Abstract
Background
A community lockdown has a profound impact on its citizens. Our objective was to identify changes in trauma patient demographics, volume, and pattern of injury following the COVID-19 lockdown.
Methods
A retrospective review was conducted at a Level-1 Trauma Center from 2017 to 2020.
Results
A downward trend in volume is seen December–April in 2020 (R2 = 0.9907). February through April showed an upward trend in 2018 and 2019 (R2= 0.80 and R2 = 0.90 respectively), but a downward trend in 2020 (R2 = 0.97). In April 2020, there was 41.6% decrease in total volume, a 47.4% decrease in blunt injury and no decrease in penetrating injury. In contrast to previous months, in April the majority of injuries occurred in home zip codes.
Conclusions
A community lockdown decreased the number of blunt trauma, however despite social distancing, did not decrease penetrating injury. Injuries were more likely to occur in home zip codes.
Keywords: COVID-19, TRAUMA, COMMUNITY LOCKDOWN, TRENDS
Introduction
The World Health Organization designated COVID-19 a global pandemic on March 16, 2020.1 In the preceding weeks most cities around the world implemented a “Stay at Home” order, for all residents not considered essential workers. A stay at home order was issued in Illinois on March 21, 2020. A community lockdown as such has a profound social, psychological, and economic impact on its citizens.2, 3, 4 These new circumstances likely result in changes in the volume and pattern of injury for the trauma patient population. However, the direction of these changes is currently unclear.
Trauma in the midst of this pandemic puts further stress on the already strained healthcare system.5 Trauma patients often require critical limited resources such as blood products, intensive care unit beds, and ventilators.6 Due to the stay at home order, social blood drives are limited, leading to the potential shortage of blood products that are often required during a trauma resuscitation. This coupled with shortages of personal protective equipment and a restricted number of personnel, serves as a healthcare dilemma.7
Numerous studies looking at data from previous outbreaks including SARS, Ebola, H1N1 and the Middle East respiratory syndrome identified a significant psychologic burden associated with quarantines.2, 3, 4 , 8, 9, 10, 11, 12 Studies have reported high symptoms of depression, anxiety, emotional disturbance, stress and post-traumatic stress disorder, as well as anger.3 , 4 , 9 , 13 The closure of non-essential businesses has resulted in an overwhelming economic burden.15 , 16 This disproportionally affects members of specific racial and socioeconomic groups as most layoffs and furloughs are occurring in the low and middle income groups, while the majority of high income groups have transitioned to working from home.17
The purpose of this study was to identify changes in patient demographics, volume, and pattern of injury resulting from the COVID-19 lockdown. With accurate and current data, targeted preventive measures can better address violence and its consequences during a time of potential resource scarcity.
Materials and methods
Study design and setting
Following Institutional Review Board approval, a retrospective chart review was conducted at an urban, Level-1 Trauma Center in Chicago, Illinois. Patients who presented between December and April for the years 2018, 2019, and 2020 were identified. In our study design, the year 2018 was defined as December 2017 through April 2018. The year 2019 was defined as December 2018 through April 2019. The year 2020 was defined as December 2019 through April 2020. December was chosen to be the first month of our comprehensive analysis as that is when the first cases of SARS- CoV-2 were reported in China and it seemed possible that some might have started altering their behavior in response to media reports. Additionally, we focused our analysis more intensely on the months of February through April. This specific analysis was conducted as we elected to examine the month prior and the month following the stay at home order of Illinois (March 21, 2020). We analyzed a three year period in order to identify trends in the year of 2020 and compare to years prior.
Inclusion criteria encompassed all patients with a trauma activation either directly admitted or transferred from an outside hospital. Patients seen for a trauma follow-up, burn follow-up or wound follow-up were excluded. Patients with missing variables in the database were also excluded from analysis. Variables analyzed included age, gender, Injury Severity Score (ISS), injury mechanism (Blunt; Penetrating), ethanol and/or drug use, injury location zip code, home zip code, comorbidities and complications. Using the same categories of complications as defined by the National Trauma Data Bank, we collected data on pneumonia, unplanned return to the ICU, stroke, urinary tract injury, acute kidney injury, decubitus ulcer, pulmonary embolism, acute lung injury, severe sepsis, deep vein thrombosis, cardiac arrest with resuscitative efforts by healthcare provider, drug or alcohol withdrawal syndrome, unplanned return to the operation room, organ/space surgical site infection, deep surgical site infection, myocardial infarction, catheter-related blood stream infection, osteomyelitis, extremity compartment syndrome, superficial surgical site infection and graft/prosthesis/flap failure.
Statistical analysis
IBM SPSS® software platform was used to analyze the data. Linear regression was performed to identify changes in volume and pattern of injury during this period. Student T test, Chi-Square test and ANOVA were used for univariate analyses. A Student T test was used for comparisons of numerical data. A Chi-Square test and ANOVA was used for comparisons of nominal data and the Bonferroni correction was applied for multiple comparisons (p-value <0.05 was considered statistically significant). The subscript letters a, b and ab represent a category whose proportions do not differ significantly from each other at the 0.05 level. If they do not share a subscript, they are significantly different. The values with the same subscript letter represent categories whose proportions did not differ significantly from each other at the 0.05 level. Nominal data are presented as number and percentage, whereas numerical data are presented as mean with standard deviation (SD).
Results
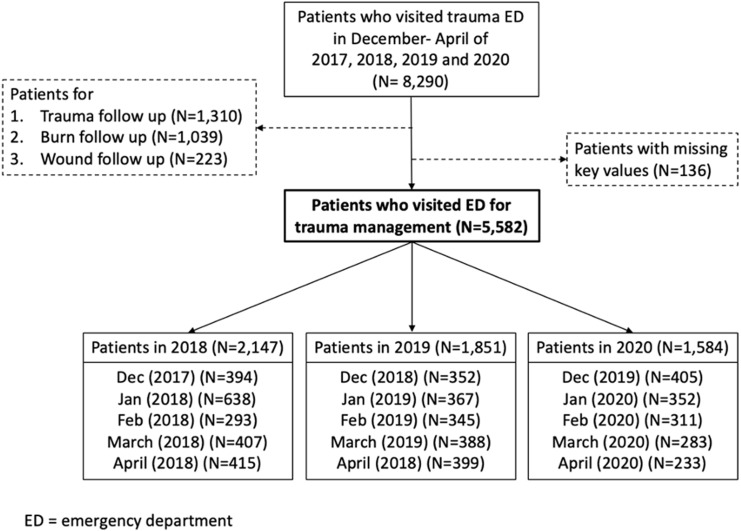
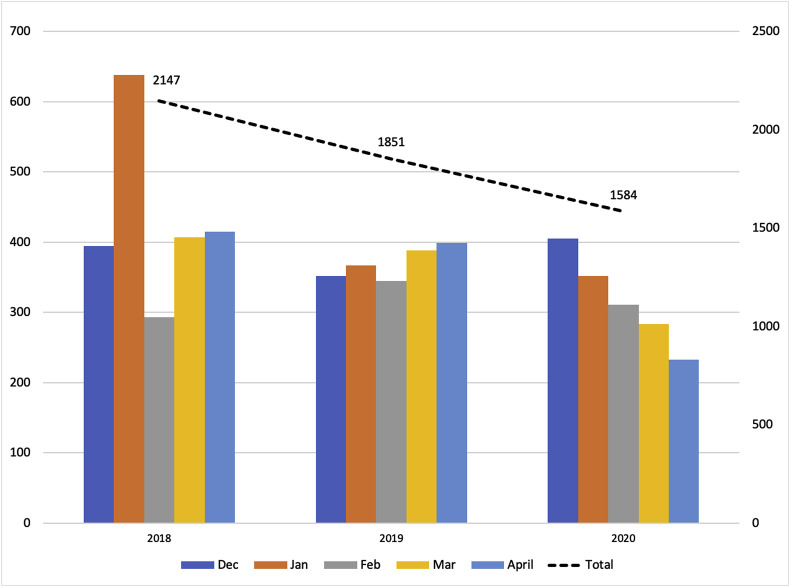
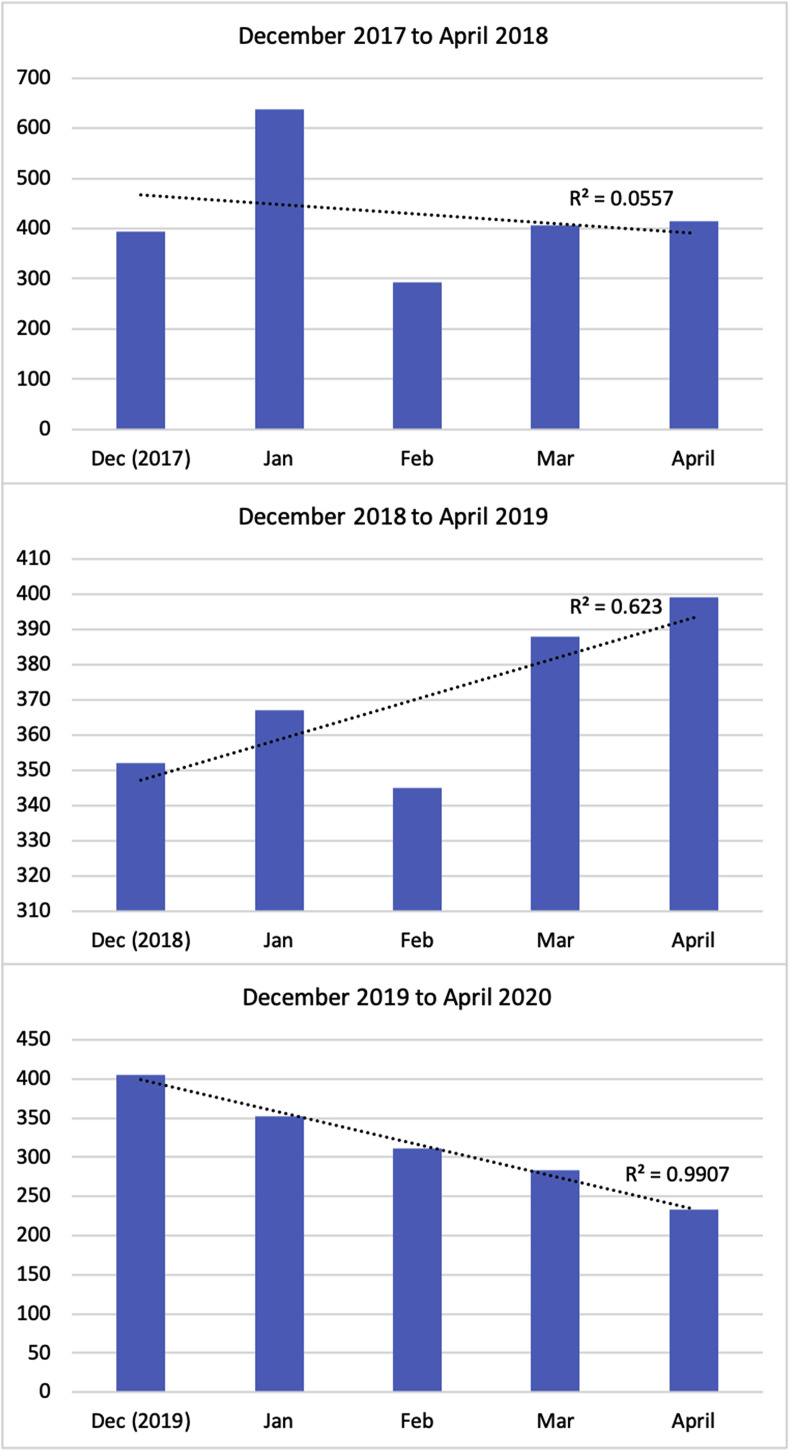
There was a total of 8290 trauma patient visits from December through April for the years 2017–2020. Following the exclusion of patients who presented for follow-up (n = 2572) and those with missing variables (n = 136) there were a total of 5582 patients who presented for trauma management. Study design and total patient distribution can be seen in Fig. 1 . A decrease in total number of trauma patients in the year of 2020 is seen in comparison to the years prior (n = 1584 < 1851 < 2147) (Fig. 2 a). When trending total number of trauma patients from December through April there is a statistically significant downward trend in 2020 (R2 = 0.9907). No such trend was seen in 2018 (R2 = 0.0557) and a moderate upward trend was seen in 2019 (R2 = 0.623).
Fig. 1.
Patient distribution.
Fig. 2a.
Trauma patients number per year (December–April; 2017–2020).
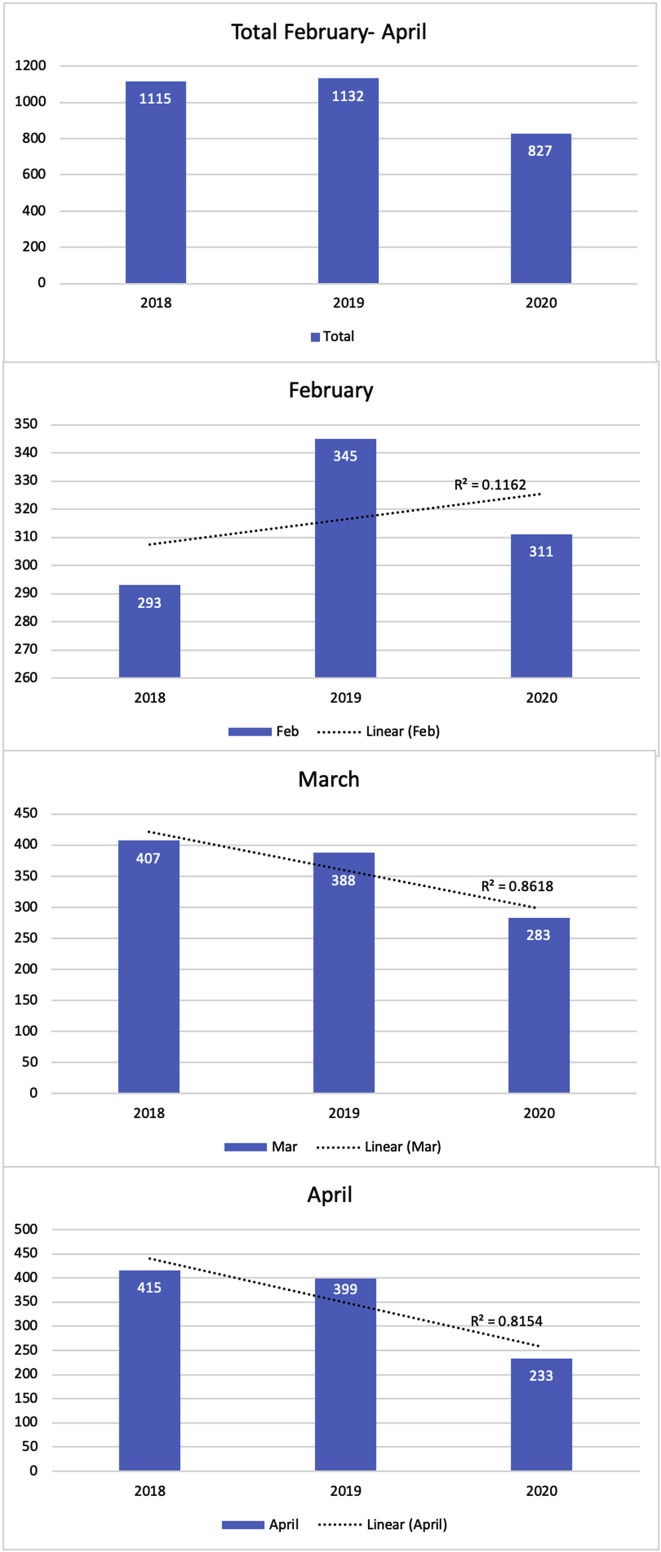
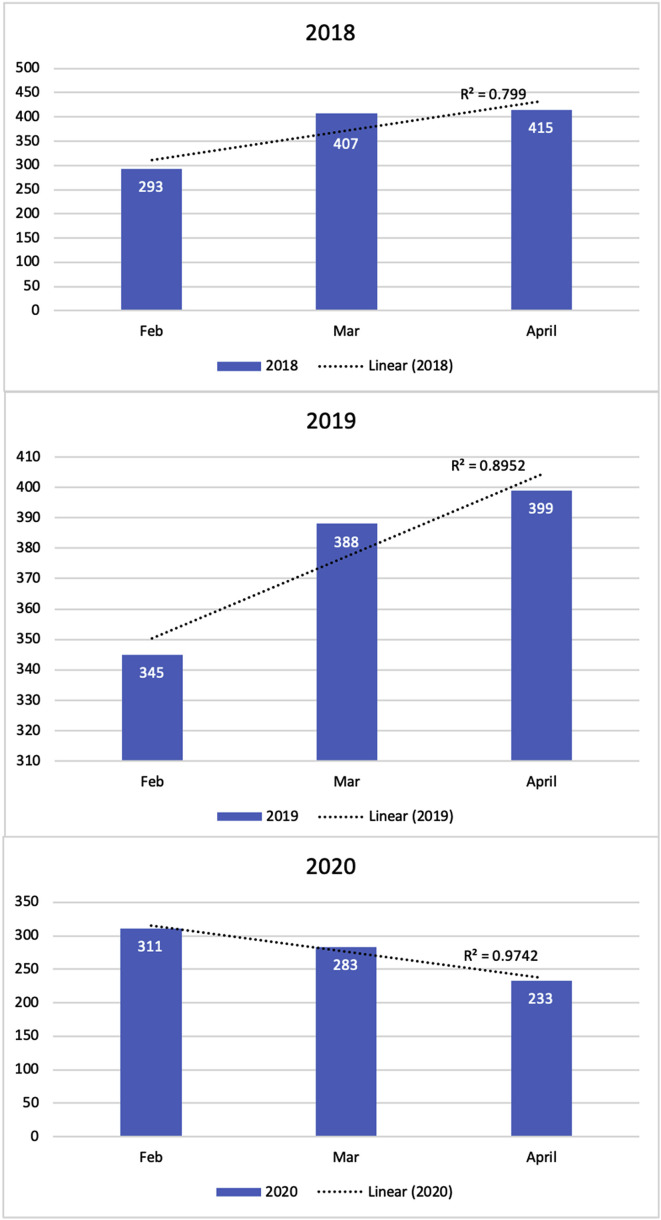
When specifically analyzing the months surrounding the stay at home order, February through April, similar numbers are seen in total number of trauma patients for 2018 and 2019 (n = 1115 and 1132 respectively (Fig. 3 a). There was however a 26.9% (n = 827) decline in 2020 overall, and a 41.6% decrease in April 2020 alone. When trending these numbers across the three years, no trend is identified for the month of February (R2 = 0.1162). There is, however, a downward trend seen in March and April (R2 = 0.8618 and 0.8154, respectively).
Fig. 3a.
Number of trauma patients per year (Feb–April; 2018–2020).
When trending the number of patients from February through April, a significant upward trend in the number of trauma patients is seen in both 2018 and 2019 (R2 = 0.799 and 0.8952 respectively). This is in contrast to a statistically significant downward trend for the year of 2020 (R2 = 0.9742) (Fig. 3 b).
Fig. 3b.
Trend in trauma patients per month (Feb–April; 2018–2020).
Trauma patient characteristics classified per month can be seen in Table 1 . When comparing April 2019 with April 2020, there was a 47.4% decrease in blunt trauma (n = 119 from 226), however there was no change in the number of penetrating injuries (n = 73 vs. 72). This accounts for a relative increase in percent penetrating trauma from 18.5% to 31.3% from the year prior. An 88% decrease in burn injury (n = 5 vs. 42) as well as percent of female trauma patients (20.2% from 32.3%) was also seen. There was no significant difference in complication rate between April 2019 and April 2020. The complication rates for February, March and April in 2020 were 3.2%, 0.4% and 3.95% respectively (p = 0.018). There was no significant difference in complication rates between February and April in 2020. The complication rates in 2019 were 5.8%, 5.4% and 5.0% respectively (p = 0.89).
Table 1.
Characteristics of trauma patients.
| 2017 December (N = 394) |
2018 December (N = 352) |
2019 December (N = 405) |
p-value |
||
| Age |
35.6 ± 19.9 |
36.3 ± 17.7 |
39.2 ± 19.2 |
0.017a |
|
| Gender (N, %) | 0.045b | ||||
| Male | 279 (70.8%) | 277 (78.7%) | 297 (73.3%) | ||
| Female |
115 (29.2%) |
75 (21.3%) |
108 (26.7%) |
||
| ISS |
6.1 ± 6.4 |
4.3 ± 6.1 |
4.7 ± 6.5 |
0.003a |
|
| Trauma mechanism (N, %) | <0.001b | ||||
| Blunt | 215 (54.6%) | 168 (47.7%) | 211 (52.1%) | ||
| Penetrating | 75 (19.0%) | 64 (18.2%) | 58 (14.3%) | ||
| Burn | 48 (12.2%) | 58 (16.5%) | 26 (6.4%) | ||
| Other or unknown | 56 (14.2%) | 62 (17.6%) | 110 (27.2%) | ||
| Ethanol use (N, %) |
75 (19.0%) |
47 (13.4%) |
57 (14.1%) |
0.060b |
|
| Drug use (N, %) |
66 (16.8%) |
70 (19.9%) |
64 (15.6%) |
0.398b |
|
| Comorbidity (N, %) |
87 (22.1%) |
37 (10.5%) |
36 (8.9%) |
<0.001b |
|
| Complication (N, %) |
1 (0.3%) |
3 (0.9%) |
8 (2.0%) |
0.052b |
|
| 2018 January (N = 638) |
2019 January (N = 367) |
2020 January (N = 352) |
p-value |
||
| Age |
35.5 ± 18.5 |
38.4 ± 19.8 |
38.6 ± 19.6 |
0.016a |
|
| Gender (N, %) | 0.136b | ||||
| Male | 477 (74.8%) | 253 (68.9%) | 256 (72.7%) | ||
| Female |
161 (25.2%) |
114 (31.1%) |
96 (27.3%) |
||
| ISS |
5.7 ± 9.2 |
4.0 ± 4.0 |
4.9 ± 5.2 |
0.006a |
|
| Trauma mechanism (N, %) | <0.001b | ||||
| Blunt | 203 (31.8%) | 197 (53.7%) | 192 (54.5%) | ||
| Penetrating | 143 (22.4%) | 45 (12.3%) | 73 (20.7%) | ||
| Burn | 91 (14.3%) | 77 (21.0%) | 29 (8.2%) | ||
| Other or unknown |
201 (31.5%) |
48 (13.1%) |
58 (16.5%) |
||
| Ethanol use (N, %) |
63 (9.9%) |
49 (13.4%) |
58 (16.5%) |
0.009b |
|
| Drug use (N, %) |
54 (8.5%) |
64 (17.4%) |
61 (17.3%) |
<0.001b |
|
| Comorbidity (N, %) |
90 (14.1%) |
63 (17.2%) |
43 (12.2%) |
0.159b |
|
| Complication (N, %) |
0 (0.0%) |
18 (4.9%) |
14 (4.0%) |
<0.001b |
|
| 2018 February (N = 293) |
2019 February (N = 345) |
2020 February (N = 311) |
p-value |
||
| Age |
39.2 ± 19.7 |
40.9 ± 20.6 |
37.8 ± 19.6 |
0.132a |
|
| Gender (N, %) | 0.427b | ||||
| Male | 212 (72.4%) | 254 (73.6%) | 215 (69.1%) | ||
| Female |
81 (27.6%) |
91 (26.4%) |
96 (30.9%) |
||
| ISS |
4.1 ± 4.2 |
5.3 ± 6.7 |
5.4 ± 5.3 |
0.014a |
|
| Trauma mechanism (N, %) | <0.001b | ||||
| Blunt | 154 (52.6%) | 175 (50.7%) | 200 (64.3%) | ||
| Penetrating | 67 (22.9%) | 46 (13.3%) | 57 (18.3%) | ||
| Burn | 45 (15.4%) | 65 (18.8%) | 27 (8.7%) | ||
| Other or unknown |
27 (9.2%) |
59 (17.1%) |
27 (8.7%) |
||
| Ethanol use (N, %) |
46 (15.7%) |
51 (14.8%) |
49 (15.8%) |
0.927b |
|
| Drug use (N, %) |
57 (19.5%) |
73 (21.2%) |
71 (22.8%) |
0.497b |
|
| Comorbidity (N, %) |
64 (21.8%) |
63 (18.3%) |
34 (10.9%) |
0.001b |
|
| Complication (N, %) |
0 (0.0%) |
20 (5.8%) |
10 (3.2%) |
<0.001b |
|
| 2018 March (N = 407) |
2019 March (N = 388) |
2020 March (N = 283) |
p-value |
||
| Age |
36.3 ± 20.3 |
37.8 ± 19.0 |
37.4 ± 19.1 |
0.543a |
|
| Gender (N, %) | 0.395b | ||||
| Male | 288 (70.8%) | 291 (75.0%) | 208 (73.5%) | ||
| Female |
119 (29.2%) |
97 (25.0%) |
75 (26.5%) |
||
| ISS |
5.1 ± 5.5 |
4.7 ± 5.2 |
5.1 ± 5.5 |
0.704a |
|
| Trauma mechanism (N, %) | 0.004b | ||||
| Blunt | 223 (54.8%)a | 236 (60.8%)a | 168 (59.4%)a | ||
| Penetrating | 86 (21.1%)a | 62 (16.0%)a | 50 (17.7%)a | ||
| Burn | 50 (12.3%)a | 48 (12.4%)a | 16 (5.7%)b | ||
| Other or unknown |
48 (11.8%)ab |
42 (10.8%)b |
49 (17.3%)a |
||
| Ethanol use (N, %) |
72 (17.7%) |
73 (18.8%) |
65 (23.0%) |
0.208b |
|
| Drug use (N, %) |
77 (18.9%) |
99 (25.5%) |
68 (24.0%) |
0.009b |
|
| Comorbidity (N, %) |
64 (21.8%) |
63 (18.3%) |
34 (10.9%) |
0.001b |
|
| Complication (N, %) |
0 (0.0%) |
21 (5.4%) |
1 (0.4%) |
<0.001b |
|
| 2018 April (N = 415) |
2019 April (N = 399) |
2020 April (N = 233) |
p-value |
||
| Age |
36.7 ± 19.5 |
35.5 ± 19.9 |
37.2 ± 20.2 |
0.532a |
|
| Gender (N, %) | 0.004b | ||||
| Male | 304 (73.3%)ab | 270 (67.7%)b | 186 (79.8%)a | ||
| Female |
111 (26.7%)ab |
129 (32.3%)b |
47 (20.2%)a |
||
| ISS |
4.6 ± 5.3 |
5.2 ± 6.0 |
5.7 ± 5.8 |
0.404a |
|
| Trauma mechanism (N, %) | <0.001b | ||||
| Blunt | 226 (54.5%)a | 226 (56.6%)a | 119 (51.1%)a | ||
| Penetrating | 108 (26.0%)a | 74 (18.5%)b | 73 (31.3%)a | ||
| Burn | 47 (11.3%)a | 42 (10.5%)a | 5 (2.1%)b | ||
| Other or unknown |
34 (8.2%)a |
57 (14.3%)b |
36 (15.5%)b |
||
| Ethanol use (N, %) | 84 (20.2%) | 82 (20.6%) | 32 (13.7%) | 0.072b | |
|
79 (73.1%) |
51(68.9%) |
58 (79.5%) |
0.344b |
|
| Drug use (N, %) | 77 (18.6%) | 90 (22.6%) | 52 (22.3%) | 0.305b | |
|
23 (21.3%) |
32 (43.2%) |
17 (23.3%) |
0.009b |
|
| Comorbidity (N, %) | 71 (17.1%)a | 47 (11.8%)ab | 19 (8.2%)b | 0.003b | |
| Complication (N, %) | 0 (0.0%)a | 20 (5.0%)b | 9 (3.9%)b | <0.001b | |
Numerical data: mean ± standard deviation.
Nominal data: N (percentage).
a, b, ab: each subscript letter denotes a category whose proportions do not differ significantly from each other at the 0.05 level.
ANOVA test.
Chi-square test.
For April 2020, there was no difference in mean age, Injury Severity Score (ISS), or percent drug or ETOH use compared to both 2018 and 2019. For the month of April, ethanol use was seen in 20.2% and 20.6% of patients in 2018 and 2019 respectively, and 13.7% in 2020 (p = 0.072). Drug use was seen in 22.6% and 22.3% of patients in both 2019 and 2020 respectively. On further analysis when looking at penetrating trauma specifically, no significant difference in alcohol use was seen between the years 2018–2020 (n = 79 (73.1%), n = 51 (68.9%) and n = 58 (79.5%) respectively; p = 0.344); for drug use within the penetrating patient populations the numbers were 21.3%, 43.2% and 23.3% respectively for 2018, 2019 and 2020 (p = 0.009).
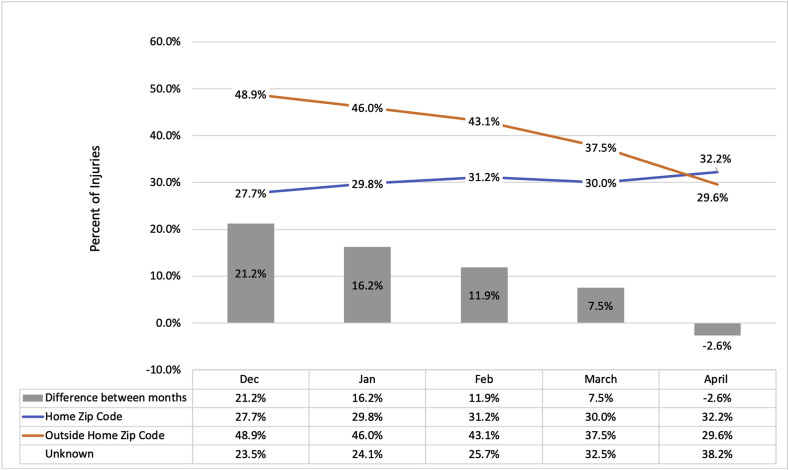
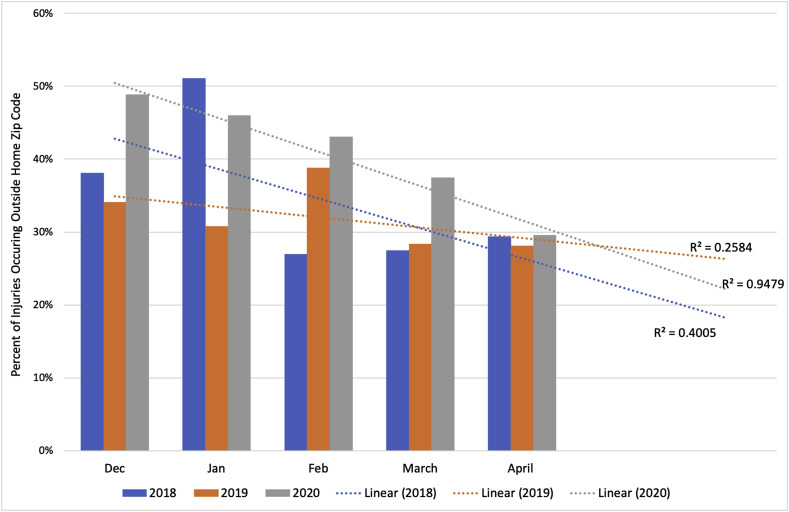
At the beginning of 2020, more injuries occurred outside of the home zip code than inside the home zip code (Fig. 4 ). As the year progressed, the gap in the number of injuries occurring outside versus inside the home zip code narrows, as injuries occurring outside of patients’ home zip codes were declining. In April, for the first time, there are more injuries occurring inside the home zip code (32.2%) than outside (29.6%). This downward trend was not seen in 2018 or 2019 (Fig. 5 ).
Fig. 4.
Trend in location of injury in the year 2020.
Fig. 5.
Percent of injuries occurring outside home zip code.
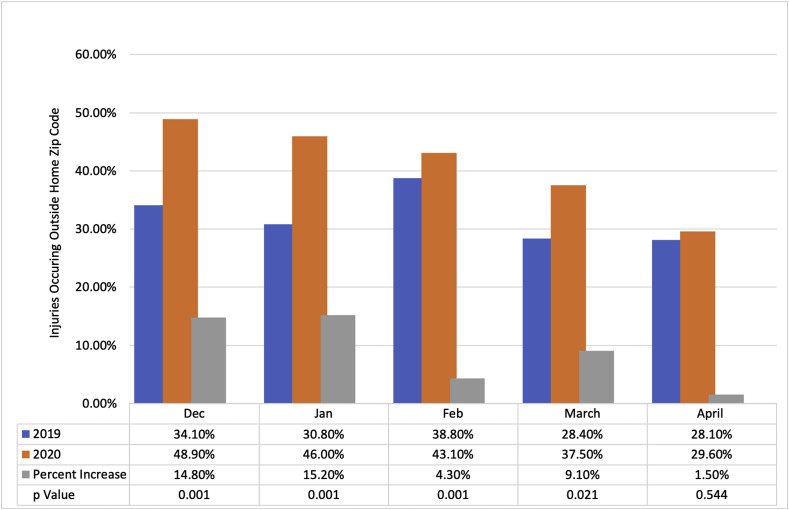
When evaluating the geographic location of where injuries occurred, there was a significant increase in percent of injuries occurring outside of the home zip code in 2020 in comparison to 2019 (Fig. 6 ). Between December and March injuries outside of home zip code increased from 34.1% to 48.9% (p < 0.001), 30.8%–46% (p < 0.001), 38.8%–43.1% (p < 0.001; subscript a, not significant on Post Hoc Bonferroni correction), and 28.4%–37.5% (p < 0.021), respectively. However, in April a significant increase between 2019 and 2020 was not seen (28.1%–29.6%, p = 0.544).
Fig. 6.
Increase in Injuries Occurring Outside Home Zip code Between 2019 and 2020.
Discussion
Historically, there is an increase in crime during times of financial uncertainty and desperation. According to the Chicago Police Department, many forms of crime including theft, burglary, sexual assault, and robbery have decreased in 2020 from 2019 (by −24%, −17%, −16%, −1% respectively from January to May 23). However, when looking at firearm-related injury specifically, there has been a 22% year to date increase in gun related incidences and a 14% percent year to date increase in murder rate in Chicago alone.18 This is comparable to that seen in New York City, Los Angeles, and Baltimore.19, 20, 21 Domestic violence has also increased in an alarming way this appears to be associated with community lockdowns.22, 23, 24, 25, 26, 27 With its increased sales and consumption during the COVID-19 pandemic,28 it has been proposed that alcohol intoxication plays a role in the increased violence seen.
In our study, a five month distribution was analyzed for the months of December through April to identify changes in volume and pattern of injury caused by the COVID-19 community lockdown. A decrease in total number of trauma patients is seen in 2020 (n = 1584) compared to 2019 and 2018 (n = 1851 and 2147 respectively) (Fig. 2a). The decrease in traumas between 2018 and 2019 is largely secondary to an isolated decline in cases for the month of January. Although causation cannot be objectively defined, it was thought to be multifactorial including increased funding and resources for violence reduction that were deployed as a result of the large spike in violence in Chicago in 2016. However, to better characterize this overall decrease in total number of trauma patients a linear regression analysis was performed (Fig. 2b). When trending total number of trauma patients from December through April there is a statistically significant downward trend in 2020 only (R2 = 0.9907). No such trend was seen in 2018 (R2 = 0.0557) and a moderate upward trend was seen in 2019 (R2 = 0.623). The significant down-trending R-squared value in 2020 verses the moderate uptrend of the R-squared value in 2019 is highly suggestive of COVID playing a contributing role in the decline in number of trauma patients in 2020.
Fig. 2b.
Trend in trauma patient number per month (Dec–April; 2017–2020).
On further linear regression analysis, specifically analyzing the months surrounding the stay at home order, a variation in the trend is identified. There was a 26.9% decline in total trauma patients in 2020 coinciding with significant downward trends in March and April (R2 = 0.86 and 0.82 respectively) following the say at home order. Prior to this order, in February of 2020, no trend is seen (R2 = 0.12, Fig. 3a). In April 2020, there was a 41.6% decrease in trauma patient volume, which is similar to the 43% decrease in total injury admissions seen in New Zealand29 and the reported 50% decline in total trauma cases in Italy.30 When observing the month to month trends, a significant increase is seen in 2018 and 2019 (R2 = 0.8 and 0.9 respectively). This is often attributed to warmer weather. This is in contrast to a significant downward trend in trauma volume from February through April for the year of 2020 (R2 = 0.97, Fig. 3b).
Following the lockdown, the number of blunt trauma patients decreased by 47.4%, however this decrease was not seen in penetrating trauma. Despite the stay at home order, the number of penetrating injury patients did not decrease. During the COVID-19 pandemic lockdown, the closure of non-essential businesses and social distancing led to a decrease in driving and motor vehicle collisions and thus the significant decrease in the blunt trauma seen in our patient population.31 Social distancing however did not decrease penetrating violence, and according to the Chicago Police Department firearm-related injury in fact increased by 22% from January to May. Our results do not take into consideration patients admitted to other institutions as well as those expired at the scene.
Similar to years prior, the majority of injuries did occur in males, however there was a percentage increase of 67.7%–80% in injuries occurring in males and a 12% decrease in injuries occurring in females. There was no change in age, severity of the injury, and in light of hospital oversaturation, there was no increase in complication rate in April 2020 compared to the year prior. Although there was a statistical increase in complication rates in April compared to March in 2020, the clinical significance of that increase is questionable given the inconsistent low value for March compared to all the values for the relevant months in 2019 and 2020.
Although the percentage of alcohol sales and consumption reportedly has increased during the COVID-19 pandemic,28 there was no evidence of an increase in either alcohol or drug use in our trauma patient population. In fact, in April there was a decrease in alcohol use from 20.6% to 13.7%, but was not found to be statistically significant (p = 0.07) (Table 1). On further analysis when looking at penetrating trauma specifically, no significant difference in alcohol use was seen (p = 0.344). In addition, there was no consistent relationship between drug use and penetrating trauma in April with values being 21.3%, 43.2% and 23.3% between 2018 and 2020 (p = 0.009). This is contrary to the belief that alcohol is a driving force for violence during the COVID-19 pandemic. According to our data, this suggests that substance abuse was not strongly associated with the violence seen in our patient population during this COVID-19 pandemic era.
In the setting of this community lockdown, it appeared people were abiding by the stay at home order. When trending percent of injuries occurring in the home zip code along-side those occurring outside of the home zip code for the year of 2020, the percent of injuries occurring outside decreased as the year progressed (Fig. 4). In April, for the first time, the percent of injuries occurring at home zip codes (32.2%) were higher compared to those occurring outside the home zip code (29.6%). This downward trend is only seen in the year 2020 (Fig. 5). In 2020, there was a jump in the percent of traumas occurring outside of the home zip code in comparison to 2019. Although the reason for more injuries occurring farther away from home in 2020 is undetermined, it is noted that no such increase in seen in April (Fig. 6).
Community lockdowns have significant psychological sequela,3 , 4 , 9 , 13 Contributing stressors included duration of quarantine, financial loss, and resource discrepancy.8 , 14 According to the U.S. Bureau of Labor Statistics, there was a 10.3% increase in the national unemployment rate in April alone. In Illinois there was a 12.3% unemployment rate increase in April with a jump from 4.2%. This is the largest spike seen in the history to date. The financial burden and resource disparity with the unemployment rate as high as 16.5% in April, has resulted in a significant stress burden.16 It is likely that this psychological recoil plays a significant role in sustained violence. Characteristics of those with higher risk factor for psychological consequences included those between ages 16–24 and with lower formal education,2 , 12 making our patient population particularly vulnerable.
Conclusion
A community lockdown decreased the total number of blunt trauma victims, however despite social distancing, did not decrease penetrating injury in our patient population. Injuries in April following the stay at home order, were more likely to occur within their home zip code. Resource allocation to combat financial, physical and psychological stressors is essential in violence prevention. Sustaining social support systems during this time should be emphasized. Resource preparation in the setting of continued violence should be anticipated in the hospital setting. Shifts in volume and pattern of injury should drive resource allocation and violence prevention.
Limitations
The limitations of our study include the retrospective nature of our study design. The dataset, like all data sets, is subject to inaccuracies in data input as well as missing data. Furthermore, our study was based off of one trauma centers experience and our results do not take into consideration patients admitted to other institutions as well as those expired at the scene.
Declaration of competing interest
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors. No authors have conflicts of interest to disclose.
Acknowledgments
Would like to thank the trauma department and staff for their exceptional hard work during this unprecedented time.
References
- 1.Icc-WHO Joint Statement . World Health Organization; 2020. An Unprecedented Private Sector Call to Action to Tackle COVID-19.https://www.who.int/news-room/detail/16-03-2020-icc-who-joint-statement-an-unprecedented-private-sector-call-to-action-to-tackle-covid-19 [Google Scholar]
- 2.Brooks S.W.R., Smith L., et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. 2020;395:912–920. doi: 10.1016/S0140-6736(20)30460-8. 10227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hawryluck L., Gold W.L., Robinson S., Pogorski S., Galea S., Styra R. SARS control and psychological effects of quarantine, Toronto, Canada. Emerg Infect Dis. 2004;10(7):1206–1212. doi: 10.3201/eid1007.030703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reynolds D.L., Garay J.R., Deamond S.L., Moran M.K., Gold W., Styra R. Understanding, compliance and psychological impact of the SARS quarantine experience. Epidemiol Infect. 2008;136(7):997–1007. doi: 10.1017/S0950268807009156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Coleman J.R., Burlew C.C., Platnick K.B., et al. Maintaining trauma care access during the COVID-19 pandemic: an urban, level-1 trauma center’s experience. Ann Surg. 2020;272(2):e58–e60. doi: 10.1097/SLA.0000000000004001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hatchimonji J.S., Swendiman R.A., Seamon M.J., Nance M.L. Trauma does not quarantine: violence during the COVID-19 pandemic. Ann Surg. 2020;272(2):e53–e54. doi: 10.1097/SLA.0000000000003996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Haut E.R., Leeds I., Livingston D.H. The effect on trauma care secondary to the COVID-19 pandemic: collateral damage from diversion of resources. Ann Surg. 2020;272(3):e204–e207. doi: 10.1097/SLA.0000000000004105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blendon R.J., Benson J.M., DesRoches C.M., Raleigh E., Taylor-Clark K. The public’s response to severe acute respiratory syndrome in Toronto and the United States. Clin Infect Dis. 2004;38(7):925–931. doi: 10.1086/382355. [DOI] [PubMed] [Google Scholar]
- 9.DiGiovanni C., Conley J., Chiu D., Zaborski J. Factors influencing compliance with quarantine in Toronto during the 2003 SARS outbreak. Biosecur Bioterror. 2004;2(4):265–272. doi: 10.1089/bsp.2004.2.265. [DOI] [PubMed] [Google Scholar]
- 10.Marjanovic Z., Greenglass E.R., Coffey S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: an online questionnaire survey. Int J Nurs Stud. 2007;44(6):991–998. doi: 10.1016/j.ijnurstu.2006.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rubin G.J., Wessely S. The psychological effects of quarantining a city. BMJ. 2020;368:m313. doi: 10.1136/bmj.m313. [DOI] [PubMed] [Google Scholar]
- 12.Taylor M.R., Agho K.E., Stevens G.J., Raphael B. Factors influencing psychological distress during a disease epidemic: data from Australia’s first outbreak of equine influenza. BMC Publ Health. 2008;8:347. doi: 10.1186/1471-2458-8-347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jeong Y.H., Song Y.-J., et al. Mental health status of people isolated due to Middle East respiratory syndrome. Epidemiol Health. 2016;38 doi: 10.4178/epih.e2016048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wilken J.A.P.P., Goode B., et al. Knowledge, attitudes, and practices among members of households actively monitored or quarantined to prevent transmission of Ebola virus disease. Prehospital Disaster Med. 2017;32:673–678. doi: 10.1017/S1049023X17006720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.State employment and unemployment summary- U.S. Bureau of labor unemployment Statistics. 2020. https://www.bls.gov/news.release/laus.nr0.htm 5/20/2020.
- 16.Local employment Statistics- United States department of labor. 2020. https://data.bls.gov/timeseries/LASST170000000000003 5/20/2020.
- 17.Talev M. Axios-Ipsos Coronavirus Index: rich sheltered, poor shafted amid virus. 2020. https://www.axios.com/axios-ipsos-coronavirus-index-rich-sheltered-poor-shafted-9e592100-b8e6-4dcd-aee0-a6516892874b.html Accessed 05/2020.
- 18.Department CP. Chicago Police department crime Statistics. 2020. https://home.chicagopolice.org/wp-content/uploads/2020/05/1_PDFsam_CompStat-Publc-2020-Week-21.pdf Updated 5/24/2020, 5/15/2020.
- 19.Department LAP. Los Angeles Police department crime citywide profile. 2020. http://assets.lapdonline.org/assets/pdf/cityprof.pdf 05/15/2020.
- 20.Sutherland M., McKenney M., Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York city, Chicago, Los Angeles and Baltimore. Am J Emerg Med. 2021;39:225–226. doi: 10.1016/j.ajem.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.New York Police department CompStat. 2020. https://www1.nyc.gov/assets/nypd/downloads/pdf/crime_statistics/cs-en-us-city.pdf Updated 5/31/2020.
- 22.Anurudran A., Yared L., Comrie C., Harrison K., Burke T. Domestic violence amid COVID-19. Int J Gynaecol Obstet. 2020;150(2):255–256. doi: 10.1002/ijgo.13247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kofman Y.B., Garfin D.R. Home is not always a haven: the domestic violence crisis amid the COVID-19 pandemic. Psychol Trauma. 2020;12(S1):S199–S201. doi: 10.1037/tra0000866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mazza M., Marano G., Lai C., Janiri L., Sani G. Danger in danger: interpersonal violence during COVID-19 quarantine. Psychiatr Res. 2020;289:113046. doi: 10.1016/j.psychres.2020.113046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sacco M.A., Caputo F., Ricci P., et al. The impact of the Covid-19 pandemic on domestic violence: the dark side of home isolation during quarantine. Med Leg J. 2020 doi: 10.1177/0025817220930553. 25817220930553. [DOI] [PubMed] [Google Scholar]
- 26.Telles L.E.B., Valenca A.M., Barros A.J.S., Da Silva A.G. Domestic violence in the COVID-19 pandemic: a forensic psychiatric perspective. Br J Psychiatry. 2020:S1516–44462020005015210. doi: 10.1590/1516-4446-2020-1060. S1516-44462020005015211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zero O., Geary M. COVID-19 and intimate partner violence: a call to action. R I Med J. 2013;103(5):57–59. 2020. [PubMed] [Google Scholar]
- 28.Rebalancing the ‘Covid-19 Effect’ on Alcohol Sales. The Nielsen Company LLC; 2020. https://www.nielsen.com/us/en/insights/article/2020/rebalancing-the-covid-19-effect-on-alcohol-sales/ [Google Scholar]
- 29.Christey G., Amey J., Campbell A., Smith A. Variation in volumes and characteristics of trauma patients admitted to a level one trauma centre during national level 4 lockdown for COVID-19 in New Zealand. N Z Med J. 2020;133(1513):81–88. [PubMed] [Google Scholar]
- 30.Fojut R. How coronavirus is affecting trauma systems in Italy. 2020. https://www.trauma-news.com/2020/03/how-coronavirus-is-affecting-trauma-systems-in-italy/
- 31.Illinois Fatal Crash Data for 2020. Illinois Department of Transportation; 2020. http://apps.dot.illinois.gov/fatalcrash/snapshot.html [Google Scholar]