Abstract
Objectives:
Short sleep duration and poor sleep quality are more prevalent among African Americans (AAs) and may be a modifiable risk factor for cardiometabolic disorders. However, research is limited about sleep-related attitudes, beliefs, and practices among AAs. Our objective was to evaluate these practices and beliefs surrounding sleep among urban-dwelling AAs.
Design:
Qualitative study comprised of five 90-minute focus groups using a semistructured interview guide.
Setting:
Five churches located on the west side of Chicago.
Participants:
Adults (N = 43) ages 25–75 years.
Measurements:
Transcripts were voice recorded, transcribed, and then coded for content analysis using NVivo 12 Pro to capture themes in the discussions.
Results:
Most participants (86%) reported sleeping less than the recommended 7 or more hours. The discrepancy between actual and desired sleep duration was nearly 3 hours per night. Participants reported that sleep is essential for mental and physical health. Napping and consuming caffeine were frequently reported techniques for coping with lack of sleep. Noise, physical discomfort, and stress were reported as barriers to sleep, and participants reported using TV and other electronics to cope with racing thoughts or worry. Many participants were diagnosed with or knew someone with obstructive sleep apnea, but few participants had been diagnosed with insomnia or were aware of nonpharmacologic insomnia treatments. Conclusion: A cycle of stress/disruptive environment, stress, rumination at night, and coping by use of electronics and daytime napping may perpetuate sleep disparities in this community. Results suggest that sleep-related interventions should include stress reduction and environmental improvements in addition to the typical sleep hygiene–related behavioral recommendations.
Keywords: Sleep beliefs, Sleep disparities, Sleep disorders, African American, Stress
Introduction
Relative to non-Hispanic whites, African Americans (AAs) have a higher prevalence of cardiometabolic diseases including cardiovascular disease, hypertension, type II diabetes, and obesity.1–3 Short sleep duration and sleep disorders such as obstructive sleep apnea (OSA) and insomnia are approximately twice as common among AAs4,5 and may be causally linked to black-white disparities in cardiometabolic disease.6–8 A multitude of factors have been linked to the sleep disparities observed in AAs, including socioeconomic factors, neighborhood dysfunction, increased medical comorbidities, obesity, and stress.9–13 Despite the large epidemiologic literature examining factors related to short sleep and poor sleep quality among AAs, only a few studies have examined the role of beliefs and attitudes about sleep in the AA community.
Although the sleep medicine literature focuses on the physiological determinants and consequences of disrupted sleep, sociological research has examined the social context and function of sleep in society (ie, why, where, with whom, to which purpose does sleep occur).14 Although previous studies have examined sleep beliefs and practices, no one has yet specifically examined sleep duration among AAs using qualitative methods.15,16 Existing studies conducted among AAs used surveys (thus lacking the depth of qualitative methods) to evaluate sleep duration or conducted focus groups to explore treatment of OSA. Grandner and colleagues17 conducted a survey to compare sleep-related beliefs and practices among older AA and white women and found that AA women were more likely to report needing more sleep (33% of AA vs 3% white women) and more likely to report snoring (39% of AA vs 72% of white women reported never snoring). There were also differences in sleep practices and behaviors. For example, AAs were more likely to report napping and nonsleep behaviors in bed (eg, watching TV). Similarly, a large survey of AAs living in New Haven, CT, reported that 72% of this sample demonstrated poor sleep quality, which was related to poorer sleep hygiene practices; greater dysfunctional attitudes about sleep, such as sleep-related worry; and lower neighborhood cohesion.18
Shaw and colleagues (2012) evaluated attitudes and beliefs regarding OSA in a sample of AA participants in a low-income community in Brooklyn, NY. Although participants commonly had misconceptions about OSA, such as the belief that it caused insomnia or coughing, participants frequently linked OSA to adverse health consequences including hypertension, decreased metabolism, and daytime sleepiness. In terms of treatment, many participants had heard of continuous positive airway pressure (CPAP); however, participants commonly reported barriers to treatment, such as fear of the overnight sleep study and concerns about the discomfort of CPAP. These studies provide valuable information regarding sleep attitudes and beliefs, but more research is needed, particularly regarding beliefs, attitudes, and norms about sleep duration and insomnia among AAs. This is a critical step in the development of interventions to address sleep disparities.
Therefore, the purpose of this study was to conduct an in-depth qualitative assessment among AAs living in the West Side of Chicago, IL, to explore perceived determinants and consequences of short sleep duration, poor sleep quality and sleep disorders among AAs. This community is adjacent to Rush University Medical center and has multiple economic and social factors (eg, crime, poverty) that are known to increase cardiovascular risk.1 The goal of our study was to use these semistructured discussions about sleep to better understand perceived factors that affect sleep among urban, low-income AA communities from their point of view with the goal of using this information about beliefs and practices to inform the design of tailored interventions to address sleep disparities. The discussions were also an initial step in partnering with the community to determine whether sleep is perceived as an important health issue and which aspects of sleep are most salient to the community.19 Focus groups were used in this study, rather than individual interviews, because we wanted to engage participants in shared discussions and interaction around sleep-related beliefs.20
Methods
Participants
This study was completed as part of a larger project called West Side Alive which is a partnership between researchers and 7 AA churches on the West Side of Chicago, IL, to conduct research to address health needs of the community. We conducted 5 focus groups of 8–10 participants per group (n = 43). Research staff who were church members and native to the community recruited focus group participants from the church and surrounding community. Staff were instructed to recruit participants who were willing to talk about health issues and not to specifically recruit based on the presence or absence of sleep problems. Eligibility criteria included the following: self-identify as AA, age ≥25 years, and member of the church or living near the churches where the focus groups were held. The age criterion was selected because of the biological changes in sleep between adolecence and adulthood (eg, circadian timing, sleep need).21 The institutional review board at Rush University Medical Center approved the study, and participants completed written informed consent.
Procedure
Focus groups were co-led by a clinical psychologist certified in behavioral sleep medicine (KGB) and a bachelor’s-level research assistant (SGG). Participants completed the consent form and a brief demographics form. The focus group used a semistructured interview guide consisting of questions designed to assess sleep practices, attitudes, and beliefs (Table 1). The groups were comprised of individuals who attended church together or lived near the church, and many participants knew each other. Although there is a possibility for the censure of unpopular views or for group think within focus groups, the moderators also had the opportunity to ask follow-up questions and query whether anyone had a differing opinion. All focus groups were audiotaped with Olympus recorders (Olympus Corporation, Center Valley, PA); transcribed verbatim; and imported into NVivo 12 Pro (QSR International, Burlington, MA), a qualitative data analysis software program, to derive themes. Focus groups lasted for approximately 60 minutes, and participants were paid $25. We scheduled 5 focus groups (1 group at a different church) based on interest/availability of the participating churches in the larger study in this community. We reached saturation on our major themes after 3 focus groups but still completed all 5 of the scheduled groups.
Table 1.
Semistructured interview guide questions for focus groups
| Amount of sleep | • How many hours of sleep do you get each night? • How much sleep do you need to be rested and at your best? |
| Routines | • What do you do to relax and get to sleep at night? • What routines do you have before bed? • Do you have a regular bedtime/wake time? |
| Sleep influences | • What are the things you think are good and bad for your sleep? • Is there anything that helps you to fall asleep? |
| Coping without sleep | • If you are unable to sleep, what do you do to cope with sleep loss? |
| Sleep disturbances | • Have you been diagnosed with a sleep disorder or know anyone who has a sleep disorder? • Do you ever fear or avoid falling asleep? |
| Sleep beliefs | • How are your family and friends' beliefs and practices around sleep the same different from your own? |
| Sleep & technology | • How does technology impact your sleep? |
A number of participants (36 of the 42) completed additional questionnaires in the month prior to the focus groups as part of a West Side Alive health screening, including additional demographics and the Patient-Reported Outcomes Measurement Information System (PROMIS) 8-item sleep disturbance measure. We have included these data in the manuscript to provide more information regarding the context surrounding the focus group answers (eg, employment, presence of sleep disturbance).
Data analysis
Sample statistics were calculated for the questionnaire data, including the brief demographic questionnaire collected at the focus groups and for the subset of participants who completed demographics and sleep quality measures in the larger study. For the questions about sleep duration needed vs obtained, responses were recorded for each participant, frequencies were counted, and values were interpreted to understand the individuals’ perception of discrepancy between desired and perceived sleep duration. Qualitative responses from the focus gropus were coded and analyzed using NVivo 12 Pro (QSR International, Burlington, MA). Data were analyzed using content analysis22 to document themes among the interview guide questions and discussion. Content analysis, as described by Janis (1965),23 is typically applied to written text and can be used to analyze the content of other communications, such as focus group transcripts.24 This method, which has been used in prior sleep-related focus groups,16 was chosen because it provides a systematic description of the responses in the groups.25 A systematic description of the groups’ discussions allowed us to analyze the content of the discussion; then, in turn, we provide an integrative perspective on links between content area in the discussion section of the paper.
Coding was conducted using a 2-phase process. First, main themes were developed after reading the transcripts (main nodes), and 2 authors (SGG, DL) coded the focus group transcripts according to the main themes; any disagreement was resolved by a third coder (JLW). Second, after discussion among the team regarding the the main nodes, the team further divided the nodes into subnodes. Finally, after reviewing the main and subnodes, the coding system was then refined by all authors. Two authors (SGG, DL) then coded all the transcripts and resolved any disagreements through a discussion which included a third author (JLW). Again, the coding system was reviewed and refined by all authors, and the 3 coding authors then re-reviewed coding across all transcripts. Coding was discussed until all authors reached agreement on the final coding. Using this iterative process, we derived 4 main themes to be as follows: (1) sleep duration and routines around sleep, (2) effects of sleep loss and coping with lack of sleep, (3) sleep influences, and (4) sleep disorders. Validity of this main coding scheme was reviewed by the entire study team.
Results
Participant characteristics
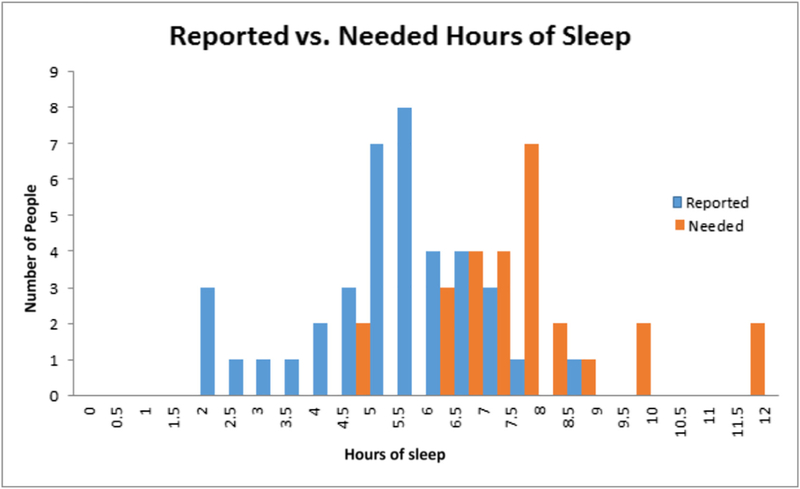
Participant characteristics are listed in Table 2. A total of 43 adults participated in the focus groups. More than half of the participants were female (n = 26, 60.46%). The age range was 26–73 years, and the average age was 52 (SD = 10.97) years. All participants were AA and resided in the neighborhood surrounding the churches where the focus groups were held. Average self-reported sleep duration was 5.2 hours, and sleep duration needed was 7.9 hours. Additional demographic and other questionnaire data were available for participants who also completed the larger study (n = 36). Demographics from these measures demonstrate that participants had a range in their educational attainment and employment status. Self-rated sleep scores indicated that most participants rated their sleep as fair, poor, or very poor (59%). PROMIS sleep disturbance scores were in the average range (M = 50.3, SD = 11, range 29–73); however, 25% demonstrated elevations (t score >55) on this measure.
Table 2.
Participant characteristics (N = 43).
| Variable | M (SD) or n (%) |
|---|---|
| Age | 52 (10.97) |
| Sex | |
| Female | 26 (60.5) |
| Male | 17 (39.5) |
| Race | |
| AA | 43 (100%) |
| Self-reported sleep | |
| Habitual duration, h | 5.2 (1.5) |
| Duration needed | 7.9 (1.7) |
| Educationa | |
| <High school | 3 (8) |
| High school or GED | 9 (25) |
| Some college or Associate’s Degree | 13 (36) |
| College degree (4 y) | 7 (19) |
| Vocational training | 4 (11) |
| Employmenta | |
| Full time | 13 (36) |
| Part time | 3 (8) |
| Disabled | 6 (17) |
| Student | 2 (6) |
| Retired | 4 (11) |
| Unemployed | 4 (11) |
| Self-employed | 3 (8.3) |
| Did not answer | 1 (3) |
| Sleep qualitya | |
| Excellent | 0 (0) |
| Very good | 4 (11) |
| Good | 10 (28) |
| Fair | 15 (42) |
| Poor | 2 (6) |
| Very poor | 4 (11) |
| PROMIS sleep disturbance t scorea | 50.3 (11.0) |
This question was available for 36 of the 43 participants who participated in the larger screening study.
Category 1: sleep duration and routines
Reported sleep duration vs reported sleep need.
Average reported sleep duration was 5.3 (SD = 1.4) hours (range 2–12 hours) (responses are graphed in Fig. 1). Most participants (86%) reported sleep duration less than 7 hours per night. The average discrepancy between reported sleep duration and reported sleep needed was 2.9 (SD = 1.9) hours. Although the average of hours of sleep needed is consistent with the public health recommendations, participants gave a wide range of answers to the question about sleep need. Most (67%) participants accurately identified that they needed 7–9 hours of sleep per night, but many reported they had difficulty achieving that many hours. For example,
I sleep from 10pm-6am. If it is solid then yeah I think I might be okay, but I never get that.Basically [I need] about 7–8 hours of sleep, and I myself say [I sleep] about 5–6 hours.I need probably 7 hours. [If I got] 8 hours I would be Superman.
Fig. 1.
Sleep duration reported vs sleep needed.
Some participants reported that they needed more than 8 hours per night to feel rested:
I need 8–12 hours.I get about 5 or 6 maybe, and I need about 10.
Other participants reported functioning well with fewer than the recommended 7–8 hours of sleep per night.
I get about 4–4 ½, but I’m good after that like … yeah I’m good … sleep is overrated.I’m at my best maybe after 5 hours. If I get 10 hours of sleep, I’ll still feel sluggish.
Participants also reported thoughts about how need for sleep varies, including that individuals need less sleep as they age and need more sleep after an active day. Others in the group tended to agree with those statements.
They say the older you get, the less you need.Depends on what you do that day.
In summary, most participants reported sleep duration less than the recommended 7–8 hours per night but lacked consensus on their beliefs regarding the amount of sleep they needed.
Sleep routines and factors that affect sleep routines.
Many participants reported a consistent bedtime that was anchored to watching the news or another television show in the hours before bed.
I go to sleep after the 10 o’clock news and automatically get up at 5:30–6 every morning.I iron my clothes, take a shower, talk to my daughter and granddaughter, fix my lunch for the next day, and watch TV at 10:30.
Participants frequently reported spending time winding down, usually watching TV before or while in bed before trying to sleep. Other activities included talking on the phone, reading, listening to sermons, and eating.
I guess I have a routine … around 9 or 9:45 I will actually get in the bed, I won’t fall asleep and I’ll turn on Criminal Minds.I’m in the bed about 7:00 or 8:00, but I’m asleep about 10:00.I eat, read, sleep in the bed.
In terms of interruptions to their sleep routines, several participants reported that caregiving for children, grandchildren, or elderly relatives affected their ability to keep a consistent sleep routine.
I don’t have a routine, because my schedule is all over the place. Usually, with family and children, there is always an issue somewhere that needs to be addressed before you go to bed.I don’t have a routine; I never not have something to do. I have two elderly parents that I take care of, and they live in different houses, so it’s like I always have something to do.
One panel of participants talked in-depth about how family members’ health emergencies frequently interrupted their sleep, but these were viewed as more important than getting a good night’s sleep.
If she gets sick and I got to take her to the doctor or something I don’t count that as a problem with sleep, it is just something that comes up, and then later I will sleep. You just do it, and I sleep when I sleep.
Many participants reported that work schedules affect their sleep. Most focus groups had 1–2 members who currently or previously worked evenings or night shifts. Several participants reported sleeping better on night shifts than day shifts. Overall, retired participants reported enjoying sleeping later or taking naps in the day.
I am expected to be in the office by a certain time. You know we have these structured lives where sleep has to go around everything else.I used to work second shift for a long time, and even though I am on first shift now, I still am a night owl. I have to make myself go to sleep. But when I used to work second shift, I got good sleep.
In summary, most participants reported having a sleep routine, but routines were affected by the inability to fall asleep (leading to several hours of nonsleep activities in bed) and by interruptions in their routines due to caregiving responsibilities.
Category 2: effects of sleep loss and coping with lack of sleep
Participants reported strong beliefs that lack of sleep impacted their psychological and physical health.
Psychological consequences.
Participants in all of the focus groups reported strong beliefs that insufficient sleep affected their mood, concentration, and alertness. Some of the comments are listed below:
Affects your attitude, makes you irritated, you have no patience, can’t stay focused, makes you too tired, emotions are changed, productivity is lower, makes you drowsy, you become forgetful, can’t think clearly, and feelings of crashing.
Physical consequences.
Participants in all focus groups reported beliefs that insufficient sleep impacts their physical health. Participants reported believing that sleep is important to avoid infection, hypertension, diabetes, and digestive dysfunction.
I have learned that when I don’t get all of my sleep it came on [a sinus infection] … and I try to get more sleep, so it doesn’t come on.Well, that [sleep] is when the body rejuvenates itself … the body needs rest. If you constantly deny your body that, you are going to get sick and break down.We can’t heal ourselves if we’re not sleeping well. I think when I used to sleep more some of my health issues were not as bad.[If you don’t sleep] … it seems like your blood pressure gets higher; your diabetes is out of control; your cholesterol gets out of control because you’re not resting.
Coping with sleep loss.
The most common techniques for coping with sleep loss were napping or dozing. Participants often reported taking naps at work, if permitted. For example,
When I’m at work, at lunchtime if I’m really tired I might try and get a snooze. Or if I’m at work and I’m not feeling good, I’ll get a snooze.I’m at the [bus] terminal, and I got 15 minutes so I’ll close my eyes for 10 minutes and I can drive [the bus] for the next 4 or 5 hours.
Additionally, consuming caffeine was also a commonly reported coping technique.
If I haven’t had enough sleep then that means, okay every time we take a break I got to get some coffee.[When I don’t sleep enough] I just know, hey, the next day, this is getting ready to be a coffee caffeine day, I will probably make two pots of coffee at work.
Other coping techniques included consuming sugar and going on a walk to promote alertness in the day. Participants in the focus groups agreed that these strategies were temporarily helpful to get through the rest of the day but were not a substitute for adequate sleep at night.
Category 3: factors that influence sleep
We discussed participants’ thoughts about factors that are helpful and harmful to getting sufficient sleep. In Table 3, we report the most common positive and negative influences on sleep and the number of times each theme was referenced in the focus groups.
Table 3.
Positive and negative sleep influences reported in 3 or more focus groups
| Sleep influences reported |
||
|---|---|---|
| No. of groups (out of 5) | No. of references in group | |
| Positive influences | ||
| TV | 5 | 31 |
| Showering/bathing before bed | 4 | 4 |
| Physical activity during the day | 4 | 6 |
| Noise in the room (eg, TV or fan) | 3 | 3 |
| Comfortable temperature | 3 | 3 |
| Listening to music | 3 | 7 |
| Reading before bed | 3 | 2 |
| Praying | 3 | 3 |
| Playing games or reading on a smartphone | 3 | 18 |
| Sleep medication | 3 | 3 |
| Dark bedroom | 3 | 6 |
| Negative influences | ||
| Stress | 5 | 47 |
| Household disruptions | 5 | 21 |
| Noise outside the household | 5 | 15 |
| Physical discomfort | 5 | 5 |
| TV | 4 | 40 |
| Light | 4 | 14 |
| Pain | 4 | 8 |
| Food | 3 | 3 |
| Caffeine | 3 | 3 |
| Awakenings to use the bathroom | 3 | 5 |
Note. Other influences included the following: positive—quiet, comfortable bed/pillow, journaling, essential oils, alcohol, and herbal supplements; negative—unfamiliar environments, uncomfortable beds, pets, and working or cleaning too late in the evening.
Positive influences on sleep.
Watching TV was the most common positive sleep influence, reported by participants in all 5 groups and mentioned most frequently.
TV.
Participants in every group reported that watching TV was helpful because it helped distract them from their thoughts or worries.
When your mind is racing, and you have the TV on you are thinking about the program but then once it goes to commercial you can kinda just doze off because your last thought is of the TV program, not the worry of how am I going to pay this or my child is this or whatever the case may be that is going on in your life.I think it just helps me focus on something else than what I might have been thinking of. If I was thinking about something along the health lines or family, it helps me to get rid of that and clear my mind.
Other participants reported the background noise and/or light from the TV helped them feel safer at night.
I can’t sleep in no pitch dark. I like to see a little something.I always had nightmares. I grew up in Cabrini Green [public housing], and there was something happening there all of the time. So I always slept with a light on or had some type of light or my TV on.
Other positive influences.
Other sleep-promoting activities included taking a hot shower or bathing before bed, engaging in physical activity during the day, listening to music, reading, medication, and praying. Three groups brought up how religion (ie, prayer, the Bible, listening to sermons) influences their sleep positively. Many of these activities were consistent with a positive wind-down routine. Participants also brought up having a dark bedroom as an environment that is good for sleep.
Negative influences on sleep.
Participants in all groups agreed upon a number of factors that led to difficulty falling asleep or getting sufficient sleep: stress, other people, noise, and sleep disorders. Other factors were mentioned by a subset of groups (Table 2).
Stress.
Stress was the most commonly mentioned barrier to sleep. Stress was discussed in every group and mentioned by numerous participants per group. Stressors included worry about children, finances, and relationships. Participants frequently discussed feeling wound up, worrying, or overthinking at bedtime. For example,
You are constantly going over that day. And then thinking about what you gotta do the next day. And they all just chime in together, and you just feel like you are crazy.I can never just shut it down. It’s the worry more so than stress. It’s the worry of what might happen or what’s going to happen, what am I going to do if so and so happens.
Household disruptions.
Participants in all of the groups also discussed disruptions due to other people in their home. Several participants reported that children in the house, sharing a bed with children or grandchildren who disrupted their sleep, and/or snoring partners.
I have a 4-year old who’s stubborn and doesn’t like to go to the bathroom, so I have to wake up to make sure that she wakes up to go to the bathroom. Otherwise, I have a mess in the morning. And that’s typically twice a night.I have a 2-year-old who’s a night owl like me so we’re up. She’s watching (TV show) I’ll be watching a movie.… my husband, his snoring is like a lawnmower killing a cat that has asthma and got shot before the lawnmower ran over it. It’s the worst thing ever.…
Noise outside the household.
Noise from neighbors playing music, watching TV, or even arguing was also a common sleep disruption.
… People upstairs they move all night they just, it’s just noisy … like moving furniture.When your neighbors [are] getting into it … like at 4:00 in the morning. I said 911 because … I got to get some sleep to be up in a couple of hours.
Physical discomfort.
Pain, sleep disorders, and frequent urination were also discussed by most of the groups. One or 2 participants in each focus group discussed pain from arthritis, back pain, migraines, and fibromyalgia. Participants also tied pain into other stressors and sleep-related behaviors such as caffeine intake.
I live with pain on a day-to-day basis.… I want to say probably 85% of the time that keeps me up that I’m in pain.… Sometimes to lay down hurts more than to sit up.Pain keeps me up, even with the pain meds I take at night that are supposed to keep the pain away; I lay down, and it is just like it don’t work. So yeah pain, that and stress is what keeps me up at night.I have chronic pain, and so I’m in pain a lot of nights. So if I take the medication for the pain which is going to cause me to go to sleep, I’m still not going to go to sleep because my intake of caffeine is canceling out.
TV.
TV was mentioned as a negative influence for some participants due to noise or the content disrupting their sleep.
Every time you turn on the news somebody being shot. That’s depressing to watch the news, and that’s all you see every day. So I don’t hardly watch the news.If I’m watching a program that I am waiting to watch, then I’ll watch the program, and I’ll continue to stay up.
Other negative influences.
Other negative influence included factors known to disrupt sleep, such as light and caffeine. Participants also reported other factors that are not known to disturb sleep such as consuming sugar or junk food and eating pork.
In summary, participants reported multiple negative influences on their sleep including stress, pain and sleep disorders, disruptions both within and outside the household, and behavioral factors such as caffeine and diet.
Category 4: sleep disorders
Sleep disorder diagnoses (self and other) are reported in Table 4. In total, 8 participants (19%) reported having been diagnosed with a sleep disorder. OSA was the most commonly reported sleep disorder among the participants (n = 5, 12%). Despite the prevalence of difficulty falling asleep, only 3 participants (7%) reported being diagnosed with insomnia. Six participants reported having a family member with OSA, and only 2 knew of a friend or family member with insomnia. Many participants accurately described OSA as a disorder of breathing. Some examples include:
I have sleep apnea so my breathing, you know, it stops sometimes during my sleep.… you take a deep breath and then you stop—be still and then about like 5–6 minutes in you start breathing again, is that sleep apnea?
Table 4.
The frequency of self or friend/family member diagnosed with a sleep disorder
| Sleep disorder | Self n | Friend or family n |
|---|---|---|
| OSA | 5 | 6 |
| Insomnia | 3 | 2 |
| Narcolepsy | 0 | 1 |
In discussing OSA, several participants reported they or their family member had difficulty with CPAP.
The mask wasn’t good for my husband. He couldn’t stand nothing on his face, we went through several different masks, and he finally found one that he would keep on some, but he still wouldn’t keep it on all the time. But my godmother, the second one they showed her she is doing pretty good.It does help you sleep but something ain’t right about that machine. I didn’t use mine, so they came and took it ‘cause you know you only get 30 days and if you don’t use it in those 30 days for so many times. But if not they come and take it. Cause it’s by Medicare and Medicaid.
A few participants reported they or their family members had positive experiences with CPAP.
With the full face one, I sleep so well.My sister has sleep apnea. She actually had Bipap first, so a higher version. But she’s on CPAP now, and she has improved. But she says her sleeping it’s so much better.
Insomnia as a diagnosis rarely came up in the discussions even though many participants reported difficulty falling asleep or staying asleep. Multiple participants reported taking medications for sleep, but few participants labeled their sleep problems as insomnia when discussing sleep medications. An example of using medications for sleep is below:
I have trouble sleeping, so I’m on medications that [are] supposed to put me to sleep. If I take those at 8, I probably go to sleep at 2, by 8 o’clock somebody is calling my name, calling my phone, starting the cycle. So then I’m up, and then I’m up all the way to 2 again. If I don’t take the medicine or I take it too late, I don’t go to sleep till about 5, 5:30.One of my close friends, she doesn’t sleep. I know it’s probably impacting her but it doesn’t seem like it is. She said she can only get like 2 or 3 hours of sleep and she’s good. She’s taking medication to sleep.
One belief expressed was that insomnia meant being awake all night.
I was diagnosed with insomnia because I wasn’t going to sleep at all, I was just staying up, like all night.I feel like I got insomnia because like I never liked sleeping … but sometimes it is aggravating because you want to go to sleep or because you’re bored and you have nothing to do. Sometimes I stay up at night, but I can’t go to sleep, then I finally fall asleep and wake up in an hour or 2. But I don’t throw away my day. It’s just like ‘alright, time to get to work.
Behavioral strategies for insomnia were rarely discussed in the groups. Only 1 participant had attended a lecture about sleep.
They don’t suggest that you have TVs in your room because the bedroom is made for you to sleep. And I was really touched by that lecture because he explained why when you go to the bedroom you should go in there to sleep. And he was adamant about that … [when you watch TV] if it’s upsetting it can cause problems with your sleeping and so I said no I can’t have that in my life.
In summary, participants were generally familiar with OSA, and many participants were either diagnosed or knew someone who had OSA. In contrast, insomnia diagnosis was rarely brought up, and participants were mostly unfamiliar with nonpharmacologic treatment recommendations for insomnia.
Discussion
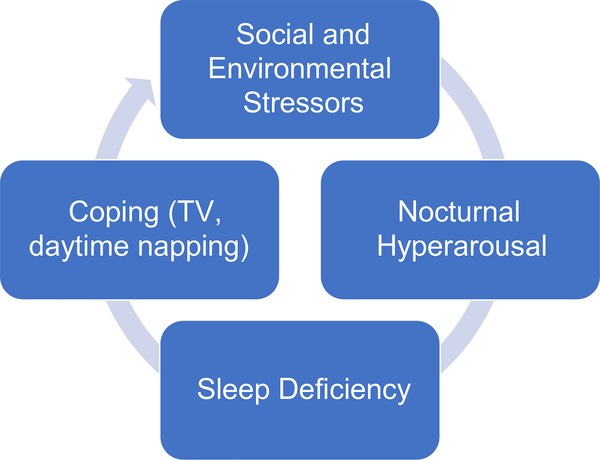
The purpose of our focus group discussions was to gain insight into understanding sleep disparities among AAs by discussing their beliefs and experiences pertaining to sleep and sleep disorders. Consistent with the methods of community-based participatory research, these focus group discussions were also the first step in engaging with this community to determine their priorities and interest in interventions to promote sleep health. Results demonstrated that, in contrast to previous research,17,26 most participants had a good understanding of the recommended sleep duration, and many were able to accurately describe sleep apnea. Also contrary to other studies (particularly conducted among men), participants reported that sleep was integral to health and performance rather than a only a necessity or burden.15 Participants reported a variety of sleep-related practices, some that are consistent with recommendations (eg, physical activity, relaxing activities before bed) and others that are discouraged practices (ie, TV in the bedroom). Figure 2 presents a conceptual model for how sleep problems and sleep practices create a vicious cycle, as described by members in all of the focus groups. Participants reported having a desire to sleep and an awareness that sleep deficiencies contribute to poor health and performance. However, they also reported having sleep disruptions due to internal (eg, stress, rumination) and external factors (eg, noise, caregiving, work schedules). Then, they reported using coping strategies for sleep loss and inability to sleep at night (eg, napping, watching TV in bed) that may themselves further disrupt sleep. TV, although typically viewed by sleep professials as a poor sleep habit, was generally regarded by many participants as a positive influence on sleep, by providing either a sense of security or a distraction from worry. Given that many of the coping strategies reported by the groups are known to disrupt sleep (caffeine, TV), this may create a cycle where the coping strategies are helpful in the short term but may then be contributing to the long-term problems of short and disrupted sleep.
Fig. 2.
Conceptual model.
There was some disagreement among participants about the use of TV to promote sleep. Some participants reported that they were unable to sleep without it, whereas other participants reported that TV interfered with sleep. There is a growing body of research that demonstrates that TV/technology use is common in the general population and disrupts sleep. A recent survey reported that 9 of 10 adults use technology in the hour before bed.27 Another survey reported that 31% of adults use a smartphone and 21% use the Internet as a sleep aid,28 both of which were associated with poorer sleep quality. Even early sociological investigations of children’s beliefs about sleep demonstrated beliefs that electronics such as TV and music facilitated sleep.29 Several participants reported to us that their bedtimes were delayed by “binge viewing” streaming media at night while attempting to wind down. Binge viewing media may contribute to poor sleep quality and daytime fatigue due to increased nocturnal cognitive hyperarousal (ie, thoughts are more active).30 Results from the focus groups suggest that, in an attempt to reduce hyperarousal, individuals may be potentially exacerbating the problem. Given that TV is perceived to provide a distraction and/or sense of security, clinicians should be aware that a firm recommendation of “TV is bad for sleep” may undermine the credibility of treatment and foster mistrust between patient and provider. Furthermore, if a treatment goal is reducing TV viewing at night, our results demonstrate that participants would need to be provided with alternative wind-down techniques to be successful.
Our focus groups also discussed diagnosis and treatment for sleep disorders, including OSA and insomnia. Despite having nearly twice the prevalence of OSA,31 diagnosis rates for OSA and CPAP compliance are lower among AAs.32,33 In contrast to prior research suggesting that AAs often have misconceptions about OSA,26 participants in our groups tended to identify that OSA was a breathing disorder, and some were able to identify family members who benefitted from CPAP. However, only 11% of participants reported an OSA diagnosis, which is probably lower than the actual prevalence in this group of middle-aged and older adults. Insomnia was also rarely reported, and only 1 participant had heard of nonpharmacologic recommendations for insomnia. Williams and colleagues34,35 have developed tailored interventions to increase the diagnosis and treatment of OSA among AAs, but to our knowledge, no studies have tailored insomnia interventions to AAs. Our results suggest that continued efforts to increase both OSA and insomnia interventions are needed in this population.
One finding of our study is that participants did not talk extensively about sleep beliefs (eg, why sleep with the TV and lights on). It took a lot of probing from the moderators for participants to talk about why they used these methods to facilitate sleep. In many cases, the responses to those interview questions were brief, 1-sentence responses or a few words. One possible reason is that the participants do not have fully articulated beliefs about sleep—that it is something they don’t discuss or think about frequently. In contrast, topics such as watching TV or leaving the lights on or off generated much more lively discussion and interaction. Another possible limitation is that the sample may also be biased toward participants with favorable attitudes toward the partnership with Rush University Medical center and therefore had greater exposure and access to health care. Strengths of this study were that we conducted in-depth conversations in settings that were comfortable to participants and included individuals with various educational and occupational backgrounds. Participants felt that it was helpful to discuss ways they could improve their sleep and get ideas from their peers. As one participant stated:
I’m grateful that you guys are coming into the community to get us to think about what is distracting us with our sleep and what helps people. Cause together when we talk we can gather good ideas to help each other. And then you can be more sensitive to what people are going through, and there are reasons why they can’t sleep.… Because sleep is very important, it affects your health.
In summary, the results of our focus group discussions demonstrate that community members view sleep as an important and understudied health issue and that use of TV and napping are perceived as methods for coping with lack of sleep and poor sleep quality. Results from this study suggest that addressing maladaptive sleep behaviors (eg, limiting caffeine, removing TV from the bedroom) is needed but may not be sufficient for improving sleep because these practices are viewed as helpful. It is imperative to also address the underlying cognitive and environmental contributors (such as?) to short sleep duration and poor sleep quality in this population.
Acknowledgments
This project was funded, in part, by grant R156HL135247. We thank the participants of our partner churches for being willing to engage in a discussion and share their thoughts with us about their sleep. Thanks to our community research staff: Catherine Banks, Gigi Fuller, Tamara Gear, Jessica Hudnall, Precious James, Kandice Jones, Patty Ringo, and Rochelle Sykes who helped recruit and organize these focus groups for us. We also thank Elizabeth Avery, MS, for assistance with data management.
References
- 1..Kochanek KA, Anderson RN. How did cause of death contriubte to racial differences in life expectency in the United States in 2010? NCHS Data Brief. 2013; 125:1–8. [PubMed] [Google Scholar]
- 2..Yang Q, Cogswell ME, Flanders WD, et al. Trends in cardiovascular health metrics and associations with all-cause and CVD mortality among US adults. JAMA. 2012; 307(12):1273–1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3..Writing Group M. Mozaffarian D, Benjamin EJ, et al. Heart disease and stroke statistics—2016 update: a report from the American Heart Association. Circulation. 2016;133(4):e38–360. [DOI] [PubMed] [Google Scholar]
- 4..Petrov ME, Lichstein KL. Differences in sleep between black and white adults: an update and future directions. Sleep Med. 2016;18:74–81. [DOI] [PubMed] [Google Scholar]
- 5..Ruiter ME, Decoster J, Jacobs L, Lichstein KL. Normal sleep in African-Americans and Caucasian-Americans: a meta-analysis. Sleep Med. 2011;12(3):209–214. [DOI] [PubMed] [Google Scholar]
- 6..Grandner MA, Petrov ME, Rattanaumpawan P, Jackson N, Platt A, Patel NP. Sleep symptoms, race/ethnicity, and socioeconomic position. J Clin Sleep Med. 2013;9 (9):897–905; 905A-905D. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7..Grandner MA, Seixas A, Shetty S, Shenoy S. Sleep duration and diabetes risk: population trends and potential mechanisms. Curr Diab Rep. 2016;16(11):106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8..Jean-Louis G, Youngstedt S, Grandner M, et al. Unequal burden of sleep-related obesity among black and white Americans. Sleep Health. 2015;1(3):169–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9..Jackson CL. Determinants of racial/ethnic disparities in disordered sleep and obesity.?. 2017;3(5):401–415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10..Johnson DA, Lisabeth L, Lewis TT, et al. The contribution of psychosocial stressors to sleep among African Americans in the Jackson Heart Study. Sleep. 2016;39(7): 1411–1419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11..Johnson DA, Lisabeth L, Hickson D, et al. The social patterning of sleep in African Americans: associations of socioeconomic position and neighborhood characteristics with sleep in the Jackson Heart Study. Sleep. 2016;39(9):1749–1759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12..Whinnery J, Jackson N, Rattanaumpawan P, Grandner MA. Short and long sleep duration associated with race/ethnicity, sociodemographics, and socioeconomic position. Sleep. 2014;37(3):601–611. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13..Desantis AS, Diez Roux AV, Moore K, Baron KG, Mujahid MS, Nieto FJ. Associations of neighborhood characteristics with sleep timing and quality: the Multi-Ethnic Study of Atherosclerosis. Sleep. 2013;36(10):1543–1551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14..Taylor B. Unconsciousness and society: the sociology of sleep. International Journal of Politics, Culture and Society. 1993;6(3):463–471. [Google Scholar]
- 15..Meadows R, Arber S, Venn S, Hilslop J. Engaging with sleep: male definitions. understandings and attitudes Sociology of Health and Illness. 2008;30(5):696–710. [DOI] [PubMed] [Google Scholar]
- 16..Golem D, Eck KM, Delaney CL, et al. “My stuffed animals help me”: the importance, barriers, and strategies for adequate sleep behaviors of school-age children and parents. Sleep Health. 2019;5(2):152–160. [DOI] [PubMed] [Google Scholar]
- 17..Grandner MA, Patel NP, Jean-Louis G, et al. Sleep-related behaviors and beliefs associated with race/ethnicity in women. J Natl Med Assoc. 2013;105(1):4–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18..Nam S, Whittemore R, Jung S, Latkin C, Kershaw T, Redeker NS. Physical neighborhood and social environment, beliefs about sleep, sleep hygiene behaviors, and sleep quality among African Americans. Sleep Health. 2018;4(3):258–264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19..Wallerstein N, Duran B, Minkler M, Foley K. Developing and maintaining partnerships with communities In: Israel B, Eng E, Schulz A, Parker E, editors. Methods in Community Based Participatory Research. San Francisco: Jossey-Bass; 2005. p. 31–51. [Google Scholar]
- 20..Kitzinger J The methodology of focus groups; the importance of interaction between research participants. Sociology of Health and Illness. 1994;16(1):103–121. [Google Scholar]
- 21..Bliwise DL, Scullin M. Normal aging In: Kryger MH, Roth T, Dement WC, editors. Principles and Practice of Sleep Medicine. Philadelphia, PA: Elsevier; 2017. p. 25–38. [Google Scholar]
- 22..Krippendorff K Content Analysis: An Introduction to its Methodology. Thousand Oaks, CA: Sage Publications; 2004. [Google Scholar]
- 23..Janis I The problem of validating content analysis In: Lasswell HD, Leites N, editors. Lanugage of Politics. Cambridge, MA: MIT; 1965. [Google Scholar]
- 24..Gavora P The state-of-the arte of content analysis. Educational Science 2015:6–18. [Google Scholar]
- 25..Berelson B Content Analysis in Communications Research. New York: Hafner Publishing Company; 1971. [Google Scholar]
- 26..Shaw R, McKenzie S, Taylor T, et al. Beliefs and attitudes toward obstructive sleep apnea evaluation and treatment among blacks. J Natl Med Assoc. 2012;104(11–12):510–519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27..Gradisar M, Wolfson AR, Harvey AG, Hale L, Rosenberg R, Czeisler CA. The sleep and technology use of Americans: findings from the National Sleep Foundation’s 2011 Sleep in America poll. J Clin Sleep Med. 2013;9(12):1291–1299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28..Exelmans L, Van den Bulck J. The use of media as a sleep aid in adults. Behav Sleep Med. 2016;14(2):121–133. [DOI] [PubMed] [Google Scholar]
- 29..Williams S, Lowe P, Griffiths F. Embodying and embedding children’s sleep: some sociological comments and observations. Sociological Research Online. 2007;12 (5):6. [Google Scholar]
- 30..Exelmans L, Van den Bulck J. Binge viewing, sleep, and the role of pre-sleep arousal. J Clin Sleep Med. 2017;13(8):1001–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31..Redline S, Tishler PV, Hans MG, Tosteson TD, Strohl KP, Spry K. Racial differences in sleep-disordered breathing in African-Americans and Caucasians. Am J Respir Crit Care Med. 1997;155(1):186–192. [DOI] [PubMed] [Google Scholar]
- 32..Billings ME, Auckley D, Benca R, et al. Race and residential socioeconomics as predictors of CPAP adherence. Sleep. 2011;34(12):1653–1658. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33..Joo MJ, Herdegen JJ. Sleep apnea in an urban public hospital: assessment of severity and treatment adherence. J Clin Sleep Med. 2007;3(3):285–288. [PMC free article] [PubMed] [Google Scholar]
- 34..Williams NJ, Grandne MA, Snipes A, et al. Racial/ethnic disparities in sleep health and health care: importance of the sociocultural context. Sleep Health. 2015;1(1):28–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35..Williams NJ, Jean-Louis G, Ravenell J, et al. A community-oriented framework to increase screening and treatment of obstructive sleep apnea among blacks. Sleep Med. 2016;18:82–87. [DOI] [PMC free article] [PubMed] [Google Scholar]