Abstract
Background
Severity of illness in COVID-19 is consistently lower in women. A focus on sex as a biological factor may suggest a potential therapeutic intervention for this disease. We assessed whether adding progesterone to standard of care (SOC) would improve clinical outcomes of hospitalized men with moderate to severe COVID-19.
Research Question
Does short-term subcutaneous administration of progesterone safely improve clinical outcome in hypoxemic men hospitalized with COVID-19?
Study Design and Methods
We conducted a pilot, randomized, open-label, controlled trial of subcutaneous progesterone in men hospitalized with confirmed moderate to severe COVID-19. Patients were randomly assigned to receive SOC plus progesterone (100 mg subcutaneously twice daily for up to 5 days) or SOC alone. In addition to assessment of safety, the primary outcome was change in clinical status on day 7. Length of hospital stay and number of days on supplemental oxygen were key secondary outcomes.
Results
Forty-two patients were enrolled from April 2020 to August 2020; 22 were randomized to the control group and 20 to the progesterone group. Two patients from the progesterone group withdrew from the study before receiving progesterone. There was a 1.5-point overall improvement in median clinical status score on a seven-point ordinal scale from baseline to day 7 in patients in the progesterone group as compared with control subjects (95% CI, 0.0-2.0; P = .024). There were no serious adverse events attributable to progesterone. Patients treated with progesterone required three fewer days of supplemental oxygen (median, 4.5 vs 7.5 days) and were hospitalized for 2.5 fewer days (median, 7.0 vs 9.5 days) as compared with control subjects.
Interpretation
Progesterone at a dose of 100 mg, twice daily by subcutaneous injection in addition to SOC, may represent a safe and effective approach for treatment in hypoxemic men with moderate to severe COVID-19.
Trial Registry
ClinicalTrials.gov; No.: NCT04365127; URL: www.clinicaltrials.gov.
Key Words: COVID-19, progesterone, sex difference in COVID-19 outcomes
As of January 2021, more than 96 million cases of COVID-19 with 2 million deaths1 have been reported; of these, men with severe illness appear to be disproportionately overrepresented, with some data suggesting that for every 10 women who are hospitalized, admitted to the ICU, or die of COVID-19, 12 men are hospitalized, 19 men are admitted to ICU, and 15 men die.2, 3, 4, 5, 6, 7
This sex disparity is attributable in part to the higher prevalence of preexisting comorbidities associated with worse COVID-19 outcomes among men.8 , 9 Men are more likely to engage in smoking and alcohol use, with greater reluctance to seek health care, which may promote poorly controlled chronic conditions.10 At a biological level, differences in gene expression and hormonal influences may favor the female sex as it relates to the course of this disease.11 , 12 Intriguingly, when women with COVID-19 were stratified by menstrual status, premenopausal women had lower rates of hospitalization, less requirement for respiratory support, and shorter duration of hospitalization compared with postmenopausal women.13
In light of these observations, progesterone, a steroid hormone produced by the ovaries during reproductive cycles, is postulated to play a role in immunomodulation of COVID-19.11 , 12 , 14 Progesterone receptors are expressed on both innate and adaptive immune cells, regulating local and systemic inflammation in premenopausal women.15 These effects include inhibition of neutrophil degranulation and free radical generation, suppression of proinflammatory cytokine production, and skewing of T-cell signaling toward the production of antiinflammatory cytokines.14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24 With increased mortality in COVID-19 associated with the development of ARDS, higher levels of endogenous progesterone in women may confer a protective factor by dampening the exaggerated inflammatory immune cascade, or “cytokine storm,” that leads to severe lung injury.25, 26, 27 In fact, in a mouse model of influenza A, exogenous progesterone administration has been shown to decrease pulmonary inflammation, reduce protein leakage into airways, and promote faster recovery by enhancing repair of pulmonary epithelial cells.28
Given the immune-modulatory properties of progesterone, the purpose of this investigator-initiated randomized study was to assess clinical efficacy and safety of subcutaneous progesterone in hypoxemic men hospitalized with COVID-19. We hypothesized that the antiinflammatory properties of progesterone could dampen the systemic cytokine response, reducing severity of illness, and shorten the need for supplemental oxygen or hospitalization.
Methods
The protocol was approved by the Cedars-Sinai Institutional Review Board. Furthermore, the study was reviewed by the Food and Drug Administration (FDA) and was authorized to proceed under an Intermediate-Sized Patient Population Expanded Access Investigational New Drug (IND 149534) protocol. e-Appendix 1 outlines the trial protocol and statistical analysis plans. All patients or legally authorized representatives provided written informed consent. This study was registered as a National Institutes of Health-sponsored randomized clinical trial.29
Patients
Eligible patients were men at least 18 years of age, hospitalized with a single positive SARS-CoV-2 real-time reverse transcription-polymerase chain reaction (rRT-PCR) test result from a nasopharyngeal swab sample obtained within 72 h of randomization. Participants were included only if they had evidence of lower respiratory tract involvement based on imaging or the presence of crackles on chest physical examination. Eligible patients had an oxygen saturation of ≤ 94% on room air, and were receiving supplemental oxygen by regular nasal cannula, face mask, or high-flow nasal cannula (HFNC) at an Fio 2 of ≤ 50%. Patients were excluded if they were receiving invasive or noninvasive mechanical ventilation. All participants, while hospitalized, were required to be receiving thromboembolism chemoprophylaxis (subcutaneous unfractionated heparin [5,000 units twice daily] or enoxaparin [40 mg daily]). Contraindications to anticoagulants precluded study enrollment. Patients were excluded if they had a history of thromboembolic disease, breast cancer, or liver transaminases greater than five times the upper limit of normal. e-Table 1 lists the full eligibility criteria.
Study Design
This was a pilot study to assess the feasibility, safety, and potential efficacy of using progesterone in hypoxemic men with COVID-19. Patients were enrolled at a single center, a large academic hospital in Los Angeles, California, between April 27 and August 5, 2020 and randomly assigned to receive institutional standard of care (SOC) with or without progesterone. Randomization was performed in an electronic case report form system (REDCap),30 , 31 1:1 with random block sizes of four, six, or eight subjects using tables generated from Stata (version 16.1; StataCorp). Block randomization was implemented to ensure that patients were equally assigned to each treatment group. Varying the block size reduced selection bias by keeping the investigator blinded to the size of the block, thus preventing predictability of the allocation of patients in a single-center study. Patients, investigators, and treating providers were not blinded to study drug assignment. The investigators were not involved in decisions concerning initiation of SOC treatment options, initiation or discontinuation of oxygen or mechanical ventilation, type or amount of supplemental oxygen, or discharge from the hospital. The clinical status assessment was made through chart review.
Patients randomized to the progesterone group received 100 mg of progesterone subcutaneously twice daily for 5 days while hospitalized. Patients who had sufficiently improved, in the judgment of the treating providers, could be discharged from the hospital before completing their assigned courses of treatment. The protocol permitted use of other agents with presumptive activity against SARS-CoV-2 if such use was part of institutional SOC. With rapidly evolving therapeutic approaches for COVID-19 during the course of this trial, the SOC may have differed for patients enrolled at different time points into the trial; concomitant therapeutic interventions are outlined in Table 1 and e-Table 2.
Table 1.
Concomitant Therapeutic Interventions
| Intervention | Progesterone Group (n = 18) [No. (%)] | Control Group (n = 22) [No. (%)] |
|---|---|---|
| Azithromycin | 10 (55.6) | 10 (45.5) |
| Remdesivir | 9 (50.0) | 15 (68.2) |
| Systemic glucocorticoids | 9 (50.0) | 15 (68.2) |
| Dexamethasone | 7 (38.9) | 10 (45.5) |
| Tocilizumab | 1 (5.6) | 4 (18.2) |
| Convalescent plasma | 0 (0.0) | 2 (9.1) |
| Hydroxychloroquine | 0 (0.0) | 1 (4.5) |
Control patients with significant clinical deterioration (requiring higher supplemental oxygen through high-flow devices or mechanical ventilation at any point during the study), or those on day 7 without clinical improvement, were permitted to cross over to receive progesterone therapy. These patients remained in their intention-to-treat group for purpose of analysis.
The protocol was amended on May 15, 2020, to include patients with chronic kidney disease, based on an FDA general recommendation to COVID-19 clinical trials to consider inclusion of at-risk populations for severe illness. The study period was shortened to 15 days from the initial 29 days to allow enrolled patients with progressive illness to participate in other investigational trials without the need to withdraw from this study. Because of a shortage of SARS-CoV-2 PCR testing supplies, an amendment was added to allow enrollment of patients with a positive PCR test result before 72 h from the time of screening and clinical evidence of progressive disease. All subjects enrolled met the initial enrollment condition with a positive PCR test result within 72 h of screening. Protocol amendments were authorized and approved by the institutional review board and FDA.
Study patients were assessed daily for 15 days or until discharge, whichever came first. Discharged patients participated in phone or video study visits on days 7 and 15. Clinical assessment performed daily during hospitalization included evaluation of clinical status with daily vital signs, oxygen supplementation type and amount, need for mechanical ventilation, adverse events, and concomitant medications. WBCs, hemoglobin, platelets, electrolytes, BUN, creatinine, liver transaminases, and inflammatory markers, if obtained as part of SOC, were monitored on days 1 through 5, 7, and 15 while patients were hospitalized. Serum free and total progesterone levels were also measured on days 1 through 5. Self-reported race and ethnicity, obtained from medical records, were collected as demographic information to assess possible differences in disease severity or treatment response. Serious adverse events and grade 3 and 4 adverse events as described in the Division of AIDS Table for Grading the Severity of Adult and Pediatric Adverse Events were recorded.
Clinical status was assessed on a seven-point ordinal scale, similarly used by Goldman et al,32 as follows: 1, death; 2, hospitalized, on invasive mechanical ventilation or extracorporeal membrane oxygenation (ECMO); 3, hospitalized, on high-flow oxygen devices; 4, hospitalized, requiring supplemental oxygen; 5, hospitalized, not requiring supplemental oxygen; 6, not hospitalized, limitation on activities; and 7, not hospitalized, no limitations on activities. If the clinical status of a hospitalized patient changed on any given study day, the patient’s worst clinical assessment score on the ordinal scale was documented.
End Point
In addition to safety and tolerability, the primary efficacy end point was change in patients’ clinical status, assessed on a seven-point ordinal scale, from baseline to day 7. Secondary end points were hospital length of stay (LOS), days of supplemental oxygen use, and need for mechanical ventilation.
Statistical Analysis
Parameter estimates from this study will be used to power a definitive study. A sample size of 20 per group (total sample size, 40) was deemed adequate to provide this estimation.
Differences between groups in primary end points were tested with an exact Wilcoxon rank-sum test with exact Hodges-Lehmann confidence limits calculated for the median shift between groups. The cumulative probability of improvement in clinical status (an increase of at least one point on a seven-point scale or live discharge) over the first 7 days was estimated by the Kaplan-Meier method, and differences across the study groups were assessed by a log-rank test. To compare LOS and duration of supplemental oxygen between groups, a separate competing-risk analysis was performed with death as a competing outcome, and data were censored when time exceeded the study end point at 15 days.33 , 34 Other measures were tested by Student t-test (parametric data) or Fisher exact test (categorical data) where appropriate. Inferential tests were considered significant when the two-tailed P value was < .05, although adjustments for multiplicity were not made because of the exploratory nature of this pilot study. Analysis was performed on an intent-to-treat basis, using SAS version 9.4 software (SAS Institute).
Post Hoc Analyses
Because several patients in both groups experienced clinical deterioration over days 2 through 6 a sensitivity analysis was performed, considering the patients’ worst status before day 7 as their baseline to capture the illness severity while assessing the change in clinical status score between the two groups. In another sensitivity analysis, for control patients who crossed over before day 7, their last clinical assessment before receiving progesterone was imputed as the day 7 assessment.
Results
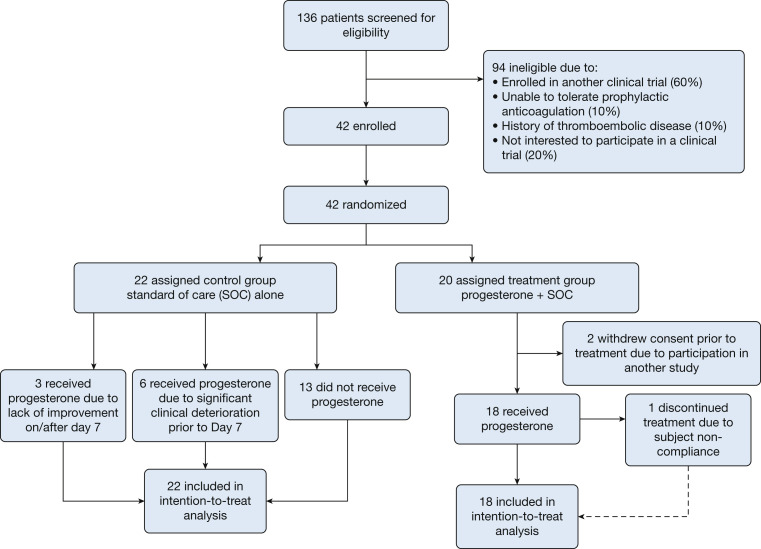
Between April 27 and August 5, 2020, 136 patients were screened and assessed for eligibility; 94 were deemed ineligible for the study. Of the 42 enrolled patients, 20 were randomized to the progesterone group and 22 to the control group. The trial completed enrollment, and the final follow-up for the last enrollee was on August 20, 2020. Two patients in the progesterone group withdrew from the study before receiving progesterone and were excluded from analysis (Fig 1 ). Nine control patients were treated with progesterone because of clinical deterioration before day 7 (n = 6, 27%) or absence of clinical improvement by day 7 (n = 3, 14%). One patient assigned to the progesterone group was repeatedly protocol-noncompliant and was transferred to another hospital on day 5 for insurance coverage reasons. For the purpose of safety evaluation, follow-up revealed that this patient died on day 7 of complications from disseminated cryptococcal infection in the setting of untreated HIV infection. All available data on this patient as obtained on days 1 through 5 of the study and clinical status on day 7 have been included in the analysis.
Figure 1.
Participant flow in a randomized clinical trial of progesterone vs standard of care in men with moderate to severe COVID-19.
Because enrollment was faster than anticipated, the trial terminated recruitment soon after the interim safety analysis. After discussion with the data safety monitoring committee, further interim analyses were deemed unnecessary.
Demographics and baseline characteristics of the study population were balanced in the two study groups (Table 2 and e-Table 3). The patient population had an overall mean age of 55.3 ± 16.4 years and a mean BMI of a 31.6 ± 9.5 kg/m2. Self-reported race and ethnicity indicated that most were white (78%) and Hispanic (60%). Most patients had comorbid conditions including hypertension, diabetes, obesity, or a combination of these. At baseline, there was no statistically significant difference in clinical status between the two groups with 85% of all patients requiring supplemental oxygen.
Table 2.
Baseline Characteristics
| Characteristic | All Subjects (N = 40) | Progesterone Group (n = 18) | Control Group (n = 22) |
|---|---|---|---|
| Age, mean ± SD, y | 55.3 ± 16.4 | 56.0 ± 17.3 | 54.6 ± 16.0 |
| Baseline BMI, mean ± SD, kg/m2 | 31.6 ± 9.5 | 31.9 ± 11.1 | 31.4 ± 8.3 |
| Race, No. (%) | |||
| White | 31 (77.5) | 12 (66.7) | 19 (86.4) |
| Black/African American | 4 (10.0) | 2 (11.1) | 2 (9.1) |
| Asian/Pacific Islander | 2 (5.0) | 1 (5.6) | 1 (4.5) |
| Other | 3 (7.5) | 3 (16.7) | 0 (0.0) |
| Ethnicities, No. (%) | |||
| Hispanic or Latino | 24 (60.0) | 10 (55.6) | 14 (63.6) |
| Not Hispanic or Latino | 16 (40.0) | 8 (44.4) | 8 (36.4) |
| Comorbidities, No. (%) | |||
| Hypertension | 19 (47.5) | 7 (38.9) | 12 (54.5) |
| Diabetes | 10 (25.0) | 4 (22.2) | 6 (27.3) |
| Obesity | 18 (45.0) | 6 (33.3) | 12 (54.5) |
Primary End Point
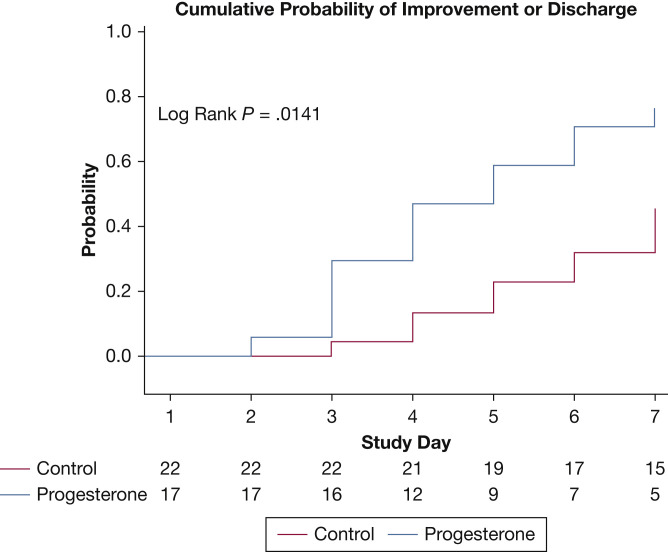
The primary outcome, ascertained as the overall change in clinical score status from baseline to day 7 on a seven-point ordinal scale, was a median of 1.5 points better for the progesterone group than the control group (95% CI, 0.0-2.0; P = .024) (Table 3 ). During the first seven study days, the cumulative probability of clinical improvement (an increase of at least one point on a seven-point scale or live discharge) was significantly higher in the progesterone group, 0.76 (95% CI, 0.55-0.93) vs 0.55 (95% CI, 0.28-0.68) in the control group (log-rank P = .014), by Kaplan-Meier estimation. One patient in the progesterone group showed improvement on day 2 but was subsequently noncompliant with study protocols and was transferred to another facility. For the purpose of this Kaplan-Meier estimation, this subject was excluded (Fig 2 ).
Table 3.
Clinical Status Based on Seven-Point Ordinal Scale
| Clinical Status | Progesterone Group (n = 18) [No. (%)] | Control Group (n = 22) [No. (%)] | P Valuea |
|---|---|---|---|
| Status at baseline, No. (%) | |||
| 3: Hospitalized; on high-flow nasal cannula | 3 (16.7) | 0 (0.0) | |
| 4: Hospitalized; requiring supplemental oxygen (not HFNC) | 11 (61.1) | 20 (90.9) | |
| 5: Hospitalized; not requiring supplemental oxygen | 4 (22.2) | 2 (9.1) | |
| Status on day 7, No. (%) | |||
| 1: Death | 1 (5.6) | 0 (0.0) | |
| 2: Hospitalized; on invasive mechanical ventilation or ECMO | 0 (0.0) | 3 (13.6) | |
| 3: Hospitalized; on high-flow nasal cannula | 2 (11.1) | 3 (13.6) | |
| 4: Hospitalized; requiring supplemental oxygen (not HFNC) | 2 (11.1) | 8 (36.4) | |
| 5: Hospitalized; not requiring supplemental oxygen | 4 (22.2) | 4 (18.2) | |
| 6: Not hospitalized; limitations on activities | 7 (38.9) | 4 (18.2) | |
| 7: Not hospitalized; no limitations on activities | 2 (11.1) | 0 (0.0) | |
| Change in status on day 7, No. (%) | |||
| +3 | 2 (11.1) | 0 (0.0) | |
| +2 | 7 (38.9) | 3 (13.6) | |
| +1 | 3 (16.7) | 4 (18.2) | |
| 0 | 3 (16.7) | 9 (40.9) | |
| –1 | 2 (11.1) | 3 (13.6) | |
| –2 | 0 (0.0) | 3 (13.6) | |
| –3 | 1 (5.6) | 0 (0.0) | |
| Change in status on day 7, median (IQR) | 1.5 (0.0 to 2.0) | 0.0 (–1.0 to 1.0) | .024 |
| Status on day 15, No. (%) | |||
| 1: Death | 1 (5.6) | 1 (4.5) | |
| 2: Hospitalized; on invasive mechanical ventilation or ECMO | 0 (0.0) | 2 (9.1) | |
| 3: Hospitalized; on high-flow nasal cannula | 0 (0.0) | 2 (9.1) | |
| 4: Hospitalized; requiring supplemental oxygen (not HFNC) | 1 (5.6) | 0 (0.0) | |
| 5: Hospitalized; not requiring supplemental oxygen | 1 (5.6) | 1 (4.5) | |
| 6: Not hospitalized; limitations on activities | 8 (44.4) | 12 (54.5) | |
| 7: Not hospitalized; no limitations on activities | 7 (38.9) | 4 (18.2) | |
| Change in status on day 15, No. (%) | |||
| +4 | 1 (5.6) | 0 (0.0) | |
| +3 | 7 (38.9) | 2 (9.1) | |
| +2 | 4 (22.2) | 14 (63.6) | |
| +1 | 4 (22.2) | 1 (4.5) | |
| 0 | 1 (5.6) | 0 (0.0) | |
| –1 | 0 (0.0) | 2 (9.1) | |
| –2 | 0 (0.0) | 2 (9.1) | |
| –3 | 1 (5.6) | 1 (4.5) | |
| Change in status on day 15, median (IQR) | 2.0 (1.0 to 3.0) | 2.0 (1.0 to 2.0) | .150 |
ECMO = extracorporeal membrane oxygenation; HFNC = high-flow nasal cannula; IQR = interquartile range.
Exact Wilcoxon rank-sum test.
Figure 2.
Cumulative probability of improvement or discharge on day 7. During the first seven study days, the cumulative probability of clinical improvement (an increase of at least one point on the seven-point scale or live discharge) was significantly higher in the progesterone group, 0.76 (95% CI, 0.55-0.93) vs 0.55 (95% CI, 0.28-0.68) in the control group (log-rank P = .014), by Kaplan-Meier estimation. One patient in the progesterone group showed improvement on day 2 but was subsequently noncompliant with study protocols and was transferred to another facility. For the purpose of this analysis, this patient was excluded.
Post Hoc Analyses
In a sensitivity analysis comparing worst clinical status before day 7 with clinical status on day 7, the progesterone group improved a median of two points more than the control group (95% CI, 1.0-2.0; P = .006) (e-Table 4). This analysis captures the illness severity while assessing the change in clinical status score between the two groups; again favoring the progesterone group.
In a sensitivity analysis in which the last clinical assessment on the seven-point ordinal scale before crossing over was imputed as the day 7 score, overall change in score from baseline to day 7 was a median of 1.5 points better for the progesterone group than the control group (95% CI, 0.0-2.0; P = .010) (e-Table 5).
Secondary End Points and Adverse Events
Among patients assigned to the progesterone group, the median number of days on supplemental oxygen was 4.5 (IQR, 2.0-6.0) compared with 7.5 (IQR, 6.0-11.0) in the control group, for a median difference of 3 days. By day 7, nine of 18 patients (50%) in the progesterone group remained hospitalized, compared with 19 of 22 patients (86%) in the control group. Patients in the progesterone group had a median LOS of 7.0 days (IQR, 4.0-9.0) whereas the control group had a median LOS of 9.5 days (IQR, 7.0-14.0). At study completion, one patient in the progesterone group remained hospitalized compared with five in the control group. Mechanical ventilation was initiated in four of 22 control patients (18%), three before day 7, compared with none in the progesterone group. Although we see evidence of improved clinical outcomes in patients receiving progesterone, with fewer days of hospitalization, and less need for supplemental oxygen or mechanical ventilation, differences between groups did not meet conventional levels of statistical significance.
Although the patients were analyzed on an intent-to-treat basis, notably one-half of the six control patients who crossed over because of clinical deterioration before day 7 progressed to require mechanical ventilation. Of those, one was successfully liberated from the ventilator before completion of the study. The remaining one-half of crossed-over patients (n = 3), despite a clear trajectory of decline, did not require mechanical ventilation and improved to discharge before completion of the study.
Administration of expanded-use access and other medications was allowed for both the control and intervention groups (Table 1 and e-Table 2). A larger percentage of the control group received remdesivir, systemic glucocorticoids, tocilizumab, and convalescent plasma, but these differences were not significant. A greater proportion but equal number of patients in the intervention arm received azithromycin, although this was also not significant.
There were no serious adverse events, including life-threatening events, attributable to progesterone. There were two thromboembolic events in one patient (5.6%) in the progesterone group and two thromboembolic events in two patients (9.1%) in the control group (Table 4 ). Overall, there was no meaningful difference in the incidence of serious adverse events between the two groups. There were two deaths, one in each group, during the total 15-day surveillance period, neither attributable to progesterone administration. There were no events requiring discontinuation of progesterone. For the control patients who crossed over, significant adverse events after progesterone administration are also listed in Table 4. Nonserious grade 3 and 4 adverse events are listed in e-Table 6.
Table 4.
Serious Adverse Events by System Organ Class and Preferred Term
| SAE | Progesterone Group (n = 18) [No. (%)] | Control Group (n = 22) [No. (%)] | Control Group After Progesteronea (n = 9) [No. (%)] |
|---|---|---|---|
| Any SAE or death | 2 (11.1) | 5 (22.7) | 3 (33.3) |
| Blood and lymphatic system disorders | |||
| Lymphocyte count decreased | 0 (0.0) | 1 (4.5) | 0 (0.0) |
| Cardiac disorders | |||
| Cardiac arrest | 0 (0.0) | 1 (4.5) | 0 (0.0) |
| Hypoperfusion | 0 (0.0) | 3 (13.6) | 2 (22.2) |
| Renal and urinary disorders | |||
| Creatinine increased | 0 (0.0) | 1 (4.5) | 0 (0.0) |
| Respiratory, thoracic, and mediastinal disorders | |||
| Hypoxia | 0 (0.0) | 4 (18.2) | 3 (33.3) |
| Vascular disorders | |||
| DVT | 1 (5.6) | 2 (9.1) | 1 (11.1) |
| Pulmonary embolism | 1 (5.6) | 0 (0.0) | 0 (0.0) |
| Death | 1 (5.6) | 1 (4.5) | 0 (0.0) |
SAE = serious adverse event.
For control patients who received progesterone due to clinical deterioration, this column represents SAEs that occurred after receiving progesterone.
Serum progesterone levels were obtained at baseline and, as anticipated, were less than 1 ng/mL in all patients. After administration of two doses of subcutaneous progesterone, goal serum levels were achieved and maintained between 11.1 and 288 ng/mL on subsequent samples. Levels as high as 288 ng/mL, which can be seen during the third trimester of pregnancy,35 were tolerated well and not associated with any adverse events.
Discussion
The current pilot study results suggest that the use of progesterone, in addition to SOC treatment measures in hospitalized men with COVID-19 who are hypoxemic, could lead to improved clinical outcomes with minimal safety concerns. We noted that addition of progesterone to SOC treatment was associated with improved clinical status assessed on a seven-point ordinal scale, a trend toward fewer days on supplemental oxygen, reduced need for mechanical ventilation, and reduced length of hospital stay.
The sex difference in illness severity and mortality outcomes in COVID-19, as well as in prior coronavirus outbreaks, has been demonstrated in multiple populations.2, 3, 4, 5, 6, 7 The concept of a less effective immune response to viral infections as a consequence of differences in sex hormones between men and women has been described previously and may be related to unequal endogenous progesterone levels, a steroid hormone with well-described antiinflammatory properties.11 , 17 , 19 , 21, 22, 23, 24 The corpus luteum produces progesterone in women with peak levels (10-20 ng/mL) during the luteal phase of the menstrual cycle.36 Adrenal glands and testes produce progesterone in men, but at much lower concentrations (0.13-0.97 ng/mL), similar to those of postmenopausal women.36, 37, 38 The role of progesterone extends beyond fertility and menstruation. It binds to glucocorticoid receptors, and indeed most immune cells express progesterone receptors.17 It is possible that higher endogenous levels of progesterone protect women from progressing to severe illness in COVID-19.
A major driver of morbidity and mortality in COVID-19 is the exuberant inflammatory response, sometimes termed a “cytokine storm,” mediated by production of proinflammatory cytokines (IL-6, IL-1β, tumor necrosis factor-α) and macrophage hyperactivation.25 , 26 Previous preclinical and clinical studies have demonstrated that the elevated concentrations of estrogen and progesterone in women are associated with inflammatory response attenuation through IL-1β and IL-12 inhibition, decreased T-cell IL-6 receptor expression, and a bias toward helper T-cell type 2 production, which secrete IL-4, IL-5, IL-10, and other antiinflammatory cytokines.24 , 39, 40, 41 Exogenous progesterone administration in mice infected with influenza A showed enhanced repair of pulmonary epithelial cells, supporting a role for this steroid hormone in reducing inflammation and promoting faster recovery.28 Although direct evidence of specific cytokine modulation is lacking in our study, the potential usefulness of progesterone in the treatment of early COVID-19 in men is compelling.
The progesterone dose of 100 mg injected subcutaneously was based on the previously demonstrated observation that a subcutaneous formulation, commercially available for use in fertility treatment outside the United States (FDA IND 102771), achieves rapid, reliable progesterone serum concentrations42 , 43 approximating the luteal phase of the menstrual cycle. We aimed to target a progesterone level between that of the luteal phase and pregnancy, the latter of which can be as high as 290 ng/mL.35 Although data on outcomes of pregnant women with COVID-19 remain inconclusive, some reports have suggested that the pulmonary disease in pregnant women may be comparable, if not milder, than in age-matched nonpregnant female control subjects.44 This may be partly due to decreased production of proinflammatory factors inherent in pregnancy.45 To maintain our target progesterone level, the dose was administered twice daily for up to 5 days. Daily serum measurements confirmed the rapid increase in and sustained levels of progesterone; as expected, levels ranged between those seen in the luteal phase of menstrual cycle and the third trimester of pregnancy.
A major concern about exogenous sex hormone administration is the development of thrombotic disease; particularly when coupled with a disease already known for its coagulopathic effects.46 This risk is most prominent in women who receive estrogen-containing contraceptives and appears to be most related to estrogen dose. In fact, progesterone-only contraceptives do not confer an increased risk of venous thromboembolic disease.47 Even IV progesterone, as used in phase 3 clinical trials of traumatic brain injury, was not associated with increased risk of thromboembolic disease.48 Nonetheless, all patients in our study received prophylactic-dose anticoagulation, as is recommended for hospitalized patients with COVID-19.49 We similarly observed that use of progesterone was safe overall and not associated with any significant increase in the risk of thromboembolism.
Limitations
This study was conducted at a large academic quaternary care medical center in the racially and ethnically diverse city of Los Angeles. Our study population was predominantly white, Hispanic, and obese, with a moderate burden of comorbidities associated with worse outcomes in COVID-19.2 Thus, the patients included in this analysis may represent those at higher risk for worse outcomes from COVID-19, which may limit the generalizability of this trial to other populations. Other limitations include the relatively small study population size, the fact that the study was unblinded, and that it was performed at a single site. Finally, with the rapidly changing climate of COVID-19 treatment approaches, patients’ receipt of other medications for COVID-19 varied somewhat over the course of the study (Table 1 and e-Table 2). These variations were similar in both groups and were not statistically significant; however, as progesterone is a steroid hormone, discerning its beneficial effect on immune modulation over that of systemic glucocorticoids is limited in this study. A further study will need to delineate the mechanism of action of progesterone and compare its efficacy with that of glucocorticoids in COVID-19.
Interpretation
This proof-of-concept pilot trial showed very encouraging outcome data, suggesting that administration of progesterone at a dose of 100 mg twice daily by subcutaneous injection may represent a safe and effective approach to the treatment of COVID-19 by improving the clinical status among men with moderate to severe illness. Further research is necessary in larger, more heterogeneous populations, including postmenopausal women and at other treatment centers, to establish the degree of clinical efficacy and to assess any other potential safety concerns of this treatment approach.
Take-home Points.
Study Question: Does the addition of subcutaneous progesterone in hypoxemic men with COVID-19 improve clinical outcomes?
Results: This study demonstrates that in men with COVID-19, the addition of progesterone for 5 days improves clinical status on day 7, reduces the need for supplemental oxygen, and reduces hospital length of stay with no significant adverse effects.
Interpretation: Addition of subcutaneous progesterone may represent a safe and novel approach to the treatment of hypoxemic men hospitalized with COVID-19.
Acknowledgments
Author contributions: S. G., Y. M., S. P., T. K., D. N., J. H., S. C., V. T., and M. L. take responsibility for all content of the manuscript, the integrity of the data, and the accuracy of the data analysis. Concept and design: S. G., Y. M., S. P., D. S., H. G., J. M., V. T., M. L.; acquisition, analysis, or interpretation of data: S. G., Y. M., S. P., D. S., T. K., D. N., J. H., S. C., C. B., R. G., H. G., J. M., V. T., M. L.; drafting of the manuscript: S. G., Y. M., S. P., D. S., T. K., D. N., J. H., S. C., R. G., H. G., C. B., J. M.; critical revision of the manuscript for important intellectual content: S. G., Y. M., D. S., R. G., V. T., M. L.; statistical analysis: H. G., C. B., J. M.; obtaining of funding: S. G.; regulatory compliance: S. G.
Financial/nonfinancial disclosures: The authors have reported to CHEST the following: S. G. and S. P. report patent pending on method of use of progesterone agonist for the treatment of COVID-19; V. T. reports grants from the NIH/NIAID ACTT [ACTT 1-3] outside the submitted work. None declared (Y. M., D. S., T. K., D. N., J. H., S. C., R. G., H. G., J. M., C. B., M. L.).
Role of sponsors: IBSA provided the study drug and provided partial financial support for this investigator-initiated study. IBSA did not oversee the study and has not participated in trial design, patient recruitment, data collection, analysis, interpretations, or preparation of this manuscript.
Other contributions: The authors thank the patients who altruistically participated in this randomized trial; Heather Jones, MD, and Darina Barnes, PharmD, for providing independent safety review; S. Ananth Karumanchi, MD, for guidance and review of the manuscript; members of the Cedars-Sinai Biobank for handling specimens; members of the Cedars-Sinai research pharmacy for dispensing the study drug; Vanessa Vasco and other members of the research team who coordinated the procedures and data entry; and members of the Cedars-Sinai IRB for reviewing and monitoring this trial at the Cedars-Sinai Medical Center.
Data-sharing statement: Requests for deidentified patient data should be sent to sara.ghandehari@cshs.org, beginning August 20, 2021. Data sharing will be considered, depending on the nature of the request, the merit of the research proposed, and the intended use of the data, and only with a signed data access agreement.
Additional information: The e-Appendix and e-Tables can be found in the Supplemental Materials section of the online article.
Footnotes
Drs Tapson and Lewis contributed equally to this article.
FUNDING/SUPPORT: This study was partially sponsored by Institut Biochimique SA (IBSA, Lugano, Switzerland). IBSA provided the study drug and partially supported this investigator-initiated study financially.
Supplementary Data
References
- 1.World Health Organization WHO Coronavirus Disease (COVID-19) Dashboard. 2020. https://covid19.who.int/
- 2.Richardson S., Hirsch J.S., Narasimhan M., et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City area. JAMA. 2020;323(20):2052–2059. doi: 10.1001/jama.2020.6775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Petrilli C.M., Jones S.A., Yang J., et al. Factors associated with hospital admission and critical illness among 5279 people with coronavirus disease 2019 in New York City: prospective cohort study. BMJ. 2020;369:m1966. doi: 10.1136/bmj.m1966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.GlobalHealth 50/50. The COVID-19 Sex-Disaggregated Data Tracker. 2020. https://globalhealth5050.org/the-sex-gender-and-covid-19-project
- 5.Guan W.J., Ni Z.Y., Hu Y., et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–1720. doi: 10.1056/NEJMoa2002032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Alkhouli M., Nanjundappa A., Annie F., Bates M.C., Bhatt D.L. Sex differences in case fatality rate of COVID-19: insights from a multinational registry. Mayo Clin Proc. 2020;95(8):1613–1620. doi: 10.1016/j.mayocp.2020.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Grasselli G., Zangrillo A., Zanella A., et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy region, Italy. JAMA. 2020;323(16):1574–1581. doi: 10.1001/jama.2020.5394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mosca L., Barrett-Connor E., Wenger N.K. Sex/gender differences in cardiovascular disease prevention: what a difference a decade makes. Circulation. 2011;124(19):2145–2154. doi: 10.1161/CIRCULATIONAHA.110.968792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ntritsos G., Franek J., Belbasis L., et al. Gender-specific estimates of COPD prevalence: a systematic review and meta-analysis. Int J Chron Obstruct Pulmon Dis. 2018;13:1507–1514. doi: 10.2147/COPD.S146390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clarke T.C., Norris T., Schiller J. Early Release of Selected Estimates Based on Data From the 2016 National Health Interview Survey. 2017. https://www.cdc.gov/nchs/data/nhis/earlyrelease/earlyrelease201705.pdf
- 11.Mauvais-Jarvis F., Klein S.L., Levin E.R. Estradiol, progesterone, immunomodulation, and COVID-19 outcomes. Endocrinology. 2020;161(9):bqaa127. doi: 10.1210/endocr/bqaa127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Haitao T., Vermunt J.V., Abeykoon J., et al. COVID-19 and sex differences: mechanisms and biomarkers. Mayo Clin Proc. 2020;95(10):2189–2203. doi: 10.1016/j.mayocp.2020.07.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ding T, Zhang J, Wang T, et al. Potential influence of menstrual status and sex hormones on female SARS-CoV-2 infection: a cross-sectional study from multicentre in Wuhan, China. Clin Infect Dis. 2021;72(9):e240-e248. [DOI] [PMC free article] [PubMed]
- 14.Dashraath P., Wong J.L.J., Lim M.X.K., et al. Coronavirus disease 2019 (COVID-19) pandemic and pregnancy. Am J Obstet Gynecol. 2020;222(6):521–531. doi: 10.1016/j.ajog.2020.03.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shah N.M., Lai P.F., Imami N., Johnson M.R. Progesterone-related immune modulation of pregnancy and labor. Front Endocrinol (Lausanne) 2019;10:198. doi: 10.3389/fendo.2019.00198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kovats S., Carreras E., Hemant A. In: Sex Hormones and Immunity to Infection. Klein S.L., Roberts C.W., editors. Springer; Berlin: 2010. Sex steroid receptors in immune cells; pp. 53–92. [Google Scholar]
- 17.Shields A.D., Wright J., Paonessa D.J., et al. Progesterone modulation of inflammatory cytokine production in a fetoplacental artery explant model. Am J Obstet Gynecol. 2005;193(3 Pt 2):1144–1148. doi: 10.1016/j.ajog.2005.05.046. [DOI] [PubMed] [Google Scholar]
- 18.Miller L., Hunt J.S. Regulation of TNF-α production in activated mouse macrophages by progesterone. J Immunol. 1998;160(10):5098–5104. [PubMed] [Google Scholar]
- 19.Par G., Geli J., Kozma N., Varga P., Szekeres-Bartho J. Progesterone regulates IL12 expression in pregnancy lymphocytes by inhibiting phospholipase A2. Am J Reprod Immunol. 2003;49(1):1–5. doi: 10.1034/j.1600-0897.2003.01149.x. [DOI] [PubMed] [Google Scholar]
- 20.Hall O.J., Klein S.L. Progesterone-based compounds affect immune responses and susceptibility to infections at diverse mucosal sites. Mucosal Immunol. 2017;10(5):1097–1107. doi: 10.1038/mi.2017.35. [DOI] [PubMed] [Google Scholar]
- 21.AbdulHussain G., Azizieh F., Makhseed M., Raghupathy R. Effects of progesterone, dydrogesterone and estrogen on the production of Th1/Th2/Th17 cytokines by lymphocytes from women with recurrent spontaneous miscarriage. J Reprod Immunol. 2020;140:103132. doi: 10.1016/j.jri.2020.103132. [DOI] [PubMed] [Google Scholar]
- 22.Buyon J.P., Korchak H.M., Rutherford L.E., Ganguly M., Weissmann G. Female hormones reduce neutrophil responsiveness in vitro. Arthritis Rheum. 1984;27(6):623–630. doi: 10.1002/art.1780270604. [DOI] [PubMed] [Google Scholar]
- 23.Hudic I., Fatusic Z., Szekeres-Bartho J., et al. Progesterone-induced blocking factor and cytokine profile in women with threatened pre-term delivery. Am J Reprod Immunol. 2009;61(5):330–337. doi: 10.1111/j.1600-0897.2009.00699.x. [DOI] [PubMed] [Google Scholar]
- 24.Piccinni M.P., Giudizi M.G., Biagiotti R., et al. Progesterone favors the development of human T helper cells producing Th2-type cytokines and promotes both IL-4 production and membrane CD30 expression in established Th1 cell clones. J Immunol. 1995;155(1):128–133. [PubMed] [Google Scholar]
- 25.Chen G., Wu D., Guo W., et al. Clinical and immunological features of severe and moderate coronavirus disease 2019. J Clin Invest. 2020;130(5):2620–2629. doi: 10.1172/JCI137244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ye Q., Wang B., Mao J. The pathogenesis and treatment of the “cytokine storm” in COVID-19. J Infect. 2020;80(6):607–613. doi: 10.1016/j.jinf.2020.03.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tzotzos S.J., Fischer B., Fischer H., Zeitlinger M. Incidence of ARDS and outcomes in hospitalized patients with COVID-19: a global literature survey. Crit Care. 2020;24(1):516. doi: 10.1186/s13054-020-03240-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hall O.J., Limjunyawong N., Vermillion M.S., et al. Progesterone-based therapy protects against influenza by promoting lung repair and recovery in females. PLoS Pathog. 2016;12(9) doi: 10.1371/journal.ppat.1005840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.National Institutes of Health Clinical Center Progesterone for the treatment of COVID-19 in hospitalized men. NCT04365127. ClinicalTrials.gov. Bethesda, MD: National Institutes of Health; 2020. https://clinicaltrials.gov/ct2/show/NCT04365127 Updated January 27, 2021.
- 30.Harris P.A., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Harris P.A., Taylor R., Minor B.L., et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208. doi: 10.1016/j.jbi.2019.103208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Goldman J.D., Lye D.C.B., Hui D.S., et al. Remdesivir for 5 or 10 days in patients with severe Covid-19. N Engl J Med. 2020;383(19):1827–1837. doi: 10.1056/NEJMoa2015301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Brock G.N., Barnes C., Ramirez J.A., Myers J. How to handle mortality when investigating length of hospital stay and time to clinical stability. BMC Med Res Methodol. 2011;11:144. doi: 10.1186/1471-2288-11-144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Fine J.P., Gray R.J. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc. 1999;94(446):496–509. [Google Scholar]
- 35.Fischbach FT, Dunning MB III, eds. Manual of Laboratory and Diagnostic Tests, 8th ed. Lippincott Williams and Wilkins; 2009.
- 36.Tea N.T., Castanier M., Roger M., Scholler R. Simultaneous radioimmunoassay of plasma progesterone and 17-hydroxyprogesterone normal values in children, in men and in women throughout the menstrual cycle and in early pregnancy. J Steroid Biochem. 1975;6(11-12):1509–1516. doi: 10.1016/0022-4731(75)90206-x. [DOI] [PubMed] [Google Scholar]
- 37.Muneyyirci-Delale O., Dalloul M., Nacharaju V.L., Altura B.M., Altura B.T. Serum ionized magnesium and calcium and sex hormones in healthy young men: importance of serum progesterone level. Fertil Steril. 1999;72(5):817–822. doi: 10.1016/s0015-0282(99)00386-6. [DOI] [PubMed] [Google Scholar]
- 38.Burtis C.A., Ashwood A.R. 3rd ed. Saunders; Philadelphia: 1999. Tietz Textbook of Clinical Chemistry. [Google Scholar]
- 39.Klein S.L., Flanagan K.L. Sex differences in immune responses. Nat Rev Immunol. 2016;16(10):626–638. doi: 10.1038/nri.2016.90. [DOI] [PubMed] [Google Scholar]
- 40.Szekeres-Bartho J., Wegmann T.G. A progesterone-dependent immunomodulatory protein alters the Th1/Th2 balance. J Reprod Immunol. 1996;31(1-2):81–95. doi: 10.1016/0165-0378(96)00964-3. [DOI] [PubMed] [Google Scholar]
- 41.Szekeres-Bartho J., Faust Z., Varga P., Szereday L., Kelemen K. The immunological pregnancy protective effect of progesterone is manifested via controlling cytokine production. Am J Reprod Immunol. 1996;35(4):348–351. doi: 10.1111/j.1600-0897.1996.tb00492.x. [DOI] [PubMed] [Google Scholar]
- 42.Cometti B. Pharmaceutical and clinical development of a novel progesterone formulation. Acta Obstet Gynecol Scand. 2015;94(suppl 161):28–37. doi: 10.1111/aogs.12765. [DOI] [PubMed] [Google Scholar]
- 43.Doblinger J., Cometti B., Trevisan S., Griesinger G. Subcutaneous progesterone is effective and safe for luteal phase support in IVF: an individual patient data meta-analysis of the phase III trials. PLoS One. 2016;11(3) doi: 10.1371/journal.pone.0151388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Qiancheng X., Jian S., Lingling P., et al. Coronavirus disease 2019 in pregnancy. Int J Infect Dis. 2020;95:376–383. doi: 10.1016/j.ijid.2020.04.065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Robinson D.P., Klein S.L. Pregnancy and pregnancy-associated hormones alter immune responses and disease pathogenesis. Horm Behav. 2012;62(3):263–271. doi: 10.1016/j.yhbeh.2012.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McFadyen J.D., Stevens H., Peter K. The emerging threat of (micro)thrombosis in COVID-19 and its therapeutic implications. Circ Res. 2020;127(4):571–587. doi: 10.1161/CIRCRESAHA.120.317447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Lidegaard O., Lokkegaard E., Svendsen A.L., Agger C. Hormonal contraception and risk of venous thromboembolism: national follow-up study. BMJ. 2009;339:b2890. doi: 10.1136/bmj.b2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Wright D.W., Yeatts S.D., Silbergleit R., et al. Very early administration of progesterone for acute traumatic brain injury. N Engl J Med. 2014;371(26):2457–2466. doi: 10.1056/NEJMoa1404304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Barnes G.D., Burnett A., Allen A., et al. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis. 2020;50(1):72–81. doi: 10.1007/s11239-020-02138-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.