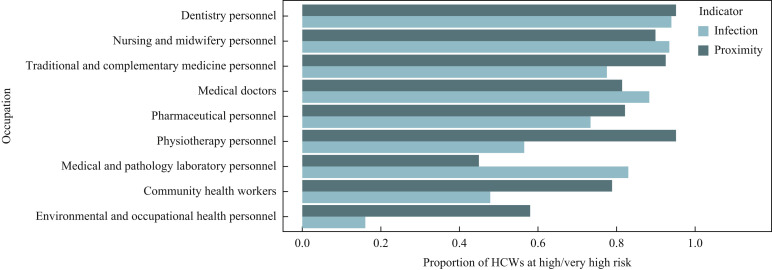
This study compared the risk of SARS-CoV-2 infection across key groups of healthcare occupations listed in the Global Health Observatory (GHO) [8], using data from surveys of US employees reported in the O∗NET database [9]. ‘Exposure to disease or infections’ and ‘physical proximity’ were used as proxy indicators for risk of SARS-CoV-2 infection. The ISCO-08 codes listed in the GHO were mapped to occupations in the O∗NET database. The mean proportion at high risk was then generated for each GHO group, with a weighting determined by the number of individuals in the USA employed in each occupation [10]. For both indicators, dentistry was the group in which the highest proportion of workers were found to be at high risk (Figure 1 ). Using the ‘physical proximity’ indicator, the proportion at high risk was approximately 80% or higher for all groups except ‘environmental and occupational health’ and ‘medical and pathology laboratory personnel’. These results emphasize that a limited definition of HCW may exclude occupations associated with the highest risk. Doctors, nurses and midwives only constitute 65.9% [95% confidence interval (CI) 60.0–72.8] of the total number of health professionals and health associate professionals.
Figure 1.
Proportion of healthcare workers (HCWs) at high risk by occupational group.
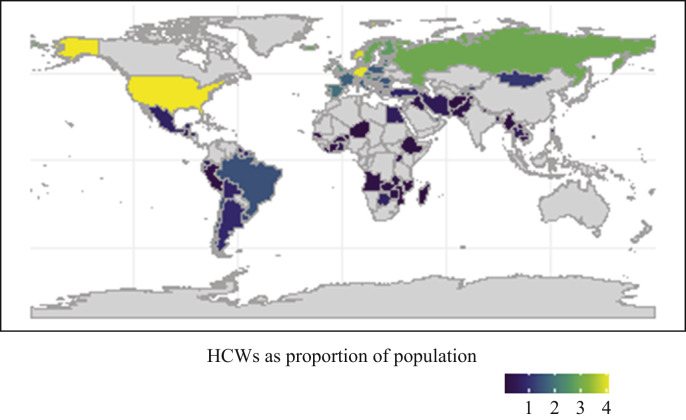
Country-level estimates for the number of HCWs at high risk were generated by mapping occupations listed as health professionals or health associate professionals in ISCO-08 on to the O∗NET occupations. Using the ‘exposure to disease or infections’ indicator, 85.2% (95% CI 83.5–87.0%) of health professionals and 74.0% (71.8–76.1%) of health associate professionals were estimated to be at high or very high risk. The ‘physical proximity’ indicator produced similar estimates of 86.7% (95% CI 85.0–88.3%) for health professionals and 83.7% (95% CI 81.9–85.6%) for health associate professionals. When these proportions were applied to the country estimates for these groups from ILOSTAT, HCWs at high risk constituted 0.64% (IQR 0.30–1.24) of the national population when using the ‘exposure to disease or infections’ indicator, and 0.68% (IQR 0.33–1.30) when using the ‘physical proximity’ indicator (Figure 2 ).
Figure 2.
National estimates for total size of the healthcare workforce as a proportion of national population. HCWs, healthcare workers.
Using this approach to estimate the proportion of HCWs at high risk globally does require extrapolation of data on working conditions in the USA to all countries in the world. It also relies on proxy indicators that do not relate specifically to risk of SARS-CoV-2 infection. However, the issue of sparsity of country-specific data on the risk of infection is not just a limitation of this analysis – it indicates that effectively identifying and vaccinating HCWs at high risk could be extremely logistically challenging.
Therefore, rather than narrowing down the estimate provided by Wang et al. [2], it is suggested that the net should be widened. There is evidence that basing estimates for the number of HCWs on doctors, nurses and midwives alone excludes some of the occupations at the highest risk. The results also suggest that the majority of HCWs could be considered at high risk (70–90%). Given that HCWs only constitute, on average, approximately 1% of the national population, it is argued that the benefit of prioritizing the vaccination of HCWs at high risk may not compensate for the additional logistical challenges of identifying those HCWs at highest risk.
Acknowledgements
CMMID COVID-19 Working Group members: Rosalind M. Eggo, Gwenan M. Knight, Stefan Flasche, Anna M. Foss, Petra Klepac, Yalda Jafari, Naomi R. Waterlow, Sophie R. Meakin, Jiayao Lei, C. Julian Villabona-Arenas, Simon R. Procter, Sam Abbott, Sebastian Funk, Nikos I. Bosse, Kathleen O'Reilly, William Waites, Kaja Abbas, Amy Gimma, Alicia Showering, Christopher I. Jarvis, Adam J. Kucharski, Akira Endo, Thibaut Jombart, Graham Medley, Oliver Brady, Rosanna C. Barnard, Jack Williams, Nicholas G. Davies, W. John Edmunds, James D. Munday, Carl A.B. Pearson, Yang Liu, Katherine E. Atkins, Hamish P. Gibbs, Timothy W. Russell, Damien C. Tully, Rachel Lowe, Samuel Clifford, Emily S. Nightingale, Joel Hellewell, Alicia Rosello, Matthew Quaife, Fabienne Krauer, Yung-Wai Desmond Chan, Fiona Yueqian Sun, Kevin van Zandvoort, Billy J. Quilty, Mihaly Koltai and Kiesha Prem.
Contributor Information
CMMID COVID-19 Working Group:
R.M. Eggo, G.M. Knight, S. Flasche, A.M. Foss, P. Klepac, Y. Jafari, N.R. Waterlow, S.R. Meakin, J. Lei, C.J. Villabona-Arenas, S.R. Procter, S. Abbott, S. Funk, N.I. Bosse, K. O'Reilly, W. Waites, K. Abbas, A. Gimma, A. Showering, C.I. Jarvis, A.J. Kucharski, A. Endo, T. Jombart, G. Medley, O. Brady, R.C. Barnard, J. Williams, N.G. Davies, W.J. Edmunds, J.D. Munday, C.A.B. Pearson, Y. Liu, K.E. Atkins, H.P. Gibbs, T.W. Russell, D.C. Tully, R. Lowe, S. Clifford, E.S. Nightingale, J. Hellewell, A. Rosello, M. Quaife, F. Krauer, Y.-W. Desmond Chan, F.Y. Sun, K. van Zandvoort, B.J. Quilty, M. Koltai, and K. Prem
Conflict of interest statement
None declared.
Funding sources
This research was funded by the National Institute for Health Research (NIHR) Health Protection Research Unit in Immunization at the London School of Hygiene and Tropical Medicine in partnership with Public Health England. The views expressed are those of the authors and not necessarily those of the National Health Service, NIHR, UK Department of Health or Public Health England.
Funding for the CMMID COVID-19 Working Group is as follows. RME: HDR UK (grant: MR/S003975/1), MRC (grant: MC_PC 19065), NIHR (grant: NIHR200908). GMK: UK Medical Research Council (grant: MR/P014658/1). SFlasche: Wellcome Trust (grant: 208812/Z/17/Z). PK: Royal Society (award RP/EA/180004), European Commission (101003688), Bill & Melinda Gates Foundation (INV-003174). YJ: LSHTM, DHSC/UKRI COVID-19 Rapid Response Initiative. NRW: Medical Research Council (grant: MR/N013638/1). SRM: Wellcome Trust (grant: 210758/Z/18/Z). JYL: Bill & Melinda Gates Foundation (INV-003174). CJVA: European Research Council Starting Grant (757688). SRP: Bill and Melinda Gates Foundation (INV-016832). SA: Wellcome Trust (grant: 210758/Z/18/Z). SFunk: Wellcome Trust (grant: 210758/Z/18/Z), NIHR (NIHR200908). NIB: Health Protection Research Unit (grant:NIHR200908). KO'R: Bill and Melinda Gates Foundation (OPP1191821). WW: MRC (grant: MR/V027956/1). KA: Bill & Melinda Gates Foundation (OPP1157270, INV-016832). AG: European Commission (EpiPose 101003688). MJ: Gates (INV-003174, INV-016832), NIHR (16/137/109, NIHR200929, NIHR200908), European Commission (EpiPose 101003688). CIJ: Global Challenges Research Fund (GCRF) project ‘RECAP’ managed through RCUK and ESRC (ES/P010873/1). AJK: Wellcome Trust (grant: 206250/Z/17/Z), NIHR (NIHR200908). AE: The Nakajima Foundation. TJ: RCUK/ESRC (grant: ES/P010873/1), UK PH RST, NIHR HPRU Modelling & Health Economics (NIHR200908). GFM: NTD Modelling Consortium by the Bill and Melinda Gates Foundation (OPP1184344). OJB: Wellcome Trust (grant: 206471/Z/17/Z). RCB: European Commission (EpiPose 101003688). JW: NIHR Health Protection Research Unit and NIHR HTA. NGD: UKRI Research England, NIHR Health Protection Research Unit in Immunisation (NIHR200929), UK MRC (MC_PC_19065). WJE: European Commission (EpiPose 101003688), NIHR (NIHR200908). JDM: Wellcome Trust (grant: 210758/Z/18/Z). CABP: Bill & Melinda Gates Foundation (OPP1184344) and the UK Foreign, Commonwealth and Development Office (FCDO)/Wellcome Trust Epidemic Preparedness Coronavirus Research Programme (ref. 221303/Z/20/Z). YL: Gates (INV-003174), NIHR (16/137/109), European Commission (101003688). KEA: European Research Council Starting Grant (757688). FGS: NIHR Health Protection Research Unit in Modelling & Health Economics, and in Immunisation. HPG: CSIGN which is part of the EDCTP2 programme supported by the European Union (grant: RIA2020EF-2983-CSIGN), Department of Health and Social Care (PR-OD-1017-20001). TWR: Wellcome Trust (grant: 206250/Z/17/Z). RL: Royal Society Dorothy Hodgkin Fellowship. SC: Wellcome Trust (grant: 208812/Z/17/Z). ESN: Gates (OPP1183986). JH: Wellcome Trust (grant: 210758/Z/18/Z). AR : NIHR (grant: PR-OD-1017-20002). MQ: European Research Council Starting Grant (#757699), Bill and Melinda Gates Foundation (INV-001754). FK: Innovation Fund of the Joint Federal Committee (grant: 01VSF18015), Wellcome Trust (UNS110424). FYS: NIHR EPIC (grant:16/137/109). KvZ: UK Foreign, Commonwealth and Development Office (FCDO)/Wellcome Trust Epidemic Preparedness Coronavirus Research Programme (ref. 221303/Z/20/Z), Elrha’s Research for Health in Humanitarian Crises (R2HC) Programme. BJQ: NIHR (16/137/109 & 16/136/46). BJQ: Bill and Melinda Gates Foundation (OPP1139859). MK: Foreign, Commonwealth and Development Office/Wellcome Trust. KP: Gates (INV-003174), European Commission (101003688).
References
- 1.World Health Organization . WHO; Geneva: 2020. WHO SAGE Roadmap for Prioritizing Uses of COVID-19 Vaccines in the Context of Limited Supply. [Google Scholar]
- 2.Wang W., Wu Q., Yang J., Dong K., Chen X., Bai X. Global, regional, and national estimates of target population sizes for COVID-19 vaccination: descriptive study. BMJ. 2020;371 doi: 10.1136/bmj.m4704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.World Health Organization . WHO; Geneva: 2008. Classifying health workers: mapping occupations to the international standard classification.http://www.who.int/hrh/statistics/workforce_statistics/en/ Available at: [last accessed February 2021] [Google Scholar]
- 4.International Labour Organization. Employees by sex and occupation – ILO modelled estimates. Geneva: ILOSTAT; n.d. Available at: https://ilostat.ilo.org/data [last accessed January 2021].
- 5.World Bank Group. Population estimates and projections. Washington, DC: World Bank; n.d. Available at: https://datacatalog.worldbank.org/dataset/population-estimates-and-projections [last accessed January 2021].
- 6.Lai X., Wang M., Qin C., Tan L., Ran L., Chen D. Coronavirus disease 2019 (COVID-2019) infection among health care workers and implications for prevention measures in a tertiary hospital in Wuhan, China. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.9666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Mutambudzi M., Niedwiedz C., Macdonald E.B., Leyland A., Mair F., Anderson J. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2020 doi: 10.1136/oemed-2020-106731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.World Health Organization . WHO; Geneva: 2018. The 2018 update, global health workforce statistics.http://www.who.int/hrh/statistics/hwfstats/ Available at: [last accessed January 2021] [Google Scholar]
- 9.O∗NET Resource Center. Work context – O∗NET 25.1 data dictionary. Available at: https://www.onetcenter.org/dictionary/25.1/excel/work_context.html [last accessed January 2021].
- 10.US Bureau of Labor Statistics. Occupational employment statistics. Washington, DC: Department of Labor; n.d. Available at: www.bls.gov/oes/[last accessed November 2020].