Description
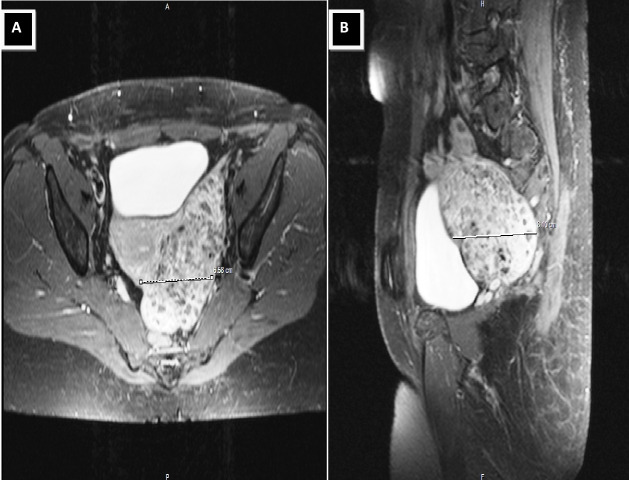
A 53-year-old postmenopausal woman presented to our emergency department with vaginal bleeding and pelvic pain. The woman had a significant medical history of hypothyroidism, and her surgical history included one caesarean section 16 years ago and appendectomy 30 years ago. Her family history was negative for malignant ovarian and breast cancer in first-degree relatives. Previous screening for cervical cancer had not been performed. Clinical and gynaecological examination presented no abnormalities, while blood analysis revealed haemoglobin of 13.3 g/L, 6.29 × 109/L leukocytes and 324 × 109/L platelets. Transvaginal ultrasonography was performed and revealed an enlarged uterus of 12×11×8 cm in size. In addition, an oval echogenic mass of 10×7 cm with a small cystic area was noticed in the pelvis near the cervix on the left side. Pelvis MRI was performed and confirmed an intramural International Federation of Gynecology and Obstetrics (FIGO)-type 6, homogenous and hypointense solid uterine tumour 11×8×6.5 cm with dilated blood vessels measuring up to 6 mm in diameter (figure 1A, B). Preoperatively, uterine leiomyosarcoma was suspected. However, MRI findings had no haemorrhage, necrosis or ill-defined margins. In addition, all tumour markers were within normal limits.
Figure 1.
(A, B) Pelvis MRI revealed an intramural, homogenous and hypointense solid uterine tumour 11×8×6.5 cm with dilated blood vessels.
The patient underwent total abdominal hysterectomy with bilateral salpingo-oophorectomy with resection of the mass as there was concern about the possibility of malignancy. She had no intraoperative or postoperative complications and was discharged home in healthy condition. Six months following the surgery, the patient has been symptom-free and has no evidence of recurrence. The final histopathology report of the soft tissue mass measuring 10.8×7.5×6.8 cm was suggestive of uterine leiomyoblastoma. Microscopic examination sections revealed no cellular atypia, mitosis or necrosis. In addition, no local infiltrating tendencies and vascular invasion were noted. Immunohistochemically, tumour cells were intensely positive for desmin, α-smooth muscle actin (αSMA), progesterone receptor and heavy caldesmon. However, the Ki-67 index was very low (1%).
Uterine leiomyoblastomas, currently referred to as epithelioid leiomyomas, clear cell type, comprise a rare subgroup of epithelioid leiomyomas.1–3 The macroscopic image of these tumours closely resembles that of typical leiomyomas in most cases. There has been, however, instances where the tumour displayed characteristics similar to leiomyosarcoma with poorly circumscribed margins, focal bleeding and areas of necrosis.1 Their size can vary from 1.5 cm to 16 cm, with a consistency that is soft in 70% and firm in 30% of the cases. Microscopically, epithelioid leiomyomas consist of sheets or groups of round or polygonal cells with eosinophilic or clear cytoplasm, which mainly contain cytolysosomes, glycogen aggregates and αSMA myofilaments.2 The tumour’s immunophenotype is distinct from typical epithelioid leiomyomas, as its cells are negative for desmin and h-caldesmon while positive for keratins and histone deacetylase 8—a marker of smooth muscle differentiation.4
The gold standard treatment of clear cell type epithelioid leiomyoma is identical to that of the typical leiomyoma and consists of total hysterectomy. Its prognosis, however, depends on the existence of tumour necrotic foci, atypia and mitoses per high-power field (HPF) under the microscope. Tumours without necrosis, atypia and less than five mitoses per HPF exhibit benign behaviour. Neoplasms that exhibit cytological atypia, regardless of degree, and five or more mitoses per 10 HPFs without tumour cell necrosis or five or more mitoses per 10 HPFs and tumour cell necrosis with cytological atypia are considered as malignant. Finally, neoplasms with one or more of the features such as 2–4 mitoses/10 HPF, size greater than 6 cm, necrosis and moderate or worse cytological atypia are classified as uterine smooth muscle tumours of unknown malignant potential and necessitate a careful follow-up.5 6
Learning points.
Uterine leiomyoblastomas are rare uterine tumours that are usually found incidentally on surgical operations because of other pathology.
Although uterine leiomyoblastomas are considered to be benign lesions, they should be viewed as neoplasms of low-grade malignancy, when histopathological characteristics such as abnormal mitoses, cellular and nuclear atypia, local infiltrating tendencies and vascular invasion appear.
Footnotes
Contributors: Contributors FM and IK had the idea of the study. FI, FM and K-MP prepared the manuscript. FM and IK critically revised the manuscript. All authors accepted the final version of the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Ip PPC, Tse KY, Tam KF. Uterine smooth muscle tumors other than the ordinary leiomyomas and leiomyosarcomas: a review of selected variants with emphasis on recent advances and unusual morphology that may cause concern for malignancy. Adv Anat Pathol 2010;17:91–112. 10.1097/PAP.0b013e3181cfb901 [DOI] [PubMed] [Google Scholar]
- 2.Mazur MT, Priest JB. Clear cell leiomyoma (leiomyoblastoma) of the uterus: ultrastructural observations. Ultrastruct Pathol 1986;10:249–55. 10.3109/01913128609032224 [DOI] [PubMed] [Google Scholar]
- 3.Watanabe K, Ogura G, Suzuki T. Leiomyoblastoma of the uterus: an immunohistochemical and electron microscopic study of distinctive tumours with immature smooth muscle cell differentiation mimicking fetal uterine myocytes. Histopathology 2003;42:379–86. 10.1046/j.1365-2559.2003.01602.x [DOI] [PubMed] [Google Scholar]
- 4.Devereaux KA, Schoolmeester JK. Smooth muscle tumors of the female genital tract. Surg Pathol Clin 2019;12:397–455. 10.1016/j.path.2019.02.004 [DOI] [PubMed] [Google Scholar]
- 5.Kumar SB, Akkem VJ, Donthi D, et al. . Epithelioid leiomyoma of uterus – a case report. J Evol Med Dent Sci 2013;2:2989–93. 10.14260/jemds/648 [DOI] [Google Scholar]
- 6.Kempson RL, Hendrickson MR. Smooth muscle, endometrial stromal, and mixed Müllerian tumors of the uterus. Mod Pathol 2000;13:328–42. 10.1038/modpathol.3880055 [DOI] [PubMed] [Google Scholar]