Abstract
Objectives
This study describes the utilization of a pediatric emergency department (ED) during the early months of the COVID-19 pandemic in the initial U.S. epicenter, including the impact on visit acuity and incidences of common diagnoses.
Study Design
We performed an observational retrospective review of patients younger than 18 years old seen in a New York City pediatric ED from March 7th to May 6th 2020, and during the same time period in 2018 and 2019. Demographics, visit details, diagnoses, and dispositions were compared. Validated algorithms were utilized to create practical diagnosis groupings and to determine the probability of a visit requiring emergent evaluation.
Results
ED visits during the pandemic decreased by 56% to an average daily census of 67 patients, from an anticipated 152. Admission rates rose from 13.3% to 17.4% (p<0.001), and the proportion of triage Emergency Severity Index level 1 and 2 patients increased by 23.7% (p<0.001). Non-emergent visits dropped from 32.3% to 27.5% (p<0.001). Several common, often low-acuity diagnoses saw disproportionate reductions in visits including headache, chest pain, and minor injuries. Concerningly, visits for suicidal ideation, suicide attempt, or self-harm increased by 100% (p<0.001) and visits for evaluating abuse or neglect decreased by 89% (p=0.01).
Conclusions
Pediatric ED utilization substantially deceased during the early months of the COVID-19 pandemic in New York City, but left relatively higher patient acuity. Healthcare systems in early epicenters must also prepare for the disproportionate impact a pandemic has on the most vulnerable pediatric patients, particularly those at risk for self-harm or abuse.
Keywords: Coronavirus, SARS-CoV-2, Volume, Acuity, Incidence, Suicide, Behavioral health, Abuse
Abbreviations: CCSR, Clinical Classification Software Refined; ED, Emergency Department; EMS, Emergency Medical Services; ESI, Emergency Severity Index; ICD-10-CM, International Classification of Diseases 10th Revision, Clinical Modification; ICU, Intensive Care Unit; LOS, Length of Stay; MERS, Middle East Respiratory Syndrome; NY, New York; NYC, New York City; PICU, Pediatric Intensive Care Unit; SARS, Severe Acute Respiratory Syndrome
1. Introduction
Soon after the first patient in New York City (NYC) was diagnosed with the coronavirus disease of 2019 (COVID-19), the number of confirmed cases in New York State (NYS) skyrocketed with NYC being labeled the national epicenter of the pandemic [1]. State and city attempts to harness resources and stem the tide of infections escalated over the initial weeks, including a “NY on PAUSE” order limiting travel, business, and public gatherings.
Adult healthcare systems faced unparalleled challenges in patient volume and acuity [[2], [3], [4], [5]]. However, in line with prior coronavirus epidemics such as the 2003 Severe Acute Respiratory Syndrome (SARS) [6,7] and the 2014 Middle East Respiratory Syndrome (MERS) [8] epidemics, pediatric emergency departments (ED's) seemed to have been spared the same influx of patients [[9], [10], [11], [12]]. Studies published to date in the U.S. have reported widespread reductions in pediatric volumes (59%–67%) and increases in acuity [[13], [14], [15], [16]]. Notably though, the multicenter studies in the literature have overwhelmingly examined general ED's rather than dedicated pediatric centers which have a higher proportion of medically complex pediatric patients [17]. Additionally, the studies to date consider a span of timepoints and a span of locations under varying levels of public health restrictions, but none focus on early epicenters of the U.S. pandemic. The largest study by Hartnett et al. [13] did not include data from NYC while another study acknowledged as a limitation the low prevalence of COVID-19 in its location [18]. From an epidemiological and system preparedness standpoint, it is important to understand how the “first-wave” of a pandemic, as experienced in NYC where there were public health restrictions and high community illness, will impact a pediatric healthcare system.
It was hypothesized that as a consequence of the increased isolation of children under the “NY on PAUSE” order, the prevalence of certain diagnoses would be more affected than others. This was particularly expected for various infectious illnesses, though Sheridan et al. [19] also described decreased pediatric ED visits for psychiatric complaints. It is unclear if these patterns hold true in a community with high disease prevalence.
By understanding the acuity and the pathology that present in the initial months of an active pandemic, we may prepare a healthcare system for pediatric resource needs during a future event. That includes identifying the most vulnerable pediatric populations and developing innovative methods for providing them care. This study examines the effect the COVID-19 pandemic had on the demographics, diagnoses, and acuity seen by a pediatric ED in the first U.S. epicenter.
2. Methods
2.1. Settings and subjects
We conducted an observational, retrospective natural experiment study surrounding the COVID-19 pandemic in NYC. The pediatric ED at the focus of this study is located in the NYC borough of Queens, considered part of the initial epicenter of the U.S. COVID-19 pandemic and serving communities prominently effected by governmental and self-imposed restrictions. It is a dedicated pediatric ED within a tertiary care children's hospital with a Level-1 pediatric trauma designation, caring for over 55,000 patients annually. The study period began March 7th, 2020, the day NYS announced a State of Emergency, and continued for two months until May 6th, 2020.
This study was approved by the Northwell Health Institutional Review Board and the Northwell Health COVID-19 Research Consortium.
2.2. Data collection
All patients younger than 18 years old evaluated in the pediatric ED during the study period in 2020 were identified and included (“COVID”). We also identified all patients younger than 18 years old evaluated in the pediatric ED during the same period in 2018 and 2019 (“Pre-COVID”), to serve as a proxy for what was anticipated absent the pandemic. Information regarding demographics, mode of arrival, triage information, primary diagnosis, length of stay and disposition were collected through routinely created hospital analytic reports. Data missing from these reports was manually collected through a chart review.
2.3. Acuity, urgency, and burden of illness
We used several variables to assess for patient acuity and burden of illness. One such tool is the Emergency Severity Index (ESI) triage tool [20], which is a common five-level ED triage stratification assigning patients level 1 (most urgent) to 5 (least urgent) on the basis of acuity and anticipated resource needs. We also classified visits as emergent and non-emergent using the NYU-ED Algorithm [21] developed by the New York University Center for Health and Public Service Research. This validated tool uses International Classification of Diseases 10th Revision, Clinical Modification (ICD-10-CM) diagnosis codes to estimate the probability of an ED visit requiring emergent medical care within 12 h. The algorithm does not categorize the urgency of visits related to alcohol use, substance abuse, injuries, or mental health as well as other diagnoses the developers felt were not prevalent enough to confidently designate as emergent or not. Disposition of patients was also used as a surrogate measure of acuity.
2.4. Diagnosis groupings
Based on a patient's primary ICD-10-CM code, visits were stratified into practical diagnosis groups using the Healthcare Cost and Utilization Project's Clinical Classification Software Refined (CCSR), version 2020.2 [22], which categorizes the over 70,000 ICD-10-CM codes into established groupings. The authors pre-selected several groupings for further analysis as they were felt to either represent a substantial percentage of ED visits, be of particular clinical interest, or anecdotaly affected by the pandemic. Several infectious diagnoses such as “Fever” and “Upper Respiratory Infection”, though common, were not selected for further analysis to avoid confounding by potential COVID-19 positive patients who were not tested.
2.5. COVID-19 patients
During the early study period, the ability to test all suspected patients for COVID-19 was severely limited and patients diagnosed with COVID-19 likely underrepresented the number of COVID-19 patients evaluated [23]. As such, for the purposes of the CCSR diagnosis groupings, COVID-19 was recoded as ‘Viral Infection’, and for the NYU-ED Algorithm it was left as unclassified.
2.6. Statistical analysis
When comparing patient visits from the COVID and Pre-COVID periods, categorical values were compared using Fisher's exact test. Continuous values and comparison of means were evaluated using 2-tailed unpaired t-tests for both parametric and non-parametric data due to the large sizes [24]. Mean values are described with standard deviation while proportions are described with 95% confidence intervals. Statistical significance was designated at p of 0.05. Statistical analyses were performed using SPSS 25 (IBM Inc., Armonk, NY, USA).
3. Results
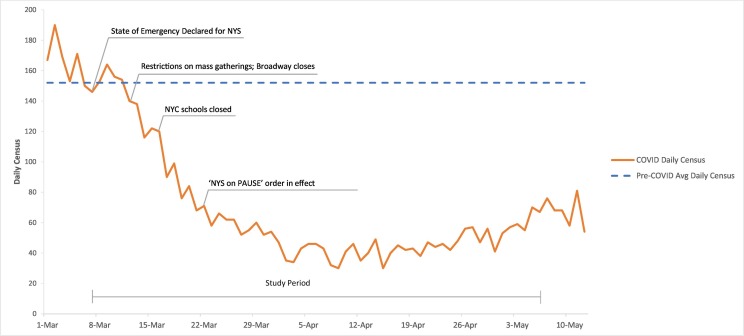
During the study period (COVID), there were 4068 patient visits in the pediatric ED, with an average daily census of 67 patients (range 30–164) (Fig. 1 ). This was 56.1% fewer visits than anticipated (9256 expected visits with a Pre-COVID average daily census of 152, range 102–206). Demographic information for visits during the COVID period and Pre-COVID period is shown in Table 1 . Mean age was not significantly different, though there were slight but statistically significant changes in age groups (p < 0.001) marked by a greater proportion of infants and adolescents compared to Pre-COVID. Table 2 displays assessments of acuity and illness burden. During the pandemic, the highest acuity ESI level 1 and 2 patients made up 18.8% of visits, compared to 15.2% of patients Pre-COVID (p < 0.001). The proportion of non-emergent visits had a 14.6% relative decrease from 32.3% of visits to 27.5% of visits (p < 0.001).
Fig. 1.
Average daily census. Study Period includes March 7th to May 6th. The solid line marks the daily census from the first reported COVID-19 case in NYS to six days after the COVID study period. The dashed line marks the average daily census during the Pre-COVID period.
Table 1.
Demographics
| Pre-COVID (2018/19) |
COVID (2020) |
P-value | |
|---|---|---|---|
| % (n = 18,513) | % (n = 4068) | ||
| Age, mean (SD) | 7.3 years (5.5) | 7.1 years (5.8) | 0.07 |
| Age group (years), (%) | <0.001 | ||
| <1 | 12.5% (2319) | 16.2% (658) | |
| 1–5 | 36.6% (6780) | 36.6% (1487) | |
| 6–12 | 29.9% (5536) | 24.7% (1003) | |
| 13–17 | 20.9% (3878) | 22.6% (920) | |
| Gender, Male (%) | 54.0% (9997) | 53.2% (2164) | 0.36 |
| Race (%)a | <0.001 | ||
| White/Caucasian | 27.0% (4991) | 25.3% (1029) | |
| Black/African American | 25.6% (4741) | 22.1% (897) | |
| Asian | 15.6% (2887) | 14.3% (580) | |
| Other/Multiracial | 30.0% (5562) | 34.8% (1414) | |
| Unknown/Declined | 1.8% (332) | 3.6% (148) | |
| Ethnicity (%)a | 0.038 | ||
| Hispanic | 18.1% (3342) | 19.5% (793) | |
| Non-Hispanic | 78.9% (14607) | 77.9% (3170) | |
| Unknown/Declined | 3.0% (564) | 2.6% (105) | |
| Insurance (%) | <0.001 | ||
| Private | 41.0% (7590) | 39.7% (1615) | |
| Public | 53.1% (9838) | 56.4% (2296) | |
| Self-pay/Uninsured | 5.9% (1085) | 3.9% (157) |
Self-reported.
Table 2.
ED Burden of Severity and Acuity
| Pre-COVID |
COVID |
P-value | |
|---|---|---|---|
| % (n) | % (n) | ||
| Mode of Arrival | <0.001 | ||
| Walk-In | 85.8% (15875) | 84.5% (3439) | |
| EMS/Transport | 13.7% (2532) | 15.5% (629) | |
| Unknown | 0.6% (106) | 0.0% (0) | |
| ESI | <0.001 | ||
| 1 | 0.4% (69) | 0.2% (9) | |
| 2 | 14.8% (2743) | 18.6% (756) | |
| 3 | 39.2% (7262) | 37.9% (1543) | |
| 4 | 39.7% (7349) | 38.4% (1564) | |
| 5 | 5.9% (1090) | 4.8% (196) | |
| Disposition | <0.001 | ||
| Transfer | 0.4% (68) | 0.5% (21) | |
| Discharge | 86.3% (15975) | 82.1% (3339) | |
| Admission | 13.3% (2470) | 17.4% (708) | |
| Admit-Medical/Surgical | 9.5% (1756) | 12.5% (510) | |
| Admit-PICU | 2.3% (423) | 2.6% (104) | |
| Admit-OR | 1.0% (178) | 1.4% (57) | |
| Admit-Psychiatry | 0.6% (113) | 0.9% (37) | |
| NYU-ED Urgency | <0.001 | ||
| Emergent | 67.8% (6449) | 72.5% (1313) | |
| Non-emergent | 32.2% (3064) | 27.5% (499) |
Abbreviations: EMS, Emergency Medical Services; ESI, Emergency Severity Index; PICU, Pediatric Intensive Care Unit; OR, Operating Room.
Overall admission rate during COVID was 17.4% with a relative risk of a patient being admitted 1.31 (CI95%: 1.21–1.41) compared to prior years, though this still equates to an absolute reduction in admissions by 57%. Of those admitted, there was not a statistically significant difference in the percentage of patients requiring ICU admissions (ICU: COVID 16.9% vs Pre-COVID 19.4%, Medical/Surgical units: COVID 83.1% vs Pre-COVID 80.6%, p = 0.17).
Twenty-seven patients were given a diagnosis code for COVID-19 and recoded as earlier described. Table 3 displays the incidences of several pre-selected diagnoses, with some incidences disproportionately lower than the 56.1% decrease in overall visits. This was particularly true for generally low-acuity complaints including non-specific chest pain (−72%, p = 0.031), headaches (−79%, p < 0.001), minor injuries (−73%, p < 0.001), and nausea/vomiting/diarrhea (−76%, p < 0.001). The largest decrease was for maltreatment and abuse (−89%, p = 0.01). Visits for suicidal ideation, suicide attempt or self-harm increased by 100% (p < 0.001) despite overall visits for psychiatric disorders decreasing by 64% (p = 0.015).
Table 3.
Visits per 2-month study period by diagnosis
| Diagnosis group(s) | Pre-COVID (naverage) | COVID (n) | Relative change | P-value |
|---|---|---|---|---|
| All diagnoses | 9256 | 4068 | −56% | n/a |
| Injuries, severea | 549 | 318 | −42% | <0.001 |
| Injuries, minorb | 677 | 181 | −73% | <0.001 |
| Abdominal pain | 550 | 196 | −64% | 0.005 |
| Nausea, vomiting, diarrheac,e | 760 | 184 | −76% | <0.001 |
| Appendicitis | 80 | 85 | +6.3% | <0.001 |
| Asthma | 368 | 103 | −72% | <0.001 |
| Foreign body | 86 | 62 | −28% | 0.001 |
| Otitis media | 194 | 66 | −66% | 0.051 |
| Urinary tract infections | 103 | 48 | −53% | 0.74 |
| Headache, including migraine | 155 | 32 | −79% | <0.001 |
| Non-specific chest pain | 93 | 26 | −72% | 0.031 |
| Convulsions or epilepsy | 167 | 89 | −47% | 0.10 |
| Suicidal ideation/attempt or self-harm | 11 | 22 | +100% | <0.001 |
| Psychiatric disordersd,e | 497 | 180 | −64% | 0.015 |
| Poisoning by drugs | 21 | 14 | −33% | 0.15 |
| Hemolytic jaundice and perinatal jaundice | 27 | 22 | −19% | 0.011 |
| Diabetes mellitus with complication | 16 | 13 | −19% | 0.046 |
| Burns | 15 | 11 | −27% | 0.12 |
| Maltreatment/abuse | 28 | 3 | −89% | 0.01 |
Includes fractures, open wounds and lacerations.
Includes contusions, superficial injuries, concussions, sprains and strains, musculoskeletal pain, and low back pain.
Includes nausea and vomiting, non-infectious gastroenteritis, and intestinal infection.
Includes anxiety disorders, bipolar disorders, depressive disorders, conduct disorders, mood disorders, schizophrenia spectrum disorders, psychotic disorders, and trauma related disorders.
Not a routine CCSR grouping.
4. Discussion
During prior coronavirus epidemics (e.g., SARS, MERS) decreased pediatric ED visits were believed to be a result of the low pediatric disease burden and the perceived risk of accessing healthcare during a public health crisis [6,25,26]. The U.S. has not experienced such a significant public health state of emergency prior to the COVID-19 pandemic. In NYC, the pandemic uniquely compounded the reduced need for medical evaluations due to milder pediatric disease [[27], [28], [29]], the perceived risk of exposure to the virus by presenting to an ED, hesitancy to utilize limited medical resources, and the comprehensive restrictions set by the “NY on PAUSE” order. In the course of our study period, there was a 56% decrease in average daily volume as compared to prior years, within the range of the published literature to date [[13], [14], [15], [16]].
As the pandemic continues, the focus has been placed on how pediatric ED's can best reallocate resources while also strategizing for a future pandemic [16,30]. Acuity and urgency are key factors. Similar to other sites, the early months of the pandemic in NYC saw acuity rise. The proportion of ESI 1 and 2 visits increased by 24% and admission rates increased by 31%. As ESI does not reflect final diagnoses, we also utilized the NYU-ED algorithm to evaluate how urgently patients required an ED visit and found the number of visits that did not require emergent medical evaluation decreased by 14.6%.
To be prepared, pediatric ED's monitor patterns of acuity, but also anticipate trends in diagnoses. Because children were confined home for much of the early pandemic, we expected increases in certain diagnoses such as accidental ingestions, burns, and foreign bodies. Though these visits did not increase as hypothesized, they did not drop nearly as much as the overall ED volume.
As predicted, low acuity complaints such as chest pain, headache, minor injuries, and nausea/vomiting/diarrhea decreased substantially. Interestingly, the diagnosis of abdominal pain considerably decreased while appendicitis did not. Therefore, children presenting with undifferentiated abdominal pain were more likely to have a true appendicitis.
One dramatic and concerning change in presentations is the 89% decrease in primary diagnoses for child abuse or maltreatment. This pattern has yet to be described elsewhere in the literature and unmistakably should not be affected by changes in ED volume alone. Indeed, during a similar time period, NYC's Administration for Children's Services received 51% fewer reports of neglect or abuse [31]. Though the cause is likely multifactorial, it is predominantly attributable to children's lack of exposure to mandated reporters, rather than such a dramatic decrease in incidences of abuse and neglect [32,33]. Data on this population and potentially missed sentinel events will need to be followed closely as the pandemic continues. Public health agencies must keep a heightened awareness of this trend to drive novel methods for intervening and monitoring children early in pandemics or crises.
An additional concerning discovery is the doubling of visits for suicidal ideation, suicide attempts, or self-injury. Though comparatively small in absolute numbers, the 100% relative increase is in stark contrast to the considerable decrease in overall behavioral health visits seen in our ED and in others' [15,19]. Children across the country are socializing less and enduring new pandemic-related stressors on their families. We postulate our unique finding of increased suicidality and self-harm is in-part a consequence of the relatively higher media attention, severity of stressors such as parental job loss, and high prevalence of COVID-19 in the NYC area during the study period. For reference, by the end of July 2020, 1 in 520 children in Queens experienced the death of a parent or caregiver to COVID-19, more than any other county in NYS [34]. In addition, access to mental health services in NYC communities was severely restricted, particularly for those who receive school-based services [35]. As many telehealth opportunities had not yet been initiated, this meant removing preventative and crisis management options for the most at-risk children. The charts of our suicidal patients included quotes such as “having stressors with current pandemic situation and has not been able to see therapist” as well as “feeling anxious about online schoolwork since school has been cancelled.”
Our findings are consistent with literature examining children in China [36] and the Netherlands [37] during the COVID-19 pandemic, quarantined individuals during the 2003 Toronto SARS epidemic [38], and individuals in NYS following the 9/11 terrorist attacks [39]: proximity to a pandemic or event epicenter and relationships with people afflicted by an event are associated with higher behavioral health concerns and ED utilization for behavioral health symptoms. These patterns suggest that as social restrictions and disease prevalence rise during an epidemic, healthcare systems and mental health providers should seek out their most high-risk patients to ensure continuity and resource availability, whether through telemedicine or behavioral health urgent care centers.
This study faces many of the common limitations of a retrospective review including dependence on data collection systems that may have missing or incorrect information. Additionally, the single-center nature of the study limits generalizability; though our broader findings of decreased visits and higher acuity reflect national patterns and our more granular results highlight the unique severity of restrictions and disease prevalence initial epicenters may face during a pandemic. Unique to this study is the inclusion of the NYU-ED Algorithm which, though previously validated [40] and utilized in the pediatric literature [41], does have inherent limitations in excluding particular diagnoses. However, as our study compares findings from year-to-year, the relative change is more meaningful than the absolute findings of one year's numbers.
Timing of the study must also be considered. As Fig. 1 displays, patient volume was higher during the earliest weeks of the pandemic, thus potentially skewing our results towards earlier trends. The COVID study period also preceded the surge of patients in NYS with Multisystem Inflammatory Syndrome of Childhood (MIS-C) [42] who would likely increase the acuity and illness burden in the ED.
5. Conclusions
During the early months of the COVID-19 pandemic in NYC, our pediatric ED saw unprecedented decreases in volume. However, the resulting patient population seeking ED care was of higher acuity, more likely to warrant emergent evaluation, and more likely to require hospitalization. As healthcare systems develop resource strategies for the current and potential future pandemics, community outreach and vigilance should target the most vulnerable pediatric patients, particularly those at high risk for self-harm or abuse who have been disproportionately affected.
Disclosure
The authors declare no conflicts of interest.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Declaration of Competing Interest
None.
References
- 1.Hasan Z., Narasimhan M. Preparing for the COVID-19 pandemic: our experience in New York. Chest. 2020;157(6):1420–1422. doi: 10.1016/j.chest.2020.03.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Flores S., Gavin N., Romney M.L., Tedeschi C., Olsen E., Heravian A., et al. COVID-19: New York City pandemic notes from the first 30 days. Am J Emerg Med. 2020;38(7):1534–1535. doi: 10.1016/j.ajem.2020.04.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ammar A., Stock A.D., Holland R., Gelfand Y., Altschul D. Managing a specialty service during the COVID-19 crisis: lessons from a New York City health system. Acad Med. 2020 doi: 10.1097/ACM.0000000000003440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Konda S.R., Dankert J.F., Merkow D., Lin C.C., Kaplan D.J., Haskel J.D., et al. COVID-19 response in the global epicenter: converting a New York City level 1 orthopedic trauma service into a hybrid orthopedic and medicine COVID-19 management team. J Orthop Trauma. 2020;34(8):411–417. doi: 10.1097/BOT.0000000000001792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Philips K., Uong A., Buckenmyer T., Cabana M.D., Hsu D., Katyal C., et al. Rapid implementation of an adult coronavirus disease 2019 unit in a Children’s hospital. J Pediatr. 2020;222:22–27. doi: 10.1016/j.jpeds.2020.04.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Boutis K., Stephens D., Lam K., Ungar W.J., Schuh S. The impact of SARS on a tertiary care pediatric emergency department. CMAJ. 2004;171(11):1353–1358. doi: 10.1503/cmaj.1031257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Heiber M., Lou W.Y. Effect of the SARS outbreak on visits to a community hospital emergency department. CJEM. 2006;8(5):323–328. doi: 10.1017/s148180350001397x. [DOI] [PubMed] [Google Scholar]
- 8.Lee S.Y., Khang Y.H., Lim H.K. Impact of the 2015 Middle East respiratory syndrome outbreak on emergency care utilization and mortality in South Korea. Yonsei Med J. 2019;60(8):796–803. doi: 10.3349/ymj.2019.60.8.796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lazzerini M., Barbi E., Apicella A., Marchetti F., Cardinale F., Trobia G. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health. 2020 doi: 10.1016/S2352-4642(20)30108-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Clavenna A., Nardelli S., Sala D., Fontana M., Biondi A., Bonati M. Impact of COVID-19 on the pattern of access to a pediatric emergency Department in the Lombardy Region. Italy Pediatr Emerg Care. 2020 doi: 10.1097/PEC.0000000000002232. [DOI] [PubMed] [Google Scholar]
- 11.Isba R., Edge R., Jenner R., Broughton E., Francis N., Butler J. Where have all the children gone? Decreases in paediatric emergency department attendances at the start of the COVID-19 pandemic of 2020. Arch Dis Child. 2020;105(7):704. doi: 10.1136/archdischild-2020-319385. [DOI] [PubMed] [Google Scholar]
- 12.Levine D.A., Fraymovich S., Platt S.L. Where have all the children gone? Pediatric perspectives on COVID-19 in New York City. Ann Emerg Med. 2020;76(1):109–110. doi: 10.1016/j.annemergmed.2020.04.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartnett K.P., Kite-Powell A., DeVies J., Coletta M.A., Boehmer T.K., Adjemian J., et al. Impact of the COVID-19 Pandemic on Emergency Department Visits - United States, January 1, 2019-May 30, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(23):699–704. doi: 10.15585/mmwr.mm6923e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Pines J.M., Zocchi M.S., Black B.S., Carlson J.N., Celedon P., Moghtaderi A., et al. Characterizing pediatric emergency department visits during the COVID-19 pandemic. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.11.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chaiyachati B.H., Agawu A., Zorc J.J., Balamuth F. Trends in pediatric emergency department utilization after institution of coronavirus Disease-19 mandatory social distancing. J Pediatr. 2020 doi: 10.1016/j.jpeds.2020.07.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Even L., Lipshaw M.J., Wilson P.M., Dean P., Kerrey B.T., Vukovic A.A. Pediatric emergency department volumes and throughput during the COVID-19 pandemic. Am J Emerg Med. 2020 doi: 10.1016/j.ajem.2020.09.074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Murtagh Kurowski E., Byczkowski T., Grupp-Phelan J.M. Comparison of emergency care delivered to children and young adults with complex chronic conditions between pediatric and general emergency departments. Acad Emerg Med. 2014;21(7):778–784. doi: 10.1111/acem.12412. [DOI] [PubMed] [Google Scholar]
- 18.Pines J.M. Freestanding emergency department visits and disasters: the case of hurricane Harvey. Am J Emerg Med. 2018;36(8):1513–1515. doi: 10.1016/j.ajem.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 19.Sheridan D.C., Cloutier R., Johnson K., Marshall R. Where have all the emergency paediatric mental health patients gone during COVID-19? Acta Paediatr. 2020 doi: 10.1111/apa.15537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Emergency Severity Index (ESI): A Triage Tool for Emergency Departments Rockville, MD: Agency for Healthcare Research and Quality. 2018. https://www.ahrq.gov/professionals/systems/hospital/esi/index.html [accessed April 27]
- 21.Billings J. NYU ED Algorithm New York, NY: NYU Center for Health and Public Service Research. https://wagner.nyu.edu/faculty/billings/nyued-background
- 22.Clinical Classifications Software Refined (CCSR) for ICD-10-CM Diagnoses v2020.2 Rockville, MD. Agency for Healthcare Research and Quality; 2020. https://www.hcup-us.ahrq.gov/toolssoftware/ccsr/ccs_refined.jsp [accessed April 14] [Google Scholar]
- 23.Rosenberg E.S., Hall E.W., Rosenthal E.M., Maxted A.M., Gowie D.L., Dufort E.M., et al. Monitoring coronavirus disease 2019 (COVID-19) through trends in influenza-like illness, laboratory-confirmed influenza, and COVID-19—New York state, excluding New York City, 1 January 2020–12 April 2020. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Fagerland M.W. t-tests, non-parametric tests, and large studies--a paradox of statistical practice? BMC Med Res Methodol. 2012;12:78. doi: 10.1186/1471-2288-12-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stockman L.J., Massoudi M.S., Helfand R., Erdman D., Siwek A.M., Anderson L.J., et al. Severe acute respiratory syndrome in children. Pediatr Infect Dis J. 2007;26(1):68–74. doi: 10.1097/01.inf.0000247136.28950.41. [DOI] [PubMed] [Google Scholar]
- 26.Memish Z.A., Al-Tawfiq J.A., Assiri A., AlRabiah F.A., Al Hajjar S., Albarrak A., et al. Middle East respiratory syndrome coronavirus disease in children. Pediatr Infect Dis J. 2014;33(9):904–906. doi: 10.1097/INF.0000000000000325. [DOI] [PubMed] [Google Scholar]
- 27.Kim L., Whitaker M., O’Halloran A., Kambhampati A., Chai S.J., Reingold A., et al. Hospitalization rates and characteristics of Children Aged <18 years hospitalized with laboratory-confirmed COVID-19 - COVID-NET, 14 States, March 1–July 25, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(32):1081–1088. doi: 10.15585/mmwr.mm6932e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.CDC Covid-Response Team. Coronavirus Disease 2019 in Children - United States, February 12–April 2, 2020. MMWR Morb Mortal Wkly Rep. 2020;69(14):422–426. doi: 10.15585/mmwr.mm6914e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kainth M.K., Goenka P.K., Williamson K.A., Fishbein J.S., Subramony A., Schleien C., et al. Early experience of COVID-19 in a US Children’ Hospital. Pediatrics. 2020 doi: 10.1542/peds.2020-003186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Walker D.M., Tolentino V.R. COVID-19: the effects on the practice of pediatric emergency medicine. Pediatr Emerg Med Pract. 2020;17(Suppl 6–3):1–15. https://www.ncbi.nlm.nih.gov/pubmed/32549038 [PubMed] [Google Scholar]
- 31.Stewart N. 2020. Child abuse cases drop 51 percent. The Authorities Are Very Worried The New York Times June 9.https://www.nytimes.com/2020/06/09/nyregion/coronavirus-nyc-child-abuse.html [Google Scholar]
- 32.U.S. Department of Health & Human Services; Administration for Children and Families; Administration on Children Youth and Family, Children’s Bureau 2018Child Maltreatment. 2020 https://www.acf.hhs.gov/cb/research-data-technology/statistics-research/child-maltreatment [Google Scholar]
- 33.Welch M., Haskins R. April 30, 2020. What COVID-19 means for America’s child welfare system. Brookings Institution.https://www.brookings.edu/research/what-covid-19-means-for-americas-child-welfare-system/ [Google Scholar]
- 34.Brundage S.C., Ramos-Callan K. 2020. COVID-19 ripple effect: the impact of COVID-19 on children in New York State. United Hospital Fund September 30.https://uhfnyc.org/publications/publication/covid-19-ripple-effect-impact-covid-19-children-new-york-state/ [Google Scholar]
- 35.Torres-Pagan L., Terepka A. School-based health centers during academic disruption: challenges and opportunity in urban mental health. Psychol Trauma. 2020;12(S1) doi: 10.1037/tra0000611. S276-S8. [DOI] [PubMed] [Google Scholar]
- 36.Jiao W.Y., Wang L.N., Liu J., Fang S.F., Jiao F.Y., Pettoello-Mantovani M., et al. Behavioral and emotional disorders in children during the COVID-19 epidemic. J Pediatr. 2020;221:264–266. doi: 10.1016/j.jpeds.2020.03.013. e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Luijten M.A.J., van Muilekom M.M., Teela L., van Oers H.A., Terwee C.B., Zijlmans J., et al. The impact of lockdown during the COVID-19 pandemic on mental and social health of children and adolescents. medRxiv. 2020 doi: 10.1101/2020.11.02.20224667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cava M.A., Fay K.E., Beanlands H.J., McCay E.A., Wignall R. The experience of quarantine for individuals affected by SARS in Toronto. Public Health Nurs. 2005;22(5):398–406. doi: 10.1111/j.0737-1209.2005.220504.x. [DOI] [PubMed] [Google Scholar]
- 39.DiMaggio C., Galea S., Richardson L.D. Emergency department visits for behavioral and mental health care after a terrorist attack. Ann Emerg Med. 2007;50(3):327–334. doi: 10.1016/j.annemergmed.2006.10.021. [DOI] [PubMed] [Google Scholar]
- 40.Ballard D.W., Price M., Fung V., Brand R., Reed M.E., Fireman B., et al. Validation of an algorithm for categorizing the severity of hospital emergency department visits. Med Care. 2010;48(1):58–63. doi: 10.1097/MLR.0b013e3181bd49ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ben-Isaac E., Schrager S.M., Keefer M., Chen A.Y. National profile of nonemergent pediatric emergency department visits. Pediatrics. 2010;125(3):454–459. doi: 10.1542/peds.2009-0544. [DOI] [PubMed] [Google Scholar]
- 42.Capone C.A., Subramony A., Sweberg T., Schneider J., Shah S., Rubin L., et al. Characteristics, cardiac involvement, and outcomes of multisystem inflammatory syndrome of childhood associated with severe acute respiratory syndrome coronavirus 2 infection. J Pediatr. 2020;224:141–145. doi: 10.1016/j.jpeds.2020.06.044. [DOI] [PMC free article] [PubMed] [Google Scholar]