Abstract
Objective
To evaluate the efficacy of an online psychosocial group intervention for parents of children with a chronic illness, in terms of anxiety and depression, and disease-related coping skills.
Methods
Parents (N = 73) participated in a parallel multicenter randomized controlled trial comparing an intervention group to a waitlist control group. In the group intervention Op Koers Online (English: On Track Online) parents learned how to use adaptive coping strategies taught with cognitive behavioral therapy and acceptance and commitment therapy techniques. Assessments (online questionnaires) took place at baseline (T0), 6-months (T1), and 12-months (T2) follow-up. Mixed-model analyses were performed to test the difference in change in outcomes between intervention (N = 34) and waitlist control group (N = 33).
Results
When compared with the waitlist control group, the intervention had a significant positive effect (p < .05) on changes in anxiety, depression, and total score T1 versus T0 (β = −.47 to −.51) and T2 versus T0 (β = −.39 to −.46), the coping skills open communication, relaxation, social support, acceptance, predictive control (β = .42–.88) and helplessness (β = −.47) T1 versus T0 and relaxation and positive thinking T2 versus T0 (β = .42–.53).
Conclusions
Parental anxiety and depression decreased, and use of adaptive coping skills improved after the intervention. The online character, the focus on parents themselves instead of on their child and the possibility for parents of children with rare illnesses to participate, are innovative and unique aspects of Op Koers Online for parents. The next step is to implement the intervention in clinical practice.
Keywords: anxiety, chronic illness, coping skills, depression, parents, psychosocial group intervention
Literature Overview
Parents of children with a chronic illness (CI) have to deal with several stressors about their child’s health including practical stressors (e.g., managing daily routines) as well as emotional challenges (e.g., worrying; Cousino & Hazen, 2013; Hatzmann et al., 2008, 2009, 2014; Pinquart, 2018). Therefore, these parents are at risk for psychosocial problems (Collis et al., 2019; Coughlin & Sethares, 2017; Haverman et al., 2013; van Oers et al., 2014) such as anxiety and depression (Pinquart, 2019a, 2019b). Parents with psychosocial problems may have more difficulties managing their child’s illness effectively (Cousino & Hazen, 2013). Moreover, parental depressive symptoms have found to be correlated to negative parenting practices (Celano et al., 2008), poor adherence (Eckshtain et al., 2010) and an increase in children’s illness symptoms over time (Otsuki et al., 2010). Given the negative consequences of parental psychosocial problems for parents themselves as well as their children, interventions to support parents of a child with a CI are needed (Pinquart, 2019b).
Transactional models of child adaption to CI recognize the importance of numerous psychosocial risk and protective factors that could be targeted and modified in interventions. The disability-stress-coping model of Wallander and Varni (1998) implies that the stressors faced by children and parents dealing with pediatric CI are multifaceted (e.g., restriction of activities, responsibility of treatment), and that the links between illness-related stressors and adjustment are moderated by appraisals and coping strategies on which several personal and family risk and protective factors are of influence (Scholten et al., 2013; Wallander & Varni, 1998).
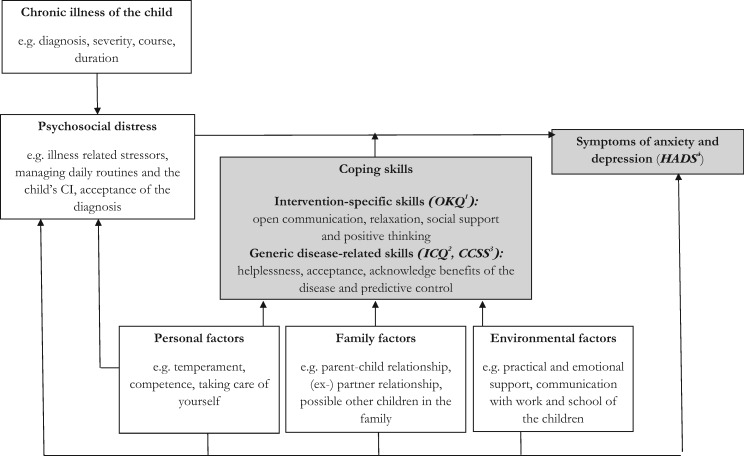
The model of Wallander and Varni (1998) was adapted for this study to explain outcomes for parents of a child with a CI (Figure 1). Coping style, known as the way people react to stressful situations, plays an important role in the model. Engaged coping (e.g., problem solving, cognitive restructuring) is proven to be more effective for good psychosocial adjustment, including anxiety and depression, than disengaged or passive coping (e.g., self-criticism, social withdrawal; Compas et al., 2012; Edgar & Skinner, 2003). Several personal (e.g., temperament), family (e.g., parent–child relationship) and environmental factors (e.g., practical and emotional support from others) have an effect on parents’ coping style (Guðmundsdóttir et al., 2006) and are therefore important determinants to address in an intervention. When engaged coping can be reached, parents will likely have better psychosocial adjustment and outcomes and more capability to manage their child’s illness effectively.
Figure 1.
Adapted version of the disability-stress-coping model of Wallander and Varni (1998) to explain symptoms of anxiety and depression in parents of a child with a chronic illness. Note.1Op Koers Questionnaire for Parents, 2Illness Cognition Questionnaire for Parents, 3Cognitive Coping Strategies Scale Parent Form, and 4Hospital Anxiety and Depression Scale.
Cognitive behavioral therapy (CBT) and acceptance and commitment therapy (ACT) are examples of therapies to teach how to use engaged coping strategies. CBT and ACT have been shown effective in improving psychological outcomes such as stress- and health-related quality of life of children with a CI and their families (Kemani et al., 2018; Law et al., 2017; Palermo et al., 2016; Wynne et al., 2019). CBT involves identifying unhelpful thoughts, challenging them, and replacing them with helpful thoughts (Butler et al., 2006). ACT, as a part of CBT, aims to reduce the influence of negative thoughts on daily life by accepting certain thoughts or situations. Exercises such as mindfulness and values elicitation to orientate participants to thoughts and activities which are in line with personally meaningful values are often used (Hayes et al., 2006). ACT could be helpful for parents of a child with a CI, since those parents often face situations which cannot be changed and ACT provides helpful tools to learn how to deal with such situations.
Studies have shown that sharing experiences with others in a similar situation is associated with a decrease of distress and improvement of mental health (Niela-Vilén et al., 2014; Ramchand et al., 2017; Tully et al., 2017). Offering group interventions to parents may therefore be an effective way to support them. Most existing group interventions which involve parents are child-focused: the parents learn how to support their child in managing the illness (Kemani et al., 2018; Palermo et al., 2016; Scholten et al., 2013). During the past years, there is more attention to psychosocial support focusing on parents themselves (Pelentsov et al., 2015). However, parents often experience practical barriers for participation in interventions, such as travel time, distance and costs, taking care of the children and absence from work (Heath et al., 2018; Pettersson et al., 2009). An online intervention can increase participation rates: it eliminates or decreases those barriers because participation from home is possible (Andrews et al., 2010; Fitzgerald et al., 2010).
Considering this, an online psychosocial CBT/ACT group intervention called Op Koers Online (English: On Track Online) for parents, focusing on parents themselves, was designed in close cooperation with parents. Parents were asked via an open access survey and focus groups what they would like in an intervention (Douma et al., 2019a). The intervention is partly based on the already existing Op Koers face-to-face intervention for children, adolescents and parents, which was proven to be effective (Scholten et al., 2013), and on Op Koers Online for adolescents of which pilot studies showed promising results on feasibility and preliminary efficacy (Douma et al., 2019b; Maurice-Stam et al., 2014). Op Koers Online is chatroom delivered without the use of video to ensure anonymity, which can be beneficial because it could be easier to talk about problems when nobody knows or sees you (Maurice-Stam et al., 2014).
In a randomized controlled trial (RCT) we aimed to answer the following research question: Is Op Koers Online for parents of a child with CI an efficacious intervention? We hypothesized that Op Koers Online for parents had a positive effect on parental anxiety and depression and on the use of adaptive coping skills. Outcomes were symptoms of anxiety and depression and disease-related coping skills, including skills that match the content of the intervention and more generic illness cognitions (see Figure 1).
Materials and Methods
Study Design
In a parallel RCT, we used the data of the online questionnaires that were completed at baseline (before randomization; T0), at 6-months (T1) and at 12-months (T2) follow-up from baseline. Approval of the Medical Ethical Committee of the Amsterdam University Medical Centers was obtained for this study. Full details of the study protocol and the intervention content were reported previously (registry number ISRCTN83623452; Douma et al., 2018). Participants from both the waitlist control and intervention group received care-as-usual and were not prevented to seek individual psychosocial treatment.
Procedure
The study was conducted between July 2016 and April 2019. Participants were recruited between July 2016 and March 2018. Recruitment was done via the outpatient clinics of nine public hospitals all over The Netherlands with information letters and pamphlets, and across the Netherlands through patient associations with online advertisement and social media. Interested parents could use the reply form attached to the information letter or pamphlet, or could send an e-mail. After a positive reply, parents were phoned by the researcher, a psychologist, to assess eligibility and to obtain informed consent. Inclusion criteria were being caregiver of a child between the ages of 0 and 18 years with a physical CI diagnosis, according to the following criteria set forth by Mokkink et al. (2008): (a) onset between ages 0 and 18; (b) diagnosis based on medical scientific knowledge; (c) the illness is not (yet) curable; and (d) the illness has been present for at least 3 months, or at least three episodes have occurred in the last year. Furthermore, having access to a laptop/computer/tablet with internet connection was necessary to participate in the intervention and to complete online questionnaires at home or at another location. Exclusion criteria were having cognitive disabilities or language problems which limited the ability to participate in the intervention and/or to fill out questionnaires. Participants received a voucher of EUR 20 after completing all assessments.
Randomization
The randomization into intervention and waitlist control group was carried out by an independent IT worker from a company for e-health development who administers the website for Op Koers Online. Block randomization with block size four was performed, based on a previously generated randomization schedule with allocation ratio 1:1. Because the recruitment period was spread out over time, randomization took place at four time points. When randomized in the intervention group, the researcher called the participant to schedule the intervention. Participants in the waitlist control group were given the opportunity to participate in the intervention after the final follow-up assessment. The researchers were not blinded to group assignment.
Intervention
The intervention consists of six weekly 90-min sessions and a booster session 4 months after the last regular session. The goal of the intervention is to prevent and/or reduce psychosocial problems by teaching the use of adaptive disease-related coping skills. In the first session parents get to know each other and receive explanation about the intervention. The following sessions each focus on a theme: session (a) the CI of the child, (b) relationships within the family, (c) taking care of yourself, and (d) relationships with others and practical support (e.g., school of the child, work). In the sixth and last session there is time to repeat topics or to resume discussions that have not been finished due to lack of time (Douma, et al., 2019a). Coping skills were addressed in every session. Depending on the subjects that came up during the session, course leaders addressed the different coping skills accordingly. To teach coping skills, CBT and ACT techniques, such as relaxation, cognitive restructuring and exercises focusing on accepting the child’s diagnosis, are used (Douma et al., 2018).
Sessions take place at a scheduled time in a secured chatroom with three to five parents under supervision of two psychologists (course leaders), who carry out the protocolled intervention. After each session, course leaders filled out a log providing information about the session: particularities of participant’s absence or situation, any technological issues and whether or not course leaders followed the intervention protocol. The log was checked by the coordinating researcher. Assessment of the log did not show any major deviations of the intervention protocol.
All course leaders (N = 22 in total; all female) from the participating hospitals are extensively trained during an 8-hour workshop in using the detailed intervention protocol. The workshop was led by the coordinating researchers of the study and took place in the Emma Children’s Hospital. It included a theoretical part and exercises to learn how to use the website.
Groups are composed based on the age of the children as much as possible for better match within groups. Parents log on to the website (http://www.opkoersonline.nl) to enter the chatroom, to read additional material about the themes, and to complete homework assignments in their personal environment. An extensive login manual with an explanation in person was provided to guide the parents through logging on and using their own personal environment.
Measures
Socio-Demographic and Illness Characteristics
Socio-demographic characteristics were obtained with an online questionnaire assessing age, gender, income, educational level, ethnicity, and former psychological help. Illness characteristics (diagnosis, duration, severity) of the child (see Table I) were assessed with this questionnaire as well. Parents rated illness severity using a proxy measure based on the occurrence of the following 13 possible consequences of CI in the past year (scale 0–13): doctor visits, hospitalization, surgery, use of medication, dietary consequences, visible malformations, nonvisible malformations, use of appliances, limitations in movements, problems with hearing, vision, and speech (0 = no and 1 = yes) and course of the disease (0 = improving/stable and 1 = deterioration/unstable).
Table I.
Socio-Demographic Characteristics of Parents Included in the Analyses
| Intervention group (N = 34) | Waitlist Control group (N = 33) | p a | |
|---|---|---|---|
| Age (in years) | 42.29 (6.36) range 30.21–59.07 | 42.71 (5.78) range 32.32–54.92 | .775 (t = .29) |
| Gender | .493 (χ2 = 1.05)b | ||
| Male | 0% | 3% | |
| Female | 100% | 97% | |
| Income | .507 (χ2 = .44) | ||
| <Modalc | 29% | 37% | |
| ≥Modal | 71% | 63% | |
| Ethnicity | .340 (χ2 = 1.48)2 | ||
| Dutch | 76% | 88% | |
| Non-Dutch | 24% | 12% | |
| Diagnosis of the child | |||
| Asthma | 5% | 6% | |
| Epilepsy | 5% | 6% | |
| Type 1 diabetes | 11% | 29% | |
| IBD | 11% | 0% | |
| Kidney disease | 11% | 6% | |
| Otherd | 57% | 53% | |
| Illness duration (in years) | 5.65 (4.52) | 6.18 (4.48) | .628 (t = .49) |
| Illness severity (Scale 0–13) | 5.29 (1.99) | 5.06 (1.92) | .627 (t = −.49) |
| Former psychological help | .803 (χ2 = .06) | ||
| Yes | 79% | 82% | |
| No | 21% | 18% | |
| Educational level parents | .177 (χ2 = 1.83) | ||
| Low/intermediatee | 44% | 61% | |
| Highf | 56% | 39% |
Group differences tested with independent samples t-tests for continuous variables and χ2-tests for categorical variables.
Fisher’s exact test.
A model income corresponds to 34,500 euros per year.
Other diseases occurred once, examples are congenital muscular dystrophy, methylmalonic acidemia, and epidermolysis bullosa.
Primary education, lower and middle vocational education, lower and middle general secondary education, higher secondary education, and pre-university education.
Higher vocational education and university.
Anxiety and Depression
The Hospital Anxiety and Depression Scale (HADS) was used to assess anxiety and depression (Bjelland et al., 2002; Zigmond & Snaith, 1983). This 14-item questionnaire is divided into two 7-item scales; anxiety (e.g., “I feel tense”), depression (e.g., “I have lost interest in my appearance”) and a total sum score of all items. Items are scored on a 4-point Likert scale (range 0 = not at all to 3 = very often). Higher scores indicate more anxiety or depression in the past week. A scale score of 8 or above (cut-off score) is considered as an indicator for clinically significant anxiety or depression for both men and women, which means that the parent may need professional help. Internal consistency (Cronbach’s alpha) was moderate to good (range .61 for anxiety to .88 for depression) in this study. Norm data representative of Dutch parents between 20 and 60 years old are available (Vingerhoets, 2012).
Disease-Related Coping Skills
The Op Koers Questionnaire for Parents (OKQ-P) assesses the use of disease-related coping skills taught in the intervention (Scholten et al., 2013). Parents are asked if they agree with 25 statements on a 4-point Likert scale (range 1 = almost never/never to 4 = always/almost always). Higher scores reflect use of more engaged coping skills. Items are divided into four subscales: open communication (nine items; e.g., “I can inform the people around me about the impact of the illness of my child myself”), relaxation (eight items; e.g., “I know how to relax myself”), social support (four items; e.g., “I am able to ask for support to the people around me”) and positive thinking (four items; e.g., “I know how to worry less about the consequences of the illness of my child”). Internal consistency (Cronbach’s alpha) was moderate to good (range .57 for positive thinking to .78 for relaxation) in this study.
The Illness Cognition Questionnaire for Parents (ICQ-P) measures parental illness cognitions that reflect different ways of assigning meaning to the CI of their child (Evers et al, 1998; Nicolaas et al., 2016). Parents have to indicate to what extent statements fit their situation on a 4-point Likert scale (ranging from 1 = not at all to 4 = completely). Higher scores indicate that statement fits the respondent’s situation to a larger degree. Items are divided over three 6-item subscales; helplessness (e.g., “The illness of my child controls my life”), acceptance (e.g., “I can handle the problems related to my child’s illness”), and disease benefits (e.g., “Dealing with the illness of my child has made me a stronger person”). Cronbach’s alphas were satisfactory (range .79–.93) in this study.
The Cognitive Coping Strategies Scale Parent Form (CCSS-PF) assesses to what extent parents of children with a chronic or life-threatening illness try to maintain a sense of cognitive control, by relying on cognitive coping strategies (Grootenhuis & Last, 2001; Grootenhuis et al., 1996). The predictive control strategy was used in this study. This domain consists of five statements (e.g., “When I think about the illness of my child, I assume it will be all right”), on which parents can indicate on a 4-point Likert scale (ranging from 1= totally agree to 4 = totally disagree) to what extent they agree. Item scores are recoded so that higher scores indicate that parents are more optimistic about the course of the child’s disease. Cronbach’s alphas were good (range .80–.85) in this study.
Data Analyses
Post-hoc power calculations based on the inclusion rates of this study with three time points indicated that differences of medium size (d = .59) between study groups over time at a significance level of p = .05 with a power of .80 (Twisk, 2013) could be detected. Preliminary analyses examined baseline differences between the intervention and waitlist control group on socio-demographic and illness characteristics and on the outcome variables. To characterize the sample in terms of anxiety and depression, percentage of parents with scores in the clinical range were compared with a Dutch norm group with χ2 tests.
Linear mixed models analyses were performed to examine efficacy of the intervention accounting for dependency of data within participants. The intraclass correlation coefficients indicated that correcting the analyses for dependency within treatment groups was not necessary, as they were not significant (or below .05). Outliers on outcome measures were rescaled according to Tabachnick and Fidell (2013). Intention-to-treat analyses were performed based on the random allocation, using the mixed-model procedure in SPSS (19.0) with full maximum likelihood estimation. Participants were included in the analyses if data at baseline (T0) were available as well as data at T1 and/or at T2. Missing data were not imputed. To facilitate interpretation of regression coefficients, all continuous scores were standardized, expressing deviations from the mean at T0. For binary-coded variables, standardized regression coefficients of .2 were considered small, .5 medium, and .8 large (Cohen, 1998).
Dependent variables were anxiety, depression and HADS total score, and disease-related coping skills. Linear mixed models were fitted with a random intercept and fixed slopes for study group (intervention vs. waitlist control), time (T1 vs. T0 and T2 vs. T0) and the interaction term study group x time. Potential differences between intervention and waitlist control group on outcome measures at T0 were controlled for by the random intercept. Because no differences were found between the intervention and the control group, no other variables were added to the models. An alpha of .05 was used to test the statistical significance of the effects.
Results
Sample Characteristics
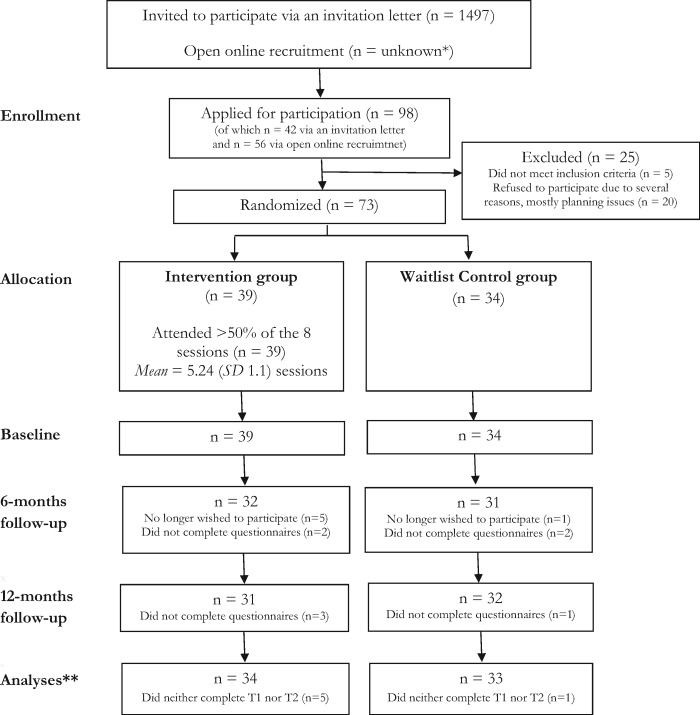
Figure 2 shows the participant flow from recruitment to follow-up. The exact number of invited parents was unknown and information of nonrespondents was lacking, because recruitment was partly done through online advertisement and patient associations. A total of 98 parents applied for participation. The majority of all applicants (57%) applied after seeing an online advertisement. Of the 98 applicants, 25 (26%) dropped out before randomization mostly due to practical problems (most common: expecting to be unable to spend enough time on study participation and/or following the intervention due to a busy family life, work, etc.). In the end, 73 parents were randomized, of whom 67 (92%) could be included in the analyses.
Figure 2.
Participant flow through the study. Note. *Open recruitment was done via patient associations, social media and advertisements on websites. The number of parents reached online is unknown and **number of participants with baseline data and at least one follow-up assessment completed.
Of the 67 parents who were included in the analyses, 34 were assigned to the intervention group (Mean age = 42.40 SD = 6.10; 100% female) and 33 to the waitlist control group (Mean age = 42.90 SD = 5.82; 97% female). No significant differences in socio-demographic and illness characteristics (Table I), psychosocial problems and outcome variables at baseline were found between the intervention and the waitlist control group. Regarding psychosocial problems at baseline, 47% of the participants in the intervention group and 27% in the waitlist control group showed clinically significant anxiety symptoms. The percentages for clinically significant depression symptoms were 29% and 24% respectively. Participants in both the intervention and the waitlist control group scored significantly more often in the clinical range than the norm group (p < .05) (van Oers et al., 2014; Vingerhoets, 2012), except for the waitlist control group on anxiety (p = .24). No adverse events occurred during the RCT.
Anxiety and Depression
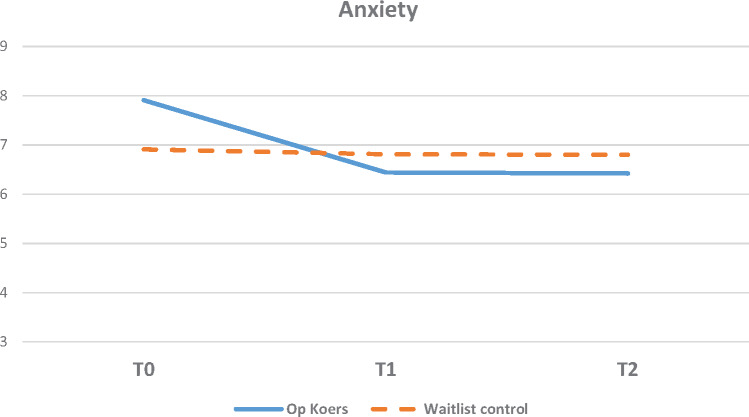
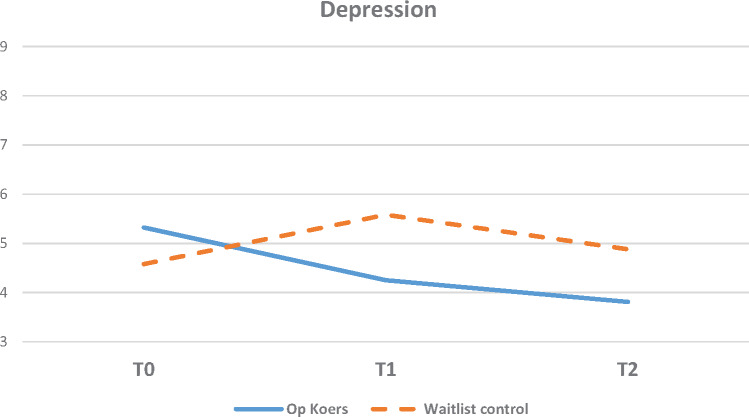
Significant beneficial effects of the intervention (p < .05) were found at 6 and 12 months follow-up (T1 and T2 vs. T0) for symptoms of anxiety (Figure 3), symptoms of depression (Figure 4) and the total score on the HADS; regression coefficients ranged from β = −.39 (anxiety T2 vs. T0) to β = −.51 (total score T1 vs. T0; Table II). The intervention group improved over time compared with baseline (T0), whereas the waitlist control group did not.
Figure 3.
Symptoms of anxiety measured with the Hospital Anxiety and Depression Scale (HADS) at T0 (baseline), T1 (6-months follow-up) and T2 (12-months follow-up); intervention (Op Koers) and waitlist control group.
Figure 4.
Symptoms of depression measured with the Hospital Anxiety and Depression Scale (HADS) at T0 (baseline), T1 (6-months follow-up) and T2 (12-months follow-up); intervention (Op Koers) and waitlist control group.
Table II.
Means, SD at Baseline (T0), 6- (T1) and 12-Month Follow-Up (T2) and Results of Linear Mixed-Model Analyses
| Intervention group |
Waitlist control group |
Intervention*time |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| T0 (N = 34) | T1 (N = 32) | T2 (N = 31) | T0 (N = 33) | T1 (N = 31) | T2 (N = 32) | T0–T1 (intervention versus waitlist control group) |
T0–T2 (intervention versus waitlist control group) |
|||
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | β [95% CI]a | p | β [95% CI]a | p | |
| Anxiety and depression (HADS)b | ||||||||||
| Anxiety | 7.91 (3.02) | 6.44 (3.25) | 6.42 (2.98) | 6.91 (3.41) | 6.81 (2.97) | 6.80 (3.22) | −.47 [−0.84; −1.0] | .014 | −.39 [−0.76; −0.01] | .043 |
| Depression | 5.32 (3.91) | 4.25 (3.36) | 3.81 (4.14) | 4.58 (3.63) | 5.58 (4.30) | 4.88 (4.26) | −.49 [−0.9; −0.08] | .020 | −.43 [−0.84; −0.02] | .039 |
| Total | 13.24 (6.22) | 10.69 (5.94) | 10.23 (6.75) | 11.48 (6.50) | 12.39 (6.53) | 11.68 (6.75) | −.51 [−0.89; −0.14] | .007 | −.46 [−0.83; −0.09] | .016 |
| Coping (OKQ−P)c | ||||||||||
| Open communication | 3.10 (0.50) | 3.39 (0.40) | 3.33 (0.48) | 3.12 (0.55) | 3.17 (0.48) | 3.18 (0.54) | .43 [0.08; 0.79] | .018 | .28 [−0.07; 0.64] | .120 |
| Relaxation | 2.74 (0.57) | 2.94 (0.49) | 2.98 (0.52) | 2.73 (0.53) | 2.62 (0.45) | 2.69 (0.47) | .49 [0.08; 0.9] | .020 | .42 [0.01; 0.83] | .043 |
| Social support | 2.84 (0.57) | 3.09 (0.55) | 3.07 (0.56) | 2.85 (0.73) | 2.73 (0.68) | 2.88 (0.74) | .52 [0.07; 0.97] | .025 | .25 [−0.2; 0.7] | .271 |
| Positive thinking | 2.64 (0.35) | 2.82 (0.37) | 2.89 (0.41) | 2.60 (0.37) | 2.60 (0.29) | 2.61 (0.36) | .37 [−0.16; 0.89] | .168 | .53 [0.01; 1.05] | .045 |
| ICQ-Pd | ||||||||||
| Helplessness | 5.58 (3.69) | 4.13 (2.79) | 3.97 (3.18) | 4.39 (3.47) | 4.87 (3.59) | 4.41 (3.47) | −.47 [−0.86; −0.09] | .017 | −.36 [−0.74; 0.03] | .067 |
| Acceptance | 10.21 (4.39) | 12.28 (4.39) | 13.06 (3.73) | 12.58 (3.29) | 12.58 (3.16) | 13.62 (3.28) | .42 [0.03; 0.82] | .037 | .30 [−0.09; 0.7] | .134 |
| Disease benefits | 10.42 (4.49) | 11.22 (4.05) | 11.61 (5.15) | 10.15 (4.51) | 10.00 (5.02) | 10.12 (4.62) | .16 [−0.2; 0.51] | .379 | .21 [−0.15; 0.56] | .253 |
| CCSS-PRe | ||||||||||
| Predictive control | 2.64 (0.28) | 2.83 (0.62) | 2.83 (0.52) | 2.53 (0.38) | 2.37 (0.62) | 2.50 (0.64) | .88 [0.11; 1.65] | .025 | .47 [−0.29; 1.24] | .223 |
Note: Significant (p < .05) intervention effects (β) are presented in bold.
95% confidence interval.
Hospital Anxiety and Depression Scale.
Op Koers Questionnaire for Parents.
Illness Cognition Questionnaire for Parents;.
Cognitive Coping Strategies Scale Parent Form.
Disease-Related Coping Skills
Significant beneficial effects of the intervention (p < .05) on use of disease-related coping skills were found at 6 months follow-up (T1 vs. T0) for open communication, relaxation, social support (OKQ-P), helplessness, and acceptance (ICQ-P), predictive control (CCSS-PF); regression coefficients ranged from β = .42 (acceptance) to β = .88 (predictive control; Table II). Significant effects at 12-months (T2 vs. T0) follow-up were found for relaxation (β = .42) and positive thinking (β = .53), whereas the intervention effect on helplessness was marginally significant (β = -.36, p = .067; Table II). Overall, the intervention group improved over time compared with baseline (T0), whereas the waitlist control group did not.
Discussion
This RCT indicated evidence for the efficacy of Op Koers Online for parents, an online psychosocial group intervention for parents of children with different types of CI: the intervention had a positive effect of medium size on symptoms of parental anxiety and depression and on the disease-related coping skills open communication, relaxation, social support, positive thinking, helplessness, acceptance and predictive control. Until now, suitable interventions for parents with a focus on parents’ own mental health and behavior have been lacking (Eccleston et al., 2015). This study contributes to the field of pediatric psychology with a protocol- and evidence-based intervention for this vulnerable group of parents. The online character, the focus on parents themselves instead of on their child and the possibility for parents of children with rare illnesses to participate, are innovative and unique aspects of Op Koers Online for parents. Moreover, this study shows the gateway of the internet for offering interventions to parents. The possibility to participate from home, thereby limiting logistical and practical barriers, increases the opportunities for participation.
Effects of Op Koers Online for parents on anxiety and depression symptoms were significant and of medium size at both follow-up moments. This is an important outcome, as depression in parents can cause poorer outcomes for the child (Eckshtain et al., 2010). According to the model of Wallander and Varni and our adapted version of that model (Figure 1), parents with better psychosocial functioning are more able to support their child with a CI adequately (Cousino & Hazen, 2013), which will likely be related to better psychosocial and illness-related outcomes for the children (Celano et al., 2008; Otsuki et al., 2010). Therefore, following Op Koers Online benefits the parents as well as the children. Op Koers Online is an important addition to the toolbox of clinicians to support parents of a child with an easily accessible group intervention.
Regarding disease-related coping skills, some of the significant intervention effects of medium size at 6-months diminished at 12 months follow-up. At 12 months, only effects on the coping skills relaxation and positive thinking were found. According to the literature, coping skills could be expected to mediate the effect of the intervention on parental anxiety and depression outcomes. In our study, continued reliance on relaxation and positive thinking may explain the long-term significant outcomes on anxiety and depression. Future research should examine the working mechanism of Op Koers Online and the possible mediating effect of relaxation and positive thinking. Furthermore, attention should be paid to the other coping skills and maintaining the effects on the long-term.
During the recruitment period, we had problems with recruiting the desired amount of participants, which is common in RCT’s (Watson & Torgerson, 2006). When implementing the intervention in clinical practice, it is important to keep in mind that professionals should invest time and effort in recruitment and guiding parents through the online environment of the intervention. Luckily, although the sample size was slightly smaller than intended, this was hardly at the expense of the power of the study. A priori power analysis was based on the detection of an intervention effect of medium size with d ≈ 50, whereas the post-hoc power analysis revealed that with the current sample size we were still able to detect an intervention effect of medium size with d = .59.
In this RCT, almost all participants were mothers. We experienced that fathers are hard to reach due to several reasons, mostly having lack of time and indicating no need for support. However, we know from the literature that fathers of children with Down syndrome do express a need for psychosocial support (Marchal et al., 2017). We recognize this finding as there were some fathers that were interested in the intervention; however, they expected mostly mothers to participate and were hesitant of participating in a group with only female participants. Although we tried to encourage those fathers to participate, this was a reason not to do so for some of them. A possible solution could be to schedule separate groups for fathers once or twice a year. In the future, caregivers should offer this option and should pay attention to motivating fathers to participate.
Strengths of this study included (a) recruitment of participants across the whole country from nine centers and via patient associations and (b) using a standardized intervention protocol which is essential for conducting sound intervention research and for implementation in clinical practice. The study had some limitations as well. First, the unknown recruitment and enrollment rates and the lack of information about nonrespondents, because of the partially online open recruitment. Second, outcomes were based on mothers, which limit the representativeness of the results. Third, we relied on self-reported outcome measurements, which had a risk for socially desirable answers or concealing of symptoms. This could have led to an overestimation of the intervention effect and should be taken into account while interpreting the results. Fourth, the baseline levels of anxiety and depression seemed higher in the intervention group than in the control group. Though the differences were not significant and the mixed models analyses corrected for baseline differences between intervention and control group, the intervention group might have had more room for improvement. Finally, the internal consistency of anxiety, open communication, social support and positive thinking was moderate on one or more time points. On the one hand, the use of scales with moderate internal consistency is acceptable for group comparisons because the internal consistency is an indication of random error and has nothing to do with systematic error (bias). On the other hand, Cronbach’s alphas should preferably be .7 or higher because the lower the internal consistency, the larger the random measurement error, and so, the more difficult to detect differences between groups. Considering the significant betas for anxiety, open communication, social support and positive thinking (see Table II), we can conclude that intervention effects were not overlooked due to moderate Cronbach’s alpha.
In conclusion, the results indicated that Op Koers Online for parents has a positive effect on maternal anxiety and depression and use of disease-related coping skills. The next step for clinical practice is to help more parents by implementing Op Koers Online for parents in hospitals across the country, by training more psychologists in using the manual to carry out the intervention. In the future, Op Koers Online can be translated for non-Dutch speaking parents in the Netherlands.
Supplementary Data
Supplementary data can be found at: https://academic.oup.com/jpepsy.
Supplementary Material
Acknowledgments
We thank the parents who participated in this study and acknowledge the contributions of the staff at the participating centers (with special thanks to the local investigators: I. M. Visser, W. Meerstra, E. M. van Dijk-Lokkart, E. Kakes, S. Jansen-Kamphorst). Finally, we would like to thank Ad Vingerhoets for providing the HADS reference data.
Funding
This study was funded by Fonds NutsOhra (FNO; grant number: 100.977).
Conflicts of interest: None declared.
References
- Andrews G., Cuijpers P., Craske M. G., McEvoy P., Titov N. (2010). Computer therapy for the anxiety and depressive disorders is effective, acceptable and practical health care: A meta-analysis. PLoS One, 5(10), e13196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjelland I., Dahl A. A., Haug T. T., Neckelmann D. (2002). The validity of the Hospital Anxiety and Depression Scale: An updated literature review. Journal of Psychosomatic Research, 52(2), 69–77. [DOI] [PubMed] [Google Scholar]
- Butler A. C., Chapman J. E., Forman E. M., Beck A. T. (2006). The empirical status of cognitive-behavioral therapy: A review of meta-analyses. Clinical Psychology Review, 26(1), 17–31. [DOI] [PubMed] [Google Scholar]
- Celano M., Bakeman R., Gaytan O., Smith C. O., Koci A., Henderson S. (2008). Caregiver depressive symptoms and observed family interaction in low‐income children with persistent asthma. Family Process, 47(1), 7–20. [DOI] [PubMed] [Google Scholar]
- Cohen J. (1998). Statistical power analysis for the behavioural sciences. Academy Press. [Google Scholar]
- Collis D., Kennedy‐Behr A., Kearney L. (2019). The impact of bowel and bladder problems on children’s quality of life and their parents: A scoping review. Child: Care, Health and Development, 45(1), 1–14. [DOI] [PubMed] [Google Scholar]
- Compas B. E., Jaser S. S., Dunn M. J., Rodriguez E. M. (2012). Coping with chronic illness in childhood and adolescence. Annual Review of Clinical Psychology, 8(1), 455–480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coughlin M. B., Sethares K. A. (2017). Chronic sorrow in parents of children with a chronic illness or disability: An integrative literature review. Journal of Pediatric Nursing, 37, 108–116. [DOI] [PubMed] [Google Scholar]
- Cousino M. K., Hazen R. A. (2013). Parenting stress among caregivers of children with chronic illness: A systematic review. Journal of Pediatric Psychology, 38(8), 809–828. [DOI] [PubMed] [Google Scholar]
- Douma M., Bouman C. P., van Oers H. A., Maurice-Stam H., Haverman L., Grootenhuis M. A., Scholten L. (2019. a). Matching psychosocial support needs of parents of a child with a chronic illness to a feasible intervention. Maternal and Child Health Journal, 24, 1238-1247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Douma M., Joosten M. M. H., Maurice-Stam H., Scholten L., Grootenhuis M. A. (2019. b). Online cognitive-behavioral group intervention for adolescents with chronic illness: A pilot study. Clinical Practice in Pediatric Psychology, 7(1), 79–92. [Google Scholar]
- Douma M., Scholten L., Maurice-Stam H., Grootenhuis M. A. (2018). Online cognitive-behavioral based group interventions for adolescents with chronic illness and parents: Study protocol of two multicenter randomized controlled trials. BMC Pediatrics, 18(1), 235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eccleston C., Fisher E., Law E., Bartlett J., Palermo T. M. (2015). Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database of Systematic Reviews, (4), CD009660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eckshtain D., Ellis D. A., Kolmodin K., Naar-King S. (2010). The effects of parental depression and parenting practices on depressive symptoms and metabolic control in urban youth with insulin dependent diabetes. Journal of Pediatric Psychology, 35(4), 426–435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edgar K., Skinner T. (2003). Illness representations and coping as predictors of emotional well-being in adolescents with type 1 diabetes. Journal of Pediatric Psychology, 28(7), 485–493. [DOI] [PubMed] [Google Scholar]
- Evers A., Kraaimaat F., Van Lankveld W., Jacobs J., Bijlsma J. (1998). Ziekte-Cognitie-Lijst (ZCL). Clinical Psychology, 69, 1026–1036. [PubMed] [Google Scholar]
- Fitzgerald T. D., Hunter P. V., Hadjistavropoulos T., Koocher G. P. (2010). Ethical and legal considerations for internet-based psychotherapy. Cognitive Behavior Therapy, 39(3), 173–187. [DOI] [PubMed] [Google Scholar]
- Grootenhuis M. A., Last B. F. (2001). Children with cancer with different survival perspectives: Defensiveness, control strategies, and psychological adjustment. Psycho‐Oncology, 10(4), 305. [DOI] [PubMed] [Google Scholar]
- Grootenhuis M. A., Last B. F., De Graaf‐Nijkerk J. H., Van Der Wel M. (1996). Secondary control strategies used by parents of children with cancer. Psycho‐Oncology, 5(2), 91–102. [Google Scholar]
- Guðmundsdóttir H., Guðmundsdóttir D., Elklit A. (2006). Risk and resistance factors for psychological distress in Icelandic parents of chronically ill children: An application of Wallander and Varni’s disability-stress-coping model. Journal of Clinical Psychology in Medical Settings, 13(3), 295–302. [Google Scholar]
- Hatzmann J., Heymans H. S., Ferrer-I-Carbonell A., van Praag B. M., Grootenhuis M. A. (2008). Hidden consequences of success in pediatrics: Parental health-related quality of life—Results from the Care Project. Pediatrics, 122(5), e1030–e1038. [DOI] [PubMed] [Google Scholar]
- Hatzmann J., Maurice-Stam H., Heymans H. S., Grootenhuis M. A. (2009). A predictive model of health related quality of life of parents of chronically ill children: The importance of care-dependency of their child and their support system. Health and Quality of Life Outcomes, 7(1), 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hatzmann J., Peek N., Heymans H., Maurice-Stam H., Grootenhuis M. (2014). Consequences of caring for a child with a chronic disease: Employment and leisure time of parents. Journal of Child Health Care, 18(4), 346–357. [DOI] [PubMed] [Google Scholar]
- Haverman L., van Oers H. A., Limperg P. F., Houtzager B. A., Huisman J., Darlington A.-S., Maurice-Stam H., Grootenhuis M. A. (2013). Development and validation of the distress thermometer for parents of a chronically ill child. The Journal of Pediatrics, 163(4), 1140–1146.e1142. [DOI] [PubMed] [Google Scholar]
- Hayes S. C., Luoma J. B., Bond F. W., Masuda A., Lillis J. (2006). Acceptance and commitment therapy: Model, processes and outcomes. Behaviour Research and Therapy, 44(1), 1–25. [DOI] [PubMed] [Google Scholar]
- Heath J., Williamson H., Williams L., Harcourt D. (2018). Parent-perceived isolation and barriers to psychosocial support: A qualitative study to investigate how peer support might help parents of burn-injured children. Scars, Burns & Healing, 4, 205951311876380.https://doi.org/10.2059513118763801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemani M. K., Kanstrup M., Jordan A., Caes L., Gauntlett-Gilbert J. (2018). Evaluation of an intensive interdisciplinary pain treatment based on acceptance and commitment therapy for adolescents with chronic pain and their parents: A nonrandomized clinical trial. Journal of Pediatric Psychology, 43(9), 981–994. [DOI] [PubMed] [Google Scholar]
- Law E. F., Fisher E., Howard W. J., Levy R., Ritterband L., Palermo T. M. (2017). Longitudinal change in parent and child functioning after internet-delivered cognitive-behavioral therapy for chronic pain. Pain, 158(10), 1992–2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchal J. P., van Oers H. A., Maurice-Stam H., Grootenhuis M. A., van Trotsenburg A. S. P., Haverman L. (2017). Distress and everyday problems in Dutch mothers and fathers of young adolescents with Down syndrome. Research in Developmental Disabilities, 67, 19–27. [DOI] [PubMed] [Google Scholar]
- Maurice-Stam H., Scholten L., de Gee E. A., van der Zanden R. A., Conijn B., Last B. F., Grootenhuis M. A. (2014). Feasibility of an online cognitive behavioral-based group intervention for adolescents treated for cancer: A pilot study. Journal of Psychosocial Oncology, 32(3), 310–321. [DOI] [PubMed] [Google Scholar]
- Mokkink L. B., Van Der Lee J. H., Grootenhuis M. A., Offringa M., Heymans H. S.; The Dutch National Consensus Committee “Chronic Diseases and Health Conditions in Childhood”. (2008). Defining chronic diseases and health conditions in childhood (0–18 years of age): National consensus in the Netherlands. European Journal of Pediatrics, 167(12), 1441–1447. [DOI] [PubMed] [Google Scholar]
- Nicolaas S. M. S., Schepers S. A., van den Bergh E. M., Evers A. W., Hoogerbrugge P. M., Grootenhuis M. A., Verhaak C. M. (2016). Illness cognitions and family adjustment: Psychometric properties of the Illness Cognition Questionnaire for parents of a child with cancer. Supportive Care in Cancer, 24(2), 529–537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Niela-Vilén H., Axelin A., Salanterä S., Melender H.-L. (2014). Internet-based peer support for parents: A systematic integrative review. International Journal of Nursing Studies, 51(11), 1524–1537. [DOI] [PubMed] [Google Scholar]
- Otsuki M., Eakin M. N., Arceneaux L. L., Rand C. S., Butz A. M., Riekert K. A. (2010). Prospective relationship between maternal depressive symptoms and asthma morbidity among inner-city African American children. Journal of Pediatric Psychology, 35(7), 758–767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palermo T. M., Law E. F., Fales J., Bromberg M. H., Jessen-Fiddick T., Tai G. (2016). Internet-delivered cognitive-behavioral treatment for adolescents with chronic pain and their parents: A randomized controlled multicenter trial. Pain, 157(1), 174–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pelentsov L. J., Laws T. A., Esterman A. J. (2015). The supportive care needs of parents caring for a child with a rare disease: A scoping review. Disability and Health Journal, 8(4), 475–491. [DOI] [PubMed] [Google Scholar]
- Pettersson C., Lindén-Boström M., Eriksson C. (2009). Reasons for non-participation in a parental program concerning underage drinking: A mixed-method study. BMC Public Health, 9(1), 478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pinquart M. (2018). Parenting stress in caregivers of children with chronic physical condition-A meta-analysis. Stress and Health, 34(2), 197–207. [DOI] [PubMed] [Google Scholar]
- Pinquart M. (2019. a). Featured article: Depressive symptoms in parents of children with chronic health conditions: A meta-analysis. Journal of Pediatric Psychology, 44(2), 139–149. [DOI] [PubMed] [Google Scholar]
- Pinquart M. (2019. b). Meta-analysis of anxiety in parents of young people with chronic health conditions. Journal of Pediatric Psychology, 44(8), 959–969. [DOI] [PubMed] [Google Scholar]
- Ramchand R., Ahluwalia S. C., Xenakis L., Apaydin E., Raaen L., Grimm G. (2017). A systematic review of peer-supported interventions for health promotion and disease prevention. Preventive Medicine, 101, 156–170. [DOI] [PubMed] [Google Scholar]
- Scholten L., Willemen A. M., Last B. F., Maurice-Stam H., van Dijk E. M., Ensink E., Zandbelt N., van der Hoop-Mooij A., Schuengel C., Grootenhuis M. A. (2013). Efficacy of psychosocial group intervention for children with chronic illness and their parents. Pediatrics, 131(4), e1196–e1203. [DOI] [PubMed] [Google Scholar]
- Tabachnick B. G., Fidell L. S. (2013). Using multivariate statistics. (6th edn).Pearson. [Google Scholar]
- Tully C., Shneider C., Monaghan M., Hilliard M. E., Streisand R. (2017). Peer coaching interventions for parents of children with type 1 diabetes. Current Diabetes Reports, 17(6), 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twisk J. W. (2013). Applied longitudinal data analysis for epidemiology: A practical guide. University Press. [Google Scholar]
- van Oers H. A., Haverman L., Limperg P. F., van Dijk-Lokkart E. M., Maurice-Stam H., Grootenhuis M. A. (2014). Anxiety and depression in mothers and fathers of a chronically ill child. Maternal and Child Health Journal, 18(8), 1993–2002. [DOI] [PubMed] [Google Scholar]
- Vingerhoets A. J. J. M. (2012). Normdata HADS. https://scholar.google.com/scholar_lookup?hl=en&publication_year=2012&author=Vingerhoets+A.J.J.M.&title=Normdata+HADS.
- Wallander J. L., Varni J. W. (1998). Effects of pediatric chronic physical disorders on child and family adjustment. Journal of Child Psychology and Psychiatry, 39(1), 29–46. [PubMed] [Google Scholar]
- Watson J. M., Torgerson D. J. (2006). Increasing recruitment to randomised trials: A review of randomised controlled trials. BMC Medical Research Methodology, 6(1), 34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wynne B., McHugh L., Gao W., Keegan D., Byrne K., Rowan C., Hartery K., Kirschbaum C., Doherty G., Cullen G., Dooley B., Mulcahy H. E. (2019). Acceptance and commitment therapy reduces psychological stress in patients with inflammatory bowel diseases. Gastroenterology, 156(4), 935–945.e931. [DOI] [PubMed] [Google Scholar]
- Zigmond A. S., Snaith R. P. (1983). The hospital anxiety and depression scale. Acta Psychiatrica Scandinavica, 67(6), 361–370. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.