Abstract
OBJECTIVE
Prediabetes has been suggested to increase risk for death; however, the definitions of prediabetes that can predict death remain elusive. We prospectively investigated the association of multiple definitions of prediabetes with the risk of death from all causes, cardiovascular disease (CVD), and cancer in Japanese workers.
RESEARCH DESIGN AND METHODS
The study included 62,785 workers who underwent a health checkup in 2010 or 2011 and were followed up for death from 2012 to March 2019. Prediabetes was defined according to fasting plasma glucose (FPG) or glycated hemoglobin (HbA1c) values or a combination of both using the American Diabetes Association (ADA) or World Health Organization (WHO)/International Expert Committee (IEC) criteria. The Cox proportional hazards regression model was used to investigate the associations.
RESULTS
Over a 7-year follow-up, 229 deaths were documented. Compared with normoglycemia, prediabetes defined according to ADA criteria was associated with a higher risk of all-cause mortality (hazard ratio [HR] 1.53; 95% CI 1.12–2.09) and death due to cancer (HR 2.37; 95% CI 1.45–3.89) but not with death due to CVD. The results were materially unchanged when prediabetes was defined according to ADA FPG, ADA HbA1c, WHO FPG, or combined WHO/IEC criteria. Diabetes was associated with the risk of all-cause, CVD, and cancer deaths.
CONCLUSIONS
In a cohort of Japanese workers, FPG- and HbA1c-defined prediabetes, according to ADA or WHO/IEC, were associated with a significantly increased risk of death from all causes and cancer but not CVD.
Introduction
Globally, an estimated 451 million and 352.1 million people are living with diabetes and prediabetes, respectively, and these numbers are expected to increase to 693 million and 587 million, respectively, by 2045 (1). The global prevalence of diabetes is particularly increasing in Asia; >60% of the diabetes population globally are Asian (2). Diabetes also imposes a significant economic impact for countries and health care systems. Japan is one of the countries with the highest numbers of adults with diabetes and prediabetes (1). Epidemiological evidence consistently shows a link between diabetes and risk of death from all causes, cardiovascular disease (CVD), cancer, and other diseases (3,4). Prediabetes also is associated with risk of chronic kidney disease (5), CVD (6), cancer (7), and all-cause mortality (8).
Although a large body of epidemiological evidence suggests diabetes as a major risk factor for death (3,4), the association between prediabetes and death is still a subject of scientific debate, and several issues remain to be answered. First, the definition of prediabetes varies among studies (8,9), and this may be a source of the heterogeneity of results with respect to the association found among studies. Thus, it is valuable to compare the strength of the association between different definitions of prediabetes and mortality risk in the same population. Second, the evidence of prediabetes and death has been derived mainly from western populations (8), but is limited among Asians (10). There are marked differences in lifestyle and culture between western populations and Asian people (11). In addition, Asians have a higher prevalence of prediabetes than their western counterparts in the same level of BMI (11). Thus, findings obtained from a western population might not be applicable to Asians, including Japanese people. Third, previous studies on prediabetes assessed the association mainly with all-cause and CVD-related deaths (8–10), but the evidence linking prediabetes with noncardiovascular-related death, including cancer-related death, is limited (12,13). Fourth, although a high prevalence of prediabetes was documented among workers (14), few data exist regarding the association between prediabetes and death in a working population (15). Such data would contribute to the promotion of measures against metabolic disorders in an occupational health setting.
To address these issues, we prospectively quantified the association of prediabetes defined according to fasting plasma glucose (FPG) level, glycated hemoglobin (HbA1c), or a combination of these values, using the cutoff points suggested by the American Diabetes Association (ADA) or the World Health Organization (WHO)/International Expert Committee (IEC), with the risk of all-cause and cause-specific mortality in a large, working population–based cohort study in Japan. We also investigated the association between diabetes and all-cause and cause-specific mortality.
Research Design and Methods
Study Design
We used data from the Japan Epidemiology Collaboration on Occupational Health (J-ECOH) Study, which is an ongoing, multicenter epidemiologic study among workers at >10 companies (16). The workers underwent annual health checkups comprising anthropometric measurements, physical examinations, laboratory examinations, and a self-administered questionnaire about medical history and health-related lifestyle factors. Almost all workers underwent the annual health checkup because it is compulsory for all employees according to the Industrial Safety and Health Act in Japan. The purpose, procedures, and format of the J-ECOH Study were explained using posters placed at each company before data collection. The participants did not provide verbal or written informed consent, but they were free to refuse and withdraw participation. This procedure conforms to the Japan Ethical Guideline for Epidemiological Research, which suggests that informed consent from each participant is not necessarily required for observational studies using existing data. The research protocol including the consent procedure was approved by the Ethics Committee of the National Center for Global Health and Medicine, Japan.
Analytic Cohort
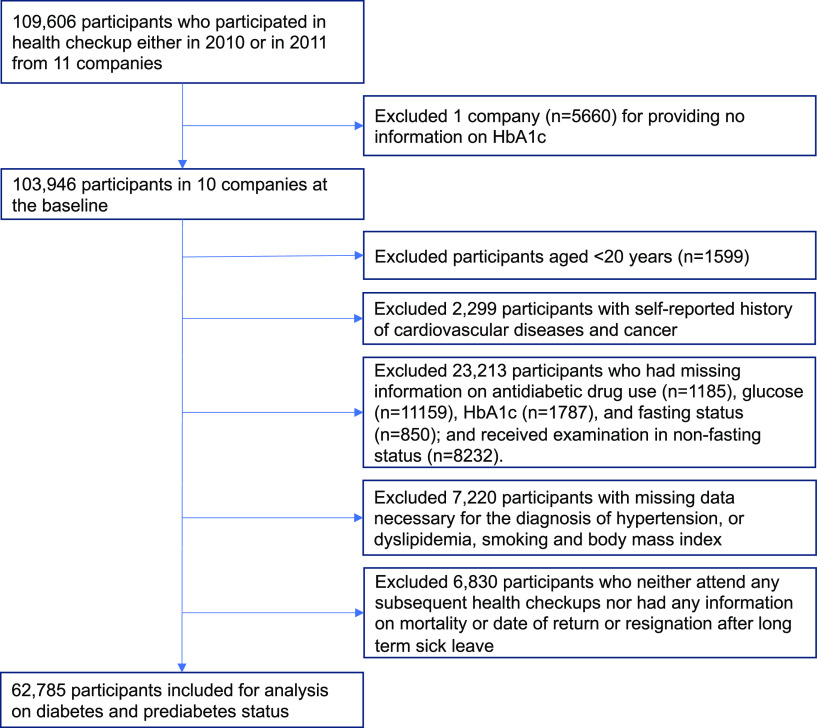
As shown in Fig. 1, 10 of 11 companies provided health check-up data including HbA1c during the 2010 or 2011 fiscal year. Of 103,946 employees in these companies, we excluded 1,599 participants aged <20 years; 2,299 with a history of CVD or cancer; 23,213 who lacked data on antidiabetic medication, blood glucose, HbA1c, and fasting status, or underwent an examination in a nonfasting condition; and 7,220 with missing data on the following covariates: hypertension (systolic blood pressure [SBP], diastolic blood pressure [DBP], and antihypertensive medication) or dyslipidemia (triglycerides [TGs], high-density lipoprotein cholesterol [HDL-C], low-density lipoprotein cholesterol [LDL-C], and lipid-lowering medication), smoking, and BMI. Of the remaining 69,615 participants, we excluded 6,830 who had no follow-up information including subsequent health checkup, CVD events, long-term sick leave, and death, leaving data on 62,785 people, aged 20–86 years, for analysis.
Figure 1.
Flowchart of the study population.
General Health Examination
Body weight and height were measured in with the participant wearing light clothes and no shoes. BMI was computed as weight in kilograms divided by height in meters squared. Blood pressure was measured in a sitting position with an automatic sphygmomanometer. Plasma blood glucose level was measured using an enzymatic or a glucose oxidase peroxidative electrode method. Blood lipid levels, including total cholesterol, LDL-C, HDL-C, and TGs, were measured enzymatically. HbA1c was measured by latex agglutination immunoassay method in five companies, high-performance liquid chromatography method in two companies, and enzymatic method in three companies. All these methods can accurately measure the stable form β‐N1‐mono‐deoxyfructosyl hemoglobin (17) and are well calibrated against the Japanese Clinical Laboratory Use Certified Reference Material (18). The resulting value, called HbA1c (Japan Diabetes Society), was converted to the NGSP equivalent value by using the following formula: HbA1c (%) = 1.02 × HbA1c (Japan Diabetes Society) (%) + 0.25% (18). All laboratories involved in the health examinations conducted at the participating companies received satisfactory scores (rank A, or score >95/100) from external quality-control agencies.
Assessment of Prediabetes and Diabetes
Following the ADA criteria, we defined prediabetes as an FPG level of 100–125 mg/dL and/or HbA1c of 5.7–6.4% and diabetes as HbA1c ≥6.5%, FPG level ≥126 mg/dL, or current use of an antidiabetic drug (19). We also defined prediabetes as an FPG level of 110–125 mg/dL and/or HbA1c of 6.0–6.4%, according to the WHO/IEC criteria (12). Other definitions of prediabetes were considered as an FPG level of 100–125 mg/dL (ADA criterion) or 110–125 mg/dL (WHO criterion) or HbA1c of 5.7–6.4% (ADA criterion) or 6.0–6.4% (IEC criterion) to evaluate whether the risk of death varies across the definitions of prediabetes. Normoglycemia was defined as values below the cutoff point for prediabetes for each diagnostic criterion.
Ascertainment of Death
Deaths occurring between April 2012 and March 2019 were identified using the within-study registration. Causes of deaths were confirmed from a death certificate (63.0%), family confirmation (10.2%), sick-leave document (18.5%), and other sources (8.3%), and were classified according to the ICD-10. The end point of the current study was death from all causes, cancer (ICD codes C00–C97), CVD (ICD codes I00–I99), and other causes.
Assessment of Covariates
Covariates included age, sex, worksite, BMI, smoking, hypertension, and dyslipidemia. We combined and classified 10 worksites into 4 sites; 6 sites with fewer than 3,000 health check examinations were aggregated. Smoking status was assessed using a self-administered questionnaire. Hypertension was defined as SBP ≥140 mmHg, DBP ≥90 mmHg, or treatment for hypertension. Dyslipidemia was defined as TG level ≥150 mg/dL, LDL-C level ≥140 mg/dL, HDL-C level <40 mg/dL, or medical treatment for dyslipidemia in accordance with the criteria of the Japan Atherosclerosis Society (20). The information on occupational physical activity and job position was available in a few participating companies, and the data format on alcohol consumption markedly differed across the participating companies. Thus, we did not consider these variables in the main analysis but adjusted for a sensitivity analysis in a major company.
Statistical Analysis
We compared the differences in characteristics between those who were included in the present analysis and those who were excluded. To show the baseline characteristics of the study population, age- and sex-adjusted proportions and means are presented across diabetes, prediabetes, and normoglycemia status. Test for trend was performed by assigning ordinal numbers to the categories of diabetes, prediabetes, and normoglycemia and treating them as a continuous variable. Person-time was calculated from 31 March 2012 (1 day before the beginning of the follow-up period) to the date of death or date of censoring, which was determined individually on the basis of available information, including annual health checkup, sick leave, retirement, or the end of follow-up (for most companies, this was March 31, 2019). The Cox proportional hazards model was used to estimate the hazard ratios (HRs) of all-cause and cause-specific mortality for each participant with prediabetes and diabetes; the participants with normoglycemia were used as the reference category. Model 1 was adjusted for baseline age (years; continuous), sex, and worksite. Model 2 was additionally adjusted for smoking status (never smoker, former smoker, or current smoker), BMI (kg/m2; continuous), hypertension (yes or no), and dyslipidemia (yes or no). The destruction of pancreatic tissue by pancreatic cancer and decreased hepatic insulin clearance in liver cancer may impair glucose metabolism (21,22); thus, to exclude the potential bias due to such mechanisms, we performed a sensitivity analysis after excluding those who died of liver cancer and pancreas cancer. In addition, given that individuals with prediabetes are more likely to progress to diabetes (23), we repeated the analysis for prediabetes–death association after excluding participants who had prediabetes at baseline and progressed to diabetes during follow-up.
We performed sensitivity analyses by excluding those who were taking either antihypertensive medication (n = 6,686) or lipid-lowering medication (n = 4,167) to remove potential effects of these drugs. In one major company (n = 36,379), we performed an analysis with additional adjustment for occupational physical activity (sedentary, mostly standing and walking often, or fairly active), job position (high position or low position), and alcohol intake (<23 g or ≥23 g ethanol/day). Two-sided P < 0.05 was regarded as statistically significant. All analyses were performed using Stata, version 14 (StataCorp, College Station, TX).
Results
Compared with participants included in the present analysis, those who were excluded were younger and less likely to be men and current smokers; had lower mean BMI, blood glucose level, and HbA1c; and had a lower prevalence of hypertension and dyslipidemia (Supplementary Table 1). Table 1 summarizes the age- and sex-adjusted baseline characteristics of the study population based on normoglycemia, prediabetes, and diabetes defined according to ADA criteria. Compared with participants with normoglycemia, participants with prediabetes and diabetes were older; more likely to be men and current smokers; had a higher prevalence of hypertension and dyslipidemia; and had higher mean BMI and mean SBP, DBP, TG, and LDL-C concentrations; but lower mean HDL-C concentration. The LDL-C concentration was slightly higher in the participants with prediabetes than in the participants with diabetes.
Table 1.
Age- and sex-adjusted baseline characteristics of the study population across normoglycemia, prediabetes, and diabetes status
| Normoglycemia | Prediabetes defined by ADA criteria | Diabetes | |
|---|---|---|---|
| No. of participants | 33,990 | 24,143 | 4,652 |
| Age (years) | 42.0 ± 0.05 | 47.9 ± 0.06 | 52.0 ± 0.14 |
| Men (%) | 81.1 | 89.8 | 94.1 |
| BMI (kg/m2) | 22.7 ± 0.02 | 24.0 ± 0.02 | 25.9 ± 0.05 |
| Current smoker (%) | 30.1 | 32.4 | 39.3 |
| SBP (mmHg) | 119.2 ± 0.08 | 122.5 ± 0.09 | 127.1 ± 0.21 |
| DBP (mmHg) | 75.2 ± 0.06 | 77.2 ± 0.06 | 78.9 ± 0.15 |
| Hypertension (%) | 13.9 | 18.7 | 33.1 |
| TGs (mg/dL) | 109.8 ± 0.50 | 130.3 ± 0.59 | 155.3 ± 1.34 |
| HDL-C (mg/dL) | 60.4 ± 0.08 | 57.4 ± 0.09 | 53.7 ± 0.21 |
| LDL-C (mg/dL) | 118.3 ± 0.17 | 124.2 ± 0.20 | 122.5 ± 0.45 |
| Dyslipidemia (%) | 38.3 | 50.8 | 62.4 |
Unless indicated otherwise, data are given as the age- and sex-adjusted (mean ± SE) or percentage distribution.
The proportion of participants with prediabetes differed between the two definitions: 38.4% and 12.8% for the ADA criteria and the WHO/IEC criteria, respectively (Table 2). During a maximum 7 years of follow-up, 229, 97, and 57 deaths were attributed to all causes, cancer, and CVD, respectively. As shown in Table 2 and Supplementary Fig. 1, the risk of all-cause mortality was significantly higher among the participants with prediabetes defined by combined ADA criteria, and multivariable-adjusted HR was 1.53 (95% CI 1.12–2.09) among the participants with prediabetes. Regarding cause-specific mortality, prediabetes according to ADA criteria was associated with an increased risk of cancer death (HR 2.37; 95% CI 1.45–3.89) but not with death due to CVD (HR 1.00; 95% CI 0.52–1.93). These results were materially unchanged when prediabetes was defined according to the WHO/IEC cutoff points; multivariable-adjusted HRs (95% CIs) were 1.46 (1.02–2.09) for all-cause mortality, 2.03 (1.24–3.32) for death due to cancer, and 0.93 (0.42–2.08) for death due to CVD. A significant increase in the risk of cancer-related death associated with prediabetes was observed even after excluding participants who died of liver cancer and pancreatic cancer (Supplementary Table 2), or after excluding those who had prediabetes at baseline and progressed to diabetes during follow-up (Supplementary Table 3). In addition, the associations of prediabetes with all-cause mortality and death due to cancer were materially unchanged after excluding those who were taking antihypertensive medication (Supplementary Table 4) or lipid-lowering medication (Supplementary Table 5).
Table 2.
Multivariable-adjusted HRs (95% CI) of all-cause and cause-specific mortality according to the baseline status of prediabetes and diabetes
| ADA criteria | WHO/IEC criteria | |||||
|---|---|---|---|---|---|---|
| Normoglycemia | Prediabetes | Diabetes | Normoglycemia | Prediabetes | Diabetes | |
| No. of participants | 33,990 | 24,143 | 4,652 | 50,114 | 8,019 | 4,652 |
| Person-years | 191,140 | 132,527 | 23,210 | 280,813 | 42,854 | 23,210 |
| All-cause mortality | ||||||
| No. of deaths | 78 | 107 | 44 | 141 | 44 | 44 |
| Model 1* | 1.00 (Ref.) | 1.61 (1.19–2.19) | 3.12 (2.10–4.63) | 1.00 (Ref.) | 1.58 (1.12–2.24) | 2.62 (1.84–3.74) |
| Model 2† | 1.00 (Ref.) | 1.53 (1.12–2.09) | 2.66 (1.76–4.03) | 1.00 (Ref.) | 1.46 (1.02–2.09) | 2.25 (1.55–3.27) |
| Cancer-related death | ||||||
| No. of deaths | 26 | 57 | 14 | 56 | 26 | 14 |
| Model 1* | 1.00 (Ref.) | 2.41 (1.48–3.92) | 2.68 (1.36–5.30) | 1.00 (Ref.) | 2.10 (1.30–3.40) | 1.86 (1.02–3.41) |
| Model 2† | 1.00 (Ref.) | 2.37 (1.45–3.89) | 2.54 (1.25–5.15) | 1.00 (Ref.) | 2.03 (1.24–3.32) | 1.75 (0.93–3.28) |
| CVD-related death | ||||||
| No. of deaths | 19 | 21 | 17 | 32 | 8 | 17 |
| Model 1* | 1.00 (Ref.) | 1.23 (0.64–2.34) | 4.60 (2.26–9.36) | 1.00 (Ref.) | 1.21 (0.55–2.67) | 4.27 (2.28–7.97) |
| Model 2† | 1.00 (Ref.) | 1.00 (0.52–1.93) | 2.74 (1.29–5.81) | 1.00 (Ref.) | 0.93 (0.42–2.08) | 2.68 (1.38–5.20) |
| Other-cause death | ||||||
| No. of deaths | 33 | 29 | 13 | 52 | 10 | 13 |
| Model 1* | 1.00 (Ref.) | 1.18 (0.70–1.99) | 2.68 (1.34–5.32) | 1.00 (Ref.) | 1.15 (0.57–2.31) | 2.52 (1.33–4.77) |
| Model 2† | 1.00 (Ref.) | 1.20 (0.70–2.04) | 2.63 (1.27–5.44) | 1.00 (Ref.) | 1.16 (0.57–2.34) | 2.44 (1.24–4.79) |
Values in bold are statistically significant. Ref., reference.
Model 1 adjusted for age (year; continuous), sex, and worksite.
Model 2 additionally adjusted for BMI (kg/m2; continuous), smoking status (never smoker, former smoker, or current smoker), hypertension (yes or no), and dyslipidemia (yes or no).
The participants with diabetes had a significantly higher risk of all-cause mortality (HR 2.66; 95% CI 1.76–4.03), death due to CVD (HR 2.74; 95% CI 1.29–5.81), and death due to cancer (HR 2.54; 95% CI 1.25–5.15) than did the participants with normoglycemia (cutoff point suggested by ADA criteria). The associations for all-cause and CVD-related deaths were virtually unchanged when normoglycemia was defined according to the WHO/IEC criteria, except for the association between diabetes and cancer-related deaths (statistically not significant).
Regarding prediabetes defined by either FPG level or HbA1c, 32.5% of the study participants had prediabetes according to the ADA FPG criteria and 18.6% according to the ADA HbA1c criteria. By WHO/IEC criteria and IEC HbA1c criteria, 9.1% and 7.5%, respectively, had prediabetes (Table 3). As shown in Table 3 and Supplementary Fig. 2, using the ADA criteria, prediabetes defined by either FPG level or HbA1c was associated with an increased risk of all cause mortality and death due to cancer but not with CVD-related death. Compared with FPG level <100 mg/dL or HbA1c <5.7%, the multivariable-adjusted HRs (95% CIs) of either ADA FPG- or ADA HbA1c-defined prediabetes were 1.51 (1.12–2.05) or 1.58 (1.15–2.17) for all-cause mortality and 2.32 (1.46–3.71) or 1.93 (1.21–3.08) for death due to cancer, respectively. Regarding the WHO/IEC criteria of prediabetes, compared with FPG level <110 mg/dL or HbA1c <6.0%, the multivariable-adjusted HRs (95% CIs) for either WHO FPG- or IEC HbA1c-defined prediabetes were 1.68 (1.15–2.43) or 1.18 (0.76–1.84) for all-cause mortality, 2.19 (1.30–3.67) or 1.73 (0.97–3.10) for death due to cancer, and 1.40 (0.63–3.10) or 0.45 (0.13–1.50) for death due to CVD, respectively.
Table 3.
Multivariable-adjusted HRs (95% CI) of all-cause and cause-specific mortality for prediabetes subgroups, using the ADA or the WHO/IEC criteria
| Definition | No. of participants | Person-years | All-cause mortality | Death Due to Cancer | Death Due to CVD | Other-cause death | |
|---|---|---|---|---|---|---|---|
| ADA criteria | |||||||
| By FPG level | |||||||
| No. of deaths by prediabetes status | 96 | 52 | 20 | 24 | |||
| Normoglycemia | FPG <100 mg/dL | 38,338 | 214,604 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Prediabetes | FPG 100–125 mg/dL | 20,385 | 112,034 | 1.51 (1.12–2.05) | 2.32 (1.46–3.71) | 1.18 (0.62–2.23) | 1.03 (0.61–1.77) |
| By HbA1c | |||||||
| No. of deaths by prediabetes status | 64 | 33 | 13 | 18 | |||
| Normoglycemia | HbA1c <5.7% | 47,224 | 265,413 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Prediabetes | HbA1c 5.7–6.4% | 11,657 | 62,129 | 1.58 (1.15–2.17) | 1.93 (1.21–3.08) | 1.03 (0.52–2.03) | 1.60 (0.90–2.87) |
| WHO/IEC criteria | |||||||
| By FPG level | |||||||
| No. of deaths by prediabetes status | 37 | 21 | 8 | 8 | |||
| Normoglycemia | FPG <110 mg/dL | 53,017 | 296,004 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Prediabetes | FPG 110–125 mg/dL | 5,706 | 30,634 | 1.68 (1.15–2.43) | 2.19 (1.30–3.67) | 1.40 (0.63–3.10) | 1.22 (0.57–2.63) |
| By HbA1c | |||||||
| No. of deaths by prediabetes status | 24 | 15 | 3 | 6 | |||
| Normoglycemia | HbA1c <6.0% | 54,145 | 302,894 | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) | 1.00 (Ref.) |
| Prediabetes | HbA1c 6.0–6.4% | 4,736 | 24,648 | 1.18 (0.76–1.84) | 1.73 (0.97–3.10) | 0.45 (0.13–1.50) | 1.13 (0.48–2.70) |
Values in bold are statistically significant. Model was adjusted for age (year, continuous), sex, worksite, BMI (kg/m2), smoking status (never smoker, former smoker, or current smoker), hypertension (yes or no), and dyslipidemia (yes or no). Ref., reference.
In exploratory analyses for varying cutoff levels of HbA1c and FPG, a significantly increased risk was observed for all-cause mortality among the participants with combined FPG levels of 100–109 mg/dL and HbA1c of 5.7–5.9%, combined FPG levels of 110–125 mg/dL and HbA1c of 6.0–6.4%, FPG levels of 110–125 mg/dL, and HbA1c of 5.7–5.9%, compared with participants with FPG levels <100 mg/dL and HbA1c <5.7%, FPG levels <100 mg/dL, and HbA1c <5.7%, respectively (Supplementary Table 6). The risk of cancer-related death was significantly higher among the participants with combined FPG levels of 100–109 mg/dL and HbA1c of 5.7–5.9%, FPG levels of 100–109 mg/dL, and HbA1c levels 5.7–5.9% compared with participants with combined FPG levels <100 mg/dL and HbA1c <5.7%, FPG levels <100 mg/dL, and HbA1c levels <5.7%, respectively (Supplementary Table 6).
In a sensitivity analysis with further adjustment for occupational physical activity, job position, and alcohol intake in one large company, we confirmed an increased risk for all-cause mortality and cancer-related death associated with prediabetes and for all-cause mortality associated with diabetes, although the association for CVD- and cancer-related deaths with diabetes was not statistically significant (Supplementary Table 7).
Conclusions
In this large prospective study of Japanese workers, prediabetes was associated with an increased risk of death from all causes and cancer, but not CVD, and the strength of the associations was similar across the different definitions of prediabetes (except for IEC HbA1c-defined prediabetes). Diabetes was significantly associated with an increased risk of all-cause, cancer-related, and CVD-related deaths. To our knowledge, this is the first study to quantify the association of different definitions of prediabetes (either FPG alone, HbA1c alone, or their combination using ADA and WHO/IEC cutoff points) with the risk of all-cause and cause-specific mortality in Asia.
The present findings of an increased risk of all-cause mortality associated with prediabetes agree with those of a meta-analysis (8) and a recent large Korean study (10). We also found the strength of the association was similar across prediabetes definitions—a finding compatible with the data of a prospective study in the United States (24). In our exploratory analyses, the risk of all-cause mortality was significantly increased among people with the combination of FPG levels of 100–109 mg/dL and HbA1c of 5.7–5.9% (HR 1.43; 95% CI 1.01–1.86) and in those with HbA1c levels of 5.7–5.9% (HR 1.73; 95% CI 1.20–2.50) (Supplementary Table 6), suggesting a need to adopt a lower HbA1c cutoff point for prediabetes in terms of mortality risk. The present findings are in line with those of two prospective studies in the United States that made head-to-head comparisons of different definitions of prediabetes at baseline in relation to the risk of all-cause mortality (15,24). Given the high transition rate from prediabetes to diabetes (25), however, it remained unclear whether prediabetes per se or the transition to diabetes increases the risk of death. By excluding people in whom diabetes developed during the follow-up, we confirmed that the prediabetes–mortality association remained elevated (marginally significant) (Supplementary Table 3), indicating prediabetes per se was a risk factor for all-cause mortality.
Consistent with the results of a meta-analysis (7) and a pooled analysis of European cohort studies (26), we found an increased risk of death due to cancer associated with prediabetes, the leading cause of death in the present working population (41.9% of total deaths). Relative risks (RRs) estimated in our study (HR 2.37 by ADA criteria and 2.03 by WHO/IEC criteria) were higher than those among Europeans (1.12) (26). In a subgroup analysis of the aforementioned meta-analysis (7), the prediabetes–cancer risk association appeared to be stronger among Asians (RR 1.50) than non-Asians (RR 1.12) (7). Prediabetes may confer greater cancer risk for Asians than non-Asians.
We found no material difference in the association of prediabetes and cancer-related death across the different definitions of prediabetes, a finding consistent with results of a meta-analysis of 16 prospective studies (7). In our exploratory analyses, the risk of cancer-related death was significantly elevated in those with combined or individual FPG levels of 100–109 mg/dL and HbA1c of 5.7–5.9% (Supplementary Table 6), suggesting a need to adopt lower FPG and HbA1c cutoff points for prediabetes (i.e., ADA rather than WHO/IEC criteria) to predict risk of death due to cancer. The association between prediabetes and cancer is biologically plausible because hyperglycemia in prediabetes produces a wide range of proinflammatory factors, which could stimulate oncogene expression and, in turn, promote tumor cell proliferation and metastasis (27).
We found no association between any definition of prediabetes and death due to CVD. This finding contrasts with the result of our previous case-control study nested in the present cohort, which showed a significant increase in the risk of CVD (myocardial infarction and stroke) associated with prediabetes within a few years before the onset of CVD (28). The inconsistency in the same study population may be ascribed to the difference in the outcome (incidence versus death) or exposure (recent past versus remote past). Authors of a meta-analysis reported a small but significant increase in the risk of CVD associated with prediabetes (RR 1.15) and found a stronger association with impaired glucose tolerance (IGT) (RR 1.23), a subtype of prediabetes (8). In the present study, participants with IGT but normal FPG and HbA1c values were misclassified as normoglycemia, leading to an attenuation of the relationship between prediabetes and CVD-related death. Similarly, there may be heterogeneity in CVD risk even among those with FPG- and HbA1c-defined prediabetes. For instance, individuals with both FPG and HbA1c criteria of prediabetes have a worse cardiometabolic profile than those meeting either FPG or HbA1c criteria (29). Moreover, ethnicity has been suggested to modify the association. A cohort study reported a significant increase in CVD risk associated with prediabetes among Europeans but not among South Asians (30). More studies are required to identify a prediabetes subtype associated with an increased risk of death due to CVD for each ethnic group.
The present finding of an increased risk of all-cause mortality (HR 2.66) among workers with diabetes is consistent with those of prospective studies of the general population in Japan (HR 1.35–1.87) (31–33), China (HR 2.0) (34), the United States (HR 1.64) (13), and specifically of workers in United States (HR 2.1 for male physicians [35] and HR 3.12 for nurses [36]), and is also consistent with the findings of one pooled study of an Asian general population (HR 1.89) (37). The variation in the magnitude of the association across studies could be partially attributed to the differences in population characteristics, diabetes care, and major causes of death. Regarding cause-specific mortality, we found a significantly higher risk of death due to CVD (HR 2.74) and cancer (HR 2.54) associated with diabetes. This result is consistent with those of prospective studies of a Japanese general population (for CVD-related death, HR was 1.76 in men and 2.49 in women) (31); for cancer-related death, HR 1.87) (32), and those of a pooled study of 22 Asian prospective studies (for CVD-related death, HR 2.00; for cancer-related death, HR 1.21) (37). Our study extends the evidence of the association between diabetes and death to a working population.
The strengths of our study include its prospective design, large sample size, and use of data from multiple companies. The study also has several limitations that warrant mention. First, the timing of postprandial glucose measurements and oral glucose tolerance tests were not available for the J-ECOH Study; thus, we could not define prediabetes on the basis of elevated postprandial glucose level and IGT. Second, workers with prediabetes and diabetes were older and had higher blood pressure and a worse lipid profile than those with normoglycemia. Despite statistical adjustment of these factors, the possibility of residual confounding cannot be ruled out. Also, data on socioeconomic status and lifestyle were not collected in a standardized manner across the participating companies. In a sensitivity analysis with the additional adjustment for occupational physical activity, job position, and alcohol intake in one major company, we confirmed that the associations for all-cause mortality and cancer-related death with prediabetes and for all-cause mortality with diabetes remained virtually the same. Third, we have no information regarding the type of diabetes each participant had. Among Japanese patients with diabetes, type 2 diabetes (74.8%) is much more common than type 1 diabetes (25.2%) (38). Fourth, the number of CVD-related deaths (n = 57) in participants with prediabetes may not be sufficient to detect a modest risk associated with prediabetes, if any. Fifth, because of the lack of information on specific types of hypertension medication (e.g., renin-angiotensin-aldosterone system inhibitors) and dyslipidemia (e.g., statins), we were unable to examine their influence. We observed similar associations, however, after excluding those who were taking these medications at baseline. Sixth, because worker health examination is mandatory in Japan, our study is less likely to be subject to bias arising from differential participation. Nevertheless, we noticed some differences in the characteristics between participants who were excluded from analysis and those who remained in the analysis, leaving a possibility of selection bias. Finally, study participants were Japanese employees at large companies. Caution should be exercised in generalizing the findings of this study.
In conclusion, this large-scale cohort study of Japanese workers showed that FPG- and HbA1c-defined prediabetes according to ADA and WHO/IEC was associated with a significant increase in the risk of all-cause mortality and death due to cancer but not due to CVD. The strength of these associations was similar across the different definitions of prediabetes. This study confirmed an increase in the risk of death from all-causes, CVD, and cancer among the patients with diabetes. These findings support the need for prevention and management of not only diabetes but also prediabetes to lower the risk of death among workers. More prospective studies are needed to clarify the association of whole prediabetes, including IGT as well as prediabetes subtype, with the risk of death.
Article Information
Acknowledgments. The authors thank Toshiteru Okubo (chairperson, Industrial Health Foundation) for scientific advice on conducting the J-ECOH Study and Rika Osawa (National Center for Global Health and Medicine) for administrative support.
Funding. This study was supported by the Industrial Health Foundation (Industrial Disease Clinical Research Grants 140202-01, 150903-01, and 170301-01), Japan Society for the Promotion of Science KAKENHI (grant 16H05251), and the National Center for Global Health and Medicine (grant 28-Shi-1206).
Duality of Interest. No potential conflicts of interest relevant to this article were reported.
Author Contributions. T.Miz and S.D. were involved in the design of the study as the principal investigators. T.N., T.H., S.Y., H.O., T.Miy., T.O., N.S., A.U., M.Y., T.K., M.E., T.Sh., M.S., S.N., T.I., A.N., K.T., T.So., M.K., and I.K. contributed to the acquisition of data; Z.I. analyzed the data and drafted the manuscript; H.H. and T.Miz. provided support on statistical analysis methods; S.A., Y.I., H.H., K.K., A.H., and T.Miz. contributed to the interpretation of study findings and critical revision of the manuscript. All authors read and approved the final manuscript. Z.I. and T.Miz. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Appendix
The Japan Epidemiology Collaboration on Occupational Health Study Group. The full list of members of the Japan Epidemiology Collaboration on Occupational Health Study Group is as follows: T. Mizoue, Y. Inoue, S. Akter, H. Hu, D.V. Hoang, T. Miki, A. Fukunaga, Z. Islam, S. Yamamoto, R.M. Shrestha and M. Konishi, National Center for Global Health and Medicine, Tokyo, Japan; A. Nanri, Fukuoka Women’s University, Fukuoka, Japan; K. Kuwahara, Teikyo University, Tokyo, Japan; S. Dohi and H. Okazaki, Mitsui Chemicals, Inc., Tokyo, Japan; K. Mizuta and M. Yamamoto, YAMAHA CORPORATION, Shizuoka, Japan; A. Uehara, Hidaka Tokushukai Hospital, Hokkaido, Japan; T. Nakagawa, S. Yamamoto, T. Honda and Y. Watanabe, Hitachi, Ltd., Ibaraki, Japan; I. Kabe, KUBOTA Corporation, Ibaraki, Japan; T. Kochi, M. Eguchi, and T. Shirasaka, Furukawa Electric Co., Ltd., Tokyo, Japan; T. Miyamoto, M. Hasegawa and M. Shirozu, Nippon Steel East Nippon Works Kimitsu Area, Chiba, Japan; M. Shimizu, N. Gonmori, and A. Ogasawara, Mizue Medical Clinic, Keihin Occupational Health Center, Kanagawa, Japan; N. Kato, Fuji Electric Co., Ltd., Kanagawa, Japan; K. Tomita, Healthplant., Tokyo, Japan; T. Imai, Occupational Health Support Company, Tokyo, Japan; A. Nishihara, Azbil Corporation, Tokyo, Japan; C. Nishiura, Tokyo Gas Co., Ltd., Tokyo, Japan; A. Hori, University of Tsukuba, Ibaraki, Japan; C. Kinugawa, Healc Co., Ltd., Tokyo, Japan; N. Sasaki and T. Ogasawara, Mitsubishi Fuso Truck and Bus Corporation, Kanagawa, Japan; M. Kawashima, Central Japan Railway Company, Aichi, Japan; M. Endo, Juntendo University, Tokyo, Japan; K. Yamamoto and R. Kuroda, The University of Tokyo, Tokyo, Japan; K. Kitahara and T. Yokoya, Mitsubishi Heavy Industries, Ltd., Kanagawa, Japan; N. Kunugita, University of Occupational and Environmental Health, Fukuoka, Japan; T. Sone, National Institute of Public Health, Saitama, Japan; M. Tatemichi and K. Fukai, Tokai University, Kanagawa, Japan; Y. Inoue, Mitsubishi Electric Corporation, Tokyo, Japan; K. Fukasawa, ADVANTAGE Risk Management Co., Ltd., Tokyo, Japan; H. Nakajima, National Defense Medical College, Saitama, Japan; T. Totsuzaki, Mizuho Health Insurance Society, Tokyo, Japan; M. Masuda, AEON Co., Ltd., Chiba, Japan; N. Sakamoto, Y. Osaki and A. Tomizawa, Health Design Inc., Tokyo, Japan; S. Nagahama, Tokyo Gas Customer Support, Tokyo, Japan; M. Ohtsu, Himawari Industrial Physician & Occupational Health Consultant Office, Saitama, Japan; M. Kawashima, Shiga University of Medical Science, Shiga, Japan.
Footnotes
A complete list of the the Japan Epidemiology Collaboration on Occupational Health Study Group can be found in the appendix.
This article contains supplementary material online at https://doi.org/10.2337/figshare.13483515.
This article is featured in a podcast available at https://www.diabetesjournals.org/content/diabetes-core-update-podcasts.
References
- 1.International Diabetes Federation . IDF Diabetes Atlas. 8th ed. Brussels, Belgium: International Diabetes Federation; 2017 [Google Scholar]
- 2.Nanditha A, Ma RC, Ramachandran A, et al. Diabetes in Asia and the Pacific: implications for the global epidemic. Diabetes Care 2016;39:472–485 [DOI] [PubMed] [Google Scholar]
- 3.Rao Kondapally Seshasai S, Kaptoge S, Thompson A, et al.; Emerging Risk Factors Collaboration . Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 2011;364:829–841 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sarwar N, Gao P, Seshasai SR, et al.; Emerging Risk Factors Collaboration . Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies [published correction appears in Lancet 2010;376:958]. Lancet 2010;375:2215–2222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Echouffo-Tcheugui JB, Narayan KM, Weisman D, Golden SH, Jaar BG. Association between prediabetes and risk of chronic kidney disease: a systematic review and meta-analysis. Diabet Med 2016;33:1615–1624 [DOI] [PubMed] [Google Scholar]
- 6.Ford ES, Zhao G, Li C. Pre-diabetes and the risk for cardiovascular disease: a systematic review of the evidence. J Am Coll Cardiol 2010;55:1310–1317 [DOI] [PubMed] [Google Scholar]
- 7.Huang Y, Cai X, Qiu M, et al. Prediabetes and the risk of cancer: a meta-analysis. Diabetologia 2014;57:2261–2269 [DOI] [PubMed] [Google Scholar]
- 8.Cai X, Zhang Y, Li M, et al. Association between prediabetes and risk of all cause mortality and cardiovascular disease: updated meta-analysis. BMJ 2020;370:m2297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deedwania P, Patel K, Fonarow GC, et al. Prediabetes is not an independent risk factor for incident heart failure, other cardiovascular events or mortality in older adults: findings from a population-based cohort study. Int J Cardiol 2013;168:3616–3622 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kim NH, Kwon TY, Yu S, et al. Increased vascular disease mortality risk in prediabetic Korean adults is mainly attributable to ischemic stroke. Stroke 2017;48:840–845 [DOI] [PubMed] [Google Scholar]
- 11.Yip WCY, Sequeira IR, Plank LD, Poppitt SD. Prevalence of pre-diabetes across ethnicities: a review of impaired fasting glucose (IFG) and impaired glucose tolerance (IGT) for classification of dysglycaemia. Nutrients 2017;9:1273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kowall B, Rathmann W, Heier M, et al. Categories of glucose tolerance and continuous glycemic measures and mortality. Eur J Epidemiol 2011;26:637–645 [DOI] [PubMed] [Google Scholar]
- 13.Li S, Wang J, Zhang B, Li X, Liu Y. Diabetes mellitus and cause-specific mortality: a population-based study. Diabetes Metab J 2019;43:319–341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Uehara A, Kurotani K, Kochi T, et al.; Japan Epidemiology Collaboration of Occupational Health Study Group . Prevalence of diabetes and pre-diabetes among workers: Japan Epidemiology Collaboration on Occupational Health Study. Diabetes Res Clin Pract 2014;106:118–127 [DOI] [PubMed] [Google Scholar]
- 15.Vistisen D, Witte DR, Brunner EJ, et al. Risk of cardiovascular disease and death in individuals with prediabetes defined by different criteria: the Whitehall II study. Diabetes Care 2018;41:899–906 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Akter S, Nakagawa T, Honda T, et al.; Japan Epidemiology Collaboration on Occupational Health Study Group . Smoking, smoking cessation, and risk of mortality in a Japanese working population - Japan Epidemiology Collaboration on Occupational Health study. Circ J 2018;82:3005–3012 [DOI] [PubMed] [Google Scholar]
- 17.Seino Y, Nanjo K, Tajima N, et al.; Committee of the Japan Diabetes Society on the Diagnostic Criteria of Diabetes Mellitus . Report of the Committee on the Classification and Diagnostic Criteria of Diabetes Mellitus. J Diabetes Investig 2010;1:212–228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kashiwagi A, Kasuga M, Araki E, et al.; Committee on the Standardization of Diabetes Mellitus‐Related Laboratory Testing of Japan Diabetes Society . International clinical harmonization of glycated hemoglobin in Japan: from Japan Diabetes Society to National Glycohemoglobin Standardization Program values. J Diabetes Investig 2012;3:39–40 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.American Diabetes Association . 2. Classification and diagnosis of diabetes: Standards of Medical Care in Diabetes—2019. Diabetes Care 2019;42(Suppl. 1):S13–S28 [DOI] [PubMed] [Google Scholar]
- 20.Teramoto T, Sasaki J, Ishibashi S, et al.; Japan Atherosclerosis Society . Executive summary of the Japan Atherosclerosis Society (JAS) guidelines for the diagnosis and prevention of atherosclerotic cardiovascular diseases in Japan - 2012 version. J Atheroscler Thromb 2013;20:517–523 [DOI] [PubMed] [Google Scholar]
- 21.Hwangbo Y, Kang D, Kang M, et al. Incidence of diabetes after cancer development: a Korean national cohort study. JAMA Oncol 2018;4:1099–1105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pannala R, Basu A, Petersen GM, Chari ST. New-onset diabetes: a potential clue to the early diagnosis of pancreatic cancer. Lancet Oncol 2009;10:88–95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang H, Shara NM, Calhoun D, Umans JG, Lee ET, Howard BV. Incidence rates and predictors of diabetes in those with prediabetes: the Strong Heart Study. Diabetes Metab Res Rev 2010;26:378–385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Warren B, Pankow JS, Matsushita K, et al. Comparative prognostic performance of definitions of prediabetes: a prospective cohort analysis of the Atherosclerosis Risk in Communities (ARIC) study. Lancet Diabetes Endocrinol 2017;5:34–42 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ezquerra-Lázaro I, Cea-Soriano L, Giraldez-García C, et al.; PREDAPS Study Group . Lifestyle factors do not explain the difference on diabetes progression according to type of prediabetes: results from a Spanish prospective cohort of prediabetic patients. Diabetes Res Clin Pract 2019;153:66–75 [DOI] [PubMed] [Google Scholar]
- 26.Zhou XH, Qiao Q, Zethelius B, et al.; DECODE Study Group . Diabetes, prediabetes and cancer mortality. Diabetologia 2010;53:1867–1876 [DOI] [PubMed] [Google Scholar]
- 27.Li W, Zhang X, Sang H, et al. Effects of hyperglycemia on the progression of tumor diseases. J Exp Clin Cancer Res 2019;38:327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hu H, Mizoue T, Sasaki N, et al.; Japan Epidemiology Collaboration on Occupational Health Study Group . Prediabetes and cardiovascular disease risk: a nested case-control study. Atherosclerosis 2018;278:1–6 [DOI] [PubMed] [Google Scholar]
- 29.Giráldez-García C, Sangrós FJ, Díaz-Redondo A, et al.; PREDAPS Study Group . Cardiometabolic risk profiles in patients with impaired fasting glucose and/or hemoglobin A1c 5.7% to 6.4%: evidence for a gradient according to diagnostic criteria: the PREDAPS study. Medicine (Baltimore) 2015;94:e1935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eastwood SV, Tillin T, Sattar N, et al. Associations between prediabetes, by three different diagnostic criteria, and incident CVD differ in South Asians and Europeans. Diabetes Care 2015;38:2325–2332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kato M, Noda M, Mizoue T, et al.; JPHC Study Group . Diagnosed diabetes and premature death among middle-aged Japanese: results from a large-scale population-based cohort study in Japan (JPHC study). BMJ Open 2015;5:e007736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Oba S, Nagata C, Nakamura K, Takatsuka N, Shimizu H. Self-reported diabetes mellitus and risk of mortality from all causes, cardiovascular disease, and cancer in Takayama: a population-based prospective cohort study in Japan. J Epidemiol 2008;18:197–203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yano Y, Kario K, Ishikawa S, et al.; JMS Cohort Study Group . Associations between diabetes, leanness, and the risk of death in the Japanese general population: the Jichi Medical School Cohort Study. Diabetes Care 2013;36:1186–1192 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bragg F, Holmes MV, Iona A, et al.; China Kadoorie Biobank Collaborative Group . Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA 2017;317:280–289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Lotufo PA, Gaziano JM, Chae CU, et al. Diabetes and all-cause and coronary heart disease mortality among US male physicians. Arch Intern Med 2001;161:242–247 [DOI] [PubMed] [Google Scholar]
- 36.Hu FB, Stampfer MJ, Solomon CG, et al. The impact of diabetes mellitus on mortality from all causes and coronary heart disease in women: 20 years of follow-up. Arch Intern Med 2001;161:1717–1723 [DOI] [PubMed] [Google Scholar]
- 37.Yang JJ, Yu D, Wen W, et al. Association of diabetes with all-cause and cause-specific mortality in Asia: a pooled analysis of more than 1 million participants. JAMA Netw Open 2019;2:e192696. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ogawa Y, Uchigata Y, Otani T, Iwamoto Y. Proportion of diabetes type in early-onset diabetes in Japan. Diabetes Care 2007;30:e30. [DOI] [PubMed] [Google Scholar]