Abstract
IgLON5 antibodies are typically associated with the insidious onset of sleep disorder, parasomnia, gait disturbance and abnormal movements, with variable response to immunosuppressive therapy. We describe a case of a 50-year-old man who presented with acute speech difficulties, headache and focal seizures followed by well-formed visual hallucinations, and later, musical hallucinations of mainstream popular music. MRI of the brain demonstrated right temporal lobe changes with corresponding epileptiform activity seen on electroencephalogram. Subsequently, IgLON5 antibodies were detected in the serum. The patient was treated with anticonvulsants, as well as azathioprine with a tapering oral prednisone course with a complete resolution of the symptoms. Our case demonstrates an unusual presentation of the rare but increasingly described anti-IgLON5 disease, with musical hallucinations. The case highlights the variable and evolving clinical phenotypes that can be seen in autoimmune central nervous system disorders.
Keywords: immunology, neurology
Background
Anti-IgLON5 disease is a rare but increasingly described clinical entity characterised by the detection of antibodies against the extracellular domain of the central nervous system (CNS) cell adhesion molecule, IgLON5. Existing literature on anti-IgLON5 disease reports an insidious onset of clinical manifestations including sleep disorders with parasomnia, bulbar symptoms, gait instability and abnormal movements.1 The true prevalence is unknown, and except for an association with certain human leucocyte antigen (HLA) alleles, no other risk factors have been identified. Unlike other autoantibody-mediated CNS disorders, most reported cases have typically had variable responses to immunomodulatory therapy with progressive decline despite treatment and the described histopathological findings resemble a tauopathy more in keeping with a neurodegenerative, rather than autoimmune process.2 We describe an atypical case of anti-IgLON5 disease characterised by acute onset musical hallucinations, the first report of such a presentation, which responded promptly to immunosuppressive therapy.
Case presentation
A 50-year-old, right-handed man, born in the Cook Islands, initially presented with sudden onset word-finding difficulties and a frontal headache. His medical history was significant for prior bariatric surgery, hypertension and gout, but he had no known neurological conditions or relevant family history.
Over the course of several days, the patient developed macropsia and dyschromatopsia with abnormal perceived distortions and discolouration of people’s faces, as well as other poorly formed visual hallucinations of various shimmering colours. Concurrently, brief episodes of impaired awareness and aphasia lasting 1 to 2 minutes were noted and electroencephalogram (EEG) demonstrated right temporal lobe discharges consistent with seizure activity.
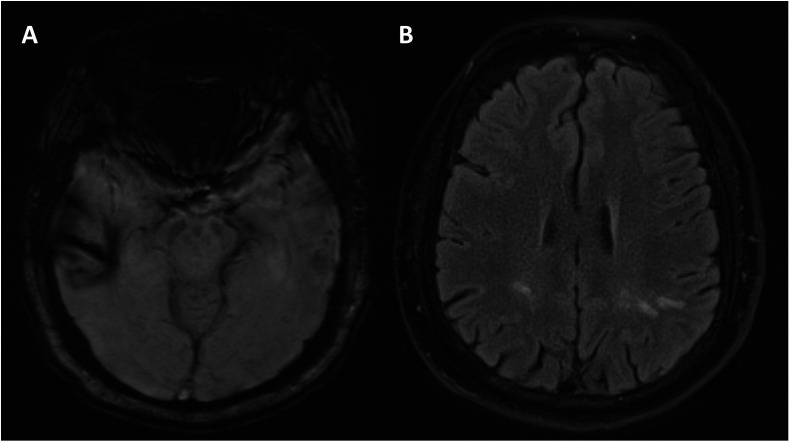
Blood investigations revealed no significant biochemical or metabolic derangements and inflammatory markers, including C-reactive protein and erythrocyte sedimentation rate, were within normal limits. MRI of the brain demonstrated haemosiderin deposition in the right temporal lobe possibly consistent with previous traumatic injury and there were patchy foci of T2 hyperintensity in the supratentorial white matter but no evidence of acute ischaemia (shown in figure 1). Cerebrospinal fluid (CSF) sampling showed no significant pleocytosis with 2×106 white cells per litre, normal glucose and protein and no growth on culture. IgLON-5 autoantibodies were detected on serum but not in CSF.
Figure 1.
Representative axial susceptibility-weighted imaging (SWI) MRI image demonstrating right temporal lobe changes consistent with haemosiderin deposition (A) and T2-weighted MRI image demonstrating patchy supratentorial white matter changes (B).
The patient was initially treated with anticonvulsants (sodium valproate, 1.5 g two times per day) with rapid resolution of seizure activity and visual hallucinations. However, he then developed distinct and continuous musical hallucinations whereby he would incessantly hear popular songs as if they were playing on the radio. These were well-formed and the patient was able to name the title and artist of each song that he was hearing; his wife kept notation of every song (online supplemental table 1). Additionally, he hallucinated that his telephone was ringing on several occasions. He did not find the hallucinations distressing or intrusive. There were no other forms of auditory hallucination nor further visual hallucinations, illusions or misperceptions.
bcr-2020-236963supp001.pdf (106.6KB, pdf)
Differential diagnosis
Several differential diagnoses were considered throughout the patient’s presentation. Cerebrovascular stroke was considered with the initial presentation of word-finding difficulties and acute onset of symptoms particularly in light of his elevated cardiovascular risk. However, ischaemia was not evident on MRI imaging and the subsequent development of hallucinations was not in keeping with a vascular phenomenon.
The right temporal haemosiderin deposition seen on MRI appeared consistent with previous traumatic injury but this was not evident on history and would not solely account for the patient’s presentation. While the discharges on EEG were in the same region, this is unlikely to account for the observed aphasia in a right-handed individual, and the musical hallucinations developed after resolution of the EEG changes with anticonvulsant therapy. The musical hallucinations were continuous, not accompanied by impaired awareness, and three additional EEGs performed while the patient was actively experiencing these were all normal making an epileptic cause unlikely.
Blood and CSF investigations showed no evidence of a toxic, metabolic or infective cause for the presentation while MRI brain showed no other space occupying lesions to account for his symptoms.
Treatment
Autoimmune encephalitis, with IgLON5 antibodies was diagnosed, and prednisone (60 mg/day) was initiated, with complete resolution of the patient’s musical hallucinations. Azathioprine (an amended dose of 25 mg/day was eventually selected due to concomitant allopurinol 300 mg/day) was commenced as immunosuppression to prophylax against relapse. Other treatments initiated included entecavir 0.5 mg daily as hepatitis B prophylaxis given serology consistent with previous exposure, and ivermectin as empiric treatment pre-immunosuppression for positive Strongyloides serology. CT scan of the chest, abdomen and pelvis and whole body positron emission tomography demonstrated no evidence of underlying malignancy.
Outcome and follow-up
Following the initial response to immunomodulatory therapy, the patient’s prednisone dose was gradually tapered over 3 months and azathioprine was continued. Erythrocyte 6-thioguanine nucleotide levels, measured on three occasions over the next 6 months, were all at levels associated with a significant immunosuppressive effect indicating appropriate azathioprine dosing. Ongoing clinical remission was maintained with no recurrence of seizure activity or hallucinations.
Discussion
Autoimmune CNS disorders mediated by pathogenic autoantibodies against plasma membrane targets have been increasingly described with the advent of modern diagnostic methods. The majority of these, such as anti-NMDA receptor disease, present with acute onset encephalitis characterised by mood and behavioural changes, cognitive dysfunction and seizures with rapid progression in the absence of treatment.3 In contrast, existing literature on anti-IgLON5 disease largely reports an insidious onset and prolonged course with distinct clinical manifestations including sleep disorders, bulbar symptoms, gait instability and abnormal movements.1
Our case of anti-IgLON5 disease describes an atypical rapid onset of symptoms and is the first report of musical hallucinations in association with IgLON5 antibodies. Hallucinations have been previously reported in anti-IgLON5 disease but these were uncommon, predominantly visual and associated with other neuropsychiatric features including delirium, depression or memory impairment4 which were not evident in our patient. Our patient’s presentation had several atypical features including an acute onset and the initial response of some symptoms to anti-epileptic therapy. Whilst other causes for our patient’s symptoms were considered, these were not evident on investigations, and the rapid improvement of the musical hallucinations with immunosuppressive therapy supports an immune-mediated cause. IgLON5 antibodies were detected in our patient’s serum but not CSF and a false positive serum antibody result is possible. The discrepancy between serum and CSF results is however consistent with subsets of patients in other anti-IgLON5 disease cohorts1 and current evidence suggests equal diagnostic sensitivity between serum and CSF testing.4
Initially reported cases of anti-IgLON5 disease had minimal responsiveness to immunomodulatory therapy and the observed tau deposition on histological specimens5 led to the hypothesis of a neurodegenerative process with the observed IgLON5 antibodies as a secondary phenomenon. The complete response to immunomodulatory therapy in our patient is in keeping with more recent case series of other successfully treated patients,4 6 that have responded to various treatment modalities including corticosteroids, intravenous immunoglobulin, plasmapheresis and traditional immunosuppressants including azathioprine. This response to therapy suggests that the IgLON5 antibodies may directly contribute to the pathogenesis of disease, rather than being an epiphenomenon. While biological models are limited, in vitro studies that have demonstrated IgG mediated internalisation of IgLON5 clusters from hippocampal neuronal cell surfaces,7 further supporting the possible role of a pathogenic antibody.
Musical hallucinations themselves are rare and have been most commonly described in the setting of auditory deprivation and psychiatric illness.8 More recently, musical hallucinations have been reported in anti-NMDA receptor encephalitis,9 as well as in the controversial diagnosis of ‘Hashimoto’s encephalopathy’,10 although the latter was prior to the modern diagnostic advent of neuronal surface autoantibodies. Neuroanatomically, the superior temporal sulcus has been suggested as a possible origin for musical hallucinations on functional imaging studies11 and it is unclear if the imaging findings in our patient were related or an ancillary finding.
In summary, our case demonstrates a previously undescribed clinical association between IgLON5 antibodies and musical hallucinations with a prompt response to immunosuppressive therapy. While we acknowledge the difficulties in confirmation of autoantibodies to novel cell surface receptors in seropositive disease with atypical features, and it is recognised that association does not necessarily equate to causation, the publication of these unusual associations may spur further research into fully elucidating the spectrum of newly described neuroimmunolgical disorders. Overall, this case highlights the heterogeneity in the features of emerging immune-mediated CNS disorders and the evolving clinical phenotype that is seen as more cases of these are found.
Learning points.
Autoantibody-mediated central nervous system disorders are increasing described and this case demonstrates the variable clinical symptoms with which they present.
Musical hallucinations are an uncommon presentation of autoimmune CNS disorders and organic causes in patients presenting with these should be considered.
Anti-IgLON5 disease can be rapidly responsive to immunomodulatory therapy, supporting a potential directly pathogenic role of the anti-IgLON5 antibody.
Footnotes
Contributors: AS contributed to the compilation of patient history, data collection and drafting of the manuscript for intellectual content; AM contributed to the compilation of patient history and data collection; NU contributed to the compilation of patient history, data collection and revised the manuscript for intellectual content. All authors read the final manuscript and approved its submission.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Gaig C, Graus F, Compta Y, et al. Clinical manifestations of the anti-IgLON5 disease. Neurology 2017;88:1736–43. 10.1212/WNL.0000000000003887 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Heidbreder A, Philipp K. Anti-IgLON 5 disease. Curr Treat Options Neurol 2018;20:29. 10.1007/s11940-018-0515-4 [DOI] [PubMed] [Google Scholar]
- 3.Lancaster E The diagnosis and treatment of autoimmune encephalitis. J Clin Neurol 2016;12:1–13. 10.3988/jcn.2016.12.1.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Honorat JA, Komorowski L, Josephs KA, et al. IgLON5 antibody: neurological accompaniments and outcomes in 20 patients. Neurol Neuroimmunol Neuroinflamm 2017;4:e385. 10.1212/NXI.0000000000000385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sabater L, Gaig C, Gelpi E, et al. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol 2014;13:575–86. 10.1016/S1474-4422(14)70051-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cabezudo-García P, Mena-Vázquez N, Estivill Torrús G, et al. Response to immunotherapy in anti-IgLON5 disease: a systematic review. Acta Neurol Scand 2020;141:263–70. 10.1111/ane.13207 [DOI] [PubMed] [Google Scholar]
- 7.Sabater L, Planagumà J, Dalmau J, et al. Cellular investigations with human antibodies associated with the anti-IgLON5 syndrome. J Neuroinflammation 2016;13:226. 10.1186/s12974-016-0689-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alvarez Perez P, Garcia-Antelo MJ, Rubio-Nazabal E. "Doctor, I hear music": a brief review about musical hallucinations. Open Neurol J 2017;11:11–14. 10.2174/1874205X01711010011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Heekin RD, Catalano MC, Frontera AT, et al. Anti-Nmda receptor encephalitis in a patient with previous psychosis and neurological abnormalities: a diagnostic challenge. Case Rep Psychiatry 2015;2015:1–4. 10.1155/2015/253891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Brusa L, Panella M, Koch G, et al. Hashimoto's encephalopathy presenting with musical hallucinosis. J Neurol 2003;250:627–8. 10.1007/s00415-003-1058-4 [DOI] [PubMed] [Google Scholar]
- 11.Bernardini F, Attademo L, Blackmon K, et al. Musical hallucinations: a brief review of functional neuroimaging findings. CNS Spectr 2017;22:397–403. 10.1017/S1092852916000870 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bcr-2020-236963supp001.pdf (106.6KB, pdf)