Abstract
In December 2019, the coronavirus disease (COVID-19) was discovered in China, causing many cases and deaths. Several studies have explored the role of environmental factors in the spread of COVID-19, emphasizing the effect of two weather parameters, humidity and temperature. Those parameters are evidently vital in affecting outbreaks of infectious respiratory diseases, like influenza; yet, such an effect on COVID-19 remains controversial. This review explores the relation between the change in weather-related factors and the transmission of the COVID-19. With seasonal variation from winter to summer and in the absence of adopting thorough public health measures, elevated temperature and humidity might not limit the COVID-19 cases. Hence, we need multidisciplinary strategies and interventions to limit the burden of this pandemic over the healthcare systems.
Keywords: COVID-19, Seasonal variation, Temperature, Humidity, Transmission, Public health
Introduction
Since December 2019, a growing number of cases for the novel coronavirus disease (COVID-19), a worldwide health disaster of this time, has been discovered in China [1,2]. COVID-19 evidently has high transmission rates among humans with about 17, 396, 943 and 675,060 confirmed cases and deaths respectively as reported until August 1, 2020 [3], worldwide, hence declared the pandemic state and enforced lockdowns everywhere [4,5]. In addition to contacting humans and public mobility, environmental variables could affect droplet transmission and viral survival, such as the influenza virus; yet, it has not been well investigated for COVID-19. The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) varied genetically from both the severe acute respiratory syndrome coronavirus 1 (SARS-CoV-1) and the Middle East respiratory syndrome coronavirus (MERS-CoV), and therefore, it might spread differently with the changing climatic variables [6, 7, 8, 9, 10, 11, 12, 13, 14, 15].
Former studies have endorsed the epidemiological hypothesis of dry and cold environments, with lower absolute humidity and temperature, support the survival and transmission of viral infections spreading via droplets while humid and warmer environments, with higher absolute humidity and temperature, suppress such transmission. Absolute humidity, atmospheric water content, and temperature have been significantly associated with other viral transmissions. For instance, the survival of influenza viruses, either in droplets or on surfaces, is longer in dry and cold air, hence growing the potential transmission [16, 17, 18, 19, 20, 21, 22, 23, 24]. Yet, there is limited research on the effect of both temperature and absolute humidity on COVID-19 spread.
Globally, COVID-19 has overwhelmed the entire economy and the public health systems in their attempts to prevent and/or control such a virus via slowing the transmission down. Therefore, understanding how environmental variables affect the current pandemic would support deciding to control the infection, particularly in warmer and more humid areas where transmission rates might have been misjudged [25]. Ending lockdowns depend partly on whether COVID-19 transmission would decrease in response to varying humidity and temperature between seasons [26]. This review examines how the variation in absolute humidity and temperature could affect the transmission of this novel virus across many areas showing that some observed patterns of transmission might be with or against the conventional hypothesis stating that the more the absolute humidity and the temperature, the lower the transmissibility and survival of COVID-19. Yet, no conclusive result is reached so far.
Highlights from evidence
WHO announced COVID-19, caused by SARS-CoV-2, as a pandemic for quickly transmitting and rapidly crushing healthcare services because of cases needing intensive care worldwide [5]. A rational debate in the coping plans for COVID-19 if the virus would spread slower in humid and hot weather. Until August 1, 2020, 216 countries and regions all over the world had shown a local spread of COVID-19, including all climate zones, from dry and cold to humid and hot areas [3]. However, some Asian countries with local spread were common traveling spots from China, hence they imported cases. Similarly, African, and South American countries, with an average high temperature, had shown local spread. Several studies, considering the seasonality of respiratory tract viruses, reported that both humidity and temperature affect the pattern of the worldwide spread of the COVID-19 pandemic [27, 28, 29, 30, 31, 32, 33, 34, 35, 36, 37, 38, 39, 40].
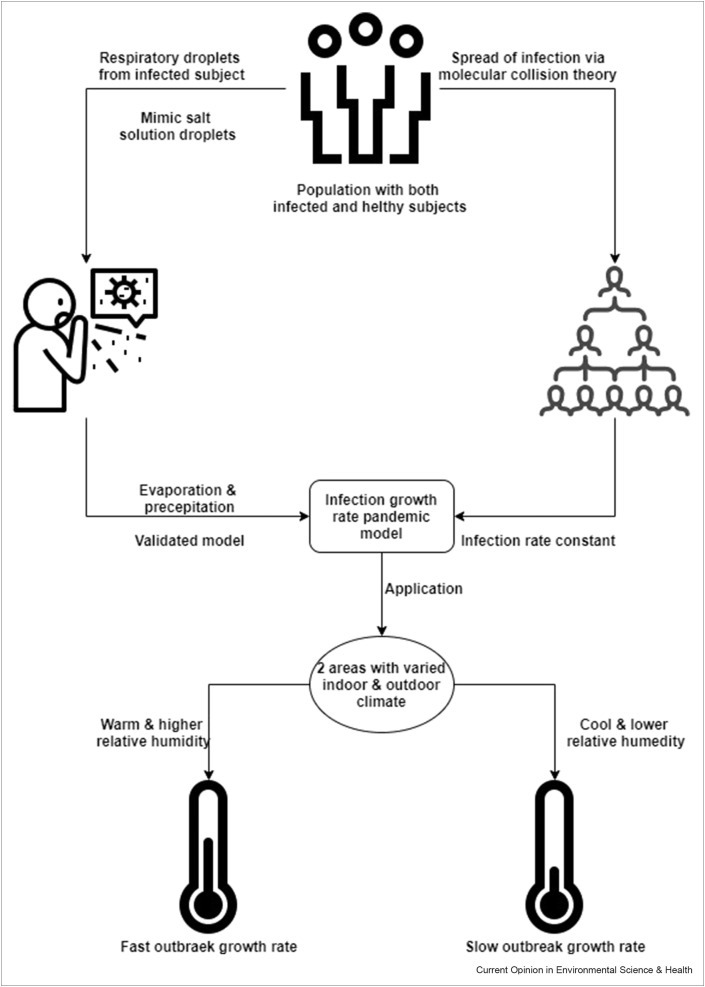
Scientists in one study developed a model to explain the sensitivity of the respiratory droplets to relative humidity and temperature and their association to COVID-19, as shown in Figure 1 . The model assumed that COVID-19 spread only by inhaling infected respiratory droplets. The vaporizing and drying time of droplets, an indicator for the infection rate constant, relies on relative humidity and temperature both indoors and outdoors, and the number of infected cases is directly associated with this infection rate constant. The study suggested that relative humidity and temperature have affected the COVID-19 spread. They found that with a similar relative humidity across two sites, COVID-19 transmits further fast at cooler temperatures compared to warmer ones, along with negligible effect upon including the measures of social enforcement [41].
Figure 1.
A model explains the sensitivity of the respiratory droplets to relative humidity and temperature and their association to COVID-19 [41].
In China, a study examined the relations between daily average relative humidity and temperature and the daily counted cases of COVID-19 in 30 districts using the generalized additive model (GAM). They found that COVID-19 daily cases’ counts were adversely associated with both the average relative humidity and temperature. The study suggested that both daily relative humidity and temperature affected the incidence of COVID-19 in some districts of China. Yet, such an effect was not consistent throughout the entire districts, where there was a spatiotemporal heterogeneity that could be caused by the meteorological attributes and intervention measures among districts [42]. Another study in 31 districts of China investigated how some meteorological factors would affect the growth of the COVID-19 outbreak, where they applied an exponential model considering the accumulated counts of confirmed cases and time. The growth of COVID-19 transmission rate, applying the condition of the doubling time of confirmed cases counts, was considered as the outcome variable applied in a linear model, which examined four exposure meteorological factors: humidity, temperature, precipitation, and wind velocity. They found that the doubling time correlates inversely to the temperature and the humidity, claiming a lower rate of COVID-19 growth with the spring and summer in the north [6]. However, a study investigated the temperature as a critical element in the COVID-19-caused infection, where researchers gathered data on both meteorological factors and daily confirmed cases from 122 cities in China. They used both piece-wise linear regression and generalized additive model (GAM) for nonlinear exploration, to analyze the relationship between COVID-19 confirmed cases and the average temperature. They found an approximate direct linear relationship between the count of COVID-19 confirmed cases and the average temperature as described by the output exposure-response graphs suggesting that the number of cases might not decrease in warmer climates [43].
Globally, a cohort study of 50 cities worldwide, having and lacking COVID-19, investigated whether the SARS-CoV-2 is associated with seasonality and the possibility of estimating transmission. The researchers claimed that COVID-19 outbreak-predominant areas had less absolute humidity and average temperature than those reported lower virus spread. Hence, the study found that the pattern of significant COVID-19 community outbreaks across controlled measures of temperature, humidity, and latitude was coherent with a seasonal respiratory virus behavior, suggesting it as a model for the likely prediction of the susceptible regions for significant COVID-19 community spread [44]. Likewise, a report from another study applied ecological modeling to compare the spread and the weather showing less transmission at a higher temperature and humidity in confirmed cases from cities in both China and the United States [34]. Similarly, a study in Spain analyzed COVID19 spatiotemporally via modeling the incidence of the reported cases regionally while counting for humidity, temperature, and sunshine. The study findings supported the hypothesis of lower disease at higher humidity and temperature [45]. Another study investigated relative humidity and temperature effects on daily-reported new COVID-19 cases and deaths for 166 countries, except for China, applying the log-linear generalized additive model. The study found that both relative humidity and temperature were adversely associated with daily-reported new COVID-19 cases and deaths (fewer cases and deaths with higher relative humidity and temperatures), suggesting that the COVID-19 spread might be slightly diminished at higher humidity and temperature [46].
Potential justifications for the gap in evidence
Most studies, added to those showing that the previous SARS-CoV-1 survived unfavorably in elevated humidity and temperatures, were considered as an adequate proof to expect that summer might enable the controlling of COVID-19 [47]; however, those observations might be confounded by the global pattern of traveling that led to slower transmission in temperate areas [48]. The worldwide transmission of the COVID-19 implies that seasonal variation cannot be regarded solely as a major modifier of spread; however, the warmer climate might moderately limit the spread of COVID-19. No proof has advised that warmer weather would limit the potency of COVID-19 spread leading to lesser required extra actions to restrict transmission [49]. Hence, it is vital to interpret these observations by considering the ongoing transmission of COVID-19 worldwide.
The studies, supporting the conventional hypothesis stating that the more the absolute humidity and the temperature, the lower the transmissibility and survival of COVID-19, showed an initial investigation and held some limitations [6,34,41,42,44, 45, 46]. For instance, the data were analyzed variably among studies where some investigators gathered either suspected, confirmed, or the total number of cases, while others quantified the incidence rates. The probability of infection is variable for the variable regions, and the population size is known to critically affect the rate of COVID-19 transmission. Different studies investigated various locations such as countries and even cities in the same country with variable sizes and densities of the population, while the incidence rate per unit population might better represent the epidemic. Hence, investigating the effect of environmental parameters on COVID-19 spread requires studying epidemic-centered areas separately from epidemic-sporadic ones. Further, the reported cases and moralities usually vary across countries for the variable testing availability, the tests’ sensitivity and specificity, and the reporting patterns. Moreover, the ecological time-series design in some studies might hold some ecological fallacy [50]. The chosen periods for the study are critical as well, where longer model periods might render higher resolving data for identifying correlations between the spread of COVID-19 and the environmental parameters, beyond just gathering pre-epidemic and post-epidemic data and missing chances to emphasize how epidemics start and end.
Besides, most of the studies used correlation analysis between the pandemic data and the meteorological factors at the early stages of the pandemic, yet, studying COVID-19 under various environmental conditions is missing. Hence, the entire ecological profile determining COVID-19 survival and transmission are yet less appreciated [51]. Further, many other key human factors (political, economic, demographic, or societal) were not included in some studies for the complicated analysis and the shortage of updated data [50]. Such factors might influence cases and deaths of COVID-19, like further features of the virus, effective searching for cases and tracing contacts, general health status, state responses, public health interventions, accessible medical resources, sanitary conditions, quarantine policies, capacities for COVID-19 prevention and control strategies, climate factors such as air pollution, individual lifestyle, and traveling pattern, rates of urbanization, among others.
Ultimately, future research from epidemiology, biomedical sciences, and ecological studies are promptly needed to explore such variables for generating more empirical evidence, involving decision-makers, public health practitioners, and the strategies in the upcoming months for controling the worldwide spread of COVID-19. Multidisciplinary strategies and interventions are needed, primarily in areas with rapidly growing rates of transmission; hence, implementing preventive measures in such areas would limit the spread and the potential crashing in the healthcare system. Eventually, more investigations on the influence of changing weather, atmospheric pollution, and other external agents previously mentioned on the spread of COVID-19 should include more areas of the world and consider the public mobility from sites of a great incidence, public vulnerability, and surveying respiratory infections. Now stakeholders should emphasize optimal social distancing, and any suggestions on the risk of COVID-19 according to only climatic data should be perceived carefully.
Conclusions
This review examined how humidity and temperature affect transmission and hence cases and deaths from COVID-19 worldwide. According to previously surveyed evidence, some findings suggested that COVID-19 transmission is inversely proportional to temperature and absolute humidity. Therefore, the seasonal variation might be a significant element influencing transmission and deaths from COVID-19; however, the maintained spread and rapidly increasing cases across a varying humidity from dry and cold areas to temperate ones show that weather changes via raised humidity and temperature in spring and summer alone would not result in a reduction in the number of cases without thorough population health interventions. The inconsistent global effect of the meteorological attributes on COVID-19 spread requires more investigations, especially on how the temperature and absolute humidity affect such spread. For the upcoming months of the summer, applying modeling techniques to analyze further climatic conditions while considering the previously mentioned variables and covering wider areas worldwide over extended periods covering different ranges of humidity and temperature might provide further precise data and enable estimating the vulnerable areas for significant COVID-19 community transmission, and hence, more focused public health efforts. The conventional wisdom of warmer climate could slow the COVID-19 spread has proven to be inconsistent with the currently evident transmission to tropical areas of the world. We still need to stick to rigorous social enforcement measures, such as social distancing, using nonmedical masks to prevent droplets entering the respiratory tract, quarantining, and contact tracing, much needed to control such a pandemic.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
This reviews comes from a themed issue on Environmental Health : Interdisciplinary medical research in the field of public and environmental health (2021)
Edited by Lotfi Aleya, Md. Sahab Uddin and Simona G. Bungau
References
- 1.Zhu N., Zhang D., Wang W., Li X., Yang B., Song J., et al. A novel coronavirus from patients with pneumonia in China, 2019. N Engl J Med. 2020;382:727–733. doi: 10.1056/NEJMoa2001017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wu F., Zhao S., Yu B., Chen Y.-M., Wang W., Song Z.-G., et al. A new coronavirus associated with human respiratory disease in China. Nature. 2020;579:265–269. doi: 10.1038/s41586-020-2008-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.WHO . 2020. Coronavirus disease (COVID-19) situation report – 194. [Google Scholar]
- 4.VOA Where did they go? Millions Left Wuhan Before Quarantine. 2020 [Google Scholar]
- 5.Callaway E. Time to use the p-word? Coronavirus enters dangerous new phase. Nature. 2020 doi: 10.1038/d41586-020-00551-1. [DOI] [PubMed] [Google Scholar]
- 6.Oliveiros B., Caramelo L., Ferreira N.C., Caramelo F. Role of temperature and humidity in the modulation of the doubling time of COVID-19 cases. MedRxiv. 2020:2020. doi: 10.1101/2020.03.05.20031872. The researchers investigated how some meteorological factors would affect the growth of COVID-19 outbreak in 31 districts of China where they applied an exponential model considering the accumulated counties of confirmed cases and time and found that the doubling time correlates inversely to the temperature and the humidity, claiming a lower rate of COVID-19 growth with the spring and summer in the north. [DOI] [Google Scholar]
- 7.NCIRD . CDC; 2020. Coronavirus | human coronavirus types. [Google Scholar]
- 8.International I.C.T.V. Int comm taxon viruses ICTV. 2020. Committee on taxonomy of viruses (ICTV)https://talk.ictvonline.org/?Redirected=true [Google Scholar]
- 9.Chan K.H., Peiris J.S.M., Lam S.Y., Poon L.L.M., Yuen K.Y., Seto W.H. The effects of temperature and relative humidity on the viability of the SARS coronavirus. Adv Virol. 2011;2011 doi: 10.1155/2011/734690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dowell S.F., Ho M.S. Seasonality of infectious diseases and severe acute respiratory syndrome-what we don't know can hurt us. Lancet Infect Dis. 2004;4:704–708. doi: 10.1016/S1473-3099(04)01177-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Altamimi A., Ahmed A.E. Climate factors and incidence of Middle East respiratory syndrome coronavirus. J Infect Public Health. 2020;13:704–708. doi: 10.1016/j.jiph.2019.11.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Yip C., Chang W.L., Yeung K.H., Yu I.T.S. Possible meteorological influence on the severe acute respiratory syndrome (SARS) community outbreak at amoy gardens, Hong Kong. J Environ Health. 2007;70:39–47. [PubMed] [Google Scholar]
- 13.Yuan J., Yun H., Lan W., Wang W., Sullivan S.G., Jia S., et al. A climatologic investigation of the SARS-CoV outbreak in Beijing, China. Am J Infect Contr. 2006;34:234–236. doi: 10.1016/j.ajic.2005.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoeman D., Fielding B.C. Coronavirus envelope protein: current knowledge. Virol J. 2019;16:69. doi: 10.1186/s12985-019-1182-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhou Z.-X., Jiang C.-Q. [Effect of environment and occupational hygiene factors of hospital infection on SARS outbreak] Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi Zhonghua Laodong Weisheng Zhiyebing Zazhi Chin J Ind Hyg Occup Dis. 2004;22:261–263. [PubMed] [Google Scholar]
- 16.Barreca A.I., Shimshack J.P. Absolute humidity, temperature, and influenza mortality: 30 years of county-level evidence from the United States. Am J Epidemiol. 2012;176(Suppl 7):S114–S122. doi: 10.1093/aje/kws259. [The researchers found that the absolute humidity has been significantly associated with respiratory viral transmissions like the influenza virus] [DOI] [PubMed] [Google Scholar]
- 17.Shaman J., Goldstein E., Lipsitch M. Absolute humidity and pandemic versus epidemic influenza. Am J Epidemiol. 2011;173:127–135. doi: 10.1093/aje/kwq347. [The researchers found that the survival of influenza viruses, either in droplets or on surfaces, is longer in dry and cold air; hence, growing the potential transmission] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mourtzoukou E.G., Falagas M.E. Exposure to cold and respiratory tract infections. Int J Tuberc Lung Dis Off J Int Union Tuberc Lung Dis. 2007;11:938–943. [PubMed] [Google Scholar]
- 19.Dalziel B.D., Kissler S., Gog J.R., Viboud C., Bjørnstad O.N., Metcalf C.J.E., et al. Urbanization and humidity shape the intensity of influenza epidemics in U.S. cities. Science. 2018;362:75–79. doi: 10.1126/science.aat6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Paynter S. Humidity and respiratory virus transmission in tropical and temperate settings. Epidemiol Infect. 2015;143:1110–1118. doi: 10.1017/S0950268814002702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Park J.-E., Son W.-S., Ryu Y., Choi S.B., Kwon O., Ahn I. Effects of temperature, humidity, and diurnal temperature range on influenza incidence in a temperate region. Influenza Other Respir Viruses. 2020;14:11–18. doi: 10.1111/irv.12682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steel J., Palese P., Lowen A.C. Transmission of a 2009 pandemic influenza virus shows a sensitivity to temperature and humidity similar to that of an H3N2 seasonal strain. J Virol. 2011;85:1400–1402. doi: 10.1128/JVI.02186-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lowen A.C., Steel J. Roles of humidity and temperature in shaping influenza seasonality. J Virol. 2014;88:7692–7695. doi: 10.1128/JVI.03544-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kudo E., Song E., Yockey L.J., Rakib T., Wong P.W., Homer R.J., et al. Low ambient humidity impairs barrier function and innate resistance against influenza infection. Proc Natl Acad Sci Unit States Am. 2019;116:10905–10910. doi: 10.1073/pnas.1902840116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Luo W., Majumder M.S., Liu D., Poirier C., Mandl K.D., Lipsitch M., et al. The role of absolute humidity on transmission rates of the COVID-19 outbreak. MedRxiv. 2020 doi: 10.1101/2020.02.12.20022467. [The researchers suggested that understanding how environmental variables affect the current outbreak would support deciding to control the infection, particularly in warmer and more humid areas where transmission rates might have been misjudged] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Jia J., Ding J., Liu S., Liao G., Li J., Duan B., et al. ArXiv200302985 Math Q-Bio; 2020. Modeling the control of COVID- 19: impact of policy interventions and meteorological factors. [Google Scholar]
- 27.Moriyama M., Hugentobler W.J., Iwasaki A. Seasonality of respiratory viral infections. Annu Rev Virol. 2020 doi: 10.1146/annurev-virology-012420-022445. [DOI] [PubMed] [Google Scholar]
- 28.AL-Rousan N., Al-Najjar H. Social Science Research Network; Rochester, NY: 2020. Nowcasting and forecasting the spreading of novel coronavirus 2019-nCoV and its association with weather variables in 30 Chinese provinces: a case study. [DOI] [Google Scholar]
- 29.Bannister-Tyrrell M., Meyer A., Faverjon C., Cameron A. MedRxiv; 2020. Preliminary evidence that higher temperatures are associated with lower incidence of COVID-19, for cases reported globally up to 29th February 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bu J., Peng D.-D., Xiao H., Yue Q., Han Y., Lin Y., et al. MedRxiv; 2020. Analysis of meteorological conditions and prediction of epidemic trend of 2019-nCoV infection in 2020. 2020.02.13.20022715. [DOI] [Google Scholar]
- 31.Bukhari Q., Jameel Y. Social Science Research Network; Rochester, NY: 2020. Will coronavirus pandemic diminish by summer? [DOI] [Google Scholar]
- 32.Chen B., Liang H., Yuan X., Hu Y., Xu M., Zhao Y., et al. Roles of meteorological conditions in COVID-19 transmission on a worldwide scale. MedRxiv. 2020:2020. doi: 10.1101/2020.03.16.20037168. [DOI] [Google Scholar]
- 33.Poirier C., Luo W., Majumder M.S., Liu D., Mandl K., Mooring T., et al. Social Science Research Network; Rochester, NY: 2020. The role of environmental factors on transmission rates of the COVID-19 outbreak: an initial assessment in two spatial scales. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wang J., Tang K., Feng K., Lin X., Lv W., Chen K., et al. Social Science Research Network; Rochester, NY: 2020. High temperature and high humidity reduce the transmission of COVID-19. [The researchers applied ecological modeling to compare the spread and the weather showing less transmission in higher temperature and humidity in confirmed cases from cities in both China and the United States] [DOI] [Google Scholar]
- 35.Wang M., Jiang A., Gong L., Luo L., Guo W., Li C., et al. Temperature significant change COVID-19 Transmission in 429 cities. MedRxiv. 2020:2020. doi: 10.1101/2020.02.22.20025791. [DOI] [Google Scholar]
- 36.Bhattacharjee S. Statistical investigation of relationship between spread of coronavirus disease (COVID-19) and environmental factors based on study of four mostly affected places of China and five mostly affected places of Italy. ArXiv200311277 Phys Q-Bio. 2020 [Google Scholar]
- 37.Gupta D. Social Science Research Network; Rochester, NY: 2020. Effect of ambient temperature on COVID-19 infection rate. [DOI] [Google Scholar]
- 38.Shi P., Dong Y., Yan H., Li X., Zhao C., Liu W., et al. The impact of temperature and absolute humidity on the coronavirus disease 2019 (COVID-19) outbreak - evidence from China. MedRxiv. 2020:2020. doi: 10.1101/2020.03.22.20038919. [DOI] [Google Scholar]
- 39.Yao Y., Pan J., Liu Z., Meng X., Wang W., Kan H., et al. No association of COVID- 19 transmission with temperature or UV radiation in Chinese cities. Eur Respir J. 2020;55 doi: 10.1183/13993003.00517-2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Liu J., Zhou J., Yao J., Zhang X., Li L., Xu X., et al. Impact of meteorological factors on the COVID-19 transmission: a multi-city study in China. Sci Total Environ. 2020;726:138513. doi: 10.1016/j.scitotenv.2020.138513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Chaudhuri S., Basu S., Kabi P., Unni V.R., Saha A. ArXiv200410929 Cond-Mat Physicsphysics Q-Bio; 2020. Modeling ambient temperature and relative humidity sensitivity of respiratory droplets and their role in Covid-19 outbreaks. The researchers applied a model to explain the sensitivity of the respiratory droplets to relative humidity and temperature and their association to COVID-19, where they found that with a similar relative humidity across two sites, COVID-19 transmits further fast at a cooler temperature compared to warmer ones along with a nonsignificant difference to the results when including the measures of social enforcement. [Google Scholar]
- 42.Qi H., Xiao S., Shi R., Ward M.P., Chen Y., Tu W., et al. COVID-19 transmission in Mainland China is associated with temperature and humidity: a time-series analysis. Sci Total Environ. 2020;728:138778. doi: 10.1016/j.scitotenv.2020.138778. The researchers examined the relations between daily average relative humidity and temperature and the daily counted cases of COVID-19 in 30 districts of China using the generalized additive model (GAM) and found that COVID-19 daily cases’ counts were adversely associated with both the average relative humidity and temperature in some districts of China. Yet, such an effect was not consistent throughout the entire districts, where there was a spatiotemporal heterogeneity. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Xie J., Zhu Y. Association between ambient temperature and COVID-19 infection in 122 cities from China. Sci Total Environ. 2020;724:138201. doi: 10.1016/j.scitotenv.2020.138201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sajadi M.M., Habibzadeh P., Vintzileos A., Shokouhi S., Miralles-Wilhelm F., Amoroso A. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19) JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.11834. The researchers studied 50 cities and reported that COVID-19 outbreak-predominant areas had less absolute humidity and average temperature than those reported lower virus spread. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Paez A., Lopez F.A., Menezes T., Cavalcanti R., Pitta M.G. d.a. R. A spatio-temporal analysis of the environmental correlates of COVID-19 incidence in Spain. Geogr Anal. 2020 doi: 10.1111/gean.12241. The researchers analyzed COVID-19 spatiotemporally in Spain via modeling the incidence of the reported cases regionally while counting for humidity, temperature, and sunshine, where findings supported the hypothesis of lower disease at higher humidity and temperatures. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Wu Y., Jing W., Liu J., Ma Q., Yuan J., Wang Y., et al. Effects of temperature and humidity on the daily new cases and new deaths of COVID-19 in 166 countries. Sci Total Environ. 2020;729:139051. doi: 10.1016/j.scitotenv.2020.139051. The researchers investigated relative humidity and temperature effects on daily-reported new COVID-19 cases and deaths for 166 countries, except for China, applying the log- linear generalized additive model and found that both relative humidity and temperature were adversely associated with daily-reported new COVID-19 cases and death. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Araujo M.B., Naimi B. Spread of SARS-CoV-2 Coronavirus likely to be constrained by climate. MedRxiv. 2020 doi: 10.1101/2020.03.12.20034728. The researchers expected that summer might enable controlling COVID-19. [DOI] [Google Scholar]
- 48.Lai S., Bogoch I., Ruktanonchai N., Watts A., Lu X., Yang W., et al. Assessing spread risk of Wuhan novel coronavirus within and beyond China, January-April 2020: a travel network-based modelling study. MedRxiv. 2020 doi: 10.1101/2020.02.04.20020479. [The researchers concluded that the global pattern of traveling was a confounder and led to slower transmission in temperate areas] [DOI] [Google Scholar]
- 49.O'Reilly K.M., Auzenbergs M., Jafari Y., Liu Y., Flasche S., Lowe R. Effective transmission across the globe: the role of climate in COVID-19 mitigation strategies. Lancet Planet Health. 2020;4:e172. doi: 10.1016/S2542-5196(20)30106-6. The researchers found that the worldwide transmission of the COVID-19 implies that seasonal variation cannot be regarded as a major modifier of spread. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Auler A.C., Cássaro F.A.M., da Silva V.O., Pires L.F. Evidence that high temperatures and intermediate relative humidity might favor the spread of COVID-19 in tropical climate: a case study for the most affected Brazilian cities. Sci Total Environ. 2020;729:139090. doi: 10.1016/j.scitotenv.2020.139090. The researchers applied the ecological time-series design that might hold some ecological fallacy where it did not consider longer durations to reflect better the association between the spread of COVID-19 and seasonal factors. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Yuan S., Jiang S.-C., Li Z.-L. Do humidity and temperature impact the spread of the novel coronavirus? Front Public Health. 2020;8 doi: 10.3389/fpubh.2020.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]