Abstract
Objective
The aim of this study was to provide a comprehensive evidence on risk factors for transmission, disease severity and COVID-19 related deaths in Africa.
Design
A systematic review has been conducted to synthesise existing evidence on risk factors affecting COVID-19 outcomes across Africa.
Data sources
Data were systematically searched from MEDLINE, Scopus, MedRxiv and BioRxiv.
Eligibility criteria
Studies for review were included if they were published in English and reported at least one risk factor and/or one health outcome. We included all relevant literature published up until 11 August 2020.
Data extraction and synthesis
We performed a systematic narrative synthesis to describe the available studies for each outcome. Data were extracted using a standardised Joanna Briggs Institute data extraction form.
Results
Fifteen articles met the inclusion criteria of which four were exclusively on Africa and the remaining 11 papers had a global focus with some data from Africa. Higher rates of infection in Africa are associated with high population density, urbanisation, transport connectivity, high volume of tourism and international trade, and high level of economic and political openness. Limited or poor access to healthcare are also associated with higher COVID-19 infection rates. Older people and individuals with chronic conditions such as HIV, tuberculosis and anaemia experience severe forms COVID-19 leading to hospitalisation and death. Similarly, high burden of chronic obstructive pulmonary disease, high prevalence of tobacco consumption and low levels of expenditure on health and low levels of global health security score contribute to COVID-19 related deaths.
Conclusions
Demographic, institutional, ecological, health system and politico-economic factors influenced the spectrum of COVID-19 infection, severity and death. We recommend multidisciplinary and integrated approaches to mitigate the identified factors and strengthen effective prevention strategies.
Keywords: public health, epidemiology, respiratory medicine (see thoracic medicine)
Strengths and limitations of this study.
Effective public health interventions against the COVID-19 pandemic require strong evidence on the risk factors associated with the disease.
The present study is the first African-focused comprehensive systematic review of its kind on a wide range of risk factors associated with the entire spectrum of COVID-19 in the Africa region.
Titles and abstracts of all publications identified by the search criteria were screened by two independent reviewers of the team.
Full-text articles were appraised using the Joanna Briggs Institute critical appraisal tools.
The available data did not allow us to carry out meta-analysis nor firmly establish causal relationships in the present study.
Introduction
The COVID-19 is a recently emerged viral disease caused by a novel single-stranded enveloped RNA (RNA) virus, known as SARS-CoV-2.1 Since the first COVID-19 case was identified in Wuhan province in China, in late December 2019, the virus has rapidly spread across the world and declared a global pandemic on 11 March 2020.2 As of 10 January 2021, the number of confirmed COVID-19 cases in the world has reached over 89.44 million with nearly 1.92 million deaths.3 Despite the late start of the pandemic, infection rate in Africa has been increasing exponentially with a total of 2.95 million confirmed cases and more than 70 thousand deaths as of 10 January 2021.4 The majority of reported cases in Africa were from South Africa and Egypt, while countries in Central Africa had recorded the least.
Given that the pandemic is caused by a novel strain of coronavirus with unknown original host,5 in the early stage of the outbreak, the risk factors associated with its transmission routes, severity and fatality risks were unclear. Several studies have been conducted to better understand the prognosis of the disease, though the level of uncertainty on viral shedding, transmissibility and disease severity remains high.6 Evidence indicates that the susceptibility to infection, being seriously ill and the risk of death are influenced by individual-level characteristics such as sociodemographic factors,7 behavioural traits8 and pre-existing medical conditions.9
While the number of people affected by the virus in Africa remains to be the lowest by global standards, which in part may be linked to the youthful age structure of the population and partly to the limited capacity for large scale testing,10 it is anticipated that the pandemic may have a profound impact in the region. First and foremost, Africa’s health system is fragile. In addition, preventive strategies such as social distancing and hand washing, which have proved effective in reducing transmission in the rest of the world, are less likely to be practical in the region due to prevailing sociocultural and economic circumstances.11 Compared with other regions, Africa is home to a large number of people living in substandard housing, which are mostly dense, inadequately ventilated and have limited access to direct water supply. The way of life in the region is largely communal. People tend to attend weddings, religious and funeral services in large numbers. Such societal and environmental factors along with the lack of awareness and access to preventive measures and the potential for low level of adherence (even when the resources are available) mean that the region will have the highest number of vulnerable populations for COVID-19 infection.12
Many countries have undertaken strict measures such as banning of public gatherings, complete lockdown of social and economic activities and closure of borders to prevent importation of cases.13 The number of new cases, however, continues to rise11 creating considerable pressure on the healthcare system.14 In the absence of effective vaccine or therapy, the ability to effectively control the spread of the pandemic hence depends on effective monitoring of new cases and on better understanding of the factors related to modes of transmission and severity of the disease. A comprehensive systematic review of African-focused COVID-19 related studies is required to strengthen public health measures and response plan against the pandemic in the continent. This review aims to provide a comprehensive evidence on risk factors for transmission, disease severity and COVID-19 related deaths in Africa.
Methods
Australia-based Ethiopian Researchers Network
At the beginning of April, 2020, a time when the COVID-19 pandemic was spreading across the globe, a group of more than 50 Australian-based Ethiopian researchers, who are active academic faculties in Australian institutions along with Ethiopian PhD students, established a working group on ‘Ethiopia and the COVID-19 pandemic’ to examine various dimensions and consequences of COVID-19 in Ethiopia. Specifically, the working group focused on four distinct thematic areas: (1) on understanding the epidemiology of COVID-19 in Ethiopia and around the globe and synthesising the lessons for the country, (2) assessing opportunities for reimagining the health system for COVID-19 pandemic response, (3) identifying potential pharmaceutical and non-pharmaceutical interventions and (4) measuring socioeconomic impact of COVID-19 in Ethiopia to support the Ethiopian government’s effort to mitigate the deadly impact of the pandemic on the population. As part of the project under the first thematic area, we conducted a systematic review to synthesise the available evidence on COVID-19 in Africa on factors affecting infection rates, severity and related deaths.
Search strategy
This systematic review is reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines.15 Potentially eligible articles were systematically searched and retrieved from Medline, PubMed and Scopus up to 11 August 2020. The following search terms, tailored to each database were used: “COVID-19” OR “coronavirus disease” OR “SARS-COV-2” OR “2019 novel coronavirus” OR “2019-nCoV” AND “Africa”. The full search strategy is summarised in online supplemental appendix 1. We used Medical Subject Headings terms to identify synonyms and text words in the appropriate syntax of each database. The search was not limited by date of publication or study design. Reference lists of included studies were manually searched for additional relevant articles. Moreover, preprint articles from the MedRxiv and BioRxiv databases were also accessed to ensure wider coverage. However, search was restricted to studies conducted in Africa and the English language only.
bmjopen-2020-044618supp001.pdf (2.3MB, pdf)
Study selection criteria
The titles and abstracts of all publications identified by the search criteria were screened by two independent reviewers of the team (AAA and BAD) to retrieve full texts for all relevant studies. Full-text articles were appraised using the Joanna Briggs Institute (JBI)16 critical appraisal tools17 (online supplemental appendix 2). All studies published in English and reported at least one risk factor and/or one health outcome were included in the review. We excluded letters to editors, correspondence, editorials and case studies. However, we included global studies that reported findings from any country in Africa.
Sociodemographic, lifestyle and behavioural, climate variables and chronic comorbid conditions, which can be at a community or national level, were considered as risk factors. Whereas COVID-19 infection rates, level of severity and COVID-19 related deaths were considered as outcomes. We adopted the definition of terms as reported in each of the included studies. Severity was referred for cases that required hospitalisation and are at high risk of death.
Data extraction
Seven members of the research team (HG, DNK, DMF, MW, ATG, BAD and AAA) extracted needed data using a standardised JBI data extraction form17 (online supplemental appendix 3). The extracted data included study authors, setting, population characteristics, study design, outcome and main findings on one or more risk factors and reported measure of association between risk factors and outcomes.
Quality and risk of bias assessment in individual studies
The JBI tools17 were used to assess the methodological quality and risk of bias (in design, conduct and analysis) of included studies (online supplemental appendix 2). The tool is used to assess the inclusion criteria, measurement of exposure and outcome variables, confounding adjustment and appropriateness of statistical analysis. All authors who participated in the data extraction also assessed the quality of studies that they extracted.
Data synthesis
A systematic narrative synthesis was conducted to describe the available studies separately for each outcome. Four steps were applied in synthesising the data: (1) reading findings and results of each study systematically and comprehensively and assessing for relevance; (2) developing a preliminary synthesis through describing each included study, grouping findings by infection, severity and death and tabulate results to identify patterns; (3) organise factors linked to the outcomes described in step 2 and thematise items around themes; and (4) explore the relationships of each factor within and among themes. Meta-analysis was not conducted because of the small number of studies identified for selected risk factors.
Patient and public involvement
Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Results
Description of studies
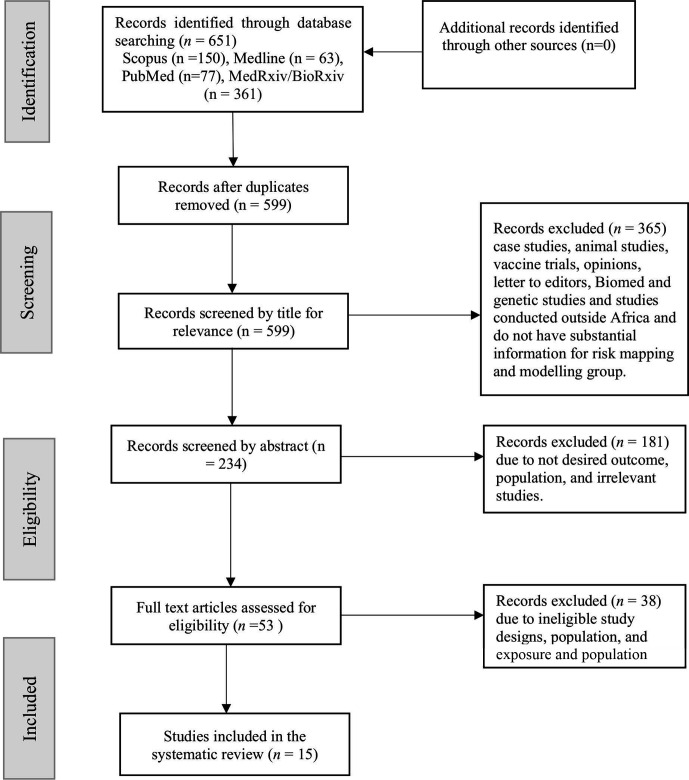
The combined search terms identified 651 records (figure 1). After removing duplicates (n=52) and unrelated studies (n=584), 53 records were eligible for full-text screening. Finally, 15 studies7–9 18–29 met the inclusion criteria and were included in this systematic review. Table 1 presents the main characteristics and outcomes of these studies. Four studies were exclusively on Africa.9 18 21 22 Two studies7 29 assessed susceptibility to COVID-19 infection, nine studies7 9 18 20 22–25 28 evaluated COVID-19 infection, three studies7 19 21 examined severity of COVID-19 infection and four studies8 24 26 27 assessed COVID-19 related death. Four studies assessed more than one outcome.7 21 24 27 As described in table 1, most studies (13) were conducted among the general population. Study designs such as modelling (n=7), cross-sectional (n=2), genetics (n=1), survey (n=4) and spatio-temporal analysis (n=1) were used in the included studies. The number of participants of those included studies for review ranges from 446 to 1.7 billion participants—the studies with the largest sample size were modelling related studies. We have annexed the quality score of all included studies in online supplemental appendix 4.
Figure 1.
PRISMA flow diagram. Figure 1 describes the flow diagram of the search strategy. PRISMA, Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
Table 1.
Characteristics of studies (n=15 studies) included in the systematic review
| Author | Setting | Population | Design | Sample (n) | COVID-19 Outcome |
Exposure | Summary of study findings |
| Bergman and Fishman18 | Africa | Adults | Modelling | 446 | Infection | Mobility | There was no statistically significant association between transmission rates and lagged mobility. However, there is limited information about Google workplace mobility data and COVID-19 infection as Apple mobility data are limited in Africa unlike other regions. |
| Clark et al19 | Africa/global | General | Modelling | 1.7 billion | Severity | Age, sex, comorbidity and continent | Individuals who are diagnosed with at least one underlying condition are at risk of severe COVID-19 disease. Although not different by sex, a total of 1.17 billion (22%) of the global population were estimated to be at risk of sever COVID-19 disease, and the prevalence of one or more comoribid condition was approximately 10% by age 25 years, 33% by 50 years and 66% by 70 years. A total of 400 million (6%) of the global population were estimated to be at risk of sever COVID-19 disease and is higher in older people. The most prevalent conditions in those aged 50+ years were CKD, CVD, CRD and diabetes— the prevalence of multimorbidity (2+ underlying chronic illness) was three times higher in Europe than in Africa (10% vs 3%). |
| Daon et al20 | Africa/global | General | Modelling | 1364 major airports (connections) | Infection | City connectivity | An outbreak of COVID-19 in Africa is most likely to originate from a passenger who travelled from Europe, and the average risk of COVID-19 infection originated from airport in Africa is 0.06, lower result compared with airports in Asia with an estimated risk of 0.51. The airport with the highest risk to initiate an outbreak in Africa is in Johannesburg with a risk estimate of 0.1. |
| Davies et al7 | Africa/global | General | Modelling | – | Infection Severity |
Age | People younger than 20 years old are roughly half susceptible as those who are older than 20 years old. In addition, 75% of infections are subclinical in children ageing between 10 and19 years as compared with 24% in people aged 70 years and above. |
| Diop et al21 | Africa | General | Modelling | – | Infection Severity |
Residence, population density, comorbidity (HIV, TB and anaemia) | The rate of COVID-19 infection increases as the population density increases. Linked to this, the rate of infection is low in rural settings than in urban areas. The study reported that comorbidity would increase severity of the disease. The rate of anaemia, TB and HIV compared with the rate of DM, HTN and obesity is higher in Africa than other continents, and these (anaemia, TB and HIV) are the underlying conditions that lead to COVID-19 related severity in Africa. |
| Gayawan et al22 | Africa | General | Spatio-temporal analysis | Not specified | Infection | Number of physicians. Number of hospital beds. |
Positive correlation was revealed between COVID-19 and number of physicians (r=0.49, p value=<0.001) and hospital beds (r=0.14, p value=0.34) though only the estimate for physicians is significant. The spatio-temporal analysis reveals that the occurrence and burden of COVID-19 in Africa varied geographically with neighbouring countries particularly in the western part of the continent, which could imply that neighbouring countries pose significant importation risk to each other. |
| Hossain et al23 | Africa/global | General | Modelling | 1 174 652 | Infection | Weather, economic openness and political democracy | Countries with warmer temperatures showed slower spread than their comparator. Countries with higher economic openness had higher infection rates than with lower economic openness. The countries with stronger political democracy had higher infection rates than with weaker political democracy. |
| Jaffe and Vera24 | Africa/global | General | Cross- sectional | Dataset of 36 countries | Infection Mortality |
Imports of goods and services, international tourism, electric power consumption and population over 65 years old | Countries that were connected to the global economy tended to have a higher risk of infection, while the risk of mortality from the disease are higher in less globalised low-income countries. Countries with higher imports of goods and services and international tourism had higher infection rates than their comparator. |
| Kubota et al25 | Africa/global | General | Modelling study | 1055 countries | Infection | Age, precipitation, temperature, international travel, BCG vaccination and malaria infection | A negative correlation between the accumulated numbers of the COVID-19 cases and the following variables: mean temperature, BCG vaccination effect and malaria infection. The study found a positive correlation between the accumulated numbers of the COVID-19 cases and the following variables: mean precipitation, the relative frequency of foreign visitors per population, GDP per person, population density and relative proportion of people ≥65 years old. |
| Maitra et al 26 | Africa/global | General | Cross-sectional | 422 582 | Mortality | Health expenditure | Countries with low health expenditure (percentage of GDP) were significantly associated with higher case fatality rate (p=0.0017). |
| Maraghi et al27 | Africa/global | Not specified | Cross-sectional | >1000 but globally | Case fatality and recovery rate | Prevention, detection, response, risk environment indices and global health security (GHS) | Prevention (r=−0.988, −0.1.0 to −0.548), p=0.012), detection (r=−0.979 (−1.000 to –0.312), p=0.021), response (r=−0.965 (−0.999 to −0.051), p=0.035) and GHS (r=−0.995 (−1.000 to −0.786), p=0.005) were negatively correlated with case fatality rate in African countries. |
| Muneer et al28 | Africa/global | General | Web-based survey (worldometer) | – | Infection | Malaria prevalence | Ahigh rate of malaria was negatively correlated with COVID-19 (r=−0.15, p=0.02). |
| Okpokoro et al8 | Africa/global | General | Ecologic study | Mortality | COPD and tobacco use | Mortality was positively correlated with COPD (rho=−0.28, p=0.09) and tobacco use (rho=−0.01, p=0.91) although not statistically significant. Similarly, the study showed that mortality was negatively correlated with life expectancy (rho=−0.09, p=0.24), quality of air (rho=−0.02, p=0.84) and life expectancy (rho=−0.24, p=0.1). | |
| Onovo et al9 | Sub-Saharan Africa (SSA) | General | Survey | – | Infection | Adult HIV incidence rate, infant’s pneumococcal conjugate-based vaccine, incidence of malaria and diarrhoea treatment for under 5 | HIV incidence (p=0.0001), pneumococcal conjugate-based vaccine (p=0.001), incidence of malaria (p=0.001) and diarrhoea treatment (p=0.002) could significantly predict COVID-19 infection in SSA. However, TB incidence (p=0.86) and smoking prevalence (p=0.53) were not statistically associated with COVID-19 infection. |
| Ortiz-Fernández and Sawalha29 | Africa/global | General | Genetics | 2504 | Susceptibility | Lower expression of ACE2 and type II transmembrane serine protease (TMPRSS2) genes |
Africans were reported to have lower expression levels of ACE2 and TMPRSS2, suggesting a lower susceptibility for SARS-CoV-2 infection in the African populations. |
CKD, chronic kidney disease; COPD, chronic obstructive pulmonary disease; CRD, chronic respiratory disease; CVD, cardiovascular diseases; DM, diabetes mellitus; GDP, gross domestic products; HTN, hypertension; TB, tuberculosis.
Factors affecting COVID-19 infection, severity and related death
Demographic, institutional, economic, environmental, health system policy, lifestyle and political factors were reported to have an effect on prevention and spread of COVID-19, so were the presence and level of chronic conditions.7–9 18–29 For example, we found that COVID-19 infection and related deaths were affected by political democracy and economic openness as measured by volume of imports of goods and services and international tourism. Furthermore, high rate of comorbid conditions was positively correlated with COVID-19 infection and related death, with people having one or more chronic conditions experiencing severe form of the disease. A detailed summary of all the relevant factors affecting the infection, severity and mortality related to COVID-19 is presented in table 2.
Table 2.
Factors associated with COVID-19 infection, severity and related death in Africa
| Outcome | Theme | Potential specific factors |
| Infection | Demographic factors | High number of people aged ≥65 years25 and high population density.21 25 |
| Health system level factors | Low number of physicians and hospitals22 and low BCG vaccination.24 | |
| Politico-economic factors | High economic openness, strong political democracy,23 more imports of goods and services, wide international tourism, high international travel24 and city connectivity.20 | |
| Environmental factor | Low mean temperature.23 25 | |
| Comorbid conditions | Low malaria infection rate,9 25 28 high HIV infection rate and under-5 diarrhoeal disease.9 | |
| Severity | Demographic factors | High percentage of older age population profile.7 19 |
| Comorbid conditions | People with HIV, TB and anaemia.19 21 | |
| Death | Health system policy factors | Low prevention, detection, response and risk environment indices.27 |
| Politico-economic factors | More imports of goods and services, wide international tourism,24 low global health security index score27 and low health expenditure (percentage of GDP).26 | |
| Chronic illness and lifestyle factors | High prevalence of chronic illness and tobacco use.8 |
COPD, chronic obstructive pulmonary disease; GDP, gross domestic product; TB, tuberculosis.
Quality and risk of bias assessment
Detailed results of the methodological quality and risk of bias assessment of individual studies according to the JBI tool are reported in online supplemental appendix 4. In summary, five (34%) studies scored 100%, six (40%) studies scored 80%–89% and three (20%) studies scored 70%–79%. Excluding studies with low scores did not materially change the results.
Discussion
The systematic review presents a comprehensive summary of the current evidence on risk factors of COVID-19 infection, severity and related deaths in Africa. Demographic, institutional, political and ecological factors were linked with high COVID-19 infection rates in Africa. The study also revealed that severe forms of COVID-19 were associated with comorbidities and specific demographic characteristics. Health system organisation and policy, politico-economic situation, prevalence of chronic conditions and lifestyle factors increase the risk of deaths associated with COVID-19.
African countries that heavily rely on international trade and tourism were likely to have higher infection rates than other countries in the region.23 24 As anticipated, the rate of COVID-19 infection was higher among densely populated countries given that the disease is mainly spread through close contact with infected persons.30 31 A similar finding was observed elsewhere.32
African countries enjoying a stable political democracy have an open economy and well-connected air and road network were found to have a higher risk of COVID-19 infection.20 23 This could be attributed to the fact that countries with strong democracy have a laissez-faire administrative system, where people are not obliged to obey and practice some public health measures that may infringe freedom of movement and the pursuit of happiness. Democratic systems also go hand in hand with law and order and a higher than average disposable income, which create opportunities for leisure and work-related travels both internally and internationally, which increase the risk of COVID-19 transmission. In addition, countries with open economies and high transport connectivity are characterised by high mobility, facilitating spread of the disease.
The studies included in this review reported mixed findings with regards to the effect of temperature on COVID-19 infection. For example, the current review indicated that people living in countries with warmer temperature are less likely to acquire infection.23 33 Contrary to this observation, some African countries such as Egypt, which enjoys warm weather through the year, are highly affected by the virus as compared with other African countries with relatively cooler temperature.34 Yao and colleagues, however,35 demonstrated that temperature had no significant association with COVID-19 infection. As highlighted in the study,32 further investigation is required to determine the role of weather on transmission and spread of COVID-19.
Age, particularly being an older person, was associated with more severe forms of COVID-19 at admission to hospital.36 This might be explained by weaker immunity among older people. Patients with coinfections such as TB are more likely to experience severe forms of COVID-19.21 TB infection is common in low-resource settings and among older adults with pre-existing conditions resulting in high vulnerability to severe form of COVID-19 infection.19 37 Evidence on the effect of COVID-19 on people with HIV and malaria is limited.38 A study by Karmen-Tuohy et al39 showed that being infected with HIV at the time of acquiring COVID-19 does not significantly increase the severity of illness or the risk of complications. However, further research is warranted as the available evidence is inconclusive. Most importantly, given the high burden of HIV and malaria in the Africa region, the molecular, genetic, clinical and environmental implications of COVID-19 on people living with HIV and malaria should be explored in greater detail.
Generally, patients with underlining chronic conditions are at a higher risk of having sever COVID-19 and related mortality. For instance, a study conducted by Cox et al38 revealed greater risk and severe forms of COVID-19 in patients with COPD. Findings of a meta-analysis of seven studies conducted in China also reported significant association between COVID-19 and hypertension, chronic respiratory disease and cardiovascular disease.40 These findings imply that countries with a high burden of chronic conditions are more likely to have more severe cases of COVID-19. People who died of COVID-19 had chronic hypertension, COPD and cardiovascular comorbidities than recovered patients.8 41 History of tobacco use was found to be associated with increased risk of COVID-19 death.8 42 Additionally, Zhou and colleagues43 found that 50% of patients who died of COVID-19 had a history of secondary bacterial infections. Chen and colleagues44 also reported that bacterial and fungal coinfections increase the risk of COVID-19 related mortality. Thus, public health and medical services responding to the pandemic in Africa should be equipped with resources that enable the identification of cases with underlining chronic conditions and provide tailored interventions.
The present review revealed that countries with effective healthcare system such as a strong disease prevention, case detection and response programme and have a strong global health security system in pace had lower case fatality rate.27 This was supported by a WHO report that the COVID-19 pandemic is straining health systems worldwide as health facilities have been overstretched and unable to operate effectively due to increased burden for health facilities and healthcare workers.45 Importantly, higher per capita expenditure on health significantly reduces the risk of COVID-19 deaths.26 This could be attributed to the fact that a strong health system with sufficient resources is both adaptive, resilient and often has the required manpower and facilities to respond to the higher demand for medical staff and supplies in treating COVID-19 cases.
The study has the following limitations. First, the results reported in the paper with respect to associated factors do not necessarily imply causality as most of the included studies were based on either cross-country or cross-sectional designs that are not suitable for studying causal relationships. Second, we have used hospital admission as one of the indicators of severity, but this may not be a sufficient criterion given that in some countries, especially in the early stage of the pandemic, all symptomatic patients were systematically hospitalised to avoid transmission. Third, included articles were limited to those written in English. Fourth, there is still limited evidence on COVID-19 in countries Africa (some of the included studies are even preprint and others are modelling based studies), and the review was unable to provide a stratified analysis by regions—authors of the modelling studies have already noted some limitations of the modelling studies. Future research on COVID-19 in the region and beyond should focus on robust epidemiological study designs that are suitable to capture causal relationships and long-term impacts of the disease.
Conclusions
This systematic review demonstrated that several demographic, institutional, political, economic, environmental, lifestyle and health system factors as well as comorbid conditions increased the risk infection, severe forms of COVID-19 and deaths related to the virus in the Africa region. The impacts of these factors should be factored in by African governments and their development partners while designing tailored and targeted interventions to mitigate effects of the disease in the region. Implementing complete lockdown measures for an extended period in African countries is difficult or at least not as easy as in western countries due to the region’s unique social and economic settings. Alternative and effective measures such as mandatory face mask use and strong contact tracing system could be the most feasible interventions to contain the pandemic in the region.46 However, it should be noted that even with a complete adherence to such public health measures, governments can only expect to mitigate the spread of the virus in the region. Eventually, safe and effective vaccines and drugs are required to end this pandemic.
Supplementary Material
Acknowledgments
We are grateful for the authors of included studies. We did not receive any specific grant for this research.
Footnotes
Twitter: @Gesesew, @FisahaHaile
BAD and AA contributed equally.
Contributors: HAG, DNK, DMF, MW, YK, ABG, YAM, HM, KAA, MAA, MMB, ATG, YAG, DMS, MDM, TKT, SA, AFA, MBA, AKG, KG, TG, LG, CTL, GDK, MWM, ABM, DYT, AGT, FHT, WT, BLW, BAD and AAA conceived the idea. BAD, DNK and AAA performed search strategy. HAG, DNK, DMF, MW, ATG, BAD and AAA screened and extracted data. DMF and MW drafted introduction, DNK drafted methods, HAG drafted results, and ATG and YAM drafted discussion and conclusion. All authors critically review and approve the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article or uploaded as supplementary information. All data relevant to the study are included in the article or uploaded as supplementary information.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
References
- 1.He F, Deng Y, Li W. Coronavirus disease 2019: what we know? J Med Virol 2020;92:719–25. 10.1002/jmv.25766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Coronavirus disease (COVID-2019) situation reports. Geneva: World Health Organization, 2020. [Google Scholar]
- 3.JHU COVID-19 dashboard by the center for systems science and Engineering (CSSE) at Johns Hopkins University (JHU). John Hopkins University & Medicine Coronavirus Resource Center, 2020. Available: https://coronavirus.jhu.edu/map.html [Accessed 10 Jan 2020].
- 4.CDC Africa CDC dashboard: COVID-19. Addis Ababa: Africa CDC, 2020. [Google Scholar]
- 5.Mackenzie JS, Smith DW. COVID-19: a novel zoonotic disease caused by a coronavirus from China: what we know and what we don't. Microbiol Aust 2020:45–MA13. 10.1071/MA20013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He X, Lau EHY, Wu P, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med 2020;26:672–5. 10.1038/s41591-020-0869-5 [DOI] [PubMed] [Google Scholar]
- 7.Davies NG, Klepac P, Liu Y, et al. Age-dependent effects in the transmission and control of COVID-19 epidemics. Nat Med 2020;26:1205–11. 10.1038/s41591-020-0962-9 [DOI] [PubMed] [Google Scholar]
- 8.Okpokoro E, Igbinomwanhia V, Jedy-Agba E. Ecologic correlation between underlying population level morbidities and COVID-19 case fatality rate among countries infected with SARS-CoV-2. medRxiv 2020. 10.1101/2020.04.28.20082370 [DOI] [Google Scholar]
- 9.Onovo A, Atobatele A, Kalaiwo A, et al. Using supervised machine learning and empirical Bayesian kriging to reveal correlates and patterns of COVID-19 disease outbreak in sub-Saharan Africa: exploratory data analysis. SSRN Journal 2020;395 10.2139/ssrn.3580721 [DOI] [Google Scholar]
- 10.Kobia F, Gitaka J. COVID-19: are Africa's diagnostic challenges blunting response effectiveness? AAS Open Res 2020;3:4. 10.12688/aasopenres.13061.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Brauer M, Zhao JT, Bennitt FB. Global access to handwashing: implications for COVID-19 control in low-income countries. medRxiv 2020. 10.1101/2020.04.07.20057117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.The Lancet COVID-19 in Africa: no room for complacency. Lancet 2020;395:1669. 10.1016/S0140-6736(20)31237-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Chen S, Yang J, Yang W, et al. COVID-19 control in China during mass population movements at new year. Lancet 2020;395:764–6. 10.1016/S0140-6736(20)30421-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nachega J, Seydi M, Zumla A. The late arrival of coronavirus disease 2019 (COVID-19) in Africa: mitigating Pan-continental spread. Clin Infect Dis 2020;71:875–8. 10.1093/cid/ciaa353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.JBI Joanna Briggs Institute reviewers’ manual. Adelaide: Joanna Briggs Institute, 2014. [Google Scholar]
- 17.Joanna Briggs Institute Joanna Briggs Institute reviewers’ manual. Adelaide, SA, 2014. [Google Scholar]
- 18.Bergman NK, Fishman R. Mobility reduction and Covid-19 transmission rates. medRxiv 2020. 10.1101/2020.05.06.20093039 [DOI] [Google Scholar]
- 19.Clark A, Jit M, Warren-Gash C. How many are at increased risk of severe COVID-19 disease? rapid global, regional and national estimates for 2020. medRxiv 2020. 10.1101/2020.04.18.20064774 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Daon Y, Thompson RN, Obolski U. Estimating COVID-19 outbreak risk through air travel. J Travel Med 2020;27:1–8. 10.1093/jtm/taaa093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Diop BZ, Ngom M, Pougué Biyong C, et al. The relatively young and rural population may limit the spread and severity of COVID-19 in Africa: a modelling study. BMJ Glob Health 2020;5:e002699. 10.1136/bmjgh-2020-002699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gayawan E, Awe OO, Oseni BM, et al. The spatio-temporal epidemic dynamics of COVID-19 outbreak in Africa. Epidemiol Infect 2020;148:e212. 10.1017/S0950268820001983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hossain MA Is the spread of COVID-19 across countries influenced by environmental, economic and social factors? medRxiv. 2020 doi: 10.1101/2020.04.08.20058164. [DOI] [Google Scholar]
- 24.Jaffe R, Vera MPO JK. Globalized low-income countries may experience higher COVID-19 mortality rates. medRxiv 2020. 10.1101/2020.03.31.20049122 [DOI] [Google Scholar]
- 25.Kubota Y, Shiono T, Kusumoto B, et al. Multiple drivers of the COVID-19 spread: the roles of climate, International mobility, and region-specific conditions. PLoS One 2020;15:e0239385. 10.1371/journal.pone.0239385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Maitra S, Biswas M, Bhattacharjee S. Case- fatality rate in COVID- 19 patients: a meta-analysis of publicly accessible database. medRxiv 2020. 10.1101/2020.04.09.20059683 [DOI] [Google Scholar]
- 27.Maraghi E, Malehi AS, Rahim F. Global health security capacity against COVID-19 outbreak and its association with the case fatality rate: an analysis of annual data from 210 countries and territories. medRxiv 2020. 10.1101/2020.04.25.20079186 [DOI] [Google Scholar]
- 28.Muneer A, Kumari K, Tripathi M. Comparative analyses revealed reduced spread of COVID-19 in malaria endemic countries. medRxiv 2020. 10.1101/2020.05.11.20097923 [DOI] [Google Scholar]
- 29.Ortiz-Fernández L, Sawalha AH. Genetic variability in the expression of the SARS-CoV-2 host cell entry factors across populations. Genes Immun 2020;21:269–72. 10.1038/s41435-020-0107-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Liu J, Liao X, Qian S, et al. Community transmission of severe acute respiratory syndrome coronavirus 2, Shenzhen, China, 2020. Emerg Infect Dis 2020;26 10.3201/eid2606.200239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Rocklöv J, Sjödin H. High population densities catalyse the spread of COVID-19. J Travel Med 2020;27:taaa038. 10.1093/jtm/taaa038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Tosepu R, Gunawan J, Effendy DS, et al. Correlation between weather and Covid-19 pandemic in Jakarta, Indonesia. Sci Total Environ 2020;725:138436. 10.1016/j.scitotenv.2020.138436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xie J, Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci Total Environ 2020;724:138201. 10.1016/j.scitotenv.2020.138201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.JHU Coronavirus COVID-19 global cases by the center for systems science and Engineering Baltimore, US: Johns Hopkins University & Medicine Coronavirus Resource Center, 2020. Available: https://coronavirus.jhu.edu/map.html[Accessed 25 Mar 2020].
- 35.Yao Y, Pan J, Liu Z, et al. No association of COVID-19 transmission with temperature or UV radiation in Chinese cities. Eur Respir J 2020;55:2000517. 10.1183/13993003.00517-2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Shi Y, Yu X, Zhao H, et al. Host susceptibility to severe COVID-19 and establishment of a host risk score: findings of 487 cases outside Wuhan. Crit Care 2020;24:1–4. 10.1186/s13054-020-2833-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Crisan-Dabija R, Grigorescu C, Pavel C-A, et al. Tuberculosis and COVID-19: lessons from the past viral outbreaks and possible future outcomes. Can Respir J 2020;2020:1–10. 10.1155/2020/1401053 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cox MJ, Loman N, Bogaert D, et al. Co-infections: potentially lethal and unexplored in COVID-19. Lancet Microbe 2020;1:e11. 10.1016/S2666-5247(20)30009-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Karmen-Tuohy S, Carlucci PM, Zervou FN, Zacharioudakis IM, et al. Outcomes among HIV-positive patients hospitalized with COVID-19. J Acquir Immune Defic Syndr 2020;85:6–10. 10.1097/QAI.0000000000002423 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yang J, Zheng Y, Gou X. Prevalence of comorbidities in the novel Wuhan coronavirus (COVID-19) infection: a systematic review and meta-analysis. Int J Infect Dis 2020;94:91–5. 10.1016/j.ijid.2020.03.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chen T, Wu D, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020;368:m1091. 10.1136/bmj.m1091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Kozak R, Prost K, Yip L, et al. Severity of coronavirus respiratory tract infections in adults admitted to acute care in Toronto, Ontario. J Clin Virol 2020;126:104338. 10.1016/j.jcv.2020.104338 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020;395:1054–62. 10.1016/S0140-6736(20)30566-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020;395:507–13. 10.1016/S0140-6736(20)30211-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Organization WH Who releases guidelines to help countries maintain essential health Servics during the COVID-19 pandemic. Geneva, Switzerland: World Health Organization, 2020. [Google Scholar]
- 46.Giordano G, Blanchini F, Bruno R, et al. Modelling the COVID-19 epidemic and implementation of population-wide interventions in Italy. Nat Med 2020;26:855–60. 10.1038/s41591-020-0883-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-044618supp001.pdf (2.3MB, pdf)